User login
Risk models fail to predict lower-GI bleeding outcomes
In cases of lower gastrointestinal bleeding (LGIB), albumin and hemoglobin levels are the best independent predictors of severe bleeding, according to investigators.
These findings came from a sobering look at LGIB risk-prediction models. While some models could predict specific outcomes with reasonable accuracy, none of the models demonstrated broad predictive power, reported Natalie Tapaskar, MD, of the department of medicine at the University of Chicago, and her colleagues.
LGIB requires intensive resource utilization and proves fatal in 5%-15% of patients, which means timely and appropriate interventions are essential, especially for those with severe bleeding.
“There are limited data on accurately predicting the risk of adverse outcomes for hospitalized patients with LGIB,” the investigators wrote in Gastrointestinal Endoscopy, “especially in comparison to patients with upper gastrointestinal bleeding (UGIB), where tools such as the Glasgow-Blatchford Bleeding Score have been validated to accurately predict important clinical outcomes.”
To assess existing risk models for LGIB, the investigators performed a prospective observational study involving 170 patients with LGIB who underwent colonoscopy during April 2016–September 2017 at the University of Chicago Medical Center. Data were collected through comprehensive medical record review.
The primary outcome was severe bleeding. This was defined by acute bleeding during the first 24 hours of admission that required a transfusion of 2 or more units of packed red blood cells, and/or caused a 20% or greater decrease in hematocrit; and/or recurrent bleeding 24 hours after clinical stability, involving rectal bleeding with an additional drop in hematocrit of 20% or more, and/or readmission for LGIB within 1 week of discharge. Secondary outcomes included blood transfusion requirements, in-hospital recurrent bleeding, length of stay, ICU admission, intervention (surgery, interventional radiology, endoscopy), and the comparative predictive ability of seven clinical risk stratification models: AIMS65, Charlson Comorbidity Index, Glasgow-Blatchford, NOBLADS, Oakland, Sengupta, and Strate. Area under the receiver operating characteristic curve (AUC) was used to compare model predictive power. Risk of adverse outcomes was calculated by univariable and multivariable logistic regression.
Results showed that median patient age was 70 years. Most of the patients (80%) were African American and slightly more than half were female (58%). These demographic factors were not predictive of severe bleeding, which occurred in about half of the cases (52%). Upon admission, patients with severe bleeding were more likely to have chronic renal failure (30% vs. 17%; P = .05), lower albumin (3.6 g/dL vs. 3.95 g/dL; P less than .0001), lower hemoglobin (8.6 g/dL vs. 11.1 g/dL; P = .0001), lower systolic blood pressure (118 mm Hg vs. 132 mm Hg; P = .01), and higher creatinine (1.3 mg/dL vs. 1 mg/dL; P = .04). After adjustment for confounding variables, the strongest independent predictors of severe bleeding were low albumin (odds ratio, 2.56 per 1-g/dL decrease; P = .02) and low hemoglobin (OR, 1.28 per 1-g/dL decrease; P = .0015).
On average, time between admission and colonoscopy was between 2 and 3 days (median, 62.2 hours). In 3 out of 4 patients (77%), etiology of LGIB was confirmed; diverticular bleeding was most common (39%), followed distantly by hemorrhoidal bleeding (15%).
Compared with milder cases, patients with severe bleeding were more likely to stay in the ICU (49% vs. 19%; P less than .0001), have a blood transfusion (85% vs 36%; P less than .0001), and need to remain in the hospital for a longer period of time (6 days vs. 4 days; P = .0009). These findings exemplify the high level of resource utilization required for LGIB and show how severe bleeding dramatically compounds intensity of care.
Further analysis showed that none of the seven risk models were predictive across all outcomes; however, some predicted specific outcomes better than others. Leaders were the Glasgow-Blatchford score for blood transfusion (AUC 0.87; P less than .0001), the Oakland score for severe bleeding (AUC 0.74; P less than .0001), the Sengupta score for ICU stay (AUC 0.74; P less than .0001), and the Strate score for both recurrent bleeding during hospital stay (AUC 0.66; P = .0008) and endoscopic intervention (AUC 0.62; P = .01).
The investigators noted that the Glasgow-Blatchford score, which also is used in cases of UGIB, has previously demonstrated accuracy in predicting blood transfusion, as it did in the present study, suggesting that, “[i]n instances where there may be uncertainty of the origin of the bleeding, the Blatchford score may be a preferential choice of risk score.”
“Overall, we found that no singular score performed best across all the outcomes studied nor did any score have an extremely strong discriminatory power for any individual variable,” the investigators wrote, concluding that “... simpler and more powerful prediction tools are required for better risk stratification in LGIB.”
The investigators reported no financial support or conflicts of interest.
*This story was updated on Jan. 31, 2019.
SOURCE: Tapaskar N et al. Gastrointest Endosc. 2018 Dec 18. doi: 10.1016/j.gie.2018.12.011.
In cases of lower gastrointestinal bleeding (LGIB), albumin and hemoglobin levels are the best independent predictors of severe bleeding, according to investigators.
These findings came from a sobering look at LGIB risk-prediction models. While some models could predict specific outcomes with reasonable accuracy, none of the models demonstrated broad predictive power, reported Natalie Tapaskar, MD, of the department of medicine at the University of Chicago, and her colleagues.
LGIB requires intensive resource utilization and proves fatal in 5%-15% of patients, which means timely and appropriate interventions are essential, especially for those with severe bleeding.
“There are limited data on accurately predicting the risk of adverse outcomes for hospitalized patients with LGIB,” the investigators wrote in Gastrointestinal Endoscopy, “especially in comparison to patients with upper gastrointestinal bleeding (UGIB), where tools such as the Glasgow-Blatchford Bleeding Score have been validated to accurately predict important clinical outcomes.”
To assess existing risk models for LGIB, the investigators performed a prospective observational study involving 170 patients with LGIB who underwent colonoscopy during April 2016–September 2017 at the University of Chicago Medical Center. Data were collected through comprehensive medical record review.
The primary outcome was severe bleeding. This was defined by acute bleeding during the first 24 hours of admission that required a transfusion of 2 or more units of packed red blood cells, and/or caused a 20% or greater decrease in hematocrit; and/or recurrent bleeding 24 hours after clinical stability, involving rectal bleeding with an additional drop in hematocrit of 20% or more, and/or readmission for LGIB within 1 week of discharge. Secondary outcomes included blood transfusion requirements, in-hospital recurrent bleeding, length of stay, ICU admission, intervention (surgery, interventional radiology, endoscopy), and the comparative predictive ability of seven clinical risk stratification models: AIMS65, Charlson Comorbidity Index, Glasgow-Blatchford, NOBLADS, Oakland, Sengupta, and Strate. Area under the receiver operating characteristic curve (AUC) was used to compare model predictive power. Risk of adverse outcomes was calculated by univariable and multivariable logistic regression.
