User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
High rates of work-related trauma, PTSD in intern physicians
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”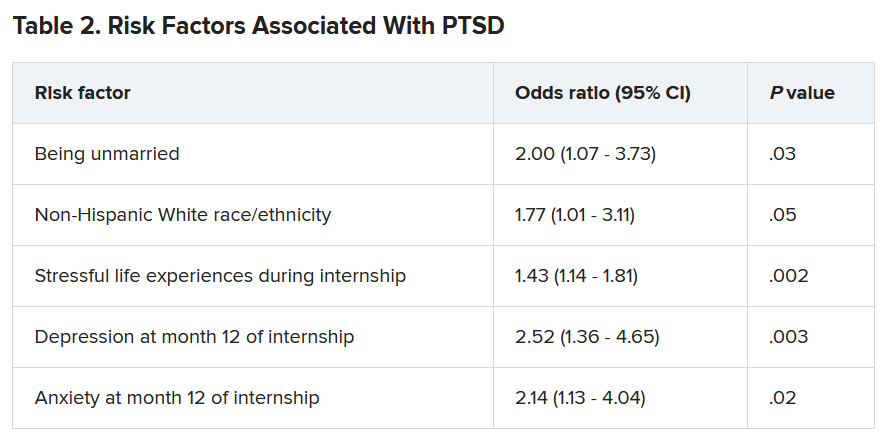
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”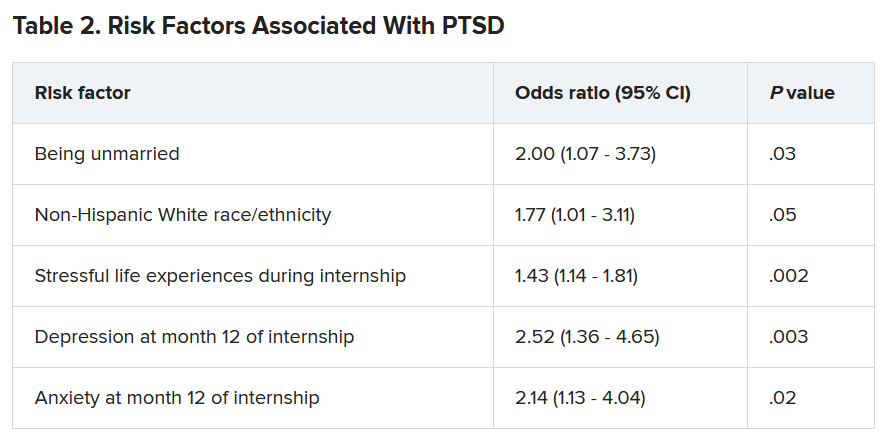
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”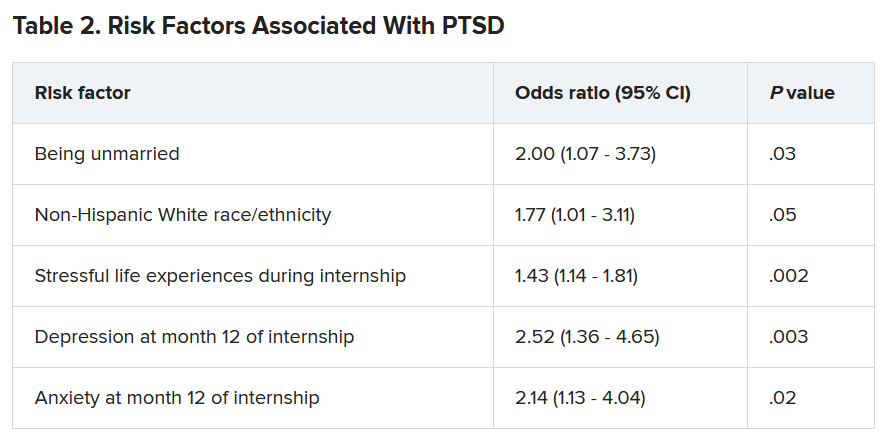
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ten killer steps to writing a great medical thriller
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
Memory benefit seen with antihypertensives crossing blood-brain barrier
Over a 3-year period, cognitively normal older adults taking BBB-crossing antihypertensives demonstrated superior verbal memory, compared with similar individuals receiving non–BBB-crossing antihypertensives, reported lead author Jean K. Ho, PhD, of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, and colleagues.
According to the investigators, the findings add color to a known link between hypertension and neurologic degeneration, and may aid the search for new therapeutic targets.
“Hypertension is a well-established risk factor for cognitive decline and dementia, possibly through its effects on both cerebrovascular disease and Alzheimer’s disease,” Dr. Ho and colleagues wrote in Hypertension. “Studies of antihypertensive treatments have reported possible salutary effects on cognition and cerebrovascular disease, as well as Alzheimer’s disease neuropathology.”
In a previous study, individuals younger than 75 years exposed to antihypertensives had an 8% decreased risk of dementia per year of use, while another trial showed that intensive blood pressure–lowering therapy reduced mild cognitive impairment by 19%.
“Despite these encouraging findings ... larger meta-analytic studies have been hampered by the fact that pharmacokinetic properties are typically not considered in existing studies or routine clinical practice,” wrote Dr. Ho and colleagues. “The present study sought to fill this gap [in that it was] a large and longitudinal meta-analytic study of existing data recoded to assess the effects of BBB-crossing potential in renin-angiotensin system [RAS] treatments among hypertensive adults.”
Methods and results
The meta-analysis included randomized clinical trials, prospective cohort studies, and retrospective observational studies. The researchers assessed data on 12,849 individuals from 14 cohorts that received either BBB-crossing or non–BBB-crossing antihypertensives.
The BBB-crossing properties of RAS treatments were identified by a literature review. Of ACE inhibitors, captopril, fosinopril, lisinopril, perindopril, ramipril, and trandolapril were classified as BBB crossing, and benazepril, enalapril, moexipril, and quinapril were classified as non–BBB-crossing. Of ARBs, telmisartan and candesartan were considered BBB-crossing, and olmesartan, eprosartan, irbesartan, and losartan were tagged as non–BBB-crossing.
Cognition was assessed via the following seven domains: executive function, attention, verbal memory learning, language, mental status, recall, and processing speed.
Compared with individuals taking non–BBB-crossing antihypertensives, those taking BBB-crossing agents had significantly superior verbal memory (recall), with a maximum effect size of 0.07 (P = .03).
According to the investigators, this finding was particularly noteworthy, as the BBB-crossing group had relatively higher vascular risk burden and lower mean education level.
“These differences make it all the more remarkable that the BBB-crossing group displayed better memory ability over time despite these cognitive disadvantages,” the investigators wrote.
Still, not all the findings favored BBB-crossing agents. Individuals in the BBB-crossing group had relatively inferior attention ability, with a minimum effect size of –0.17 (P = .02).
The other cognitive measures were not significantly different between groups.
Clinicians may consider findings after accounting for other factors
Principal investigator Daniel A. Nation, PhD, associate professor of psychological science and a faculty member of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, suggested that the small difference in verbal memory between groups could be clinically significant over a longer period of time.
“Although the overall effect size was pretty small, if you look at how long it would take for someone [with dementia] to progress over many years of decline, it would actually end up being a pretty big effect,” Dr. Nation said in an interview. “Small effect sizes could actually end up preventing a lot of cases of dementia,” he added.
The conflicting results in the BBB-crossing group – better verbal memory but worse attention ability – were “surprising,” he noted.
“I sort of didn’t believe it at first,” Dr. Nation said, “because the memory finding is sort of replication – we’d observed the same exact effect on memory in a smaller sample in another study. ... The attention [finding], going another way, was a new thing.”
Dr. Nation suggested that the intergroup differences in attention ability may stem from idiosyncrasies of the tests used to measure that domain, which can be impacted by cardiovascular or brain vascular disease. Or it could be caused by something else entirely, he said, noting that further investigation is needed.
He added that the improvements in verbal memory within the BBB-crossing group could be caused by direct effects on the brain. He pointed out that certain ACE polymorphisms have been linked with Alzheimer’s disease risk, and those same polymorphisms, in animal models, lead to neurodegeneration, with reversal possible through administration of ACE inhibitors.
“It could be that what we’re observing has nothing really to do with blood pressure,” Dr. Nation explained. “This could be a neuronal effect on learning memory systems.”
He went on to suggest that clinicians may consider these findings when selecting antihypertensive agents for their patients, with the caveat that all other prescribing factors have already been taking to account.
“In the event that you’re going to give an ACE inhibitor or an angiotensin receptor blocker anyway, and it ends up being a somewhat arbitrary decision in terms of which specific drug you’re going to give, then perhaps this is a piece of information you would take into account – that one gets in the brain and one doesn’t – in somebody at risk for cognitive decline,” Dr. Nation said.
Exact mechanisms of action unknown
Hélène Girouard, PhD, assistant professor of pharmacology and physiology at the University of Montreal, said in an interview that the findings are “of considerable importance, knowing that brain alterations could begin as much as 30 years before manifestation of dementia.”
Since 2003, Dr. Girouard has been studying the cognitive effects of antihypertensive medications. She noted that previous studies involving rodents “have shown beneficial effects [of BBB-crossing antihypertensive drugs] on cognition independent of their effects on blood pressure.”
The drugs’ exact mechanisms of action, however, remain elusive, according to Dr. Girouard, who offered several possible explanations, including amelioration of BBB disruption, brain inflammation, cerebral blood flow dysregulation, cholinergic dysfunction, and neurologic deficits. “Whether these mechanisms may explain Ho and colleagues’ observations remains to be established,” she added.
Andrea L. Schneider, MD, PhD, assistant professor of neurology at the University of Pennsylvania, Philadelphia, applauded the study, but ultimately suggested that more research is needed to impact clinical decision-making.
“The results of this important and well-done study suggest that further investigation into targeted mechanism-based approaches to selecting hypertension treatment agents, with a specific focus on cognitive outcomes, is warranted,” Dr. Schneider said in an interview. “Before changing clinical practice, further work is necessary to disentangle contributions of medication mechanism, comorbid vascular risk factors, and achieved blood pressure reduction, among others.”
The investigators disclosed support from the National Institutes of Health, the Alzheimer’s Association, the Waksman Foundation of Japan, and others. The interviewees reported no relevant conflicts of interest.
Over a 3-year period, cognitively normal older adults taking BBB-crossing antihypertensives demonstrated superior verbal memory, compared with similar individuals receiving non–BBB-crossing antihypertensives, reported lead author Jean K. Ho, PhD, of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, and colleagues.
According to the investigators, the findings add color to a known link between hypertension and neurologic degeneration, and may aid the search for new therapeutic targets.
“Hypertension is a well-established risk factor for cognitive decline and dementia, possibly through its effects on both cerebrovascular disease and Alzheimer’s disease,” Dr. Ho and colleagues wrote in Hypertension. “Studies of antihypertensive treatments have reported possible salutary effects on cognition and cerebrovascular disease, as well as Alzheimer’s disease neuropathology.”
In a previous study, individuals younger than 75 years exposed to antihypertensives had an 8% decreased risk of dementia per year of use, while another trial showed that intensive blood pressure–lowering therapy reduced mild cognitive impairment by 19%.
“Despite these encouraging findings ... larger meta-analytic studies have been hampered by the fact that pharmacokinetic properties are typically not considered in existing studies or routine clinical practice,” wrote Dr. Ho and colleagues. “The present study sought to fill this gap [in that it was] a large and longitudinal meta-analytic study of existing data recoded to assess the effects of BBB-crossing potential in renin-angiotensin system [RAS] treatments among hypertensive adults.”
Methods and results
The meta-analysis included randomized clinical trials, prospective cohort studies, and retrospective observational studies. The researchers assessed data on 12,849 individuals from 14 cohorts that received either BBB-crossing or non–BBB-crossing antihypertensives.
