User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Vaccine mismatch: What to do after dose 1 when plans change
Ideally, Americans receiving their Pfizer/BioNTech or Moderna COVID-19 vaccines will get both doses from the same manufacturer, said Gregory Poland, MD, a vaccinologist at the Mayo Clinic in Rochester, Minn.
After all, that’s how they were tested for efficacy and safety, and it was results from those studies that led to emergency use authorization (EUA) being granted by the Food and Drug Administration.
But states and countries have struggled to keep up with the demand for vaccine, and more flexible vaccination schedules could help.
So researchers are exploring whether it is safe and effective to get the first and second doses from different manufacturers. And they are even wondering whether mixing doses from different manufacturers could increase effectiveness, particularly in light of emerging variants.
It’s called the “interchangeability issue,” said Dr. Poland, who has gotten a steady stream of questions about it.
For example, a patient recently asked about options for his father, who had gotten his first dose of the AstraZeneca vaccine in Ecuador, but had since moved to the United States, where that product has not been approved for use.
Dr. Poland said in an interview that he prefaces each answer with: “I’ve got no science for what I’m about to tell you.”
In this particular case, he recommended that the man’s father talk with his doctor about his level of COVID-19 risk and consider whether he should gamble on the AstraZeneca vaccine getting approved in the United States soon, or whether he should ask for a second dose from one of the three vaccines currently approved.
On March 22, 2021, AstraZeneca released positive results from its phase 3 trial, which will likely speed its path toward use in the United States.
Although clinical trials have started to test combinations and boosters, there’s currently no definitive evidence from human trials on mixing COVID vaccines, Dr. Poland pointed out.
But a study of a mixed-vaccine regimen is currently underway in the United Kingdom.
Participants in that 13-month trial will be given the Oxford/AstraZeneca and Pfizer/BioNTech vaccines in different combinations and at different intervals. The first results from that trial are expected this summer.
And interim results from a trial combining Russia’s Sputnik V and the AstraZeneca vaccines are expected in 2 months, according to a Reuters report.
Mix only in ‘exceptional situations’
The Centers for Disease Control and Prevention has been hesitant to open the door to mixing Pfizer and Moderna vaccinations, noting that the two “are not interchangeable.” But CDC guidance has changed slightly. Now, instead of saying the two vaccines should not be mixed, CDC guidance says they can be mixed in “exceptional situations,” and that the second dose can be administered up to 6 weeks after the first dose.
It is reasonable to assume that mixing COVID-19 vaccines that use the same platform – such as the mRNA platform used by both the Pfizer and Moderna vaccines – will be acceptable, Dr. Poland said, although human trials have not proven that.
However, it is unclear whether vaccines that use different platforms can be mixed. Can the first dose of an mRNA vaccine be followed by an adenovirus-based vaccine, like the Johnson & Johnson product or Novavax, if that vaccine is granted an EUA?
Ross Kedl, PhD, a vaccine researcher and professor of immunology at the University of Colorado at Denver, Aurora, said matching vaccine platforms might not be the preferred vaccination strategy.
He disagreed that there’s a lack of science surrounding the issue, and said all signs point to mixing as not only a good option, but probably a better one.
Researcher says science backs mixing
A mix of two different vaccine platforms likely enhances immunity, Dr. Kedl said. The heterologous prime-boost strategy has been used in animal studies for decades, “and it is well known that this promotes a much better immune response than when immunizing with the same vaccine twice.
“If you think about it in a Venn diagram sort of way, it makes sense,” he said in an interview. “Each vaccine has a number of components in it that influence immunity in various ways, but between the two of them, they only have one component that is similar. In the case of the coronavirus vaccines, the one thing both have in common is the spike protein from SARS-CoV-2. In essence, this gives you two shots at generating immunity against the one thing in each vaccine you care most about, but only one shot for the other vaccine components in each platform, resulting in an amplified response against the common target.”
In fact, the heterologous prime-boost vaccination strategy has proven to be effective in humans in early studies.
For example, an Ebola regimen that consisted of an adenovirus vector, similar to the AstraZeneca COVID vaccine, and a modified vaccinia virus vector showed promise in a phase 1 study. And an HIV regimen that consisted of the combination of a DNA vaccine, similar to the Pfizer and Moderna mRNA vaccines, and another viral vector showed encouraging results in a proof-of-concept study.
In both these cases, the heterologous prime-boost strategy was far better than single-vaccine prime-boost regimens, Dr. Kedl pointed out. And neither study reported any safety issues with the combinations.
For now, it’s best to stick with the same manufacturer for both shots, as the CDC guidance suggests, he said, agreeing with Dr. Poland.
But “I would be very surprised if we didn’t move to a mixing of vaccine platforms for the population,” Dr. Kedl said.
A version of this article first appeared on Medscape.com.
Ideally, Americans receiving their Pfizer/BioNTech or Moderna COVID-19 vaccines will get both doses from the same manufacturer, said Gregory Poland, MD, a vaccinologist at the Mayo Clinic in Rochester, Minn.
After all, that’s how they were tested for efficacy and safety, and it was results from those studies that led to emergency use authorization (EUA) being granted by the Food and Drug Administration.
But states and countries have struggled to keep up with the demand for vaccine, and more flexible vaccination schedules could help.
So researchers are exploring whether it is safe and effective to get the first and second doses from different manufacturers. And they are even wondering whether mixing doses from different manufacturers could increase effectiveness, particularly in light of emerging variants.
It’s called the “interchangeability issue,” said Dr. Poland, who has gotten a steady stream of questions about it.
For example, a patient recently asked about options for his father, who had gotten his first dose of the AstraZeneca vaccine in Ecuador, but had since moved to the United States, where that product has not been approved for use.
Dr. Poland said in an interview that he prefaces each answer with: “I’ve got no science for what I’m about to tell you.”
In this particular case, he recommended that the man’s father talk with his doctor about his level of COVID-19 risk and consider whether he should gamble on the AstraZeneca vaccine getting approved in the United States soon, or whether he should ask for a second dose from one of the three vaccines currently approved.
On March 22, 2021, AstraZeneca released positive results from its phase 3 trial, which will likely speed its path toward use in the United States.
Although clinical trials have started to test combinations and boosters, there’s currently no definitive evidence from human trials on mixing COVID vaccines, Dr. Poland pointed out.
But a study of a mixed-vaccine regimen is currently underway in the United Kingdom.
Participants in that 13-month trial will be given the Oxford/AstraZeneca and Pfizer/BioNTech vaccines in different combinations and at different intervals. The first results from that trial are expected this summer.
And interim results from a trial combining Russia’s Sputnik V and the AstraZeneca vaccines are expected in 2 months, according to a Reuters report.
Mix only in ‘exceptional situations’
The Centers for Disease Control and Prevention has been hesitant to open the door to mixing Pfizer and Moderna vaccinations, noting that the two “are not interchangeable.” But CDC guidance has changed slightly. Now, instead of saying the two vaccines should not be mixed, CDC guidance says they can be mixed in “exceptional situations,” and that the second dose can be administered up to 6 weeks after the first dose.
It is reasonable to assume that mixing COVID-19 vaccines that use the same platform – such as the mRNA platform used by both the Pfizer and Moderna vaccines – will be acceptable, Dr. Poland said, although human trials have not proven that.
However, it is unclear whether vaccines that use different platforms can be mixed. Can the first dose of an mRNA vaccine be followed by an adenovirus-based vaccine, like the Johnson & Johnson product or Novavax, if that vaccine is granted an EUA?
Ross Kedl, PhD, a vaccine researcher and professor of immunology at the University of Colorado at Denver, Aurora, said matching vaccine platforms might not be the preferred vaccination strategy.
He disagreed that there’s a lack of science surrounding the issue, and said all signs point to mixing as not only a good option, but probably a better one.
Researcher says science backs mixing
A mix of two different vaccine platforms likely enhances immunity, Dr. Kedl said. The heterologous prime-boost strategy has been used in animal studies for decades, “and it is well known that this promotes a much better immune response than when immunizing with the same vaccine twice.
“If you think about it in a Venn diagram sort of way, it makes sense,” he said in an interview. “Each vaccine has a number of components in it that influence immunity in various ways, but between the two of them, they only have one component that is similar. In the case of the coronavirus vaccines, the one thing both have in common is the spike protein from SARS-CoV-2. In essence, this gives you two shots at generating immunity against the one thing in each vaccine you care most about, but only one shot for the other vaccine components in each platform, resulting in an amplified response against the common target.”
In fact, the heterologous prime-boost vaccination strategy has proven to be effective in humans in early studies.
For example, an Ebola regimen that consisted of an adenovirus vector, similar to the AstraZeneca COVID vaccine, and a modified vaccinia virus vector showed promise in a phase 1 study. And an HIV regimen that consisted of the combination of a DNA vaccine, similar to the Pfizer and Moderna mRNA vaccines, and another viral vector showed encouraging results in a proof-of-concept study.
In both these cases, the heterologous prime-boost strategy was far better than single-vaccine prime-boost regimens, Dr. Kedl pointed out. And neither study reported any safety issues with the combinations.
For now, it’s best to stick with the same manufacturer for both shots, as the CDC guidance suggests, he said, agreeing with Dr. Poland.
But “I would be very surprised if we didn’t move to a mixing of vaccine platforms for the population,” Dr. Kedl said.
A version of this article first appeared on Medscape.com.
Ideally, Americans receiving their Pfizer/BioNTech or Moderna COVID-19 vaccines will get both doses from the same manufacturer, said Gregory Poland, MD, a vaccinologist at the Mayo Clinic in Rochester, Minn.
After all, that’s how they were tested for efficacy and safety, and it was results from those studies that led to emergency use authorization (EUA) being granted by the Food and Drug Administration.
But states and countries have struggled to keep up with the demand for vaccine, and more flexible vaccination schedules could help.
So researchers are exploring whether it is safe and effective to get the first and second doses from different manufacturers. And they are even wondering whether mixing doses from different manufacturers could increase effectiveness, particularly in light of emerging variants.
It’s called the “interchangeability issue,” said Dr. Poland, who has gotten a steady stream of questions about it.
For example, a patient recently asked about options for his father, who had gotten his first dose of the AstraZeneca vaccine in Ecuador, but had since moved to the United States, where that product has not been approved for use.
Dr. Poland said in an interview that he prefaces each answer with: “I’ve got no science for what I’m about to tell you.”
In this particular case, he recommended that the man’s father talk with his doctor about his level of COVID-19 risk and consider whether he should gamble on the AstraZeneca vaccine getting approved in the United States soon, or whether he should ask for a second dose from one of the three vaccines currently approved.
On March 22, 2021, AstraZeneca released positive results from its phase 3 trial, which will likely speed its path toward use in the United States.
Although clinical trials have started to test combinations and boosters, there’s currently no definitive evidence from human trials on mixing COVID vaccines, Dr. Poland pointed out.
But a study of a mixed-vaccine regimen is currently underway in the United Kingdom.
Participants in that 13-month trial will be given the Oxford/AstraZeneca and Pfizer/BioNTech vaccines in different combinations and at different intervals. The first results from that trial are expected this summer.
And interim results from a trial combining Russia’s Sputnik V and the AstraZeneca vaccines are expected in 2 months, according to a Reuters report.
Mix only in ‘exceptional situations’
The Centers for Disease Control and Prevention has been hesitant to open the door to mixing Pfizer and Moderna vaccinations, noting that the two “are not interchangeable.” But CDC guidance has changed slightly. Now, instead of saying the two vaccines should not be mixed, CDC guidance says they can be mixed in “exceptional situations,” and that the second dose can be administered up to 6 weeks after the first dose.
It is reasonable to assume that mixing COVID-19 vaccines that use the same platform – such as the mRNA platform used by both the Pfizer and Moderna vaccines – will be acceptable, Dr. Poland said, although human trials have not proven that.
However, it is unclear whether vaccines that use different platforms can be mixed. Can the first dose of an mRNA vaccine be followed by an adenovirus-based vaccine, like the Johnson & Johnson product or Novavax, if that vaccine is granted an EUA?
Ross Kedl, PhD, a vaccine researcher and professor of immunology at the University of Colorado at Denver, Aurora, said matching vaccine platforms might not be the preferred vaccination strategy.
He disagreed that there’s a lack of science surrounding the issue, and said all signs point to mixing as not only a good option, but probably a better one.
Researcher says science backs mixing
A mix of two different vaccine platforms likely enhances immunity, Dr. Kedl said. The heterologous prime-boost strategy has been used in animal studies for decades, “and it is well known that this promotes a much better immune response than when immunizing with the same vaccine twice.
“If you think about it in a Venn diagram sort of way, it makes sense,” he said in an interview. “Each vaccine has a number of components in it that influence immunity in various ways, but between the two of them, they only have one component that is similar. In the case of the coronavirus vaccines, the one thing both have in common is the spike protein from SARS-CoV-2. In essence, this gives you two shots at generating immunity against the one thing in each vaccine you care most about, but only one shot for the other vaccine components in each platform, resulting in an amplified response against the common target.”
In fact, the heterologous prime-boost vaccination strategy has proven to be effective in humans in early studies.
For example, an Ebola regimen that consisted of an adenovirus vector, similar to the AstraZeneca COVID vaccine, and a modified vaccinia virus vector showed promise in a phase 1 study. And an HIV regimen that consisted of the combination of a DNA vaccine, similar to the Pfizer and Moderna mRNA vaccines, and another viral vector showed encouraging results in a proof-of-concept study.
In both these cases, the heterologous prime-boost strategy was far better than single-vaccine prime-boost regimens, Dr. Kedl pointed out. And neither study reported any safety issues with the combinations.
For now, it’s best to stick with the same manufacturer for both shots, as the CDC guidance suggests, he said, agreeing with Dr. Poland.
But “I would be very surprised if we didn’t move to a mixing of vaccine platforms for the population,” Dr. Kedl said.
A version of this article first appeared on Medscape.com.
Rhythm and blues: Using heart rate to diagnose depression
Depression might be a disorder of the brain, but its harms aren’t confined to the cranium. Prolonged depression has been linked with a slew of health problems, from impaired immune function to gastrointestinal dysfunction. It’s also been linked with cardiovascular disease (CVD), even increasing the risk for heart attack and a disrupted heart rate. Now, researchers are exploring whether heart function could be a valuable biomarker in informing depression diagnosis and treatment.
Major depressive disorder has proved difficult to diagnose and treat, and biomarkers that indicate a depressive episode or suggest specific interventions would be an attractive solution to its clinically nebulous nature.
Currently, diagnosing depression relies on the patients effectively communicating their symptoms. If the patient does receive a diagnosis, treating it remains a matter of trial and error. It takes weeks to know whether a treatment is working, and in only one-third of cases does the condition go into remission after the patient is initially prescribed an antidepressant. Even after successful treatment, it’s challenging to identify who might be at risk for relapse, and when. Research now shows that cardiac biomarkers may be a way improve this picture. Clinicians could use changes in heart rate to both inform depression diagnosis and gauge a patient’s predicted response to treatment.
Given the increased risk for CVD among people with depression and the link between heart rate changes and CVD risk, these biomarkers could have implications for heart health, too. “We need more than just the current toolkit,” said Amit Shah, MD, a cardiologist and assistant professor of epidemiology at Emory University, Atlanta. “Ultimately, what we’re trying to do is develop interventions not only for depression but also for the associated physical health problems related to depression, in particular, cardiovascular disease,” he said. These overlapping interests – and the prospect of clinically considering both conditions in tandem – mean this research is “really worth its weight in gold,” added Dr. Shah.
The data on heart rate biomarkers
Patients with depression are often found to have lower heart rate variability (HRV) and higher heart rates. Scientists don’t know the mechanisms underpinning this relationship but think changes in the autonomic nervous system during depression, as well as stress generally, have a role.
Rébecca Robillard, PhD, is the head scientist of the Clinical Sleep Research Platform at the Royal’s Institute of Mental Health Research, Ottawa, Ont. In a 2019 study published in BMC Psychiatry, Dr. Robillard’s team used electrocardiogram recordings from sleep studies to see whether heart rate abnormalities were associated with depression. Using a profiling algorithm to analyze heart rate and HRV data, the team identified persons with depression with 80% accuracy among 174 people with sleep complaints.
Dr. Robillard said.
In another study, Stephan Claes, MD, PhD, psychiatrist and professor of psychiatry at Katholieke Universiteit Leuven, Belgium, and his group tested the biomarker potential of heart rate and HRV data that were continuously recorded over several days. They too used an algorithm to distinguish 16 people with treatment-resistant depression from 16 without depression. Within the depression group, they used the algorithm to distinguish patients who had received ketamine treatment from those who had not.
The algorithm could differentiate between the depressed and nondepressed groups with 90% accuracy. Those with depression had higher overall heart rates, particularly at night, and lower HRV. Dr. Claes noted that, unlike in other studies, “the most reliable parameter that we had for this prediction was the heart rate, not the HRV.” After treatment, heart rates improved, but HRV remained the same.
Although their study has not yet been peer reviewed and more research is needed, Dr. Claes said that increased heart rate, especially during the night, could eventually serve as a warning sign of depression relapse. “That would allow a quicker referral to care and better care because of earlier intervention,” he said.
Finding a signal amid the noise
But heart rate and HRV aren’t foolproof biomarkers. Some studies have found that antidepressant use lowers HRV and that HRV changes aren’t unique to depression. There’s the added complication that depression often overlaps with other mental disorders.
“I think we’ve been very disappointed about the success of using particular biomarkers for particular disorders, because the majority of mental disorders are very heterogeneous,” said Andrew Kemp, PhD, psychology professor at Swansea University, Swansea, Wales. “A particular biomarker will, at the end of the day, be just one particular aspect of the overall profile that clinicians will have on particular individuals.”
The clinical utility of a heart rate–depression connection may go both ways.
For instance, depression could serve as a warning sign for atrial fibrillation, according to research from Parveen K. Garg, MD, associate professor of clinical medicine at the University of Southern California, Los Angeles. In a study involving more than 6,000 people, Dr. Garg showed that higher scores on depression scales correlated with a higher risk for the occurrence of atrial fibrillation over a follow-up period of about 13 years.
Depression is associated with other heart conditions as well. “A lot of data seem to suggest that just the presence of depression can increase risk for a whole range of cardiovascular problems,” said Dr. Garg. Epidemiologic studies have found associations between depression and the development of coronary heart disease and a modest increased risk for stroke.
“Things going on in your brain also have effects on the rest of your body,” said Dr. Garg. “Just recognizing this link, that maybe mental illness has an effect on other illnesses or diseases that can affect other parts of your body – I think that’s something we can share now.”
A version of this article first appeared on Medscape.com.
Depression might be a disorder of the brain, but its harms aren’t confined to the cranium. Prolonged depression has been linked with a slew of health problems, from impaired immune function to gastrointestinal dysfunction. It’s also been linked with cardiovascular disease (CVD), even increasing the risk for heart attack and a disrupted heart rate. Now, researchers are exploring whether heart function could be a valuable biomarker in informing depression diagnosis and treatment.
Major depressive disorder has proved difficult to diagnose and treat, and biomarkers that indicate a depressive episode or suggest specific interventions would be an attractive solution to its clinically nebulous nature.
