User login
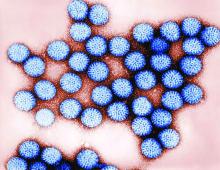
A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
[email protected]
On Twitter @EAZTweets
Rotavirus is the leading cause of diarrhea-associated death in children aged under 5 years, and with 85% of all deaths occurring in Africa and Asia, proper channels of vaccine dissemination are critical. There is no question to the positive influence of rotavirus vaccines, as research suggests they could save 2.46 million children’s lives and prevent another 83 million from living with a disability between 2011 and 2030.
While two vaccines, Rotarix and RotaTeq, are already being introduced to patients in 48 countries, diminishing vaccine uptake is standing in the way of these interventions reaching their full potential. Despite subsidies from Gavi (the vaccine alliance) and the World Health Organization, costs are still too high and the necessity for cold storage poses a financial and logistical problem for a majority of high risk countries. The BRV-PV vaccine developed by Serum Institute of India seems to be a step in the right direction in helping to ease this burden.
While its efficacy is modest, BRV-PV has shown promise through its heat stability as well as its cost, which falls between the prices of the two already available vaccines.
It is not perfect; as a freeze-dried vaccine, it may pose problems in areas where oral liquid, all-in-one vaccinations are preferred. Yet, there is no doubt that an increase in affordable, programmatically suitable options will help achieve the goal of ending rotavirus related deaths globally.
Mathuram Santosham, MD, is professor of pediatrics and pediatric infectious diseases at Johns Hopkins University, Baltimore. Duncan Steele, PhD, is a microbiologist and deputy director and strategic lead for enteric vaccines and enteric and diarrheal diseases for the Bill & Melinda Gates Foundation, Seattle. They coauthored the editorial regarding the article by Isanaka et al. (N Engl J Med. 2017 March 23;376[12]:1170-2). Dr. Santosham reported no relevant financial disclosures. Dr. Steele reports that he is employed at the Bill & Melinda Gates Foundation, which has supported through funding, the development of multiple rotavirus vaccine candidates including the lyophilized rotavirus vaccine produced by Serum Institute.
Rotavirus is the leading cause of diarrhea-associated death in children aged under 5 years, and with 85% of all deaths occurring in Africa and Asia, proper channels of vaccine dissemination are critical. There is no question to the positive influence of rotavirus vaccines, as research suggests they could save 2.46 million children’s lives and prevent another 83 million from living with a disability between 2011 and 2030.
While two vaccines, Rotarix and RotaTeq, are already being introduced to patients in 48 countries, diminishing vaccine uptake is standing in the way of these interventions reaching their full potential. Despite subsidies from Gavi (the vaccine alliance) and the World Health Organization, costs are still too high and the necessity for cold storage poses a financial and logistical problem for a majority of high risk countries. The BRV-PV vaccine developed by Serum Institute of India seems to be a step in the right direction in helping to ease this burden.
While its efficacy is modest, BRV-PV has shown promise through its heat stability as well as its cost, which falls between the prices of the two already available vaccines.
It is not perfect; as a freeze-dried vaccine, it may pose problems in areas where oral liquid, all-in-one vaccinations are preferred. Yet, there is no doubt that an increase in affordable, programmatically suitable options will help achieve the goal of ending rotavirus related deaths globally.
Mathuram Santosham, MD, is professor of pediatrics and pediatric infectious diseases at Johns Hopkins University, Baltimore. Duncan Steele, PhD, is a microbiologist and deputy director and strategic lead for enteric vaccines and enteric and diarrheal diseases for the Bill & Melinda Gates Foundation, Seattle. They coauthored the editorial regarding the article by Isanaka et al. (N Engl J Med. 2017 March 23;376[12]:1170-2). Dr. Santosham reported no relevant financial disclosures. Dr. Steele reports that he is employed at the Bill & Melinda Gates Foundation, which has supported through funding, the development of multiple rotavirus vaccine candidates including the lyophilized rotavirus vaccine produced by Serum Institute.
Rotavirus is the leading cause of diarrhea-associated death in children aged under 5 years, and with 85% of all deaths occurring in Africa and Asia, proper channels of vaccine dissemination are critical. There is no question to the positive influence of rotavirus vaccines, as research suggests they could save 2.46 million children’s lives and prevent another 83 million from living with a disability between 2011 and 2030.