The BBB-crossing properties of RAS treatments were identified by a literature review. Of ACE inhibitors, captopril, fosinopril, lisinopril, perindopril, ramipril, and trandolapril were classified as BBB crossing, and benazepril, enalapril, moexipril, and quinapril were classified as non–BBB-crossing. Of ARBs, telmisartan and candesartan were considered BBB-crossing, and olmesartan, eprosartan, irbesartan, and losartan were tagged as non–BBB-crossing.
Cognition was assessed via the following seven domains: executive function, attention, verbal memory learning, language, mental status, recall, and processing speed.
Compared with individuals taking non–BBB-crossing antihypertensives, those taking BBB-crossing agents had significantly superior verbal memory (recall), with a maximum effect size of 0.07 (P = .03).
According to the investigators, this finding was particularly noteworthy, as the BBB-crossing group had relatively higher vascular risk burden and lower mean education level.
“These differences make it all the more remarkable that the BBB-crossing group displayed better memory ability over time despite these cognitive disadvantages,” the investigators wrote.
Still, not all the findings favored BBB-crossing agents. Individuals in the BBB-crossing group had relatively inferior attention ability, with a minimum effect size of –0.17 (P = .02).
The other cognitive measures were not significantly different between groups.
Clinicians may consider findings after accounting for other factors
Principal investigator Daniel A. Nation, PhD, associate professor of psychological science and a faculty member of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, suggested that the small difference in verbal memory between groups could be clinically significant over a longer period of time.
“Although the overall effect size was pretty small, if you look at how long it would take for someone [with dementia] to progress over many years of decline, it would actually end up being a pretty big effect,” Dr. Nation said in an interview. “Small effect sizes could actually end up preventing a lot of cases of dementia,” he added.
The conflicting results in the BBB-crossing group – better verbal memory but worse attention ability – were “surprising,” he noted.
“I sort of didn’t believe it at first,” Dr. Nation said, “because the memory finding is sort of replication – we’d observed the same exact effect on memory in a smaller sample in another study. ... The attention [finding], going another way, was a new thing.”
Dr. Nation suggested that the intergroup differences in attention ability may stem from idiosyncrasies of the tests used to measure that domain, which can be impacted by cardiovascular or brain vascular disease. Or it could be caused by something else entirely, he said, noting that further investigation is needed.
He added that the improvements in verbal memory within the BBB-crossing group could be caused by direct effects on the brain. He pointed out that certain ACE polymorphisms have been linked with Alzheimer’s disease risk, and those same polymorphisms, in animal models, lead to neurodegeneration, with reversal possible through administration of ACE inhibitors.
“It could be that what we’re observing has nothing really to do with blood pressure,” Dr. Nation explained. “This could be a neuronal effect on learning memory systems.”
He went on to suggest that clinicians may consider these findings when selecting antihypertensive agents for their patients, with the caveat that all other prescribing factors have already been taking to account.
“In the event that you’re going to give an ACE inhibitor or an angiotensin receptor blocker anyway, and it ends up being a somewhat arbitrary decision in terms of which specific drug you’re going to give, then perhaps this is a piece of information you would take into account – that one gets in the brain and one doesn’t – in somebody at risk for cognitive decline,” Dr. Nation said.
Exact mechanisms of action unknown
Hélène Girouard, PhD, assistant professor of pharmacology and physiology at the University of Montreal, said in an interview that the findings are “of considerable importance, knowing that brain alterations could begin as much as 30 years before manifestation of dementia.”
Since 2003, Dr. Girouard has been studying the cognitive effects of antihypertensive medications. She noted that previous studies involving rodents “have shown beneficial effects [of BBB-crossing antihypertensive drugs] on cognition independent of their effects on blood pressure.”
The drugs’ exact mechanisms of action, however, remain elusive, according to Dr. Girouard, who offered several possible explanations, including amelioration of BBB disruption, brain inflammation, cerebral blood flow dysregulation, cholinergic dysfunction, and neurologic deficits. “Whether these mechanisms may explain Ho and colleagues’ observations remains to be established,” she added.
Andrea L. Schneider, MD, PhD, assistant professor of neurology at the University of Pennsylvania, Philadelphia, applauded the study, but ultimately suggested that more research is needed to impact clinical decision-making.
“The results of this important and well-done study suggest that further investigation into targeted mechanism-based approaches to selecting hypertension treatment agents, with a specific focus on cognitive outcomes, is warranted,” Dr. Schneider said in an interview. “Before changing clinical practice, further work is necessary to disentangle contributions of medication mechanism, comorbid vascular risk factors, and achieved blood pressure reduction, among others.”
The investigators disclosed support from the National Institutes of Health, the Alzheimer’s Association, the Waksman Foundation of Japan, and others. The interviewees reported no relevant conflicts of interest.
Over a 3-year period, cognitively normal older adults taking BBB-crossing antihypertensives demonstrated superior verbal memory, compared with similar individuals receiving non–BBB-crossing antihypertensives, reported lead author Jean K. Ho, PhD, of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, and colleagues.
According to the investigators, the findings add color to a known link between hypertension and neurologic degeneration, and may aid the search for new therapeutic targets.
“Hypertension is a well-established risk factor for cognitive decline and dementia, possibly through its effects on both cerebrovascular disease and Alzheimer’s disease,” Dr. Ho and colleagues wrote in Hypertension. “Studies of antihypertensive treatments have reported possible salutary effects on cognition and cerebrovascular disease, as well as Alzheimer’s disease neuropathology.”
In a previous study, individuals younger than 75 years exposed to antihypertensives had an 8% decreased risk of dementia per year of use, while another trial showed that intensive blood pressure–lowering therapy reduced mild cognitive impairment by 19%.
“Despite these encouraging findings ... larger meta-analytic studies have been hampered by the fact that pharmacokinetic properties are typically not considered in existing studies or routine clinical practice,” wrote Dr. Ho and colleagues. “The present study sought to fill this gap [in that it was] a large and longitudinal meta-analytic study of existing data recoded to assess the effects of BBB-crossing potential in renin-angiotensin system [RAS] treatments among hypertensive adults.”
Methods and results
The meta-analysis included randomized clinical trials, prospective cohort studies, and retrospective observational studies. The researchers assessed data on 12,849 individuals from 14 cohorts that received either BBB-crossing or non–BBB-crossing antihypertensives.
The BBB-crossing properties of RAS treatments were identified by a literature review. Of ACE inhibitors, captopril, fosinopril, lisinopril, perindopril, ramipril, and trandolapril were classified as BBB crossing, and benazepril, enalapril, moexipril, and quinapril were classified as non–BBB-crossing. Of ARBs, telmisartan and candesartan were considered BBB-crossing, and olmesartan, eprosartan, irbesartan, and losartan were tagged as non–BBB-crossing.
Cognition was assessed via the following seven domains: executive function, attention, verbal memory learning, language, mental status, recall, and processing speed.
Compared with individuals taking non–BBB-crossing antihypertensives, those taking BBB-crossing agents had significantly superior verbal memory (recall), with a maximum effect size of 0.07 (P = .03).
According to the investigators, this finding was particularly noteworthy, as the BBB-crossing group had relatively higher vascular risk burden and lower mean education level.
“These differences make it all the more remarkable that the BBB-crossing group displayed better memory ability over time despite these cognitive disadvantages,” the investigators wrote.
Still, not all the findings favored BBB-crossing agents. Individuals in the BBB-crossing group had relatively inferior attention ability, with a minimum effect size of –0.17 (P = .02).
The other cognitive measures were not significantly different between groups.
Clinicians may consider findings after accounting for other factors
Principal investigator Daniel A. Nation, PhD, associate professor of psychological science and a faculty member of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, suggested that the small difference in verbal memory between groups could be clinically significant over a longer period of time.
“Although the overall effect size was pretty small, if you look at how long it would take for someone [with dementia] to progress over many years of decline, it would actually end up being a pretty big effect,” Dr. Nation said in an interview. “Small effect sizes could actually end up preventing a lot of cases of dementia,” he added.
The conflicting results in the BBB-crossing group – better verbal memory but worse attention ability – were “surprising,” he noted.
“I sort of didn’t believe it at first,” Dr. Nation said, “because the memory finding is sort of replication – we’d observed the same exact effect on memory in a smaller sample in another study. ... The attention [finding], going another way, was a new thing.”
Dr. Nation suggested that the intergroup differences in attention ability may stem from idiosyncrasies of the tests used to measure that domain, which can be impacted by cardiovascular or brain vascular disease. Or it could be caused by something else entirely, he said, noting that further investigation is needed.
He added that the improvements in verbal memory within the BBB-crossing group could be caused by direct effects on the brain. He pointed out that certain ACE polymorphisms have been linked with Alzheimer’s disease risk, and those same polymorphisms, in animal models, lead to neurodegeneration, with reversal possible through administration of ACE inhibitors.
“It could be that what we’re observing has nothing really to do with blood pressure,” Dr. Nation explained. “This could be a neuronal effect on learning memory systems.”
He went on to suggest that clinicians may consider these findings when selecting antihypertensive agents for their patients, with the caveat that all other prescribing factors have already been taking to account.
“In the event that you’re going to give an ACE inhibitor or an angiotensin receptor blocker anyway, and it ends up being a somewhat arbitrary decision in terms of which specific drug you’re going to give, then perhaps this is a piece of information you would take into account – that one gets in the brain and one doesn’t – in somebody at risk for cognitive decline,” Dr. Nation said.
Exact mechanisms of action unknown
Hélène Girouard, PhD, assistant professor of pharmacology and physiology at the University of Montreal, said in an interview that the findings are “of considerable importance, knowing that brain alterations could begin as much as 30 years before manifestation of dementia.”
Since 2003, Dr. Girouard has been studying the cognitive effects of antihypertensive medications. She noted that previous studies involving rodents “have shown beneficial effects [of BBB-crossing antihypertensive drugs] on cognition independent of their effects on blood pressure.”
The drugs’ exact mechanisms of action, however, remain elusive, according to Dr. Girouard, who offered several possible explanations, including amelioration of BBB disruption, brain inflammation, cerebral blood flow dysregulation, cholinergic dysfunction, and neurologic deficits. “Whether these mechanisms may explain Ho and colleagues’ observations remains to be established,” she added.
Andrea L. Schneider, MD, PhD, assistant professor of neurology at the University of Pennsylvania, Philadelphia, applauded the study, but ultimately suggested that more research is needed to impact clinical decision-making.
“The results of this important and well-done study suggest that further investigation into targeted mechanism-based approaches to selecting hypertension treatment agents, with a specific focus on cognitive outcomes, is warranted,” Dr. Schneider said in an interview. “Before changing clinical practice, further work is necessary to disentangle contributions of medication mechanism, comorbid vascular risk factors, and achieved blood pressure reduction, among others.”
The investigators disclosed support from the National Institutes of Health, the Alzheimer’s Association, the Waksman Foundation of Japan, and others. The interviewees reported no relevant conflicts of interest.
FROM HYPERTENSION
How dreams might prepare you for what’s next
What you experience in your dreams might feel random and disjointed, but that chaos during sleep might serve a function, according to Erin Wamsley, PhD, an associate professor of psychology and neuroscience at Furman University in Greenville, S.C. In fact, evidence uncovered by Dr. Wamsley and associates suggests that
Previous research and anecdotal evidence have shown that dreams use fragments of past experiences, Dr. Wamsley explained. While studying dreams, her team found that the mind is using select fragments of past experiences to prepare for a known upcoming event.
“This is new evidence that dreams reflect a memory-processing function,” said Dr. Wamsley, who presented the work at the virtual annual meeting of the Associated Professional Sleep Societies.
Some high performers already use past experiences to excel in future events. For instance, Michael Phelps, the most decorated Olympic swimmer, with 28 medals, would “mentally rehearse” his swims for up to 2 hours per day, according to his coach, Bob Bowman.