Results showed that median patient age was 70 years. Most of the patients (80%) were African American and slightly more than half were female (58%). These demographic factors were not predictive of severe bleeding, which occurred in about half of the cases (52%). Upon admission, patients with severe bleeding were more likely to have chronic renal failure (30% vs. 17%; P = .05), lower albumin (3.6 g/dL vs. 3.95 g/dL; P less than .0001), lower hemoglobin (8.6 g/dL vs. 11.1 g/dL; P = .0001), lower systolic blood pressure (118 mm Hg vs. 132 mm Hg; P = .01), and higher creatinine (1.3 mg/dL vs. 1 mg/dL; P = .04). After adjustment for confounding variables, the strongest independent predictors of severe bleeding were low albumin (odds ratio, 2.56 per 1-g/dL decrease; P = .02) and low hemoglobin (OR, 1.28 per 1-g/dL decrease; P = .0015).
On average, time between admission and colonoscopy was between 2 and 3 days (median, 62.2 hours). In 3 out of 4 patients (77%), etiology of LGIB was confirmed; diverticular bleeding was most common (39%), followed distantly by hemorrhoidal bleeding (15%).
Compared with milder cases, patients with severe bleeding were more likely to stay in the ICU (49% vs. 19%; P less than .0001), have a blood transfusion (85% vs 36%; P less than .0001), and need to remain in the hospital for a longer period of time (6 days vs. 4 days; P = .0009). These findings exemplify the high level of resource utilization required for LGIB and show how severe bleeding dramatically compounds intensity of care.
Further analysis showed that none of the seven risk models were predictive across all outcomes; however, some predicted specific outcomes better than others. Leaders were the Glasgow-Blatchford score for blood transfusion (AUC 0.87; P less than .0001), the Oakland score for severe bleeding (AUC 0.74; P less than .0001), the Sengupta score for ICU stay (AUC 0.74; P less than .0001), and the Strate score for both recurrent bleeding during hospital stay (AUC 0.66; P = .0008) and endoscopic intervention (AUC 0.62; P = .01).
The investigators noted that the Glasgow-Blatchford score, which also is used in cases of UGIB, has previously demonstrated accuracy in predicting blood transfusion, as it did in the present study, suggesting that, “[i]n instances where there may be uncertainty of the origin of the bleeding, the Blatchford score may be a preferential choice of risk score.”
“Overall, we found that no singular score performed best across all the outcomes studied nor did any score have an extremely strong discriminatory power for any individual variable,” the investigators wrote, concluding that “... simpler and more powerful prediction tools are required for better risk stratification in LGIB.”
The investigators reported no financial support or conflicts of interest.
*This story was updated on Jan. 31, 2019.
SOURCE: Tapaskar N et al. Gastrointest Endosc. 2018 Dec 18. doi: 10.1016/j.gie.2018.12.011.
In cases of lower gastrointestinal bleeding (LGIB), albumin and hemoglobin levels are the best independent predictors of severe bleeding, according to investigators.
These findings came from a sobering look at LGIB risk-prediction models. While some models could predict specific outcomes with reasonable accuracy, none of the models demonstrated broad predictive power, reported Natalie Tapaskar, MD, of the department of medicine at the University of Chicago, and her colleagues.
LGIB requires intensive resource utilization and proves fatal in 5%-15% of patients, which means timely and appropriate interventions are essential, especially for those with severe bleeding.
“There are limited data on accurately predicting the risk of adverse outcomes for hospitalized patients with LGIB,” the investigators wrote in Gastrointestinal Endoscopy, “especially in comparison to patients with upper gastrointestinal bleeding (UGIB), where tools such as the Glasgow-Blatchford Bleeding Score have been validated to accurately predict important clinical outcomes.”
To assess existing risk models for LGIB, the investigators performed a prospective observational study involving 170 patients with LGIB who underwent colonoscopy during April 2016–September 2017 at the University of Chicago Medical Center. Data were collected through comprehensive medical record review.
The primary outcome was severe bleeding. This was defined by acute bleeding during the first 24 hours of admission that required a transfusion of 2 or more units of packed red blood cells, and/or caused a 20% or greater decrease in hematocrit; and/or recurrent bleeding 24 hours after clinical stability, involving rectal bleeding with an additional drop in hematocrit of 20% or more, and/or readmission for LGIB within 1 week of discharge. Secondary outcomes included blood transfusion requirements, in-hospital recurrent bleeding, length of stay, ICU admission, intervention (surgery, interventional radiology, endoscopy), and the comparative predictive ability of seven clinical risk stratification models: AIMS65, Charlson Comorbidity Index, Glasgow-Blatchford, NOBLADS, Oakland, Sengupta, and Strate. Area under the receiver operating characteristic curve (AUC) was used to compare model predictive power. Risk of adverse outcomes was calculated by univariable and multivariable logistic regression.
Results showed that median patient age was 70 years. Most of the patients (80%) were African American and slightly more than half were female (58%). These demographic factors were not predictive of severe bleeding, which occurred in about half of the cases (52%). Upon admission, patients with severe bleeding were more likely to have chronic renal failure (30% vs. 17%; P = .05), lower albumin (3.6 g/dL vs. 3.95 g/dL; P less than .0001), lower hemoglobin (8.6 g/dL vs. 11.1 g/dL; P = .0001), lower systolic blood pressure (118 mm Hg vs. 132 mm Hg; P = .01), and higher creatinine (1.3 mg/dL vs. 1 mg/dL; P = .04). After adjustment for confounding variables, the strongest independent predictors of severe bleeding were low albumin (odds ratio, 2.56 per 1-g/dL decrease; P = .02) and low hemoglobin (OR, 1.28 per 1-g/dL decrease; P = .0015).
On average, time between admission and colonoscopy was between 2 and 3 days (median, 62.2 hours). In 3 out of 4 patients (77%), etiology of LGIB was confirmed; diverticular bleeding was most common (39%), followed distantly by hemorrhoidal bleeding (15%).
Compared with milder cases, patients with severe bleeding were more likely to stay in the ICU (49% vs. 19%; P less than .0001), have a blood transfusion (85% vs 36%; P less than .0001), and need to remain in the hospital for a longer period of time (6 days vs. 4 days; P = .0009). These findings exemplify the high level of resource utilization required for LGIB and show how severe bleeding dramatically compounds intensity of care.
