User login
A 34-year-old woman came to our clinic because she was concerned about her thumbnail, which had turned green. Although her finger didn’t hurt, she was bothered by its appearance. Several months earlier, the woman had sought care at a different clinic because the same nail had become brittle and come loose from the nail bed, which was spongy. The physician advised her that she had onychomycosis and prescribed ciclopirox lacquer, but it didn’t help.
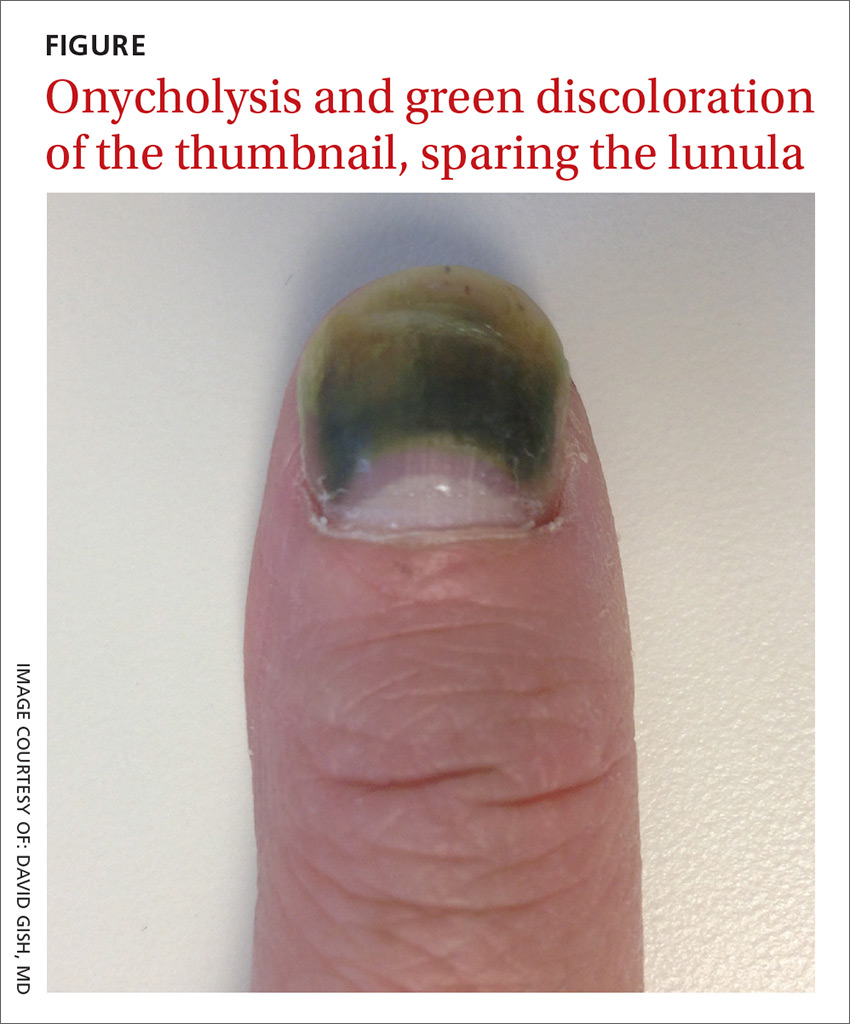
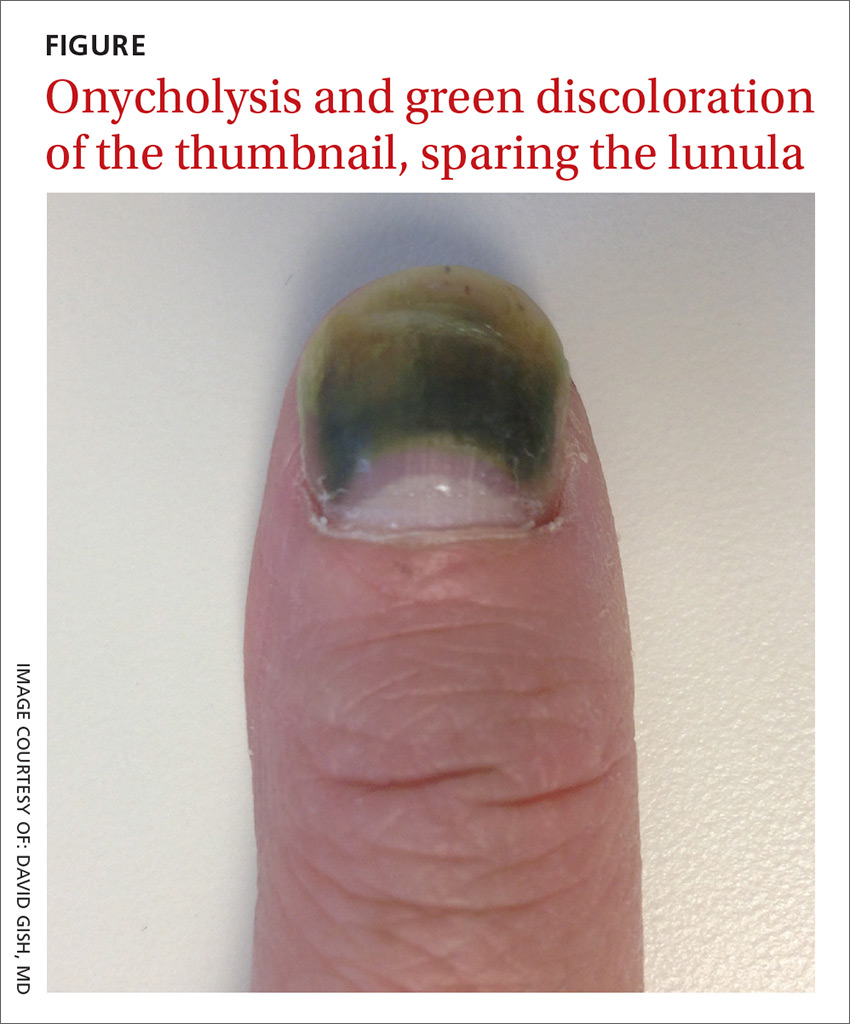
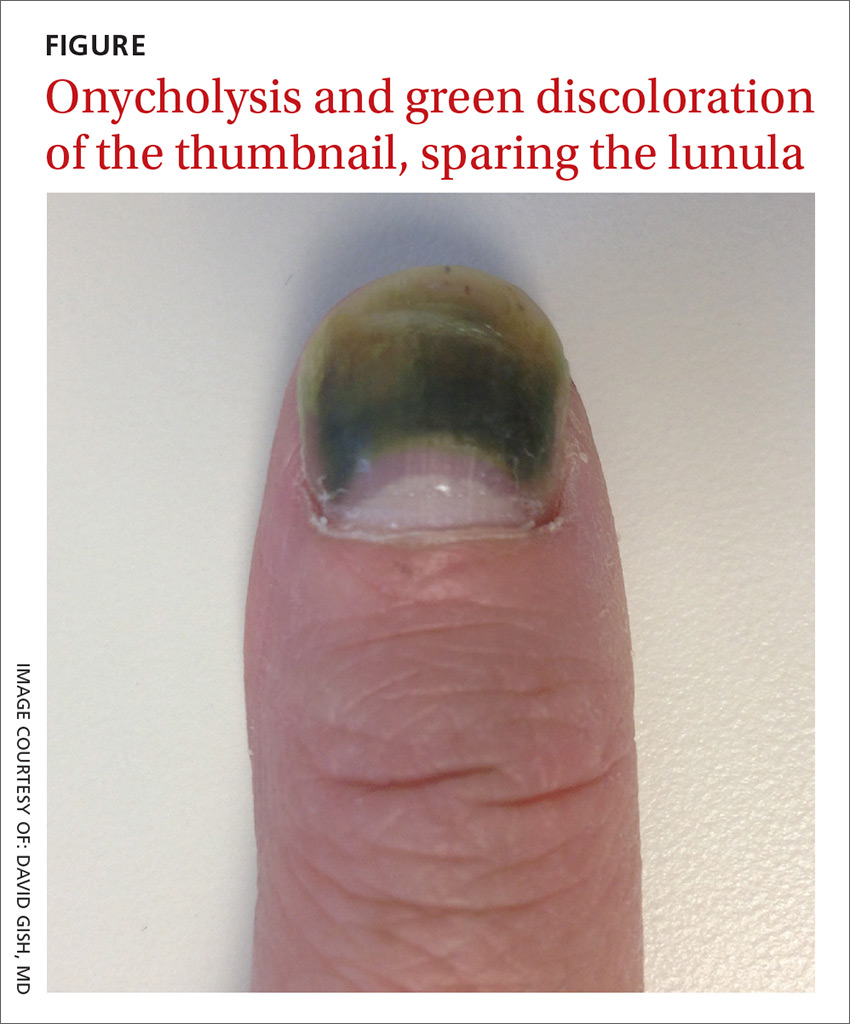
Over the next 3 weeks, she noticed a faint green hue developing at the tip of the nail, which expanded and intensified in color (FIGURE). The patient was a mother who worked at home, washed dishes by hand daily, and bathed her children. Her past medical history was significant for type 1 diabetes mellitus and Hashimoto’s thyroiditis. She had no other symptoms.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Green nail syndrome caused by Pseudomonas aeruginosa
This patient had green nail syndrome (GNS), an infection of the nail bed caused by Pseudomonas aeruginosa. These bacteria produce pyocyanin, a blue-green pigment that discolors the nail.1 GNS often occurs in patients with prior nail problems, such as onychomycosis, onycholysis, trauma, chronic paronychia, or psoriasis.
