User login
AVAHO
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]


Will TP53-mutated AML respond to immunotherapy?
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
NATIONAL HARBOR, MD. – New research has shown increased immune infiltration in patients with TP53-mutated acute myeloid leukemia (AML).
Patients with TP53-mutated AML had higher levels of T-cell infiltration, immune checkpoint molecules, and interferon (IFN)–gamma signaling than patients with wild-type TP53.
These findings may indicate that patients with TP53-mutated AML will respond to T-cell targeting immunotherapies, but more investigation is needed, according to Sergio Rutella, MD, PhD, of Nottingham (England) Trent University.
Dr. Rutella described the findings at the annual meeting of the Society for Immunotherapy of Cancer.
He and his colleagues recently identified subgroups of AML, called “immune infiltrated” and “immune depleted,” that can predict chemotherapy resistance and response to flotetuzumab (ASH 2019, Abstract 460). However, the team has not determined the genetic drivers of immune infiltration in AML.*
With the current study, Dr. Rutella and his colleagues wanted to determine if TP53 mutations are associated with the AML immune milieu and see if TP53-mutated patients might benefit from immunotherapy.
Discovery cohort
The researchers first analyzed 147 patients with non-promyelocytic AML from the Cancer Genome Atlas. In total, 9% of these patients (n = 13) had TP53-mutated AML. The researchers assessed how 45 immune gene and biological activity signatures correlated with prognostic molecular lesions (TP53 mutations, FLT3-ITD, etc.) and clinical outcomes in this cohort.
The data showed that immune subtypes were associated with overall survival (OS). The median OS was 11.8 months in patients with immune-infiltrated AML, 16.4 months in patients with intermediate AML, and 25.8 months in patients with immune-depleted AML.
The inflammatory chemokine score (P = .011), IDO1 score (P = .027), IFN-gamma score (P = .036), and B7H3 score (P = .045) were all significantly associated with OS. In fact, these factors were all better predictors of OS than cytogenetic risk score (P = .049).
The IFN-gamma score, inflammatory chemokine score, and lymphoid score were all significantly higher in TP53-mutated patients than in patients with RUNX1 mutations, NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .05).
Likewise, the tumor inflammation signature score was significantly higher among TP53-mutated patients than among patients with NPM1 mutations, FLT3-ITD (with or without NPM1 mutations), and TET2/DNMT3A/ASXL1 mutations (P values ranging from less than .0001 to .01).
Validation cohort and bone marrow samples
The researchers also looked at data from a validation cohort, which consisted of 140 patients with non-promyelocytic AML in the Beat AML Master Trial. Twelve percent of these patients (n = 17) had TP53 mutations.
Data in this cohort showed that CD3G messenger RNA (mRNA) was significantly higher in TP53-mutated AML than in TP53-wild-type AML (P = .04). The same was true for CD8A mRNA (P = .0002) and GZMB mRNA (P = .0005).
Likewise, IFN-gamma mRNA (P = .0052), IFIT2 mRNA (P = .0064), and IFIT3 mRNA (P = .003) were all significantly higher in patients with TP53-mutated AML.
Lastly, the researchers analyzed gene expression profiles of bone marrow samples from patients with AML, 36 with mutated TP53 and 24 with wild-type TP53.
The team found that IFN-gamma–induced genes (IFNG and IRF1), markers of T-cell infiltration (CD8A and CD3G) and senescence (EOMES, KLRD1, and HRAS), immune checkpoint molecules (IDO1, LAG3, PDL1, and VISTA), effector function molecules (GZMB, GZMK, and GZMM), and proinflammatory cytokines (IL17A and TNF) were all significantly overexpressed in TP53-mutated AML.
Among the top overexpressed genes in TP53-mutated AML were genes associated with IFN signaling and inflammation pathways – IL-33, IL-6, IFN-gamma, OASL, RIPK2, TNFAIP3, CSF1, and PTGER4. The IL-17 and TNF signaling pathways were the most enriched pathways in TP53-mutated AML.
“Our analysis of primary bone marrow samples showed that TP53-mutated samples are enriched in IL-17, TNF, and IFN signaling molecules, and show higher levels of T-cell infiltrations and immune checkpoints relative to their wild-type counterparts,” Dr. Rutella said.
“The in silico analysis indicated that TP53-mutated cases will show higher levels of T-cell infiltration, immune checkpoints, and IFN-gamma signaling, compared with AML subgroups without risk-defining molecular lesions,” he added. “This is speculative. Whether TP53-mutated AML can be amenable to respond to T-cell targeting immunotherapies is still to be determined.”
Dr. Rutella reported research support from NanoString Technologies, MacroGenics, and Kura Oncology.
SOURCE: Rutella S et al. SITC 2019. Abstract O3.
*This article was updated on 11/19/2019.
REPORTING FROM SITC 2019
CAR T-cell ‘cocktail’ may overcome antigen escape relapse
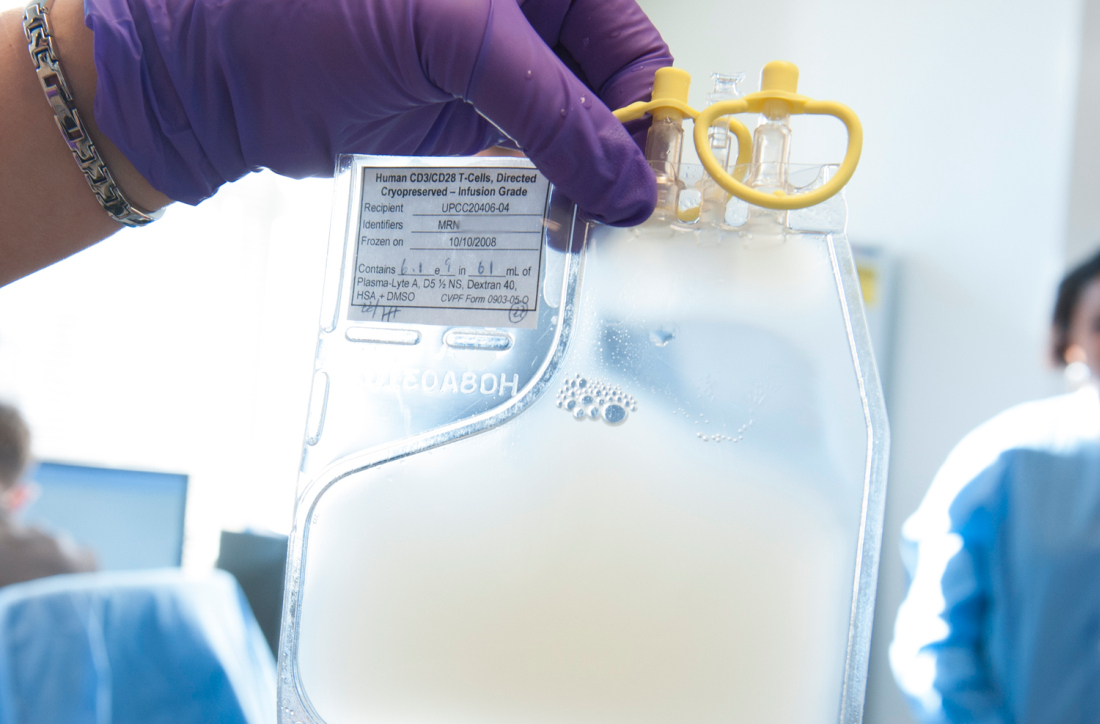
A chimeric antigen receptor (CAR) T-cell “cocktail” targeting both CD19 and CD22 could improve outcomes for patients with refractory or relapsed B-cell malignancies, according to investigators.
This dual approach, which appeared safe and effective, may be able to overcome antigen escape relapse, reported Na Wang, MD, of Huazhong University of Science and Technology in China, and colleagues.
The investigators tested this method in an open-label, single-arm pilot study involving 89 patients with refractory/relapsed B cell malignancies. Of these, 51 patients had B-cell acute lymphoblastic leukemia (B-ALL), while the remaining 38 had non-Hodgkin lymphoma (NHL). All patients had dual expression of CD19 and CD22 on malignant B cells, good performance status, and “essentially” normal organ function, the investigators reported in Blood.
Following lymphodepletion, patients were infused with CAR19 and CAR22 T cells, then evaluated for responses with imaging or bone marrow aspiration on a monthly basis for 6 months, then every 3 months thereafter.
