User login
Hospitalist System Performance in Taiwan
In Taiwan, the national health insurance (NHI) implemented since 19951 has extended its coverage to almost the entire population. It may serve as a model for other countries looking to implement a universal health insurance system.2, 3 However, due to the low copayment for services, there are increasing admission rates and hospitalizations.2, 4 Admission rates, in particular, have nearly tripled for those who have been previously uninsured prior to the NHI program.2 In terms of hospital care, internal medicine and surgery are not favorite areas of specialty in the NHI system because inpatient care has a high workload but relatively low salaries.2, 5, 6 Consequently, there is now a shortage of primary inpatient care staff in Taiwan. The hospitalist system may be a solution to this problem.
The role of a hospitalist system has been discussed since 1996.7 Although its pros and cons are still debatable,8 the hospitalist system has grown in recent decades and there is a wide acceptance that hospitalists can efficiently care for inpatients.4, 9, 10 However, most related studies are in Western countries.4, 6, 11 It has rarely been studied in Asian countries and in those with NHI programs.
This study therefore aimed to investigate whether the hospitalist system, working within the NHI system in Taiwan, can be efficient in saving costs, maintaining quality care, and managing a high volume of in patients.
Materials and Methods
This prospective observational study was conducted in the National Taiwan University Hospital (NTUH), a tertiary‐care referral center in northern Taiwan, and approved by the hospital's Institutional Review Board. The program was also registered on Clinicaltrial.gov (identifier NCT00997646). A 36‐bed hospitalist‐run ward (HW) was set up in October 2009 in NTUH. For performance comparison, two 36‐bed internist‐run wards (IWs) were selected. The three wards were geographically separated.
Study Subjects
All patients age >18 years from the emergency department (ED) were admitted into one of the three wards based on the diagnosis category determined by the ED physicians. A patient was admitted by bed managers who were blinded to the study. Cases were categorized as diseases of general medicine, such as congestive heart failure, pneumonia, exacerbation of chronic obstructive pulmonary disease, cellulitis, ischemic stroke, urinary tract infection, and gastrointestinal bleeding.
Patients with severe illnesses requiring admission to intensive care units were excluded. Research assistants who were blinded to the patient stratification performed the patients' identification and data collection. Patient care was determined by the respective medical teams without any interference from this study.
Care‐Team Structure
The HW was set up with 3 attending physicians certified by a board of internal medicine and 6 nurse practitioners. All staff members worked full‐time to provide primary inpatient care. For comparison (Table 1), each IW had a set‐up of 3 attending physicians licensed by a board of internal medicine, one chief resident, 3 junior residents, and 3 interns. The attending physicians of the IWs visited their inpatients every workday and delegated primary care to residents on night shifts and weekends.
| Hospitalist‐Run Ward | Internist‐Run Wards | |
|---|---|---|
| ||
| Team member, per ward | 3 AP, 6 NP | 3 AP, 1 CR, 3 JR, 3 intern |
| Beds, per ward | 36 | 36 |
| Inpatient care of AP | Full time | Once daily |
| Who prescribes care order? | AP | AP, CR, JR |
| Who executes order? | NP | JR, intern |
| AP duty | Inpatient care; research | Inpatient/outpatient care; work of subspecialty; research |
| Bed manager | NP/AP | CR |
Clinical Characteristics
The patients' clinical characteristics, laboratory data, hospital course, and outcomes were recorded. The clinical characteristics included age, gender, underlying comorbidities, activities of daily living, and admission diagnosis. Charlson scores and Barthel's scores represented underlying comorbidities and activities of daily living, respectively. These were calculated as described in previous studies.11, 12 Admission costs paid for by the Taiwan NHI was defined as an inpatient's expenditure paid to the hospital by the institute of NHI. Total admission cost included expenses paid for by NHI and the patient's out‐of‐pocket expenditure not covered by NHI. A primary care physician was defined if the patient had visited the same doctor's clinic three times or more within one year prior to admission.8 Patients were followed‐up for 30 days after discharge by telephone, or until readmission.
Propensity Score Methods
Propensity score‐matching was used to balance observed covariates between the 2 care groups. It was defined as the conditional probability for being admitted to the HW, as a binary dependent variable, under a set of measurements. Factors that were significantly different (P < 0.05) between the 2 groups in univariate analysis were included in a multivariable logistic regression model to predict HW admission. The predicted probability derived from the logistic equation was used as the propensity score for each individual.
Patients in the HW and IWs were pooled and sorted according to their propensity score in ascending order. The selection process began from the first two cases with the lowest propensity score. If one was admitted to the HW and the other to an IW, both were selected as a matched pair. If this was not the case, then four cases were included. If there were two HW patients and two IW cases, the four were selected as two matched pairs. In the same way, HW and IW cases were matched by their propensity score in 1:1, 2:2, or 3:3 blocks. A patient who did not have a suitable match within the acceptable rank range was excluded from further analysis. The matching process moved down the sort list until all possible matched pairs were included and the selected patients formed a matched 1:1 pair in both groups.
Statistical Analysis
Intergroup differences were compared using independent t test for numerical variables and chi‐square test for categorical variables. Curves of probability of staying in the hospital within 30 days were generated using the Kaplan‐Meier method and compared using the log‐rank test. A logistic regression model was used for the propensity score match using the SPSS software version 13.0 (SPSS, Chicago, IL). The probability that indicated patient admission to the HW in both groups was used to draw box‐plots. After the 1:1 matched groups were assembled, the clinical characteristics were compared accordingly.
Results
From November 2009 to January 2010, 810 patients admitted from the ED to the study wards were enrolled. Among them, 377 were admitted to the HW and 433 to the IWs. Analysis of admission days showed that 84 (22%) and 53 (12%) patients were admitted to the HW and IWs, respectively, on weekends (P < 0.001).
Compared to the IW patients, the HW patients were older (age >65 years) and had poorer functional status by Barthel's scores (Table 2). Admission diagnosis was similar in both groups, except for pneumonia and urinary tract infection, which were higher in the HW patients. There was a primary care physician in 242 (64%) HW and 282 (65%) IW patients (P = 0.781).
The Charlson score, representing underlying comorbidity, was higher in the HW group (P = 0.002). Moreover, patients with severe liver cirrhosis (Child‐Pugh class C) were more frequently admitted to the HW (P = 0.018). Underlying malignancy, severe chronic kidney disease (estimated creatinine clearance <30 mL/min), and chronic respiratory failure requiring mechanical ventilator support were more associated with HW admission, although not statistically significantly (P = 0.064, 0.072, and 0.104, respectively).
