User login
AVAHO
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]


Ten-year results support partial breast irradiation
SAN ANTONIO – For patients with early, low-risk breast cancer, accelerated partial breast irradiation (APBI) may be considered a standard alternative to whole breast irradiation, according to investigators.
This conclusion was based on 10-year follow-up results from the APBI IMRT Florence phase III trial, which showed that APBI was associated with significantly fewer adverse events and better cosmetic results than whole breast irradiation without increasing risks of tumor recurrence or mortality, reported lead author Irco Meattini, MD, of the University of Florence, Italy, and colleagues.
“As we well know, recent developments in radiation oncology ... show a move toward a deescalation strategy for early breast cancer, including accelerated and nonaccelerated partial breast irradiation,” Dr. Meattini said during a presentation at the San Antonio Breast Cancer Symposium. “What we have learned from [previous] phase 3 trials [is that with adequate patient selection for] partial breast irradiation, safety profile and cosmetic outcome are strongly associated with technique – the approach, the dose, the number of fractions per day, and the total dose.”
The current phase 3 trial, which enrolled 520 patients with early breast cancer, aimed to determine long-term efficacy, safety, and cosmetic outcomes for partial versus whole breast irradiation. All patients enrolled were at least 40 years of age and had a maximum pathological tumor size of 25 mm. Patients were randomized in a 1:1 ratio to receive either whole breast irradiation (WBI) at a dose of 50 Gy in 25 fractions, followed by 10 Gy in five fractions delivered to the tumor bed; or APBI, which was delivered to the tumor bed at a dose of 30 Gy in five daily fractions.
The primary endpoint was ipsilateral breast tumor recurrence (IBTR). Secondary endpoints were overall survival, breast cancer–specific survival, distant metastasis-free survival, locoregional recurrences, and contralateral breast cancer. Adverse events and cosmesis also were evaluated.
Five-year results, previously reported, revealed no significant difference in survival rates or IBTR between treatment techniques, and results of the present 10-year analysis maintained these findings. Between groups, no significant differences were observed in any of the primary or secondary endpoints, suggesting that major efficacy outcomes were unaffected by type of irradiation delivered.
While major efficacy endpoints were comparable between groups, safety profiles and cosmetic results differed significantly.
Adverse events of all levels of severity were significantly more common with WBI than APBI. Grade 2 or higher acute adverse events occurred in 37.7% of patients treated with WBI, compared with just 2.0% of patients treated with APBI (P = .0001). The rate of grade 2 or higher adverse events was also significantly higher in the WBI group than in the APBI group in the late setting, albeit with a narrower margin than in the acute setting (2.7% vs 0%; P = .015). Skin toxicity rates followed a similar pattern, favoring APBI both in the acute phase (66.5% vs. 21.1%; P = .0001) and the late phase (30.0% vs. 4.5%; P = .0001).
In further support of APBI, cosmetic results, as measured by the Harvard Breast Cosmesis Scale, were significantly better in the APBI group than in the WBI group. Both physicians and patients were significantly more likely to report good or excellent cosmetic results with APBI than WBI.
“APBI might be considered a standard alternative to WBI in low risk and very low risk early breast cancer patients,” Dr. Meattini concluded.
The investigators reported no disclosures.
SOURCE: Meattini et al. SABCS. 2019 Dec 12. Abstract GS4-06.
SAN ANTONIO – For patients with early, low-risk breast cancer, accelerated partial breast irradiation (APBI) may be considered a standard alternative to whole breast irradiation, according to investigators.
This conclusion was based on 10-year follow-up results from the APBI IMRT Florence phase III trial, which showed that APBI was associated with significantly fewer adverse events and better cosmetic results than whole breast irradiation without increasing risks of tumor recurrence or mortality, reported lead author Irco Meattini, MD, of the University of Florence, Italy, and colleagues.
“As we well know, recent developments in radiation oncology ... show a move toward a deescalation strategy for early breast cancer, including accelerated and nonaccelerated partial breast irradiation,” Dr. Meattini said during a presentation at the San Antonio Breast Cancer Symposium. “What we have learned from [previous] phase 3 trials [is that with adequate patient selection for] partial breast irradiation, safety profile and cosmetic outcome are strongly associated with technique – the approach, the dose, the number of fractions per day, and the total dose.”
The current phase 3 trial, which enrolled 520 patients with early breast cancer, aimed to determine long-term efficacy, safety, and cosmetic outcomes for partial versus whole breast irradiation. All patients enrolled were at least 40 years of age and had a maximum pathological tumor size of 25 mm. Patients were randomized in a 1:1 ratio to receive either whole breast irradiation (WBI) at a dose of 50 Gy in 25 fractions, followed by 10 Gy in five fractions delivered to the tumor bed; or APBI, which was delivered to the tumor bed at a dose of 30 Gy in five daily fractions.
The primary endpoint was ipsilateral breast tumor recurrence (IBTR). Secondary endpoints were overall survival, breast cancer–specific survival, distant metastasis-free survival, locoregional recurrences, and contralateral breast cancer. Adverse events and cosmesis also were evaluated.
Five-year results, previously reported, revealed no significant difference in survival rates or IBTR between treatment techniques, and results of the present 10-year analysis maintained these findings. Between groups, no significant differences were observed in any of the primary or secondary endpoints, suggesting that major efficacy outcomes were unaffected by type of irradiation delivered.
While major efficacy endpoints were comparable between groups, safety profiles and cosmetic results differed significantly.
Adverse events of all levels of severity were significantly more common with WBI than APBI. Grade 2 or higher acute adverse events occurred in 37.7% of patients treated with WBI, compared with just 2.0% of patients treated with APBI (P = .0001). The rate of grade 2 or higher adverse events was also significantly higher in the WBI group than in the APBI group in the late setting, albeit with a narrower margin than in the acute setting (2.7% vs 0%; P = .015). Skin toxicity rates followed a similar pattern, favoring APBI both in the acute phase (66.5% vs. 21.1%; P = .0001) and the late phase (30.0% vs. 4.5%; P = .0001).
In further support of APBI, cosmetic results, as measured by the Harvard Breast Cosmesis Scale, were significantly better in the APBI group than in the WBI group. Both physicians and patients were significantly more likely to report good or excellent cosmetic results with APBI than WBI.
“APBI might be considered a standard alternative to WBI in low risk and very low risk early breast cancer patients,” Dr. Meattini concluded.
The investigators reported no disclosures.
SOURCE: Meattini et al. SABCS. 2019 Dec 12. Abstract GS4-06.
SAN ANTONIO – For patients with early, low-risk breast cancer, accelerated partial breast irradiation (APBI) may be considered a standard alternative to whole breast irradiation, according to investigators.
This conclusion was based on 10-year follow-up results from the APBI IMRT Florence phase III trial, which showed that APBI was associated with significantly fewer adverse events and better cosmetic results than whole breast irradiation without increasing risks of tumor recurrence or mortality, reported lead author Irco Meattini, MD, of the University of Florence, Italy, and colleagues.
“As we well know, recent developments in radiation oncology ... show a move toward a deescalation strategy for early breast cancer, including accelerated and nonaccelerated partial breast irradiation,” Dr. Meattini said during a presentation at the San Antonio Breast Cancer Symposium. “What we have learned from [previous] phase 3 trials [is that with adequate patient selection for] partial breast irradiation, safety profile and cosmetic outcome are strongly associated with technique – the approach, the dose, the number of fractions per day, and the total dose.”
The current phase 3 trial, which enrolled 520 patients with early breast cancer, aimed to determine long-term efficacy, safety, and cosmetic outcomes for partial versus whole breast irradiation. All patients enrolled were at least 40 years of age and had a maximum pathological tumor size of 25 mm. Patients were randomized in a 1:1 ratio to receive either whole breast irradiation (WBI) at a dose of 50 Gy in 25 fractions, followed by 10 Gy in five fractions delivered to the tumor bed; or APBI, which was delivered to the tumor bed at a dose of 30 Gy in five daily fractions.
The primary endpoint was ipsilateral breast tumor recurrence (IBTR). Secondary endpoints were overall survival, breast cancer–specific survival, distant metastasis-free survival, locoregional recurrences, and contralateral breast cancer. Adverse events and cosmesis also were evaluated.
Five-year results, previously reported, revealed no significant difference in survival rates or IBTR between treatment techniques, and results of the present 10-year analysis maintained these findings. Between groups, no significant differences were observed in any of the primary or secondary endpoints, suggesting that major efficacy outcomes were unaffected by type of irradiation delivered.
While major efficacy endpoints were comparable between groups, safety profiles and cosmetic results differed significantly.
Adverse events of all levels of severity were significantly more common with WBI than APBI. Grade 2 or higher acute adverse events occurred in 37.7% of patients treated with WBI, compared with just 2.0% of patients treated with APBI (P = .0001). The rate of grade 2 or higher adverse events was also significantly higher in the WBI group than in the APBI group in the late setting, albeit with a narrower margin than in the acute setting (2.7% vs 0%; P = .015). Skin toxicity rates followed a similar pattern, favoring APBI both in the acute phase (66.5% vs. 21.1%; P = .0001) and the late phase (30.0% vs. 4.5%; P = .0001).
In further support of APBI, cosmetic results, as measured by the Harvard Breast Cosmesis Scale, were significantly better in the APBI group than in the WBI group. Both physicians and patients were significantly more likely to report good or excellent cosmetic results with APBI than WBI.
“APBI might be considered a standard alternative to WBI in low risk and very low risk early breast cancer patients,” Dr. Meattini concluded.
The investigators reported no disclosures.
SOURCE: Meattini et al. SABCS. 2019 Dec 12. Abstract GS4-06.
REPORTING FROM SABCS 2019
New evidence further supports starting CRC screening at age 45
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
SAN ANTONIO – The American Cancer Society’s 2018 qualified recommendation to lower the starting age for colorectal cancer screening from 50 to 45 years in average-risk individuals has picked up new support from a New Hampshire Colonoscopy Registry analysis.
Data from the population-based statewide colonoscopy registry demonstrated that the prevalence of both advanced adenomas and clinically significant serrated polyps was closely similar for average-risk New Hampshirites age 45-49 years and for those age 50-54, Lynn F. Butterly, MD, reported at the annual meeting of the American College of Gastroenterology.