After 30 days, most patients with ALL (96%) achieved a minimal residual disease-negative complete response or complete response with incomplete count recovery. After a median follow-up of 16.7 months, almost half of these responders relapsed (49%), median progression-free survival was 13.6 months, and overall survival was 31 months.
With a minimum follow-up of 3 months, half of the patients with NHL (50%) achieved complete responses, with the caveat that two patients who died of septic shock and severe cytokine release syndrome were excluded from this efficacy analysis. After a median follow-up of 14.4 months, in the NHL group, median progression-free survival was 9.9 months and overall survival was 18 months.
Across disease types, almost all patients (95.5%) experienced cytokine release syndrome, with more than three-quarters (77.6%) categorized as grade 1 or 2. CAR T cell-related encephalopathy syndrome (CRES) occurred in 13.5% of patients; most were low grade, apart from one case that was grade 4. In total, 12 patients died due to adverse events.
“The severe [adverse events] were mostly cytopenias and the most frequent fatal [adverse event] was lung infection, which was attributable in part to the high disease burden and heavy pretreatment of the enrolled patients,” the investigators wrote. “Nearly all the high-grade CRS and CRES were reversible and occurred in similar incidences as previously reported. Thus, the sequential infusion of CAR19/22 T-cell “cocktail” was an efficient and well-tolerated approach to circumvent antigen loss of CD19 or CD22.”
The investigators reported having no conflicts of interest.
SOURCE: Wang N et al. 2019 Oct 29. doi: 10.1182/blood.2019000017.
A chimeric antigen receptor (CAR) T-cell “cocktail” targeting both CD19 and CD22 could improve outcomes for patients with refractory or relapsed B-cell malignancies, according to investigators.
This dual approach, which appeared safe and effective, may be able to overcome antigen escape relapse, reported Na Wang, MD, of Huazhong University of Science and Technology in China, and colleagues.
The investigators tested this method in an open-label, single-arm pilot study involving 89 patients with refractory/relapsed B cell malignancies. Of these, 51 patients had B-cell acute lymphoblastic leukemia (B-ALL), while the remaining 38 had non-Hodgkin lymphoma (NHL). All patients had dual expression of CD19 and CD22 on malignant B cells, good performance status, and “essentially” normal organ function, the investigators reported in Blood.
Following lymphodepletion, patients were infused with CAR19 and CAR22 T cells, then evaluated for responses with imaging or bone marrow aspiration on a monthly basis for 6 months, then every 3 months thereafter.
After 30 days, most patients with ALL (96%) achieved a minimal residual disease-negative complete response or complete response with incomplete count recovery. After a median follow-up of 16.7 months, almost half of these responders relapsed (49%), median progression-free survival was 13.6 months, and overall survival was 31 months.
With a minimum follow-up of 3 months, half of the patients with NHL (50%) achieved complete responses, with the caveat that two patients who died of septic shock and severe cytokine release syndrome were excluded from this efficacy analysis. After a median follow-up of 14.4 months, in the NHL group, median progression-free survival was 9.9 months and overall survival was 18 months.
Across disease types, almost all patients (95.5%) experienced cytokine release syndrome, with more than three-quarters (77.6%) categorized as grade 1 or 2. CAR T cell-related encephalopathy syndrome (CRES) occurred in 13.5% of patients; most were low grade, apart from one case that was grade 4. In total, 12 patients died due to adverse events.
“The severe [adverse events] were mostly cytopenias and the most frequent fatal [adverse event] was lung infection, which was attributable in part to the high disease burden and heavy pretreatment of the enrolled patients,” the investigators wrote. “Nearly all the high-grade CRS and CRES were reversible and occurred in similar incidences as previously reported. Thus, the sequential infusion of CAR19/22 T-cell “cocktail” was an efficient and well-tolerated approach to circumvent antigen loss of CD19 or CD22.”
The investigators reported having no conflicts of interest.
SOURCE: Wang N et al. 2019 Oct 29. doi: 10.1182/blood.2019000017.
A chimeric antigen receptor (CAR) T-cell “cocktail” targeting both CD19 and CD22 could improve outcomes for patients with refractory or relapsed B-cell malignancies, according to investigators.
This dual approach, which appeared safe and effective, may be able to overcome antigen escape relapse, reported Na Wang, MD, of Huazhong University of Science and Technology in China, and colleagues.
The investigators tested this method in an open-label, single-arm pilot study involving 89 patients with refractory/relapsed B cell malignancies. Of these, 51 patients had B-cell acute lymphoblastic leukemia (B-ALL), while the remaining 38 had non-Hodgkin lymphoma (NHL). All patients had dual expression of CD19 and CD22 on malignant B cells, good performance status, and “essentially” normal organ function, the investigators reported in Blood.
Following lymphodepletion, patients were infused with CAR19 and CAR22 T cells, then evaluated for responses with imaging or bone marrow aspiration on a monthly basis for 6 months, then every 3 months thereafter.
After 30 days, most patients with ALL (96%) achieved a minimal residual disease-negative complete response or complete response with incomplete count recovery. After a median follow-up of 16.7 months, almost half of these responders relapsed (49%), median progression-free survival was 13.6 months, and overall survival was 31 months.
With a minimum follow-up of 3 months, half of the patients with NHL (50%) achieved complete responses, with the caveat that two patients who died of septic shock and severe cytokine release syndrome were excluded from this efficacy analysis. After a median follow-up of 14.4 months, in the NHL group, median progression-free survival was 9.9 months and overall survival was 18 months.
Across disease types, almost all patients (95.5%) experienced cytokine release syndrome, with more than three-quarters (77.6%) categorized as grade 1 or 2. CAR T cell-related encephalopathy syndrome (CRES) occurred in 13.5% of patients; most were low grade, apart from one case that was grade 4. In total, 12 patients died due to adverse events.
“The severe [adverse events] were mostly cytopenias and the most frequent fatal [adverse event] was lung infection, which was attributable in part to the high disease burden and heavy pretreatment of the enrolled patients,” the investigators wrote. “Nearly all the high-grade CRS and CRES were reversible and occurred in similar incidences as previously reported. Thus, the sequential infusion of CAR19/22 T-cell “cocktail” was an efficient and well-tolerated approach to circumvent antigen loss of CD19 or CD22.”
The investigators reported having no conflicts of interest.
SOURCE: Wang N et al. 2019 Oct 29. doi: 10.1182/blood.2019000017.
FROM BLOOD
Nivolumab-ipilimumab combo has ‘robust’ clinical benefit in sorafenib-treated HCC patients
BOSTON – The combination of nivolumab and ipilimumab provided a “robust” clinical benefit and had manageable hepatic adverse events in a phase 2 study of sorafenib-treated patients with advanced hepatocellular carcinoma (HCC), an investigator said at the annual meeting of the American Association for the Study of Liver Diseases.
Response rates for the combination treatment exceeded 30% in CheckMate 040, with median overall survival approaching 23 months in one arm of this randomized trial, said Bruno Sangro, MD, PhD, of Clinica Universidad de Navarra, Pamplona, Spain.
The combination had a manageable safety profile with no new safety signals, and most immune-mediated adverse events resolved, including hepatic events, Dr. Sango said in an oral abstract session.
“The favorable benefit/risk profile observed we believe warrants further investigation in patients with HCC,” Dr. Sangro said in his presentation to attendees, adding that a phase 3 study of the combination is already ongoing.
On Nov. 11, 2019, Bristol-Myers Squibb announced its application for nivolumab plus ipilimumab for previously treated advanced HCC had been accepted for priority review by the Food and Drug Administration, which had furthermore granted breakthrough therapy designation for that potential indication.
In September 2017, the FDA approved nivolumab as monotherapy for patients with HCC previously treated with sorafenib. That action was based on results from CheckMate 040 showing on overall response rate of 14% and a median overall survival of 15 months, Dr. Sangro said.
The combination of the programmed death–1 inhibitor nivolumab and the CTLA-4 inhibitor ipilimumab, which has shown durable responses in other tumor types, may promote synergistic immune activity in HCC through their distinct but complementary mechanisms, according to the investigator.
The first report on the combination of nivolumab plus ipilimumab in CheckMate 040, reported earlier this year at the annual meeting of the American Society of Clinical Oncology, indicated that the combination produced responses that were robust and durable.
