User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Keep menstrual cramps away the dietary prevention way
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
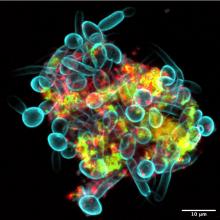
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Previous endemic coronavirus encounters linked with long COVID
People who develop long COVID may be responding more strongly to a non–SARS-CoV-2 virus they encountered in the past than to SARS-CoV-2, a study by researchers at Harvard Medical School suggests.
Long COVID, also called postacute sequelae of COVID-19 (PASC), causes various symptoms that persist at least 4 weeks after the initial SARS-CoV-2 infection, they write in the preprint server medRxiv. Four authors explained their research into possible mechanisms of long COVID in an interview.
“Immunity to non-COVID endemic coronaviruses may play a role in who develops PASC,” co–lead author Jonathan D. Herman, MD, PhD, said. “There’s still so much more we need to understand, but it is striking that back-boosting of immune responses to coronavirus OC43 was uniquely enriched in individuals with PASC.”
“In the study, individuals with PASC preferentially generated stronger responses to previously encountered cold-causing coronaviruses,” co–senior author Galit Alter, PhD, said.
“Instead of generating strong SARS-CoV-2 immunity, they bolstered a response to a different coronavirus, potentially making their response less effective in clearing SARS-CoV-2. Surprisingly, most of the individuals had been vaccinated – and they still maintained this unusual antibody response – pointing to new therapeutic pathways to treat PASC,” Dr. Alter said.
Humoral immunity offers a clue to long-COVID origins
One-fifth of COVID-19 patients progress to long COVID, but which patients develop PASC and why are not well understood, the authors write.
“Antibodies represent powerful biomarkers that have been used for decades to diagnose disease. However, antibodies also provide a powerful source of information on previous infections. The use of antibody profiling, here, pointed to the presence of incomplete antibody responses to SARS-CoV-2 in individuals with PASC,” Dr. Alter said.
The researchers reviewed the medical records of patients in the Mass General Brigham health care system in Boston, including referrals from rheumatologists of participants diagnosed with COVID-19 outside the MGB system, starting on March 1, 2020.
They focused on patients with systemic autoimmune rheumatic diseases (SARDs) because their tendency toward inflammation and autoantibody production may make them more susceptible to PASC and enrich for specific inflammatory-driven endotypes.
All 43 participants had COVID-19 without hospital admission and SARDs. Patients treated only for fibromyalgia, osteoarthritis, mechanical back pain, gout, or pseudogout without a SARD were excluded from the study.
Overall, 79% of participants were female, 35% had rheumatoid arthritis, 19% had psoriatic arthritis, and 95% had received a COVID-19 vaccine.
The researchers used systems serology to perform comprehensive antibody profiling against SARS-CoV-2 and a panel of endemic pathogens or routine vaccine antigens.
Long-COVID patients had a distinct immune response
Overall, 17 patients developed PASC and 26 did not, and in those with PASC, they found a distinct humoral immune response. Patients with PASC:
- harbored less inflamed and weaker Fc-gamma receptor–binding anti–SARS-CoV-2 antibodies;
- showed a significantly expanded and more inflamed antibody response against endemic coronavirus OC43; and
- mounted more avid IgM responses and developed expanded inflammatory OC43 S2–specific Fc-receptor–binding responses, which were linked to cross reactivity across SARS-CoV-2 and common coronaviruses.
“Strengths of the study include the detailed phenotypes of cases after COVID-19, particularly to classify PASC presence or absence, as well as the depth and breadth of antibody profiling. This allowed us to identify a humoral immune signature of PASC,” said co–senior author Jeffrey A. Sparks, MD, MMSc.
“However, the study was limited in its size to investigate different types of PASC, such as fatigue or lung symptoms, that may have biologic differences. Also, all patients in the study had a preexisting rheumatic disease,” he acknowledged.
“A substantial portion of patients with COVID-19 will develop PASC, which can have substantial impact on health and quality of life,” said co–senior author Zachary S. Wallace, MD, MS. “Given the higher risk of COVID-19 in many patients with rheumatic disease, it is important to understand the etiology of PASC in this vulnerable population, to enable future diagnostic and therapeutic advances.”
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California, San Diego, in La Jolla, who was not involved in the study, called the findings interesting even though the results will not immediately affect patient care.
“There may be a link between previous non–SARS-CoV-2 coronavirus infection and PASC,” he added. “Perhaps, by understanding why some people do and do not get PASC, we can develop treatments for the condition.
“This paper is a preprint and will need to go through peer review,” Dr. Smith said. “There are many elements that need to be scrutinized. For example, there is no definition of PASC that is universally accepted, so how did that play into this study?”
Mark Cameron, PhD, associate professor in the department of population and quantitative health sciences at Case Western Reserve University, Cleveland, called this a strong study from a strong group, although it is a preprint prior to peer review.
“In this initial study, the scientists focused on people who had rheumatic disease before getting COVID-19, knowing they are at higher risk for lasting complications and hopefully are more immunologically similar when diagnosed with long COVID – a single ‘endotype’ or group of patients with similar clinical symptoms and background,” he noted.
“Our immune system’s memory sometimes fails to effectively fight a new virus that looks too much like a virus it saw before. This ineffective immune response can set up various problems, including the poor recoveries we see in people with long COVID,” he said.
“OC43 probably emerged in the late 1800s and probably caused a pandemic of severe respiratory illness between 1889 and 1890, previously thought to be a flu,” Dr. Cameron recalled. “OC43 is still around as an endemic coronavirus, usually causing mild or moderate upper-respiratory infections.”
COVID-19 immunity is complex, and previous SARS-CoV-2 infection doesn’t guarantee we won't get COVID-19 again, especially as new variants emerge, added Dr. Cameron, who also was not involved in the study.
“This study may help us better understand the risks and possible mechanisms associated with COVID-19 and long COVID in the face of previous coronavirus infections,” he said. “It may also help guide future COVID-19 therapies and vaccines.”
The authors plan further related research.
The study received grant support and an anonymous donation. Dr. Alter, Dr. Sparks, and Dr. Wallace report financial relationships with the pharmaceutical industry. All other authors, and Dr. Davey and Dr. Cameron, report no conflicts of interest with the study. All experts commented by email.
* This story was updated 10/12/2022.
People who develop long COVID may be responding more strongly to a non–SARS-CoV-2 virus they encountered in the past than to SARS-CoV-2, a study by researchers at Harvard Medical School suggests.
Long COVID, also called postacute sequelae of COVID-19 (PASC), causes various symptoms that persist at least 4 weeks after the initial SARS-CoV-2 infection, they write in the preprint server medRxiv. Four authors explained their research into possible mechanisms of long COVID in an interview.
“Immunity to non-COVID endemic coronaviruses may play a role in who develops PASC,” co–lead author Jonathan D. Herman, MD, PhD, said. “There’s still so much more we need to understand, but it is striking that back-boosting of immune responses to coronavirus OC43 was uniquely enriched in individuals with PASC.”
“In the study, individuals with PASC preferentially generated stronger responses to previously encountered cold-causing coronaviruses,” co–senior author Galit Alter, PhD, said.
“Instead of generating strong SARS-CoV-2 immunity, they bolstered a response to a different coronavirus, potentially making their response less effective in clearing SARS-CoV-2. Surprisingly, most of the individuals had been vaccinated – and they still maintained this unusual antibody response – pointing to new therapeutic pathways to treat PASC,” Dr. Alter said.
Humoral immunity offers a clue to long-COVID origins
One-fifth of COVID-19 patients progress to long COVID, but which patients develop PASC and why are not well understood, the authors write.
“Antibodies represent powerful biomarkers that have been used for decades to diagnose disease. However, antibodies also provide a powerful source of information on previous infections. The use of antibody profiling, here, pointed to the presence of incomplete antibody responses to SARS-CoV-2 in individuals with PASC,” Dr. Alter said.
The researchers reviewed the medical records of patients in the Mass General Brigham health care system in Boston, including referrals from rheumatologists of participants diagnosed with COVID-19 outside the MGB system, starting on March 1, 2020.
They focused on patients with systemic autoimmune rheumatic diseases (SARDs) because their tendency toward inflammation and autoantibody production may make them more susceptible to PASC and enrich for specific inflammatory-driven endotypes.
All 43 participants had COVID-19 without hospital admission and SARDs. Patients treated only for fibromyalgia, osteoarthritis, mechanical back pain, gout, or pseudogout without a SARD were excluded from the study.
Overall, 79% of participants were female, 35% had rheumatoid arthritis, 19% had psoriatic arthritis, and 95% had received a COVID-19 vaccine.
The researchers used systems serology to perform comprehensive antibody profiling against SARS-CoV-2 and a panel of endemic pathogens or routine vaccine antigens.
Long-COVID patients had a distinct immune response
Overall, 17 patients developed PASC and 26 did not, and in those with PASC, they found a distinct humoral immune response. Patients with PASC:
- harbored less inflamed and weaker Fc-gamma receptor–binding anti–SARS-CoV-2 antibodies;
- showed a significantly expanded and more inflamed antibody response against endemic coronavirus OC43; and
- mounted more avid IgM responses and developed expanded inflammatory OC43 S2–specific Fc-receptor–binding responses, which were linked to cross reactivity across SARS-CoV-2 and common coronaviruses.
“Strengths of the study include the detailed phenotypes of cases after COVID-19, particularly to classify PASC presence or absence, as well as the depth and breadth of antibody profiling. This allowed us to identify a humoral immune signature of PASC,” said co–senior author Jeffrey A. Sparks, MD, MMSc.
“However, the study was limited in its size to investigate different types of PASC, such as fatigue or lung symptoms, that may have biologic differences. Also, all patients in the study had a preexisting rheumatic disease,” he acknowledged.
“A substantial portion of patients with COVID-19 will develop PASC, which can have substantial impact on health and quality of life,” said co–senior author Zachary S. Wallace, MD, MS. “Given the higher risk of COVID-19 in many patients with rheumatic disease, it is important to understand the etiology of PASC in this vulnerable population, to enable future diagnostic and therapeutic advances.”
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California, San Diego, in La Jolla, who was not involved in the study, called the findings interesting even though the results will not immediately affect patient care.
“There may be a link between previous non–SARS-CoV-2 coronavirus infection and PASC,” he added. “Perhaps, by understanding why some people do and do not get PASC, we can develop treatments for the condition.
“This paper is a preprint and will need to go through peer review,” Dr. Smith said. “There are many elements that need to be scrutinized. For example, there is no definition of PASC that is universally accepted, so how did that play into this study?”
Mark Cameron, PhD, associate professor in the department of population and quantitative health sciences at Case Western Reserve University, Cleveland, called this a strong study from a strong group, although it is a preprint prior to peer review.
“In this initial study, the scientists focused on people who had rheumatic disease before getting COVID-19, knowing they are at higher risk for lasting complications and hopefully are more immunologically similar when diagnosed with long COVID – a single ‘endotype’ or group of patients with similar clinical symptoms and background,” he noted.
“Our immune system’s memory sometimes fails to effectively fight a new virus that looks too much like a virus it saw before. This ineffective immune response can set up various problems, including the poor recoveries we see in people with long COVID,” he said.
“OC43 probably emerged in the late 1800s and probably caused a pandemic of severe respiratory illness between 1889 and 1890, previously thought to be a flu,” Dr. Cameron recalled. “OC43 is still around as an endemic coronavirus, usually causing mild or moderate upper-respiratory infections.”
COVID-19 immunity is complex, and previous SARS-CoV-2 infection doesn’t guarantee we won't get COVID-19 again, especially as new variants emerge, added Dr. Cameron, who also was not involved in the study.
“This study may help us better understand the risks and possible mechanisms associated with COVID-19 and long COVID in the face of previous coronavirus infections,” he said. “It may also help guide future COVID-19 therapies and vaccines.”
The authors plan further related research.
The study received grant support and an anonymous donation. Dr. Alter, Dr. Sparks, and Dr. Wallace report financial relationships with the pharmaceutical industry. All other authors, and Dr. Davey and Dr. Cameron, report no conflicts of interest with the study. All experts commented by email.
* This story was updated 10/12/2022.
People who develop long COVID may be responding more strongly to a non–SARS-CoV-2 virus they encountered in the past than to SARS-CoV-2, a study by researchers at Harvard Medical School suggests.
Long COVID, also called postacute sequelae of COVID-19 (PASC), causes various symptoms that persist at least 4 weeks after the initial SARS-CoV-2 infection, they write in the preprint server medRxiv. Four authors explained their research into possible mechanisms of long COVID in an interview.
“Immunity to non-COVID endemic coronaviruses may play a role in who develops PASC,” co–lead author Jonathan D. Herman, MD, PhD, said. “There’s still so much more we need to understand, but it is striking that back-boosting of immune responses to coronavirus OC43 was uniquely enriched in individuals with PASC.”
“In the study, individuals with PASC preferentially generated stronger responses to previously encountered cold-causing coronaviruses,” co–senior author Galit Alter, PhD, said.
“Instead of generating strong SARS-CoV-2 immunity, they bolstered a response to a different coronavirus, potentially making their response less effective in clearing SARS-CoV-2. Surprisingly, most of the individuals had been vaccinated – and they still maintained this unusual antibody response – pointing to new therapeutic pathways to treat PASC,” Dr. Alter said.
Humoral immunity offers a clue to long-COVID origins
One-fifth of COVID-19 patients progress to long COVID, but which patients develop PASC and why are not well understood, the authors write.
“Antibodies represent powerful biomarkers that have been used for decades to diagnose disease. However, antibodies also provide a powerful source of information on previous infections. The use of antibody profiling, here, pointed to the presence of incomplete antibody responses to SARS-CoV-2 in individuals with PASC,” Dr. Alter said.
The researchers reviewed the medical records of patients in the Mass General Brigham health care system in Boston, including referrals from rheumatologists of participants diagnosed with COVID-19 outside the MGB system, starting on March 1, 2020.
They focused on patients with systemic autoimmune rheumatic diseases (SARDs) because their tendency toward inflammation and autoantibody production may make them more susceptible to PASC and enrich for specific inflammatory-driven endotypes.
All 43 participants had COVID-19 without hospital admission and SARDs. Patients treated only for fibromyalgia, osteoarthritis, mechanical back pain, gout, or pseudogout without a SARD were excluded from the study.
Overall, 79% of participants were female, 35% had rheumatoid arthritis, 19% had psoriatic arthritis, and 95% had received a COVID-19 vaccine.
The researchers used systems serology to perform comprehensive antibody profiling against SARS-CoV-2 and a panel of endemic pathogens or routine vaccine antigens.
Long-COVID patients had a distinct immune response
Overall, 17 patients developed PASC and 26 did not, and in those with PASC, they found a distinct humoral immune response. Patients with PASC:
- harbored less inflamed and weaker Fc-gamma receptor–binding anti–SARS-CoV-2 antibodies;
- showed a significantly expanded and more inflamed antibody response against endemic coronavirus OC43; and
- mounted more avid IgM responses and developed expanded inflammatory OC43 S2–specific Fc-receptor–binding responses, which were linked to cross reactivity across SARS-CoV-2 and common coronaviruses.
“Strengths of the study include the detailed phenotypes of cases after COVID-19, particularly to classify PASC presence or absence, as well as the depth and breadth of antibody profiling. This allowed us to identify a humoral immune signature of PASC,” said co–senior author Jeffrey A. Sparks, MD, MMSc.
