User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Younger heart disease onset tied to higher dementia risk
TOPLINE:
, with the risk highest — at 36% — if onset is before age 45, results of a large observational study show.
METHODOLOGY:
- The study included 432,667 of the more than 500,000 participants in the UK Biobank, with a mean age of 56.9 years, 50,685 (11.7%) of whom had CHD and 50,445 had data on age at CHD onset.
- Researchers divided participants into three groups according to age at CHD onset (below 45 years, 45-59 years, and 60 years and older), and carried out a propensity score matching analysis.
- Outcomes included all-cause dementia, AD, and VD.
- Covariates included age, sex, race, educational level, body mass index, low-density lipoprotein cholesterol, smoking status, alcohol intake, exercise, depressed mood, hypertension, diabetes, statin use, and apolipoprotein E4 status.
TAKEAWAY:
- During a median follow-up of 12.8 years, researchers identified 5876 cases of all-cause dementia, 2540 cases of AD, and 1220 cases of VD.
- Fully adjusted models showed participants with CHD had significantly higher risks than those without CHD of developing all-cause dementia (hazard ratio [HR], 1.36; 95% CI, 1.28-1.45; P < .001), AD (HR, 1.13; 95% CI, 1.02-1.24; P = .019), and VD (HR, 1.78; 95% CI, 1.56-2.02; P < .001). The higher risk for VD suggests CHD has a more profound influence on neuropathologic changes involved in this dementia type, said the authors.
- Those with CHD diagnosed at a younger age had higher risks of developing dementia (HR per 10-year decrease in age, 1.25; 95% CI, 1.20-1.30 for all-cause dementia, 1.29; 95% CI, 1.20-1.38 for AD, and 1.22; 95% CI, 1.13-1.31 for VD; P for all < .001).
- Propensity score matching analysis showed patients with CHD had significantly higher risks for dementia compared with matched controls, with the highest risk seen in patients diagnosed before age 45 (HR, 2.40; 95% CI, 1.79-3.20; P < .001), followed by those diagnosed between 45 and 59 years (HR, 1.46; 95% CI, 1.32-1.62; P < .001) and at or above 60 years (HR, 1.11; 95% CI, 1.03-1.19; P = .005), with similar results for AD and VD.
IN PRACTICE:
The findings suggest “additional attention should be paid to the cognitive status of patients with CHD, especially the ones diagnosed with CHD at a young age,” the authors conclude, noting that “timely intervention, such as cognitive training, could be implemented once signs of cognitive deteriorations are detected.”
SOURCE:
The study was conducted by Jie Liang, BS, School of Nursing, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, and colleagues. It was published online on November 29, 2023, in the Journal of the American Heart Association.
LIMITATIONS:
As this is an observational study, it can’t conclude a causal relationship. Although the authors adjusted for many potential confounders, unknown risk factors that also contribute to CHD can’t be ruled out. As the study excluded 69,744 participants, selection bias is possible. The study included a mostly White population.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China, the Non-Profit Central Research Institute Fund of the Chinese Academy of Medical Sciences, and the China Medical Board. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, with the risk highest — at 36% — if onset is before age 45, results of a large observational study show.
METHODOLOGY:
- The study included 432,667 of the more than 500,000 participants in the UK Biobank, with a mean age of 56.9 years, 50,685 (11.7%) of whom had CHD and 50,445 had data on age at CHD onset.
- Researchers divided participants into three groups according to age at CHD onset (below 45 years, 45-59 years, and 60 years and older), and carried out a propensity score matching analysis.
- Outcomes included all-cause dementia, AD, and VD.
- Covariates included age, sex, race, educational level, body mass index, low-density lipoprotein cholesterol, smoking status, alcohol intake, exercise, depressed mood, hypertension, diabetes, statin use, and apolipoprotein E4 status.
TAKEAWAY:
- During a median follow-up of 12.8 years, researchers identified 5876 cases of all-cause dementia, 2540 cases of AD, and 1220 cases of VD.
- Fully adjusted models showed participants with CHD had significantly higher risks than those without CHD of developing all-cause dementia (hazard ratio [HR], 1.36; 95% CI, 1.28-1.45; P < .001), AD (HR, 1.13; 95% CI, 1.02-1.24; P = .019), and VD (HR, 1.78; 95% CI, 1.56-2.02; P < .001). The higher risk for VD suggests CHD has a more profound influence on neuropathologic changes involved in this dementia type, said the authors.
- Those with CHD diagnosed at a younger age had higher risks of developing dementia (HR per 10-year decrease in age, 1.25; 95% CI, 1.20-1.30 for all-cause dementia, 1.29; 95% CI, 1.20-1.38 for AD, and 1.22; 95% CI, 1.13-1.31 for VD; P for all < .001).
- Propensity score matching analysis showed patients with CHD had significantly higher risks for dementia compared with matched controls, with the highest risk seen in patients diagnosed before age 45 (HR, 2.40; 95% CI, 1.79-3.20; P < .001), followed by those diagnosed between 45 and 59 years (HR, 1.46; 95% CI, 1.32-1.62; P < .001) and at or above 60 years (HR, 1.11; 95% CI, 1.03-1.19; P = .005), with similar results for AD and VD.
IN PRACTICE:
The findings suggest “additional attention should be paid to the cognitive status of patients with CHD, especially the ones diagnosed with CHD at a young age,” the authors conclude, noting that “timely intervention, such as cognitive training, could be implemented once signs of cognitive deteriorations are detected.”
SOURCE:
The study was conducted by Jie Liang, BS, School of Nursing, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, and colleagues. It was published online on November 29, 2023, in the Journal of the American Heart Association.
LIMITATIONS:
As this is an observational study, it can’t conclude a causal relationship. Although the authors adjusted for many potential confounders, unknown risk factors that also contribute to CHD can’t be ruled out. As the study excluded 69,744 participants, selection bias is possible. The study included a mostly White population.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China, the Non-Profit Central Research Institute Fund of the Chinese Academy of Medical Sciences, and the China Medical Board. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, with the risk highest — at 36% — if onset is before age 45, results of a large observational study show.
METHODOLOGY:
- The study included 432,667 of the more than 500,000 participants in the UK Biobank, with a mean age of 56.9 years, 50,685 (11.7%) of whom had CHD and 50,445 had data on age at CHD onset.
- Researchers divided participants into three groups according to age at CHD onset (below 45 years, 45-59 years, and 60 years and older), and carried out a propensity score matching analysis.
- Outcomes included all-cause dementia, AD, and VD.
- Covariates included age, sex, race, educational level, body mass index, low-density lipoprotein cholesterol, smoking status, alcohol intake, exercise, depressed mood, hypertension, diabetes, statin use, and apolipoprotein E4 status.
TAKEAWAY:
- During a median follow-up of 12.8 years, researchers identified 5876 cases of all-cause dementia, 2540 cases of AD, and 1220 cases of VD.
- Fully adjusted models showed participants with CHD had significantly higher risks than those without CHD of developing all-cause dementia (hazard ratio [HR], 1.36; 95% CI, 1.28-1.45; P < .001), AD (HR, 1.13; 95% CI, 1.02-1.24; P = .019), and VD (HR, 1.78; 95% CI, 1.56-2.02; P < .001). The higher risk for VD suggests CHD has a more profound influence on neuropathologic changes involved in this dementia type, said the authors.
- Those with CHD diagnosed at a younger age had higher risks of developing dementia (HR per 10-year decrease in age, 1.25; 95% CI, 1.20-1.30 for all-cause dementia, 1.29; 95% CI, 1.20-1.38 for AD, and 1.22; 95% CI, 1.13-1.31 for VD; P for all < .001).
- Propensity score matching analysis showed patients with CHD had significantly higher risks for dementia compared with matched controls, with the highest risk seen in patients diagnosed before age 45 (HR, 2.40; 95% CI, 1.79-3.20; P < .001), followed by those diagnosed between 45 and 59 years (HR, 1.46; 95% CI, 1.32-1.62; P < .001) and at or above 60 years (HR, 1.11; 95% CI, 1.03-1.19; P = .005), with similar results for AD and VD.
IN PRACTICE:
The findings suggest “additional attention should be paid to the cognitive status of patients with CHD, especially the ones diagnosed with CHD at a young age,” the authors conclude, noting that “timely intervention, such as cognitive training, could be implemented once signs of cognitive deteriorations are detected.”
SOURCE:
The study was conducted by Jie Liang, BS, School of Nursing, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, and colleagues. It was published online on November 29, 2023, in the Journal of the American Heart Association.
LIMITATIONS:
As this is an observational study, it can’t conclude a causal relationship. Although the authors adjusted for many potential confounders, unknown risk factors that also contribute to CHD can’t be ruled out. As the study excluded 69,744 participants, selection bias is possible. The study included a mostly White population.
DISCLOSURES:
The study was supported by the National Natural Science Foundation of China, the Non-Profit Central Research Institute Fund of the Chinese Academy of Medical Sciences, and the China Medical Board. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Can AI enhance mental health treatment?
Three questions for clinicians
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Three questions for clinicians
Three questions for clinicians
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Artificial intelligence (AI) is already impacting the mental health care space, with several new tools available to both clinicians and patients. While this technology could be a game-changer amid a mental health crisis and clinician shortage, there are important ethical and efficacy concerns clinicians should be aware of.
Current use cases illustrate both the potential and risks of AI. On one hand, AI has the potential to improve patient care with tools that can support diagnoses and inform treatment decisions at scale. The UK’s National Health Service is using an AI-powered diagnostic tool to help clinicians diagnose mental health disorders and determine the severity of a patient’s needs. Other tools leverage AI to analyze a patient’s voice for signs of depression or anxiety.
On the other hand, there are serious potential risks involving privacy, bias, and misinformation. One chatbot tool designed to counsel patients through disordered eating was shut down after giving problematic weight-loss advice.
The number of AI tools in the healthcare space is expected to increase fivefold by 2035. Keeping up with these advances is just as important for clinicians as keeping up with the latest medication and treatment options. That means being aware of both the limitations and the potential of AI. Here are three questions clinicians can ask as they explore ways to integrate these tools into their practice while navigating the risks.
• How can AI augment, not replace, the work of my staff?
For example, documentation and the use of electronic health records have consistently been linked to clinician burnout. Using AI to cut down on documentation would leave clinicians with more time and energy to focus on patient care.
One study from the National Library of Medicine found that physicians who did not have enough time to complete documentation were nearly three times more likely to report burnout. In some cases, clinic schedules were deliberately shortened to allow time for documentation.
New tools are emerging that use audio recording, transcription services, and large language models to generate clinical summaries and other documentation support. Amazon and 3M have partnered to solve documentation challenges using AI. This is an area I’ll definitely be keeping an eye on as it develops.
• Do I have patient consent to use this tool?
Since most AI tools remain relatively new, there is a gap in the legal and regulatory framework needed to ensure patient privacy and data protection. Clinicians should draw on existing guardrails and best practices to protect patient privacy and prioritize informed consent. The bottom line: Patients need to know how their data will be used and agree to it.
In the example above regarding documentation, a clinician should obtain patient consent before using technology that records or transcribes sessions. This extends to disclosing the use of AI chat tools and other touch points that occur between sessions. One mental health nonprofit has come under fire for using ChatGPT to provide mental health counseling to thousands of patients who weren’t aware the responses were generated by AI.
Beyond disclosing the use of these tools, clinicians should sufficiently explain how they work to ensure patients understand what they’re consenting to. Some technology companies offer guidance on how informed consent applies to their products and even offer template consent forms to support clinicians. Ultimately, accountability for maintaining patient privacy rests with the clinician, not the company behind the AI tool.
• Where is there a risk of bias?
There has been much discussion around the issue of bias within large language models in particular, since these programs will inherit any bias from the data points or text used to train them. However, there is often little to no visibility into how these models are trained, the algorithms they rely on, and how efficacy is measured.
This is especially concerning within the mental health care space, where bias can contribute to lower-quality care based on a patient’s race, gender or other characteristics. One systemic review published in JAMA Network Open found that most of the AI models used for psychiatric diagnoses that have been studied had a high overall risk of bias — which can lead to outputs that are misleading or incorrect, which can be dangerous in the healthcare field.
It’s important to keep the risk of bias top-of-mind when exploring AI tools and consider whether a tool would pose any direct harm to patients. Clinicians should have active oversight with any use of AI and, ultimately, consider an AI tool’s outputs alongside their own insights, expertise, and instincts.
Clinicians have the power to shape AI’s impact
While there is plenty to be excited about as these new tools develop, clinicians should explore AI with an eye toward the risks as well as the rewards. Practitioners have a significant opportunity to help shape how this technology develops by making informed decisions about which products to invest in and holding tech companies accountable. By educating patients, prioritizing informed consent, and seeking ways to augment their work that ultimately improve quality and scale of care, clinicians can help ensure positive outcomes while minimizing unintended consequences.
Dr. Patel-Dunn is a psychiatrist and chief medical officer at Lifestance Health, Scottsdale, Ariz.
Just gas? New study on colic suggests some longer-term implications
Pediatricians commonly are asked to see infants presenting with symptoms of colic. The frequent and intense crying associated with colic is understandably quite distressing to parents, who often worry about a serious underlying medical cause. There also is the stress of trying to soothe an irritable infant who often does not seem to respond to the typical interventions.
Conventional wisdom about colic has been that the behaviors are the result of some gastrointestinal problem that, while not perfectly understood, tends to be mercifully self-limited and not predictive of future medical or mental health problems. This perspective then leads to pediatricians typically offering mainly sympathy and reassurance at these visits.
A new study,1 however, challenges some of this traditional thinking. The data come from a remarkable longitudinal study called the Generation R Study (R being Rotterdam in the Netherlands) that has prospectively studied a group of nearly 5,000 children from before birth into adolescence. Colic symptoms were briefly assessed when infants were about 3 months old and emotional-behavioral problems have been prospectively measured at multiple time points subsequently using well-validated rating scales.
The main finding of the study was and, to a lesser extent, in adolescence. This held for both internalizing problems (like anxiety and depressive symptoms) and externalizing problems (like defiance and aggressive behavior). At age 10, participants also underwent an MRI scan and those who were excessive criers as infants were found to have a smaller amygdala, a region known for being important in regulating emotions.