Nail disease disrupts the integumentary barrier and allows a portal of entry for bacteria. Scanning electron microscopy of patients with GNS has shown that fungal infections create tunnel-like structures in the nail keratin, and P aeruginosa grows in these spaces.2 Nails with prior nail disease that are chronically exposed to moisture are at greatest risk of developing GNS,3,4 and it is typical for only one nail to be involved.5Pseudomonas is the most common bacterial infection of the nails, but is not well known because it is rarely reported and patients often don’t seek care.6
In our patient’s case, her prior onychomycosis helped to create a favorable environment for the growth of the bacteria. Onycholysis—characterized by separation of the nail plate from the nail bed—was also present in our patient, based on her description of a “spongy” nail bed and loose nail, allowing moisture and bacteria to infiltrate the space. Onycholysis is associated with hypothyroidism, which the patient also had.7 The frequent soaking of her hands during dishwashing and bathing her children helped to provide the moist environment in which Pseudomonas thrives.
As was the case in this patient, GNS is often painless, or may be accompanied by mild tenderness of the nail. Patients may seek treatment primarily for cosmetic reasons.
GNS can be diagnosed by clinical observation and characteristic pigmentation along with an appropriate patient history.4 Culture of the nail bed may be helpful if bacterial resistance or co-infection with fungal organisms is suspected.
Changes in nail color can be a sign of many conditions
Nail discoloration, or chromonychia, can present in a variety of colors. Nail findings may represent an isolated disease or provide an important clinical clue to other systemic diseases.8 The specific shade of discoloration helps to differentiate the underlying pathology.