“However, the study was limited in its size to investigate different types of PASC, such as fatigue or lung symptoms, that may have biologic differences. Also, all patients in the study had a preexisting rheumatic disease,” he acknowledged.
“A substantial portion of patients with COVID-19 will develop PASC, which can have substantial impact on health and quality of life,” said co–senior author Zachary S. Wallace, MD, MS. “Given the higher risk of COVID-19 in many patients with rheumatic disease, it is important to understand the etiology of PASC in this vulnerable population, to enable future diagnostic and therapeutic advances.”
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California, San Diego, in La Jolla, who was not involved in the study, called the findings interesting even though the results will not immediately affect patient care.
“There may be a link between previous non–SARS-CoV-2 coronavirus infection and PASC,” he added. “Perhaps, by understanding why some people do and do not get PASC, we can develop treatments for the condition.
“This paper is a preprint and will need to go through peer review,” Dr. Smith said. “There are many elements that need to be scrutinized. For example, there is no definition of PASC that is universally accepted, so how did that play into this study?”
Mark Cameron, PhD, associate professor in the department of population and quantitative health sciences at Case Western Reserve University, Cleveland, called this a strong study from a strong group, although it is a preprint prior to peer review.
“In this initial study, the scientists focused on people who had rheumatic disease before getting COVID-19, knowing they are at higher risk for lasting complications and hopefully are more immunologically similar when diagnosed with long COVID – a single ‘endotype’ or group of patients with similar clinical symptoms and background,” he noted.
“Our immune system’s memory sometimes fails to effectively fight a new virus that looks too much like a virus it saw before. This ineffective immune response can set up various problems, including the poor recoveries we see in people with long COVID,” he said.
“OC43 probably emerged in the late 1800s and probably caused a pandemic of severe respiratory illness between 1889 and 1890, previously thought to be a flu,” Dr. Cameron recalled. “OC43 is still around as an endemic coronavirus, usually causing mild or moderate upper-respiratory infections.”
COVID-19 immunity is complex, and previous SARS-CoV-2 infection doesn’t guarantee we won't get COVID-19 again, especially as new variants emerge, added Dr. Cameron, who also was not involved in the study.
“This study may help us better understand the risks and possible mechanisms associated with COVID-19 and long COVID in the face of previous coronavirus infections,” he said. “It may also help guide future COVID-19 therapies and vaccines.”
The authors plan further related research.
The study received grant support and an anonymous donation. Dr. Alter, Dr. Sparks, and Dr. Wallace report financial relationships with the pharmaceutical industry. All other authors, and Dr. Davey and Dr. Cameron, report no conflicts of interest with the study. All experts commented by email.
* This story was updated 10/12/2022.
FROM MEDRXIV
IVIG proves effective for dermatomyositis in phase 3 trial
With use of intravenous immunoglobulin for the treatment of adults with dermatomyositis, a significantly higher percentage of patients experienced at least minimal improvement in disease activity in comparison with placebo in the first-ever phase 3 trial of the blood-product therapy for the condition.
Until this trial, published in the New England Journal of Medicine, there had not been an extensive evaluation of IVIG for the treatment of dermatomyositis, the study’s authors noted.
Glucocorticoids are typically offered as first-line therapy, followed by various immunosuppressants. IVIG is composed of purified liquid IgG concentrates from human plasma. It has been prescribed off label as second- or third-line therapy for dermatomyositis, usually along with immunosuppressive drugs. In European guidelines, it has been recommended as a glucocorticoid-sparing agent for patients with this condition.
“The study provides support that IVIG is effective in treating the signs and symptoms of patients with dermatomyositis, at least in the short term,” said David Fiorentino, MD, PhD, professor of dermatology and associate residency program director at Stanford Health Care, Stanford, California, who was not involved in the study.
“IVIG appears to be effective for patients with any severity level and works relatively quickly [within 1 month of therapy],” he added. “IVIG is effective in treating both the muscle symptoms as well as the rash of dermatomyositis, which is important, as both organ systems can cause significant patient morbidity in this disease.”
Time to improvement was shorter with IVIG than with placebo (a median of 35 days vs. 115 days), said Kathryn H. Dao, MD, associate professor in the division of rheumatic diseases at the University of Texas Southwestern Medical Center, Dallas, who was not involved in the study.
The study’s greatest strengths are its international, multicenter, randomized, placebo-controlled design, Dr. Dao said. In addition, “these patients were permitted to be on background medicines that we typically use in real-world situations.”
Study methodology
Researchers led by Rohit Aggarwal, MD, of the division of rheumatology and clinical immunology at the University of Pittsburgh, recruited patients aged 18-80 years with active dermatomyositis. Individuals were randomly assigned in a 1:1 ratio to receive either IVIG at a dose of 2.0 g/kg of body weight or placebo (0.9% sodium chloride) every 4 weeks for 16 weeks.
Those who were administered placebo and those who did not experience confirmed clinical deterioration while receiving IVIG could participate in an open-label extension phase for another 24 weeks.
The primary endpoint was a response, defined as a Total Improvement Score (TIS) of at least 20 (indicating at least minimal improvement) at week 16 and no confirmed deterioration up to week 16. The TIS is a weighted composite score that reflects the change in a core set of six measures of myositis activity over time. Scores span from 0 to 100, with higher scores indicating more significant improvement.
Secondary endpoints
Key secondary endpoints included moderate improvement (TIS ≥ 40) and major improvement (TIS ≥ 60) and change in score on the Cutaneous Dermatomyositis Disease Area and Severity Index.
A total of 95 patients underwent randomization; 47 patients received IVIG and 48 received placebo. At 16 weeks, a TIS of at least 20 occurred in 37 of 47 (79%) patients who received IVIG and in 21 of 48 (44%) patients with placebo (difference, 35%; 95% confidence interval, 17%-53%; P < .001).
The results with respect to the secondary endpoints, including at least moderate improvement and major improvement, were generally in the same direction as the results of the primary endpoint analysis, except for change in creatine kinase (CK) level (an individual core measure of the TIS), which did not differ meaningfully between the two groups.
Adverse events
Over the course of 40 weeks, 282 treatment-related adverse events were documented among patients who received IVIG. Headache was experienced by 42%, pyrexia by 19%, and nausea by 16%. Nine serious adverse events occurred and were believed to be associated with IVIG, including six thromboembolic events.
Despite the favorable outcome observed with IVIG, in an editorial that accompanied the study, Anthony A. Amato, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, noted that “most of the core components of the TIS are subjective. Because of the high percentage of patients who had a response with placebo, large numbers of patients will be needed in future trials to show a significant difference between trial groups, or the primary endpoint would need to be set higher (e.g., a TIS of ≥40).”
Dr. Dao thought it was significant that the study proactively assessed patients for venous thrombotic events (VTEs) after each infusion. There were eight events in six patients who received IVIG. “Of interest and possibly practice changing is the finding that slowing the IVIG infusion rate from 0.12 to 0.04 mL/kg per minute reduced the incidence of VTEs from 1.54/100 patient-months to 0.54/100 patient-months,” she said. “This is important, as it informs clinicians that IVIG infusion rates should be slower for patients with active dermatomyositis to reduce the risk for blood clots.”
Study weaknesses
A considerable proportion of patients with dermatomyositis do not have clinical muscle involvement but do have rash and do not substantially differ in any other ways from those with classic dermatomyositis, Dr. Fiorentino said.
“These patients were not eligible to enter the trial, and so we have no data on the efficacy of IVIG in this population,” he said. “Unfortunately, these patients might now be denied insurance reimbursement for IVIG therapy, given that they are not part of the indicated patient population in the label.”
In addition, there is limited information about Black, Asian, or Hispanic patients because few of those patients participated in the study. That is also the case for patients younger than 18, which for this disease is relevant because incidence peaks in younger patients (juvenile dermatomyositis), Dr. Fiorentino noted.
Among the study’s weaknesses, Dr. Dao noted that more than 70% of participants were women. The study was short in duration, fewer than half of patients underwent muscle biopsy to confirm myositis, and only two thirds of patients underwent electromyography/nerve conduction studies to show evidence of myositis. There was a high placebo response (44%), the CK values were not high at the start of the trial, and they did not change with treatment.
No analysis was performed to evaluate the efficacy of IVIG across dermatomyositis subgroups – defined by autoantibodies – but the study likely was not powered to do so. These subgroups might respond differently to IVIG, yielding important information, Fiorentino said.
The study provided efficacy data for only one formulation of IVIG, Octagam 10%, which was approved for dermatomyositis by the Food and Drug Administration in 2021 on the basis of this trial. However, in the United States, patients with dermatomyositis are treated with multiple brands of IVIG. “The decision around IVIG brand is largely determined by third-party payers, and for the most part, the different brands are used interchangeably from the standpoint of the treating provider,” Dr. Fiorentino said. “This will likely continue to be the case, as the results of this study are generally being extrapolated to all brands of IVIG.”
Multiple IVIG brands that have been used for immune-mediated diseases differ in concentration, content of IgA, sugar concentration, additives, and preparations (for example, the need for reconstitution vs. being ready to use), Dr. Dao said. Octagam 10% is the only brand approved by the FDA for adult dermatomyositis; hence, cost can be an issue for patients if other brands are used off label. The typical cost of IVIG is $100-$400 per gram; a typical course of treatment is estimated to be $30,000-$40,000 per month. “However, if Octagam is not available or a patient has a reaction to it, clinicians may use other IVIG brands as deemed medically necessary to treat their patients,” she said.
Dr. Aggarwal has financial relationships with more than 15 pharmaceutical companies, including Octapharma, which provided financial support for this trial. Some of the coauthors were employees of Octapharma or had financial relationships with the company. Dr. Dao disclosed no relevant financial relationships. Dr. Fiorentino has conducted sponsored research for Pfizer and Argenyx, has received research funding from Serono, and is a paid adviser to Bristol-Myers Squibb, Janssen, Acelyrin, and Corbus.
A version of this article first appeared on Medscape.com.
With use of intravenous immunoglobulin for the treatment of adults with dermatomyositis, a significantly higher percentage of patients experienced at least minimal improvement in disease activity in comparison with placebo in the first-ever phase 3 trial of the blood-product therapy for the condition.
Until this trial, published in the New England Journal of Medicine, there had not been an extensive evaluation of IVIG for the treatment of dermatomyositis, the study’s authors noted.
Glucocorticoids are typically offered as first-line therapy, followed by various immunosuppressants. IVIG is composed of purified liquid IgG concentrates from human plasma. It has been prescribed off label as second- or third-line therapy for dermatomyositis, usually along with immunosuppressive drugs. In European guidelines, it has been recommended as a glucocorticoid-sparing agent for patients with this condition.
“The study provides support that IVIG is effective in treating the signs and symptoms of patients with dermatomyositis, at least in the short term,” said David Fiorentino, MD, PhD, professor of dermatology and associate residency program director at Stanford Health Care, Stanford, California, who was not involved in the study.
“IVIG appears to be effective for patients with any severity level and works relatively quickly [within 1 month of therapy],” he added. “IVIG is effective in treating both the muscle symptoms as well as the rash of dermatomyositis, which is important, as both organ systems can cause significant patient morbidity in this disease.”
Time to improvement was shorter with IVIG than with placebo (a median of 35 days vs. 115 days), said Kathryn H. Dao, MD, associate professor in the division of rheumatic diseases at the University of Texas Southwestern Medical Center, Dallas, who was not involved in the study.
The study’s greatest strengths are its international, multicenter, randomized, placebo-controlled design, Dr. Dao said. In addition, “these patients were permitted to be on background medicines that we typically use in real-world situations.”
Study methodology
Researchers led by Rohit Aggarwal, MD, of the division of rheumatology and clinical immunology at the University of Pittsburgh, recruited patients aged 18-80 years with active dermatomyositis. Individuals were randomly assigned in a 1:1 ratio to receive either IVIG at a dose of 2.0 g/kg of body weight or placebo (0.9% sodium chloride) every 4 weeks for 16 weeks.
Those who were administered placebo and those who did not experience confirmed clinical deterioration while receiving IVIG could participate in an open-label extension phase for another 24 weeks.
The primary endpoint was a response, defined as a Total Improvement Score (TIS) of at least 20 (indicating at least minimal improvement) at week 16 and no confirmed deterioration up to week 16. The TIS is a weighted composite score that reflects the change in a core set of six measures of myositis activity over time. Scores span from 0 to 100, with higher scores indicating more significant improvement.
Secondary endpoints
Key secondary endpoints included moderate improvement (TIS ≥ 40) and major improvement (TIS ≥ 60) and change in score on the Cutaneous Dermatomyositis Disease Area and Severity Index.
A total of 95 patients underwent randomization; 47 patients received IVIG and 48 received placebo. At 16 weeks, a TIS of at least 20 occurred in 37 of 47 (79%) patients who received IVIG and in 21 of 48 (44%) patients with placebo (difference, 35%; 95% confidence interval, 17%-53%; P < .001).
The results with respect to the secondary endpoints, including at least moderate improvement and major improvement, were generally in the same direction as the results of the primary endpoint analysis, except for change in creatine kinase (CK) level (an individual core measure of the TIS), which did not differ meaningfully between the two groups.
Adverse events
Over the course of 40 weeks, 282 treatment-related adverse events were documented among patients who received IVIG. Headache was experienced by 42%, pyrexia by 19%, and nausea by 16%. Nine serious adverse events occurred and were believed to be associated with IVIG, including six thromboembolic events.
Despite the favorable outcome observed with IVIG, in an editorial that accompanied the study, Anthony A. Amato, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, noted that “most of the core components of the TIS are subjective. Because of the high percentage of patients who had a response with placebo, large numbers of patients will be needed in future trials to show a significant difference between trial groups, or the primary endpoint would need to be set higher (e.g., a TIS of ≥40).”
Dr. Dao thought it was significant that the study proactively assessed patients for venous thrombotic events (VTEs) after each infusion. There were eight events in six patients who received IVIG. “Of interest and possibly practice changing is the finding that slowing the IVIG infusion rate from 0.12 to 0.04 mL/kg per minute reduced the incidence of VTEs from 1.54/100 patient-months to 0.54/100 patient-months,” she said. “This is important, as it informs clinicians that IVIG infusion rates should be slower for patients with active dermatomyositis to reduce the risk for blood clots.”
Study weaknesses
A considerable proportion of patients with dermatomyositis do not have clinical muscle involvement but do have rash and do not substantially differ in any other ways from those with classic dermatomyositis, Dr. Fiorentino said.
“These patients were not eligible to enter the trial, and so we have no data on the efficacy of IVIG in this population,” he said. “Unfortunately, these patients might now be denied insurance reimbursement for IVIG therapy, given that they are not part of the indicated patient population in the label.”
In addition, there is limited information about Black, Asian, or Hispanic patients because few of those patients participated in the study. That is also the case for patients younger than 18, which for this disease is relevant because incidence peaks in younger patients (juvenile dermatomyositis), Dr. Fiorentino noted.
Among the study’s weaknesses, Dr. Dao noted that more than 70% of participants were women. The study was short in duration, fewer than half of patients underwent muscle biopsy to confirm myositis, and only two thirds of patients underwent electromyography/nerve conduction studies to show evidence of myositis. There was a high placebo response (44%), the CK values were not high at the start of the trial, and they did not change with treatment.
No analysis was performed to evaluate the efficacy of IVIG across dermatomyositis subgroups – defined by autoantibodies – but the study likely was not powered to do so. These subgroups might respond differently to IVIG, yielding important information, Fiorentino said.