The authors concluded that colicky behavior in infancy may reflect some underlying temperamental vulnerabilities and may have more predictive value than previously thought. The connection between excessive crying and a measurable brain region difference later in life is also interesting, although these kinds of brain imaging findings have been notoriously difficult to interpret clinically.
Overall, this is a solid study that deserves to be considered. Colic may reflect a bit more than most of us have been taught and shouldn’t necessarily be “shrugged off,” as the authors state in their discussion.
At the same time, however, it is important not to overinterpret the findings. The magnitude of the effects were on the small side (about 0.2 of a standard deviation) and most children with excessive crying in early infancy did not manifest high levels of mental health problems later in life. The mothers of high crying infants also had slightly higher levels of mental health problems themselves so there could be other mechanisms at work here, such as genetic differences between the two groups.
So how could a pediatrician best use this new information without taking things too far? Regardless of the question of whether the excessive crying infancy is a true risk factor for later behavior problems (in the causal sense) or whether it represents more of a marker for something else, its presence so early in life offers an opportunity. Primary care clinicians would still likely want to provide the reassurance that has typically been given in these visits but perhaps with the caveat that some of these kids go on to struggle a bit more with mental health and that they might benefit from some additional support. We are not talking about prophylactic medications here, but something like additional parenting skills. Especially if you, as the pediatrician, suspect that the parents might benefit from expanding their parenting toolkit already, here is a nice opportunity to invite them to learn some new approaches and skills — framed in a way that focuses on the temperament of the child rather than any “deficits” you perceive in the parents. Some parents may be more receptive and less defensive to the idea of participating in parent training under the framework that they are doing this because they have a temperamentally more challenging child (rather than feeling that they are deficient in basic parenting skills).
It’s always a good idea to know about what resources are available in the community when it comes to teaching parenting skills. In addition to scientifically supported books and podcasts, there has been a steady increase in reliable websites, apps, and other digital platforms related to parenting, as well as standard in-person groups and classes. This could also be a great use of an integrated behavioral health professional for practices fortunate enough to have one.
In summary, there is some new evidence that colic can represent a little more than “just gas,” and while we shouldn’t take this one study to the extreme, there may be some good opportunities here to discuss and support good parenting practices in general.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
1. Sammallahti S et al. Excessive crying, behavior problems, and amygdala volume: A study from infancy to adolescence. J Am Acad Child Adolesc Psychiatry. 2023 Jun;62(6):675-83. doi: 10.1016/j.jaac.2023.01.014.
Pediatricians commonly are asked to see infants presenting with symptoms of colic. The frequent and intense crying associated with colic is understandably quite distressing to parents, who often worry about a serious underlying medical cause. There also is the stress of trying to soothe an irritable infant who often does not seem to respond to the typical interventions.
Conventional wisdom about colic has been that the behaviors are the result of some gastrointestinal problem that, while not perfectly understood, tends to be mercifully self-limited and not predictive of future medical or mental health problems. This perspective then leads to pediatricians typically offering mainly sympathy and reassurance at these visits.
A new study,1 however, challenges some of this traditional thinking. The data come from a remarkable longitudinal study called the Generation R Study (R being Rotterdam in the Netherlands) that has prospectively studied a group of nearly 5,000 children from before birth into adolescence. Colic symptoms were briefly assessed when infants were about 3 months old and emotional-behavioral problems have been prospectively measured at multiple time points subsequently using well-validated rating scales.
The main finding of the study was and, to a lesser extent, in adolescence. This held for both internalizing problems (like anxiety and depressive symptoms) and externalizing problems (like defiance and aggressive behavior). At age 10, participants also underwent an MRI scan and those who were excessive criers as infants were found to have a smaller amygdala, a region known for being important in regulating emotions.
The authors concluded that colicky behavior in infancy may reflect some underlying temperamental vulnerabilities and may have more predictive value than previously thought. The connection between excessive crying and a measurable brain region difference later in life is also interesting, although these kinds of brain imaging findings have been notoriously difficult to interpret clinically.
Overall, this is a solid study that deserves to be considered. Colic may reflect a bit more than most of us have been taught and shouldn’t necessarily be “shrugged off,” as the authors state in their discussion.
At the same time, however, it is important not to overinterpret the findings. The magnitude of the effects were on the small side (about 0.2 of a standard deviation) and most children with excessive crying in early infancy did not manifest high levels of mental health problems later in life. The mothers of high crying infants also had slightly higher levels of mental health problems themselves so there could be other mechanisms at work here, such as genetic differences between the two groups.
So how could a pediatrician best use this new information without taking things too far? Regardless of the question of whether the excessive crying infancy is a true risk factor for later behavior problems (in the causal sense) or whether it represents more of a marker for something else, its presence so early in life offers an opportunity. Primary care clinicians would still likely want to provide the reassurance that has typically been given in these visits but perhaps with the caveat that some of these kids go on to struggle a bit more with mental health and that they might benefit from some additional support. We are not talking about prophylactic medications here, but something like additional parenting skills. Especially if you, as the pediatrician, suspect that the parents might benefit from expanding their parenting toolkit already, here is a nice opportunity to invite them to learn some new approaches and skills — framed in a way that focuses on the temperament of the child rather than any “deficits” you perceive in the parents. Some parents may be more receptive and less defensive to the idea of participating in parent training under the framework that they are doing this because they have a temperamentally more challenging child (rather than feeling that they are deficient in basic parenting skills).
It’s always a good idea to know about what resources are available in the community when it comes to teaching parenting skills. In addition to scientifically supported books and podcasts, there has been a steady increase in reliable websites, apps, and other digital platforms related to parenting, as well as standard in-person groups and classes. This could also be a great use of an integrated behavioral health professional for practices fortunate enough to have one.
In summary, there is some new evidence that colic can represent a little more than “just gas,” and while we shouldn’t take this one study to the extreme, there may be some good opportunities here to discuss and support good parenting practices in general.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
1. Sammallahti S et al. Excessive crying, behavior problems, and amygdala volume: A study from infancy to adolescence. J Am Acad Child Adolesc Psychiatry. 2023 Jun;62(6):675-83. doi: 10.1016/j.jaac.2023.01.014.
Pediatricians commonly are asked to see infants presenting with symptoms of colic. The frequent and intense crying associated with colic is understandably quite distressing to parents, who often worry about a serious underlying medical cause. There also is the stress of trying to soothe an irritable infant who often does not seem to respond to the typical interventions.
Conventional wisdom about colic has been that the behaviors are the result of some gastrointestinal problem that, while not perfectly understood, tends to be mercifully self-limited and not predictive of future medical or mental health problems. This perspective then leads to pediatricians typically offering mainly sympathy and reassurance at these visits.
A new study,1 however, challenges some of this traditional thinking. The data come from a remarkable longitudinal study called the Generation R Study (R being Rotterdam in the Netherlands) that has prospectively studied a group of nearly 5,000 children from before birth into adolescence. Colic symptoms were briefly assessed when infants were about 3 months old and emotional-behavioral problems have been prospectively measured at multiple time points subsequently using well-validated rating scales.
The main finding of the study was and, to a lesser extent, in adolescence. This held for both internalizing problems (like anxiety and depressive symptoms) and externalizing problems (like defiance and aggressive behavior). At age 10, participants also underwent an MRI scan and those who were excessive criers as infants were found to have a smaller amygdala, a region known for being important in regulating emotions.
The authors concluded that colicky behavior in infancy may reflect some underlying temperamental vulnerabilities and may have more predictive value than previously thought. The connection between excessive crying and a measurable brain region difference later in life is also interesting, although these kinds of brain imaging findings have been notoriously difficult to interpret clinically.
Overall, this is a solid study that deserves to be considered. Colic may reflect a bit more than most of us have been taught and shouldn’t necessarily be “shrugged off,” as the authors state in their discussion.
At the same time, however, it is important not to overinterpret the findings. The magnitude of the effects were on the small side (about 0.2 of a standard deviation) and most children with excessive crying in early infancy did not manifest high levels of mental health problems later in life. The mothers of high crying infants also had slightly higher levels of mental health problems themselves so there could be other mechanisms at work here, such as genetic differences between the two groups.
So how could a pediatrician best use this new information without taking things too far? Regardless of the question of whether the excessive crying infancy is a true risk factor for later behavior problems (in the causal sense) or whether it represents more of a marker for something else, its presence so early in life offers an opportunity. Primary care clinicians would still likely want to provide the reassurance that has typically been given in these visits but perhaps with the caveat that some of these kids go on to struggle a bit more with mental health and that they might benefit from some additional support. We are not talking about prophylactic medications here, but something like additional parenting skills. Especially if you, as the pediatrician, suspect that the parents might benefit from expanding their parenting toolkit already, here is a nice opportunity to invite them to learn some new approaches and skills — framed in a way that focuses on the temperament of the child rather than any “deficits” you perceive in the parents. Some parents may be more receptive and less defensive to the idea of participating in parent training under the framework that they are doing this because they have a temperamentally more challenging child (rather than feeling that they are deficient in basic parenting skills).
It’s always a good idea to know about what resources are available in the community when it comes to teaching parenting skills. In addition to scientifically supported books and podcasts, there has been a steady increase in reliable websites, apps, and other digital platforms related to parenting, as well as standard in-person groups and classes. This could also be a great use of an integrated behavioral health professional for practices fortunate enough to have one.
In summary, there is some new evidence that colic can represent a little more than “just gas,” and while we shouldn’t take this one study to the extreme, there may be some good opportunities here to discuss and support good parenting practices in general.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
1. Sammallahti S et al. Excessive crying, behavior problems, and amygdala volume: A study from infancy to adolescence. J Am Acad Child Adolesc Psychiatry. 2023 Jun;62(6):675-83. doi: 10.1016/j.jaac.2023.01.014.
Adverse events in childhood alter brain function
In a meta-analysis of 83 functional magnetic resonance imaging (fMRI) studies that included more than 5000 patients, exposure to adversity was associated with higher amygdala reactivity and lower prefrontal cortical reactivity across a range of task domains.
The altered responses were only observed in studies including adult participants and were clearest in participants who had been exposed to severe threat and trauma. Children and adolescents did not show significant adversity-related differences in brain function.
“By integrating the results from 83 previous brain imaging studies, we were able to provide what is arguably the clearest evidence to date that adults who have been exposed to early life trauma have different brain responses to psychological challenges,” senior author Marco Leyton, PhD, professor of psychiatry and director of the Temperament Adversity Biology Lab at McGill University in Montreal, Quebec, Canada, said in a press release. “This includes exaggerated responses in a region that processes emotionally intense information (the amygdala) and reduced responses in a region that helps people regulate emotions and associated behaviors (the frontal cortex).”
The findings were published in JAMA Network Open.
Changes in Reactivity
“One big issue we have in psychology, and especially in neuroscience, is that single-study results are often not reproducible,” lead author Niki Hosseini-Kamkar, PhD, neuroimaging research associate at Atlas Institute for Veterans and Families at Royal Ottawa Hospital, said in an interview.
“It was very important to me to use a meta-analysis to get an overall picture of what brain regions are consistently reported across all these different studies. That is what we did here,” she added. Dr. Hosseini-Kamkar conducted this analysis while she was a postdoctoral research fellow at McGill University in Montreal.
She and her group examined adversity exposure and brain function in the following four domains of task-based fMRI: emotion processing, memory processing, inhibitory control, and reward processing. Their study included 5242 participants. The researchers used multilevel kernel density analyses (MKDA) to analyze the data more accurately.
Adversity exposure was associated with higher amygdala reactivity (P < .001) and lower prefrontal cortical reactivity (P < .001), compared with controls with no adversity exposure.
Threat types of adversity were associated with greater blood-oxygen-level-dependent (BOLD) responses in the superior temporal gyrus and lower prefrontal cortex activity in participants exposed to threat, compared with controls.
Analysis of studies of inhibitory control tasks found greater activity in the claustrum, anterior cingulate cortex, and insula in the adversity-exposed participants, compared with controls.
In addition, studies that administered emotion processing tasks showed greater amygdala reactivity and lower prefrontal cortex (superior frontal gyrus) reactivity in the adversity exposure group, compared with controls.
“The main takeaway is that there’s an exaggerated activity in the amygdala, and diminished prefrontal cortex activity, and together, this might point to a mechanism for how a history of adversity diminishes the ability to cope with later stressors and can therefore heighten susceptibility to mental illness,” said Dr. Hosseini-Kamkar.
‘Important Next Step’
“Overall, the meta-analysis by Dr. Hosseini-Kamkar and colleagues represents an important next step in understanding associations of adversity exposure with brain function while highlighting the importance of considering the role of development,” wrote Dylan G. Gee, PhD, associate professor of psychology at Yale University in New Haven, Connecticut, and Alexis Brieant, PhD, assistant professor of research or creative works at the University of Vermont in Burlington, in an accompanying commentary.
They also applauded the authors for their use of MKDA. They noted that the technique “allows inferences about the consistency and specificity of brain activation across studies and is thought to be more robust to small sample sizes than activation likelihood estimation (ALE) meta-analysis.”
Dr. Gee and Dr. Brieant also observed that a recent ALE meta-analysis failed to find a link between adversity and brain function. “Although it is important to note that the file drawer problem — by which researchers are less likely to publish null results — presents challenges to the inferences that can be drawn in the current work, the current study may provide complementary information to prior ALE meta-analyses.”
Epigenetic Changes?
Commenting on the findings for this article, Victor Fornari, MD, director of child and adolescent psychiatry at Northwell Health in Glen Oaks, New York, said, “Historically, when someone went through a traumatic event, they were told to just get over it, because somehow trauma doesn’t have a lasting impact on the brain.” Dr. Fornari was not involved in the research.
“We have certainly learned so much more over the past decade about early adversity and that it does have a profound impact on the brain and probably even epigenetic changes in our genes,” Dr. Fornari said.
“This is a very important avenue of investigation. People are really trying to understand if there are biological markers that we can actually measure in the brain that will offer us a window to better understand the consequence of adversity, as well as possible avenues of treatment.”
No funding source for this study was reported. Dr. Leyton, Dr. Hosseini-Kamkar, and Dr. Fornari report no relevant financial relationships. Gee reports receiving grants from the National Science Foundation and National Institutes of Health outside the submitted work. Dr. Brieant reports receiving grants from the National Institute of Mental Health outside the submitted work.
A version of this article appeared on Medscape.com.
In a meta-analysis of 83 functional magnetic resonance imaging (fMRI) studies that included more than 5000 patients, exposure to adversity was associated with higher amygdala reactivity and lower prefrontal cortical reactivity across a range of task domains.