Yellow nail syndrome. As the name implies, this syndrome typically causes yellow discoloration of the nail (although yellow-green is also possible). Yellow nail syndrome is believed to be due to microvascular permeability, which also accounts for its associated clinical triad: hypoalbuminemia, pleural effusion, and lymphedema. Yellow nail syndrome may be seen in patients with bronchiectasis, internal malignancies, immunodeficiency, and rheumatoid arthritis.8
Nail bed hematoma. Among the most common causes of nail discoloration, these lesions typically appear as reddish to reddish-black, depending on the age of the bleed, and will often have streaks at the distal margin of the lesion.9 Risk factors for hemorrhage include blood thinners and clotting disorders. Subungual hemorrhages that do not grow out with the nail, or that recur in the same place, may require biopsy.9
Subungual melanoma causes black-brown discoloration of the nails, and may form a longitudinal band in the nail.9 Longitudinal melanonychia is a common variant in African American individuals.10 Features that increase the likelihood of melanoma include a family history of melanoma, a sudden change in the appearance of the lesion, band width greater than 3 mm, pigment changes extending into the cuticle (known as Hutchinson’s sign), and nail plate disruption.
Dermoscopy, the technique of using surface microscopy to examine the skin, may be helpful in distinguishing nail lesions. (See a video on how to perform dermoscopy here: http://bit.ly/2pyJ3xN.)