The study provided efficacy data for only one formulation of IVIG, Octagam 10%, which was approved for dermatomyositis by the Food and Drug Administration in 2021 on the basis of this trial. However, in the United States, patients with dermatomyositis are treated with multiple brands of IVIG. “The decision around IVIG brand is largely determined by third-party payers, and for the most part, the different brands are used interchangeably from the standpoint of the treating provider,” Dr. Fiorentino said. “This will likely continue to be the case, as the results of this study are generally being extrapolated to all brands of IVIG.”
Multiple IVIG brands that have been used for immune-mediated diseases differ in concentration, content of IgA, sugar concentration, additives, and preparations (for example, the need for reconstitution vs. being ready to use), Dr. Dao said. Octagam 10% is the only brand approved by the FDA for adult dermatomyositis; hence, cost can be an issue for patients if other brands are used off label. The typical cost of IVIG is $100-$400 per gram; a typical course of treatment is estimated to be $30,000-$40,000 per month. “However, if Octagam is not available or a patient has a reaction to it, clinicians may use other IVIG brands as deemed medically necessary to treat their patients,” she said.
Dr. Aggarwal has financial relationships with more than 15 pharmaceutical companies, including Octapharma, which provided financial support for this trial. Some of the coauthors were employees of Octapharma or had financial relationships with the company. Dr. Dao disclosed no relevant financial relationships. Dr. Fiorentino has conducted sponsored research for Pfizer and Argenyx, has received research funding from Serono, and is a paid adviser to Bristol-Myers Squibb, Janssen, Acelyrin, and Corbus.
A version of this article first appeared on Medscape.com.
With use of intravenous immunoglobulin for the treatment of adults with dermatomyositis, a significantly higher percentage of patients experienced at least minimal improvement in disease activity in comparison with placebo in the first-ever phase 3 trial of the blood-product therapy for the condition.
Until this trial, published in the New England Journal of Medicine, there had not been an extensive evaluation of IVIG for the treatment of dermatomyositis, the study’s authors noted.
Glucocorticoids are typically offered as first-line therapy, followed by various immunosuppressants. IVIG is composed of purified liquid IgG concentrates from human plasma. It has been prescribed off label as second- or third-line therapy for dermatomyositis, usually along with immunosuppressive drugs. In European guidelines, it has been recommended as a glucocorticoid-sparing agent for patients with this condition.
“The study provides support that IVIG is effective in treating the signs and symptoms of patients with dermatomyositis, at least in the short term,” said David Fiorentino, MD, PhD, professor of dermatology and associate residency program director at Stanford Health Care, Stanford, California, who was not involved in the study.
“IVIG appears to be effective for patients with any severity level and works relatively quickly [within 1 month of therapy],” he added. “IVIG is effective in treating both the muscle symptoms as well as the rash of dermatomyositis, which is important, as both organ systems can cause significant patient morbidity in this disease.”
Time to improvement was shorter with IVIG than with placebo (a median of 35 days vs. 115 days), said Kathryn H. Dao, MD, associate professor in the division of rheumatic diseases at the University of Texas Southwestern Medical Center, Dallas, who was not involved in the study.
The study’s greatest strengths are its international, multicenter, randomized, placebo-controlled design, Dr. Dao said. In addition, “these patients were permitted to be on background medicines that we typically use in real-world situations.”
Study methodology
Researchers led by Rohit Aggarwal, MD, of the division of rheumatology and clinical immunology at the University of Pittsburgh, recruited patients aged 18-80 years with active dermatomyositis. Individuals were randomly assigned in a 1:1 ratio to receive either IVIG at a dose of 2.0 g/kg of body weight or placebo (0.9% sodium chloride) every 4 weeks for 16 weeks.
Those who were administered placebo and those who did not experience confirmed clinical deterioration while receiving IVIG could participate in an open-label extension phase for another 24 weeks.
The primary endpoint was a response, defined as a Total Improvement Score (TIS) of at least 20 (indicating at least minimal improvement) at week 16 and no confirmed deterioration up to week 16. The TIS is a weighted composite score that reflects the change in a core set of six measures of myositis activity over time. Scores span from 0 to 100, with higher scores indicating more significant improvement.
Secondary endpoints
Key secondary endpoints included moderate improvement (TIS ≥ 40) and major improvement (TIS ≥ 60) and change in score on the Cutaneous Dermatomyositis Disease Area and Severity Index.
A total of 95 patients underwent randomization; 47 patients received IVIG and 48 received placebo. At 16 weeks, a TIS of at least 20 occurred in 37 of 47 (79%) patients who received IVIG and in 21 of 48 (44%) patients with placebo (difference, 35%; 95% confidence interval, 17%-53%; P < .001).
The results with respect to the secondary endpoints, including at least moderate improvement and major improvement, were generally in the same direction as the results of the primary endpoint analysis, except for change in creatine kinase (CK) level (an individual core measure of the TIS), which did not differ meaningfully between the two groups.
Adverse events
Over the course of 40 weeks, 282 treatment-related adverse events were documented among patients who received IVIG. Headache was experienced by 42%, pyrexia by 19%, and nausea by 16%. Nine serious adverse events occurred and were believed to be associated with IVIG, including six thromboembolic events.
Despite the favorable outcome observed with IVIG, in an editorial that accompanied the study, Anthony A. Amato, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, noted that “most of the core components of the TIS are subjective. Because of the high percentage of patients who had a response with placebo, large numbers of patients will be needed in future trials to show a significant difference between trial groups, or the primary endpoint would need to be set higher (e.g., a TIS of ≥40).”
Dr. Dao thought it was significant that the study proactively assessed patients for venous thrombotic events (VTEs) after each infusion. There were eight events in six patients who received IVIG. “Of interest and possibly practice changing is the finding that slowing the IVIG infusion rate from 0.12 to 0.04 mL/kg per minute reduced the incidence of VTEs from 1.54/100 patient-months to 0.54/100 patient-months,” she said. “This is important, as it informs clinicians that IVIG infusion rates should be slower for patients with active dermatomyositis to reduce the risk for blood clots.”
Study weaknesses
A considerable proportion of patients with dermatomyositis do not have clinical muscle involvement but do have rash and do not substantially differ in any other ways from those with classic dermatomyositis, Dr. Fiorentino said.
“These patients were not eligible to enter the trial, and so we have no data on the efficacy of IVIG in this population,” he said. “Unfortunately, these patients might now be denied insurance reimbursement for IVIG therapy, given that they are not part of the indicated patient population in the label.”
In addition, there is limited information about Black, Asian, or Hispanic patients because few of those patients participated in the study. That is also the case for patients younger than 18, which for this disease is relevant because incidence peaks in younger patients (juvenile dermatomyositis), Dr. Fiorentino noted.
Among the study’s weaknesses, Dr. Dao noted that more than 70% of participants were women. The study was short in duration, fewer than half of patients underwent muscle biopsy to confirm myositis, and only two thirds of patients underwent electromyography/nerve conduction studies to show evidence of myositis. There was a high placebo response (44%), the CK values were not high at the start of the trial, and they did not change with treatment.
No analysis was performed to evaluate the efficacy of IVIG across dermatomyositis subgroups – defined by autoantibodies – but the study likely was not powered to do so. These subgroups might respond differently to IVIG, yielding important information, Fiorentino said.
The study provided efficacy data for only one formulation of IVIG, Octagam 10%, which was approved for dermatomyositis by the Food and Drug Administration in 2021 on the basis of this trial. However, in the United States, patients with dermatomyositis are treated with multiple brands of IVIG. “The decision around IVIG brand is largely determined by third-party payers, and for the most part, the different brands are used interchangeably from the standpoint of the treating provider,” Dr. Fiorentino said. “This will likely continue to be the case, as the results of this study are generally being extrapolated to all brands of IVIG.”
Multiple IVIG brands that have been used for immune-mediated diseases differ in concentration, content of IgA, sugar concentration, additives, and preparations (for example, the need for reconstitution vs. being ready to use), Dr. Dao said. Octagam 10% is the only brand approved by the FDA for adult dermatomyositis; hence, cost can be an issue for patients if other brands are used off label. The typical cost of IVIG is $100-$400 per gram; a typical course of treatment is estimated to be $30,000-$40,000 per month. “However, if Octagam is not available or a patient has a reaction to it, clinicians may use other IVIG brands as deemed medically necessary to treat their patients,” she said.
Dr. Aggarwal has financial relationships with more than 15 pharmaceutical companies, including Octapharma, which provided financial support for this trial. Some of the coauthors were employees of Octapharma or had financial relationships with the company. Dr. Dao disclosed no relevant financial relationships. Dr. Fiorentino has conducted sponsored research for Pfizer and Argenyx, has received research funding from Serono, and is a paid adviser to Bristol-Myers Squibb, Janssen, Acelyrin, and Corbus.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
How do patients with chronic urticaria fare during pregnancy?
In addition, the rates of preterm births and medical problems of newborns in patients with CU are similar to those of the normal population and not linked to treatment used during pregnancy.
Those are the key findings from an analysis of new data from PREG-CU, an international, multicenter study of the Urticaria Centers of Reference and Excellence (UCARE) network. Results from the first PREG-CU analysis published in 2021 found that CU improved in about half of patients with CU during pregnancy. “However, two in five patients reported acute exacerbations of CU especially at the beginning and end of pregnancy,” investigators led by Emek Kocatürk, MD, of the department of dermatology and UCARE at Koç University School of Medicine, Istanbul, wrote in the new study, recently published in the Journal of the European Academy of Dermatology and Venereology.
“In addition, 1 in 10 pregnant CU patients required urticaria emergency care and 1 of 6 had angioedema during pregnancy,” they said. Risk factors for worsening CU during pregnancy, they added, were “mild disease and no angioedema before pregnancy, not taking treatment before pregnancy, chronic inducible urticaria, CU worsening during a previous pregnancy, stress as a driver of exacerbations, and treatment during pregnancy.”
Analysis involved 288 pregnant women
To optimize treatment of CU during pregnancy and to better understand how treatment affects pregnancy outcomes, the researchers analyzed 288 pregnancies in 288 women with CU from 13 countries and 21 centers worldwide. Their mean age at pregnancy was 32.1 years, and their mean duration of CU was 84.9 months. Prior to pregnancy, 35.7% of patients rated the severity of their CU symptoms as mild, 34.2% rated it as moderate, and 29.7% rated it as severe.
The researchers found that during pregnancy, 60% of patients used urticaria medication, including standard-dose second-generation H1-antihistamines (35.1%), first-generation H1-antihistamines (7.6%), high-dose second-generation H1-antihistamines (5.6%), and omalizumab (5.6%). The preterm birth rate was 10.2%, which was similar between patients who did and did not receive treatment during pregnancy (11.6% vs. 8.7%, respectively; P = .59).
On multivariate logistic regression, two predictors for preterm birth emerged: giving birth to twins (a 13.3-fold increased risk; P = .016) and emergency referrals for CU (a 4.3-fold increased risk; P =.016). The cesarean delivery rate was 51.3%, and more than 90% of newborns were healthy at birth. There was no link between any patient or disease characteristics or treatments and medical problems at birth.
In other findings, 78.8% of women with CU breastfed their babies. Of the 58 patients who did not breastfeed, 20.7% indicated severe urticaria/angioedema and/or taking medications as the main reason for not breastfeeding.
“Most CU patients use treatment during pregnancy and such treatments, especially second generation H1 antihistamines, seem to be safe during pregnancy regardless of the trimester,” the researchers concluded. “Outcomes of pregnancy in patients with CU were similar compared to the general population and not linked to treatment used during pregnancy. Notably, emergency referral for CU was an independent risk factor for preterm birth,” and the high cesarean delivery rate was “probably linked to comorbidities associated with the disease,” they added. “Overall, these findings suggest that patients should continue their treatments using an individualized dose to provide optimal symptom control.”
International guidelines
The authors noted that international guidelines for the management of urticaria published in 2022 suggest that modern second-generation H1-antihistamines should be used for pregnant patients, preferably loratadine with a possible extrapolation to desloratadine, cetirizine, or levocetirizine.
“Similarly, in this population, we found that cetirizine and loratadine were the most commonly used antihistamines, followed by levocetirizine and fexofenadine,” Dr. Kocatürk and colleagues wrote.
“Guidelines also suggest that the use of first-generation H1-antihistamines should be avoided given their sedative effects; but if these are to be given, it would be wise to know that use of first-generation H1-antihistamines immediately before parturition could cause respiratory depression and other adverse effects in the neonate,” they added, noting that chlorpheniramine and diphenhydramine are the first-generation H1-antihistamines with the greatest evidence of safety in pregnancy.
They acknowledged certain limitations of the analysis, including its retrospective design and the fact that there were no data on low birth weight, small for gestational age, or miscarriage rates. In addition, disease activity or severity during pregnancy and after birth were not monitored.
Asked to comment on these results, Raj Chovatiya, MD, PhD, who directs the center for eczema and itch in the department of dermatology at Northwestern University, Chicago, noted that despite a higher prevalence of CU among females compared with males, very little is known about how the condition is managed during pregnancy. “This retrospective study shows that most patients continue to utilize CU treatment during pregnancy (primarily second-generation antihistamines), with similar birth outcomes as the general population,” he said. “Interestingly, cesarean rates were higher among mothers with CU, and emergency CU referral was a risk factor for preterm birth. While additional prospective studies are needed, these results suggest that CU patients should be carefully managed, particularly during pregnancy, when treatment should be optimized.”
Dr. Kocatürk reported having received personal fees from Novartis, Ibrahim Etem-Menarini, and Sanofi, outside the submitted work. Many coauthors reported having numerous financial disclosures. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arcutis, Arena, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
In addition, the rates of preterm births and medical problems of newborns in patients with CU are similar to those of the normal population and not linked to treatment used during pregnancy.
Those are the key findings from an analysis of new data from PREG-CU, an international, multicenter study of the Urticaria Centers of Reference and Excellence (UCARE) network. Results from the first PREG-CU analysis published in 2021 found that CU improved in about half of patients with CU during pregnancy. “However, two in five patients reported acute exacerbations of CU especially at the beginning and end of pregnancy,” investigators led by Emek Kocatürk, MD, of the department of dermatology and UCARE at Koç University School of Medicine, Istanbul, wrote in the new study, recently published in the Journal of the European Academy of Dermatology and Venereology.
“In addition, 1 in 10 pregnant CU patients required urticaria emergency care and 1 of 6 had angioedema during pregnancy,” they said. Risk factors for worsening CU during pregnancy, they added, were “mild disease and no angioedema before pregnancy, not taking treatment before pregnancy, chronic inducible urticaria, CU worsening during a previous pregnancy, stress as a driver of exacerbations, and treatment during pregnancy.”
Analysis involved 288 pregnant women
To optimize treatment of CU during pregnancy and to better understand how treatment affects pregnancy outcomes, the researchers analyzed 288 pregnancies in 288 women with CU from 13 countries and 21 centers worldwide. Their mean age at pregnancy was 32.1 years, and their mean duration of CU was 84.9 months. Prior to pregnancy, 35.7% of patients rated the severity of their CU symptoms as mild, 34.2% rated it as moderate, and 29.7% rated it as severe.
The researchers found that during pregnancy, 60% of patients used urticaria medication, including standard-dose second-generation H1-antihistamines (35.1%), first-generation H1-antihistamines (7.6%), high-dose second-generation H1-antihistamines (5.6%), and omalizumab (5.6%). The preterm birth rate was 10.2%, which was similar between patients who did and did not receive treatment during pregnancy (11.6% vs. 8.7%, respectively; P = .59).