“The clinical implication is that our data support the recommendation to begin average-risk colorectal cancer screening at age 45,” declared Dr. Butterly, a gastroenterologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
The American Cancer Society recommendation to lower the initial screening age was designed to address a disturbing national trend: the climbing incidence of colorectal cancer in young adults. Indeed, the incidence increased by 55% among 20- to 49-year-olds during 1995-2016, even while falling by 38% in individuals age 50 years and older. The 2018 recommendation was billed as “qualified” because it was based upon predictive modeling and National Cancer Institute Surveillance, Epidemiology, and End Results data which have been criticized as subject to potential bias. Several studies conducted in Korea and other Asian countries have reported a lower colorectal cancer risk in the younger adult population than in those age 50 or older, but questions have been raised about the applicability of such data to the U.S. population.
For Dr. Butterly and coinvestigators, the research imperative was clear: “We need to generate U.S. outcomes data for average-risk individuals age 45-49, versus those over age 50, for whom colorectal cancer screening is already strongly recommended.”
Toward that end, the investigators turned to the New Hampshire Colonoscopy Registry, which contains detailed data on 200,000 colonoscopies, with some 400 variables recorded per patient. To zero in on an average-risk population below age 50, they restricted the analysis to patients undergoing their first colonoscopy for evaluation of low-risk conditions including abdominal pain or constipation while excluding those with GI bleeding, iron-deficiency anemia, abnormal imaging, or a family history of colorectal cancer.
The final study population included 42,600 New Hampshire residents who underwent their first colonoscopy. The key outcomes were the prevalence of advanced adenomas, defined as adenomas more than 1 cm in size, or with high-grade dysplasia or villous elements, and the prevalence of clinically significant serrated polyps larger than 1 cm, or larger than 5 mm if proximally located, as well as traditional serrated adenomas and those with sessile features.
The prevalence of advanced adenomas in 1,870 average-risk patients aged 45-49 years was 3.7% and nearly identical at 3.6% in 22,160 individuals undergoing screening colonoscopy at age 50-54. The rate of clinically significant serrated polyps was 5.9% in the 45- to 49-year-olds, closely similar to the 6.1% rate in patients age 50-54.
Of note, the prevalence of advanced adenomas was just 1.1% in individuals younger than age 40 years, jumping to 3.0% among 40- to 44-year-olds, 5.1% in those age 55-59, and 6.9% at age 60 or more. Clinically significant serrated polyps followed a similar pattern, with rates of 3.0% before age 40, 5.1% in 40- to 44-year-olds, 6.6% in 55- to 59-year-olds, and 6.0% in those who were older.
In a multivariate logistic regression analysis adjusted for sex, body mass index, smoking, and other potential confounders, 45- to 49-year-olds were at a 243% increased risk of finding advanced adenomas on colonoscopy, compared with those less than 40 years old, while the 50- to 54-year-olds had a virtually identical 244% increased risk.
Dr. Butterly noted that there are now 15,000 cases of colorectal cancer occurring annually in individuals under age 50 in the United States, with 3,600 deaths.
“Prevention of colorectal cancer in young, productive individuals is an essential clinical imperative that must be addressed,” she concluded.
She reported having no financial conflicts regarding her study.
REPORTING FROM ACG 2019
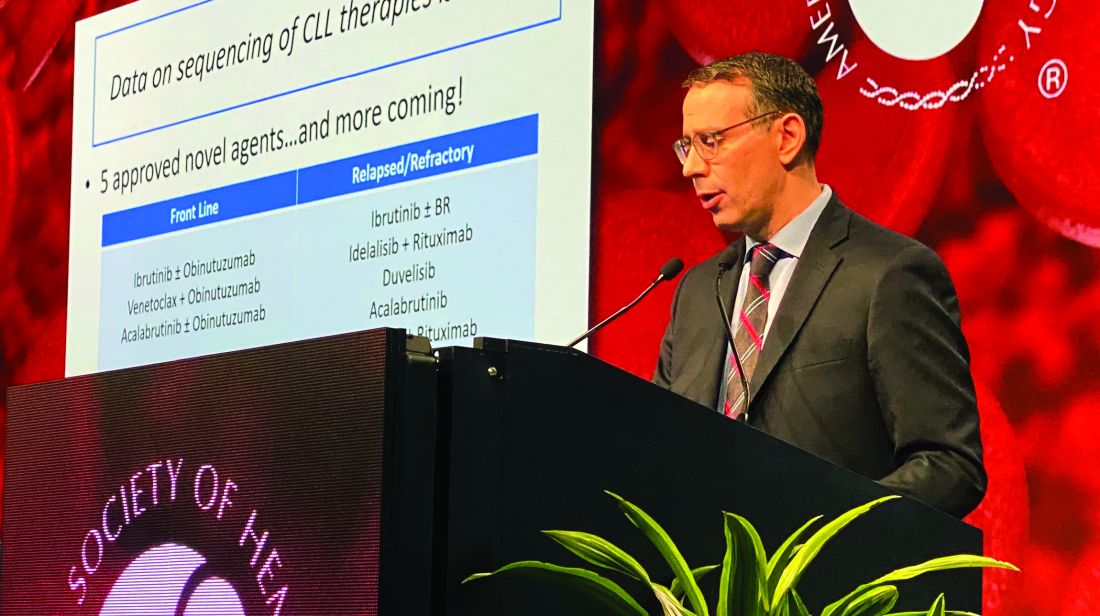
Efficacy of postvenetoclax therapy may depend on prior agent exposure in CLL
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
REPORTING FROM ASH 2019
Study halted; ‘hyperprogression’ seen with nivolumab for R/R PTCL
ORLANDO – There is an urgent need for new therapies to treat relapsed or refractory peripheral T-cell lymphoma, but results of a phase 2 study suggest that monotherapy with the immune checkpoint inhibitor nivolumab (Opdivo) is not the hoped-for salvage treatment.
An interim analysis of data on 12 patients with peripheral T-cell lymphoma (PTCL) treated with nivolumab monotherapy showed an overall response rate of 33%, consisting of 2 complete responses and 2 partial responses. But the responses were short lived, and one patient had hyperprogressive disease – dramatic progression within one cycle of treatment – while two more had progression within two cycles, leading to a trial halt, reported N. Nora Bennani, MD, from the Mayo Clinic in Rochester, Minn.
“These findings likely reflect the distinct biology of PTCL and should be considered when designing future studies using checkpoint inhibitors in these diseases,” she said at the annual meeting of the American Society of Hematology.
The rationale for using an immune checkpoint inhibitor directed against the programmed death–1 protein and its ligands (PD and PD-L1/2) is that malignant cells in PTCL induce a profoundly immunosuppressive tumor microenvironment. Checkpoint inhibitors have shown strong activity against relapsed Hodgkin lymphoma, and the Mayo Clinic researchers speculated that an anti-PD-1 agent could have a similar effect in PTCL.
They had originally planned to enroll 29 patients into a phase 2 trial with nivolumab delivered 240 mg every 2 weeks for eight cycles, followed by a dose of 480 mg given every 4 weeks until disease progression or intolerable toxicities.
Patients were eligible if they had biopsy-confirmed relapsed or refractory PTCL, measurable disease on cross-sectional imaging of at least 1.5 cm, and prior systemic chemoimmunotherapy and/or autologous stem cell transplantation.
The interim analysis included 12 patients who received at least one dose of nivolumab. Of the 12 patients, 6 had angioimmunoblastic T-cell lymphoma (AITL), 3 had PTCL not otherwise specified, and 1 each had ALK-negative anaplastic large cell lymphoma (ALK-ALCL), enteropathy-associated T-cell lymphoma (EATL), or hepatosplenic gamma/delta T-cell lymphoma.
All patients had Ann Arbor stage III/IV disease, and 11 had extranodal involvement.
As noted, there were 4 responses among the 12 patients, consisting of 1 complete response in the patient with ALK-ALCL and 1 in a patient with AITL, and 2 partial responses – 1 in a patient with PTCL-NOS, and 1 in the patient with EATL.
The median progression-free survival for all 12 patients was short at 2.7 months, and the median overall survival was estimated at 6.7 months.
“It was staggering to see this: The duration of response was significantly short, less than 2 months,” Dr. Bennani said.
Nonhematologic toxicities were seen in 5 of the 12 patients (42%), and hematologic adverse events occurred in 3 (25%). All patients are now off treatment, 10 because of disease progression, 1 because of acute pancreatitis, and the aforementioned patient with hyperprogressive disease.
The patient with hyperprogressive disease had significant progression in tonsillar and cervical lymphadenopathy within 7-10 days of nivolumab infusion, with biopsy-proven AITL in the involved nodes.
“I believe that, in this patient population, combination therapies will be key. I think checkpoint blockers alone are not going to be sufficient to see meaningful outcomes in these patients,” Dr. Bennani said in an interview.
“An overall response rate of 33% is significant, because most other agents that were FDA approved in this patient population have response rates around 30%,” she said, adding that it’s possible that the patients with rapid progression had disease too advanced to be effectively treated with a checkpoint inhibitor.
“Ideally however, if we want to move forward, it will need to be with combinations of checkpoint inhibitors with HDAC [histone deacetylase] inhibitors, hypomethylating agents, or even PI3 kinase inhibitors,” she said.
The study was supported by Bristol-Myers Squibb. Dr. Bennani reported research funding and advisory board activities for Bristol-Myers Squibb and others.
SOURCE: Bennani NN et al. ASH 2019, Abstract 467.
ORLANDO – There is an urgent need for new therapies to treat relapsed or refractory peripheral T-cell lymphoma, but results of a phase 2 study suggest that monotherapy with the immune checkpoint inhibitor nivolumab (Opdivo) is not the hoped-for salvage treatment.
An interim analysis of data on 12 patients with peripheral T-cell lymphoma (PTCL) treated with nivolumab monotherapy showed an overall response rate of 33%, consisting of 2 complete responses and 2 partial responses. But the responses were short lived, and one patient had hyperprogressive disease – dramatic progression within one cycle of treatment – while two more had progression within two cycles, leading to a trial halt, reported N. Nora Bennani, MD, from the Mayo Clinic in Rochester, Minn.
“These findings likely reflect the distinct biology of PTCL and should be considered when designing future studies using checkpoint inhibitors in these diseases,” she said at the annual meeting of the American Society of Hematology.