Further analysis showed that none of the seven risk models were predictive across all outcomes; however, some predicted specific outcomes better than others. Leaders were the Glasgow-Blatchford score for blood transfusion (AUC 0.87; P less than .0001), the Oakland score for severe bleeding (AUC 0.74; P less than .0001), the Sengupta score for ICU stay (AUC 0.74; P less than .0001), and the Strate score for both recurrent bleeding during hospital stay (AUC 0.66; P = .0008) and endoscopic intervention (AUC 0.62; P = .01).
The investigators noted that the Glasgow-Blatchford score, which also is used in cases of UGIB, has previously demonstrated accuracy in predicting blood transfusion, as it did in the present study, suggesting that, “[i]n instances where there may be uncertainty of the origin of the bleeding, the Blatchford score may be a preferential choice of risk score.”
“Overall, we found that no singular score performed best across all the outcomes studied nor did any score have an extremely strong discriminatory power for any individual variable,” the investigators wrote, concluding that “... simpler and more powerful prediction tools are required for better risk stratification in LGIB.”
The investigators reported no financial support or conflicts of interest.
*This story was updated on Jan. 31, 2019.
SOURCE: Tapaskar N et al. Gastrointest Endosc. 2018 Dec 18. doi: 10.1016/j.gie.2018.12.011.
FROM GASTROINTESTINAL ENDOSCOPY
Key clinical point: In cases of lower gastrointestinal bleeding (LGIB), albumin and hemoglobin levels are the best independent predictors of severe bleeding.
Major finding: After adjustment for confounding variables, low albumin upon admission was the strongest independent predictor of severe bleeding (OR, 2.56 per 1 g/dL decrease; P = .02).
Study details: A prospective, observational study of 170 patients with LGIB who underwent colonoscopy during April 2016–September 2017 at the University of Chicago Medical Center.
Disclosures: The investigators reported no financial support or conflicts of interest.
Source: Tapaskar N et al. Gastrointest Endosc. 2018 Dec 18. doi: 10.1016/j.gie.2018.12.011.
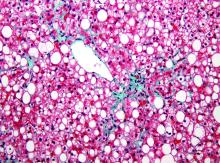
Impaired clot lysis associated with mild bleeding symptoms
Patients with self-reported mild bleeding symptoms may have impaired clot lysis, according to investigators. This finding is remarkable because it contrasts with known bleeding disorders, such as hemophilia, which are associated with enhanced clot lysis, reported lead author Minka J.A. Vries, MD, of the Cardiovascular Research Institute Maastricht (CARIM) at Maastricht (the Netherlands) University and her colleagues.
The observational study, which included 335 patients undergoing elective surgery at Maastricht University Medical Center, was conducted to better understand lysis capacity, which is challenging to assess in a clinical setting. Although the Euglobulin Lysis Time (ELT) is often used in the clinic, it cannot determine the influence of hemostatic proteins or formation of a fibrin clot under physiological conditions.
“In the more recently developed lysis assays,” the investigators wrote in Thrombosis Research, “the turbidity lysis assay and the tissue plasminogen activator–rotational thromboelastometry (tPA-ROTEM) [assay], all plasma proteins are present and fibrin is formed under more physiological conditions for the measurement of fibrinolysis.” These two tests were used in the present study.
Of the 335 adult patients, 240 had self-reported mild bleeding symptoms, and 95 did not. Patients with bleeding disorders, thrombocytopenia, or anemia were excluded, as were pregnant women and those taking blood thinners or NSAIDs. Along with assessing time parameters of fibrinolysis, clot-associated proteins were measured for possible imbalances.
“We hypothesized that clot lysis capacity is enhanced in patients with mild bleeding symptoms,” the investigators wrote, based on other bleeding disorders. Surprisingly, the results told a different story.
After adjusting for sex, BMI, and age, patients with bleeding symptoms had lower tPA-ROTEM lysis speed (beta −0.35; P = .007) and longer tPA-ROTEM lysis time (beta 0.29; P = .022) than did patients without bleeding symptoms. The investigators found that tPA-ROTEM measurements depended on factor II, factor XII, alpha2-antiplasmin, plasminogen, thrombin activatable fibrinolysis inhibitor (TAFI), and plasminogen activator inhibitor–1 (PAI-1) level. In contrast, turbidity lysis assay measurements were not significantly different between groups. This latter assay was influenced by alpha2-antiplasmin, TAFI, and PAI-1.
“We did not find evidence for systemic hyperfibrinolytic capacity in patients reporting mild bleeding symptoms in comparison to patients not reporting bleeding symptoms,” the investigators concluded. “tPA-ROTEM even suggested a slower clot lysis in these patients. Though this may appear counterintuitive, our results are in line with two papers assessing systemic clot lysis in mild bleeders.”
While this phenomenon gains supporting evidence, it remains poorly understood.
“We have no good explanation for these findings,” the investigators noted.
This study was funded by the Sint Annadal Foundation Maastricht, Maastricht University Medical Centre, CTMM INCOAG Maastricht, Cardiovascular Research Institute Maastricht, and the British Heart Foundation. No conflicts of interest were reported.
SOURCE: Vries MJA et al. Thromb Res. 2018 Dec 4. doi: 10.1016/j.thromres.2018.12.004.
Patients with self-reported mild bleeding symptoms may have impaired clot lysis, according to investigators. This finding is remarkable because it contrasts with known bleeding disorders, such as hemophilia, which are associated with enhanced clot lysis, reported lead author Minka J.A. Vries, MD, of the Cardiovascular Research Institute Maastricht (CARIM) at Maastricht (the Netherlands) University and her colleagues.
The observational study, which included 335 patients undergoing elective surgery at Maastricht University Medical Center, was conducted to better understand lysis capacity, which is challenging to assess in a clinical setting. Although the Euglobulin Lysis Time (ELT) is often used in the clinic, it cannot determine the influence of hemostatic proteins or formation of a fibrin clot under physiological conditions.
“In the more recently developed lysis assays,” the investigators wrote in Thrombosis Research, “the turbidity lysis assay and the tissue plasminogen activator–rotational thromboelastometry (tPA-ROTEM) [assay], all plasma proteins are present and fibrin is formed under more physiological conditions for the measurement of fibrinolysis.” These two tests were used in the present study.
Of the 335 adult patients, 240 had self-reported mild bleeding symptoms, and 95 did not. Patients with bleeding disorders, thrombocytopenia, or anemia were excluded, as were pregnant women and those taking blood thinners or NSAIDs. Along with assessing time parameters of fibrinolysis, clot-associated proteins were measured for possible imbalances.
“We hypothesized that clot lysis capacity is enhanced in patients with mild bleeding symptoms,” the investigators wrote, based on other bleeding disorders. Surprisingly, the results told a different story.
