User login
AVAHO
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]


CDC notes sharp declines in breast and cervical cancer screening
The new data come from the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), a program that provides cancer screening services to women with low income and inadequate health insurance.
The data show that the total number of screenings funded by the NBCCEDP declined by 87% for breast cancer screening and by 84% for cervical cancer screening in April 2020 in comparison with the previous 5-year averages for that month.
The declines in breast cancer screening varied from 84% among Hispanic women to 98% among American Indian/Alaskan Native women. The declines in cervical cancer screening varied from 82% among Black women to 92% among Asian Pacific Islander women.
In April 2020, breast cancer screening declined by 86% in metro areas, 88% in urban areas, and 89% in rural areas in comparison with respective 5-year averages. For cervical cancer screenings, the corresponding declines were 85%, 77%, and 82%.
The findings are consistent with those from studies conducted in insured populations, note the authors, led by the Amy DeGroff, PhD, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
“Prolonged delays in screening related to the COVID-19 pandemic may lead to delayed diagnoses, poor health consequences, and an increase in cancer disparities among women already experiencing health inequities,” the CDC states in a press release.
Women from racial and ethnic minority groups already face a disproportionate burden of cervical and breast cancers in the United States: Black women and Hispanic women have the highest rates of cervical cancer incidence (8.3 and 8.9 per 100,000 women, respectively, vs. 7.3 per 100,000 among White women) and the highest rates of cervical cancer deaths. Black women have the highest rate of breast cancer death (26.9 per 100,000 women, vs. 19.4 per 100,000 among White women), the study authors explain.
Although the volume of screening began to recover in May 2020 – test volumes for breast and cervical cancer were 39% and 40% below the 5-year average by June 2020 – breast cancer screening in rural areas remained 52% below the 5-year average, they report.
The findings were published online June 30 in Preventive Medicine.
“This study highlights a decline in cancer screening among women of racial and ethnic minority groups with low incomes when their access to medical services decreased at the beginning of the pandemic,” Dr. DeGroff comments in the CDC press release.
The findings “reinforce the need to safely maintain routine health care services during the pandemic, especially when the health care environment meets COVID-19 safety guidelines,” she adds.
The investigators used NBCCEDP administrative and program data reported to the CDC by awardees – organizations that receive funding to implement the NBCCEDP – to assess the impact of COVID-19 on the number of breast and cervical cancer screening tests administered through the program and the effects of COVID-19 on the availability of screening services and NBCCEDP awardees’ capacity to support partner clinics.
A total of 630,264 breast and 594,566 cervical cancer screening tests were conducted during the review period of January-June 2015-2020.
Despite COVID-related challenges, “a large number of awardees reported flexibility and creative efforts to reach women and support clinics’ resumption of clinical care, including screening, during the COVID-19 pandemic,” the authors write.
“[The] CDC encourages health care professionals to help minimize delays in testing by continuing routine cancer screening for women having symptoms or at high risk for breast or cervical cancer,” Dr. DeGroff commented. “The Early Detection Program can help women overcome barriers to health equity by educating them about the importance of routine screening, addressing their concerns about COVID-19 transmission, and helping them to safely access screening through interventions like patient navigation.”
Future studies will examine the effect of the pandemic on screening during the second half of 2020, when surges of COVID-19 and their timing varied geographically, they note.
A version of this article first appeared on Medscape.com.
The new data come from the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), a program that provides cancer screening services to women with low income and inadequate health insurance.
The data show that the total number of screenings funded by the NBCCEDP declined by 87% for breast cancer screening and by 84% for cervical cancer screening in April 2020 in comparison with the previous 5-year averages for that month.
The declines in breast cancer screening varied from 84% among Hispanic women to 98% among American Indian/Alaskan Native women. The declines in cervical cancer screening varied from 82% among Black women to 92% among Asian Pacific Islander women.
In April 2020, breast cancer screening declined by 86% in metro areas, 88% in urban areas, and 89% in rural areas in comparison with respective 5-year averages. For cervical cancer screenings, the corresponding declines were 85%, 77%, and 82%.
The findings are consistent with those from studies conducted in insured populations, note the authors, led by the Amy DeGroff, PhD, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
“Prolonged delays in screening related to the COVID-19 pandemic may lead to delayed diagnoses, poor health consequences, and an increase in cancer disparities among women already experiencing health inequities,” the CDC states in a press release.
Women from racial and ethnic minority groups already face a disproportionate burden of cervical and breast cancers in the United States: Black women and Hispanic women have the highest rates of cervical cancer incidence (8.3 and 8.9 per 100,000 women, respectively, vs. 7.3 per 100,000 among White women) and the highest rates of cervical cancer deaths. Black women have the highest rate of breast cancer death (26.9 per 100,000 women, vs. 19.4 per 100,000 among White women), the study authors explain.
Although the volume of screening began to recover in May 2020 – test volumes for breast and cervical cancer were 39% and 40% below the 5-year average by June 2020 – breast cancer screening in rural areas remained 52% below the 5-year average, they report.
The findings were published online June 30 in Preventive Medicine.
“This study highlights a decline in cancer screening among women of racial and ethnic minority groups with low incomes when their access to medical services decreased at the beginning of the pandemic,” Dr. DeGroff comments in the CDC press release.
The findings “reinforce the need to safely maintain routine health care services during the pandemic, especially when the health care environment meets COVID-19 safety guidelines,” she adds.
The investigators used NBCCEDP administrative and program data reported to the CDC by awardees – organizations that receive funding to implement the NBCCEDP – to assess the impact of COVID-19 on the number of breast and cervical cancer screening tests administered through the program and the effects of COVID-19 on the availability of screening services and NBCCEDP awardees’ capacity to support partner clinics.
A total of 630,264 breast and 594,566 cervical cancer screening tests were conducted during the review period of January-June 2015-2020.
Despite COVID-related challenges, “a large number of awardees reported flexibility and creative efforts to reach women and support clinics’ resumption of clinical care, including screening, during the COVID-19 pandemic,” the authors write.
“[The] CDC encourages health care professionals to help minimize delays in testing by continuing routine cancer screening for women having symptoms or at high risk for breast or cervical cancer,” Dr. DeGroff commented. “The Early Detection Program can help women overcome barriers to health equity by educating them about the importance of routine screening, addressing their concerns about COVID-19 transmission, and helping them to safely access screening through interventions like patient navigation.”
Future studies will examine the effect of the pandemic on screening during the second half of 2020, when surges of COVID-19 and their timing varied geographically, they note.
A version of this article first appeared on Medscape.com.
The new data come from the National Breast and Cervical Cancer Early Detection Program (NBCCEDP), a program that provides cancer screening services to women with low income and inadequate health insurance.
The data show that the total number of screenings funded by the NBCCEDP declined by 87% for breast cancer screening and by 84% for cervical cancer screening in April 2020 in comparison with the previous 5-year averages for that month.
The declines in breast cancer screening varied from 84% among Hispanic women to 98% among American Indian/Alaskan Native women. The declines in cervical cancer screening varied from 82% among Black women to 92% among Asian Pacific Islander women.
In April 2020, breast cancer screening declined by 86% in metro areas, 88% in urban areas, and 89% in rural areas in comparison with respective 5-year averages. For cervical cancer screenings, the corresponding declines were 85%, 77%, and 82%.
The findings are consistent with those from studies conducted in insured populations, note the authors, led by the Amy DeGroff, PhD, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion.
“Prolonged delays in screening related to the COVID-19 pandemic may lead to delayed diagnoses, poor health consequences, and an increase in cancer disparities among women already experiencing health inequities,” the CDC states in a press release.
Women from racial and ethnic minority groups already face a disproportionate burden of cervical and breast cancers in the United States: Black women and Hispanic women have the highest rates of cervical cancer incidence (8.3 and 8.9 per 100,000 women, respectively, vs. 7.3 per 100,000 among White women) and the highest rates of cervical cancer deaths. Black women have the highest rate of breast cancer death (26.9 per 100,000 women, vs. 19.4 per 100,000 among White women), the study authors explain.
Although the volume of screening began to recover in May 2020 – test volumes for breast and cervical cancer were 39% and 40% below the 5-year average by June 2020 – breast cancer screening in rural areas remained 52% below the 5-year average, they report.
The findings were published online June 30 in Preventive Medicine.
“This study highlights a decline in cancer screening among women of racial and ethnic minority groups with low incomes when their access to medical services decreased at the beginning of the pandemic,” Dr. DeGroff comments in the CDC press release.
The findings “reinforce the need to safely maintain routine health care services during the pandemic, especially when the health care environment meets COVID-19 safety guidelines,” she adds.
The investigators used NBCCEDP administrative and program data reported to the CDC by awardees – organizations that receive funding to implement the NBCCEDP – to assess the impact of COVID-19 on the number of breast and cervical cancer screening tests administered through the program and the effects of COVID-19 on the availability of screening services and NBCCEDP awardees’ capacity to support partner clinics.
A total of 630,264 breast and 594,566 cervical cancer screening tests were conducted during the review period of January-June 2015-2020.
Despite COVID-related challenges, “a large number of awardees reported flexibility and creative efforts to reach women and support clinics’ resumption of clinical care, including screening, during the COVID-19 pandemic,” the authors write.
“[The] CDC encourages health care professionals to help minimize delays in testing by continuing routine cancer screening for women having symptoms or at high risk for breast or cervical cancer,” Dr. DeGroff commented. “The Early Detection Program can help women overcome barriers to health equity by educating them about the importance of routine screening, addressing their concerns about COVID-19 transmission, and helping them to safely access screening through interventions like patient navigation.”
Future studies will examine the effect of the pandemic on screening during the second half of 2020, when surges of COVID-19 and their timing varied geographically, they note.
A version of this article first appeared on Medscape.com.
No increase in breast cancer risk with fertility treatments
No link between fertility treatment and an increase in the risk for breast cancer was found in the largest study of the issue to date.
This study “provides the evidence needed to reassure women and couples seeking fertility treatments,” commented senior author Sesh Sunkara, MD, a reproductive medicine specialist at King’s College London in a press release.
With an increasing number of women seeking help to become mothers, the question “is a matter of great importance” and a source of considerable concern among patients, the study authors comment.
This is the largest meta-analysis to date, involving 1.8 million women who were followed for an average of 27 years. The investigators found no link with the use of gonadotropins or clomiphene citrate to increase egg production in fertility cycles.
There has been concern over the years that fertility treatment could stimulate estrogen-sensitive precursor breast cancer cells.
More than 4,000 studies of this issue have been conducted since 1990, and results have been conflicting. The investigators analyzed results from the 20 strongest ones.
The new meta-analysis included nine retrospective studies, five case-control studies, five prospective studies, and one comparative study
The team cautioned that the quality of evidence in even these top 20 studies was “very low” but that such an approach is perhaps the best possible on this issue because a randomized trial among women seeking help to have children would be “ethically challenging.”
In the study, the team compared breast cancer incidence among women who underwent ovarian stimulation with the incidence in both age-matched unexposed women in the general population and unexposed infertile women.
There was no significant increase in the risk for breast cancer among women treated with any ovarian stimulation drug (pooled odds ratio, 1.03; 95% confidence interval, 0.86-1.23, but with substantial heterogeneity between study outcomes).
There was also no increased risk when the analysis was limited to the eight studies in which women were treated with both gonadotropins and clomiphene citrate (pooled OR, 0.92; 95% CI, 0.52-1.60, with substantial heterogeneity).
The authors noted that, among the many study limitations, no distinction was made between physiological dosing for anovulation and supraphysiological dosing for in vitro fertilization cycles. In addition, because the treated women were generally young, the follow-up period fell short of the age at which they’d be most at risk for breast cancer.
Individual patient data were also not available, but 14 studies did adjust for confounders, including weight, race, parity, age at first birth, age at menarche, and family history of breast cancer.
Although the findings are reassuring, “further long-term and detailed studies are now needed to confirm” them, Kotryna Temcinaite, PhD, senior research communications manager at the U.K. charity Breast Cancer Now, said in the press release.
A version of this article first appeared on Medscape.com.
No link between fertility treatment and an increase in the risk for breast cancer was found in the largest study of the issue to date.
This study “provides the evidence needed to reassure women and couples seeking fertility treatments,” commented senior author Sesh Sunkara, MD, a reproductive medicine specialist at King’s College London in a press release.
With an increasing number of women seeking help to become mothers, the question “is a matter of great importance” and a source of considerable concern among patients, the study authors comment.
This is the largest meta-analysis to date, involving 1.8 million women who were followed for an average of 27 years. The investigators found no link with the use of gonadotropins or clomiphene citrate to increase egg production in fertility cycles.
There has been concern over the years that fertility treatment could stimulate estrogen-sensitive precursor breast cancer cells.
More than 4,000 studies of this issue have been conducted since 1990, and results have been conflicting. The investigators analyzed results from the 20 strongest ones.
The new meta-analysis included nine retrospective studies, five case-control studies, five prospective studies, and one comparative study
The team cautioned that the quality of evidence in even these top 20 studies was “very low” but that such an approach is perhaps the best possible on this issue because a randomized trial among women seeking help to have children would be “ethically challenging.”
In the study, the team compared breast cancer incidence among women who underwent ovarian stimulation with the incidence in both age-matched unexposed women in the general population and unexposed infertile women.
There was no significant increase in the risk for breast cancer among women treated with any ovarian stimulation drug (pooled odds ratio, 1.03; 95% confidence interval, 0.86-1.23, but with substantial heterogeneity between study outcomes).
There was also no increased risk when the analysis was limited to the eight studies in which women were treated with both gonadotropins and clomiphene citrate (pooled OR, 0.92; 95% CI, 0.52-1.60, with substantial heterogeneity).
The authors noted that, among the many study limitations, no distinction was made between physiological dosing for anovulation and supraphysiological dosing for in vitro fertilization cycles. In addition, because the treated women were generally young, the follow-up period fell short of the age at which they’d be most at risk for breast cancer.
Individual patient data were also not available, but 14 studies did adjust for confounders, including weight, race, parity, age at first birth, age at menarche, and family history of breast cancer.
Although the findings are reassuring, “further long-term and detailed studies are now needed to confirm” them, Kotryna Temcinaite, PhD, senior research communications manager at the U.K. charity Breast Cancer Now, said in the press release.
A version of this article first appeared on Medscape.com.
No link between fertility treatment and an increase in the risk for breast cancer was found in the largest study of the issue to date.
This study “provides the evidence needed to reassure women and couples seeking fertility treatments,” commented senior author Sesh Sunkara, MD, a reproductive medicine specialist at King’s College London in a press release.
With an increasing number of women seeking help to become mothers, the question “is a matter of great importance” and a source of considerable concern among patients, the study authors comment.
This is the largest meta-analysis to date, involving 1.8 million women who were followed for an average of 27 years. The investigators found no link with the use of gonadotropins or clomiphene citrate to increase egg production in fertility cycles.
There has been concern over the years that fertility treatment could stimulate estrogen-sensitive precursor breast cancer cells.
More than 4,000 studies of this issue have been conducted since 1990, and results have been conflicting. The investigators analyzed results from the 20 strongest ones.
The new meta-analysis included nine retrospective studies, five case-control studies, five prospective studies, and one comparative study
The team cautioned that the quality of evidence in even these top 20 studies was “very low” but that such an approach is perhaps the best possible on this issue because a randomized trial among women seeking help to have children would be “ethically challenging.”
In the study, the team compared breast cancer incidence among women who underwent ovarian stimulation with the incidence in both age-matched unexposed women in the general population and unexposed infertile women.
There was no significant increase in the risk for breast cancer among women treated with any ovarian stimulation drug (pooled odds ratio, 1.03; 95% confidence interval, 0.86-1.23, but with substantial heterogeneity between study outcomes).
There was also no increased risk when the analysis was limited to the eight studies in which women were treated with both gonadotropins and clomiphene citrate (pooled OR, 0.92; 95% CI, 0.52-1.60, with substantial heterogeneity).
The authors noted that, among the many study limitations, no distinction was made between physiological dosing for anovulation and supraphysiological dosing for in vitro fertilization cycles. In addition, because the treated women were generally young, the follow-up period fell short of the age at which they’d be most at risk for breast cancer.
Individual patient data were also not available, but 14 studies did adjust for confounders, including weight, race, parity, age at first birth, age at menarche, and family history of breast cancer.
Although the findings are reassuring, “further long-term and detailed studies are now needed to confirm” them, Kotryna Temcinaite, PhD, senior research communications manager at the U.K. charity Breast Cancer Now, said in the press release.
A version of this article first appeared on Medscape.com.