On multivariate logistic regression, two predictors for preterm birth emerged: giving birth to twins (a 13.3-fold increased risk; P = .016) and emergency referrals for CU (a 4.3-fold increased risk; P =.016). The cesarean delivery rate was 51.3%, and more than 90% of newborns were healthy at birth. There was no link between any patient or disease characteristics or treatments and medical problems at birth.
In other findings, 78.8% of women with CU breastfed their babies. Of the 58 patients who did not breastfeed, 20.7% indicated severe urticaria/angioedema and/or taking medications as the main reason for not breastfeeding.
“Most CU patients use treatment during pregnancy and such treatments, especially second generation H1 antihistamines, seem to be safe during pregnancy regardless of the trimester,” the researchers concluded. “Outcomes of pregnancy in patients with CU were similar compared to the general population and not linked to treatment used during pregnancy. Notably, emergency referral for CU was an independent risk factor for preterm birth,” and the high cesarean delivery rate was “probably linked to comorbidities associated with the disease,” they added. “Overall, these findings suggest that patients should continue their treatments using an individualized dose to provide optimal symptom control.”
International guidelines
The authors noted that international guidelines for the management of urticaria published in 2022 suggest that modern second-generation H1-antihistamines should be used for pregnant patients, preferably loratadine with a possible extrapolation to desloratadine, cetirizine, or levocetirizine.
“Similarly, in this population, we found that cetirizine and loratadine were the most commonly used antihistamines, followed by levocetirizine and fexofenadine,” Dr. Kocatürk and colleagues wrote.
“Guidelines also suggest that the use of first-generation H1-antihistamines should be avoided given their sedative effects; but if these are to be given, it would be wise to know that use of first-generation H1-antihistamines immediately before parturition could cause respiratory depression and other adverse effects in the neonate,” they added, noting that chlorpheniramine and diphenhydramine are the first-generation H1-antihistamines with the greatest evidence of safety in pregnancy.
They acknowledged certain limitations of the analysis, including its retrospective design and the fact that there were no data on low birth weight, small for gestational age, or miscarriage rates. In addition, disease activity or severity during pregnancy and after birth were not monitored.
Asked to comment on these results, Raj Chovatiya, MD, PhD, who directs the center for eczema and itch in the department of dermatology at Northwestern University, Chicago, noted that despite a higher prevalence of CU among females compared with males, very little is known about how the condition is managed during pregnancy. “This retrospective study shows that most patients continue to utilize CU treatment during pregnancy (primarily second-generation antihistamines), with similar birth outcomes as the general population,” he said. “Interestingly, cesarean rates were higher among mothers with CU, and emergency CU referral was a risk factor for preterm birth. While additional prospective studies are needed, these results suggest that CU patients should be carefully managed, particularly during pregnancy, when treatment should be optimized.”
Dr. Kocatürk reported having received personal fees from Novartis, Ibrahim Etem-Menarini, and Sanofi, outside the submitted work. Many coauthors reported having numerous financial disclosures. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arcutis, Arena, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
In addition, the rates of preterm births and medical problems of newborns in patients with CU are similar to those of the normal population and not linked to treatment used during pregnancy.
Those are the key findings from an analysis of new data from PREG-CU, an international, multicenter study of the Urticaria Centers of Reference and Excellence (UCARE) network. Results from the first PREG-CU analysis published in 2021 found that CU improved in about half of patients with CU during pregnancy. “However, two in five patients reported acute exacerbations of CU especially at the beginning and end of pregnancy,” investigators led by Emek Kocatürk, MD, of the department of dermatology and UCARE at Koç University School of Medicine, Istanbul, wrote in the new study, recently published in the Journal of the European Academy of Dermatology and Venereology.
“In addition, 1 in 10 pregnant CU patients required urticaria emergency care and 1 of 6 had angioedema during pregnancy,” they said. Risk factors for worsening CU during pregnancy, they added, were “mild disease and no angioedema before pregnancy, not taking treatment before pregnancy, chronic inducible urticaria, CU worsening during a previous pregnancy, stress as a driver of exacerbations, and treatment during pregnancy.”
Analysis involved 288 pregnant women
To optimize treatment of CU during pregnancy and to better understand how treatment affects pregnancy outcomes, the researchers analyzed 288 pregnancies in 288 women with CU from 13 countries and 21 centers worldwide. Their mean age at pregnancy was 32.1 years, and their mean duration of CU was 84.9 months. Prior to pregnancy, 35.7% of patients rated the severity of their CU symptoms as mild, 34.2% rated it as moderate, and 29.7% rated it as severe.
The researchers found that during pregnancy, 60% of patients used urticaria medication, including standard-dose second-generation H1-antihistamines (35.1%), first-generation H1-antihistamines (7.6%), high-dose second-generation H1-antihistamines (5.6%), and omalizumab (5.6%). The preterm birth rate was 10.2%, which was similar between patients who did and did not receive treatment during pregnancy (11.6% vs. 8.7%, respectively; P = .59).
On multivariate logistic regression, two predictors for preterm birth emerged: giving birth to twins (a 13.3-fold increased risk; P = .016) and emergency referrals for CU (a 4.3-fold increased risk; P =.016). The cesarean delivery rate was 51.3%, and more than 90% of newborns were healthy at birth. There was no link between any patient or disease characteristics or treatments and medical problems at birth.
In other findings, 78.8% of women with CU breastfed their babies. Of the 58 patients who did not breastfeed, 20.7% indicated severe urticaria/angioedema and/or taking medications as the main reason for not breastfeeding.
“Most CU patients use treatment during pregnancy and such treatments, especially second generation H1 antihistamines, seem to be safe during pregnancy regardless of the trimester,” the researchers concluded. “Outcomes of pregnancy in patients with CU were similar compared to the general population and not linked to treatment used during pregnancy. Notably, emergency referral for CU was an independent risk factor for preterm birth,” and the high cesarean delivery rate was “probably linked to comorbidities associated with the disease,” they added. “Overall, these findings suggest that patients should continue their treatments using an individualized dose to provide optimal symptom control.”
International guidelines
The authors noted that international guidelines for the management of urticaria published in 2022 suggest that modern second-generation H1-antihistamines should be used for pregnant patients, preferably loratadine with a possible extrapolation to desloratadine, cetirizine, or levocetirizine.
“Similarly, in this population, we found that cetirizine and loratadine were the most commonly used antihistamines, followed by levocetirizine and fexofenadine,” Dr. Kocatürk and colleagues wrote.
“Guidelines also suggest that the use of first-generation H1-antihistamines should be avoided given their sedative effects; but if these are to be given, it would be wise to know that use of first-generation H1-antihistamines immediately before parturition could cause respiratory depression and other adverse effects in the neonate,” they added, noting that chlorpheniramine and diphenhydramine are the first-generation H1-antihistamines with the greatest evidence of safety in pregnancy.
They acknowledged certain limitations of the analysis, including its retrospective design and the fact that there were no data on low birth weight, small for gestational age, or miscarriage rates. In addition, disease activity or severity during pregnancy and after birth were not monitored.
Asked to comment on these results, Raj Chovatiya, MD, PhD, who directs the center for eczema and itch in the department of dermatology at Northwestern University, Chicago, noted that despite a higher prevalence of CU among females compared with males, very little is known about how the condition is managed during pregnancy. “This retrospective study shows that most patients continue to utilize CU treatment during pregnancy (primarily second-generation antihistamines), with similar birth outcomes as the general population,” he said. “Interestingly, cesarean rates were higher among mothers with CU, and emergency CU referral was a risk factor for preterm birth. While additional prospective studies are needed, these results suggest that CU patients should be carefully managed, particularly during pregnancy, when treatment should be optimized.”
Dr. Kocatürk reported having received personal fees from Novartis, Ibrahim Etem-Menarini, and Sanofi, outside the submitted work. Many coauthors reported having numerous financial disclosures. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arcutis, Arena, Incyte, Pfizer, Regeneron, and Sanofi Genzyme.
FROM JEADV
Physicians speak out: Why they love or hate incentive bonuses
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Incentive bonuses have long been part and parcel of many physicians’ compensation packages. They allow doctors in some specialties to boost their compensation by tens of thousands of dollars.
Often tied to metrics that doctors must hit,
A recent Medscape poll asked what physicians think about incentive bonuses and whether or not tying metrics to salary is an outdated practice that interferes with the integrity of a physician’s job or contributes to excellence in patient care and increased productivity.
Here is what 406 physicians who answered the poll, which ran from Aug. 17 to Sept. 1, had to say about incentive bonuses:
More than half the physicians polled (58%) received an incentive bonus in 2021. Of those who received a bonus, 44% received up to $25,000. Almost 30% received $25,001-$50,000 in incentive bonus money. Only 14% received more than $100,000.
When we asked physicians which metrics they prefer their bonus to be based on, a large majority (64%) agreed quality of care was most relevant. Other metrics that respondents think appropriate included professionalism (40%), patient outcomes (40%), patient satisfaction (34%), patient volume (26%), market expansion (7%), and other (3%).
The problem with bonuses
Once thought to improve quality and consistency of care, incentive bonuses may be falling out of favor. Developing, administrating, and tracking them may be cumbersome for the institutions that advocate for them. For instance, determining who gave quality care and how to measure that care can be difficult.
What’s more, some top health care employers, Mayo Clinic and Kaiser Permanente, have switched from the incentive bonus model to straight salaries. Data show that the number of tests patients have and the number of treatments they try decreases when doctors receive straight salaries.
In fact, 74% of the polled physicians think that bonuses can result in consequences like unnecessary tests and higher patient costs. Three-fourths of respondents don’t think incentives improve patient care either.
Physicians have long thought incentive bonuses can also have unintended consequences. For example, tying a physician’s monetary reward to metrics such as patient outcomes, like adherence to treatment protocols, may mean that noncompliant patients can jeopardize your metrics and prevent physicians from getting bonuses.
A Merritt Hawkins’ 2019 Review of Physician and Advanced Practitioner Recruiting Incentives found that 56% of bonuses are based in whole or in part on metrics like a patient’s adherence.
Additionally, tying monetary rewards to patient volume encourages some physicians to overbook patients, work more and longer hours, and risk burnout to meet their bonus criteria.
When we asked how hard it was to meet metrics in the Medscape poll, 45% of respondents who receive incentive bonuses said it was somewhat or very difficult. Only 9% consider it very easy. And 71% of physicians say their bonus is at risk because of not meeting their metrics.
Not surprisingly, large pay-for-performance bonuses are only offered to certain specialists and physician specialties in high demand. An orthopedist, for example, can earn up to an average of $126,000 in incentive bonuses, while a pediatrician brings in an average of $28,000, according to the Medscape Physician Compensation Report 2022.
Yet physicians are still torn
Despite these negatives, physicians are split about whether bonuses are good for doctors. The poll shows 51% said no, and 49% said yes. Further, physicians were split 50-50 on whether the bonus makes physicians more productive. Interestingly though, 76% think the bonus compensation method should be phased out in favor of straight salaries.
But many physicians may welcome the “lump sum” nature of receiving large bonuses at certain times of the year to help pay off student loan debt or other expenses, or are just comfortable having a bonus.
Financially speaking
If you have the choice, you may fare better by taking a higher salary and eliminating a bonus. Receiving your pay throughout the year may be preferable to receiving large lump sums only at certain times. Another thing to remember about your incentive bonus is that they are sometimes taxed more heavily based on “supplemental income.” The IRS considers bonuses supplemental to your income, so they may have a higher withholding rate, which can feel penalizing. You may have noticed the extra withholding in your last bonus check.
A version of this article first appeared on Medscape.com.
Three COVID scenarios that could spell trouble for the fall
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dupilumab study outlines benefits, safety profile in infants, preschoolers with atopic dermatitis
at 31 treatment centers in North America and Europe.
Children younger than 6 years with moderate to severe AD have few options if their symptoms are uncontrolled with topical therapies, and persistent itchiness has a negative impact on quality of life for patients and families, Amy S. Paller, MD, professor and chair of dermatology, and professor of pediatrics at Northwestern University, Chicago, and colleagues wrote in the study, published in the Lancet.
The study was the basis of the Food and Drug Administration expanded approval of dupilumab in June 2022, to include children aged 6 months to 5 years with moderate to severe AD, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Regulatory submission for this age group is under review by the European Medicines Agency, and by regulatory authorities in other countries, according to the manufacturers.
Dupilumab (Dupixent), which inhibits the signaling of the interleukin-4 and IL-13 pathways, was first approved in 2017 for treating adults with moderate to severe AD.
“There has not been a biologic approved before at such a young age, and for such a common disease,” Dr. Paller said in an interview. “This is the drug that has revolutionized care of the most common inflammatory skin disease in children, and this is the pivotal study that brought it to market for the youngest children who suffer from the severe forms.”
The study also sets a precedent for a lower threshold for starting systemic medication in young children for treating moderate to severe disease given the absence of severe side effects and no need for lab monitoring, Dr. Paller noted. However, dupilumab will also be closely watched “for both impact on the developing immune system and the possibility that it will alter the long-term course of the eczema and the development of allergic comorbidities, such as lowering the risk of developing asthma, GI, allergy, and possibly other conditions.”
In the study, the researchers randomized 83 children aged 6 months up to 6 years to treatment with dupilumab, administered subcutaneously, and 79 to placebo every 4 weeks for 16 weeks; both groups also received topical corticosteroids. Dosage of dupilumab was based on body weight; those with a body weight of 5-15 kg received 200 mg, while those with a body weight of 15-30 kg received 300 mg. The primary endpoint was the proportion of patients with clear or almost clear skin at 16 weeks, defined as scores of 0 or 1 on the Investigator’s Global Assessment.
After 16 weeks, 28% of dupilumab patients met the primary endpoint versus 4% of those on placebo (P < .0001). In addition, 53% of dupilumab patients met the key secondary endpoint of a 75% improvement from baseline in Eczema Area and Severity Index, compared with 11% of patients on placebo (P < .0001). Treatment with dupilumab also resulted in significantly greater improvements in pruritus and skin pain, and sleep quality, as well as improved quality of life for patients and their caregivers, the authors reported.
Overall, adverse event rates were slightly lower in the dupilumab-treated patients, compared with patients on placebo (64% vs. 74%); there were no adverse events related to dupilumab that were serious or resulted in treatment discontinuation. Treatment-emergent adverse effects that were reported in 3% or more of patients and affected more of those on dupilumab than those on placebo included molluscum contagiosum (5% vs. 3%), viral gastroenteritis (4% vs. 0), rhinorrhea (5% vs. 1%), dental caries (5% vs. 0), and conjunctivitis (4% vs 0).
The rate of skin infections among the children on dupilumab was 12% vs. 24% among those on placebo.
Severe and treatment-related adverse events also were similar in both subgroups of body weight.
The findings were limited by the small number of patients younger than 2 years and the lack of study sites outside of North America and Europe, the researchers noted. However, the results were strengthened by the randomized, double-blind design and use of background topical therapy to provide a real-world safety and efficacy assessment in a very young population.
Overcoming injection issues
The safety profile for dupilumab, which is of the highest importance, “did not surprise me at all,” Dr. Paller said in an interview. “My only surprise is that the placebo injections actually led to more injection site reactions than [with] dupilumab, but numbers were quite low in both groups.” (Rates were 2% among those on dupilumab and 3% among those on placebo.)
