User login
Acne fulminans is an uncommon and debilitating disease that presents as an acute eruption of nodular and ulcerative acne lesions with associated systemic symptoms.1,2 Although its underlying pathophysiology is not well understood, it occurs commonly during treatment of severe acne (eg, acne conglobata) with isotretinoin in young adolescent males.3 Zaba et al4 indicated that an underlying genetic disorder, increase in serum androgen levels, or presence of autoimmune disorders may contribute to the development of acne fulminans.
Isotretinoin and doxycycline also can potentially induce development of neutrophilic dermatoses including Sweet syndrome and pyoderma gangrenosum in patients with severe acne lesions, which can be clinically similar to an acne fulminans eruption. The neutrophilic dermatosis is characterized by the acute appearance of painful ulcerative papulonodules accompanied by systemic symptoms including fever and leukocytosis.
Case Report
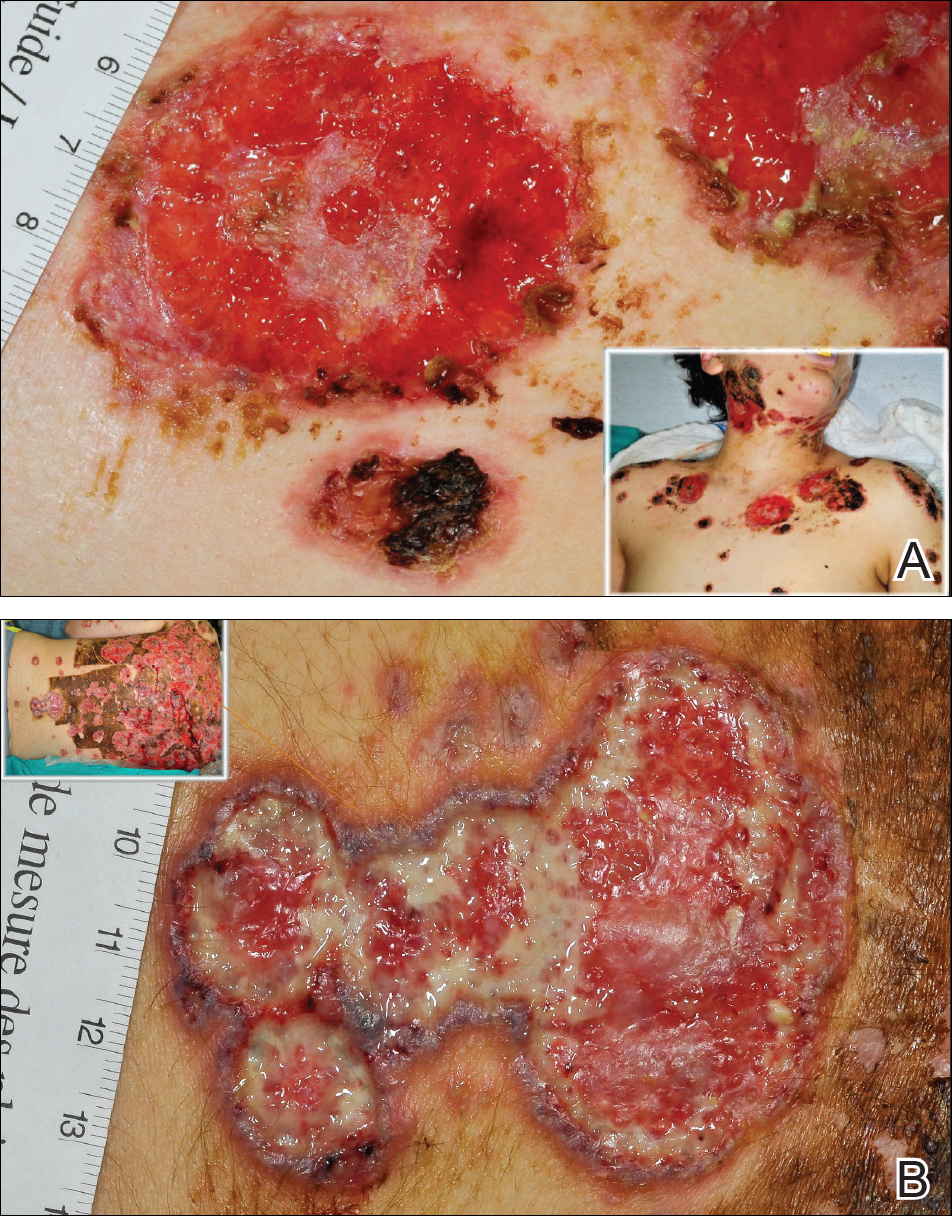
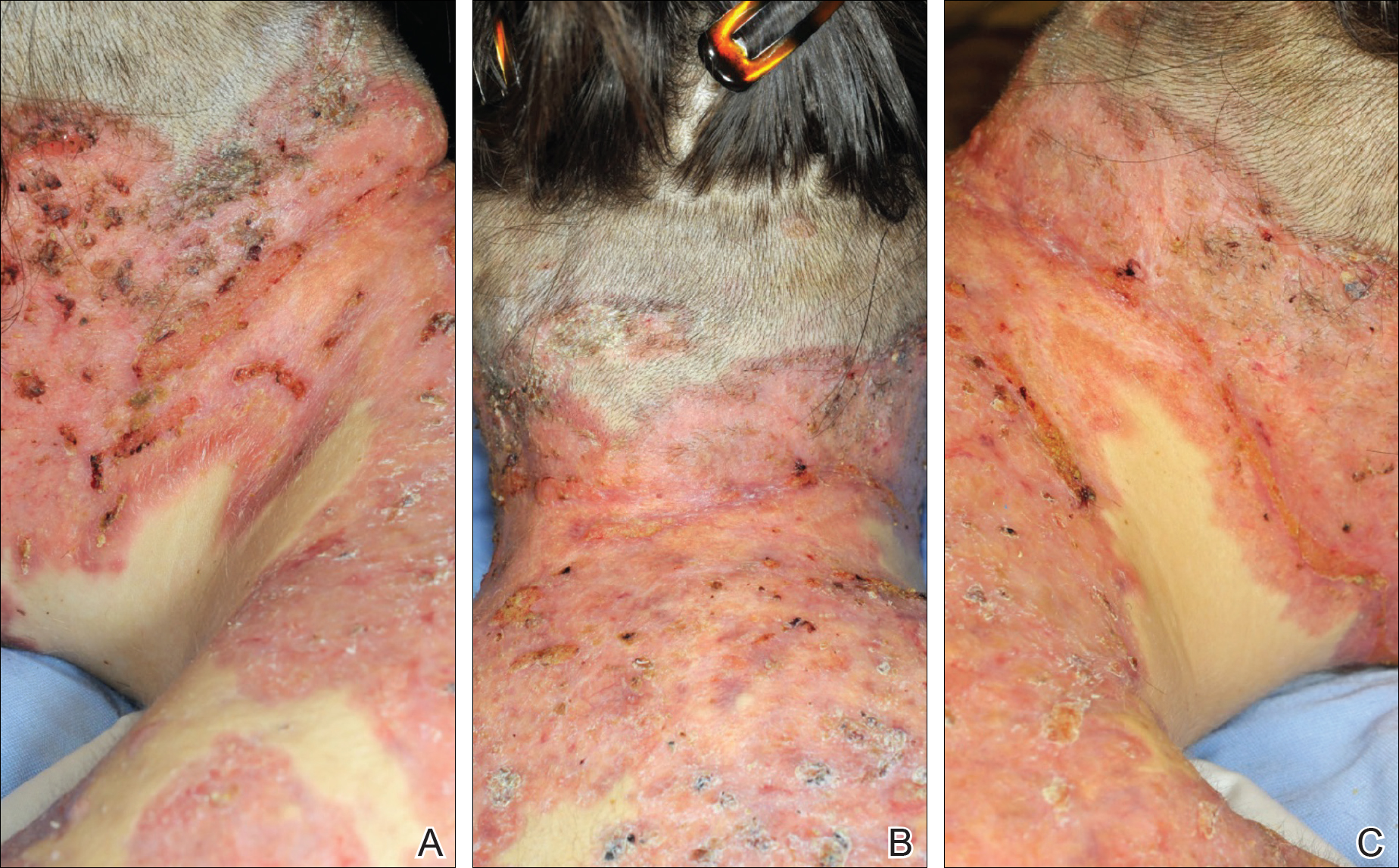
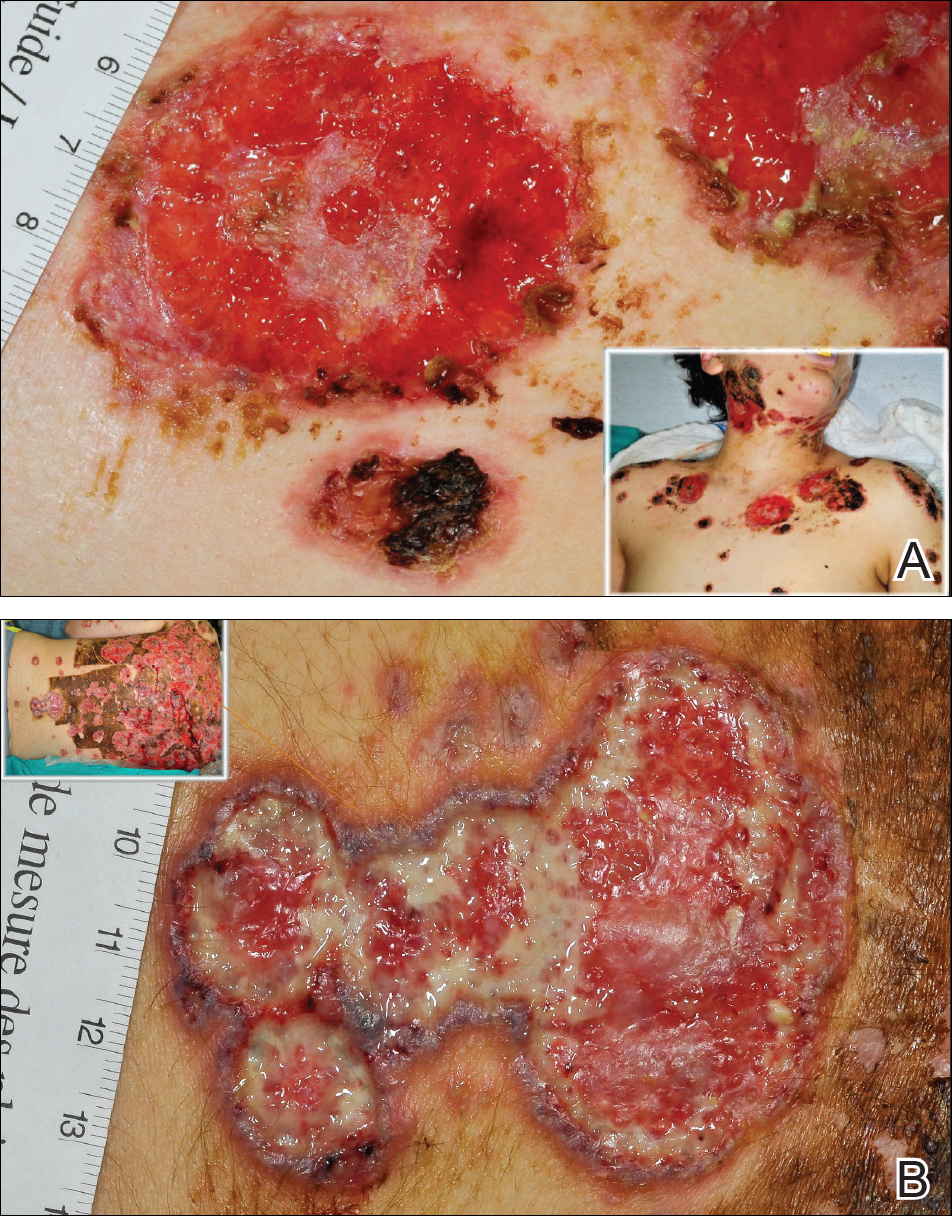
A 13-year-old adolescent boy was initially assessed by his family physician 2 months prior and started on oral doxycycline 100 mg twice daily for acne conglobata on the back. Unfortunately, the acne lesions, especially those on the upper back (Figure 1), started getting worse after 1 month of treatment with doxycycline; thus, he subsequently was switched to oral isotretinoin 0.5 mg/kg once daily. Less than 2 weeks later, the acne lesions worsened, and the patient also developed severe generalized arthralgia, myalgia, and fever (>38.3°C). He acutely developed hundreds of ulcerative plaques covering the entire trunk, upper extremities, face, and neck.

He was admitted to the Stollery Children’s Hospital (Edmonton, Alberta, Canada) and was assessed by the dermatology, rheumatology, and general pediatric teams (Figure 2). He initially was investigated for the potential presence of autoinflammatory disorders, such as PAPA syndrome (pyogenic arthritis, pyoderma gangrenosum, acne) and SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, osteitis).