Currently, diagnosing depression relies on the patients effectively communicating their symptoms. If the patient does receive a diagnosis, treating it remains a matter of trial and error. It takes weeks to know whether a treatment is working, and in only one-third of cases does the condition go into remission after the patient is initially prescribed an antidepressant. Even after successful treatment, it’s challenging to identify who might be at risk for relapse, and when. Research now shows that cardiac biomarkers may be a way improve this picture. Clinicians could use changes in heart rate to both inform depression diagnosis and gauge a patient’s predicted response to treatment.
Given the increased risk for CVD among people with depression and the link between heart rate changes and CVD risk, these biomarkers could have implications for heart health, too. “We need more than just the current toolkit,” said Amit Shah, MD, a cardiologist and assistant professor of epidemiology at Emory University, Atlanta. “Ultimately, what we’re trying to do is develop interventions not only for depression but also for the associated physical health problems related to depression, in particular, cardiovascular disease,” he said. These overlapping interests – and the prospect of clinically considering both conditions in tandem – mean this research is “really worth its weight in gold,” added Dr. Shah.
The data on heart rate biomarkers
Patients with depression are often found to have lower heart rate variability (HRV) and higher heart rates. Scientists don’t know the mechanisms underpinning this relationship but think changes in the autonomic nervous system during depression, as well as stress generally, have a role.
Rébecca Robillard, PhD, is the head scientist of the Clinical Sleep Research Platform at the Royal’s Institute of Mental Health Research, Ottawa, Ont. In a 2019 study published in BMC Psychiatry, Dr. Robillard’s team used electrocardiogram recordings from sleep studies to see whether heart rate abnormalities were associated with depression. Using a profiling algorithm to analyze heart rate and HRV data, the team identified persons with depression with 80% accuracy among 174 people with sleep complaints.
Dr. Robillard said.
In another study, Stephan Claes, MD, PhD, psychiatrist and professor of psychiatry at Katholieke Universiteit Leuven, Belgium, and his group tested the biomarker potential of heart rate and HRV data that were continuously recorded over several days. They too used an algorithm to distinguish 16 people with treatment-resistant depression from 16 without depression. Within the depression group, they used the algorithm to distinguish patients who had received ketamine treatment from those who had not.
The algorithm could differentiate between the depressed and nondepressed groups with 90% accuracy. Those with depression had higher overall heart rates, particularly at night, and lower HRV. Dr. Claes noted that, unlike in other studies, “the most reliable parameter that we had for this prediction was the heart rate, not the HRV.” After treatment, heart rates improved, but HRV remained the same.
Although their study has not yet been peer reviewed and more research is needed, Dr. Claes said that increased heart rate, especially during the night, could eventually serve as a warning sign of depression relapse. “That would allow a quicker referral to care and better care because of earlier intervention,” he said.
Finding a signal amid the noise
But heart rate and HRV aren’t foolproof biomarkers. Some studies have found that antidepressant use lowers HRV and that HRV changes aren’t unique to depression. There’s the added complication that depression often overlaps with other mental disorders.
“I think we’ve been very disappointed about the success of using particular biomarkers for particular disorders, because the majority of mental disorders are very heterogeneous,” said Andrew Kemp, PhD, psychology professor at Swansea University, Swansea, Wales. “A particular biomarker will, at the end of the day, be just one particular aspect of the overall profile that clinicians will have on particular individuals.”
The clinical utility of a heart rate–depression connection may go both ways.
For instance, depression could serve as a warning sign for atrial fibrillation, according to research from Parveen K. Garg, MD, associate professor of clinical medicine at the University of Southern California, Los Angeles. In a study involving more than 6,000 people, Dr. Garg showed that higher scores on depression scales correlated with a higher risk for the occurrence of atrial fibrillation over a follow-up period of about 13 years.
Depression is associated with other heart conditions as well. “A lot of data seem to suggest that just the presence of depression can increase risk for a whole range of cardiovascular problems,” said Dr. Garg. Epidemiologic studies have found associations between depression and the development of coronary heart disease and a modest increased risk for stroke.
“Things going on in your brain also have effects on the rest of your body,” said Dr. Garg. “Just recognizing this link, that maybe mental illness has an effect on other illnesses or diseases that can affect other parts of your body – I think that’s something we can share now.”
A version of this article first appeared on Medscape.com.
Depression might be a disorder of the brain, but its harms aren’t confined to the cranium. Prolonged depression has been linked with a slew of health problems, from impaired immune function to gastrointestinal dysfunction. It’s also been linked with cardiovascular disease (CVD), even increasing the risk for heart attack and a disrupted heart rate. Now, researchers are exploring whether heart function could be a valuable biomarker in informing depression diagnosis and treatment.
Major depressive disorder has proved difficult to diagnose and treat, and biomarkers that indicate a depressive episode or suggest specific interventions would be an attractive solution to its clinically nebulous nature.
Currently, diagnosing depression relies on the patients effectively communicating their symptoms. If the patient does receive a diagnosis, treating it remains a matter of trial and error. It takes weeks to know whether a treatment is working, and in only one-third of cases does the condition go into remission after the patient is initially prescribed an antidepressant. Even after successful treatment, it’s challenging to identify who might be at risk for relapse, and when. Research now shows that cardiac biomarkers may be a way improve this picture. Clinicians could use changes in heart rate to both inform depression diagnosis and gauge a patient’s predicted response to treatment.
Given the increased risk for CVD among people with depression and the link between heart rate changes and CVD risk, these biomarkers could have implications for heart health, too. “We need more than just the current toolkit,” said Amit Shah, MD, a cardiologist and assistant professor of epidemiology at Emory University, Atlanta. “Ultimately, what we’re trying to do is develop interventions not only for depression but also for the associated physical health problems related to depression, in particular, cardiovascular disease,” he said. These overlapping interests – and the prospect of clinically considering both conditions in tandem – mean this research is “really worth its weight in gold,” added Dr. Shah.
The data on heart rate biomarkers
Patients with depression are often found to have lower heart rate variability (HRV) and higher heart rates. Scientists don’t know the mechanisms underpinning this relationship but think changes in the autonomic nervous system during depression, as well as stress generally, have a role.
Rébecca Robillard, PhD, is the head scientist of the Clinical Sleep Research Platform at the Royal’s Institute of Mental Health Research, Ottawa, Ont. In a 2019 study published in BMC Psychiatry, Dr. Robillard’s team used electrocardiogram recordings from sleep studies to see whether heart rate abnormalities were associated with depression. Using a profiling algorithm to analyze heart rate and HRV data, the team identified persons with depression with 80% accuracy among 174 people with sleep complaints.
Dr. Robillard said.
In another study, Stephan Claes, MD, PhD, psychiatrist and professor of psychiatry at Katholieke Universiteit Leuven, Belgium, and his group tested the biomarker potential of heart rate and HRV data that were continuously recorded over several days. They too used an algorithm to distinguish 16 people with treatment-resistant depression from 16 without depression. Within the depression group, they used the algorithm to distinguish patients who had received ketamine treatment from those who had not.
The algorithm could differentiate between the depressed and nondepressed groups with 90% accuracy. Those with depression had higher overall heart rates, particularly at night, and lower HRV. Dr. Claes noted that, unlike in other studies, “the most reliable parameter that we had for this prediction was the heart rate, not the HRV.” After treatment, heart rates improved, but HRV remained the same.
Although their study has not yet been peer reviewed and more research is needed, Dr. Claes said that increased heart rate, especially during the night, could eventually serve as a warning sign of depression relapse. “That would allow a quicker referral to care and better care because of earlier intervention,” he said.
Finding a signal amid the noise
But heart rate and HRV aren’t foolproof biomarkers. Some studies have found that antidepressant use lowers HRV and that HRV changes aren’t unique to depression. There’s the added complication that depression often overlaps with other mental disorders.
“I think we’ve been very disappointed about the success of using particular biomarkers for particular disorders, because the majority of mental disorders are very heterogeneous,” said Andrew Kemp, PhD, psychology professor at Swansea University, Swansea, Wales. “A particular biomarker will, at the end of the day, be just one particular aspect of the overall profile that clinicians will have on particular individuals.”
The clinical utility of a heart rate–depression connection may go both ways.
For instance, depression could serve as a warning sign for atrial fibrillation, according to research from Parveen K. Garg, MD, associate professor of clinical medicine at the University of Southern California, Los Angeles. In a study involving more than 6,000 people, Dr. Garg showed that higher scores on depression scales correlated with a higher risk for the occurrence of atrial fibrillation over a follow-up period of about 13 years.
Depression is associated with other heart conditions as well. “A lot of data seem to suggest that just the presence of depression can increase risk for a whole range of cardiovascular problems,” said Dr. Garg. Epidemiologic studies have found associations between depression and the development of coronary heart disease and a modest increased risk for stroke.
“Things going on in your brain also have effects on the rest of your body,” said Dr. Garg. “Just recognizing this link, that maybe mental illness has an effect on other illnesses or diseases that can affect other parts of your body – I think that’s something we can share now.”
A version of this article first appeared on Medscape.com.
National Psoriasis Foundation recommends some stop methotrexate for 2 weeks after J&J vaccine
The , Joel M. Gelfand, MD, said at Innovations in Dermatology: Virtual Spring Conference 2021.
The new guidance states: “Patients 60 or older who have at least one comorbidity associated with an increased risk for poor COVID-19 outcomes, and who are taking methotrexate with well-controlled psoriatic disease, may, in consultation with their prescriber, consider holding it for 2 weeks after receiving the Ad26.COV2.S [Johnson & Johnson] vaccine in order to potentially improve vaccine response.”
The key word here is “potentially.” There is no hard evidence that a 2-week hold on methotrexate after receiving the killed adenovirus vaccine will actually provide a clinically meaningful benefit. But it’s a hypothetical possibility. The rationale stems from a small randomized trial conducted in South Korea several years ago in which patients with rheumatoid arthritis were assigned to hold or continue their methotrexate for the first 2 weeks after receiving an inactivated-virus influenza vaccine. The antibody response to the vaccine was better in those who temporarily halted their methotrexate, explained Dr. Gelfand, cochair of the NPF COVID-19 Task Force and professor of dermatology and of epidemiology at the University of Pennsylvania, Philadelphia.
“If you have a patient on methotrexate who’s 60 or older and whose psoriasis is completely controlled and quiescent and the patient is concerned about how well the vaccine is going to work, this is a reasonable thing to consider in someone who’s at higher risk for poor outcomes if they get infected,” he said.
If the informed patient wants to continue on methotrexate without interruption, that’s fine, too, in light of the lack of compelling evidence on this issue, the dermatologist added at the conference, sponsored by MedscapeLIVE! and the producers of the Hawaii Dermatology Seminar and Caribbean Dermatology Symposium.
The NPF task force does not extend the recommendation to consider holding methotrexate in recipients of the mRNA-based Moderna and Pfizer vaccines because of their very different mechanisms of action. Nor is it recommended to hold biologic agents after receiving any of the available COVID-19 vaccines. Studies have shown no altered immunologic response to influenza or pneumococcal vaccines in patients who continued on tumor necrosis factor inhibitors or interleukin-17 inhibitors. The interleukin-23 inhibitors haven’t been studied in this regard.
The task force recommends that most psoriasis patients should continue on treatment throughout the pandemic, and newly diagnosed patients should commence appropriate therapy as if there was no pandemic.
“We’ve learned that many patients who stopped their treatment for psoriatic disease early in the pandemic came to regret that decision because their psoriasis flared and got worse and required reinstitution of therapy,” Dr. Gelfand said. “The current data is largely reassuring that if there is an effect of our therapies on the risk of COVID, it must be rather small and therefore unlikely to be clinically meaningful for our patients.”
Dr. Gelfand reported serving as a consultant to and recipient of institutional research grants from Pfizer and numerous other pharmaceutical companies.
MedscapeLIVE and this news organization are owned by the same parent company.
The , Joel M. Gelfand, MD, said at Innovations in Dermatology: Virtual Spring Conference 2021.
The new guidance states: “Patients 60 or older who have at least one comorbidity associated with an increased risk for poor COVID-19 outcomes, and who are taking methotrexate with well-controlled psoriatic disease, may, in consultation with their prescriber, consider holding it for 2 weeks after receiving the Ad26.COV2.S [Johnson & Johnson] vaccine in order to potentially improve vaccine response.”
The key word here is “potentially.” There is no hard evidence that a 2-week hold on methotrexate after receiving the killed adenovirus vaccine will actually provide a clinically meaningful benefit. But it’s a hypothetical possibility. The rationale stems from a small randomized trial conducted in South Korea several years ago in which patients with rheumatoid arthritis were assigned to hold or continue their methotrexate for the first 2 weeks after receiving an inactivated-virus influenza vaccine. The antibody response to the vaccine was better in those who temporarily halted their methotrexate, explained Dr. Gelfand, cochair of the NPF COVID-19 Task Force and professor of dermatology and of epidemiology at the University of Pennsylvania, Philadelphia.
“If you have a patient on methotrexate who’s 60 or older and whose psoriasis is completely controlled and quiescent and the patient is concerned about how well the vaccine is going to work, this is a reasonable thing to consider in someone who’s at higher risk for poor outcomes if they get infected,” he said.
If the informed patient wants to continue on methotrexate without interruption, that’s fine, too, in light of the lack of compelling evidence on this issue, the dermatologist added at the conference, sponsored by MedscapeLIVE! and the producers of the Hawaii Dermatology Seminar and Caribbean Dermatology Symposium.
The NPF task force does not extend the recommendation to consider holding methotrexate in recipients of the mRNA-based Moderna and Pfizer vaccines because of their very different mechanisms of action. Nor is it recommended to hold biologic agents after receiving any of the available COVID-19 vaccines. Studies have shown no altered immunologic response to influenza or pneumococcal vaccines in patients who continued on tumor necrosis factor inhibitors or interleukin-17 inhibitors. The interleukin-23 inhibitors haven’t been studied in this regard.
The task force recommends that most psoriasis patients should continue on treatment throughout the pandemic, and newly diagnosed patients should commence appropriate therapy as if there was no pandemic.
“We’ve learned that many patients who stopped their treatment for psoriatic disease early in the pandemic came to regret that decision because their psoriasis flared and got worse and required reinstitution of therapy,” Dr. Gelfand said. “The current data is largely reassuring that if there is an effect of our therapies on the risk of COVID, it must be rather small and therefore unlikely to be clinically meaningful for our patients.”
Dr. Gelfand reported serving as a consultant to and recipient of institutional research grants from Pfizer and numerous other pharmaceutical companies.
MedscapeLIVE and this news organization are owned by the same parent company.
The , Joel M. Gelfand, MD, said at Innovations in Dermatology: Virtual Spring Conference 2021.
The new guidance states: “Patients 60 or older who have at least one comorbidity associated with an increased risk for poor COVID-19 outcomes, and who are taking methotrexate with well-controlled psoriatic disease, may, in consultation with their prescriber, consider holding it for 2 weeks after receiving the Ad26.COV2.S [Johnson & Johnson] vaccine in order to potentially improve vaccine response.”
The key word here is “potentially.” There is no hard evidence that a 2-week hold on methotrexate after receiving the killed adenovirus vaccine will actually provide a clinically meaningful benefit. But it’s a hypothetical possibility. The rationale stems from a small randomized trial conducted in South Korea several years ago in which patients with rheumatoid arthritis were assigned to hold or continue their methotrexate for the first 2 weeks after receiving an inactivated-virus influenza vaccine. The antibody response to the vaccine was better in those who temporarily halted their methotrexate, explained Dr. Gelfand, cochair of the NPF COVID-19 Task Force and professor of dermatology and of epidemiology at the University of Pennsylvania, Philadelphia.
“If you have a patient on methotrexate who’s 60 or older and whose psoriasis is completely controlled and quiescent and the patient is concerned about how well the vaccine is going to work, this is a reasonable thing to consider in someone who’s at higher risk for poor outcomes if they get infected,” he said.
If the informed patient wants to continue on methotrexate without interruption, that’s fine, too, in light of the lack of compelling evidence on this issue, the dermatologist added at the conference, sponsored by MedscapeLIVE! and the producers of the Hawaii Dermatology Seminar and Caribbean Dermatology Symposium.
The NPF task force does not extend the recommendation to consider holding methotrexate in recipients of the mRNA-based Moderna and Pfizer vaccines because of their very different mechanisms of action. Nor is it recommended to hold biologic agents after receiving any of the available COVID-19 vaccines. Studies have shown no altered immunologic response to influenza or pneumococcal vaccines in patients who continued on tumor necrosis factor inhibitors or interleukin-17 inhibitors. The interleukin-23 inhibitors haven’t been studied in this regard.
The task force recommends that most psoriasis patients should continue on treatment throughout the pandemic, and newly diagnosed patients should commence appropriate therapy as if there was no pandemic.
“We’ve learned that many patients who stopped their treatment for psoriatic disease early in the pandemic came to regret that decision because their psoriasis flared and got worse and required reinstitution of therapy,” Dr. Gelfand said. “The current data is largely reassuring that if there is an effect of our therapies on the risk of COVID, it must be rather small and therefore unlikely to be clinically meaningful for our patients.”
Dr. Gelfand reported serving as a consultant to and recipient of institutional research grants from Pfizer and numerous other pharmaceutical companies.
MedscapeLIVE and this news organization are owned by the same parent company.
FROM INNOVATIONS IN DERMATOLOGY
Child abuse tied to persistent inflammation in later life
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People who suffer abuse as children continue to have higher levels of inflammatory biomarkers as adults, likely placing them at increased risk for chronic health problems, new research shows.
In a study assessing trajectories of inflammation over a 3-year period in healthy adults, those who reported higher rates of physical, sexual, or emotional abuse had higher levels of bioinflammatory blood markers versus those who reported lower rates of abuse. These individuals also had significantly higher rates of loneliness and depression.
“These adverse experiences that people can have in childhood and adolescence really can continue to influence our health at a biological level well into adulthood,” investigator Megan E. Renna, PhD, postdoctoral fellow at Ohio State University, Columbus, said in an interview.
“There may be a somewhat invisible biological effect of that abuse later on in life, in addition to all of the psychological distress that could go along with those experiences,” she added.
The findings were presented at the virtual Anxiety and Depression Association of America Conference 2021.
Need for intervention
Ages ranged from 47 to 67 years (mean age, 57 years), 81% were women, all were relatively healthy, and there were low rates of medical comorbidities.
Participant data on physical, emotional, and sexual abuse prior to age 18 were ascertained using the Childhood Experiences Questionnaire. Blood samples were assayed for cytokines interleukin-6, IL-8, IL-1 beta and tumor necrosis factor–alpha at each visit.
After controlling for age, sex, body mass index, and medical comorbidities, results showed markers of inflammation increased at a greater rate over time in participants with higher rates of physical (P = .05) and sexual abuse (P = .02), compared with those with no history of childhood abuse.
“So, inflammation was increasing at a faster rate across those three visits for people with versus without an abuse history. And this was abuse experienced before age 18, but the mean age of our participants was about 57,” said Dr. Renna.
“It is likely that emotional abuse plays a role in inflammation but we did not have a big enough sample to show significance,” she added.
Participants who had reported childhood abuse also demonstrated significantly higher rates of loneliness and depression across all visits than those without a history of abuse.
“One of the things this work really highlights is the need for intervention for these children and adolescents who are experiencing abuse. This may have a helpful impact on their psychological health as they age, as well as their physical health,” Dr. Renna said.