Dr. Sangro reported data on 148 patients with advanced HCC previously treated with sorafenib randomized to one of three different dosing regimens with nivolumab plus ipilimumab.
Response rates ranged from 31% to 32% in the three arms, while one particular dosing regimen given every 3 weeks for four cycles had a median overall survival of 22.8 months.
“Just to give a perspective, let me remind you that patients receiving placebo post sorafenib in a number of phase 3 trials have very consistently shown median overall survivals of around 8 months,” Dr. Sangro told attendees.
Hepatic treatment-related adverse events of any grade reported within 30 days of the last dose were seen in 39% of patients in that arm, Dr. Sangro said.
Hepatic events thought to be immune mediated were typically managed with a short course of high-dose corticosteroids, according to Dr. Sangro, who said no patients rechallenged with treatment experienced a recurrence of the event.
Most of the hepatic adverse events occurred early, with a median time to onset of 5.6-8.1 weeks, he said, and most resolved at a median of 6.1-7.9 weeks.
In the ongoing phase 3 CheckMate 9DW study, patients with advanced HCC who are naive to systemic therapy are being randomized to the combination of nivolumab plus ipilimumab, or to the investigators’ choice of either sorafenib or lenvatinib, with a primary endpoint of overall survival, Dr. Sangro said.
The study was supported by Bristol-Myers Squibb and ONO Pharmaceutical. Dr. Sangro reported disclosures related to Adaptimmune, AstraZeneca, Bayer, Bristol-Myers Squibb, BTG, Merck, Onxeo, Sirtex Medical, Terumo, H3 Biomedicine, Ipsen, Lilly, Exelixis, Roche, and Ipsen.
SOURCE: Sangro B et al. The Liver Meeting 2019, Abstract 200.
BOSTON – The combination of nivolumab and ipilimumab provided a “robust” clinical benefit and had manageable hepatic adverse events in a phase 2 study of sorafenib-treated patients with advanced hepatocellular carcinoma (HCC), an investigator said at the annual meeting of the American Association for the Study of Liver Diseases.
Response rates for the combination treatment exceeded 30% in CheckMate 040, with median overall survival approaching 23 months in one arm of this randomized trial, said Bruno Sangro, MD, PhD, of Clinica Universidad de Navarra, Pamplona, Spain.
The combination had a manageable safety profile with no new safety signals, and most immune-mediated adverse events resolved, including hepatic events, Dr. Sango said in an oral abstract session.
“The favorable benefit/risk profile observed we believe warrants further investigation in patients with HCC,” Dr. Sangro said in his presentation to attendees, adding that a phase 3 study of the combination is already ongoing.
On Nov. 11, 2019, Bristol-Myers Squibb announced its application for nivolumab plus ipilimumab for previously treated advanced HCC had been accepted for priority review by the Food and Drug Administration, which had furthermore granted breakthrough therapy designation for that potential indication.
In September 2017, the FDA approved nivolumab as monotherapy for patients with HCC previously treated with sorafenib. That action was based on results from CheckMate 040 showing on overall response rate of 14% and a median overall survival of 15 months, Dr. Sangro said.
The combination of the programmed death–1 inhibitor nivolumab and the CTLA-4 inhibitor ipilimumab, which has shown durable responses in other tumor types, may promote synergistic immune activity in HCC through their distinct but complementary mechanisms, according to the investigator.
The first report on the combination of nivolumab plus ipilimumab in CheckMate 040, reported earlier this year at the annual meeting of the American Society of Clinical Oncology, indicated that the combination produced responses that were robust and durable.
Dr. Sangro reported data on 148 patients with advanced HCC previously treated with sorafenib randomized to one of three different dosing regimens with nivolumab plus ipilimumab.
Response rates ranged from 31% to 32% in the three arms, while one particular dosing regimen given every 3 weeks for four cycles had a median overall survival of 22.8 months.
“Just to give a perspective, let me remind you that patients receiving placebo post sorafenib in a number of phase 3 trials have very consistently shown median overall survivals of around 8 months,” Dr. Sangro told attendees.
Hepatic treatment-related adverse events of any grade reported within 30 days of the last dose were seen in 39% of patients in that arm, Dr. Sangro said.
Hepatic events thought to be immune mediated were typically managed with a short course of high-dose corticosteroids, according to Dr. Sangro, who said no patients rechallenged with treatment experienced a recurrence of the event.
Most of the hepatic adverse events occurred early, with a median time to onset of 5.6-8.1 weeks, he said, and most resolved at a median of 6.1-7.9 weeks.
In the ongoing phase 3 CheckMate 9DW study, patients with advanced HCC who are naive to systemic therapy are being randomized to the combination of nivolumab plus ipilimumab, or to the investigators’ choice of either sorafenib or lenvatinib, with a primary endpoint of overall survival, Dr. Sangro said.
The study was supported by Bristol-Myers Squibb and ONO Pharmaceutical. Dr. Sangro reported disclosures related to Adaptimmune, AstraZeneca, Bayer, Bristol-Myers Squibb, BTG, Merck, Onxeo, Sirtex Medical, Terumo, H3 Biomedicine, Ipsen, Lilly, Exelixis, Roche, and Ipsen.
SOURCE: Sangro B et al. The Liver Meeting 2019, Abstract 200.
BOSTON – The combination of nivolumab and ipilimumab provided a “robust” clinical benefit and had manageable hepatic adverse events in a phase 2 study of sorafenib-treated patients with advanced hepatocellular carcinoma (HCC), an investigator said at the annual meeting of the American Association for the Study of Liver Diseases.
Response rates for the combination treatment exceeded 30% in CheckMate 040, with median overall survival approaching 23 months in one arm of this randomized trial, said Bruno Sangro, MD, PhD, of Clinica Universidad de Navarra, Pamplona, Spain.
The combination had a manageable safety profile with no new safety signals, and most immune-mediated adverse events resolved, including hepatic events, Dr. Sango said in an oral abstract session.
“The favorable benefit/risk profile observed we believe warrants further investigation in patients with HCC,” Dr. Sangro said in his presentation to attendees, adding that a phase 3 study of the combination is already ongoing.
On Nov. 11, 2019, Bristol-Myers Squibb announced its application for nivolumab plus ipilimumab for previously treated advanced HCC had been accepted for priority review by the Food and Drug Administration, which had furthermore granted breakthrough therapy designation for that potential indication.
In September 2017, the FDA approved nivolumab as monotherapy for patients with HCC previously treated with sorafenib. That action was based on results from CheckMate 040 showing on overall response rate of 14% and a median overall survival of 15 months, Dr. Sangro said.
The combination of the programmed death–1 inhibitor nivolumab and the CTLA-4 inhibitor ipilimumab, which has shown durable responses in other tumor types, may promote synergistic immune activity in HCC through their distinct but complementary mechanisms, according to the investigator.
The first report on the combination of nivolumab plus ipilimumab in CheckMate 040, reported earlier this year at the annual meeting of the American Society of Clinical Oncology, indicated that the combination produced responses that were robust and durable.
Dr. Sangro reported data on 148 patients with advanced HCC previously treated with sorafenib randomized to one of three different dosing regimens with nivolumab plus ipilimumab.
Response rates ranged from 31% to 32% in the three arms, while one particular dosing regimen given every 3 weeks for four cycles had a median overall survival of 22.8 months.
“Just to give a perspective, let me remind you that patients receiving placebo post sorafenib in a number of phase 3 trials have very consistently shown median overall survivals of around 8 months,” Dr. Sangro told attendees.
Hepatic treatment-related adverse events of any grade reported within 30 days of the last dose were seen in 39% of patients in that arm, Dr. Sangro said.
Hepatic events thought to be immune mediated were typically managed with a short course of high-dose corticosteroids, according to Dr. Sangro, who said no patients rechallenged with treatment experienced a recurrence of the event.
Most of the hepatic adverse events occurred early, with a median time to onset of 5.6-8.1 weeks, he said, and most resolved at a median of 6.1-7.9 weeks.
In the ongoing phase 3 CheckMate 9DW study, patients with advanced HCC who are naive to systemic therapy are being randomized to the combination of nivolumab plus ipilimumab, or to the investigators’ choice of either sorafenib or lenvatinib, with a primary endpoint of overall survival, Dr. Sangro said.