Racial and economic disparities persist in endometrial cancer care
Women who were Black, Latina, American Indian, or Alaska Native were significantly less likely than White women to receive guidelines-adherent treatment for endometrial cancer, based on data from more than 80,000 women.
The incidence of uterine cancer has increased across all ethnicities in recent decades, and adherence to the National Comprehensive Cancer Network treatment guidelines has been associated with improved survival, wrote Victoria A. Rodriguez, MSW, MPH, of the University of California, Irvine, and colleagues. “To date, however, there are few studies that have looked at endometrial cancer disparities with adherence to National Comprehensive Cancer Network treatment guidelines.”
In a retrospective study published in Obstetrics & Gynecology, the researchers used data from the SEER (Surveillance, Epidemiology, and End Results) database between Jan. 1, 2006, and Dec. 31, 2015. The study population included 83,883 women aged 18 years and older who were diagnosed with their first or only endometrial carcinoma. The primary dependent variable was adherence to the NCCN guidelines for the initial course of treatment, which included a combination of therapies based on cancer subtype and the extent of the disease, the researchers said.
The researchers combined the guidelines and the corresponding data from the SEER database to create “a binary variable representing adherence to [NCCN] guidelines (1 = adherent treatment, 0 = nonadherent treatment).”
Approximately 60% of the total patient population received guidelines-adherent treatment. In a multivariate analysis, Black women, Latina women, and American Indian or Alaska Native women were significantly less likely than White women to receive such treatment (odds ratios, 0.88, 0.92, and 0.82, respectively), controlling for factors including neighborhood socioeconomic status, age, and stage at diagnosis, year of diagnosis, histology, and disease grade. Asian women and Native Hawaiian/Pacific Islander women were significantly more likely to received guidelines-adherent treatment, compared with White women (OR, 1.14 and 1.19, respectively).
The researchers also found a significant gradient in guidelines-adherent treatment based on neighborhood socioeconomic status. Relative to the highest neighborhood socioeconomic status group, women in the lower groups had significantly lower odds of receiving guidelines-adherent treatment, with ORs of 0.89, 0.84, 0.80, and 0.73, respectively, for the high-middle neighborhood socioeconomic group, the middle group, the low-middle group, and the lowest group (P < .001 for all).
“Our study is novel in that it examines neighborhood socioeconomic disparities in the understudied context of treatment adherence for endometrial cancer,” the researchers noted.
The study findings were limited by several factors in including the retrospective design and potential for unmeasured confounding variables not included in SEER, such as hospital and physician characteristics, the researchers said. Also, the SEER data set was limited to only the first course of treatment, and did not include information on patient comorbidities that might affect treatment.
“Future research should qualitatively explore reasons for nonadherent treatment within endometrial cancer and other cancer sites among various racial-ethnic groups and socioeconomic status groups, with special attention to low-income women of color,” the researchers emphasized. More research on the impact of comorbidities on a patient’s ability to receive guidelines-based care should be used to inform whether comorbidities should be part of the NCCN guidelines.
However, the results were strengthened by the large sample size and diverse population, so the findings are generalizable to the overall U.S. population, the researchers said.
“Interventions are needed to ensure that equitable cancer treatment practices are available for all individuals regardless of their racial-ethnic or socioeconomic backgrounds,” they concluded.
Pursue optimal treatment to curb mortality
Even more concerning than the increase in the incidence of endometrial cancer in the United States is the increase in mortality from this disease, said Emma C. Rossi, MD, of the University of North Carolina at Chapel Hill, in an interview.
“Therefore, it is critical that we identify factors which might be contributing to the increasing lethality of this cancer,” she emphasized. “One such potential factor is race, as it has been observed that Black race is associated with an increased risk of death from endometrial cancer. Historically, this was attributed to the more aggressive subtypes of endometrial cancer (such as serous) which have a higher incidence among Black women. However, more recently, population-based studies have identified that this worse prognosis is independent of histologic cell type,” which suggests that something in our health care delivery is contributing to these worse outcomes.
“The present study helps to confirm these concerning associations, shedding some light on contributory factors, in this case, modifiable (adherence to recommended guidelines) and less modifiable (neighborhood socioeconomic environments) [ones],” Dr. Rossi noted. “The guidelines that are established by the NCCN are chosen after they have been shown to be associated with improved outcomes (including either survival or quality of life), and therefore lack of adherence to these outcomes may suggest inferior quality care is being delivered.”
Studies such as this are helpful in exposing the problem of treatment disparity to help identify sources of problems to develop solutions, she added.
The results should inspire clinicians “to feel agency in changing these outcomes, albeit by tackling very difficult social, political, and health system shortfalls,” she said.
Identify barriers to care
Barriers to greater adherence to guidelines-based care include varying definitions of such care, Dr. Rossi said.
“This is particularly true for surgical management of endometrial cancer, which remains controversial with respect to lymph node assessment. Lack of surgical staging with lymph node assessment was considered noncompliant care for this study; however, lymphadenectomy has not specifically, in and of itself, been associated with improved outcomes, and therefore some surgeons argue against performing it routinely,” she explained.
“Lack of access to sophisticated surgical tools and advanced surgical techniques may account for nonguidelines-based care in the patients with early-stage endometrial cancer; however, there are likely other differences in the ability to deliver guideline-concordant care (such as chemotherapy and radiation therapy) for advanced-stage cancers,” Dr. Rossi said. “Patient and provider positive attitudes toward adjuvant therapy, access to transportation, supportive home environments, paid sick leave, well-controlled or minimal comorbidities are all factors which promote the administration of complex adjuvant therapies such as chemotherapy and radiation. In low-resource neighborhoods and minority communities, barriers to these factors may be contributing to nonguidelines-concordant care.”
Dr. Rossi emphasized the need to “dive deeper into these data at individual health-system and provider levels.” For example, research is needed to compare the practice patterns and models of high-performing clinical practices with lower-performing practices in terms of factors such as tumor boards, journal review, peer review, dashboards, and metrics. By doing so, “we can ensure that we are understanding where and why variations in care are occurring,” Dr. Rossi said.
The study was supported in part by the Faculty Mentor Program Fellowship from the University of California, Irvine, graduate division. Ms. Rodriguez was supported in part by a grant from the National Cancer Institute. The researchers had no financial conflicts to disclose. Dr. Rossi had no financial conflicts to disclose.
Women who were Black, Latina, American Indian, or Alaska Native were significantly less likely than White women to receive guidelines-adherent treatment for endometrial cancer, based on data from more than 80,000 women.
The incidence of uterine cancer has increased across all ethnicities in recent decades, and adherence to the National Comprehensive Cancer Network treatment guidelines has been associated with improved survival, wrote Victoria A. Rodriguez, MSW, MPH, of the University of California, Irvine, and colleagues. “To date, however, there are few studies that have looked at endometrial cancer disparities with adherence to National Comprehensive Cancer Network treatment guidelines.”
In a retrospective study published in Obstetrics & Gynecology, the researchers used data from the SEER (Surveillance, Epidemiology, and End Results) database between Jan. 1, 2006, and Dec. 31, 2015. The study population included 83,883 women aged 18 years and older who were diagnosed with their first or only endometrial carcinoma. The primary dependent variable was adherence to the NCCN guidelines for the initial course of treatment, which included a combination of therapies based on cancer subtype and the extent of the disease, the researchers said.
The researchers combined the guidelines and the corresponding data from the SEER database to create “a binary variable representing adherence to [NCCN] guidelines (1 = adherent treatment, 0 = nonadherent treatment).”
Approximately 60% of the total patient population received guidelines-adherent treatment. In a multivariate analysis, Black women, Latina women, and American Indian or Alaska Native women were significantly less likely than White women to receive such treatment (odds ratios, 0.88, 0.92, and 0.82, respectively), controlling for factors including neighborhood socioeconomic status, age, and stage at diagnosis, year of diagnosis, histology, and disease grade. Asian women and Native Hawaiian/Pacific Islander women were significantly more likely to received guidelines-adherent treatment, compared with White women (OR, 1.14 and 1.19, respectively).
The researchers also found a significant gradient in guidelines-adherent treatment based on neighborhood socioeconomic status. Relative to the highest neighborhood socioeconomic status group, women in the lower groups had significantly lower odds of receiving guidelines-adherent treatment, with ORs of 0.89, 0.84, 0.80, and 0.73, respectively, for the high-middle neighborhood socioeconomic group, the middle group, the low-middle group, and the lowest group (P < .001 for all).
“Our study is novel in that it examines neighborhood socioeconomic disparities in the understudied context of treatment adherence for endometrial cancer,” the researchers noted.
The study findings were limited by several factors in including the retrospective design and potential for unmeasured confounding variables not included in SEER, such as hospital and physician characteristics, the researchers said. Also, the SEER data set was limited to only the first course of treatment, and did not include information on patient comorbidities that might affect treatment.
“Future research should qualitatively explore reasons for nonadherent treatment within endometrial cancer and other cancer sites among various racial-ethnic groups and socioeconomic status groups, with special attention to low-income women of color,” the researchers emphasized. More research on the impact of comorbidities on a patient’s ability to receive guidelines-based care should be used to inform whether comorbidities should be part of the NCCN guidelines.
However, the results were strengthened by the large sample size and diverse population, so the findings are generalizable to the overall U.S. population, the researchers said.
“Interventions are needed to ensure that equitable cancer treatment practices are available for all individuals regardless of their racial-ethnic or socioeconomic backgrounds,” they concluded.
Pursue optimal treatment to curb mortality
Even more concerning than the increase in the incidence of endometrial cancer in the United States is the increase in mortality from this disease, said Emma C. Rossi, MD, of the University of North Carolina at Chapel Hill, in an interview.
“Therefore, it is critical that we identify factors which might be contributing to the increasing lethality of this cancer,” she emphasized. “One such potential factor is race, as it has been observed that Black race is associated with an increased risk of death from endometrial cancer. Historically, this was attributed to the more aggressive subtypes of endometrial cancer (such as serous) which have a higher incidence among Black women. However, more recently, population-based studies have identified that this worse prognosis is independent of histologic cell type,” which suggests that something in our health care delivery is contributing to these worse outcomes.
“The present study helps to confirm these concerning associations, shedding some light on contributory factors, in this case, modifiable (adherence to recommended guidelines) and less modifiable (neighborhood socioeconomic environments) [ones],” Dr. Rossi noted. “The guidelines that are established by the NCCN are chosen after they have been shown to be associated with improved outcomes (including either survival or quality of life), and therefore lack of adherence to these outcomes may suggest inferior quality care is being delivered.”
Studies such as this are helpful in exposing the problem of treatment disparity to help identify sources of problems to develop solutions, she added.
The results should inspire clinicians “to feel agency in changing these outcomes, albeit by tackling very difficult social, political, and health system shortfalls,” she said.
Identify barriers to care
Barriers to greater adherence to guidelines-based care include varying definitions of such care, Dr. Rossi said.
“This is particularly true for surgical management of endometrial cancer, which remains controversial with respect to lymph node assessment. Lack of surgical staging with lymph node assessment was considered noncompliant care for this study; however, lymphadenectomy has not specifically, in and of itself, been associated with improved outcomes, and therefore some surgeons argue against performing it routinely,” she explained.
“Lack of access to sophisticated surgical tools and advanced surgical techniques may account for nonguidelines-based care in the patients with early-stage endometrial cancer; however, there are likely other differences in the ability to deliver guideline-concordant care (such as chemotherapy and radiation therapy) for advanced-stage cancers,” Dr. Rossi said. “Patient and provider positive attitudes toward adjuvant therapy, access to transportation, supportive home environments, paid sick leave, well-controlled or minimal comorbidities are all factors which promote the administration of complex adjuvant therapies such as chemotherapy and radiation. In low-resource neighborhoods and minority communities, barriers to these factors may be contributing to nonguidelines-concordant care.”
Dr. Rossi emphasized the need to “dive deeper into these data at individual health-system and provider levels.” For example, research is needed to compare the practice patterns and models of high-performing clinical practices with lower-performing practices in terms of factors such as tumor boards, journal review, peer review, dashboards, and metrics. By doing so, “we can ensure that we are understanding where and why variations in care are occurring,” Dr. Rossi said.
The study was supported in part by the Faculty Mentor Program Fellowship from the University of California, Irvine, graduate division. Ms. Rodriguez was supported in part by a grant from the National Cancer Institute. The researchers had no financial conflicts to disclose. Dr. Rossi had no financial conflicts to disclose.
Women who were Black, Latina, American Indian, or Alaska Native were significantly less likely than White women to receive guidelines-adherent treatment for endometrial cancer, based on data from more than 80,000 women.
The incidence of uterine cancer has increased across all ethnicities in recent decades, and adherence to the National Comprehensive Cancer Network treatment guidelines has been associated with improved survival, wrote Victoria A. Rodriguez, MSW, MPH, of the University of California, Irvine, and colleagues. “To date, however, there are few studies that have looked at endometrial cancer disparities with adherence to National Comprehensive Cancer Network treatment guidelines.”
In a retrospective study published in Obstetrics & Gynecology, the researchers used data from the SEER (Surveillance, Epidemiology, and End Results) database between Jan. 1, 2006, and Dec. 31, 2015. The study population included 83,883 women aged 18 years and older who were diagnosed with their first or only endometrial carcinoma. The primary dependent variable was adherence to the NCCN guidelines for the initial course of treatment, which included a combination of therapies based on cancer subtype and the extent of the disease, the researchers said.
The researchers combined the guidelines and the corresponding data from the SEER database to create “a binary variable representing adherence to [NCCN] guidelines (1 = adherent treatment, 0 = nonadherent treatment).”
Approximately 60% of the total patient population received guidelines-adherent treatment. In a multivariate analysis, Black women, Latina women, and American Indian or Alaska Native women were significantly less likely than White women to receive such treatment (odds ratios, 0.88, 0.92, and 0.82, respectively), controlling for factors including neighborhood socioeconomic status, age, and stage at diagnosis, year of diagnosis, histology, and disease grade. Asian women and Native Hawaiian/Pacific Islander women were significantly more likely to received guidelines-adherent treatment, compared with White women (OR, 1.14 and 1.19, respectively).
The researchers also found a significant gradient in guidelines-adherent treatment based on neighborhood socioeconomic status. Relative to the highest neighborhood socioeconomic status group, women in the lower groups had significantly lower odds of receiving guidelines-adherent treatment, with ORs of 0.89, 0.84, 0.80, and 0.73, respectively, for the high-middle neighborhood socioeconomic group, the middle group, the low-middle group, and the lowest group (P < .001 for all).
“Our study is novel in that it examines neighborhood socioeconomic disparities in the understudied context of treatment adherence for endometrial cancer,” the researchers noted.
The study findings were limited by several factors in including the retrospective design and potential for unmeasured confounding variables not included in SEER, such as hospital and physician characteristics, the researchers said. Also, the SEER data set was limited to only the first course of treatment, and did not include information on patient comorbidities that might affect treatment.
“Future research should qualitatively explore reasons for nonadherent treatment within endometrial cancer and other cancer sites among various racial-ethnic groups and socioeconomic status groups, with special attention to low-income women of color,” the researchers emphasized. More research on the impact of comorbidities on a patient’s ability to receive guidelines-based care should be used to inform whether comorbidities should be part of the NCCN guidelines.
However, the results were strengthened by the large sample size and diverse population, so the findings are generalizable to the overall U.S. population, the researchers said.
“Interventions are needed to ensure that equitable cancer treatment practices are available for all individuals regardless of their racial-ethnic or socioeconomic backgrounds,” they concluded.
Pursue optimal treatment to curb mortality
Even more concerning than the increase in the incidence of endometrial cancer in the United States is the increase in mortality from this disease, said Emma C. Rossi, MD, of the University of North Carolina at Chapel Hill, in an interview.
“Therefore, it is critical that we identify factors which might be contributing to the increasing lethality of this cancer,” she emphasized. “One such potential factor is race, as it has been observed that Black race is associated with an increased risk of death from endometrial cancer. Historically, this was attributed to the more aggressive subtypes of endometrial cancer (such as serous) which have a higher incidence among Black women. However, more recently, population-based studies have identified that this worse prognosis is independent of histologic cell type,” which suggests that something in our health care delivery is contributing to these worse outcomes.
“The present study helps to confirm these concerning associations, shedding some light on contributory factors, in this case, modifiable (adherence to recommended guidelines) and less modifiable (neighborhood socioeconomic environments) [ones],” Dr. Rossi noted. “The guidelines that are established by the NCCN are chosen after they have been shown to be associated with improved outcomes (including either survival or quality of life), and therefore lack of adherence to these outcomes may suggest inferior quality care is being delivered.”
Studies such as this are helpful in exposing the problem of treatment disparity to help identify sources of problems to develop solutions, she added.