Nonmelanocytic lesions tend to have homogeneously distributed pigment, while melanocytic lesions contain granules of pigment in cellular inclusions. Any suspicion of melanoma warrants a punch biopsy.11
Medication-induced effects. Minocycline may cause bluish nail discoloration similar to that produced by infection with P aeruginosa, but it is rare for only a single nail to be involved. In addition, pigmentation changes are often present elsewhere on the body, including the sclerae, teeth, and pinna.
Another medication known to color the nails blue is colloidal silver, which is still sold as a dietary supplement or homeopathic remedy to treat a wide range of ailments.6 (Of note: In 1999, the Food and Drug Administration issued a final rule saying that colloidal silver isn’t safe or effective for treating any disease or condition.12)
Glomus tumor. Another cause of blue nails is glomus tumors, relatively uncommon perivascular neoplasms that are typically found in the subungual region. These tumors are generally accompanied by localized tenderness, cold sensitivity, and paroxysms of excruciating pain that are disproportional to the size of the tumor.
Imaging studies may aid in the diagnosis, in addition to pathologic confirmation. Magnetic resonance imaging is the most sensitive imaging modality; if a glomus tumor is present, it most often appears as a well-circumscribed T2 hyperintense lesion.13
Exogenous pigmentation. Nails may become discolored due to exposure to various toxins or chemicals. Frequent culprits include eosin, methylene blue, henna, hair dye, and tobacco.9
Antibiotics and measures to keep the nail dry will help resolve infection
When chronic nail wetness is a contributing factor, treatment begins with measures to keep the nails dry. In addition, either topical or systemic antibiotics may be used to eradicate the infection. Topical applications with agents such as nadifloxacin have been shown to be effective in several case reports,3 but large-scale controlled trials are lacking. Fluoroquinolones are regarded as first-line systemic treatment.5 Briefly soaking the nail in a diluted sodium hypochlorite (bleach) solution also helps to suppress bacterial growth. Nail extraction may be required in refractory cases.
For our patient, we prescribed ciprofloxacin 500 mg twice a day for 10 days, plus bleach soaks (one part bleach to 4 parts water) twice a day. We recommended that our patient wear gloves for household tasks that involved immersing her hands in water, and drying her finger with a hair dryer after bathing.
CORRESPONDENCE
David Gish, MD, University of Virginia Health System, 1215 Lee St. Charlottesville, VA 22908; [email protected].
1. Greene SL, Su WP, Muller SA. Pseudomonas aeruginosa infections of the skin. Am Fam Physician. 1984;29:193-200.
2. de Almeida HL Jr, Duquia RP, de Castro LA, et al. Scanning electron microscopy of the green nail. Int J Dermatol. 2010;49:962-963.
3. Hengge UR, Bardeli V. Images in clinical medicine. Green nails. N Engl J Med. 2009;360:1125.
4. Chiriac A, Brzezinski P, Foia L, et al. Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons. Clin Interv Aging. 2015;10:265-267.
5. Müller S, Ebnöther M, Itin P. Green nail syndrome (Pseudomonas aeruginosa nail infection): Two cases successfully treated with topical nadifloxacin, an acne medication. Case Rep Dermatol. 2014;6:180-184.
6. Raam R, DeClerck B, Jhun P, et al. That’s some weird nail polish you got there! Ann Emerg Med. 2015;66:585-588.
7. Gregoriou S, Argyriou G, Larios G, et al. Nail disorders and systemic disease: what the nails tell us. J Fam Pract. 2008;57:509-514.
8. Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician. 2004;69:1417-1424.
9. Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol. 2007;56:835-847.
10. Buka R, Friedman KA, Phelps RG, et al. Childhood longitudinal melanonychia: case reports and review of the literature. Mt Sinai J Med. 2001;68:331-335.
11. Tully AS, Trayes KP, Studdiford JS. Evaluation of nail abnormalities. Am Fam Physician. 2012;85:779-787.
12. US Food and Drug Administration. Over-the-counter drug products containing colloidal silver ingredients or silver salts. 1999. Available at: https://www.fda.gov/ohrms/dockets/98fr/081799a.txt. Accessed April 11, 2017.