The study was supported by Bristol-Myers Squibb and ONO Pharmaceutical. Dr. Sangro reported disclosures related to Adaptimmune, AstraZeneca, Bayer, Bristol-Myers Squibb, BTG, Merck, Onxeo, Sirtex Medical, Terumo, H3 Biomedicine, Ipsen, Lilly, Exelixis, Roche, and Ipsen.
SOURCE: Sangro B et al. The Liver Meeting 2019, Abstract 200.
REPORTING FROM THE LIVER MEETING 2019
Gene signature may help guide initial CLL treatment choice
A novel 17-gene expression signature may help guide the choice of initial treatment in patients with IGHV-unmutated chronic lymphocytic leukemia (CLL), according to findings of a retrospective dual cohort study.
“[Fludarabine, cyclophosphamide, and rituximab] was the first regimen to improve progression-free survival and overall survival in patients with chronic lymphocytic leukaemia, and has become a gold-standard chemoimmunotherapy regimen in physically fit patients,” wrote the investigators, who were led by Carmen D. Herling, MD, of the Center for Integrated Oncology, Cologne, Germany; and Kevin R. Coombes, PhD, of Ohio State University, Columbus.
While several studies demonstrate that young, fit patients with mutated IGHV gene and no high-risk cytogenetic abnormalities achieve durable remission with the FCR (fludarabine, cyclophosphamide, and rituximab) regimen, there have been no studies to identify if this is true for patients with unmutated IGHV gene, they reported in the Lancet Oncology.
The investigators performed transcriptional profiling using peripheral blood samples collected from two cohorts of patients with CLL who were treated with frontline FCR.
The discovery and training cohort consisted of 101 patients (65% with IGHV-unmutated disease) treated at the MD Anderson Cancer Center who had a median follow-up of about 12 years. The validation cohort consisted of 109 patients with IGHV-unmutated disease treated on the German CLL8 single-arm trial who had a median follow-up of about 6 years.
A total of 1,136 genes showed a significant univariate association with time to progression. Ultimately, 17 of these genes – most of them involved in purine metabolism and oxidative phosphorylation – were included in the expression signature.
Among patients with IGHV-unmutated CLL, the 17-gene signature discriminated between two groups having differing time to progression after their frontline FCR chemoimmunotherapy: an unfavorable prognosis group and an intermediate prognosis group.
The unfavorable prognosis group had a significantly higher relative risk of progression in both the discovery/training cohort (hazard ratio, 3.83; P less than .0001) and the validation cohort (HR, 1.90; P = .008). In the validation cohort, the median time to progression was 39 months among patients with a signature-defined unfavorable prognosis, compared with 59 months among patients with a signature-defined intermediate prognosis.
“We would recommend testing the value of the 17-gene signature in a prospective study that compares FCR treatment with alternative therapies, such as ibrutinib, as part of a randomised clinical trial,” the investigators wrote.
Dr. Herling reported financial disclosures related to Hoffmann-La Roche, and Dr. Coombes reported grants from the National Institutes of Health. The study was funded by the Chronic Lymphocytic Leukaemia Global Research Foundation and the National Institutes of Health/National Cancer Institute.
SOURCE: Herling CD et al. Lancet Oncol. 2019;20(11):1576-86.
A novel 17-gene expression signature may help guide the choice of initial treatment in patients with IGHV-unmutated chronic lymphocytic leukemia (CLL), according to findings of a retrospective dual cohort study.
“[Fludarabine, cyclophosphamide, and rituximab] was the first regimen to improve progression-free survival and overall survival in patients with chronic lymphocytic leukaemia, and has become a gold-standard chemoimmunotherapy regimen in physically fit patients,” wrote the investigators, who were led by Carmen D. Herling, MD, of the Center for Integrated Oncology, Cologne, Germany; and Kevin R. Coombes, PhD, of Ohio State University, Columbus.
While several studies demonstrate that young, fit patients with mutated IGHV gene and no high-risk cytogenetic abnormalities achieve durable remission with the FCR (fludarabine, cyclophosphamide, and rituximab) regimen, there have been no studies to identify if this is true for patients with unmutated IGHV gene, they reported in the Lancet Oncology.
The investigators performed transcriptional profiling using peripheral blood samples collected from two cohorts of patients with CLL who were treated with frontline FCR.
The discovery and training cohort consisted of 101 patients (65% with IGHV-unmutated disease) treated at the MD Anderson Cancer Center who had a median follow-up of about 12 years. The validation cohort consisted of 109 patients with IGHV-unmutated disease treated on the German CLL8 single-arm trial who had a median follow-up of about 6 years.
A total of 1,136 genes showed a significant univariate association with time to progression. Ultimately, 17 of these genes – most of them involved in purine metabolism and oxidative phosphorylation – were included in the expression signature.
Among patients with IGHV-unmutated CLL, the 17-gene signature discriminated between two groups having differing time to progression after their frontline FCR chemoimmunotherapy: an unfavorable prognosis group and an intermediate prognosis group.
The unfavorable prognosis group had a significantly higher relative risk of progression in both the discovery/training cohort (hazard ratio, 3.83; P less than .0001) and the validation cohort (HR, 1.90; P = .008). In the validation cohort, the median time to progression was 39 months among patients with a signature-defined unfavorable prognosis, compared with 59 months among patients with a signature-defined intermediate prognosis.
“We would recommend testing the value of the 17-gene signature in a prospective study that compares FCR treatment with alternative therapies, such as ibrutinib, as part of a randomised clinical trial,” the investigators wrote.
Dr. Herling reported financial disclosures related to Hoffmann-La Roche, and Dr. Coombes reported grants from the National Institutes of Health. The study was funded by the Chronic Lymphocytic Leukaemia Global Research Foundation and the National Institutes of Health/National Cancer Institute.
SOURCE: Herling CD et al. Lancet Oncol. 2019;20(11):1576-86.
A novel 17-gene expression signature may help guide the choice of initial treatment in patients with IGHV-unmutated chronic lymphocytic leukemia (CLL), according to findings of a retrospective dual cohort study.
“[Fludarabine, cyclophosphamide, and rituximab] was the first regimen to improve progression-free survival and overall survival in patients with chronic lymphocytic leukaemia, and has become a gold-standard chemoimmunotherapy regimen in physically fit patients,” wrote the investigators, who were led by Carmen D. Herling, MD, of the Center for Integrated Oncology, Cologne, Germany; and Kevin R. Coombes, PhD, of Ohio State University, Columbus.
While several studies demonstrate that young, fit patients with mutated IGHV gene and no high-risk cytogenetic abnormalities achieve durable remission with the FCR (fludarabine, cyclophosphamide, and rituximab) regimen, there have been no studies to identify if this is true for patients with unmutated IGHV gene, they reported in the Lancet Oncology.
The investigators performed transcriptional profiling using peripheral blood samples collected from two cohorts of patients with CLL who were treated with frontline FCR.
The discovery and training cohort consisted of 101 patients (65% with IGHV-unmutated disease) treated at the MD Anderson Cancer Center who had a median follow-up of about 12 years. The validation cohort consisted of 109 patients with IGHV-unmutated disease treated on the German CLL8 single-arm trial who had a median follow-up of about 6 years.
A total of 1,136 genes showed a significant univariate association with time to progression. Ultimately, 17 of these genes – most of them involved in purine metabolism and oxidative phosphorylation – were included in the expression signature.
Among patients with IGHV-unmutated CLL, the 17-gene signature discriminated between two groups having differing time to progression after their frontline FCR chemoimmunotherapy: an unfavorable prognosis group and an intermediate prognosis group.
The unfavorable prognosis group had a significantly higher relative risk of progression in both the discovery/training cohort (hazard ratio, 3.83; P less than .0001) and the validation cohort (HR, 1.90; P = .008). In the validation cohort, the median time to progression was 39 months among patients with a signature-defined unfavorable prognosis, compared with 59 months among patients with a signature-defined intermediate prognosis.
“We would recommend testing the value of the 17-gene signature in a prospective study that compares FCR treatment with alternative therapies, such as ibrutinib, as part of a randomised clinical trial,” the investigators wrote.
Dr. Herling reported financial disclosures related to Hoffmann-La Roche, and Dr. Coombes reported grants from the National Institutes of Health. The study was funded by the Chronic Lymphocytic Leukaemia Global Research Foundation and the National Institutes of Health/National Cancer Institute.
SOURCE: Herling CD et al. Lancet Oncol. 2019;20(11):1576-86.