After adjusting for sex, BMI, and age, patients with bleeding symptoms had lower tPA-ROTEM lysis speed (beta −0.35; P = .007) and longer tPA-ROTEM lysis time (beta 0.29; P = .022) than did patients without bleeding symptoms. The investigators found that tPA-ROTEM measurements depended on factor II, factor XII, alpha2-antiplasmin, plasminogen, thrombin activatable fibrinolysis inhibitor (TAFI), and plasminogen activator inhibitor–1 (PAI-1) level. In contrast, turbidity lysis assay measurements were not significantly different between groups. This latter assay was influenced by alpha2-antiplasmin, TAFI, and PAI-1.
“We did not find evidence for systemic hyperfibrinolytic capacity in patients reporting mild bleeding symptoms in comparison to patients not reporting bleeding symptoms,” the investigators concluded. “tPA-ROTEM even suggested a slower clot lysis in these patients. Though this may appear counterintuitive, our results are in line with two papers assessing systemic clot lysis in mild bleeders.”
While this phenomenon gains supporting evidence, it remains poorly understood.
“We have no good explanation for these findings,” the investigators noted.
This study was funded by the Sint Annadal Foundation Maastricht, Maastricht University Medical Centre, CTMM INCOAG Maastricht, Cardiovascular Research Institute Maastricht, and the British Heart Foundation. No conflicts of interest were reported.
SOURCE: Vries MJA et al. Thromb Res. 2018 Dec 4. doi: 10.1016/j.thromres.2018.12.004.
Patients with self-reported mild bleeding symptoms may have impaired clot lysis, according to investigators. This finding is remarkable because it contrasts with known bleeding disorders, such as hemophilia, which are associated with enhanced clot lysis, reported lead author Minka J.A. Vries, MD, of the Cardiovascular Research Institute Maastricht (CARIM) at Maastricht (the Netherlands) University and her colleagues.
The observational study, which included 335 patients undergoing elective surgery at Maastricht University Medical Center, was conducted to better understand lysis capacity, which is challenging to assess in a clinical setting. Although the Euglobulin Lysis Time (ELT) is often used in the clinic, it cannot determine the influence of hemostatic proteins or formation of a fibrin clot under physiological conditions.
“In the more recently developed lysis assays,” the investigators wrote in Thrombosis Research, “the turbidity lysis assay and the tissue plasminogen activator–rotational thromboelastometry (tPA-ROTEM) [assay], all plasma proteins are present and fibrin is formed under more physiological conditions for the measurement of fibrinolysis.” These two tests were used in the present study.
Of the 335 adult patients, 240 had self-reported mild bleeding symptoms, and 95 did not. Patients with bleeding disorders, thrombocytopenia, or anemia were excluded, as were pregnant women and those taking blood thinners or NSAIDs. Along with assessing time parameters of fibrinolysis, clot-associated proteins were measured for possible imbalances.
“We hypothesized that clot lysis capacity is enhanced in patients with mild bleeding symptoms,” the investigators wrote, based on other bleeding disorders. Surprisingly, the results told a different story.
After adjusting for sex, BMI, and age, patients with bleeding symptoms had lower tPA-ROTEM lysis speed (beta −0.35; P = .007) and longer tPA-ROTEM lysis time (beta 0.29; P = .022) than did patients without bleeding symptoms. The investigators found that tPA-ROTEM measurements depended on factor II, factor XII, alpha2-antiplasmin, plasminogen, thrombin activatable fibrinolysis inhibitor (TAFI), and plasminogen activator inhibitor–1 (PAI-1) level. In contrast, turbidity lysis assay measurements were not significantly different between groups. This latter assay was influenced by alpha2-antiplasmin, TAFI, and PAI-1.
“We did not find evidence for systemic hyperfibrinolytic capacity in patients reporting mild bleeding symptoms in comparison to patients not reporting bleeding symptoms,” the investigators concluded. “tPA-ROTEM even suggested a slower clot lysis in these patients. Though this may appear counterintuitive, our results are in line with two papers assessing systemic clot lysis in mild bleeders.”
While this phenomenon gains supporting evidence, it remains poorly understood.
“We have no good explanation for these findings,” the investigators noted.
This study was funded by the Sint Annadal Foundation Maastricht, Maastricht University Medical Centre, CTMM INCOAG Maastricht, Cardiovascular Research Institute Maastricht, and the British Heart Foundation. No conflicts of interest were reported.
SOURCE: Vries MJA et al. Thromb Res. 2018 Dec 4. doi: 10.1016/j.thromres.2018.12.004.
FROM THROMBOSIS RESEARCH
Key clinical point: Patients with self-reported mild bleeding symptoms may have impaired clot lysis, in contrast with known bleeding disorders.
Major finding: Patients with mild bleeding had longer whole blood tissue plasminogen activator-rotational thromboelastometry lysis times (P = .022) than did patients without symptoms.
Study details: An observational study of 335 adult patients undergoing elective surgery.
Disclosures: This study was funded by the Sint Annadal Foundation, Maastricht University Medical Center, CTMM INCOAG Maastricht, Cardiovascular Research Institute Maastricht, and the British Heart Foundation. No conflicts of interest were reported.
Source: Vries MJA et al. Thromb Res. 2018 Dec 4. doi: 10.1016/j.thromres.2018.12.004.
Many misunderstand purpose of tumor profiling research
Although most cancer patients and parents of cancer patients understand that genomic tumor profiling research aims to improve care for future patients, many also believe that the process will benefit present treatment, according to a recent survey conducted at four academic treatment centers.
Misunderstandings were most common among less-educated individuals and those with little genetic knowledge, reported lead author Jonathan M. Marron, MD, MPH, of the Dana-Farber Cancer Institute in Boston and his colleagues.
Previous surveys have shown that “up to 60% of research participants demonstrate evidence of therapeutic misconception,” the investigators wrote in JCO Precision Oncology, referring to “the belief that the primary purpose of research is therapeutic in nature rather than acquisition of generalizable knowledge.”
“Although advances in targeted therapeutics generate great excitement, they may also blur the line between research and clinical care,” the investigators wrote. As such therapeutics become more common, so may misconceptions.
To evaluate current views of genomic tumor profiling research, the investigators surveyed 45 cancer patients and parents of cancer patients at four academic treatment centers. All patients were aged 30 years or younger at enrollment and undergoing tumor profiling; parents were asked to respond if patients were younger than 18 years.
The survey was divided into two sections: basic understanding and comprehensive understanding. To achieve basic understanding, a respondent needed to recognize that “the primary purpose was not to improve the patient’s treatment.” To achieve comprehensive understanding, the respondent needed to recognize four facts: “primary purpose was not to improve patient’s treatment,” “primary purpose was to improve treatment of future patients,” “there may not be direct medical benefit,” and “most likely result of participation was not increased likelihood of cure.”