‘Considerable interest’
In a comment, ADAA President Luana Marques, PhD, Harvard Medical School, Boston, said research is “consistently indicating that childhood adversity puts individuals at risk for a host of problems, including inflammatory concerns, which are precursors for other physical illnesses.”
Such results “demonstrate the importance of early identification and intervention of possible traumatic experiences for youth, and how early intervention at the parent level might also be helpful,” said Dr. Marques, who was not involved with the research.
Also commenting on the study, Charles B. Nemeroff, MD, PhD, professor and chair in the department of psychiatry and behavioral science at the University of Texas at Austin, and president-elect of the ADAA, said in an interview that the findings are pertinent for the field.
“The investigators demonstrated that a history of childhood physical or sexual abuse was associated with a greater inflammatory response, and this is of considerable interest because this increased inflammatory response very likely contributes to the well-documented increased prevalence of serious medical disorders such as heart disease, diabetes, and cancer in victims of child abuse and neglect,” said Dr. Nemeroff, who was not associated with the research.
Dr. Renna, Dr. Marques, and Dr. Nemeroff disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 ‘long-haul’ symptoms overlap with ME/CFS
People experiencing long-term symptoms following acute COVID-19 infection are increasingly meeting criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a phenomenon that highlights the need for unified research and clinical approaches, speakers said at a press briefing March 25 held by the advocacy group MEAction.
“Post-COVID lingering illness was predictable. Similar lingering fatigue syndromes have been reported in the scientific literature for nearly 100 years, following a variety of well-documented infections with viruses, bacteria, fungi, and even protozoa,” said Anthony Komaroff, MD, professor of medicine at Harvard Medical School, Boston.
Core criteria for ME/CFS established by the Institute of Medicine in 2015 include substantial decrement in functioning for at least 6 months, postexertional malaise (PEM), or a worsening of symptoms following even minor exertion (often described as “crashes”), unrefreshing sleep, and cognitive impairment and/or orthostatic intolerance.
Patients with ME/CFS also commonly experience painful headaches, muscle or joint aches, and allergies/other sensitivities. Although many patients can trace their symptoms to an initiating infection, “the cause is often unclear because the diagnosis is often delayed for months or years after symptom onset,” said Lucinda Bateman, MD, founder of the Bateman Horne Center, Salt Lake City, who leads a clinician coalition that aims to improve ME/CFS management.
In an international survey of 3762 COVID-19 “long-haulers” published in a preprint in December of 2020, the most frequent symptoms reported at least 6 months after illness onset were fatigue in 78%, PEM in 72%, and cognitive dysfunction (“brain fog”) in 55%. At the time of the survey, 45% reported requiring reduced work schedules because of their illness, and 22% reported being unable to work at all.
Dr. Bateman said those findings align with her experience so far with 12 COVID-19 “long haulers” who self-referred to her ME/CFS and fibromyalgia specialty clinic. Nine of the 12 met criteria for postural orthostatic tachycardia syndrome (POTS) based on the 10-minute NASA Lean Test, she said, and half also met the 2016 American College of Rheumatology criteria for fibromyalgia.
“Some were severely impaired. We suspect a small fiber polyneuropathy in about half, and mast cell activation syndrome in more than half. We look forward to doing more testing,” Dr. Bateman said.
To be sure, Dr. Komaroff noted, there are some differences. “Long COVID” patients will often experience breathlessness and ongoing anosmia (loss of taste and smell), which aren’t typical of ME/CFS.
But, he said, “many of the symptoms are quite similar ... My guess is that ME/CFS is an illness with a final common pathway that can be triggered by different things,” said Dr. Komaroff, a senior physician at Brigham and Women’s Hospital in Boston, and editor-in-chief of the Harvard Health Letter.
Based on previous data about CFS suggesting a 10% rate of symptoms persisting at least a year following a variety of infectious agents and the predicted 200 million COVID-19 cases globally by the end of 2021, Dr. Komaroff estimated that about 20 million cases of “long COVID” would be expected in the next year.
‘A huge investment’
On the research side, the National Institutes of Health recently appropriated $1.15 billion dollars over the next 4 years to investigate “the heterogeneity in the recovery process after COVID and to develop treatments for those suffering from [postacute COVID-19 syndrome]” according to a Feb. 5, 2021, blog from the National Institute of Neurological Disorders and Stroke (NINDS).
That same day, another NINDS blog announced “new resources for large-scale ME/CFS research” and emphasized the tie-in with long–COVID-19 syndrome.
“That’s a huge investment. In my opinion, there will be several lingering illnesses following COVID,” Dr. Komaroff said, adding, “It’s my bet that long COVID will prove to be caused by certain kinds of abnormalities in the brain, some of the same abnormalities already identified in ME/CFS. Research will determine whether that’s right or wrong.”
In 2017, NINDS had announced a large increase in funding for ME/CFS research, including the creation of four dedicated research centers. In April 2019, NINDS held a 2-day conference highlighting that ongoing work, as reported by Medscape Medical News.
During the briefing, NINDS clinical director Avindra Nath, MD, described a comprehensive ongoing ME/CFS intramural study he’s been leading since 2016.
He’s now also overseeing two long–COVID-19 studies, one of which has a protocol similar to that of the ME/CFS study and will include individuals who are still experiencing long-term symptoms following confirmed cases of COVID-19. The aim is to screen about 1,300 patients. Several task forces are now examining all of these data together.
“Each aspect is now being analyzed … What we learn from one applies to the other,” Dr. Nath said.
Advice for clinicians
In interviews, Dr. Bateman and Dr. Nath offered clinical advice for managing patients who meet ME/CFS criteria, whether they had confirmed or suspected COVID-19, a different infection, or unknown trigger(s).
Dr. Bateman advised that clinicians assess patients for each of the symptoms individually. “Besides exercise intolerance and PEM, the most commonly missed is orthostatic intolerance. It really doesn’t matter what the cause is, it’s amenable to supportive treatment. It’s one aspect of the illness that contributes to severely impaired function. My plea to all physicians would be for sure to assess for [orthostatic intolerance], and gain an understanding about activity management and avoiding PEM symptoms.”
Dr. Nath noted that an often-challenging situation is when tests for the infectious agent and other blood work come back negative, yet the patient still reports multiple debilitating symptoms. This has been a particular issue with long COVID-19, since many patients became ill early in the pandemic before the polymerase chain reaction (PCR) tests for SARS-CoV-2 were widely available.
“The physician can only order tests that are available at their labs. I think what the physician should do is handle symptoms symptomatically but also refer patients to specialists who are taking care of these patients or to research studies,” he said.
Dr. Bateman added, “Whether they had a documented COVID infection – we just have to let go of that in 2020. Way too many people didn’t have access to a test or the timing wasn’t amenable. If people meet criteria for ME/CFS, it’s irrelevant … It’s mainly a clinical diagnosis. It’s not reliant on identifying the infectious trigger.”
Dr. Komaroff, who began caring for then-termed “chronic fatigue syndrome” patients and researching the condition more than 30 years ago, said that “every cloud has its silver lining. The increased focus on postinfectious fatigue syndrome is a silver lining in my mind around the terrible dark cloud that is the pandemic of COVID.”
Dr. Komaroff has received personal fees from Serimmune Inc., Ono Pharma, and Deallus, and grants from the NIH. Dr. Bateman is employed by the Bateman Horne Center, which receives grants from the NIH, and fees from Exagen Inc., and Teva Pharmaceutical. Dr. Nath is an NIH employee.
A version of this article first appeared on Medscape.com.
People experiencing long-term symptoms following acute COVID-19 infection are increasingly meeting criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a phenomenon that highlights the need for unified research and clinical approaches, speakers said at a press briefing March 25 held by the advocacy group MEAction.
“Post-COVID lingering illness was predictable. Similar lingering fatigue syndromes have been reported in the scientific literature for nearly 100 years, following a variety of well-documented infections with viruses, bacteria, fungi, and even protozoa,” said Anthony Komaroff, MD, professor of medicine at Harvard Medical School, Boston.
Core criteria for ME/CFS established by the Institute of Medicine in 2015 include substantial decrement in functioning for at least 6 months, postexertional malaise (PEM), or a worsening of symptoms following even minor exertion (often described as “crashes”), unrefreshing sleep, and cognitive impairment and/or orthostatic intolerance.
Patients with ME/CFS also commonly experience painful headaches, muscle or joint aches, and allergies/other sensitivities. Although many patients can trace their symptoms to an initiating infection, “the cause is often unclear because the diagnosis is often delayed for months or years after symptom onset,” said Lucinda Bateman, MD, founder of the Bateman Horne Center, Salt Lake City, who leads a clinician coalition that aims to improve ME/CFS management.
In an international survey of 3762 COVID-19 “long-haulers” published in a preprint in December of 2020, the most frequent symptoms reported at least 6 months after illness onset were fatigue in 78%, PEM in 72%, and cognitive dysfunction (“brain fog”) in 55%. At the time of the survey, 45% reported requiring reduced work schedules because of their illness, and 22% reported being unable to work at all.
Dr. Bateman said those findings align with her experience so far with 12 COVID-19 “long haulers” who self-referred to her ME/CFS and fibromyalgia specialty clinic. Nine of the 12 met criteria for postural orthostatic tachycardia syndrome (POTS) based on the 10-minute NASA Lean Test, she said, and half also met the 2016 American College of Rheumatology criteria for fibromyalgia.
“Some were severely impaired. We suspect a small fiber polyneuropathy in about half, and mast cell activation syndrome in more than half. We look forward to doing more testing,” Dr. Bateman said.
To be sure, Dr. Komaroff noted, there are some differences. “Long COVID” patients will often experience breathlessness and ongoing anosmia (loss of taste and smell), which aren’t typical of ME/CFS.
But, he said, “many of the symptoms are quite similar ... My guess is that ME/CFS is an illness with a final common pathway that can be triggered by different things,” said Dr. Komaroff, a senior physician at Brigham and Women’s Hospital in Boston, and editor-in-chief of the Harvard Health Letter.
Based on previous data about CFS suggesting a 10% rate of symptoms persisting at least a year following a variety of infectious agents and the predicted 200 million COVID-19 cases globally by the end of 2021, Dr. Komaroff estimated that about 20 million cases of “long COVID” would be expected in the next year.
‘A huge investment’
On the research side, the National Institutes of Health recently appropriated $1.15 billion dollars over the next 4 years to investigate “the heterogeneity in the recovery process after COVID and to develop treatments for those suffering from [postacute COVID-19 syndrome]” according to a Feb. 5, 2021, blog from the National Institute of Neurological Disorders and Stroke (NINDS).
That same day, another NINDS blog announced “new resources for large-scale ME/CFS research” and emphasized the tie-in with long–COVID-19 syndrome.
“That’s a huge investment. In my opinion, there will be several lingering illnesses following COVID,” Dr. Komaroff said, adding, “It’s my bet that long COVID will prove to be caused by certain kinds of abnormalities in the brain, some of the same abnormalities already identified in ME/CFS. Research will determine whether that’s right or wrong.”
In 2017, NINDS had announced a large increase in funding for ME/CFS research, including the creation of four dedicated research centers. In April 2019, NINDS held a 2-day conference highlighting that ongoing work, as reported by Medscape Medical News.
During the briefing, NINDS clinical director Avindra Nath, MD, described a comprehensive ongoing ME/CFS intramural study he’s been leading since 2016.
He’s now also overseeing two long–COVID-19 studies, one of which has a protocol similar to that of the ME/CFS study and will include individuals who are still experiencing long-term symptoms following confirmed cases of COVID-19. The aim is to screen about 1,300 patients. Several task forces are now examining all of these data together.
“Each aspect is now being analyzed … What we learn from one applies to the other,” Dr. Nath said.
Advice for clinicians
In interviews, Dr. Bateman and Dr. Nath offered clinical advice for managing patients who meet ME/CFS criteria, whether they had confirmed or suspected COVID-19, a different infection, or unknown trigger(s).
Dr. Bateman advised that clinicians assess patients for each of the symptoms individually. “Besides exercise intolerance and PEM, the most commonly missed is orthostatic intolerance. It really doesn’t matter what the cause is, it’s amenable to supportive treatment. It’s one aspect of the illness that contributes to severely impaired function. My plea to all physicians would be for sure to assess for [orthostatic intolerance], and gain an understanding about activity management and avoiding PEM symptoms.”
Dr. Nath noted that an often-challenging situation is when tests for the infectious agent and other blood work come back negative, yet the patient still reports multiple debilitating symptoms. This has been a particular issue with long COVID-19, since many patients became ill early in the pandemic before the polymerase chain reaction (PCR) tests for SARS-CoV-2 were widely available.
“The physician can only order tests that are available at their labs. I think what the physician should do is handle symptoms symptomatically but also refer patients to specialists who are taking care of these patients or to research studies,” he said.
Dr. Bateman added, “Whether they had a documented COVID infection – we just have to let go of that in 2020. Way too many people didn’t have access to a test or the timing wasn’t amenable. If people meet criteria for ME/CFS, it’s irrelevant … It’s mainly a clinical diagnosis. It’s not reliant on identifying the infectious trigger.”
Dr. Komaroff, who began caring for then-termed “chronic fatigue syndrome” patients and researching the condition more than 30 years ago, said that “every cloud has its silver lining. The increased focus on postinfectious fatigue syndrome is a silver lining in my mind around the terrible dark cloud that is the pandemic of COVID.”
Dr. Komaroff has received personal fees from Serimmune Inc., Ono Pharma, and Deallus, and grants from the NIH. Dr. Bateman is employed by the Bateman Horne Center, which receives grants from the NIH, and fees from Exagen Inc., and Teva Pharmaceutical. Dr. Nath is an NIH employee.
A version of this article first appeared on Medscape.com.
People experiencing long-term symptoms following acute COVID-19 infection are increasingly meeting criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a phenomenon that highlights the need for unified research and clinical approaches, speakers said at a press briefing March 25 held by the advocacy group MEAction.
“Post-COVID lingering illness was predictable. Similar lingering fatigue syndromes have been reported in the scientific literature for nearly 100 years, following a variety of well-documented infections with viruses, bacteria, fungi, and even protozoa,” said Anthony Komaroff, MD, professor of medicine at Harvard Medical School, Boston.
Core criteria for ME/CFS established by the Institute of Medicine in 2015 include substantial decrement in functioning for at least 6 months, postexertional malaise (PEM), or a worsening of symptoms following even minor exertion (often described as “crashes”), unrefreshing sleep, and cognitive impairment and/or orthostatic intolerance.
Patients with ME/CFS also commonly experience painful headaches, muscle or joint aches, and allergies/other sensitivities. Although many patients can trace their symptoms to an initiating infection, “the cause is often unclear because the diagnosis is often delayed for months or years after symptom onset,” said Lucinda Bateman, MD, founder of the Bateman Horne Center, Salt Lake City, who leads a clinician coalition that aims to improve ME/CFS management.
In an international survey of 3762 COVID-19 “long-haulers” published in a preprint in December of 2020, the most frequent symptoms reported at least 6 months after illness onset were fatigue in 78%, PEM in 72%, and cognitive dysfunction (“brain fog”) in 55%. At the time of the survey, 45% reported requiring reduced work schedules because of their illness, and 22% reported being unable to work at all.
Dr. Bateman said those findings align with her experience so far with 12 COVID-19 “long haulers” who self-referred to her ME/CFS and fibromyalgia specialty clinic. Nine of the 12 met criteria for postural orthostatic tachycardia syndrome (POTS) based on the 10-minute NASA Lean Test, she said, and half also met the 2016 American College of Rheumatology criteria for fibromyalgia.
“Some were severely impaired. We suspect a small fiber polyneuropathy in about half, and mast cell activation syndrome in more than half. We look forward to doing more testing,” Dr. Bateman said.
To be sure, Dr. Komaroff noted, there are some differences. “Long COVID” patients will often experience breathlessness and ongoing anosmia (loss of taste and smell), which aren’t typical of ME/CFS.
But, he said, “many of the symptoms are quite similar ... My guess is that ME/CFS is an illness with a final common pathway that can be triggered by different things,” said Dr. Komaroff, a senior physician at Brigham and Women’s Hospital in Boston, and editor-in-chief of the Harvard Health Letter.
Based on previous data about CFS suggesting a 10% rate of symptoms persisting at least a year following a variety of infectious agents and the predicted 200 million COVID-19 cases globally by the end of 2021, Dr. Komaroff estimated that about 20 million cases of “long COVID” would be expected in the next year.
‘A huge investment’
On the research side, the National Institutes of Health recently appropriated $1.15 billion dollars over the next 4 years to investigate “the heterogeneity in the recovery process after COVID and to develop treatments for those suffering from [postacute COVID-19 syndrome]” according to a Feb. 5, 2021, blog from the National Institute of Neurological Disorders and Stroke (NINDS).
That same day, another NINDS blog announced “new resources for large-scale ME/CFS research” and emphasized the tie-in with long–COVID-19 syndrome.
“That’s a huge investment. In my opinion, there will be several lingering illnesses following COVID,” Dr. Komaroff said, adding, “It’s my bet that long COVID will prove to be caused by certain kinds of abnormalities in the brain, some of the same abnormalities already identified in ME/CFS. Research will determine whether that’s right or wrong.”
In 2017, NINDS had announced a large increase in funding for ME/CFS research, including the creation of four dedicated research centers. In April 2019, NINDS held a 2-day conference highlighting that ongoing work, as reported by Medscape Medical News.
During the briefing, NINDS clinical director Avindra Nath, MD, described a comprehensive ongoing ME/CFS intramural study he’s been leading since 2016.
He’s now also overseeing two long–COVID-19 studies, one of which has a protocol similar to that of the ME/CFS study and will include individuals who are still experiencing long-term symptoms following confirmed cases of COVID-19. The aim is to screen about 1,300 patients. Several task forces are now examining all of these data together.
“Each aspect is now being analyzed … What we learn from one applies to the other,” Dr. Nath said.
Advice for clinicians
In interviews, Dr. Bateman and Dr. Nath offered clinical advice for managing patients who meet ME/CFS criteria, whether they had confirmed or suspected COVID-19, a different infection, or unknown trigger(s).
Dr. Bateman advised that clinicians assess patients for each of the symptoms individually. “Besides exercise intolerance and PEM, the most commonly missed is orthostatic intolerance. It really doesn’t matter what the cause is, it’s amenable to supportive treatment. It’s one aspect of the illness that contributes to severely impaired function. My plea to all physicians would be for sure to assess for [orthostatic intolerance], and gain an understanding about activity management and avoiding PEM symptoms.”
Dr. Nath noted that an often-challenging situation is when tests for the infectious agent and other blood work come back negative, yet the patient still reports multiple debilitating symptoms. This has been a particular issue with long COVID-19, since many patients became ill early in the pandemic before the polymerase chain reaction (PCR) tests for SARS-CoV-2 were widely available.
“The physician can only order tests that are available at their labs. I think what the physician should do is handle symptoms symptomatically but also refer patients to specialists who are taking care of these patients or to research studies,” he said.
Dr. Bateman added, “Whether they had a documented COVID infection – we just have to let go of that in 2020. Way too many people didn’t have access to a test or the timing wasn’t amenable. If people meet criteria for ME/CFS, it’s irrelevant … It’s mainly a clinical diagnosis. It’s not reliant on identifying the infectious trigger.”