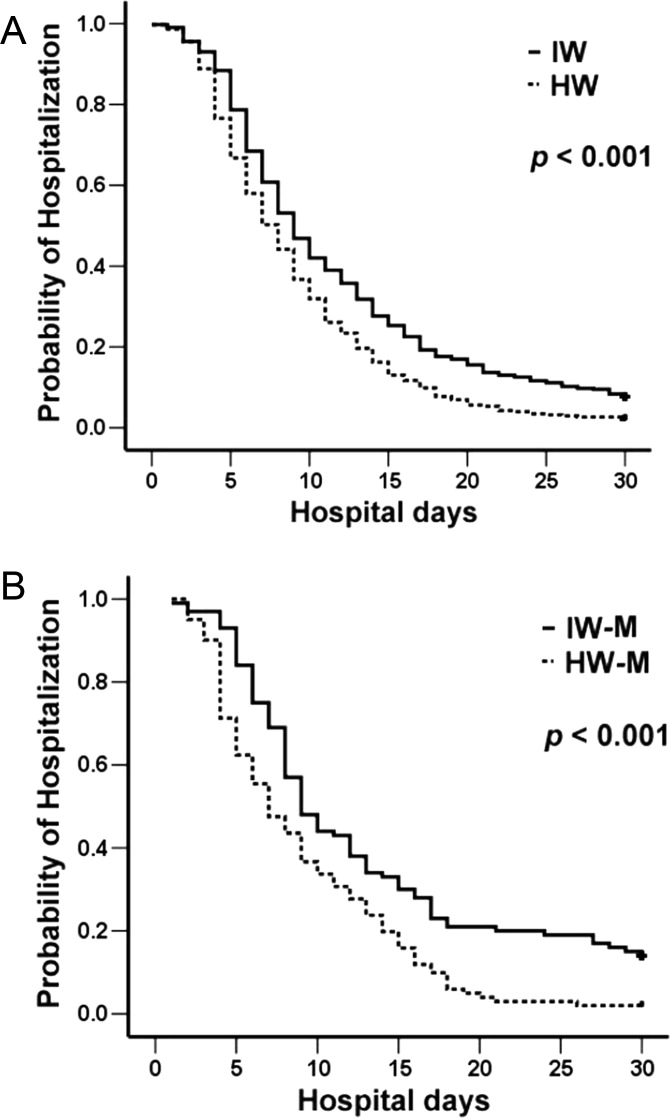
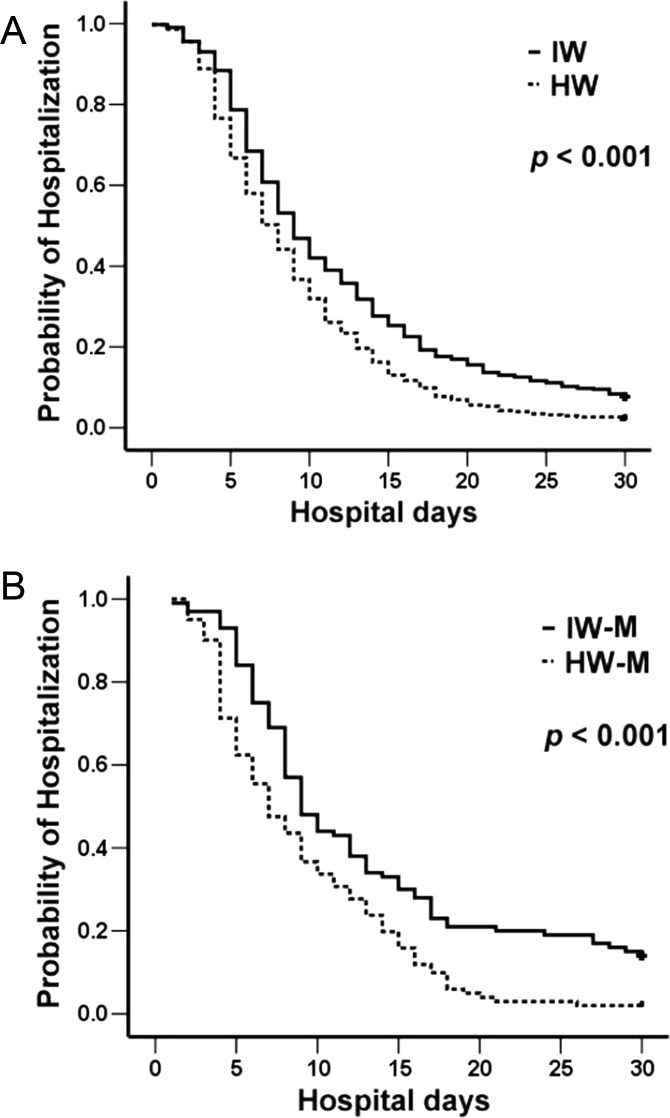
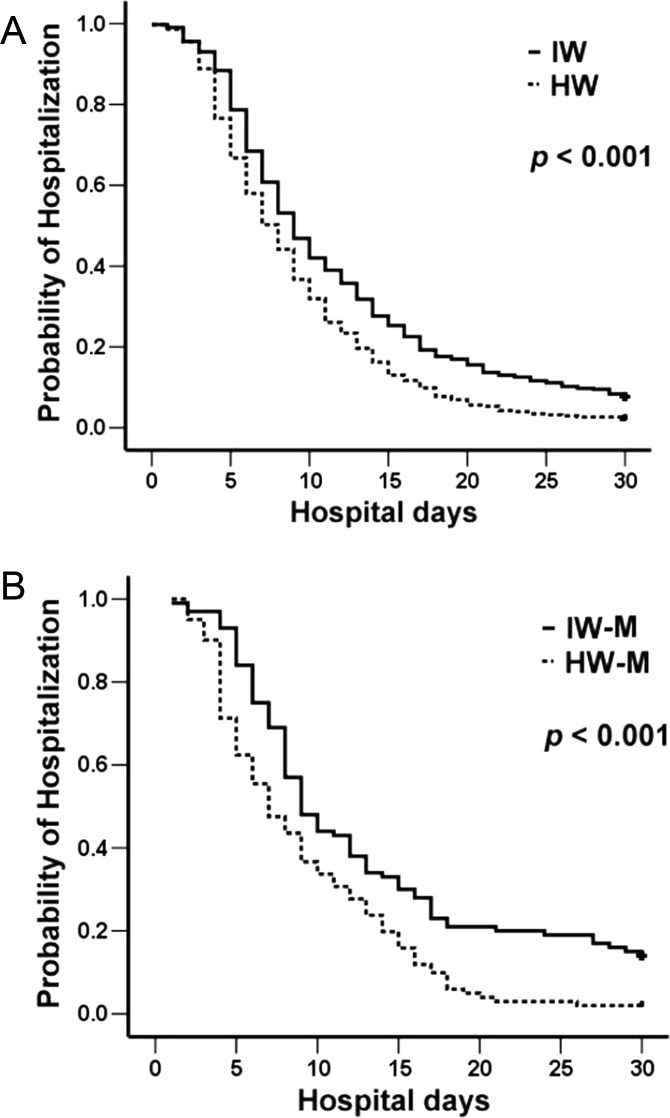
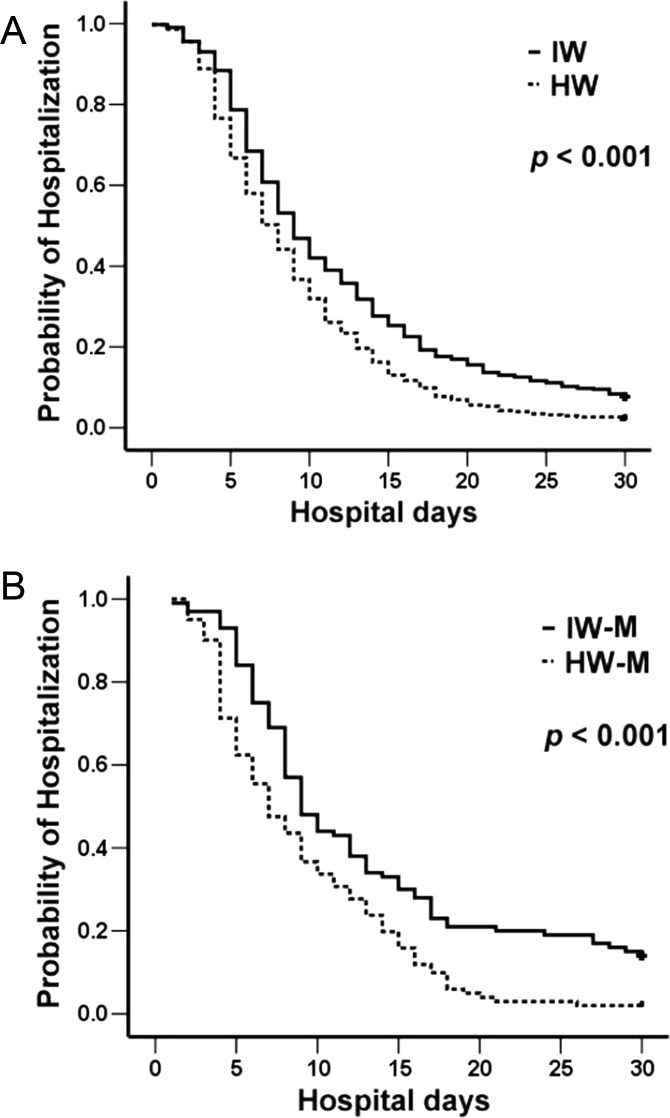
The average admission cost was lower in HW patients than in IW patients, whether paid for by NHI ($1640.2 vs $2933.8 per patient, P = 0.001) or by the total admission cost ($2223.4 vs $3700.8 per patient, P = 0.001) (Table 3). Similarly, there was a shorter average length of stay (LOS) in the HW patients (9.3 vs 13.1 days, P < 0.001), who were discharged earlier than IW patients (Figure 1A). Regarding cost per patient‐day, the total daily cost was similar between the two groups (P = 0.560).
| Hospitalist‐Run Ward (n = 377) | Internist‐Run Wards (n = 433) | P‐Value | |
|---|---|---|---|
| |||
| Age >65 years old | 237 (63) | 240 (55) | 0.032 |
| Gender, male | 210 (56) | 243 (56) | 0.905 |
| Barthel's score | 61 35 | 70 33 | <0.001 |
| Charlson score | 3.7 3.4 | 3.0 3.2 | 0.002 |
| Admission diagnosis | |||
| Pneumonia | 106 (28) | 88 (20) | 0.010 |
| Exacerbation of COPD | 18 (5) | 15 (3) | 0.347 |
| Congestive heart failure | 12 (3) | 19 (4) | 0.373 |
| Upper gastrointestinal bleeding | 55 (15) | 58 (13) | 0.625 |
| Intra‐abdominal infection | 36 (10) | 47 (11) | 0.541 |
| Urinary tract infection | 85 (23) | 69 (16) | 0.017 |
| Cellulitis | 20 (5) | 18 (4) | 0.441 |
| Ischemic stroke | 12 (3) | 21 (5) | 0.231 |
| Others* | 117 (31) | 164 (38) | 0.041 |
| Laboratory data in the initial admission | |||
| Leukocyte count, /L | 11372 7962 | 10377 6422 | 0.050 |
| Hemoglobin, g/dL | 12.7 12.8 | 12.3 8.6 | 0.714 |
| Platelet count, K/L | 219 124 | 205 108 | 0.102 |
| Blood urea nitrogen, mg/dL | 33.2 27.7 | 24.1 17.4 | <0.001 |
| Creatinine, mg/dL | 1.9 2.9 | 1.6 2.8 | 0.080 |
| Total bilirubin, mg/dL | 2.2 3.7 | 2.3 3.6 | 0.826 |
| C‐reactive protein, mg/dL | 8.0 7.7 | 6.0 6.4 | 0.008 |
More patients in the HW group signed the do‐not‐resuscitate (DNR) consent (P < 0.001) and died during the hospital course, although the difference was not statistically significant (P = 0.068). Among those who expired during hospitalization, DNR consent was signed by 42 (90%) HW and 27 (68%) IW patients (P = 0.014). Among those discharged, 57 (17.2%) HW and 70 (17.6%) IW patients were lost to follow‐up. There was no difference in the 30‐day readmission for any cause between the two groups (P = 0.992).