Forty-four out of 45 survey participants responded. Of these, 30 (68%) demonstrated basic understanding, and 24 (55%) had comprehensive understanding. Respondents with higher education were more likely to answer correctly, with 81% showing basic understanding and 73% showing comprehensive understanding; among less-educated respondents, only half (50%) had basic understanding, and about 1 out of 4 (28%) had comprehensive understanding. Similar disparities were observed among respondents with more versus less genetic knowledge. Almost all respondents (93%) who thought that profiling would help present treatment also believed it would benefit future patients.
Taken as a whole, these findings suggest that therapeutic misconception in genomic tumor profiling research is relatively common, which echoes previous findings. The investigators recommended that clinicians anticipate these knowledge gaps and aim to overcome them.
“Interventional work to improve participant understanding of these complexities and nuances is necessary as sequencing moves from the laboratory to the clinic,” the investigators concluded. “Such work can guide pediatric oncologists in how to manage expectations and best counsel patients and families about the meaning and significance of clinical profiling results.”
The study was funded by Hyundai Hope on Wheels, the Friends for Life Foundation, the Gillmore Fund, National Institutes of Health, and others. The investigators reported financial affiliations with Merck, Millennium, Novartis, Roche, Amgen, and others.
SOURCE: Marron et al. JCO Precis Oncol. 2019 Jan 22. doi: 10.1200/PO.18.00176.
Although most cancer patients and parents of cancer patients understand that genomic tumor profiling research aims to improve care for future patients, many also believe that the process will benefit present treatment, according to a recent survey conducted at four academic treatment centers.
Misunderstandings were most common among less-educated individuals and those with little genetic knowledge, reported lead author Jonathan M. Marron, MD, MPH, of the Dana-Farber Cancer Institute in Boston and his colleagues.
Previous surveys have shown that “up to 60% of research participants demonstrate evidence of therapeutic misconception,” the investigators wrote in JCO Precision Oncology, referring to “the belief that the primary purpose of research is therapeutic in nature rather than acquisition of generalizable knowledge.”
“Although advances in targeted therapeutics generate great excitement, they may also blur the line between research and clinical care,” the investigators wrote. As such therapeutics become more common, so may misconceptions.
To evaluate current views of genomic tumor profiling research, the investigators surveyed 45 cancer patients and parents of cancer patients at four academic treatment centers. All patients were aged 30 years or younger at enrollment and undergoing tumor profiling; parents were asked to respond if patients were younger than 18 years.
The survey was divided into two sections: basic understanding and comprehensive understanding. To achieve basic understanding, a respondent needed to recognize that “the primary purpose was not to improve the patient’s treatment.” To achieve comprehensive understanding, the respondent needed to recognize four facts: “primary purpose was not to improve patient’s treatment,” “primary purpose was to improve treatment of future patients,” “there may not be direct medical benefit,” and “most likely result of participation was not increased likelihood of cure.”
Forty-four out of 45 survey participants responded. Of these, 30 (68%) demonstrated basic understanding, and 24 (55%) had comprehensive understanding. Respondents with higher education were more likely to answer correctly, with 81% showing basic understanding and 73% showing comprehensive understanding; among less-educated respondents, only half (50%) had basic understanding, and about 1 out of 4 (28%) had comprehensive understanding. Similar disparities were observed among respondents with more versus less genetic knowledge. Almost all respondents (93%) who thought that profiling would help present treatment also believed it would benefit future patients.
Taken as a whole, these findings suggest that therapeutic misconception in genomic tumor profiling research is relatively common, which echoes previous findings. The investigators recommended that clinicians anticipate these knowledge gaps and aim to overcome them.
“Interventional work to improve participant understanding of these complexities and nuances is necessary as sequencing moves from the laboratory to the clinic,” the investigators concluded. “Such work can guide pediatric oncologists in how to manage expectations and best counsel patients and families about the meaning and significance of clinical profiling results.”
The study was funded by Hyundai Hope on Wheels, the Friends for Life Foundation, the Gillmore Fund, National Institutes of Health, and others. The investigators reported financial affiliations with Merck, Millennium, Novartis, Roche, Amgen, and others.
SOURCE: Marron et al. JCO Precis Oncol. 2019 Jan 22. doi: 10.1200/PO.18.00176.
Although most cancer patients and parents of cancer patients understand that genomic tumor profiling research aims to improve care for future patients, many also believe that the process will benefit present treatment, according to a recent survey conducted at four academic treatment centers.
Misunderstandings were most common among less-educated individuals and those with little genetic knowledge, reported lead author Jonathan M. Marron, MD, MPH, of the Dana-Farber Cancer Institute in Boston and his colleagues.
Previous surveys have shown that “up to 60% of research participants demonstrate evidence of therapeutic misconception,” the investigators wrote in JCO Precision Oncology, referring to “the belief that the primary purpose of research is therapeutic in nature rather than acquisition of generalizable knowledge.”
“Although advances in targeted therapeutics generate great excitement, they may also blur the line between research and clinical care,” the investigators wrote. As such therapeutics become more common, so may misconceptions.
To evaluate current views of genomic tumor profiling research, the investigators surveyed 45 cancer patients and parents of cancer patients at four academic treatment centers. All patients were aged 30 years or younger at enrollment and undergoing tumor profiling; parents were asked to respond if patients were younger than 18 years.
The survey was divided into two sections: basic understanding and comprehensive understanding. To achieve basic understanding, a respondent needed to recognize that “the primary purpose was not to improve the patient’s treatment.” To achieve comprehensive understanding, the respondent needed to recognize four facts: “primary purpose was not to improve patient’s treatment,” “primary purpose was to improve treatment of future patients,” “there may not be direct medical benefit,” and “most likely result of participation was not increased likelihood of cure.”
Forty-four out of 45 survey participants responded. Of these, 30 (68%) demonstrated basic understanding, and 24 (55%) had comprehensive understanding. Respondents with higher education were more likely to answer correctly, with 81% showing basic understanding and 73% showing comprehensive understanding; among less-educated respondents, only half (50%) had basic understanding, and about 1 out of 4 (28%) had comprehensive understanding. Similar disparities were observed among respondents with more versus less genetic knowledge. Almost all respondents (93%) who thought that profiling would help present treatment also believed it would benefit future patients.
Taken as a whole, these findings suggest that therapeutic misconception in genomic tumor profiling research is relatively common, which echoes previous findings. The investigators recommended that clinicians anticipate these knowledge gaps and aim to overcome them.
“Interventional work to improve participant understanding of these complexities and nuances is necessary as sequencing moves from the laboratory to the clinic,” the investigators concluded. “Such work can guide pediatric oncologists in how to manage expectations and best counsel patients and families about the meaning and significance of clinical profiling results.”