The altered responses were only observed in studies including adult participants and were clearest in participants who had been exposed to severe threat and trauma. Children and adolescents did not show significant adversity-related differences in brain function.
“By integrating the results from 83 previous brain imaging studies, we were able to provide what is arguably the clearest evidence to date that adults who have been exposed to early life trauma have different brain responses to psychological challenges,” senior author Marco Leyton, PhD, professor of psychiatry and director of the Temperament Adversity Biology Lab at McGill University in Montreal, Quebec, Canada, said in a press release. “This includes exaggerated responses in a region that processes emotionally intense information (the amygdala) and reduced responses in a region that helps people regulate emotions and associated behaviors (the frontal cortex).”
The findings were published in JAMA Network Open.
Changes in Reactivity
“One big issue we have in psychology, and especially in neuroscience, is that single-study results are often not reproducible,” lead author Niki Hosseini-Kamkar, PhD, neuroimaging research associate at Atlas Institute for Veterans and Families at Royal Ottawa Hospital, said in an interview.
“It was very important to me to use a meta-analysis to get an overall picture of what brain regions are consistently reported across all these different studies. That is what we did here,” she added. Dr. Hosseini-Kamkar conducted this analysis while she was a postdoctoral research fellow at McGill University in Montreal.
She and her group examined adversity exposure and brain function in the following four domains of task-based fMRI: emotion processing, memory processing, inhibitory control, and reward processing. Their study included 5242 participants. The researchers used multilevel kernel density analyses (MKDA) to analyze the data more accurately.
Adversity exposure was associated with higher amygdala reactivity (P < .001) and lower prefrontal cortical reactivity (P < .001), compared with controls with no adversity exposure.
Threat types of adversity were associated with greater blood-oxygen-level-dependent (BOLD) responses in the superior temporal gyrus and lower prefrontal cortex activity in participants exposed to threat, compared with controls.
Analysis of studies of inhibitory control tasks found greater activity in the claustrum, anterior cingulate cortex, and insula in the adversity-exposed participants, compared with controls.
In addition, studies that administered emotion processing tasks showed greater amygdala reactivity and lower prefrontal cortex (superior frontal gyrus) reactivity in the adversity exposure group, compared with controls.
“The main takeaway is that there’s an exaggerated activity in the amygdala, and diminished prefrontal cortex activity, and together, this might point to a mechanism for how a history of adversity diminishes the ability to cope with later stressors and can therefore heighten susceptibility to mental illness,” said Dr. Hosseini-Kamkar.
‘Important Next Step’
“Overall, the meta-analysis by Dr. Hosseini-Kamkar and colleagues represents an important next step in understanding associations of adversity exposure with brain function while highlighting the importance of considering the role of development,” wrote Dylan G. Gee, PhD, associate professor of psychology at Yale University in New Haven, Connecticut, and Alexis Brieant, PhD, assistant professor of research or creative works at the University of Vermont in Burlington, in an accompanying commentary.
They also applauded the authors for their use of MKDA. They noted that the technique “allows inferences about the consistency and specificity of brain activation across studies and is thought to be more robust to small sample sizes than activation likelihood estimation (ALE) meta-analysis.”
Dr. Gee and Dr. Brieant also observed that a recent ALE meta-analysis failed to find a link between adversity and brain function. “Although it is important to note that the file drawer problem — by which researchers are less likely to publish null results — presents challenges to the inferences that can be drawn in the current work, the current study may provide complementary information to prior ALE meta-analyses.”
Epigenetic Changes?
Commenting on the findings for this article, Victor Fornari, MD, director of child and adolescent psychiatry at Northwell Health in Glen Oaks, New York, said, “Historically, when someone went through a traumatic event, they were told to just get over it, because somehow trauma doesn’t have a lasting impact on the brain.” Dr. Fornari was not involved in the research.
“We have certainly learned so much more over the past decade about early adversity and that it does have a profound impact on the brain and probably even epigenetic changes in our genes,” Dr. Fornari said.
“This is a very important avenue of investigation. People are really trying to understand if there are biological markers that we can actually measure in the brain that will offer us a window to better understand the consequence of adversity, as well as possible avenues of treatment.”
No funding source for this study was reported. Dr. Leyton, Dr. Hosseini-Kamkar, and Dr. Fornari report no relevant financial relationships. Gee reports receiving grants from the National Science Foundation and National Institutes of Health outside the submitted work. Dr. Brieant reports receiving grants from the National Institute of Mental Health outside the submitted work.
A version of this article appeared on Medscape.com.
In a meta-analysis of 83 functional magnetic resonance imaging (fMRI) studies that included more than 5000 patients, exposure to adversity was associated with higher amygdala reactivity and lower prefrontal cortical reactivity across a range of task domains.
The altered responses were only observed in studies including adult participants and were clearest in participants who had been exposed to severe threat and trauma. Children and adolescents did not show significant adversity-related differences in brain function.
“By integrating the results from 83 previous brain imaging studies, we were able to provide what is arguably the clearest evidence to date that adults who have been exposed to early life trauma have different brain responses to psychological challenges,” senior author Marco Leyton, PhD, professor of psychiatry and director of the Temperament Adversity Biology Lab at McGill University in Montreal, Quebec, Canada, said in a press release. “This includes exaggerated responses in a region that processes emotionally intense information (the amygdala) and reduced responses in a region that helps people regulate emotions and associated behaviors (the frontal cortex).”
The findings were published in JAMA Network Open.
Changes in Reactivity
“One big issue we have in psychology, and especially in neuroscience, is that single-study results are often not reproducible,” lead author Niki Hosseini-Kamkar, PhD, neuroimaging research associate at Atlas Institute for Veterans and Families at Royal Ottawa Hospital, said in an interview.
“It was very important to me to use a meta-analysis to get an overall picture of what brain regions are consistently reported across all these different studies. That is what we did here,” she added. Dr. Hosseini-Kamkar conducted this analysis while she was a postdoctoral research fellow at McGill University in Montreal.
She and her group examined adversity exposure and brain function in the following four domains of task-based fMRI: emotion processing, memory processing, inhibitory control, and reward processing. Their study included 5242 participants. The researchers used multilevel kernel density analyses (MKDA) to analyze the data more accurately.
Adversity exposure was associated with higher amygdala reactivity (P < .001) and lower prefrontal cortical reactivity (P < .001), compared with controls with no adversity exposure.
Threat types of adversity were associated with greater blood-oxygen-level-dependent (BOLD) responses in the superior temporal gyrus and lower prefrontal cortex activity in participants exposed to threat, compared with controls.
Analysis of studies of inhibitory control tasks found greater activity in the claustrum, anterior cingulate cortex, and insula in the adversity-exposed participants, compared with controls.
In addition, studies that administered emotion processing tasks showed greater amygdala reactivity and lower prefrontal cortex (superior frontal gyrus) reactivity in the adversity exposure group, compared with controls.
“The main takeaway is that there’s an exaggerated activity in the amygdala, and diminished prefrontal cortex activity, and together, this might point to a mechanism for how a history of adversity diminishes the ability to cope with later stressors and can therefore heighten susceptibility to mental illness,” said Dr. Hosseini-Kamkar.
‘Important Next Step’
“Overall, the meta-analysis by Dr. Hosseini-Kamkar and colleagues represents an important next step in understanding associations of adversity exposure with brain function while highlighting the importance of considering the role of development,” wrote Dylan G. Gee, PhD, associate professor of psychology at Yale University in New Haven, Connecticut, and Alexis Brieant, PhD, assistant professor of research or creative works at the University of Vermont in Burlington, in an accompanying commentary.
They also applauded the authors for their use of MKDA. They noted that the technique “allows inferences about the consistency and specificity of brain activation across studies and is thought to be more robust to small sample sizes than activation likelihood estimation (ALE) meta-analysis.”
Dr. Gee and Dr. Brieant also observed that a recent ALE meta-analysis failed to find a link between adversity and brain function. “Although it is important to note that the file drawer problem — by which researchers are less likely to publish null results — presents challenges to the inferences that can be drawn in the current work, the current study may provide complementary information to prior ALE meta-analyses.”
Epigenetic Changes?
Commenting on the findings for this article, Victor Fornari, MD, director of child and adolescent psychiatry at Northwell Health in Glen Oaks, New York, said, “Historically, when someone went through a traumatic event, they were told to just get over it, because somehow trauma doesn’t have a lasting impact on the brain.” Dr. Fornari was not involved in the research.
“We have certainly learned so much more over the past decade about early adversity and that it does have a profound impact on the brain and probably even epigenetic changes in our genes,” Dr. Fornari said.
“This is a very important avenue of investigation. People are really trying to understand if there are biological markers that we can actually measure in the brain that will offer us a window to better understand the consequence of adversity, as well as possible avenues of treatment.”
No funding source for this study was reported. Dr. Leyton, Dr. Hosseini-Kamkar, and Dr. Fornari report no relevant financial relationships. Gee reports receiving grants from the National Science Foundation and National Institutes of Health outside the submitted work. Dr. Brieant reports receiving grants from the National Institute of Mental Health outside the submitted work.
A version of this article appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Clinician responsibilities during times of geopolitical conflict
In the realm of clinical psychology and psychiatry, our primary duty and commitment is (and should be) to the well-being of our patients. Yet, as we find ourselves in an era marked by escalating geopolitical conflict, such as the Israel-Hamas war, probably more aptly titled the Israeli-Hamas-Hezbollah-Houthi war (a clarification that elucidates a later point), clinicians are increasingly confronted with ethical dilemmas that extend far beyond what is outlined in our code of ethics.
These challenges are not only impacting us on a personal level but are also spilling over into our professional lives, creating a divisive and non-collegial environment within the healthcare community. We commit to “do no harm” when delivering care and yet we are doing harm to one another as colleagues.
We are no strangers to the complexities of human behavior and the intricate tapestry of emotions that are involved with our professional work. However, the current geopolitical landscape has added an extra layer of difficulty to our already taxing professional lives. We are, after all, human first with unconscious drives that govern how we negotiate cognitive dissonance and our need for the illusion of absolute justice as Yuval Noah Harari explains in a recent podcast.
Humans are notoriously bad at holding the multiplicity of experience in mind and various (often competing narratives) that impede the capacity for nuanced thinking. We would like to believe we are better and more capable than the average person in doing so, but divisiveness in our profession has become disturbingly pronounced, making it essential for us to carve out reflective space, more than ever.
The personal and professional divide
Geopolitical conflicts like the current war have a unique capacity to ignite strong emotions and deeply held convictions. It’s not hard to quickly become embroiled in passionate and engaged debate.
While discussion and discourse are healthy, these are bleeding into professional spheres, creating rifts within our clinical communities and contributing to a culture where not everyone feels safe. Look at any professional listserv in medicine or psychology and you will find the evidence. It should be an immediate call to action that we need to be fostering a different type of environment.
The impact of divisiveness is profound, hindering opportunities for collaboration, mentorship, and the free exchange of ideas among clinicians. It may lead to misunderstandings, mistrust, and an erosion of the support systems we rely on, ultimately diverting energy away from the pursuit of providing quality patient-care.
Balancing obligations and limits
Because of the inherent power differential that accompanies being in a provider role (physician and psychologist alike), we have a social and moral responsibility to be mindful of what we share – for the sake of humanity. There is an implicit assumption that a provider’s guidance should be adhered to and respected. In other words, words carry tremendous weight and deeply matter, and people in the general public ascribe significant meaning to messages put out by professionals.
When providers steer from their lanes of professional expertise to provide the general public with opinions or recommendations on nonmedical topics, problematic precedents can be set. We may be doing people a disservice.
Unfortunately, I have heard several anecdotes about clinicians who spend their patient’s time in session pushing their own ideological agendas. The patient-provider relationship is founded on principles of trust, empathy, and collaboration, with the primary goal of improving overall well-being and addressing a specific presenting problem. Of course, issues emerge that need to be addressed outside of the initial scope of treatment, an inherent part of the process. However, a grave concern emerges when clinicians initiate dialogue that is not meaningful to a patient, disclose and discuss their personal ideologies, or put pressure on patients to explain their beliefs in an attempt to change the patients’ minds.
Clinicians pushing their own agenda during patient sessions is antithetical to the objectives of psychotherapy and compromises the therapeutic alliance by diverting the focus of care in a way that serves the clinician rather than the client. It is quite the opposite of the patient-centered care that we strive for in training and practice.
Even within one’s theoretical professional scope of competence, I have seen the impact of emotions running high during this conflict, and have witnessed trained professionals making light of, or even mocking, hostages and their behavior upon release. These are care providers who could elucidate the complexities of captor-captive dynamics and the impact of trauma for the general public, yet they are contributing to dangerous perceptions and divisiveness.
I have also seen providers justify sexual violence, diminishing survivor and witness testimony due to ideological differences and strong personal beliefs. This is harmful to those impacted and does a disservice to our profession at large. In a helping profession we should strive to support and advocate for anyone who has been maltreated or experienced any form of victimization, violence, or abuse. This should be a professional standard.
As clinicians, we have an ethical obligation to uphold the well-being, autonomy, and dignity of our patients — and humanity. It is crucial to recognize the limits of our expertise and the ethical concerns that can arise in light of geopolitical conflict. How can we balance our duty to provide psychological support while also being cautious about delving into the realms of political analysis, foreign policy, or international relations?
The pitfalls of well-intentioned speaking out
In the age of social media and instant communication, a critical aspect to consider is the role of speaking out. The point I made above, in naming all partaking in the current conflict, speaks to this issue.
As providers and programs, we must be mindful of the inadvertent harm that can arise from making brief, underdeveloped, uninformed, or emotionally charged statements. Expressing opinions without a solid understanding of the historical, cultural, and political nuances of a conflict can contribute to misinformation and further polarization.
Anecdotally, there appears to be some significant degree of bias emerging within professional fields (e.g., psychology, medicine) and an innate calling for providers to “weigh in” as the war continues. Obviously, physicians and psychologists are trained to provide care and to be humanistic and empathic, but the majority do not have expertise in geopolitics or a nuanced awareness of the complexities of the conflict in the Middle East.
While hearts may be in the right place, issuing statements on complicated humanitarian/political situations can inadvertently have unintended and harmful consequences (in terms of antisemitism and islamophobia, increased incidence of hate crimes, and colleagues not feeling safe within professional societies or member organizations).