13. Glazebrook KN, Laundre BJ, Schiefer TK, et al. Imaging features of glomus tumors. Skeletal Radiol. 2011;40:855-862.
A 34-year-old woman came to our clinic because she was concerned about her thumbnail, which had turned green. Although her finger didn’t hurt, she was bothered by its appearance. Several months earlier, the woman had sought care at a different clinic because the same nail had become brittle and come loose from the nail bed, which was spongy. The physician advised her that she had onychomycosis and prescribed ciclopirox lacquer, but it didn’t help.
Over the next 3 weeks, she noticed a faint green hue developing at the tip of the nail, which expanded and intensified in color (FIGURE). The patient was a mother who worked at home, washed dishes by hand daily, and bathed her children. Her past medical history was significant for type 1 diabetes mellitus and Hashimoto’s thyroiditis. She had no other symptoms.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Green nail syndrome caused by Pseudomonas aeruginosa
This patient had green nail syndrome (GNS), an infection of the nail bed caused by Pseudomonas aeruginosa. These bacteria produce pyocyanin, a blue-green pigment that discolors the nail.1 GNS often occurs in patients with prior nail problems, such as onychomycosis, onycholysis, trauma, chronic paronychia, or psoriasis.
Nail disease disrupts the integumentary barrier and allows a portal of entry for bacteria. Scanning electron microscopy of patients with GNS has shown that fungal infections create tunnel-like structures in the nail keratin, and P aeruginosa grows in these spaces.2 Nails with prior nail disease that are chronically exposed to moisture are at greatest risk of developing GNS,3,4 and it is typical for only one nail to be involved.5Pseudomonas is the most common bacterial infection of the nails, but is not well known because it is rarely reported and patients often don’t seek care.6
In our patient’s case, her prior onychomycosis helped to create a favorable environment for the growth of the bacteria. Onycholysis—characterized by separation of the nail plate from the nail bed—was also present in our patient, based on her description of a “spongy” nail bed and loose nail, allowing moisture and bacteria to infiltrate the space. Onycholysis is associated with hypothyroidism, which the patient also had.7 The frequent soaking of her hands during dishwashing and bathing her children helped to provide the moist environment in which Pseudomonas thrives.
As was the case in this patient, GNS is often painless, or may be accompanied by mild tenderness of the nail. Patients may seek treatment primarily for cosmetic reasons.
GNS can be diagnosed by clinical observation and characteristic pigmentation along with an appropriate patient history.4 Culture of the nail bed may be helpful if bacterial resistance or co-infection with fungal organisms is suspected.
Changes in nail color can be a sign of many conditions
Nail discoloration, or chromonychia, can present in a variety of colors. Nail findings may represent an isolated disease or provide an important clinical clue to other systemic diseases.8 The specific shade of discoloration helps to differentiate the underlying pathology.
Yellow nail syndrome. As the name implies, this syndrome typically causes yellow discoloration of the nail (although yellow-green is also possible). Yellow nail syndrome is believed to be due to microvascular permeability, which also accounts for its associated clinical triad: hypoalbuminemia, pleural effusion, and lymphedema. Yellow nail syndrome may be seen in patients with bronchiectasis, internal malignancies, immunodeficiency, and rheumatoid arthritis.8
Nail bed hematoma. Among the most common causes of nail discoloration, these lesions typically appear as reddish to reddish-black, depending on the age of the bleed, and will often have streaks at the distal margin of the lesion.9 Risk factors for hemorrhage include blood thinners and clotting disorders. Subungual hemorrhages that do not grow out with the nail, or that recur in the same place, may require biopsy.9
Subungual melanoma causes black-brown discoloration of the nails, and may form a longitudinal band in the nail.9 Longitudinal melanonychia is a common variant in African American individuals.10 Features that increase the likelihood of melanoma include a family history of melanoma, a sudden change in the appearance of the lesion, band width greater than 3 mm, pigment changes extending into the cuticle (known as Hutchinson’s sign), and nail plate disruption.
Dermoscopy, the technique of using surface microscopy to examine the skin, may be helpful in distinguishing nail lesions. (See a video on how to perform dermoscopy here: http://bit.ly/2pyJ3xN.)