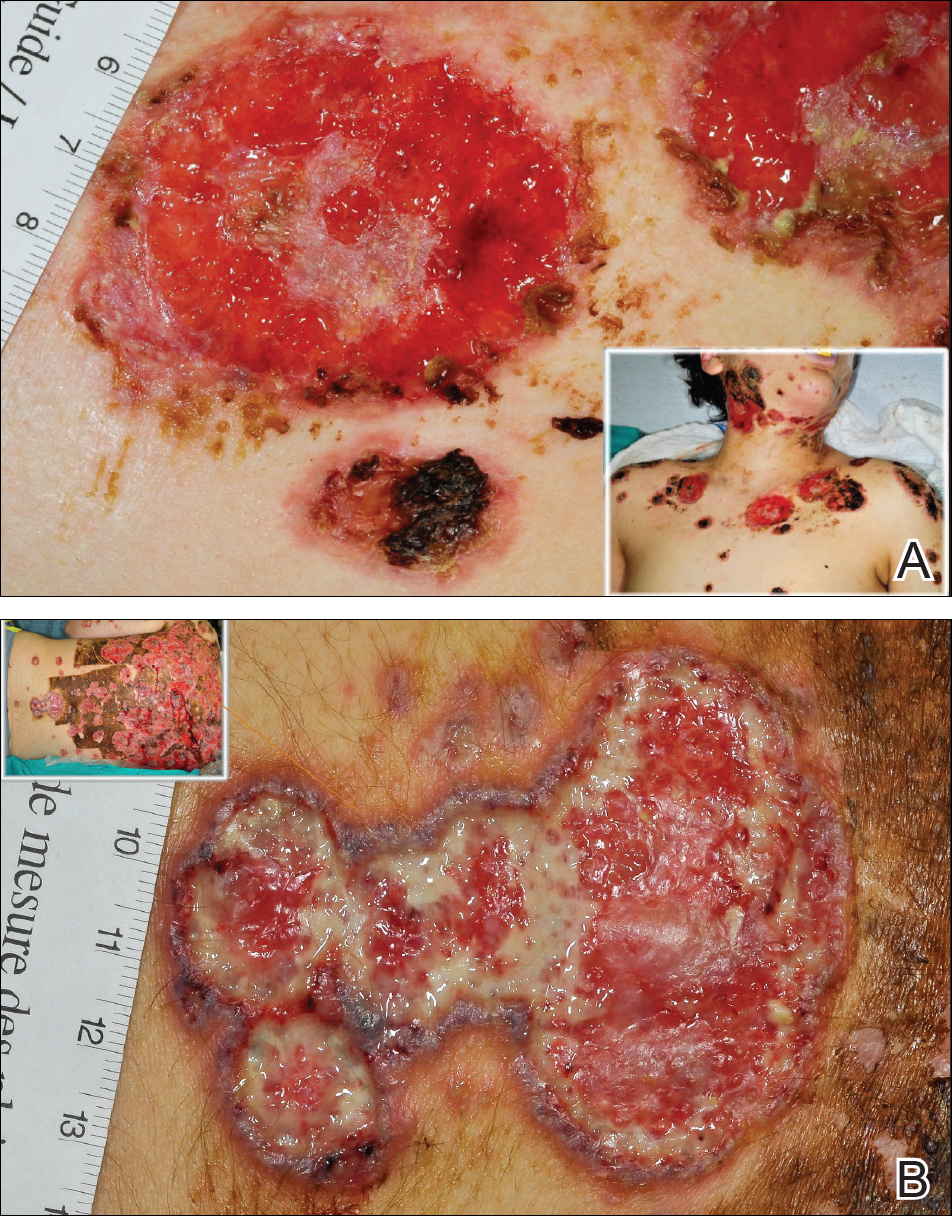
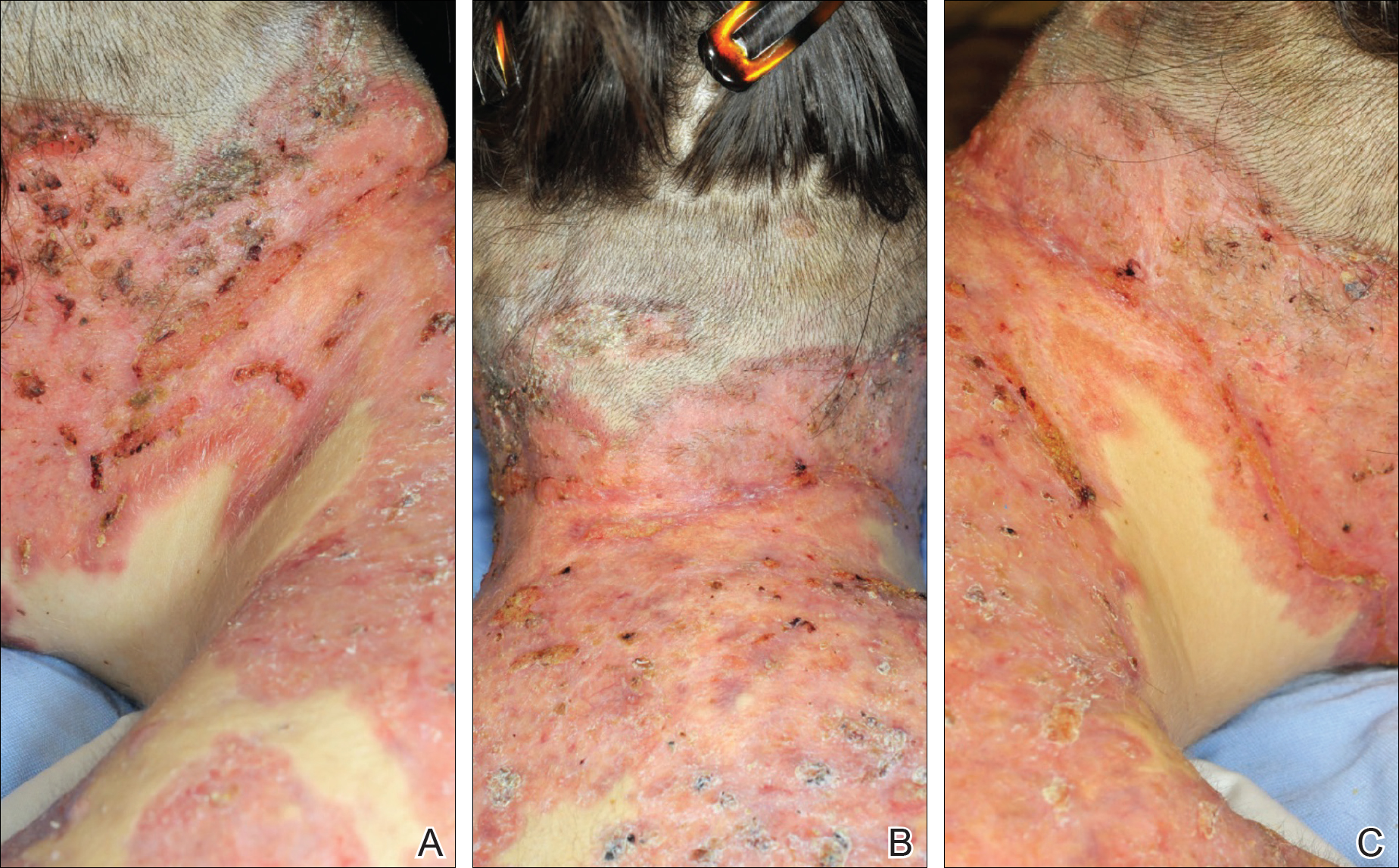
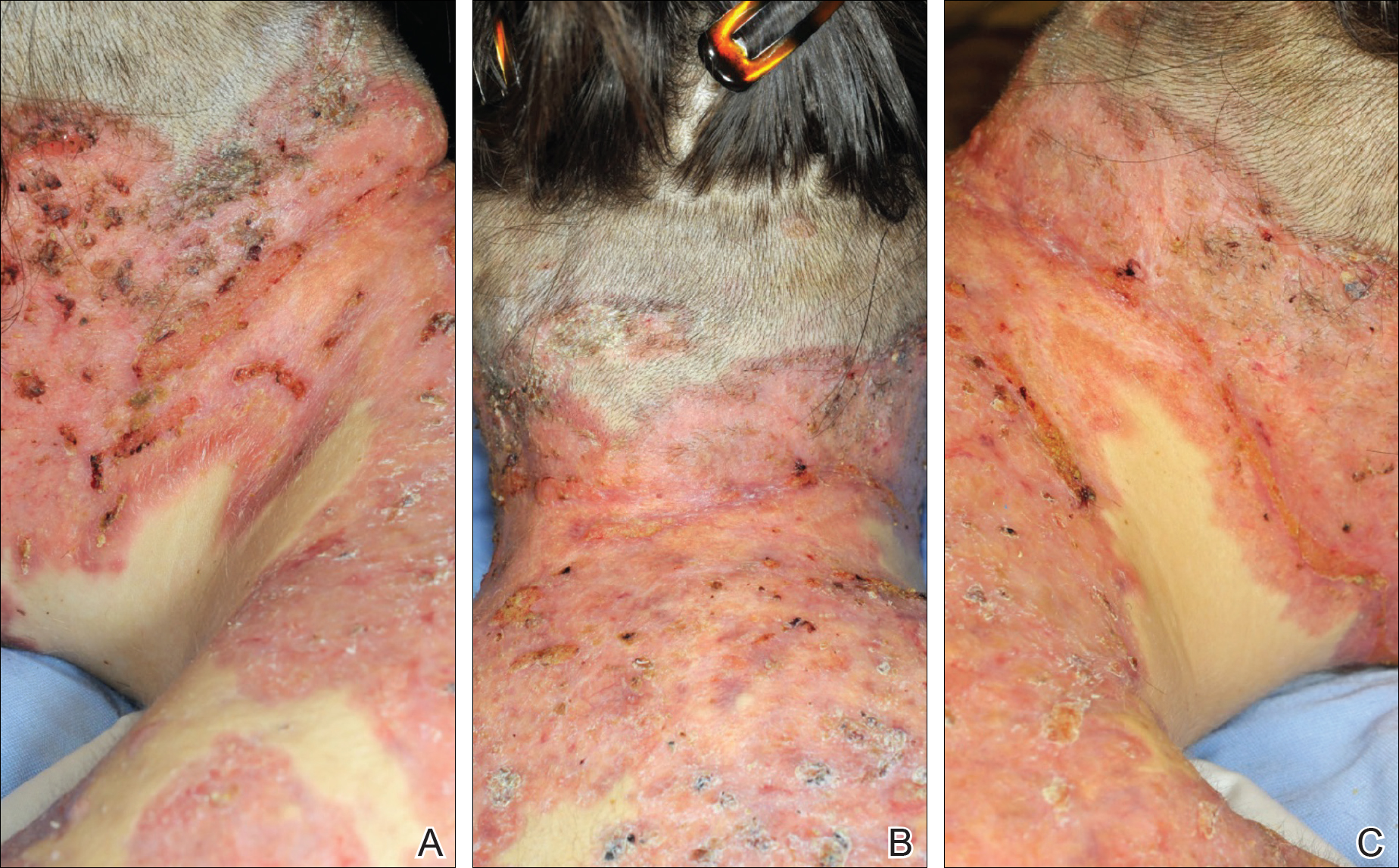
The patient initially was treated with prednisone 30 mg once daily for 3 weeks; dapsone 50 mg once daily and colchicine 0.6 mg twice daily were added while attempting to slowly wean off the prednisone (starting at 30 mg daily and reducing by 5 mg every other week). An attempt to discontinue the prednisone after 2 months was followed by immediate recurrence of the lesions (Figure 3), and the prednisone was restarted for another month. He was subsequently switched to oral cyclosporine 5 mg/kg once daily and achieved considerable improvement in his skin condition (Figure 4).
