User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
COVID-19 cases highlight longstanding racial disparities in health care
African Americans are overrepresented among patients who have died as a result of the COVID-19 pandemic, but the current crisis puts a spotlight on long-standing racial disparities in health care and health access in the United States, according to David R. Williams, PhD, a professor of public health at the Harvard T.H. Chan School of Public Health in Boston.
Dr. Williams, a social scientist specializing in the link between race and health, is a professor of African and African American Studies and of Sociology at Harvard. He spoke on the topic of racial disparities amid the COVID-19 pandemic in a teleconference sponsored by the Robert Wood Johnson Foundation.
“Many Americans are shocked” by the higher mortality rates among African American COVID-19 patients, said Dr. Williams. However, data from decades of research show that “black people in America live sicker and shorter lives,” he said.
Keys to the increased mortality among African Americans include an increased prevalence of risk factors, increased risk for exposure to the virus because of socioeconomic factors, and less access to health care if they do become ill, he said.
Many minority individuals work outside the home in areas deemed essential during the pandemic, such as transit, delivery, maintenance, cleaning, and in businesses such as grocery stores, although in general “race continues to matter for health at every level of income and education,” Dr. Williams said.
In addition, social distance guidelines are not realistic for many people in high-density, low-income areas, who often live in shared, multigenerational housing, he said.
Data show that individuals with chronic conditions such as diabetes and cardiovascular disease are more likely to die as a result of COVID-19, and minority populations are more likely to develop these conditions at younger ages, Dr. Williams noted. Access to health care also plays a role. Many minority individuals of lower socioeconomic status are less likely to have health insurance, or if they do, may have Medicaid, which is not consistently accepted, he said. Also, some low-income neighborhoods lack convenient access to primary care and thus to screening services, he noted.
Dr. Williams said the COVID-19 pandemic could serve as an opportunity to examine and improve health care services for underserved communities. In the short term, “we need to collect data so we can see patterns” and address pressing needs, he said, but long-term goals should “prioritize investments that would create healthy homes and communities,” he emphasized.
A recent study from the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report cited COVID-NET (the COVID-19 Associated Hospitalization Surveillance Network) as showing that, in their catchment population, “approximately 59% of residents are white, 18% are black, and 14% are Hispanic; however, among 580 hospitalized COVID-19 patients with race/ethnicity data, approximately 45% were white, 33% were black, and 8% were Hispanic, suggesting that black populations might be disproportionately affected by COVID-19,” the researchers said.
“These findings, including the potential impact of both sex and race on COVID-19–associated hospitalization rates, need to be confirmed with additional data,” according to the report.
Collecting racial/ethnic information is not always feasible on the front lines, and many areas still face shortages of ventilators and protective equipment, said Dr. Williams.
“I want to salute the providers on the front lines of this pandemic, many putting their own lives at risk, I want to acknowledge the good that they are doing,” Dr. Williams emphasized. He noted that all of us, himself included, may have conscious or unconscious stereotypes, but the key is to acknowledge the potential for these thoughts and feelings and continue to provide the best care.
Clyde W. Yancy, MD, of Northwestern University in Chicago, expressed similar concerns about disparity in COVID-19 cases in an editorial published on April 15 in JAMA.
“Researchers have emphasized older age, male sex, hypertension, diabetes, obesity, concomitant cardiovascular diseases (including coronary artery disease and heart failure), and myocardial injury as important risk factors associated with worse outcomes,” wrote Dr. Yancy. However, evidence also suggests that “persons who are African American or black are contracting SARS-CoV-2 at higher rates and are more likely to die,” he said.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
“Even though these data are preliminary and further study is warranted, the pattern is irrefutable: Underrepresented minorities are developing COVID-19 infection more frequently and dying disproportionately,” said Dr. Yancy.
Dr. Williams’ and Dr. Yancy’s comments were supported by an analysis of COVID-19 patient data from several areas of the country conducted by the Washington Post. In that analysis, data showed that several counties with a majority black population showed three times the rate of COVID-19 infections and approximately six times as many deaths compared with counties with a majority of white residents.
“The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event,” said Dr. Yancy. “Certainly, within the broad and powerful economic and legislative engines of the US, there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain,” he said.
Dr. Williams had no financial conflicts to disclose. Dr. Yancy had no financial conflicts to disclose.
SOURCES: Yancy CW. JAMA 2020 Apr 15. doi: 10.1001/jama.2020.6548Garg S et al. MMWR Morb Mortal Wkly Rep 2020 Apr 8;69:458-64.
Thebault R et al. The coronavirus is infecting and killing black Americans at an alarmingly high rate. Washington Post. 2020 Apr 7.
African Americans are overrepresented among patients who have died as a result of the COVID-19 pandemic, but the current crisis puts a spotlight on long-standing racial disparities in health care and health access in the United States, according to David R. Williams, PhD, a professor of public health at the Harvard T.H. Chan School of Public Health in Boston.
Dr. Williams, a social scientist specializing in the link between race and health, is a professor of African and African American Studies and of Sociology at Harvard. He spoke on the topic of racial disparities amid the COVID-19 pandemic in a teleconference sponsored by the Robert Wood Johnson Foundation.
“Many Americans are shocked” by the higher mortality rates among African American COVID-19 patients, said Dr. Williams. However, data from decades of research show that “black people in America live sicker and shorter lives,” he said.
Keys to the increased mortality among African Americans include an increased prevalence of risk factors, increased risk for exposure to the virus because of socioeconomic factors, and less access to health care if they do become ill, he said.
Many minority individuals work outside the home in areas deemed essential during the pandemic, such as transit, delivery, maintenance, cleaning, and in businesses such as grocery stores, although in general “race continues to matter for health at every level of income and education,” Dr. Williams said.
In addition, social distance guidelines are not realistic for many people in high-density, low-income areas, who often live in shared, multigenerational housing, he said.
Data show that individuals with chronic conditions such as diabetes and cardiovascular disease are more likely to die as a result of COVID-19, and minority populations are more likely to develop these conditions at younger ages, Dr. Williams noted. Access to health care also plays a role. Many minority individuals of lower socioeconomic status are less likely to have health insurance, or if they do, may have Medicaid, which is not consistently accepted, he said. Also, some low-income neighborhoods lack convenient access to primary care and thus to screening services, he noted.
Dr. Williams said the COVID-19 pandemic could serve as an opportunity to examine and improve health care services for underserved communities. In the short term, “we need to collect data so we can see patterns” and address pressing needs, he said, but long-term goals should “prioritize investments that would create healthy homes and communities,” he emphasized.
A recent study from the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report cited COVID-NET (the COVID-19 Associated Hospitalization Surveillance Network) as showing that, in their catchment population, “approximately 59% of residents are white, 18% are black, and 14% are Hispanic; however, among 580 hospitalized COVID-19 patients with race/ethnicity data, approximately 45% were white, 33% were black, and 8% were Hispanic, suggesting that black populations might be disproportionately affected by COVID-19,” the researchers said.
“These findings, including the potential impact of both sex and race on COVID-19–associated hospitalization rates, need to be confirmed with additional data,” according to the report.
Collecting racial/ethnic information is not always feasible on the front lines, and many areas still face shortages of ventilators and protective equipment, said Dr. Williams.
“I want to salute the providers on the front lines of this pandemic, many putting their own lives at risk, I want to acknowledge the good that they are doing,” Dr. Williams emphasized. He noted that all of us, himself included, may have conscious or unconscious stereotypes, but the key is to acknowledge the potential for these thoughts and feelings and continue to provide the best care.
Clyde W. Yancy, MD, of Northwestern University in Chicago, expressed similar concerns about disparity in COVID-19 cases in an editorial published on April 15 in JAMA.
“Researchers have emphasized older age, male sex, hypertension, diabetes, obesity, concomitant cardiovascular diseases (including coronary artery disease and heart failure), and myocardial injury as important risk factors associated with worse outcomes,” wrote Dr. Yancy. However, evidence also suggests that “persons who are African American or black are contracting SARS-CoV-2 at higher rates and are more likely to die,” he said.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
“Even though these data are preliminary and further study is warranted, the pattern is irrefutable: Underrepresented minorities are developing COVID-19 infection more frequently and dying disproportionately,” said Dr. Yancy.
Dr. Williams’ and Dr. Yancy’s comments were supported by an analysis of COVID-19 patient data from several areas of the country conducted by the Washington Post. In that analysis, data showed that several counties with a majority black population showed three times the rate of COVID-19 infections and approximately six times as many deaths compared with counties with a majority of white residents.
“The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event,” said Dr. Yancy. “Certainly, within the broad and powerful economic and legislative engines of the US, there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain,” he said.
Dr. Williams had no financial conflicts to disclose. Dr. Yancy had no financial conflicts to disclose.
SOURCES: Yancy CW. JAMA 2020 Apr 15. doi: 10.1001/jama.2020.6548Garg S et al. MMWR Morb Mortal Wkly Rep 2020 Apr 8;69:458-64.
Thebault R et al. The coronavirus is infecting and killing black Americans at an alarmingly high rate. Washington Post. 2020 Apr 7.
African Americans are overrepresented among patients who have died as a result of the COVID-19 pandemic, but the current crisis puts a spotlight on long-standing racial disparities in health care and health access in the United States, according to David R. Williams, PhD, a professor of public health at the Harvard T.H. Chan School of Public Health in Boston.
Dr. Williams, a social scientist specializing in the link between race and health, is a professor of African and African American Studies and of Sociology at Harvard. He spoke on the topic of racial disparities amid the COVID-19 pandemic in a teleconference sponsored by the Robert Wood Johnson Foundation.
“Many Americans are shocked” by the higher mortality rates among African American COVID-19 patients, said Dr. Williams. However, data from decades of research show that “black people in America live sicker and shorter lives,” he said.
Keys to the increased mortality among African Americans include an increased prevalence of risk factors, increased risk for exposure to the virus because of socioeconomic factors, and less access to health care if they do become ill, he said.
Many minority individuals work outside the home in areas deemed essential during the pandemic, such as transit, delivery, maintenance, cleaning, and in businesses such as grocery stores, although in general “race continues to matter for health at every level of income and education,” Dr. Williams said.
In addition, social distance guidelines are not realistic for many people in high-density, low-income areas, who often live in shared, multigenerational housing, he said.
Data show that individuals with chronic conditions such as diabetes and cardiovascular disease are more likely to die as a result of COVID-19, and minority populations are more likely to develop these conditions at younger ages, Dr. Williams noted. Access to health care also plays a role. Many minority individuals of lower socioeconomic status are less likely to have health insurance, or if they do, may have Medicaid, which is not consistently accepted, he said. Also, some low-income neighborhoods lack convenient access to primary care and thus to screening services, he noted.
Dr. Williams said the COVID-19 pandemic could serve as an opportunity to examine and improve health care services for underserved communities. In the short term, “we need to collect data so we can see patterns” and address pressing needs, he said, but long-term goals should “prioritize investments that would create healthy homes and communities,” he emphasized.
A recent study from the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report cited COVID-NET (the COVID-19 Associated Hospitalization Surveillance Network) as showing that, in their catchment population, “approximately 59% of residents are white, 18% are black, and 14% are Hispanic; however, among 580 hospitalized COVID-19 patients with race/ethnicity data, approximately 45% were white, 33% were black, and 8% were Hispanic, suggesting that black populations might be disproportionately affected by COVID-19,” the researchers said.
“These findings, including the potential impact of both sex and race on COVID-19–associated hospitalization rates, need to be confirmed with additional data,” according to the report.
Collecting racial/ethnic information is not always feasible on the front lines, and many areas still face shortages of ventilators and protective equipment, said Dr. Williams.
“I want to salute the providers on the front lines of this pandemic, many putting their own lives at risk, I want to acknowledge the good that they are doing,” Dr. Williams emphasized. He noted that all of us, himself included, may have conscious or unconscious stereotypes, but the key is to acknowledge the potential for these thoughts and feelings and continue to provide the best care.