The results should inspire clinicians “to feel agency in changing these outcomes, albeit by tackling very difficult social, political, and health system shortfalls,” she said.
Identify barriers to care
Barriers to greater adherence to guidelines-based care include varying definitions of such care, Dr. Rossi said.
“This is particularly true for surgical management of endometrial cancer, which remains controversial with respect to lymph node assessment. Lack of surgical staging with lymph node assessment was considered noncompliant care for this study; however, lymphadenectomy has not specifically, in and of itself, been associated with improved outcomes, and therefore some surgeons argue against performing it routinely,” she explained.
“Lack of access to sophisticated surgical tools and advanced surgical techniques may account for nonguidelines-based care in the patients with early-stage endometrial cancer; however, there are likely other differences in the ability to deliver guideline-concordant care (such as chemotherapy and radiation therapy) for advanced-stage cancers,” Dr. Rossi said. “Patient and provider positive attitudes toward adjuvant therapy, access to transportation, supportive home environments, paid sick leave, well-controlled or minimal comorbidities are all factors which promote the administration of complex adjuvant therapies such as chemotherapy and radiation. In low-resource neighborhoods and minority communities, barriers to these factors may be contributing to nonguidelines-concordant care.”
Dr. Rossi emphasized the need to “dive deeper into these data at individual health-system and provider levels.” For example, research is needed to compare the practice patterns and models of high-performing clinical practices with lower-performing practices in terms of factors such as tumor boards, journal review, peer review, dashboards, and metrics. By doing so, “we can ensure that we are understanding where and why variations in care are occurring,” Dr. Rossi said.
The study was supported in part by the Faculty Mentor Program Fellowship from the University of California, Irvine, graduate division. Ms. Rodriguez was supported in part by a grant from the National Cancer Institute. The researchers had no financial conflicts to disclose. Dr. Rossi had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Early-onset CRC associated with longer survival
Individuals diagnosed with primary colorectal cancer (CRC) at less than 50 years of age have better survival outcomes than individuals diagnosed at 51-55 years, based on data from more than 750,000 patients.
This finding emphasizes the importance of early CRC detection in younger individuals, reported lead author En Cheng, MD, PhD, of Yale University, New Haven, Conn., and colleagues.
“Early-onset CRC (i.e., CRC diagnosed at age less than 50 years) has been characterized by unique clinical, genetic, and epigenetic characteristics, and thus it may be associated with different survival from CRC diagnosed among individuals older than 50 years,” the investigators wrote in JAMA Network Open. Previous studies comparing survival times across age groups have yielded inconsistent results.
To gain a better understanding, the investigator conducted a retrospective study using data from the National Cancer Database. Excluding patients with primary CRC who had concomitant diagnosis, history of other malignant tumors, noninvasive adenocarcinoma, or missing data, the final dataset included 769,871 patients. Early-onset CRC was defined by age less than 50 years, whereas later-onset CRC was defined by ages 51-55 years.
“Individuals diagnosed at age 50 years were excluded to minimize an apparent screening detection bias at age 50 years in our population, given that these individuals disproportionately presented with earlier stages,” the investigators wrote.
Initial comparisons across groups revealed several significant differences. Individuals in the early-onset group were more often women (47.3% vs. 43.8%; P < .001), members of races in the “other” category (6.9% vs. 5.9%; P < .001), and Medicaid patients (12.3% vs. 10.3%; P < .001). They were also more likely to be diagnosed with stage IV cancer (27.8% vs 24.1%; P < .001) and have rectal tumors (29.3% vs. 28.7%; P = .004).
In the unadjusted Kaplan-Meier analysis, patients with early-onset CRC had a lower 10-year survival rate (53.6%; 95% CI, 53.2%-54.0% vs. 54.3%; 95% CI, 53.8%-54.8%; P < .001). The fully adjusted model revealed significantly higher survival for early-onset patients, compared with later-onset patients (adjusted hazard ratio, 0.95; 95% CI, 0.93-0.96; P < .001) . This disparity deepened when adjusting only for stage (HR, 0.89; 95% CI, 0.88-0.90; P < .001).
Survival was longest among patients 35-39 years (aHR, 0.88; 95% CI, 0.84-0.92; P < .001), compared with those aged 51-55, and among early-onset individuals with stage I disease (a HR, 0.87; 95% CI, 0.81-0.93; P < .001) or stage II disease (a HR, 0.86; 95% CI, 0.82-0.90; P < .001), compared with those having the same stages of later-onset CRC. No survival advantage was observed among patients diagnosed at age 25 or younger or those with stage III or IV disease.
“Interestingly, hereditary nonpolyposis colorectal cancer, owing to underlying mismatch repair deficiency, is associated with superior survival and is often diagnosed in individuals from ages 35-45 years,” the investigators noted. “In contrast, adenomatous polyposis coli syndrome is more common in individuals who are diagnosed with CRC at age younger than 20 years (10%), compared with those diagnosed at later ages (0.1%), and adenomatous polyposis coli syndrome is not associated with a survival advantage. These high penetrance syndromes could partly account for the relative heterogeneity in survival across ages among individuals with early-onset CRC.”
Cautious about interpretation
Dr. Cheng and colleagues concluded their publication with a disclaimer: “Our finding of a survival advantage associated with early-onset CRC among younger individuals should be interpreted cautiously, given that the advantage had a small magnitude and was heterogeneous by age and stage,” they wrote. “Further study is needed to understand the underlying heterogeneity of survival by age and stage among individuals with early-onset CRC.”
Kirbi L. Yelorda, MD, of Stanford (Calif.) University, and colleagues, had a similar interpretation.
“These results offer support for effectiveness of treatment in patients diagnosed with CRC at younger ages; however, they must be interpreted within the context of epidemiological and biological factors,” Dr. Yelorda and colleagues wrote in an accompanying editorial.
The findings also suggest that the recent reduction in recommended screening age by the U.S. Preventive Services Task Force – from 50 years to 45 years – is warranted, they added, but screening younger patients remains unnecessary.
“While these results do not suggest that screening should start for patients younger than 45 years, they do support the benefit of early detection in young patients,” Dr. Yelorda and colleagues wrote, noting a “fairly low incidence rate” among individuals younger than 45, which is insufficient to justify the risk-to-benefit ratio and increased costs associated with expanded screening.
Important but not surprising
It’s “not surprising” that early-onset patients typically have better survival than later-onset patients, according to Joseph C. Anderson, MD, associate professor at White River Junction Veterans Affairs Medical Center, Hartford, Vt.; Geisel School of Medicine at Dartmouth, Hanover, N.H.; and the University of Connecticut, Farmington.
“They’re younger, have less comorbidities, and can tolerate chemotherapy,” Dr. Anderson said in an interview. “It’s not surprising that people do poorly with later stages. Younger people are no exception.”
Dr. Anderson, who previously coauthored an editorial weighing the pros and cons of earlier screening, noted that earlier screening is needed because of the rising incidence of late-stage diagnoses among younger patients, which, as the study found, are associated with worse outcomes.
Beyond adherence to screening recommendations, Dr. Anderson urged clinicians to be aggressive when doing a workup of CRC symptoms in younger patients, among whom delayed diagnoses are more common.
“We can’t just say it’s something more benign, like hemorrhoids, like we used to,” Dr. Anderson said. “Somebody who’s 30 years old and having rectal bleeding needs to be evaluated promptly – there can’t be a delay.”
The study was supported by the National Institutes of Health and Stand Up To Cancer (grant administered by the American Association for Cancer Research). The investigators disclosed relationships with Evergrande Group, Janssen, Revolution Medicines, and others. One editorialist reported serving as a member of the USPSTF when the guideline for colorectal cancer was developed, and being a coauthor on the guideline. No other disclosures were reported among editorialists. Dr. Anderson reported no relevant conflicts of interest.
Individuals diagnosed with primary colorectal cancer (CRC) at less than 50 years of age have better survival outcomes than individuals diagnosed at 51-55 years, based on data from more than 750,000 patients.
This finding emphasizes the importance of early CRC detection in younger individuals, reported lead author En Cheng, MD, PhD, of Yale University, New Haven, Conn., and colleagues.
“Early-onset CRC (i.e., CRC diagnosed at age less than 50 years) has been characterized by unique clinical, genetic, and epigenetic characteristics, and thus it may be associated with different survival from CRC diagnosed among individuals older than 50 years,” the investigators wrote in JAMA Network Open. Previous studies comparing survival times across age groups have yielded inconsistent results.
To gain a better understanding, the investigator conducted a retrospective study using data from the National Cancer Database. Excluding patients with primary CRC who had concomitant diagnosis, history of other malignant tumors, noninvasive adenocarcinoma, or missing data, the final dataset included 769,871 patients. Early-onset CRC was defined by age less than 50 years, whereas later-onset CRC was defined by ages 51-55 years.
“Individuals diagnosed at age 50 years were excluded to minimize an apparent screening detection bias at age 50 years in our population, given that these individuals disproportionately presented with earlier stages,” the investigators wrote.
Initial comparisons across groups revealed several significant differences. Individuals in the early-onset group were more often women (47.3% vs. 43.8%; P < .001), members of races in the “other” category (6.9% vs. 5.9%; P < .001), and Medicaid patients (12.3% vs. 10.3%; P < .001). They were also more likely to be diagnosed with stage IV cancer (27.8% vs 24.1%; P < .001) and have rectal tumors (29.3% vs. 28.7%; P = .004).
In the unadjusted Kaplan-Meier analysis, patients with early-onset CRC had a lower 10-year survival rate (53.6%; 95% CI, 53.2%-54.0% vs. 54.3%; 95% CI, 53.8%-54.8%; P < .001). The fully adjusted model revealed significantly higher survival for early-onset patients, compared with later-onset patients (adjusted hazard ratio, 0.95; 95% CI, 0.93-0.96; P < .001) . This disparity deepened when adjusting only for stage (HR, 0.89; 95% CI, 0.88-0.90; P < .001).
Survival was longest among patients 35-39 years (aHR, 0.88; 95% CI, 0.84-0.92; P < .001), compared with those aged 51-55, and among early-onset individuals with stage I disease (a HR, 0.87; 95% CI, 0.81-0.93; P < .001) or stage II disease (a HR, 0.86; 95% CI, 0.82-0.90; P < .001), compared with those having the same stages of later-onset CRC. No survival advantage was observed among patients diagnosed at age 25 or younger or those with stage III or IV disease.
“Interestingly, hereditary nonpolyposis colorectal cancer, owing to underlying mismatch repair deficiency, is associated with superior survival and is often diagnosed in individuals from ages 35-45 years,” the investigators noted. “In contrast, adenomatous polyposis coli syndrome is more common in individuals who are diagnosed with CRC at age younger than 20 years (10%), compared with those diagnosed at later ages (0.1%), and adenomatous polyposis coli syndrome is not associated with a survival advantage. These high penetrance syndromes could partly account for the relative heterogeneity in survival across ages among individuals with early-onset CRC.”
Cautious about interpretation
Dr. Cheng and colleagues concluded their publication with a disclaimer: “Our finding of a survival advantage associated with early-onset CRC among younger individuals should be interpreted cautiously, given that the advantage had a small magnitude and was heterogeneous by age and stage,” they wrote. “Further study is needed to understand the underlying heterogeneity of survival by age and stage among individuals with early-onset CRC.”
Kirbi L. Yelorda, MD, of Stanford (Calif.) University, and colleagues, had a similar interpretation.
“These results offer support for effectiveness of treatment in patients diagnosed with CRC at younger ages; however, they must be interpreted within the context of epidemiological and biological factors,” Dr. Yelorda and colleagues wrote in an accompanying editorial.
The findings also suggest that the recent reduction in recommended screening age by the U.S. Preventive Services Task Force – from 50 years to 45 years – is warranted, they added, but screening younger patients remains unnecessary.
“While these results do not suggest that screening should start for patients younger than 45 years, they do support the benefit of early detection in young patients,” Dr. Yelorda and colleagues wrote, noting a “fairly low incidence rate” among individuals younger than 45, which is insufficient to justify the risk-to-benefit ratio and increased costs associated with expanded screening.
Important but not surprising
It’s “not surprising” that early-onset patients typically have better survival than later-onset patients, according to Joseph C. Anderson, MD, associate professor at White River Junction Veterans Affairs Medical Center, Hartford, Vt.; Geisel School of Medicine at Dartmouth, Hanover, N.H.; and the University of Connecticut, Farmington.
“They’re younger, have less comorbidities, and can tolerate chemotherapy,” Dr. Anderson said in an interview. “It’s not surprising that people do poorly with later stages. Younger people are no exception.”
Dr. Anderson, who previously coauthored an editorial weighing the pros and cons of earlier screening, noted that earlier screening is needed because of the rising incidence of late-stage diagnoses among younger patients, which, as the study found, are associated with worse outcomes.
Beyond adherence to screening recommendations, Dr. Anderson urged clinicians to be aggressive when doing a workup of CRC symptoms in younger patients, among whom delayed diagnoses are more common.
“We can’t just say it’s something more benign, like hemorrhoids, like we used to,” Dr. Anderson said. “Somebody who’s 30 years old and having rectal bleeding needs to be evaluated promptly – there can’t be a delay.”
The study was supported by the National Institutes of Health and Stand Up To Cancer (grant administered by the American Association for Cancer Research). The investigators disclosed relationships with Evergrande Group, Janssen, Revolution Medicines, and others. One editorialist reported serving as a member of the USPSTF when the guideline for colorectal cancer was developed, and being a coauthor on the guideline. No other disclosures were reported among editorialists. Dr. Anderson reported no relevant conflicts of interest.
Individuals diagnosed with primary colorectal cancer (CRC) at less than 50 years of age have better survival outcomes than individuals diagnosed at 51-55 years, based on data from more than 750,000 patients.
This finding emphasizes the importance of early CRC detection in younger individuals, reported lead author En Cheng, MD, PhD, of Yale University, New Haven, Conn., and colleagues.
“Early-onset CRC (i.e., CRC diagnosed at age less than 50 years) has been characterized by unique clinical, genetic, and epigenetic characteristics, and thus it may be associated with different survival from CRC diagnosed among individuals older than 50 years,” the investigators wrote in JAMA Network Open. Previous studies comparing survival times across age groups have yielded inconsistent results.
To gain a better understanding, the investigator conducted a retrospective study using data from the National Cancer Database. Excluding patients with primary CRC who had concomitant diagnosis, history of other malignant tumors, noninvasive adenocarcinoma, or missing data, the final dataset included 769,871 patients. Early-onset CRC was defined by age less than 50 years, whereas later-onset CRC was defined by ages 51-55 years.
“Individuals diagnosed at age 50 years were excluded to minimize an apparent screening detection bias at age 50 years in our population, given that these individuals disproportionately presented with earlier stages,” the investigators wrote.
Initial comparisons across groups revealed several significant differences. Individuals in the early-onset group were more often women (47.3% vs. 43.8%; P < .001), members of races in the “other” category (6.9% vs. 5.9%; P < .001), and Medicaid patients (12.3% vs. 10.3%; P < .001). They were also more likely to be diagnosed with stage IV cancer (27.8% vs 24.1%; P < .001) and have rectal tumors (29.3% vs. 28.7%; P = .004).
In the unadjusted Kaplan-Meier analysis, patients with early-onset CRC had a lower 10-year survival rate (53.6%; 95% CI, 53.2%-54.0% vs. 54.3%; 95% CI, 53.8%-54.8%; P < .001). The fully adjusted model revealed significantly higher survival for early-onset patients, compared with later-onset patients (adjusted hazard ratio, 0.95; 95% CI, 0.93-0.96; P < .001) . This disparity deepened when adjusting only for stage (HR, 0.89; 95% CI, 0.88-0.90; P < .001).
Survival was longest among patients 35-39 years (aHR, 0.88; 95% CI, 0.84-0.92; P < .001), compared with those aged 51-55, and among early-onset individuals with stage I disease (a HR, 0.87; 95% CI, 0.81-0.93; P < .001) or stage II disease (a HR, 0.86; 95% CI, 0.82-0.90; P < .001), compared with those having the same stages of later-onset CRC. No survival advantage was observed among patients diagnosed at age 25 or younger or those with stage III or IV disease.
“Interestingly, hereditary nonpolyposis colorectal cancer, owing to underlying mismatch repair deficiency, is associated with superior survival and is often diagnosed in individuals from ages 35-45 years,” the investigators noted. “In contrast, adenomatous polyposis coli syndrome is more common in individuals who are diagnosed with CRC at age younger than 20 years (10%), compared with those diagnosed at later ages (0.1%), and adenomatous polyposis coli syndrome is not associated with a survival advantage. These high penetrance syndromes could partly account for the relative heterogeneity in survival across ages among individuals with early-onset CRC.”