Using sleep to strengthen this process is an exciting prospect that scientists have been eager to figure out, said Allison Brager, PhD, director of human performance at the U.S. Army Warrior Fitness Training Center. Deep REM sleep can lead to improved learning and memory, she said. “So, hypothetically, better dreams mean better sleep, and that equals better performance.”
For their research, Dr. Wamsley’s team hooked 48 students up to a polysomnography machine to measure sleep cycles and how often they were in a deep REM sleep. The students who took part in the study spent the night in a sleep lab.
The students were woken up multiple times during the night and asked to report what they were dreaming about.
In the morning, they were given their reports and asked to identify familiar features or potential sources for particular dreams. More than half the dreams were tied to a memory the students recalled. One-quarter of the dreams were related to specific upcoming events the students reported. And about 40% of the dreams with a future event in them also included memories of past experiences. This was more common the longer the students dreamed, the scientists explained.
And this was also more common later in the night, possibly because the dreamer is closer to waking and the anticipated event is approaching, Dr. Wamsley said.
Studying dreams is a tricky, subjective business and not always taken as seriously as other aspects of sleep and neuroscience because it involves questions of human consciousness itself, said Erik Hoel, PhD, a research assistant professor of neuroscience at Tufts University in Medford, Mass.
In a recent report published in Patterns, he suggested that our weirdest dreams help our brains process our day-to-day experiences in a way that enables deeper learning.
“This type of research is challenged by the method,” Dr. Hoel said.
In the Wamsley study, “waking people up from a deep sleep and asking them to recollect their dream content will only get you part of the experience because it fades so quickly.” That said, the value of connecting what happens as a result could be meaningful, he noted. For example, study participants could be asked whether their future event went as planned and whether they think the outcome was related to how well they “prepared” in their dreams.
Even then, it would still be a subjective analysis. But going in those directions might lead to meaningful new training, Dr. Hoel said.
And training yourself to recall only specific memories right before sleep might prepare your mind in a focused way for certain events, from giving a presentation to having a difficult conversation with someone, or maybe even winning at the Olympics.
A version of this article first appeared on WebMD.com.
What you experience in your dreams might feel random and disjointed, but that chaos during sleep might serve a function, according to Erin Wamsley, PhD, an associate professor of psychology and neuroscience at Furman University in Greenville, S.C. In fact, evidence uncovered by Dr. Wamsley and associates suggests that
Previous research and anecdotal evidence have shown that dreams use fragments of past experiences, Dr. Wamsley explained. While studying dreams, her team found that the mind is using select fragments of past experiences to prepare for a known upcoming event.
“This is new evidence that dreams reflect a memory-processing function,” said Dr. Wamsley, who presented the work at the virtual annual meeting of the Associated Professional Sleep Societies.
Some high performers already use past experiences to excel in future events. For instance, Michael Phelps, the most decorated Olympic swimmer, with 28 medals, would “mentally rehearse” his swims for up to 2 hours per day, according to his coach, Bob Bowman.
Using sleep to strengthen this process is an exciting prospect that scientists have been eager to figure out, said Allison Brager, PhD, director of human performance at the U.S. Army Warrior Fitness Training Center. Deep REM sleep can lead to improved learning and memory, she said. “So, hypothetically, better dreams mean better sleep, and that equals better performance.”
For their research, Dr. Wamsley’s team hooked 48 students up to a polysomnography machine to measure sleep cycles and how often they were in a deep REM sleep. The students who took part in the study spent the night in a sleep lab.
The students were woken up multiple times during the night and asked to report what they were dreaming about.
In the morning, they were given their reports and asked to identify familiar features or potential sources for particular dreams. More than half the dreams were tied to a memory the students recalled. One-quarter of the dreams were related to specific upcoming events the students reported. And about 40% of the dreams with a future event in them also included memories of past experiences. This was more common the longer the students dreamed, the scientists explained.
And this was also more common later in the night, possibly because the dreamer is closer to waking and the anticipated event is approaching, Dr. Wamsley said.
Studying dreams is a tricky, subjective business and not always taken as seriously as other aspects of sleep and neuroscience because it involves questions of human consciousness itself, said Erik Hoel, PhD, a research assistant professor of neuroscience at Tufts University in Medford, Mass.
In a recent report published in Patterns, he suggested that our weirdest dreams help our brains process our day-to-day experiences in a way that enables deeper learning.
“This type of research is challenged by the method,” Dr. Hoel said.
In the Wamsley study, “waking people up from a deep sleep and asking them to recollect their dream content will only get you part of the experience because it fades so quickly.” That said, the value of connecting what happens as a result could be meaningful, he noted. For example, study participants could be asked whether their future event went as planned and whether they think the outcome was related to how well they “prepared” in their dreams.
Even then, it would still be a subjective analysis. But going in those directions might lead to meaningful new training, Dr. Hoel said.
And training yourself to recall only specific memories right before sleep might prepare your mind in a focused way for certain events, from giving a presentation to having a difficult conversation with someone, or maybe even winning at the Olympics.
A version of this article first appeared on WebMD.com.
What you experience in your dreams might feel random and disjointed, but that chaos during sleep might serve a function, according to Erin Wamsley, PhD, an associate professor of psychology and neuroscience at Furman University in Greenville, S.C. In fact, evidence uncovered by Dr. Wamsley and associates suggests that
Previous research and anecdotal evidence have shown that dreams use fragments of past experiences, Dr. Wamsley explained. While studying dreams, her team found that the mind is using select fragments of past experiences to prepare for a known upcoming event.
“This is new evidence that dreams reflect a memory-processing function,” said Dr. Wamsley, who presented the work at the virtual annual meeting of the Associated Professional Sleep Societies.
Some high performers already use past experiences to excel in future events. For instance, Michael Phelps, the most decorated Olympic swimmer, with 28 medals, would “mentally rehearse” his swims for up to 2 hours per day, according to his coach, Bob Bowman.
Using sleep to strengthen this process is an exciting prospect that scientists have been eager to figure out, said Allison Brager, PhD, director of human performance at the U.S. Army Warrior Fitness Training Center. Deep REM sleep can lead to improved learning and memory, she said. “So, hypothetically, better dreams mean better sleep, and that equals better performance.”
For their research, Dr. Wamsley’s team hooked 48 students up to a polysomnography machine to measure sleep cycles and how often they were in a deep REM sleep. The students who took part in the study spent the night in a sleep lab.
The students were woken up multiple times during the night and asked to report what they were dreaming about.
In the morning, they were given their reports and asked to identify familiar features or potential sources for particular dreams. More than half the dreams were tied to a memory the students recalled. One-quarter of the dreams were related to specific upcoming events the students reported. And about 40% of the dreams with a future event in them also included memories of past experiences. This was more common the longer the students dreamed, the scientists explained.
And this was also more common later in the night, possibly because the dreamer is closer to waking and the anticipated event is approaching, Dr. Wamsley said.
Studying dreams is a tricky, subjective business and not always taken as seriously as other aspects of sleep and neuroscience because it involves questions of human consciousness itself, said Erik Hoel, PhD, a research assistant professor of neuroscience at Tufts University in Medford, Mass.
In a recent report published in Patterns, he suggested that our weirdest dreams help our brains process our day-to-day experiences in a way that enables deeper learning.
“This type of research is challenged by the method,” Dr. Hoel said.
In the Wamsley study, “waking people up from a deep sleep and asking them to recollect their dream content will only get you part of the experience because it fades so quickly.” That said, the value of connecting what happens as a result could be meaningful, he noted. For example, study participants could be asked whether their future event went as planned and whether they think the outcome was related to how well they “prepared” in their dreams.
Even then, it would still be a subjective analysis. But going in those directions might lead to meaningful new training, Dr. Hoel said.
And training yourself to recall only specific memories right before sleep might prepare your mind in a focused way for certain events, from giving a presentation to having a difficult conversation with someone, or maybe even winning at the Olympics.
A version of this article first appeared on WebMD.com.
FROM SLEEP 2021
Cortical surface changes tied to risk for movement disorders in schizophrenia
Schizophrenia patients with parkinsonism show distinctive patterns of cortical surface markers, compared with schizophrenia patients without parkinsonism and healthy controls, results of a multimodal magnetic resonance imaging study suggest.
Sensorimotor abnormalities are common in schizophrenia patients, however, “the neurobiological mechanisms underlying parkinsonism in [schizophrenia], which in treated samples represents the unity of interplay between spontaneous and antipsychotic drug-exacerbated movement disorder, are poorly understood,” wrote Robert Christian Wolf, MD, of Heidelberg (Germany) University, and colleagues.
In a study published in Schizophrenia Research (2021 May;231:54-60), the investigators examined brain imaging findings from 20 healthy controls, 38 schizophrenia patients with parkinsonism (SZ-P), and 35 schizophrenia patients without parkinsonism (SZ-nonP). Dr. Wolf and colleagues examined three cortical surface markers: cortical thickness, complexity of cortical folding, and sulcus depth.
Compared with SZ-nonP patients, the SZ-P patients showed significantly increased complexity of cortical folding in the left supplementary motor cortex (SMC) and significantly decreased left postcentral sulcus (PCS) depth. In addition, left SMC activity was higher in both SZ-P and SZ-nonP patient groups, compared with controls.
In a regression analysis, the researchers examined relationships between parkinsonism severity and brain structure. They found that parkinsonism severity was negatively associated with left middle frontal complexity of cortical folding and left anterior cingulate cortex cortical thickness.
“Overall, the data support the notion that cortical features of distinct neurodevelopmental origin, particularly cortical folding indices such as [complexity of cortical folding] and sulcus depth, contribute to the pathogenesis of parkinsonism in SZ,” the researchers wrote.
The study findings were limited by several factors, including the cross-sectional design, the potential limitations of the Simpson-Angus Scale in characterizing parkinsonism, the inability to record lifetime antibiotics exposure in the patient population, and the inability to identify changes in brain stem nuclei, the researchers noted. However, the results were strengthened by the well-matched study groups and use of multimodal MRI, they said.
Consequently, “,” and suggest a link between abnormal neurodevelopmental processes and an increased risk for movement disorders in schizophrenia, they concluded.
The study was funded by the German Research Foundation and the German Federal Ministry of Education and Research. Dr. Wolf and colleagues disclosed no conflicts.
Schizophrenia patients with parkinsonism show distinctive patterns of cortical surface markers, compared with schizophrenia patients without parkinsonism and healthy controls, results of a multimodal magnetic resonance imaging study suggest.
Sensorimotor abnormalities are common in schizophrenia patients, however, “the neurobiological mechanisms underlying parkinsonism in [schizophrenia], which in treated samples represents the unity of interplay between spontaneous and antipsychotic drug-exacerbated movement disorder, are poorly understood,” wrote Robert Christian Wolf, MD, of Heidelberg (Germany) University, and colleagues.
In a study published in Schizophrenia Research (2021 May;231:54-60), the investigators examined brain imaging findings from 20 healthy controls, 38 schizophrenia patients with parkinsonism (SZ-P), and 35 schizophrenia patients without parkinsonism (SZ-nonP). Dr. Wolf and colleagues examined three cortical surface markers: cortical thickness, complexity of cortical folding, and sulcus depth.
Compared with SZ-nonP patients, the SZ-P patients showed significantly increased complexity of cortical folding in the left supplementary motor cortex (SMC) and significantly decreased left postcentral sulcus (PCS) depth. In addition, left SMC activity was higher in both SZ-P and SZ-nonP patient groups, compared with controls.
In a regression analysis, the researchers examined relationships between parkinsonism severity and brain structure. They found that parkinsonism severity was negatively associated with left middle frontal complexity of cortical folding and left anterior cingulate cortex cortical thickness.