Clyde W. Yancy, MD, of Northwestern University in Chicago, expressed similar concerns about disparity in COVID-19 cases in an editorial published on April 15 in JAMA.
“Researchers have emphasized older age, male sex, hypertension, diabetes, obesity, concomitant cardiovascular diseases (including coronary artery disease and heart failure), and myocardial injury as important risk factors associated with worse outcomes,” wrote Dr. Yancy. However, evidence also suggests that “persons who are African American or black are contracting SARS-CoV-2 at higher rates and are more likely to die,” he said.
“Why is this uniquely important to me? I am an academic cardiologist; I study health care disparities; and I am a black man,” he wrote.
“Even though these data are preliminary and further study is warranted, the pattern is irrefutable: Underrepresented minorities are developing COVID-19 infection more frequently and dying disproportionately,” said Dr. Yancy.
Dr. Williams’ and Dr. Yancy’s comments were supported by an analysis of COVID-19 patient data from several areas of the country conducted by the Washington Post. In that analysis, data showed that several counties with a majority black population showed three times the rate of COVID-19 infections and approximately six times as many deaths compared with counties with a majority of white residents.
“The U.S. has needed a trigger to fully address health care disparities; COVID-19 may be that bellwether event,” said Dr. Yancy. “Certainly, within the broad and powerful economic and legislative engines of the US, there is room to definitively address a scourge even worse than COVID-19: health care disparities. It only takes will. It is time to end the refrain,” he said.
Dr. Williams had no financial conflicts to disclose. Dr. Yancy had no financial conflicts to disclose.
SOURCES: Yancy CW. JAMA 2020 Apr 15. doi: 10.1001/jama.2020.6548Garg S et al. MMWR Morb Mortal Wkly Rep 2020 Apr 8;69:458-64.
Thebault R et al. The coronavirus is infecting and killing black Americans at an alarmingly high rate. Washington Post. 2020 Apr 7.
FROM A TELECONFERENCE SPONSORED BY THE ROBERT WOOD JOHNSON FOUNDATION
Call for volunteers for palliative care in COVID-19
While working in health care has never been easy, the COVID-19 pandemic has brought on an entirely new dimension to the challenges that clinicians face. Many of the daily concerns we once had now pale in comparison with the weight of this historic pandemic. Anxiety about the survival of our patients is compounded by our own physical and emotional exhaustion, concern for our loved ones, and fear for our own safety while on the front lines. Through this seemingly insurmountable array of challenges, survival mode kicks in. We come into the hospital every day, put on our mask and gowns, and focus on providing the care we’ve been trained for. That’s what we do best – keeping on.
However, the sheer volume of patients grows by the day, including those who are critically ill and ventilated. With hundreds of deaths every day in New York City, and ICUs filled beyond three times capacity, our frontline clinicians are overstretched, exhausted, and in need of additional help. Emergency codes are called overhead at staggering frequencies. Our colleagues on the front lines are unfortunately becoming sick themselves, and those who are healthy are working extra shifts, at a pace they can only keep up for so long.
The heartbreaking reality of this pandemic is that our connection with our patients and families is fading amid the chaos. Many infection prevention policies prohibit families from physically visiting the hospitals. The scariest parts of a hospitalization – gasping for air, before intubation, and the final moments before death – are tragically occurring alone. The support we are able to give occurs behind masks and fogged goggles. There’s not a clinician I know who doesn’t want better for patients and families – and we can mobilize to do so.
At NYC Health + Hospitals, the largest public health system in the United States, and a hot zone of the COVID-19 pandemic, we’ve taken major steps to mitigate this tragedy. Our palliative care clinicians have stepped up to help reconnect the patients with their families. We secured hundreds of tablets to enable video calls, and improved inpatient work flows to facilitate updates to families. We bolstered support from our palliative care clinicians to our ICU teams and are expanding capacity to initiate goals of care conversations earlier, through automatic triggers and proactive discussions with our hospitalist teams. Last but certainly not least, we are calling out across the country for our willing colleagues who can volunteer their time remotely via telehealth to support our patients, families, and staff here in NYC Health + Hospitals.
We have been encouraged by the resolve and commitment of our friends and colleagues from all corners of the country. NYC Health + Hospitals is receiving many brave volunteers who are rising to the call and assisting in whatever way they can. If you are proficient in goals-of-care conversations and/or trained in palliative care and willing, please sign up here to volunteer remotely via telemedicine. We are still in the beginning of this war; this struggle will continue for months even after public eye has turned away. Our patients and frontline staff need your help.
Thank you and stay safe.
Dr. Cho is chief value officer at NYC Health + Hospitals, and clinical associate professor of medicine at New York University. He is a member of the Hospitalist’s editorial advisory board. Ms. Israilov is the inaugural Quality and Safety Student Scholar at NYC Health + Hospitals. She is an MD candidate at the Icahn School of Medicine at Mount Sinai, New York.
While working in health care has never been easy, the COVID-19 pandemic has brought on an entirely new dimension to the challenges that clinicians face. Many of the daily concerns we once had now pale in comparison with the weight of this historic pandemic. Anxiety about the survival of our patients is compounded by our own physical and emotional exhaustion, concern for our loved ones, and fear for our own safety while on the front lines. Through this seemingly insurmountable array of challenges, survival mode kicks in. We come into the hospital every day, put on our mask and gowns, and focus on providing the care we’ve been trained for. That’s what we do best – keeping on.
However, the sheer volume of patients grows by the day, including those who are critically ill and ventilated. With hundreds of deaths every day in New York City, and ICUs filled beyond three times capacity, our frontline clinicians are overstretched, exhausted, and in need of additional help. Emergency codes are called overhead at staggering frequencies. Our colleagues on the front lines are unfortunately becoming sick themselves, and those who are healthy are working extra shifts, at a pace they can only keep up for so long.
The heartbreaking reality of this pandemic is that our connection with our patients and families is fading amid the chaos. Many infection prevention policies prohibit families from physically visiting the hospitals. The scariest parts of a hospitalization – gasping for air, before intubation, and the final moments before death – are tragically occurring alone. The support we are able to give occurs behind masks and fogged goggles. There’s not a clinician I know who doesn’t want better for patients and families – and we can mobilize to do so.
At NYC Health + Hospitals, the largest public health system in the United States, and a hot zone of the COVID-19 pandemic, we’ve taken major steps to mitigate this tragedy. Our palliative care clinicians have stepped up to help reconnect the patients with their families. We secured hundreds of tablets to enable video calls, and improved inpatient work flows to facilitate updates to families. We bolstered support from our palliative care clinicians to our ICU teams and are expanding capacity to initiate goals of care conversations earlier, through automatic triggers and proactive discussions with our hospitalist teams. Last but certainly not least, we are calling out across the country for our willing colleagues who can volunteer their time remotely via telehealth to support our patients, families, and staff here in NYC Health + Hospitals.
We have been encouraged by the resolve and commitment of our friends and colleagues from all corners of the country. NYC Health + Hospitals is receiving many brave volunteers who are rising to the call and assisting in whatever way they can. If you are proficient in goals-of-care conversations and/or trained in palliative care and willing, please sign up here to volunteer remotely via telemedicine. We are still in the beginning of this war; this struggle will continue for months even after public eye has turned away. Our patients and frontline staff need your help.
Thank you and stay safe.
Dr. Cho is chief value officer at NYC Health + Hospitals, and clinical associate professor of medicine at New York University. He is a member of the Hospitalist’s editorial advisory board. Ms. Israilov is the inaugural Quality and Safety Student Scholar at NYC Health + Hospitals. She is an MD candidate at the Icahn School of Medicine at Mount Sinai, New York.
While working in health care has never been easy, the COVID-19 pandemic has brought on an entirely new dimension to the challenges that clinicians face. Many of the daily concerns we once had now pale in comparison with the weight of this historic pandemic. Anxiety about the survival of our patients is compounded by our own physical and emotional exhaustion, concern for our loved ones, and fear for our own safety while on the front lines. Through this seemingly insurmountable array of challenges, survival mode kicks in. We come into the hospital every day, put on our mask and gowns, and focus on providing the care we’ve been trained for. That’s what we do best – keeping on.
However, the sheer volume of patients grows by the day, including those who are critically ill and ventilated. With hundreds of deaths every day in New York City, and ICUs filled beyond three times capacity, our frontline clinicians are overstretched, exhausted, and in need of additional help. Emergency codes are called overhead at staggering frequencies. Our colleagues on the front lines are unfortunately becoming sick themselves, and those who are healthy are working extra shifts, at a pace they can only keep up for so long.
The heartbreaking reality of this pandemic is that our connection with our patients and families is fading amid the chaos. Many infection prevention policies prohibit families from physically visiting the hospitals. The scariest parts of a hospitalization – gasping for air, before intubation, and the final moments before death – are tragically occurring alone. The support we are able to give occurs behind masks and fogged goggles. There’s not a clinician I know who doesn’t want better for patients and families – and we can mobilize to do so.
At NYC Health + Hospitals, the largest public health system in the United States, and a hot zone of the COVID-19 pandemic, we’ve taken major steps to mitigate this tragedy. Our palliative care clinicians have stepped up to help reconnect the patients with their families. We secured hundreds of tablets to enable video calls, and improved inpatient work flows to facilitate updates to families. We bolstered support from our palliative care clinicians to our ICU teams and are expanding capacity to initiate goals of care conversations earlier, through automatic triggers and proactive discussions with our hospitalist teams. Last but certainly not least, we are calling out across the country for our willing colleagues who can volunteer their time remotely via telehealth to support our patients, families, and staff here in NYC Health + Hospitals.
We have been encouraged by the resolve and commitment of our friends and colleagues from all corners of the country. NYC Health + Hospitals is receiving many brave volunteers who are rising to the call and assisting in whatever way they can. If you are proficient in goals-of-care conversations and/or trained in palliative care and willing, please sign up here to volunteer remotely via telemedicine. We are still in the beginning of this war; this struggle will continue for months even after public eye has turned away. Our patients and frontline staff need your help.
Thank you and stay safe.
Dr. Cho is chief value officer at NYC Health + Hospitals, and clinical associate professor of medicine at New York University. He is a member of the Hospitalist’s editorial advisory board. Ms. Israilov is the inaugural Quality and Safety Student Scholar at NYC Health + Hospitals. She is an MD candidate at the Icahn School of Medicine at Mount Sinai, New York.
Balancing ethics with empathy
My patients and their families have never been more anxious. In the pediatric ED where I practice, everyone is on edge. The COVID-19 pandemic has amplified the feelings of anxious anticipation and uncertainty that families have when they bring their child to the ED. People are scared that their children have the virus or that they will contract it in this high-risk environment. Both are reasonable fears. As a doctor, it has never been more difficult for me to lessen that anxiety.
Every doctor has a version of an interpersonal toolkit they use to project confidence, maintain calm, and convey empathy. Parts of it are taught in medical school, but most components are learned by trial and error. For me, it starts with speaking clearly and directly. If I can do this successfully, it allows parents to understand my recommendations and feel comfortable with my expertise. But words alone are rarely enough to gain trust. For most people, trusting a doctor requires believing that the physician is empathetic and invested in their care or the care of their loved one.
My experience is that, in the short, high-intensity interactions of the ED, this often has to be achieved with body language and facial expressions. We use so many little movements in interactions with patients: a knowing smile, kind eyes, a timely frown, open arms. These gestures would typically show parents I understand how they feel, and I am invested in the health of their child. Hidden behind my mask, face shield, gown, and gloves, I remain a black box. I dispense advice but struggle to convey that it comes from someone who cares.