Dr. Komaroff, who began caring for then-termed “chronic fatigue syndrome” patients and researching the condition more than 30 years ago, said that “every cloud has its silver lining. The increased focus on postinfectious fatigue syndrome is a silver lining in my mind around the terrible dark cloud that is the pandemic of COVID.”
Dr. Komaroff has received personal fees from Serimmune Inc., Ono Pharma, and Deallus, and grants from the NIH. Dr. Bateman is employed by the Bateman Horne Center, which receives grants from the NIH, and fees from Exagen Inc., and Teva Pharmaceutical. Dr. Nath is an NIH employee.
A version of this article first appeared on Medscape.com.
Step therapy: Inside the fight against insurance companies and fail-first medicine
Every day Melissa Fulton, RN, MSN, FNP, APRN-C, shows up to work, she’s ready for another fight. An advanced practice nurse who specializes in multiple sclerosis care, Ms. Fulton said she typically spends more than a third of her time battling it out with insurance companies over drugs she knows her patients need but that insurers don’t want to cover. Instead, they want the patient to first receive less expensive and often less efficacious drugs, even if that goes against recommendations and, in some cases, against the patient’s medical history.
The maddening protocol – familiar to health care providers everywhere – is known as “step therapy.” It forces patients to try alternative medications – medications that often fail – before receiving the one initially prescribed. The process can take weeks or months, which is time that some patients don’t have. Step therapy was sold as a way to lower costs. However, beyond the ethically problematic notion of forcing sick patients to receiver cheaper alternatives that are ineffective, research has also shown it may actually be more costly in the long run.
Ms. Fulton, who works at Saunders Medical Center in Wahoo, Neb., is a veteran in the war against step therapy. She is used to pushing her appeals up the insurance company chain of command, past nonmedical reviewers, until her patient’s case finally lands on the desk of someone with a neurology background. She said that can take three or four appeals – a judge might even get involved – and the patient could still lose. “This happens constantly,” she said, “but we fight like hell.”
Fortunately, life may soon get a little easier for Ms. Fulton. In late March, a bill to restrict step therapy made it through the Nebraska state legislature and is on its way to the governor’s desk. The Step Therapy Reform Act doesn’t outright ban the practice; however, it will put guardrails in place. It requires that insurers respond to appeals within certain time frames, and it creates key exemptions.
When the governor signs off, Nebraska will join more than two dozen other states that already have step therapy restrictions on the books, according to Hannah Lynch, MPS, associate director of federal government relations and health policy at the National Psoriasis Foundation, a leading advocate to reform and protect against the insurance practice. “There’s a lot of frustration out there,” Ms. Lynch said. “It really hinders providers’ ability to make decisions they think will have the best outcomes.”
Driven by coalitions of doctors, nurses, and patients, laws reining in step therapy have been adopted at a relatively quick clip, mostly within the past 5 years. Recent additions include South Dakota and North Carolina, which adopted step therapy laws in 2020, and Arkansas, which passed a law earlier this year.
Ms. Lynch attributed growing support to rising out-of-pocket drug costs and the introduction of biologic drugs, which are often more effective but also more expensive. Like Nebraska’s law, most step therapy reform legislation carves out exemptions and requires timely appeals processes; however, many of the laws still have significant gaps, such as not including certain types of insurance plans.
Ideally, Ms. Lynch said, the protections would apply to all types of health plans that are regulated at the state level, such as Medicaid, state employee health plans, and coverage sold through state insurance exchanges. Closing loopholes in the laws is a top priority for advocates, she added, pointing to work currently underway in Arkansas to extend its new protections to Medicaid expansion patients.
“With so many outside stakeholders, you have to compromise – it’s a give and take,” Ms. Lynch said. Still, when it comes to fighting step therapy, she says, “Any protection on the books is always our first goal when we go into a state.”
Putting patients first
Lisa Arkin, MD, a pediatric dermatologist at the University of Wisconsin–Madison, said she finds herself “swimming upstream every day in the fight with insurance.” Her patients are typically on their second or third stop and have more complex disorders. Dr. Arkin said that the problem with step therapy is that it tries to squeeze all patients into the same box, even if the circumstances don’t fit.
Her state passed restrictions on step therapy in 2019, but the measures only went into effect last year. Under the Wisconsin law, patients can be granted an exemption if an alternative treatment is contraindicated, likely to cause harm, or expected to be ineffective. Patients can also be exempt if their current treatment is working.
Dr. Arkin, an outspoken advocate for curbing step therapy, says the Wisconsin law is “very strong.” However, because it only applies to certain health plans – state employee health plans and those purchased in the state’s health insurance exchange – fewer than half the state’s patients benefit from its protections. She notes that some of the most severe presentations she treats occur in patients who rely on Medicaid coverage and already face barriers to care.
“I’m a doctor who puts up a fuss [with insurers], but that’s not fair – we shouldn’t have to do that,” Dr. Arkin said. “To me, it’s really critical to make this an even playing field so this law affords protection to everyone I see in the clinic.”
Major medical associations caution against step therapy as well. The American Society of Clinical Oncology and the American Medical Association have called out the risks to patient safety and health. In fact, in 2019, after the Centers for Medicare & Medicaid Services gave new authority to Medicare Advantage plans to start using step therapy, dozens of national medical groups called out the agency for allowing a practice that could potentially hurt patients and undercut the physician-patient decision-making process.
Last year, in a new position paper from the American College of Physicians, authors laid out recommendations for combating step therapy’s side effects. These recommendations included making related data transparent to the public and minimizing the policy’s disruptions to care. Jacqueline W. Fincher, MD, MACP, a member of the committee that issued the position paper and who is a primary care physician in Georgia, said such insurance practices need to be designed with “strong input from frontline physicians, not clipboard physicians.
“What we want from insurers is understanding, transparency, and the least burdensome protocol to provide patients the care they need at a cost-effective price they can afford,” said Dr. Fincher, who is also the current president of the ACP. “The focus needs to be on what’s in the patient’s best interest.”
Every year a new fight
“We all dread January,” said Dr. Fincher. That is the worst month, she added, because new health benefits go into effect, which means patients who are responding well to certain treatments may suddenly face new restrictions.
Another aggravating aspect of step therapy? It is often difficult – if not impossible – to access information on specific step therapy protocols in a patient’s health plan in real time in the exam room, where treatment conversations actually take place. In a more patient-centered world, Dr. Fincher said, she would be able to use the electronic health record system to quickly identify whether a patient’s plan covers a particular treatment and, if not, what the alternatives are.
Georgia’s new step therapy law went into effect last year. Like laws in other states, it spells out step therapy exemptions and sets time frames in which insurers must respond to exceptions and appeals. Dr. Fincher, who spoke in favor of the new law, said she’s “happy for any step forward.” Still, the growing burden of prior authorization rules are an utter “time sink” for her and her staff.
“I have to justify my decisions to nondoctors before I even get to a doctor, and that’s really frustrating,” she said. “We’re talking about people here, not widgets.”
Advocates in Nevada are hoping this is the year a step therapy bill will make it into law in their state. As of March, one had yet to be introduced in the state legislature. Tom McCoy, director of state government affairs at the Nevada Chronic Care Collaborative, said existing Nevada law already prohibits nonmedical drug switching during a policy year; however, insurers can still make changes the following year.
A bill to rein in step therapy was proposed previously, Mr. McCoy said, but it never got off the ground. The collaborative, as well as about two dozen organizations representing Nevada providers and patients, are now calling on state lawmakers to make the issue a priority in the current session.
“The health plans have a lot of power – a lot,” Mr. McCoy said. “We’re hoping to get a [legislative] sponsor in 2021 ... but it’s also been a really hard year to connect legislators with patients and doctors, and being able to hear their stories really does make a difference.”
In Nebraska, Marcus Snow, MD, a rheumatologist at Nebraska Medicine, in Omaha, said that the state’s new step therapy law will be a “great first step in helping to provide some guardrails” around the practice. He noted that turnaround requirements for insurer responses are “sorely needed.” However, he said that, because the bill doesn’t apply to all health plans, many Nebraskans still won’t benefit.
Dealing with step therapy is a daily “headache” for Dr. Snow, who says navigating the bureaucracy of prior authorization seems to be getting worse every year. Like his peers around the country, he spends an inordinate amount of time pushing appeals up the insurance company ranks to get access to treatments he believes will be most effective. But Snow says that, more than just being a mountain of tiresome red tape, these practices also intrude on the patient-provider relationship, casting an unsettling sense of uncertainty that the ultimate decision about the best course of action isn’t up to the doctor and patient at all.
“In the end, the insurance company is the judge and jury of my prescription,” Dr. Snow said. “They’d argue I can still prescribe it, but if it costs $70,000 a year – I don’t know who can afford that.”
Ms. Lynch, at the National Psoriasis Foundation, said their step therapy advocacy will continue to take a two-pronged approach. They will push for new and expanded protections at both state and federal levels. Protections are needed at both levels to make sure that all health plans regulated by all entities are covered. In the U.S. Senate and the House, step therapy bills were reintroduced this year. They would apply to health plans subject to the federal Employee Retirement Income Security Act, which governs employer-sponsored health coverage, and could close a big gap in existing protections. Oregon, New Jersey, and Arizona are at the top of the foundation’s advocacy list this year, according to Ms. Lynch.
“Folks are really starting to pay more attention to this issue,” she said. “And hearing those real-world stories and frustrations is definitely one of the most effective tools we have.”
A version of this article first appeared on Medscape.com.
Every day Melissa Fulton, RN, MSN, FNP, APRN-C, shows up to work, she’s ready for another fight. An advanced practice nurse who specializes in multiple sclerosis care, Ms. Fulton said she typically spends more than a third of her time battling it out with insurance companies over drugs she knows her patients need but that insurers don’t want to cover. Instead, they want the patient to first receive less expensive and often less efficacious drugs, even if that goes against recommendations and, in some cases, against the patient’s medical history.
The maddening protocol – familiar to health care providers everywhere – is known as “step therapy.” It forces patients to try alternative medications – medications that often fail – before receiving the one initially prescribed. The process can take weeks or months, which is time that some patients don’t have. Step therapy was sold as a way to lower costs. However, beyond the ethically problematic notion of forcing sick patients to receiver cheaper alternatives that are ineffective, research has also shown it may actually be more costly in the long run.
Ms. Fulton, who works at Saunders Medical Center in Wahoo, Neb., is a veteran in the war against step therapy. She is used to pushing her appeals up the insurance company chain of command, past nonmedical reviewers, until her patient’s case finally lands on the desk of someone with a neurology background. She said that can take three or four appeals – a judge might even get involved – and the patient could still lose. “This happens constantly,” she said, “but we fight like hell.”
Fortunately, life may soon get a little easier for Ms. Fulton. In late March, a bill to restrict step therapy made it through the Nebraska state legislature and is on its way to the governor’s desk. The Step Therapy Reform Act doesn’t outright ban the practice; however, it will put guardrails in place. It requires that insurers respond to appeals within certain time frames, and it creates key exemptions.
When the governor signs off, Nebraska will join more than two dozen other states that already have step therapy restrictions on the books, according to Hannah Lynch, MPS, associate director of federal government relations and health policy at the National Psoriasis Foundation, a leading advocate to reform and protect against the insurance practice. “There’s a lot of frustration out there,” Ms. Lynch said. “It really hinders providers’ ability to make decisions they think will have the best outcomes.”
Driven by coalitions of doctors, nurses, and patients, laws reining in step therapy have been adopted at a relatively quick clip, mostly within the past 5 years. Recent additions include South Dakota and North Carolina, which adopted step therapy laws in 2020, and Arkansas, which passed a law earlier this year.
Ms. Lynch attributed growing support to rising out-of-pocket drug costs and the introduction of biologic drugs, which are often more effective but also more expensive. Like Nebraska’s law, most step therapy reform legislation carves out exemptions and requires timely appeals processes; however, many of the laws still have significant gaps, such as not including certain types of insurance plans.
Ideally, Ms. Lynch said, the protections would apply to all types of health plans that are regulated at the state level, such as Medicaid, state employee health plans, and coverage sold through state insurance exchanges. Closing loopholes in the laws is a top priority for advocates, she added, pointing to work currently underway in Arkansas to extend its new protections to Medicaid expansion patients.
“With so many outside stakeholders, you have to compromise – it’s a give and take,” Ms. Lynch said. Still, when it comes to fighting step therapy, she says, “Any protection on the books is always our first goal when we go into a state.”
Putting patients first
Lisa Arkin, MD, a pediatric dermatologist at the University of Wisconsin–Madison, said she finds herself “swimming upstream every day in the fight with insurance.” Her patients are typically on their second or third stop and have more complex disorders. Dr. Arkin said that the problem with step therapy is that it tries to squeeze all patients into the same box, even if the circumstances don’t fit.
Her state passed restrictions on step therapy in 2019, but the measures only went into effect last year. Under the Wisconsin law, patients can be granted an exemption if an alternative treatment is contraindicated, likely to cause harm, or expected to be ineffective. Patients can also be exempt if their current treatment is working.
Dr. Arkin, an outspoken advocate for curbing step therapy, says the Wisconsin law is “very strong.” However, because it only applies to certain health plans – state employee health plans and those purchased in the state’s health insurance exchange – fewer than half the state’s patients benefit from its protections. She notes that some of the most severe presentations she treats occur in patients who rely on Medicaid coverage and already face barriers to care.
“I’m a doctor who puts up a fuss [with insurers], but that’s not fair – we shouldn’t have to do that,” Dr. Arkin said. “To me, it’s really critical to make this an even playing field so this law affords protection to everyone I see in the clinic.”
Major medical associations caution against step therapy as well. The American Society of Clinical Oncology and the American Medical Association have called out the risks to patient safety and health. In fact, in 2019, after the Centers for Medicare & Medicaid Services gave new authority to Medicare Advantage plans to start using step therapy, dozens of national medical groups called out the agency for allowing a practice that could potentially hurt patients and undercut the physician-patient decision-making process.
Last year, in a new position paper from the American College of Physicians, authors laid out recommendations for combating step therapy’s side effects. These recommendations included making related data transparent to the public and minimizing the policy’s disruptions to care. Jacqueline W. Fincher, MD, MACP, a member of the committee that issued the position paper and who is a primary care physician in Georgia, said such insurance practices need to be designed with “strong input from frontline physicians, not clipboard physicians.
“What we want from insurers is understanding, transparency, and the least burdensome protocol to provide patients the care they need at a cost-effective price they can afford,” said Dr. Fincher, who is also the current president of the ACP. “The focus needs to be on what’s in the patient’s best interest.”
Every year a new fight
“We all dread January,” said Dr. Fincher. That is the worst month, she added, because new health benefits go into effect, which means patients who are responding well to certain treatments may suddenly face new restrictions.
Another aggravating aspect of step therapy? It is often difficult – if not impossible – to access information on specific step therapy protocols in a patient’s health plan in real time in the exam room, where treatment conversations actually take place. In a more patient-centered world, Dr. Fincher said, she would be able to use the electronic health record system to quickly identify whether a patient’s plan covers a particular treatment and, if not, what the alternatives are.
Georgia’s new step therapy law went into effect last year. Like laws in other states, it spells out step therapy exemptions and sets time frames in which insurers must respond to exceptions and appeals. Dr. Fincher, who spoke in favor of the new law, said she’s “happy for any step forward.” Still, the growing burden of prior authorization rules are an utter “time sink” for her and her staff.
“I have to justify my decisions to nondoctors before I even get to a doctor, and that’s really frustrating,” she said. “We’re talking about people here, not widgets.”
Advocates in Nevada are hoping this is the year a step therapy bill will make it into law in their state. As of March, one had yet to be introduced in the state legislature. Tom McCoy, director of state government affairs at the Nevada Chronic Care Collaborative, said existing Nevada law already prohibits nonmedical drug switching during a policy year; however, insurers can still make changes the following year.
A bill to rein in step therapy was proposed previously, Mr. McCoy said, but it never got off the ground. The collaborative, as well as about two dozen organizations representing Nevada providers and patients, are now calling on state lawmakers to make the issue a priority in the current session.
“The health plans have a lot of power – a lot,” Mr. McCoy said. “We’re hoping to get a [legislative] sponsor in 2021 ... but it’s also been a really hard year to connect legislators with patients and doctors, and being able to hear their stories really does make a difference.”
In Nebraska, Marcus Snow, MD, a rheumatologist at Nebraska Medicine, in Omaha, said that the state’s new step therapy law will be a “great first step in helping to provide some guardrails” around the practice. He noted that turnaround requirements for insurer responses are “sorely needed.” However, he said that, because the bill doesn’t apply to all health plans, many Nebraskans still won’t benefit.
Dealing with step therapy is a daily “headache” for Dr. Snow, who says navigating the bureaucracy of prior authorization seems to be getting worse every year. Like his peers around the country, he spends an inordinate amount of time pushing appeals up the insurance company ranks to get access to treatments he believes will be most effective. But Snow says that, more than just being a mountain of tiresome red tape, these practices also intrude on the patient-provider relationship, casting an unsettling sense of uncertainty that the ultimate decision about the best course of action isn’t up to the doctor and patient at all.
“In the end, the insurance company is the judge and jury of my prescription,” Dr. Snow said. “They’d argue I can still prescribe it, but if it costs $70,000 a year – I don’t know who can afford that.”
Ms. Lynch, at the National Psoriasis Foundation, said their step therapy advocacy will continue to take a two-pronged approach. They will push for new and expanded protections at both state and federal levels. Protections are needed at both levels to make sure that all health plans regulated by all entities are covered. In the U.S. Senate and the House, step therapy bills were reintroduced this year. They would apply to health plans subject to the federal Employee Retirement Income Security Act, which governs employer-sponsored health coverage, and could close a big gap in existing protections. Oregon, New Jersey, and Arizona are at the top of the foundation’s advocacy list this year, according to Ms. Lynch.
“Folks are really starting to pay more attention to this issue,” she said. “And hearing those real-world stories and frustrations is definitely one of the most effective tools we have.”
A version of this article first appeared on Medscape.com.
Every day Melissa Fulton, RN, MSN, FNP, APRN-C, shows up to work, she’s ready for another fight. An advanced practice nurse who specializes in multiple sclerosis care, Ms. Fulton said she typically spends more than a third of her time battling it out with insurance companies over drugs she knows her patients need but that insurers don’t want to cover. Instead, they want the patient to first receive less expensive and often less efficacious drugs, even if that goes against recommendations and, in some cases, against the patient’s medical history.
The maddening protocol – familiar to health care providers everywhere – is known as “step therapy.” It forces patients to try alternative medications – medications that often fail – before receiving the one initially prescribed. The process can take weeks or months, which is time that some patients don’t have. Step therapy was sold as a way to lower costs. However, beyond the ethically problematic notion of forcing sick patients to receiver cheaper alternatives that are ineffective, research has also shown it may actually be more costly in the long run.
Ms. Fulton, who works at Saunders Medical Center in Wahoo, Neb., is a veteran in the war against step therapy. She is used to pushing her appeals up the insurance company chain of command, past nonmedical reviewers, until her patient’s case finally lands on the desk of someone with a neurology background. She said that can take three or four appeals – a judge might even get involved – and the patient could still lose. “This happens constantly,” she said, “but we fight like hell.”