Cautious about interpretation
Dr. Cheng and colleagues concluded their publication with a disclaimer: “Our finding of a survival advantage associated with early-onset CRC among younger individuals should be interpreted cautiously, given that the advantage had a small magnitude and was heterogeneous by age and stage,” they wrote. “Further study is needed to understand the underlying heterogeneity of survival by age and stage among individuals with early-onset CRC.”
Kirbi L. Yelorda, MD, of Stanford (Calif.) University, and colleagues, had a similar interpretation.
“These results offer support for effectiveness of treatment in patients diagnosed with CRC at younger ages; however, they must be interpreted within the context of epidemiological and biological factors,” Dr. Yelorda and colleagues wrote in an accompanying editorial.
The findings also suggest that the recent reduction in recommended screening age by the U.S. Preventive Services Task Force – from 50 years to 45 years – is warranted, they added, but screening younger patients remains unnecessary.
“While these results do not suggest that screening should start for patients younger than 45 years, they do support the benefit of early detection in young patients,” Dr. Yelorda and colleagues wrote, noting a “fairly low incidence rate” among individuals younger than 45, which is insufficient to justify the risk-to-benefit ratio and increased costs associated with expanded screening.
Important but not surprising
It’s “not surprising” that early-onset patients typically have better survival than later-onset patients, according to Joseph C. Anderson, MD, associate professor at White River Junction Veterans Affairs Medical Center, Hartford, Vt.; Geisel School of Medicine at Dartmouth, Hanover, N.H.; and the University of Connecticut, Farmington.
“They’re younger, have less comorbidities, and can tolerate chemotherapy,” Dr. Anderson said in an interview. “It’s not surprising that people do poorly with later stages. Younger people are no exception.”
Dr. Anderson, who previously coauthored an editorial weighing the pros and cons of earlier screening, noted that earlier screening is needed because of the rising incidence of late-stage diagnoses among younger patients, which, as the study found, are associated with worse outcomes.
Beyond adherence to screening recommendations, Dr. Anderson urged clinicians to be aggressive when doing a workup of CRC symptoms in younger patients, among whom delayed diagnoses are more common.
“We can’t just say it’s something more benign, like hemorrhoids, like we used to,” Dr. Anderson said. “Somebody who’s 30 years old and having rectal bleeding needs to be evaluated promptly – there can’t be a delay.”
The study was supported by the National Institutes of Health and Stand Up To Cancer (grant administered by the American Association for Cancer Research). The investigators disclosed relationships with Evergrande Group, Janssen, Revolution Medicines, and others. One editorialist reported serving as a member of the USPSTF when the guideline for colorectal cancer was developed, and being a coauthor on the guideline. No other disclosures were reported among editorialists. Dr. Anderson reported no relevant conflicts of interest.
FROM JAMA NETWORK OPEN
Ponatinib/blinatumomab start strong against Ph+ALL
For adults with Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL), frontline therapy with the chemotherapy-free combination of ponatinib (Iclusig) and blinatumomab (Blincyto) shows promise as an alternative to early hematopoietic stem cell transplantation (HSCT), investigators in a single-arm phase 2 study reported.
In an interim analysis of the combination in patients with newly diagnosed or relapsed/refractory Ph+ALL or lymphoid accelerated or blast phase chronic myeloid leukemia (CML), 20 patients who received it as frontline therapy had a rate of complete responses (CR) or complete responses with partial recovery of blood counts (CRp) of 100% and a complete molecular remission (CMR) rate of 85%, reported Nicholas Short, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“This translated into an estimated 2-year overall survival of 93%, with no patients undergoing transplant in first remission, and none having relapse at last follow-up,” he said in an oral abstract presented during the European Hematology Association annual congress.
Among patients with relapsed/refractory Ph+ALL, the CR/CRp rate was 89%, the CMR rate was 88%, and the estimated 2-year overall survival rate was 53%, he said.
Transplants on hold
“The big selling point is the ability to avoid stem cell transplant, which is not always the first thing you do in Ph-positive ALL, but it’s always on your mind,” said Gwen Nichols, MD, chief medical officer of the Leukemia and Lymphoma Society, who was not involved in the study.
“It looks, albeit with very limited follow-up, that patients haven’t relapsed yet such that transplant would be necessary. Anything we can do to avoid people having long-term complications that go along with an allogeneic transplant is a step in the right direction,” she said in an interview.
One combination, three cohorts
Ph+ALL comprises about 25% of all adult ALL. The standard of care in newly diagnosed patients is chemotherapy plus a tyrosine kinase inhibitor (TKI) targeted against the BCR-ABL transcript.
Ponatinib is a pan-BCR-ABL TKI that has been shown to have activity against ALL with T315I mutations, which are present in about 75% of the cases of relapsed disease, Dr. Short said.
Blinatumomab is a bi-specific T-cell engager (BiTe) that has been shown to be effective as monotherapy against relapsed/refractory Ph+ALL as monotherapy and in combination with dasatinib.
Dr. Short and colleagues enrolled patients with newly diagnosed or relapsed/refractory Ph+ALL or lymphoid accelerated or blast phase CML. Patients in the frontline cohort could have received one or two prior lines of chemotherapy with or without a TKI.
The patients all had Eastern Cooperative Oncology Group performance status of 0-2, and adequate liver function.
Patients with clinically significant cardiovascular disease or central nervous system disease pathology were excluded, except that patients with CNS leukemia could be enrolled.
The induction phase consisted of 30 mg ponatinib daily plus blinatumomab standard dosing on a 4-week-on, 2-week-off schedule. Patients in CMR, defined for frontline patients as undetectable BCR-ABL transcripts by polymerase chain reaction, then received up to four consolidation cycles of the regimen with ponatinib at a 15-mg dose, followed by 5 years of ponatinib 15-mg maintenance. All patients also received CNS prophylaxis with 12 cycles of intrathecal chemotherapy with alternating administration of methotrexate and cytarabine.
Of the 35 patients treated to date with the combination, 20 with Ph+ALL received it as frontline therapy and 10 received it for relapsed/refractory disease; 5 patients with CML in lymphoid blast phase also were treated.
High CMR, CR rates
As noted before, the CMR rate, the primary endpoint among patients with newly diagnosed Ph+ALL, was 85%, with a CR/CRp rate of 100%. Six of the patients in the frontline group and one in the salvage therapy group had CRs but were positive for minimal residual disease (MRD) at study outset.
The CR/CRp rate for the entire cohort of 28 patients (excluding those with a CR at start) was 96%, with only 1 patient who had relapsed/refractory disease not having a CR. This patient had received ponatinib in a prior salvage regimen.
The CMR rate among the entire cohort was 79%, with 85% of patients in the frontline ALL cohort having a CMR, 88% in the relapsed/refractory cohort, and 40% in the CML cohort. There were no early deaths among any patients.
“After one cycle of ponatinib plus blinatumomab, 84% of frontline patients had achieved at least a major molecular response, and 58% had achieved a CMR. Among those with relapsed/refractory Ph+ALL, 75% achieved CMR after one cycle of therapy,” Dr. Short said.
Of the 20 frontline patients in CR, one patient experienced visual changes and possible stroke that were considered possibly related to the study medication. This patient was taken off study. During a later maintenance regimen this patient developed a non-ST elevation myocardial infarction and died from postprocedural bleeding and hypovolemic shock following a cardiac catheterization procedure.
The remainder of patients in the frontline cohort had ongoing responses without the need for HSCT at last follow-up. There were no relapses, with a median duration of CR of 6 months,
Among the 10 with relapsed/refractory Ph+ALL, one did not have a response, and the remaining 9 had CR/CRps.
Of the latter groups, four went on to allogeneic HSCT and three were still alive; one patient who underwent a transplant experienced a relapse and died. One additional patient was alive with relapsed disease with T315I and E255V mutations at the time of relapse, one patient in CR who went off study due to insurance issues died from an unknown cause, and the three remaining patients had ongoing responses without transplant.
Among the five patients with CML in lymphoid blast phase, two had relapses, but both are still alive and currently in remission, and three have ongoing responses without transplant.
After a median follow-up of 12 months the 1-year event-free survival (EFS) rate for the entire 35-patient group was 76%, and the 2-year EFS was 70%.
The 1-year overall survival rate was 93%, and the 2-year OS rate was 80%.
Among patients in the frontline group, the 1-year and 2-year EFS and OS rates were all 93%.
For the relapsed/refractory cohort, the estimated 2-year EFS was 41% and OS was 53%. For the CML cohort, the 2-year EFS was 60%, with all patients still alive at last follow-up.
There were no grade 4 adverse events on study. Grade 3 adverse events considered at least possibly related to study treatment were elevated lipase, fever/febrile neutropenia, increased alanine aminotransferase, cerebrovascular ischemia, hypertension, pancreatitis, deep vein thrombosis, and encephalopathy. There were no cases of grade 3 cytokine release syndrome or tremor.
The study was sponsored by MD Anderson Cancer Center with collaboration from the National Cancer Institute, Amgen, and Takeda. Dr. Short has disclosed relationships with Amgen and Takeda. Dr. Nichols reported having no conflicts of interest.
For adults with Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL), frontline therapy with the chemotherapy-free combination of ponatinib (Iclusig) and blinatumomab (Blincyto) shows promise as an alternative to early hematopoietic stem cell transplantation (HSCT), investigators in a single-arm phase 2 study reported.
In an interim analysis of the combination in patients with newly diagnosed or relapsed/refractory Ph+ALL or lymphoid accelerated or blast phase chronic myeloid leukemia (CML), 20 patients who received it as frontline therapy had a rate of complete responses (CR) or complete responses with partial recovery of blood counts (CRp) of 100% and a complete molecular remission (CMR) rate of 85%, reported Nicholas Short, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“This translated into an estimated 2-year overall survival of 93%, with no patients undergoing transplant in first remission, and none having relapse at last follow-up,” he said in an oral abstract presented during the European Hematology Association annual congress.
Among patients with relapsed/refractory Ph+ALL, the CR/CRp rate was 89%, the CMR rate was 88%, and the estimated 2-year overall survival rate was 53%, he said.
Transplants on hold
“The big selling point is the ability to avoid stem cell transplant, which is not always the first thing you do in Ph-positive ALL, but it’s always on your mind,” said Gwen Nichols, MD, chief medical officer of the Leukemia and Lymphoma Society, who was not involved in the study.
“It looks, albeit with very limited follow-up, that patients haven’t relapsed yet such that transplant would be necessary. Anything we can do to avoid people having long-term complications that go along with an allogeneic transplant is a step in the right direction,” she said in an interview.
One combination, three cohorts
Ph+ALL comprises about 25% of all adult ALL. The standard of care in newly diagnosed patients is chemotherapy plus a tyrosine kinase inhibitor (TKI) targeted against the BCR-ABL transcript.
Ponatinib is a pan-BCR-ABL TKI that has been shown to have activity against ALL with T315I mutations, which are present in about 75% of the cases of relapsed disease, Dr. Short said.
Blinatumomab is a bi-specific T-cell engager (BiTe) that has been shown to be effective as monotherapy against relapsed/refractory Ph+ALL as monotherapy and in combination with dasatinib.
Dr. Short and colleagues enrolled patients with newly diagnosed or relapsed/refractory Ph+ALL or lymphoid accelerated or blast phase CML. Patients in the frontline cohort could have received one or two prior lines of chemotherapy with or without a TKI.
The patients all had Eastern Cooperative Oncology Group performance status of 0-2, and adequate liver function.
Patients with clinically significant cardiovascular disease or central nervous system disease pathology were excluded, except that patients with CNS leukemia could be enrolled.
The induction phase consisted of 30 mg ponatinib daily plus blinatumomab standard dosing on a 4-week-on, 2-week-off schedule. Patients in CMR, defined for frontline patients as undetectable BCR-ABL transcripts by polymerase chain reaction, then received up to four consolidation cycles of the regimen with ponatinib at a 15-mg dose, followed by 5 years of ponatinib 15-mg maintenance. All patients also received CNS prophylaxis with 12 cycles of intrathecal chemotherapy with alternating administration of methotrexate and cytarabine.
Of the 35 patients treated to date with the combination, 20 with Ph+ALL received it as frontline therapy and 10 received it for relapsed/refractory disease; 5 patients with CML in lymphoid blast phase also were treated.
High CMR, CR rates
As noted before, the CMR rate, the primary endpoint among patients with newly diagnosed Ph+ALL, was 85%, with a CR/CRp rate of 100%. Six of the patients in the frontline group and one in the salvage therapy group had CRs but were positive for minimal residual disease (MRD) at study outset.
The CR/CRp rate for the entire cohort of 28 patients (excluding those with a CR at start) was 96%, with only 1 patient who had relapsed/refractory disease not having a CR. This patient had received ponatinib in a prior salvage regimen.
The CMR rate among the entire cohort was 79%, with 85% of patients in the frontline ALL cohort having a CMR, 88% in the relapsed/refractory cohort, and 40% in the CML cohort. There were no early deaths among any patients.
“After one cycle of ponatinib plus blinatumomab, 84% of frontline patients had achieved at least a major molecular response, and 58% had achieved a CMR. Among those with relapsed/refractory Ph+ALL, 75% achieved CMR after one cycle of therapy,” Dr. Short said.
Of the 20 frontline patients in CR, one patient experienced visual changes and possible stroke that were considered possibly related to the study medication. This patient was taken off study. During a later maintenance regimen this patient developed a non-ST elevation myocardial infarction and died from postprocedural bleeding and hypovolemic shock following a cardiac catheterization procedure.
The remainder of patients in the frontline cohort had ongoing responses without the need for HSCT at last follow-up. There were no relapses, with a median duration of CR of 6 months,
Among the 10 with relapsed/refractory Ph+ALL, one did not have a response, and the remaining 9 had CR/CRps.
Of the latter groups, four went on to allogeneic HSCT and three were still alive; one patient who underwent a transplant experienced a relapse and died. One additional patient was alive with relapsed disease with T315I and E255V mutations at the time of relapse, one patient in CR who went off study due to insurance issues died from an unknown cause, and the three remaining patients had ongoing responses without transplant.
Among the five patients with CML in lymphoid blast phase, two had relapses, but both are still alive and currently in remission, and three have ongoing responses without transplant.
After a median follow-up of 12 months the 1-year event-free survival (EFS) rate for the entire 35-patient group was 76%, and the 2-year EFS was 70%.
The 1-year overall survival rate was 93%, and the 2-year OS rate was 80%.
Among patients in the frontline group, the 1-year and 2-year EFS and OS rates were all 93%.
For the relapsed/refractory cohort, the estimated 2-year EFS was 41% and OS was 53%. For the CML cohort, the 2-year EFS was 60%, with all patients still alive at last follow-up.
There were no grade 4 adverse events on study. Grade 3 adverse events considered at least possibly related to study treatment were elevated lipase, fever/febrile neutropenia, increased alanine aminotransferase, cerebrovascular ischemia, hypertension, pancreatitis, deep vein thrombosis, and encephalopathy. There were no cases of grade 3 cytokine release syndrome or tremor.
The study was sponsored by MD Anderson Cancer Center with collaboration from the National Cancer Institute, Amgen, and Takeda. Dr. Short has disclosed relationships with Amgen and Takeda. Dr. Nichols reported having no conflicts of interest.
For adults with Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ALL), frontline therapy with the chemotherapy-free combination of ponatinib (Iclusig) and blinatumomab (Blincyto) shows promise as an alternative to early hematopoietic stem cell transplantation (HSCT), investigators in a single-arm phase 2 study reported.
In an interim analysis of the combination in patients with newly diagnosed or relapsed/refractory Ph+ALL or lymphoid accelerated or blast phase chronic myeloid leukemia (CML), 20 patients who received it as frontline therapy had a rate of complete responses (CR) or complete responses with partial recovery of blood counts (CRp) of 100% and a complete molecular remission (CMR) rate of 85%, reported Nicholas Short, MD, of the University of Texas MD Anderson Cancer Center in Houston.
“This translated into an estimated 2-year overall survival of 93%, with no patients undergoing transplant in first remission, and none having relapse at last follow-up,” he said in an oral abstract presented during the European Hematology Association annual congress.
Among patients with relapsed/refractory Ph+ALL, the CR/CRp rate was 89%, the CMR rate was 88%, and the estimated 2-year overall survival rate was 53%, he said.
Transplants on hold
“The big selling point is the ability to avoid stem cell transplant, which is not always the first thing you do in Ph-positive ALL, but it’s always on your mind,” said Gwen Nichols, MD, chief medical officer of the Leukemia and Lymphoma Society, who was not involved in the study.