FROM LANCET ONCOLOGY
Neoantigen vaccine appears safe and active in NSCLC
NATIONAL HARBOR, MD. – Trial results suggest a personalized vaccination approach is feasible and safe, and the vaccine can produce clinical responses in patients with non–small cell lung cancer (NSCLC).
The neoantigen vaccine produced only grade 1 adverse events, yielded responses in patients with epidermal growth factor receptor (EGFR) mutations, and proved particularly effective in patients who were also receiving an EGFR inhibitor.
“EGFR inhibitors seemed to reduce tumor immunosuppression barriers and may enhance antitumor immune responses before and during immunization, suggesting there may be a potential synergy of EGFR with immunotherapies,” Gregory A. Lizee, PhD, of University of Texas MD Anderson Cancer Center, Houston, said at the annual meeting of the Society for Immunotherapy of Cancer.
The research began with an elderly patient who had heavily pretreated NSCLC (Oncoimmunology. 2016;5[12]:e1238539). Dr. Lizee and colleagues used tumor mutational profiling and human leukocyte antigen (HLA) typing to develop a personalized peptide vaccine for the patient. He received the vaccine along with topical imiquimod and had multiple lung tumor nodules regress. However, the patient also had liver metastasis that remained refractory to treatment, and he ultimately died.
To investigate this treatment approach in a larger group, Dr. Lizee and colleagues began a phase 1b trial of patients with advanced NSCLC (ChiCTR-IIR-16009867). As with the prior patient, the researchers designed personalized peptide vaccines for the trial subjects based on mutational profiling of 508 cancer-associated genes and high-resolution HLA typing. The peptides were selected based on nonsynonymous somatic tumor–associated mutations with variant allele frequency greater than 0.04 and the highest predicted neoantigen peptide binding to each patient’s HLA class I and II molecules. The vaccines targeted up to eight independent somatic mutations (mean, 3.75 mutations).
In all, 31 patients provided lung tumor biopsies and peripheral blood for mutational and HLA analyses. The researchers designed 27 personalized neoantigen vaccines, and 24 patients were ultimately vaccinated. This translates to a vaccination rate of 77%, which suggests this treatment approach is feasible, Dr. Lizee said.
Of the 24 vaccinated patients, 18 had adenocarcinoma, and 6 had squamous cell carcinoma. All patients had received multiple prior therapies, including surgery, chemotherapy, radiation, and EGFR inhibitors.
Each patient was vaccinated with a personalized mixture of short and long neoantigen peptides (mean, 9.4 peptides) dissolved in isotonic saline. Patients received at least 12 weekly immunizations and had topical imiquimod applied over the injection site for costimulation through toll-like receptor 7. The 16 patients with EGFR mutations were given the option of continuing on an EGFR inhibitor, and 9 patients elected to do so.
Results
Dr. Lizee said this treatment approach was “very safe,” with only grade 1 treatment-related adverse events. The events were fatigue (n = 2), rash (n = 1), and fever (n = 1).
Seven patients achieved a response after vaccination, and one patient achieved a complete response. All seven responders had EGFR mutations, and four of them were receiving an EGFR inhibitor.
The patients on an EGFR inhibitor had significantly better overall survival than that of EGFR-mutated patients who had stopped taking an EGFR inhibitor – 13.8 months and 7.6 months, respectively (P = .038).
Immune profiling revealed that neoantigen-specific T-cell reactivity was associated with clinical responses. The researchers observed EGFR neoantigen-specific T-cell responses in five responders. In three responders, the strongest response was against a peptide encompassing the L858R driver mutation.
The researchers also found evidence of synergy between EGFR inhibitor therapy and the peptide vaccine. EGFR inhibition caused immunomodulatory pathways in EGFR-mutated cancer cells to favor immune-cell infiltration and HLA-mediated antigen presentation.
“Our mechanistic working model is that, in the circulation, the personalized vaccine increased the T-cell frequency,” Dr. Lizee said. “The EGFR inhibitor increased chemokines and antigen presentation at the tumor site, which then attracted those T cells to migrate to the tumor. Then, recognition of the antigen caused interferon gamma [to increase], which caused, potentially, a feed-forward loop by increasing chemokines and antigen presentation further.”
This research is sponsored by Tianjin Beichen Hospital and funded by Tianjin HengJia Biotechnology Development Co. Ltd. Dr. Lizee disclosed a consulting relationship with Tianjin HengJia Biotechnology Development Co. Ltd.
SOURCE: Lizee G et al. SITC 2019. Abstract O18.
NATIONAL HARBOR, MD. – Trial results suggest a personalized vaccination approach is feasible and safe, and the vaccine can produce clinical responses in patients with non–small cell lung cancer (NSCLC).
The neoantigen vaccine produced only grade 1 adverse events, yielded responses in patients with epidermal growth factor receptor (EGFR) mutations, and proved particularly effective in patients who were also receiving an EGFR inhibitor.
“EGFR inhibitors seemed to reduce tumor immunosuppression barriers and may enhance antitumor immune responses before and during immunization, suggesting there may be a potential synergy of EGFR with immunotherapies,” Gregory A. Lizee, PhD, of University of Texas MD Anderson Cancer Center, Houston, said at the annual meeting of the Society for Immunotherapy of Cancer.
The research began with an elderly patient who had heavily pretreated NSCLC (Oncoimmunology. 2016;5[12]:e1238539). Dr. Lizee and colleagues used tumor mutational profiling and human leukocyte antigen (HLA) typing to develop a personalized peptide vaccine for the patient. He received the vaccine along with topical imiquimod and had multiple lung tumor nodules regress. However, the patient also had liver metastasis that remained refractory to treatment, and he ultimately died.
To investigate this treatment approach in a larger group, Dr. Lizee and colleagues began a phase 1b trial of patients with advanced NSCLC (ChiCTR-IIR-16009867). As with the prior patient, the researchers designed personalized peptide vaccines for the trial subjects based on mutational profiling of 508 cancer-associated genes and high-resolution HLA typing. The peptides were selected based on nonsynonymous somatic tumor–associated mutations with variant allele frequency greater than 0.04 and the highest predicted neoantigen peptide binding to each patient’s HLA class I and II molecules. The vaccines targeted up to eight independent somatic mutations (mean, 3.75 mutations).
In all, 31 patients provided lung tumor biopsies and peripheral blood for mutational and HLA analyses. The researchers designed 27 personalized neoantigen vaccines, and 24 patients were ultimately vaccinated. This translates to a vaccination rate of 77%, which suggests this treatment approach is feasible, Dr. Lizee said.
Of the 24 vaccinated patients, 18 had adenocarcinoma, and 6 had squamous cell carcinoma. All patients had received multiple prior therapies, including surgery, chemotherapy, radiation, and EGFR inhibitors.
Each patient was vaccinated with a personalized mixture of short and long neoantigen peptides (mean, 9.4 peptides) dissolved in isotonic saline. Patients received at least 12 weekly immunizations and had topical imiquimod applied over the injection site for costimulation through toll-like receptor 7. The 16 patients with EGFR mutations were given the option of continuing on an EGFR inhibitor, and 9 patients elected to do so.
Results
Dr. Lizee said this treatment approach was “very safe,” with only grade 1 treatment-related adverse events. The events were fatigue (n = 2), rash (n = 1), and fever (n = 1).
Seven patients achieved a response after vaccination, and one patient achieved a complete response. All seven responders had EGFR mutations, and four of them were receiving an EGFR inhibitor.
The patients on an EGFR inhibitor had significantly better overall survival than that of EGFR-mutated patients who had stopped taking an EGFR inhibitor – 13.8 months and 7.6 months, respectively (P = .038).
Immune profiling revealed that neoantigen-specific T-cell reactivity was associated with clinical responses. The researchers observed EGFR neoantigen-specific T-cell responses in five responders. In three responders, the strongest response was against a peptide encompassing the L858R driver mutation.
The researchers also found evidence of synergy between EGFR inhibitor therapy and the peptide vaccine. EGFR inhibition caused immunomodulatory pathways in EGFR-mutated cancer cells to favor immune-cell infiltration and HLA-mediated antigen presentation.
“Our mechanistic working model is that, in the circulation, the personalized vaccine increased the T-cell frequency,” Dr. Lizee said. “The EGFR inhibitor increased chemokines and antigen presentation at the tumor site, which then attracted those T cells to migrate to the tumor. Then, recognition of the antigen caused interferon gamma [to increase], which caused, potentially, a feed-forward loop by increasing chemokines and antigen presentation further.”