At the beginning of the pandemic, I would skirt the rules of personal protective equipment (PPE) usage to try and get a moment of human connection. I might appear in the doorway of a patient’s room, smile, and introduce myself before putting on my mask and goggles. If a parent seemed to expect a firm handshake, I would give one, careful to wash my hands before and after. As the guidelines around PPE usage have become more consistent and the danger of the virus increasingly evident, I have cut out these little indulgences. I wear a mask and eye protection from the moment I enter the ED until I leave. I touch as few patients as possible and generally stand 6 feet or more from everyone I talk to.
I believe most providers would agree; these precautions are the only ethical way to see patients during the pandemic. Patients and families are entitled to health care workers who are doing everything they can to protect themselves and those around them. As long as the pandemic lasts, patients and providers will need to recalibrate their expectations of interpersonal interactions. For the time being, good doctors might be defined as much by their PPE adherence as by their ability to connect with patients.
Dr. Shapiro is a clinical instructor of pediatrics at the George Washington University and a clinical associate in the division of emergency medicine at Children’s National Hospital, both in Washington. He said he had no relevant financial disclosures. Email Dr. Shapiro at [email protected].
My patients and their families have never been more anxious. In the pediatric ED where I practice, everyone is on edge. The COVID-19 pandemic has amplified the feelings of anxious anticipation and uncertainty that families have when they bring their child to the ED. People are scared that their children have the virus or that they will contract it in this high-risk environment. Both are reasonable fears. As a doctor, it has never been more difficult for me to lessen that anxiety.
Every doctor has a version of an interpersonal toolkit they use to project confidence, maintain calm, and convey empathy. Parts of it are taught in medical school, but most components are learned by trial and error. For me, it starts with speaking clearly and directly. If I can do this successfully, it allows parents to understand my recommendations and feel comfortable with my expertise. But words alone are rarely enough to gain trust. For most people, trusting a doctor requires believing that the physician is empathetic and invested in their care or the care of their loved one.
My experience is that, in the short, high-intensity interactions of the ED, this often has to be achieved with body language and facial expressions. We use so many little movements in interactions with patients: a knowing smile, kind eyes, a timely frown, open arms. These gestures would typically show parents I understand how they feel, and I am invested in the health of their child. Hidden behind my mask, face shield, gown, and gloves, I remain a black box. I dispense advice but struggle to convey that it comes from someone who cares.
At the beginning of the pandemic, I would skirt the rules of personal protective equipment (PPE) usage to try and get a moment of human connection. I might appear in the doorway of a patient’s room, smile, and introduce myself before putting on my mask and goggles. If a parent seemed to expect a firm handshake, I would give one, careful to wash my hands before and after. As the guidelines around PPE usage have become more consistent and the danger of the virus increasingly evident, I have cut out these little indulgences. I wear a mask and eye protection from the moment I enter the ED until I leave. I touch as few patients as possible and generally stand 6 feet or more from everyone I talk to.
I believe most providers would agree; these precautions are the only ethical way to see patients during the pandemic. Patients and families are entitled to health care workers who are doing everything they can to protect themselves and those around them. As long as the pandemic lasts, patients and providers will need to recalibrate their expectations of interpersonal interactions. For the time being, good doctors might be defined as much by their PPE adherence as by their ability to connect with patients.
Dr. Shapiro is a clinical instructor of pediatrics at the George Washington University and a clinical associate in the division of emergency medicine at Children’s National Hospital, both in Washington. He said he had no relevant financial disclosures. Email Dr. Shapiro at [email protected].
My patients and their families have never been more anxious. In the pediatric ED where I practice, everyone is on edge. The COVID-19 pandemic has amplified the feelings of anxious anticipation and uncertainty that families have when they bring their child to the ED. People are scared that their children have the virus or that they will contract it in this high-risk environment. Both are reasonable fears. As a doctor, it has never been more difficult for me to lessen that anxiety.
Every doctor has a version of an interpersonal toolkit they use to project confidence, maintain calm, and convey empathy. Parts of it are taught in medical school, but most components are learned by trial and error. For me, it starts with speaking clearly and directly. If I can do this successfully, it allows parents to understand my recommendations and feel comfortable with my expertise. But words alone are rarely enough to gain trust. For most people, trusting a doctor requires believing that the physician is empathetic and invested in their care or the care of their loved one.
My experience is that, in the short, high-intensity interactions of the ED, this often has to be achieved with body language and facial expressions. We use so many little movements in interactions with patients: a knowing smile, kind eyes, a timely frown, open arms. These gestures would typically show parents I understand how they feel, and I am invested in the health of their child. Hidden behind my mask, face shield, gown, and gloves, I remain a black box. I dispense advice but struggle to convey that it comes from someone who cares.
At the beginning of the pandemic, I would skirt the rules of personal protective equipment (PPE) usage to try and get a moment of human connection. I might appear in the doorway of a patient’s room, smile, and introduce myself before putting on my mask and goggles. If a parent seemed to expect a firm handshake, I would give one, careful to wash my hands before and after. As the guidelines around PPE usage have become more consistent and the danger of the virus increasingly evident, I have cut out these little indulgences. I wear a mask and eye protection from the moment I enter the ED until I leave. I touch as few patients as possible and generally stand 6 feet or more from everyone I talk to.
I believe most providers would agree; these precautions are the only ethical way to see patients during the pandemic. Patients and families are entitled to health care workers who are doing everything they can to protect themselves and those around them. As long as the pandemic lasts, patients and providers will need to recalibrate their expectations of interpersonal interactions. For the time being, good doctors might be defined as much by their PPE adherence as by their ability to connect with patients.
Dr. Shapiro is a clinical instructor of pediatrics at the George Washington University and a clinical associate in the division of emergency medicine at Children’s National Hospital, both in Washington. He said he had no relevant financial disclosures. Email Dr. Shapiro at [email protected].
Pandemic strains blood supply for COVID-19 and noninfected patients
The COVID-19 pandemic is putting a strain on the blood supply and could be putting people – including those who normally get transfusions, such as patients with sickle cell disease and cancer – at risk.
“Around the beginning of March, the hematology community got wind of what was going on because the blood banks were saying think about your patients and begin to restrict blood usage because we are expecting an increase in usage for COVID-positive ICU patients,” Ifeyinwa (Ify) Osunkwo, MD, a specialist in hematology and sickle cell disease at Levine Cancer Institute in Charlotte, N.C., said in an interview.
“I think that was the first call to arms around hematology ... you don’t want to shortchange somebody who is well and who is being sustained by life-giving transfusions and cut out their transfusion therapy because you are hoping to use the blood for people who are coming in with COVID-19,” she continued. “That is an ethical dilemma that no doctor wants to have to go through. But the reality is we have to do something to make it work for everybody.”
And the timing of the social restrictions due to the pandemic has added additional strain on the blood supply.
“Over the winter, traditionally, blood drives slow down because of the flu and different viruses,” she noted. “The spring and the summer are when we see the biggest recruitment and uptake of blood donation. COVID-19 hit [and] a lot of the blood drives that were traditionally scheduled to supply blood for the country have been canceled because of the new guidance for social distancing.”
Another big source of blood are health care professionals themselves and they may not be able to donate because of the extra hours being worked because of the pandemic.
In speaking about the needs for traditional patients such as those who are dealing with cancer or leukemia or sickle cell diseases as well as those who are being treated for COVID-19 in North Carolina, “we are not at the critical point, but I am a little bit nervous that we may get there because they are not going to up the usual blood drives anytime this summer. We project [sometime] in the fall, but maybe not even then. So there needs to be a significant call-out for people to make every effort to donate blood,” said Dr. Osunkwo. She added that in places such as New York City that are hot spots for the COVID-19 outbreak, the need is likely a lot greater.
She recalled a recent incident at a New York hospital that highlighted how those managing blood supplies are being restrictive and how this could be harming patients.
“A sickle cell patient came in with COVID-19 and the treatment recommendation was do a red blood cell exchange but the blood bank was nervous about getting enough blood to supply for that exchange transfusion,” she said, noting that the doctor still went to bat for that patient to get the needed treatment. “We gave her the supporting evidence that when you are on treatment for sickle cell disease, you tend to do better if you get COVID-19 or any other viral infection. The symptoms of COVID-19 in sickle cell disease is acute chest syndrome, for which the treatment is red blood cell exchange. Not doing that for [these patients] is really not giving them the optimal way of managing their disease, and managing their disease in the setting of COVID-19.”
To that end, Dr. Osunkwo stressed that doctors need to be doing all they can to get the word out that blood is needed and that the American Red Cross and other donation organizations are making it safe for people to donate. She has been using social media to highlight when her fellow doctors and others make donations as a way to motivate individuals.
“Everybody can do something during this pandemic,” she said. “Don’t feel like you are not working, that you are not a frontline worker, that you have nothing to contribute. You can donate blood. Your cousin can donate blood. You can tell your friends, your neighbors, your relatives, your enemies to go donate. We will take every kind of blood we can get because people are needing it more now. Even though we canceled elective surgeries, my patients when they get COVID-19, they need more blood ... than they usually do during their regular sickle cell admission. It is going to be the same for people who have other blood disorders like cancer and leukemia. We can’t stop life-saving treatments just because we have the COVID pandemic.”
Dr. Osunkwo also praised recent actions taken by the Food and Drug Administration to lessen some of the deferral periods for when an individual can donate.
The FDA on April 2 issued three sets of revised recommendations aimed at getting more people eligible to donate blood. All of the revised recommendations will remain in effect after the COVID-19 health emergency is declared over.
The first revised recommendation makes changes to December 2015 guidance.
For male blood donors who would have been deferred for having sex with another male partner, the deferral period has been reduced from 12 months to 3 months. That deferral period change also applies to female donors who had sex with a man who had sex with another man as well as for those with recent tattoos and piercings.
The second recommendation revises guidance from August 2013 and relates to the risk of transfusion-transmitted malaria.
Under the new recommendations, for those who traveled to malaria-endemic areas (and are residents of malaria non-endemic countries), the FDA is lowering the recommended deferral period from 12 months to 3 months, and also provides notices of an alternate procedure that permits donations without a deferral period provided the blood components are pathogen-reduced using an FDA-approved pathogen reduction device.
The third recommendation finalizes draft guidance from January that eliminates the referral period for donors who spent time in certain European countries or were on military bases in Europe and were previously considered to have been exposed to a potential risk of transmission of Creutzfeldt-Jakob Disease or Variant Creutzfeldt-Jakob Disease.
Dr. Osunkwo reports consultancy and being on the speakers bureau and participating in the advisory board for Novartis, and relationships with a variety of other pharmaceutical companies. She is the editor-in-chief for Hematology News.
The COVID-19 pandemic is putting a strain on the blood supply and could be putting people – including those who normally get transfusions, such as patients with sickle cell disease and cancer – at risk.
“Around the beginning of March, the hematology community got wind of what was going on because the blood banks were saying think about your patients and begin to restrict blood usage because we are expecting an increase in usage for COVID-positive ICU patients,” Ifeyinwa (Ify) Osunkwo, MD, a specialist in hematology and sickle cell disease at Levine Cancer Institute in Charlotte, N.C., said in an interview.
“I think that was the first call to arms around hematology ... you don’t want to shortchange somebody who is well and who is being sustained by life-giving transfusions and cut out their transfusion therapy because you are hoping to use the blood for people who are coming in with COVID-19,” she continued. “That is an ethical dilemma that no doctor wants to have to go through. But the reality is we have to do something to make it work for everybody.”
And the timing of the social restrictions due to the pandemic has added additional strain on the blood supply.
“Over the winter, traditionally, blood drives slow down because of the flu and different viruses,” she noted. “The spring and the summer are when we see the biggest recruitment and uptake of blood donation. COVID-19 hit [and] a lot of the blood drives that were traditionally scheduled to supply blood for the country have been canceled because of the new guidance for social distancing.”