Fortunately, life may soon get a little easier for Ms. Fulton. In late March, a bill to restrict step therapy made it through the Nebraska state legislature and is on its way to the governor’s desk. The Step Therapy Reform Act doesn’t outright ban the practice; however, it will put guardrails in place. It requires that insurers respond to appeals within certain time frames, and it creates key exemptions.
When the governor signs off, Nebraska will join more than two dozen other states that already have step therapy restrictions on the books, according to Hannah Lynch, MPS, associate director of federal government relations and health policy at the National Psoriasis Foundation, a leading advocate to reform and protect against the insurance practice. “There’s a lot of frustration out there,” Ms. Lynch said. “It really hinders providers’ ability to make decisions they think will have the best outcomes.”
Driven by coalitions of doctors, nurses, and patients, laws reining in step therapy have been adopted at a relatively quick clip, mostly within the past 5 years. Recent additions include South Dakota and North Carolina, which adopted step therapy laws in 2020, and Arkansas, which passed a law earlier this year.
Ms. Lynch attributed growing support to rising out-of-pocket drug costs and the introduction of biologic drugs, which are often more effective but also more expensive. Like Nebraska’s law, most step therapy reform legislation carves out exemptions and requires timely appeals processes; however, many of the laws still have significant gaps, such as not including certain types of insurance plans.
Ideally, Ms. Lynch said, the protections would apply to all types of health plans that are regulated at the state level, such as Medicaid, state employee health plans, and coverage sold through state insurance exchanges. Closing loopholes in the laws is a top priority for advocates, she added, pointing to work currently underway in Arkansas to extend its new protections to Medicaid expansion patients.
“With so many outside stakeholders, you have to compromise – it’s a give and take,” Ms. Lynch said. Still, when it comes to fighting step therapy, she says, “Any protection on the books is always our first goal when we go into a state.”
Putting patients first
Lisa Arkin, MD, a pediatric dermatologist at the University of Wisconsin–Madison, said she finds herself “swimming upstream every day in the fight with insurance.” Her patients are typically on their second or third stop and have more complex disorders. Dr. Arkin said that the problem with step therapy is that it tries to squeeze all patients into the same box, even if the circumstances don’t fit.
Her state passed restrictions on step therapy in 2019, but the measures only went into effect last year. Under the Wisconsin law, patients can be granted an exemption if an alternative treatment is contraindicated, likely to cause harm, or expected to be ineffective. Patients can also be exempt if their current treatment is working.
Dr. Arkin, an outspoken advocate for curbing step therapy, says the Wisconsin law is “very strong.” However, because it only applies to certain health plans – state employee health plans and those purchased in the state’s health insurance exchange – fewer than half the state’s patients benefit from its protections. She notes that some of the most severe presentations she treats occur in patients who rely on Medicaid coverage and already face barriers to care.
“I’m a doctor who puts up a fuss [with insurers], but that’s not fair – we shouldn’t have to do that,” Dr. Arkin said. “To me, it’s really critical to make this an even playing field so this law affords protection to everyone I see in the clinic.”
Major medical associations caution against step therapy as well. The American Society of Clinical Oncology and the American Medical Association have called out the risks to patient safety and health. In fact, in 2019, after the Centers for Medicare & Medicaid Services gave new authority to Medicare Advantage plans to start using step therapy, dozens of national medical groups called out the agency for allowing a practice that could potentially hurt patients and undercut the physician-patient decision-making process.
Last year, in a new position paper from the American College of Physicians, authors laid out recommendations for combating step therapy’s side effects. These recommendations included making related data transparent to the public and minimizing the policy’s disruptions to care. Jacqueline W. Fincher, MD, MACP, a member of the committee that issued the position paper and who is a primary care physician in Georgia, said such insurance practices need to be designed with “strong input from frontline physicians, not clipboard physicians.
“What we want from insurers is understanding, transparency, and the least burdensome protocol to provide patients the care they need at a cost-effective price they can afford,” said Dr. Fincher, who is also the current president of the ACP. “The focus needs to be on what’s in the patient’s best interest.”
Every year a new fight
“We all dread January,” said Dr. Fincher. That is the worst month, she added, because new health benefits go into effect, which means patients who are responding well to certain treatments may suddenly face new restrictions.
Another aggravating aspect of step therapy? It is often difficult – if not impossible – to access information on specific step therapy protocols in a patient’s health plan in real time in the exam room, where treatment conversations actually take place. In a more patient-centered world, Dr. Fincher said, she would be able to use the electronic health record system to quickly identify whether a patient’s plan covers a particular treatment and, if not, what the alternatives are.
Georgia’s new step therapy law went into effect last year. Like laws in other states, it spells out step therapy exemptions and sets time frames in which insurers must respond to exceptions and appeals. Dr. Fincher, who spoke in favor of the new law, said she’s “happy for any step forward.” Still, the growing burden of prior authorization rules are an utter “time sink” for her and her staff.
“I have to justify my decisions to nondoctors before I even get to a doctor, and that’s really frustrating,” she said. “We’re talking about people here, not widgets.”
Advocates in Nevada are hoping this is the year a step therapy bill will make it into law in their state. As of March, one had yet to be introduced in the state legislature. Tom McCoy, director of state government affairs at the Nevada Chronic Care Collaborative, said existing Nevada law already prohibits nonmedical drug switching during a policy year; however, insurers can still make changes the following year.
A bill to rein in step therapy was proposed previously, Mr. McCoy said, but it never got off the ground. The collaborative, as well as about two dozen organizations representing Nevada providers and patients, are now calling on state lawmakers to make the issue a priority in the current session.
“The health plans have a lot of power – a lot,” Mr. McCoy said. “We’re hoping to get a [legislative] sponsor in 2021 ... but it’s also been a really hard year to connect legislators with patients and doctors, and being able to hear their stories really does make a difference.”
In Nebraska, Marcus Snow, MD, a rheumatologist at Nebraska Medicine, in Omaha, said that the state’s new step therapy law will be a “great first step in helping to provide some guardrails” around the practice. He noted that turnaround requirements for insurer responses are “sorely needed.” However, he said that, because the bill doesn’t apply to all health plans, many Nebraskans still won’t benefit.
Dealing with step therapy is a daily “headache” for Dr. Snow, who says navigating the bureaucracy of prior authorization seems to be getting worse every year. Like his peers around the country, he spends an inordinate amount of time pushing appeals up the insurance company ranks to get access to treatments he believes will be most effective. But Snow says that, more than just being a mountain of tiresome red tape, these practices also intrude on the patient-provider relationship, casting an unsettling sense of uncertainty that the ultimate decision about the best course of action isn’t up to the doctor and patient at all.
“In the end, the insurance company is the judge and jury of my prescription,” Dr. Snow said. “They’d argue I can still prescribe it, but if it costs $70,000 a year – I don’t know who can afford that.”
Ms. Lynch, at the National Psoriasis Foundation, said their step therapy advocacy will continue to take a two-pronged approach. They will push for new and expanded protections at both state and federal levels. Protections are needed at both levels to make sure that all health plans regulated by all entities are covered. In the U.S. Senate and the House, step therapy bills were reintroduced this year. They would apply to health plans subject to the federal Employee Retirement Income Security Act, which governs employer-sponsored health coverage, and could close a big gap in existing protections. Oregon, New Jersey, and Arizona are at the top of the foundation’s advocacy list this year, according to Ms. Lynch.
“Folks are really starting to pay more attention to this issue,” she said. “And hearing those real-world stories and frustrations is definitely one of the most effective tools we have.”
A version of this article first appeared on Medscape.com.
Encephalopathy common, often lethal in hospitalized patients with COVID-19
, new research shows. Results of a retrospective study show that of almost 4,500 patients with COVID-19, 12% were diagnosed with TME. Of these, 78% developed encephalopathy immediately prior to hospital admission. Septic encephalopathy, hypoxic-ischemic encephalopathy (HIE), and uremia were the most common causes, although multiple causes were present in close to 80% of patients. TME was also associated with a 24% higher risk of in-hospital death.
“We found that close to one in eight patients who were hospitalized with COVID-19 had TME that was not attributed to the effects of sedatives, and that this is incredibly common among these patients who are critically ill” said lead author Jennifer A. Frontera, MD, New York University.
“The general principle of our findings is to be more aggressive in TME; and from a neurologist perspective, the way to do this is to eliminate the effects of sedation, which is a confounder,” she said.
The study was published online March 16 in Neurocritical Care.
Drilling down
“Many neurological complications of COVID-19 are sequelae of severe illness or secondary effects of multisystem organ failure, but our previous work identified TME as the most common neurological complication,” Dr. Frontera said.
Previous research investigating encephalopathy among patients with COVID-19 included patients who may have been sedated or have had a positive Confusion Assessment Method (CAM) result.
“A lot of the delirium literature is effectively heterogeneous because there are a number of patients who are on sedative medication that, if you could turn it off, these patients would return to normal. Some may have underlying neurological issues that can be addressed, but you can›t get to the bottom of this unless you turn off the sedation,” Dr. Frontera noted.
“We wanted to be specific and try to drill down to see what the underlying cause of the encephalopathy was,” she said.
The researchers retrospectively analyzed data on 4,491 patients (≥ 18 years old) with COVID-19 who were admitted to four New York City hospitals between March 1, 2020, and May 20, 2020. Of these, 559 (12%) with TME were compared with 3,932 patients without TME.
The researchers looked at index admissions and included patients who had:
- New changes in mental status or significant worsening of mental status (in patients with baseline abnormal mental status).
- Hyperglycemia or with transient focal neurologic deficits that resolved with glucose correction.
- An adequate washout of sedating medications (when relevant) prior to mental status assessment.
Potential etiologies included electrolyte abnormalities, organ failure, hypertensive encephalopathy, sepsis or active infection, fever, nutritional deficiency, and environmental injury.
Foreign environment
Most (78%) of the 559 patients diagnosed with TME had already developed encephalopathy immediately prior to hospital admission, the authors report. The most common etiologies of TME among hospitalized patients with COVID-19 are listed below.
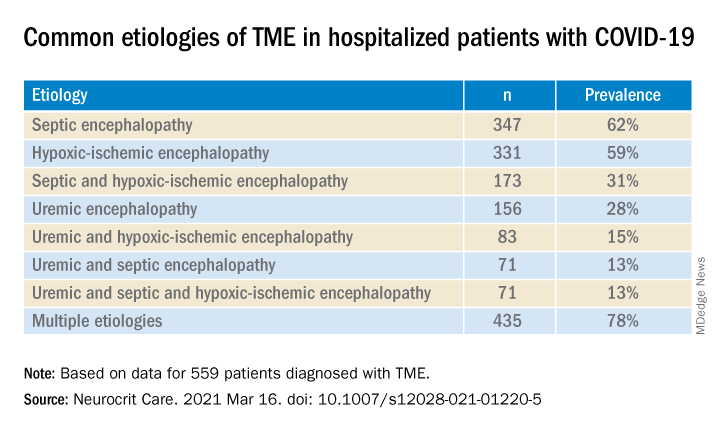
Compared with patients without TME, those with TME – (all Ps < .001):
- Were older (76 vs. 62 years).
- Had higher rates of dementia (27% vs. 3%).
- Had higher rates of psychiatric history (20% vs. 10%).
- Were more often intubated (37% vs. 20%).
- Had a longer length of hospital stay (7.9 vs. 6.0 days).
- Were less often discharged home (25% vs. 66%).
“It’s no surprise that older patients and people with dementia or psychiatric illness are predisposed to becoming encephalopathic,” said Dr. Frontera. “Being in a foreign environment, such as a hospital, or being sleep-deprived in the ICU is likely to make them more confused during their hospital stay.”
Delirium as a symptom
In-hospital mortality or discharge to hospice was considerably higher in the TME versus non-TME patients (44% vs. 18%, respectively).
When the researchers adjusted for confounders (age, sex, race, worse Sequential Organ Failure Assessment score during hospitalization, ventilator status, study week, hospital location, and ICU care level) and excluded patients receiving only comfort care, they found that TME was associated with a 24% increased risk of in-hospital death (30% in patients with TME vs. 16% in those without TME).
The highest mortality risk was associated with hypoxemia, with 42% of patients with HIE dying during hospitalization, compared with 16% of patients without HIE (adjusted hazard ratio 1.56; 95% confidence interval, 1.21-2.00; P = .001).
“Not all patients who are intubated require sedation, but there’s generally a lot of hesitation in reducing or stopping sedation in some patients,” Dr. Frontera observed.
She acknowledged there are “many extremely sick patients whom you can’t ventilate without sedation.”
Nevertheless, “delirium in and of itself does not cause death. It’s a symptom, not a disease, and we have to figure out what causes it. Delirium might not need to be sedated, and it’s more important to see what the causal problem is.”
Independent predictor of death
Commenting on the study, Panayiotis N. Varelas, MD, PhD, vice president of the Neurocritical Care Society, said the study “approached the TME issue better than previously, namely allowing time for sedatives to wear off to have a better sample of patients with this syndrome.”
Dr. Varelas, who is chairman of the department of neurology and professor of neurology at Albany (N.Y.) Medical College, emphasized that TME “is not benign and, in patients with COVID-19, it is an independent predictor of in-hospital mortality.”
“One should take all possible measures … to avoid desaturation and hypotensive episodes and also aggressively treat SAE and uremic encephalopathy in hopes of improving the outcomes,” added Dr. Varelas, who was not involved with the study.
Also commenting on the study, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University in New York, who was not associated with the research, said it “nicely distinguishes among the different causes of encephalopathy, including sepsis, hypoxia, and kidney failure … emphasizing just how sick these patients are.”
The study received no direct funding. Individual investigators were supported by grants from the National Institute on Aging and the National Institute of Neurological Disorders and Stroke. The investigators, Dr. Varelas, and Dr. Elkind have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Results of a retrospective study show that of almost 4,500 patients with COVID-19, 12% were diagnosed with TME. Of these, 78% developed encephalopathy immediately prior to hospital admission. Septic encephalopathy, hypoxic-ischemic encephalopathy (HIE), and uremia were the most common causes, although multiple causes were present in close to 80% of patients. TME was also associated with a 24% higher risk of in-hospital death.
“We found that close to one in eight patients who were hospitalized with COVID-19 had TME that was not attributed to the effects of sedatives, and that this is incredibly common among these patients who are critically ill” said lead author Jennifer A. Frontera, MD, New York University.
“The general principle of our findings is to be more aggressive in TME; and from a neurologist perspective, the way to do this is to eliminate the effects of sedation, which is a confounder,” she said.
The study was published online March 16 in Neurocritical Care.
Drilling down
“Many neurological complications of COVID-19 are sequelae of severe illness or secondary effects of multisystem organ failure, but our previous work identified TME as the most common neurological complication,” Dr. Frontera said.
Previous research investigating encephalopathy among patients with COVID-19 included patients who may have been sedated or have had a positive Confusion Assessment Method (CAM) result.
“A lot of the delirium literature is effectively heterogeneous because there are a number of patients who are on sedative medication that, if you could turn it off, these patients would return to normal. Some may have underlying neurological issues that can be addressed, but you can›t get to the bottom of this unless you turn off the sedation,” Dr. Frontera noted.
“We wanted to be specific and try to drill down to see what the underlying cause of the encephalopathy was,” she said.
The researchers retrospectively analyzed data on 4,491 patients (≥ 18 years old) with COVID-19 who were admitted to four New York City hospitals between March 1, 2020, and May 20, 2020. Of these, 559 (12%) with TME were compared with 3,932 patients without TME.
The researchers looked at index admissions and included patients who had:
- New changes in mental status or significant worsening of mental status (in patients with baseline abnormal mental status).
- Hyperglycemia or with transient focal neurologic deficits that resolved with glucose correction.
- An adequate washout of sedating medications (when relevant) prior to mental status assessment.
Potential etiologies included electrolyte abnormalities, organ failure, hypertensive encephalopathy, sepsis or active infection, fever, nutritional deficiency, and environmental injury.
Foreign environment
Most (78%) of the 559 patients diagnosed with TME had already developed encephalopathy immediately prior to hospital admission, the authors report. The most common etiologies of TME among hospitalized patients with COVID-19 are listed below.
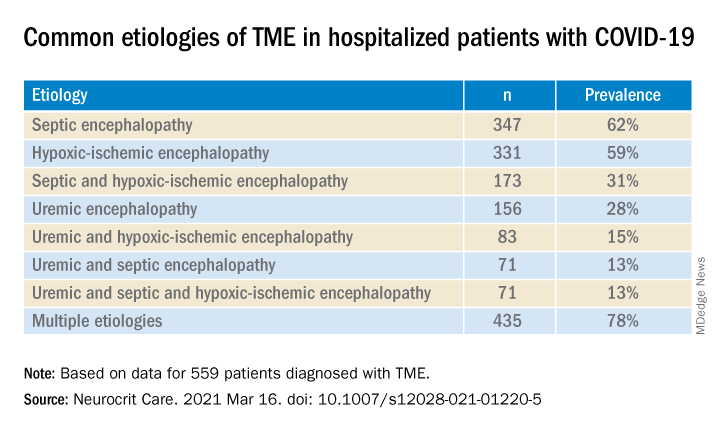
Compared with patients without TME, those with TME – (all Ps < .001):
- Were older (76 vs. 62 years).
- Had higher rates of dementia (27% vs. 3%).
- Had higher rates of psychiatric history (20% vs. 10%).
- Were more often intubated (37% vs. 20%).
- Had a longer length of hospital stay (7.9 vs. 6.0 days).
- Were less often discharged home (25% vs. 66%).
“It’s no surprise that older patients and people with dementia or psychiatric illness are predisposed to becoming encephalopathic,” said Dr. Frontera. “Being in a foreign environment, such as a hospital, or being sleep-deprived in the ICU is likely to make them more confused during their hospital stay.”
Delirium as a symptom
In-hospital mortality or discharge to hospice was considerably higher in the TME versus non-TME patients (44% vs. 18%, respectively).
When the researchers adjusted for confounders (age, sex, race, worse Sequential Organ Failure Assessment score during hospitalization, ventilator status, study week, hospital location, and ICU care level) and excluded patients receiving only comfort care, they found that TME was associated with a 24% increased risk of in-hospital death (30% in patients with TME vs. 16% in those without TME).
The highest mortality risk was associated with hypoxemia, with 42% of patients with HIE dying during hospitalization, compared with 16% of patients without HIE (adjusted hazard ratio 1.56; 95% confidence interval, 1.21-2.00; P = .001).
“Not all patients who are intubated require sedation, but there’s generally a lot of hesitation in reducing or stopping sedation in some patients,” Dr. Frontera observed.
She acknowledged there are “many extremely sick patients whom you can’t ventilate without sedation.”
Nevertheless, “delirium in and of itself does not cause death. It’s a symptom, not a disease, and we have to figure out what causes it. Delirium might not need to be sedated, and it’s more important to see what the causal problem is.”
Independent predictor of death
Commenting on the study, Panayiotis N. Varelas, MD, PhD, vice president of the Neurocritical Care Society, said the study “approached the TME issue better than previously, namely allowing time for sedatives to wear off to have a better sample of patients with this syndrome.”
Dr. Varelas, who is chairman of the department of neurology and professor of neurology at Albany (N.Y.) Medical College, emphasized that TME “is not benign and, in patients with COVID-19, it is an independent predictor of in-hospital mortality.”