Due to baseline differences, propensity score‐matching was performed and 101 pairs of patients were selected according to the probability generated from factors significantly different in univariate analysis (ie, age >65 years, pneumonia or urinary tract infections, Charlson score, Barthel's score, and blood urea nitrogen and C‐reactive protein levels on initial admission). The clinical characteristics of the 202 patients were shown in Table 4.
| Hospitalist‐Run Ward (n = 377) | Internist‐Run Wards (n = 433) | P‐Value | |
|---|---|---|---|
| |||
| Length of hospital stay, days | 9.3 6.7 | 13.1 12.4 | <0.001 |
| Total admission cost: $ per patient | 2223.4 3428.2 | 3700.8 8010.7 | 0.001 |
| Admission cost paid by NHI: $ per patient | 1640.2 2403.3 | 2933.8 7460.7 | 0.001 |
| In‐hospital mortality | 47 (12) | 37 (9) | 0.068 |
| Do‐not‐resuscitate consent | 74 (20) | 34 (8) | <0.001 |
| 30‐Day readmission* | 71 (22) | 83 (21) | 0.922 |
| Hospitalist‐Run Ward (n = 101) | Internist‐Run Wards (n = 101) | P‐Value | |
|---|---|---|---|
| |||
| Age >65 years old | 59 (58) | 59 (58) | 1.000 |
| Gender, Male | 55 (54) | 50 (50) | 0.481 |
| Barthel's score | 66 34 | 65 35 | 0.897 |
| Charlson score | 3.2 3.2 | 3.6 3.5 | 0.437 |
| Admission diagnosis | |||
| Pneumonia | 31 (31) | 27 (27) | 0.534 |
| Exacerbation of COPD | 4 (4) | 5 (5) | 0.733 |
| Congestive heart failure | 2 (2) | 2 (2) | 1.000 |
| Gastrointestinal bleeding | 10 (10) | 8 (8) | 0.621 |
| Intra‐abdominal infection | 18 (18) | 10 (10) | 0.103 |
| Urinary tract infection | 22 (22) | 21 (21) | 0.864 |
| Cellulitis | 6 (6) | 5 (5) | 0.757 |
| Ischemic stroke | 2 (2) | 0 | 0.155 |
| Others* | 39 (39) | 30 (30) | 0.182 |
| Laboratory data in the initial admission | |||
| Leukocyte count, /L | 12487 6288 | 11430 7718 | 0.287 |
| Hemoglobin, g/dL | 12.8 13.7 | 12.5 7.5 | 0.803 |
| Platelet count, K/L | 212 102 | 207 103 | 0.710 |
| Blood urea nitrogen, mg/dL | 25.5 19.7 | 24.7 17.5 | 0.773 |
| Creatinine, mg/dL | 1.5 1.2 | 1.6 1.5 | 0.979 |
| Total bilirubin, mg/dL | 2.0 7.0 | 2.0 6.9 | 0.963 |
| C‐reactive protein, mg/dL | 6.9 7.7 | 7.0 6.4 | 0.859 |
| Length of hospital stay, days | 9.2 6.4 | 15.2 13.8 | <0.001 |
| Do‐not‐resuscitate consent | 18 (18) | 6 (6) | 0.009 |
| Total admission cost: $ per patient | 2019.4 1709.3 | 5608.9 14244.8 | 0.013 |
| Cost paid by NHI: $ per patient | 1463.4 1404.6 | 4665.8 13553.3 | 0.019 |
| In‐hospital mortality | 9 (9) | 7 (7) | 0.602 |
| 30‐Day postdischarge readmission | 17 (18) | 21 (22) | 0.492 |
Both groups had almost the same propensity scores (P = 0.970; see online Supporting Information). Patients in the HW group had significantly lower admission cost, shorter LOS (Figure 1B), and more DNR consent, but similar in‐hospital mortality and readmission rates (Table 4).
DISCUSSION
The hospitalist system, which has been practiced for years in the United States, has not really been reported in Asia.13 Under the universal NHI system, this system has been studied in terms of treating patients in a Taiwan referral center. This study is the first to report on a hospitalist system in an Asian country with an NHI program. The hospitalist system in this study demonstrates efficient performance even though the patients have multiple comorbidities, compared to those in the general medical wards. By propensity score‐matching, admission costs of the hospitalist‐run ward are significantly lower than those of the internist‐run wards despite similar mortality and readmission rates.
The average LOS is reduced by 29% in HW patients and this plays a major role in cost reduction.14, 15 The reason may be the hospitalist's full‐time care, which allows for prompt decision‐making and close interaction with the patients' families.16 These families thus understand the treatment planning and prognosis. Furthermore, the hospitalist system continues working on weekends. As a result, patients are discharged without delay, even on holidays.
The aim of reducing LOS and costs is important because hospital income will decrease under the payment by disease‐related group (DRG) being implemented by the NHI system.17 A shortage of inpatient physicians may also develop due to the high workload but relatively low remuneration.2, 18 In contrast, a hospitalist care system that integrates nurse practitioners demands less human resources and saves on costs. In the future, it may be one of the solutions for hospitals aiming to maintain financial balance.
Another important issue in the NHI coverage is the increasing number of patients in the ED, which seems to be overflowing.19 In a previous Taiwan report, there are 7.1 patients per day who are staying in the ED for more than 72 hours, despite indications for admission.20 The delay is possibly due to the lack of available beds in the inpatient department.21 Amidst increasing demands for admission under the NHI and an aging society,2, 20 experience suggests that a hospitalist care system is a promising alternative to address the high ED patient volumes, especially on holidays. Howell et al. have also demonstrated that hospitalist‐driven bed management enhances the bed utility rate.21, 22 Since the current study also shows reduced LOS in the HW, patients will have a faster turn‐over rate and thereby assist in alleviating ED overcrowding.
Although the LOS of the patients here is comparable to that reported by the Taiwan NHI,2 it is far longer than that reported in the United States (around 4.75.2 days).4, 23 One possible explanation is the social and cultural determinants, including hospital‐ or physician‐dependence.24 In literature from Japan and Taiwan, hospitalization is as long as 13 weeks.25, 26 In addition, the average admission cost is reportedly around $1540 per patient‐day in the US, around 6 times that in this study ($266.6 per patient‐day).4 In the aging society of Taiwan,27 the NHI‐required copayment for admission may be relatively low, such that patients (or their families) may be misled that hospital care is better and hesitate to be discharged.2830
Regarding quality of care and patient safety, the in‐hospital mortality and the 30‐day readmission rates are similar in both groups, although disease severity and underlying comorbidities are worse in the HW at the start. This is consistent with previous reports that hospitalists can manage inpatient as well as internist care systems.4, 23 However, because this study has been performed in a tertiary referral center, patients may be more severely ill, such that the inpatient mortality and 30‐day readmission rates are as high as 10.3% and 21.11%, respectively.31, 32 Nonetheless, generalizing the hospitalist system to regional or district hospitals remains a concern, and this warrants further study.
This study has two other limitations. First, it is an observational study and patients have different demographics even though propensity score‐matching has been performed. Second, the patients were hospitalized without a standardized treatment protocol.
In conclusion, under the NHI system in Taiwan, a hospitalist system can have higher efficiency in shortening LOS and reducing cost than an internist care system, and still have similar hospital mortality and readmission rates. A hospitalist system may address the issue of high patient volume by increasing ward utilization. It can be recommended in a country with NHI that has a shortage of inpatient care staff.
- ,,,.Health system reform in the Republic of China. Formulating policy in a market‐based health system.JAMA.1995;273:777–781.
- ,,.A 10‐year experience with universal health insurance in Taiwan: measuring changes in health and health disparity.Ann Intern Med.2008;148:258–267.
- ,.Learning from Taiwan: experience with universal health insurance.Ann Intern Med.2008;148:313–314.
- ,,,,,.Outcomes of care by hospitalists, general internists, and family physicians.N Engl J Med.2007;357:2589–2600.