Another big source of blood are health care professionals themselves and they may not be able to donate because of the extra hours being worked because of the pandemic.
In speaking about the needs for traditional patients such as those who are dealing with cancer or leukemia or sickle cell diseases as well as those who are being treated for COVID-19 in North Carolina, “we are not at the critical point, but I am a little bit nervous that we may get there because they are not going to up the usual blood drives anytime this summer. We project [sometime] in the fall, but maybe not even then. So there needs to be a significant call-out for people to make every effort to donate blood,” said Dr. Osunkwo. She added that in places such as New York City that are hot spots for the COVID-19 outbreak, the need is likely a lot greater.
She recalled a recent incident at a New York hospital that highlighted how those managing blood supplies are being restrictive and how this could be harming patients.
“A sickle cell patient came in with COVID-19 and the treatment recommendation was do a red blood cell exchange but the blood bank was nervous about getting enough blood to supply for that exchange transfusion,” she said, noting that the doctor still went to bat for that patient to get the needed treatment. “We gave her the supporting evidence that when you are on treatment for sickle cell disease, you tend to do better if you get COVID-19 or any other viral infection. The symptoms of COVID-19 in sickle cell disease is acute chest syndrome, for which the treatment is red blood cell exchange. Not doing that for [these patients] is really not giving them the optimal way of managing their disease, and managing their disease in the setting of COVID-19.”
To that end, Dr. Osunkwo stressed that doctors need to be doing all they can to get the word out that blood is needed and that the American Red Cross and other donation organizations are making it safe for people to donate. She has been using social media to highlight when her fellow doctors and others make donations as a way to motivate individuals.
“Everybody can do something during this pandemic,” she said. “Don’t feel like you are not working, that you are not a frontline worker, that you have nothing to contribute. You can donate blood. Your cousin can donate blood. You can tell your friends, your neighbors, your relatives, your enemies to go donate. We will take every kind of blood we can get because people are needing it more now. Even though we canceled elective surgeries, my patients when they get COVID-19, they need more blood ... than they usually do during their regular sickle cell admission. It is going to be the same for people who have other blood disorders like cancer and leukemia. We can’t stop life-saving treatments just because we have the COVID pandemic.”
Dr. Osunkwo also praised recent actions taken by the Food and Drug Administration to lessen some of the deferral periods for when an individual can donate.
The FDA on April 2 issued three sets of revised recommendations aimed at getting more people eligible to donate blood. All of the revised recommendations will remain in effect after the COVID-19 health emergency is declared over.
The first revised recommendation makes changes to December 2015 guidance.
For male blood donors who would have been deferred for having sex with another male partner, the deferral period has been reduced from 12 months to 3 months. That deferral period change also applies to female donors who had sex with a man who had sex with another man as well as for those with recent tattoos and piercings.
The second recommendation revises guidance from August 2013 and relates to the risk of transfusion-transmitted malaria.
Under the new recommendations, for those who traveled to malaria-endemic areas (and are residents of malaria non-endemic countries), the FDA is lowering the recommended deferral period from 12 months to 3 months, and also provides notices of an alternate procedure that permits donations without a deferral period provided the blood components are pathogen-reduced using an FDA-approved pathogen reduction device.
The third recommendation finalizes draft guidance from January that eliminates the referral period for donors who spent time in certain European countries or were on military bases in Europe and were previously considered to have been exposed to a potential risk of transmission of Creutzfeldt-Jakob Disease or Variant Creutzfeldt-Jakob Disease.
Dr. Osunkwo reports consultancy and being on the speakers bureau and participating in the advisory board for Novartis, and relationships with a variety of other pharmaceutical companies. She is the editor-in-chief for Hematology News.
The COVID-19 pandemic is putting a strain on the blood supply and could be putting people – including those who normally get transfusions, such as patients with sickle cell disease and cancer – at risk.
“Around the beginning of March, the hematology community got wind of what was going on because the blood banks were saying think about your patients and begin to restrict blood usage because we are expecting an increase in usage for COVID-positive ICU patients,” Ifeyinwa (Ify) Osunkwo, MD, a specialist in hematology and sickle cell disease at Levine Cancer Institute in Charlotte, N.C., said in an interview.
“I think that was the first call to arms around hematology ... you don’t want to shortchange somebody who is well and who is being sustained by life-giving transfusions and cut out their transfusion therapy because you are hoping to use the blood for people who are coming in with COVID-19,” she continued. “That is an ethical dilemma that no doctor wants to have to go through. But the reality is we have to do something to make it work for everybody.”
And the timing of the social restrictions due to the pandemic has added additional strain on the blood supply.
“Over the winter, traditionally, blood drives slow down because of the flu and different viruses,” she noted. “The spring and the summer are when we see the biggest recruitment and uptake of blood donation. COVID-19 hit [and] a lot of the blood drives that were traditionally scheduled to supply blood for the country have been canceled because of the new guidance for social distancing.”
Another big source of blood are health care professionals themselves and they may not be able to donate because of the extra hours being worked because of the pandemic.
In speaking about the needs for traditional patients such as those who are dealing with cancer or leukemia or sickle cell diseases as well as those who are being treated for COVID-19 in North Carolina, “we are not at the critical point, but I am a little bit nervous that we may get there because they are not going to up the usual blood drives anytime this summer. We project [sometime] in the fall, but maybe not even then. So there needs to be a significant call-out for people to make every effort to donate blood,” said Dr. Osunkwo. She added that in places such as New York City that are hot spots for the COVID-19 outbreak, the need is likely a lot greater.
She recalled a recent incident at a New York hospital that highlighted how those managing blood supplies are being restrictive and how this could be harming patients.
“A sickle cell patient came in with COVID-19 and the treatment recommendation was do a red blood cell exchange but the blood bank was nervous about getting enough blood to supply for that exchange transfusion,” she said, noting that the doctor still went to bat for that patient to get the needed treatment. “We gave her the supporting evidence that when you are on treatment for sickle cell disease, you tend to do better if you get COVID-19 or any other viral infection. The symptoms of COVID-19 in sickle cell disease is acute chest syndrome, for which the treatment is red blood cell exchange. Not doing that for [these patients] is really not giving them the optimal way of managing their disease, and managing their disease in the setting of COVID-19.”
To that end, Dr. Osunkwo stressed that doctors need to be doing all they can to get the word out that blood is needed and that the American Red Cross and other donation organizations are making it safe for people to donate. She has been using social media to highlight when her fellow doctors and others make donations as a way to motivate individuals.
“Everybody can do something during this pandemic,” she said. “Don’t feel like you are not working, that you are not a frontline worker, that you have nothing to contribute. You can donate blood. Your cousin can donate blood. You can tell your friends, your neighbors, your relatives, your enemies to go donate. We will take every kind of blood we can get because people are needing it more now. Even though we canceled elective surgeries, my patients when they get COVID-19, they need more blood ... than they usually do during their regular sickle cell admission. It is going to be the same for people who have other blood disorders like cancer and leukemia. We can’t stop life-saving treatments just because we have the COVID pandemic.”
Dr. Osunkwo also praised recent actions taken by the Food and Drug Administration to lessen some of the deferral periods for when an individual can donate.
The FDA on April 2 issued three sets of revised recommendations aimed at getting more people eligible to donate blood. All of the revised recommendations will remain in effect after the COVID-19 health emergency is declared over.
The first revised recommendation makes changes to December 2015 guidance.
For male blood donors who would have been deferred for having sex with another male partner, the deferral period has been reduced from 12 months to 3 months. That deferral period change also applies to female donors who had sex with a man who had sex with another man as well as for those with recent tattoos and piercings.
The second recommendation revises guidance from August 2013 and relates to the risk of transfusion-transmitted malaria.
Under the new recommendations, for those who traveled to malaria-endemic areas (and are residents of malaria non-endemic countries), the FDA is lowering the recommended deferral period from 12 months to 3 months, and also provides notices of an alternate procedure that permits donations without a deferral period provided the blood components are pathogen-reduced using an FDA-approved pathogen reduction device.
The third recommendation finalizes draft guidance from January that eliminates the referral period for donors who spent time in certain European countries or were on military bases in Europe and were previously considered to have been exposed to a potential risk of transmission of Creutzfeldt-Jakob Disease or Variant Creutzfeldt-Jakob Disease.
Dr. Osunkwo reports consultancy and being on the speakers bureau and participating in the advisory board for Novartis, and relationships with a variety of other pharmaceutical companies. She is the editor-in-chief for Hematology News.
“I have to watch my bank accounts closely”: a solo practitioner during COVID-19
Medicine, as often said, is a business.
That’s often forgotten in a crisis, such as COVID-19, and with good reason. Our training in medicine is needed to care for the sick and find ways to prevent disease. Things like money are in the background when it comes to the emergencies of saving lives and helping the sick.
But that doesn’t mean finances don’t matter. They’re always in the background for medical practices of all sizes – just like any business.
Some practices have closed for patient and staff safety. I haven’t gone that far, as some people still need me. I am, after all, a doctor.
So I’m alone in my office, my staff working from home. That helps cut some lines of transmission there.
Like everyone else, I’m also doing telemedicine, and even a few phone appointments. These keep all involved safe, but also have a lot of limitations. They’re fine for checking up on stable, established patients, or following up on test results. But certainly not for new patients or established ones with new problems.
After all, you can’t evaluate a foot drop, extrapyramidal rigidity, or do an EMG/NCV over the video-phone connection.
In-person appointments are spaced out to minimize the number of people in my waiting room. Patients are told not to come in if they’re sick, and I insist we both be wearing masks (of pretty much any kind at this point). Common-use pens, such as those out in the waiting room, are wiped down with alcohol between uses.
With only two staff members, there really isn’t anyone extraneous to cut. I’ve stopped taking a paycheck so I can keep paying them, my rent, and the other miscellaneous costs of running an office.
I’ve always taken a bonus only at the end of the year, after all the other accounts have been paid, and take only a modest regular salary. In this case, that’s worked to my advantage, as I had more cash on hand when the emergency started. While not a huge amount, it’s enough to buy me some time, maybe several weeks, to see how this plays out. After that I’d have to tap into a line of credit, which obviously no one wants to do.
Telemedicine and the few office patients I’m seeing are a trickle of revenue. It’s better than nothing, but certainly isn’t enough to keep the door open and lights on.
That said, I’m not ungrateful. I’m well aware how fortunate my practice and family are compared to many others during this time. I haven’t had to ask for a pass on a mortgage or rent payment – yet. My staff and I have been together since 2004. I’m not going to break up a great team now.
I have no idea when things will turn around and people will start to come in. Your guess is as good as mine. I suspect the trickle will slowly increase at some point, then suddenly there will be a surge of calls for appointments from people who’ve been putting off coming in. Even then, though, I’ll likely space appointments apart and keep using a mask until it appears things are stable. There are going to be further waves of infections, and we don’t know how bad they’ll be.
Like everyone else, I can only hope for the best.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Medicine, as often said, is a business.
That’s often forgotten in a crisis, such as COVID-19, and with good reason. Our training in medicine is needed to care for the sick and find ways to prevent disease. Things like money are in the background when it comes to the emergencies of saving lives and helping the sick.
But that doesn’t mean finances don’t matter. They’re always in the background for medical practices of all sizes – just like any business.
Some practices have closed for patient and staff safety. I haven’t gone that far, as some people still need me. I am, after all, a doctor.
So I’m alone in my office, my staff working from home. That helps cut some lines of transmission there.
Like everyone else, I’m also doing telemedicine, and even a few phone appointments. These keep all involved safe, but also have a lot of limitations. They’re fine for checking up on stable, established patients, or following up on test results. But certainly not for new patients or established ones with new problems.
After all, you can’t evaluate a foot drop, extrapyramidal rigidity, or do an EMG/NCV over the video-phone connection.