The rationale for using an immune checkpoint inhibitor directed against the programmed death–1 protein and its ligands (PD and PD-L1/2) is that malignant cells in PTCL induce a profoundly immunosuppressive tumor microenvironment. Checkpoint inhibitors have shown strong activity against relapsed Hodgkin lymphoma, and the Mayo Clinic researchers speculated that an anti-PD-1 agent could have a similar effect in PTCL.
They had originally planned to enroll 29 patients into a phase 2 trial with nivolumab delivered 240 mg every 2 weeks for eight cycles, followed by a dose of 480 mg given every 4 weeks until disease progression or intolerable toxicities.
Patients were eligible if they had biopsy-confirmed relapsed or refractory PTCL, measurable disease on cross-sectional imaging of at least 1.5 cm, and prior systemic chemoimmunotherapy and/or autologous stem cell transplantation.
The interim analysis included 12 patients who received at least one dose of nivolumab. Of the 12 patients, 6 had angioimmunoblastic T-cell lymphoma (AITL), 3 had PTCL not otherwise specified, and 1 each had ALK-negative anaplastic large cell lymphoma (ALK-ALCL), enteropathy-associated T-cell lymphoma (EATL), or hepatosplenic gamma/delta T-cell lymphoma.
All patients had Ann Arbor stage III/IV disease, and 11 had extranodal involvement.
As noted, there were 4 responses among the 12 patients, consisting of 1 complete response in the patient with ALK-ALCL and 1 in a patient with AITL, and 2 partial responses – 1 in a patient with PTCL-NOS, and 1 in the patient with EATL.
The median progression-free survival for all 12 patients was short at 2.7 months, and the median overall survival was estimated at 6.7 months.
“It was staggering to see this: The duration of response was significantly short, less than 2 months,” Dr. Bennani said.
Nonhematologic toxicities were seen in 5 of the 12 patients (42%), and hematologic adverse events occurred in 3 (25%). All patients are now off treatment, 10 because of disease progression, 1 because of acute pancreatitis, and the aforementioned patient with hyperprogressive disease.
The patient with hyperprogressive disease had significant progression in tonsillar and cervical lymphadenopathy within 7-10 days of nivolumab infusion, with biopsy-proven AITL in the involved nodes.
“I believe that, in this patient population, combination therapies will be key. I think checkpoint blockers alone are not going to be sufficient to see meaningful outcomes in these patients,” Dr. Bennani said in an interview.
“An overall response rate of 33% is significant, because most other agents that were FDA approved in this patient population have response rates around 30%,” she said, adding that it’s possible that the patients with rapid progression had disease too advanced to be effectively treated with a checkpoint inhibitor.
“Ideally however, if we want to move forward, it will need to be with combinations of checkpoint inhibitors with HDAC [histone deacetylase] inhibitors, hypomethylating agents, or even PI3 kinase inhibitors,” she said.
The study was supported by Bristol-Myers Squibb. Dr. Bennani reported research funding and advisory board activities for Bristol-Myers Squibb and others.
SOURCE: Bennani NN et al. ASH 2019, Abstract 467.
ORLANDO – There is an urgent need for new therapies to treat relapsed or refractory peripheral T-cell lymphoma, but results of a phase 2 study suggest that monotherapy with the immune checkpoint inhibitor nivolumab (Opdivo) is not the hoped-for salvage treatment.
An interim analysis of data on 12 patients with peripheral T-cell lymphoma (PTCL) treated with nivolumab monotherapy showed an overall response rate of 33%, consisting of 2 complete responses and 2 partial responses. But the responses were short lived, and one patient had hyperprogressive disease – dramatic progression within one cycle of treatment – while two more had progression within two cycles, leading to a trial halt, reported N. Nora Bennani, MD, from the Mayo Clinic in Rochester, Minn.
“These findings likely reflect the distinct biology of PTCL and should be considered when designing future studies using checkpoint inhibitors in these diseases,” she said at the annual meeting of the American Society of Hematology.
The rationale for using an immune checkpoint inhibitor directed against the programmed death–1 protein and its ligands (PD and PD-L1/2) is that malignant cells in PTCL induce a profoundly immunosuppressive tumor microenvironment. Checkpoint inhibitors have shown strong activity against relapsed Hodgkin lymphoma, and the Mayo Clinic researchers speculated that an anti-PD-1 agent could have a similar effect in PTCL.
They had originally planned to enroll 29 patients into a phase 2 trial with nivolumab delivered 240 mg every 2 weeks for eight cycles, followed by a dose of 480 mg given every 4 weeks until disease progression or intolerable toxicities.
Patients were eligible if they had biopsy-confirmed relapsed or refractory PTCL, measurable disease on cross-sectional imaging of at least 1.5 cm, and prior systemic chemoimmunotherapy and/or autologous stem cell transplantation.
The interim analysis included 12 patients who received at least one dose of nivolumab. Of the 12 patients, 6 had angioimmunoblastic T-cell lymphoma (AITL), 3 had PTCL not otherwise specified, and 1 each had ALK-negative anaplastic large cell lymphoma (ALK-ALCL), enteropathy-associated T-cell lymphoma (EATL), or hepatosplenic gamma/delta T-cell lymphoma.
All patients had Ann Arbor stage III/IV disease, and 11 had extranodal involvement.
As noted, there were 4 responses among the 12 patients, consisting of 1 complete response in the patient with ALK-ALCL and 1 in a patient with AITL, and 2 partial responses – 1 in a patient with PTCL-NOS, and 1 in the patient with EATL.
The median progression-free survival for all 12 patients was short at 2.7 months, and the median overall survival was estimated at 6.7 months.
“It was staggering to see this: The duration of response was significantly short, less than 2 months,” Dr. Bennani said.
Nonhematologic toxicities were seen in 5 of the 12 patients (42%), and hematologic adverse events occurred in 3 (25%). All patients are now off treatment, 10 because of disease progression, 1 because of acute pancreatitis, and the aforementioned patient with hyperprogressive disease.
The patient with hyperprogressive disease had significant progression in tonsillar and cervical lymphadenopathy within 7-10 days of nivolumab infusion, with biopsy-proven AITL in the involved nodes.
“I believe that, in this patient population, combination therapies will be key. I think checkpoint blockers alone are not going to be sufficient to see meaningful outcomes in these patients,” Dr. Bennani said in an interview.
“An overall response rate of 33% is significant, because most other agents that were FDA approved in this patient population have response rates around 30%,” she said, adding that it’s possible that the patients with rapid progression had disease too advanced to be effectively treated with a checkpoint inhibitor.
“Ideally however, if we want to move forward, it will need to be with combinations of checkpoint inhibitors with HDAC [histone deacetylase] inhibitors, hypomethylating agents, or even PI3 kinase inhibitors,” she said.
The study was supported by Bristol-Myers Squibb. Dr. Bennani reported research funding and advisory board activities for Bristol-Myers Squibb and others.
SOURCE: Bennani NN et al. ASH 2019, Abstract 467.
REPORTING FROM ASH 2019
Care coordination, equity can eliminate disparities for nonwhite patients with DLBCL
ORLANDO – Patients with diffuse large B-cell lymphoma (DLBCL) who are members of an ethnic or racial minority do not have worse outcomes than whites when they receive appropriate treatment and institutional support, a study on disparities in cancer care shows.
Although previous studies have shown that minorities with DLBCL have worse outcomes than do whites, results of a study comparing outcomes from 155 patients of white heritage with those of 41 patients from black, Hispanic, or other minority backgrounds found no significant differences in either progression-free survival (PFS) or overall survival in 2 years over follow-up, reported Nilanjan Ghosh, MD, PhD, from the Levine Cancer Institute, Atrium Health, in Charlotte, N.C.
He attributes the results to his center’s robust nurse navigation program, equal access among all patients – regardless of ability to pay – to standard treatments, and to the availability of clinical trial participation and stem cell transplantation.
“I think a key message is that if you are able to offer the same treatment and clinical trials to people irrespective of their race or socioeconomic status and can provide support, you can get equal outcomes as long as the biology is the same in both groups,” he said at a briefing prior to presentation of data in an oral abstract session at the annual meeting of the American Society of Hematology.
Dr. Ghosh pointed to four separate studies that showed that minority populations with DLBCL have worse outcomes than did whites, and noted that both uninsured and Medicaid-insured patients have also been shown to have poorer results, suggesting a role of socioeconomic factors in determining who gets optimum care and who does not.
The investigators compared PFS and OS among white and nonwhite patients with DLBCL treated in their institution, which has a safety-net cancer center. They also looked at the frequencies of clinical trial participation and stem cell transplantation between the groups.
The study included all patients with de novo DLBCL who presented to their center during January 2016–January 2019. They used patient-reported descriptors of race/ethnicity to create one of two cohorts: either self-identified whites (155 patients) or nonwhites (41), a group that included black patients, Hispanic patients, Asian Americans, and Native Americans.
The authors collected data on demographics, disease characteristics (including revised International Prognostic Index and double-hit status), insurance data, treatment, trial enrollment, progression, and death.
They found that nonwhites were significantly younger at diagnosis (median 56 vs. 64 years; P = .007), with an even distribution between the sexes in each group.
Two-thirds of both white and nonwhite patients had government insurance (Medicare or Medicaid). Of the remaining patients, 33% of white had private insurance, compared with 27% of nonwhites. No whites were uninsured, but 3 of the 41 nonwhites (7%) had no insurance.
Of the 155 white patients, 121 (86%) received nurse navigation services, as did 33 of 41 (81%) of nonwhites. The services include lodging assistance for homeless patients, transportation services for patients without cars, and care coordination among primary care physicians, oncologists, and other specialists. The services are part of the center’s standard practice, with excess costs, if any, folded into the budget, Dr. Ghosh said.
Looking at disease characteristics and treatment, the investigators found that risk profiles were similar between the groups. A higher percentage of whites had double-hit lymphoma (11% vs. 7%), but this difference was not statistically significant.
The investigators also found that in their program race was not a barrier to optimum therapy, with 96% of whites and 98% of nonwhites receiving frontline therapy with an anthracycline and rituximab-based regimen, and 4% and 2%, respectively received a non–anthracycline based regimen.
In each group, 39% of patients had disease that either relapsed or was refractory to frontline therapy.
In all, 11% of whites and 12% of nonwhites enrolled in clinical trials, 11% and 19%, respectively, underwent stem cell transplantation.
For patients with relapsed/refractory disease, the 2-year PFS rates were 60% for whites, and 63% for nonwhites, and the 2-year OS rates were 74% and 81%, respectively.