Comment
Thomson and Cunliffe5 reported a small case series of 11 young male patients with a mean age of 17 years who presented with severe worsening of their acne eruptions after taking isotretinoin, and they all responded well to an oral steroid. In another study, Bottomley and Cunliffe6 indicated that young male patients with notable acne on the trunk who are receiving a minimum dose of 0.5 mg/kg once daily of isotretinoin are at considerable risk for severe worsening of their skin condition.
Although severe worsening of acne lesions leading to acne fulminans or neutrophilic dermatosis secondary to isotretinoin or even doxycycline use is a rare entity, precautionary steps should be taken prior to treating acne conglobata patients with these agents. A review of PubMed articles indexed for MEDLINE using the terms acne, acne conglobata, and doxycycline revealed 2 prior cases of worsening acne in patients treated with doxycycline.7,8 Therefore, any patient presenting with acute worsening of an acne eruption while being treated with isotretinoin or doxycycline needs to be assessed for potential diagnosis of drug-induced acne fulminans or neutrophilic dermatosis.
It has been clearly documented in the literature that both doxycycline and isotretinoin can induce or exacerbate neutrophilic dermatoses in patients with severe underlying acne.6-8 The presentation may be mistaken for worsening acne, leading to inappropriate initiation or increase in the dose of isotretinoin therapy and worsening of the disease with potentially devastating disfiguring consequences. These patients tend to respond well to high-dose oral steroids alone or in combination with dapsone. A slow steroid taper over several months is recommended due to a high tendency for recurrence.
- Grando LR, Leite OG, Cestari TF. Pseudo-acne fulminans associated with oral isotretinoin. An Bras Dermatol. 2014;89:657-659.
- Burns RE, Colville JM. Acne conglobata with septicemia. Arch Dermatol. 1959;79:361-363.
- Karvonen SL. Acne fulminans: report of clinical findings and treatment of twenty-four patients. J Am Acad Dermatol. 1993;28:572-579.
- Zaba R, Schwartz R, Jarmuda S, et al. Acne fulminans: explosive systemic form of acne. J Eur Acad Dermatol Venereol. 2011;25:501-507.
- Thomson KF, Cunliffe WJ. Acne fulminans ‘sine fulminans.’ Clin Exp Dermatol. 2000;25:299-301.
- Bottomley WW, Cunliffe WJ. Severe flares of acne following isotretinoin: large closed comedones (macrocomedones) are a risk factor. Acta Derm Venereol. 1993;73:74.
- Weinstein M, Laxer R, Debosz J, et al. Doxycycline-induced cutaneous inflammation with systemic symptoms in a patient with acne vulgaris. J Cutan Med Surg. 2013;17:283-286.
- Yeo PM, Koh WL, Ang CC, et al. Paradoxical worsening of truncal acne with doxycycline. Ann Acad Med Singapore. 2016;45:430-431.
Acne fulminans is an uncommon and debilitating disease that presents as an acute eruption of nodular and ulcerative acne lesions with associated systemic symptoms.1,2 Although its underlying pathophysiology is not well understood, it occurs commonly during treatment of severe acne (eg, acne conglobata) with isotretinoin in young adolescent males.3 Zaba et al4 indicated that an underlying genetic disorder, increase in serum androgen levels, or presence of autoimmune disorders may contribute to the development of acne fulminans.
Isotretinoin and doxycycline also can potentially induce development of neutrophilic dermatoses including Sweet syndrome and pyoderma gangrenosum in patients with severe acne lesions, which can be clinically similar to an acne fulminans eruption. The neutrophilic dermatosis is characterized by the acute appearance of painful ulcerative papulonodules accompanied by systemic symptoms including fever and leukocytosis.
Case Report
A 13-year-old adolescent boy was initially assessed by his family physician 2 months prior and started on oral doxycycline 100 mg twice daily for acne conglobata on the back. Unfortunately, the acne lesions, especially those on the upper back (Figure 1), started getting worse after 1 month of treatment with doxycycline; thus, he subsequently was switched to oral isotretinoin 0.5 mg/kg once daily. Less than 2 weeks later, the acne lesions worsened, and the patient also developed severe generalized arthralgia, myalgia, and fever (>38.3°C). He acutely developed hundreds of ulcerative plaques covering the entire trunk, upper extremities, face, and neck.