“Overall, the data support the notion that cortical features of distinct neurodevelopmental origin, particularly cortical folding indices such as [complexity of cortical folding] and sulcus depth, contribute to the pathogenesis of parkinsonism in SZ,” the researchers wrote.
The study findings were limited by several factors, including the cross-sectional design, the potential limitations of the Simpson-Angus Scale in characterizing parkinsonism, the inability to record lifetime antibiotics exposure in the patient population, and the inability to identify changes in brain stem nuclei, the researchers noted. However, the results were strengthened by the well-matched study groups and use of multimodal MRI, they said.
Consequently, “,” and suggest a link between abnormal neurodevelopmental processes and an increased risk for movement disorders in schizophrenia, they concluded.
The study was funded by the German Research Foundation and the German Federal Ministry of Education and Research. Dr. Wolf and colleagues disclosed no conflicts.
Schizophrenia patients with parkinsonism show distinctive patterns of cortical surface markers, compared with schizophrenia patients without parkinsonism and healthy controls, results of a multimodal magnetic resonance imaging study suggest.
Sensorimotor abnormalities are common in schizophrenia patients, however, “the neurobiological mechanisms underlying parkinsonism in [schizophrenia], which in treated samples represents the unity of interplay between spontaneous and antipsychotic drug-exacerbated movement disorder, are poorly understood,” wrote Robert Christian Wolf, MD, of Heidelberg (Germany) University, and colleagues.
In a study published in Schizophrenia Research (2021 May;231:54-60), the investigators examined brain imaging findings from 20 healthy controls, 38 schizophrenia patients with parkinsonism (SZ-P), and 35 schizophrenia patients without parkinsonism (SZ-nonP). Dr. Wolf and colleagues examined three cortical surface markers: cortical thickness, complexity of cortical folding, and sulcus depth.
Compared with SZ-nonP patients, the SZ-P patients showed significantly increased complexity of cortical folding in the left supplementary motor cortex (SMC) and significantly decreased left postcentral sulcus (PCS) depth. In addition, left SMC activity was higher in both SZ-P and SZ-nonP patient groups, compared with controls.
In a regression analysis, the researchers examined relationships between parkinsonism severity and brain structure. They found that parkinsonism severity was negatively associated with left middle frontal complexity of cortical folding and left anterior cingulate cortex cortical thickness.
“Overall, the data support the notion that cortical features of distinct neurodevelopmental origin, particularly cortical folding indices such as [complexity of cortical folding] and sulcus depth, contribute to the pathogenesis of parkinsonism in SZ,” the researchers wrote.
The study findings were limited by several factors, including the cross-sectional design, the potential limitations of the Simpson-Angus Scale in characterizing parkinsonism, the inability to record lifetime antibiotics exposure in the patient population, and the inability to identify changes in brain stem nuclei, the researchers noted. However, the results were strengthened by the well-matched study groups and use of multimodal MRI, they said.
Consequently, “,” and suggest a link between abnormal neurodevelopmental processes and an increased risk for movement disorders in schizophrenia, they concluded.
The study was funded by the German Research Foundation and the German Federal Ministry of Education and Research. Dr. Wolf and colleagues disclosed no conflicts.
FROM SCHIZOPHRENIA RESEARCH
Is trouble falling asleep a modifiable risk factor for dementia?
, new research suggests.
Trouble falling asleep “may be a modifiable risk factor for later-life cognitive impairment and dementia,” said lead author Afsara Zaheed, a PhD candidate in clinical science, department of psychology, University of Michigan, Ann Arbor.
“Patients should also be aware of the importance of insomnia on cognitive functioning so that they can bring up these concerns with their providers early,” she said.
The findings were presented at Virtual SLEEP 2021, the 35th Annual Meeting of the Associated Professional Sleep Societies.
Poor sleep common with age
As many as one-half of older adults report having poor sleep quality and insomnia, and growing evidence suggests that insomnia may be a unique risk factor for cognitive decline in later life, Ms. Zaheed explained.
To investigate further, the researchers analyzed data on 2,496 adults aged 51 years and older who were participants in the Health and Retirement Study, a longitudinal study of aging in a nationally representative population of older adults.
In 2002, participants were asked how often they had trouble falling asleep, woke up during the night, woke up too early, and were not able to fall asleep again and how often they felt really rested when they woke up in the morning.
In 2016, participants’ cognition was assessed using a battery of neuropsychological tests that gauged episodic memory, executive function, language, visuospatial/construction, and processing speed.
Analyses controlled for sociodemographics, baseline global cognitive performance, and the influence of depressive symptoms and vascular disease.
Compared with other insomnia symptoms, having difficulty falling asleep in 2002 was the main insomnia symptom that was predictive of cognitive impairment 14 years later, in 2016.
More frequent trouble falling asleep was predictive of poorer episodic memory, executive function, language, processing speed, and visuospatial performance.
The associations between sleep initiation and later cognitive impairment were partially explained by depressive symptoms and vascular disease burden for all domains except episodic memory, which was only partially explained by depressive symptoms.
Unclear mechanism
Ms. Zaheed said research is needed to uncover neurophysiologic mechanisms underlying the observed associations. “It may be that chronic difficulty with falling asleep is associated with inflammatory or metabolic processes that negatively affect brain structure and function over time,” she said.
“Insomnia has also been linked with higher accumulation of protein aggregates in the brain that disrupt cell communication and are characteristic of late-life disorders such as Alzheimer’s disease,” she added.
“While our project did not directly investigate these potential causal pathways between insomnia and cognition, our results suggest that investigating these potential mechanisms is an important area for future research,” Ms. Zaheed said.
“While additional intervention research is needed to determine whether targeting insomnia in older patients can have lasting cognitive benefits, results from this study suggest that discussing insomnia symptoms at the primary care level may be beneficial for both doctors and patients,” she added.
“By targeting insomnia – for example, through an evidence-based cognitive–behavioral therapy approach – individuals may improve various mental and physical health outcomes in addition to improving their sleep quality,” Ms. Zaheed said.
Reached for comment, Shaheen E. Lakhan, MD, PhD, neurologist in Newton, Massachusetts, said, “There is a strong link between chronic sleep disturbances and cognitive impairment, including dementia.”
“This study further supports this link and specifically calls out initiating sleep (as opposed to staying asleep) as the culprit. It also raises the hypothesis that the link is primarily mediated by depression and vascular disease; however, the verdict is still out,” said Dr. Lakhan.
The study was funded by the National Institute on Aging. Ms. Zaheed and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Trouble falling asleep “may be a modifiable risk factor for later-life cognitive impairment and dementia,” said lead author Afsara Zaheed, a PhD candidate in clinical science, department of psychology, University of Michigan, Ann Arbor.
“Patients should also be aware of the importance of insomnia on cognitive functioning so that they can bring up these concerns with their providers early,” she said.
The findings were presented at Virtual SLEEP 2021, the 35th Annual Meeting of the Associated Professional Sleep Societies.
Poor sleep common with age
As many as one-half of older adults report having poor sleep quality and insomnia, and growing evidence suggests that insomnia may be a unique risk factor for cognitive decline in later life, Ms. Zaheed explained.
To investigate further, the researchers analyzed data on 2,496 adults aged 51 years and older who were participants in the Health and Retirement Study, a longitudinal study of aging in a nationally representative population of older adults.
In 2002, participants were asked how often they had trouble falling asleep, woke up during the night, woke up too early, and were not able to fall asleep again and how often they felt really rested when they woke up in the morning.
In 2016, participants’ cognition was assessed using a battery of neuropsychological tests that gauged episodic memory, executive function, language, visuospatial/construction, and processing speed.
Analyses controlled for sociodemographics, baseline global cognitive performance, and the influence of depressive symptoms and vascular disease.
Compared with other insomnia symptoms, having difficulty falling asleep in 2002 was the main insomnia symptom that was predictive of cognitive impairment 14 years later, in 2016.
More frequent trouble falling asleep was predictive of poorer episodic memory, executive function, language, processing speed, and visuospatial performance.
The associations between sleep initiation and later cognitive impairment were partially explained by depressive symptoms and vascular disease burden for all domains except episodic memory, which was only partially explained by depressive symptoms.
Unclear mechanism
Ms. Zaheed said research is needed to uncover neurophysiologic mechanisms underlying the observed associations. “It may be that chronic difficulty with falling asleep is associated with inflammatory or metabolic processes that negatively affect brain structure and function over time,” she said.
“Insomnia has also been linked with higher accumulation of protein aggregates in the brain that disrupt cell communication and are characteristic of late-life disorders such as Alzheimer’s disease,” she added.
“While our project did not directly investigate these potential causal pathways between insomnia and cognition, our results suggest that investigating these potential mechanisms is an important area for future research,” Ms. Zaheed said.
“While additional intervention research is needed to determine whether targeting insomnia in older patients can have lasting cognitive benefits, results from this study suggest that discussing insomnia symptoms at the primary care level may be beneficial for both doctors and patients,” she added.
“By targeting insomnia – for example, through an evidence-based cognitive–behavioral therapy approach – individuals may improve various mental and physical health outcomes in addition to improving their sleep quality,” Ms. Zaheed said.
Reached for comment, Shaheen E. Lakhan, MD, PhD, neurologist in Newton, Massachusetts, said, “There is a strong link between chronic sleep disturbances and cognitive impairment, including dementia.”
“This study further supports this link and specifically calls out initiating sleep (as opposed to staying asleep) as the culprit. It also raises the hypothesis that the link is primarily mediated by depression and vascular disease; however, the verdict is still out,” said Dr. Lakhan.
The study was funded by the National Institute on Aging. Ms. Zaheed and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Trouble falling asleep “may be a modifiable risk factor for later-life cognitive impairment and dementia,” said lead author Afsara Zaheed, a PhD candidate in clinical science, department of psychology, University of Michigan, Ann Arbor.
“Patients should also be aware of the importance of insomnia on cognitive functioning so that they can bring up these concerns with their providers early,” she said.
The findings were presented at Virtual SLEEP 2021, the 35th Annual Meeting of the Associated Professional Sleep Societies.
Poor sleep common with age
As many as one-half of older adults report having poor sleep quality and insomnia, and growing evidence suggests that insomnia may be a unique risk factor for cognitive decline in later life, Ms. Zaheed explained.
To investigate further, the researchers analyzed data on 2,496 adults aged 51 years and older who were participants in the Health and Retirement Study, a longitudinal study of aging in a nationally representative population of older adults.
In 2002, participants were asked how often they had trouble falling asleep, woke up during the night, woke up too early, and were not able to fall asleep again and how often they felt really rested when they woke up in the morning.
In 2016, participants’ cognition was assessed using a battery of neuropsychological tests that gauged episodic memory, executive function, language, visuospatial/construction, and processing speed.
Analyses controlled for sociodemographics, baseline global cognitive performance, and the influence of depressive symptoms and vascular disease.
Compared with other insomnia symptoms, having difficulty falling asleep in 2002 was the main insomnia symptom that was predictive of cognitive impairment 14 years later, in 2016.
More frequent trouble falling asleep was predictive of poorer episodic memory, executive function, language, processing speed, and visuospatial performance.
The associations between sleep initiation and later cognitive impairment were partially explained by depressive symptoms and vascular disease burden for all domains except episodic memory, which was only partially explained by depressive symptoms.
Unclear mechanism
Ms. Zaheed said research is needed to uncover neurophysiologic mechanisms underlying the observed associations. “It may be that chronic difficulty with falling asleep is associated with inflammatory or metabolic processes that negatively affect brain structure and function over time,” she said.
“Insomnia has also been linked with higher accumulation of protein aggregates in the brain that disrupt cell communication and are characteristic of late-life disorders such as Alzheimer’s disease,” she added.
“While our project did not directly investigate these potential causal pathways between insomnia and cognition, our results suggest that investigating these potential mechanisms is an important area for future research,” Ms. Zaheed said.