The study was funded by Hyundai Hope on Wheels, the Friends for Life Foundation, the Gillmore Fund, National Institutes of Health, and others. The investigators reported financial affiliations with Merck, Millennium, Novartis, Roche, Amgen, and others.
SOURCE: Marron et al. JCO Precis Oncol. 2019 Jan 22. doi: 10.1200/PO.18.00176.
FROM JCO PRECISION ONCOLOGY
Key clinical point: Although most cancer patients and parents of cancer patients understand that genomic tumor profiling research aims to improve care for future patients, many also believe that the process will benefit present treatment.
Major finding: Fifty-five percent of respondents demonstrated comprehensive understanding the purpose of genomic tumor profiling research.
Study details: A survey of 45 cancer patients and parents of cancer patients conducted at four academic treatment centers.
Disclosures: The study was funded by Hyundai Hope on Wheels, the Friends for Life Foundation, the Gillmore Fund, National Institutes of Health, and others. The investigators reported financial affiliations with Merck, Millennium, Novartis, Roche, Amgen, and others.
Source: Marron et al. JCO Precis Oncol. 2019 Jan 22. doi: 10.1200/PO.18.00176.
Self-reporting extends lung cancer survival
Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance, according to a recent French study.
Self-reporting may notify care providers about adverse effects or recurrence earlier than imaging, suggested lead author, Fabrice Denis, MD, PhD, of Institut Inter-régional de Cancérologie Jean Bernard in Le Mans, France, and his colleagues. Findings were published in a letter in JAMA.
In 2017, a similar, single-center study showed that web-based symptom reporting could improve survival in patients undergoing chemotherapy. The lead investigator on that trial was Ethan Basch, MD, who coauthored the present publication.
The current, prospective study involved 121 patients treated at five centers in France between June 2014 and December 2017. Eligibility required a diagnosis of nonprogressive, metastatic lung cancer, including stage III or IV non–small cell or small cell disease. Patients were treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Patients in the control group had standard follow-up with imaging every 3-6 months. In contrast, the patient-reported outcomes (PRO) group completed a weekly online survey of 13 common symptoms between follow-up visits. If patients reported symptoms that matched with predefined criteria for severity or worsening, then the treating oncologist was notified.
When an 18-month interim analysis showed significant survival advantage in the PRO group, recruitment was stopped, and control patients were moved to the PRO group. After 2 years of follow-up, 40 patients (66.7%) in the control group had died, compared with 29 patients (47.5%) in the PRO group. Before censoring for crossover, median overall survival (OS) was 22.5 months in the PRO group, compared with 14.9 months in the control group (P = .03). Censoring for crossover widened the gap between groups by more than a month (22.5 vs. 13.5 months; P = .005).
“A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier,” the investigators concluded.
The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer institute, Lilly, and others.
SOURCE: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance, according to a recent French study.
Self-reporting may notify care providers about adverse effects or recurrence earlier than imaging, suggested lead author, Fabrice Denis, MD, PhD, of Institut Inter-régional de Cancérologie Jean Bernard in Le Mans, France, and his colleagues. Findings were published in a letter in JAMA.
In 2017, a similar, single-center study showed that web-based symptom reporting could improve survival in patients undergoing chemotherapy. The lead investigator on that trial was Ethan Basch, MD, who coauthored the present publication.
The current, prospective study involved 121 patients treated at five centers in France between June 2014 and December 2017. Eligibility required a diagnosis of nonprogressive, metastatic lung cancer, including stage III or IV non–small cell or small cell disease. Patients were treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Patients in the control group had standard follow-up with imaging every 3-6 months. In contrast, the patient-reported outcomes (PRO) group completed a weekly online survey of 13 common symptoms between follow-up visits. If patients reported symptoms that matched with predefined criteria for severity or worsening, then the treating oncologist was notified.
When an 18-month interim analysis showed significant survival advantage in the PRO group, recruitment was stopped, and control patients were moved to the PRO group. After 2 years of follow-up, 40 patients (66.7%) in the control group had died, compared with 29 patients (47.5%) in the PRO group. Before censoring for crossover, median overall survival (OS) was 22.5 months in the PRO group, compared with 14.9 months in the control group (P = .03). Censoring for crossover widened the gap between groups by more than a month (22.5 vs. 13.5 months; P = .005).
“A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier,” the investigators concluded.
The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer institute, Lilly, and others.
SOURCE: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance, according to a recent French study.
Self-reporting may notify care providers about adverse effects or recurrence earlier than imaging, suggested lead author, Fabrice Denis, MD, PhD, of Institut Inter-régional de Cancérologie Jean Bernard in Le Mans, France, and his colleagues. Findings were published in a letter in JAMA.
In 2017, a similar, single-center study showed that web-based symptom reporting could improve survival in patients undergoing chemotherapy. The lead investigator on that trial was Ethan Basch, MD, who coauthored the present publication.
The current, prospective study involved 121 patients treated at five centers in France between June 2014 and December 2017. Eligibility required a diagnosis of nonprogressive, metastatic lung cancer, including stage III or IV non–small cell or small cell disease. Patients were treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Patients in the control group had standard follow-up with imaging every 3-6 months. In contrast, the patient-reported outcomes (PRO) group completed a weekly online survey of 13 common symptoms between follow-up visits. If patients reported symptoms that matched with predefined criteria for severity or worsening, then the treating oncologist was notified.
When an 18-month interim analysis showed significant survival advantage in the PRO group, recruitment was stopped, and control patients were moved to the PRO group. After 2 years of follow-up, 40 patients (66.7%) in the control group had died, compared with 29 patients (47.5%) in the PRO group. Before censoring for crossover, median overall survival (OS) was 22.5 months in the PRO group, compared with 14.9 months in the control group (P = .03). Censoring for crossover widened the gap between groups by more than a month (22.5 vs. 13.5 months; P = .005).
“A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier,” the investigators concluded.
The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer institute, Lilly, and others.
SOURCE: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
FROM JAMA
Key clinical point: Patients with nonprogressive, metastatic lung cancer who report symptoms through a weekly, web-based monitoring system may survive longer than those who undergo standard imaging surveillance.
Major finding: Median overall survival (OS) of patients in the web-based monitoring group was 22.5 months versus 13.5 months for patients in the standard imaging group (P = .005).
Study details: A prospective study of 121 nonprogressive, metastatic lung cancer patients being treated with antiangiogenic therapy, chemotherapy, immunotherapy, or tyrosine kinase inhibitors.
Disclosures: The study was funded by SIVAN Innovation. Investigators reported financial affiliations with AstraZeneca, SIVAN Innovation, Ipsen, Roche, the National Cancer Institute, Lilly, and others.