Unsophisticated, overly simplistic, and reductionistic statements that do not adequately convey nuance will not reflect the range of experience reflected by providers in the field (or the patients we treat). It is essential for clinicians and institutions putting out public statements to engage in deep reflection and utilize discernment. We must recognize that our words carry weight, given our position of influence as treatment providers. To minimize harm, we should seek to provide information that is fair, vetted, and balanced, and encourage open, respectful dialogue rather than asserting definitive positions.
Ultimately, as providers we must strive to seek unity and inclusivity amidst the current challenges. It is important for us to embody a spirit of collaboration during a time demarcated by deep fragmentation.
By acknowledging our limitations, promoting informed discussion, and avoiding the pitfalls of uninformed advocacy, we can contribute to a more compassionate and understanding world, even in the face of the most divisive geopolitical conflicts. We have an obligation to uphold when it comes to ourselves as professionals, and we need to foster healthy, respectful dialogue while maintaining an awareness of our blind spots.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She is an affiliate of Baptist West Kendall Hospital/FIU Family Medicine Residency Program and serves as president on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. The opinions expressed by Dr. Feldman are her own and do not represent the institutions with which she is affiliated. She has no disclosures.
In the realm of clinical psychology and psychiatry, our primary duty and commitment is (and should be) to the well-being of our patients. Yet, as we find ourselves in an era marked by escalating geopolitical conflict, such as the Israel-Hamas war, probably more aptly titled the Israeli-Hamas-Hezbollah-Houthi war (a clarification that elucidates a later point), clinicians are increasingly confronted with ethical dilemmas that extend far beyond what is outlined in our code of ethics.
These challenges are not only impacting us on a personal level but are also spilling over into our professional lives, creating a divisive and non-collegial environment within the healthcare community. We commit to “do no harm” when delivering care and yet we are doing harm to one another as colleagues.
We are no strangers to the complexities of human behavior and the intricate tapestry of emotions that are involved with our professional work. However, the current geopolitical landscape has added an extra layer of difficulty to our already taxing professional lives. We are, after all, human first with unconscious drives that govern how we negotiate cognitive dissonance and our need for the illusion of absolute justice as Yuval Noah Harari explains in a recent podcast.
Humans are notoriously bad at holding the multiplicity of experience in mind and various (often competing narratives) that impede the capacity for nuanced thinking. We would like to believe we are better and more capable than the average person in doing so, but divisiveness in our profession has become disturbingly pronounced, making it essential for us to carve out reflective space, more than ever.
The personal and professional divide
Geopolitical conflicts like the current war have a unique capacity to ignite strong emotions and deeply held convictions. It’s not hard to quickly become embroiled in passionate and engaged debate.
While discussion and discourse are healthy, these are bleeding into professional spheres, creating rifts within our clinical communities and contributing to a culture where not everyone feels safe. Look at any professional listserv in medicine or psychology and you will find the evidence. It should be an immediate call to action that we need to be fostering a different type of environment.
The impact of divisiveness is profound, hindering opportunities for collaboration, mentorship, and the free exchange of ideas among clinicians. It may lead to misunderstandings, mistrust, and an erosion of the support systems we rely on, ultimately diverting energy away from the pursuit of providing quality patient-care.
Balancing obligations and limits
Because of the inherent power differential that accompanies being in a provider role (physician and psychologist alike), we have a social and moral responsibility to be mindful of what we share – for the sake of humanity. There is an implicit assumption that a provider’s guidance should be adhered to and respected. In other words, words carry tremendous weight and deeply matter, and people in the general public ascribe significant meaning to messages put out by professionals.
When providers steer from their lanes of professional expertise to provide the general public with opinions or recommendations on nonmedical topics, problematic precedents can be set. We may be doing people a disservice.
Unfortunately, I have heard several anecdotes about clinicians who spend their patient’s time in session pushing their own ideological agendas. The patient-provider relationship is founded on principles of trust, empathy, and collaboration, with the primary goal of improving overall well-being and addressing a specific presenting problem. Of course, issues emerge that need to be addressed outside of the initial scope of treatment, an inherent part of the process. However, a grave concern emerges when clinicians initiate dialogue that is not meaningful to a patient, disclose and discuss their personal ideologies, or put pressure on patients to explain their beliefs in an attempt to change the patients’ minds.
Clinicians pushing their own agenda during patient sessions is antithetical to the objectives of psychotherapy and compromises the therapeutic alliance by diverting the focus of care in a way that serves the clinician rather than the client. It is quite the opposite of the patient-centered care that we strive for in training and practice.
Even within one’s theoretical professional scope of competence, I have seen the impact of emotions running high during this conflict, and have witnessed trained professionals making light of, or even mocking, hostages and their behavior upon release. These are care providers who could elucidate the complexities of captor-captive dynamics and the impact of trauma for the general public, yet they are contributing to dangerous perceptions and divisiveness.
I have also seen providers justify sexual violence, diminishing survivor and witness testimony due to ideological differences and strong personal beliefs. This is harmful to those impacted and does a disservice to our profession at large. In a helping profession we should strive to support and advocate for anyone who has been maltreated or experienced any form of victimization, violence, or abuse. This should be a professional standard.
As clinicians, we have an ethical obligation to uphold the well-being, autonomy, and dignity of our patients — and humanity. It is crucial to recognize the limits of our expertise and the ethical concerns that can arise in light of geopolitical conflict. How can we balance our duty to provide psychological support while also being cautious about delving into the realms of political analysis, foreign policy, or international relations?
The pitfalls of well-intentioned speaking out
In the age of social media and instant communication, a critical aspect to consider is the role of speaking out. The point I made above, in naming all partaking in the current conflict, speaks to this issue.
As providers and programs, we must be mindful of the inadvertent harm that can arise from making brief, underdeveloped, uninformed, or emotionally charged statements. Expressing opinions without a solid understanding of the historical, cultural, and political nuances of a conflict can contribute to misinformation and further polarization.
Anecdotally, there appears to be some significant degree of bias emerging within professional fields (e.g., psychology, medicine) and an innate calling for providers to “weigh in” as the war continues. Obviously, physicians and psychologists are trained to provide care and to be humanistic and empathic, but the majority do not have expertise in geopolitics or a nuanced awareness of the complexities of the conflict in the Middle East.
While hearts may be in the right place, issuing statements on complicated humanitarian/political situations can inadvertently have unintended and harmful consequences (in terms of antisemitism and islamophobia, increased incidence of hate crimes, and colleagues not feeling safe within professional societies or member organizations).
Unsophisticated, overly simplistic, and reductionistic statements that do not adequately convey nuance will not reflect the range of experience reflected by providers in the field (or the patients we treat). It is essential for clinicians and institutions putting out public statements to engage in deep reflection and utilize discernment. We must recognize that our words carry weight, given our position of influence as treatment providers. To minimize harm, we should seek to provide information that is fair, vetted, and balanced, and encourage open, respectful dialogue rather than asserting definitive positions.
Ultimately, as providers we must strive to seek unity and inclusivity amidst the current challenges. It is important for us to embody a spirit of collaboration during a time demarcated by deep fragmentation.
By acknowledging our limitations, promoting informed discussion, and avoiding the pitfalls of uninformed advocacy, we can contribute to a more compassionate and understanding world, even in the face of the most divisive geopolitical conflicts. We have an obligation to uphold when it comes to ourselves as professionals, and we need to foster healthy, respectful dialogue while maintaining an awareness of our blind spots.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She is an affiliate of Baptist West Kendall Hospital/FIU Family Medicine Residency Program and serves as president on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. The opinions expressed by Dr. Feldman are her own and do not represent the institutions with which she is affiliated. She has no disclosures.
In the realm of clinical psychology and psychiatry, our primary duty and commitment is (and should be) to the well-being of our patients. Yet, as we find ourselves in an era marked by escalating geopolitical conflict, such as the Israel-Hamas war, probably more aptly titled the Israeli-Hamas-Hezbollah-Houthi war (a clarification that elucidates a later point), clinicians are increasingly confronted with ethical dilemmas that extend far beyond what is outlined in our code of ethics.
These challenges are not only impacting us on a personal level but are also spilling over into our professional lives, creating a divisive and non-collegial environment within the healthcare community. We commit to “do no harm” when delivering care and yet we are doing harm to one another as colleagues.
We are no strangers to the complexities of human behavior and the intricate tapestry of emotions that are involved with our professional work. However, the current geopolitical landscape has added an extra layer of difficulty to our already taxing professional lives. We are, after all, human first with unconscious drives that govern how we negotiate cognitive dissonance and our need for the illusion of absolute justice as Yuval Noah Harari explains in a recent podcast.
Humans are notoriously bad at holding the multiplicity of experience in mind and various (often competing narratives) that impede the capacity for nuanced thinking. We would like to believe we are better and more capable than the average person in doing so, but divisiveness in our profession has become disturbingly pronounced, making it essential for us to carve out reflective space, more than ever.
The personal and professional divide
Geopolitical conflicts like the current war have a unique capacity to ignite strong emotions and deeply held convictions. It’s not hard to quickly become embroiled in passionate and engaged debate.
While discussion and discourse are healthy, these are bleeding into professional spheres, creating rifts within our clinical communities and contributing to a culture where not everyone feels safe. Look at any professional listserv in medicine or psychology and you will find the evidence. It should be an immediate call to action that we need to be fostering a different type of environment.
The impact of divisiveness is profound, hindering opportunities for collaboration, mentorship, and the free exchange of ideas among clinicians. It may lead to misunderstandings, mistrust, and an erosion of the support systems we rely on, ultimately diverting energy away from the pursuit of providing quality patient-care.
Balancing obligations and limits
Because of the inherent power differential that accompanies being in a provider role (physician and psychologist alike), we have a social and moral responsibility to be mindful of what we share – for the sake of humanity. There is an implicit assumption that a provider’s guidance should be adhered to and respected. In other words, words carry tremendous weight and deeply matter, and people in the general public ascribe significant meaning to messages put out by professionals.
When providers steer from their lanes of professional expertise to provide the general public with opinions or recommendations on nonmedical topics, problematic precedents can be set. We may be doing people a disservice.
Unfortunately, I have heard several anecdotes about clinicians who spend their patient’s time in session pushing their own ideological agendas. The patient-provider relationship is founded on principles of trust, empathy, and collaboration, with the primary goal of improving overall well-being and addressing a specific presenting problem. Of course, issues emerge that need to be addressed outside of the initial scope of treatment, an inherent part of the process. However, a grave concern emerges when clinicians initiate dialogue that is not meaningful to a patient, disclose and discuss their personal ideologies, or put pressure on patients to explain their beliefs in an attempt to change the patients’ minds.
Clinicians pushing their own agenda during patient sessions is antithetical to the objectives of psychotherapy and compromises the therapeutic alliance by diverting the focus of care in a way that serves the clinician rather than the client. It is quite the opposite of the patient-centered care that we strive for in training and practice.
Even within one’s theoretical professional scope of competence, I have seen the impact of emotions running high during this conflict, and have witnessed trained professionals making light of, or even mocking, hostages and their behavior upon release. These are care providers who could elucidate the complexities of captor-captive dynamics and the impact of trauma for the general public, yet they are contributing to dangerous perceptions and divisiveness.
I have also seen providers justify sexual violence, diminishing survivor and witness testimony due to ideological differences and strong personal beliefs. This is harmful to those impacted and does a disservice to our profession at large. In a helping profession we should strive to support and advocate for anyone who has been maltreated or experienced any form of victimization, violence, or abuse. This should be a professional standard.
As clinicians, we have an ethical obligation to uphold the well-being, autonomy, and dignity of our patients — and humanity. It is crucial to recognize the limits of our expertise and the ethical concerns that can arise in light of geopolitical conflict. How can we balance our duty to provide psychological support while also being cautious about delving into the realms of political analysis, foreign policy, or international relations?
The pitfalls of well-intentioned speaking out
In the age of social media and instant communication, a critical aspect to consider is the role of speaking out. The point I made above, in naming all partaking in the current conflict, speaks to this issue.
As providers and programs, we must be mindful of the inadvertent harm that can arise from making brief, underdeveloped, uninformed, or emotionally charged statements. Expressing opinions without a solid understanding of the historical, cultural, and political nuances of a conflict can contribute to misinformation and further polarization.
Anecdotally, there appears to be some significant degree of bias emerging within professional fields (e.g., psychology, medicine) and an innate calling for providers to “weigh in” as the war continues. Obviously, physicians and psychologists are trained to provide care and to be humanistic and empathic, but the majority do not have expertise in geopolitics or a nuanced awareness of the complexities of the conflict in the Middle East.
While hearts may be in the right place, issuing statements on complicated humanitarian/political situations can inadvertently have unintended and harmful consequences (in terms of antisemitism and islamophobia, increased incidence of hate crimes, and colleagues not feeling safe within professional societies or member organizations).
Unsophisticated, overly simplistic, and reductionistic statements that do not adequately convey nuance will not reflect the range of experience reflected by providers in the field (or the patients we treat). It is essential for clinicians and institutions putting out public statements to engage in deep reflection and utilize discernment. We must recognize that our words carry weight, given our position of influence as treatment providers. To minimize harm, we should seek to provide information that is fair, vetted, and balanced, and encourage open, respectful dialogue rather than asserting definitive positions.
Ultimately, as providers we must strive to seek unity and inclusivity amidst the current challenges. It is important for us to embody a spirit of collaboration during a time demarcated by deep fragmentation.
By acknowledging our limitations, promoting informed discussion, and avoiding the pitfalls of uninformed advocacy, we can contribute to a more compassionate and understanding world, even in the face of the most divisive geopolitical conflicts. We have an obligation to uphold when it comes to ourselves as professionals, and we need to foster healthy, respectful dialogue while maintaining an awareness of our blind spots.
Dr. Feldman is a licensed clinical psychologist in private practice in Miami. She is an adjunct professor in the College of Psychology at Nova Southeastern University, Fort Lauderdale, Fla., where she teaches clinical psychology doctoral students. She is an affiliate of Baptist West Kendall Hospital/FIU Family Medicine Residency Program and serves as president on the board of directors of The Southeast Florida Association for Psychoanalytic Psychology. The opinions expressed by Dr. Feldman are her own and do not represent the institutions with which she is affiliated. She has no disclosures.