Nonmelanocytic lesions tend to have homogeneously distributed pigment, while melanocytic lesions contain granules of pigment in cellular inclusions. Any suspicion of melanoma warrants a punch biopsy.11
Medication-induced effects. Minocycline may cause bluish nail discoloration similar to that produced by infection with P aeruginosa, but it is rare for only a single nail to be involved. In addition, pigmentation changes are often present elsewhere on the body, including the sclerae, teeth, and pinna.
Another medication known to color the nails blue is colloidal silver, which is still sold as a dietary supplement or homeopathic remedy to treat a wide range of ailments.6 (Of note: In 1999, the Food and Drug Administration issued a final rule saying that colloidal silver isn’t safe or effective for treating any disease or condition.12)
Glomus tumor. Another cause of blue nails is glomus tumors, relatively uncommon perivascular neoplasms that are typically found in the subungual region. These tumors are generally accompanied by localized tenderness, cold sensitivity, and paroxysms of excruciating pain that are disproportional to the size of the tumor.
Imaging studies may aid in the diagnosis, in addition to pathologic confirmation. Magnetic resonance imaging is the most sensitive imaging modality; if a glomus tumor is present, it most often appears as a well-circumscribed T2 hyperintense lesion.13
Exogenous pigmentation. Nails may become discolored due to exposure to various toxins or chemicals. Frequent culprits include eosin, methylene blue, henna, hair dye, and tobacco.9
Antibiotics and measures to keep the nail dry will help resolve infection
When chronic nail wetness is a contributing factor, treatment begins with measures to keep the nails dry. In addition, either topical or systemic antibiotics may be used to eradicate the infection. Topical applications with agents such as nadifloxacin have been shown to be effective in several case reports,3 but large-scale controlled trials are lacking. Fluoroquinolones are regarded as first-line systemic treatment.5 Briefly soaking the nail in a diluted sodium hypochlorite (bleach) solution also helps to suppress bacterial growth. Nail extraction may be required in refractory cases.
For our patient, we prescribed ciprofloxacin 500 mg twice a day for 10 days, plus bleach soaks (one part bleach to 4 parts water) twice a day. We recommended that our patient wear gloves for household tasks that involved immersing her hands in water, and drying her finger with a hair dryer after bathing.
CORRESPONDENCE
David Gish, MD, University of Virginia Health System, 1215 Lee St. Charlottesville, VA 22908; [email protected].
A 34-year-old woman came to our clinic because she was concerned about her thumbnail, which had turned green. Although her finger didn’t hurt, she was bothered by its appearance. Several months earlier, the woman had sought care at a different clinic because the same nail had become brittle and come loose from the nail bed, which was spongy. The physician advised her that she had onychomycosis and prescribed ciclopirox lacquer, but it didn’t help.
Over the next 3 weeks, she noticed a faint green hue developing at the tip of the nail, which expanded and intensified in color (FIGURE). The patient was a mother who worked at home, washed dishes by hand daily, and bathed her children. Her past medical history was significant for type 1 diabetes mellitus and Hashimoto’s thyroiditis. She had no other symptoms.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Green nail syndrome caused by Pseudomonas aeruginosa
This patient had green nail syndrome (GNS), an infection of the nail bed caused by Pseudomonas aeruginosa. These bacteria produce pyocyanin, a blue-green pigment that discolors the nail.1 GNS often occurs in patients with prior nail problems, such as onychomycosis, onycholysis, trauma, chronic paronychia, or psoriasis.
Nail disease disrupts the integumentary barrier and allows a portal of entry for bacteria. Scanning electron microscopy of patients with GNS has shown that fungal infections create tunnel-like structures in the nail keratin, and P aeruginosa grows in these spaces.2 Nails with prior nail disease that are chronically exposed to moisture are at greatest risk of developing GNS,3,4 and it is typical for only one nail to be involved.5Pseudomonas is the most common bacterial infection of the nails, but is not well known because it is rarely reported and patients often don’t seek care.6
In our patient’s case, her prior onychomycosis helped to create a favorable environment for the growth of the bacteria. Onycholysis—characterized by separation of the nail plate from the nail bed—was also present in our patient, based on her description of a “spongy” nail bed and loose nail, allowing moisture and bacteria to infiltrate the space. Onycholysis is associated with hypothyroidism, which the patient also had.7 The frequent soaking of her hands during dishwashing and bathing her children helped to provide the moist environment in which Pseudomonas thrives.