- ,.The effect of universal health insurance on health care utilization in Taiwan. Results from a natural experiment.JAMA.1997;278:89–93.
- ,,,,,.The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: a path analysis.Ind Health.2009;47:166–172.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,,.Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301:1671–1680.
- ,,,,.Hospitalists and the quality of care in hospitals.Arch Intern Med.2009;169:1389–1394.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360:1102–1112.
- ,,,,.The use of Charlson comorbidity index for patients revisiting the emergency department within 72 hours.Chang Gung Med J.2007;30:437–444.
- ,,,.Reliability of the Barthel Index when used with older people.Age Ageing.2005;34:228–232.
- .The hospitalist movement—a complex adaptive response to fragmentation of care in hospitals.Ann Acad Med Singapore.2008;37:145–150.
- ,,,,,.Determinants of hospitalist efficiency: a qualitative and quantitative study.Med Care Res Rev.2009;66:682–702.
- .The critical role of hospitalists in controlling healthcare costs.J Hosp Med.2010;5:127–132.
- .The relationship between hospitalists and primary care physicians.Ann Intern Med.2010;152:474.
- ,,,,,.Using diagnosis‐related groups. The situation in the United Kingdom National Health Service and in Germany.Eur J Health Econ.2004;5:287–289.
- ,,,,.Factors influencing medical students' choice of specialty.J Formos Med Assoc.2006;105:489–496.
- ,,,,.Factors associated with frequent use of emergency services in a medical center.J Formos Med Assoc.2003;102:222–228.
- ,,, et al.ED overcrowding in Taiwan: facts and strategies.Am J Emerg Med.1999;17:198–202.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–811.
- ,,,.Hospitalist bed management effecting throughput from the emergency department to the intensive care unit.J Crit Care.2010;25:184–189.
- ,,,.A comparison of two hospitalist models with traditional care in a community teaching hospital.Am J Med.2005;118:536–543.
- ,,,.Factors associated with tocolytic hospitalizations in Taiwan: evidence from a population‐based and longitudinal study from 1997 to 2004.BMC Pregnancy Childbirth.2009;9:59.
- ,,.Complicated parapneumonic effusion and empyema in children.J Microbiol Immunol Infect.2006;39:483–488.
- ,,, et al.Efficacy of corticosteroids in the treatment of community‐acquired pneumonia requiring hospitalization.Lung.2007;185:249–255.
- ,,.Analysis of population projections for Taiwan area: 2008 to 2056.Taiwan Economic Forum.2009;7:36–69.
- ,,,,.Why Taiwanese hospice patients want to stay in hospital: health‐care professionals' beliefs and solutions.Support Care Cancer.2004;12:285–292.
- ,,.Patient characteristics predict occurrence and outcome of complaints against physicians: a study from a medical center in central Taiwan.J Formos Med Assoc.2009;108:126–134.
- ,.The demand for healthcare under Taiwan's national health insurance: a count data model approach.Expert Rev Pharmacoecon Outcomes Res.2009;9:13–22.
- ,.Feasibility and validity of International Classification of Diseases based case mix indices.BMC Health Serv Res.2006;6:125.
- ,,,,,.Non‐tuberculous mycobacterial pleurisy: an 8‐year single‐centre experience in Taiwan.Int J Tuberc Lung Dis.2010;14:635–641, p 634 follows 641.
In Taiwan, the national health insurance (NHI) implemented since 19951 has extended its coverage to almost the entire population. It may serve as a model for other countries looking to implement a universal health insurance system.2, 3 However, due to the low copayment for services, there are increasing admission rates and hospitalizations.2, 4 Admission rates, in particular, have nearly tripled for those who have been previously uninsured prior to the NHI program.2 In terms of hospital care, internal medicine and surgery are not favorite areas of specialty in the NHI system because inpatient care has a high workload but relatively low salaries.2, 5, 6 Consequently, there is now a shortage of primary inpatient care staff in Taiwan. The hospitalist system may be a solution to this problem.
The role of a hospitalist system has been discussed since 1996.7 Although its pros and cons are still debatable,8 the hospitalist system has grown in recent decades and there is a wide acceptance that hospitalists can efficiently care for inpatients.4, 9, 10 However, most related studies are in Western countries.4, 6, 11 It has rarely been studied in Asian countries and in those with NHI programs.
This study therefore aimed to investigate whether the hospitalist system, working within the NHI system in Taiwan, can be efficient in saving costs, maintaining quality care, and managing a high volume of in patients.
Materials and Methods
This prospective observational study was conducted in the National Taiwan University Hospital (NTUH), a tertiary‐care referral center in northern Taiwan, and approved by the hospital's Institutional Review Board. The program was also registered on Clinicaltrial.gov (identifier NCT00997646). A 36‐bed hospitalist‐run ward (HW) was set up in October 2009 in NTUH. For performance comparison, two 36‐bed internist‐run wards (IWs) were selected. The three wards were geographically separated.
Study Subjects
All patients age >18 years from the emergency department (ED) were admitted into one of the three wards based on the diagnosis category determined by the ED physicians. A patient was admitted by bed managers who were blinded to the study. Cases were categorized as diseases of general medicine, such as congestive heart failure, pneumonia, exacerbation of chronic obstructive pulmonary disease, cellulitis, ischemic stroke, urinary tract infection, and gastrointestinal bleeding.
Patients with severe illnesses requiring admission to intensive care units were excluded. Research assistants who were blinded to the patient stratification performed the patients' identification and data collection. Patient care was determined by the respective medical teams without any interference from this study.
Care‐Team Structure
The HW was set up with 3 attending physicians certified by a board of internal medicine and 6 nurse practitioners. All staff members worked full‐time to provide primary inpatient care. For comparison (Table 1), each IW had a set‐up of 3 attending physicians licensed by a board of internal medicine, one chief resident, 3 junior residents, and 3 interns. The attending physicians of the IWs visited their inpatients every workday and delegated primary care to residents on night shifts and weekends.
| Hospitalist‐Run Ward | Internist‐Run Wards | |
|---|---|---|
| ||
| Team member, per ward | 3 AP, 6 NP | 3 AP, 1 CR, 3 JR, 3 intern |
| Beds, per ward | 36 | 36 |
| Inpatient care of AP | Full time | Once daily |
| Who prescribes care order? | AP | AP, CR, JR |
| Who executes order? | NP | JR, intern |
| AP duty | Inpatient care; research | Inpatient/outpatient care; work of subspecialty; research |
| Bed manager | NP/AP | CR |
Clinical Characteristics
The patients' clinical characteristics, laboratory data, hospital course, and outcomes were recorded. The clinical characteristics included age, gender, underlying comorbidities, activities of daily living, and admission diagnosis. Charlson scores and Barthel's scores represented underlying comorbidities and activities of daily living, respectively. These were calculated as described in previous studies.11, 12 Admission costs paid for by the Taiwan NHI was defined as an inpatient's expenditure paid to the hospital by the institute of NHI. Total admission cost included expenses paid for by NHI and the patient's out‐of‐pocket expenditure not covered by NHI. A primary care physician was defined if the patient had visited the same doctor's clinic three times or more within one year prior to admission.8 Patients were followed‐up for 30 days after discharge by telephone, or until readmission.
Propensity Score Methods
Propensity score‐matching was used to balance observed covariates between the 2 care groups. It was defined as the conditional probability for being admitted to the HW, as a binary dependent variable, under a set of measurements. Factors that were significantly different (P < 0.05) between the 2 groups in univariate analysis were included in a multivariable logistic regression model to predict HW admission. The predicted probability derived from the logistic equation was used as the propensity score for each individual.
Patients in the HW and IWs were pooled and sorted according to their propensity score in ascending order. The selection process began from the first two cases with the lowest propensity score. If one was admitted to the HW and the other to an IW, both were selected as a matched pair. If this was not the case, then four cases were included. If there were two HW patients and two IW cases, the four were selected as two matched pairs. In the same way, HW and IW cases were matched by their propensity score in 1:1, 2:2, or 3:3 blocks. A patient who did not have a suitable match within the acceptable rank range was excluded from further analysis. The matching process moved down the sort list until all possible matched pairs were included and the selected patients formed a matched 1:1 pair in both groups.
Statistical Analysis
Intergroup differences were compared using independent t test for numerical variables and chi‐square test for categorical variables. Curves of probability of staying in the hospital within 30 days were generated using the Kaplan‐Meier method and compared using the log‐rank test. A logistic regression model was used for the propensity score match using the SPSS software version 13.0 (SPSS, Chicago, IL). The probability that indicated patient admission to the HW in both groups was used to draw box‐plots. After the 1:1 matched groups were assembled, the clinical characteristics were compared accordingly.
Results
From November 2009 to January 2010, 810 patients admitted from the ED to the study wards were enrolled. Among them, 377 were admitted to the HW and 433 to the IWs. Analysis of admission days showed that 84 (22%) and 53 (12%) patients were admitted to the HW and IWs, respectively, on weekends (P < 0.001).