Excessive TV-watching tied to elevated risk for dementia, Parkinson’s disease, and depression
TOPLINE:
whereas a limited amount of daily computer use that is not work-related is linked to a lower risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 473,184 people aged 39-72 years from the UK Biobank who were enrolled from 2006 to 2010 and followed until a diagnosis of dementia, PD, depression, death, or study end (2018 for Wales residents; 2021 for residents of England and Scotland).
- Participants reported on the number of hours they spent outside of work exercising, watching television, and using the computer.
- MRI was conducted to determine participants’ brain volume.
TAKEAWAY:
- During the study, 6096 people developed dementia, 3000 developed PD, 23,600 developed depression, 1200 developed dementia and depression, and 486 developed PD and depression.
- Compared with those who watched TV for under 1 hour per day, those who reported watching 4 or more hours per day had a 28% higher risk for dementia (adjusted hazard ratio [aHR], 1.28; 95% CI, 1.17-1.39), a 35% higher risk for depression, (aHR, 1.35; 95% CI, 1.29-1.40) and a 16% greater risk for PD (aHR, 1.16; 95% CI, 1.03-1.29).
- However, moderate computer use outside of work seemed somewhat protective. Participants who used the computer for 30-60 minutes per day had lower risks for dementia (aHR, 0.68; 95% CI, 0.64-0.72), PD, (aHR, 0.86; 95% CI, 0.79-0.93), and depression (aHR, 0.85; 95% CI, 0.83-0.88) compared with those who reported the lowest levels of computer usage.
- Replacing 30 minutes per day of computer time with an equal amount of structured exercise was associated with decreased risk for dementia (aHR, 0.74; 95% CI, 0.85-0.95) and PD (aHR, 0.84; 95% CI, 0.78-0.90).
IN PRACTICE:
The association between extended periods of TV use and higher risk for PD and dementia could be explained by a lack of activity, the authors note. They add that sedentary behavior is, “associated with biomarkers of low-grade inflammation and changes in inflammation markers that could initiate and or worsen neuroinflammation and contribute to neurodegeneration.”
SOURCE:
Hanzhang Wu, PhD, of Tianjin University of Traditional Medicine in Tianjin, China, led the study, which was published online in the International Journal of Behavioral Nutrition and Physical Activity.
LIMITATIONS:
Screen behaviors were assessed using self-report measures, which is subject to recall bias. Also, there may have been variables confounding the findings for which investigators did not account.
DISCLOSURES:
The study was funded by the National Natural Science Foundation of China, the Tianjin Major Public Health Science and Technology Project, the National Health Commission of China, the Food Science and Technology Foundation of Chinese Institute of Food Science and Technology, the China Cohort Consortium, and the Chinese Nutrition Society Nutrition Research Foundation–DSM Research Fund, China. There were no disclosures reported.
Eve Bender has no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
whereas a limited amount of daily computer use that is not work-related is linked to a lower risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 473,184 people aged 39-72 years from the UK Biobank who were enrolled from 2006 to 2010 and followed until a diagnosis of dementia, PD, depression, death, or study end (2018 for Wales residents; 2021 for residents of England and Scotland).
- Participants reported on the number of hours they spent outside of work exercising, watching television, and using the computer.
- MRI was conducted to determine participants’ brain volume.
TAKEAWAY:
- During the study, 6096 people developed dementia, 3000 developed PD, 23,600 developed depression, 1200 developed dementia and depression, and 486 developed PD and depression.
- Compared with those who watched TV for under 1 hour per day, those who reported watching 4 or more hours per day had a 28% higher risk for dementia (adjusted hazard ratio [aHR], 1.28; 95% CI, 1.17-1.39), a 35% higher risk for depression, (aHR, 1.35; 95% CI, 1.29-1.40) and a 16% greater risk for PD (aHR, 1.16; 95% CI, 1.03-1.29).
- However, moderate computer use outside of work seemed somewhat protective. Participants who used the computer for 30-60 minutes per day had lower risks for dementia (aHR, 0.68; 95% CI, 0.64-0.72), PD, (aHR, 0.86; 95% CI, 0.79-0.93), and depression (aHR, 0.85; 95% CI, 0.83-0.88) compared with those who reported the lowest levels of computer usage.
- Replacing 30 minutes per day of computer time with an equal amount of structured exercise was associated with decreased risk for dementia (aHR, 0.74; 95% CI, 0.85-0.95) and PD (aHR, 0.84; 95% CI, 0.78-0.90).
IN PRACTICE:
The association between extended periods of TV use and higher risk for PD and dementia could be explained by a lack of activity, the authors note. They add that sedentary behavior is, “associated with biomarkers of low-grade inflammation and changes in inflammation markers that could initiate and or worsen neuroinflammation and contribute to neurodegeneration.”
SOURCE:
Hanzhang Wu, PhD, of Tianjin University of Traditional Medicine in Tianjin, China, led the study, which was published online in the International Journal of Behavioral Nutrition and Physical Activity.
LIMITATIONS:
Screen behaviors were assessed using self-report measures, which is subject to recall bias. Also, there may have been variables confounding the findings for which investigators did not account.
DISCLOSURES:
The study was funded by the National Natural Science Foundation of China, the Tianjin Major Public Health Science and Technology Project, the National Health Commission of China, the Food Science and Technology Foundation of Chinese Institute of Food Science and Technology, the China Cohort Consortium, and the Chinese Nutrition Society Nutrition Research Foundation–DSM Research Fund, China. There were no disclosures reported.
Eve Bender has no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
whereas a limited amount of daily computer use that is not work-related is linked to a lower risk for dementia.
METHODOLOGY:
- Investigators analyzed data on 473,184 people aged 39-72 years from the UK Biobank who were enrolled from 2006 to 2010 and followed until a diagnosis of dementia, PD, depression, death, or study end (2018 for Wales residents; 2021 for residents of England and Scotland).
- Participants reported on the number of hours they spent outside of work exercising, watching television, and using the computer.
- MRI was conducted to determine participants’ brain volume.
TAKEAWAY:
- During the study, 6096 people developed dementia, 3000 developed PD, 23,600 developed depression, 1200 developed dementia and depression, and 486 developed PD and depression.
- Compared with those who watched TV for under 1 hour per day, those who reported watching 4 or more hours per day had a 28% higher risk for dementia (adjusted hazard ratio [aHR], 1.28; 95% CI, 1.17-1.39), a 35% higher risk for depression, (aHR, 1.35; 95% CI, 1.29-1.40) and a 16% greater risk for PD (aHR, 1.16; 95% CI, 1.03-1.29).
- However, moderate computer use outside of work seemed somewhat protective. Participants who used the computer for 30-60 minutes per day had lower risks for dementia (aHR, 0.68; 95% CI, 0.64-0.72), PD, (aHR, 0.86; 95% CI, 0.79-0.93), and depression (aHR, 0.85; 95% CI, 0.83-0.88) compared with those who reported the lowest levels of computer usage.
- Replacing 30 minutes per day of computer time with an equal amount of structured exercise was associated with decreased risk for dementia (aHR, 0.74; 95% CI, 0.85-0.95) and PD (aHR, 0.84; 95% CI, 0.78-0.90).
IN PRACTICE:
The association between extended periods of TV use and higher risk for PD and dementia could be explained by a lack of activity, the authors note. They add that sedentary behavior is, “associated with biomarkers of low-grade inflammation and changes in inflammation markers that could initiate and or worsen neuroinflammation and contribute to neurodegeneration.”
SOURCE:
Hanzhang Wu, PhD, of Tianjin University of Traditional Medicine in Tianjin, China, led the study, which was published online in the International Journal of Behavioral Nutrition and Physical Activity.
LIMITATIONS:
Screen behaviors were assessed using self-report measures, which is subject to recall bias. Also, there may have been variables confounding the findings for which investigators did not account.
DISCLOSURES:
The study was funded by the National Natural Science Foundation of China, the Tianjin Major Public Health Science and Technology Project, the National Health Commission of China, the Food Science and Technology Foundation of Chinese Institute of Food Science and Technology, the China Cohort Consortium, and the Chinese Nutrition Society Nutrition Research Foundation–DSM Research Fund, China. There were no disclosures reported.
Eve Bender has no relevant financial relationships.
A version of this article appeared on Medscape.com.
Sleep disorders linked to increased mortality risk in epilepsy
ORLANDO — , new research shows.
SUDEP is a major concern for patients with epilepsy, said study investigator Marion Lazaj, MSc, Center for Neuroscience Studies, Queen’s University, Kingston, Ontario, Canada, but she believes that SUDEP risk assessment is overly focused on seizure control.
“We want to push the idea that this mortality risk assessment needs to be widened to include sleep factors, and not just sleep disorders but even sleep disturbances,” said Ms. Lazaj.
She also believes physicians should routinely discuss SUDEP with their patients with epilepsy. Given that the incidence of SUDEP is only about 1%, many clinicians don’t want to unduly frighten their patients, she added.
The findings were presented at the annual meeting of the American Epilepsy Society (AES).
The retrospective study included chart data from 1,506 consecutive patients diagnosed with epilepsy at a single center over 4 years. The mean age of participants was about 37 years but there was a large age range, said Ms. Lazaj.
The cohort was divided into two groups. Group 1 included 1130 patients without a comorbid sleep disorder, and Group 2 had 376 patients with a primary comorbid sleep disorder, mostly obstructive sleep apnea (OSA) but also restless leg syndrome or insomnia.
They gathered demographic information including age, sex, employment status, education, and epilepsy-related data such as epilepsy type, duration, the number of anti-seizure medications and relevant information from hospital and emergency room (ER) records.
SUDEP Inventory
Researchers assessed SUDEP risk using the revised SUDEP-7 risk inventory. The first four items on this inventory focus on generalized tonic clonic seizure activity and occurrence while others assess the number of antiseizure medicines, epilepsy duration, and the presence of other developmental delays.
Investigators then stratified patients into high risk (score on the SUDEP-7 of 5 or greater) and low mortality risk (score less than 5).
Results showed a significant association between a high mortality risk and having a comorbid sleep disorder (P = .033). Researchers also looked at all-cause mortality, including drownings and suicides, and found a similar significant association (P = .026). There was also an association between high risk and accidents and trauma (P = .042).
The researchers had access to overnight diagnostic polysomnography data for a smaller group of patients. Here, they found decreased sleep efficiency (P =.0098), increased spontaneous arousal index (P = .034), and prolonged sleep onset latency (P = .0000052) were all significantly associated with high SUDEP risk.
From the polysomnographic data, researchers found high SUDEP risk was significantly associated with a diagnosis of OSA (P = .034).
Powerful Study
Commenting on the findings, Gordon F. Buchanan, MD, PhD, Beth L. Tross epilepsy associate professor, Department of Neurology, University of Iowa Carver College of Medicine, Iowa City, said he was “very excited” by the research.
“That this study attempts to look through data in a retrospective way and see if there’s additional risk with having comorbid sleep disorders is really interesting and I think really powerful,” he said.
Sleep disorders “are potentially a really simple thing that we can screen for and test for,” he added. He also noted that additional research is needed to replicate the findings.
Dr. Buchanan acknowledged that the SUDEP-7 inventory is not a particularly good tool and said there is a need for a better means of assessment that includes sleep disorders and other factors like sleep states and circadian rhythm, which he said affect SUDEP risk.
Ms. Lazaj and Dr. Buchanan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ORLANDO — , new research shows.
SUDEP is a major concern for patients with epilepsy, said study investigator Marion Lazaj, MSc, Center for Neuroscience Studies, Queen’s University, Kingston, Ontario, Canada, but she believes that SUDEP risk assessment is overly focused on seizure control.
“We want to push the idea that this mortality risk assessment needs to be widened to include sleep factors, and not just sleep disorders but even sleep disturbances,” said Ms. Lazaj.
She also believes physicians should routinely discuss SUDEP with their patients with epilepsy. Given that the incidence of SUDEP is only about 1%, many clinicians don’t want to unduly frighten their patients, she added.
The findings were presented at the annual meeting of the American Epilepsy Society (AES).
The retrospective study included chart data from 1,506 consecutive patients diagnosed with epilepsy at a single center over 4 years. The mean age of participants was about 37 years but there was a large age range, said Ms. Lazaj.
The cohort was divided into two groups. Group 1 included 1130 patients without a comorbid sleep disorder, and Group 2 had 376 patients with a primary comorbid sleep disorder, mostly obstructive sleep apnea (OSA) but also restless leg syndrome or insomnia.
They gathered demographic information including age, sex, employment status, education, and epilepsy-related data such as epilepsy type, duration, the number of anti-seizure medications and relevant information from hospital and emergency room (ER) records.
SUDEP Inventory
Researchers assessed SUDEP risk using the revised SUDEP-7 risk inventory. The first four items on this inventory focus on generalized tonic clonic seizure activity and occurrence while others assess the number of antiseizure medicines, epilepsy duration, and the presence of other developmental delays.
Investigators then stratified patients into high risk (score on the SUDEP-7 of 5 or greater) and low mortality risk (score less than 5).
Results showed a significant association between a high mortality risk and having a comorbid sleep disorder (P = .033). Researchers also looked at all-cause mortality, including drownings and suicides, and found a similar significant association (P = .026). There was also an association between high risk and accidents and trauma (P = .042).
The researchers had access to overnight diagnostic polysomnography data for a smaller group of patients. Here, they found decreased sleep efficiency (P =.0098), increased spontaneous arousal index (P = .034), and prolonged sleep onset latency (P = .0000052) were all significantly associated with high SUDEP risk.
From the polysomnographic data, researchers found high SUDEP risk was significantly associated with a diagnosis of OSA (P = .034).
Powerful Study
Commenting on the findings, Gordon F. Buchanan, MD, PhD, Beth L. Tross epilepsy associate professor, Department of Neurology, University of Iowa Carver College of Medicine, Iowa City, said he was “very excited” by the research.
“That this study attempts to look through data in a retrospective way and see if there’s additional risk with having comorbid sleep disorders is really interesting and I think really powerful,” he said.
Sleep disorders “are potentially a really simple thing that we can screen for and test for,” he added. He also noted that additional research is needed to replicate the findings.
Dr. Buchanan acknowledged that the SUDEP-7 inventory is not a particularly good tool and said there is a need for a better means of assessment that includes sleep disorders and other factors like sleep states and circadian rhythm, which he said affect SUDEP risk.