As was the case in this patient, GNS is often painless, or may be accompanied by mild tenderness of the nail. Patients may seek treatment primarily for cosmetic reasons.
GNS can be diagnosed by clinical observation and characteristic pigmentation along with an appropriate patient history.4 Culture of the nail bed may be helpful if bacterial resistance or co-infection with fungal organisms is suspected.
Changes in nail color can be a sign of many conditions
Nail discoloration, or chromonychia, can present in a variety of colors. Nail findings may represent an isolated disease or provide an important clinical clue to other systemic diseases.8 The specific shade of discoloration helps to differentiate the underlying pathology.
Yellow nail syndrome. As the name implies, this syndrome typically causes yellow discoloration of the nail (although yellow-green is also possible). Yellow nail syndrome is believed to be due to microvascular permeability, which also accounts for its associated clinical triad: hypoalbuminemia, pleural effusion, and lymphedema. Yellow nail syndrome may be seen in patients with bronchiectasis, internal malignancies, immunodeficiency, and rheumatoid arthritis.8
Nail bed hematoma. Among the most common causes of nail discoloration, these lesions typically appear as reddish to reddish-black, depending on the age of the bleed, and will often have streaks at the distal margin of the lesion.9 Risk factors for hemorrhage include blood thinners and clotting disorders. Subungual hemorrhages that do not grow out with the nail, or that recur in the same place, may require biopsy.9
Subungual melanoma causes black-brown discoloration of the nails, and may form a longitudinal band in the nail.9 Longitudinal melanonychia is a common variant in African American individuals.10 Features that increase the likelihood of melanoma include a family history of melanoma, a sudden change in the appearance of the lesion, band width greater than 3 mm, pigment changes extending into the cuticle (known as Hutchinson’s sign), and nail plate disruption.
Dermoscopy, the technique of using surface microscopy to examine the skin, may be helpful in distinguishing nail lesions. (See a video on how to perform dermoscopy here: http://bit.ly/2pyJ3xN.)
Nonmelanocytic lesions tend to have homogeneously distributed pigment, while melanocytic lesions contain granules of pigment in cellular inclusions. Any suspicion of melanoma warrants a punch biopsy.11
Medication-induced effects. Minocycline may cause bluish nail discoloration similar to that produced by infection with P aeruginosa, but it is rare for only a single nail to be involved. In addition, pigmentation changes are often present elsewhere on the body, including the sclerae, teeth, and pinna.
Another medication known to color the nails blue is colloidal silver, which is still sold as a dietary supplement or homeopathic remedy to treat a wide range of ailments.6 (Of note: In 1999, the Food and Drug Administration issued a final rule saying that colloidal silver isn’t safe or effective for treating any disease or condition.12)
Glomus tumor. Another cause of blue nails is glomus tumors, relatively uncommon perivascular neoplasms that are typically found in the subungual region. These tumors are generally accompanied by localized tenderness, cold sensitivity, and paroxysms of excruciating pain that are disproportional to the size of the tumor.
Imaging studies may aid in the diagnosis, in addition to pathologic confirmation. Magnetic resonance imaging is the most sensitive imaging modality; if a glomus tumor is present, it most often appears as a well-circumscribed T2 hyperintense lesion.13
Exogenous pigmentation. Nails may become discolored due to exposure to various toxins or chemicals. Frequent culprits include eosin, methylene blue, henna, hair dye, and tobacco.9
Antibiotics and measures to keep the nail dry will help resolve infection
When chronic nail wetness is a contributing factor, treatment begins with measures to keep the nails dry. In addition, either topical or systemic antibiotics may be used to eradicate the infection. Topical applications with agents such as nadifloxacin have been shown to be effective in several case reports,3 but large-scale controlled trials are lacking. Fluoroquinolones are regarded as first-line systemic treatment.5 Briefly soaking the nail in a diluted sodium hypochlorite (bleach) solution also helps to suppress bacterial growth. Nail extraction may be required in refractory cases.
For our patient, we prescribed ciprofloxacin 500 mg twice a day for 10 days, plus bleach soaks (one part bleach to 4 parts water) twice a day. We recommended that our patient wear gloves for household tasks that involved immersing her hands in water, and drying her finger with a hair dryer after bathing.