Dr. Ghosh and colleagues concluded that “our safety net cancer center, with extensive nurse navigator support and access to standard treatments, stem cell transplants, and cutting-edge clinical trials may abrogate the inferior outcomes in minority populations that have been previously reported.”
The study was internally funded. Dr. Ghosh reported consulting fees, research funding, speakers bureau activity, and/or honoraria from multiple companies.
SOURCE: Hu B et al. ASH 2019. Abstract 425.
ORLANDO – Patients with diffuse large B-cell lymphoma (DLBCL) who are members of an ethnic or racial minority do not have worse outcomes than whites when they receive appropriate treatment and institutional support, a study on disparities in cancer care shows.
Although previous studies have shown that minorities with DLBCL have worse outcomes than do whites, results of a study comparing outcomes from 155 patients of white heritage with those of 41 patients from black, Hispanic, or other minority backgrounds found no significant differences in either progression-free survival (PFS) or overall survival in 2 years over follow-up, reported Nilanjan Ghosh, MD, PhD, from the Levine Cancer Institute, Atrium Health, in Charlotte, N.C.
He attributes the results to his center’s robust nurse navigation program, equal access among all patients – regardless of ability to pay – to standard treatments, and to the availability of clinical trial participation and stem cell transplantation.
“I think a key message is that if you are able to offer the same treatment and clinical trials to people irrespective of their race or socioeconomic status and can provide support, you can get equal outcomes as long as the biology is the same in both groups,” he said at a briefing prior to presentation of data in an oral abstract session at the annual meeting of the American Society of Hematology.
Dr. Ghosh pointed to four separate studies that showed that minority populations with DLBCL have worse outcomes than did whites, and noted that both uninsured and Medicaid-insured patients have also been shown to have poorer results, suggesting a role of socioeconomic factors in determining who gets optimum care and who does not.
The investigators compared PFS and OS among white and nonwhite patients with DLBCL treated in their institution, which has a safety-net cancer center. They also looked at the frequencies of clinical trial participation and stem cell transplantation between the groups.
The study included all patients with de novo DLBCL who presented to their center during January 2016–January 2019. They used patient-reported descriptors of race/ethnicity to create one of two cohorts: either self-identified whites (155 patients) or nonwhites (41), a group that included black patients, Hispanic patients, Asian Americans, and Native Americans.
The authors collected data on demographics, disease characteristics (including revised International Prognostic Index and double-hit status), insurance data, treatment, trial enrollment, progression, and death.
They found that nonwhites were significantly younger at diagnosis (median 56 vs. 64 years; P = .007), with an even distribution between the sexes in each group.
Two-thirds of both white and nonwhite patients had government insurance (Medicare or Medicaid). Of the remaining patients, 33% of white had private insurance, compared with 27% of nonwhites. No whites were uninsured, but 3 of the 41 nonwhites (7%) had no insurance.
Of the 155 white patients, 121 (86%) received nurse navigation services, as did 33 of 41 (81%) of nonwhites. The services include lodging assistance for homeless patients, transportation services for patients without cars, and care coordination among primary care physicians, oncologists, and other specialists. The services are part of the center’s standard practice, with excess costs, if any, folded into the budget, Dr. Ghosh said.
Looking at disease characteristics and treatment, the investigators found that risk profiles were similar between the groups. A higher percentage of whites had double-hit lymphoma (11% vs. 7%), but this difference was not statistically significant.
The investigators also found that in their program race was not a barrier to optimum therapy, with 96% of whites and 98% of nonwhites receiving frontline therapy with an anthracycline and rituximab-based regimen, and 4% and 2%, respectively received a non–anthracycline based regimen.
In each group, 39% of patients had disease that either relapsed or was refractory to frontline therapy.
In all, 11% of whites and 12% of nonwhites enrolled in clinical trials, 11% and 19%, respectively, underwent stem cell transplantation.
For patients with relapsed/refractory disease, the 2-year PFS rates were 60% for whites, and 63% for nonwhites, and the 2-year OS rates were 74% and 81%, respectively.
Dr. Ghosh and colleagues concluded that “our safety net cancer center, with extensive nurse navigator support and access to standard treatments, stem cell transplants, and cutting-edge clinical trials may abrogate the inferior outcomes in minority populations that have been previously reported.”
The study was internally funded. Dr. Ghosh reported consulting fees, research funding, speakers bureau activity, and/or honoraria from multiple companies.
SOURCE: Hu B et al. ASH 2019. Abstract 425.
ORLANDO – Patients with diffuse large B-cell lymphoma (DLBCL) who are members of an ethnic or racial minority do not have worse outcomes than whites when they receive appropriate treatment and institutional support, a study on disparities in cancer care shows.
Although previous studies have shown that minorities with DLBCL have worse outcomes than do whites, results of a study comparing outcomes from 155 patients of white heritage with those of 41 patients from black, Hispanic, or other minority backgrounds found no significant differences in either progression-free survival (PFS) or overall survival in 2 years over follow-up, reported Nilanjan Ghosh, MD, PhD, from the Levine Cancer Institute, Atrium Health, in Charlotte, N.C.
He attributes the results to his center’s robust nurse navigation program, equal access among all patients – regardless of ability to pay – to standard treatments, and to the availability of clinical trial participation and stem cell transplantation.
“I think a key message is that if you are able to offer the same treatment and clinical trials to people irrespective of their race or socioeconomic status and can provide support, you can get equal outcomes as long as the biology is the same in both groups,” he said at a briefing prior to presentation of data in an oral abstract session at the annual meeting of the American Society of Hematology.
Dr. Ghosh pointed to four separate studies that showed that minority populations with DLBCL have worse outcomes than did whites, and noted that both uninsured and Medicaid-insured patients have also been shown to have poorer results, suggesting a role of socioeconomic factors in determining who gets optimum care and who does not.
The investigators compared PFS and OS among white and nonwhite patients with DLBCL treated in their institution, which has a safety-net cancer center. They also looked at the frequencies of clinical trial participation and stem cell transplantation between the groups.
The study included all patients with de novo DLBCL who presented to their center during January 2016–January 2019. They used patient-reported descriptors of race/ethnicity to create one of two cohorts: either self-identified whites (155 patients) or nonwhites (41), a group that included black patients, Hispanic patients, Asian Americans, and Native Americans.
The authors collected data on demographics, disease characteristics (including revised International Prognostic Index and double-hit status), insurance data, treatment, trial enrollment, progression, and death.
They found that nonwhites were significantly younger at diagnosis (median 56 vs. 64 years; P = .007), with an even distribution between the sexes in each group.
Two-thirds of both white and nonwhite patients had government insurance (Medicare or Medicaid). Of the remaining patients, 33% of white had private insurance, compared with 27% of nonwhites. No whites were uninsured, but 3 of the 41 nonwhites (7%) had no insurance.
Of the 155 white patients, 121 (86%) received nurse navigation services, as did 33 of 41 (81%) of nonwhites. The services include lodging assistance for homeless patients, transportation services for patients without cars, and care coordination among primary care physicians, oncologists, and other specialists. The services are part of the center’s standard practice, with excess costs, if any, folded into the budget, Dr. Ghosh said.
Looking at disease characteristics and treatment, the investigators found that risk profiles were similar between the groups. A higher percentage of whites had double-hit lymphoma (11% vs. 7%), but this difference was not statistically significant.
The investigators also found that in their program race was not a barrier to optimum therapy, with 96% of whites and 98% of nonwhites receiving frontline therapy with an anthracycline and rituximab-based regimen, and 4% and 2%, respectively received a non–anthracycline based regimen.
In each group, 39% of patients had disease that either relapsed or was refractory to frontline therapy.
In all, 11% of whites and 12% of nonwhites enrolled in clinical trials, 11% and 19%, respectively, underwent stem cell transplantation.
For patients with relapsed/refractory disease, the 2-year PFS rates were 60% for whites, and 63% for nonwhites, and the 2-year OS rates were 74% and 81%, respectively.
Dr. Ghosh and colleagues concluded that “our safety net cancer center, with extensive nurse navigator support and access to standard treatments, stem cell transplants, and cutting-edge clinical trials may abrogate the inferior outcomes in minority populations that have been previously reported.”
The study was internally funded. Dr. Ghosh reported consulting fees, research funding, speakers bureau activity, and/or honoraria from multiple companies.
SOURCE: Hu B et al. ASH 2019. Abstract 425.
REPORTING FROM ASH 2019
Aspirin plus a DOAC may do more harm than good in some
ORLANDO – in a large registry-based cohort.
The study, which involved a cohort of 2,045 patients who were followed at 6 anticoagulation clinics in Michigan during January 2009–June 2019, also found no apparent improvement in thrombosis incidence with the addition of aspirin, Jordan K. Schaefer, MD, reported during a press briefing at the annual meeting of the American Society of Hematology.
Of the cohort patients, 639 adults who received a DOAC plus aspirin after VTE or for NVAF without a clear indication were compared with 639 propensity-matched controls. The bleeding event rate per 100 patient years was 39.50 vs. 32.32 at an average of 15.2 months of follow-up in the combination therapy and DOAC monotherapy groups, respectively, said Dr. Schaefer of the division of hematology/oncology, department of internal medicine, University of Michigan, Ann Arbor.
“This result was statistically significant for clinically relevant non-major bleeding, with an 18.7 rate per 100 patient years, compared with 13.5 for DOAC monotherapy,” (P = .02), he said. “We also saw a significant increase in non-major bleeding with combination therapy, compared with direct oral anticoagulant monotherapy” (rate, 32.82 vs. 25.88; P =.04).
No significant difference was seen overall (P =.07) or for other specific types of bleeding, he noted.
The observed rates of thrombosis in the groups, respectively, were 2.35 and 2.23 per 100 patient years (P =.95), he said, noting that patients on combination therapy also had more emergency department visits and hospitalizations, but those differences were not statistically significant.
“Direct-acting oral anticoagulants, which include apixaban, dabigatran, edoxaban, and rivaroxaban, are increasingly used in clinical practice for indications that include the prevention of strokes for patients with nonvalvular atrial fibrillation, and the treatment and secondary prevention of venous thromboembolic disease,” Dr. Schaefer said.
Aspirin is commonly used in clinical practice for various indications, including primary prevention of heart attacks, strokes, and colorectal cancer, as well as for thromboprophylaxis in patients with certain blood disorders or with certain cardiac devices, he added.