“One should take all possible measures … to avoid desaturation and hypotensive episodes and also aggressively treat SAE and uremic encephalopathy in hopes of improving the outcomes,” added Dr. Varelas, who was not involved with the study.
Also commenting on the study, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University in New York, who was not associated with the research, said it “nicely distinguishes among the different causes of encephalopathy, including sepsis, hypoxia, and kidney failure … emphasizing just how sick these patients are.”
The study received no direct funding. Individual investigators were supported by grants from the National Institute on Aging and the National Institute of Neurological Disorders and Stroke. The investigators, Dr. Varelas, and Dr. Elkind have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows. Results of a retrospective study show that of almost 4,500 patients with COVID-19, 12% were diagnosed with TME. Of these, 78% developed encephalopathy immediately prior to hospital admission. Septic encephalopathy, hypoxic-ischemic encephalopathy (HIE), and uremia were the most common causes, although multiple causes were present in close to 80% of patients. TME was also associated with a 24% higher risk of in-hospital death.
“We found that close to one in eight patients who were hospitalized with COVID-19 had TME that was not attributed to the effects of sedatives, and that this is incredibly common among these patients who are critically ill” said lead author Jennifer A. Frontera, MD, New York University.
“The general principle of our findings is to be more aggressive in TME; and from a neurologist perspective, the way to do this is to eliminate the effects of sedation, which is a confounder,” she said.
The study was published online March 16 in Neurocritical Care.
Drilling down
“Many neurological complications of COVID-19 are sequelae of severe illness or secondary effects of multisystem organ failure, but our previous work identified TME as the most common neurological complication,” Dr. Frontera said.
Previous research investigating encephalopathy among patients with COVID-19 included patients who may have been sedated or have had a positive Confusion Assessment Method (CAM) result.
“A lot of the delirium literature is effectively heterogeneous because there are a number of patients who are on sedative medication that, if you could turn it off, these patients would return to normal. Some may have underlying neurological issues that can be addressed, but you can›t get to the bottom of this unless you turn off the sedation,” Dr. Frontera noted.
“We wanted to be specific and try to drill down to see what the underlying cause of the encephalopathy was,” she said.
The researchers retrospectively analyzed data on 4,491 patients (≥ 18 years old) with COVID-19 who were admitted to four New York City hospitals between March 1, 2020, and May 20, 2020. Of these, 559 (12%) with TME were compared with 3,932 patients without TME.
The researchers looked at index admissions and included patients who had:
- New changes in mental status or significant worsening of mental status (in patients with baseline abnormal mental status).
- Hyperglycemia or with transient focal neurologic deficits that resolved with glucose correction.
- An adequate washout of sedating medications (when relevant) prior to mental status assessment.
Potential etiologies included electrolyte abnormalities, organ failure, hypertensive encephalopathy, sepsis or active infection, fever, nutritional deficiency, and environmental injury.
Foreign environment
Most (78%) of the 559 patients diagnosed with TME had already developed encephalopathy immediately prior to hospital admission, the authors report. The most common etiologies of TME among hospitalized patients with COVID-19 are listed below.
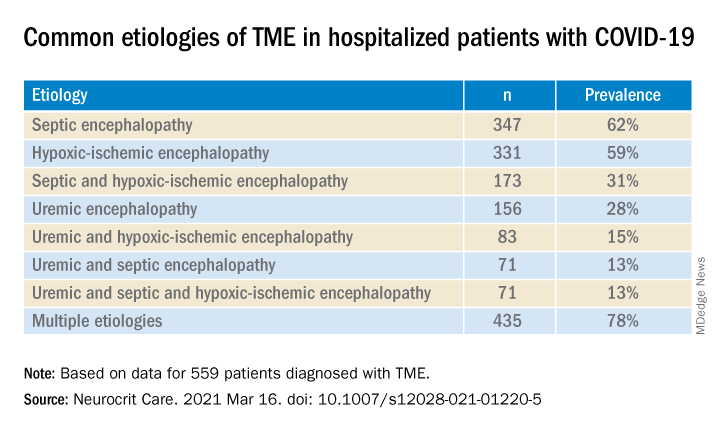
Compared with patients without TME, those with TME – (all Ps < .001):
- Were older (76 vs. 62 years).
- Had higher rates of dementia (27% vs. 3%).
- Had higher rates of psychiatric history (20% vs. 10%).
- Were more often intubated (37% vs. 20%).
- Had a longer length of hospital stay (7.9 vs. 6.0 days).
- Were less often discharged home (25% vs. 66%).
“It’s no surprise that older patients and people with dementia or psychiatric illness are predisposed to becoming encephalopathic,” said Dr. Frontera. “Being in a foreign environment, such as a hospital, or being sleep-deprived in the ICU is likely to make them more confused during their hospital stay.”
Delirium as a symptom
In-hospital mortality or discharge to hospice was considerably higher in the TME versus non-TME patients (44% vs. 18%, respectively).
When the researchers adjusted for confounders (age, sex, race, worse Sequential Organ Failure Assessment score during hospitalization, ventilator status, study week, hospital location, and ICU care level) and excluded patients receiving only comfort care, they found that TME was associated with a 24% increased risk of in-hospital death (30% in patients with TME vs. 16% in those without TME).
The highest mortality risk was associated with hypoxemia, with 42% of patients with HIE dying during hospitalization, compared with 16% of patients without HIE (adjusted hazard ratio 1.56; 95% confidence interval, 1.21-2.00; P = .001).
“Not all patients who are intubated require sedation, but there’s generally a lot of hesitation in reducing or stopping sedation in some patients,” Dr. Frontera observed.
She acknowledged there are “many extremely sick patients whom you can’t ventilate without sedation.”
Nevertheless, “delirium in and of itself does not cause death. It’s a symptom, not a disease, and we have to figure out what causes it. Delirium might not need to be sedated, and it’s more important to see what the causal problem is.”
Independent predictor of death
Commenting on the study, Panayiotis N. Varelas, MD, PhD, vice president of the Neurocritical Care Society, said the study “approached the TME issue better than previously, namely allowing time for sedatives to wear off to have a better sample of patients with this syndrome.”
Dr. Varelas, who is chairman of the department of neurology and professor of neurology at Albany (N.Y.) Medical College, emphasized that TME “is not benign and, in patients with COVID-19, it is an independent predictor of in-hospital mortality.”
“One should take all possible measures … to avoid desaturation and hypotensive episodes and also aggressively treat SAE and uremic encephalopathy in hopes of improving the outcomes,” added Dr. Varelas, who was not involved with the study.
Also commenting on the study, Mitchell Elkind, MD, professor of neurology and epidemiology at Columbia University in New York, who was not associated with the research, said it “nicely distinguishes among the different causes of encephalopathy, including sepsis, hypoxia, and kidney failure … emphasizing just how sick these patients are.”
The study received no direct funding. Individual investigators were supported by grants from the National Institute on Aging and the National Institute of Neurological Disorders and Stroke. The investigators, Dr. Varelas, and Dr. Elkind have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROCRITICAL CARE
New expert guidance on ketamine for resistant depression
An international panel of mood disorder experts has published guidance on how to safely and effectively use ketamine and esketamine to treat adults with treatment-resistant depression (TRD).
“Ketamine and esketamine are the first rapid-onset treatments for adults with TRD, and there was an international need for best-practice guidance on the deft and safe implementation of ketamine and esketamine at the point of care, as none previously existed,” first author Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, said in an interview.
“This need has only been amplified by the significant increase in the number of clinics and centers providing this treatment,” added Dr. McIntyre, head of the mood disorders psychopharmacology unit.
Their article was published online March 17 in the American Journal of Psychiatry.
Insufficient evidence of long-term efficacy
As reported by this news organization, the U.S. Food and Drug Administration (FDA) approved esketamine nasal spray (Spravato) for TRD in March 2019.
In August 2020, the FDA updated the approval to include adults with major depression and suicidal thoughts or actions.
To provide clinical guidance, Dr. McIntyre and colleagues synthesized the available literature on the efficacy, safety, and tolerability of ketamine and esketamine for TRD.
The evidence, they note, supports the rapid-onset (within 1-2 days) efficacy of esketamine and ketamine in TRD.
The strongest evidence of efficacy is for intranasal esketamine and intravenous ketamine. There is insufficient evidence for oral, subcutaneous, or intramuscular ketamine for TRD, they report.
Intranasal esketamine demonstrates efficacy, safety, and tolerability for up to 1 year in adults with TRD. Evidence for long-term efficacy, safety, and tolerability of intravenous ketamine for patients with TRD is insufficient, the group notes.
They also note that esketamine is approved in the United States for major depression in association with suicidal ideation or behavior and that it has been proven to reduce suicide completion.
Safety concerns with ketamine and esketamine identified in the literature include, but are not limited to, psychiatric, neurologic/cognitive, genitourinary, and hemodynamic effects.
Implementation checklist
The group has developed an “implementation checklist” for use of ketamine/esketamine in clinical practice.
Starting with patient selection, they note that appropriate patients are those with a confirmed diagnosis of TRD for whom psychosis and other conditions that would significantly affect the risk-benefit ratio have been ruled out.
They suggest that a physical examination and monitoring of vital signs be undertaken during treatment and during posttreatment surveillance. A urine drug screen should be considered if appropriate.
The group advises that esketamine and ketamine be administered only in settings with multidisciplinary personnel, including, but not limited to, those with expertise in the assessment of mood disorders.
Clinics should be equipped with appropriate cardiorespiratory monitoring and be capable of psychiatric assessment of dissociation and psychotomimetic effects.
Depressive symptoms should be measured, and the authors suggest assessing for anxiety, cognitive function, well-being, and psychosocial function.
Patients should be monitored immediately after treatment to ensure cardiorespiratory stability, clear sensorium, and attenuation of dissociative and psychotomimetic effects.
The United States and some other countries require a risk evaluation and mitigation strategy (REMS) when administering esketamine. Regarding the REMS, it is advised that all patients be monitored for a minimum of 2 hours before discharge.
Patients should arrange for reliable transportation for each appointment, and they should be advised not to operate motor vehicles or hazardous machinery without at least one night of sleep.
, only worsened by COVID-19,” said Dr. McIntyre.
“Clinicians of different professional backgrounds have been interested in ketamine/esketamine, and we are extraordinarily pleased to see our international guidelines published,” he added.
‘Extremely useful’
Reached for comment, Alan Schatzberg, MD, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said this document “puts a lot of information in one place as far as what we know and what we don’t know right now, and that’s helpful. I think it’s an attempt to have a kind of a somewhat objective review of the literature, and it’s in a good journal.”
The article, Dr. Schatzberg added, “could be extremely useful for someone who is considering whether ketamine is useful for a patient or what they can tell a patient about ketamine, that is, about how long they might need, is it going to work, will it continue to work, and the level of data we have either on benefits or side effects.”
The research had no specific funding. The original article contains a complete list of author disclosures. Dr. Schatzberg has received grant support from Janssen; has served as a consultant for Alkermes, Avanir, Brain Resource, Bracket, Compass, Delpor, Epiodyne, GLG, Jazz, Janssen Pharmaceuticals, Lundbeck/Takeda, McKinsey and Company, Merck, Myriad Genetics, Neuronetics, Owl Analytics, Pfizer, Sage, Sunovion, and Xhale; holds equity in Corcept (cofounder), Delpor, Dermira, Epiodyne, Gilead, Incyte Genetics, Intersect ENT, Madrigal, Merck, Owl Analytics, Seattle Genetics, Titan, and Xhale; and is listed as an inventor on patents for pharmacogenetics and antiglucocorticoid use in the prediction of antidepressant response.
A version of this article first appeared on Medscape.com.
An international panel of mood disorder experts has published guidance on how to safely and effectively use ketamine and esketamine to treat adults with treatment-resistant depression (TRD).
“Ketamine and esketamine are the first rapid-onset treatments for adults with TRD, and there was an international need for best-practice guidance on the deft and safe implementation of ketamine and esketamine at the point of care, as none previously existed,” first author Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, said in an interview.
“This need has only been amplified by the significant increase in the number of clinics and centers providing this treatment,” added Dr. McIntyre, head of the mood disorders psychopharmacology unit.
Their article was published online March 17 in the American Journal of Psychiatry.
Insufficient evidence of long-term efficacy
As reported by this news organization, the U.S. Food and Drug Administration (FDA) approved esketamine nasal spray (Spravato) for TRD in March 2019.
In August 2020, the FDA updated the approval to include adults with major depression and suicidal thoughts or actions.
To provide clinical guidance, Dr. McIntyre and colleagues synthesized the available literature on the efficacy, safety, and tolerability of ketamine and esketamine for TRD.
The evidence, they note, supports the rapid-onset (within 1-2 days) efficacy of esketamine and ketamine in TRD.
The strongest evidence of efficacy is for intranasal esketamine and intravenous ketamine. There is insufficient evidence for oral, subcutaneous, or intramuscular ketamine for TRD, they report.
Intranasal esketamine demonstrates efficacy, safety, and tolerability for up to 1 year in adults with TRD. Evidence for long-term efficacy, safety, and tolerability of intravenous ketamine for patients with TRD is insufficient, the group notes.
They also note that esketamine is approved in the United States for major depression in association with suicidal ideation or behavior and that it has been proven to reduce suicide completion.
Safety concerns with ketamine and esketamine identified in the literature include, but are not limited to, psychiatric, neurologic/cognitive, genitourinary, and hemodynamic effects.
Implementation checklist
The group has developed an “implementation checklist” for use of ketamine/esketamine in clinical practice.
Starting with patient selection, they note that appropriate patients are those with a confirmed diagnosis of TRD for whom psychosis and other conditions that would significantly affect the risk-benefit ratio have been ruled out.
They suggest that a physical examination and monitoring of vital signs be undertaken during treatment and during posttreatment surveillance. A urine drug screen should be considered if appropriate.
The group advises that esketamine and ketamine be administered only in settings with multidisciplinary personnel, including, but not limited to, those with expertise in the assessment of mood disorders.
Clinics should be equipped with appropriate cardiorespiratory monitoring and be capable of psychiatric assessment of dissociation and psychotomimetic effects.
Depressive symptoms should be measured, and the authors suggest assessing for anxiety, cognitive function, well-being, and psychosocial function.
Patients should be monitored immediately after treatment to ensure cardiorespiratory stability, clear sensorium, and attenuation of dissociative and psychotomimetic effects.
The United States and some other countries require a risk evaluation and mitigation strategy (REMS) when administering esketamine. Regarding the REMS, it is advised that all patients be monitored for a minimum of 2 hours before discharge.
Patients should arrange for reliable transportation for each appointment, and they should be advised not to operate motor vehicles or hazardous machinery without at least one night of sleep.
, only worsened by COVID-19,” said Dr. McIntyre.
“Clinicians of different professional backgrounds have been interested in ketamine/esketamine, and we are extraordinarily pleased to see our international guidelines published,” he added.
‘Extremely useful’
Reached for comment, Alan Schatzberg, MD, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said this document “puts a lot of information in one place as far as what we know and what we don’t know right now, and that’s helpful. I think it’s an attempt to have a kind of a somewhat objective review of the literature, and it’s in a good journal.”
The article, Dr. Schatzberg added, “could be extremely useful for someone who is considering whether ketamine is useful for a patient or what they can tell a patient about ketamine, that is, about how long they might need, is it going to work, will it continue to work, and the level of data we have either on benefits or side effects.”
The research had no specific funding. The original article contains a complete list of author disclosures. Dr. Schatzberg has received grant support from Janssen; has served as a consultant for Alkermes, Avanir, Brain Resource, Bracket, Compass, Delpor, Epiodyne, GLG, Jazz, Janssen Pharmaceuticals, Lundbeck/Takeda, McKinsey and Company, Merck, Myriad Genetics, Neuronetics, Owl Analytics, Pfizer, Sage, Sunovion, and Xhale; holds equity in Corcept (cofounder), Delpor, Dermira, Epiodyne, Gilead, Incyte Genetics, Intersect ENT, Madrigal, Merck, Owl Analytics, Seattle Genetics, Titan, and Xhale; and is listed as an inventor on patents for pharmacogenetics and antiglucocorticoid use in the prediction of antidepressant response.
A version of this article first appeared on Medscape.com.
An international panel of mood disorder experts has published guidance on how to safely and effectively use ketamine and esketamine to treat adults with treatment-resistant depression (TRD).
“Ketamine and esketamine are the first rapid-onset treatments for adults with TRD, and there was an international need for best-practice guidance on the deft and safe implementation of ketamine and esketamine at the point of care, as none previously existed,” first author Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, said in an interview.
“This need has only been amplified by the significant increase in the number of clinics and centers providing this treatment,” added Dr. McIntyre, head of the mood disorders psychopharmacology unit.
Their article was published online March 17 in the American Journal of Psychiatry.
Insufficient evidence of long-term efficacy
As reported by this news organization, the U.S. Food and Drug Administration (FDA) approved esketamine nasal spray (Spravato) for TRD in March 2019.
In August 2020, the FDA updated the approval to include adults with major depression and suicidal thoughts or actions.
To provide clinical guidance, Dr. McIntyre and colleagues synthesized the available literature on the efficacy, safety, and tolerability of ketamine and esketamine for TRD.
The evidence, they note, supports the rapid-onset (within 1-2 days) efficacy of esketamine and ketamine in TRD.
The strongest evidence of efficacy is for intranasal esketamine and intravenous ketamine. There is insufficient evidence for oral, subcutaneous, or intramuscular ketamine for TRD, they report.
Intranasal esketamine demonstrates efficacy, safety, and tolerability for up to 1 year in adults with TRD. Evidence for long-term efficacy, safety, and tolerability of intravenous ketamine for patients with TRD is insufficient, the group notes.
They also note that esketamine is approved in the United States for major depression in association with suicidal ideation or behavior and that it has been proven to reduce suicide completion.
Safety concerns with ketamine and esketamine identified in the literature include, but are not limited to, psychiatric, neurologic/cognitive, genitourinary, and hemodynamic effects.
Implementation checklist
The group has developed an “implementation checklist” for use of ketamine/esketamine in clinical practice.
Starting with patient selection, they note that appropriate patients are those with a confirmed diagnosis of TRD for whom psychosis and other conditions that would significantly affect the risk-benefit ratio have been ruled out.
They suggest that a physical examination and monitoring of vital signs be undertaken during treatment and during posttreatment surveillance. A urine drug screen should be considered if appropriate.
The group advises that esketamine and ketamine be administered only in settings with multidisciplinary personnel, including, but not limited to, those with expertise in the assessment of mood disorders.
Clinics should be equipped with appropriate cardiorespiratory monitoring and be capable of psychiatric assessment of dissociation and psychotomimetic effects.
Depressive symptoms should be measured, and the authors suggest assessing for anxiety, cognitive function, well-being, and psychosocial function.
Patients should be monitored immediately after treatment to ensure cardiorespiratory stability, clear sensorium, and attenuation of dissociative and psychotomimetic effects.
The United States and some other countries require a risk evaluation and mitigation strategy (REMS) when administering esketamine. Regarding the REMS, it is advised that all patients be monitored for a minimum of 2 hours before discharge.
Patients should arrange for reliable transportation for each appointment, and they should be advised not to operate motor vehicles or hazardous machinery without at least one night of sleep.
, only worsened by COVID-19,” said Dr. McIntyre.
“Clinicians of different professional backgrounds have been interested in ketamine/esketamine, and we are extraordinarily pleased to see our international guidelines published,” he added.