“It looks, albeit with very limited follow-up, that patients haven’t relapsed yet such that transplant would be necessary. Anything we can do to avoid people having long-term complications that go along with an allogeneic transplant is a step in the right direction,” she said in an interview.
One combination, three cohorts
Ph+ALL comprises about 25% of all adult ALL. The standard of care in newly diagnosed patients is chemotherapy plus a tyrosine kinase inhibitor (TKI) targeted against the BCR-ABL transcript.
Ponatinib is a pan-BCR-ABL TKI that has been shown to have activity against ALL with T315I mutations, which are present in about 75% of the cases of relapsed disease, Dr. Short said.
Blinatumomab is a bi-specific T-cell engager (BiTe) that has been shown to be effective as monotherapy against relapsed/refractory Ph+ALL as monotherapy and in combination with dasatinib.
Dr. Short and colleagues enrolled patients with newly diagnosed or relapsed/refractory Ph+ALL or lymphoid accelerated or blast phase CML. Patients in the frontline cohort could have received one or two prior lines of chemotherapy with or without a TKI.
The patients all had Eastern Cooperative Oncology Group performance status of 0-2, and adequate liver function.
Patients with clinically significant cardiovascular disease or central nervous system disease pathology were excluded, except that patients with CNS leukemia could be enrolled.
The induction phase consisted of 30 mg ponatinib daily plus blinatumomab standard dosing on a 4-week-on, 2-week-off schedule. Patients in CMR, defined for frontline patients as undetectable BCR-ABL transcripts by polymerase chain reaction, then received up to four consolidation cycles of the regimen with ponatinib at a 15-mg dose, followed by 5 years of ponatinib 15-mg maintenance. All patients also received CNS prophylaxis with 12 cycles of intrathecal chemotherapy with alternating administration of methotrexate and cytarabine.
Of the 35 patients treated to date with the combination, 20 with Ph+ALL received it as frontline therapy and 10 received it for relapsed/refractory disease; 5 patients with CML in lymphoid blast phase also were treated.
High CMR, CR rates
As noted before, the CMR rate, the primary endpoint among patients with newly diagnosed Ph+ALL, was 85%, with a CR/CRp rate of 100%. Six of the patients in the frontline group and one in the salvage therapy group had CRs but were positive for minimal residual disease (MRD) at study outset.
The CR/CRp rate for the entire cohort of 28 patients (excluding those with a CR at start) was 96%, with only 1 patient who had relapsed/refractory disease not having a CR. This patient had received ponatinib in a prior salvage regimen.
The CMR rate among the entire cohort was 79%, with 85% of patients in the frontline ALL cohort having a CMR, 88% in the relapsed/refractory cohort, and 40% in the CML cohort. There were no early deaths among any patients.
“After one cycle of ponatinib plus blinatumomab, 84% of frontline patients had achieved at least a major molecular response, and 58% had achieved a CMR. Among those with relapsed/refractory Ph+ALL, 75% achieved CMR after one cycle of therapy,” Dr. Short said.
Of the 20 frontline patients in CR, one patient experienced visual changes and possible stroke that were considered possibly related to the study medication. This patient was taken off study. During a later maintenance regimen this patient developed a non-ST elevation myocardial infarction and died from postprocedural bleeding and hypovolemic shock following a cardiac catheterization procedure.
The remainder of patients in the frontline cohort had ongoing responses without the need for HSCT at last follow-up. There were no relapses, with a median duration of CR of 6 months,
Among the 10 with relapsed/refractory Ph+ALL, one did not have a response, and the remaining 9 had CR/CRps.
Of the latter groups, four went on to allogeneic HSCT and three were still alive; one patient who underwent a transplant experienced a relapse and died. One additional patient was alive with relapsed disease with T315I and E255V mutations at the time of relapse, one patient in CR who went off study due to insurance issues died from an unknown cause, and the three remaining patients had ongoing responses without transplant.
Among the five patients with CML in lymphoid blast phase, two had relapses, but both are still alive and currently in remission, and three have ongoing responses without transplant.
After a median follow-up of 12 months the 1-year event-free survival (EFS) rate for the entire 35-patient group was 76%, and the 2-year EFS was 70%.
The 1-year overall survival rate was 93%, and the 2-year OS rate was 80%.
Among patients in the frontline group, the 1-year and 2-year EFS and OS rates were all 93%.
For the relapsed/refractory cohort, the estimated 2-year EFS was 41% and OS was 53%. For the CML cohort, the 2-year EFS was 60%, with all patients still alive at last follow-up.
There were no grade 4 adverse events on study. Grade 3 adverse events considered at least possibly related to study treatment were elevated lipase, fever/febrile neutropenia, increased alanine aminotransferase, cerebrovascular ischemia, hypertension, pancreatitis, deep vein thrombosis, and encephalopathy. There were no cases of grade 3 cytokine release syndrome or tremor.
The study was sponsored by MD Anderson Cancer Center with collaboration from the National Cancer Institute, Amgen, and Takeda. Dr. Short has disclosed relationships with Amgen and Takeda. Dr. Nichols reported having no conflicts of interest.
FROM EHA 2021
Novel molecule prolongs half-life of bleeding disorder treatments
A novel therapeutic approach using aptamers – short single strands of DNA or RNA designed to selectively bind to a target – shows promise for treating von Willebrand Disease (VWD), and other congenital bleed disorders such as hemophilia A, investigators say.
In a proof-of-concept study using healthy volunteers, the experimental anti–von Willebrand factor (VWF) molecule BT200 appeared to decrease clearance of VWF and resulted in a twofold increase in endogenous levels of VWF and factor VIII at low doses.
BT200 is currently being explored in a phase 2 trial in patients with hemophilia A and VWD type 2B, Katarina Kovacevic, MPharm, from the Medical University of Vienna, reported at the European Hematology Association annual congress.
“We expect to see a half-life increase of 2 to 4 times of factor VIII products, which will allow us to have a longer time between treatments,” she said in an oral abstract presentation (Abstract S302).
Lab-made nucleotide strings
Aptamers are sometimes call “chemical antibodies” because of their high affinity and high specificity for extracellular targets, Dr. Kovacevic said. Unlike conventional humanized or human-derived antibodies, however, they are nonimmunogenic and are less costly to manufacture.
In a previous study from her center, a different anti-VWF aptamer labeled ARC1779 increased plasma levels of VWF, factor VIII, and platelet counts in patients with VWD type 2B.
However, the drug was inconvenient to use, requiring 72-hour infusions, she noted.
In a study published in Feb. 4, 2021 in Scientific Reports, Dr. Kovacevic and colleagues reported that BT200 blocks VWF and platelet function in patients with ischemic strokes, even in the presence of high levels of VWF in patients with left carotid artery atherosclerotic strokes.
The ability of the molecule to block VWF platelet binding may explain how the anti-VWF agent actually results in higher circulating levels of VWF, which also carries factor VIII, said Veronica H. Flood, MD, a VWD specialist at Children’s Hospital of Wisconsin and associate professor at the Medical College of Wisconsin in Milwaukee.
“It might inhibit clearance of the von Willebrand factor, so it’s almost like this was an incidental side effect,” she said in an interview. “Incidentally, this happens to also give you higher levels of the von Willebrand factor and the factor VIII, and with a longer half-life than anything we currently have, so it’s a super-creative strategy,” she said.
Dr. Flood was not involved in the study.
Long half-life
BT200 is a third-generation peglyated anti-VWF aptamer that has been shown in preclinical studies to have a long half-life in nonhuman primates. It inhibits the A1 domain of VWF to prevent it from binding to platelet glycoprotein 1b (GP1b).
In the randomized, double-blind, placebo-controlled trial reported at the EHA congress, 88 healthy volunteers received single doses of BT200 ranging from 0.l8 mg to 48 mg by subcutaneous injection or intravenous infusion, 8 received multiple doses, 8 were evaluated for possible interactions with desmopressin, and 8 were evaluated for bioavailability of the aptamer.
The investigators observed a dose-related increase in BT200 concentrations, with a mean plasma terminal elimination half life of between 118 and 284 hours (about 5-12 days). There was also a dose-dependent increase in bioavailability of the agents, reaching 90% at the highest dose level.
The ability of BT200 to inhibit the A1 domains of VWF also was dose dependent, with the largest effect seen with doses of 12 mg and higher. The molecule decreased VWF activity and ristocetin-induced platelet aggregation, and prolonged collagen adenosine diphosphate closure time.
At the highest doses, BT200 caused complete inhibition of VWF (P < .001), and volunteers developed clinical signs of mild mucosal bleeding.
But the aptamer also increased in a dose-dependent fashion VWF antigen levels and factor VIII clotting activity more than fourfold (P <.001).
“This resulted in increased thrombogenicity as measured by thrombin generation and enhanced clotting. In the absence of an increase in VWF propeptide levels, this effect is considered due to decreased clearance of VWF,” the investigators wrote in the study abstract.
They noted that they saw a clinically meaningful twofold increase in both VWF and factor VIII at doses lower than 6 mg.
‘Super-exciting strategy’
“This trial identified a novel mechanism of action for BT200: It decreases the clearance of VWF/FVIII, which can be exploited for congenital bleeding disorders. This built a solid foundation for an ongoing basket trial in patients with von Willebrand disease or hemophilia A, which already confirms the expected effect sizes,” Dr. Kovacevic and colleagues wrote.
“I will be interested to see what the clinical side effects are, because there may be some off-target effects, but in reality it is a super-exciting strategy, and there is really a dire need for longer half-life products for these patients,” Dr. Flood said.
The study was sponsored by Band Therapeutics, a division of Guardian Therapeutics. Dr. Kovacevic and Dr. Flood reported having no conflicts of interest to disclose.
A novel therapeutic approach using aptamers – short single strands of DNA or RNA designed to selectively bind to a target – shows promise for treating von Willebrand Disease (VWD), and other congenital bleed disorders such as hemophilia A, investigators say.
In a proof-of-concept study using healthy volunteers, the experimental anti–von Willebrand factor (VWF) molecule BT200 appeared to decrease clearance of VWF and resulted in a twofold increase in endogenous levels of VWF and factor VIII at low doses.
BT200 is currently being explored in a phase 2 trial in patients with hemophilia A and VWD type 2B, Katarina Kovacevic, MPharm, from the Medical University of Vienna, reported at the European Hematology Association annual congress.
“We expect to see a half-life increase of 2 to 4 times of factor VIII products, which will allow us to have a longer time between treatments,” she said in an oral abstract presentation (Abstract S302).
Lab-made nucleotide strings
Aptamers are sometimes call “chemical antibodies” because of their high affinity and high specificity for extracellular targets, Dr. Kovacevic said. Unlike conventional humanized or human-derived antibodies, however, they are nonimmunogenic and are less costly to manufacture.
In a previous study from her center, a different anti-VWF aptamer labeled ARC1779 increased plasma levels of VWF, factor VIII, and platelet counts in patients with VWD type 2B.
However, the drug was inconvenient to use, requiring 72-hour infusions, she noted.
In a study published in Feb. 4, 2021 in Scientific Reports, Dr. Kovacevic and colleagues reported that BT200 blocks VWF and platelet function in patients with ischemic strokes, even in the presence of high levels of VWF in patients with left carotid artery atherosclerotic strokes.
The ability of the molecule to block VWF platelet binding may explain how the anti-VWF agent actually results in higher circulating levels of VWF, which also carries factor VIII, said Veronica H. Flood, MD, a VWD specialist at Children’s Hospital of Wisconsin and associate professor at the Medical College of Wisconsin in Milwaukee.
“It might inhibit clearance of the von Willebrand factor, so it’s almost like this was an incidental side effect,” she said in an interview. “Incidentally, this happens to also give you higher levels of the von Willebrand factor and the factor VIII, and with a longer half-life than anything we currently have, so it’s a super-creative strategy,” she said.
Dr. Flood was not involved in the study.
Long half-life
BT200 is a third-generation peglyated anti-VWF aptamer that has been shown in preclinical studies to have a long half-life in nonhuman primates. It inhibits the A1 domain of VWF to prevent it from binding to platelet glycoprotein 1b (GP1b).
In the randomized, double-blind, placebo-controlled trial reported at the EHA congress, 88 healthy volunteers received single doses of BT200 ranging from 0.l8 mg to 48 mg by subcutaneous injection or intravenous infusion, 8 received multiple doses, 8 were evaluated for possible interactions with desmopressin, and 8 were evaluated for bioavailability of the aptamer.
The investigators observed a dose-related increase in BT200 concentrations, with a mean plasma terminal elimination half life of between 118 and 284 hours (about 5-12 days). There was also a dose-dependent increase in bioavailability of the agents, reaching 90% at the highest dose level.
The ability of BT200 to inhibit the A1 domains of VWF also was dose dependent, with the largest effect seen with doses of 12 mg and higher. The molecule decreased VWF activity and ristocetin-induced platelet aggregation, and prolonged collagen adenosine diphosphate closure time.
At the highest doses, BT200 caused complete inhibition of VWF (P < .001), and volunteers developed clinical signs of mild mucosal bleeding.
But the aptamer also increased in a dose-dependent fashion VWF antigen levels and factor VIII clotting activity more than fourfold (P <.001).
“This resulted in increased thrombogenicity as measured by thrombin generation and enhanced clotting. In the absence of an increase in VWF propeptide levels, this effect is considered due to decreased clearance of VWF,” the investigators wrote in the study abstract.
They noted that they saw a clinically meaningful twofold increase in both VWF and factor VIII at doses lower than 6 mg.
‘Super-exciting strategy’
“This trial identified a novel mechanism of action for BT200: It decreases the clearance of VWF/FVIII, which can be exploited for congenital bleeding disorders. This built a solid foundation for an ongoing basket trial in patients with von Willebrand disease or hemophilia A, which already confirms the expected effect sizes,” Dr. Kovacevic and colleagues wrote.
“I will be interested to see what the clinical side effects are, because there may be some off-target effects, but in reality it is a super-exciting strategy, and there is really a dire need for longer half-life products for these patients,” Dr. Flood said.
The study was sponsored by Band Therapeutics, a division of Guardian Therapeutics. Dr. Kovacevic and Dr. Flood reported having no conflicts of interest to disclose.
A novel therapeutic approach using aptamers – short single strands of DNA or RNA designed to selectively bind to a target – shows promise for treating von Willebrand Disease (VWD), and other congenital bleed disorders such as hemophilia A, investigators say.
In a proof-of-concept study using healthy volunteers, the experimental anti–von Willebrand factor (VWF) molecule BT200 appeared to decrease clearance of VWF and resulted in a twofold increase in endogenous levels of VWF and factor VIII at low doses.
BT200 is currently being explored in a phase 2 trial in patients with hemophilia A and VWD type 2B, Katarina Kovacevic, MPharm, from the Medical University of Vienna, reported at the European Hematology Association annual congress.
“We expect to see a half-life increase of 2 to 4 times of factor VIII products, which will allow us to have a longer time between treatments,” she said in an oral abstract presentation (Abstract S302).
Lab-made nucleotide strings
Aptamers are sometimes call “chemical antibodies” because of their high affinity and high specificity for extracellular targets, Dr. Kovacevic said. Unlike conventional humanized or human-derived antibodies, however, they are nonimmunogenic and are less costly to manufacture.
In a previous study from her center, a different anti-VWF aptamer labeled ARC1779 increased plasma levels of VWF, factor VIII, and platelet counts in patients with VWD type 2B.
However, the drug was inconvenient to use, requiring 72-hour infusions, she noted.
In a study published in Feb. 4, 2021 in Scientific Reports, Dr. Kovacevic and colleagues reported that BT200 blocks VWF and platelet function in patients with ischemic strokes, even in the presence of high levels of VWF in patients with left carotid artery atherosclerotic strokes.
The ability of the molecule to block VWF platelet binding may explain how the anti-VWF agent actually results in higher circulating levels of VWF, which also carries factor VIII, said Veronica H. Flood, MD, a VWD specialist at Children’s Hospital of Wisconsin and associate professor at the Medical College of Wisconsin in Milwaukee.
“It might inhibit clearance of the von Willebrand factor, so it’s almost like this was an incidental side effect,” she said in an interview. “Incidentally, this happens to also give you higher levels of the von Willebrand factor and the factor VIII, and with a longer half-life than anything we currently have, so it’s a super-creative strategy,” she said.
Dr. Flood was not involved in the study.
Long half-life
BT200 is a third-generation peglyated anti-VWF aptamer that has been shown in preclinical studies to have a long half-life in nonhuman primates. It inhibits the A1 domain of VWF to prevent it from binding to platelet glycoprotein 1b (GP1b).