“While additional intervention research is needed to determine whether targeting insomnia in older patients can have lasting cognitive benefits, results from this study suggest that discussing insomnia symptoms at the primary care level may be beneficial for both doctors and patients,” she added.
“By targeting insomnia – for example, through an evidence-based cognitive–behavioral therapy approach – individuals may improve various mental and physical health outcomes in addition to improving their sleep quality,” Ms. Zaheed said.
Reached for comment, Shaheen E. Lakhan, MD, PhD, neurologist in Newton, Massachusetts, said, “There is a strong link between chronic sleep disturbances and cognitive impairment, including dementia.”
“This study further supports this link and specifically calls out initiating sleep (as opposed to staying asleep) as the culprit. It also raises the hypothesis that the link is primarily mediated by depression and vascular disease; however, the verdict is still out,” said Dr. Lakhan.
The study was funded by the National Institute on Aging. Ms. Zaheed and Dr. Lakhan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Insomnia in children tied to mood and anxiety disorders in adulthood
, new research indicates. However, insomnia symptoms in childhood that remit in the transition to adolescence do not confer increased risk of mood or anxiety disorders later on, the study found.
“As insomnia symptoms may precipitate or maintain internalizing disorders, our findings further reinforce the need for early sleep interventions to prevent future mental health disorders,” said lead investigator Julio Fernandez-Mendoza, PhD, associate professor at Penn State University, Hershey.
He presented his research at Virtual SLEEP 2021, the 35th annual meeting of the Associated Professional Sleep Societies.
Results ‘very clear’
The findings are based on data from the Penn State Child Cohort, a longitudinal, population-based sample of 700 children with a median age of 9 years, including 421 who were followed up 8 years later as adolescents (median age, 16 years) and 502 who were followed up 15 years later as young adults (median age, 24 years).
The data are “very clear that the risk of having internalizing disorders in young adulthood associated with having persistent insomnia symptoms, since childhood through adolescence into young adulthood,” Dr. Fernandez-Mendoza said in his presentation.
A persistent developmental trajectory was associated with a threefold increased risk of adult internalizing disorder (hazard ratio, 3.19).
The risk of having an internalizing disorder in young adulthood associated with newly developing (incident) insomnia symptoms is about twofold higher (HR, 1.94), whereas the risk associated with the waxing and waning pattern of insomnia is 1.5-fold (HR, 1.53) higher and only marginally significant, he reported.
An equally important finding, said Dr. Fernandez-Mendoza, is that those who had remitted insomnia symptoms in the transition to adolescence and throughout young adulthood were not at increased risk of having an internalizing disorder in young adulthood.
“Insomnia symptoms in a persistent manner associated with long-term adverse mental health outcomes, but remission of those insomnia symptoms associated with a good prognosis,” he said.
It’s also important to note, he said, that about 40% of children do not outgrow their insomnia symptoms in the transition to adolescence and are at risk of developing mental health disorders later on during early adulthood.
Reached for comment, Nitun Verma, MD, a spokesperson for the American Academy of Sleep Medicine, said: “There is a connection with mood and anxiety disorders with sleep, especially insomnia. This is a good reminder that reviewing someone’s sleep habits should always be a part of assessing someone’s mental health.”
A version of this article first appeared on Medscape.com.
, new research indicates. However, insomnia symptoms in childhood that remit in the transition to adolescence do not confer increased risk of mood or anxiety disorders later on, the study found.
“As insomnia symptoms may precipitate or maintain internalizing disorders, our findings further reinforce the need for early sleep interventions to prevent future mental health disorders,” said lead investigator Julio Fernandez-Mendoza, PhD, associate professor at Penn State University, Hershey.
He presented his research at Virtual SLEEP 2021, the 35th annual meeting of the Associated Professional Sleep Societies.
Results ‘very clear’
The findings are based on data from the Penn State Child Cohort, a longitudinal, population-based sample of 700 children with a median age of 9 years, including 421 who were followed up 8 years later as adolescents (median age, 16 years) and 502 who were followed up 15 years later as young adults (median age, 24 years).
The data are “very clear that the risk of having internalizing disorders in young adulthood associated with having persistent insomnia symptoms, since childhood through adolescence into young adulthood,” Dr. Fernandez-Mendoza said in his presentation.
A persistent developmental trajectory was associated with a threefold increased risk of adult internalizing disorder (hazard ratio, 3.19).
The risk of having an internalizing disorder in young adulthood associated with newly developing (incident) insomnia symptoms is about twofold higher (HR, 1.94), whereas the risk associated with the waxing and waning pattern of insomnia is 1.5-fold (HR, 1.53) higher and only marginally significant, he reported.
An equally important finding, said Dr. Fernandez-Mendoza, is that those who had remitted insomnia symptoms in the transition to adolescence and throughout young adulthood were not at increased risk of having an internalizing disorder in young adulthood.
“Insomnia symptoms in a persistent manner associated with long-term adverse mental health outcomes, but remission of those insomnia symptoms associated with a good prognosis,” he said.
It’s also important to note, he said, that about 40% of children do not outgrow their insomnia symptoms in the transition to adolescence and are at risk of developing mental health disorders later on during early adulthood.
Reached for comment, Nitun Verma, MD, a spokesperson for the American Academy of Sleep Medicine, said: “There is a connection with mood and anxiety disorders with sleep, especially insomnia. This is a good reminder that reviewing someone’s sleep habits should always be a part of assessing someone’s mental health.”
A version of this article first appeared on Medscape.com.
, new research indicates. However, insomnia symptoms in childhood that remit in the transition to adolescence do not confer increased risk of mood or anxiety disorders later on, the study found.
“As insomnia symptoms may precipitate or maintain internalizing disorders, our findings further reinforce the need for early sleep interventions to prevent future mental health disorders,” said lead investigator Julio Fernandez-Mendoza, PhD, associate professor at Penn State University, Hershey.
He presented his research at Virtual SLEEP 2021, the 35th annual meeting of the Associated Professional Sleep Societies.
Results ‘very clear’
The findings are based on data from the Penn State Child Cohort, a longitudinal, population-based sample of 700 children with a median age of 9 years, including 421 who were followed up 8 years later as adolescents (median age, 16 years) and 502 who were followed up 15 years later as young adults (median age, 24 years).
The data are “very clear that the risk of having internalizing disorders in young adulthood associated with having persistent insomnia symptoms, since childhood through adolescence into young adulthood,” Dr. Fernandez-Mendoza said in his presentation.
A persistent developmental trajectory was associated with a threefold increased risk of adult internalizing disorder (hazard ratio, 3.19).
The risk of having an internalizing disorder in young adulthood associated with newly developing (incident) insomnia symptoms is about twofold higher (HR, 1.94), whereas the risk associated with the waxing and waning pattern of insomnia is 1.5-fold (HR, 1.53) higher and only marginally significant, he reported.
An equally important finding, said Dr. Fernandez-Mendoza, is that those who had remitted insomnia symptoms in the transition to adolescence and throughout young adulthood were not at increased risk of having an internalizing disorder in young adulthood.
“Insomnia symptoms in a persistent manner associated with long-term adverse mental health outcomes, but remission of those insomnia symptoms associated with a good prognosis,” he said.
It’s also important to note, he said, that about 40% of children do not outgrow their insomnia symptoms in the transition to adolescence and are at risk of developing mental health disorders later on during early adulthood.
Reached for comment, Nitun Verma, MD, a spokesperson for the American Academy of Sleep Medicine, said: “There is a connection with mood and anxiety disorders with sleep, especially insomnia. This is a good reminder that reviewing someone’s sleep habits should always be a part of assessing someone’s mental health.”
A version of this article first appeared on Medscape.com.
Neurodegeneration complicates psychiatric care for Parkinson’s patients
Managing depression and anxiety in Parkinson’s disease should start with a review of medications and involve multidisciplinary care, according to a recent summary of evidence.
“Depression and anxiety have a complex relationship with the disease and while the exact mechanism for this association is unknown, both disturbances occur with increased prevalence across the disease course and when present earlier in life, increase the risk of PD by about twofold,” wrote Gregory M. Pontone, MD, of Johns Hopkins University, Baltimore, and colleagues.
Randomized trials to guide treatment of anxiety and depression in patients with Parkinson’s disease (PD) are limited, the researchers noted. However, data from a longitudinal study showed that PD patients whose depression remitted spontaneously or responded to treatment were able to attain a level of function similar to that of never-depressed PD patients, Dr. Pontone and colleagues said.
The researchers offered a pair of treatment algorithms to help guide clinicians in managing depression and anxiety in PD. However, a caveat to keep in mind is that “the benefit of antidepressant medications, used for depression or anxiety, can be confounded when motor symptoms are not optimally treated,” the researchers emphasized.
For depression, the researchers advised starting with some lab work; “at a minimum we suggest checking a complete blood count, metabolic panel, TSH, B12, and folate,” they noted. They recommended an antidepressant, cognitive-behavioral therapy, or both, as a first-line treatment, such as monotherapy with selective norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors. They advised titrating the chosen monotherapy to a minimum effective dose over a 2- to 3-week period to assess response.
“We recommend continuing antidepressant therapy for at least 1 year based on literature in non-PD populations and anecdotal clinical experience. At 1 year, if not in remission, consider continuing treatment or augmenting to improve response,” the researchers said.
, and they recommended using anxiety rating scales to diagnose anxiety in PD. “Given the high prevalence of atypical anxiety syndromes in PD and their potential association with both motor and nonmotor symptoms of the disease, working with the neurologist to achieve optimal control of PD is an essential first step to alleviating anxiety,” they emphasized.
The researchers also advised addressing comorbidities, including cardiovascular disease, chronic pain, diabetes, gastrointestinal issues, hyperthyroidism, and lung disease, all of which can be associated with anxiety. Once comorbidities are addressed, they advised caution given the lack of evidence for efficacy of both pharmacologic and nonpharmacologic anxiety treatments for PD patients. However, first-tier treatment for anxiety could include monotherapy with serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors, they said.
PD patients with depression and anxiety also may benefit from nonpharmacologic interventions, including exercise, mindfulness, relaxation therapy, and cognitive behavioral therapy the researchers said.
Although the algorithm may not differ significantly from current treatment protocols, it highlights aspects unique to PD patients, the researchers said. In particular, the algorithm shows “that interventions used for motor symptoms, for example, dopamine agonists, may be especially potent for mood in the PD population and that augmentation strategies, such as antipsychotics and lithium, may not be well tolerated given their outsized risk of adverse events in PD,” they said.
“While an article of this kind cannot hope to address the gap in knowledge on comparative efficacy between interventions, it can guide readers on the best strategies for implementation and risk mitigation in PD – essentially focusing more on effectiveness,” they concluded.
The study received no outside funding. Dr. Pontone disclosed serving as a consultant for Acadia Pharmaceuticals and Concert Pharmaceuticals.
Managing depression and anxiety in Parkinson’s disease should start with a review of medications and involve multidisciplinary care, according to a recent summary of evidence.
“Depression and anxiety have a complex relationship with the disease and while the exact mechanism for this association is unknown, both disturbances occur with increased prevalence across the disease course and when present earlier in life, increase the risk of PD by about twofold,” wrote Gregory M. Pontone, MD, of Johns Hopkins University, Baltimore, and colleagues.
Randomized trials to guide treatment of anxiety and depression in patients with Parkinson’s disease (PD) are limited, the researchers noted. However, data from a longitudinal study showed that PD patients whose depression remitted spontaneously or responded to treatment were able to attain a level of function similar to that of never-depressed PD patients, Dr. Pontone and colleagues said.
The researchers offered a pair of treatment algorithms to help guide clinicians in managing depression and anxiety in PD. However, a caveat to keep in mind is that “the benefit of antidepressant medications, used for depression or anxiety, can be confounded when motor symptoms are not optimally treated,” the researchers emphasized.