‘Extremely useful’
Reached for comment, Alan Schatzberg, MD, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said this document “puts a lot of information in one place as far as what we know and what we don’t know right now, and that’s helpful. I think it’s an attempt to have a kind of a somewhat objective review of the literature, and it’s in a good journal.”
The article, Dr. Schatzberg added, “could be extremely useful for someone who is considering whether ketamine is useful for a patient or what they can tell a patient about ketamine, that is, about how long they might need, is it going to work, will it continue to work, and the level of data we have either on benefits or side effects.”
The research had no specific funding. The original article contains a complete list of author disclosures. Dr. Schatzberg has received grant support from Janssen; has served as a consultant for Alkermes, Avanir, Brain Resource, Bracket, Compass, Delpor, Epiodyne, GLG, Jazz, Janssen Pharmaceuticals, Lundbeck/Takeda, McKinsey and Company, Merck, Myriad Genetics, Neuronetics, Owl Analytics, Pfizer, Sage, Sunovion, and Xhale; holds equity in Corcept (cofounder), Delpor, Dermira, Epiodyne, Gilead, Incyte Genetics, Intersect ENT, Madrigal, Merck, Owl Analytics, Seattle Genetics, Titan, and Xhale; and is listed as an inventor on patents for pharmacogenetics and antiglucocorticoid use in the prediction of antidepressant response.
A version of this article first appeared on Medscape.com.
A paleolithic raw bar, and the human brush with extinction
This essay is adapted from the newly released book, “A History of the Human Brain: From the Sea Sponge to CRISPR, How Our Brain Evolved.”
“He was a bold man that first ate an oyster.” – Jonathan Swift
That man or, just as likely, that woman, may have done so out of necessity. It was either eat this glistening, gray blob of briny goo or perish.
Beginning 190,000 years ago, a glacial age we identify today as Marine Isotope Stage 6, or MIS6, had set in, cooling and drying out much of the planet. There was widespread drought, leaving the African plains a harsher, more barren substrate for survival – an arena of competition, desperation, and starvation for many species, including ours. Some estimates have the sapiens population dipping to just a few hundred people during MIS6. Like other apes today, we were an endangered species. But through some nexus of intelligence, ecological exploitation, and luck, we managed. Anthropologists argue over what part of Africa would’ve been hospitable enough to rescue sapiens from Darwinian oblivion. Arizona State University archaeologist Curtis Marean, PhD, believes the continent’s southern shore is a good candidate.
For 2 decades, Dr. Marean has overseen excavations at a site called Pinnacle Point on the South African coast. The region has over 9,000 plant species, including the world’s most diverse population of geophytes, plants with underground energy-storage organs such as bulbs, tubers, and rhizomes. These subterranean stores are rich in calories and carbohydrates, and, by virtue of being buried, are protected from most other species (save the occasional tool-wielding chimpanzee). They are also adapted to cold climates and, when cooked, easily digested. All in all, a coup for hunter-gatherers.
The other enticement at Pinnacle Point could be found with a few easy steps toward the sea. Mollusks. Geological samples from MIS6 show South Africa’s shores were packed with mussels, oysters, clams, and a variety of sea snails. We almost certainly turned to them for nutrition.
Dr. Marean’s research suggests that, sometime around 160,000 years ago, at least one group of sapiens began supplementing their terrestrial diet by exploiting the region’s rich shellfish beds. This is the oldest evidence to date of humans consistently feasting on seafood – easy, predictable, immobile calories. No hunting required. As inland Africa dried up, learning to shuck mussels and oysters was a key adaptation to coastal living, one that supported our later migration out of the continent.
Dr. Marean believes the change in behavior was possible thanks to our already keen brains, which supported an ability to track tides, especially spring tides. Spring tides occur twice a month with each new and full moon and result in the greatest difference between high and low tidewaters. The people of Pinnacle Point learned to exploit this cycle. “By tracking tides, we would have had easy, reliable access to high-quality proteins and fats from shellfish every 2 weeks as the ocean receded,” he says. “Whereas you can’t rely on land animals to always be in the same place at the same time.” Work by Jan De Vynck, PhD, a professor at Nelson Mandela University in South Africa, supports this idea, showing that foraging shellfish beds under optimal tidal conditions can yield a staggering 3,500 calories per hour!
“I don’t know if we owe our existence to seafood, but it was certainly important for the population [that Dr.] Curtis studies. That place is full of mussels,” said Ian Tattersall, PhD, curator emeritus with the American Museum of Natural History in New York.
“And I like the idea that during a population bottleneck we got creative and learned how to focus on marine resources.” Innovations, Dr. Tattersall explained, typically occur in small, fixed populations. Large populations have too much genetic inertia to support radical innovation; the status quo is enough to survive. “If you’re looking for evolutionary innovation, you have to look at smaller groups.”
MIS6 wasn’t the only near-extinction in our past. During the Pleistocene epoch, roughly 2.5 million to 12,000 years ago, humans tended to maintain a small population, hovering around a million and later growing to maybe 8 million at most. Periodically, our numbers dipped as climate shifts, natural disasters, and food shortages brought us dangerously close to extinction. Modern humans are descended from the hearty survivors of these bottlenecks.
One especially dire stretch occurred around 1 million years ago. Our effective population (the number of breeding individuals) shriveled to around 18,000, smaller than that of other apes at the time. Worse, our genetic diversity – the insurance policy on evolutionary success and the ability to adapt – plummeted. A similar near extinction may have occurred around 75,000 years ago, the result of a massive volcanic eruption in Sumatra.
Our smarts and adaptability helped us endure these tough times – omnivorism helped us weather scarcity.
A sea of vitamins
Both Dr. Marean and Dr. Tattersall agree that the sapiens hanging on in southern Africa couldn’t have lived entirely on shellfish.
Most likely they also spent time hunting and foraging roots inland, making pilgrimages to the sea during spring tides. Dr. Marean believes coastal cuisine may have allowed a paltry human population to hang on until climate change led to more hospitable terrain. He’s not entirely sold on the idea that marine life was necessarily a driver of human brain evolution.
By the time we incorporated seafood into our diets we were already smart, our brains shaped through millennia of selection for intelligence. “Being a marine forager requires a certain degree of sophisticated smarts,” he said. It requires tracking the lunar cycle and planning excursions to the coast at the right times. Shellfish were simply another source of calories.
Unless you ask Michael Crawford.
Dr. Crawford is a professor at Imperial College London and a strident believer that our brains are those of sea creatures. Sort of.
In 1972, he copublished a paper concluding that the brain is structurally and functionally dependent on an omega-3 fatty acid called docosahexaenoic acid, or DHA. The human brain is composed of nearly 60% fat, so it’s not surprising that certain fats are important to brain health. Nearly 50 years after Dr. Crawford’s study, omega-3 supplements are now a multi-billion-dollar business.
Omega-3s, or more formally, omega-3 polyunsaturated fatty acids (PUFAs), are essential fats, meaning they aren’t produced by the body and must be obtained through diet. We get them from vegetable oils, nuts, seeds, and animals that eat such things. But take an informal poll, and you’ll find most people probably associate omega fatty acids with fish and other seafood.
In the 1970s and 1980s, scientists took notice of the low rates of heart disease in Eskimo communities. Research linked their cardiovascular health to a high-fish diet (though fish cannot produce omega-3s, they source them from algae), and eventually the medical and scientific communities began to rethink fat. Study after study found omega-3 fatty acids to be healthy. They were linked with a lower risk for heart disease and overall mortality. All those decades of parents forcing various fish oils on their grimacing children now had some science behind them. There is such a thing as a good fat.
, especially DHA and eicosapentaenoic acid, or EPA. Omega fats provide structure to neuronal cell membranes and are crucial in neuron-to-neuron communication. They increase levels of a protein called brain-derived neurotrophic factor (BDNF), which supports neuronal growth and survival. A growing body of evidence shows omega-3 supplementation may slow down the process of neurodegeneration, the gradual deterioration of the brain that results in Alzheimer’s disease and other forms of dementia.
Popping a daily omega-3 supplement or, better still, eating a seafood-rich diet, may increase blood flow to the brain. In 2019, the International Society for Nutritional Psychiatry Research recommended omega-3s as an adjunct therapy for major depressive disorder. PUFAs appear to reduce the risk for and severity of mood disorders such as depression and to boost attention in children with ADHD as effectively as drug therapies.
Many researchers claim there would’ve been plenty of DHA available on land to support early humans, and marine foods were just one of many sources.
Not Dr. Crawford.
He believes that brain development and function are not only dependent on DHA but, in fact, DHA sourced from the sea was critical to mammalian brain evolution. “The animal brain evolved 600 million years ago in the ocean and was dependent on DHA, as well as compounds such as iodine, which is also in short supply on land,” he said. “To build a brain, you need these building blocks, which were rich at sea and on rocky shores.”
Dr. Crawford cites his early biochemical work showing DHA isn’t readily accessible from the muscle tissue of land animals. Using DHA tagged with a radioactive isotope, he and his colleagues in the 1970s found that “ready-made” DHA, like that found in shellfish, is incorporated into the developing rat brain with 10-fold greater efficiency than plant- and land animal–sourced DHA, where it exists as its metabolic precursor alpha-linolenic acid. “I’m afraid the idea that ample DHA was available from the fats of animals on the savanna is just not true,” he disputes. According to Dr. Crawford, our tiny, wormlike ancestors were able to evolve primitive nervous systems and flit through the silt thanks to the abundance of healthy fat to be had by living in the ocean and consuming algae.
For over 40 years, Dr. Crawford has argued that rising rates of mental illness are a result of post–World War II dietary changes, especially the move toward land-sourced food and the medical community’s subsequent support of low-fat diets. He feels that omega-3s from seafood were critical to humans’ rapid neural march toward higher cognition, and are therefore critical to brain health. “The continued rise in mental illness is an incredibly important threat to mankind and society, and moving away from marine foods is a major contributor,” said Dr. Crawford.
University of Sherbrooke (Que.) physiology professor Stephen Cunnane, PhD, tends to agree that aquatically sourced nutrients were crucial to human evolution. It’s the importance of coastal living he’s not sure about. He believes hominins would’ve incorporated fish from lakes and rivers into their diet for millions of years. In his view, it wasn’t just omega-3s that contributed to our big brains, but a cluster of nutrients found in fish: iodine, iron, zinc, copper, and selenium among them. “I think DHA was hugely important to our evolution and brain health but I don’t think it was a magic bullet all by itself,” he said. “Numerous other nutrients found in fish and shellfish were very probably important, too, and are now known to be good for the brain.”
Dr. Marean agrees. “Accessing the marine food chain could have had a huge impact on fertility, survival, and overall health, including brain health, in part, due to the high return on omega-3 fatty acids and other nutrients.” But, he speculates, before MIS6, hominins would have had access to plenty of brain-healthy terrestrial nutrition, including meat from animals that consumed omega-3–rich plants and grains.
Dr. Cunnane agrees with Dr. Marean to a degree. He’s confident that higher intelligence evolved gradually over millions of years as mutations inching the cognitive needle forward conferred survival and reproductive advantages – but he maintains that certain advantages like, say, being able to shuck an oyster, allowed an already intelligent brain to thrive.
Foraging marine life in the waters off of Africa likely played an important role in keeping some of our ancestors alive and supported our subsequent propagation throughout the world. By this point, the human brain was already a marvel of consciousness and computing, not too dissimilar to the one we carry around today.
In all likelihood, Pleistocene humans probably got their nutrients and calories wherever they could. If we lived inland, we hunted. Maybe we speared the occasional catfish. We sourced nutrients from fruits, leaves, and nuts. A few times a month, those of us near the coast enjoyed a feast of mussels and oysters.
Dr. Stetka is an editorial director at Medscape.com, a former neuroscience researcher, and a nonpracticing physician. A version of this article first appeared on Medscape.
This essay is adapted from the newly released book, “A History of the Human Brain: From the Sea Sponge to CRISPR, How Our Brain Evolved.”
“He was a bold man that first ate an oyster.” – Jonathan Swift
That man or, just as likely, that woman, may have done so out of necessity. It was either eat this glistening, gray blob of briny goo or perish.
Beginning 190,000 years ago, a glacial age we identify today as Marine Isotope Stage 6, or MIS6, had set in, cooling and drying out much of the planet. There was widespread drought, leaving the African plains a harsher, more barren substrate for survival – an arena of competition, desperation, and starvation for many species, including ours. Some estimates have the sapiens population dipping to just a few hundred people during MIS6. Like other apes today, we were an endangered species. But through some nexus of intelligence, ecological exploitation, and luck, we managed. Anthropologists argue over what part of Africa would’ve been hospitable enough to rescue sapiens from Darwinian oblivion. Arizona State University archaeologist Curtis Marean, PhD, believes the continent’s southern shore is a good candidate.
For 2 decades, Dr. Marean has overseen excavations at a site called Pinnacle Point on the South African coast. The region has over 9,000 plant species, including the world’s most diverse population of geophytes, plants with underground energy-storage organs such as bulbs, tubers, and rhizomes. These subterranean stores are rich in calories and carbohydrates, and, by virtue of being buried, are protected from most other species (save the occasional tool-wielding chimpanzee). They are also adapted to cold climates and, when cooked, easily digested. All in all, a coup for hunter-gatherers.
The other enticement at Pinnacle Point could be found with a few easy steps toward the sea. Mollusks. Geological samples from MIS6 show South Africa’s shores were packed with mussels, oysters, clams, and a variety of sea snails. We almost certainly turned to them for nutrition.
Dr. Marean’s research suggests that, sometime around 160,000 years ago, at least one group of sapiens began supplementing their terrestrial diet by exploiting the region’s rich shellfish beds. This is the oldest evidence to date of humans consistently feasting on seafood – easy, predictable, immobile calories. No hunting required. As inland Africa dried up, learning to shuck mussels and oysters was a key adaptation to coastal living, one that supported our later migration out of the continent.
Dr. Marean believes the change in behavior was possible thanks to our already keen brains, which supported an ability to track tides, especially spring tides. Spring tides occur twice a month with each new and full moon and result in the greatest difference between high and low tidewaters. The people of Pinnacle Point learned to exploit this cycle. “By tracking tides, we would have had easy, reliable access to high-quality proteins and fats from shellfish every 2 weeks as the ocean receded,” he says. “Whereas you can’t rely on land animals to always be in the same place at the same time.” Work by Jan De Vynck, PhD, a professor at Nelson Mandela University in South Africa, supports this idea, showing that foraging shellfish beds under optimal tidal conditions can yield a staggering 3,500 calories per hour!
“I don’t know if we owe our existence to seafood, but it was certainly important for the population [that Dr.] Curtis studies. That place is full of mussels,” said Ian Tattersall, PhD, curator emeritus with the American Museum of Natural History in New York.
“And I like the idea that during a population bottleneck we got creative and learned how to focus on marine resources.” Innovations, Dr. Tattersall explained, typically occur in small, fixed populations. Large populations have too much genetic inertia to support radical innovation; the status quo is enough to survive. “If you’re looking for evolutionary innovation, you have to look at smaller groups.”
MIS6 wasn’t the only near-extinction in our past. During the Pleistocene epoch, roughly 2.5 million to 12,000 years ago, humans tended to maintain a small population, hovering around a million and later growing to maybe 8 million at most. Periodically, our numbers dipped as climate shifts, natural disasters, and food shortages brought us dangerously close to extinction. Modern humans are descended from the hearty survivors of these bottlenecks.
One especially dire stretch occurred around 1 million years ago. Our effective population (the number of breeding individuals) shriveled to around 18,000, smaller than that of other apes at the time. Worse, our genetic diversity – the insurance policy on evolutionary success and the ability to adapt – plummeted. A similar near extinction may have occurred around 75,000 years ago, the result of a massive volcanic eruption in Sumatra.
Our smarts and adaptability helped us endure these tough times – omnivorism helped us weather scarcity.
A sea of vitamins
Both Dr. Marean and Dr. Tattersall agree that the sapiens hanging on in southern Africa couldn’t have lived entirely on shellfish.
Most likely they also spent time hunting and foraging roots inland, making pilgrimages to the sea during spring tides. Dr. Marean believes coastal cuisine may have allowed a paltry human population to hang on until climate change led to more hospitable terrain. He’s not entirely sold on the idea that marine life was necessarily a driver of human brain evolution.
By the time we incorporated seafood into our diets we were already smart, our brains shaped through millennia of selection for intelligence. “Being a marine forager requires a certain degree of sophisticated smarts,” he said. It requires tracking the lunar cycle and planning excursions to the coast at the right times. Shellfish were simply another source of calories.
Unless you ask Michael Crawford.
Dr. Crawford is a professor at Imperial College London and a strident believer that our brains are those of sea creatures. Sort of.
In 1972, he copublished a paper concluding that the brain is structurally and functionally dependent on an omega-3 fatty acid called docosahexaenoic acid, or DHA. The human brain is composed of nearly 60% fat, so it’s not surprising that certain fats are important to brain health. Nearly 50 years after Dr. Crawford’s study, omega-3 supplements are now a multi-billion-dollar business.
Omega-3s, or more formally, omega-3 polyunsaturated fatty acids (PUFAs), are essential fats, meaning they aren’t produced by the body and must be obtained through diet. We get them from vegetable oils, nuts, seeds, and animals that eat such things. But take an informal poll, and you’ll find most people probably associate omega fatty acids with fish and other seafood.
In the 1970s and 1980s, scientists took notice of the low rates of heart disease in Eskimo communities. Research linked their cardiovascular health to a high-fish diet (though fish cannot produce omega-3s, they source them from algae), and eventually the medical and scientific communities began to rethink fat. Study after study found omega-3 fatty acids to be healthy. They were linked with a lower risk for heart disease and overall mortality. All those decades of parents forcing various fish oils on their grimacing children now had some science behind them. There is such a thing as a good fat.
, especially DHA and eicosapentaenoic acid, or EPA. Omega fats provide structure to neuronal cell membranes and are crucial in neuron-to-neuron communication. They increase levels of a protein called brain-derived neurotrophic factor (BDNF), which supports neuronal growth and survival. A growing body of evidence shows omega-3 supplementation may slow down the process of neurodegeneration, the gradual deterioration of the brain that results in Alzheimer’s disease and other forms of dementia.
Popping a daily omega-3 supplement or, better still, eating a seafood-rich diet, may increase blood flow to the brain. In 2019, the International Society for Nutritional Psychiatry Research recommended omega-3s as an adjunct therapy for major depressive disorder. PUFAs appear to reduce the risk for and severity of mood disorders such as depression and to boost attention in children with ADHD as effectively as drug therapies.
Many researchers claim there would’ve been plenty of DHA available on land to support early humans, and marine foods were just one of many sources.
Not Dr. Crawford.
He believes that brain development and function are not only dependent on DHA but, in fact, DHA sourced from the sea was critical to mammalian brain evolution. “The animal brain evolved 600 million years ago in the ocean and was dependent on DHA, as well as compounds such as iodine, which is also in short supply on land,” he said. “To build a brain, you need these building blocks, which were rich at sea and on rocky shores.”