Compared to the IW patients, the HW patients were older (age >65 years) and had poorer functional status by Barthel's scores (Table 2). Admission diagnosis was similar in both groups, except for pneumonia and urinary tract infection, which were higher in the HW patients. There was a primary care physician in 242 (64%) HW and 282 (65%) IW patients (P = 0.781).
The Charlson score, representing underlying comorbidity, was higher in the HW group (P = 0.002). Moreover, patients with severe liver cirrhosis (Child‐Pugh class C) were more frequently admitted to the HW (P = 0.018). Underlying malignancy, severe chronic kidney disease (estimated creatinine clearance <30 mL/min), and chronic respiratory failure requiring mechanical ventilator support were more associated with HW admission, although not statistically significantly (P = 0.064, 0.072, and 0.104, respectively).
The average admission cost was lower in HW patients than in IW patients, whether paid for by NHI ($1640.2 vs $2933.8 per patient, P = 0.001) or by the total admission cost ($2223.4 vs $3700.8 per patient, P = 0.001) (Table 3). Similarly, there was a shorter average length of stay (LOS) in the HW patients (9.3 vs 13.1 days, P < 0.001), who were discharged earlier than IW patients (Figure 1A). Regarding cost per patient‐day, the total daily cost was similar between the two groups (P = 0.560).
| Hospitalist‐Run Ward (n = 377) | Internist‐Run Wards (n = 433) | P‐Value | |
|---|---|---|---|
| |||
| Age >65 years old | 237 (63) | 240 (55) | 0.032 |
| Gender, male | 210 (56) | 243 (56) | 0.905 |
| Barthel's score | 61 35 | 70 33 | <0.001 |
| Charlson score | 3.7 3.4 | 3.0 3.2 | 0.002 |
| Admission diagnosis | |||
| Pneumonia | 106 (28) | 88 (20) | 0.010 |
| Exacerbation of COPD | 18 (5) | 15 (3) | 0.347 |
| Congestive heart failure | 12 (3) | 19 (4) | 0.373 |
| Upper gastrointestinal bleeding | 55 (15) | 58 (13) | 0.625 |
| Intra‐abdominal infection | 36 (10) | 47 (11) | 0.541 |
| Urinary tract infection | 85 (23) | 69 (16) | 0.017 |
| Cellulitis | 20 (5) | 18 (4) | 0.441 |
| Ischemic stroke | 12 (3) | 21 (5) | 0.231 |
| Others* | 117 (31) | 164 (38) | 0.041 |
| Laboratory data in the initial admission | |||
| Leukocyte count, /L | 11372 7962 | 10377 6422 | 0.050 |
| Hemoglobin, g/dL | 12.7 12.8 | 12.3 8.6 | 0.714 |
| Platelet count, K/L | 219 124 | 205 108 | 0.102 |
| Blood urea nitrogen, mg/dL | 33.2 27.7 | 24.1 17.4 | <0.001 |
| Creatinine, mg/dL | 1.9 2.9 | 1.6 2.8 | 0.080 |
| Total bilirubin, mg/dL | 2.2 3.7 | 2.3 3.6 | 0.826 |
| C‐reactive protein, mg/dL | 8.0 7.7 | 6.0 6.4 | 0.008 |
More patients in the HW group signed the do‐not‐resuscitate (DNR) consent (P < 0.001) and died during the hospital course, although the difference was not statistically significant (P = 0.068). Among those who expired during hospitalization, DNR consent was signed by 42 (90%) HW and 27 (68%) IW patients (P = 0.014). Among those discharged, 57 (17.2%) HW and 70 (17.6%) IW patients were lost to follow‐up. There was no difference in the 30‐day readmission for any cause between the two groups (P = 0.992).
Due to baseline differences, propensity score‐matching was performed and 101 pairs of patients were selected according to the probability generated from factors significantly different in univariate analysis (ie, age >65 years, pneumonia or urinary tract infections, Charlson score, Barthel's score, and blood urea nitrogen and C‐reactive protein levels on initial admission). The clinical characteristics of the 202 patients were shown in Table 4.
| Hospitalist‐Run Ward (n = 377) | Internist‐Run Wards (n = 433) | P‐Value | |
|---|---|---|---|
| |||
| Length of hospital stay, days | 9.3 6.7 | 13.1 12.4 | <0.001 |
| Total admission cost: $ per patient | 2223.4 3428.2 | 3700.8 8010.7 | 0.001 |
| Admission cost paid by NHI: $ per patient | 1640.2 2403.3 | 2933.8 7460.7 | 0.001 |
| In‐hospital mortality | 47 (12) | 37 (9) | 0.068 |
| Do‐not‐resuscitate consent | 74 (20) | 34 (8) | <0.001 |
| 30‐Day readmission* | 71 (22) | 83 (21) | 0.922 |
| Hospitalist‐Run Ward (n = 101) | Internist‐Run Wards (n = 101) | P‐Value | |
|---|---|---|---|
| |||
| Age >65 years old | 59 (58) | 59 (58) | 1.000 |
| Gender, Male | 55 (54) | 50 (50) | 0.481 |
| Barthel's score | 66 34 | 65 35 | 0.897 |
| Charlson score | 3.2 3.2 | 3.6 3.5 | 0.437 |
| Admission diagnosis | |||
| Pneumonia | 31 (31) | 27 (27) | 0.534 |
| Exacerbation of COPD | 4 (4) | 5 (5) | 0.733 |
| Congestive heart failure | 2 (2) | 2 (2) | 1.000 |
| Gastrointestinal bleeding | 10 (10) | 8 (8) | 0.621 |
| Intra‐abdominal infection | 18 (18) | 10 (10) | 0.103 |
| Urinary tract infection | 22 (22) | 21 (21) | 0.864 |
| Cellulitis | 6 (6) | 5 (5) | 0.757 |
| Ischemic stroke | 2 (2) | 0 | 0.155 |
| Others* | 39 (39) | 30 (30) | 0.182 |
| Laboratory data in the initial admission | |||
| Leukocyte count, /L | 12487 6288 | 11430 7718 | 0.287 |
| Hemoglobin, g/dL | 12.8 13.7 | 12.5 7.5 | 0.803 |
| Platelet count, K/L | 212 102 | 207 103 | 0.710 |
| Blood urea nitrogen, mg/dL | 25.5 19.7 | 24.7 17.5 | 0.773 |
| Creatinine, mg/dL | 1.5 1.2 | 1.6 1.5 | 0.979 |
| Total bilirubin, mg/dL | 2.0 7.0 | 2.0 6.9 | 0.963 |
| C‐reactive protein, mg/dL | 6.9 7.7 | 7.0 6.4 | 0.859 |
| Length of hospital stay, days | 9.2 6.4 | 15.2 13.8 | <0.001 |
| Do‐not‐resuscitate consent | 18 (18) | 6 (6) | 0.009 |
| Total admission cost: $ per patient | 2019.4 1709.3 | 5608.9 14244.8 | 0.013 |
| Cost paid by NHI: $ per patient | 1463.4 1404.6 | 4665.8 13553.3 | 0.019 |
| In‐hospital mortality | 9 (9) | 7 (7) | 0.602 |
| 30‐Day postdischarge readmission | 17 (18) | 21 (22) | 0.492 |
Both groups had almost the same propensity scores (P = 0.970; see online Supporting Information). Patients in the HW group had significantly lower admission cost, shorter LOS (Figure 1B), and more DNR consent, but similar in‐hospital mortality and readmission rates (Table 4).
DISCUSSION
The hospitalist system, which has been practiced for years in the United States, has not really been reported in Asia.13 Under the universal NHI system, this system has been studied in terms of treating patients in a Taiwan referral center. This study is the first to report on a hospitalist system in an Asian country with an NHI program. The hospitalist system in this study demonstrates efficient performance even though the patients have multiple comorbidities, compared to those in the general medical wards. By propensity score‐matching, admission costs of the hospitalist‐run ward are significantly lower than those of the internist‐run wards despite similar mortality and readmission rates.
The average LOS is reduced by 29% in HW patients and this plays a major role in cost reduction.14, 15 The reason may be the hospitalist's full‐time care, which allows for prompt decision‐making and close interaction with the patients' families.16 These families thus understand the treatment planning and prognosis. Furthermore, the hospitalist system continues working on weekends. As a result, patients are discharged without delay, even on holidays.
The aim of reducing LOS and costs is important because hospital income will decrease under the payment by disease‐related group (DRG) being implemented by the NHI system.17 A shortage of inpatient physicians may also develop due to the high workload but relatively low remuneration.2, 18 In contrast, a hospitalist care system that integrates nurse practitioners demands less human resources and saves on costs. In the future, it may be one of the solutions for hospitals aiming to maintain financial balance.