For depression, the researchers advised starting with some lab work; “at a minimum we suggest checking a complete blood count, metabolic panel, TSH, B12, and folate,” they noted. They recommended an antidepressant, cognitive-behavioral therapy, or both, as a first-line treatment, such as monotherapy with selective norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors. They advised titrating the chosen monotherapy to a minimum effective dose over a 2- to 3-week period to assess response.
“We recommend continuing antidepressant therapy for at least 1 year based on literature in non-PD populations and anecdotal clinical experience. At 1 year, if not in remission, consider continuing treatment or augmenting to improve response,” the researchers said.
, and they recommended using anxiety rating scales to diagnose anxiety in PD. “Given the high prevalence of atypical anxiety syndromes in PD and their potential association with both motor and nonmotor symptoms of the disease, working with the neurologist to achieve optimal control of PD is an essential first step to alleviating anxiety,” they emphasized.
The researchers also advised addressing comorbidities, including cardiovascular disease, chronic pain, diabetes, gastrointestinal issues, hyperthyroidism, and lung disease, all of which can be associated with anxiety. Once comorbidities are addressed, they advised caution given the lack of evidence for efficacy of both pharmacologic and nonpharmacologic anxiety treatments for PD patients. However, first-tier treatment for anxiety could include monotherapy with serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors, they said.
PD patients with depression and anxiety also may benefit from nonpharmacologic interventions, including exercise, mindfulness, relaxation therapy, and cognitive behavioral therapy the researchers said.
Although the algorithm may not differ significantly from current treatment protocols, it highlights aspects unique to PD patients, the researchers said. In particular, the algorithm shows “that interventions used for motor symptoms, for example, dopamine agonists, may be especially potent for mood in the PD population and that augmentation strategies, such as antipsychotics and lithium, may not be well tolerated given their outsized risk of adverse events in PD,” they said.
“While an article of this kind cannot hope to address the gap in knowledge on comparative efficacy between interventions, it can guide readers on the best strategies for implementation and risk mitigation in PD – essentially focusing more on effectiveness,” they concluded.
The study received no outside funding. Dr. Pontone disclosed serving as a consultant for Acadia Pharmaceuticals and Concert Pharmaceuticals.
Managing depression and anxiety in Parkinson’s disease should start with a review of medications and involve multidisciplinary care, according to a recent summary of evidence.
“Depression and anxiety have a complex relationship with the disease and while the exact mechanism for this association is unknown, both disturbances occur with increased prevalence across the disease course and when present earlier in life, increase the risk of PD by about twofold,” wrote Gregory M. Pontone, MD, of Johns Hopkins University, Baltimore, and colleagues.
Randomized trials to guide treatment of anxiety and depression in patients with Parkinson’s disease (PD) are limited, the researchers noted. However, data from a longitudinal study showed that PD patients whose depression remitted spontaneously or responded to treatment were able to attain a level of function similar to that of never-depressed PD patients, Dr. Pontone and colleagues said.
The researchers offered a pair of treatment algorithms to help guide clinicians in managing depression and anxiety in PD. However, a caveat to keep in mind is that “the benefit of antidepressant medications, used for depression or anxiety, can be confounded when motor symptoms are not optimally treated,” the researchers emphasized.
For depression, the researchers advised starting with some lab work; “at a minimum we suggest checking a complete blood count, metabolic panel, TSH, B12, and folate,” they noted. They recommended an antidepressant, cognitive-behavioral therapy, or both, as a first-line treatment, such as monotherapy with selective norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors. They advised titrating the chosen monotherapy to a minimum effective dose over a 2- to 3-week period to assess response.
“We recommend continuing antidepressant therapy for at least 1 year based on literature in non-PD populations and anecdotal clinical experience. At 1 year, if not in remission, consider continuing treatment or augmenting to improve response,” the researchers said.
, and they recommended using anxiety rating scales to diagnose anxiety in PD. “Given the high prevalence of atypical anxiety syndromes in PD and their potential association with both motor and nonmotor symptoms of the disease, working with the neurologist to achieve optimal control of PD is an essential first step to alleviating anxiety,” they emphasized.
The researchers also advised addressing comorbidities, including cardiovascular disease, chronic pain, diabetes, gastrointestinal issues, hyperthyroidism, and lung disease, all of which can be associated with anxiety. Once comorbidities are addressed, they advised caution given the lack of evidence for efficacy of both pharmacologic and nonpharmacologic anxiety treatments for PD patients. However, first-tier treatment for anxiety could include monotherapy with serotonin-norepinephrine reuptake inhibitors or selective serotonin reuptake inhibitors, they said.
PD patients with depression and anxiety also may benefit from nonpharmacologic interventions, including exercise, mindfulness, relaxation therapy, and cognitive behavioral therapy the researchers said.
Although the algorithm may not differ significantly from current treatment protocols, it highlights aspects unique to PD patients, the researchers said. In particular, the algorithm shows “that interventions used for motor symptoms, for example, dopamine agonists, may be especially potent for mood in the PD population and that augmentation strategies, such as antipsychotics and lithium, may not be well tolerated given their outsized risk of adverse events in PD,” they said.
“While an article of this kind cannot hope to address the gap in knowledge on comparative efficacy between interventions, it can guide readers on the best strategies for implementation and risk mitigation in PD – essentially focusing more on effectiveness,” they concluded.
The study received no outside funding. Dr. Pontone disclosed serving as a consultant for Acadia Pharmaceuticals and Concert Pharmaceuticals.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Long-acting injectable antipsychotics deserve first-line consideration
Long-acting injectable (LAI) antipsychotic therapies continue to be largely reserved for patients who already have adherence issues. But most patients, including first-episode patients, should be considering drugs with this mode of delivery for their broad array of advantages, according to an overview presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Due to the perception that long-acting injectables are for coercive applications, patients are not hearing about the many reasons this option might be preferable,” reported Diana Perkins, MD, MPH, professor, department of psychiatry, University of North Carolina, Chapel Hill.
According to Dr. Perkins, patients starting treatment for first-episode schizophrenia are particularly unlikely to even hear about injectable therapies even though “these might be the best candidates.”
The advantage of LAI in first-episode patients is that it takes adherence off the table as a risk for treatment failure. Ultimately, many patients educated about LAI in the context of other options, prefer LAI, according to Dr. Perkins, and she provided data to support these assertions.
Of several published articles reporting that patients fail to discuss LAI with patients, one was published last year (J Clin Psychopharmacol. 2020 Jul/Aug;40:346-9). For evidence that patients prefer LAI over pills for antipsychotic treatment, Dr. Perkins cited a study with data from more than 1,400 patients (Patient Prefer Adherence. 2020;14:1093-102).
In this latter analysis, 77% of patients preferred LAI over pills, Dr. Perkins reported at the virtual meeting, presented by MedscapeLive. Moreover, 50% of patients preferred every-3-month injections over monthly injections. For those who preferred LAI, the reasons included the convenience of avoiding daily therapy but also the empowerment derived from feeling healthier from not having to depend on a daily schedule of treatment.
LAI has benefits independent of adherence
“Some patients prefer injectables because the daily pills remind them of their illness even when they are feeling well,” Dr. Perkins said.
By eliminating pills and pill bottles, injections also provide a certain degree of confidentiality, said Dr. Perkins. She said that LAI, which avoids the peaks and troughs inherent in pill taking, provides more consistent drug levels even to the degree that doses can sometimes be lowered and adverse events reduced.
Yet, of all the reasons that patients might want to consider LAI, the most compelling is a lower risk of failure from inadequate adherence to daily pills. The evidence that patients do not take daily pills for chronic diseases, whether schizophrenia or any other illness that requires maintenance regimens for persistent disease control, is extensive and overwhelming, according to Dr. Perkins, who cited multiple studies.
For schizophrenia, with a relapsing and remitting pattern of symptoms, poor adherence is a particular risk. When symptoms abate, the cue and motivation for adherence dissipates.
“Most patients with schizophrenia already have some ambivalence about taking their medication.
When patients forget their daily pills or when the they decide to skip doses when they feel well, they do not necessarily tell their physicians.
Poor adherence often goes unrecognized
“Clinicians are not very good at estimating adherence in their patients,” Dr. Perkins said. While she listed several strategies to help patients adhere to daily pills, she also said that LAI should not be discounted as a means to circumvent this problem altogether.
Importantly, suboptimal adherence by itself places the patient at a high risk for relapse. In one study of partial adherence, delayed doses were associated with increased risk of hospitalization overall, but each increment in further delay led to still more risk (Psychiatr Serv. 2004;55:886-91).
Imperfect adherence to daily pills is very common. In one study evaluating 34,000 veterans with schizophrenia, the proportion with consistently good adherence over the 12 months of study was not quite 40% (J Clin Psychiatry. 2006 Oct;67[10]:1542-50). While most of the remaining were intermittently adherent, more than 15% of the populations was consistently poorly adherent.
Simple regimens and adherence closely linked
In general, the simpler the regimen, the greater the adherence, according to Dr. Perkins. For oral therapies, one pill per day is associated with greater adherence than is more than one. LAI, which is even simpler, is consistently associated with a large relative advantage. In one comparative study, 77% were adherent to LAI versus about 30% (P < .001) over a period of 12 months (Ment Health Clin. 2018 Mar 26;8[2]:56-62).
In a large recently published meta-analysis, LAI was associated with objective advantages over oral therapy (Lancet Psychiatry. 2021 May 1;8:[5]387-404). This included a statistically significant lower risk of hospitalizations or relapses for LAI over oral therapy whether the two modes of delivery were compared in randomized controls studies (RR 0.88; P = .033) or cohort studies (RR 0.92; P = .0044).
Overall, clinicians should discard several false assumptions about LAI, including the fact they are not appropriate in first-episode disease and that patients will not elect to take LAI if informed of the choices, according to Dr. Perkins. Rather than just listing LAI among options, Dr. Perkins suggested that clinicians should specifically explain the many advantages.
“When people say I do not like shots, this is not necessarily a no,” she said. If patients understand the potential for a reduced risk of relapse without having to take a daily pill, injections might be preferable whether or not they like shots in particular.
This is not an isolated view among experienced physicians. John M. Kane, MD, chairman of psychiatry, Zucker Hillside Hospital, Northwell Health, Glen Oaks, N.Y., also sees LAI as method of drug delivery that should be considered widely in schizophrenia.
“I am in complete agreement with Dr. Perkins that long-acting injectable formulations of antipsychotic medications should be presented routinely to patients and families as an option for illness management and relapse prevention,” said Dr. Kane, who was a coauthor of the meta-analysis published in Lancet Psychiatry.
“This would include patients early in the course of illness who currently have an unnecessarily high risk of relapse and hospitalization,” he added.
MedscapeLive and this news organization are owned by the same parent company. Dr. Perkins has a financial relationship with Alkermes. Dr. Kane has financial relationships with Abbott, AstraZeneca, Bristol-Myers Squibb, Janssen, Lilly, Otsuka, Pfizer, and Wyeth.
Long-acting injectable (LAI) antipsychotic therapies continue to be largely reserved for patients who already have adherence issues. But most patients, including first-episode patients, should be considering drugs with this mode of delivery for their broad array of advantages, according to an overview presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Due to the perception that long-acting injectables are for coercive applications, patients are not hearing about the many reasons this option might be preferable,” reported Diana Perkins, MD, MPH, professor, department of psychiatry, University of North Carolina, Chapel Hill.
According to Dr. Perkins, patients starting treatment for first-episode schizophrenia are particularly unlikely to even hear about injectable therapies even though “these might be the best candidates.”
The advantage of LAI in first-episode patients is that it takes adherence off the table as a risk for treatment failure. Ultimately, many patients educated about LAI in the context of other options, prefer LAI, according to Dr. Perkins, and she provided data to support these assertions.