Source: Denis F et al. JAMA. 2019 Jan 22;321(3):306-7.
High postpartum breast cancer metastasis risk may persist for a decade
Increased risk of metastasis associated with postpartum breast cancer (PPBC) in women 45 years or younger may persist for 10 years after childbirth, a finding that may give reason to extend the 5-year window currently defining PPBC.
Analysis of more than 700 patients showed that risk of metastasis was approximately twofold higher for a decade after childbirth, with risks about 3.5- to fivefold higher in women diagnosed with stage I or II disease, reported lead author Erica Goddard, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues. Regardless of parity status, patients diagnosed with stage III disease had poor outcomes.
“The high risk for metastasis is independent of poor prognostic indicators, including biological subtype, stage, age, or year of diagnosis,” the investigators wrote in JAMA Network Open. “Yet, PPBC is an underrecognized subset of breast cancer, and few studies address the associated high risk for metastasis.”
The cohort study involved 701 women 45 years or younger who were diagnosed with breast cancer between 1981 and 2014. Early cases were retrospective, until the study switched to a prospective method in 2004. The investigators analyzed rates of distant metastasis and looked for associations with tumor cell proliferation, lymphovascular invasion, lymph node involvement, and other clinical attributes. Distant metastasis was defined by spread beyond the ipsilateral breast or local draining lymph node, as detected by physical exam, imaging, and/or pathological testing. The investigators also stained available tumor samples for Ki67 positivity, which is used for prognostic purposes, and to distinguish between ER-positive luminal A versus ER-positive luminal B disease.
Compared with nulliparous patients, women under 45 who were diagnosed with PPBC within 5 years of childbirth were 2.13 times as likely to develop metastasis (P = .009). This risk persisted for 5 more years. Women diagnosed within 5-10 years of childbirth showed a similar hazard ratio, of 2.23 (P = .006). After 10 years, the hazard ratio dropped to 1.6, but this value was statistically insignificant (P = .13). Patients identified with stage I or II disease had more dramatic risk profiles, with hazard ratios of 3.5 and 5.2, for diagnoses up to 5 years postpartum, and diagnoses 5-10 years postpartum, respectively. These findings suggest that, for some patients, the 5- to 10-year window may be the riskiest time for metastasis, and, incidentally, one that has historically been excluded from the definition of PPBC.
In addition, patients diagnosed with estrogen receptor–positive breast cancer within 10 years of childbirth had outcomes similar to those of nulliparous women with estrogen receptor–negative breast cancer, and postpartum women with estrogen receptor–negative breast cancer had worse outcomes than did nulliparous women with the same subtype. Furthermore, PPBC was associated with higher rates of lymph node involvement and lymphovascular invasion. Collectively, these findings suggest that PPBC is generally more aggressive than nulliparous breast cancer. In contrast, Ki67 positivity, identifying the luminal B subtype, was associated with worse outcome regardless of parity status, but this finding was statistically insignificant.
“[T]hese data suggest that stages I and II breast cancer in patients with PPBC diagnosed within 10 years of parturition may be underestimated in their risk for metastasis, as parity status is not currently factored into clinical decision-making algorithms, such as the National Comprehensive Cancer Network guidelines,” the investigators concluded. “In sum, we suggest that poor-prognostic PPBC is an increasing problem that merits more dedicated research.”
The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
SOURCE: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.
Increased risk of metastasis associated with postpartum breast cancer (PPBC) in women 45 years or younger may persist for 10 years after childbirth, a finding that may give reason to extend the 5-year window currently defining PPBC.
Analysis of more than 700 patients showed that risk of metastasis was approximately twofold higher for a decade after childbirth, with risks about 3.5- to fivefold higher in women diagnosed with stage I or II disease, reported lead author Erica Goddard, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues. Regardless of parity status, patients diagnosed with stage III disease had poor outcomes.
“The high risk for metastasis is independent of poor prognostic indicators, including biological subtype, stage, age, or year of diagnosis,” the investigators wrote in JAMA Network Open. “Yet, PPBC is an underrecognized subset of breast cancer, and few studies address the associated high risk for metastasis.”
The cohort study involved 701 women 45 years or younger who were diagnosed with breast cancer between 1981 and 2014. Early cases were retrospective, until the study switched to a prospective method in 2004. The investigators analyzed rates of distant metastasis and looked for associations with tumor cell proliferation, lymphovascular invasion, lymph node involvement, and other clinical attributes. Distant metastasis was defined by spread beyond the ipsilateral breast or local draining lymph node, as detected by physical exam, imaging, and/or pathological testing. The investigators also stained available tumor samples for Ki67 positivity, which is used for prognostic purposes, and to distinguish between ER-positive luminal A versus ER-positive luminal B disease.
Compared with nulliparous patients, women under 45 who were diagnosed with PPBC within 5 years of childbirth were 2.13 times as likely to develop metastasis (P = .009). This risk persisted for 5 more years. Women diagnosed within 5-10 years of childbirth showed a similar hazard ratio, of 2.23 (P = .006). After 10 years, the hazard ratio dropped to 1.6, but this value was statistically insignificant (P = .13). Patients identified with stage I or II disease had more dramatic risk profiles, with hazard ratios of 3.5 and 5.2, for diagnoses up to 5 years postpartum, and diagnoses 5-10 years postpartum, respectively. These findings suggest that, for some patients, the 5- to 10-year window may be the riskiest time for metastasis, and, incidentally, one that has historically been excluded from the definition of PPBC.
In addition, patients diagnosed with estrogen receptor–positive breast cancer within 10 years of childbirth had outcomes similar to those of nulliparous women with estrogen receptor–negative breast cancer, and postpartum women with estrogen receptor–negative breast cancer had worse outcomes than did nulliparous women with the same subtype. Furthermore, PPBC was associated with higher rates of lymph node involvement and lymphovascular invasion. Collectively, these findings suggest that PPBC is generally more aggressive than nulliparous breast cancer. In contrast, Ki67 positivity, identifying the luminal B subtype, was associated with worse outcome regardless of parity status, but this finding was statistically insignificant.
“[T]hese data suggest that stages I and II breast cancer in patients with PPBC diagnosed within 10 years of parturition may be underestimated in their risk for metastasis, as parity status is not currently factored into clinical decision-making algorithms, such as the National Comprehensive Cancer Network guidelines,” the investigators concluded. “In sum, we suggest that poor-prognostic PPBC is an increasing problem that merits more dedicated research.”
The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
SOURCE: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.
Increased risk of metastasis associated with postpartum breast cancer (PPBC) in women 45 years or younger may persist for 10 years after childbirth, a finding that may give reason to extend the 5-year window currently defining PPBC.