“Aspirin is used for the secondary prevention of thrombosis for patients with known coronary artery disease, peripheral artery disease, or carotid artery disease,” he said. “And while adding aspirin to a DOAC is often appropriate after acute coronary syndromes or percutaneous coronary intervention, many patients receive the combination therapy without a clear indication, he said, noting that increasing evidence in recent years, largely from patients treated with warfarin and aspirin, suggest that the approach may do more harm than good for certain patients.
Specifically, there’s a question of whether aspirin is increasing the rates of bleeding without protecting patients from adverse thrombotic outcomes.
“This has specifically been a concern for patients who are on full-dose anticoagulation,” he said.
In the current study, patient demographics, comorbidities, and concurrent medications were well balanced in the treatment and control groups after propensity score matching, he said, noting that patients with a history of heart valve replacement, recent MI, or less than 3 months of follow-up were excluded.
“These findings need to be confirmed in larger studies, but until such data [are] available, clinicians and patients should continue to balance the relative risks and benefits of adding aspirin to their direct oral anticoagulant therapy,” Dr. Schaefer said. “Further research needs to evaluate key subgroups to see if any particular population may benefit from combination therapy compared to DOAC therapy alone.”
Dr. Schaefer reported having no disclosures.
SOURCE: Schaeffer J et al. ASH 2019. Abstract 787.
ORLANDO – in a large registry-based cohort.
The study, which involved a cohort of 2,045 patients who were followed at 6 anticoagulation clinics in Michigan during January 2009–June 2019, also found no apparent improvement in thrombosis incidence with the addition of aspirin, Jordan K. Schaefer, MD, reported during a press briefing at the annual meeting of the American Society of Hematology.
Of the cohort patients, 639 adults who received a DOAC plus aspirin after VTE or for NVAF without a clear indication were compared with 639 propensity-matched controls. The bleeding event rate per 100 patient years was 39.50 vs. 32.32 at an average of 15.2 months of follow-up in the combination therapy and DOAC monotherapy groups, respectively, said Dr. Schaefer of the division of hematology/oncology, department of internal medicine, University of Michigan, Ann Arbor.
“This result was statistically significant for clinically relevant non-major bleeding, with an 18.7 rate per 100 patient years, compared with 13.5 for DOAC monotherapy,” (P = .02), he said. “We also saw a significant increase in non-major bleeding with combination therapy, compared with direct oral anticoagulant monotherapy” (rate, 32.82 vs. 25.88; P =.04).
No significant difference was seen overall (P =.07) or for other specific types of bleeding, he noted.
The observed rates of thrombosis in the groups, respectively, were 2.35 and 2.23 per 100 patient years (P =.95), he said, noting that patients on combination therapy also had more emergency department visits and hospitalizations, but those differences were not statistically significant.
“Direct-acting oral anticoagulants, which include apixaban, dabigatran, edoxaban, and rivaroxaban, are increasingly used in clinical practice for indications that include the prevention of strokes for patients with nonvalvular atrial fibrillation, and the treatment and secondary prevention of venous thromboembolic disease,” Dr. Schaefer said.
Aspirin is commonly used in clinical practice for various indications, including primary prevention of heart attacks, strokes, and colorectal cancer, as well as for thromboprophylaxis in patients with certain blood disorders or with certain cardiac devices, he added.
“Aspirin is used for the secondary prevention of thrombosis for patients with known coronary artery disease, peripheral artery disease, or carotid artery disease,” he said. “And while adding aspirin to a DOAC is often appropriate after acute coronary syndromes or percutaneous coronary intervention, many patients receive the combination therapy without a clear indication, he said, noting that increasing evidence in recent years, largely from patients treated with warfarin and aspirin, suggest that the approach may do more harm than good for certain patients.
Specifically, there’s a question of whether aspirin is increasing the rates of bleeding without protecting patients from adverse thrombotic outcomes.
“This has specifically been a concern for patients who are on full-dose anticoagulation,” he said.
In the current study, patient demographics, comorbidities, and concurrent medications were well balanced in the treatment and control groups after propensity score matching, he said, noting that patients with a history of heart valve replacement, recent MI, or less than 3 months of follow-up were excluded.
“These findings need to be confirmed in larger studies, but until such data [are] available, clinicians and patients should continue to balance the relative risks and benefits of adding aspirin to their direct oral anticoagulant therapy,” Dr. Schaefer said. “Further research needs to evaluate key subgroups to see if any particular population may benefit from combination therapy compared to DOAC therapy alone.”
Dr. Schaefer reported having no disclosures.
SOURCE: Schaeffer J et al. ASH 2019. Abstract 787.
ORLANDO – in a large registry-based cohort.
The study, which involved a cohort of 2,045 patients who were followed at 6 anticoagulation clinics in Michigan during January 2009–June 2019, also found no apparent improvement in thrombosis incidence with the addition of aspirin, Jordan K. Schaefer, MD, reported during a press briefing at the annual meeting of the American Society of Hematology.
Of the cohort patients, 639 adults who received a DOAC plus aspirin after VTE or for NVAF without a clear indication were compared with 639 propensity-matched controls. The bleeding event rate per 100 patient years was 39.50 vs. 32.32 at an average of 15.2 months of follow-up in the combination therapy and DOAC monotherapy groups, respectively, said Dr. Schaefer of the division of hematology/oncology, department of internal medicine, University of Michigan, Ann Arbor.
“This result was statistically significant for clinically relevant non-major bleeding, with an 18.7 rate per 100 patient years, compared with 13.5 for DOAC monotherapy,” (P = .02), he said. “We also saw a significant increase in non-major bleeding with combination therapy, compared with direct oral anticoagulant monotherapy” (rate, 32.82 vs. 25.88; P =.04).
No significant difference was seen overall (P =.07) or for other specific types of bleeding, he noted.
The observed rates of thrombosis in the groups, respectively, were 2.35 and 2.23 per 100 patient years (P =.95), he said, noting that patients on combination therapy also had more emergency department visits and hospitalizations, but those differences were not statistically significant.
“Direct-acting oral anticoagulants, which include apixaban, dabigatran, edoxaban, and rivaroxaban, are increasingly used in clinical practice for indications that include the prevention of strokes for patients with nonvalvular atrial fibrillation, and the treatment and secondary prevention of venous thromboembolic disease,” Dr. Schaefer said.
Aspirin is commonly used in clinical practice for various indications, including primary prevention of heart attacks, strokes, and colorectal cancer, as well as for thromboprophylaxis in patients with certain blood disorders or with certain cardiac devices, he added.
“Aspirin is used for the secondary prevention of thrombosis for patients with known coronary artery disease, peripheral artery disease, or carotid artery disease,” he said. “And while adding aspirin to a DOAC is often appropriate after acute coronary syndromes or percutaneous coronary intervention, many patients receive the combination therapy without a clear indication, he said, noting that increasing evidence in recent years, largely from patients treated with warfarin and aspirin, suggest that the approach may do more harm than good for certain patients.
Specifically, there’s a question of whether aspirin is increasing the rates of bleeding without protecting patients from adverse thrombotic outcomes.
“This has specifically been a concern for patients who are on full-dose anticoagulation,” he said.
In the current study, patient demographics, comorbidities, and concurrent medications were well balanced in the treatment and control groups after propensity score matching, he said, noting that patients with a history of heart valve replacement, recent MI, or less than 3 months of follow-up were excluded.
“These findings need to be confirmed in larger studies, but until such data [are] available, clinicians and patients should continue to balance the relative risks and benefits of adding aspirin to their direct oral anticoagulant therapy,” Dr. Schaefer said. “Further research needs to evaluate key subgroups to see if any particular population may benefit from combination therapy compared to DOAC therapy alone.”
Dr. Schaefer reported having no disclosures.
SOURCE: Schaeffer J et al. ASH 2019. Abstract 787.
REPORTING FROM ASH 2019
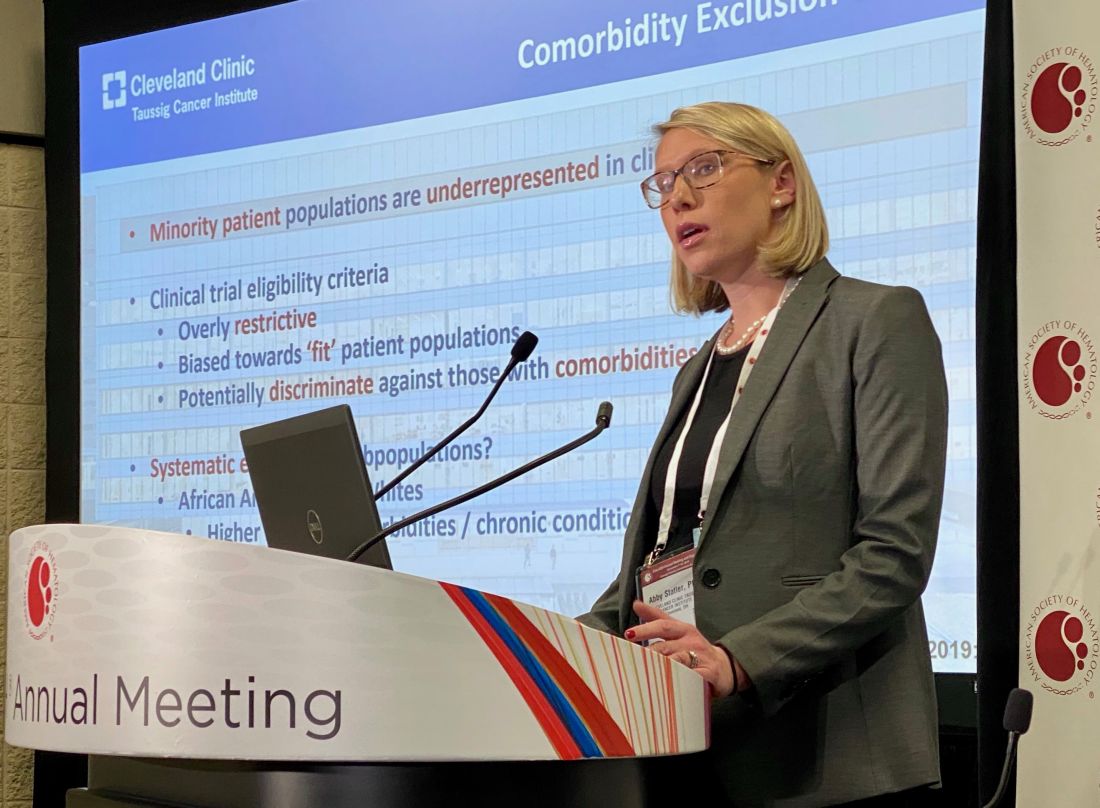
Kidney function in African American AML patients not linked to reduced survival compared with whites
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
ORLANDO – While African Americans with acute myeloid leukemia were more likely to have evidence of abnormal kidney function, the excess of this comorbidity didn’t affect overall survival, compared with whites, according to a study of more than 1,000 patients.