Of several published articles reporting that patients fail to discuss LAI with patients, one was published last year (J Clin Psychopharmacol. 2020 Jul/Aug;40:346-9). For evidence that patients prefer LAI over pills for antipsychotic treatment, Dr. Perkins cited a study with data from more than 1,400 patients (Patient Prefer Adherence. 2020;14:1093-102).
In this latter analysis, 77% of patients preferred LAI over pills, Dr. Perkins reported at the virtual meeting, presented by MedscapeLive. Moreover, 50% of patients preferred every-3-month injections over monthly injections. For those who preferred LAI, the reasons included the convenience of avoiding daily therapy but also the empowerment derived from feeling healthier from not having to depend on a daily schedule of treatment.
LAI has benefits independent of adherence
“Some patients prefer injectables because the daily pills remind them of their illness even when they are feeling well,” Dr. Perkins said.
By eliminating pills and pill bottles, injections also provide a certain degree of confidentiality, said Dr. Perkins. She said that LAI, which avoids the peaks and troughs inherent in pill taking, provides more consistent drug levels even to the degree that doses can sometimes be lowered and adverse events reduced.
Yet, of all the reasons that patients might want to consider LAI, the most compelling is a lower risk of failure from inadequate adherence to daily pills. The evidence that patients do not take daily pills for chronic diseases, whether schizophrenia or any other illness that requires maintenance regimens for persistent disease control, is extensive and overwhelming, according to Dr. Perkins, who cited multiple studies.
For schizophrenia, with a relapsing and remitting pattern of symptoms, poor adherence is a particular risk. When symptoms abate, the cue and motivation for adherence dissipates.
“Most patients with schizophrenia already have some ambivalence about taking their medication.
When patients forget their daily pills or when the they decide to skip doses when they feel well, they do not necessarily tell their physicians.
Poor adherence often goes unrecognized
“Clinicians are not very good at estimating adherence in their patients,” Dr. Perkins said. While she listed several strategies to help patients adhere to daily pills, she also said that LAI should not be discounted as a means to circumvent this problem altogether.
Importantly, suboptimal adherence by itself places the patient at a high risk for relapse. In one study of partial adherence, delayed doses were associated with increased risk of hospitalization overall, but each increment in further delay led to still more risk (Psychiatr Serv. 2004;55:886-91).
Imperfect adherence to daily pills is very common. In one study evaluating 34,000 veterans with schizophrenia, the proportion with consistently good adherence over the 12 months of study was not quite 40% (J Clin Psychiatry. 2006 Oct;67[10]:1542-50). While most of the remaining were intermittently adherent, more than 15% of the populations was consistently poorly adherent.
Simple regimens and adherence closely linked
In general, the simpler the regimen, the greater the adherence, according to Dr. Perkins. For oral therapies, one pill per day is associated with greater adherence than is more than one. LAI, which is even simpler, is consistently associated with a large relative advantage. In one comparative study, 77% were adherent to LAI versus about 30% (P < .001) over a period of 12 months (Ment Health Clin. 2018 Mar 26;8[2]:56-62).
In a large recently published meta-analysis, LAI was associated with objective advantages over oral therapy (Lancet Psychiatry. 2021 May 1;8:[5]387-404). This included a statistically significant lower risk of hospitalizations or relapses for LAI over oral therapy whether the two modes of delivery were compared in randomized controls studies (RR 0.88; P = .033) or cohort studies (RR 0.92; P = .0044).
Overall, clinicians should discard several false assumptions about LAI, including the fact they are not appropriate in first-episode disease and that patients will not elect to take LAI if informed of the choices, according to Dr. Perkins. Rather than just listing LAI among options, Dr. Perkins suggested that clinicians should specifically explain the many advantages.
“When people say I do not like shots, this is not necessarily a no,” she said. If patients understand the potential for a reduced risk of relapse without having to take a daily pill, injections might be preferable whether or not they like shots in particular.
This is not an isolated view among experienced physicians. John M. Kane, MD, chairman of psychiatry, Zucker Hillside Hospital, Northwell Health, Glen Oaks, N.Y., also sees LAI as method of drug delivery that should be considered widely in schizophrenia.
“I am in complete agreement with Dr. Perkins that long-acting injectable formulations of antipsychotic medications should be presented routinely to patients and families as an option for illness management and relapse prevention,” said Dr. Kane, who was a coauthor of the meta-analysis published in Lancet Psychiatry.
“This would include patients early in the course of illness who currently have an unnecessarily high risk of relapse and hospitalization,” he added.
MedscapeLive and this news organization are owned by the same parent company. Dr. Perkins has a financial relationship with Alkermes. Dr. Kane has financial relationships with Abbott, AstraZeneca, Bristol-Myers Squibb, Janssen, Lilly, Otsuka, Pfizer, and Wyeth.
Long-acting injectable (LAI) antipsychotic therapies continue to be largely reserved for patients who already have adherence issues. But most patients, including first-episode patients, should be considering drugs with this mode of delivery for their broad array of advantages, according to an overview presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Due to the perception that long-acting injectables are for coercive applications, patients are not hearing about the many reasons this option might be preferable,” reported Diana Perkins, MD, MPH, professor, department of psychiatry, University of North Carolina, Chapel Hill.
According to Dr. Perkins, patients starting treatment for first-episode schizophrenia are particularly unlikely to even hear about injectable therapies even though “these might be the best candidates.”
The advantage of LAI in first-episode patients is that it takes adherence off the table as a risk for treatment failure. Ultimately, many patients educated about LAI in the context of other options, prefer LAI, according to Dr. Perkins, and she provided data to support these assertions.
Of several published articles reporting that patients fail to discuss LAI with patients, one was published last year (J Clin Psychopharmacol. 2020 Jul/Aug;40:346-9). For evidence that patients prefer LAI over pills for antipsychotic treatment, Dr. Perkins cited a study with data from more than 1,400 patients (Patient Prefer Adherence. 2020;14:1093-102).
In this latter analysis, 77% of patients preferred LAI over pills, Dr. Perkins reported at the virtual meeting, presented by MedscapeLive. Moreover, 50% of patients preferred every-3-month injections over monthly injections. For those who preferred LAI, the reasons included the convenience of avoiding daily therapy but also the empowerment derived from feeling healthier from not having to depend on a daily schedule of treatment.
LAI has benefits independent of adherence
“Some patients prefer injectables because the daily pills remind them of their illness even when they are feeling well,” Dr. Perkins said.
By eliminating pills and pill bottles, injections also provide a certain degree of confidentiality, said Dr. Perkins. She said that LAI, which avoids the peaks and troughs inherent in pill taking, provides more consistent drug levels even to the degree that doses can sometimes be lowered and adverse events reduced.
Yet, of all the reasons that patients might want to consider LAI, the most compelling is a lower risk of failure from inadequate adherence to daily pills. The evidence that patients do not take daily pills for chronic diseases, whether schizophrenia or any other illness that requires maintenance regimens for persistent disease control, is extensive and overwhelming, according to Dr. Perkins, who cited multiple studies.
For schizophrenia, with a relapsing and remitting pattern of symptoms, poor adherence is a particular risk. When symptoms abate, the cue and motivation for adherence dissipates.
“Most patients with schizophrenia already have some ambivalence about taking their medication.
When patients forget their daily pills or when the they decide to skip doses when they feel well, they do not necessarily tell their physicians.
Poor adherence often goes unrecognized
“Clinicians are not very good at estimating adherence in their patients,” Dr. Perkins said. While she listed several strategies to help patients adhere to daily pills, she also said that LAI should not be discounted as a means to circumvent this problem altogether.
Importantly, suboptimal adherence by itself places the patient at a high risk for relapse. In one study of partial adherence, delayed doses were associated with increased risk of hospitalization overall, but each increment in further delay led to still more risk (Psychiatr Serv. 2004;55:886-91).
Imperfect adherence to daily pills is very common. In one study evaluating 34,000 veterans with schizophrenia, the proportion with consistently good adherence over the 12 months of study was not quite 40% (J Clin Psychiatry. 2006 Oct;67[10]:1542-50). While most of the remaining were intermittently adherent, more than 15% of the populations was consistently poorly adherent.
Simple regimens and adherence closely linked
In general, the simpler the regimen, the greater the adherence, according to Dr. Perkins. For oral therapies, one pill per day is associated with greater adherence than is more than one. LAI, which is even simpler, is consistently associated with a large relative advantage. In one comparative study, 77% were adherent to LAI versus about 30% (P < .001) over a period of 12 months (Ment Health Clin. 2018 Mar 26;8[2]:56-62).
In a large recently published meta-analysis, LAI was associated with objective advantages over oral therapy (Lancet Psychiatry. 2021 May 1;8:[5]387-404). This included a statistically significant lower risk of hospitalizations or relapses for LAI over oral therapy whether the two modes of delivery were compared in randomized controls studies (RR 0.88; P = .033) or cohort studies (RR 0.92; P = .0044).
Overall, clinicians should discard several false assumptions about LAI, including the fact they are not appropriate in first-episode disease and that patients will not elect to take LAI if informed of the choices, according to Dr. Perkins. Rather than just listing LAI among options, Dr. Perkins suggested that clinicians should specifically explain the many advantages.
“When people say I do not like shots, this is not necessarily a no,” she said. If patients understand the potential for a reduced risk of relapse without having to take a daily pill, injections might be preferable whether or not they like shots in particular.
This is not an isolated view among experienced physicians. John M. Kane, MD, chairman of psychiatry, Zucker Hillside Hospital, Northwell Health, Glen Oaks, N.Y., also sees LAI as method of drug delivery that should be considered widely in schizophrenia.
“I am in complete agreement with Dr. Perkins that long-acting injectable formulations of antipsychotic medications should be presented routinely to patients and families as an option for illness management and relapse prevention,” said Dr. Kane, who was a coauthor of the meta-analysis published in Lancet Psychiatry.
“This would include patients early in the course of illness who currently have an unnecessarily high risk of relapse and hospitalization,” he added.
MedscapeLive and this news organization are owned by the same parent company. Dr. Perkins has a financial relationship with Alkermes. Dr. Kane has financial relationships with Abbott, AstraZeneca, Bristol-Myers Squibb, Janssen, Lilly, Otsuka, Pfizer, and Wyeth.
FROM CP/AACP PSYCHIATRY UPDATE
Telemedicine is poised to drive new models of care
Telemedicine has been proposed as a solution for an array of health care access problems over decades of gradual growth. The vast ramping up of , according to an update at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
“The cat is out of the bag,” said Jaspal Singh, MD, professor of medicine, Atrium Health, Charlotte, N.C. Due to changes in access and reimbursement to telemedicine driven by the pandemic, he said, “we now have permission to explore new models of care.”
Prior to February 2020, telemedicine was crawling forward at a leisurely pace, according to Dr. Singh. After March 2020, it broke into a run due to enormous demand and was met by a rapid response from the U.S. Congress. The first of four legislative bills that directly or indirectly supported telemedicine was passed on March 6, 2020.
The Centers for Medicare and Medicaid Services responded in kind, making modifications in a number of rules that removed obstacles to telehealth. One modification on April 6, 2020, for example, removed the requirement for a preexisting relationship between the clinician and patient, Dr. Singh said. The CMS also subsequently modified reimbursement policies in order to make telemedicine more tenable for physicians.
Given the risk of contagion from face-to-face encounters, telemedicine in the early days of the pandemic was not just attractive but the only practical and safe approach to medical care in many circumstances. Physicians and patients were anxious for health care that did not require in-office visits even though many critical issues for telemedicine, including its relative effectiveness, had not yet been fully evaluated.
Much has been learned regarding the feasibility and acceptability of telemedicine during the pandemic, but Dr. Singh noted that quality of care relative to in-person visits remains weakly supported for most indications. Indeed, he outlined sizable list of incompletely resolved issues, including optimal payment models, management of privacy concerns, and how to balance advantages to disadvantages.