The major barrier to the use of dupilumab in clinical practice is the requirement for injection, which, she explained, can be “unbearable for some young children, and thus becomes impossible for parents because of lack of cooperation and their intensified concern about giving the injection,” because of their child’s response.
“We like to administer the first dose in the office, allowing us to teach parents a few tricks related to proper technique,” including audio and visual distraction, tactile stimulation before and during the injection, use of topical anesthetic if helpful, “and making sure that the medication is at room temperature before administration,” she said. Cost is another potential barrier; however, even public insurance has been covering the medication, often after optimized use of topical medications has been unsuccessful.
Future research questions
As for additional research, the current study had a relatively small number of patients younger than 2 years, and more data are needed for this age group, said Dr. Paller. “We also need better understanding of the safety of dupilumab administration when live vaccines are administered. Finally, we certainly want to know what additional effects dupilumab may have beyond just the efficacy for treating eczema.”
In particular, these questions include whether dupilumab modifies the long-term course of the disease, possibly reducing the risk of persistence of disease with advancing age, or even cures the disease if started at a young age, she said. In addition, research has yet to show whether dupilumab might reduce the risk of other atopic disorders, such as asthma, food allergy, and allergic rhinitis.
“Ongoing studies and real-life experiences in the next several years will help us to answer these questions,” Dr. Paller said.
Data support safety, efficacy, quality of life
AD is associated with immense quality of life impairment, Raj Chovatiya, MD, of Northwestern University, Chicago, said in an interview. Most AD is initially diagnosed in early childhood, but previous treatment options for those with moderate to severe disease have been limited by safety concerns, which adds to the burden on infants and young children, and their parents and caregivers, said Dr. Chovatiya, who was not involved in the study.
“This phase 3 study showed that dupilumab, a fully human monoclonal antibody that selectively inhibits IL-4 and IL-13 mediated type 2 inflammatory signaling, provided both meaningful and statistically significant improvement in AD severity, extent of disease, and itch in patients,” he said. Dupilumab also improved children’s sleep quality and the overall quality of life in both patients and caregivers.
“These findings were quite similar to those described in older children and adults, where dupilumab is already approved for the treatment of moderate-severe AD and has demonstrated real-world safety and efficacy,” said Dr. Chovatiya. However, “the current study was limited to only a short-term analysis of 16 weeks, an ongoing open-label study should further address long-term treatment responses.”
The study was supported by Sanofi and Regeneron Pharmaceuticals. In addition to being an investigator for Regeneron, and several other pharmaceutical companies, Dr. Paller has been a consultant with honorarium for Regeneron, Sanofi, and multiple other companies. Dr. Chovatiya disclosed serving as a consultant and speaker for Regeneron and Sanofi, but was not involved in the current study.
at 31 treatment centers in North America and Europe.
Children younger than 6 years with moderate to severe AD have few options if their symptoms are uncontrolled with topical therapies, and persistent itchiness has a negative impact on quality of life for patients and families, Amy S. Paller, MD, professor and chair of dermatology, and professor of pediatrics at Northwestern University, Chicago, and colleagues wrote in the study, published in the Lancet.
The study was the basis of the Food and Drug Administration expanded approval of dupilumab in June 2022, to include children aged 6 months to 5 years with moderate to severe AD, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Regulatory submission for this age group is under review by the European Medicines Agency, and by regulatory authorities in other countries, according to the manufacturers.
Dupilumab (Dupixent), which inhibits the signaling of the interleukin-4 and IL-13 pathways, was first approved in 2017 for treating adults with moderate to severe AD.
“There has not been a biologic approved before at such a young age, and for such a common disease,” Dr. Paller said in an interview. “This is the drug that has revolutionized care of the most common inflammatory skin disease in children, and this is the pivotal study that brought it to market for the youngest children who suffer from the severe forms.”
The study also sets a precedent for a lower threshold for starting systemic medication in young children for treating moderate to severe disease given the absence of severe side effects and no need for lab monitoring, Dr. Paller noted. However, dupilumab will also be closely watched “for both impact on the developing immune system and the possibility that it will alter the long-term course of the eczema and the development of allergic comorbidities, such as lowering the risk of developing asthma, GI, allergy, and possibly other conditions.”
In the study, the researchers randomized 83 children aged 6 months up to 6 years to treatment with dupilumab, administered subcutaneously, and 79 to placebo every 4 weeks for 16 weeks; both groups also received topical corticosteroids. Dosage of dupilumab was based on body weight; those with a body weight of 5-15 kg received 200 mg, while those with a body weight of 15-30 kg received 300 mg. The primary endpoint was the proportion of patients with clear or almost clear skin at 16 weeks, defined as scores of 0 or 1 on the Investigator’s Global Assessment.
After 16 weeks, 28% of dupilumab patients met the primary endpoint versus 4% of those on placebo (P < .0001). In addition, 53% of dupilumab patients met the key secondary endpoint of a 75% improvement from baseline in Eczema Area and Severity Index, compared with 11% of patients on placebo (P < .0001). Treatment with dupilumab also resulted in significantly greater improvements in pruritus and skin pain, and sleep quality, as well as improved quality of life for patients and their caregivers, the authors reported.
Overall, adverse event rates were slightly lower in the dupilumab-treated patients, compared with patients on placebo (64% vs. 74%); there were no adverse events related to dupilumab that were serious or resulted in treatment discontinuation. Treatment-emergent adverse effects that were reported in 3% or more of patients and affected more of those on dupilumab than those on placebo included molluscum contagiosum (5% vs. 3%), viral gastroenteritis (4% vs. 0), rhinorrhea (5% vs. 1%), dental caries (5% vs. 0), and conjunctivitis (4% vs 0).
The rate of skin infections among the children on dupilumab was 12% vs. 24% among those on placebo.
Severe and treatment-related adverse events also were similar in both subgroups of body weight.
The findings were limited by the small number of patients younger than 2 years and the lack of study sites outside of North America and Europe, the researchers noted. However, the results were strengthened by the randomized, double-blind design and use of background topical therapy to provide a real-world safety and efficacy assessment in a very young population.
Overcoming injection issues
The safety profile for dupilumab, which is of the highest importance, “did not surprise me at all,” Dr. Paller said in an interview. “My only surprise is that the placebo injections actually led to more injection site reactions than [with] dupilumab, but numbers were quite low in both groups.” (Rates were 2% among those on dupilumab and 3% among those on placebo.)
The major barrier to the use of dupilumab in clinical practice is the requirement for injection, which, she explained, can be “unbearable for some young children, and thus becomes impossible for parents because of lack of cooperation and their intensified concern about giving the injection,” because of their child’s response.
“We like to administer the first dose in the office, allowing us to teach parents a few tricks related to proper technique,” including audio and visual distraction, tactile stimulation before and during the injection, use of topical anesthetic if helpful, “and making sure that the medication is at room temperature before administration,” she said. Cost is another potential barrier; however, even public insurance has been covering the medication, often after optimized use of topical medications has been unsuccessful.
Future research questions
As for additional research, the current study had a relatively small number of patients younger than 2 years, and more data are needed for this age group, said Dr. Paller. “We also need better understanding of the safety of dupilumab administration when live vaccines are administered. Finally, we certainly want to know what additional effects dupilumab may have beyond just the efficacy for treating eczema.”
In particular, these questions include whether dupilumab modifies the long-term course of the disease, possibly reducing the risk of persistence of disease with advancing age, or even cures the disease if started at a young age, she said. In addition, research has yet to show whether dupilumab might reduce the risk of other atopic disorders, such as asthma, food allergy, and allergic rhinitis.
“Ongoing studies and real-life experiences in the next several years will help us to answer these questions,” Dr. Paller said.
Data support safety, efficacy, quality of life
AD is associated with immense quality of life impairment, Raj Chovatiya, MD, of Northwestern University, Chicago, said in an interview. Most AD is initially diagnosed in early childhood, but previous treatment options for those with moderate to severe disease have been limited by safety concerns, which adds to the burden on infants and young children, and their parents and caregivers, said Dr. Chovatiya, who was not involved in the study.
“This phase 3 study showed that dupilumab, a fully human monoclonal antibody that selectively inhibits IL-4 and IL-13 mediated type 2 inflammatory signaling, provided both meaningful and statistically significant improvement in AD severity, extent of disease, and itch in patients,” he said. Dupilumab also improved children’s sleep quality and the overall quality of life in both patients and caregivers.
“These findings were quite similar to those described in older children and adults, where dupilumab is already approved for the treatment of moderate-severe AD and has demonstrated real-world safety and efficacy,” said Dr. Chovatiya. However, “the current study was limited to only a short-term analysis of 16 weeks, an ongoing open-label study should further address long-term treatment responses.”
The study was supported by Sanofi and Regeneron Pharmaceuticals. In addition to being an investigator for Regeneron, and several other pharmaceutical companies, Dr. Paller has been a consultant with honorarium for Regeneron, Sanofi, and multiple other companies. Dr. Chovatiya disclosed serving as a consultant and speaker for Regeneron and Sanofi, but was not involved in the current study.
at 31 treatment centers in North America and Europe.
Children younger than 6 years with moderate to severe AD have few options if their symptoms are uncontrolled with topical therapies, and persistent itchiness has a negative impact on quality of life for patients and families, Amy S. Paller, MD, professor and chair of dermatology, and professor of pediatrics at Northwestern University, Chicago, and colleagues wrote in the study, published in the Lancet.
The study was the basis of the Food and Drug Administration expanded approval of dupilumab in June 2022, to include children aged 6 months to 5 years with moderate to severe AD, whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. Regulatory submission for this age group is under review by the European Medicines Agency, and by regulatory authorities in other countries, according to the manufacturers.
Dupilumab (Dupixent), which inhibits the signaling of the interleukin-4 and IL-13 pathways, was first approved in 2017 for treating adults with moderate to severe AD.
“There has not been a biologic approved before at such a young age, and for such a common disease,” Dr. Paller said in an interview. “This is the drug that has revolutionized care of the most common inflammatory skin disease in children, and this is the pivotal study that brought it to market for the youngest children who suffer from the severe forms.”
The study also sets a precedent for a lower threshold for starting systemic medication in young children for treating moderate to severe disease given the absence of severe side effects and no need for lab monitoring, Dr. Paller noted. However, dupilumab will also be closely watched “for both impact on the developing immune system and the possibility that it will alter the long-term course of the eczema and the development of allergic comorbidities, such as lowering the risk of developing asthma, GI, allergy, and possibly other conditions.”
In the study, the researchers randomized 83 children aged 6 months up to 6 years to treatment with dupilumab, administered subcutaneously, and 79 to placebo every 4 weeks for 16 weeks; both groups also received topical corticosteroids. Dosage of dupilumab was based on body weight; those with a body weight of 5-15 kg received 200 mg, while those with a body weight of 15-30 kg received 300 mg. The primary endpoint was the proportion of patients with clear or almost clear skin at 16 weeks, defined as scores of 0 or 1 on the Investigator’s Global Assessment.
After 16 weeks, 28% of dupilumab patients met the primary endpoint versus 4% of those on placebo (P < .0001). In addition, 53% of dupilumab patients met the key secondary endpoint of a 75% improvement from baseline in Eczema Area and Severity Index, compared with 11% of patients on placebo (P < .0001). Treatment with dupilumab also resulted in significantly greater improvements in pruritus and skin pain, and sleep quality, as well as improved quality of life for patients and their caregivers, the authors reported.
Overall, adverse event rates were slightly lower in the dupilumab-treated patients, compared with patients on placebo (64% vs. 74%); there were no adverse events related to dupilumab that were serious or resulted in treatment discontinuation. Treatment-emergent adverse effects that were reported in 3% or more of patients and affected more of those on dupilumab than those on placebo included molluscum contagiosum (5% vs. 3%), viral gastroenteritis (4% vs. 0), rhinorrhea (5% vs. 1%), dental caries (5% vs. 0), and conjunctivitis (4% vs 0).
The rate of skin infections among the children on dupilumab was 12% vs. 24% among those on placebo.
Severe and treatment-related adverse events also were similar in both subgroups of body weight.
The findings were limited by the small number of patients younger than 2 years and the lack of study sites outside of North America and Europe, the researchers noted. However, the results were strengthened by the randomized, double-blind design and use of background topical therapy to provide a real-world safety and efficacy assessment in a very young population.
Overcoming injection issues
The safety profile for dupilumab, which is of the highest importance, “did not surprise me at all,” Dr. Paller said in an interview. “My only surprise is that the placebo injections actually led to more injection site reactions than [with] dupilumab, but numbers were quite low in both groups.” (Rates were 2% among those on dupilumab and 3% among those on placebo.)
The major barrier to the use of dupilumab in clinical practice is the requirement for injection, which, she explained, can be “unbearable for some young children, and thus becomes impossible for parents because of lack of cooperation and their intensified concern about giving the injection,” because of their child’s response.
“We like to administer the first dose in the office, allowing us to teach parents a few tricks related to proper technique,” including audio and visual distraction, tactile stimulation before and during the injection, use of topical anesthetic if helpful, “and making sure that the medication is at room temperature before administration,” she said. Cost is another potential barrier; however, even public insurance has been covering the medication, often after optimized use of topical medications has been unsuccessful.
Future research questions
As for additional research, the current study had a relatively small number of patients younger than 2 years, and more data are needed for this age group, said Dr. Paller. “We also need better understanding of the safety of dupilumab administration when live vaccines are administered. Finally, we certainly want to know what additional effects dupilumab may have beyond just the efficacy for treating eczema.”
In particular, these questions include whether dupilumab modifies the long-term course of the disease, possibly reducing the risk of persistence of disease with advancing age, or even cures the disease if started at a young age, she said. In addition, research has yet to show whether dupilumab might reduce the risk of other atopic disorders, such as asthma, food allergy, and allergic rhinitis.
“Ongoing studies and real-life experiences in the next several years will help us to answer these questions,” Dr. Paller said.
Data support safety, efficacy, quality of life
AD is associated with immense quality of life impairment, Raj Chovatiya, MD, of Northwestern University, Chicago, said in an interview. Most AD is initially diagnosed in early childhood, but previous treatment options for those with moderate to severe disease have been limited by safety concerns, which adds to the burden on infants and young children, and their parents and caregivers, said Dr. Chovatiya, who was not involved in the study.
“This phase 3 study showed that dupilumab, a fully human monoclonal antibody that selectively inhibits IL-4 and IL-13 mediated type 2 inflammatory signaling, provided both meaningful and statistically significant improvement in AD severity, extent of disease, and itch in patients,” he said. Dupilumab also improved children’s sleep quality and the overall quality of life in both patients and caregivers.
“These findings were quite similar to those described in older children and adults, where dupilumab is already approved for the treatment of moderate-severe AD and has demonstrated real-world safety and efficacy,” said Dr. Chovatiya. However, “the current study was limited to only a short-term analysis of 16 weeks, an ongoing open-label study should further address long-term treatment responses.”
The study was supported by Sanofi and Regeneron Pharmaceuticals. In addition to being an investigator for Regeneron, and several other pharmaceutical companies, Dr. Paller has been a consultant with honorarium for Regeneron, Sanofi, and multiple other companies. Dr. Chovatiya disclosed serving as a consultant and speaker for Regeneron and Sanofi, but was not involved in the current study.
FROM THE LANCET
Evusheld PrEP may protect immunocompromised patients from severe COVID-19
Tixagevimab copackaged with cilgavimab (Evusheld) is a safe and effective preexposure prophylaxis (PrEP) in patients undergoing B-cell-depleting therapies who have poor immune response to COVID-19 vaccination and are at high risk for serious COVID-19 illness, a small, single-site study suggests.