A total of 63% of African Americans with acute myeloid leukemia (AML) presented with a renal function abnormality that could have excluded them from a clinical trial, compared with 56% in the overall cohort; however, analysis of outcomes data suggested that renal function abnormalities were not associated with decreased survival in African Americans versus whites, said Abby Statler, PhD, MPH, of the Cleveland Clinic.
The findings may have implications for the design of clinical trials that might exclude patients on the basis of comorbidities that don’t actually affect survival, according to Dr. Statler.
“If we’re able to liberalize renal function eligibility criteria ... this may reduce racial disparities in clinical trial enrollment, which might be a major step in improving the diversity of cancer patient populations,” Dr. Statler said in a press conference at the annual meeting of the American Society of Hematology.
Overly restrictive criteria could be a significant barrier to clinical trial enrollment among minority patient populations, according to Dr. Statler.
Eligibility criteria are generally biased toward “fit” patient populations, which means they may discriminate against less-fit groups, such as African Americans who, compared with whites, have higher rates of comorbidities and report poorer overall health, according to Dr. Statler.
Laura Michaelis, MD, who chaired the press conference, said these findings suggest current clinical trial designs may be “too restrictive.”
“Once it’s published and validated, [these] data should definitely make us think twice about when you limit a patient’s enrollment in a trial,” Dr. Michaelis said in an interview.
Restrictive eligibility criteria may not only limit access to minority populations, but also may slow clinical trial accrual and completion, and make it harder to generalize clinical trial findings to the overall population, said Dr. Michaelis, associate professor of medicine in the division of hematology and oncology, Medical College of Wisconsin, Milwaukee.
The study by Dr. Statler and colleagues included 1,040 AML patients who received chemotherapy at Cleveland Clinic between 2003 and 2019. About 10% of the patients in the analysis were African American and 90% were white.
Median overall survival was not significantly different by race, at 13.7 months for African Americans and 14.9 months for whites (P = 0.89), according to results published in the study abstract.
Mild creatinine elevation did not appear to affect survival in this study, according to the investigator. Survival was not significantly different between patients with normal creatinine and those with creatinine up to 1.5 times the upper limit of normal. However, higher levels of creatinine were significantly associated with worse survival, Dr. Statler said.
Further analyses showed that these survival findings by creatinine level held up specifically in the African American subgroup as well, Dr. Statler said in the press conference.
Dr. Statler provided no disclosures related to the presentation. Study coauthors described disclosures related to Amgen, SimulStat, Bristol-Myers Squibb, Takeda, Pfizer, Novartis, Celgene Corporation, Abbvie, and Incyte, among others.
SOURCE: Statler A et al. ASH 2019, Abstract 381.
REPORTING FROM ASH 2019
Myeloma patients over age 70 can benefit from auto-HC transplant
ORLANDO – Age 70 may be the new 60, at least when it comes to outcomes following autologous hematopoietic cell transplantation (auto-HCT) in multiple myeloma.
A large-scale study looking at transplant outcomes across age groups in multiple myeloma patients found similar rates of nonrelapse mortality, relapse/progression, progression-free survival, and overall survival between patients who were aged 70 years and older and those who were aged 60-69 years.
“Age has no implication in terms of the antimyeloma effect of transplant,” Anita D’Souza, MD, of the Medical College of Wisconsin, Milwaukee, said at the annual meeting of the American Society of Hematology.
The study analyzed outcomes from 15,999 multiple myeloma patients aged 20 years or older in the United States who received a single auto-HCT with melphalan conditioning within 12 months of diagnosis between 2013 and 2017. Within that dataset, the researchers compared outcomes from 7,032 patients aged 60-69 years and 2,092 patients aged 70 years and older.
This is the largest study of auto-HCT in older adults with multiple myeloma, the researchers said, and provides important data about the benefit of transplant at any age.
Univariate analysis showed that 100-day nonrelapse mortality was higher in patients aged 70 years and older – at 1% – compared with younger patients (P less than .01). Also, 2-year overall survival was lower in older adults – at 86% – compared with 60- to 69-year-olds (P less than .01).
However, on multivariate analysis with 60- to 69-year-olds as the reference group, patients older than age 70 years had similar nonrelapse mortality (hazard ratio [HR] 1.3, 95% confidence interval [CI] 1, 1.7, P = .06). The same trends were seen for relapse/progression (HR 1.0, 95% CI, 0.9-1, P = .6), progression-free survival (HR 1.1, 95% CI 1-1.2, P = .2), and overall survival (HR 1.2, 95% CI 1-1.4, P = .03). Given the large sample size, a P value of .01 was considered statistically significant.
Over the course of the study period, the percentage of patients aged 70 and older who received a transplant grew each year, rising to 28% by 2017. But Dr. D’Souza said that number is still too low given the safety and efficacy of auto-HCT in these patients.
“Every patient with myeloma should be referred to a transplant center,” she said.
Dr. D’Souza reported financial disclosures related to EDO-Mundapharma, Merck, Prothena, Sanofi, TeneoBio, Prothena, Pfizer, Imbrium, and Akcea. Other study authors reported financial relationships with multiple companies including Celgene, Takeda, BMS, and Janssen.
SOURCE: Munshi PN et al. ASH 2019, Abstract 782.
ORLANDO – Age 70 may be the new 60, at least when it comes to outcomes following autologous hematopoietic cell transplantation (auto-HCT) in multiple myeloma.
A large-scale study looking at transplant outcomes across age groups in multiple myeloma patients found similar rates of nonrelapse mortality, relapse/progression, progression-free survival, and overall survival between patients who were aged 70 years and older and those who were aged 60-69 years.
“Age has no implication in terms of the antimyeloma effect of transplant,” Anita D’Souza, MD, of the Medical College of Wisconsin, Milwaukee, said at the annual meeting of the American Society of Hematology.
The study analyzed outcomes from 15,999 multiple myeloma patients aged 20 years or older in the United States who received a single auto-HCT with melphalan conditioning within 12 months of diagnosis between 2013 and 2017. Within that dataset, the researchers compared outcomes from 7,032 patients aged 60-69 years and 2,092 patients aged 70 years and older.
This is the largest study of auto-HCT in older adults with multiple myeloma, the researchers said, and provides important data about the benefit of transplant at any age.
Univariate analysis showed that 100-day nonrelapse mortality was higher in patients aged 70 years and older – at 1% – compared with younger patients (P less than .01). Also, 2-year overall survival was lower in older adults – at 86% – compared with 60- to 69-year-olds (P less than .01).
However, on multivariate analysis with 60- to 69-year-olds as the reference group, patients older than age 70 years had similar nonrelapse mortality (hazard ratio [HR] 1.3, 95% confidence interval [CI] 1, 1.7, P = .06). The same trends were seen for relapse/progression (HR 1.0, 95% CI, 0.9-1, P = .6), progression-free survival (HR 1.1, 95% CI 1-1.2, P = .2), and overall survival (HR 1.2, 95% CI 1-1.4, P = .03). Given the large sample size, a P value of .01 was considered statistically significant.
Over the course of the study period, the percentage of patients aged 70 and older who received a transplant grew each year, rising to 28% by 2017. But Dr. D’Souza said that number is still too low given the safety and efficacy of auto-HCT in these patients.
“Every patient with myeloma should be referred to a transplant center,” she said.
Dr. D’Souza reported financial disclosures related to EDO-Mundapharma, Merck, Prothena, Sanofi, TeneoBio, Prothena, Pfizer, Imbrium, and Akcea. Other study authors reported financial relationships with multiple companies including Celgene, Takeda, BMS, and Janssen.
SOURCE: Munshi PN et al. ASH 2019, Abstract 782.
ORLANDO – Age 70 may be the new 60, at least when it comes to outcomes following autologous hematopoietic cell transplantation (auto-HCT) in multiple myeloma.
A large-scale study looking at transplant outcomes across age groups in multiple myeloma patients found similar rates of nonrelapse mortality, relapse/progression, progression-free survival, and overall survival between patients who were aged 70 years and older and those who were aged 60-69 years.
“Age has no implication in terms of the antimyeloma effect of transplant,” Anita D’Souza, MD, of the Medical College of Wisconsin, Milwaukee, said at the annual meeting of the American Society of Hematology.
The study analyzed outcomes from 15,999 multiple myeloma patients aged 20 years or older in the United States who received a single auto-HCT with melphalan conditioning within 12 months of diagnosis between 2013 and 2017. Within that dataset, the researchers compared outcomes from 7,032 patients aged 60-69 years and 2,092 patients aged 70 years and older.
This is the largest study of auto-HCT in older adults with multiple myeloma, the researchers said, and provides important data about the benefit of transplant at any age.
Univariate analysis showed that 100-day nonrelapse mortality was higher in patients aged 70 years and older – at 1% – compared with younger patients (P less than .01). Also, 2-year overall survival was lower in older adults – at 86% – compared with 60- to 69-year-olds (P less than .01).
However, on multivariate analysis with 60- to 69-year-olds as the reference group, patients older than age 70 years had similar nonrelapse mortality (hazard ratio [HR] 1.3, 95% confidence interval [CI] 1, 1.7, P = .06). The same trends were seen for relapse/progression (HR 1.0, 95% CI, 0.9-1, P = .6), progression-free survival (HR 1.1, 95% CI 1-1.2, P = .2), and overall survival (HR 1.2, 95% CI 1-1.4, P = .03). Given the large sample size, a P value of .01 was considered statistically significant.
Over the course of the study period, the percentage of patients aged 70 and older who received a transplant grew each year, rising to 28% by 2017. But Dr. D’Souza said that number is still too low given the safety and efficacy of auto-HCT in these patients.
“Every patient with myeloma should be referred to a transplant center,” she said.
Dr. D’Souza reported financial disclosures related to EDO-Mundapharma, Merck, Prothena, Sanofi, TeneoBio, Prothena, Pfizer, Imbrium, and Akcea. Other study authors reported financial relationships with multiple companies including Celgene, Takeda, BMS, and Janssen.