This research is sponsored by Tianjin Beichen Hospital and funded by Tianjin HengJia Biotechnology Development Co. Ltd. Dr. Lizee disclosed a consulting relationship with Tianjin HengJia Biotechnology Development Co. Ltd.
SOURCE: Lizee G et al. SITC 2019. Abstract O18.
NATIONAL HARBOR, MD. – Trial results suggest a personalized vaccination approach is feasible and safe, and the vaccine can produce clinical responses in patients with non–small cell lung cancer (NSCLC).
The neoantigen vaccine produced only grade 1 adverse events, yielded responses in patients with epidermal growth factor receptor (EGFR) mutations, and proved particularly effective in patients who were also receiving an EGFR inhibitor.
“EGFR inhibitors seemed to reduce tumor immunosuppression barriers and may enhance antitumor immune responses before and during immunization, suggesting there may be a potential synergy of EGFR with immunotherapies,” Gregory A. Lizee, PhD, of University of Texas MD Anderson Cancer Center, Houston, said at the annual meeting of the Society for Immunotherapy of Cancer.
The research began with an elderly patient who had heavily pretreated NSCLC (Oncoimmunology. 2016;5[12]:e1238539). Dr. Lizee and colleagues used tumor mutational profiling and human leukocyte antigen (HLA) typing to develop a personalized peptide vaccine for the patient. He received the vaccine along with topical imiquimod and had multiple lung tumor nodules regress. However, the patient also had liver metastasis that remained refractory to treatment, and he ultimately died.
To investigate this treatment approach in a larger group, Dr. Lizee and colleagues began a phase 1b trial of patients with advanced NSCLC (ChiCTR-IIR-16009867). As with the prior patient, the researchers designed personalized peptide vaccines for the trial subjects based on mutational profiling of 508 cancer-associated genes and high-resolution HLA typing. The peptides were selected based on nonsynonymous somatic tumor–associated mutations with variant allele frequency greater than 0.04 and the highest predicted neoantigen peptide binding to each patient’s HLA class I and II molecules. The vaccines targeted up to eight independent somatic mutations (mean, 3.75 mutations).
In all, 31 patients provided lung tumor biopsies and peripheral blood for mutational and HLA analyses. The researchers designed 27 personalized neoantigen vaccines, and 24 patients were ultimately vaccinated. This translates to a vaccination rate of 77%, which suggests this treatment approach is feasible, Dr. Lizee said.
Of the 24 vaccinated patients, 18 had adenocarcinoma, and 6 had squamous cell carcinoma. All patients had received multiple prior therapies, including surgery, chemotherapy, radiation, and EGFR inhibitors.
Each patient was vaccinated with a personalized mixture of short and long neoantigen peptides (mean, 9.4 peptides) dissolved in isotonic saline. Patients received at least 12 weekly immunizations and had topical imiquimod applied over the injection site for costimulation through toll-like receptor 7. The 16 patients with EGFR mutations were given the option of continuing on an EGFR inhibitor, and 9 patients elected to do so.
Results
Dr. Lizee said this treatment approach was “very safe,” with only grade 1 treatment-related adverse events. The events were fatigue (n = 2), rash (n = 1), and fever (n = 1).
Seven patients achieved a response after vaccination, and one patient achieved a complete response. All seven responders had EGFR mutations, and four of them were receiving an EGFR inhibitor.
The patients on an EGFR inhibitor had significantly better overall survival than that of EGFR-mutated patients who had stopped taking an EGFR inhibitor – 13.8 months and 7.6 months, respectively (P = .038).
Immune profiling revealed that neoantigen-specific T-cell reactivity was associated with clinical responses. The researchers observed EGFR neoantigen-specific T-cell responses in five responders. In three responders, the strongest response was against a peptide encompassing the L858R driver mutation.
The researchers also found evidence of synergy between EGFR inhibitor therapy and the peptide vaccine. EGFR inhibition caused immunomodulatory pathways in EGFR-mutated cancer cells to favor immune-cell infiltration and HLA-mediated antigen presentation.
“Our mechanistic working model is that, in the circulation, the personalized vaccine increased the T-cell frequency,” Dr. Lizee said. “The EGFR inhibitor increased chemokines and antigen presentation at the tumor site, which then attracted those T cells to migrate to the tumor. Then, recognition of the antigen caused interferon gamma [to increase], which caused, potentially, a feed-forward loop by increasing chemokines and antigen presentation further.”
This research is sponsored by Tianjin Beichen Hospital and funded by Tianjin HengJia Biotechnology Development Co. Ltd. Dr. Lizee disclosed a consulting relationship with Tianjin HengJia Biotechnology Development Co. Ltd.
SOURCE: Lizee G et al. SITC 2019. Abstract O18.
REPORTING FROM SITC 2019
Combo produces disappointing PFS, promising OS in metastatic colorectal cancer
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
REPORTING FROM SITC 2019
Lorlatinib induces deep responses in ROS1-positive NSCLC
The tyrosine kinase inhibitor (TKI) lorlatinib showed deep responses and intracranial activity in both TKI-pretreated and TKI-naive patients with advanced ROS1-positive non–small cell lung cancer (NSCLC), according to results from a phase 1-2 trial.
“We investigated the antitumour activity and safety of lorlatinib in advanced, ROS1-positive NSCLC,” wrote Alice T. Shaw, MD, PhD, of Massachusetts General Hospital Cancer Center, Boston, and colleagues. Their report is in The Lancet Oncology.
The single-arm, open-label study included 69 patients with advanced ROS1-positive disease with or without CNS involvement. The effects of lorlatinib were evaluated across 28 institutions in 12 different countries around the globe.
At baseline, the median age of study participants was 54 years (range, 44-61 years), and 57% were positive for brain metastases.
Study participants received 100 mg of oral lorlatinib once daily in repeated 21-day cycles. Drug therapy was continued until death, disease progression, unacceptable toxicity, or withdrawal of consent.
The primary outcome measured was intracranial and overall response. Activity outcomes were evaluated in subjects given a minimum of one dose of lorlatinib.
A total of 58% of patients were previously treated with crizotinib, while 30% of patients were TKI-naive. Among 40 crizotinib-pretreated patients, 14 patients (35%) had an objective response, with a median duration of response and PFS of 13.8 and 8.5 months, respectively.
Among 21 TKI-naive patients, 13 patients (62%) had an objective response, with a median duration of response and PFS of 25.3 and 21 months, respectively.
“Intracranial responses were achieved in seven (64%) of 11 TKI-naive patients and 12 (50%) of 24 previous crizotinib-only patients,” they reported.
With respect to safety, serious lorlatinib-related adverse events were observed in 7% of patients, with no therapy-related deaths reported. The most frequently seen grade 3-4 TEAEs were hypertriglyceridemia (19%) and hypercholesterolemia (14%).
The researchers noted a key limitation of the study was the small sample size; however, due to the rare nature of ROS1 rearrangements in patients with NSCLC, increasing enrollment for future studies could be challenging.
“Because crizotinib-refractory patients have few treatment options, lorlatinib could represent an important next-line targeted agent,” they concluded.
Pfizer funded the study. The authors reported financial affiliations with Ariad, Blueprint Medicines, Chugai Pharmaceutical, Daiichi Sankyo, EMD Serono, Pfizer, KSQ Therapeutics, Servier, TP Therapeutics, and other companies.
SOURCE: Shaw AT et al. Lancet Oncol. 2019 Oct 25. doi: 10.1016/S1470-2045(19)30655-2.
The tyrosine kinase inhibitor (TKI) crizotinib was recently established as an optimal first-line treatment option for patients with ROS1-positive non–small cell lung cancer (NSCLC). Despite strong efficacy seen in clinical trials, disease progression can still occur in patients on crizotinib, often through the development of resistance, which is largely the result of on-target mutations, such as Gly2032Arg.
Early results suggest the novel oral TKI candidate, lorlatinib, a potent inhibitor of the Gly2032Arg mutation, may be a treatment of choice in patients with crizotinib-resistance. Recent phase 1 data showed lorlatinib had antitumor activity in ROS1-positive patients.
Correspondingly, the deep and durable responses reported by Dr. Shaw and colleagues represents a significant milestone for lorlatinib, particularly in the setting of crizotinib resistance, where a paucity of later-line treatment options exist. In comparison to platinum-pemetrexed chemotherapy, lorlatinib is better tolerated and has demonstrated potent intracranial activity, which may prevent or delay CNS progression in the disease.