Evusheld, the only COVID-19 PrEP option available, has Emergency Use Authorization (EUA) from the Food and Drug Administration for treatment of immunocompromised patients who may not respond sufficiently to COVID-19 vaccination and patients who’ve had a severe adverse reaction to COVID-19 vaccination.
“We report the largest real-world experience of Evusheld in this population, and our findings are encouraging,” lead study author Cassandra Calabrese, DO, rheumatologist and infectious disease specialist at Cleveland Clinic, said in an interview.
“Of 412 patients who received Evusheld, 12 [2.9%] developed breakthrough COVID-19, with 11 having mild courses and 1 who required hospitalization but recovered,” she added.
“Our data suggest that Evusheld PrEP, in combination with aggressive outpatient treatment of COVID-19, is likely effective in lowering risk of severe COVID in this vulnerable group.
“Practitioners who care for patients with immune-mediated inflammatory diseases should triage high-risk patients for Evusheld as well as rapid diagnosis and aggressive outpatient therapy if infected,” Dr. Calabrese advised.
For the study, Dr. Calabrese and colleagues at Cleveland Clinic searched the health care system pharmacy records for patients with immune‐mediated inflammatory diseases (IMIDs) or inborn errors of humoral immunity (IEI) who met the criteria to receive Evusheld. The researchers included patients on B-cell-depleting therapies or with humoral IEI who had received at least one dose of Evusheld and were later diagnosed with COVID-19, and they excluded those treated with B-cell-depleting therapies for cancer.
EVUSHELD was well tolerated
After extracting data on COVID-19 infection, vaccination status, and outcomes, they found that, between Jan. 18 and May 28, 2022, 412 patients with IMIDs or humoral IEI received Evusheld. No deaths occurred among these patients and, overall, they tolerated the medication well.
All 12 patients who experienced breakthrough COVID-19 infection were treated with B-cell-depleting therapies. Among the 12 patients:
- Six patients developed infection 13-84 (median 19) days after receiving 150 mg/150 mg tixagevimab/cilgavimab.
- Six patients developed infection 19-72 (median of 38.5) days after either a single dose of 300 mg/300 mg or a second dose of 150 mg/150 mg.
- Eleven patients had mild illness and recovered at home; one patient was hospitalized and treated with high-flow oxygen. All cases had been vaccinated against COVID-19 (five received two vaccinations, six received three, and one received four).
- One possible serious adverse event involved a patient with COVID-19 and immune-mediated thrombocytopenia (ITP) who was hospitalized soon after receiving Evusheld with ITP flare that resolved with intravenous immunoglobulin.
Dr. Calabrese acknowledged limitations to the study, including few patients, lack of a comparator group, and the study period falling during the Omicron wave.
“Also, nine of the breakthrough cases received additional COVID-19 therapy (oral antiviral or monoclonal antibody), which falls within standard of care for this high-risk group but prevents ascribing effectiveness to individual components of the regimen,” she added.
“Evusheld is authorized for PrEP against COVID-19 in patients at high risk for severe COVID due to suboptimal vaccine responses. This includes patients receiving B-cell-depleting drugs like rituximab, and patients with inborn errors of humoral immunity,” Dr. Calabrese explained.
“It is well known that this group of patients is at very high risk for severe COVID and death, even when fully vaccinated, and it has become clear that more strategies are needed to protect this vulnerable group, including use of Evusheld as well as aggressive treatment if infected,” she added.
Evusheld not always easy to obtain
Although the medication has been available in the United States since January 2022, Dr. Calabrese said, patients may not receive it because of barriers including lack of both awareness and access.
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California San Diego, in La Jolla, said in an interview that he was not surprised by the results, but added that the study was conducted in too few patients to draw any strong conclusions or affect patient care.
“This small study that showed that breakthrough infections occurred but were generally mild, provides a small glimpse of real-world use of tixagevimab/cilgavimab as PrEP for immunocompromised persons,” said Dr. Smith, who was not involved in the study.
“In the setting of Omicron and vaccination, I would expect the same outcomes reported even without the treatment,” he added.
Dr. Smith recommends larger related randomized, controlled trials to provide clinicians with sufficient data to guide them in their patient care.
Graham Snyder, MD, associate professor in the division of infectious diseases at the University of Pittsburgh and medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, noted that the study “adds to a quickly growing literature on the real-world benefits of tixagevimab/cilgavimab to protect vulnerable individuals with weakened immune systems from the complications of COVID-19.
“This study provides a modest addition to our understanding of the role and benefit of Evusheld,” Dr. Snyder said in an interview. “By characterizing only patients who have received Evusheld without an untreated comparison group, we can’t draw any inference about the extent of benefit the agent provided to these patients.
“Substantial data already show that this agent is effective in preventing complications of COVID-19 infection in immunocompromised individuals,” added Dr. Snyder, who was not involved in the study.
“ ‘Immunocompromised’ represents a very diverse set of clinical conditions,” he said. “The research agenda should therefore focus on a more refined description of the effect in specific populations and a continued understanding of the effect of Evusheld in the context of updated vaccination strategies and changing virus ecology.”
Dr. Calabrese and her colleagues wrote that larger, controlled trials are underway.
FDA: Evusheld may not neutralize certain SARS-CoV-2 variants
“The biggest unanswered question is how Evusheld will hold up against new variants,” Dr. Calabrese said.
In an Oct. 3, 2022, update, the Food and Drug Administration released a statement about the risk of developing COVID-19 from SARS-CoV-2 variants that are not neutralized by Evusheld. The statement mentions an updated fact sheet that describes reduced protection from Evusheld against the Omicron subvariant BA.4.6, which accounted for nearly 13% of all new COVID-19 cases in the United States in the week ending Oct. 1.
There was no outside funding for the study. Dr. Smith reported no relevant financial conflicts of interest. Dr. Snyder said he is an unpaid adviser to an AstraZeneca observational study that’s assessing the real-world effectiveness of Evusheld.
Tixagevimab copackaged with cilgavimab (Evusheld) is a safe and effective preexposure prophylaxis (PrEP) in patients undergoing B-cell-depleting therapies who have poor immune response to COVID-19 vaccination and are at high risk for serious COVID-19 illness, a small, single-site study suggests.
Evusheld, the only COVID-19 PrEP option available, has Emergency Use Authorization (EUA) from the Food and Drug Administration for treatment of immunocompromised patients who may not respond sufficiently to COVID-19 vaccination and patients who’ve had a severe adverse reaction to COVID-19 vaccination.
“We report the largest real-world experience of Evusheld in this population, and our findings are encouraging,” lead study author Cassandra Calabrese, DO, rheumatologist and infectious disease specialist at Cleveland Clinic, said in an interview.
“Of 412 patients who received Evusheld, 12 [2.9%] developed breakthrough COVID-19, with 11 having mild courses and 1 who required hospitalization but recovered,” she added.
“Our data suggest that Evusheld PrEP, in combination with aggressive outpatient treatment of COVID-19, is likely effective in lowering risk of severe COVID in this vulnerable group.
“Practitioners who care for patients with immune-mediated inflammatory diseases should triage high-risk patients for Evusheld as well as rapid diagnosis and aggressive outpatient therapy if infected,” Dr. Calabrese advised.
For the study, Dr. Calabrese and colleagues at Cleveland Clinic searched the health care system pharmacy records for patients with immune‐mediated inflammatory diseases (IMIDs) or inborn errors of humoral immunity (IEI) who met the criteria to receive Evusheld. The researchers included patients on B-cell-depleting therapies or with humoral IEI who had received at least one dose of Evusheld and were later diagnosed with COVID-19, and they excluded those treated with B-cell-depleting therapies for cancer.
EVUSHELD was well tolerated
After extracting data on COVID-19 infection, vaccination status, and outcomes, they found that, between Jan. 18 and May 28, 2022, 412 patients with IMIDs or humoral IEI received Evusheld. No deaths occurred among these patients and, overall, they tolerated the medication well.
All 12 patients who experienced breakthrough COVID-19 infection were treated with B-cell-depleting therapies. Among the 12 patients:
- Six patients developed infection 13-84 (median 19) days after receiving 150 mg/150 mg tixagevimab/cilgavimab.
- Six patients developed infection 19-72 (median of 38.5) days after either a single dose of 300 mg/300 mg or a second dose of 150 mg/150 mg.
- Eleven patients had mild illness and recovered at home; one patient was hospitalized and treated with high-flow oxygen. All cases had been vaccinated against COVID-19 (five received two vaccinations, six received three, and one received four).
- One possible serious adverse event involved a patient with COVID-19 and immune-mediated thrombocytopenia (ITP) who was hospitalized soon after receiving Evusheld with ITP flare that resolved with intravenous immunoglobulin.
Dr. Calabrese acknowledged limitations to the study, including few patients, lack of a comparator group, and the study period falling during the Omicron wave.
“Also, nine of the breakthrough cases received additional COVID-19 therapy (oral antiviral or monoclonal antibody), which falls within standard of care for this high-risk group but prevents ascribing effectiveness to individual components of the regimen,” she added.
“Evusheld is authorized for PrEP against COVID-19 in patients at high risk for severe COVID due to suboptimal vaccine responses. This includes patients receiving B-cell-depleting drugs like rituximab, and patients with inborn errors of humoral immunity,” Dr. Calabrese explained.
“It is well known that this group of patients is at very high risk for severe COVID and death, even when fully vaccinated, and it has become clear that more strategies are needed to protect this vulnerable group, including use of Evusheld as well as aggressive treatment if infected,” she added.
Evusheld not always easy to obtain
Although the medication has been available in the United States since January 2022, Dr. Calabrese said, patients may not receive it because of barriers including lack of both awareness and access.
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California San Diego, in La Jolla, said in an interview that he was not surprised by the results, but added that the study was conducted in too few patients to draw any strong conclusions or affect patient care.
“This small study that showed that breakthrough infections occurred but were generally mild, provides a small glimpse of real-world use of tixagevimab/cilgavimab as PrEP for immunocompromised persons,” said Dr. Smith, who was not involved in the study.
“In the setting of Omicron and vaccination, I would expect the same outcomes reported even without the treatment,” he added.
Dr. Smith recommends larger related randomized, controlled trials to provide clinicians with sufficient data to guide them in their patient care.
Graham Snyder, MD, associate professor in the division of infectious diseases at the University of Pittsburgh and medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, noted that the study “adds to a quickly growing literature on the real-world benefits of tixagevimab/cilgavimab to protect vulnerable individuals with weakened immune systems from the complications of COVID-19.
“This study provides a modest addition to our understanding of the role and benefit of Evusheld,” Dr. Snyder said in an interview. “By characterizing only patients who have received Evusheld without an untreated comparison group, we can’t draw any inference about the extent of benefit the agent provided to these patients.
“Substantial data already show that this agent is effective in preventing complications of COVID-19 infection in immunocompromised individuals,” added Dr. Snyder, who was not involved in the study.
“ ‘Immunocompromised’ represents a very diverse set of clinical conditions,” he said. “The research agenda should therefore focus on a more refined description of the effect in specific populations and a continued understanding of the effect of Evusheld in the context of updated vaccination strategies and changing virus ecology.”
Dr. Calabrese and her colleagues wrote that larger, controlled trials are underway.
FDA: Evusheld may not neutralize certain SARS-CoV-2 variants
“The biggest unanswered question is how Evusheld will hold up against new variants,” Dr. Calabrese said.
In an Oct. 3, 2022, update, the Food and Drug Administration released a statement about the risk of developing COVID-19 from SARS-CoV-2 variants that are not neutralized by Evusheld. The statement mentions an updated fact sheet that describes reduced protection from Evusheld against the Omicron subvariant BA.4.6, which accounted for nearly 13% of all new COVID-19 cases in the United States in the week ending Oct. 1.
There was no outside funding for the study. Dr. Smith reported no relevant financial conflicts of interest. Dr. Snyder said he is an unpaid adviser to an AstraZeneca observational study that’s assessing the real-world effectiveness of Evusheld.
Tixagevimab copackaged with cilgavimab (Evusheld) is a safe and effective preexposure prophylaxis (PrEP) in patients undergoing B-cell-depleting therapies who have poor immune response to COVID-19 vaccination and are at high risk for serious COVID-19 illness, a small, single-site study suggests.
Evusheld, the only COVID-19 PrEP option available, has Emergency Use Authorization (EUA) from the Food and Drug Administration for treatment of immunocompromised patients who may not respond sufficiently to COVID-19 vaccination and patients who’ve had a severe adverse reaction to COVID-19 vaccination.
“We report the largest real-world experience of Evusheld in this population, and our findings are encouraging,” lead study author Cassandra Calabrese, DO, rheumatologist and infectious disease specialist at Cleveland Clinic, said in an interview.
“Of 412 patients who received Evusheld, 12 [2.9%] developed breakthrough COVID-19, with 11 having mild courses and 1 who required hospitalization but recovered,” she added.
“Our data suggest that Evusheld PrEP, in combination with aggressive outpatient treatment of COVID-19, is likely effective in lowering risk of severe COVID in this vulnerable group.
“Practitioners who care for patients with immune-mediated inflammatory diseases should triage high-risk patients for Evusheld as well as rapid diagnosis and aggressive outpatient therapy if infected,” Dr. Calabrese advised.
For the study, Dr. Calabrese and colleagues at Cleveland Clinic searched the health care system pharmacy records for patients with immune‐mediated inflammatory diseases (IMIDs) or inborn errors of humoral immunity (IEI) who met the criteria to receive Evusheld. The researchers included patients on B-cell-depleting therapies or with humoral IEI who had received at least one dose of Evusheld and were later diagnosed with COVID-19, and they excluded those treated with B-cell-depleting therapies for cancer.
EVUSHELD was well tolerated
After extracting data on COVID-19 infection, vaccination status, and outcomes, they found that, between Jan. 18 and May 28, 2022, 412 patients with IMIDs or humoral IEI received Evusheld. No deaths occurred among these patients and, overall, they tolerated the medication well.
All 12 patients who experienced breakthrough COVID-19 infection were treated with B-cell-depleting therapies. Among the 12 patients:
- Six patients developed infection 13-84 (median 19) days after receiving 150 mg/150 mg tixagevimab/cilgavimab.
- Six patients developed infection 19-72 (median of 38.5) days after either a single dose of 300 mg/300 mg or a second dose of 150 mg/150 mg.
- Eleven patients had mild illness and recovered at home; one patient was hospitalized and treated with high-flow oxygen. All cases had been vaccinated against COVID-19 (five received two vaccinations, six received three, and one received four).
- One possible serious adverse event involved a patient with COVID-19 and immune-mediated thrombocytopenia (ITP) who was hospitalized soon after receiving Evusheld with ITP flare that resolved with intravenous immunoglobulin.
Dr. Calabrese acknowledged limitations to the study, including few patients, lack of a comparator group, and the study period falling during the Omicron wave.
“Also, nine of the breakthrough cases received additional COVID-19 therapy (oral antiviral or monoclonal antibody), which falls within standard of care for this high-risk group but prevents ascribing effectiveness to individual components of the regimen,” she added.
“Evusheld is authorized for PrEP against COVID-19 in patients at high risk for severe COVID due to suboptimal vaccine responses. This includes patients receiving B-cell-depleting drugs like rituximab, and patients with inborn errors of humoral immunity,” Dr. Calabrese explained.