He was admitted to the Stollery Children’s Hospital (Edmonton, Alberta, Canada) and was assessed by the dermatology, rheumatology, and general pediatric teams (Figure 2). He initially was investigated for the potential presence of autoinflammatory disorders, such as PAPA syndrome (pyogenic arthritis, pyoderma gangrenosum, acne) and SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, osteitis).

The patient initially was treated with prednisone 30 mg once daily for 3 weeks; dapsone 50 mg once daily and colchicine 0.6 mg twice daily were added while attempting to slowly wean off the prednisone (starting at 30 mg daily and reducing by 5 mg every other week). An attempt to discontinue the prednisone after 2 months was followed by immediate recurrence of the lesions (Figure 3), and the prednisone was restarted for another month. He was subsequently switched to oral cyclosporine 5 mg/kg once daily and achieved considerable improvement in his skin condition (Figure 4).
Comment
Thomson and Cunliffe5 reported a small case series of 11 young male patients with a mean age of 17 years who presented with severe worsening of their acne eruptions after taking isotretinoin, and they all responded well to an oral steroid. In another study, Bottomley and Cunliffe6 indicated that young male patients with notable acne on the trunk who are receiving a minimum dose of 0.5 mg/kg once daily of isotretinoin are at considerable risk for severe worsening of their skin condition.
Although severe worsening of acne lesions leading to acne fulminans or neutrophilic dermatosis secondary to isotretinoin or even doxycycline use is a rare entity, precautionary steps should be taken prior to treating acne conglobata patients with these agents. A review of PubMed articles indexed for MEDLINE using the terms acne, acne conglobata, and doxycycline revealed 2 prior cases of worsening acne in patients treated with doxycycline.7,8 Therefore, any patient presenting with acute worsening of an acne eruption while being treated with isotretinoin or doxycycline needs to be assessed for potential diagnosis of drug-induced acne fulminans or neutrophilic dermatosis.
It has been clearly documented in the literature that both doxycycline and isotretinoin can induce or exacerbate neutrophilic dermatoses in patients with severe underlying acne.6-8 The presentation may be mistaken for worsening acne, leading to inappropriate initiation or increase in the dose of isotretinoin therapy and worsening of the disease with potentially devastating disfiguring consequences. These patients tend to respond well to high-dose oral steroids alone or in combination with dapsone. A slow steroid taper over several months is recommended due to a high tendency for recurrence.
Acne fulminans is an uncommon and debilitating disease that presents as an acute eruption of nodular and ulcerative acne lesions with associated systemic symptoms.1,2 Although its underlying pathophysiology is not well understood, it occurs commonly during treatment of severe acne (eg, acne conglobata) with isotretinoin in young adolescent males.3 Zaba et al4 indicated that an underlying genetic disorder, increase in serum androgen levels, or presence of autoimmune disorders may contribute to the development of acne fulminans.
Isotretinoin and doxycycline also can potentially induce development of neutrophilic dermatoses including Sweet syndrome and pyoderma gangrenosum in patients with severe acne lesions, which can be clinically similar to an acne fulminans eruption. The neutrophilic dermatosis is characterized by the acute appearance of painful ulcerative papulonodules accompanied by systemic symptoms including fever and leukocytosis.
Case Report
A 13-year-old adolescent boy was initially assessed by his family physician 2 months prior and started on oral doxycycline 100 mg twice daily for acne conglobata on the back. Unfortunately, the acne lesions, especially those on the upper back (Figure 1), started getting worse after 1 month of treatment with doxycycline; thus, he subsequently was switched to oral isotretinoin 0.5 mg/kg once daily. Less than 2 weeks later, the acne lesions worsened, and the patient also developed severe generalized arthralgia, myalgia, and fever (>38.3°C). He acutely developed hundreds of ulcerative plaques covering the entire trunk, upper extremities, face, and neck.

He was admitted to the Stollery Children’s Hospital (Edmonton, Alberta, Canada) and was assessed by the dermatology, rheumatology, and general pediatric teams (Figure 2). He initially was investigated for the potential presence of autoinflammatory disorders, such as PAPA syndrome (pyogenic arthritis, pyoderma gangrenosum, acne) and SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, osteitis).

The patient initially was treated with prednisone 30 mg once daily for 3 weeks; dapsone 50 mg once daily and colchicine 0.6 mg twice daily were added while attempting to slowly wean off the prednisone (starting at 30 mg daily and reducing by 5 mg every other week). An attempt to discontinue the prednisone after 2 months was followed by immediate recurrence of the lesions (Figure 3), and the prednisone was restarted for another month. He was subsequently switched to oral cyclosporine 5 mg/kg once daily and achieved considerable improvement in his skin condition (Figure 4).