One question that remains from the current study is whether other ROS1 TKI drug candidates, such as repotrectinib and entrectinib, will show similar results to lorlatinib. Several trials are presently ongoing in an attempt to help answer this, and other remaining questions.
Michaël Duruisseaux, MD, PhD, is affiliated with the Hospices Civils de Lyon (France), Universit é Claude Bernard Lyon. Dr. Duruisseaux reported financial affiliations with Boehringer Ingelheim, Bristol-Myers Squibb, Roche, and Takeda. These comments are adapted from his editorial (Lancet Oncol. 2019 Oct 25. doi: 10.1016/S1470-2045[19]30716-8 ).
The tyrosine kinase inhibitor (TKI) crizotinib was recently established as an optimal first-line treatment option for patients with ROS1-positive non–small cell lung cancer (NSCLC). Despite strong efficacy seen in clinical trials, disease progression can still occur in patients on crizotinib, often through the development of resistance, which is largely the result of on-target mutations, such as Gly2032Arg.
Early results suggest the novel oral TKI candidate, lorlatinib, a potent inhibitor of the Gly2032Arg mutation, may be a treatment of choice in patients with crizotinib-resistance. Recent phase 1 data showed lorlatinib had antitumor activity in ROS1-positive patients.
Correspondingly, the deep and durable responses reported by Dr. Shaw and colleagues represents a significant milestone for lorlatinib, particularly in the setting of crizotinib resistance, where a paucity of later-line treatment options exist. In comparison to platinum-pemetrexed chemotherapy, lorlatinib is better tolerated and has demonstrated potent intracranial activity, which may prevent or delay CNS progression in the disease.
One question that remains from the current study is whether other ROS1 TKI drug candidates, such as repotrectinib and entrectinib, will show similar results to lorlatinib. Several trials are presently ongoing in an attempt to help answer this, and other remaining questions.
Michaël Duruisseaux, MD, PhD, is affiliated with the Hospices Civils de Lyon (France), Universit é Claude Bernard Lyon. Dr. Duruisseaux reported financial affiliations with Boehringer Ingelheim, Bristol-Myers Squibb, Roche, and Takeda. These comments are adapted from his editorial (Lancet Oncol. 2019 Oct 25. doi: 10.1016/S1470-2045[19]30716-8 ).
The tyrosine kinase inhibitor (TKI) crizotinib was recently established as an optimal first-line treatment option for patients with ROS1-positive non–small cell lung cancer (NSCLC). Despite strong efficacy seen in clinical trials, disease progression can still occur in patients on crizotinib, often through the development of resistance, which is largely the result of on-target mutations, such as Gly2032Arg.
Early results suggest the novel oral TKI candidate, lorlatinib, a potent inhibitor of the Gly2032Arg mutation, may be a treatment of choice in patients with crizotinib-resistance. Recent phase 1 data showed lorlatinib had antitumor activity in ROS1-positive patients.
Correspondingly, the deep and durable responses reported by Dr. Shaw and colleagues represents a significant milestone for lorlatinib, particularly in the setting of crizotinib resistance, where a paucity of later-line treatment options exist. In comparison to platinum-pemetrexed chemotherapy, lorlatinib is better tolerated and has demonstrated potent intracranial activity, which may prevent or delay CNS progression in the disease.
One question that remains from the current study is whether other ROS1 TKI drug candidates, such as repotrectinib and entrectinib, will show similar results to lorlatinib. Several trials are presently ongoing in an attempt to help answer this, and other remaining questions.
Michaël Duruisseaux, MD, PhD, is affiliated with the Hospices Civils de Lyon (France), Universit é Claude Bernard Lyon. Dr. Duruisseaux reported financial affiliations with Boehringer Ingelheim, Bristol-Myers Squibb, Roche, and Takeda. These comments are adapted from his editorial (Lancet Oncol. 2019 Oct 25. doi: 10.1016/S1470-2045[19]30716-8 ).
The tyrosine kinase inhibitor (TKI) lorlatinib showed deep responses and intracranial activity in both TKI-pretreated and TKI-naive patients with advanced ROS1-positive non–small cell lung cancer (NSCLC), according to results from a phase 1-2 trial.
“We investigated the antitumour activity and safety of lorlatinib in advanced, ROS1-positive NSCLC,” wrote Alice T. Shaw, MD, PhD, of Massachusetts General Hospital Cancer Center, Boston, and colleagues. Their report is in The Lancet Oncology.
The single-arm, open-label study included 69 patients with advanced ROS1-positive disease with or without CNS involvement. The effects of lorlatinib were evaluated across 28 institutions in 12 different countries around the globe.
At baseline, the median age of study participants was 54 years (range, 44-61 years), and 57% were positive for brain metastases.
Study participants received 100 mg of oral lorlatinib once daily in repeated 21-day cycles. Drug therapy was continued until death, disease progression, unacceptable toxicity, or withdrawal of consent.
The primary outcome measured was intracranial and overall response. Activity outcomes were evaluated in subjects given a minimum of one dose of lorlatinib.
A total of 58% of patients were previously treated with crizotinib, while 30% of patients were TKI-naive. Among 40 crizotinib-pretreated patients, 14 patients (35%) had an objective response, with a median duration of response and PFS of 13.8 and 8.5 months, respectively.
Among 21 TKI-naive patients, 13 patients (62%) had an objective response, with a median duration of response and PFS of 25.3 and 21 months, respectively.
“Intracranial responses were achieved in seven (64%) of 11 TKI-naive patients and 12 (50%) of 24 previous crizotinib-only patients,” they reported.
With respect to safety, serious lorlatinib-related adverse events were observed in 7% of patients, with no therapy-related deaths reported. The most frequently seen grade 3-4 TEAEs were hypertriglyceridemia (19%) and hypercholesterolemia (14%).
The researchers noted a key limitation of the study was the small sample size; however, due to the rare nature of ROS1 rearrangements in patients with NSCLC, increasing enrollment for future studies could be challenging.
“Because crizotinib-refractory patients have few treatment options, lorlatinib could represent an important next-line targeted agent,” they concluded.
Pfizer funded the study. The authors reported financial affiliations with Ariad, Blueprint Medicines, Chugai Pharmaceutical, Daiichi Sankyo, EMD Serono, Pfizer, KSQ Therapeutics, Servier, TP Therapeutics, and other companies.
SOURCE: Shaw AT et al. Lancet Oncol. 2019 Oct 25. doi: 10.1016/S1470-2045(19)30655-2.
The tyrosine kinase inhibitor (TKI) lorlatinib showed deep responses and intracranial activity in both TKI-pretreated and TKI-naive patients with advanced ROS1-positive non–small cell lung cancer (NSCLC), according to results from a phase 1-2 trial.
“We investigated the antitumour activity and safety of lorlatinib in advanced, ROS1-positive NSCLC,” wrote Alice T. Shaw, MD, PhD, of Massachusetts General Hospital Cancer Center, Boston, and colleagues. Their report is in The Lancet Oncology.
The single-arm, open-label study included 69 patients with advanced ROS1-positive disease with or without CNS involvement. The effects of lorlatinib were evaluated across 28 institutions in 12 different countries around the globe.
At baseline, the median age of study participants was 54 years (range, 44-61 years), and 57% were positive for brain metastases.
Study participants received 100 mg of oral lorlatinib once daily in repeated 21-day cycles. Drug therapy was continued until death, disease progression, unacceptable toxicity, or withdrawal of consent.
The primary outcome measured was intracranial and overall response. Activity outcomes were evaluated in subjects given a minimum of one dose of lorlatinib.
A total of 58% of patients were previously treated with crizotinib, while 30% of patients were TKI-naive. Among 40 crizotinib-pretreated patients, 14 patients (35%) had an objective response, with a median duration of response and PFS of 13.8 and 8.5 months, respectively.
Among 21 TKI-naive patients, 13 patients (62%) had an objective response, with a median duration of response and PFS of 25.3 and 21 months, respectively.
“Intracranial responses were achieved in seven (64%) of 11 TKI-naive patients and 12 (50%) of 24 previous crizotinib-only patients,” they reported.
With respect to safety, serious lorlatinib-related adverse events were observed in 7% of patients, with no therapy-related deaths reported. The most frequently seen grade 3-4 TEAEs were hypertriglyceridemia (19%) and hypercholesterolemia (14%).