SOURCE: Munshi PN et al. ASH 2019, Abstract 782.
REPORTING FROM ASH 2019
Bispecific CAR T-cells yield high response rate in relapsed/refractory myeloma
ORLANDO – A dual-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated a high overall response rate, a long response duration, and manageable safety in patients with relapsed or refractory multiple myeloma, according to an investigator in a phase 1 study.
The overall response rate exceeded 90%, and about three-quarters of patients remained progression-free at 9 months after treatment with the CAR T-cell therapy, which targets both B-cell maturation antigen (BCMA) and CD38, the study investigator reported.
Grade 3 or greater cytokine release syndrome (CRS) occurred in about one-quarter of the patients, and no neurotoxicity was observed, according to investigator Yu Hu, MD, of Tongji Medical College in Hubei, China.
“,” Dr. Hu said in a press conference.
Short-term relapse has been a “major challenge” with current CAR T-cell therapies currently under investigation for myeloma, most of which target BCMA, according to Dr. Hu.
He said the bispecific CAR T-cell therapy under investigation, known as BM38, was designed to target antigen loss and increase persistence of effector cells. According to the investigator, this was the first study to focus on an anti-BCMA and CD38 dual-targeted CAR T-cell therapy for patients with relapsed or refractory multiple myeloma.
Gary J. Schiller, MD, of UCLA Health, who moderated the press conference, said that while dual-targeting is a potentially “attractive” approach in these hard-to-treat patients, further follow-up is needed to see duration of response and to see if antigen escape re-emerges.
“Cellular therapy is costly, in terms of toxicity as well as financial costs, so you would like to see what the durability of responses is before engaging in that as a late-stage therapy, not to mention moving it up front,” Dr. Schiller said in an interview.
The median progression-free survival (PFS) duration had not been reached at the time of this report, though the 9-month PFS rate was 78.87%, according to the data presented by Dr. Hu.
In the phase 1 study, 22 patients received BM38 CAR T-cell infusions following a fludarabine and cyclophosphamide preconditioning regimen. The median patient age was 59 years, and 50% were male. Nearly three-quarters (72%) had a cytogenetic abnormality, and the median number of prior therapies approached four (range, two to nine prior therapies).
Twenty of the patients (90.9%) had a response: 12 who achieved stringent complete remission, 2 with very good partial response, 5 with partial responses, and 1 with a minimal response.
Of 9 patients with extramedullary disease, 8 achieved partial or complete elimination of tumors, Dr. Hu said in his presentation.
Cytokine release syndrome occurred in 20 patients (90.91%), 5 of whom experienced severe cases (22.73%), according to the reported data. There was no observed neurotoxicity, according to the report, while almost all had hematologic toxicities. Three experienced hepatotoxicity and one had nephrotoxicity, according to Dr. Hu.
The phase 1 study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project Fund of Hubei Province of China, and Cellyan Therapeutics. The senior author of the study was affiliated with Cellyan Therapeutics. Dr. Hu and coauthors reported that they had no relevant conflicts of interest to declare.
SOURCE: Li C et al. ASH 2019. Abstract 930.
ORLANDO – A dual-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated a high overall response rate, a long response duration, and manageable safety in patients with relapsed or refractory multiple myeloma, according to an investigator in a phase 1 study.
The overall response rate exceeded 90%, and about three-quarters of patients remained progression-free at 9 months after treatment with the CAR T-cell therapy, which targets both B-cell maturation antigen (BCMA) and CD38, the study investigator reported.
Grade 3 or greater cytokine release syndrome (CRS) occurred in about one-quarter of the patients, and no neurotoxicity was observed, according to investigator Yu Hu, MD, of Tongji Medical College in Hubei, China.
“,” Dr. Hu said in a press conference.
Short-term relapse has been a “major challenge” with current CAR T-cell therapies currently under investigation for myeloma, most of which target BCMA, according to Dr. Hu.
He said the bispecific CAR T-cell therapy under investigation, known as BM38, was designed to target antigen loss and increase persistence of effector cells. According to the investigator, this was the first study to focus on an anti-BCMA and CD38 dual-targeted CAR T-cell therapy for patients with relapsed or refractory multiple myeloma.
Gary J. Schiller, MD, of UCLA Health, who moderated the press conference, said that while dual-targeting is a potentially “attractive” approach in these hard-to-treat patients, further follow-up is needed to see duration of response and to see if antigen escape re-emerges.
“Cellular therapy is costly, in terms of toxicity as well as financial costs, so you would like to see what the durability of responses is before engaging in that as a late-stage therapy, not to mention moving it up front,” Dr. Schiller said in an interview.
The median progression-free survival (PFS) duration had not been reached at the time of this report, though the 9-month PFS rate was 78.87%, according to the data presented by Dr. Hu.
In the phase 1 study, 22 patients received BM38 CAR T-cell infusions following a fludarabine and cyclophosphamide preconditioning regimen. The median patient age was 59 years, and 50% were male. Nearly three-quarters (72%) had a cytogenetic abnormality, and the median number of prior therapies approached four (range, two to nine prior therapies).
Twenty of the patients (90.9%) had a response: 12 who achieved stringent complete remission, 2 with very good partial response, 5 with partial responses, and 1 with a minimal response.
Of 9 patients with extramedullary disease, 8 achieved partial or complete elimination of tumors, Dr. Hu said in his presentation.
Cytokine release syndrome occurred in 20 patients (90.91%), 5 of whom experienced severe cases (22.73%), according to the reported data. There was no observed neurotoxicity, according to the report, while almost all had hematologic toxicities. Three experienced hepatotoxicity and one had nephrotoxicity, according to Dr. Hu.
The phase 1 study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project Fund of Hubei Province of China, and Cellyan Therapeutics. The senior author of the study was affiliated with Cellyan Therapeutics. Dr. Hu and coauthors reported that they had no relevant conflicts of interest to declare.
SOURCE: Li C et al. ASH 2019. Abstract 930.
ORLANDO – A dual-targeted chimeric antigen receptor (CAR) T-cell therapy has demonstrated a high overall response rate, a long response duration, and manageable safety in patients with relapsed or refractory multiple myeloma, according to an investigator in a phase 1 study.
The overall response rate exceeded 90%, and about three-quarters of patients remained progression-free at 9 months after treatment with the CAR T-cell therapy, which targets both B-cell maturation antigen (BCMA) and CD38, the study investigator reported.
Grade 3 or greater cytokine release syndrome (CRS) occurred in about one-quarter of the patients, and no neurotoxicity was observed, according to investigator Yu Hu, MD, of Tongji Medical College in Hubei, China.
“,” Dr. Hu said in a press conference.
Short-term relapse has been a “major challenge” with current CAR T-cell therapies currently under investigation for myeloma, most of which target BCMA, according to Dr. Hu.
He said the bispecific CAR T-cell therapy under investigation, known as BM38, was designed to target antigen loss and increase persistence of effector cells. According to the investigator, this was the first study to focus on an anti-BCMA and CD38 dual-targeted CAR T-cell therapy for patients with relapsed or refractory multiple myeloma.
Gary J. Schiller, MD, of UCLA Health, who moderated the press conference, said that while dual-targeting is a potentially “attractive” approach in these hard-to-treat patients, further follow-up is needed to see duration of response and to see if antigen escape re-emerges.
“Cellular therapy is costly, in terms of toxicity as well as financial costs, so you would like to see what the durability of responses is before engaging in that as a late-stage therapy, not to mention moving it up front,” Dr. Schiller said in an interview.
The median progression-free survival (PFS) duration had not been reached at the time of this report, though the 9-month PFS rate was 78.87%, according to the data presented by Dr. Hu.
In the phase 1 study, 22 patients received BM38 CAR T-cell infusions following a fludarabine and cyclophosphamide preconditioning regimen. The median patient age was 59 years, and 50% were male. Nearly three-quarters (72%) had a cytogenetic abnormality, and the median number of prior therapies approached four (range, two to nine prior therapies).
Twenty of the patients (90.9%) had a response: 12 who achieved stringent complete remission, 2 with very good partial response, 5 with partial responses, and 1 with a minimal response.
Of 9 patients with extramedullary disease, 8 achieved partial or complete elimination of tumors, Dr. Hu said in his presentation.
Cytokine release syndrome occurred in 20 patients (90.91%), 5 of whom experienced severe cases (22.73%), according to the reported data. There was no observed neurotoxicity, according to the report, while almost all had hematologic toxicities. Three experienced hepatotoxicity and one had nephrotoxicity, according to Dr. Hu.
The phase 1 study was supported by the National Natural Science Foundation of China, the Major Technological Innovation Special Project Fund of Hubei Province of China, and Cellyan Therapeutics. The senior author of the study was affiliated with Cellyan Therapeutics. Dr. Hu and coauthors reported that they had no relevant conflicts of interest to declare.
SOURCE: Li C et al. ASH 2019. Abstract 930.
REPORTING FROM ASH 2019
High complete response rate seen with novel CAR-T for myeloma
ORLANDO – A novel chimeric antigen receptor T (CAR T) cell construct is associated with deep clinical responses in patients with multiple myeloma for whom prior lines of therapy – some numbering in the double digits – have failed.
Among 29 patients with multiple myeloma enrolled in a phase 1b/2 trial of JNJ-4528, the overall response rate (ORR) at 6 months median follow-up was 100%, including 69% complete responses, with 27 patients remaining free of disease progression at a median of 6 months, reported Deepu Madduri, MD, of Icahn School of Medicine at Mount Sinai, New York.
“These are very heavily pretreated patients, and so getting early and deep responses is quite amazing,” she said at a briefing prior to presentation of the data at the annual meeting of the American Society of Hematology.
JNJ-4528 is a second-generation CAR T containing two single-domain antibodies targeted against B-cell maturation protein (BCMA). As previously reported, an identical CAR T cell construct showed a high overall response with manageable toxicities in 74 patients with relapsed/refractory multiple myeloma. JNJ-4528 was granted a breakthrough therapy designation for relapsed/refractory multiple myeloma by the Food and Drug Administration on Dec. 6, 2019, and a priority medicines (PRIME) designation by the European Medicines Agency in April 2019.
BCMA was first described in myeloma in 2004 as a mechanism for the growth and survival of malignant plasma cells. Several research groups are currently investigating CAR T cells or monoclonal antibodies targeted to BCMA. The product closest to receiving FDA approval is likely BB2121.