In the randomized, double-blind, placebo-controlled trial reported at the EHA congress, 88 healthy volunteers received single doses of BT200 ranging from 0.l8 mg to 48 mg by subcutaneous injection or intravenous infusion, 8 received multiple doses, 8 were evaluated for possible interactions with desmopressin, and 8 were evaluated for bioavailability of the aptamer.
The investigators observed a dose-related increase in BT200 concentrations, with a mean plasma terminal elimination half life of between 118 and 284 hours (about 5-12 days). There was also a dose-dependent increase in bioavailability of the agents, reaching 90% at the highest dose level.
The ability of BT200 to inhibit the A1 domains of VWF also was dose dependent, with the largest effect seen with doses of 12 mg and higher. The molecule decreased VWF activity and ristocetin-induced platelet aggregation, and prolonged collagen adenosine diphosphate closure time.
At the highest doses, BT200 caused complete inhibition of VWF (P < .001), and volunteers developed clinical signs of mild mucosal bleeding.
But the aptamer also increased in a dose-dependent fashion VWF antigen levels and factor VIII clotting activity more than fourfold (P <.001).
“This resulted in increased thrombogenicity as measured by thrombin generation and enhanced clotting. In the absence of an increase in VWF propeptide levels, this effect is considered due to decreased clearance of VWF,” the investigators wrote in the study abstract.
They noted that they saw a clinically meaningful twofold increase in both VWF and factor VIII at doses lower than 6 mg.
‘Super-exciting strategy’
“This trial identified a novel mechanism of action for BT200: It decreases the clearance of VWF/FVIII, which can be exploited for congenital bleeding disorders. This built a solid foundation for an ongoing basket trial in patients with von Willebrand disease or hemophilia A, which already confirms the expected effect sizes,” Dr. Kovacevic and colleagues wrote.
“I will be interested to see what the clinical side effects are, because there may be some off-target effects, but in reality it is a super-exciting strategy, and there is really a dire need for longer half-life products for these patients,” Dr. Flood said.
The study was sponsored by Band Therapeutics, a division of Guardian Therapeutics. Dr. Kovacevic and Dr. Flood reported having no conflicts of interest to disclose.
FROM EHA 2021
Rapid update to ASCO breast cancer guidelines after OlympiA data
The American Society of Clinical Oncology (ASCO) now recommends offering 1 year of adjuvant olaparib therapy to patients with early-stage HER2-negative, BRCA-mutated breast cancer who have completed chemotherapy and local treatment.
The change in management of hereditary breast cancer is outlined in an update to 2020 guidelines, and it comes as a “rapid recommendation” on the heels of the phase 3 OlympiA trial results, which indicated a 42% improvement in invasive and distant disease-free survival with the PARP inhibitor olaparib (Lynparza) in comparison with placebo.
The OlympiA trial results, as reported by this news organization, were presented during the plenary session of the ASCO 2021 annual meeting and were published June 3 in The New England Journal of Medicine.
“These clear and positive data prompted ASCO to issue a provisional update of the guideline recommendation focused specifically on the role of olaparib in this setting,” states an ASCO press release.
The previous 2020 guidelines stated: “There are insufficient data ... to recommend a PARP inhibitor for patients with nonmetastatic breast cancer.” The OlympiA trial changed that. ASCO now recommends that patients with early-stage, HER2-negative, BRCA-mutated breast cancer at high risk for recurrence be offered olaparib after completion of chemotherapy and local treatment, including radiotherapy.
The update states: “For those who had surgery first, adjuvant olaparib is recommended for patients with TNBC [triple-negative breast cancer] and tumor size greater than 2 cm or any involved axillary nodes. For patients with hormone receptor–positive disease, adjuvant olaparib is recommended for those with at least four involved axillary lymph nodes. For patients who had neoadjuvant chemotherapy, adjuvant olaparib is recommended for patients with TNBC and any residual cancer. Adjuvant olaparib is recommended for patients with residual disease and an estrogen receptor status and tumor grade (CSP+EG) score greater than or equal to 3.”
“The findings from the OlympiA trial – presented just last week – mark a significant improvement in the care of these patients,” Julie Garlow, MD, ASCO’s executive vice president and chief medical officer, states in the ASCO press release.
“ASCO’s Expert Guideline Panel and Evidence-based Medicine Committee noted this and then quickly produced and provisionally approved this guideline update to enable patients to begin to benefit from this research advance as quickly as possible,” she said.
A formal assessment and submission for publication in the Journal of Clinical Oncology will follow the release notes.
A version of this article first appeared on Medscape.com.
The American Society of Clinical Oncology (ASCO) now recommends offering 1 year of adjuvant olaparib therapy to patients with early-stage HER2-negative, BRCA-mutated breast cancer who have completed chemotherapy and local treatment.
The change in management of hereditary breast cancer is outlined in an update to 2020 guidelines, and it comes as a “rapid recommendation” on the heels of the phase 3 OlympiA trial results, which indicated a 42% improvement in invasive and distant disease-free survival with the PARP inhibitor olaparib (Lynparza) in comparison with placebo.
The OlympiA trial results, as reported by this news organization, were presented during the plenary session of the ASCO 2021 annual meeting and were published June 3 in The New England Journal of Medicine.
“These clear and positive data prompted ASCO to issue a provisional update of the guideline recommendation focused specifically on the role of olaparib in this setting,” states an ASCO press release.
The previous 2020 guidelines stated: “There are insufficient data ... to recommend a PARP inhibitor for patients with nonmetastatic breast cancer.” The OlympiA trial changed that. ASCO now recommends that patients with early-stage, HER2-negative, BRCA-mutated breast cancer at high risk for recurrence be offered olaparib after completion of chemotherapy and local treatment, including radiotherapy.
The update states: “For those who had surgery first, adjuvant olaparib is recommended for patients with TNBC [triple-negative breast cancer] and tumor size greater than 2 cm or any involved axillary nodes. For patients with hormone receptor–positive disease, adjuvant olaparib is recommended for those with at least four involved axillary lymph nodes. For patients who had neoadjuvant chemotherapy, adjuvant olaparib is recommended for patients with TNBC and any residual cancer. Adjuvant olaparib is recommended for patients with residual disease and an estrogen receptor status and tumor grade (CSP+EG) score greater than or equal to 3.”
“The findings from the OlympiA trial – presented just last week – mark a significant improvement in the care of these patients,” Julie Garlow, MD, ASCO’s executive vice president and chief medical officer, states in the ASCO press release.
“ASCO’s Expert Guideline Panel and Evidence-based Medicine Committee noted this and then quickly produced and provisionally approved this guideline update to enable patients to begin to benefit from this research advance as quickly as possible,” she said.
A formal assessment and submission for publication in the Journal of Clinical Oncology will follow the release notes.
A version of this article first appeared on Medscape.com.
The American Society of Clinical Oncology (ASCO) now recommends offering 1 year of adjuvant olaparib therapy to patients with early-stage HER2-negative, BRCA-mutated breast cancer who have completed chemotherapy and local treatment.
The change in management of hereditary breast cancer is outlined in an update to 2020 guidelines, and it comes as a “rapid recommendation” on the heels of the phase 3 OlympiA trial results, which indicated a 42% improvement in invasive and distant disease-free survival with the PARP inhibitor olaparib (Lynparza) in comparison with placebo.
The OlympiA trial results, as reported by this news organization, were presented during the plenary session of the ASCO 2021 annual meeting and were published June 3 in The New England Journal of Medicine.
“These clear and positive data prompted ASCO to issue a provisional update of the guideline recommendation focused specifically on the role of olaparib in this setting,” states an ASCO press release.
The previous 2020 guidelines stated: “There are insufficient data ... to recommend a PARP inhibitor for patients with nonmetastatic breast cancer.” The OlympiA trial changed that. ASCO now recommends that patients with early-stage, HER2-negative, BRCA-mutated breast cancer at high risk for recurrence be offered olaparib after completion of chemotherapy and local treatment, including radiotherapy.
The update states: “For those who had surgery first, adjuvant olaparib is recommended for patients with TNBC [triple-negative breast cancer] and tumor size greater than 2 cm or any involved axillary nodes. For patients with hormone receptor–positive disease, adjuvant olaparib is recommended for those with at least four involved axillary lymph nodes. For patients who had neoadjuvant chemotherapy, adjuvant olaparib is recommended for patients with TNBC and any residual cancer. Adjuvant olaparib is recommended for patients with residual disease and an estrogen receptor status and tumor grade (CSP+EG) score greater than or equal to 3.”
“The findings from the OlympiA trial – presented just last week – mark a significant improvement in the care of these patients,” Julie Garlow, MD, ASCO’s executive vice president and chief medical officer, states in the ASCO press release.
“ASCO’s Expert Guideline Panel and Evidence-based Medicine Committee noted this and then quickly produced and provisionally approved this guideline update to enable patients to begin to benefit from this research advance as quickly as possible,” she said.
A formal assessment and submission for publication in the Journal of Clinical Oncology will follow the release notes.
A version of this article first appeared on Medscape.com.
Reduced-intensity transplant benefits older patients with AML
Among older patients with acute myeloid leukemia (AML), survival is significantly better when they undergo reduced-intensity conditioning (RIC) before receiving an allogeneic hematopoietic cell transplant (HCT) at first remission. This improvement in survival is seen regardless of key factors such as genotype and the status of minimal residual disease (MRD) after initial chemotherapy, results from two large randomized trials show.
“Two consecutive trials of more than 1,500 older AML patients above 60 years of age demonstrate a consistent benefit for RIC transplant in first remission,” said first author Nigel Russell, MD, of Guy’s Hospital, London, and Nottingham University, England. “This benefit is seen independent of their post-course 1 MRD status,” he added.
Dr. Russell presented the new data at the European Hematology Association (EHA) 2021 Annual Meeting.
Commenting on the study, Charles Craddock, MD, said in an interview that the results “confirm the growing importance of RIC transplantation as a central treatment management strategy in high-risk AML and in this population high risk patients over 60.”
“[These findings] reinforce the evolving treatment paradigm that, in fit adults over 60 with AML, hematopoietic cell transplantation should be considered an essential component of their management plan,” said Dr. Craddock, academic director of the Center for Clinical Haematology, Queen Elizabeth Hospital, Birmingham, England.
Patients with AML who are older than 60 years can achieve complete remission with intensive chemotherapy alone; however, relapse is common, and only about 20% survive for 5 years, Dr. Russell explained.
HCT significantly improves survival outcomes, and the development of RIC has made transplantation accessible to high-risk patients by making the procedure more tolerable with lower toxicity in comparison with conventional conditioning regimens.
However, there is ongoing debate over the prognostic effect of key factors in pretransplant conditioning that may be predictive of the risk for post-transplant relapse – in particular, the presence of MRD after the first course of conditioning, he explained.
To more closely investigate those factors and the rate of survival of older patients with AML who undergo RIC transplant, Dr. Russell and his colleagues evaluated results from the National Cancer Research Institute’s (NCRI) AML16 trial, which was conducted from 2006 to 2012, and interim results from the NCRI AML18 trial, which started in 2015 and is ongoing.
Both trials employed double induction of daunorubicin and clofarabine or, in the AML16 trial, AraC ± gemtuzumab, and in the AML18 trial, daunorubicin and AraC (DA) + gemtuzumab.
In AML18, patients who were MRD positive after course 1 were randomly assigned to undergo either an intensification randomization after either FLAG-Ida or DA+cladribine or DA alone.
In AML16, of 983 patients in first complete response, 144 (15%) subsequently underwent RIC transplant. The median follow-up for survival from complete response was 45 months.
In the AML18 trial, of 847 patients, 648 patients achieved complete response. Among them, 201 (31%) underwent transplant. The median follow-up of survival was 45 months.
The results of both trials showed greater benefit with RIC transplant versus chemotherapy alone.
In the AML16 trial, among patients aged 60 to 70 who received RIC, survival at 5 years was significantly improved compared with chemotherapy alone (37% vs. 19%; hazard ratio, 0.65; 95% confidence interval, 0.52-0.82; P < .001).
In AML16, the higher survival benefit in comparison with chemotherapy alone was observed in the RIC group across subgroups of risk level, as stratified according to in the multivariate Wheatley risk group score. Subgroup stratification was based on age, cytogenics, and other factors (HR, 0.66; 95% CI, 0.53-0.83; P < .001).
Importantly, the survival benefits were significantly greater with RIC transplant regardless of MRD-negative or MRD-positive status after course 1 (HR, 0.68; 95% CI, 0.54-0.85; P < .001).
Allograft transplant was also more favorable regardless of FLT3 ITD or NPM1 mutation status (P for heterogeneity by genetic subgroups, 0.61).
In AML16, no groups were found to have benefited more with RIC. Consequently, the criteria for transplant in AML18 trial were based on patients’ health status and donor availability.
An interim analysis of the ongoing AML 18 trial further underscored an overall benefit of RIC transplant. Rates of 3-year survival from remission were 48% with RIC transplant, versus 37.4% with chemotherapy alone (P = .027). The benefit was independent of MRD status after conditioning course 1, similar to the AML16 results (HR, 0.71; 95% CI, 0.54-0.95; P = .02).
Although the rate of transplantation in the AML18 trial was higher among patients who were MRD positive in comparison with those who were MRD negative (36% vs. 24.8%), the rates of post-transplant survival were not significantly different between those who were MRD positive and those who were MRD negative after course 1 (51.1% vs. 46.6% at 3 years; P = .84).
The authors evaluated the effects of a second conditioning course on transplant outcomes among patients who did not initially achieve an MRD-negative complete remission.
They found that 60% of patients did convert from MRD-positive to MRD-negative status after course 2. Among those patients, the survival versus chemotherapy alone was substantially higher (HR, 0.32; 95% CI, 0.11-0.92) compared to those who remained MRD-negative (HR 0.74; 95% CI, 0.32-1.72).
However, the authors note that, owing to a lack of heterogeneity, the results don’t necessarily mean that the patients who remained MRD positive did not also benefit from transplant.
“There was a significant benefit for transplant in those who converted to MRD negativity,” Dr. Russell said.
“With a hazard ratio of .32, this was far superior to those who remained MRD-positive post course 2,” he said.
“These results show that MRD status after course 1 is important information in terms of response to therapy and can alter your treatment strategy if you’re considering a transplant as an option for these patients,” Dr. Russell told this news organization.
In further commenting, Dr. Craddock said the research highlights the importance of randomized trials with regard to whether patients who are MRD-positive before transplant will benefit from an additional course of therapy to reduce the MRD load.
“Most get two courses, but the question is, if they are still MRD positive, should they get a third course, and if so, what should that look like?” he said.
“There are currently no randomized controlled trials to address that ongoing question, and they need to be done,” he added.
Dr. Russell has relationships with Pfizer, Astellas, and Jazz Pharma. Dr. Craddock has a relationship with Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Among older patients with acute myeloid leukemia (AML), survival is significantly better when they undergo reduced-intensity conditioning (RIC) before receiving an allogeneic hematopoietic cell transplant (HCT) at first remission. This improvement in survival is seen regardless of key factors such as genotype and the status of minimal residual disease (MRD) after initial chemotherapy, results from two large randomized trials show.
“Two consecutive trials of more than 1,500 older AML patients above 60 years of age demonstrate a consistent benefit for RIC transplant in first remission,” said first author Nigel Russell, MD, of Guy’s Hospital, London, and Nottingham University, England. “This benefit is seen independent of their post-course 1 MRD status,” he added.
Dr. Russell presented the new data at the European Hematology Association (EHA) 2021 Annual Meeting.
Commenting on the study, Charles Craddock, MD, said in an interview that the results “confirm the growing importance of RIC transplantation as a central treatment management strategy in high-risk AML and in this population high risk patients over 60.”
“[These findings] reinforce the evolving treatment paradigm that, in fit adults over 60 with AML, hematopoietic cell transplantation should be considered an essential component of their management plan,” said Dr. Craddock, academic director of the Center for Clinical Haematology, Queen Elizabeth Hospital, Birmingham, England.
Patients with AML who are older than 60 years can achieve complete remission with intensive chemotherapy alone; however, relapse is common, and only about 20% survive for 5 years, Dr. Russell explained.
HCT significantly improves survival outcomes, and the development of RIC has made transplantation accessible to high-risk patients by making the procedure more tolerable with lower toxicity in comparison with conventional conditioning regimens.
However, there is ongoing debate over the prognostic effect of key factors in pretransplant conditioning that may be predictive of the risk for post-transplant relapse – in particular, the presence of MRD after the first course of conditioning, he explained.
To more closely investigate those factors and the rate of survival of older patients with AML who undergo RIC transplant, Dr. Russell and his colleagues evaluated results from the National Cancer Research Institute’s (NCRI) AML16 trial, which was conducted from 2006 to 2012, and interim results from the NCRI AML18 trial, which started in 2015 and is ongoing.