CORRESPONDENCE
David Gish, MD, University of Virginia Health System, 1215 Lee St. Charlottesville, VA 22908; [email protected].
1. Greene SL, Su WP, Muller SA. Pseudomonas aeruginosa infections of the skin. Am Fam Physician. 1984;29:193-200.
2. de Almeida HL Jr, Duquia RP, de Castro LA, et al. Scanning electron microscopy of the green nail. Int J Dermatol. 2010;49:962-963.
3. Hengge UR, Bardeli V. Images in clinical medicine. Green nails. N Engl J Med. 2009;360:1125.
4. Chiriac A, Brzezinski P, Foia L, et al. Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons. Clin Interv Aging. 2015;10:265-267.
5. Müller S, Ebnöther M, Itin P. Green nail syndrome (Pseudomonas aeruginosa nail infection): Two cases successfully treated with topical nadifloxacin, an acne medication. Case Rep Dermatol. 2014;6:180-184.
6. Raam R, DeClerck B, Jhun P, et al. That’s some weird nail polish you got there! Ann Emerg Med. 2015;66:585-588.
7. Gregoriou S, Argyriou G, Larios G, et al. Nail disorders and systemic disease: what the nails tell us. J Fam Pract. 2008;57:509-514.
8. Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician. 2004;69:1417-1424.
9. Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol. 2007;56:835-847.
10. Buka R, Friedman KA, Phelps RG, et al. Childhood longitudinal melanonychia: case reports and review of the literature. Mt Sinai J Med. 2001;68:331-335.
11. Tully AS, Trayes KP, Studdiford JS. Evaluation of nail abnormalities. Am Fam Physician. 2012;85:779-787.
12. US Food and Drug Administration. Over-the-counter drug products containing colloidal silver ingredients or silver salts. 1999. Available at: https://www.fda.gov/ohrms/dockets/98fr/081799a.txt. Accessed April 11, 2017.
13. Glazebrook KN, Laundre BJ, Schiefer TK, et al. Imaging features of glomus tumors. Skeletal Radiol. 2011;40:855-862.
1. Greene SL, Su WP, Muller SA. Pseudomonas aeruginosa infections of the skin. Am Fam Physician. 1984;29:193-200.
2. de Almeida HL Jr, Duquia RP, de Castro LA, et al. Scanning electron microscopy of the green nail. Int J Dermatol. 2010;49:962-963.
3. Hengge UR, Bardeli V. Images in clinical medicine. Green nails. N Engl J Med. 2009;360:1125.
4. Chiriac A, Brzezinski P, Foia L, et al. Chloronychia: green nail syndrome caused by Pseudomonas aeruginosa in elderly persons. Clin Interv Aging. 2015;10:265-267.
5. Müller S, Ebnöther M, Itin P. Green nail syndrome (Pseudomonas aeruginosa nail infection): Two cases successfully treated with topical nadifloxacin, an acne medication. Case Rep Dermatol. 2014;6:180-184.
6. Raam R, DeClerck B, Jhun P, et al. That’s some weird nail polish you got there! Ann Emerg Med. 2015;66:585-588.
7. Gregoriou S, Argyriou G, Larios G, et al. Nail disorders and systemic disease: what the nails tell us. J Fam Pract. 2008;57:509-514.
8. Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: clues to systemic disease. Am Fam Physician. 2004;69:1417-1424.
9. Braun RP, Baran R, Le Gal FA, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol. 2007;56:835-847.
10. Buka R, Friedman KA, Phelps RG, et al. Childhood longitudinal melanonychia: case reports and review of the literature. Mt Sinai J Med. 2001;68:331-335.
11. Tully AS, Trayes KP, Studdiford JS. Evaluation of nail abnormalities. Am Fam Physician. 2012;85:779-787.
12. US Food and Drug Administration. Over-the-counter drug products containing colloidal silver ingredients or silver salts. 1999. Available at: https://www.fda.gov/ohrms/dockets/98fr/081799a.txt. Accessed April 11, 2017.
13. Glazebrook KN, Laundre BJ, Schiefer TK, et al. Imaging features of glomus tumors. Skeletal Radiol. 2011;40:855-862.