Another important issue in the NHI coverage is the increasing number of patients in the ED, which seems to be overflowing.19 In a previous Taiwan report, there are 7.1 patients per day who are staying in the ED for more than 72 hours, despite indications for admission.20 The delay is possibly due to the lack of available beds in the inpatient department.21 Amidst increasing demands for admission under the NHI and an aging society,2, 20 experience suggests that a hospitalist care system is a promising alternative to address the high ED patient volumes, especially on holidays. Howell et al. have also demonstrated that hospitalist‐driven bed management enhances the bed utility rate.21, 22 Since the current study also shows reduced LOS in the HW, patients will have a faster turn‐over rate and thereby assist in alleviating ED overcrowding.
Although the LOS of the patients here is comparable to that reported by the Taiwan NHI,2 it is far longer than that reported in the United States (around 4.75.2 days).4, 23 One possible explanation is the social and cultural determinants, including hospital‐ or physician‐dependence.24 In literature from Japan and Taiwan, hospitalization is as long as 13 weeks.25, 26 In addition, the average admission cost is reportedly around $1540 per patient‐day in the US, around 6 times that in this study ($266.6 per patient‐day).4 In the aging society of Taiwan,27 the NHI‐required copayment for admission may be relatively low, such that patients (or their families) may be misled that hospital care is better and hesitate to be discharged.2830
Regarding quality of care and patient safety, the in‐hospital mortality and the 30‐day readmission rates are similar in both groups, although disease severity and underlying comorbidities are worse in the HW at the start. This is consistent with previous reports that hospitalists can manage inpatient as well as internist care systems.4, 23 However, because this study has been performed in a tertiary referral center, patients may be more severely ill, such that the inpatient mortality and 30‐day readmission rates are as high as 10.3% and 21.11%, respectively.31, 32 Nonetheless, generalizing the hospitalist system to regional or district hospitals remains a concern, and this warrants further study.
This study has two other limitations. First, it is an observational study and patients have different demographics even though propensity score‐matching has been performed. Second, the patients were hospitalized without a standardized treatment protocol.
In conclusion, under the NHI system in Taiwan, a hospitalist system can have higher efficiency in shortening LOS and reducing cost than an internist care system, and still have similar hospital mortality and readmission rates. A hospitalist system may address the issue of high patient volume by increasing ward utilization. It can be recommended in a country with NHI that has a shortage of inpatient care staff.
In Taiwan, the national health insurance (NHI) implemented since 19951 has extended its coverage to almost the entire population. It may serve as a model for other countries looking to implement a universal health insurance system.2, 3 However, due to the low copayment for services, there are increasing admission rates and hospitalizations.2, 4 Admission rates, in particular, have nearly tripled for those who have been previously uninsured prior to the NHI program.2 In terms of hospital care, internal medicine and surgery are not favorite areas of specialty in the NHI system because inpatient care has a high workload but relatively low salaries.2, 5, 6 Consequently, there is now a shortage of primary inpatient care staff in Taiwan. The hospitalist system may be a solution to this problem.
The role of a hospitalist system has been discussed since 1996.7 Although its pros and cons are still debatable,8 the hospitalist system has grown in recent decades and there is a wide acceptance that hospitalists can efficiently care for inpatients.4, 9, 10 However, most related studies are in Western countries.4, 6, 11 It has rarely been studied in Asian countries and in those with NHI programs.
This study therefore aimed to investigate whether the hospitalist system, working within the NHI system in Taiwan, can be efficient in saving costs, maintaining quality care, and managing a high volume of in patients.
Materials and Methods
This prospective observational study was conducted in the National Taiwan University Hospital (NTUH), a tertiary‐care referral center in northern Taiwan, and approved by the hospital's Institutional Review Board. The program was also registered on Clinicaltrial.gov (identifier NCT00997646). A 36‐bed hospitalist‐run ward (HW) was set up in October 2009 in NTUH. For performance comparison, two 36‐bed internist‐run wards (IWs) were selected. The three wards were geographically separated.
Study Subjects
All patients age >18 years from the emergency department (ED) were admitted into one of the three wards based on the diagnosis category determined by the ED physicians. A patient was admitted by bed managers who were blinded to the study. Cases were categorized as diseases of general medicine, such as congestive heart failure, pneumonia, exacerbation of chronic obstructive pulmonary disease, cellulitis, ischemic stroke, urinary tract infection, and gastrointestinal bleeding.
Patients with severe illnesses requiring admission to intensive care units were excluded. Research assistants who were blinded to the patient stratification performed the patients' identification and data collection. Patient care was determined by the respective medical teams without any interference from this study.
Care‐Team Structure
The HW was set up with 3 attending physicians certified by a board of internal medicine and 6 nurse practitioners. All staff members worked full‐time to provide primary inpatient care. For comparison (Table 1), each IW had a set‐up of 3 attending physicians licensed by a board of internal medicine, one chief resident, 3 junior residents, and 3 interns. The attending physicians of the IWs visited their inpatients every workday and delegated primary care to residents on night shifts and weekends.
| Hospitalist‐Run Ward | Internist‐Run Wards | |
|---|---|---|
| ||
| Team member, per ward | 3 AP, 6 NP | 3 AP, 1 CR, 3 JR, 3 intern |
| Beds, per ward | 36 | 36 |
| Inpatient care of AP | Full time | Once daily |
| Who prescribes care order? | AP | AP, CR, JR |
| Who executes order? | NP | JR, intern |
| AP duty | Inpatient care; research | Inpatient/outpatient care; work of subspecialty; research |
| Bed manager | NP/AP | CR |
Clinical Characteristics
The patients' clinical characteristics, laboratory data, hospital course, and outcomes were recorded. The clinical characteristics included age, gender, underlying comorbidities, activities of daily living, and admission diagnosis. Charlson scores and Barthel's scores represented underlying comorbidities and activities of daily living, respectively. These were calculated as described in previous studies.11, 12 Admission costs paid for by the Taiwan NHI was defined as an inpatient's expenditure paid to the hospital by the institute of NHI. Total admission cost included expenses paid for by NHI and the patient's out‐of‐pocket expenditure not covered by NHI. A primary care physician was defined if the patient had visited the same doctor's clinic three times or more within one year prior to admission.8 Patients were followed‐up for 30 days after discharge by telephone, or until readmission.
Propensity Score Methods
Propensity score‐matching was used to balance observed covariates between the 2 care groups. It was defined as the conditional probability for being admitted to the HW, as a binary dependent variable, under a set of measurements. Factors that were significantly different (P < 0.05) between the 2 groups in univariate analysis were included in a multivariable logistic regression model to predict HW admission. The predicted probability derived from the logistic equation was used as the propensity score for each individual.
Patients in the HW and IWs were pooled and sorted according to their propensity score in ascending order. The selection process began from the first two cases with the lowest propensity score. If one was admitted to the HW and the other to an IW, both were selected as a matched pair. If this was not the case, then four cases were included. If there were two HW patients and two IW cases, the four were selected as two matched pairs. In the same way, HW and IW cases were matched by their propensity score in 1:1, 2:2, or 3:3 blocks. A patient who did not have a suitable match within the acceptable rank range was excluded from further analysis. The matching process moved down the sort list until all possible matched pairs were included and the selected patients formed a matched 1:1 pair in both groups.
Statistical Analysis
Intergroup differences were compared using independent t test for numerical variables and chi‐square test for categorical variables. Curves of probability of staying in the hospital within 30 days were generated using the Kaplan‐Meier method and compared using the log‐rank test. A logistic regression model was used for the propensity score match using the SPSS software version 13.0 (SPSS, Chicago, IL). The probability that indicated patient admission to the HW in both groups was used to draw box‐plots. After the 1:1 matched groups were assembled, the clinical characteristics were compared accordingly.
Results
From November 2009 to January 2010, 810 patients admitted from the ED to the study wards were enrolled. Among them, 377 were admitted to the HW and 433 to the IWs. Analysis of admission days showed that 84 (22%) and 53 (12%) patients were admitted to the HW and IWs, respectively, on weekends (P < 0.001).
Compared to the IW patients, the HW patients were older (age >65 years) and had poorer functional status by Barthel's scores (Table 2). Admission diagnosis was similar in both groups, except for pneumonia and urinary tract infection, which were higher in the HW patients. There was a primary care physician in 242 (64%) HW and 282 (65%) IW patients (P = 0.781).
The Charlson score, representing underlying comorbidity, was higher in the HW group (P = 0.002). Moreover, patients with severe liver cirrhosis (Child‐Pugh class C) were more frequently admitted to the HW (P = 0.018). Underlying malignancy, severe chronic kidney disease (estimated creatinine clearance <30 mL/min), and chronic respiratory failure requiring mechanical ventilator support were more associated with HW admission, although not statistically significantly (P = 0.064, 0.072, and 0.104, respectively).