Ms. Lazaj and Dr. Buchanan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ORLANDO — , new research shows.
SUDEP is a major concern for patients with epilepsy, said study investigator Marion Lazaj, MSc, Center for Neuroscience Studies, Queen’s University, Kingston, Ontario, Canada, but she believes that SUDEP risk assessment is overly focused on seizure control.
“We want to push the idea that this mortality risk assessment needs to be widened to include sleep factors, and not just sleep disorders but even sleep disturbances,” said Ms. Lazaj.
She also believes physicians should routinely discuss SUDEP with their patients with epilepsy. Given that the incidence of SUDEP is only about 1%, many clinicians don’t want to unduly frighten their patients, she added.
The findings were presented at the annual meeting of the American Epilepsy Society (AES).
The retrospective study included chart data from 1,506 consecutive patients diagnosed with epilepsy at a single center over 4 years. The mean age of participants was about 37 years but there was a large age range, said Ms. Lazaj.
The cohort was divided into two groups. Group 1 included 1130 patients without a comorbid sleep disorder, and Group 2 had 376 patients with a primary comorbid sleep disorder, mostly obstructive sleep apnea (OSA) but also restless leg syndrome or insomnia.
They gathered demographic information including age, sex, employment status, education, and epilepsy-related data such as epilepsy type, duration, the number of anti-seizure medications and relevant information from hospital and emergency room (ER) records.
SUDEP Inventory
Researchers assessed SUDEP risk using the revised SUDEP-7 risk inventory. The first four items on this inventory focus on generalized tonic clonic seizure activity and occurrence while others assess the number of antiseizure medicines, epilepsy duration, and the presence of other developmental delays.
Investigators then stratified patients into high risk (score on the SUDEP-7 of 5 or greater) and low mortality risk (score less than 5).
Results showed a significant association between a high mortality risk and having a comorbid sleep disorder (P = .033). Researchers also looked at all-cause mortality, including drownings and suicides, and found a similar significant association (P = .026). There was also an association between high risk and accidents and trauma (P = .042).
The researchers had access to overnight diagnostic polysomnography data for a smaller group of patients. Here, they found decreased sleep efficiency (P =.0098), increased spontaneous arousal index (P = .034), and prolonged sleep onset latency (P = .0000052) were all significantly associated with high SUDEP risk.
From the polysomnographic data, researchers found high SUDEP risk was significantly associated with a diagnosis of OSA (P = .034).
Powerful Study
Commenting on the findings, Gordon F. Buchanan, MD, PhD, Beth L. Tross epilepsy associate professor, Department of Neurology, University of Iowa Carver College of Medicine, Iowa City, said he was “very excited” by the research.
“That this study attempts to look through data in a retrospective way and see if there’s additional risk with having comorbid sleep disorders is really interesting and I think really powerful,” he said.
Sleep disorders “are potentially a really simple thing that we can screen for and test for,” he added. He also noted that additional research is needed to replicate the findings.
Dr. Buchanan acknowledged that the SUDEP-7 inventory is not a particularly good tool and said there is a need for a better means of assessment that includes sleep disorders and other factors like sleep states and circadian rhythm, which he said affect SUDEP risk.
Ms. Lazaj and Dr. Buchanan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AES 2023
Are you sure your patient is alive?
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.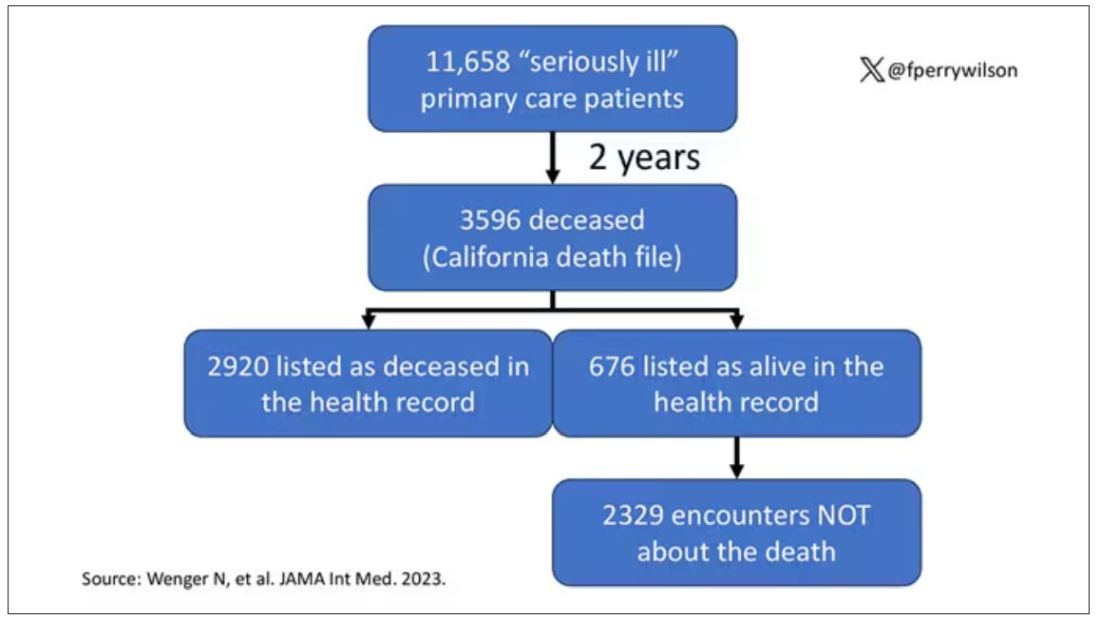
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.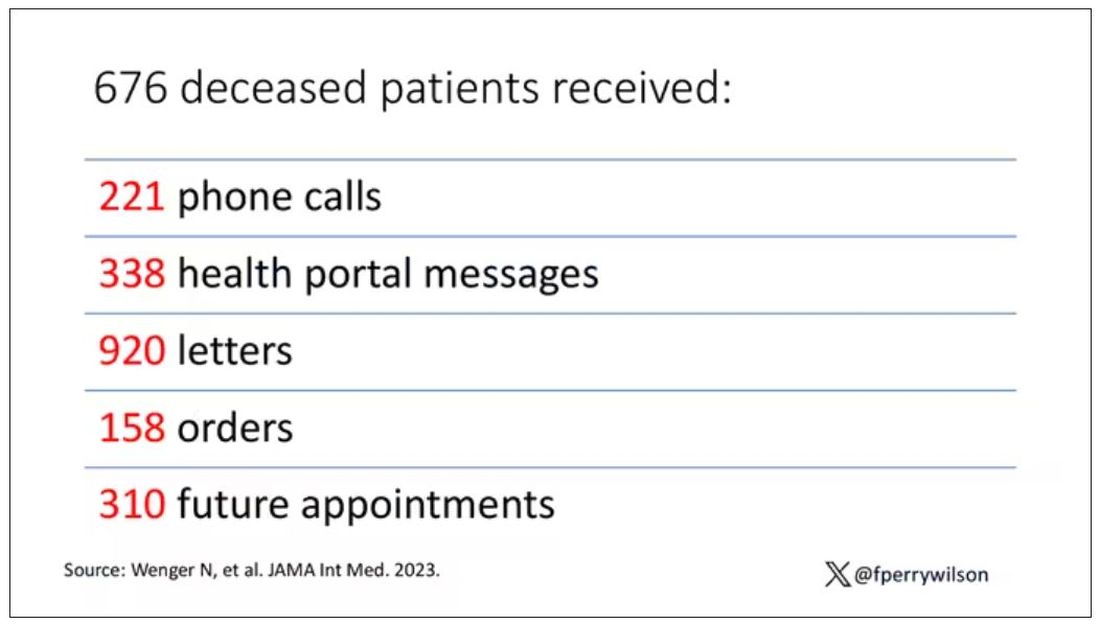
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.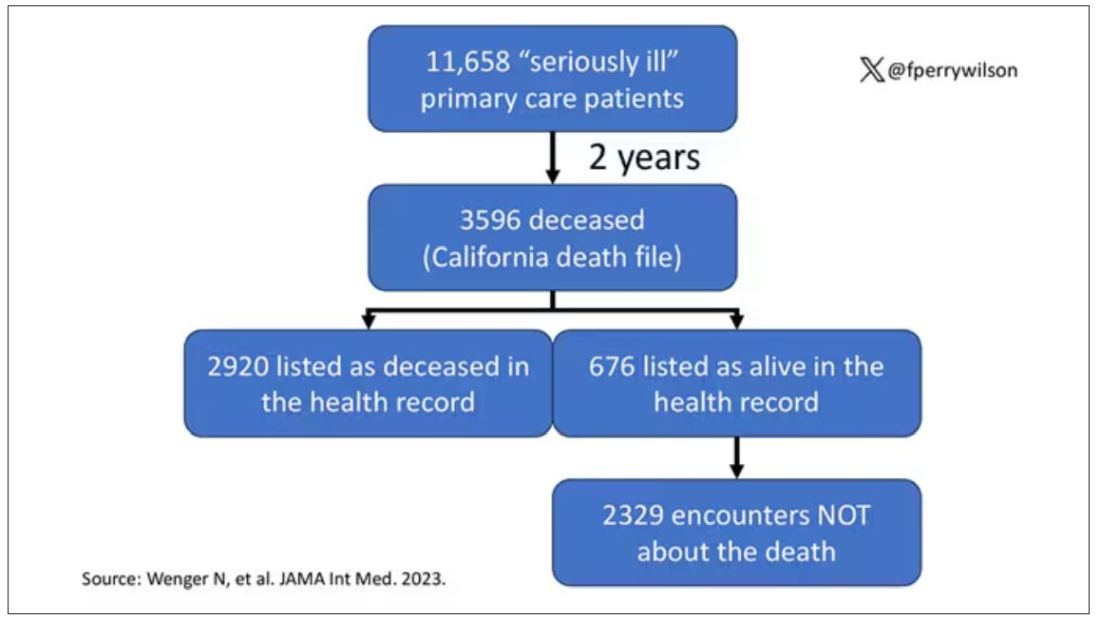
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.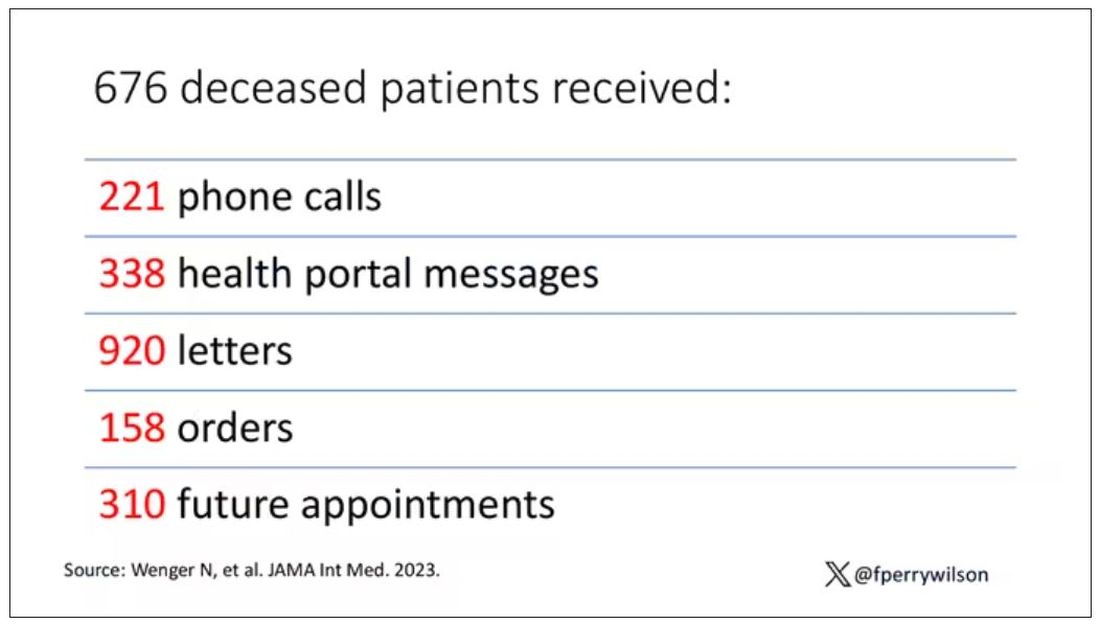
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.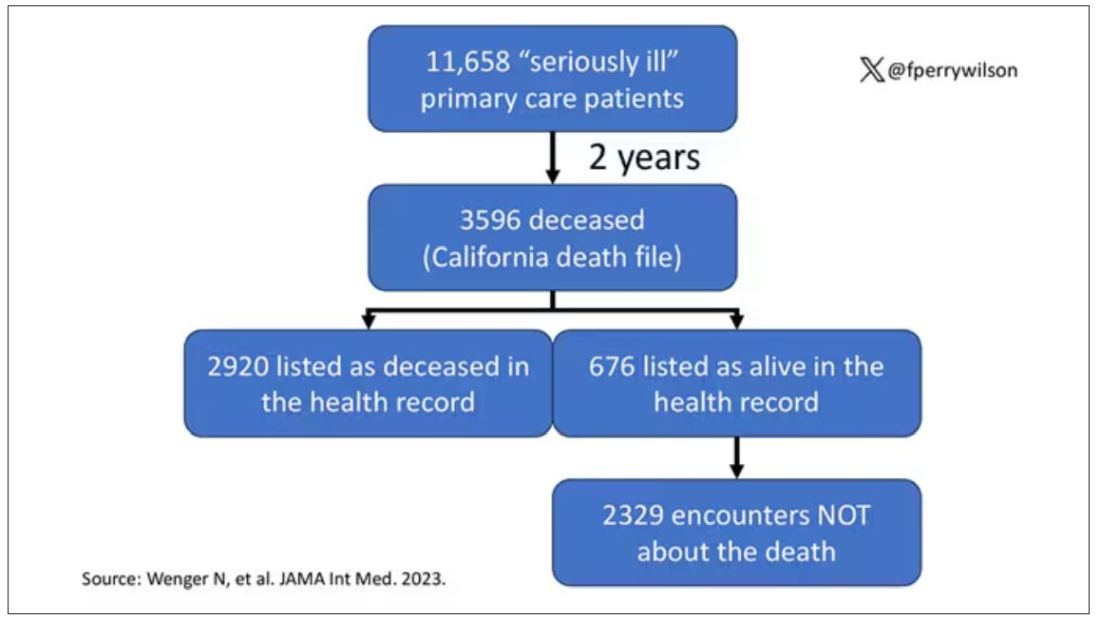
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.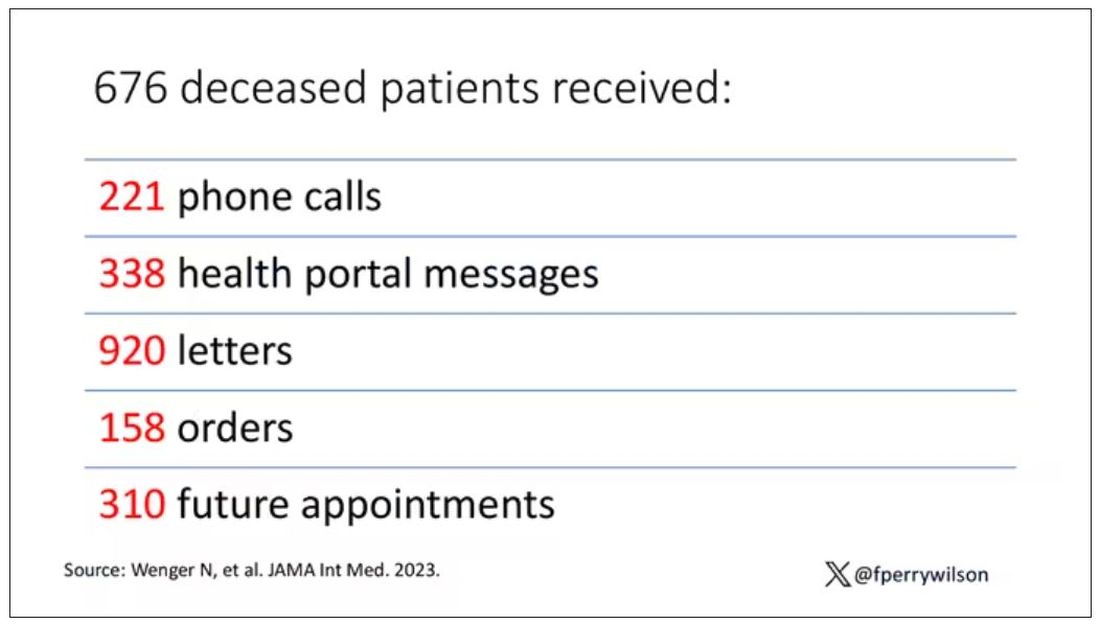
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
MDMA therapy for loneliness? Researchers say it could work
Some call the drug “ecstasy” or “molly.” Researchers are calling it a potential tool to help treat loneliness.