The researchers noted a key limitation of the study was the small sample size; however, due to the rare nature of ROS1 rearrangements in patients with NSCLC, increasing enrollment for future studies could be challenging.
“Because crizotinib-refractory patients have few treatment options, lorlatinib could represent an important next-line targeted agent,” they concluded.
Pfizer funded the study. The authors reported financial affiliations with Ariad, Blueprint Medicines, Chugai Pharmaceutical, Daiichi Sankyo, EMD Serono, Pfizer, KSQ Therapeutics, Servier, TP Therapeutics, and other companies.
SOURCE: Shaw AT et al. Lancet Oncol. 2019 Oct 25. doi: 10.1016/S1470-2045(19)30655-2.
FROM THE LANCET ONCOLOGY
Direct-acting antiviral treatment linked to lower mortality in patients with HCC history
BOSTON – For patients with a complete response following treatment for hepatitis C virus (HCV)–related hepatocellular carcinoma (HCC), treatment with direct-acting antiviral therapy was linked to significantly reduced mortality compared with no such treatment, according to results of a large cohort study.
The mortality benefit associated with direct-acting antiviral (DAA) therapy was consistent across most subgroups, suggesting that the association was driven by achieving sustained virological response (SVR), according to Amit G. Singal, MD, associate professor of medicine at UT Southwestern Medical Center, Dallas.
Those results suggest that DAA therapy in patients with a history of HCC is not only safe, but is also beneficial, Dr. Singal said at the annual meeting of the American Association for the Study of Liver Diseases.
“To be slightly controversial, I think that this changes the paradigm in this subgroup of patients from ‘can be treated’ for their hepatitis C to ‘should be treated,’ ” he concluded in an oral presentation of the results.
While DAA treatment is proven to reduce risk of incident HCC in patients with cirrhosis, the risk-benefit ratio is “less clear” in patients with a history of HCC following complete response, according to Dr. Singal.
Moreover, concerns were raised about the safety of DAA therapy in patients with an HCC history, after early data suggested a potentially higher recurrence risk, he added.
In the current multicenter, retrospective North American cohort study, Dr. Singal and colleagues reviewed data for 797 patients with HCV–related HCC who achieved complete response following ablation, resection, radiotherapy, transarterial chemoembolization, or transarterial radioembolization.
Treatment with DAA therapy was associated with improved overall survival, according to results of multivariable analysis, with a hazard ratio of 0.54 (95% confidence interval, 0.33-0.90). Median time from HCC complete response to death was 25.7 months for the DAA treatment group, versus 11.5 months for the untreated group.
The association between DAA treatment and death was apparently driven by SVR, as reduced mortality was seen in the DAA-treated patients who did achieve SVR, but not in those without SVR, Dr. Singal reported.
While these findings together suggest that DAA treatment is linked to reduced mortality after HCC complete response, prospective studies are needed to confirm this association, Dr. Singal said.
Dr. Singal reported disclosures related to AbbVie, Bayer, BMS, Eisai, Exact Sciences, Exelixis, Genentech, Gilead FOCUS, Glycotest, GRAIL, Merck, Roche, TARGET Pharmasolutions, and Wako Diagnostics.
SOURCE: Singal AG et al. The Liver Meeting 2019, Abstract 199.
BOSTON – For patients with a complete response following treatment for hepatitis C virus (HCV)–related hepatocellular carcinoma (HCC), treatment with direct-acting antiviral therapy was linked to significantly reduced mortality compared with no such treatment, according to results of a large cohort study.
The mortality benefit associated with direct-acting antiviral (DAA) therapy was consistent across most subgroups, suggesting that the association was driven by achieving sustained virological response (SVR), according to Amit G. Singal, MD, associate professor of medicine at UT Southwestern Medical Center, Dallas.
Those results suggest that DAA therapy in patients with a history of HCC is not only safe, but is also beneficial, Dr. Singal said at the annual meeting of the American Association for the Study of Liver Diseases.
“To be slightly controversial, I think that this changes the paradigm in this subgroup of patients from ‘can be treated’ for their hepatitis C to ‘should be treated,’ ” he concluded in an oral presentation of the results.
While DAA treatment is proven to reduce risk of incident HCC in patients with cirrhosis, the risk-benefit ratio is “less clear” in patients with a history of HCC following complete response, according to Dr. Singal.
Moreover, concerns were raised about the safety of DAA therapy in patients with an HCC history, after early data suggested a potentially higher recurrence risk, he added.
In the current multicenter, retrospective North American cohort study, Dr. Singal and colleagues reviewed data for 797 patients with HCV–related HCC who achieved complete response following ablation, resection, radiotherapy, transarterial chemoembolization, or transarterial radioembolization.
Treatment with DAA therapy was associated with improved overall survival, according to results of multivariable analysis, with a hazard ratio of 0.54 (95% confidence interval, 0.33-0.90). Median time from HCC complete response to death was 25.7 months for the DAA treatment group, versus 11.5 months for the untreated group.
The association between DAA treatment and death was apparently driven by SVR, as reduced mortality was seen in the DAA-treated patients who did achieve SVR, but not in those without SVR, Dr. Singal reported.
While these findings together suggest that DAA treatment is linked to reduced mortality after HCC complete response, prospective studies are needed to confirm this association, Dr. Singal said.
Dr. Singal reported disclosures related to AbbVie, Bayer, BMS, Eisai, Exact Sciences, Exelixis, Genentech, Gilead FOCUS, Glycotest, GRAIL, Merck, Roche, TARGET Pharmasolutions, and Wako Diagnostics.
SOURCE: Singal AG et al. The Liver Meeting 2019, Abstract 199.
BOSTON – For patients with a complete response following treatment for hepatitis C virus (HCV)–related hepatocellular carcinoma (HCC), treatment with direct-acting antiviral therapy was linked to significantly reduced mortality compared with no such treatment, according to results of a large cohort study.
The mortality benefit associated with direct-acting antiviral (DAA) therapy was consistent across most subgroups, suggesting that the association was driven by achieving sustained virological response (SVR), according to Amit G. Singal, MD, associate professor of medicine at UT Southwestern Medical Center, Dallas.
Those results suggest that DAA therapy in patients with a history of HCC is not only safe, but is also beneficial, Dr. Singal said at the annual meeting of the American Association for the Study of Liver Diseases.
“To be slightly controversial, I think that this changes the paradigm in this subgroup of patients from ‘can be treated’ for their hepatitis C to ‘should be treated,’ ” he concluded in an oral presentation of the results.
While DAA treatment is proven to reduce risk of incident HCC in patients with cirrhosis, the risk-benefit ratio is “less clear” in patients with a history of HCC following complete response, according to Dr. Singal.
Moreover, concerns were raised about the safety of DAA therapy in patients with an HCC history, after early data suggested a potentially higher recurrence risk, he added.
In the current multicenter, retrospective North American cohort study, Dr. Singal and colleagues reviewed data for 797 patients with HCV–related HCC who achieved complete response following ablation, resection, radiotherapy, transarterial chemoembolization, or transarterial radioembolization.
Treatment with DAA therapy was associated with improved overall survival, according to results of multivariable analysis, with a hazard ratio of 0.54 (95% confidence interval, 0.33-0.90). Median time from HCC complete response to death was 25.7 months for the DAA treatment group, versus 11.5 months for the untreated group.
The association between DAA treatment and death was apparently driven by SVR, as reduced mortality was seen in the DAA-treated patients who did achieve SVR, but not in those without SVR, Dr. Singal reported.
While these findings together suggest that DAA treatment is linked to reduced mortality after HCC complete response, prospective studies are needed to confirm this association, Dr. Singal said.
Dr. Singal reported disclosures related to AbbVie, Bayer, BMS, Eisai, Exact Sciences, Exelixis, Genentech, Gilead FOCUS, Glycotest, GRAIL, Merck, Roche, TARGET Pharmasolutions, and Wako Diagnostics.
SOURCE: Singal AG et al. The Liver Meeting 2019, Abstract 199.
REPORTING FROM THE LIVER MEETING 2019
Armored CAR T cells elicit responses in NHL patients
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
REPORTING FROM SITC 2019
Combo shows promise for checkpoint inhibitor-refractory urothelial carcinoma
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
REPORTING FROM SITC 2019