Comment
Thomson and Cunliffe5 reported a small case series of 11 young male patients with a mean age of 17 years who presented with severe worsening of their acne eruptions after taking isotretinoin, and they all responded well to an oral steroid. In another study, Bottomley and Cunliffe6 indicated that young male patients with notable acne on the trunk who are receiving a minimum dose of 0.5 mg/kg once daily of isotretinoin are at considerable risk for severe worsening of their skin condition.
Although severe worsening of acne lesions leading to acne fulminans or neutrophilic dermatosis secondary to isotretinoin or even doxycycline use is a rare entity, precautionary steps should be taken prior to treating acne conglobata patients with these agents. A review of PubMed articles indexed for MEDLINE using the terms acne, acne conglobata, and doxycycline revealed 2 prior cases of worsening acne in patients treated with doxycycline.7,8 Therefore, any patient presenting with acute worsening of an acne eruption while being treated with isotretinoin or doxycycline needs to be assessed for potential diagnosis of drug-induced acne fulminans or neutrophilic dermatosis.
It has been clearly documented in the literature that both doxycycline and isotretinoin can induce or exacerbate neutrophilic dermatoses in patients with severe underlying acne.6-8 The presentation may be mistaken for worsening acne, leading to inappropriate initiation or increase in the dose of isotretinoin therapy and worsening of the disease with potentially devastating disfiguring consequences. These patients tend to respond well to high-dose oral steroids alone or in combination with dapsone. A slow steroid taper over several months is recommended due to a high tendency for recurrence.
- Grando LR, Leite OG, Cestari TF. Pseudo-acne fulminans associated with oral isotretinoin. An Bras Dermatol. 2014;89:657-659.
- Burns RE, Colville JM. Acne conglobata with septicemia. Arch Dermatol. 1959;79:361-363.
- Karvonen SL. Acne fulminans: report of clinical findings and treatment of twenty-four patients. J Am Acad Dermatol. 1993;28:572-579.
- Zaba R, Schwartz R, Jarmuda S, et al. Acne fulminans: explosive systemic form of acne. J Eur Acad Dermatol Venereol. 2011;25:501-507.
- Thomson KF, Cunliffe WJ. Acne fulminans ‘sine fulminans.’ Clin Exp Dermatol. 2000;25:299-301.
- Bottomley WW, Cunliffe WJ. Severe flares of acne following isotretinoin: large closed comedones (macrocomedones) are a risk factor. Acta Derm Venereol. 1993;73:74.
- Weinstein M, Laxer R, Debosz J, et al. Doxycycline-induced cutaneous inflammation with systemic symptoms in a patient with acne vulgaris. J Cutan Med Surg. 2013;17:283-286.
- Yeo PM, Koh WL, Ang CC, et al. Paradoxical worsening of truncal acne with doxycycline. Ann Acad Med Singapore. 2016;45:430-431.
- Grando LR, Leite OG, Cestari TF. Pseudo-acne fulminans associated with oral isotretinoin. An Bras Dermatol. 2014;89:657-659.
- Burns RE, Colville JM. Acne conglobata with septicemia. Arch Dermatol. 1959;79:361-363.
- Karvonen SL. Acne fulminans: report of clinical findings and treatment of twenty-four patients. J Am Acad Dermatol. 1993;28:572-579.
- Zaba R, Schwartz R, Jarmuda S, et al. Acne fulminans: explosive systemic form of acne. J Eur Acad Dermatol Venereol. 2011;25:501-507.
- Thomson KF, Cunliffe WJ. Acne fulminans ‘sine fulminans.’ Clin Exp Dermatol. 2000;25:299-301.
- Bottomley WW, Cunliffe WJ. Severe flares of acne following isotretinoin: large closed comedones (macrocomedones) are a risk factor. Acta Derm Venereol. 1993;73:74.
- Weinstein M, Laxer R, Debosz J, et al. Doxycycline-induced cutaneous inflammation with systemic symptoms in a patient with acne vulgaris. J Cutan Med Surg. 2013;17:283-286.
- Yeo PM, Koh WL, Ang CC, et al. Paradoxical worsening of truncal acne with doxycycline. Ann Acad Med Singapore. 2016;45:430-431.
Resident Pearl
- Doxycycline and isotretinoin have been widely used for treatment of inflammatory and nodulocystic acne. Although outstanding results can be achieved, paradoxical worsening of acne while starting these medications has been described. In patients with severe acne (ie, acne conglobata), initiation of doxycycline and especially isotretinoin at regular dosages as the sole treatment can impose devastating risks on the patient. These patients are best treated with a combination of low-dose isotretinoin (at the beginning) with a moderate dose of steroids, which should be gradually tapered while the isotretinoin dose is increased to 0.5 to 1 mg/kg once daily.