While two vaccines, Rotarix and RotaTeq, are already being introduced to patients in 48 countries, diminishing vaccine uptake is standing in the way of these interventions reaching their full potential. Despite subsidies from Gavi (the vaccine alliance) and the World Health Organization, costs are still too high and the necessity for cold storage poses a financial and logistical problem for a majority of high risk countries. The BRV-PV vaccine developed by Serum Institute of India seems to be a step in the right direction in helping to ease this burden.
While its efficacy is modest, BRV-PV has shown promise through its heat stability as well as its cost, which falls between the prices of the two already available vaccines.
It is not perfect; as a freeze-dried vaccine, it may pose problems in areas where oral liquid, all-in-one vaccinations are preferred. Yet, there is no doubt that an increase in affordable, programmatically suitable options will help achieve the goal of ending rotavirus related deaths globally.
Mathuram Santosham, MD, is professor of pediatrics and pediatric infectious diseases at Johns Hopkins University, Baltimore. Duncan Steele, PhD, is a microbiologist and deputy director and strategic lead for enteric vaccines and enteric and diarrheal diseases for the Bill & Melinda Gates Foundation, Seattle. They coauthored the editorial regarding the article by Isanaka et al. (N Engl J Med. 2017 March 23;376[12]:1170-2). Dr. Santosham reported no relevant financial disclosures. Dr. Steele reports that he is employed at the Bill & Melinda Gates Foundation, which has supported through funding, the development of multiple rotavirus vaccine candidates including the lyophilized rotavirus vaccine produced by Serum Institute.
A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
[email protected]
On Twitter @EAZTweets
A new low-cost rotavirus gastroenteritis vaccine that does not require cold storage showed a vaccine efficacy of 67% in a per-protocol test of 3,508 Nigerien infants, according to a study by Sheila Isanaka of the department of research at Epicentre, Paris, and her associates.
In a double blind, placebo-controlled test of the oral bovine rotavirus pentavalent vaccine (BRV-PV), 31 severe cases of rotavirus were found in the vaccinated group of 1,780, while 87 cases were found in the placebo group of 1,728 (2.14 vs. 6.44 cases per 100 person-years, respectively), according to Ms. Isanaka and her colleagues (N Engl J Med. 2017 Mar 23;376[12]:1121-30).
Researchers gathered infants with severe symptoms and administered three injections of either BRV-PV or the placebo from August 2014 through November 2015. The BRV-PV vaccine, manufactured by Serum Institute of India, contains the rotavirus serotypes G1, G2, G3, G4, and G9.
With regard to adverse events, there was no distinction between the two groups (P greater than .15). According to medical investigators, the most common cause of deaths – 27 and 22 in the vaccine and placebo groups, respectively – was infections and infestations (in 37 infants) and metabolism and nutrition disorders (in 6).
Part of what makes this vaccine unique is its shelf life of 2 years when kept at 37° C, or 6 months at 40° C, a key point for Ms. Isanaka and her colleagues.
“The global supply of the vaccines is constrained, and unreliable transportation and storage systems make delivery of vaccines that require refrigeration difficult,” Ms. Isanaka and her colleagues reported. “The introduction of BRV-PV may help to minimize the burden on already strained immunization programs.” The vaccine is also “for sale at or below the current price of the two WHO prequalified vaccines that are supported by the Gavi alliance,” making it possibly more financially accessible as well.
While the per-protocol test found efficacy at 67%, the intention-to-treat population reported a higher efficacy of 73%. Ms. Isanaka and her colleagues believe this number “may more closely represent the efficacy under real-world conditions,” due to the more flexible vaccination schedule.
This study was limited by a short time frame, which did not allow researchers to gather genotyping data pertaining to the efficacy against changing serotypes. BRV-PV also was not given consistently with the oral polio vaccine.
The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.
[email protected]
On Twitter @EAZTweets
Key clinical point:
Major finding: Of 3,508 infants studied, 31 cases of severe rotavirus gastroenteritis were found in the vaccine group, and 87 cases in the placebo group, putting efficacy at 67%.
Data source: Double blind, placebo-controlled test of 3,508 Nigerian infants whose symptoms were measured via 20-point Vesikari scoring.
Disclosures: The study was supported by Médecins sans Frontières Operational Center in Geneva and the Kavli Foundation. Ms. Isanaka’s institution, Epicentre, receives core funding from Médecins sans Frontières. Ms. McNeal reports grant support from Epicentre for the study, and other support from Merck and GlaxoSmithKline outside the submitted work. None of the other researchers had relevant financial disclosures.