As public health experts sound the alarm on a rising loneliness epidemic in the United States and across the globe,
In the latest study, MDMA “led to a robust increase in feelings of connection” among people socializing in a controlled setting. Participants were dosed with either MDMA or a placebo and asked to chat with a stranger. Afterward, those who took MDMA said their companion was more responsive and attentive, and that they had plenty in common. The drug also “increased participants’ ratings of liking their partners, feeling connected and finding the conversation enjoyable and meaningful.”
The study was small — just 18 participants — but its results “have implications for MDMA-assisted therapy,” the authors wrote. “This feeling of connectedness could help patients feel safe and trusting, thereby facilitating deeper emotional exploration.”
MDMA “really does seem to make people want to interact more with other people,” says Harriet de Wit, PhD, a neuropharmacologist at the University of Chicago and one of the study’s authors. The results echo those of earlier research using psychedelics like LSD or psilocybin.
It’s important to note that any intervention involving MDMA or psychedelics would be a drug-assisted therapy — that is, used in conjunction with the appropriate therapy and in a therapeutic setting. MDMA-assisted therapy has already drawn popular and scientific attention, as it recently cleared clinical trials for treating posttraumatic stress disorder (PTSD) and may be nearing approval by the US Food and Drug Administration (FDA).
According to Friederike Holze, PhD, psychopharmacologist at the University of Basel, in Switzerland, “there could be a place” for MDMA and psychedelics in treating chronic loneliness, but only under professional supervision.
There would have to be clear guidelines too, says Joshua Woolley, MD, PhD, a psychiatrist at the University of California, San Francisco.
MDMA and psychedelics “induce this plastic state, a state where people can change. They feel open, they feel like things are possible,” Dr. Woolley says. Then, with therapy, “you can help them change.”
Loneliness Can Impact Our Health
On top of the mental health ramifications, the physiologic effects of loneliness could have grave consequences over time. In observational studies, loneliness has been linked to higher risks for cancer and heart disease, and shorter lifespan. One third of Americans over 45 say they are chronically lonely.
Chronic loneliness changes how we think and behave, research shows. It makes us fear contact with others and see them in a more negative light, as more threatening and less trustworthy. Lonely people prefer to stand farther apart from strangers and avoid touch.
This is where MDMA-assisted therapies could potentially help, by easing these defensive tendencies, according to Dr. Woolley.
MDMA, Psychedelics, and Social Behavior
MDMA, or 3,4-methylenedioxymethamphetamine, is a hybrid between a stimulant and a psychedelic. In Dr. de Wit’s earlier experiments, volunteers given MDMA engaged more in communal activities, chatting, and playing games. They used more positive words during social encounters than those who had received a placebo. And after MDMA, people felt less rejected if they were slighted in Cyberball — a virtual ball-tossing game commonly used to measure the effects of social exclusion.
MDMA has been shown to reduce people’s response to other’s negative emotions, diminishing activation of the amygdala (the brain’s fear center) while looking at pictures of angry faces.
This could be helpful. “If you perceive a person’s natural expression as being a little bit angry, if that disappears, then you might be more inclined to interact,” de Wit says.
However, there may be downsides, too. If a drug makes people more trusting and willing to connect, they could be taken advantage of. This is why, Dr. Woolley says, “psychedelics have been used in cults.”
MDMA may also make the experience of touch more pleasant. In a series of experiments in 2019, researchers gently stroked volunteers ’ arms with a goat-hair brush, mimicking the comforting gestures one may receive from a loved one. At the same time, the scientists monitored the volunteers’ facial muscles. People on MDMA perceived gentle touch as more pleasant than those on placebo, and their smile muscles activated more.
MDMA and psychedelics boost social behaviors in animals, too — suggesting that their effects on relationships have a biological basis. Rats on MDMA are more likely to lie next to each other, and mice become more resilient to social stress. Even octopuses become more outgoing after a dose of MDMA, choosing to spend more time with other octopuses instead of a new toy. Classic psychedelics show similar effects — LSD, for example, makes mice more social.
Psychedelics can induce a sense of a “dissolution of the self-other boundary,” Dr. Woolley says. People who take them often say it’s “helped them feel more connected to themselves and other people.” LSD, first synthesized in 1938, may help increase empathy in some people.
Psilocybin, a compound found in over 200 species of mushrooms and used for centuries in Mesoamerican rituals, also seems to boost empathy, with effects persisting for at least seven days. In Cyberball, the online ball-throwing game, people who took psilocybin felt less socially rejected, an outcome reflected in their brain activation patterns in one study — the areas responsible for social-pain processing appeared to dim after a dose.
Making It Legal and Putting It to Use
In 2020, Oregon became the first state to establish a regulatory framework for psilocybin for therapeutic use, and Colorado followed suit in 2022. Such therapeutic applications of psilocybin could help fight loneliness as well, Dr. Woolley believes, because a “ common symptom of depression is that people feel socially withdrawn and lack motivation, ” he says. As mentioned above, MDMA-assisted therapy is also nearing FDA approval for PTSD.
What remain unclear are the exact mechanisms at play.
“MDMA releases oxytocin, and it does that through serotonin receptors,” Dr. de Wit says. Serotonin activates 5-HT1A receptors in the hypothalamus, releasing oxytocin into the bloodstream. In Dr. de Wit’s recent experiments, the more people felt connected after taking MDMA, the more oxytocin was found circulating in their bodies. (Another drug, methamphetamine, also upped the levels of oxytocin but did not increase feelings of connectedness.)
“It’s likely that both something in the serotonin system independent of oxytocin, and oxytocin itself, contribute,” Dr. de Wit says. Dopamine, a neurotransmitter responsible for motivation, appears to increase as well.
The empathy-boosting effects of LSD also seem to be at least partly driven by oxytocin, experiments published in 2021 revealed. Studies in mice, meanwhile, suggest that glutamate, a chemical messenger in the brain, may be behind some of LSD’s prosocial effects.
Scientists are fairly certain which receptors these drugs bind to and which neurotransmitters they affect. “How that gets translated into these higher-order things like empathy and feeling connected to the world, we don’t totally understand,” Dr. Woolley says.
Challenges and the Future
Although MDMA and psychedelics are largely considered safe when taken in a legal, medically controlled setting, there is reason to be cautious.
“They have relatively low impact on the body, like heart rate increase or blood pressure increase. But they might leave some disturbing psychological effects,” says Dr. Holze. Scientists routinely screen experiment volunteers for their risk for psychiatric disorders.
Although risk for addiction is low with both MDMA and psychedelics, there is always some risk for misuse. MDMA “ can produce feelings of well-being, and then people might use it repeatedly, ” Dr. de Wit says. “ That doesn ’ t seem to be a problem for really a lot of people, but it could easily happen. ”
Still, possibilities remain for MDMA in the fight against loneliness.
“[People] feel open, they feel like things are possible, they feel like they’re unstuck,” Dr. Woolley says. “You can harness that in psychotherapy.”
A version of this article appeared on Medscape.com.
Some call the drug “ecstasy” or “molly.” Researchers are calling it a potential tool to help treat loneliness.
As public health experts sound the alarm on a rising loneliness epidemic in the United States and across the globe,
In the latest study, MDMA “led to a robust increase in feelings of connection” among people socializing in a controlled setting. Participants were dosed with either MDMA or a placebo and asked to chat with a stranger. Afterward, those who took MDMA said their companion was more responsive and attentive, and that they had plenty in common. The drug also “increased participants’ ratings of liking their partners, feeling connected and finding the conversation enjoyable and meaningful.”
The study was small — just 18 participants — but its results “have implications for MDMA-assisted therapy,” the authors wrote. “This feeling of connectedness could help patients feel safe and trusting, thereby facilitating deeper emotional exploration.”
MDMA “really does seem to make people want to interact more with other people,” says Harriet de Wit, PhD, a neuropharmacologist at the University of Chicago and one of the study’s authors. The results echo those of earlier research using psychedelics like LSD or psilocybin.
It’s important to note that any intervention involving MDMA or psychedelics would be a drug-assisted therapy — that is, used in conjunction with the appropriate therapy and in a therapeutic setting. MDMA-assisted therapy has already drawn popular and scientific attention, as it recently cleared clinical trials for treating posttraumatic stress disorder (PTSD) and may be nearing approval by the US Food and Drug Administration (FDA).
According to Friederike Holze, PhD, psychopharmacologist at the University of Basel, in Switzerland, “there could be a place” for MDMA and psychedelics in treating chronic loneliness, but only under professional supervision.
There would have to be clear guidelines too, says Joshua Woolley, MD, PhD, a psychiatrist at the University of California, San Francisco.
MDMA and psychedelics “induce this plastic state, a state where people can change. They feel open, they feel like things are possible,” Dr. Woolley says. Then, with therapy, “you can help them change.”
Loneliness Can Impact Our Health
On top of the mental health ramifications, the physiologic effects of loneliness could have grave consequences over time. In observational studies, loneliness has been linked to higher risks for cancer and heart disease, and shorter lifespan. One third of Americans over 45 say they are chronically lonely.
Chronic loneliness changes how we think and behave, research shows. It makes us fear contact with others and see them in a more negative light, as more threatening and less trustworthy. Lonely people prefer to stand farther apart from strangers and avoid touch.
This is where MDMA-assisted therapies could potentially help, by easing these defensive tendencies, according to Dr. Woolley.
MDMA, Psychedelics, and Social Behavior
MDMA, or 3,4-methylenedioxymethamphetamine, is a hybrid between a stimulant and a psychedelic. In Dr. de Wit’s earlier experiments, volunteers given MDMA engaged more in communal activities, chatting, and playing games. They used more positive words during social encounters than those who had received a placebo. And after MDMA, people felt less rejected if they were slighted in Cyberball — a virtual ball-tossing game commonly used to measure the effects of social exclusion.
MDMA has been shown to reduce people’s response to other’s negative emotions, diminishing activation of the amygdala (the brain’s fear center) while looking at pictures of angry faces.
This could be helpful. “If you perceive a person’s natural expression as being a little bit angry, if that disappears, then you might be more inclined to interact,” de Wit says.
However, there may be downsides, too. If a drug makes people more trusting and willing to connect, they could be taken advantage of. This is why, Dr. Woolley says, “psychedelics have been used in cults.”
MDMA may also make the experience of touch more pleasant. In a series of experiments in 2019, researchers gently stroked volunteers ’ arms with a goat-hair brush, mimicking the comforting gestures one may receive from a loved one. At the same time, the scientists monitored the volunteers’ facial muscles. People on MDMA perceived gentle touch as more pleasant than those on placebo, and their smile muscles activated more.
MDMA and psychedelics boost social behaviors in animals, too — suggesting that their effects on relationships have a biological basis. Rats on MDMA are more likely to lie next to each other, and mice become more resilient to social stress. Even octopuses become more outgoing after a dose of MDMA, choosing to spend more time with other octopuses instead of a new toy. Classic psychedelics show similar effects — LSD, for example, makes mice more social.
Psychedelics can induce a sense of a “dissolution of the self-other boundary,” Dr. Woolley says. People who take them often say it’s “helped them feel more connected to themselves and other people.” LSD, first synthesized in 1938, may help increase empathy in some people.
Psilocybin, a compound found in over 200 species of mushrooms and used for centuries in Mesoamerican rituals, also seems to boost empathy, with effects persisting for at least seven days. In Cyberball, the online ball-throwing game, people who took psilocybin felt less socially rejected, an outcome reflected in their brain activation patterns in one study — the areas responsible for social-pain processing appeared to dim after a dose.
Making It Legal and Putting It to Use
In 2020, Oregon became the first state to establish a regulatory framework for psilocybin for therapeutic use, and Colorado followed suit in 2022. Such therapeutic applications of psilocybin could help fight loneliness as well, Dr. Woolley believes, because a “ common symptom of depression is that people feel socially withdrawn and lack motivation, ” he says. As mentioned above, MDMA-assisted therapy is also nearing FDA approval for PTSD.