For patients and physicians, the strengths of telemedicine include greater convenience made possible by the elimination of travel and waiting rooms. For the health care system, it can include less infrastructure and overhead. For many physicians, telemedicine might be perceived as more efficient.
On the other hand, some patients might feel that a clinical encounter is incomplete without a physical examination even when the physician does not feel the physical examination is needed, according to Dr. Singh. He cited a survey suggesting nearly half of patients expressed concern about a lack of connection to health care providers following a virtual visit.
In the same 2020 National Poll on Healthy Aging 2020 survey conducted by the University of Michigan 67% of respondents reported that the quality of care was not as good as that provided by in-patient visits, and 24% expressed concern about privacy. However, at the time the poll was taken in May 2020, experience with telemedicine among many of the respondents may have been limited. As telemedicine is integrated into routine care, perceptions might change as experience increases.
A distinction between telemedicine in routine care and telemedicine as a strategy to respond to a pandemic is important, Dr. Singh indicated. Dr. Singh was the lead author for a position paper on telemedicine for the diagnosis and treatment of sleep disorders from the American Academy of Sleep Medicine 5 years ago, but he acknowledged that models of care might differ when responding to abnormal surges in health care demand.
The surge in demand for COVID-19–related care engendered numerous innovative solutions. As examples, Dr. Singh recounted how a virtual hospital was created at his own institution. In a published study, 1,477 patients diagnosed with COVID-19 over a 6-week period remained at home and received care in a virtual observation unit (VCU) or a virtual acute care unit (VACU) . Only a small percentage required eventual hospital admission. In the VACU, patients were able to receive advanced care including IV fluids and some form of respiratory support .
It is unclear how the COVID-19 pandemic will change telemedicine. Now, with declining cases of the infection, telemedicine is back to a walk after the sprint required during the height of the pandemic, according to Dr. Singh. However, Dr. Singh thinks many physicians and patients will have a different perception of telemedicine after the widespread exposure to this type of care.
In terms of the relative role of in-patient and virtual visits across indications, “we do not know how this will play out, but we will probably end up toggling between the two,” Dr. Singh said.
This is an area that is being followed closely by the CHEST Health Policy and Advocacy Committee, according to Kathleen Sarmiento, MD, director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System. A member of that committee and moderator of the session in which Dr. Singh spoke,
Dr. Sarmiento called the effort to bring permanent coverage of telehealth services “the shared responsibility of every medical society engaged in advocacy.”
However, she cautioned that there might be intended and unintended consequences from telehealth that require analysis to develop policies that are in the best interests of effective care. She said, the “ACCP, along with its sister societies, does have a role in supporting the evaluation of the impact of these changes on both patients and providers in the fields of pulmonary medicine, critical care, and sleep medicine.”
Dr. Singh reports a financial relationship with AstraZeneca. Dr. Sarmiento reports no relevant financial relationship with AstraZeneca.
Telemedicine has been proposed as a solution for an array of health care access problems over decades of gradual growth. The vast ramping up of , according to an update at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
“The cat is out of the bag,” said Jaspal Singh, MD, professor of medicine, Atrium Health, Charlotte, N.C. Due to changes in access and reimbursement to telemedicine driven by the pandemic, he said, “we now have permission to explore new models of care.”
Prior to February 2020, telemedicine was crawling forward at a leisurely pace, according to Dr. Singh. After March 2020, it broke into a run due to enormous demand and was met by a rapid response from the U.S. Congress. The first of four legislative bills that directly or indirectly supported telemedicine was passed on March 6, 2020.
The Centers for Medicare and Medicaid Services responded in kind, making modifications in a number of rules that removed obstacles to telehealth. One modification on April 6, 2020, for example, removed the requirement for a preexisting relationship between the clinician and patient, Dr. Singh said. The CMS also subsequently modified reimbursement policies in order to make telemedicine more tenable for physicians.
Given the risk of contagion from face-to-face encounters, telemedicine in the early days of the pandemic was not just attractive but the only practical and safe approach to medical care in many circumstances. Physicians and patients were anxious for health care that did not require in-office visits even though many critical issues for telemedicine, including its relative effectiveness, had not yet been fully evaluated.
Much has been learned regarding the feasibility and acceptability of telemedicine during the pandemic, but Dr. Singh noted that quality of care relative to in-person visits remains weakly supported for most indications. Indeed, he outlined sizable list of incompletely resolved issues, including optimal payment models, management of privacy concerns, and how to balance advantages to disadvantages.
For patients and physicians, the strengths of telemedicine include greater convenience made possible by the elimination of travel and waiting rooms. For the health care system, it can include less infrastructure and overhead. For many physicians, telemedicine might be perceived as more efficient.
On the other hand, some patients might feel that a clinical encounter is incomplete without a physical examination even when the physician does not feel the physical examination is needed, according to Dr. Singh. He cited a survey suggesting nearly half of patients expressed concern about a lack of connection to health care providers following a virtual visit.
In the same 2020 National Poll on Healthy Aging 2020 survey conducted by the University of Michigan 67% of respondents reported that the quality of care was not as good as that provided by in-patient visits, and 24% expressed concern about privacy. However, at the time the poll was taken in May 2020, experience with telemedicine among many of the respondents may have been limited. As telemedicine is integrated into routine care, perceptions might change as experience increases.
A distinction between telemedicine in routine care and telemedicine as a strategy to respond to a pandemic is important, Dr. Singh indicated. Dr. Singh was the lead author for a position paper on telemedicine for the diagnosis and treatment of sleep disorders from the American Academy of Sleep Medicine 5 years ago, but he acknowledged that models of care might differ when responding to abnormal surges in health care demand.
The surge in demand for COVID-19–related care engendered numerous innovative solutions. As examples, Dr. Singh recounted how a virtual hospital was created at his own institution. In a published study, 1,477 patients diagnosed with COVID-19 over a 6-week period remained at home and received care in a virtual observation unit (VCU) or a virtual acute care unit (VACU) . Only a small percentage required eventual hospital admission. In the VACU, patients were able to receive advanced care including IV fluids and some form of respiratory support .
It is unclear how the COVID-19 pandemic will change telemedicine. Now, with declining cases of the infection, telemedicine is back to a walk after the sprint required during the height of the pandemic, according to Dr. Singh. However, Dr. Singh thinks many physicians and patients will have a different perception of telemedicine after the widespread exposure to this type of care.
In terms of the relative role of in-patient and virtual visits across indications, “we do not know how this will play out, but we will probably end up toggling between the two,” Dr. Singh said.
This is an area that is being followed closely by the CHEST Health Policy and Advocacy Committee, according to Kathleen Sarmiento, MD, director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System. A member of that committee and moderator of the session in which Dr. Singh spoke,
Dr. Sarmiento called the effort to bring permanent coverage of telehealth services “the shared responsibility of every medical society engaged in advocacy.”
However, she cautioned that there might be intended and unintended consequences from telehealth that require analysis to develop policies that are in the best interests of effective care. She said, the “ACCP, along with its sister societies, does have a role in supporting the evaluation of the impact of these changes on both patients and providers in the fields of pulmonary medicine, critical care, and sleep medicine.”
Dr. Singh reports a financial relationship with AstraZeneca. Dr. Sarmiento reports no relevant financial relationship with AstraZeneca.
Telemedicine has been proposed as a solution for an array of health care access problems over decades of gradual growth. The vast ramping up of , according to an update at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
“The cat is out of the bag,” said Jaspal Singh, MD, professor of medicine, Atrium Health, Charlotte, N.C. Due to changes in access and reimbursement to telemedicine driven by the pandemic, he said, “we now have permission to explore new models of care.”
Prior to February 2020, telemedicine was crawling forward at a leisurely pace, according to Dr. Singh. After March 2020, it broke into a run due to enormous demand and was met by a rapid response from the U.S. Congress. The first of four legislative bills that directly or indirectly supported telemedicine was passed on March 6, 2020.
The Centers for Medicare and Medicaid Services responded in kind, making modifications in a number of rules that removed obstacles to telehealth. One modification on April 6, 2020, for example, removed the requirement for a preexisting relationship between the clinician and patient, Dr. Singh said. The CMS also subsequently modified reimbursement policies in order to make telemedicine more tenable for physicians.
Given the risk of contagion from face-to-face encounters, telemedicine in the early days of the pandemic was not just attractive but the only practical and safe approach to medical care in many circumstances. Physicians and patients were anxious for health care that did not require in-office visits even though many critical issues for telemedicine, including its relative effectiveness, had not yet been fully evaluated.
Much has been learned regarding the feasibility and acceptability of telemedicine during the pandemic, but Dr. Singh noted that quality of care relative to in-person visits remains weakly supported for most indications. Indeed, he outlined sizable list of incompletely resolved issues, including optimal payment models, management of privacy concerns, and how to balance advantages to disadvantages.
For patients and physicians, the strengths of telemedicine include greater convenience made possible by the elimination of travel and waiting rooms. For the health care system, it can include less infrastructure and overhead. For many physicians, telemedicine might be perceived as more efficient.
On the other hand, some patients might feel that a clinical encounter is incomplete without a physical examination even when the physician does not feel the physical examination is needed, according to Dr. Singh. He cited a survey suggesting nearly half of patients expressed concern about a lack of connection to health care providers following a virtual visit.
In the same 2020 National Poll on Healthy Aging 2020 survey conducted by the University of Michigan 67% of respondents reported that the quality of care was not as good as that provided by in-patient visits, and 24% expressed concern about privacy. However, at the time the poll was taken in May 2020, experience with telemedicine among many of the respondents may have been limited. As telemedicine is integrated into routine care, perceptions might change as experience increases.
A distinction between telemedicine in routine care and telemedicine as a strategy to respond to a pandemic is important, Dr. Singh indicated. Dr. Singh was the lead author for a position paper on telemedicine for the diagnosis and treatment of sleep disorders from the American Academy of Sleep Medicine 5 years ago, but he acknowledged that models of care might differ when responding to abnormal surges in health care demand.
The surge in demand for COVID-19–related care engendered numerous innovative solutions. As examples, Dr. Singh recounted how a virtual hospital was created at his own institution. In a published study, 1,477 patients diagnosed with COVID-19 over a 6-week period remained at home and received care in a virtual observation unit (VCU) or a virtual acute care unit (VACU) . Only a small percentage required eventual hospital admission. In the VACU, patients were able to receive advanced care including IV fluids and some form of respiratory support .
It is unclear how the COVID-19 pandemic will change telemedicine. Now, with declining cases of the infection, telemedicine is back to a walk after the sprint required during the height of the pandemic, according to Dr. Singh. However, Dr. Singh thinks many physicians and patients will have a different perception of telemedicine after the widespread exposure to this type of care.
In terms of the relative role of in-patient and virtual visits across indications, “we do not know how this will play out, but we will probably end up toggling between the two,” Dr. Singh said.
This is an area that is being followed closely by the CHEST Health Policy and Advocacy Committee, according to Kathleen Sarmiento, MD, director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System. A member of that committee and moderator of the session in which Dr. Singh spoke,
Dr. Sarmiento called the effort to bring permanent coverage of telehealth services “the shared responsibility of every medical society engaged in advocacy.”
However, she cautioned that there might be intended and unintended consequences from telehealth that require analysis to develop policies that are in the best interests of effective care. She said, the “ACCP, along with its sister societies, does have a role in supporting the evaluation of the impact of these changes on both patients and providers in the fields of pulmonary medicine, critical care, and sleep medicine.”
Dr. Singh reports a financial relationship with AstraZeneca. Dr. Sarmiento reports no relevant financial relationship with AstraZeneca.
FROM A HEALTH POLICY AND ADVOCACY CONFERENCE