User login
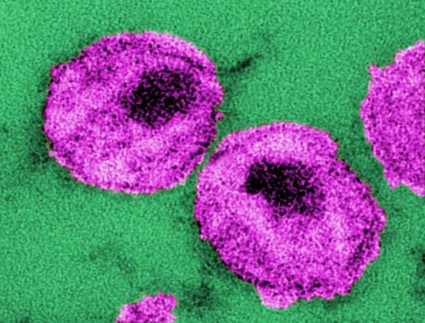
New federal guidelines outline steps to prevent infection in HIV-negative individuals at high risk of acquiring HIV through heterosexual sex.
The Centers for Disease Control and Prevention issued the interim recommendations pending the debut of a more complete set of HIV prevention guidelines both for heterosexuals and men who have sex with men (MSM).
The guidance comes on the heels of a new drug approval for pre-exposure prophylaxis (PrEP). In July, the Food and Drug Administration approved Truvada, the combination of tenofovir disoproxil fumarate plus emtricitabine (TDF/FTC), for PrEP in HIV-negative men and women who are at high risk for HIV acquisition through sexual intercourse.
Previous CDC guidance in January 2011 addressed PrEP in MSM (MMWR 2011;60:65-8).
The latest CDC document specifically addresses the use of PrEP in individuals who are at risk via heterosexual sex (MMWR 2012;61:586-9). The recommendations include new data about PrEP among heterosexual men and women (N. Engl. J. Med. 2012;367:399-434), as well as new information about pregnancy and other safety issues.
Both interim documents will remain valid until the CDC and other public health agencies complete a comprehensive set of HIV prevention recommendations on PrEP in both MSM and heterosexually active adults at high risk for HIV acquisition, the CDC said.
There are several new recommendations for initiating PrEP in individuals who are at very high risk for acquisition of HIV via penile-vaginal sex with a known HIV-positive partner:
• Prior to initiation: Confirm that the person is HIV-negative immediately before initiating TDF/FTC. Determine if the HIV-infected partner is receiving antiretroviral therapy, and if not, assist with a patient’s transition to care. Screen for hepatitis B and other sexually transmitted infections (STIs) and treat any that are detected. Check creatinine clearance, confirming that the calculated value is 60 mL/min or greater.
Determine if women are planning to become pregnant, are currently pregnant, or are breastfeeding. Women should be advised that PrEP safety during pregnancy has not been fully assessed, but that no harm has been reported. PrEP should not be prescribed for women who are breastfeeding.
• Beginning the PrEP regimen: Prescribe one Truvada tablet daily, with no more than a 90-day supply, renewable only after HIV testing confirms that patient remains HIV uninfected. For women, ensure that a pregnancy test is negative or, if pregnant, that the patient has been informed about PrEP use during pregnancy. Provide risk reduction and PrEP medication-adherence counseling and condoms.
• Follow-up during PrEP: Every 2-3 months, perform an HIV test and a pregnancy test for women, assess risk behaviors and STI symptoms, and test and treat if present. Counsel the individual regarding medication adherence, risk reduction, and condom use. Check serum creatinine and calculate creatinine clearance 3 months after initiation, then every 6 months while on PrEP medication. Test for bacterial STIs every 6 months, regardless of symptoms.
• Discontinuing PrEP: This may be necessary because of patient requests, safety concerns, or acquisition of HIV infection. If HIV status is unknown, a test should be performed. If a patient is HIV-positive, link the patient to HIV care. If active hepatitis B infection is diagnosed, consider continuing medication for that infection. If the individual is pregnant, communicate and coordinate with the prenatal-care provider about the patient’s PrEP use.
New federal guidelines outline steps to prevent infection in HIV-negative individuals at high risk of acquiring HIV through heterosexual sex.
The Centers for Disease Control and Prevention issued the interim recommendations pending the debut of a more complete set of HIV prevention guidelines both for heterosexuals and men who have sex with men (MSM).
The guidance comes on the heels of a new drug approval for pre-exposure prophylaxis (PrEP). In July, the Food and Drug Administration approved Truvada, the combination of tenofovir disoproxil fumarate plus emtricitabine (TDF/FTC), for PrEP in HIV-negative men and women who are at high risk for HIV acquisition through sexual intercourse.
Previous CDC guidance in January 2011 addressed PrEP in MSM (MMWR 2011;60:65-8).
The latest CDC document specifically addresses the use of PrEP in individuals who are at risk via heterosexual sex (MMWR 2012;61:586-9). The recommendations include new data about PrEP among heterosexual men and women (N. Engl. J. Med. 2012;367:399-434), as well as new information about pregnancy and other safety issues.
Both interim documents will remain valid until the CDC and other public health agencies complete a comprehensive set of HIV prevention recommendations on PrEP in both MSM and heterosexually active adults at high risk for HIV acquisition, the CDC said.