Both trials employed double induction of daunorubicin and clofarabine or, in the AML16 trial, AraC ± gemtuzumab, and in the AML18 trial, daunorubicin and AraC (DA) + gemtuzumab.
In AML18, patients who were MRD positive after course 1 were randomly assigned to undergo either an intensification randomization after either FLAG-Ida or DA+cladribine or DA alone.
In AML16, of 983 patients in first complete response, 144 (15%) subsequently underwent RIC transplant. The median follow-up for survival from complete response was 45 months.
In the AML18 trial, of 847 patients, 648 patients achieved complete response. Among them, 201 (31%) underwent transplant. The median follow-up of survival was 45 months.
The results of both trials showed greater benefit with RIC transplant versus chemotherapy alone.
In the AML16 trial, among patients aged 60 to 70 who received RIC, survival at 5 years was significantly improved compared with chemotherapy alone (37% vs. 19%; hazard ratio, 0.65; 95% confidence interval, 0.52-0.82; P < .001).
In AML16, the higher survival benefit in comparison with chemotherapy alone was observed in the RIC group across subgroups of risk level, as stratified according to in the multivariate Wheatley risk group score. Subgroup stratification was based on age, cytogenics, and other factors (HR, 0.66; 95% CI, 0.53-0.83; P < .001).
Importantly, the survival benefits were significantly greater with RIC transplant regardless of MRD-negative or MRD-positive status after course 1 (HR, 0.68; 95% CI, 0.54-0.85; P < .001).
Allograft transplant was also more favorable regardless of FLT3 ITD or NPM1 mutation status (P for heterogeneity by genetic subgroups, 0.61).
In AML16, no groups were found to have benefited more with RIC. Consequently, the criteria for transplant in AML18 trial were based on patients’ health status and donor availability.
An interim analysis of the ongoing AML 18 trial further underscored an overall benefit of RIC transplant. Rates of 3-year survival from remission were 48% with RIC transplant, versus 37.4% with chemotherapy alone (P = .027). The benefit was independent of MRD status after conditioning course 1, similar to the AML16 results (HR, 0.71; 95% CI, 0.54-0.95; P = .02).
Although the rate of transplantation in the AML18 trial was higher among patients who were MRD positive in comparison with those who were MRD negative (36% vs. 24.8%), the rates of post-transplant survival were not significantly different between those who were MRD positive and those who were MRD negative after course 1 (51.1% vs. 46.6% at 3 years; P = .84).
The authors evaluated the effects of a second conditioning course on transplant outcomes among patients who did not initially achieve an MRD-negative complete remission.
They found that 60% of patients did convert from MRD-positive to MRD-negative status after course 2. Among those patients, the survival versus chemotherapy alone was substantially higher (HR, 0.32; 95% CI, 0.11-0.92) compared to those who remained MRD-negative (HR 0.74; 95% CI, 0.32-1.72).
However, the authors note that, owing to a lack of heterogeneity, the results don’t necessarily mean that the patients who remained MRD positive did not also benefit from transplant.
“There was a significant benefit for transplant in those who converted to MRD negativity,” Dr. Russell said.
“With a hazard ratio of .32, this was far superior to those who remained MRD-positive post course 2,” he said.
“These results show that MRD status after course 1 is important information in terms of response to therapy and can alter your treatment strategy if you’re considering a transplant as an option for these patients,” Dr. Russell told this news organization.
In further commenting, Dr. Craddock said the research highlights the importance of randomized trials with regard to whether patients who are MRD-positive before transplant will benefit from an additional course of therapy to reduce the MRD load.
“Most get two courses, but the question is, if they are still MRD positive, should they get a third course, and if so, what should that look like?” he said.
“There are currently no randomized controlled trials to address that ongoing question, and they need to be done,” he added.
Dr. Russell has relationships with Pfizer, Astellas, and Jazz Pharma. Dr. Craddock has a relationship with Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
Among older patients with acute myeloid leukemia (AML), survival is significantly better when they undergo reduced-intensity conditioning (RIC) before receiving an allogeneic hematopoietic cell transplant (HCT) at first remission. This improvement in survival is seen regardless of key factors such as genotype and the status of minimal residual disease (MRD) after initial chemotherapy, results from two large randomized trials show.
“Two consecutive trials of more than 1,500 older AML patients above 60 years of age demonstrate a consistent benefit for RIC transplant in first remission,” said first author Nigel Russell, MD, of Guy’s Hospital, London, and Nottingham University, England. “This benefit is seen independent of their post-course 1 MRD status,” he added.
Dr. Russell presented the new data at the European Hematology Association (EHA) 2021 Annual Meeting.
Commenting on the study, Charles Craddock, MD, said in an interview that the results “confirm the growing importance of RIC transplantation as a central treatment management strategy in high-risk AML and in this population high risk patients over 60.”
“[These findings] reinforce the evolving treatment paradigm that, in fit adults over 60 with AML, hematopoietic cell transplantation should be considered an essential component of their management plan,” said Dr. Craddock, academic director of the Center for Clinical Haematology, Queen Elizabeth Hospital, Birmingham, England.
Patients with AML who are older than 60 years can achieve complete remission with intensive chemotherapy alone; however, relapse is common, and only about 20% survive for 5 years, Dr. Russell explained.
HCT significantly improves survival outcomes, and the development of RIC has made transplantation accessible to high-risk patients by making the procedure more tolerable with lower toxicity in comparison with conventional conditioning regimens.
However, there is ongoing debate over the prognostic effect of key factors in pretransplant conditioning that may be predictive of the risk for post-transplant relapse – in particular, the presence of MRD after the first course of conditioning, he explained.
To more closely investigate those factors and the rate of survival of older patients with AML who undergo RIC transplant, Dr. Russell and his colleagues evaluated results from the National Cancer Research Institute’s (NCRI) AML16 trial, which was conducted from 2006 to 2012, and interim results from the NCRI AML18 trial, which started in 2015 and is ongoing.
Both trials employed double induction of daunorubicin and clofarabine or, in the AML16 trial, AraC ± gemtuzumab, and in the AML18 trial, daunorubicin and AraC (DA) + gemtuzumab.
In AML18, patients who were MRD positive after course 1 were randomly assigned to undergo either an intensification randomization after either FLAG-Ida or DA+cladribine or DA alone.
In AML16, of 983 patients in first complete response, 144 (15%) subsequently underwent RIC transplant. The median follow-up for survival from complete response was 45 months.
In the AML18 trial, of 847 patients, 648 patients achieved complete response. Among them, 201 (31%) underwent transplant. The median follow-up of survival was 45 months.
The results of both trials showed greater benefit with RIC transplant versus chemotherapy alone.
In the AML16 trial, among patients aged 60 to 70 who received RIC, survival at 5 years was significantly improved compared with chemotherapy alone (37% vs. 19%; hazard ratio, 0.65; 95% confidence interval, 0.52-0.82; P < .001).
In AML16, the higher survival benefit in comparison with chemotherapy alone was observed in the RIC group across subgroups of risk level, as stratified according to in the multivariate Wheatley risk group score. Subgroup stratification was based on age, cytogenics, and other factors (HR, 0.66; 95% CI, 0.53-0.83; P < .001).
Importantly, the survival benefits were significantly greater with RIC transplant regardless of MRD-negative or MRD-positive status after course 1 (HR, 0.68; 95% CI, 0.54-0.85; P < .001).
Allograft transplant was also more favorable regardless of FLT3 ITD or NPM1 mutation status (P for heterogeneity by genetic subgroups, 0.61).
In AML16, no groups were found to have benefited more with RIC. Consequently, the criteria for transplant in AML18 trial were based on patients’ health status and donor availability.
An interim analysis of the ongoing AML 18 trial further underscored an overall benefit of RIC transplant. Rates of 3-year survival from remission were 48% with RIC transplant, versus 37.4% with chemotherapy alone (P = .027). The benefit was independent of MRD status after conditioning course 1, similar to the AML16 results (HR, 0.71; 95% CI, 0.54-0.95; P = .02).
Although the rate of transplantation in the AML18 trial was higher among patients who were MRD positive in comparison with those who were MRD negative (36% vs. 24.8%), the rates of post-transplant survival were not significantly different between those who were MRD positive and those who were MRD negative after course 1 (51.1% vs. 46.6% at 3 years; P = .84).
The authors evaluated the effects of a second conditioning course on transplant outcomes among patients who did not initially achieve an MRD-negative complete remission.
They found that 60% of patients did convert from MRD-positive to MRD-negative status after course 2. Among those patients, the survival versus chemotherapy alone was substantially higher (HR, 0.32; 95% CI, 0.11-0.92) compared to those who remained MRD-negative (HR 0.74; 95% CI, 0.32-1.72).
However, the authors note that, owing to a lack of heterogeneity, the results don’t necessarily mean that the patients who remained MRD positive did not also benefit from transplant.
“There was a significant benefit for transplant in those who converted to MRD negativity,” Dr. Russell said.
“With a hazard ratio of .32, this was far superior to those who remained MRD-positive post course 2,” he said.
“These results show that MRD status after course 1 is important information in terms of response to therapy and can alter your treatment strategy if you’re considering a transplant as an option for these patients,” Dr. Russell told this news organization.
In further commenting, Dr. Craddock said the research highlights the importance of randomized trials with regard to whether patients who are MRD-positive before transplant will benefit from an additional course of therapy to reduce the MRD load.
“Most get two courses, but the question is, if they are still MRD positive, should they get a third course, and if so, what should that look like?” he said.
“There are currently no randomized controlled trials to address that ongoing question, and they need to be done,” he added.
Dr. Russell has relationships with Pfizer, Astellas, and Jazz Pharma. Dr. Craddock has a relationship with Bristol-Myers Squibb.
A version of this article first appeared on Medscape.com.
DCIS: Biosignature helps guide postlumpectomy decisions
A biosignature tool helps women avoid unnecessary radiotherapy after undergoing lumpectomy for ductal carcinoma in situ (DCIS) – and also identifies women who need more intense treatment.
The DCISionRT test (PreludeDx) and its response subtype (Rst) biosignature provide personalized risk assessment, explains Frank Vicini, MD, a radiation oncologist at GenesisCare and a member of NRG Oncology, Pontiac, Mich.
He presented data on the test at a poster at the recent American Society of Clinical Oncology Annual Meeting.
They can also identify patients who would likely benefit from radiotherapy, Dr. Vicini reported.
The tool shows promise for identifying those whose cancer is likely to recur despite undergoing postlumpectomy radiotherapy – women who might benefit from intensified or alternate treatment approaches, he added.
The latter finding is particularly provocative because it suggests that the biosignatures “may appropriately identify patients with very radioresistant ductal carcinoma in situ,” Benjamin D. Smith, MD, commented during a poster discussion session at the meeting.
“I think these findings merit validation in translational research models,” said Dr. Smith, a radiation oncologist and professor of radiation oncology and health services research at the University of Texas MD Anderson Cancer Center, Houston.
DCISionRT, Rst, and risk
DCISionRT combines molecular biology innovations with risk-based scores to assess risk for recurrence, which is classified as either low or elevated, according to the test developer, PreludeDx.
Dr. Vicini and colleagues used the test to classify tissue samples from 485 women who were part of previous DCISionRT validation cohorts in Sweden, Australia, and the United States. The patients underwent breast cancer surgery (BCS) with or without radiotherapy between 1996 and 2011.
The Rst biosignature was used to further categorize those in the elevated-risk group as having a good response subtype (good Rst) or a poor response subtype (poor Rst) after BCS plus radiotherapy.
Radiotherapy was associated with significantly reduced recurrence rates among women with elevated risk and a good Rst (the hazard ratios for ipsilateral breast tumor recurrence [IBTR] and invasive breast cancer [IBC] were 0.18 and 0.15, respectively).
No radiotherapy benefit was seen among those with elevated risk and poor Rst.
The investigators also reported that, among patients with a poor Rst, 10-year IBTR and IBC rates were 25% and 16%, respectively, regardless of whether they received radiotherapy. These rates were much higher than the rates among women with good Rst (6.6% and 4.5%; hazard ratio, 3.6 and 4.4, respectively).
No significant difference was seen in 10-year IBTR and IBC rates among patients in the low-risk group, with or without radiotherapy.
Traditional clinicopathologic risk factors, including age younger than 50 years, grade 3 disease, and tumor size greater than 2.5 cm, did not identify poor versus good response subtypes in this cohort, and on multivariable analysis, neither of these factors nor endocrine therapy was significantly associated with IBTR or IBC.
Prospective validation needed
In his discussion, Dr. Smith said that the study provides “important data” that further validate the DCISionRT platform alone for assessing risk among women with DCIS who undergo BCS. But it is the Rst biosignature, which allows clinicians to “predict radioresistance of residual malignant chromogens following lumpectomy plus radiation therapy,” that really stands out, he added.
From the data presented, “it is reasonable to conclude that patients with a poor Rst score treated with lumpectomy and radiation had a much higher risk of in-breast tumor recurrence than one might predict or anticipate based on existing published randomized clinical trial data,” he said.
“In my opinion, it is very important to prospectively validate this finding with other cohorts,” he said. “Moving forward, I think there may come a time where there may be interest in studying radiosensitizing agents for poor-Rst ductal carcinoma in situ that are resistant to standard doses of radiation, and it may be that we consider the Rst as a factor moving forward in selecting patients for BCT versus mastectomy.”
However, because 75% of patients at elevated risk with poor Rst who undergo lumpectomy and radiotherapy do not experience recurrence in the decade following their treatment, it would be “inappropriate and misguided” to start recommending mastectomy for patients at DCISionRT elevated risk who have poor Rst, he said.
The study was funded by PreludeDx. Dr. Vicini reported employment with 21st Century Oncology and financial relationships with ImpediMed, Prelude Therapeutics, and Concure Oncology. Dr. Smith, through his employer, has an equity interest in Oncora Medical through a partnership agreement. He also has an uncompensated relationship with the American Society for Radiation Oncology.
A version of this article first appeared on Medscape.com.
A biosignature tool helps women avoid unnecessary radiotherapy after undergoing lumpectomy for ductal carcinoma in situ (DCIS) – and also identifies women who need more intense treatment.
The DCISionRT test (PreludeDx) and its response subtype (Rst) biosignature provide personalized risk assessment, explains Frank Vicini, MD, a radiation oncologist at GenesisCare and a member of NRG Oncology, Pontiac, Mich.
He presented data on the test at a poster at the recent American Society of Clinical Oncology Annual Meeting.
They can also identify patients who would likely benefit from radiotherapy, Dr. Vicini reported.
The tool shows promise for identifying those whose cancer is likely to recur despite undergoing postlumpectomy radiotherapy – women who might benefit from intensified or alternate treatment approaches, he added.
The latter finding is particularly provocative because it suggests that the biosignatures “may appropriately identify patients with very radioresistant ductal carcinoma in situ,” Benjamin D. Smith, MD, commented during a poster discussion session at the meeting.
“I think these findings merit validation in translational research models,” said Dr. Smith, a radiation oncologist and professor of radiation oncology and health services research at the University of Texas MD Anderson Cancer Center, Houston.
DCISionRT, Rst, and risk
DCISionRT combines molecular biology innovations with risk-based scores to assess risk for recurrence, which is classified as either low or elevated, according to the test developer, PreludeDx.
Dr. Vicini and colleagues used the test to classify tissue samples from 485 women who were part of previous DCISionRT validation cohorts in Sweden, Australia, and the United States. The patients underwent breast cancer surgery (BCS) with or without radiotherapy between 1996 and 2011.
The Rst biosignature was used to further categorize those in the elevated-risk group as having a good response subtype (good Rst) or a poor response subtype (poor Rst) after BCS plus radiotherapy.
Radiotherapy was associated with significantly reduced recurrence rates among women with elevated risk and a good Rst (the hazard ratios for ipsilateral breast tumor recurrence [IBTR] and invasive breast cancer [IBC] were 0.18 and 0.15, respectively).
No radiotherapy benefit was seen among those with elevated risk and poor Rst.
The investigators also reported that, among patients with a poor Rst, 10-year IBTR and IBC rates were 25% and 16%, respectively, regardless of whether they received radiotherapy. These rates were much higher than the rates among women with good Rst (6.6% and 4.5%; hazard ratio, 3.6 and 4.4, respectively).
No significant difference was seen in 10-year IBTR and IBC rates among patients in the low-risk group, with or without radiotherapy.
Traditional clinicopathologic risk factors, including age younger than 50 years, grade 3 disease, and tumor size greater than 2.5 cm, did not identify poor versus good response subtypes in this cohort, and on multivariable analysis, neither of these factors nor endocrine therapy was significantly associated with IBTR or IBC.