“It is well known that this group of patients is at very high risk for severe COVID and death, even when fully vaccinated, and it has become clear that more strategies are needed to protect this vulnerable group, including use of Evusheld as well as aggressive treatment if infected,” she added.
Evusheld not always easy to obtain
Although the medication has been available in the United States since January 2022, Dr. Calabrese said, patients may not receive it because of barriers including lack of both awareness and access.
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California San Diego, in La Jolla, said in an interview that he was not surprised by the results, but added that the study was conducted in too few patients to draw any strong conclusions or affect patient care.
“This small study that showed that breakthrough infections occurred but were generally mild, provides a small glimpse of real-world use of tixagevimab/cilgavimab as PrEP for immunocompromised persons,” said Dr. Smith, who was not involved in the study.
“In the setting of Omicron and vaccination, I would expect the same outcomes reported even without the treatment,” he added.
Dr. Smith recommends larger related randomized, controlled trials to provide clinicians with sufficient data to guide them in their patient care.
Graham Snyder, MD, associate professor in the division of infectious diseases at the University of Pittsburgh and medical director of infection prevention and hospital epidemiology at the University of Pittsburgh Medical Center, noted that the study “adds to a quickly growing literature on the real-world benefits of tixagevimab/cilgavimab to protect vulnerable individuals with weakened immune systems from the complications of COVID-19.
“This study provides a modest addition to our understanding of the role and benefit of Evusheld,” Dr. Snyder said in an interview. “By characterizing only patients who have received Evusheld without an untreated comparison group, we can’t draw any inference about the extent of benefit the agent provided to these patients.
“Substantial data already show that this agent is effective in preventing complications of COVID-19 infection in immunocompromised individuals,” added Dr. Snyder, who was not involved in the study.
“ ‘Immunocompromised’ represents a very diverse set of clinical conditions,” he said. “The research agenda should therefore focus on a more refined description of the effect in specific populations and a continued understanding of the effect of Evusheld in the context of updated vaccination strategies and changing virus ecology.”
Dr. Calabrese and her colleagues wrote that larger, controlled trials are underway.
FDA: Evusheld may not neutralize certain SARS-CoV-2 variants
“The biggest unanswered question is how Evusheld will hold up against new variants,” Dr. Calabrese said.
In an Oct. 3, 2022, update, the Food and Drug Administration released a statement about the risk of developing COVID-19 from SARS-CoV-2 variants that are not neutralized by Evusheld. The statement mentions an updated fact sheet that describes reduced protection from Evusheld against the Omicron subvariant BA.4.6, which accounted for nearly 13% of all new COVID-19 cases in the United States in the week ending Oct. 1.
There was no outside funding for the study. Dr. Smith reported no relevant financial conflicts of interest. Dr. Snyder said he is an unpaid adviser to an AstraZeneca observational study that’s assessing the real-world effectiveness of Evusheld.
FROM RMD OPEN
Noninvasive combination procedure effective for upper arm fat reduction, muscle toning
DENVER – , according to results from a study that analyzed results with MRI and other measures at two dermatology practices.
Simultaneous use of HIFEM and RF has been shown to be safe and effective “for fat reduction and muscle toning in various body parts,” lead study author Carolyn Jacob, MD, founder and director of Chicago Cosmetic Surgery and Dermatology, wrote in an abstract presented at the annual meeting of the American Society for Dermatologic Surgery. This study investigated the effect of the HIFEM and RF procedure on muscle toning and adipose tissue in the upper arms.
In what Dr. Jacob described as the first study of its kind because magnetic resonance imaging (MRI) was used to evaluate results, she and her coauthors enrolled 34 patients aged 23-72 years at two centers who had a BMI in the range of 18.5-33.9 kg/m2. The patients underwent four 30-minute bilateral procedures over the upper arms spaced 1 week apart with the Emsculpt NEO (BTL Aesthetics), which simultaneously delivers HIFEM and RF therapy.
NEO small sized applicators were used, which at the time of the study were under investigation but have since been cleared for use with the device. According to the manufacturer’s website, Emsculpt NEO is indicated for noninvasive lipolysis of the abdomen and thighs and reduction in the circumference of the abdomen and thighs in patients with skin types I-VI; and for noninvasive lipolysis of the upper arms “limited to skin types II and III and BMI 30 or under.”
The investigators measured changes in fat and triceps muscle tissue via MRI at baseline, 1-month, and 3-month follow-up visits. They also obtained digital photographs, administered patient questionnaires regarding comfort and satisfaction, and monitored safety of the treatments.
Of the 28 patients who completed their 1-month follow-up visit, analysis of MRI images showed a 22.3% average decrease in fat tissue from baseline MRIs (a decrease of 4.0 ± 1.2 mm; P < .01) and a 21.5% average increase in muscle mass (an increase of 8.2 ± 2.3 mm; P < .001). For the 25 patients who completed their 3-month follow-up visit, analysis of MRI images showed a 25.5% average decrease in fat tissue (a decrease of 4.9 ± 1.5 mm; P < .01) and a 23.9% average increase in muscle mass (an increase of 8.9 ± 2.0 mm; P < .001).
The analysis of questionnaires revealed high patient satisfaction with the results (87.1%), high comfort during the treatment (91.2%), and a low Visual Analogue Scale (VAS) score (1.6 ± 2.0) used to evaluate pain.
“This study shows that HIFEM and RF consistently increases muscle and decreases fat,” Dr. Jacob said in an interview. “It’s the only study on the triceps showing MRI evidence of fat loss with a nonsurgical body shaping device.”
She characterized the learning curve for the Emsculpt NEO as “small, as the previous Emsculpt small applicators have a similar fit.”
Pooja Sodha, MD, director of the center for laser and cosmetic dermatology at George Washington University, Washington, who was asked to comment on the study, said that the combination of radiofrequency energy and high-intensity focused electromagnetic technology triggers heat-induced damage of adipose tissue and muscle strengthening, respectively, to improve overall appearance and tone.
“Simultaneous delivery is the key here, and the real technological superhero, allowing us to take advantage of the synergistic effects of the muscle contractions and the tissue heating,” Dr. Sodha told this news organization. “Earlier this year, we saw published data on success with abdominal contouring with similar fat reduction and muscle enhancement as reported in this study, and these results persisted at 6 months,” with some declines noted at that time, she said.
“It is very encouraging and exciting to have similar effectiveness and safety for the arms, with such high satisfaction and comfort,” she added.
Dr. Jacob disclosed that she has conducted research studies for BTL Aesthetics since 2017 and is a member of the company’s advisory board. Dr. Sodha reported having no financial disclosures.
DENVER – , according to results from a study that analyzed results with MRI and other measures at two dermatology practices.
Simultaneous use of HIFEM and RF has been shown to be safe and effective “for fat reduction and muscle toning in various body parts,” lead study author Carolyn Jacob, MD, founder and director of Chicago Cosmetic Surgery and Dermatology, wrote in an abstract presented at the annual meeting of the American Society for Dermatologic Surgery. This study investigated the effect of the HIFEM and RF procedure on muscle toning and adipose tissue in the upper arms.
In what Dr. Jacob described as the first study of its kind because magnetic resonance imaging (MRI) was used to evaluate results, she and her coauthors enrolled 34 patients aged 23-72 years at two centers who had a BMI in the range of 18.5-33.9 kg/m2. The patients underwent four 30-minute bilateral procedures over the upper arms spaced 1 week apart with the Emsculpt NEO (BTL Aesthetics), which simultaneously delivers HIFEM and RF therapy.
NEO small sized applicators were used, which at the time of the study were under investigation but have since been cleared for use with the device. According to the manufacturer’s website, Emsculpt NEO is indicated for noninvasive lipolysis of the abdomen and thighs and reduction in the circumference of the abdomen and thighs in patients with skin types I-VI; and for noninvasive lipolysis of the upper arms “limited to skin types II and III and BMI 30 or under.”
The investigators measured changes in fat and triceps muscle tissue via MRI at baseline, 1-month, and 3-month follow-up visits. They also obtained digital photographs, administered patient questionnaires regarding comfort and satisfaction, and monitored safety of the treatments.
Of the 28 patients who completed their 1-month follow-up visit, analysis of MRI images showed a 22.3% average decrease in fat tissue from baseline MRIs (a decrease of 4.0 ± 1.2 mm; P < .01) and a 21.5% average increase in muscle mass (an increase of 8.2 ± 2.3 mm; P < .001). For the 25 patients who completed their 3-month follow-up visit, analysis of MRI images showed a 25.5% average decrease in fat tissue (a decrease of 4.9 ± 1.5 mm; P < .01) and a 23.9% average increase in muscle mass (an increase of 8.9 ± 2.0 mm; P < .001).
The analysis of questionnaires revealed high patient satisfaction with the results (87.1%), high comfort during the treatment (91.2%), and a low Visual Analogue Scale (VAS) score (1.6 ± 2.0) used to evaluate pain.
“This study shows that HIFEM and RF consistently increases muscle and decreases fat,” Dr. Jacob said in an interview. “It’s the only study on the triceps showing MRI evidence of fat loss with a nonsurgical body shaping device.”
She characterized the learning curve for the Emsculpt NEO as “small, as the previous Emsculpt small applicators have a similar fit.”
Pooja Sodha, MD, director of the center for laser and cosmetic dermatology at George Washington University, Washington, who was asked to comment on the study, said that the combination of radiofrequency energy and high-intensity focused electromagnetic technology triggers heat-induced damage of adipose tissue and muscle strengthening, respectively, to improve overall appearance and tone.
“Simultaneous delivery is the key here, and the real technological superhero, allowing us to take advantage of the synergistic effects of the muscle contractions and the tissue heating,” Dr. Sodha told this news organization. “Earlier this year, we saw published data on success with abdominal contouring with similar fat reduction and muscle enhancement as reported in this study, and these results persisted at 6 months,” with some declines noted at that time, she said.
“It is very encouraging and exciting to have similar effectiveness and safety for the arms, with such high satisfaction and comfort,” she added.
Dr. Jacob disclosed that she has conducted research studies for BTL Aesthetics since 2017 and is a member of the company’s advisory board. Dr. Sodha reported having no financial disclosures.
DENVER – , according to results from a study that analyzed results with MRI and other measures at two dermatology practices.
Simultaneous use of HIFEM and RF has been shown to be safe and effective “for fat reduction and muscle toning in various body parts,” lead study author Carolyn Jacob, MD, founder and director of Chicago Cosmetic Surgery and Dermatology, wrote in an abstract presented at the annual meeting of the American Society for Dermatologic Surgery. This study investigated the effect of the HIFEM and RF procedure on muscle toning and adipose tissue in the upper arms.
In what Dr. Jacob described as the first study of its kind because magnetic resonance imaging (MRI) was used to evaluate results, she and her coauthors enrolled 34 patients aged 23-72 years at two centers who had a BMI in the range of 18.5-33.9 kg/m2. The patients underwent four 30-minute bilateral procedures over the upper arms spaced 1 week apart with the Emsculpt NEO (BTL Aesthetics), which simultaneously delivers HIFEM and RF therapy.
NEO small sized applicators were used, which at the time of the study were under investigation but have since been cleared for use with the device. According to the manufacturer’s website, Emsculpt NEO is indicated for noninvasive lipolysis of the abdomen and thighs and reduction in the circumference of the abdomen and thighs in patients with skin types I-VI; and for noninvasive lipolysis of the upper arms “limited to skin types II and III and BMI 30 or under.”
The investigators measured changes in fat and triceps muscle tissue via MRI at baseline, 1-month, and 3-month follow-up visits. They also obtained digital photographs, administered patient questionnaires regarding comfort and satisfaction, and monitored safety of the treatments.
Of the 28 patients who completed their 1-month follow-up visit, analysis of MRI images showed a 22.3% average decrease in fat tissue from baseline MRIs (a decrease of 4.0 ± 1.2 mm; P < .01) and a 21.5% average increase in muscle mass (an increase of 8.2 ± 2.3 mm; P < .001). For the 25 patients who completed their 3-month follow-up visit, analysis of MRI images showed a 25.5% average decrease in fat tissue (a decrease of 4.9 ± 1.5 mm; P < .01) and a 23.9% average increase in muscle mass (an increase of 8.9 ± 2.0 mm; P < .001).
The analysis of questionnaires revealed high patient satisfaction with the results (87.1%), high comfort during the treatment (91.2%), and a low Visual Analogue Scale (VAS) score (1.6 ± 2.0) used to evaluate pain.
“This study shows that HIFEM and RF consistently increases muscle and decreases fat,” Dr. Jacob said in an interview. “It’s the only study on the triceps showing MRI evidence of fat loss with a nonsurgical body shaping device.”
She characterized the learning curve for the Emsculpt NEO as “small, as the previous Emsculpt small applicators have a similar fit.”
Pooja Sodha, MD, director of the center for laser and cosmetic dermatology at George Washington University, Washington, who was asked to comment on the study, said that the combination of radiofrequency energy and high-intensity focused electromagnetic technology triggers heat-induced damage of adipose tissue and muscle strengthening, respectively, to improve overall appearance and tone.
“Simultaneous delivery is the key here, and the real technological superhero, allowing us to take advantage of the synergistic effects of the muscle contractions and the tissue heating,” Dr. Sodha told this news organization. “Earlier this year, we saw published data on success with abdominal contouring with similar fat reduction and muscle enhancement as reported in this study, and these results persisted at 6 months,” with some declines noted at that time, she said.
“It is very encouraging and exciting to have similar effectiveness and safety for the arms, with such high satisfaction and comfort,” she added.
Dr. Jacob disclosed that she has conducted research studies for BTL Aesthetics since 2017 and is a member of the company’s advisory board. Dr. Sodha reported having no financial disclosures.
AT ASDS 2022
‘Low and Slow’ hyperthermic treatment being evaluated for superficial and nodular BCCs
DENVER –
At the annual meeting of the American Society for Dermatologic Surgery, Christopher Zachary, MD, and colleagues described a novel, noninvasive standardized controlled hyperthermia and mapping protocol (CHAMP) designed to help clinicians with margin assessment and treatment of superficial and nodular basal cell cancers (BCCs). “There’s considerable interest on the part of the public in having CHAMP treatment for their BCCs,” Dr. Zachary, professor and chair emeritus, University of California, Irvine, told this news organization in advance of the meeting.
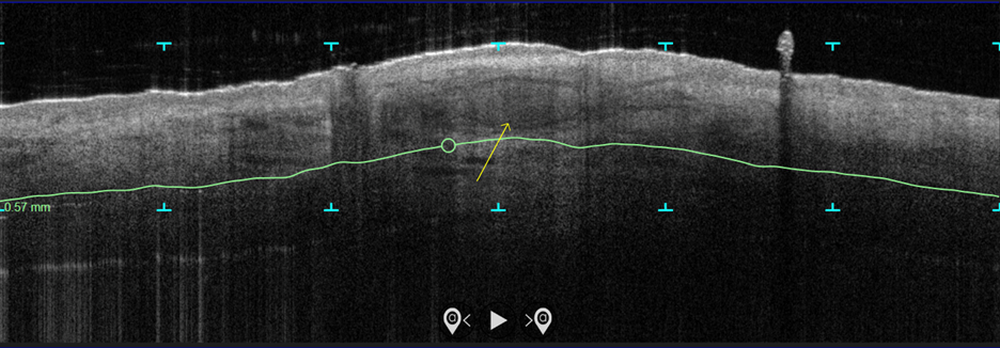
In the study, which is being conducted at three centers and plans to enroll 100 patients, more than 70 patients with biopsy-proven superficial and nodular BCCs have been scanned with the VivoSight Dx optical coherence tomography (OCT) device to map BCC tumor margins. Next, they were treated with the Sciton 1,064-nm Er:YAG laser equipped with a 4-mm beam diameter scan pattern with no overlap and an 8-millisecond pulse duration, randomized to either 120 J/cm2 pulses, until tissue graying and contraction was observed, or a novel controlled hyperthermia technique known as “Low and Slow” using repeated 25 J/cm2 pulses under thermal camera imaging to maintain a consistent temperature of 55º C for 60 seconds.