There are several new recommendations for initiating PrEP in individuals who are at very high risk for acquisition of HIV via penile-vaginal sex with a known HIV-positive partner:
• Prior to initiation: Confirm that the person is HIV-negative immediately before initiating TDF/FTC. Determine if the HIV-infected partner is receiving antiretroviral therapy, and if not, assist with a patient’s transition to care. Screen for hepatitis B and other sexually transmitted infections (STIs) and treat any that are detected. Check creatinine clearance, confirming that the calculated value is 60 mL/min or greater.
Determine if women are planning to become pregnant, are currently pregnant, or are breastfeeding. Women should be advised that PrEP safety during pregnancy has not been fully assessed, but that no harm has been reported. PrEP should not be prescribed for women who are breastfeeding.
• Beginning the PrEP regimen: Prescribe one Truvada tablet daily, with no more than a 90-day supply, renewable only after HIV testing confirms that patient remains HIV uninfected. For women, ensure that a pregnancy test is negative or, if pregnant, that the patient has been informed about PrEP use during pregnancy. Provide risk reduction and PrEP medication-adherence counseling and condoms.
• Follow-up during PrEP: Every 2-3 months, perform an HIV test and a pregnancy test for women, assess risk behaviors and STI symptoms, and test and treat if present. Counsel the individual regarding medication adherence, risk reduction, and condom use. Check serum creatinine and calculate creatinine clearance 3 months after initiation, then every 6 months while on PrEP medication. Test for bacterial STIs every 6 months, regardless of symptoms.
• Discontinuing PrEP: This may be necessary because of patient requests, safety concerns, or acquisition of HIV infection. If HIV status is unknown, a test should be performed. If a patient is HIV-positive, link the patient to HIV care. If active hepatitis B infection is diagnosed, consider continuing medication for that infection. If the individual is pregnant, communicate and coordinate with the prenatal-care provider about the patient’s PrEP use.
New federal guidelines outline steps to prevent infection in HIV-negative individuals at high risk of acquiring HIV through heterosexual sex.
The Centers for Disease Control and Prevention issued the interim recommendations pending the debut of a more complete set of HIV prevention guidelines both for heterosexuals and men who have sex with men (MSM).
The guidance comes on the heels of a new drug approval for pre-exposure prophylaxis (PrEP). In July, the Food and Drug Administration approved Truvada, the combination of tenofovir disoproxil fumarate plus emtricitabine (TDF/FTC), for PrEP in HIV-negative men and women who are at high risk for HIV acquisition through sexual intercourse.
Previous CDC guidance in January 2011 addressed PrEP in MSM (MMWR 2011;60:65-8).
The latest CDC document specifically addresses the use of PrEP in individuals who are at risk via heterosexual sex (MMWR 2012;61:586-9). The recommendations include new data about PrEP among heterosexual men and women (N. Engl. J. Med. 2012;367:399-434), as well as new information about pregnancy and other safety issues.
Both interim documents will remain valid until the CDC and other public health agencies complete a comprehensive set of HIV prevention recommendations on PrEP in both MSM and heterosexually active adults at high risk for HIV acquisition, the CDC said.
There are several new recommendations for initiating PrEP in individuals who are at very high risk for acquisition of HIV via penile-vaginal sex with a known HIV-positive partner:
• Prior to initiation: Confirm that the person is HIV-negative immediately before initiating TDF/FTC. Determine if the HIV-infected partner is receiving antiretroviral therapy, and if not, assist with a patient’s transition to care. Screen for hepatitis B and other sexually transmitted infections (STIs) and treat any that are detected. Check creatinine clearance, confirming that the calculated value is 60 mL/min or greater.
Determine if women are planning to become pregnant, are currently pregnant, or are breastfeeding. Women should be advised that PrEP safety during pregnancy has not been fully assessed, but that no harm has been reported. PrEP should not be prescribed for women who are breastfeeding.
• Beginning the PrEP regimen: Prescribe one Truvada tablet daily, with no more than a 90-day supply, renewable only after HIV testing confirms that patient remains HIV uninfected. For women, ensure that a pregnancy test is negative or, if pregnant, that the patient has been informed about PrEP use during pregnancy. Provide risk reduction and PrEP medication-adherence counseling and condoms.
• Follow-up during PrEP: Every 2-3 months, perform an HIV test and a pregnancy test for women, assess risk behaviors and STI symptoms, and test and treat if present. Counsel the individual regarding medication adherence, risk reduction, and condom use. Check serum creatinine and calculate creatinine clearance 3 months after initiation, then every 6 months while on PrEP medication. Test for bacterial STIs every 6 months, regardless of symptoms.
• Discontinuing PrEP: This may be necessary because of patient requests, safety concerns, or acquisition of HIV infection. If HIV status is unknown, a test should be performed. If a patient is HIV-positive, link the patient to HIV care. If active hepatitis B infection is diagnosed, consider continuing medication for that infection. If the individual is pregnant, communicate and coordinate with the prenatal-care provider about the patient’s PrEP use.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT