User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
‘We will get through this’: Advice for lessening your pandemic anxiety
The COVID-19 pandemic is an experience that is unprecedented in our lifetime. It is having a pervasive effect due to how mysterious, potentially dangerous, and sustained it is. We don’t know how bad it’s going to get or how long it’s going to last. We have natural disasters like hurricanes and earthquakes, but they are limited in time and scope. But this global pandemic is something we can’t put our arms around just yet, breeding uncertainty, worry, and fear. This is where mental health professionals need to come in.
The populations being affected by this pandemic can be placed into different groups on the basis of their mental health consequences and needs. First you have, for lack of a better term, “the worried well.” These are people with no preexisting mental disorder who are naturally worried by this and are trying to take appropriate actions to protect themselves and prepare. For such individuals, the equivalent of mental health first-aid should be useful (we’ll come back to that in a moment). Given the proper guidance and sources of information, most such people should be able to manage the anxiety, worry, and dysphoria associated with this critical pandemic.
Then there are those who have preexisting mental conditions related to mood, anxiety, stress, or obsessive tendencies. They are probably going to have an increase in their symptoms, and as such, a corresponding need for adjusting treatment. This may require an increase in their existing medications or the addition of an ad hoc medication, or perhaps more frequent contact with their doctor or therapist.
Because travel and direct visitation is discouraged at the moment, virtual methods of communication should be used to speak with these patients. Such methods have long existed but haven’t been adopted in large numbers; this may be the impetus to finally make it happen. Using the telephone, FaceTime, Skype, WebEx, Zoom, and other means of videoconferencing should be feasible. As billing procedures are being adapted for this moment, there’s no reason why individuals shouldn’t be able to contact their mental health provider.
Substance abuse is also a condition vulnerable to the stress effects of this pandemic. This will prompt or tempt those to use substances that they’ve abused or turned to in the past as a way of self-medicating and assuaging their anxiety and worry.
It’s possible that the pandemic could find its way into delusions or exacerbate symptoms, but somewhat paradoxically, people with serious mental illnesses often respond more calmly to crises than do individuals without them. As a result, the number of these patients requiring emergency room admission for possible exacerbation of symptoms is probably not going to be that much greater than normal.
How to Cope With an Unprecedented Situation
For the worried well and for the clinicians who have understandable fears about exposure, there are several things you can try to manage your anxiety. There are concentric circles of concern that you have to maintain. Think of it like the instructions on an airplane when, if there’s a drop in cabin pressure, you’re asked to apply your own oxygen mask first before placing one on your child. In the same way, you must first think about protecting yourself by limiting your exposure and monitoring your own physical state for any symptoms. But then you must be concerned about your family, your friends, and also society. This is a situation where the impulse and the ethos of worrying about your fellow persons—being your brother’s keeper—is imperative.
The epidemic has been successfully managed in some countries, like Singapore and China, which, once they got on top of it, were able to limit contagion in a very dramatic way. But these are authoritarian governments. The United States doesn’t work that way, which is what makes appealing to the principle of caring for others so crucial. You can protect yourself, but if other people aren’t also protected, it may not matter. You have to worry not just about yourself but about everyone else.
When it comes to stress management, I recommend not catastrophizing or watching the news media 24/7. Distract yourself with other work or recreational activities. Reach out and communicate—virtually, of course—with friends, family, and healthcare providers as needed. Staying in touch acts not just as a diversion but also as an outlet for assuaging your feelings, your sense of being in this alone, feeling isolated.
There are also cognitive reframing mechanisms you can employ. Consider that although this is bad, some countries have already gone through it. And we’ll get through it too. You’ll understandably ask yourself what it would mean if you were to be exposed. In most cases you can say, “I’m going to have the flu and symptoms that are not going to be pleasant, but I’ve had the flu or serious sickness before.”
Remember that there are already antiretroviral treatments being tested in clinical trials and showing efficacy. It’s good to know that before this pandemic ends, some of these treatments will probably be clinically applied, mostly to those who are severely affected and in intensive care.
Diagnose yourself. Monitor your state. Determine whether the stress is really having an impact on you. Is it affecting your sleep, appetite, concentration, mood? And if you do have a preexisting psychiatric condition, don’t feel afraid to reach out to your mental health provider. Understand that you’re going to be anxious, which may aggravate your symptoms and require an adjustment in your treatment. That’s okay. It’s to be expected and your provider should be available to help you.
Controlling this outbreak via the same epidemiologic infectious disease prevention guidance that works in authoritarian societies is not going to be applicable here because of the liberties that we experience in American society. What will determine our success is the belief that we’re in this together, that we’re going to help each other. We should be proud of that, as it shows how Americans and people around the world stand up in situations like this.
Let’s also note that even though everybody is affected and undergoing previously unimaginable levels of anticipated stress and dislocation, it’s the healthcare providers who are really on the frontlines. They’re under tremendous pressure to continue to perform heroically, at great risk to themselves. They deserve a real debt of gratitude.
We will get through this, but as we do, it will not end until we’ve undergone an extreme test of our character. I certainly hope and trust that we will be up to it.
Dr. Jeffrey A. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association.
Disclosure: Jeffrey A. Lieberman, MD, has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, advisor, consultant, or trustee for Clintara; Intracellular Therapies. Received research grant from Alkermes; Biomarin; EnVivo/Forum; Genentech; Novartis/Novation; Sunovion. Patent: Repligen.
This article first appeared on Medscape.com.
The COVID-19 pandemic is an experience that is unprecedented in our lifetime. It is having a pervasive effect due to how mysterious, potentially dangerous, and sustained it is. We don’t know how bad it’s going to get or how long it’s going to last. We have natural disasters like hurricanes and earthquakes, but they are limited in time and scope. But this global pandemic is something we can’t put our arms around just yet, breeding uncertainty, worry, and fear. This is where mental health professionals need to come in.
The populations being affected by this pandemic can be placed into different groups on the basis of their mental health consequences and needs. First you have, for lack of a better term, “the worried well.” These are people with no preexisting mental disorder who are naturally worried by this and are trying to take appropriate actions to protect themselves and prepare. For such individuals, the equivalent of mental health first-aid should be useful (we’ll come back to that in a moment). Given the proper guidance and sources of information, most such people should be able to manage the anxiety, worry, and dysphoria associated with this critical pandemic.
Then there are those who have preexisting mental conditions related to mood, anxiety, stress, or obsessive tendencies. They are probably going to have an increase in their symptoms, and as such, a corresponding need for adjusting treatment. This may require an increase in their existing medications or the addition of an ad hoc medication, or perhaps more frequent contact with their doctor or therapist.
Because travel and direct visitation is discouraged at the moment, virtual methods of communication should be used to speak with these patients. Such methods have long existed but haven’t been adopted in large numbers; this may be the impetus to finally make it happen. Using the telephone, FaceTime, Skype, WebEx, Zoom, and other means of videoconferencing should be feasible. As billing procedures are being adapted for this moment, there’s no reason why individuals shouldn’t be able to contact their mental health provider.
Substance abuse is also a condition vulnerable to the stress effects of this pandemic. This will prompt or tempt those to use substances that they’ve abused or turned to in the past as a way of self-medicating and assuaging their anxiety and worry.
It’s possible that the pandemic could find its way into delusions or exacerbate symptoms, but somewhat paradoxically, people with serious mental illnesses often respond more calmly to crises than do individuals without them. As a result, the number of these patients requiring emergency room admission for possible exacerbation of symptoms is probably not going to be that much greater than normal.
How to Cope With an Unprecedented Situation
For the worried well and for the clinicians who have understandable fears about exposure, there are several things you can try to manage your anxiety. There are concentric circles of concern that you have to maintain. Think of it like the instructions on an airplane when, if there’s a drop in cabin pressure, you’re asked to apply your own oxygen mask first before placing one on your child. In the same way, you must first think about protecting yourself by limiting your exposure and monitoring your own physical state for any symptoms. But then you must be concerned about your family, your friends, and also society. This is a situation where the impulse and the ethos of worrying about your fellow persons—being your brother’s keeper—is imperative.
The epidemic has been successfully managed in some countries, like Singapore and China, which, once they got on top of it, were able to limit contagion in a very dramatic way. But these are authoritarian governments. The United States doesn’t work that way, which is what makes appealing to the principle of caring for others so crucial. You can protect yourself, but if other people aren’t also protected, it may not matter. You have to worry not just about yourself but about everyone else.
When it comes to stress management, I recommend not catastrophizing or watching the news media 24/7. Distract yourself with other work or recreational activities. Reach out and communicate—virtually, of course—with friends, family, and healthcare providers as needed. Staying in touch acts not just as a diversion but also as an outlet for assuaging your feelings, your sense of being in this alone, feeling isolated.
There are also cognitive reframing mechanisms you can employ. Consider that although this is bad, some countries have already gone through it. And we’ll get through it too. You’ll understandably ask yourself what it would mean if you were to be exposed. In most cases you can say, “I’m going to have the flu and symptoms that are not going to be pleasant, but I’ve had the flu or serious sickness before.”
Remember that there are already antiretroviral treatments being tested in clinical trials and showing efficacy. It’s good to know that before this pandemic ends, some of these treatments will probably be clinically applied, mostly to those who are severely affected and in intensive care.
Diagnose yourself. Monitor your state. Determine whether the stress is really having an impact on you. Is it affecting your sleep, appetite, concentration, mood? And if you do have a preexisting psychiatric condition, don’t feel afraid to reach out to your mental health provider. Understand that you’re going to be anxious, which may aggravate your symptoms and require an adjustment in your treatment. That’s okay. It’s to be expected and your provider should be available to help you.
Controlling this outbreak via the same epidemiologic infectious disease prevention guidance that works in authoritarian societies is not going to be applicable here because of the liberties that we experience in American society. What will determine our success is the belief that we’re in this together, that we’re going to help each other. We should be proud of that, as it shows how Americans and people around the world stand up in situations like this.
Let’s also note that even though everybody is affected and undergoing previously unimaginable levels of anticipated stress and dislocation, it’s the healthcare providers who are really on the frontlines. They’re under tremendous pressure to continue to perform heroically, at great risk to themselves. They deserve a real debt of gratitude.
We will get through this, but as we do, it will not end until we’ve undergone an extreme test of our character. I certainly hope and trust that we will be up to it.
Dr. Jeffrey A. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association.
Disclosure: Jeffrey A. Lieberman, MD, has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, advisor, consultant, or trustee for Clintara; Intracellular Therapies. Received research grant from Alkermes; Biomarin; EnVivo/Forum; Genentech; Novartis/Novation; Sunovion. Patent: Repligen.
This article first appeared on Medscape.com.
The COVID-19 pandemic is an experience that is unprecedented in our lifetime. It is having a pervasive effect due to how mysterious, potentially dangerous, and sustained it is. We don’t know how bad it’s going to get or how long it’s going to last. We have natural disasters like hurricanes and earthquakes, but they are limited in time and scope. But this global pandemic is something we can’t put our arms around just yet, breeding uncertainty, worry, and fear. This is where mental health professionals need to come in.
The populations being affected by this pandemic can be placed into different groups on the basis of their mental health consequences and needs. First you have, for lack of a better term, “the worried well.” These are people with no preexisting mental disorder who are naturally worried by this and are trying to take appropriate actions to protect themselves and prepare. For such individuals, the equivalent of mental health first-aid should be useful (we’ll come back to that in a moment). Given the proper guidance and sources of information, most such people should be able to manage the anxiety, worry, and dysphoria associated with this critical pandemic.
Then there are those who have preexisting mental conditions related to mood, anxiety, stress, or obsessive tendencies. They are probably going to have an increase in their symptoms, and as such, a corresponding need for adjusting treatment. This may require an increase in their existing medications or the addition of an ad hoc medication, or perhaps more frequent contact with their doctor or therapist.
Because travel and direct visitation is discouraged at the moment, virtual methods of communication should be used to speak with these patients. Such methods have long existed but haven’t been adopted in large numbers; this may be the impetus to finally make it happen. Using the telephone, FaceTime, Skype, WebEx, Zoom, and other means of videoconferencing should be feasible. As billing procedures are being adapted for this moment, there’s no reason why individuals shouldn’t be able to contact their mental health provider.
Substance abuse is also a condition vulnerable to the stress effects of this pandemic. This will prompt or tempt those to use substances that they’ve abused or turned to in the past as a way of self-medicating and assuaging their anxiety and worry.
It’s possible that the pandemic could find its way into delusions or exacerbate symptoms, but somewhat paradoxically, people with serious mental illnesses often respond more calmly to crises than do individuals without them. As a result, the number of these patients requiring emergency room admission for possible exacerbation of symptoms is probably not going to be that much greater than normal.
How to Cope With an Unprecedented Situation
For the worried well and for the clinicians who have understandable fears about exposure, there are several things you can try to manage your anxiety. There are concentric circles of concern that you have to maintain. Think of it like the instructions on an airplane when, if there’s a drop in cabin pressure, you’re asked to apply your own oxygen mask first before placing one on your child. In the same way, you must first think about protecting yourself by limiting your exposure and monitoring your own physical state for any symptoms. But then you must be concerned about your family, your friends, and also society. This is a situation where the impulse and the ethos of worrying about your fellow persons—being your brother’s keeper—is imperative.
The epidemic has been successfully managed in some countries, like Singapore and China, which, once they got on top of it, were able to limit contagion in a very dramatic way. But these are authoritarian governments. The United States doesn’t work that way, which is what makes appealing to the principle of caring for others so crucial. You can protect yourself, but if other people aren’t also protected, it may not matter. You have to worry not just about yourself but about everyone else.
When it comes to stress management, I recommend not catastrophizing or watching the news media 24/7. Distract yourself with other work or recreational activities. Reach out and communicate—virtually, of course—with friends, family, and healthcare providers as needed. Staying in touch acts not just as a diversion but also as an outlet for assuaging your feelings, your sense of being in this alone, feeling isolated.
There are also cognitive reframing mechanisms you can employ. Consider that although this is bad, some countries have already gone through it. And we’ll get through it too. You’ll understandably ask yourself what it would mean if you were to be exposed. In most cases you can say, “I’m going to have the flu and symptoms that are not going to be pleasant, but I’ve had the flu or serious sickness before.”
Remember that there are already antiretroviral treatments being tested in clinical trials and showing efficacy. It’s good to know that before this pandemic ends, some of these treatments will probably be clinically applied, mostly to those who are severely affected and in intensive care.
Diagnose yourself. Monitor your state. Determine whether the stress is really having an impact on you. Is it affecting your sleep, appetite, concentration, mood? And if you do have a preexisting psychiatric condition, don’t feel afraid to reach out to your mental health provider. Understand that you’re going to be anxious, which may aggravate your symptoms and require an adjustment in your treatment. That’s okay. It’s to be expected and your provider should be available to help you.
Controlling this outbreak via the same epidemiologic infectious disease prevention guidance that works in authoritarian societies is not going to be applicable here because of the liberties that we experience in American society. What will determine our success is the belief that we’re in this together, that we’re going to help each other. We should be proud of that, as it shows how Americans and people around the world stand up in situations like this.
Let’s also note that even though everybody is affected and undergoing previously unimaginable levels of anticipated stress and dislocation, it’s the healthcare providers who are really on the frontlines. They’re under tremendous pressure to continue to perform heroically, at great risk to themselves. They deserve a real debt of gratitude.
We will get through this, but as we do, it will not end until we’ve undergone an extreme test of our character. I certainly hope and trust that we will be up to it.
Dr. Jeffrey A. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association.
Disclosure: Jeffrey A. Lieberman, MD, has disclosed the following relevant financial relationships: Served as a director, officer, partner, employee, advisor, consultant, or trustee for Clintara; Intracellular Therapies. Received research grant from Alkermes; Biomarin; EnVivo/Forum; Genentech; Novartis/Novation; Sunovion. Patent: Repligen.
This article first appeared on Medscape.com.
U.S. lifts visa halt to boost COVID-19 physician workforce
New information from the US State Department indicates that it is lifting the suspension on visas for foreign-trained medical professionals, a move that has promise for boosting the US physician workforce battling COVID-19.
The move may also help physicians extend their visas.
The communication late last week follows a March 18 announcement that, because of COVID-19, the United States was suspending routine processing of immigrant and nonimmigrant visas, including the J and H visas, at embassies and consulates worldwide.
As reported by Medscape Medical News, the Educational Commission for Foreign Medical Graduates (ECFMG) appealed to the State Department to lift the suspension, noting that 4222 graduates of medical schools outside the United States who had matched into residencies in the United States and were ready to start on July 1 would not get the visas most of them need to begin training.
The State Department lifted the suspensions and issued this update:
“We encourage medical professionals with an approved US non-immigrant or immigrant visa petition (I-129, I-140, or similar) or a certificate of eligibility in an approved exchange visitor program (DS-2019), particularly those working to treat or mitigate the effects of COVID-19, to review the website of their nearest embassy or consulate for procedures to request a visa appointment.”
The State Department also issued guidance for foreign medical professionals already in the United States:
“J-1 Alien Physicians (medical residents) may consult with their program sponsor, ECFMG, to extend their programs in the United States. Generally, a J-1 program for a foreign medical resident can be extended one year at a time for up to seven years.
“Note that the expiration date on a US visa does not determine how long one can be in the United States. The way to confirm one’s required departure date is here : https://i94.cbp.dhs.gov/I94/#/home.
“Those who need to extend their stay or adjust their visa status must apply with USCIS (US Citizenship and Immigration Services).”
Complications Still Exist
ECFMG’s CEO, William W. Pinsky, MD, told Medscape Medical News that, although they welcomed the news from the State Department, there are still unanswered questions.
ECFMG explained that J-1 visas are currently granted only 30 days before the residency program begins.
However, travel to the United States may still be difficult in June, Pinsky said, and physicians may need to be quarantined for 2 weeks upon arrival.
“We’re still having some discussion with the Department of State on whether that regulation could be relaxed and they could come in earlier,” he said.
He cautioned that even after a J-1 visa application is made, the physician’s home country has to endorse the application.
Pinsky said he did not yet know whether that would be a problem.
He also said that, in response to New York’s plea for more healthcare workers, ECFMG is offering to verify education and licensing credentials for physicians educated outside the United States at no cost.
Individual hospitals and regulatory authorities can decide whether there may be roles in some capacity for physicians who have graduated from medical school, even if they have not completed residency or have not been licensed, he said.
This article first appeared on Medscape.com.
New information from the US State Department indicates that it is lifting the suspension on visas for foreign-trained medical professionals, a move that has promise for boosting the US physician workforce battling COVID-19.
The move may also help physicians extend their visas.
The communication late last week follows a March 18 announcement that, because of COVID-19, the United States was suspending routine processing of immigrant and nonimmigrant visas, including the J and H visas, at embassies and consulates worldwide.
As reported by Medscape Medical News, the Educational Commission for Foreign Medical Graduates (ECFMG) appealed to the State Department to lift the suspension, noting that 4222 graduates of medical schools outside the United States who had matched into residencies in the United States and were ready to start on July 1 would not get the visas most of them need to begin training.
The State Department lifted the suspensions and issued this update:
“We encourage medical professionals with an approved US non-immigrant or immigrant visa petition (I-129, I-140, or similar) or a certificate of eligibility in an approved exchange visitor program (DS-2019), particularly those working to treat or mitigate the effects of COVID-19, to review the website of their nearest embassy or consulate for procedures to request a visa appointment.”
The State Department also issued guidance for foreign medical professionals already in the United States:
“J-1 Alien Physicians (medical residents) may consult with their program sponsor, ECFMG, to extend their programs in the United States. Generally, a J-1 program for a foreign medical resident can be extended one year at a time for up to seven years.
“Note that the expiration date on a US visa does not determine how long one can be in the United States. The way to confirm one’s required departure date is here : https://i94.cbp.dhs.gov/I94/#/home.
“Those who need to extend their stay or adjust their visa status must apply with USCIS (US Citizenship and Immigration Services).”
Complications Still Exist
ECFMG’s CEO, William W. Pinsky, MD, told Medscape Medical News that, although they welcomed the news from the State Department, there are still unanswered questions.
ECFMG explained that J-1 visas are currently granted only 30 days before the residency program begins.
However, travel to the United States may still be difficult in June, Pinsky said, and physicians may need to be quarantined for 2 weeks upon arrival.
“We’re still having some discussion with the Department of State on whether that regulation could be relaxed and they could come in earlier,” he said.
He cautioned that even after a J-1 visa application is made, the physician’s home country has to endorse the application.
Pinsky said he did not yet know whether that would be a problem.
He also said that, in response to New York’s plea for more healthcare workers, ECFMG is offering to verify education and licensing credentials for physicians educated outside the United States at no cost.
Individual hospitals and regulatory authorities can decide whether there may be roles in some capacity for physicians who have graduated from medical school, even if they have not completed residency or have not been licensed, he said.
This article first appeared on Medscape.com.
New information from the US State Department indicates that it is lifting the suspension on visas for foreign-trained medical professionals, a move that has promise for boosting the US physician workforce battling COVID-19.
The move may also help physicians extend their visas.
The communication late last week follows a March 18 announcement that, because of COVID-19, the United States was suspending routine processing of immigrant and nonimmigrant visas, including the J and H visas, at embassies and consulates worldwide.
As reported by Medscape Medical News, the Educational Commission for Foreign Medical Graduates (ECFMG) appealed to the State Department to lift the suspension, noting that 4222 graduates of medical schools outside the United States who had matched into residencies in the United States and were ready to start on July 1 would not get the visas most of them need to begin training.
The State Department lifted the suspensions and issued this update:
“We encourage medical professionals with an approved US non-immigrant or immigrant visa petition (I-129, I-140, or similar) or a certificate of eligibility in an approved exchange visitor program (DS-2019), particularly those working to treat or mitigate the effects of COVID-19, to review the website of their nearest embassy or consulate for procedures to request a visa appointment.”
The State Department also issued guidance for foreign medical professionals already in the United States:
“J-1 Alien Physicians (medical residents) may consult with their program sponsor, ECFMG, to extend their programs in the United States. Generally, a J-1 program for a foreign medical resident can be extended one year at a time for up to seven years.
“Note that the expiration date on a US visa does not determine how long one can be in the United States. The way to confirm one’s required departure date is here : https://i94.cbp.dhs.gov/I94/#/home.
“Those who need to extend their stay or adjust their visa status must apply with USCIS (US Citizenship and Immigration Services).”
Complications Still Exist
ECFMG’s CEO, William W. Pinsky, MD, told Medscape Medical News that, although they welcomed the news from the State Department, there are still unanswered questions.
ECFMG explained that J-1 visas are currently granted only 30 days before the residency program begins.
However, travel to the United States may still be difficult in June, Pinsky said, and physicians may need to be quarantined for 2 weeks upon arrival.
“We’re still having some discussion with the Department of State on whether that regulation could be relaxed and they could come in earlier,” he said.
He cautioned that even after a J-1 visa application is made, the physician’s home country has to endorse the application.
Pinsky said he did not yet know whether that would be a problem.
He also said that, in response to New York’s plea for more healthcare workers, ECFMG is offering to verify education and licensing credentials for physicians educated outside the United States at no cost.
Individual hospitals and regulatory authorities can decide whether there may be roles in some capacity for physicians who have graduated from medical school, even if they have not completed residency or have not been licensed, he said.
This article first appeared on Medscape.com.
Sunshine on my shoulders
On March 26, 2020, it’s hard to write or think of anything beyond the COVID-19 pandemic. Those of you who are on the front lines of the battle may find it strange that I am just a bit envious. Having stepped back from clinical medicine nearly a decade ago, it is frustrating to feel that there is little I can do to help other than offering to venture into the grocery store to shop for friends and neighbors who feel more vulnerable than I do.
Here in Maine, we are blessed by geographic isolation that for the moment seems to have damped the surge from the metropolitan centers to our south. But, the virus is here and, as the state with the oldest population, we are beginning to be affected.
For nearly a century, we could count on the outhouses here in Maine would be stocked with outdated Sears Roebucks catalogs when toilet paper was in short supply. Many outhouses remain but Sears Roebucks and its catalogs have disappeared from the landscape. I take a little comfort in the learning that I’m not the only human on the planet who can envision the horror of a week or even a day without toilet paper.
So I am left to sit on the sidelines and watch how my fellow Mainers are coping with the anxiety, depression, and loneliness that come with the forced social isolation. It is pretty clear that walking outside has become the coping strategy of choice. On a usual March day the walkers comprise a skimpy mix of dog walkers and wannabe arctic explorers testing the weather-defying capabilities of their high-tech outerwear. But, to say the least, this is not a usual March and the number of walkers has surged bolstered by gym rats forced off their sweat-drenched ellipticals and treadmills.
This increase in outdoor activity is clearly perceptible even on an overcast day, but it is far less than one would expect given the magnitude of the disruption to everyone’s routines. But, when the sun comes out! The doors fly open and onto the sidewalks and quiet rural roads spill scores of people I haven’t seen for months and in some cases decades. One can almost hear John Denver singing “sunshine on my shoulders makes me happy.” Everyone is smiling and waving to each other. It feels as though the community has, at least for a few hours, been able to throw off the burden of angst that the pandemic laid on us.
There has been a good bit of research about seasonal affective disorder, and I suspect that almost everyone has heard about the value of sunshine for depression. But it is unfortunate that the psychological benefits of just being outdoors – even on an overcast day – has gone pretty much unpublicized. As part of their marketing strategy, a local company that specializes in recreational clothing and gear is encouraging its customers to become “outsiders.” It may be that the pandemic will make more people realize the psychological benefits of being active outside. As physicians we should continue to encourage our patients to be more active and remind them that they don’t need to wait for a sunny day to do so.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” He has no relevant financial disclosures. Email him at [email protected].
On March 26, 2020, it’s hard to write or think of anything beyond the COVID-19 pandemic. Those of you who are on the front lines of the battle may find it strange that I am just a bit envious. Having stepped back from clinical medicine nearly a decade ago, it is frustrating to feel that there is little I can do to help other than offering to venture into the grocery store to shop for friends and neighbors who feel more vulnerable than I do.
Here in Maine, we are blessed by geographic isolation that for the moment seems to have damped the surge from the metropolitan centers to our south. But, the virus is here and, as the state with the oldest population, we are beginning to be affected.
For nearly a century, we could count on the outhouses here in Maine would be stocked with outdated Sears Roebucks catalogs when toilet paper was in short supply. Many outhouses remain but Sears Roebucks and its catalogs have disappeared from the landscape. I take a little comfort in the learning that I’m not the only human on the planet who can envision the horror of a week or even a day without toilet paper.
So I am left to sit on the sidelines and watch how my fellow Mainers are coping with the anxiety, depression, and loneliness that come with the forced social isolation. It is pretty clear that walking outside has become the coping strategy of choice. On a usual March day the walkers comprise a skimpy mix of dog walkers and wannabe arctic explorers testing the weather-defying capabilities of their high-tech outerwear. But, to say the least, this is not a usual March and the number of walkers has surged bolstered by gym rats forced off their sweat-drenched ellipticals and treadmills.
This increase in outdoor activity is clearly perceptible even on an overcast day, but it is far less than one would expect given the magnitude of the disruption to everyone’s routines. But, when the sun comes out! The doors fly open and onto the sidewalks and quiet rural roads spill scores of people I haven’t seen for months and in some cases decades. One can almost hear John Denver singing “sunshine on my shoulders makes me happy.” Everyone is smiling and waving to each other. It feels as though the community has, at least for a few hours, been able to throw off the burden of angst that the pandemic laid on us.
There has been a good bit of research about seasonal affective disorder, and I suspect that almost everyone has heard about the value of sunshine for depression. But it is unfortunate that the psychological benefits of just being outdoors – even on an overcast day – has gone pretty much unpublicized. As part of their marketing strategy, a local company that specializes in recreational clothing and gear is encouraging its customers to become “outsiders.” It may be that the pandemic will make more people realize the psychological benefits of being active outside. As physicians we should continue to encourage our patients to be more active and remind them that they don’t need to wait for a sunny day to do so.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” He has no relevant financial disclosures. Email him at [email protected].
On March 26, 2020, it’s hard to write or think of anything beyond the COVID-19 pandemic. Those of you who are on the front lines of the battle may find it strange that I am just a bit envious. Having stepped back from clinical medicine nearly a decade ago, it is frustrating to feel that there is little I can do to help other than offering to venture into the grocery store to shop for friends and neighbors who feel more vulnerable than I do.
Here in Maine, we are blessed by geographic isolation that for the moment seems to have damped the surge from the metropolitan centers to our south. But, the virus is here and, as the state with the oldest population, we are beginning to be affected.
For nearly a century, we could count on the outhouses here in Maine would be stocked with outdated Sears Roebucks catalogs when toilet paper was in short supply. Many outhouses remain but Sears Roebucks and its catalogs have disappeared from the landscape. I take a little comfort in the learning that I’m not the only human on the planet who can envision the horror of a week or even a day without toilet paper.
So I am left to sit on the sidelines and watch how my fellow Mainers are coping with the anxiety, depression, and loneliness that come with the forced social isolation. It is pretty clear that walking outside has become the coping strategy of choice. On a usual March day the walkers comprise a skimpy mix of dog walkers and wannabe arctic explorers testing the weather-defying capabilities of their high-tech outerwear. But, to say the least, this is not a usual March and the number of walkers has surged bolstered by gym rats forced off their sweat-drenched ellipticals and treadmills.
This increase in outdoor activity is clearly perceptible even on an overcast day, but it is far less than one would expect given the magnitude of the disruption to everyone’s routines. But, when the sun comes out! The doors fly open and onto the sidewalks and quiet rural roads spill scores of people I haven’t seen for months and in some cases decades. One can almost hear John Denver singing “sunshine on my shoulders makes me happy.” Everyone is smiling and waving to each other. It feels as though the community has, at least for a few hours, been able to throw off the burden of angst that the pandemic laid on us.
There has been a good bit of research about seasonal affective disorder, and I suspect that almost everyone has heard about the value of sunshine for depression. But it is unfortunate that the psychological benefits of just being outdoors – even on an overcast day – has gone pretty much unpublicized. As part of their marketing strategy, a local company that specializes in recreational clothing and gear is encouraging its customers to become “outsiders.” It may be that the pandemic will make more people realize the psychological benefits of being active outside. As physicians we should continue to encourage our patients to be more active and remind them that they don’t need to wait for a sunny day to do so.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” He has no relevant financial disclosures. Email him at [email protected].
New guidance on management of acute CVD during COVID-19
The Chinese Society of Cardiology (CSC) has issued a consensus statement on the management of cardiac emergencies during the COVID-19 pandemic.
The document first appeared in the Chinese Journal of Cardiology, and a translated version was published in Circulation. The consensus statement was developed by 125 medical experts in the fields of cardiovascular disease and infectious disease. This included 23 experts currently working in Wuhan, China.
Three overarching principles guided their recommendations.
- The highest priority is prevention and control of transmission (including protecting staff).
- Patients should be assessed both for COVID-19 and for cardiovascular issues.
- At all times, all interventions and therapies provided should be in concordance with directives of infection control authorities.
“Considering that some asymptomatic patients may be a source of infection and transmission, all patients with severe emergent cardiovascular diseases should be managed as suspected cases of COVID-19 in Hubei Province,” noted writing chair and cardiologist Yaling Han, MD, of the General Hospital of Northern Theater Command in Shenyang, China.
In areas outside Hubei Province, where COVID-19 was less prevalent, this “infected until proven otherwise” approach was also recommended, although not as strictly.
Diagnosing CVD and COVID-19 simultaneously
In patients with emergent cardiovascular needs in whom COVID-19 has not been ruled out, quarantine in a single-bed room is needed, they wrote. The patient should be monitored for clinical manifestations of the disease, and undergo COVID-19 nucleic acid testing as soon as possible.
After infection control is considered, including limiting risk for infection to health care workers, risk assessment that weighs the relative advantages and disadvantages of treating the cardiovascular disease while preventing transmission can be considered, the investigators wrote.
At all times, transfers to different areas of the hospital and between hospitals should be minimized to reduce the risk for infection transmission.
The authors also recommended the use of “select laboratory tests with definitive sensitivity and specificity for disease diagnosis or assessment.”
For patients with acute aortic syndrome or acute pulmonary embolism, this means CT angiography. When acute pulmonary embolism is suspected, D-dimer testing and deep vein ultrasound can be employed, and for patients with acute coronary syndrome, ordinary electrocardiography and standard biomarkers for cardiac injury are preferred.
In addition, “all patients should undergo lung CT examination to evaluate for imaging features typical of COVID-19. ... Chest x-ray is not recommended because of a high rate of false negative diagnosis,” the authors wrote.
Intervene with caution
Medical therapy should be optimized in patients with emergent cardiovascular issues, with invasive strategies for diagnosis and therapy used “with caution,” according to the Chinese experts.
Conditions for which conservative medical treatment is recommended during COVID-19 pandemic include ST-segment elevation MI (STEMI) where thrombolytic therapy is indicated, STEMI when the optimal window for revascularization has passed, high-risk non-STEMI (NSTEMI), patients with uncomplicated Stanford type B aortic dissection, acute pulmonary embolism, acute exacerbation of heart failure, and hypertensive emergency.
“Vigilance should be paid to avoid misdiagnosing patients with pulmonary infarction as COVID-19 pneumonia,” they noted.
Diagnoses warranting invasive intervention are limited to STEMI with hemodynamic instability, life-threatening NSTEMI, Stanford type A or complex type B acute aortic dissection, bradyarrhythmia complicated by syncope or unstable hemodynamics mandating implantation of a device, and pulmonary embolism with hemodynamic instability for whom intravenous thrombolytics are too risky.
Interventions should be done in a cath lab or operating room with negative-pressure ventilation, with strict periprocedural disinfection. Personal protective equipment should also be of the strictest level.
In patients for whom COVID-19 cannot be ruled out presenting in a region with low incidence of COVID-19, interventions should only be considered for more severe cases and undertaken in a cath lab, electrophysiology lab, or operating room “with more than standard disinfection procedures that fulfill regulatory mandates for infection control.”
If negative-pressure ventilation is not available, air conditioning (for example, laminar flow and ventilation) should be stopped.
Establish plans now
“We operationalized all of these strategies at Beth Israel Deaconess Medical Center several weeks ago, since Boston had that early outbreak with the Biogen conference, but I suspect many institutions nationally are still formulating plans,” said Dhruv Kazi, MD, MSc, in an interview.
Although COVID-19 is “primarily a single-organ disease – it destroys the lungs” – transmission of infection to cardiology providers was an early problem that needed to be addressed, said Dr. Kazi. “We now know that a cardiologist seeing a patient who reports shortness of breath and then leans in to carefully auscultate the lungs and heart can get exposed if not provided adequate personal protective equipment; hence the cancellation of elective procedures, conversion of most elective visits to telemedicine, if possible, and the use of surgical/N95 masks in clinic and on rounds.”
Regarding the CSC recommendation to consider medical over invasive management, Dr. Kazi noteed that this works better in a setting where rapid testing is available. “Where that is not the case – as in the U.S. – resorting to conservative therapy for all COVID suspect cases will result in suboptimal care, particularly when nine out of every 10 COVID suspects will eventually rule out.”
One of his biggest worries now is that patients simply won’t come. Afraid of being exposed to COVID-19, patients with MIs and strokes may avoid or delay coming to the hospital.
“There is some evidence that this occurred in Wuhan, and I’m starting to see anecdotal evidence of this in Boston,” said Dr. Kazi. “We need to remind our patients that, if they experience symptoms of a heart attack or stroke, they deserve the same lifesaving treatment we offered before this pandemic set in. They should not try and sit it out.”
A version of this article originally appeared on Medscape.com.
The Chinese Society of Cardiology (CSC) has issued a consensus statement on the management of cardiac emergencies during the COVID-19 pandemic.
The document first appeared in the Chinese Journal of Cardiology, and a translated version was published in Circulation. The consensus statement was developed by 125 medical experts in the fields of cardiovascular disease and infectious disease. This included 23 experts currently working in Wuhan, China.
Three overarching principles guided their recommendations.
- The highest priority is prevention and control of transmission (including protecting staff).
- Patients should be assessed both for COVID-19 and for cardiovascular issues.
- At all times, all interventions and therapies provided should be in concordance with directives of infection control authorities.
“Considering that some asymptomatic patients may be a source of infection and transmission, all patients with severe emergent cardiovascular diseases should be managed as suspected cases of COVID-19 in Hubei Province,” noted writing chair and cardiologist Yaling Han, MD, of the General Hospital of Northern Theater Command in Shenyang, China.
In areas outside Hubei Province, where COVID-19 was less prevalent, this “infected until proven otherwise” approach was also recommended, although not as strictly.
Diagnosing CVD and COVID-19 simultaneously
In patients with emergent cardiovascular needs in whom COVID-19 has not been ruled out, quarantine in a single-bed room is needed, they wrote. The patient should be monitored for clinical manifestations of the disease, and undergo COVID-19 nucleic acid testing as soon as possible.
After infection control is considered, including limiting risk for infection to health care workers, risk assessment that weighs the relative advantages and disadvantages of treating the cardiovascular disease while preventing transmission can be considered, the investigators wrote.
At all times, transfers to different areas of the hospital and between hospitals should be minimized to reduce the risk for infection transmission.
The authors also recommended the use of “select laboratory tests with definitive sensitivity and specificity for disease diagnosis or assessment.”
For patients with acute aortic syndrome or acute pulmonary embolism, this means CT angiography. When acute pulmonary embolism is suspected, D-dimer testing and deep vein ultrasound can be employed, and for patients with acute coronary syndrome, ordinary electrocardiography and standard biomarkers for cardiac injury are preferred.
In addition, “all patients should undergo lung CT examination to evaluate for imaging features typical of COVID-19. ... Chest x-ray is not recommended because of a high rate of false negative diagnosis,” the authors wrote.
Intervene with caution
Medical therapy should be optimized in patients with emergent cardiovascular issues, with invasive strategies for diagnosis and therapy used “with caution,” according to the Chinese experts.
Conditions for which conservative medical treatment is recommended during COVID-19 pandemic include ST-segment elevation MI (STEMI) where thrombolytic therapy is indicated, STEMI when the optimal window for revascularization has passed, high-risk non-STEMI (NSTEMI), patients with uncomplicated Stanford type B aortic dissection, acute pulmonary embolism, acute exacerbation of heart failure, and hypertensive emergency.
“Vigilance should be paid to avoid misdiagnosing patients with pulmonary infarction as COVID-19 pneumonia,” they noted.
Diagnoses warranting invasive intervention are limited to STEMI with hemodynamic instability, life-threatening NSTEMI, Stanford type A or complex type B acute aortic dissection, bradyarrhythmia complicated by syncope or unstable hemodynamics mandating implantation of a device, and pulmonary embolism with hemodynamic instability for whom intravenous thrombolytics are too risky.
Interventions should be done in a cath lab or operating room with negative-pressure ventilation, with strict periprocedural disinfection. Personal protective equipment should also be of the strictest level.
In patients for whom COVID-19 cannot be ruled out presenting in a region with low incidence of COVID-19, interventions should only be considered for more severe cases and undertaken in a cath lab, electrophysiology lab, or operating room “with more than standard disinfection procedures that fulfill regulatory mandates for infection control.”
If negative-pressure ventilation is not available, air conditioning (for example, laminar flow and ventilation) should be stopped.
Establish plans now
“We operationalized all of these strategies at Beth Israel Deaconess Medical Center several weeks ago, since Boston had that early outbreak with the Biogen conference, but I suspect many institutions nationally are still formulating plans,” said Dhruv Kazi, MD, MSc, in an interview.
Although COVID-19 is “primarily a single-organ disease – it destroys the lungs” – transmission of infection to cardiology providers was an early problem that needed to be addressed, said Dr. Kazi. “We now know that a cardiologist seeing a patient who reports shortness of breath and then leans in to carefully auscultate the lungs and heart can get exposed if not provided adequate personal protective equipment; hence the cancellation of elective procedures, conversion of most elective visits to telemedicine, if possible, and the use of surgical/N95 masks in clinic and on rounds.”
Regarding the CSC recommendation to consider medical over invasive management, Dr. Kazi noteed that this works better in a setting where rapid testing is available. “Where that is not the case – as in the U.S. – resorting to conservative therapy for all COVID suspect cases will result in suboptimal care, particularly when nine out of every 10 COVID suspects will eventually rule out.”
One of his biggest worries now is that patients simply won’t come. Afraid of being exposed to COVID-19, patients with MIs and strokes may avoid or delay coming to the hospital.
“There is some evidence that this occurred in Wuhan, and I’m starting to see anecdotal evidence of this in Boston,” said Dr. Kazi. “We need to remind our patients that, if they experience symptoms of a heart attack or stroke, they deserve the same lifesaving treatment we offered before this pandemic set in. They should not try and sit it out.”
A version of this article originally appeared on Medscape.com.
The Chinese Society of Cardiology (CSC) has issued a consensus statement on the management of cardiac emergencies during the COVID-19 pandemic.
The document first appeared in the Chinese Journal of Cardiology, and a translated version was published in Circulation. The consensus statement was developed by 125 medical experts in the fields of cardiovascular disease and infectious disease. This included 23 experts currently working in Wuhan, China.
Three overarching principles guided their recommendations.
- The highest priority is prevention and control of transmission (including protecting staff).
- Patients should be assessed both for COVID-19 and for cardiovascular issues.
- At all times, all interventions and therapies provided should be in concordance with directives of infection control authorities.
“Considering that some asymptomatic patients may be a source of infection and transmission, all patients with severe emergent cardiovascular diseases should be managed as suspected cases of COVID-19 in Hubei Province,” noted writing chair and cardiologist Yaling Han, MD, of the General Hospital of Northern Theater Command in Shenyang, China.
In areas outside Hubei Province, where COVID-19 was less prevalent, this “infected until proven otherwise” approach was also recommended, although not as strictly.
Diagnosing CVD and COVID-19 simultaneously
In patients with emergent cardiovascular needs in whom COVID-19 has not been ruled out, quarantine in a single-bed room is needed, they wrote. The patient should be monitored for clinical manifestations of the disease, and undergo COVID-19 nucleic acid testing as soon as possible.
After infection control is considered, including limiting risk for infection to health care workers, risk assessment that weighs the relative advantages and disadvantages of treating the cardiovascular disease while preventing transmission can be considered, the investigators wrote.
At all times, transfers to different areas of the hospital and between hospitals should be minimized to reduce the risk for infection transmission.
The authors also recommended the use of “select laboratory tests with definitive sensitivity and specificity for disease diagnosis or assessment.”
For patients with acute aortic syndrome or acute pulmonary embolism, this means CT angiography. When acute pulmonary embolism is suspected, D-dimer testing and deep vein ultrasound can be employed, and for patients with acute coronary syndrome, ordinary electrocardiography and standard biomarkers for cardiac injury are preferred.
In addition, “all patients should undergo lung CT examination to evaluate for imaging features typical of COVID-19. ... Chest x-ray is not recommended because of a high rate of false negative diagnosis,” the authors wrote.
Intervene with caution
Medical therapy should be optimized in patients with emergent cardiovascular issues, with invasive strategies for diagnosis and therapy used “with caution,” according to the Chinese experts.
Conditions for which conservative medical treatment is recommended during COVID-19 pandemic include ST-segment elevation MI (STEMI) where thrombolytic therapy is indicated, STEMI when the optimal window for revascularization has passed, high-risk non-STEMI (NSTEMI), patients with uncomplicated Stanford type B aortic dissection, acute pulmonary embolism, acute exacerbation of heart failure, and hypertensive emergency.
“Vigilance should be paid to avoid misdiagnosing patients with pulmonary infarction as COVID-19 pneumonia,” they noted.
Diagnoses warranting invasive intervention are limited to STEMI with hemodynamic instability, life-threatening NSTEMI, Stanford type A or complex type B acute aortic dissection, bradyarrhythmia complicated by syncope or unstable hemodynamics mandating implantation of a device, and pulmonary embolism with hemodynamic instability for whom intravenous thrombolytics are too risky.
Interventions should be done in a cath lab or operating room with negative-pressure ventilation, with strict periprocedural disinfection. Personal protective equipment should also be of the strictest level.
In patients for whom COVID-19 cannot be ruled out presenting in a region with low incidence of COVID-19, interventions should only be considered for more severe cases and undertaken in a cath lab, electrophysiology lab, or operating room “with more than standard disinfection procedures that fulfill regulatory mandates for infection control.”
If negative-pressure ventilation is not available, air conditioning (for example, laminar flow and ventilation) should be stopped.
Establish plans now
“We operationalized all of these strategies at Beth Israel Deaconess Medical Center several weeks ago, since Boston had that early outbreak with the Biogen conference, but I suspect many institutions nationally are still formulating plans,” said Dhruv Kazi, MD, MSc, in an interview.
Although COVID-19 is “primarily a single-organ disease – it destroys the lungs” – transmission of infection to cardiology providers was an early problem that needed to be addressed, said Dr. Kazi. “We now know that a cardiologist seeing a patient who reports shortness of breath and then leans in to carefully auscultate the lungs and heart can get exposed if not provided adequate personal protective equipment; hence the cancellation of elective procedures, conversion of most elective visits to telemedicine, if possible, and the use of surgical/N95 masks in clinic and on rounds.”
Regarding the CSC recommendation to consider medical over invasive management, Dr. Kazi noteed that this works better in a setting where rapid testing is available. “Where that is not the case – as in the U.S. – resorting to conservative therapy for all COVID suspect cases will result in suboptimal care, particularly when nine out of every 10 COVID suspects will eventually rule out.”
One of his biggest worries now is that patients simply won’t come. Afraid of being exposed to COVID-19, patients with MIs and strokes may avoid or delay coming to the hospital.
“There is some evidence that this occurred in Wuhan, and I’m starting to see anecdotal evidence of this in Boston,” said Dr. Kazi. “We need to remind our patients that, if they experience symptoms of a heart attack or stroke, they deserve the same lifesaving treatment we offered before this pandemic set in. They should not try and sit it out.”
A version of this article originally appeared on Medscape.com.
FDA issues EUA allowing hydroxychloroquine sulfate, chloroquine phosphate treatment in COVID-19
The Food and Drug Administration issued an Emergency Use Authorization on March 28, 2020, allowing for the usage of hydroxychloroquine sulfate and chloroquine phosphate products in certain hospitalized patients with COVID-19.
The products, currently stored by the Strategic National Stockpile, will be distributed by the SNS to states so that doctors may prescribe the drugs to adolescent and adult patients hospitalized with COVID-19 in the absence of appropriate or feasible clinical trials. The SNS will work with the Federal Emergency Management Agency to ship the products to states.
According to the Emergency Use Authorization, fact sheets will be provided to health care providers and patients with important information about hydroxychloroquine sulfate and chloroquine phosphate, including the risks of using them to treat COVID-19.
The Food and Drug Administration issued an Emergency Use Authorization on March 28, 2020, allowing for the usage of hydroxychloroquine sulfate and chloroquine phosphate products in certain hospitalized patients with COVID-19.
The products, currently stored by the Strategic National Stockpile, will be distributed by the SNS to states so that doctors may prescribe the drugs to adolescent and adult patients hospitalized with COVID-19 in the absence of appropriate or feasible clinical trials. The SNS will work with the Federal Emergency Management Agency to ship the products to states.
According to the Emergency Use Authorization, fact sheets will be provided to health care providers and patients with important information about hydroxychloroquine sulfate and chloroquine phosphate, including the risks of using them to treat COVID-19.
The Food and Drug Administration issued an Emergency Use Authorization on March 28, 2020, allowing for the usage of hydroxychloroquine sulfate and chloroquine phosphate products in certain hospitalized patients with COVID-19.
The products, currently stored by the Strategic National Stockpile, will be distributed by the SNS to states so that doctors may prescribe the drugs to adolescent and adult patients hospitalized with COVID-19 in the absence of appropriate or feasible clinical trials. The SNS will work with the Federal Emergency Management Agency to ship the products to states.
According to the Emergency Use Authorization, fact sheets will be provided to health care providers and patients with important information about hydroxychloroquine sulfate and chloroquine phosphate, including the risks of using them to treat COVID-19.
Are psychiatrists more prepared for COVID-19 than we think?
Helping patients navigate surreal situations is what we do
A meme has been going around the Internet in which a Muppet is dressed as a doctor, and the caption declares: “If you don’t want to be intubated by a psychiatrist, stay home!” This meme is meant as a commentary on health care worker shortages. But it also touches on the concerns of psychiatrists who might be questioning our role in the pandemic, given that we are physicians who do not regularly rely on labs or imaging to guide treatment. And we rarely even touch our patients.
As observed by Henry A. Nasrallah, MD, editor in chief of Current Psychiatry, who referred to anxiety as endemic during a viral pandemic (Current Psychiatry. 2020 April;19[4]:e3-5), our society is experiencing intense psychological repercussions from the pandemic. These repercussions will evolve from anxiety to despair, and for some, to resilience.
All jokes aside about the medical knowledge of psychiatrists, we are on the cutting edge of how to address the pandemic of fear and uncertainty gripping individuals and society across the nation.
Isn’t it our role as psychiatrists to help people face the reality of personal and societal crises? Aren’t we trained to help people find their internal reserves, bolster them with medications and/or psychotherapy, and prepare them to respond to challenges? I propose that our training and particular experience of hearing patients’ stories has indeed prepared us to receive surreal information and package it into a palatable, even therapeutic, form for our patients.
I’d like to present two cases I’ve recently seen during the first stages of the COVID-19 pandemic juxtaposed with patients I saw during “normal” times. These cases show that, as psychiatrists, we are prepared to face the psychological impact of this crisis.
A patient called me about worsened anxiety after she’d been sidelined at home from her job as a waitress and was currently spending 12 hours a day with her overbearing mother. She had always used her work to buffer her anxiety, as the fast pace of the restaurant kept her from ruminating.
The call reminded me of ones I’d receive from female patients during the MeToo movement and particularly during the Brett Kavanaugh confirmation hearings for the Supreme Court, in which a sexual assault victim and alleged perpetrator faced off on television. During therapy and medication management sessions alike, I would talk to women struggling with the number of news stories about victims coming forward after sexual assault. They were reliving their humiliations, and despite the empowering nature of the movement, they felt vulnerable in the shadow of memories of their perpetrators.
The advice I gave then is similar to the guidance I give now, and also is closely related to the Centers for Disease Control and Prevention advice on its website on how to manage the mental health impact of COVID-19. People can be informed without suffering by taking these steps:
- Limit the amount of news and social media consumed, and if possible, try to schedule news consumption into discrete periods that are not close to bedtime or other periods meant for relaxation.
- Reach out to loved ones and friends who remind you of strength and better times.
- Make time to relax and unwind, either through resting or engaging in an activity you enjoy.
- Take care of your body and mind with exercise.
- Try for 8 hours of sleep a night (even if it doesn’t happen).
- Use techniques such as meditating, doing yoga, or breathing to practice focusing your attention somewhere.
All of our lives have been disrupted by COVID-19 and acknowledging this to patients can help them feel less isolated and vulnerable. Our patients with diagnosed psychiatric disorders will be more susceptible to crippling anxiety, exacerbations in panic attacks, obsessive-compulsive disorder symptoms, and resurgence of suicidal ideation in the face of uncertainty and despair. They may also be more likely to experience the socioeconomic fallout of this pandemic. But it’s not just these individuals who will be hit with intense feelings as we wonder what the next day, month, or 6 months hold for us, our families, our friends, our country, and our world.
Recently, I had one of the more surreal experiences of my professional life. I work as a consulation-liaison psychiatrist on the medical wards, and I was consulted to treat a young woman from Central America with schizophrenia who made a serious suicide attempt in mid-February before COVID-19 was part of the lexicon.
After an overdose, she developed aspiration pneumonia and acute respiratory distress syndrome and ended up in the ICU on a respirator for 3 weeks. Her doctors and family were certain she would die, but she miraculously survived. By the time she was extubated and less delirious from her medically induced coma, the hospital had restricted all visitors because of COVID-19.
Because I speak Spanish, we developed as decent a working relationship as we could, considering the patient’s delirium and blunted affect. On top of restarting her antipsychotics, I had to inform her that her family was no longer allowed to come visit her. Outside of this room, I vacillated on how to tell a woman with a history of paranoia that the hospital would not allow her family to visit because we were in the middle of a pandemic. A contagious virus had quickly spread around the world, cases were now spiking in the United States, much of the country was on lockdown, and the hospital was limiting visitors because asymptomatic individuals could bring the virus into the hospital or be infected by asymptomatic staff.
As the words came out of my mouth, she looked at me as I have looked at psychotic individuals as they spin me yarns of impossible explanation for their symptoms when I know they’re simply psychotic and living in an alternate reality. Imagine just waking up from a coma and your doctor coming in to tell you: “The U.S. is on lockdown because a deadly virus is spreading throughout our country.” You’d think you’ve woken up in a zombie film. Yet, the patient simply nodded and asked: “Will I be able to use the phone to call my family?” I sighed with relief and helped her dial her brother’s number.
Haven’t we all listened to insane stories while keeping a straight face and then answered with a politely bland question? Just a few months ago, I treated a homeless woman with schizophrenia who calmly explained to me that her large malignant ovarian tumor (which I could see protruding under her gown) was the unborn heir of Queen Victoria and Prince Albert. If she allowed the doctors to take it out (that is, treat her cancer) she’d be assassinated by the Russian intelligence agency. She refused to let the doctors sentence her to death. Ultimately, we allowed her to refuse treatment. Despite a month of treatment with antipsychotic medication, her psychotic beliefs did not change, and we could not imagine forcing her through surgery and chemotherapy. She died in hospice.
I’ve walked the valleys of bizarro land many times. Working through the dark reality of COVID-19 should be no match for us psychiatrists who have listened to dark stories and responded with words of comfort or empathic silence. As mental health clinicians, I believe we are well equipped to fight on the front lines of the pandemic of fear that has arrested our country. We can make ourselves available to our patients, friends, family, and institutions – medical or otherwise – that are grappling with how to cope with the psychological impact of COVID-19.
Dr. Posada is a consultation-liaison psychiatry fellow with the Inova Fairfax Hospital/George Washington University program in Falls Church, Va., and associate producer of the MDedge Psychcast. She changed key details about the patients discussed to protect their confidentiality. Dr. Posada has no conflicts of interest.
Helping patients navigate surreal situations is what we do
Helping patients navigate surreal situations is what we do
A meme has been going around the Internet in which a Muppet is dressed as a doctor, and the caption declares: “If you don’t want to be intubated by a psychiatrist, stay home!” This meme is meant as a commentary on health care worker shortages. But it also touches on the concerns of psychiatrists who might be questioning our role in the pandemic, given that we are physicians who do not regularly rely on labs or imaging to guide treatment. And we rarely even touch our patients.
As observed by Henry A. Nasrallah, MD, editor in chief of Current Psychiatry, who referred to anxiety as endemic during a viral pandemic (Current Psychiatry. 2020 April;19[4]:e3-5), our society is experiencing intense psychological repercussions from the pandemic. These repercussions will evolve from anxiety to despair, and for some, to resilience.
All jokes aside about the medical knowledge of psychiatrists, we are on the cutting edge of how to address the pandemic of fear and uncertainty gripping individuals and society across the nation.
Isn’t it our role as psychiatrists to help people face the reality of personal and societal crises? Aren’t we trained to help people find their internal reserves, bolster them with medications and/or psychotherapy, and prepare them to respond to challenges? I propose that our training and particular experience of hearing patients’ stories has indeed prepared us to receive surreal information and package it into a palatable, even therapeutic, form for our patients.
I’d like to present two cases I’ve recently seen during the first stages of the COVID-19 pandemic juxtaposed with patients I saw during “normal” times. These cases show that, as psychiatrists, we are prepared to face the psychological impact of this crisis.
A patient called me about worsened anxiety after she’d been sidelined at home from her job as a waitress and was currently spending 12 hours a day with her overbearing mother. She had always used her work to buffer her anxiety, as the fast pace of the restaurant kept her from ruminating.
The call reminded me of ones I’d receive from female patients during the MeToo movement and particularly during the Brett Kavanaugh confirmation hearings for the Supreme Court, in which a sexual assault victim and alleged perpetrator faced off on television. During therapy and medication management sessions alike, I would talk to women struggling with the number of news stories about victims coming forward after sexual assault. They were reliving their humiliations, and despite the empowering nature of the movement, they felt vulnerable in the shadow of memories of their perpetrators.
The advice I gave then is similar to the guidance I give now, and also is closely related to the Centers for Disease Control and Prevention advice on its website on how to manage the mental health impact of COVID-19. People can be informed without suffering by taking these steps:
- Limit the amount of news and social media consumed, and if possible, try to schedule news consumption into discrete periods that are not close to bedtime or other periods meant for relaxation.
- Reach out to loved ones and friends who remind you of strength and better times.
- Make time to relax and unwind, either through resting or engaging in an activity you enjoy.
- Take care of your body and mind with exercise.
- Try for 8 hours of sleep a night (even if it doesn’t happen).
- Use techniques such as meditating, doing yoga, or breathing to practice focusing your attention somewhere.
All of our lives have been disrupted by COVID-19 and acknowledging this to patients can help them feel less isolated and vulnerable. Our patients with diagnosed psychiatric disorders will be more susceptible to crippling anxiety, exacerbations in panic attacks, obsessive-compulsive disorder symptoms, and resurgence of suicidal ideation in the face of uncertainty and despair. They may also be more likely to experience the socioeconomic fallout of this pandemic. But it’s not just these individuals who will be hit with intense feelings as we wonder what the next day, month, or 6 months hold for us, our families, our friends, our country, and our world.
Recently, I had one of the more surreal experiences of my professional life. I work as a consulation-liaison psychiatrist on the medical wards, and I was consulted to treat a young woman from Central America with schizophrenia who made a serious suicide attempt in mid-February before COVID-19 was part of the lexicon.
After an overdose, she developed aspiration pneumonia and acute respiratory distress syndrome and ended up in the ICU on a respirator for 3 weeks. Her doctors and family were certain she would die, but she miraculously survived. By the time she was extubated and less delirious from her medically induced coma, the hospital had restricted all visitors because of COVID-19.
Because I speak Spanish, we developed as decent a working relationship as we could, considering the patient’s delirium and blunted affect. On top of restarting her antipsychotics, I had to inform her that her family was no longer allowed to come visit her. Outside of this room, I vacillated on how to tell a woman with a history of paranoia that the hospital would not allow her family to visit because we were in the middle of a pandemic. A contagious virus had quickly spread around the world, cases were now spiking in the United States, much of the country was on lockdown, and the hospital was limiting visitors because asymptomatic individuals could bring the virus into the hospital or be infected by asymptomatic staff.
As the words came out of my mouth, she looked at me as I have looked at psychotic individuals as they spin me yarns of impossible explanation for their symptoms when I know they’re simply psychotic and living in an alternate reality. Imagine just waking up from a coma and your doctor coming in to tell you: “The U.S. is on lockdown because a deadly virus is spreading throughout our country.” You’d think you’ve woken up in a zombie film. Yet, the patient simply nodded and asked: “Will I be able to use the phone to call my family?” I sighed with relief and helped her dial her brother’s number.
Haven’t we all listened to insane stories while keeping a straight face and then answered with a politely bland question? Just a few months ago, I treated a homeless woman with schizophrenia who calmly explained to me that her large malignant ovarian tumor (which I could see protruding under her gown) was the unborn heir of Queen Victoria and Prince Albert. If she allowed the doctors to take it out (that is, treat her cancer) she’d be assassinated by the Russian intelligence agency. She refused to let the doctors sentence her to death. Ultimately, we allowed her to refuse treatment. Despite a month of treatment with antipsychotic medication, her psychotic beliefs did not change, and we could not imagine forcing her through surgery and chemotherapy. She died in hospice.
I’ve walked the valleys of bizarro land many times. Working through the dark reality of COVID-19 should be no match for us psychiatrists who have listened to dark stories and responded with words of comfort or empathic silence. As mental health clinicians, I believe we are well equipped to fight on the front lines of the pandemic of fear that has arrested our country. We can make ourselves available to our patients, friends, family, and institutions – medical or otherwise – that are grappling with how to cope with the psychological impact of COVID-19.
Dr. Posada is a consultation-liaison psychiatry fellow with the Inova Fairfax Hospital/George Washington University program in Falls Church, Va., and associate producer of the MDedge Psychcast. She changed key details about the patients discussed to protect their confidentiality. Dr. Posada has no conflicts of interest.
A meme has been going around the Internet in which a Muppet is dressed as a doctor, and the caption declares: “If you don’t want to be intubated by a psychiatrist, stay home!” This meme is meant as a commentary on health care worker shortages. But it also touches on the concerns of psychiatrists who might be questioning our role in the pandemic, given that we are physicians who do not regularly rely on labs or imaging to guide treatment. And we rarely even touch our patients.
As observed by Henry A. Nasrallah, MD, editor in chief of Current Psychiatry, who referred to anxiety as endemic during a viral pandemic (Current Psychiatry. 2020 April;19[4]:e3-5), our society is experiencing intense psychological repercussions from the pandemic. These repercussions will evolve from anxiety to despair, and for some, to resilience.
All jokes aside about the medical knowledge of psychiatrists, we are on the cutting edge of how to address the pandemic of fear and uncertainty gripping individuals and society across the nation.
Isn’t it our role as psychiatrists to help people face the reality of personal and societal crises? Aren’t we trained to help people find their internal reserves, bolster them with medications and/or psychotherapy, and prepare them to respond to challenges? I propose that our training and particular experience of hearing patients’ stories has indeed prepared us to receive surreal information and package it into a palatable, even therapeutic, form for our patients.
I’d like to present two cases I’ve recently seen during the first stages of the COVID-19 pandemic juxtaposed with patients I saw during “normal” times. These cases show that, as psychiatrists, we are prepared to face the psychological impact of this crisis.
A patient called me about worsened anxiety after she’d been sidelined at home from her job as a waitress and was currently spending 12 hours a day with her overbearing mother. She had always used her work to buffer her anxiety, as the fast pace of the restaurant kept her from ruminating.
The call reminded me of ones I’d receive from female patients during the MeToo movement and particularly during the Brett Kavanaugh confirmation hearings for the Supreme Court, in which a sexual assault victim and alleged perpetrator faced off on television. During therapy and medication management sessions alike, I would talk to women struggling with the number of news stories about victims coming forward after sexual assault. They were reliving their humiliations, and despite the empowering nature of the movement, they felt vulnerable in the shadow of memories of their perpetrators.
The advice I gave then is similar to the guidance I give now, and also is closely related to the Centers for Disease Control and Prevention advice on its website on how to manage the mental health impact of COVID-19. People can be informed without suffering by taking these steps:
- Limit the amount of news and social media consumed, and if possible, try to schedule news consumption into discrete periods that are not close to bedtime or other periods meant for relaxation.
- Reach out to loved ones and friends who remind you of strength and better times.
- Make time to relax and unwind, either through resting or engaging in an activity you enjoy.
- Take care of your body and mind with exercise.
- Try for 8 hours of sleep a night (even if it doesn’t happen).
- Use techniques such as meditating, doing yoga, or breathing to practice focusing your attention somewhere.
All of our lives have been disrupted by COVID-19 and acknowledging this to patients can help them feel less isolated and vulnerable. Our patients with diagnosed psychiatric disorders will be more susceptible to crippling anxiety, exacerbations in panic attacks, obsessive-compulsive disorder symptoms, and resurgence of suicidal ideation in the face of uncertainty and despair. They may also be more likely to experience the socioeconomic fallout of this pandemic. But it’s not just these individuals who will be hit with intense feelings as we wonder what the next day, month, or 6 months hold for us, our families, our friends, our country, and our world.
Recently, I had one of the more surreal experiences of my professional life. I work as a consulation-liaison psychiatrist on the medical wards, and I was consulted to treat a young woman from Central America with schizophrenia who made a serious suicide attempt in mid-February before COVID-19 was part of the lexicon.
After an overdose, she developed aspiration pneumonia and acute respiratory distress syndrome and ended up in the ICU on a respirator for 3 weeks. Her doctors and family were certain she would die, but she miraculously survived. By the time she was extubated and less delirious from her medically induced coma, the hospital had restricted all visitors because of COVID-19.
Because I speak Spanish, we developed as decent a working relationship as we could, considering the patient’s delirium and blunted affect. On top of restarting her antipsychotics, I had to inform her that her family was no longer allowed to come visit her. Outside of this room, I vacillated on how to tell a woman with a history of paranoia that the hospital would not allow her family to visit because we were in the middle of a pandemic. A contagious virus had quickly spread around the world, cases were now spiking in the United States, much of the country was on lockdown, and the hospital was limiting visitors because asymptomatic individuals could bring the virus into the hospital or be infected by asymptomatic staff.
As the words came out of my mouth, she looked at me as I have looked at psychotic individuals as they spin me yarns of impossible explanation for their symptoms when I know they’re simply psychotic and living in an alternate reality. Imagine just waking up from a coma and your doctor coming in to tell you: “The U.S. is on lockdown because a deadly virus is spreading throughout our country.” You’d think you’ve woken up in a zombie film. Yet, the patient simply nodded and asked: “Will I be able to use the phone to call my family?” I sighed with relief and helped her dial her brother’s number.
Haven’t we all listened to insane stories while keeping a straight face and then answered with a politely bland question? Just a few months ago, I treated a homeless woman with schizophrenia who calmly explained to me that her large malignant ovarian tumor (which I could see protruding under her gown) was the unborn heir of Queen Victoria and Prince Albert. If she allowed the doctors to take it out (that is, treat her cancer) she’d be assassinated by the Russian intelligence agency. She refused to let the doctors sentence her to death. Ultimately, we allowed her to refuse treatment. Despite a month of treatment with antipsychotic medication, her psychotic beliefs did not change, and we could not imagine forcing her through surgery and chemotherapy. She died in hospice.
I’ve walked the valleys of bizarro land many times. Working through the dark reality of COVID-19 should be no match for us psychiatrists who have listened to dark stories and responded with words of comfort or empathic silence. As mental health clinicians, I believe we are well equipped to fight on the front lines of the pandemic of fear that has arrested our country. We can make ourselves available to our patients, friends, family, and institutions – medical or otherwise – that are grappling with how to cope with the psychological impact of COVID-19.
Dr. Posada is a consultation-liaison psychiatry fellow with the Inova Fairfax Hospital/George Washington University program in Falls Church, Va., and associate producer of the MDedge Psychcast. She changed key details about the patients discussed to protect their confidentiality. Dr. Posada has no conflicts of interest.
In the Phoenix area, we are in a lull before the coronavirus storm
“There is no sound save the throb of the blowers and the vibration of the hard-driven engines. There is little motion as the gun crews man their guns and the fire-control details stand with heads bent and their hands clapped over their headphones. Somewhere out there are the enemy planes.”
That’s from one of my favorite WW2 histories, “Torpedo Junction,” by Robert J. Casey. He was a reporter stationed on board the cruiser USS Salt Lake City. The entry is from a day in February 1942 when the ship was part of a force that bombarded the Japanese encampment on Wake Island. The excerpt describes the scene later that afternoon, as they awaited a counterattack from Japanese planes.
For some reason that paragraph kept going through my mind this past Sunday afternoon, in the comparatively mundane situation of sitting in the hospital library signing off on my dictations and reviewing test results. I certainly was in no danger of being bombed or strafed, yet ...
Around me, the hospital was preparing for battle. As I rounded, most of the beds were empty and many of the floors above me were shut down and darkened. Waiting rooms were empty. If you hadn’t read the news you’d think there was a sudden lull in the health care world.
But the real truth is that it’s the calm before an anticipated storm. The elective procedures have all been canceled. Nonurgent outpatient tests are on hold. Only the sickest are being admitted, and they’re being sent out as soon as possible. Every bed possible is being kept open for the feared onslaught of coronavirus patients in the coming weeks. Protective equipment, already in short supply, is being stockpiled as it becomes available. Plans have been made to erect triage tents in the parking lots.
I sit in the library and think of this. It’s quiet except for the soft hum of the air conditioning blowers as Phoenix starts to warm up for another summer. The muted purr of the computer’s hard drive as I click away on the keys. On the floors above me the nurses and respiratory techs and doctors go about their daily business of patient care, wondering when the real battle will begin (probably 2-3 weeks from the time of this writing, if not sooner).
These are scary times. I’d be lying if I said I wasn’t frightened about what might happen to me, my family, my friends, my coworkers, my patients.
The people working in the hospital above me are in the same boat, all nervous about what’s going to happen. None of them is any more immune to coronavirus than the people they’ll be treating.
But, like the crew of the USS Salt Lake City, they’re ready to do their jobs. Because it’s part of what drove each of us into our own part of this field. Because we care and want to help. And health care doesn’t work unless the whole team does.
I respect them all for it. I always have and always will, and now more than ever.
Good luck.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
“There is no sound save the throb of the blowers and the vibration of the hard-driven engines. There is little motion as the gun crews man their guns and the fire-control details stand with heads bent and their hands clapped over their headphones. Somewhere out there are the enemy planes.”
That’s from one of my favorite WW2 histories, “Torpedo Junction,” by Robert J. Casey. He was a reporter stationed on board the cruiser USS Salt Lake City. The entry is from a day in February 1942 when the ship was part of a force that bombarded the Japanese encampment on Wake Island. The excerpt describes the scene later that afternoon, as they awaited a counterattack from Japanese planes.
For some reason that paragraph kept going through my mind this past Sunday afternoon, in the comparatively mundane situation of sitting in the hospital library signing off on my dictations and reviewing test results. I certainly was in no danger of being bombed or strafed, yet ...
Around me, the hospital was preparing for battle. As I rounded, most of the beds were empty and many of the floors above me were shut down and darkened. Waiting rooms were empty. If you hadn’t read the news you’d think there was a sudden lull in the health care world.
But the real truth is that it’s the calm before an anticipated storm. The elective procedures have all been canceled. Nonurgent outpatient tests are on hold. Only the sickest are being admitted, and they’re being sent out as soon as possible. Every bed possible is being kept open for the feared onslaught of coronavirus patients in the coming weeks. Protective equipment, already in short supply, is being stockpiled as it becomes available. Plans have been made to erect triage tents in the parking lots.
I sit in the library and think of this. It’s quiet except for the soft hum of the air conditioning blowers as Phoenix starts to warm up for another summer. The muted purr of the computer’s hard drive as I click away on the keys. On the floors above me the nurses and respiratory techs and doctors go about their daily business of patient care, wondering when the real battle will begin (probably 2-3 weeks from the time of this writing, if not sooner).
These are scary times. I’d be lying if I said I wasn’t frightened about what might happen to me, my family, my friends, my coworkers, my patients.
The people working in the hospital above me are in the same boat, all nervous about what’s going to happen. None of them is any more immune to coronavirus than the people they’ll be treating.
But, like the crew of the USS Salt Lake City, they’re ready to do their jobs. Because it’s part of what drove each of us into our own part of this field. Because we care and want to help. And health care doesn’t work unless the whole team does.
I respect them all for it. I always have and always will, and now more than ever.
Good luck.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
“There is no sound save the throb of the blowers and the vibration of the hard-driven engines. There is little motion as the gun crews man their guns and the fire-control details stand with heads bent and their hands clapped over their headphones. Somewhere out there are the enemy planes.”
That’s from one of my favorite WW2 histories, “Torpedo Junction,” by Robert J. Casey. He was a reporter stationed on board the cruiser USS Salt Lake City. The entry is from a day in February 1942 when the ship was part of a force that bombarded the Japanese encampment on Wake Island. The excerpt describes the scene later that afternoon, as they awaited a counterattack from Japanese planes.
For some reason that paragraph kept going through my mind this past Sunday afternoon, in the comparatively mundane situation of sitting in the hospital library signing off on my dictations and reviewing test results. I certainly was in no danger of being bombed or strafed, yet ...
Around me, the hospital was preparing for battle. As I rounded, most of the beds were empty and many of the floors above me were shut down and darkened. Waiting rooms were empty. If you hadn’t read the news you’d think there was a sudden lull in the health care world.
But the real truth is that it’s the calm before an anticipated storm. The elective procedures have all been canceled. Nonurgent outpatient tests are on hold. Only the sickest are being admitted, and they’re being sent out as soon as possible. Every bed possible is being kept open for the feared onslaught of coronavirus patients in the coming weeks. Protective equipment, already in short supply, is being stockpiled as it becomes available. Plans have been made to erect triage tents in the parking lots.
I sit in the library and think of this. It’s quiet except for the soft hum of the air conditioning blowers as Phoenix starts to warm up for another summer. The muted purr of the computer’s hard drive as I click away on the keys. On the floors above me the nurses and respiratory techs and doctors go about their daily business of patient care, wondering when the real battle will begin (probably 2-3 weeks from the time of this writing, if not sooner).
These are scary times. I’d be lying if I said I wasn’t frightened about what might happen to me, my family, my friends, my coworkers, my patients.
The people working in the hospital above me are in the same boat, all nervous about what’s going to happen. None of them is any more immune to coronavirus than the people they’ll be treating.
But, like the crew of the USS Salt Lake City, they’re ready to do their jobs. Because it’s part of what drove each of us into our own part of this field. Because we care and want to help. And health care doesn’t work unless the whole team does.
I respect them all for it. I always have and always will, and now more than ever.
Good luck.
Dr. Block has a solo neurology practice in Scottsdale, Ariz. He has no relevant disclosures.
Physician couples draft wills, face tough questions amid COVID-19
Not long ago, weekends for Cornelia Griggs, MD, meant making trips to the grocery store, chasing after two active toddlers, and eating brunch with her husband after a busy work week. But life has changed dramatically for the family since the spread of COVID-19. On a recent weekend, Dr. Griggs and her husband, Robert Goldstone, MD, spent their days off drafting a will.
“We’re both doctors, and we know that health care workers have an increased risk of contracting COVID,” said Dr. Griggs, a pediatric surgery fellow at Columbia University Irving Medical Center in New York. “It felt like the responsible thing to do: Have a will in place to make sure our wishes are clear about who would manage our property and assets, and who would take care of our kids – God forbid.”
Outlining their final wishes is among many difficult decisions the doctors, both 36, have been forced to make in recent weeks. Dr. Goldstone, a general surgeon at Massachusetts General Hospital in Boston, is no longer returning to New York during his time off, said Dr. Griggs, who has had known COVID-19 exposures. The couple’s children, aged 4 and almost 2, are temporarily living with their grandparents in Connecticut to decrease their exposure risk.
“I felt like it was safer for all of them to be there while I was going back and forth from the hospital,” Dr. Griggs said. “My husband is in Boston. The kids are in Connecticut and I’m in New York. That inherently is hard because our whole family is split up. I don’t know when it will be safe for me to see them again.”
Health professional couples across the country are facing similar challenges as they navigate the risk of contracting COVID-19 at work, while trying to protect their families at home. From childcare dilemmas to quarantine quandaries to end-of-life considerations, partners who work in health care are confronting tough questions as the pandemic continues.
The biggest challenge is the uncertainty, says Angela Weyand, MD, an Ann Arbor, Mich.–based pediatric hematologist/oncologist who shares two young daughters with husband Ted Claflin, MD, a physical medicine and rehabilitation physician. Dr. Weyand said she and her husband are primarily working remotely now, but she knows that one or both could be deployed to the hospital to help care for patients, if the need arises. Nearby Detroit has been labeled a coronavirus “hot spot” by the U.S. Surgeon General.
“Right now, I think our biggest fear is spreading coronavirus to those we love, especially those in higher risk groups,” she said. “At the same time, we are also concerned about our own health and our future ability to be there for our children, a fear that, thankfully, neither one of us has ever had to face before. We are trying to take things one day at a time, acknowledging all that we have to be grateful for, and also learning to accept that many things right now are outside of our control.”
Dr. Weyand, 38, and her husband, 40, finalized their wills in March.
“We have been working on them for quite some time, but before now, there has never been any urgency,” Dr. Weyand said. “Hearing about the high rate of infection in health care workers and the increasing number of deaths in young healthy people made us realize that this should be a priority.”
Dallas internist Bethany Agusala, MD, 36, and her husband, Kartik Agusala, MD, 41, a cardiologist, recently spent time engaged in the same activity. The couple, who work for the University of Texas Southwestern Medical Center, have two children, aged 2 and 4.
“The chances are hopefully small that something bad would happen to either one of us, but it just seemed like a good time to get [a will] in place,” Dr. Bethany Agusala said in an interview. “It’s never an easy thing to think about.
Pediatric surgeon Chethan Sathya, MD, 34, and his wife, 31, a physician assistant, have vastly altered their home routine to prevent the risk of exposure to their 16-month-old daughter. Dr. Sathya works for the Northwell Health System in New York, which has hundreds of hospitalized patients with COVID-19, Dr. Sathya said in an interview. He did not want to disclose his wife's name or institution, but said she works in a COVID-19 unit at a New York hospital.
When his wife returns home, she removes all of her clothes and places them in a bag, showers, and then isolates herself in the bedroom. Dr. Sathya brings his wife meals and then remains in a different room with their baby.
“It’s only been a few days,” he said. “We’re going to decide: Does she just stay in one room at all times or when she doesn’t work for a few days then after 1 day, can she come out? Should she get a hotel room elsewhere? These are the considerations.”
They employ an older nanny whom they also worry about, and with whom they try to limit contact, said Dr. Sathya, who practices at Cohen Children’s Medical Center. In a matter of weeks, Dr. Sathya anticipates he will be called upon to assist in some form with the COVID crisis.
“We haven’t figured that out. I’m not sure what we’ll do,” he said. “There is no perfect solution. You have to adapt. It’s very difficult to do so when you’re living in a condo in New York.”
For Dr. Griggs, life is much quieter at home without her husband and two “laughing, wiggly,” toddlers. Weekends are now defined by resting, video calls with her family, and exercising, when it’s safe, said Dr. Griggs, who recently penned a New York Times opinion piece about the pandemic and is also active on social media regarding personal protective equipment. She calls her husband her “rock” who never fails to put a smile on her face when they chat from across the miles. Her advice for other health care couples is to take it “one day at a time.”
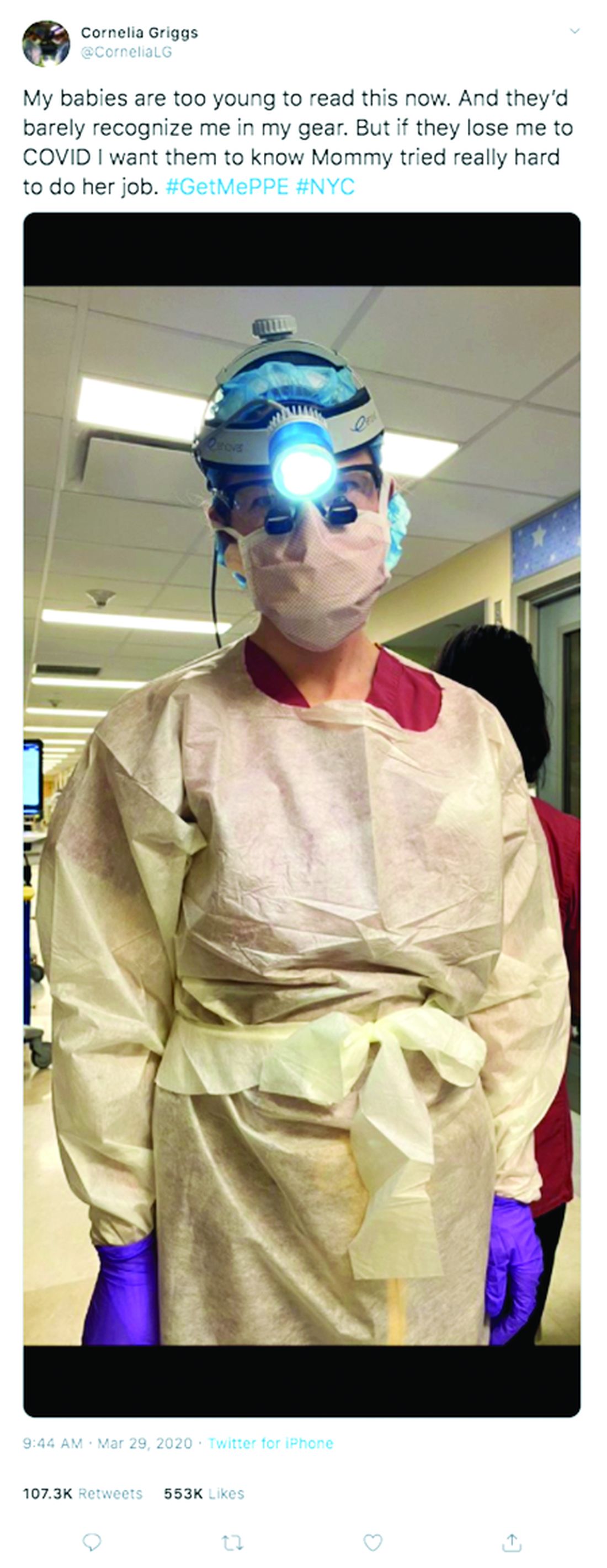
“Don’t try to make plans weeks in advance or let your mind go to a dark place,” she said. “It’s so easy to feel overwhelmed. The only way to get through this is to focus on surviving each day.”
Editor's Note, 3/31/20: Due to incorrect information provided, the hospital where Dr. Sathya's wife works was misidentified. We have removed the name of that hospital. The story does not include his wife's employer, because Dr. Sathya did not have permission to disclose her workplace and she wishes to remain anonymous.
Not long ago, weekends for Cornelia Griggs, MD, meant making trips to the grocery store, chasing after two active toddlers, and eating brunch with her husband after a busy work week. But life has changed dramatically for the family since the spread of COVID-19. On a recent weekend, Dr. Griggs and her husband, Robert Goldstone, MD, spent their days off drafting a will.
“We’re both doctors, and we know that health care workers have an increased risk of contracting COVID,” said Dr. Griggs, a pediatric surgery fellow at Columbia University Irving Medical Center in New York. “It felt like the responsible thing to do: Have a will in place to make sure our wishes are clear about who would manage our property and assets, and who would take care of our kids – God forbid.”
Outlining their final wishes is among many difficult decisions the doctors, both 36, have been forced to make in recent weeks. Dr. Goldstone, a general surgeon at Massachusetts General Hospital in Boston, is no longer returning to New York during his time off, said Dr. Griggs, who has had known COVID-19 exposures. The couple’s children, aged 4 and almost 2, are temporarily living with their grandparents in Connecticut to decrease their exposure risk.
“I felt like it was safer for all of them to be there while I was going back and forth from the hospital,” Dr. Griggs said. “My husband is in Boston. The kids are in Connecticut and I’m in New York. That inherently is hard because our whole family is split up. I don’t know when it will be safe for me to see them again.”
Health professional couples across the country are facing similar challenges as they navigate the risk of contracting COVID-19 at work, while trying to protect their families at home. From childcare dilemmas to quarantine quandaries to end-of-life considerations, partners who work in health care are confronting tough questions as the pandemic continues.
The biggest challenge is the uncertainty, says Angela Weyand, MD, an Ann Arbor, Mich.–based pediatric hematologist/oncologist who shares two young daughters with husband Ted Claflin, MD, a physical medicine and rehabilitation physician. Dr. Weyand said she and her husband are primarily working remotely now, but she knows that one or both could be deployed to the hospital to help care for patients, if the need arises. Nearby Detroit has been labeled a coronavirus “hot spot” by the U.S. Surgeon General.
“Right now, I think our biggest fear is spreading coronavirus to those we love, especially those in higher risk groups,” she said. “At the same time, we are also concerned about our own health and our future ability to be there for our children, a fear that, thankfully, neither one of us has ever had to face before. We are trying to take things one day at a time, acknowledging all that we have to be grateful for, and also learning to accept that many things right now are outside of our control.”
Dr. Weyand, 38, and her husband, 40, finalized their wills in March.
“We have been working on them for quite some time, but before now, there has never been any urgency,” Dr. Weyand said. “Hearing about the high rate of infection in health care workers and the increasing number of deaths in young healthy people made us realize that this should be a priority.”
Dallas internist Bethany Agusala, MD, 36, and her husband, Kartik Agusala, MD, 41, a cardiologist, recently spent time engaged in the same activity. The couple, who work for the University of Texas Southwestern Medical Center, have two children, aged 2 and 4.
“The chances are hopefully small that something bad would happen to either one of us, but it just seemed like a good time to get [a will] in place,” Dr. Bethany Agusala said in an interview. “It’s never an easy thing to think about.
Pediatric surgeon Chethan Sathya, MD, 34, and his wife, 31, a physician assistant, have vastly altered their home routine to prevent the risk of exposure to their 16-month-old daughter. Dr. Sathya works for the Northwell Health System in New York, which has hundreds of hospitalized patients with COVID-19, Dr. Sathya said in an interview. He did not want to disclose his wife's name or institution, but said she works in a COVID-19 unit at a New York hospital.
When his wife returns home, she removes all of her clothes and places them in a bag, showers, and then isolates herself in the bedroom. Dr. Sathya brings his wife meals and then remains in a different room with their baby.
“It’s only been a few days,” he said. “We’re going to decide: Does she just stay in one room at all times or when she doesn’t work for a few days then after 1 day, can she come out? Should she get a hotel room elsewhere? These are the considerations.”
They employ an older nanny whom they also worry about, and with whom they try to limit contact, said Dr. Sathya, who practices at Cohen Children’s Medical Center. In a matter of weeks, Dr. Sathya anticipates he will be called upon to assist in some form with the COVID crisis.
“We haven’t figured that out. I’m not sure what we’ll do,” he said. “There is no perfect solution. You have to adapt. It’s very difficult to do so when you’re living in a condo in New York.”
For Dr. Griggs, life is much quieter at home without her husband and two “laughing, wiggly,” toddlers. Weekends are now defined by resting, video calls with her family, and exercising, when it’s safe, said Dr. Griggs, who recently penned a New York Times opinion piece about the pandemic and is also active on social media regarding personal protective equipment. She calls her husband her “rock” who never fails to put a smile on her face when they chat from across the miles. Her advice for other health care couples is to take it “one day at a time.”
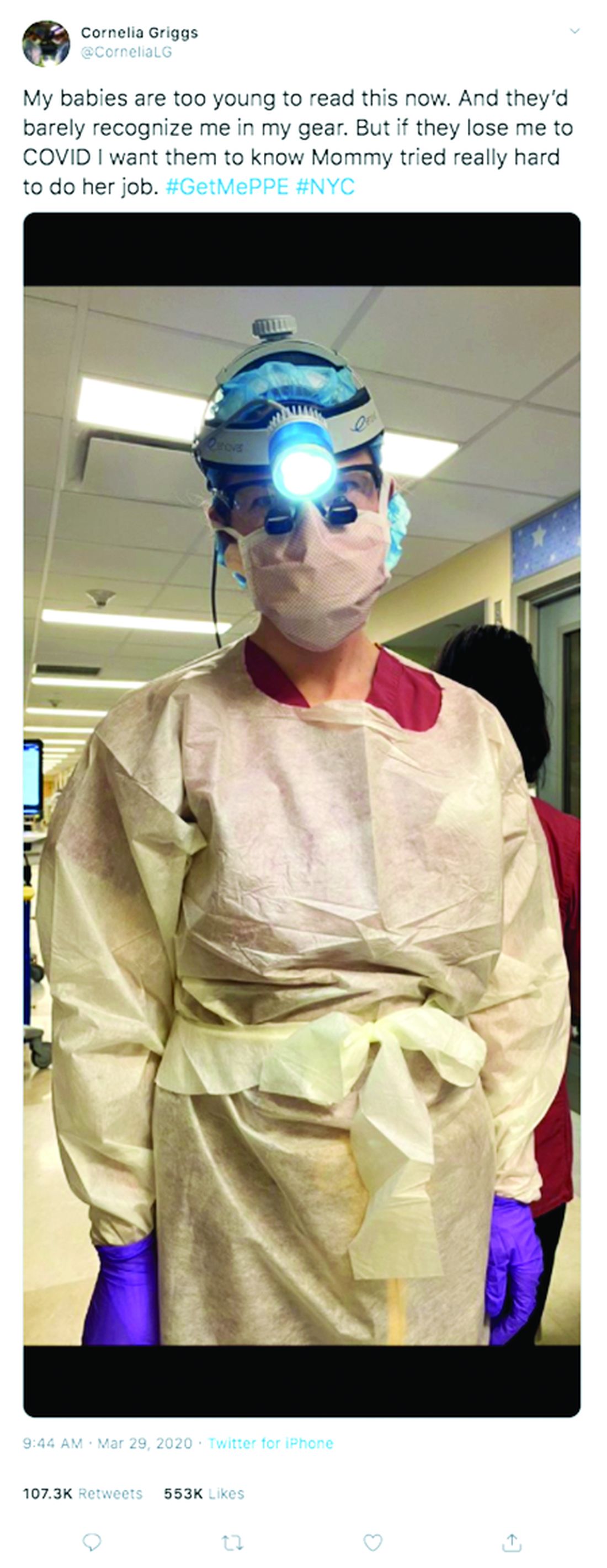
“Don’t try to make plans weeks in advance or let your mind go to a dark place,” she said. “It’s so easy to feel overwhelmed. The only way to get through this is to focus on surviving each day.”
Editor's Note, 3/31/20: Due to incorrect information provided, the hospital where Dr. Sathya's wife works was misidentified. We have removed the name of that hospital. The story does not include his wife's employer, because Dr. Sathya did not have permission to disclose her workplace and she wishes to remain anonymous.
Not long ago, weekends for Cornelia Griggs, MD, meant making trips to the grocery store, chasing after two active toddlers, and eating brunch with her husband after a busy work week. But life has changed dramatically for the family since the spread of COVID-19. On a recent weekend, Dr. Griggs and her husband, Robert Goldstone, MD, spent their days off drafting a will.
“We’re both doctors, and we know that health care workers have an increased risk of contracting COVID,” said Dr. Griggs, a pediatric surgery fellow at Columbia University Irving Medical Center in New York. “It felt like the responsible thing to do: Have a will in place to make sure our wishes are clear about who would manage our property and assets, and who would take care of our kids – God forbid.”
Outlining their final wishes is among many difficult decisions the doctors, both 36, have been forced to make in recent weeks. Dr. Goldstone, a general surgeon at Massachusetts General Hospital in Boston, is no longer returning to New York during his time off, said Dr. Griggs, who has had known COVID-19 exposures. The couple’s children, aged 4 and almost 2, are temporarily living with their grandparents in Connecticut to decrease their exposure risk.
“I felt like it was safer for all of them to be there while I was going back and forth from the hospital,” Dr. Griggs said. “My husband is in Boston. The kids are in Connecticut and I’m in New York. That inherently is hard because our whole family is split up. I don’t know when it will be safe for me to see them again.”
Health professional couples across the country are facing similar challenges as they navigate the risk of contracting COVID-19 at work, while trying to protect their families at home. From childcare dilemmas to quarantine quandaries to end-of-life considerations, partners who work in health care are confronting tough questions as the pandemic continues.
The biggest challenge is the uncertainty, says Angela Weyand, MD, an Ann Arbor, Mich.–based pediatric hematologist/oncologist who shares two young daughters with husband Ted Claflin, MD, a physical medicine and rehabilitation physician. Dr. Weyand said she and her husband are primarily working remotely now, but she knows that one or both could be deployed to the hospital to help care for patients, if the need arises. Nearby Detroit has been labeled a coronavirus “hot spot” by the U.S. Surgeon General.
“Right now, I think our biggest fear is spreading coronavirus to those we love, especially those in higher risk groups,” she said. “At the same time, we are also concerned about our own health and our future ability to be there for our children, a fear that, thankfully, neither one of us has ever had to face before. We are trying to take things one day at a time, acknowledging all that we have to be grateful for, and also learning to accept that many things right now are outside of our control.”
Dr. Weyand, 38, and her husband, 40, finalized their wills in March.
“We have been working on them for quite some time, but before now, there has never been any urgency,” Dr. Weyand said. “Hearing about the high rate of infection in health care workers and the increasing number of deaths in young healthy people made us realize that this should be a priority.”
Dallas internist Bethany Agusala, MD, 36, and her husband, Kartik Agusala, MD, 41, a cardiologist, recently spent time engaged in the same activity. The couple, who work for the University of Texas Southwestern Medical Center, have two children, aged 2 and 4.
“The chances are hopefully small that something bad would happen to either one of us, but it just seemed like a good time to get [a will] in place,” Dr. Bethany Agusala said in an interview. “It’s never an easy thing to think about.
Pediatric surgeon Chethan Sathya, MD, 34, and his wife, 31, a physician assistant, have vastly altered their home routine to prevent the risk of exposure to their 16-month-old daughter. Dr. Sathya works for the Northwell Health System in New York, which has hundreds of hospitalized patients with COVID-19, Dr. Sathya said in an interview. He did not want to disclose his wife's name or institution, but said she works in a COVID-19 unit at a New York hospital.
When his wife returns home, she removes all of her clothes and places them in a bag, showers, and then isolates herself in the bedroom. Dr. Sathya brings his wife meals and then remains in a different room with their baby.
“It’s only been a few days,” he said. “We’re going to decide: Does she just stay in one room at all times or when she doesn’t work for a few days then after 1 day, can she come out? Should she get a hotel room elsewhere? These are the considerations.”
They employ an older nanny whom they also worry about, and with whom they try to limit contact, said Dr. Sathya, who practices at Cohen Children’s Medical Center. In a matter of weeks, Dr. Sathya anticipates he will be called upon to assist in some form with the COVID crisis.
“We haven’t figured that out. I’m not sure what we’ll do,” he said. “There is no perfect solution. You have to adapt. It’s very difficult to do so when you’re living in a condo in New York.”
For Dr. Griggs, life is much quieter at home without her husband and two “laughing, wiggly,” toddlers. Weekends are now defined by resting, video calls with her family, and exercising, when it’s safe, said Dr. Griggs, who recently penned a New York Times opinion piece about the pandemic and is also active on social media regarding personal protective equipment. She calls her husband her “rock” who never fails to put a smile on her face when they chat from across the miles. Her advice for other health care couples is to take it “one day at a time.”
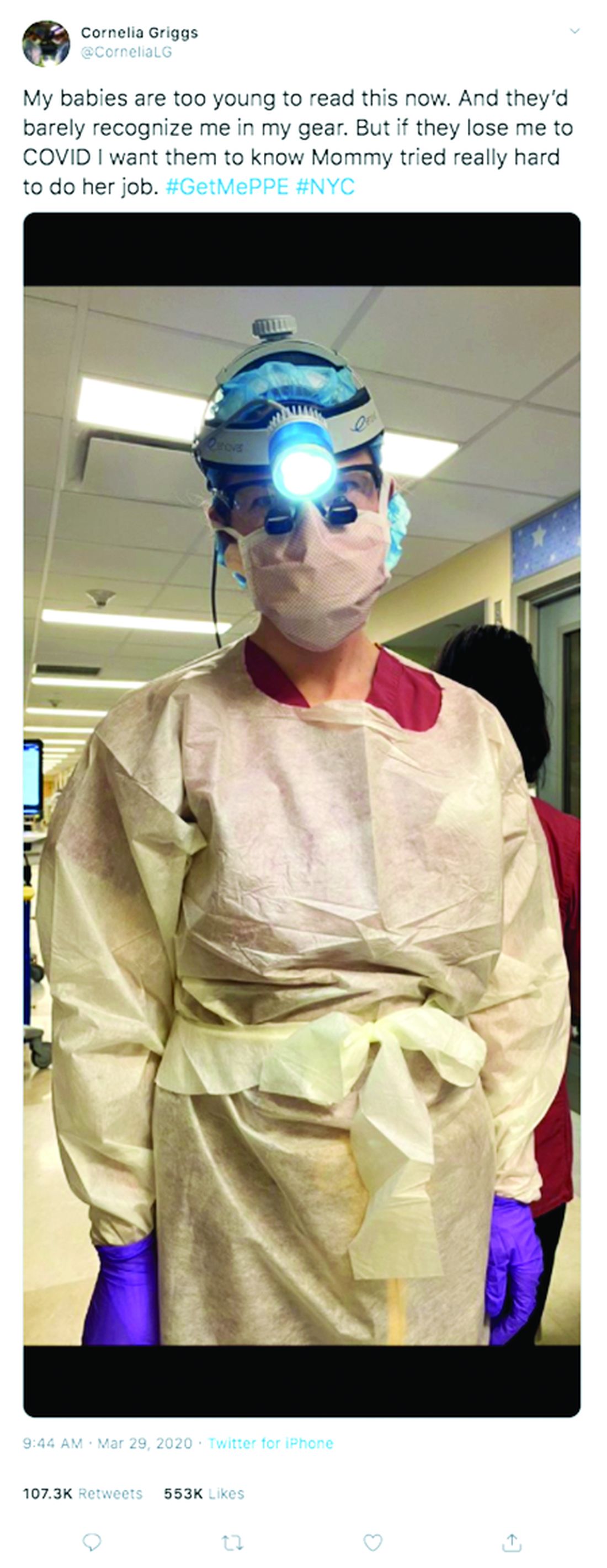
“Don’t try to make plans weeks in advance or let your mind go to a dark place,” she said. “It’s so easy to feel overwhelmed. The only way to get through this is to focus on surviving each day.”
Editor's Note, 3/31/20: Due to incorrect information provided, the hospital where Dr. Sathya's wife works was misidentified. We have removed the name of that hospital. The story does not include his wife's employer, because Dr. Sathya did not have permission to disclose her workplace and she wishes to remain anonymous.
Before the COVID-19 surge hits your facility, take steps to boost capacity
, according to a physician leader and a health workforce expert.
Polly Pittman, PhD, is hearing a lot of concern among health care workers that it’s difficult to find definitive and accurate information about how best to protect themselves and their families, she said during a webinar by the Alliance for Health Policy titled Health System Capacity: Protecting Frontline Health Workers. “The knowledge base is evolving very quickly,” said Dr. Pittman, Fitzhugh Mullan Professor of Health Workforce Equity at the Milken Institute School of Public Health, George Washington University, Washington.
Stephen Parodi, MD, agreed that effective communication is job one in the health care workplace during the crisis. “I can’t stress enough ... that communications are paramount and you can’t overcommunicate,” said Dr. Parodi, executive vice president of external affairs, communications, and brand at the Permanente Federation and associate executive director of the Permanente Medical Group, Vallejo, Calif.
“We’re in a situation of confusion and improvisation right now,” regarding protection of health care workers, said Dr. Pittman. The potential exists for “a downward spiral where you have the lack of training, the shortages in terms of protective gear, weakening of guidelines, and confusion regarding guidelines at federal level, creating a potential cascade” that may result in “moral distress and fatigue. ... That’s not occurring now, but that’s the danger” unless the personal protective equipment (PPE) situation is adequately addressed very soon, she said.
Dr. Pittman also pointed out the concerns that many of the 18 million U.S. health care workers have for their families should they themselves fall ill or transmit coronavirus to family members. “The danger exists of a mass exodus. People don’t have to show up at work, and they won’t show up at work if they don’t feel supported and safe.”
Dr. Parodi said that the Permanente organization is on a better footing than many workplaces. “We actually had an early experience because of the work that we did to support the Diamond Princess cruise ship evacuees from Yokahama in February.” That ship was quarantined upon arrival in Yokahama on Feb. 3 because a passenger had a confirmed test for SARS-CoV-2 infection, and a quarter of the 428 Americans on board subsequently tested positive. Most of them were evacuated to California or Texas. “That actually gave us the experience for providing care within the hospital setting – and also for containment strategies,” he said.
“We quickly understood that we needed to move to a mitigation strategy,” said Dr. Parodi. Use of PPE has been “tailored for how the virus is spread.” In the absence of the risk of aerosol transmission from certain procedures, health care workers use gowns, gloves, surgical masks, and goggles.
Because of anticipated “supply chain shortfalls,” Dr. Parodi said that his organization implemented Centers for Disease Control and Prevention guidelines for reuse and extended use of N95 respirators early on. “Even if you’re not in a locale that’s been hit, you need to be on wartime footing for preserving PPE.”
Telehealth, said Dr. Parodi, has been implemented “in a huge way” throughout the Permanente system. “We have reduced primary care visits by 90% in the past week, and also subspecialty visits by 50%. … A large amount of the workforce can work from home. We turned off elective surgeries more than a week ago to reduce the number of patients who are requiring intensive care.” Making these changes means the organization is more prepared now for a surge they expect in the coming weeks.
Dr. Pittman voiced an opinion widely shared by those who are implementing large-scale telehealth efforts “We’re going to learn a lot. Many of the traditional doctor-patient visits can be done by telemedicine in the future.”
Knowledge about local trends in infection rates is key to preparedness. “We’ve ramped up testing, to understand what’s happening in the community,” said Dr. Parodi, noting that test turnaround time is currently running 8-24 hours. Tightening up this window can free up resources when an admitted patient’s test is negative.
Still, some national projections forecast a need for hospital beds at two to three times current capacity – or even more, said Dr. Parodi.
He noted that Permanente is “working hand in glove with state authorities throughout the country.” Efforts include establishing alternative sites for assessment and testing, as well as opening up closed hospitals and working with the National Guard and the Department of Defense to prepare mobile hospital units that can be deployed in areas with peak infection rates. “Having all of those options available to us is critically important,” he said.
To mitigate potential provider shortages, Dr. Pittman said, “All members of the care team could potentially do more” than their current licenses allow. Expanding the scope of practice for pharmacists, clinical laboratory staff, licensed practical nurses, and medical assistants can help with efficient care delivery.
Other measures include expedited licensing for near-graduates and nonpracticing foreign medical graduates, as well as relicensing for retired health care personnel and those who are not currently working directly with patients, she said.
Getting these things done “requires leadership on behalf of the licensing bodies,” as well as coordination with state regulatory authorities, Dr. Pittman pointed out.
Dr. Parodi called for state and federal governments to implement emergency declarations that suspend some existing health codes to achieve repurposing of staff. Getting these measures in place now will allow facilities “to be able to provide that in-time training now before the surge occurs. ... We are actively developing plans knowing that there’s going to be a need for more critical care.”
The game plan at Permanente, he said, is to repurpose critical care physicians to provide consultations to multiple hospitalists who are providing the bulk of frontline care. At the same time, they plan to repurpose other specialists to backfill the hospitalists, and to repurpose family medicine physicians to supplement staff in emergency departments and other frontline intake areas.
All the organizational measures being taken won’t be in vain if they increase preparedness for the long battle ahead, he said. “We need to double down on the work. ... We need to continue social distancing, and we’ve got to ramp up testing. Until we do that we have to hold the line on basic public health measures.”
Dr. Parodi is employed by Permanente. The panelists reported no disclosures relevant to the presentation, which was sponsored by the Alliance for Health Policy, the Commonwealth Fund, and the National Institute for Health Care Management Foundation.
, according to a physician leader and a health workforce expert.
Polly Pittman, PhD, is hearing a lot of concern among health care workers that it’s difficult to find definitive and accurate information about how best to protect themselves and their families, she said during a webinar by the Alliance for Health Policy titled Health System Capacity: Protecting Frontline Health Workers. “The knowledge base is evolving very quickly,” said Dr. Pittman, Fitzhugh Mullan Professor of Health Workforce Equity at the Milken Institute School of Public Health, George Washington University, Washington.
Stephen Parodi, MD, agreed that effective communication is job one in the health care workplace during the crisis. “I can’t stress enough ... that communications are paramount and you can’t overcommunicate,” said Dr. Parodi, executive vice president of external affairs, communications, and brand at the Permanente Federation and associate executive director of the Permanente Medical Group, Vallejo, Calif.
“We’re in a situation of confusion and improvisation right now,” regarding protection of health care workers, said Dr. Pittman. The potential exists for “a downward spiral where you have the lack of training, the shortages in terms of protective gear, weakening of guidelines, and confusion regarding guidelines at federal level, creating a potential cascade” that may result in “moral distress and fatigue. ... That’s not occurring now, but that’s the danger” unless the personal protective equipment (PPE) situation is adequately addressed very soon, she said.
Dr. Pittman also pointed out the concerns that many of the 18 million U.S. health care workers have for their families should they themselves fall ill or transmit coronavirus to family members. “The danger exists of a mass exodus. People don’t have to show up at work, and they won’t show up at work if they don’t feel supported and safe.”
Dr. Parodi said that the Permanente organization is on a better footing than many workplaces. “We actually had an early experience because of the work that we did to support the Diamond Princess cruise ship evacuees from Yokahama in February.” That ship was quarantined upon arrival in Yokahama on Feb. 3 because a passenger had a confirmed test for SARS-CoV-2 infection, and a quarter of the 428 Americans on board subsequently tested positive. Most of them were evacuated to California or Texas. “That actually gave us the experience for providing care within the hospital setting – and also for containment strategies,” he said.
“We quickly understood that we needed to move to a mitigation strategy,” said Dr. Parodi. Use of PPE has been “tailored for how the virus is spread.” In the absence of the risk of aerosol transmission from certain procedures, health care workers use gowns, gloves, surgical masks, and goggles.
Because of anticipated “supply chain shortfalls,” Dr. Parodi said that his organization implemented Centers for Disease Control and Prevention guidelines for reuse and extended use of N95 respirators early on. “Even if you’re not in a locale that’s been hit, you need to be on wartime footing for preserving PPE.”
Telehealth, said Dr. Parodi, has been implemented “in a huge way” throughout the Permanente system. “We have reduced primary care visits by 90% in the past week, and also subspecialty visits by 50%. … A large amount of the workforce can work from home. We turned off elective surgeries more than a week ago to reduce the number of patients who are requiring intensive care.” Making these changes means the organization is more prepared now for a surge they expect in the coming weeks.
Dr. Pittman voiced an opinion widely shared by those who are implementing large-scale telehealth efforts “We’re going to learn a lot. Many of the traditional doctor-patient visits can be done by telemedicine in the future.”
Knowledge about local trends in infection rates is key to preparedness. “We’ve ramped up testing, to understand what’s happening in the community,” said Dr. Parodi, noting that test turnaround time is currently running 8-24 hours. Tightening up this window can free up resources when an admitted patient’s test is negative.
Still, some national projections forecast a need for hospital beds at two to three times current capacity – or even more, said Dr. Parodi.
He noted that Permanente is “working hand in glove with state authorities throughout the country.” Efforts include establishing alternative sites for assessment and testing, as well as opening up closed hospitals and working with the National Guard and the Department of Defense to prepare mobile hospital units that can be deployed in areas with peak infection rates. “Having all of those options available to us is critically important,” he said.
To mitigate potential provider shortages, Dr. Pittman said, “All members of the care team could potentially do more” than their current licenses allow. Expanding the scope of practice for pharmacists, clinical laboratory staff, licensed practical nurses, and medical assistants can help with efficient care delivery.
Other measures include expedited licensing for near-graduates and nonpracticing foreign medical graduates, as well as relicensing for retired health care personnel and those who are not currently working directly with patients, she said.
Getting these things done “requires leadership on behalf of the licensing bodies,” as well as coordination with state regulatory authorities, Dr. Pittman pointed out.
Dr. Parodi called for state and federal governments to implement emergency declarations that suspend some existing health codes to achieve repurposing of staff. Getting these measures in place now will allow facilities “to be able to provide that in-time training now before the surge occurs. ... We are actively developing plans knowing that there’s going to be a need for more critical care.”
The game plan at Permanente, he said, is to repurpose critical care physicians to provide consultations to multiple hospitalists who are providing the bulk of frontline care. At the same time, they plan to repurpose other specialists to backfill the hospitalists, and to repurpose family medicine physicians to supplement staff in emergency departments and other frontline intake areas.
All the organizational measures being taken won’t be in vain if they increase preparedness for the long battle ahead, he said. “We need to double down on the work. ... We need to continue social distancing, and we’ve got to ramp up testing. Until we do that we have to hold the line on basic public health measures.”
Dr. Parodi is employed by Permanente. The panelists reported no disclosures relevant to the presentation, which was sponsored by the Alliance for Health Policy, the Commonwealth Fund, and the National Institute for Health Care Management Foundation.
, according to a physician leader and a health workforce expert.
Polly Pittman, PhD, is hearing a lot of concern among health care workers that it’s difficult to find definitive and accurate information about how best to protect themselves and their families, she said during a webinar by the Alliance for Health Policy titled Health System Capacity: Protecting Frontline Health Workers. “The knowledge base is evolving very quickly,” said Dr. Pittman, Fitzhugh Mullan Professor of Health Workforce Equity at the Milken Institute School of Public Health, George Washington University, Washington.
Stephen Parodi, MD, agreed that effective communication is job one in the health care workplace during the crisis. “I can’t stress enough ... that communications are paramount and you can’t overcommunicate,” said Dr. Parodi, executive vice president of external affairs, communications, and brand at the Permanente Federation and associate executive director of the Permanente Medical Group, Vallejo, Calif.
“We’re in a situation of confusion and improvisation right now,” regarding protection of health care workers, said Dr. Pittman. The potential exists for “a downward spiral where you have the lack of training, the shortages in terms of protective gear, weakening of guidelines, and confusion regarding guidelines at federal level, creating a potential cascade” that may result in “moral distress and fatigue. ... That’s not occurring now, but that’s the danger” unless the personal protective equipment (PPE) situation is adequately addressed very soon, she said.
Dr. Pittman also pointed out the concerns that many of the 18 million U.S. health care workers have for their families should they themselves fall ill or transmit coronavirus to family members. “The danger exists of a mass exodus. People don’t have to show up at work, and they won’t show up at work if they don’t feel supported and safe.”
Dr. Parodi said that the Permanente organization is on a better footing than many workplaces. “We actually had an early experience because of the work that we did to support the Diamond Princess cruise ship evacuees from Yokahama in February.” That ship was quarantined upon arrival in Yokahama on Feb. 3 because a passenger had a confirmed test for SARS-CoV-2 infection, and a quarter of the 428 Americans on board subsequently tested positive. Most of them were evacuated to California or Texas. “That actually gave us the experience for providing care within the hospital setting – and also for containment strategies,” he said.
“We quickly understood that we needed to move to a mitigation strategy,” said Dr. Parodi. Use of PPE has been “tailored for how the virus is spread.” In the absence of the risk of aerosol transmission from certain procedures, health care workers use gowns, gloves, surgical masks, and goggles.
Because of anticipated “supply chain shortfalls,” Dr. Parodi said that his organization implemented Centers for Disease Control and Prevention guidelines for reuse and extended use of N95 respirators early on. “Even if you’re not in a locale that’s been hit, you need to be on wartime footing for preserving PPE.”
Telehealth, said Dr. Parodi, has been implemented “in a huge way” throughout the Permanente system. “We have reduced primary care visits by 90% in the past week, and also subspecialty visits by 50%. … A large amount of the workforce can work from home. We turned off elective surgeries more than a week ago to reduce the number of patients who are requiring intensive care.” Making these changes means the organization is more prepared now for a surge they expect in the coming weeks.
Dr. Pittman voiced an opinion widely shared by those who are implementing large-scale telehealth efforts “We’re going to learn a lot. Many of the traditional doctor-patient visits can be done by telemedicine in the future.”
Knowledge about local trends in infection rates is key to preparedness. “We’ve ramped up testing, to understand what’s happening in the community,” said Dr. Parodi, noting that test turnaround time is currently running 8-24 hours. Tightening up this window can free up resources when an admitted patient’s test is negative.
Still, some national projections forecast a need for hospital beds at two to three times current capacity – or even more, said Dr. Parodi.
He noted that Permanente is “working hand in glove with state authorities throughout the country.” Efforts include establishing alternative sites for assessment and testing, as well as opening up closed hospitals and working with the National Guard and the Department of Defense to prepare mobile hospital units that can be deployed in areas with peak infection rates. “Having all of those options available to us is critically important,” he said.
To mitigate potential provider shortages, Dr. Pittman said, “All members of the care team could potentially do more” than their current licenses allow. Expanding the scope of practice for pharmacists, clinical laboratory staff, licensed practical nurses, and medical assistants can help with efficient care delivery.
Other measures include expedited licensing for near-graduates and nonpracticing foreign medical graduates, as well as relicensing for retired health care personnel and those who are not currently working directly with patients, she said.
Getting these things done “requires leadership on behalf of the licensing bodies,” as well as coordination with state regulatory authorities, Dr. Pittman pointed out.
Dr. Parodi called for state and federal governments to implement emergency declarations that suspend some existing health codes to achieve repurposing of staff. Getting these measures in place now will allow facilities “to be able to provide that in-time training now before the surge occurs. ... We are actively developing plans knowing that there’s going to be a need for more critical care.”
The game plan at Permanente, he said, is to repurpose critical care physicians to provide consultations to multiple hospitalists who are providing the bulk of frontline care. At the same time, they plan to repurpose other specialists to backfill the hospitalists, and to repurpose family medicine physicians to supplement staff in emergency departments and other frontline intake areas.
All the organizational measures being taken won’t be in vain if they increase preparedness for the long battle ahead, he said. “We need to double down on the work. ... We need to continue social distancing, and we’ve got to ramp up testing. Until we do that we have to hold the line on basic public health measures.”
Dr. Parodi is employed by Permanente. The panelists reported no disclosures relevant to the presentation, which was sponsored by the Alliance for Health Policy, the Commonwealth Fund, and the National Institute for Health Care Management Foundation.
REPORTING FROM AN ALLIANCE FOR HEALTH POLICY WEBINAR
FDA okays emergency use of convalescent plasma for seriously ill COVID-19 patients
As the proportion of patients infected with COVID-19 continues to rise in the United States, the Food and Drug Administration is facilitating access to COVID-19 convalescent plasma for use in patients with serious or immediately life-threatening COVID-19 infections.
While clinical trials are underway to evaluate the safety and efficacy of administering convalescent plasma to patients with COVID-19, the FDA is granting clinicians permission for use of investigational convalescent plasma under single-patient emergency Investigational New Drug Applications (INDs), since no known cure exists and a vaccine is more than 1 year away from becoming available.
This allows the use of an investigational drug for the treatment of an individual patient by a licensed physician upon FDA authorization. This does not include the use of COVID-19 convalescent plasma for the prevention of infection, according to a statement issued by the agency on March 24.
“It is possible that convalescent plasma that contains antibodies to SARS-CoV-2 (the virus that causes COVID-19) might be effective against the infection,” the FDA statement reads. “Use of convalescent plasma has been studied in outbreaks of other respiratory infections, including the 2009-2010 H1N1 influenza virus pandemic, 2003 SARS-CoV-1 epidemic, and the 2012 MERS-CoV epidemic. Although promising, convalescent plasma has not been shown to be effective in every disease studied.”
“I think the FDA got caught initially a little flat-footed when it came to the development of COVID-19 tests, but they’re quickly catching up,” Peter J. Pitts, who was the FDA’s associate commissioner from 2002 to 2004, said in an interview. “I think that the attitude now is, ‘If it’s safe, let’s create a pathway to see how these things work in the real world.’ I think that’s going to be as true for treatments to lessen the symptoms and shorten the duration of the disease, as well as convalescent plasma as a potential alternative to a yet-to-be-developed vaccine.”
At the University of Washington School of Medicine, Seattle, Terry B. Gernsheimer, MD, and her colleagues are recruiting recovered COVID-19 patients to donate plasma for seriously ill patients affected with the virus. “The thought of using convalescent plasma makes total sense, because it’s immediately available, and it’s something that we can try to give people,” said Dr. Gernsheimer, a hematologist who is professor of medicine at the medical school. “It’s been used in China, and reports should be coming out shortly about their experience with this.”
In a case series that appeared in JAMA on March 27 (doi: 10.1001/jama.2020.4783), Chinese researchers led by Chenguang Shen, PhD, reported findings from five critically ill COVID-19 patients with acute respiratory distress syndrome who received a transfusion with convalescent plasma at Shenzhen Third People’s Hospital 10 and 22 days after hospital admission. The patients ranged in age from 36 to 73 years, three were men, and all were receiving mechanical ventilation at the time of treatment.
Dr. Shen and colleagues reported that viral loads decreased and became negative within 12 days following the transfusion. Three of the patients were discharged from the hospital after a length of stay that ranged from 51 to 55 days, and two remain in stable condition at 37 days after the transfusion. The researchers pointed out that all patients received antiviral agents, including interferon and lopinavir/ritonavir, during and following convalescent plasma treatment, “which also may have contributed to the viral clearance observed.”
Under the FDA policy on emergency IND use, COVID-19 convalescent plasma must only be collected from recovered individuals if they are eligible to donate blood, required testing must be performed, and the donation must be found suitable.
Potential donors “are going to be screened the way all blood donors are screened,” Dr. Gernsheimer said. “It’s not going to be any less safe than any unit of plasma that’s on the shelf that comes from our volunteer donors. There are always transfusion reactions that we have to worry about, [and] there are potentially unknown pathogens that we don’t yet know about that we are not yet testing for. It’s the regular risk we see with any unit of plasma.”
She added that COVID-19 survivors appear to start increasing their titer of the antibody around day 28. “We’ll be looking for recovered individuals who have had a documented infection, and whose symptoms started about 28 days before we collect,” she said.
The FDA advises clinicians to address several considerations for donor eligibility, including prior diagnosis of COVID-19 documented by a laboratory test; complete resolution of symptoms at least 14 days prior to donation; female donors negative for HLA antibodies or male donors, and negative results for COVID-19 either from one or more nasopharyngeal swab specimens or by a molecular diagnostic test from blood. [A partial list of available tests can be accessed on the FDA website.] The agency also advises that donors have defined SARS-CoV-2–neutralizing antibody titers, if testing can be conducted (optimally greater than 1:320).
Patients eligible to receive COVID-19 convalescent plasma must have a severe or immediately life-threatening infection with laboratory-confirmed COVID-19. The agency defines severe disease as dyspnea, respiratory frequency of 30 per minute or greater, blood oxygen saturation of 93% or less, partial pressure of arterial oxygen to fraction of inspired oxygen ratio of less than 300, and/or lung infiltrates of greater than 50% within 24-48 hours. Life-threatening disease is defined as respiratory failure, septic shock, and/or multiple organ dysfunction or failure. Patients must provide informed consent.
The potential risks of receiving COVID-19 convalescent plasma remain unknown, according to Dr. Gernsheimer. “What some people have thought about is, could there be such an inflammatory response with the virus that we would initially see these patients get worse?” she said. “My understanding is that has not occurred in China yet, but we don’t have all those data. But we always worry if we have something that’s going to cause inflammation around an infection, for example, that could initially make it more difficult to breathe if it’s a lung infection. So far, my understanding is that has not been seen.”
For COVID-19 convalescent plasma authorization requests that require a response within 4-8 hours, requesting clinicians may complete form 3296 and submit it by email to [email protected].
For COVID-19 convalescent plasma authorization requests that require a response in less than 4 hours, or if the clinician is unable to complete and submit form 3926 because of extenuating circumstances, verbal authorization can be sought by calling the FDA’s Office of Emergency Operations at 1-866-300-4374.
The FDA is working with the National Institutes of Health, the Centers for Disease Control and Prevention, and other government partners to develop protocols for use by multiple investigators in order to coordinate the collection and use of COVID-19 convalescent plasma.
“It’s crucial that data be captured for every patient so that we really understand what safety and effectiveness looks like on as close to a real-world level as we can, as quickly as we can,” said Mr. Pitts, who is president and cofounder of the Center for Medicine in the Public Interest, and who also does consulting work for the FDA. “I understand that health care professionals are overworked and overburdened right now. I applaud them for their heroic work. But that doesn’t mean that we can shirk off collecting the data. When I was at the FDA, I helped address the SARS epidemic. The agency attitude at that point was, ‘Let’s get things that just might work through the process, as long as the cure isn’t going to be worse than the disease.’ I think that’s the attitude that’s leading the charge today.”
As the proportion of patients infected with COVID-19 continues to rise in the United States, the Food and Drug Administration is facilitating access to COVID-19 convalescent plasma for use in patients with serious or immediately life-threatening COVID-19 infections.
While clinical trials are underway to evaluate the safety and efficacy of administering convalescent plasma to patients with COVID-19, the FDA is granting clinicians permission for use of investigational convalescent plasma under single-patient emergency Investigational New Drug Applications (INDs), since no known cure exists and a vaccine is more than 1 year away from becoming available.
This allows the use of an investigational drug for the treatment of an individual patient by a licensed physician upon FDA authorization. This does not include the use of COVID-19 convalescent plasma for the prevention of infection, according to a statement issued by the agency on March 24.
“It is possible that convalescent plasma that contains antibodies to SARS-CoV-2 (the virus that causes COVID-19) might be effective against the infection,” the FDA statement reads. “Use of convalescent plasma has been studied in outbreaks of other respiratory infections, including the 2009-2010 H1N1 influenza virus pandemic, 2003 SARS-CoV-1 epidemic, and the 2012 MERS-CoV epidemic. Although promising, convalescent plasma has not been shown to be effective in every disease studied.”
“I think the FDA got caught initially a little flat-footed when it came to the development of COVID-19 tests, but they’re quickly catching up,” Peter J. Pitts, who was the FDA’s associate commissioner from 2002 to 2004, said in an interview. “I think that the attitude now is, ‘If it’s safe, let’s create a pathway to see how these things work in the real world.’ I think that’s going to be as true for treatments to lessen the symptoms and shorten the duration of the disease, as well as convalescent plasma as a potential alternative to a yet-to-be-developed vaccine.”
At the University of Washington School of Medicine, Seattle, Terry B. Gernsheimer, MD, and her colleagues are recruiting recovered COVID-19 patients to donate plasma for seriously ill patients affected with the virus. “The thought of using convalescent plasma makes total sense, because it’s immediately available, and it’s something that we can try to give people,” said Dr. Gernsheimer, a hematologist who is professor of medicine at the medical school. “It’s been used in China, and reports should be coming out shortly about their experience with this.”
In a case series that appeared in JAMA on March 27 (doi: 10.1001/jama.2020.4783), Chinese researchers led by Chenguang Shen, PhD, reported findings from five critically ill COVID-19 patients with acute respiratory distress syndrome who received a transfusion with convalescent plasma at Shenzhen Third People’s Hospital 10 and 22 days after hospital admission. The patients ranged in age from 36 to 73 years, three were men, and all were receiving mechanical ventilation at the time of treatment.
Dr. Shen and colleagues reported that viral loads decreased and became negative within 12 days following the transfusion. Three of the patients were discharged from the hospital after a length of stay that ranged from 51 to 55 days, and two remain in stable condition at 37 days after the transfusion. The researchers pointed out that all patients received antiviral agents, including interferon and lopinavir/ritonavir, during and following convalescent plasma treatment, “which also may have contributed to the viral clearance observed.”
Under the FDA policy on emergency IND use, COVID-19 convalescent plasma must only be collected from recovered individuals if they are eligible to donate blood, required testing must be performed, and the donation must be found suitable.
Potential donors “are going to be screened the way all blood donors are screened,” Dr. Gernsheimer said. “It’s not going to be any less safe than any unit of plasma that’s on the shelf that comes from our volunteer donors. There are always transfusion reactions that we have to worry about, [and] there are potentially unknown pathogens that we don’t yet know about that we are not yet testing for. It’s the regular risk we see with any unit of plasma.”
She added that COVID-19 survivors appear to start increasing their titer of the antibody around day 28. “We’ll be looking for recovered individuals who have had a documented infection, and whose symptoms started about 28 days before we collect,” she said.
The FDA advises clinicians to address several considerations for donor eligibility, including prior diagnosis of COVID-19 documented by a laboratory test; complete resolution of symptoms at least 14 days prior to donation; female donors negative for HLA antibodies or male donors, and negative results for COVID-19 either from one or more nasopharyngeal swab specimens or by a molecular diagnostic test from blood. [A partial list of available tests can be accessed on the FDA website.] The agency also advises that donors have defined SARS-CoV-2–neutralizing antibody titers, if testing can be conducted (optimally greater than 1:320).
Patients eligible to receive COVID-19 convalescent plasma must have a severe or immediately life-threatening infection with laboratory-confirmed COVID-19. The agency defines severe disease as dyspnea, respiratory frequency of 30 per minute or greater, blood oxygen saturation of 93% or less, partial pressure of arterial oxygen to fraction of inspired oxygen ratio of less than 300, and/or lung infiltrates of greater than 50% within 24-48 hours. Life-threatening disease is defined as respiratory failure, septic shock, and/or multiple organ dysfunction or failure. Patients must provide informed consent.
The potential risks of receiving COVID-19 convalescent plasma remain unknown, according to Dr. Gernsheimer. “What some people have thought about is, could there be such an inflammatory response with the virus that we would initially see these patients get worse?” she said. “My understanding is that has not occurred in China yet, but we don’t have all those data. But we always worry if we have something that’s going to cause inflammation around an infection, for example, that could initially make it more difficult to breathe if it’s a lung infection. So far, my understanding is that has not been seen.”
For COVID-19 convalescent plasma authorization requests that require a response within 4-8 hours, requesting clinicians may complete form 3296 and submit it by email to [email protected].
For COVID-19 convalescent plasma authorization requests that require a response in less than 4 hours, or if the clinician is unable to complete and submit form 3926 because of extenuating circumstances, verbal authorization can be sought by calling the FDA’s Office of Emergency Operations at 1-866-300-4374.
The FDA is working with the National Institutes of Health, the Centers for Disease Control and Prevention, and other government partners to develop protocols for use by multiple investigators in order to coordinate the collection and use of COVID-19 convalescent plasma.
“It’s crucial that data be captured for every patient so that we really understand what safety and effectiveness looks like on as close to a real-world level as we can, as quickly as we can,” said Mr. Pitts, who is president and cofounder of the Center for Medicine in the Public Interest, and who also does consulting work for the FDA. “I understand that health care professionals are overworked and overburdened right now. I applaud them for their heroic work. But that doesn’t mean that we can shirk off collecting the data. When I was at the FDA, I helped address the SARS epidemic. The agency attitude at that point was, ‘Let’s get things that just might work through the process, as long as the cure isn’t going to be worse than the disease.’ I think that’s the attitude that’s leading the charge today.”
As the proportion of patients infected with COVID-19 continues to rise in the United States, the Food and Drug Administration is facilitating access to COVID-19 convalescent plasma for use in patients with serious or immediately life-threatening COVID-19 infections.
While clinical trials are underway to evaluate the safety and efficacy of administering convalescent plasma to patients with COVID-19, the FDA is granting clinicians permission for use of investigational convalescent plasma under single-patient emergency Investigational New Drug Applications (INDs), since no known cure exists and a vaccine is more than 1 year away from becoming available.
This allows the use of an investigational drug for the treatment of an individual patient by a licensed physician upon FDA authorization. This does not include the use of COVID-19 convalescent plasma for the prevention of infection, according to a statement issued by the agency on March 24.
“It is possible that convalescent plasma that contains antibodies to SARS-CoV-2 (the virus that causes COVID-19) might be effective against the infection,” the FDA statement reads. “Use of convalescent plasma has been studied in outbreaks of other respiratory infections, including the 2009-2010 H1N1 influenza virus pandemic, 2003 SARS-CoV-1 epidemic, and the 2012 MERS-CoV epidemic. Although promising, convalescent plasma has not been shown to be effective in every disease studied.”
“I think the FDA got caught initially a little flat-footed when it came to the development of COVID-19 tests, but they’re quickly catching up,” Peter J. Pitts, who was the FDA’s associate commissioner from 2002 to 2004, said in an interview. “I think that the attitude now is, ‘If it’s safe, let’s create a pathway to see how these things work in the real world.’ I think that’s going to be as true for treatments to lessen the symptoms and shorten the duration of the disease, as well as convalescent plasma as a potential alternative to a yet-to-be-developed vaccine.”
At the University of Washington School of Medicine, Seattle, Terry B. Gernsheimer, MD, and her colleagues are recruiting recovered COVID-19 patients to donate plasma for seriously ill patients affected with the virus. “The thought of using convalescent plasma makes total sense, because it’s immediately available, and it’s something that we can try to give people,” said Dr. Gernsheimer, a hematologist who is professor of medicine at the medical school. “It’s been used in China, and reports should be coming out shortly about their experience with this.”
In a case series that appeared in JAMA on March 27 (doi: 10.1001/jama.2020.4783), Chinese researchers led by Chenguang Shen, PhD, reported findings from five critically ill COVID-19 patients with acute respiratory distress syndrome who received a transfusion with convalescent plasma at Shenzhen Third People’s Hospital 10 and 22 days after hospital admission. The patients ranged in age from 36 to 73 years, three were men, and all were receiving mechanical ventilation at the time of treatment.
Dr. Shen and colleagues reported that viral loads decreased and became negative within 12 days following the transfusion. Three of the patients were discharged from the hospital after a length of stay that ranged from 51 to 55 days, and two remain in stable condition at 37 days after the transfusion. The researchers pointed out that all patients received antiviral agents, including interferon and lopinavir/ritonavir, during and following convalescent plasma treatment, “which also may have contributed to the viral clearance observed.”
Under the FDA policy on emergency IND use, COVID-19 convalescent plasma must only be collected from recovered individuals if they are eligible to donate blood, required testing must be performed, and the donation must be found suitable.
Potential donors “are going to be screened the way all blood donors are screened,” Dr. Gernsheimer said. “It’s not going to be any less safe than any unit of plasma that’s on the shelf that comes from our volunteer donors. There are always transfusion reactions that we have to worry about, [and] there are potentially unknown pathogens that we don’t yet know about that we are not yet testing for. It’s the regular risk we see with any unit of plasma.”
She added that COVID-19 survivors appear to start increasing their titer of the antibody around day 28. “We’ll be looking for recovered individuals who have had a documented infection, and whose symptoms started about 28 days before we collect,” she said.
The FDA advises clinicians to address several considerations for donor eligibility, including prior diagnosis of COVID-19 documented by a laboratory test; complete resolution of symptoms at least 14 days prior to donation; female donors negative for HLA antibodies or male donors, and negative results for COVID-19 either from one or more nasopharyngeal swab specimens or by a molecular diagnostic test from blood. [A partial list of available tests can be accessed on the FDA website.] The agency also advises that donors have defined SARS-CoV-2–neutralizing antibody titers, if testing can be conducted (optimally greater than 1:320).
Patients eligible to receive COVID-19 convalescent plasma must have a severe or immediately life-threatening infection with laboratory-confirmed COVID-19. The agency defines severe disease as dyspnea, respiratory frequency of 30 per minute or greater, blood oxygen saturation of 93% or less, partial pressure of arterial oxygen to fraction of inspired oxygen ratio of less than 300, and/or lung infiltrates of greater than 50% within 24-48 hours. Life-threatening disease is defined as respiratory failure, septic shock, and/or multiple organ dysfunction or failure. Patients must provide informed consent.
The potential risks of receiving COVID-19 convalescent plasma remain unknown, according to Dr. Gernsheimer. “What some people have thought about is, could there be such an inflammatory response with the virus that we would initially see these patients get worse?” she said. “My understanding is that has not occurred in China yet, but we don’t have all those data. But we always worry if we have something that’s going to cause inflammation around an infection, for example, that could initially make it more difficult to breathe if it’s a lung infection. So far, my understanding is that has not been seen.”
For COVID-19 convalescent plasma authorization requests that require a response within 4-8 hours, requesting clinicians may complete form 3296 and submit it by email to [email protected].
For COVID-19 convalescent plasma authorization requests that require a response in less than 4 hours, or if the clinician is unable to complete and submit form 3926 because of extenuating circumstances, verbal authorization can be sought by calling the FDA’s Office of Emergency Operations at 1-866-300-4374.
The FDA is working with the National Institutes of Health, the Centers for Disease Control and Prevention, and other government partners to develop protocols for use by multiple investigators in order to coordinate the collection and use of COVID-19 convalescent plasma.
“It’s crucial that data be captured for every patient so that we really understand what safety and effectiveness looks like on as close to a real-world level as we can, as quickly as we can,” said Mr. Pitts, who is president and cofounder of the Center for Medicine in the Public Interest, and who also does consulting work for the FDA. “I understand that health care professionals are overworked and overburdened right now. I applaud them for their heroic work. But that doesn’t mean that we can shirk off collecting the data. When I was at the FDA, I helped address the SARS epidemic. The agency attitude at that point was, ‘Let’s get things that just might work through the process, as long as the cure isn’t going to be worse than the disease.’ I think that’s the attitude that’s leading the charge today.”