In-person appointments are spaced out to minimize the number of people in my waiting room. Patients are told not to come in if they’re sick, and I insist we both be wearing masks (of pretty much any kind at this point). Common-use pens, such as those out in the waiting room, are wiped down with alcohol between uses.
With only two staff members, there really isn’t anyone extraneous to cut. I’ve stopped taking a paycheck so I can keep paying them, my rent, and the other miscellaneous costs of running an office.
I’ve always taken a bonus only at the end of the year, after all the other accounts have been paid, and take only a modest regular salary. In this case, that’s worked to my advantage, as I had more cash on hand when the emergency started. While not a huge amount, it’s enough to buy me some time, maybe several weeks, to see how this plays out. After that I’d have to tap into a line of credit, which obviously no one wants to do.
Telemedicine and the few office patients I’m seeing are a trickle of revenue. It’s better than nothing, but certainly isn’t enough to keep the door open and lights on.
That said, I’m not ungrateful. I’m well aware how fortunate my practice and family are compared to many others during this time. I haven’t had to ask for a pass on a mortgage or rent payment – yet. My staff and I have been together since 2004. I’m not going to break up a great team now.
I have no idea when things will turn around and people will start to come in. Your guess is as good as mine. I suspect the trickle will slowly increase at some point, then suddenly there will be a surge of calls for appointments from people who’ve been putting off coming in. Even then, though, I’ll likely space appointments apart and keep using a mask until it appears things are stable. There are going to be further waves of infections, and we don’t know how bad they’ll be.
Like everyone else, I can only hope for the best.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Medicine, as often said, is a business.
That’s often forgotten in a crisis, such as COVID-19, and with good reason. Our training in medicine is needed to care for the sick and find ways to prevent disease. Things like money are in the background when it comes to the emergencies of saving lives and helping the sick.
But that doesn’t mean finances don’t matter. They’re always in the background for medical practices of all sizes – just like any business.
Some practices have closed for patient and staff safety. I haven’t gone that far, as some people still need me. I am, after all, a doctor.
So I’m alone in my office, my staff working from home. That helps cut some lines of transmission there.
Like everyone else, I’m also doing telemedicine, and even a few phone appointments. These keep all involved safe, but also have a lot of limitations. They’re fine for checking up on stable, established patients, or following up on test results. But certainly not for new patients or established ones with new problems.
After all, you can’t evaluate a foot drop, extrapyramidal rigidity, or do an EMG/NCV over the video-phone connection.
In-person appointments are spaced out to minimize the number of people in my waiting room. Patients are told not to come in if they’re sick, and I insist we both be wearing masks (of pretty much any kind at this point). Common-use pens, such as those out in the waiting room, are wiped down with alcohol between uses.
With only two staff members, there really isn’t anyone extraneous to cut. I’ve stopped taking a paycheck so I can keep paying them, my rent, and the other miscellaneous costs of running an office.
I’ve always taken a bonus only at the end of the year, after all the other accounts have been paid, and take only a modest regular salary. In this case, that’s worked to my advantage, as I had more cash on hand when the emergency started. While not a huge amount, it’s enough to buy me some time, maybe several weeks, to see how this plays out. After that I’d have to tap into a line of credit, which obviously no one wants to do.
Telemedicine and the few office patients I’m seeing are a trickle of revenue. It’s better than nothing, but certainly isn’t enough to keep the door open and lights on.
That said, I’m not ungrateful. I’m well aware how fortunate my practice and family are compared to many others during this time. I haven’t had to ask for a pass on a mortgage or rent payment – yet. My staff and I have been together since 2004. I’m not going to break up a great team now.
I have no idea when things will turn around and people will start to come in. Your guess is as good as mine. I suspect the trickle will slowly increase at some point, then suddenly there will be a surge of calls for appointments from people who’ve been putting off coming in. Even then, though, I’ll likely space appointments apart and keep using a mask until it appears things are stable. There are going to be further waves of infections, and we don’t know how bad they’ll be.
Like everyone else, I can only hope for the best.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Making something ordinary out of the extraordinary
These are tough times for families, children, and practices. In this case, the entire world is going through it at the same time, leaving no escape. There are so many new things each of us needs to do, and for some of the challenges, we are completely thwarted by safety restrictions from doing anything. Adults and children alike are trying to work or learn at home in new ways. This also means that old daily routines have been broken. The sense of disorientation is pervasive. Although it is only one part of what is needed, reestablishing routines can go a long way toward restoring a sense of control and meaning that you can institute for yourself and recommend to your patients.
Examples of such change include natural disasters such as COVID-19, deaths, or separations from loved ones, but also moving, job loss, or new financial instability. Many families and many doctors and staff are experiencing several of these at once these days.
Evidence from studies of times of major disruption such as divorce, a death, war, and natural disasters show that parenting tends to shift to being less organized, with less overall discipline or more arbitrary punishment, and, in some cases, less parent-child connection. Children, on their part, also tend to act differently under these conditions. They are more irritable, upset, anxious, clingy, and aggressive, and also tend to regress in recent developmental achievements such as maintaining toileting and sleep patterns. Parents often do not see the connection to the stress and react to these behaviors in ways that may make things worse by scolding or punishing.
I was really surprised to hear Daniel Kahneman, PhD, Nobel laureate in economics, talk about how even he has trouble judging risk based on mathematical probability. Instead, he recognizes that adults decide about risk based on the behavior of the people around them – when others act worried or agitated, the person does too. Children, even more than adults, must decide if they are safe based on the behavior of the adults around them. When parents maintain routines as closely as possible after a major disruption, children feel reassured that they can expect continuity of their relationship – their most important lifeboat. If their parents keep doing the things they are used to, children basically feel safe.
Simple aspects of sameness important to children are very familiar to pediatricians: always wanting the same spoon, the sandwich cut the same way, only chicken nuggets from a certain store. This tends to be true in typically developing toddlers, preschool, and some school-aged children. The desire to have the same story read to them multiple times – until parents are ready to scream! – is another sign of the importance of predictable routines to children. All of these are best accommodated during times of stress rather than trying to “avoid making a bad habit.” All disruptions of routine are even more disorienting for children with intellectual disabilities or those on the autism spectrum who are generally less able to understand or control their world. Children and adults with preexisting anxiety disorders also are more likely to have more severe reactions to major disruptions and need extra understanding.
Routines for eating at least something at regular times – even if the food is not as interesting as prior fare – provide a sense of security, as well as stabilizing blood sugar and bowel patterns. Keeping patterns of washing hands, sitting together as a family, and interacting in conversation, rather than watching TV news, allow an oasis of respite from ongoing stresses. Family meals are also known to promote learning, vocabulary growth, and better behavior.
Setting a schedule for schooling, play, hygiene, and exercise may seem silly when parents and children are home all day, but it instills a sense of meaning to the day. Making a visual schedule for younger children or a written or online one for older children can be a shared activity in itself. I remember hearing about how important changing clothes and cleaning teeth were to prisoners of war during World War II in maintaining a sense of normalcy in that time of chaos.
Exercise is particularly important to set as a routine as it directly reduces stress – even if it may need to take new forms. While there are lots of online exercise programs for adults, it is better for everyone to go outside if they can manage adequate personal spacing. There they can experience the orderly changing of the seasons and the weather, as well as soak up some sunshine. Interactive parent-child play serves multiple purposes of stress relief, seeing each other more relaxed, interacting, and having fun!
Routines for sleep are especially important. To fall asleep under normal circumstances requires a sense of safety, perhaps for evolutionary reasons because of the vulnerability of the paralysis that is part of REM sleep stages. Fear at bedtime is common in young children, as is disorientation in the elderly. Both respond to reassuring bedtime routines done the same way every night, such as brushing teeth, changing clothes, washing up, reading or being read to, and praying – if these were the previous habit. When there has been a major disruption, these routines take on added importance, even if some modifications need to be made in sleep location, privacy, etc. Keeping schedules for naps, bedtime, and wake time as stable as possible makes sleep onset easier and sleep maintenance more likely. It also increases the chances of adequate sleep duration. Getting enough sleep stabilizes mood, reduces irritability, and improves daytime concentration and problem-solving skills. These all are especially needed by adults as well as children when there are major disruptions.
Maintaining chores at times of disruption can be extra difficult, plus this may seem to parents like an added stress for their already-stressed child. But in fact, children are reassured by adults’ continuing these requirements. Not only is an expectation that chores be done a signal that life can be expected to proceed normally, but having children do things to help – such as cleaning up, restocking soap and towels, or emptying trash – gives them an active role and hence some sense of control.
Discipline is, in essence, also a routine. Maintaining standards for kindness to others and following rules can be especially difficult when life has been disrupted because emotional lability is more likely in both adults and children when severely stressed. It is important for parents to consider the source of the misbehavior as possibly stress related and to interrupt it in a gentle and understanding way. A parent might say: “I know you are upset by all the changes. It is even more important now than ever to be kind to your brother.” Under stressful conditions, it is especially important to ask how the child was feeling when acting up, but also to “speak for them” about possible stress-related reasons for their behavior. While parents may correctly say that their child will “take advantage of this excuse,” it is still a teaching opportunity. Children have little insight into these connections to their feelings and actions, but they can learn.
Times when old patterns are disrupted also are times for making new habits. The main new habit I recommend for stress relief and overall mental health are the practices of mindfulness or meditation. Mindfulness may be easier to teach children as it involves paying close attention to one’s thoughts, feelings, and sensations, but doing this without judgment. Children often are naturally better at this than adults, who have layered on more experiences to their thoughts. We pediatricians, as well as the parents we serve, can benefit – especially in stressful times – from sharing in the simple ways children experience the world.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
These are tough times for families, children, and practices. In this case, the entire world is going through it at the same time, leaving no escape. There are so many new things each of us needs to do, and for some of the challenges, we are completely thwarted by safety restrictions from doing anything. Adults and children alike are trying to work or learn at home in new ways. This also means that old daily routines have been broken. The sense of disorientation is pervasive. Although it is only one part of what is needed, reestablishing routines can go a long way toward restoring a sense of control and meaning that you can institute for yourself and recommend to your patients.
Examples of such change include natural disasters such as COVID-19, deaths, or separations from loved ones, but also moving, job loss, or new financial instability. Many families and many doctors and staff are experiencing several of these at once these days.
Evidence from studies of times of major disruption such as divorce, a death, war, and natural disasters show that parenting tends to shift to being less organized, with less overall discipline or more arbitrary punishment, and, in some cases, less parent-child connection. Children, on their part, also tend to act differently under these conditions. They are more irritable, upset, anxious, clingy, and aggressive, and also tend to regress in recent developmental achievements such as maintaining toileting and sleep patterns. Parents often do not see the connection to the stress and react to these behaviors in ways that may make things worse by scolding or punishing.
I was really surprised to hear Daniel Kahneman, PhD, Nobel laureate in economics, talk about how even he has trouble judging risk based on mathematical probability. Instead, he recognizes that adults decide about risk based on the behavior of the people around them – when others act worried or agitated, the person does too. Children, even more than adults, must decide if they are safe based on the behavior of the adults around them. When parents maintain routines as closely as possible after a major disruption, children feel reassured that they can expect continuity of their relationship – their most important lifeboat. If their parents keep doing the things they are used to, children basically feel safe.
Simple aspects of sameness important to children are very familiar to pediatricians: always wanting the same spoon, the sandwich cut the same way, only chicken nuggets from a certain store. This tends to be true in typically developing toddlers, preschool, and some school-aged children. The desire to have the same story read to them multiple times – until parents are ready to scream! – is another sign of the importance of predictable routines to children. All of these are best accommodated during times of stress rather than trying to “avoid making a bad habit.” All disruptions of routine are even more disorienting for children with intellectual disabilities or those on the autism spectrum who are generally less able to understand or control their world. Children and adults with preexisting anxiety disorders also are more likely to have more severe reactions to major disruptions and need extra understanding.