The average admission cost was lower in HW patients than in IW patients, whether paid for by NHI ($1640.2 vs $2933.8 per patient, P = 0.001) or by the total admission cost ($2223.4 vs $3700.8 per patient, P = 0.001) (Table 3). Similarly, there was a shorter average length of stay (LOS) in the HW patients (9.3 vs 13.1 days, P < 0.001), who were discharged earlier than IW patients (Figure 1A). Regarding cost per patient‐day, the total daily cost was similar between the two groups (P = 0.560).
| Hospitalist‐Run Ward (n = 377) | Internist‐Run Wards (n = 433) | P‐Value | |
|---|---|---|---|
| |||
| Age >65 years old | 237 (63) | 240 (55) | 0.032 |
| Gender, male | 210 (56) | 243 (56) | 0.905 |
| Barthel's score | 61 35 | 70 33 | <0.001 |
| Charlson score | 3.7 3.4 | 3.0 3.2 | 0.002 |
| Admission diagnosis | |||
| Pneumonia | 106 (28) | 88 (20) | 0.010 |
| Exacerbation of COPD | 18 (5) | 15 (3) | 0.347 |
| Congestive heart failure | 12 (3) | 19 (4) | 0.373 |
| Upper gastrointestinal bleeding | 55 (15) | 58 (13) | 0.625 |
| Intra‐abdominal infection | 36 (10) | 47 (11) | 0.541 |
| Urinary tract infection | 85 (23) | 69 (16) | 0.017 |
| Cellulitis | 20 (5) | 18 (4) | 0.441 |
| Ischemic stroke | 12 (3) | 21 (5) | 0.231 |
| Others* | 117 (31) | 164 (38) | 0.041 |
| Laboratory data in the initial admission | |||
| Leukocyte count, /L | 11372 7962 | 10377 6422 | 0.050 |
| Hemoglobin, g/dL | 12.7 12.8 | 12.3 8.6 | 0.714 |
| Platelet count, K/L | 219 124 | 205 108 | 0.102 |
| Blood urea nitrogen, mg/dL | 33.2 27.7 | 24.1 17.4 | <0.001 |
| Creatinine, mg/dL | 1.9 2.9 | 1.6 2.8 | 0.080 |
| Total bilirubin, mg/dL | 2.2 3.7 | 2.3 3.6 | 0.826 |
| C‐reactive protein, mg/dL | 8.0 7.7 | 6.0 6.4 | 0.008 |
More patients in the HW group signed the do‐not‐resuscitate (DNR) consent (P < 0.001) and died during the hospital course, although the difference was not statistically significant (P = 0.068). Among those who expired during hospitalization, DNR consent was signed by 42 (90%) HW and 27 (68%) IW patients (P = 0.014). Among those discharged, 57 (17.2%) HW and 70 (17.6%) IW patients were lost to follow‐up. There was no difference in the 30‐day readmission for any cause between the two groups (P = 0.992).
Due to baseline differences, propensity score‐matching was performed and 101 pairs of patients were selected according to the probability generated from factors significantly different in univariate analysis (ie, age >65 years, pneumonia or urinary tract infections, Charlson score, Barthel's score, and blood urea nitrogen and C‐reactive protein levels on initial admission). The clinical characteristics of the 202 patients were shown in Table 4.
| Hospitalist‐Run Ward (n = 377) | Internist‐Run Wards (n = 433) | P‐Value | |
|---|---|---|---|
| |||
| Length of hospital stay, days | 9.3 6.7 | 13.1 12.4 | <0.001 |
| Total admission cost: $ per patient | 2223.4 3428.2 | 3700.8 8010.7 | 0.001 |
| Admission cost paid by NHI: $ per patient | 1640.2 2403.3 | 2933.8 7460.7 | 0.001 |
| In‐hospital mortality | 47 (12) | 37 (9) | 0.068 |
| Do‐not‐resuscitate consent | 74 (20) | 34 (8) | <0.001 |
| 30‐Day readmission* | 71 (22) | 83 (21) | 0.922 |
| Hospitalist‐Run Ward (n = 101) | Internist‐Run Wards (n = 101) | P‐Value | |
|---|---|---|---|
| |||
| Age >65 years old | 59 (58) | 59 (58) | 1.000 |
| Gender, Male | 55 (54) | 50 (50) | 0.481 |
| Barthel's score | 66 34 | 65 35 | 0.897 |
| Charlson score | 3.2 3.2 | 3.6 3.5 | 0.437 |
| Admission diagnosis | |||
| Pneumonia | 31 (31) | 27 (27) | 0.534 |
| Exacerbation of COPD | 4 (4) | 5 (5) | 0.733 |
| Congestive heart failure | 2 (2) | 2 (2) | 1.000 |
| Gastrointestinal bleeding | 10 (10) | 8 (8) | 0.621 |
| Intra‐abdominal infection | 18 (18) | 10 (10) | 0.103 |
| Urinary tract infection | 22 (22) | 21 (21) | 0.864 |
| Cellulitis | 6 (6) | 5 (5) | 0.757 |
| Ischemic stroke | 2 (2) | 0 | 0.155 |
| Others* | 39 (39) | 30 (30) | 0.182 |
| Laboratory data in the initial admission | |||
| Leukocyte count, /L | 12487 6288 | 11430 7718 | 0.287 |
| Hemoglobin, g/dL | 12.8 13.7 | 12.5 7.5 | 0.803 |
| Platelet count, K/L | 212 102 | 207 103 | 0.710 |
| Blood urea nitrogen, mg/dL | 25.5 19.7 | 24.7 17.5 | 0.773 |
| Creatinine, mg/dL | 1.5 1.2 | 1.6 1.5 | 0.979 |
| Total bilirubin, mg/dL | 2.0 7.0 | 2.0 6.9 | 0.963 |
| C‐reactive protein, mg/dL | 6.9 7.7 | 7.0 6.4 | 0.859 |
| Length of hospital stay, days | 9.2 6.4 | 15.2 13.8 | <0.001 |
| Do‐not‐resuscitate consent | 18 (18) | 6 (6) | 0.009 |
| Total admission cost: $ per patient | 2019.4 1709.3 | 5608.9 14244.8 | 0.013 |
| Cost paid by NHI: $ per patient | 1463.4 1404.6 | 4665.8 13553.3 | 0.019 |
| In‐hospital mortality | 9 (9) | 7 (7) | 0.602 |
| 30‐Day postdischarge readmission | 17 (18) | 21 (22) | 0.492 |
Both groups had almost the same propensity scores (P = 0.970; see online Supporting Information). Patients in the HW group had significantly lower admission cost, shorter LOS (Figure 1B), and more DNR consent, but similar in‐hospital mortality and readmission rates (Table 4).
DISCUSSION
The hospitalist system, which has been practiced for years in the United States, has not really been reported in Asia.13 Under the universal NHI system, this system has been studied in terms of treating patients in a Taiwan referral center. This study is the first to report on a hospitalist system in an Asian country with an NHI program. The hospitalist system in this study demonstrates efficient performance even though the patients have multiple comorbidities, compared to those in the general medical wards. By propensity score‐matching, admission costs of the hospitalist‐run ward are significantly lower than those of the internist‐run wards despite similar mortality and readmission rates.
The average LOS is reduced by 29% in HW patients and this plays a major role in cost reduction.14, 15 The reason may be the hospitalist's full‐time care, which allows for prompt decision‐making and close interaction with the patients' families.16 These families thus understand the treatment planning and prognosis. Furthermore, the hospitalist system continues working on weekends. As a result, patients are discharged without delay, even on holidays.
The aim of reducing LOS and costs is important because hospital income will decrease under the payment by disease‐related group (DRG) being implemented by the NHI system.17 A shortage of inpatient physicians may also develop due to the high workload but relatively low remuneration.2, 18 In contrast, a hospitalist care system that integrates nurse practitioners demands less human resources and saves on costs. In the future, it may be one of the solutions for hospitals aiming to maintain financial balance.
Another important issue in the NHI coverage is the increasing number of patients in the ED, which seems to be overflowing.19 In a previous Taiwan report, there are 7.1 patients per day who are staying in the ED for more than 72 hours, despite indications for admission.20 The delay is possibly due to the lack of available beds in the inpatient department.21 Amidst increasing demands for admission under the NHI and an aging society,2, 20 experience suggests that a hospitalist care system is a promising alternative to address the high ED patient volumes, especially on holidays. Howell et al. have also demonstrated that hospitalist‐driven bed management enhances the bed utility rate.21, 22 Since the current study also shows reduced LOS in the HW, patients will have a faster turn‐over rate and thereby assist in alleviating ED overcrowding.