Prospective validation needed
In his discussion, Dr. Smith said that the study provides “important data” that further validate the DCISionRT platform alone for assessing risk among women with DCIS who undergo BCS. But it is the Rst biosignature, which allows clinicians to “predict radioresistance of residual malignant chromogens following lumpectomy plus radiation therapy,” that really stands out, he added.
From the data presented, “it is reasonable to conclude that patients with a poor Rst score treated with lumpectomy and radiation had a much higher risk of in-breast tumor recurrence than one might predict or anticipate based on existing published randomized clinical trial data,” he said.
“In my opinion, it is very important to prospectively validate this finding with other cohorts,” he said. “Moving forward, I think there may come a time where there may be interest in studying radiosensitizing agents for poor-Rst ductal carcinoma in situ that are resistant to standard doses of radiation, and it may be that we consider the Rst as a factor moving forward in selecting patients for BCT versus mastectomy.”
However, because 75% of patients at elevated risk with poor Rst who undergo lumpectomy and radiotherapy do not experience recurrence in the decade following their treatment, it would be “inappropriate and misguided” to start recommending mastectomy for patients at DCISionRT elevated risk who have poor Rst, he said.
The study was funded by PreludeDx. Dr. Vicini reported employment with 21st Century Oncology and financial relationships with ImpediMed, Prelude Therapeutics, and Concure Oncology. Dr. Smith, through his employer, has an equity interest in Oncora Medical through a partnership agreement. He also has an uncompensated relationship with the American Society for Radiation Oncology.
A version of this article first appeared on Medscape.com.
A biosignature tool helps women avoid unnecessary radiotherapy after undergoing lumpectomy for ductal carcinoma in situ (DCIS) – and also identifies women who need more intense treatment.
The DCISionRT test (PreludeDx) and its response subtype (Rst) biosignature provide personalized risk assessment, explains Frank Vicini, MD, a radiation oncologist at GenesisCare and a member of NRG Oncology, Pontiac, Mich.
He presented data on the test at a poster at the recent American Society of Clinical Oncology Annual Meeting.
They can also identify patients who would likely benefit from radiotherapy, Dr. Vicini reported.
The tool shows promise for identifying those whose cancer is likely to recur despite undergoing postlumpectomy radiotherapy – women who might benefit from intensified or alternate treatment approaches, he added.
The latter finding is particularly provocative because it suggests that the biosignatures “may appropriately identify patients with very radioresistant ductal carcinoma in situ,” Benjamin D. Smith, MD, commented during a poster discussion session at the meeting.
“I think these findings merit validation in translational research models,” said Dr. Smith, a radiation oncologist and professor of radiation oncology and health services research at the University of Texas MD Anderson Cancer Center, Houston.
DCISionRT, Rst, and risk
DCISionRT combines molecular biology innovations with risk-based scores to assess risk for recurrence, which is classified as either low or elevated, according to the test developer, PreludeDx.
Dr. Vicini and colleagues used the test to classify tissue samples from 485 women who were part of previous DCISionRT validation cohorts in Sweden, Australia, and the United States. The patients underwent breast cancer surgery (BCS) with or without radiotherapy between 1996 and 2011.
The Rst biosignature was used to further categorize those in the elevated-risk group as having a good response subtype (good Rst) or a poor response subtype (poor Rst) after BCS plus radiotherapy.
Radiotherapy was associated with significantly reduced recurrence rates among women with elevated risk and a good Rst (the hazard ratios for ipsilateral breast tumor recurrence [IBTR] and invasive breast cancer [IBC] were 0.18 and 0.15, respectively).
No radiotherapy benefit was seen among those with elevated risk and poor Rst.
The investigators also reported that, among patients with a poor Rst, 10-year IBTR and IBC rates were 25% and 16%, respectively, regardless of whether they received radiotherapy. These rates were much higher than the rates among women with good Rst (6.6% and 4.5%; hazard ratio, 3.6 and 4.4, respectively).
No significant difference was seen in 10-year IBTR and IBC rates among patients in the low-risk group, with or without radiotherapy.
Traditional clinicopathologic risk factors, including age younger than 50 years, grade 3 disease, and tumor size greater than 2.5 cm, did not identify poor versus good response subtypes in this cohort, and on multivariable analysis, neither of these factors nor endocrine therapy was significantly associated with IBTR or IBC.
Prospective validation needed
In his discussion, Dr. Smith said that the study provides “important data” that further validate the DCISionRT platform alone for assessing risk among women with DCIS who undergo BCS. But it is the Rst biosignature, which allows clinicians to “predict radioresistance of residual malignant chromogens following lumpectomy plus radiation therapy,” that really stands out, he added.
From the data presented, “it is reasonable to conclude that patients with a poor Rst score treated with lumpectomy and radiation had a much higher risk of in-breast tumor recurrence than one might predict or anticipate based on existing published randomized clinical trial data,” he said.
“In my opinion, it is very important to prospectively validate this finding with other cohorts,” he said. “Moving forward, I think there may come a time where there may be interest in studying radiosensitizing agents for poor-Rst ductal carcinoma in situ that are resistant to standard doses of radiation, and it may be that we consider the Rst as a factor moving forward in selecting patients for BCT versus mastectomy.”
However, because 75% of patients at elevated risk with poor Rst who undergo lumpectomy and radiotherapy do not experience recurrence in the decade following their treatment, it would be “inappropriate and misguided” to start recommending mastectomy for patients at DCISionRT elevated risk who have poor Rst, he said.
The study was funded by PreludeDx. Dr. Vicini reported employment with 21st Century Oncology and financial relationships with ImpediMed, Prelude Therapeutics, and Concure Oncology. Dr. Smith, through his employer, has an equity interest in Oncora Medical through a partnership agreement. He also has an uncompensated relationship with the American Society for Radiation Oncology.
A version of this article first appeared on Medscape.com.
Americans’ sun protection practices fall short of intentions
commissioned by the American Academy of Dermatology.
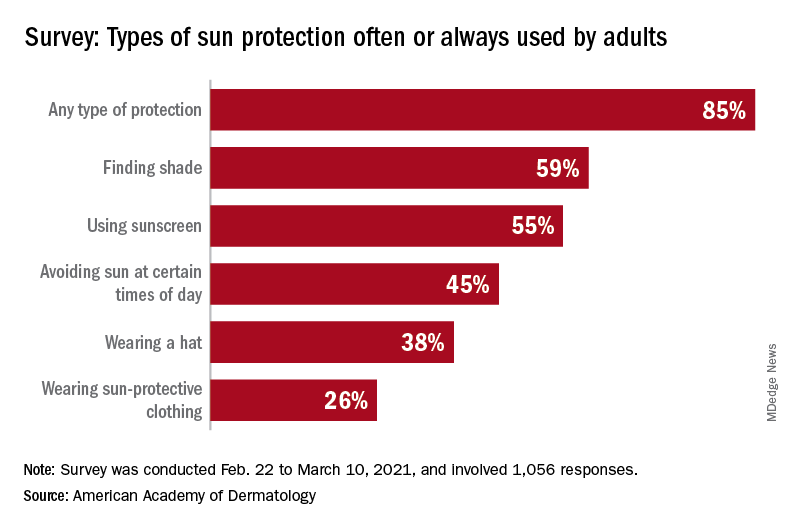
With the pandemic seemingly behind it, the United States enters the summer months facing the paradox of sun protection. Four out of five adults know that sunscreen should be reapplied every 2 hours when they’re outdoors, but only one in three make the actual effort, and 77% are likely to use sunscreen at the beach or a pool, compared with 41% when they’re gardening or working outside on their homes, the AAD reported.
“These findings are surprising and seem to suggest that many people do not take skin cancer seriously or perhaps believe skin cancer won’t happen to them,” Robert T. Brodell, MD, professor of dermatology at the University of Mississippi Medical Center, Jackson, said in a written statement from the AAD, adding that “unprotected exposure to ultraviolet rays is the most preventable risk factor for skin cancer, including melanoma.”
A quarter of all survey respondents reported getting sunburned in 2020, with the youngest adults most likely to feel the wrath of the sun. Sunburn was reported by 43% of those aged 18-23 years, 37% of those aged 24-39, 25% of the 40- to 55-year-olds, 12% of the 56- to 74-year-olds, and 7% of those aged 75 and older. More than a quarter of those who got sunburned said that it was bad enough to make their clothes feel uncomfortable, the academy said.
“Americans see the damaging effects of the sun on their skin as they get older, and two out of three look back and wish they had been more careful. But when it comes to cancer, specifically, most feel unconcerned in spite of their own risk,” according to a statement from Versta Research, which conducted the poll on behalf of the AAD. The survey was conducted from Feb. 22 to March 10, 2021, and involved 1,056 respondents, with a ±3% margin of error.
The lack of concern for skin cancer looks like this: More than two-thirds of the respondents (69%) have at least one possible risk factor – lighter skin tone, blue or green eyes, more than 50 moles, family history – but only 36% expressed concern about developing it. “Indeed, half of survey respondents (49%) say they are more worried about avoiding sunburn than they are about preventing skin cancer, and a third (32%) are more worried about avoiding premature wrinkles than they are about preventing cancer,” the AAD said.
The AAD is considering the creation of a social media quiz or interactive tool, and if the results of this survey were recast as a potential “Knowledge and Awareness Quiz” and graded with a traditional scheme (A = 90%-100%, B = 80%-89%, etc.), then 34% of the respondents would have failed, 15% would have gotten a D, and only 5% would have earned an A, the academy noted.
commissioned by the American Academy of Dermatology.
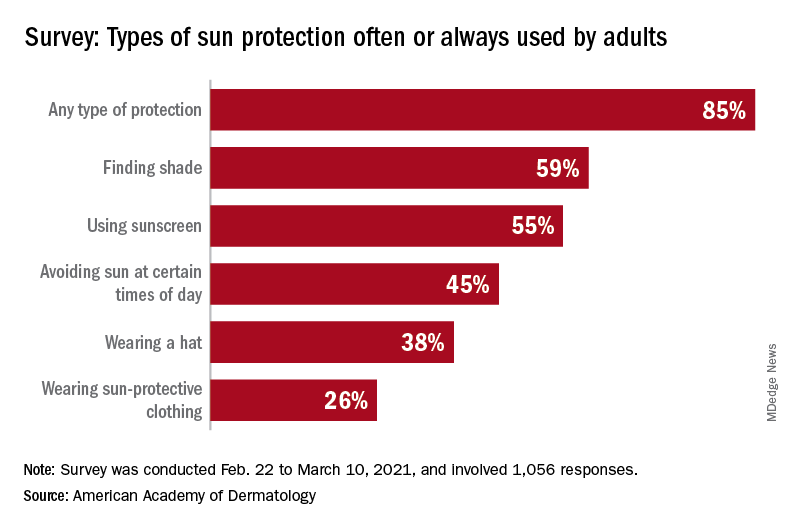
With the pandemic seemingly behind it, the United States enters the summer months facing the paradox of sun protection. Four out of five adults know that sunscreen should be reapplied every 2 hours when they’re outdoors, but only one in three make the actual effort, and 77% are likely to use sunscreen at the beach or a pool, compared with 41% when they’re gardening or working outside on their homes, the AAD reported.
“These findings are surprising and seem to suggest that many people do not take skin cancer seriously or perhaps believe skin cancer won’t happen to them,” Robert T. Brodell, MD, professor of dermatology at the University of Mississippi Medical Center, Jackson, said in a written statement from the AAD, adding that “unprotected exposure to ultraviolet rays is the most preventable risk factor for skin cancer, including melanoma.”
A quarter of all survey respondents reported getting sunburned in 2020, with the youngest adults most likely to feel the wrath of the sun. Sunburn was reported by 43% of those aged 18-23 years, 37% of those aged 24-39, 25% of the 40- to 55-year-olds, 12% of the 56- to 74-year-olds, and 7% of those aged 75 and older. More than a quarter of those who got sunburned said that it was bad enough to make their clothes feel uncomfortable, the academy said.
“Americans see the damaging effects of the sun on their skin as they get older, and two out of three look back and wish they had been more careful. But when it comes to cancer, specifically, most feel unconcerned in spite of their own risk,” according to a statement from Versta Research, which conducted the poll on behalf of the AAD. The survey was conducted from Feb. 22 to March 10, 2021, and involved 1,056 respondents, with a ±3% margin of error.
The lack of concern for skin cancer looks like this: More than two-thirds of the respondents (69%) have at least one possible risk factor – lighter skin tone, blue or green eyes, more than 50 moles, family history – but only 36% expressed concern about developing it. “Indeed, half of survey respondents (49%) say they are more worried about avoiding sunburn than they are about preventing skin cancer, and a third (32%) are more worried about avoiding premature wrinkles than they are about preventing cancer,” the AAD said.
The AAD is considering the creation of a social media quiz or interactive tool, and if the results of this survey were recast as a potential “Knowledge and Awareness Quiz” and graded with a traditional scheme (A = 90%-100%, B = 80%-89%, etc.), then 34% of the respondents would have failed, 15% would have gotten a D, and only 5% would have earned an A, the academy noted.
commissioned by the American Academy of Dermatology.
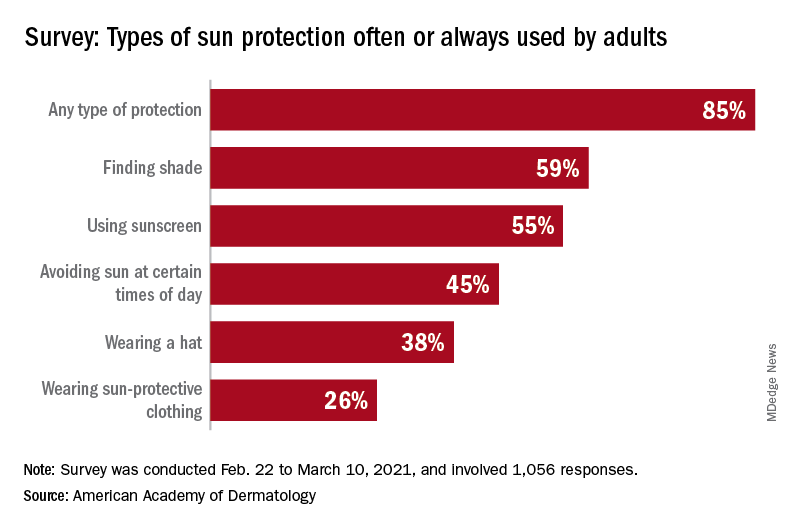
With the pandemic seemingly behind it, the United States enters the summer months facing the paradox of sun protection. Four out of five adults know that sunscreen should be reapplied every 2 hours when they’re outdoors, but only one in three make the actual effort, and 77% are likely to use sunscreen at the beach or a pool, compared with 41% when they’re gardening or working outside on their homes, the AAD reported.
“These findings are surprising and seem to suggest that many people do not take skin cancer seriously or perhaps believe skin cancer won’t happen to them,” Robert T. Brodell, MD, professor of dermatology at the University of Mississippi Medical Center, Jackson, said in a written statement from the AAD, adding that “unprotected exposure to ultraviolet rays is the most preventable risk factor for skin cancer, including melanoma.”
A quarter of all survey respondents reported getting sunburned in 2020, with the youngest adults most likely to feel the wrath of the sun. Sunburn was reported by 43% of those aged 18-23 years, 37% of those aged 24-39, 25% of the 40- to 55-year-olds, 12% of the 56- to 74-year-olds, and 7% of those aged 75 and older. More than a quarter of those who got sunburned said that it was bad enough to make their clothes feel uncomfortable, the academy said.
“Americans see the damaging effects of the sun on their skin as they get older, and two out of three look back and wish they had been more careful. But when it comes to cancer, specifically, most feel unconcerned in spite of their own risk,” according to a statement from Versta Research, which conducted the poll on behalf of the AAD. The survey was conducted from Feb. 22 to March 10, 2021, and involved 1,056 respondents, with a ±3% margin of error.
The lack of concern for skin cancer looks like this: More than two-thirds of the respondents (69%) have at least one possible risk factor – lighter skin tone, blue or green eyes, more than 50 moles, family history – but only 36% expressed concern about developing it. “Indeed, half of survey respondents (49%) say they are more worried about avoiding sunburn than they are about preventing skin cancer, and a third (32%) are more worried about avoiding premature wrinkles than they are about preventing cancer,” the AAD said.
The AAD is considering the creation of a social media quiz or interactive tool, and if the results of this survey were recast as a potential “Knowledge and Awareness Quiz” and graded with a traditional scheme (A = 90%-100%, B = 80%-89%, etc.), then 34% of the respondents would have failed, 15% would have gotten a D, and only 5% would have earned an A, the academy noted.