Dr. Crawford cites his early biochemical work showing DHA isn’t readily accessible from the muscle tissue of land animals. Using DHA tagged with a radioactive isotope, he and his colleagues in the 1970s found that “ready-made” DHA, like that found in shellfish, is incorporated into the developing rat brain with 10-fold greater efficiency than plant- and land animal–sourced DHA, where it exists as its metabolic precursor alpha-linolenic acid. “I’m afraid the idea that ample DHA was available from the fats of animals on the savanna is just not true,” he disputes. According to Dr. Crawford, our tiny, wormlike ancestors were able to evolve primitive nervous systems and flit through the silt thanks to the abundance of healthy fat to be had by living in the ocean and consuming algae.
For over 40 years, Dr. Crawford has argued that rising rates of mental illness are a result of post–World War II dietary changes, especially the move toward land-sourced food and the medical community’s subsequent support of low-fat diets. He feels that omega-3s from seafood were critical to humans’ rapid neural march toward higher cognition, and are therefore critical to brain health. “The continued rise in mental illness is an incredibly important threat to mankind and society, and moving away from marine foods is a major contributor,” said Dr. Crawford.
University of Sherbrooke (Que.) physiology professor Stephen Cunnane, PhD, tends to agree that aquatically sourced nutrients were crucial to human evolution. It’s the importance of coastal living he’s not sure about. He believes hominins would’ve incorporated fish from lakes and rivers into their diet for millions of years. In his view, it wasn’t just omega-3s that contributed to our big brains, but a cluster of nutrients found in fish: iodine, iron, zinc, copper, and selenium among them. “I think DHA was hugely important to our evolution and brain health but I don’t think it was a magic bullet all by itself,” he said. “Numerous other nutrients found in fish and shellfish were very probably important, too, and are now known to be good for the brain.”
Dr. Marean agrees. “Accessing the marine food chain could have had a huge impact on fertility, survival, and overall health, including brain health, in part, due to the high return on omega-3 fatty acids and other nutrients.” But, he speculates, before MIS6, hominins would have had access to plenty of brain-healthy terrestrial nutrition, including meat from animals that consumed omega-3–rich plants and grains.
Dr. Cunnane agrees with Dr. Marean to a degree. He’s confident that higher intelligence evolved gradually over millions of years as mutations inching the cognitive needle forward conferred survival and reproductive advantages – but he maintains that certain advantages like, say, being able to shuck an oyster, allowed an already intelligent brain to thrive.
Foraging marine life in the waters off of Africa likely played an important role in keeping some of our ancestors alive and supported our subsequent propagation throughout the world. By this point, the human brain was already a marvel of consciousness and computing, not too dissimilar to the one we carry around today.
In all likelihood, Pleistocene humans probably got their nutrients and calories wherever they could. If we lived inland, we hunted. Maybe we speared the occasional catfish. We sourced nutrients from fruits, leaves, and nuts. A few times a month, those of us near the coast enjoyed a feast of mussels and oysters.
Dr. Stetka is an editorial director at Medscape.com, a former neuroscience researcher, and a nonpracticing physician. A version of this article first appeared on Medscape.
This essay is adapted from the newly released book, “A History of the Human Brain: From the Sea Sponge to CRISPR, How Our Brain Evolved.”
“He was a bold man that first ate an oyster.” – Jonathan Swift
That man or, just as likely, that woman, may have done so out of necessity. It was either eat this glistening, gray blob of briny goo or perish.
Beginning 190,000 years ago, a glacial age we identify today as Marine Isotope Stage 6, or MIS6, had set in, cooling and drying out much of the planet. There was widespread drought, leaving the African plains a harsher, more barren substrate for survival – an arena of competition, desperation, and starvation for many species, including ours. Some estimates have the sapiens population dipping to just a few hundred people during MIS6. Like other apes today, we were an endangered species. But through some nexus of intelligence, ecological exploitation, and luck, we managed. Anthropologists argue over what part of Africa would’ve been hospitable enough to rescue sapiens from Darwinian oblivion. Arizona State University archaeologist Curtis Marean, PhD, believes the continent’s southern shore is a good candidate.
For 2 decades, Dr. Marean has overseen excavations at a site called Pinnacle Point on the South African coast. The region has over 9,000 plant species, including the world’s most diverse population of geophytes, plants with underground energy-storage organs such as bulbs, tubers, and rhizomes. These subterranean stores are rich in calories and carbohydrates, and, by virtue of being buried, are protected from most other species (save the occasional tool-wielding chimpanzee). They are also adapted to cold climates and, when cooked, easily digested. All in all, a coup for hunter-gatherers.
The other enticement at Pinnacle Point could be found with a few easy steps toward the sea. Mollusks. Geological samples from MIS6 show South Africa’s shores were packed with mussels, oysters, clams, and a variety of sea snails. We almost certainly turned to them for nutrition.
Dr. Marean’s research suggests that, sometime around 160,000 years ago, at least one group of sapiens began supplementing their terrestrial diet by exploiting the region’s rich shellfish beds. This is the oldest evidence to date of humans consistently feasting on seafood – easy, predictable, immobile calories. No hunting required. As inland Africa dried up, learning to shuck mussels and oysters was a key adaptation to coastal living, one that supported our later migration out of the continent.
Dr. Marean believes the change in behavior was possible thanks to our already keen brains, which supported an ability to track tides, especially spring tides. Spring tides occur twice a month with each new and full moon and result in the greatest difference between high and low tidewaters. The people of Pinnacle Point learned to exploit this cycle. “By tracking tides, we would have had easy, reliable access to high-quality proteins and fats from shellfish every 2 weeks as the ocean receded,” he says. “Whereas you can’t rely on land animals to always be in the same place at the same time.” Work by Jan De Vynck, PhD, a professor at Nelson Mandela University in South Africa, supports this idea, showing that foraging shellfish beds under optimal tidal conditions can yield a staggering 3,500 calories per hour!
“I don’t know if we owe our existence to seafood, but it was certainly important for the population [that Dr.] Curtis studies. That place is full of mussels,” said Ian Tattersall, PhD, curator emeritus with the American Museum of Natural History in New York.
“And I like the idea that during a population bottleneck we got creative and learned how to focus on marine resources.” Innovations, Dr. Tattersall explained, typically occur in small, fixed populations. Large populations have too much genetic inertia to support radical innovation; the status quo is enough to survive. “If you’re looking for evolutionary innovation, you have to look at smaller groups.”
MIS6 wasn’t the only near-extinction in our past. During the Pleistocene epoch, roughly 2.5 million to 12,000 years ago, humans tended to maintain a small population, hovering around a million and later growing to maybe 8 million at most. Periodically, our numbers dipped as climate shifts, natural disasters, and food shortages brought us dangerously close to extinction. Modern humans are descended from the hearty survivors of these bottlenecks.
One especially dire stretch occurred around 1 million years ago. Our effective population (the number of breeding individuals) shriveled to around 18,000, smaller than that of other apes at the time. Worse, our genetic diversity – the insurance policy on evolutionary success and the ability to adapt – plummeted. A similar near extinction may have occurred around 75,000 years ago, the result of a massive volcanic eruption in Sumatra.
Our smarts and adaptability helped us endure these tough times – omnivorism helped us weather scarcity.
A sea of vitamins
Both Dr. Marean and Dr. Tattersall agree that the sapiens hanging on in southern Africa couldn’t have lived entirely on shellfish.
Most likely they also spent time hunting and foraging roots inland, making pilgrimages to the sea during spring tides. Dr. Marean believes coastal cuisine may have allowed a paltry human population to hang on until climate change led to more hospitable terrain. He’s not entirely sold on the idea that marine life was necessarily a driver of human brain evolution.
By the time we incorporated seafood into our diets we were already smart, our brains shaped through millennia of selection for intelligence. “Being a marine forager requires a certain degree of sophisticated smarts,” he said. It requires tracking the lunar cycle and planning excursions to the coast at the right times. Shellfish were simply another source of calories.
Unless you ask Michael Crawford.
Dr. Crawford is a professor at Imperial College London and a strident believer that our brains are those of sea creatures. Sort of.
In 1972, he copublished a paper concluding that the brain is structurally and functionally dependent on an omega-3 fatty acid called docosahexaenoic acid, or DHA. The human brain is composed of nearly 60% fat, so it’s not surprising that certain fats are important to brain health. Nearly 50 years after Dr. Crawford’s study, omega-3 supplements are now a multi-billion-dollar business.
Omega-3s, or more formally, omega-3 polyunsaturated fatty acids (PUFAs), are essential fats, meaning they aren’t produced by the body and must be obtained through diet. We get them from vegetable oils, nuts, seeds, and animals that eat such things. But take an informal poll, and you’ll find most people probably associate omega fatty acids with fish and other seafood.
In the 1970s and 1980s, scientists took notice of the low rates of heart disease in Eskimo communities. Research linked their cardiovascular health to a high-fish diet (though fish cannot produce omega-3s, they source them from algae), and eventually the medical and scientific communities began to rethink fat. Study after study found omega-3 fatty acids to be healthy. They were linked with a lower risk for heart disease and overall mortality. All those decades of parents forcing various fish oils on their grimacing children now had some science behind them. There is such a thing as a good fat.
, especially DHA and eicosapentaenoic acid, or EPA. Omega fats provide structure to neuronal cell membranes and are crucial in neuron-to-neuron communication. They increase levels of a protein called brain-derived neurotrophic factor (BDNF), which supports neuronal growth and survival. A growing body of evidence shows omega-3 supplementation may slow down the process of neurodegeneration, the gradual deterioration of the brain that results in Alzheimer’s disease and other forms of dementia.
Popping a daily omega-3 supplement or, better still, eating a seafood-rich diet, may increase blood flow to the brain. In 2019, the International Society for Nutritional Psychiatry Research recommended omega-3s as an adjunct therapy for major depressive disorder. PUFAs appear to reduce the risk for and severity of mood disorders such as depression and to boost attention in children with ADHD as effectively as drug therapies.
Many researchers claim there would’ve been plenty of DHA available on land to support early humans, and marine foods were just one of many sources.
Not Dr. Crawford.
He believes that brain development and function are not only dependent on DHA but, in fact, DHA sourced from the sea was critical to mammalian brain evolution. “The animal brain evolved 600 million years ago in the ocean and was dependent on DHA, as well as compounds such as iodine, which is also in short supply on land,” he said. “To build a brain, you need these building blocks, which were rich at sea and on rocky shores.”
Dr. Crawford cites his early biochemical work showing DHA isn’t readily accessible from the muscle tissue of land animals. Using DHA tagged with a radioactive isotope, he and his colleagues in the 1970s found that “ready-made” DHA, like that found in shellfish, is incorporated into the developing rat brain with 10-fold greater efficiency than plant- and land animal–sourced DHA, where it exists as its metabolic precursor alpha-linolenic acid. “I’m afraid the idea that ample DHA was available from the fats of animals on the savanna is just not true,” he disputes. According to Dr. Crawford, our tiny, wormlike ancestors were able to evolve primitive nervous systems and flit through the silt thanks to the abundance of healthy fat to be had by living in the ocean and consuming algae.
For over 40 years, Dr. Crawford has argued that rising rates of mental illness are a result of post–World War II dietary changes, especially the move toward land-sourced food and the medical community’s subsequent support of low-fat diets. He feels that omega-3s from seafood were critical to humans’ rapid neural march toward higher cognition, and are therefore critical to brain health. “The continued rise in mental illness is an incredibly important threat to mankind and society, and moving away from marine foods is a major contributor,” said Dr. Crawford.
University of Sherbrooke (Que.) physiology professor Stephen Cunnane, PhD, tends to agree that aquatically sourced nutrients were crucial to human evolution. It’s the importance of coastal living he’s not sure about. He believes hominins would’ve incorporated fish from lakes and rivers into their diet for millions of years. In his view, it wasn’t just omega-3s that contributed to our big brains, but a cluster of nutrients found in fish: iodine, iron, zinc, copper, and selenium among them. “I think DHA was hugely important to our evolution and brain health but I don’t think it was a magic bullet all by itself,” he said. “Numerous other nutrients found in fish and shellfish were very probably important, too, and are now known to be good for the brain.”
Dr. Marean agrees. “Accessing the marine food chain could have had a huge impact on fertility, survival, and overall health, including brain health, in part, due to the high return on omega-3 fatty acids and other nutrients.” But, he speculates, before MIS6, hominins would have had access to plenty of brain-healthy terrestrial nutrition, including meat from animals that consumed omega-3–rich plants and grains.
Dr. Cunnane agrees with Dr. Marean to a degree. He’s confident that higher intelligence evolved gradually over millions of years as mutations inching the cognitive needle forward conferred survival and reproductive advantages – but he maintains that certain advantages like, say, being able to shuck an oyster, allowed an already intelligent brain to thrive.
Foraging marine life in the waters off of Africa likely played an important role in keeping some of our ancestors alive and supported our subsequent propagation throughout the world. By this point, the human brain was already a marvel of consciousness and computing, not too dissimilar to the one we carry around today.
In all likelihood, Pleistocene humans probably got their nutrients and calories wherever they could. If we lived inland, we hunted. Maybe we speared the occasional catfish. We sourced nutrients from fruits, leaves, and nuts. A few times a month, those of us near the coast enjoyed a feast of mussels and oysters.
Dr. Stetka is an editorial director at Medscape.com, a former neuroscience researcher, and a nonpracticing physician. A version of this article first appeared on Medscape.
In U.S., lockdowns added 2 pounds per month
Americans gained nearly 2 pounds per month under COVID-19 shelter-in-place orders in 2020, according to a new study published March 22, 2021, in JAMA Network Open.
Those who kept the same lockdown habits could have gained 20 pounds during the past year, the study authors said.
“We know that weight gain is a public health problem in the U.S. already, so anything making it worse is definitely concerning, and shelter-in-place orders are so ubiquitous that the sheer number of people affected by this makes it extremely relevant,” Gregory Marcus, MD, the senior author and a cardiologist at the University of California, San Francisco, told the New York Times.
Dr. Marcus and colleagues analyzed more than 7,000 weight measurements from 269 people in 37 states who used Bluetooth-connected scales from Feb. 1 to June 1, 2020. Among the participants, about 52% were women, 77% were White, and they had an average age of 52 years.
The research team found that participants had a steady weight gain of more than half a pound every 10 days. That equals about 1.5-2 pounds per month.
Many of the participants were losing weight before the shelter-in-place orders went into effect, Dr. Marcus said. The lockdown effects could be even greater for those who weren’t losing weight before.
“It’s reasonable to assume these individuals are more engaged with their health in general, and more disciplined and on top of things,” he said. “That suggests we could be underestimating – that this is the tip of the iceberg.”
The small study doesn’t represent all of the nation and can’t be generalized to the U.S. population, the study authors noted, but it’s an indicator of what happened during the pandemic. The participants’ weight increased regardless of their location and chronic medical conditions.
Overall, people don’t move around as much during lockdowns, the UCSF researchers reported in another study published in Annals of Internal Medicine in November 2020. According to smartphone data, daily step counts decreased by 27% in March 2020. The step counts increased again throughout the summer but still remained lower than before the COVID-19 pandemic.
“The detrimental health outcomes suggested by these data demonstrate a need to identify concurrent strategies to mitigate weight gain,” the authors wrote in the JAMA Network Open study, “such as encouraging healthy diets and exploring ways to enhance physical activity, as local governments consider new constraints in response to SARS-CoV-2 and potential future pandemics.”
A version of this article first appeared on WebMD.com.
Americans gained nearly 2 pounds per month under COVID-19 shelter-in-place orders in 2020, according to a new study published March 22, 2021, in JAMA Network Open.
Those who kept the same lockdown habits could have gained 20 pounds during the past year, the study authors said.
“We know that weight gain is a public health problem in the U.S. already, so anything making it worse is definitely concerning, and shelter-in-place orders are so ubiquitous that the sheer number of people affected by this makes it extremely relevant,” Gregory Marcus, MD, the senior author and a cardiologist at the University of California, San Francisco, told the New York Times.
Dr. Marcus and colleagues analyzed more than 7,000 weight measurements from 269 people in 37 states who used Bluetooth-connected scales from Feb. 1 to June 1, 2020. Among the participants, about 52% were women, 77% were White, and they had an average age of 52 years.
The research team found that participants had a steady weight gain of more than half a pound every 10 days. That equals about 1.5-2 pounds per month.
Many of the participants were losing weight before the shelter-in-place orders went into effect, Dr. Marcus said. The lockdown effects could be even greater for those who weren’t losing weight before.
“It’s reasonable to assume these individuals are more engaged with their health in general, and more disciplined and on top of things,” he said. “That suggests we could be underestimating – that this is the tip of the iceberg.”
The small study doesn’t represent all of the nation and can’t be generalized to the U.S. population, the study authors noted, but it’s an indicator of what happened during the pandemic. The participants’ weight increased regardless of their location and chronic medical conditions.
Overall, people don’t move around as much during lockdowns, the UCSF researchers reported in another study published in Annals of Internal Medicine in November 2020. According to smartphone data, daily step counts decreased by 27% in March 2020. The step counts increased again throughout the summer but still remained lower than before the COVID-19 pandemic.
“The detrimental health outcomes suggested by these data demonstrate a need to identify concurrent strategies to mitigate weight gain,” the authors wrote in the JAMA Network Open study, “such as encouraging healthy diets and exploring ways to enhance physical activity, as local governments consider new constraints in response to SARS-CoV-2 and potential future pandemics.”
A version of this article first appeared on WebMD.com.
Americans gained nearly 2 pounds per month under COVID-19 shelter-in-place orders in 2020, according to a new study published March 22, 2021, in JAMA Network Open.
Those who kept the same lockdown habits could have gained 20 pounds during the past year, the study authors said.
“We know that weight gain is a public health problem in the U.S. already, so anything making it worse is definitely concerning, and shelter-in-place orders are so ubiquitous that the sheer number of people affected by this makes it extremely relevant,” Gregory Marcus, MD, the senior author and a cardiologist at the University of California, San Francisco, told the New York Times.
Dr. Marcus and colleagues analyzed more than 7,000 weight measurements from 269 people in 37 states who used Bluetooth-connected scales from Feb. 1 to June 1, 2020. Among the participants, about 52% were women, 77% were White, and they had an average age of 52 years.
The research team found that participants had a steady weight gain of more than half a pound every 10 days. That equals about 1.5-2 pounds per month.
Many of the participants were losing weight before the shelter-in-place orders went into effect, Dr. Marcus said. The lockdown effects could be even greater for those who weren’t losing weight before.
“It’s reasonable to assume these individuals are more engaged with their health in general, and more disciplined and on top of things,” he said. “That suggests we could be underestimating – that this is the tip of the iceberg.”
The small study doesn’t represent all of the nation and can’t be generalized to the U.S. population, the study authors noted, but it’s an indicator of what happened during the pandemic. The participants’ weight increased regardless of their location and chronic medical conditions.
Overall, people don’t move around as much during lockdowns, the UCSF researchers reported in another study published in Annals of Internal Medicine in November 2020. According to smartphone data, daily step counts decreased by 27% in March 2020. The step counts increased again throughout the summer but still remained lower than before the COVID-19 pandemic.
“The detrimental health outcomes suggested by these data demonstrate a need to identify concurrent strategies to mitigate weight gain,” the authors wrote in the JAMA Network Open study, “such as encouraging healthy diets and exploring ways to enhance physical activity, as local governments consider new constraints in response to SARS-CoV-2 and potential future pandemics.”
A version of this article first appeared on WebMD.com.