Although the LOS of the patients here is comparable to that reported by the Taiwan NHI,2 it is far longer than that reported in the United States (around 4.75.2 days).4, 23 One possible explanation is the social and cultural determinants, including hospital‐ or physician‐dependence.24 In literature from Japan and Taiwan, hospitalization is as long as 13 weeks.25, 26 In addition, the average admission cost is reportedly around $1540 per patient‐day in the US, around 6 times that in this study ($266.6 per patient‐day).4 In the aging society of Taiwan,27 the NHI‐required copayment for admission may be relatively low, such that patients (or their families) may be misled that hospital care is better and hesitate to be discharged.2830
Regarding quality of care and patient safety, the in‐hospital mortality and the 30‐day readmission rates are similar in both groups, although disease severity and underlying comorbidities are worse in the HW at the start. This is consistent with previous reports that hospitalists can manage inpatient as well as internist care systems.4, 23 However, because this study has been performed in a tertiary referral center, patients may be more severely ill, such that the inpatient mortality and 30‐day readmission rates are as high as 10.3% and 21.11%, respectively.31, 32 Nonetheless, generalizing the hospitalist system to regional or district hospitals remains a concern, and this warrants further study.
This study has two other limitations. First, it is an observational study and patients have different demographics even though propensity score‐matching has been performed. Second, the patients were hospitalized without a standardized treatment protocol.
In conclusion, under the NHI system in Taiwan, a hospitalist system can have higher efficiency in shortening LOS and reducing cost than an internist care system, and still have similar hospital mortality and readmission rates. A hospitalist system may address the issue of high patient volume by increasing ward utilization. It can be recommended in a country with NHI that has a shortage of inpatient care staff.
- ,,,.Health system reform in the Republic of China. Formulating policy in a market‐based health system.JAMA.1995;273:777–781.
- ,,.A 10‐year experience with universal health insurance in Taiwan: measuring changes in health and health disparity.Ann Intern Med.2008;148:258–267.
- ,.Learning from Taiwan: experience with universal health insurance.Ann Intern Med.2008;148:313–314.
- ,,,,,.Outcomes of care by hospitalists, general internists, and family physicians.N Engl J Med.2007;357:2589–2600.
- ,.The effect of universal health insurance on health care utilization in Taiwan. Results from a natural experiment.JAMA.1997;278:89–93.
- ,,,,,.The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: a path analysis.Ind Health.2009;47:166–172.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,,.Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301:1671–1680.
- ,,,,.Hospitalists and the quality of care in hospitals.Arch Intern Med.2009;169:1389–1394.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360:1102–1112.
- ,,,,.The use of Charlson comorbidity index for patients revisiting the emergency department within 72 hours.Chang Gung Med J.2007;30:437–444.
- ,,,.Reliability of the Barthel Index when used with older people.Age Ageing.2005;34:228–232.
- .The hospitalist movement—a complex adaptive response to fragmentation of care in hospitals.Ann Acad Med Singapore.2008;37:145–150.
- ,,,,,.Determinants of hospitalist efficiency: a qualitative and quantitative study.Med Care Res Rev.2009;66:682–702.
- .The critical role of hospitalists in controlling healthcare costs.J Hosp Med.2010;5:127–132.
- .The relationship between hospitalists and primary care physicians.Ann Intern Med.2010;152:474.
- ,,,,,.Using diagnosis‐related groups. The situation in the United Kingdom National Health Service and in Germany.Eur J Health Econ.2004;5:287–289.
- ,,,,.Factors influencing medical students' choice of specialty.J Formos Med Assoc.2006;105:489–496.
- ,,,,.Factors associated with frequent use of emergency services in a medical center.J Formos Med Assoc.2003;102:222–228.
- ,,, et al.ED overcrowding in Taiwan: facts and strategies.Am J Emerg Med.1999;17:198–202.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–811.
- ,,,.Hospitalist bed management effecting throughput from the emergency department to the intensive care unit.J Crit Care.2010;25:184–189.
- ,,,.A comparison of two hospitalist models with traditional care in a community teaching hospital.Am J Med.2005;118:536–543.
- ,,,.Factors associated with tocolytic hospitalizations in Taiwan: evidence from a population‐based and longitudinal study from 1997 to 2004.BMC Pregnancy Childbirth.2009;9:59.
- ,,.Complicated parapneumonic effusion and empyema in children.J Microbiol Immunol Infect.2006;39:483–488.
- ,,, et al.Efficacy of corticosteroids in the treatment of community‐acquired pneumonia requiring hospitalization.Lung.2007;185:249–255.
- ,,.Analysis of population projections for Taiwan area: 2008 to 2056.Taiwan Economic Forum.2009;7:36–69.
- ,,,,.Why Taiwanese hospice patients want to stay in hospital: health‐care professionals' beliefs and solutions.Support Care Cancer.2004;12:285–292.
- ,,.Patient characteristics predict occurrence and outcome of complaints against physicians: a study from a medical center in central Taiwan.J Formos Med Assoc.2009;108:126–134.
- ,.The demand for healthcare under Taiwan's national health insurance: a count data model approach.Expert Rev Pharmacoecon Outcomes Res.2009;9:13–22.
- ,.Feasibility and validity of International Classification of Diseases based case mix indices.BMC Health Serv Res.2006;6:125.
- ,,,,,.Non‐tuberculous mycobacterial pleurisy: an 8‐year single‐centre experience in Taiwan.Int J Tuberc Lung Dis.2010;14:635–641, p 634 follows 641.
- ,,,.Health system reform in the Republic of China. Formulating policy in a market‐based health system.JAMA.1995;273:777–781.
- ,,.A 10‐year experience with universal health insurance in Taiwan: measuring changes in health and health disparity.Ann Intern Med.2008;148:258–267.
- ,.Learning from Taiwan: experience with universal health insurance.Ann Intern Med.2008;148:313–314.
- ,,,,,.Outcomes of care by hospitalists, general internists, and family physicians.N Engl J Med.2007;357:2589–2600.
- ,.The effect of universal health insurance on health care utilization in Taiwan. Results from a natural experiment.JAMA.1997;278:89–93.
- ,,,,,.The interrelationships between working conditions, job satisfaction, burnout and mental health among hospital physicians in Japan: a path analysis.Ind Health.2009;47:166–172.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,,,.Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults.JAMA.2009;301:1671–1680.
- ,,,,.Hospitalists and the quality of care in hospitals.Arch Intern Med.2009;169:1389–1394.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360:1102–1112.
- ,,,,.The use of Charlson comorbidity index for patients revisiting the emergency department within 72 hours.Chang Gung Med J.2007;30:437–444.
- ,,,.Reliability of the Barthel Index when used with older people.Age Ageing.2005;34:228–232.
- .The hospitalist movement—a complex adaptive response to fragmentation of care in hospitals.Ann Acad Med Singapore.2008;37:145–150.
- ,,,,,.Determinants of hospitalist efficiency: a qualitative and quantitative study.Med Care Res Rev.2009;66:682–702.
- .The critical role of hospitalists in controlling healthcare costs.J Hosp Med.2010;5:127–132.
- .The relationship between hospitalists and primary care physicians.Ann Intern Med.2010;152:474.
- ,,,,,.Using diagnosis‐related groups. The situation in the United Kingdom National Health Service and in Germany.Eur J Health Econ.2004;5:287–289.
- ,,,,.Factors influencing medical students' choice of specialty.J Formos Med Assoc.2006;105:489–496.
- ,,,,.Factors associated with frequent use of emergency services in a medical center.J Formos Med Assoc.2003;102:222–228.
- ,,, et al.ED overcrowding in Taiwan: facts and strategies.Am J Emerg Med.1999;17:198–202.
- ,,,,,.Active bed management by hospitalists and emergency department throughput.Ann Intern Med.2008;149:804–811.
- ,,,.Hospitalist bed management effecting throughput from the emergency department to the intensive care unit.J Crit Care.2010;25:184–189.
- ,,,.A comparison of two hospitalist models with traditional care in a community teaching hospital.Am J Med.2005;118:536–543.
- ,,,.Factors associated with tocolytic hospitalizations in Taiwan: evidence from a population‐based and longitudinal study from 1997 to 2004.BMC Pregnancy Childbirth.2009;9:59.
- ,,.Complicated parapneumonic effusion and empyema in children.J Microbiol Immunol Infect.2006;39:483–488.
- ,,, et al.Efficacy of corticosteroids in the treatment of community‐acquired pneumonia requiring hospitalization.Lung.2007;185:249–255.
- ,,.Analysis of population projections for Taiwan area: 2008 to 2056.Taiwan Economic Forum.2009;7:36–69.
- ,,,,.Why Taiwanese hospice patients want to stay in hospital: health‐care professionals' beliefs and solutions.Support Care Cancer.2004;12:285–292.
- ,,.Patient characteristics predict occurrence and outcome of complaints against physicians: a study from a medical center in central Taiwan.J Formos Med Assoc.2009;108:126–134.
- ,.The demand for healthcare under Taiwan's national health insurance: a count data model approach.Expert Rev Pharmacoecon Outcomes Res.2009;9:13–22.
- ,.Feasibility and validity of International Classification of Diseases based case mix indices.BMC Health Serv Res.2006;6:125.
- ,,,,,.Non‐tuberculous mycobacterial pleurisy: an 8‐year single‐centre experience in Taiwan.Int J Tuberc Lung Dis.2010;14:635–641, p 634 follows 641.
Copyright © 2011 Society of Hospital Medicine