At ASH 2019, Dr. Madduri presented results from the phase 1b portion of the CARTITUDE-1 trial. The investigators enrolled patients with multiple myeloma with measurable diseases as assessed by M-protein or serum free light chain levels who had experienced disease progression on at least 3 prior lines of therapy, or whose disease was refractory to at least two lines of therapy with a proteasome inhibitor, immunomodulatory drug (IMiD), and an anti-CD38 antibody.
Patients underwent apheresis for T-cell collection, with bridging therapy allowed until the expanded T cells could be delivered.
Following T-cell depletion with cyclophosphamide 300 mg/m2 and fludarabine 30 mg/m2 over 3 days, patients received a single weight-based infusion (compared with fixed-dose infusions used with other CAR T cell constructs).
The dose was targeted at 0.75x106 CAR-positive cells/kg, with a target range of 0.5–1.0x106, administered 5-7 days after the start of the conditioning regimen.
A total of 29 patients, median age 60, were evaluable for the safety and efficacy endpoints. One-fourth of the patients had a high-risk cytogenetic profile. The patients had received a median of 5 prior lines of therapy, with one patient receiving 18 prior lines. Of the 29 patients, 25 (86%) had previously undergone autologous transplantation.
As noted before, the ORR after a median follow-up of 6 months was 100%, with 69% completer responses, 17% very good partial responses, and 14% partial responses. The median time to complete response was 1 month (range 1 to 9 months). All but two patients remained free of disease progression at the median 6-month follow-up.
Nearly all patients (27) developed cytokine release syndrome (CRS), and one patient with prolonged grade 4 CRS died from related complications 99 days after infusion.
The median time to onset of CRS was 7 days with more than 90% of cases occurring between days 5 and 9.
Neurotoxicities, specifically immune effector cell–associated neurotoxicity syndrome (ICANS), were infrequent in CRS, and when they did occur were generally low grade, with only 1 grade 3 ICANS event.
Asked in an interview whether the impressive response rates seen with JNJ-4528 might persist over time, Dr. Madduri acknowledged that follow-up is still relatively short.
“This product is unique in that has a CD8 central memory phenotype preferentially, and we’re hoping that this would play a central role in the durability of response because they’re memory cells, but I think at this time we don’t know,” she said.
The CARTITUDE-1 trial is funded by Janssen Research & Development. Dr. Madduri disclosed serving as a consultant to Janssen and to Takeda, Foundation Medicine, AbbVie, and Celgene.
SOURCE: Madduri D et al. ASH 2019. Abstract 577.
ORLANDO – A novel chimeric antigen receptor T (CAR T) cell construct is associated with deep clinical responses in patients with multiple myeloma for whom prior lines of therapy – some numbering in the double digits – have failed.
Among 29 patients with multiple myeloma enrolled in a phase 1b/2 trial of JNJ-4528, the overall response rate (ORR) at 6 months median follow-up was 100%, including 69% complete responses, with 27 patients remaining free of disease progression at a median of 6 months, reported Deepu Madduri, MD, of Icahn School of Medicine at Mount Sinai, New York.
“These are very heavily pretreated patients, and so getting early and deep responses is quite amazing,” she said at a briefing prior to presentation of the data at the annual meeting of the American Society of Hematology.
JNJ-4528 is a second-generation CAR T containing two single-domain antibodies targeted against B-cell maturation protein (BCMA). As previously reported, an identical CAR T cell construct showed a high overall response with manageable toxicities in 74 patients with relapsed/refractory multiple myeloma. JNJ-4528 was granted a breakthrough therapy designation for relapsed/refractory multiple myeloma by the Food and Drug Administration on Dec. 6, 2019, and a priority medicines (PRIME) designation by the European Medicines Agency in April 2019.
BCMA was first described in myeloma in 2004 as a mechanism for the growth and survival of malignant plasma cells. Several research groups are currently investigating CAR T cells or monoclonal antibodies targeted to BCMA. The product closest to receiving FDA approval is likely BB2121.
At ASH 2019, Dr. Madduri presented results from the phase 1b portion of the CARTITUDE-1 trial. The investigators enrolled patients with multiple myeloma with measurable diseases as assessed by M-protein or serum free light chain levels who had experienced disease progression on at least 3 prior lines of therapy, or whose disease was refractory to at least two lines of therapy with a proteasome inhibitor, immunomodulatory drug (IMiD), and an anti-CD38 antibody.
Patients underwent apheresis for T-cell collection, with bridging therapy allowed until the expanded T cells could be delivered.
Following T-cell depletion with cyclophosphamide 300 mg/m2 and fludarabine 30 mg/m2 over 3 days, patients received a single weight-based infusion (compared with fixed-dose infusions used with other CAR T cell constructs).
The dose was targeted at 0.75x106 CAR-positive cells/kg, with a target range of 0.5–1.0x106, administered 5-7 days after the start of the conditioning regimen.
A total of 29 patients, median age 60, were evaluable for the safety and efficacy endpoints. One-fourth of the patients had a high-risk cytogenetic profile. The patients had received a median of 5 prior lines of therapy, with one patient receiving 18 prior lines. Of the 29 patients, 25 (86%) had previously undergone autologous transplantation.
As noted before, the ORR after a median follow-up of 6 months was 100%, with 69% completer responses, 17% very good partial responses, and 14% partial responses. The median time to complete response was 1 month (range 1 to 9 months). All but two patients remained free of disease progression at the median 6-month follow-up.
Nearly all patients (27) developed cytokine release syndrome (CRS), and one patient with prolonged grade 4 CRS died from related complications 99 days after infusion.
The median time to onset of CRS was 7 days with more than 90% of cases occurring between days 5 and 9.
Neurotoxicities, specifically immune effector cell–associated neurotoxicity syndrome (ICANS), were infrequent in CRS, and when they did occur were generally low grade, with only 1 grade 3 ICANS event.
Asked in an interview whether the impressive response rates seen with JNJ-4528 might persist over time, Dr. Madduri acknowledged that follow-up is still relatively short.
“This product is unique in that has a CD8 central memory phenotype preferentially, and we’re hoping that this would play a central role in the durability of response because they’re memory cells, but I think at this time we don’t know,” she said.
The CARTITUDE-1 trial is funded by Janssen Research & Development. Dr. Madduri disclosed serving as a consultant to Janssen and to Takeda, Foundation Medicine, AbbVie, and Celgene.
SOURCE: Madduri D et al. ASH 2019. Abstract 577.
ORLANDO – A novel chimeric antigen receptor T (CAR T) cell construct is associated with deep clinical responses in patients with multiple myeloma for whom prior lines of therapy – some numbering in the double digits – have failed.
Among 29 patients with multiple myeloma enrolled in a phase 1b/2 trial of JNJ-4528, the overall response rate (ORR) at 6 months median follow-up was 100%, including 69% complete responses, with 27 patients remaining free of disease progression at a median of 6 months, reported Deepu Madduri, MD, of Icahn School of Medicine at Mount Sinai, New York.
“These are very heavily pretreated patients, and so getting early and deep responses is quite amazing,” she said at a briefing prior to presentation of the data at the annual meeting of the American Society of Hematology.
JNJ-4528 is a second-generation CAR T containing two single-domain antibodies targeted against B-cell maturation protein (BCMA). As previously reported, an identical CAR T cell construct showed a high overall response with manageable toxicities in 74 patients with relapsed/refractory multiple myeloma. JNJ-4528 was granted a breakthrough therapy designation for relapsed/refractory multiple myeloma by the Food and Drug Administration on Dec. 6, 2019, and a priority medicines (PRIME) designation by the European Medicines Agency in April 2019.
BCMA was first described in myeloma in 2004 as a mechanism for the growth and survival of malignant plasma cells. Several research groups are currently investigating CAR T cells or monoclonal antibodies targeted to BCMA. The product closest to receiving FDA approval is likely BB2121.
At ASH 2019, Dr. Madduri presented results from the phase 1b portion of the CARTITUDE-1 trial. The investigators enrolled patients with multiple myeloma with measurable diseases as assessed by M-protein or serum free light chain levels who had experienced disease progression on at least 3 prior lines of therapy, or whose disease was refractory to at least two lines of therapy with a proteasome inhibitor, immunomodulatory drug (IMiD), and an anti-CD38 antibody.
Patients underwent apheresis for T-cell collection, with bridging therapy allowed until the expanded T cells could be delivered.
Following T-cell depletion with cyclophosphamide 300 mg/m2 and fludarabine 30 mg/m2 over 3 days, patients received a single weight-based infusion (compared with fixed-dose infusions used with other CAR T cell constructs).
The dose was targeted at 0.75x106 CAR-positive cells/kg, with a target range of 0.5–1.0x106, administered 5-7 days after the start of the conditioning regimen.
A total of 29 patients, median age 60, were evaluable for the safety and efficacy endpoints. One-fourth of the patients had a high-risk cytogenetic profile. The patients had received a median of 5 prior lines of therapy, with one patient receiving 18 prior lines. Of the 29 patients, 25 (86%) had previously undergone autologous transplantation.
As noted before, the ORR after a median follow-up of 6 months was 100%, with 69% completer responses, 17% very good partial responses, and 14% partial responses. The median time to complete response was 1 month (range 1 to 9 months). All but two patients remained free of disease progression at the median 6-month follow-up.
Nearly all patients (27) developed cytokine release syndrome (CRS), and one patient with prolonged grade 4 CRS died from related complications 99 days after infusion.
The median time to onset of CRS was 7 days with more than 90% of cases occurring between days 5 and 9.
Neurotoxicities, specifically immune effector cell–associated neurotoxicity syndrome (ICANS), were infrequent in CRS, and when they did occur were generally low grade, with only 1 grade 3 ICANS event.
Asked in an interview whether the impressive response rates seen with JNJ-4528 might persist over time, Dr. Madduri acknowledged that follow-up is still relatively short.
“This product is unique in that has a CD8 central memory phenotype preferentially, and we’re hoping that this would play a central role in the durability of response because they’re memory cells, but I think at this time we don’t know,” she said.
The CARTITUDE-1 trial is funded by Janssen Research & Development. Dr. Madduri disclosed serving as a consultant to Janssen and to Takeda, Foundation Medicine, AbbVie, and Celgene.
SOURCE: Madduri D et al. ASH 2019. Abstract 577.
REPORTING FROM ASH 2019