What remain unclear are the exact mechanisms at play.
“MDMA releases oxytocin, and it does that through serotonin receptors,” Dr. de Wit says. Serotonin activates 5-HT1A receptors in the hypothalamus, releasing oxytocin into the bloodstream. In Dr. de Wit’s recent experiments, the more people felt connected after taking MDMA, the more oxytocin was found circulating in their bodies. (Another drug, methamphetamine, also upped the levels of oxytocin but did not increase feelings of connectedness.)
“It’s likely that both something in the serotonin system independent of oxytocin, and oxytocin itself, contribute,” Dr. de Wit says. Dopamine, a neurotransmitter responsible for motivation, appears to increase as well.
The empathy-boosting effects of LSD also seem to be at least partly driven by oxytocin, experiments published in 2021 revealed. Studies in mice, meanwhile, suggest that glutamate, a chemical messenger in the brain, may be behind some of LSD’s prosocial effects.
Scientists are fairly certain which receptors these drugs bind to and which neurotransmitters they affect. “How that gets translated into these higher-order things like empathy and feeling connected to the world, we don’t totally understand,” Dr. Woolley says.
Challenges and the Future
Although MDMA and psychedelics are largely considered safe when taken in a legal, medically controlled setting, there is reason to be cautious.
“They have relatively low impact on the body, like heart rate increase or blood pressure increase. But they might leave some disturbing psychological effects,” says Dr. Holze. Scientists routinely screen experiment volunteers for their risk for psychiatric disorders.
Although risk for addiction is low with both MDMA and psychedelics, there is always some risk for misuse. MDMA “ can produce feelings of well-being, and then people might use it repeatedly, ” Dr. de Wit says. “ That doesn ’ t seem to be a problem for really a lot of people, but it could easily happen. ”
Still, possibilities remain for MDMA in the fight against loneliness.
“[People] feel open, they feel like things are possible, they feel like they’re unstuck,” Dr. Woolley says. “You can harness that in psychotherapy.”
A version of this article appeared on Medscape.com.
Some call the drug “ecstasy” or “molly.” Researchers are calling it a potential tool to help treat loneliness.
As public health experts sound the alarm on a rising loneliness epidemic in the United States and across the globe,
In the latest study, MDMA “led to a robust increase in feelings of connection” among people socializing in a controlled setting. Participants were dosed with either MDMA or a placebo and asked to chat with a stranger. Afterward, those who took MDMA said their companion was more responsive and attentive, and that they had plenty in common. The drug also “increased participants’ ratings of liking their partners, feeling connected and finding the conversation enjoyable and meaningful.”
The study was small — just 18 participants — but its results “have implications for MDMA-assisted therapy,” the authors wrote. “This feeling of connectedness could help patients feel safe and trusting, thereby facilitating deeper emotional exploration.”
MDMA “really does seem to make people want to interact more with other people,” says Harriet de Wit, PhD, a neuropharmacologist at the University of Chicago and one of the study’s authors. The results echo those of earlier research using psychedelics like LSD or psilocybin.
It’s important to note that any intervention involving MDMA or psychedelics would be a drug-assisted therapy — that is, used in conjunction with the appropriate therapy and in a therapeutic setting. MDMA-assisted therapy has already drawn popular and scientific attention, as it recently cleared clinical trials for treating posttraumatic stress disorder (PTSD) and may be nearing approval by the US Food and Drug Administration (FDA).
According to Friederike Holze, PhD, psychopharmacologist at the University of Basel, in Switzerland, “there could be a place” for MDMA and psychedelics in treating chronic loneliness, but only under professional supervision.
There would have to be clear guidelines too, says Joshua Woolley, MD, PhD, a psychiatrist at the University of California, San Francisco.
MDMA and psychedelics “induce this plastic state, a state where people can change. They feel open, they feel like things are possible,” Dr. Woolley says. Then, with therapy, “you can help them change.”
Loneliness Can Impact Our Health
On top of the mental health ramifications, the physiologic effects of loneliness could have grave consequences over time. In observational studies, loneliness has been linked to higher risks for cancer and heart disease, and shorter lifespan. One third of Americans over 45 say they are chronically lonely.
Chronic loneliness changes how we think and behave, research shows. It makes us fear contact with others and see them in a more negative light, as more threatening and less trustworthy. Lonely people prefer to stand farther apart from strangers and avoid touch.
This is where MDMA-assisted therapies could potentially help, by easing these defensive tendencies, according to Dr. Woolley.
MDMA, Psychedelics, and Social Behavior
MDMA, or 3,4-methylenedioxymethamphetamine, is a hybrid between a stimulant and a psychedelic. In Dr. de Wit’s earlier experiments, volunteers given MDMA engaged more in communal activities, chatting, and playing games. They used more positive words during social encounters than those who had received a placebo. And after MDMA, people felt less rejected if they were slighted in Cyberball — a virtual ball-tossing game commonly used to measure the effects of social exclusion.
MDMA has been shown to reduce people’s response to other’s negative emotions, diminishing activation of the amygdala (the brain’s fear center) while looking at pictures of angry faces.
This could be helpful. “If you perceive a person’s natural expression as being a little bit angry, if that disappears, then you might be more inclined to interact,” de Wit says.
However, there may be downsides, too. If a drug makes people more trusting and willing to connect, they could be taken advantage of. This is why, Dr. Woolley says, “psychedelics have been used in cults.”
MDMA may also make the experience of touch more pleasant. In a series of experiments in 2019, researchers gently stroked volunteers ’ arms with a goat-hair brush, mimicking the comforting gestures one may receive from a loved one. At the same time, the scientists monitored the volunteers’ facial muscles. People on MDMA perceived gentle touch as more pleasant than those on placebo, and their smile muscles activated more.
MDMA and psychedelics boost social behaviors in animals, too — suggesting that their effects on relationships have a biological basis. Rats on MDMA are more likely to lie next to each other, and mice become more resilient to social stress. Even octopuses become more outgoing after a dose of MDMA, choosing to spend more time with other octopuses instead of a new toy. Classic psychedelics show similar effects — LSD, for example, makes mice more social.
Psychedelics can induce a sense of a “dissolution of the self-other boundary,” Dr. Woolley says. People who take them often say it’s “helped them feel more connected to themselves and other people.” LSD, first synthesized in 1938, may help increase empathy in some people.
Psilocybin, a compound found in over 200 species of mushrooms and used for centuries in Mesoamerican rituals, also seems to boost empathy, with effects persisting for at least seven days. In Cyberball, the online ball-throwing game, people who took psilocybin felt less socially rejected, an outcome reflected in their brain activation patterns in one study — the areas responsible for social-pain processing appeared to dim after a dose.
Making It Legal and Putting It to Use
In 2020, Oregon became the first state to establish a regulatory framework for psilocybin for therapeutic use, and Colorado followed suit in 2022. Such therapeutic applications of psilocybin could help fight loneliness as well, Dr. Woolley believes, because a “ common symptom of depression is that people feel socially withdrawn and lack motivation, ” he says. As mentioned above, MDMA-assisted therapy is also nearing FDA approval for PTSD.
What remain unclear are the exact mechanisms at play.
“MDMA releases oxytocin, and it does that through serotonin receptors,” Dr. de Wit says. Serotonin activates 5-HT1A receptors in the hypothalamus, releasing oxytocin into the bloodstream. In Dr. de Wit’s recent experiments, the more people felt connected after taking MDMA, the more oxytocin was found circulating in their bodies. (Another drug, methamphetamine, also upped the levels of oxytocin but did not increase feelings of connectedness.)
“It’s likely that both something in the serotonin system independent of oxytocin, and oxytocin itself, contribute,” Dr. de Wit says. Dopamine, a neurotransmitter responsible for motivation, appears to increase as well.
The empathy-boosting effects of LSD also seem to be at least partly driven by oxytocin, experiments published in 2021 revealed. Studies in mice, meanwhile, suggest that glutamate, a chemical messenger in the brain, may be behind some of LSD’s prosocial effects.
Scientists are fairly certain which receptors these drugs bind to and which neurotransmitters they affect. “How that gets translated into these higher-order things like empathy and feeling connected to the world, we don’t totally understand,” Dr. Woolley says.
Challenges and the Future
Although MDMA and psychedelics are largely considered safe when taken in a legal, medically controlled setting, there is reason to be cautious.
“They have relatively low impact on the body, like heart rate increase or blood pressure increase. But they might leave some disturbing psychological effects,” says Dr. Holze. Scientists routinely screen experiment volunteers for their risk for psychiatric disorders.
Although risk for addiction is low with both MDMA and psychedelics, there is always some risk for misuse. MDMA “ can produce feelings of well-being, and then people might use it repeatedly, ” Dr. de Wit says. “ That doesn ’ t seem to be a problem for really a lot of people, but it could easily happen. ”
Still, possibilities remain for MDMA in the fight against loneliness.
“[People] feel open, they feel like things are possible, they feel like they’re unstuck,” Dr. Woolley says. “You can harness that in psychotherapy.”
A version of this article appeared on Medscape.com.
Higher blood levels of oleic acid tied to depression
TOPLINE:
National survey data reveal an association between higher serum oleic acid levels and depression in adults, new research shows.
METHODOLOGY:
Oleic acid is the most abundant fatty acid in plasma and has been associated with multiple neurologic diseases. However, the relationship between oleic acid and depression is unclear.
This cross-sectional analyzed data on 4459 adults from the 2011-2014 National Health and Nutrition Examination Survey (NHANES).
Multivariable logistic regression models adjusting for demographics, health and lifestyle factors quantified the association between oleic acid levels and depression. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) with depression defined as a score ≥ 10.
TAKEAWAY:
Serum oleic acid levels were positively associated with depression before and after multivariable adjustment.
After adjusting for all covariates, for every 1 mmol/L increase in serum oleic acid levels, the prevalence of depression increased by 40% (adjusted odds ratio [aOR], 1.40; 95% CI, 1.03-1.90).
Adults in the top quartile of oleic acid (≥ 2.51 mmol/L) had a greater than twofold higher likelihood of depression (aOR, 2.22; 95% CI, 1.04-4.73) compared with peers in the lowest quartile (≤ 1.54 mmol/L).
IN PRACTICE:
“A better understanding of the role of oleic acid in depression may lead to new preventive and therapeutic methods. Thus, carefully designed prospective studies are necessary to explore the positive effects of changing serum oleic acid levels through diet, medicine, or other measures on depression,” the authors write.
SOURCE:
The study, with first author Jiahui Yin of Shandong University of Traditional Chinese Medicine in Jinan, China, was published online on November 16, 2023 in BMC Psychiatry .
LIMITATIONS:
The cross-sectional study can’t prove causality. The findings may not apply to clinically diagnosed major depressive disorder.
DISCLOSURES:
The study had no specific funding. The authors report no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
National survey data reveal an association between higher serum oleic acid levels and depression in adults, new research shows.
METHODOLOGY:
Oleic acid is the most abundant fatty acid in plasma and has been associated with multiple neurologic diseases. However, the relationship between oleic acid and depression is unclear.
This cross-sectional analyzed data on 4459 adults from the 2011-2014 National Health and Nutrition Examination Survey (NHANES).
Multivariable logistic regression models adjusting for demographics, health and lifestyle factors quantified the association between oleic acid levels and depression. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) with depression defined as a score ≥ 10.
TAKEAWAY:
Serum oleic acid levels were positively associated with depression before and after multivariable adjustment.
After adjusting for all covariates, for every 1 mmol/L increase in serum oleic acid levels, the prevalence of depression increased by 40% (adjusted odds ratio [aOR], 1.40; 95% CI, 1.03-1.90).
Adults in the top quartile of oleic acid (≥ 2.51 mmol/L) had a greater than twofold higher likelihood of depression (aOR, 2.22; 95% CI, 1.04-4.73) compared with peers in the lowest quartile (≤ 1.54 mmol/L).
IN PRACTICE:
“A better understanding of the role of oleic acid in depression may lead to new preventive and therapeutic methods. Thus, carefully designed prospective studies are necessary to explore the positive effects of changing serum oleic acid levels through diet, medicine, or other measures on depression,” the authors write.
SOURCE:
The study, with first author Jiahui Yin of Shandong University of Traditional Chinese Medicine in Jinan, China, was published online on November 16, 2023 in BMC Psychiatry .
LIMITATIONS:
The cross-sectional study can’t prove causality. The findings may not apply to clinically diagnosed major depressive disorder.
DISCLOSURES:
The study had no specific funding. The authors report no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
National survey data reveal an association between higher serum oleic acid levels and depression in adults, new research shows.
METHODOLOGY:
Oleic acid is the most abundant fatty acid in plasma and has been associated with multiple neurologic diseases. However, the relationship between oleic acid and depression is unclear.
This cross-sectional analyzed data on 4459 adults from the 2011-2014 National Health and Nutrition Examination Survey (NHANES).
Multivariable logistic regression models adjusting for demographics, health and lifestyle factors quantified the association between oleic acid levels and depression. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) with depression defined as a score ≥ 10.
TAKEAWAY:
Serum oleic acid levels were positively associated with depression before and after multivariable adjustment.
After adjusting for all covariates, for every 1 mmol/L increase in serum oleic acid levels, the prevalence of depression increased by 40% (adjusted odds ratio [aOR], 1.40; 95% CI, 1.03-1.90).
Adults in the top quartile of oleic acid (≥ 2.51 mmol/L) had a greater than twofold higher likelihood of depression (aOR, 2.22; 95% CI, 1.04-4.73) compared with peers in the lowest quartile (≤ 1.54 mmol/L).
IN PRACTICE:
“A better understanding of the role of oleic acid in depression may lead to new preventive and therapeutic methods. Thus, carefully designed prospective studies are necessary to explore the positive effects of changing serum oleic acid levels through diet, medicine, or other measures on depression,” the authors write.
SOURCE:
The study, with first author Jiahui Yin of Shandong University of Traditional Chinese Medicine in Jinan, China, was published online on November 16, 2023 in BMC Psychiatry .
LIMITATIONS:
The cross-sectional study can’t prove causality. The findings may not apply to clinically diagnosed major depressive disorder.
DISCLOSURES:
The study had no specific funding. The authors report no conflicts of interest.
A version of this article first appeared on Medscape.com.