Routines for eating at least something at regular times – even if the food is not as interesting as prior fare – provide a sense of security, as well as stabilizing blood sugar and bowel patterns. Keeping patterns of washing hands, sitting together as a family, and interacting in conversation, rather than watching TV news, allow an oasis of respite from ongoing stresses. Family meals are also known to promote learning, vocabulary growth, and better behavior.
Setting a schedule for schooling, play, hygiene, and exercise may seem silly when parents and children are home all day, but it instills a sense of meaning to the day. Making a visual schedule for younger children or a written or online one for older children can be a shared activity in itself. I remember hearing about how important changing clothes and cleaning teeth were to prisoners of war during World War II in maintaining a sense of normalcy in that time of chaos.
Exercise is particularly important to set as a routine as it directly reduces stress – even if it may need to take new forms. While there are lots of online exercise programs for adults, it is better for everyone to go outside if they can manage adequate personal spacing. There they can experience the orderly changing of the seasons and the weather, as well as soak up some sunshine. Interactive parent-child play serves multiple purposes of stress relief, seeing each other more relaxed, interacting, and having fun!
Routines for sleep are especially important. To fall asleep under normal circumstances requires a sense of safety, perhaps for evolutionary reasons because of the vulnerability of the paralysis that is part of REM sleep stages. Fear at bedtime is common in young children, as is disorientation in the elderly. Both respond to reassuring bedtime routines done the same way every night, such as brushing teeth, changing clothes, washing up, reading or being read to, and praying – if these were the previous habit. When there has been a major disruption, these routines take on added importance, even if some modifications need to be made in sleep location, privacy, etc. Keeping schedules for naps, bedtime, and wake time as stable as possible makes sleep onset easier and sleep maintenance more likely. It also increases the chances of adequate sleep duration. Getting enough sleep stabilizes mood, reduces irritability, and improves daytime concentration and problem-solving skills. These all are especially needed by adults as well as children when there are major disruptions.
Maintaining chores at times of disruption can be extra difficult, plus this may seem to parents like an added stress for their already-stressed child. But in fact, children are reassured by adults’ continuing these requirements. Not only is an expectation that chores be done a signal that life can be expected to proceed normally, but having children do things to help – such as cleaning up, restocking soap and towels, or emptying trash – gives them an active role and hence some sense of control.
Discipline is, in essence, also a routine. Maintaining standards for kindness to others and following rules can be especially difficult when life has been disrupted because emotional lability is more likely in both adults and children when severely stressed. It is important for parents to consider the source of the misbehavior as possibly stress related and to interrupt it in a gentle and understanding way. A parent might say: “I know you are upset by all the changes. It is even more important now than ever to be kind to your brother.” Under stressful conditions, it is especially important to ask how the child was feeling when acting up, but also to “speak for them” about possible stress-related reasons for their behavior. While parents may correctly say that their child will “take advantage of this excuse,” it is still a teaching opportunity. Children have little insight into these connections to their feelings and actions, but they can learn.
Times when old patterns are disrupted also are times for making new habits. The main new habit I recommend for stress relief and overall mental health are the practices of mindfulness or meditation. Mindfulness may be easier to teach children as it involves paying close attention to one’s thoughts, feelings, and sensations, but doing this without judgment. Children often are naturally better at this than adults, who have layered on more experiences to their thoughts. We pediatricians, as well as the parents we serve, can benefit – especially in stressful times – from sharing in the simple ways children experience the world.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
These are tough times for families, children, and practices. In this case, the entire world is going through it at the same time, leaving no escape. There are so many new things each of us needs to do, and for some of the challenges, we are completely thwarted by safety restrictions from doing anything. Adults and children alike are trying to work or learn at home in new ways. This also means that old daily routines have been broken. The sense of disorientation is pervasive. Although it is only one part of what is needed, reestablishing routines can go a long way toward restoring a sense of control and meaning that you can institute for yourself and recommend to your patients.
Examples of such change include natural disasters such as COVID-19, deaths, or separations from loved ones, but also moving, job loss, or new financial instability. Many families and many doctors and staff are experiencing several of these at once these days.
Evidence from studies of times of major disruption such as divorce, a death, war, and natural disasters show that parenting tends to shift to being less organized, with less overall discipline or more arbitrary punishment, and, in some cases, less parent-child connection. Children, on their part, also tend to act differently under these conditions. They are more irritable, upset, anxious, clingy, and aggressive, and also tend to regress in recent developmental achievements such as maintaining toileting and sleep patterns. Parents often do not see the connection to the stress and react to these behaviors in ways that may make things worse by scolding or punishing.
I was really surprised to hear Daniel Kahneman, PhD, Nobel laureate in economics, talk about how even he has trouble judging risk based on mathematical probability. Instead, he recognizes that adults decide about risk based on the behavior of the people around them – when others act worried or agitated, the person does too. Children, even more than adults, must decide if they are safe based on the behavior of the adults around them. When parents maintain routines as closely as possible after a major disruption, children feel reassured that they can expect continuity of their relationship – their most important lifeboat. If their parents keep doing the things they are used to, children basically feel safe.
Simple aspects of sameness important to children are very familiar to pediatricians: always wanting the same spoon, the sandwich cut the same way, only chicken nuggets from a certain store. This tends to be true in typically developing toddlers, preschool, and some school-aged children. The desire to have the same story read to them multiple times – until parents are ready to scream! – is another sign of the importance of predictable routines to children. All of these are best accommodated during times of stress rather than trying to “avoid making a bad habit.” All disruptions of routine are even more disorienting for children with intellectual disabilities or those on the autism spectrum who are generally less able to understand or control their world. Children and adults with preexisting anxiety disorders also are more likely to have more severe reactions to major disruptions and need extra understanding.
Routines for eating at least something at regular times – even if the food is not as interesting as prior fare – provide a sense of security, as well as stabilizing blood sugar and bowel patterns. Keeping patterns of washing hands, sitting together as a family, and interacting in conversation, rather than watching TV news, allow an oasis of respite from ongoing stresses. Family meals are also known to promote learning, vocabulary growth, and better behavior.
Setting a schedule for schooling, play, hygiene, and exercise may seem silly when parents and children are home all day, but it instills a sense of meaning to the day. Making a visual schedule for younger children or a written or online one for older children can be a shared activity in itself. I remember hearing about how important changing clothes and cleaning teeth were to prisoners of war during World War II in maintaining a sense of normalcy in that time of chaos.
Exercise is particularly important to set as a routine as it directly reduces stress – even if it may need to take new forms. While there are lots of online exercise programs for adults, it is better for everyone to go outside if they can manage adequate personal spacing. There they can experience the orderly changing of the seasons and the weather, as well as soak up some sunshine. Interactive parent-child play serves multiple purposes of stress relief, seeing each other more relaxed, interacting, and having fun!
Routines for sleep are especially important. To fall asleep under normal circumstances requires a sense of safety, perhaps for evolutionary reasons because of the vulnerability of the paralysis that is part of REM sleep stages. Fear at bedtime is common in young children, as is disorientation in the elderly. Both respond to reassuring bedtime routines done the same way every night, such as brushing teeth, changing clothes, washing up, reading or being read to, and praying – if these were the previous habit. When there has been a major disruption, these routines take on added importance, even if some modifications need to be made in sleep location, privacy, etc. Keeping schedules for naps, bedtime, and wake time as stable as possible makes sleep onset easier and sleep maintenance more likely. It also increases the chances of adequate sleep duration. Getting enough sleep stabilizes mood, reduces irritability, and improves daytime concentration and problem-solving skills. These all are especially needed by adults as well as children when there are major disruptions.
Maintaining chores at times of disruption can be extra difficult, plus this may seem to parents like an added stress for their already-stressed child. But in fact, children are reassured by adults’ continuing these requirements. Not only is an expectation that chores be done a signal that life can be expected to proceed normally, but having children do things to help – such as cleaning up, restocking soap and towels, or emptying trash – gives them an active role and hence some sense of control.
Discipline is, in essence, also a routine. Maintaining standards for kindness to others and following rules can be especially difficult when life has been disrupted because emotional lability is more likely in both adults and children when severely stressed. It is important for parents to consider the source of the misbehavior as possibly stress related and to interrupt it in a gentle and understanding way. A parent might say: “I know you are upset by all the changes. It is even more important now than ever to be kind to your brother.” Under stressful conditions, it is especially important to ask how the child was feeling when acting up, but also to “speak for them” about possible stress-related reasons for their behavior. While parents may correctly say that their child will “take advantage of this excuse,” it is still a teaching opportunity. Children have little insight into these connections to their feelings and actions, but they can learn.
Times when old patterns are disrupted also are times for making new habits. The main new habit I recommend for stress relief and overall mental health are the practices of mindfulness or meditation. Mindfulness may be easier to teach children as it involves paying close attention to one’s thoughts, feelings, and sensations, but doing this without judgment. Children often are naturally better at this than adults, who have layered on more experiences to their thoughts. We pediatricians, as well as the parents we serve, can benefit – especially in stressful times – from sharing in the simple ways children experience the world.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
Severe COVID-19 may lower hemoglobin levels
A meta-analysis of four applicable studies found that the hemoglobin value was significantly lower in COVID-19 patients with severe disease, compared with those with milder forms, according to a letter to the editor of Hematology Transfusion and Cell Therapy by Giuseppe Lippi, MD, of the University of Verona (Italy) and colleague.
The four studies comprised 1,210 COVID-19 patients (224 with severe disease; 18.5%). The primary endpoint was defined as a composite of admission to the ICU, need of mechanical ventilation or death. The heterogeneity among the studies was high.
Overall, the hemoglobin value was found to be significantly lower in COVID-19 patients with severe disease than in those with milder forms, yielding a weighted mean difference of −7.1 g/L, with a 95% confidence interval of −8.3 g/L to −5.9 g/L.
“Initial assessment and longitudinal monitoring of hemoglobin values seems advisable in patients with the SARS-CoV-2 infection, whereby a progressive decrease in the hemoglobin concentration may reflect a worse clinical progression,” the authors stated. They also suggested that studies should be “urgently planned to assess whether transfusion support (e.g., with administration of blood or packed red blood cells) may be helpful in this clinical setting to prevent evolution into severe disease and death.”
The authors declared the had no conflicts of interest.
SOURCE: Lippi G et al. Hematol Transfus Cell Ther. 2020 Apr 11; doi:10.1016/j.htct.2020.03.001.
A meta-analysis of four applicable studies found that the hemoglobin value was significantly lower in COVID-19 patients with severe disease, compared with those with milder forms, according to a letter to the editor of Hematology Transfusion and Cell Therapy by Giuseppe Lippi, MD, of the University of Verona (Italy) and colleague.
The four studies comprised 1,210 COVID-19 patients (224 with severe disease; 18.5%). The primary endpoint was defined as a composite of admission to the ICU, need of mechanical ventilation or death. The heterogeneity among the studies was high.
Overall, the hemoglobin value was found to be significantly lower in COVID-19 patients with severe disease than in those with milder forms, yielding a weighted mean difference of −7.1 g/L, with a 95% confidence interval of −8.3 g/L to −5.9 g/L.
“Initial assessment and longitudinal monitoring of hemoglobin values seems advisable in patients with the SARS-CoV-2 infection, whereby a progressive decrease in the hemoglobin concentration may reflect a worse clinical progression,” the authors stated. They also suggested that studies should be “urgently planned to assess whether transfusion support (e.g., with administration of blood or packed red blood cells) may be helpful in this clinical setting to prevent evolution into severe disease and death.”
The authors declared the had no conflicts of interest.
SOURCE: Lippi G et al. Hematol Transfus Cell Ther. 2020 Apr 11; doi:10.1016/j.htct.2020.03.001.
A meta-analysis of four applicable studies found that the hemoglobin value was significantly lower in COVID-19 patients with severe disease, compared with those with milder forms, according to a letter to the editor of Hematology Transfusion and Cell Therapy by Giuseppe Lippi, MD, of the University of Verona (Italy) and colleague.
The four studies comprised 1,210 COVID-19 patients (224 with severe disease; 18.5%). The primary endpoint was defined as a composite of admission to the ICU, need of mechanical ventilation or death. The heterogeneity among the studies was high.
Overall, the hemoglobin value was found to be significantly lower in COVID-19 patients with severe disease than in those with milder forms, yielding a weighted mean difference of −7.1 g/L, with a 95% confidence interval of −8.3 g/L to −5.9 g/L.
“Initial assessment and longitudinal monitoring of hemoglobin values seems advisable in patients with the SARS-CoV-2 infection, whereby a progressive decrease in the hemoglobin concentration may reflect a worse clinical progression,” the authors stated. They also suggested that studies should be “urgently planned to assess whether transfusion support (e.g., with administration of blood or packed red blood cells) may be helpful in this clinical setting to prevent evolution into severe disease and death.”
The authors declared the had no conflicts of interest.
SOURCE: Lippi G et al. Hematol Transfus Cell Ther. 2020 Apr 11; doi:10.1016/j.htct.2020.03.001.
FROM HEMATOLOGY, TRANSFUSION AND CELL THERAPY
COVID-19: When health care personnel become patients
according to the Centers for Disease Control and Prevention.
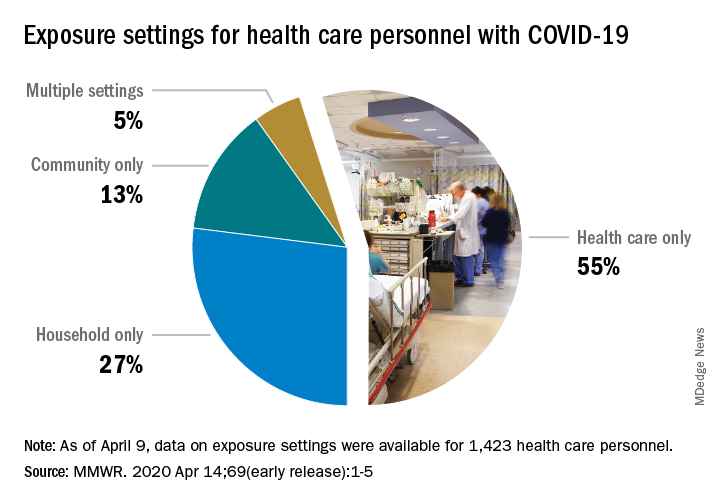
That number, however, is probably an underestimation because health care personnel (HCP) status was available for just over 49,000 of the 315,000 COVID-19 cases reported to the CDC as of April 9. Of the cases with known HCP status, 9,282 (19%) were health care personnel, Matthew J. Stuckey, PhD, and the CDC’s COVID-19 Response Team said.
“The number of cases in HCP reported here must be considered a lower bound because additional cases likely have gone unidentified or unreported,” they said.
The median age of the nearly 9,300 HCP with COVID-19 was 42 years, and the majority (55%) were aged 16-44 years; another 21% were 45-54, 18% were 55-64, and 6% were age 65 and over. The oldest group, however, represented 10 of the 27 known HCP deaths, the investigators reported in the Morbidity and Mortality Weekly Report.
The majority of infected HCP (55%) reported exposure to a COVID-19 patient in the health care setting, but “there were also known exposures in households and in the community, highlighting the potential for exposure in multiple settings, especially as community transmission increases,” the response team said.
Since “contact tracing after recognized occupational exposures likely will fail to identify many HCP at risk for developing COVID-19,” other measures will probably be needed to “reduce the risk for infected HCP transmitting the virus to colleagues and patients,” they added.
HCP with COVID-19 were less likely to be hospitalized (8%-10%) than the overall population (21%-31%), which “might reflect the younger median age … of HCP patients, compared with that of reported COVID-19 patients overall, as well as prioritization of HCP for testing, which might identify less-severe illness,” the investigators suggested.
The prevalence of underlying conditions in HCP patients, 38%, was the same as all patients with COVID-19, and 92% of the HCP patients presented with fever, cough, or shortness of breath. Two-thirds of all HCP reported muscle aches, and 65% reported headache, the CDC response team noted.
“It is critical to make every effort to ensure the health and safety of this essential national workforce of approximately 18 million HCP, both at work and in the community,” they wrote.
SOURCE: Stuckey MJ et al. MMWR. Apr 14;69(early release):1-5.
according to the Centers for Disease Control and Prevention.
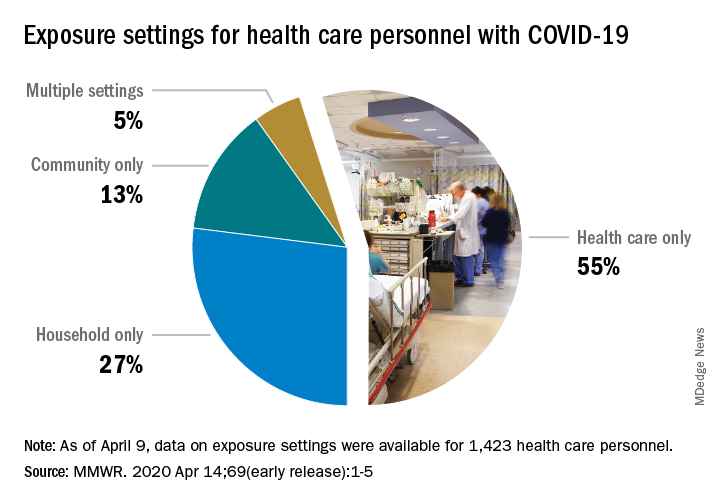
That number, however, is probably an underestimation because health care personnel (HCP) status was available for just over 49,000 of the 315,000 COVID-19 cases reported to the CDC as of April 9. Of the cases with known HCP status, 9,282 (19%) were health care personnel, Matthew J. Stuckey, PhD, and the CDC’s COVID-19 Response Team said.
“The number of cases in HCP reported here must be considered a lower bound because additional cases likely have gone unidentified or unreported,” they said.
The median age of the nearly 9,300 HCP with COVID-19 was 42 years, and the majority (55%) were aged 16-44 years; another 21% were 45-54, 18% were 55-64, and 6% were age 65 and over. The oldest group, however, represented 10 of the 27 known HCP deaths, the investigators reported in the Morbidity and Mortality Weekly Report.
The majority of infected HCP (55%) reported exposure to a COVID-19 patient in the health care setting, but “there were also known exposures in households and in the community, highlighting the potential for exposure in multiple settings, especially as community transmission increases,” the response team said.
Since “contact tracing after recognized occupational exposures likely will fail to identify many HCP at risk for developing COVID-19,” other measures will probably be needed to “reduce the risk for infected HCP transmitting the virus to colleagues and patients,” they added.
HCP with COVID-19 were less likely to be hospitalized (8%-10%) than the overall population (21%-31%), which “might reflect the younger median age … of HCP patients, compared with that of reported COVID-19 patients overall, as well as prioritization of HCP for testing, which might identify less-severe illness,” the investigators suggested.
The prevalence of underlying conditions in HCP patients, 38%, was the same as all patients with COVID-19, and 92% of the HCP patients presented with fever, cough, or shortness of breath. Two-thirds of all HCP reported muscle aches, and 65% reported headache, the CDC response team noted.
“It is critical to make every effort to ensure the health and safety of this essential national workforce of approximately 18 million HCP, both at work and in the community,” they wrote.
SOURCE: Stuckey MJ et al. MMWR. Apr 14;69(early release):1-5.
according to the Centers for Disease Control and Prevention.
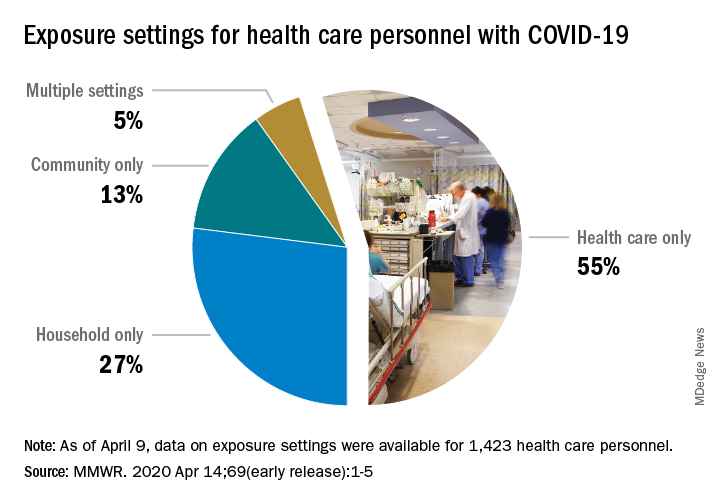
That number, however, is probably an underestimation because health care personnel (HCP) status was available for just over 49,000 of the 315,000 COVID-19 cases reported to the CDC as of April 9. Of the cases with known HCP status, 9,282 (19%) were health care personnel, Matthew J. Stuckey, PhD, and the CDC’s COVID-19 Response Team said.
“The number of cases in HCP reported here must be considered a lower bound because additional cases likely have gone unidentified or unreported,” they said.
The median age of the nearly 9,300 HCP with COVID-19 was 42 years, and the majority (55%) were aged 16-44 years; another 21% were 45-54, 18% were 55-64, and 6% were age 65 and over. The oldest group, however, represented 10 of the 27 known HCP deaths, the investigators reported in the Morbidity and Mortality Weekly Report.
The majority of infected HCP (55%) reported exposure to a COVID-19 patient in the health care setting, but “there were also known exposures in households and in the community, highlighting the potential for exposure in multiple settings, especially as community transmission increases,” the response team said.
Since “contact tracing after recognized occupational exposures likely will fail to identify many HCP at risk for developing COVID-19,” other measures will probably be needed to “reduce the risk for infected HCP transmitting the virus to colleagues and patients,” they added.
HCP with COVID-19 were less likely to be hospitalized (8%-10%) than the overall population (21%-31%), which “might reflect the younger median age … of HCP patients, compared with that of reported COVID-19 patients overall, as well as prioritization of HCP for testing, which might identify less-severe illness,” the investigators suggested.
The prevalence of underlying conditions in HCP patients, 38%, was the same as all patients with COVID-19, and 92% of the HCP patients presented with fever, cough, or shortness of breath. Two-thirds of all HCP reported muscle aches, and 65% reported headache, the CDC response team noted.
“It is critical to make every effort to ensure the health and safety of this essential national workforce of approximately 18 million HCP, both at work and in the community,” they wrote.
SOURCE: Stuckey MJ et al. MMWR. Apr 14;69(early release):1-5.
FROM THE MMWR
FDA approves emergency use of saliva test to detect COVID-19
As the race to develop rapid testing for COVID-19 expands, the Food and Drug Administration has granted emergency approval for an approach that uses saliva as the primary test biomaterial.
According to a document provided to the FDA, the Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab from individuals suspected of COVID-19 by their health care clinicians. To expand on this assay, Rutgers University–based RUCDR Infinite Biologics developed a saliva collection method in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The document states that Samples are transported for RNA extraction and are tested within 48 hours of collection. In saliva samples obtained from 60 patients evaluated by the researchers, all were in agreement with the presence of COVID-19.
“If shown to be as accurate as nasopharyngeal and oropharyngeal samples, saliva as a biomatrix offers the advantage of not generating aerosols or creating as many respiratory droplets during specimen procurement, therefore decreasing the risk of transmission to the health care worker doing the testing,” said Matthew P. Cheng, MDCM, of the division of infectious diseases at McGill University Health Centre, Montreal, who was not involved in development of the test but who has written about diagnostic testing for the virus.
“Also, it may be easy enough for patients to do saliva self-collection at home. However, it is important to note that SARS-CoV-2 tests on saliva have not yet undergone the more rigorous evaluation of full FDA authorization, and saliva is not a preferred specimen type of the FDA nor the [Centers for Disease Control and Prevention] for respiratory virus testing.”
In a prepared statement, Andrew I. Brooks, PhD, chief operating officer at RUCDR Infinite Biologics, said the saliva collection method enables clinicians to preserve personal protective equipment for use in patient care instead of testing. “We can significantly increase the number of people tested each and every day as self-collection of saliva is quicker and more scalable than swab collections,” he said. “All of this combined will have a tremendous impact on testing in New Jersey and across the United States.”
The tests are currently available to the RWJBarnabas Health network, based in West Orange, N.J., which has partnered with Rutgers University.
As the race to develop rapid testing for COVID-19 expands, the Food and Drug Administration has granted emergency approval for an approach that uses saliva as the primary test biomaterial.
According to a document provided to the FDA, the Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab from individuals suspected of COVID-19 by their health care clinicians. To expand on this assay, Rutgers University–based RUCDR Infinite Biologics developed a saliva collection method in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The document states that Samples are transported for RNA extraction and are tested within 48 hours of collection. In saliva samples obtained from 60 patients evaluated by the researchers, all were in agreement with the presence of COVID-19.
“If shown to be as accurate as nasopharyngeal and oropharyngeal samples, saliva as a biomatrix offers the advantage of not generating aerosols or creating as many respiratory droplets during specimen procurement, therefore decreasing the risk of transmission to the health care worker doing the testing,” said Matthew P. Cheng, MDCM, of the division of infectious diseases at McGill University Health Centre, Montreal, who was not involved in development of the test but who has written about diagnostic testing for the virus.
“Also, it may be easy enough for patients to do saliva self-collection at home. However, it is important to note that SARS-CoV-2 tests on saliva have not yet undergone the more rigorous evaluation of full FDA authorization, and saliva is not a preferred specimen type of the FDA nor the [Centers for Disease Control and Prevention] for respiratory virus testing.”
In a prepared statement, Andrew I. Brooks, PhD, chief operating officer at RUCDR Infinite Biologics, said the saliva collection method enables clinicians to preserve personal protective equipment for use in patient care instead of testing. “We can significantly increase the number of people tested each and every day as self-collection of saliva is quicker and more scalable than swab collections,” he said. “All of this combined will have a tremendous impact on testing in New Jersey and across the United States.”
The tests are currently available to the RWJBarnabas Health network, based in West Orange, N.J., which has partnered with Rutgers University.
As the race to develop rapid testing for COVID-19 expands, the Food and Drug Administration has granted emergency approval for an approach that uses saliva as the primary test biomaterial.
According to a document provided to the FDA, the Rutgers Clinical Genomics Laboratory TaqPath SARS-CoV-2 Assay is intended for the qualitative detection of nucleic acid from SARS-CoV-2 in oropharyngeal (throat) swab, nasopharyngeal swab, anterior nasal swab, mid-turbinate nasal swab from individuals suspected of COVID-19 by their health care clinicians. To expand on this assay, Rutgers University–based RUCDR Infinite Biologics developed a saliva collection method in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The document states that Samples are transported for RNA extraction and are tested within 48 hours of collection. In saliva samples obtained from 60 patients evaluated by the researchers, all were in agreement with the presence of COVID-19.
“If shown to be as accurate as nasopharyngeal and oropharyngeal samples, saliva as a biomatrix offers the advantage of not generating aerosols or creating as many respiratory droplets during specimen procurement, therefore decreasing the risk of transmission to the health care worker doing the testing,” said Matthew P. Cheng, MDCM, of the division of infectious diseases at McGill University Health Centre, Montreal, who was not involved in development of the test but who has written about diagnostic testing for the virus.
“Also, it may be easy enough for patients to do saliva self-collection at home. However, it is important to note that SARS-CoV-2 tests on saliva have not yet undergone the more rigorous evaluation of full FDA authorization, and saliva is not a preferred specimen type of the FDA nor the [Centers for Disease Control and Prevention] for respiratory virus testing.”
In a prepared statement, Andrew I. Brooks, PhD, chief operating officer at RUCDR Infinite Biologics, said the saliva collection method enables clinicians to preserve personal protective equipment for use in patient care instead of testing. “We can significantly increase the number of people tested each and every day as self-collection of saliva is quicker and more scalable than swab collections,” he said. “All of this combined will have a tremendous impact on testing in New Jersey and across the United States.”
The tests are currently available to the RWJBarnabas Health network, based in West Orange, N.J., which has partnered with Rutgers University.
Learning about the curve
Empty shelves that once cradled toilet paper rolls; lines of shoppers, some with masks; waiting 6 feet or at least a shopping cart length apart to get into grocery stores; hazmat-suited workers loading body bags into makeshift mortuaries ... These are the images we have come to associate with the COVID-19 pandemic. But then there also are the graphs and charts, none of them bearing good news. Some are difficult to interpret because they may be missing a key ingredient, such as a scale. Day to day fluctuations in the timeliness of the data points can make valid comparisons impossible. In most cases, it is too early to look at the graphs and hope for the big picture. Whether you are concerned about the stock market or the number of new cases of the virus in your county, you are hoping to see some graphic depiction of a favorable trend.
We have suddenly learned about the urgency of a process called “flattening the curve.” Are we doing as good a job of flattening as we could be? Are we doing better than France or Spain? Or are we heading toward an Italianesque apocalypse? Who is going to tell us when the flattening is for real and not just a 2- or 3-day statistical aberration?
The curves we are obsessed with today are those showing us new cases and new deaths. But And we won’t be seeing this curve in four-color graphics on the front page of our newspapers. It is the learning curve, and we want it to be as steep as we can make it without any hint of flattening in the foreseeable future.
We need to learn more about corona-like viruses. Why are some of us more vulnerable? We need to learn more about contagion. Does the 6-foot guideline make any sense? How long are viral particles floating in the air capable of initiating disease? What about air flow and dilution? Can we build a cruise ship or airplane that will be less of a health hazard?
More importantly, we need to learn to be better prepared. Even before the pandemic there have been shortages in intravenous solutions and drugs of critical importance to common diseases. Can we learn how to create reliable and affordable supply chains that allow researchers and developers to make a reasonable profit? Can we relearn to value science? Can we learn to invest more heavily in epidemiology and make it a specialty that attracts our best thinkers and communicators? Then can we elect officials who will share our trust in their recommendations?
Can we do a better job of resolving the tension between those who believe in a strong federal government and those who believe in local autonomy because we are seeing every day that this is an issue of survival, not just coexistence? Can we learn that the globalization that has allowed this viral spread can also be leveraged to beat it into submission?
Over the last half century there has been an unfortunate flattening of the learning curve. Ironically we have seen exponential growth among hi-tech industries that have forced us to keep abreast of new developments. But along with this has been a growing skepticism about value of scientific investigation. It is time we climbed back on that steep learning curve. The view gets better the higher we climb.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Empty shelves that once cradled toilet paper rolls; lines of shoppers, some with masks; waiting 6 feet or at least a shopping cart length apart to get into grocery stores; hazmat-suited workers loading body bags into makeshift mortuaries ... These are the images we have come to associate with the COVID-19 pandemic. But then there also are the graphs and charts, none of them bearing good news. Some are difficult to interpret because they may be missing a key ingredient, such as a scale. Day to day fluctuations in the timeliness of the data points can make valid comparisons impossible. In most cases, it is too early to look at the graphs and hope for the big picture. Whether you are concerned about the stock market or the number of new cases of the virus in your county, you are hoping to see some graphic depiction of a favorable trend.
We have suddenly learned about the urgency of a process called “flattening the curve.” Are we doing as good a job of flattening as we could be? Are we doing better than France or Spain? Or are we heading toward an Italianesque apocalypse? Who is going to tell us when the flattening is for real and not just a 2- or 3-day statistical aberration?
The curves we are obsessed with today are those showing us new cases and new deaths. But And we won’t be seeing this curve in four-color graphics on the front page of our newspapers. It is the learning curve, and we want it to be as steep as we can make it without any hint of flattening in the foreseeable future.
We need to learn more about corona-like viruses. Why are some of us more vulnerable? We need to learn more about contagion. Does the 6-foot guideline make any sense? How long are viral particles floating in the air capable of initiating disease? What about air flow and dilution? Can we build a cruise ship or airplane that will be less of a health hazard?
More importantly, we need to learn to be better prepared. Even before the pandemic there have been shortages in intravenous solutions and drugs of critical importance to common diseases. Can we learn how to create reliable and affordable supply chains that allow researchers and developers to make a reasonable profit? Can we relearn to value science? Can we learn to invest more heavily in epidemiology and make it a specialty that attracts our best thinkers and communicators? Then can we elect officials who will share our trust in their recommendations?
Can we do a better job of resolving the tension between those who believe in a strong federal government and those who believe in local autonomy because we are seeing every day that this is an issue of survival, not just coexistence? Can we learn that the globalization that has allowed this viral spread can also be leveraged to beat it into submission?
Over the last half century there has been an unfortunate flattening of the learning curve. Ironically we have seen exponential growth among hi-tech industries that have forced us to keep abreast of new developments. But along with this has been a growing skepticism about value of scientific investigation. It is time we climbed back on that steep learning curve. The view gets better the higher we climb.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Empty shelves that once cradled toilet paper rolls; lines of shoppers, some with masks; waiting 6 feet or at least a shopping cart length apart to get into grocery stores; hazmat-suited workers loading body bags into makeshift mortuaries ... These are the images we have come to associate with the COVID-19 pandemic. But then there also are the graphs and charts, none of them bearing good news. Some are difficult to interpret because they may be missing a key ingredient, such as a scale. Day to day fluctuations in the timeliness of the data points can make valid comparisons impossible. In most cases, it is too early to look at the graphs and hope for the big picture. Whether you are concerned about the stock market or the number of new cases of the virus in your county, you are hoping to see some graphic depiction of a favorable trend.
We have suddenly learned about the urgency of a process called “flattening the curve.” Are we doing as good a job of flattening as we could be? Are we doing better than France or Spain? Or are we heading toward an Italianesque apocalypse? Who is going to tell us when the flattening is for real and not just a 2- or 3-day statistical aberration?
The curves we are obsessed with today are those showing us new cases and new deaths. But And we won’t be seeing this curve in four-color graphics on the front page of our newspapers. It is the learning curve, and we want it to be as steep as we can make it without any hint of flattening in the foreseeable future.
We need to learn more about corona-like viruses. Why are some of us more vulnerable? We need to learn more about contagion. Does the 6-foot guideline make any sense? How long are viral particles floating in the air capable of initiating disease? What about air flow and dilution? Can we build a cruise ship or airplane that will be less of a health hazard?
More importantly, we need to learn to be better prepared. Even before the pandemic there have been shortages in intravenous solutions and drugs of critical importance to common diseases. Can we learn how to create reliable and affordable supply chains that allow researchers and developers to make a reasonable profit? Can we relearn to value science? Can we learn to invest more heavily in epidemiology and make it a specialty that attracts our best thinkers and communicators? Then can we elect officials who will share our trust in their recommendations?
Can we do a better job of resolving the tension between those who believe in a strong federal government and those who believe in local autonomy because we are seeing every day that this is an issue of survival, not just coexistence? Can we learn that the globalization that has allowed this viral spread can also be leveraged to beat it into submission?
Over the last half century there has been an unfortunate flattening of the learning curve. Ironically we have seen exponential growth among hi-tech industries that have forced us to keep abreast of new developments. But along with this has been a growing skepticism about value of scientific investigation. It is time we climbed back on that steep learning curve. The view gets better the higher we climb.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].