The researchers reassessed the tissue response both clinically and by OCT at 3 months and the patients were retreated with the same method if residual BCC was demonstrated. At 3-12 months post treatment, the lesion sites were saucerized and examined histologically by step sections to confirm clearance.
“In contrast to the more commonly performed ‘standard’ long-pulse 1,064-nm laser tumor coagulation, where the end point is graying and contraction of tissue, the new controlled ‘Low and Slow’ technique heats the tissue to 55º C for 60 seconds, avoids ulceration, and induces apoptotic tumor disappearance by a caspase-3 and -7 mechanism,” Dr. Zachary explained in an interview. “It’s a gentler process that allows patients an alternative to second intention wounds that occur after electrodessication and curettage or Mohs,” he added, noting that CHAMP is not intended for the treatment of more complex, large, recurrent, or infiltrative BCCs.
In both study arms, the majority of patients enrolled to date have been found to be free of tumor at 3 months by clinical and OCT examination. “The study is ongoing, but the current numbers indicate that 9 out of 10 superficial and nodular BCCs are free of tumor at 3-12 months after the last treatment,” Dr. Zachary said. The standard-treatment arm, where tissue was treated to a gray color with tissue contraction, generally resulted in more blistering and tissue necrosis with prolonged healing, compared with the Low and Slow–controlled hyperthermia arm. BCC lesions treated in the controlled hyperthermia arm had a lilac gray color with “a surprising increase” in the Doppler blood flow rate, compared with those in the standard-treatment arm, he noted.
“Blood flow following the standard technique is dramatically reduced immediately post treatment, which accounts in part for the frequent ulceration and slow healing in that group,” Dr. Zachary said.
He acknowledged certain limitations of the study, including its relatively small sample size and the fact that the optimal treatment parameters of the Low and Slow technique have yet to be realized. “It could be that we will achieve better results at 50º C for 70 seconds or similar,” he said. “While this technique will not in any way reduce the great benefits of Mohs surgery for complex BCCs, it will benefit those with simpler superficial and nodular BCCs, particularly in those who are not good surgical candidates.”
As an aside, Dr. Zachary supports the increased use of OCT scanners to improve the ability to diagnose and assess the lateral and deep margins of skin cancers. “I think that all dermatology residents should understand how to use these devices,” he said. “I’m convinced they are going to be useful in their clinical practice in the future.”
Keith L. Duffy, MD, who was asked to comment on the work, said that the study demonstrates novel ways to use existing and developing technologies in dermatology and highlights the intersection of aesthetic, surgical, and medical dermatology. “CHAMP is promising as shown by the data in the abstract and I am eager to see the final results of the study with an eye toward final cure rate and cosmesis,” said Dr. Duffy, associate professor of dermatology at the University of Utah, Salt Lake City.
“In my estimation, this technology will need to prove to be superior in one or both of these parameters in order to be considered a first- or second-line therapy,” he added. “My practice for these types of basal cell carcinomas is a simple one pass of curettage with aluminum chloride or pressure for hemostasis. The healing is fast, the cosmesis is excellent, and the cure rate is more than 90% for this simple in-office destruction. However, for those with access to this technology and proficiency with its use, CHAMP may become a viable alternative to our existing destructive methods. I look forward to seeing the published results of this multicenter trial.”
This study is being funded by Michelson Diagnostics. Sciton provided the long-pulsed 1,064-nm lasers devices being used in the trial. Neither Dr. Zachary nor Dr. Duffy reported having relevant disclosures.
DENVER –
At the annual meeting of the American Society for Dermatologic Surgery, Christopher Zachary, MD, and colleagues described a novel, noninvasive standardized controlled hyperthermia and mapping protocol (CHAMP) designed to help clinicians with margin assessment and treatment of superficial and nodular basal cell cancers (BCCs). “There’s considerable interest on the part of the public in having CHAMP treatment for their BCCs,” Dr. Zachary, professor and chair emeritus, University of California, Irvine, told this news organization in advance of the meeting.
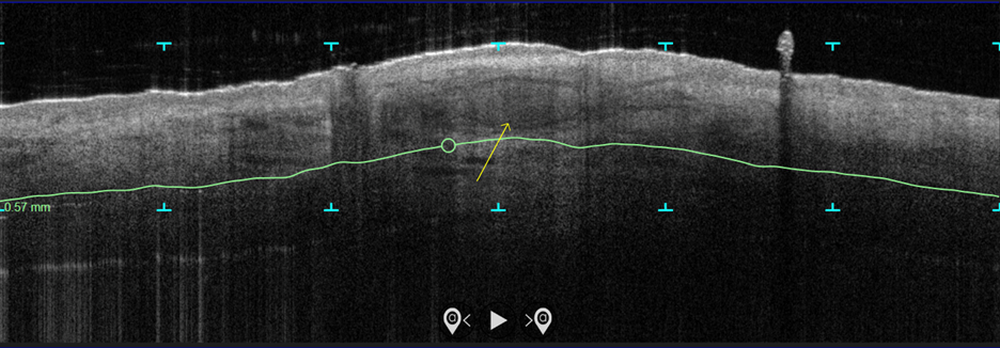
In the study, which is being conducted at three centers and plans to enroll 100 patients, more than 70 patients with biopsy-proven superficial and nodular BCCs have been scanned with the VivoSight Dx optical coherence tomography (OCT) device to map BCC tumor margins. Next, they were treated with the Sciton 1,064-nm Er:YAG laser equipped with a 4-mm beam diameter scan pattern with no overlap and an 8-millisecond pulse duration, randomized to either 120 J/cm2 pulses, until tissue graying and contraction was observed, or a novel controlled hyperthermia technique known as “Low and Slow” using repeated 25 J/cm2 pulses under thermal camera imaging to maintain a consistent temperature of 55º C for 60 seconds.
The researchers reassessed the tissue response both clinically and by OCT at 3 months and the patients were retreated with the same method if residual BCC was demonstrated. At 3-12 months post treatment, the lesion sites were saucerized and examined histologically by step sections to confirm clearance.
“In contrast to the more commonly performed ‘standard’ long-pulse 1,064-nm laser tumor coagulation, where the end point is graying and contraction of tissue, the new controlled ‘Low and Slow’ technique heats the tissue to 55º C for 60 seconds, avoids ulceration, and induces apoptotic tumor disappearance by a caspase-3 and -7 mechanism,” Dr. Zachary explained in an interview. “It’s a gentler process that allows patients an alternative to second intention wounds that occur after electrodessication and curettage or Mohs,” he added, noting that CHAMP is not intended for the treatment of more complex, large, recurrent, or infiltrative BCCs.
In both study arms, the majority of patients enrolled to date have been found to be free of tumor at 3 months by clinical and OCT examination. “The study is ongoing, but the current numbers indicate that 9 out of 10 superficial and nodular BCCs are free of tumor at 3-12 months after the last treatment,” Dr. Zachary said. The standard-treatment arm, where tissue was treated to a gray color with tissue contraction, generally resulted in more blistering and tissue necrosis with prolonged healing, compared with the Low and Slow–controlled hyperthermia arm. BCC lesions treated in the controlled hyperthermia arm had a lilac gray color with “a surprising increase” in the Doppler blood flow rate, compared with those in the standard-treatment arm, he noted.
“Blood flow following the standard technique is dramatically reduced immediately post treatment, which accounts in part for the frequent ulceration and slow healing in that group,” Dr. Zachary said.
He acknowledged certain limitations of the study, including its relatively small sample size and the fact that the optimal treatment parameters of the Low and Slow technique have yet to be realized. “It could be that we will achieve better results at 50º C for 70 seconds or similar,” he said. “While this technique will not in any way reduce the great benefits of Mohs surgery for complex BCCs, it will benefit those with simpler superficial and nodular BCCs, particularly in those who are not good surgical candidates.”
As an aside, Dr. Zachary supports the increased use of OCT scanners to improve the ability to diagnose and assess the lateral and deep margins of skin cancers. “I think that all dermatology residents should understand how to use these devices,” he said. “I’m convinced they are going to be useful in their clinical practice in the future.”
Keith L. Duffy, MD, who was asked to comment on the work, said that the study demonstrates novel ways to use existing and developing technologies in dermatology and highlights the intersection of aesthetic, surgical, and medical dermatology. “CHAMP is promising as shown by the data in the abstract and I am eager to see the final results of the study with an eye toward final cure rate and cosmesis,” said Dr. Duffy, associate professor of dermatology at the University of Utah, Salt Lake City.
“In my estimation, this technology will need to prove to be superior in one or both of these parameters in order to be considered a first- or second-line therapy,” he added. “My practice for these types of basal cell carcinomas is a simple one pass of curettage with aluminum chloride or pressure for hemostasis. The healing is fast, the cosmesis is excellent, and the cure rate is more than 90% for this simple in-office destruction. However, for those with access to this technology and proficiency with its use, CHAMP may become a viable alternative to our existing destructive methods. I look forward to seeing the published results of this multicenter trial.”
This study is being funded by Michelson Diagnostics. Sciton provided the long-pulsed 1,064-nm lasers devices being used in the trial. Neither Dr. Zachary nor Dr. Duffy reported having relevant disclosures.
DENVER –
At the annual meeting of the American Society for Dermatologic Surgery, Christopher Zachary, MD, and colleagues described a novel, noninvasive standardized controlled hyperthermia and mapping protocol (CHAMP) designed to help clinicians with margin assessment and treatment of superficial and nodular basal cell cancers (BCCs). “There’s considerable interest on the part of the public in having CHAMP treatment for their BCCs,” Dr. Zachary, professor and chair emeritus, University of California, Irvine, told this news organization in advance of the meeting.
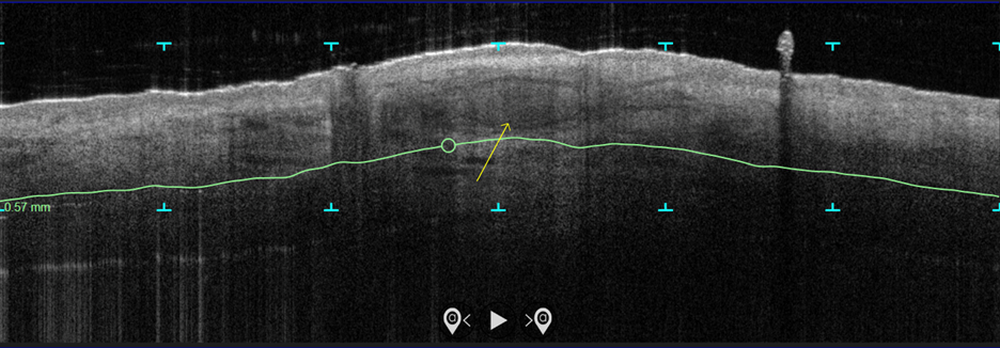
In the study, which is being conducted at three centers and plans to enroll 100 patients, more than 70 patients with biopsy-proven superficial and nodular BCCs have been scanned with the VivoSight Dx optical coherence tomography (OCT) device to map BCC tumor margins. Next, they were treated with the Sciton 1,064-nm Er:YAG laser equipped with a 4-mm beam diameter scan pattern with no overlap and an 8-millisecond pulse duration, randomized to either 120 J/cm2 pulses, until tissue graying and contraction was observed, or a novel controlled hyperthermia technique known as “Low and Slow” using repeated 25 J/cm2 pulses under thermal camera imaging to maintain a consistent temperature of 55º C for 60 seconds.
The researchers reassessed the tissue response both clinically and by OCT at 3 months and the patients were retreated with the same method if residual BCC was demonstrated. At 3-12 months post treatment, the lesion sites were saucerized and examined histologically by step sections to confirm clearance.
“In contrast to the more commonly performed ‘standard’ long-pulse 1,064-nm laser tumor coagulation, where the end point is graying and contraction of tissue, the new controlled ‘Low and Slow’ technique heats the tissue to 55º C for 60 seconds, avoids ulceration, and induces apoptotic tumor disappearance by a caspase-3 and -7 mechanism,” Dr. Zachary explained in an interview. “It’s a gentler process that allows patients an alternative to second intention wounds that occur after electrodessication and curettage or Mohs,” he added, noting that CHAMP is not intended for the treatment of more complex, large, recurrent, or infiltrative BCCs.
In both study arms, the majority of patients enrolled to date have been found to be free of tumor at 3 months by clinical and OCT examination. “The study is ongoing, but the current numbers indicate that 9 out of 10 superficial and nodular BCCs are free of tumor at 3-12 months after the last treatment,” Dr. Zachary said. The standard-treatment arm, where tissue was treated to a gray color with tissue contraction, generally resulted in more blistering and tissue necrosis with prolonged healing, compared with the Low and Slow–controlled hyperthermia arm. BCC lesions treated in the controlled hyperthermia arm had a lilac gray color with “a surprising increase” in the Doppler blood flow rate, compared with those in the standard-treatment arm, he noted.
“Blood flow following the standard technique is dramatically reduced immediately post treatment, which accounts in part for the frequent ulceration and slow healing in that group,” Dr. Zachary said.
He acknowledged certain limitations of the study, including its relatively small sample size and the fact that the optimal treatment parameters of the Low and Slow technique have yet to be realized. “It could be that we will achieve better results at 50º C for 70 seconds or similar,” he said. “While this technique will not in any way reduce the great benefits of Mohs surgery for complex BCCs, it will benefit those with simpler superficial and nodular BCCs, particularly in those who are not good surgical candidates.”
As an aside, Dr. Zachary supports the increased use of OCT scanners to improve the ability to diagnose and assess the lateral and deep margins of skin cancers. “I think that all dermatology residents should understand how to use these devices,” he said. “I’m convinced they are going to be useful in their clinical practice in the future.”
Keith L. Duffy, MD, who was asked to comment on the work, said that the study demonstrates novel ways to use existing and developing technologies in dermatology and highlights the intersection of aesthetic, surgical, and medical dermatology. “CHAMP is promising as shown by the data in the abstract and I am eager to see the final results of the study with an eye toward final cure rate and cosmesis,” said Dr. Duffy, associate professor of dermatology at the University of Utah, Salt Lake City.
“In my estimation, this technology will need to prove to be superior in one or both of these parameters in order to be considered a first- or second-line therapy,” he added. “My practice for these types of basal cell carcinomas is a simple one pass of curettage with aluminum chloride or pressure for hemostasis. The healing is fast, the cosmesis is excellent, and the cure rate is more than 90% for this simple in-office destruction. However, for those with access to this technology and proficiency with its use, CHAMP may become a viable alternative to our existing destructive methods. I look forward to seeing the published results of this multicenter trial.”
This study is being funded by Michelson Diagnostics. Sciton provided the long-pulsed 1,064-nm lasers devices being used in the trial. Neither Dr. Zachary nor Dr. Duffy reported having relevant disclosures.
AT ASDS 2022