Analysis of more than 700 patients showed that risk of metastasis was approximately twofold higher for a decade after childbirth, with risks about 3.5- to fivefold higher in women diagnosed with stage I or II disease, reported lead author Erica Goddard, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues. Regardless of parity status, patients diagnosed with stage III disease had poor outcomes.
“The high risk for metastasis is independent of poor prognostic indicators, including biological subtype, stage, age, or year of diagnosis,” the investigators wrote in JAMA Network Open. “Yet, PPBC is an underrecognized subset of breast cancer, and few studies address the associated high risk for metastasis.”
The cohort study involved 701 women 45 years or younger who were diagnosed with breast cancer between 1981 and 2014. Early cases were retrospective, until the study switched to a prospective method in 2004. The investigators analyzed rates of distant metastasis and looked for associations with tumor cell proliferation, lymphovascular invasion, lymph node involvement, and other clinical attributes. Distant metastasis was defined by spread beyond the ipsilateral breast or local draining lymph node, as detected by physical exam, imaging, and/or pathological testing. The investigators also stained available tumor samples for Ki67 positivity, which is used for prognostic purposes, and to distinguish between ER-positive luminal A versus ER-positive luminal B disease.
Compared with nulliparous patients, women under 45 who were diagnosed with PPBC within 5 years of childbirth were 2.13 times as likely to develop metastasis (P = .009). This risk persisted for 5 more years. Women diagnosed within 5-10 years of childbirth showed a similar hazard ratio, of 2.23 (P = .006). After 10 years, the hazard ratio dropped to 1.6, but this value was statistically insignificant (P = .13). Patients identified with stage I or II disease had more dramatic risk profiles, with hazard ratios of 3.5 and 5.2, for diagnoses up to 5 years postpartum, and diagnoses 5-10 years postpartum, respectively. These findings suggest that, for some patients, the 5- to 10-year window may be the riskiest time for metastasis, and, incidentally, one that has historically been excluded from the definition of PPBC.
In addition, patients diagnosed with estrogen receptor–positive breast cancer within 10 years of childbirth had outcomes similar to those of nulliparous women with estrogen receptor–negative breast cancer, and postpartum women with estrogen receptor–negative breast cancer had worse outcomes than did nulliparous women with the same subtype. Furthermore, PPBC was associated with higher rates of lymph node involvement and lymphovascular invasion. Collectively, these findings suggest that PPBC is generally more aggressive than nulliparous breast cancer. In contrast, Ki67 positivity, identifying the luminal B subtype, was associated with worse outcome regardless of parity status, but this finding was statistically insignificant.
“[T]hese data suggest that stages I and II breast cancer in patients with PPBC diagnosed within 10 years of parturition may be underestimated in their risk for metastasis, as parity status is not currently factored into clinical decision-making algorithms, such as the National Comprehensive Cancer Network guidelines,” the investigators concluded. “In sum, we suggest that poor-prognostic PPBC is an increasing problem that merits more dedicated research.”
The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
SOURCE: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.
FROM JAMA NETWORK OPEN
Key clinical point: Increased risk of metastasis associated with postpartum breast cancer in women 45 years or younger may persist for 10 years after childbirth, instead of 5 years, as previously reported.
Major finding: Compared with nulliparous breast cancer patients, women 45 years or younger diagnosed with breast cancer within 5-10 years of childbirth were 2.23 times as likely to develop metastasis.
Study details: A retrospective and prospective cohort study involving 701 women with stage I, II, or III breast cancer who were 45 years or younger at time of diagnosis.
Disclosures: The study was funded by the National Cancer Institute, the National Institutes of Health, the U.S. Department of Defense, and other organizations. Dr. Goddard reported funding from the NCI and NIH. Dr. Mori reported financial support from the Department of Defense.
Source: Goddard et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.6997.
Checkpoint inhibitors linked to rare, but serious immune-related side effects
Checkpoint inhibitors can cause rare, but serious, hematological immune-related adverse events (hem-irAEs), which require early detection and intervention, according to a recent French study.
Immune thrombocytopenia, hemolytic anemia, and neutropenia were the most common hem-irAEs in the population, reported lead author, Nicolas Delanoy, MD, of Gustave Roussy, Université Paris-Saclay, Villejuif, France, and his colleagues.
“About 71% of patients treated have any-grade irAEs and 10% have grade 3-4 irAEs after anti-PD-1 immunotherapy,” the investigators wrote. The report is in The Lancet Haematology. “In most cases, they involve the skin, gastrointestinal tract, thyroid or endocrine glands, liver, lungs, or joints. However, all organs can potentially be affected, including the hemopoietic system.”
Despite this possibility, few reports detail the frequency or character of hematological toxicities from immunotherapy.
The present study involved 948 patients who entered into three French registries between 2014 and 2018. The first registry, consisting of 745 patients, was observed prospectively during checkpoint inhibitor therapy. The other two registries provided retrospective data on confirmed irAEs or hem-irAEs.
Among 745 patients followed during checkpoint inhibitor therapy, four developed hem-irAEs, providing an incidence rate of 0.5%. The other two databases added 31 patients with confirmed hem-irAEs, allowing for characterization of 35 total cases.
The group of 35 patients had a median age of 65 years, with more men (n = 21) than women (n = 14). Melanoma was the most common type of malignancy (43%), followed by non–small-cell lung cancer (34%), lymphoma (11%), and others. The majority of patients received nivolumab (57%), slightly fewer received pembrolizumab (40%), and a small minority received atezolizumab (3%).
Immune thrombocytopenia, hemolytic anemia, and neutropenia were the most common hem-irAEs, each occurring in nine patients (26%). Five patients (14%) had aplastic anemia or pancytopenia, two patients had bicytopenia (6%; neutropenia and anemia or thrombocytopenia and anemia), and one patient had pure red cell aplasia (3%).
Hem-irAEs resolved in 60% of patients, but two patients (6%) died due to febrile neutropenia. Overall, 71% of hem-irAEs were grade 4.
These findings suggest that hem-irAEs are rare, but they are often serious, and potentially life-threatening, the researchers noted.
In 7 of 35 patients (20%) who were rechallenged with checkpoint inhibitor therapy, 3 (43%) had recurrence of hem-irAEs. This finding should elicit caution and close monitoring if rechallenge is elected.
“This observational study encourages further, in-depth investigations of hematological immune toxicities, to search for biomarkers that can be helpful for earlier detection,” the investigators concluded.
This study was funded by Gustave Roussy and the Gustave Roussy Immunotherapy Program. Dr. Delanoy reported nonfinancial support from Sanofi and other authors reported financial relationships with pharmaceutical companies.
SOURCE: Delanoy N et al. Lancet Haematol. 2018 Dec 4. doi: 10.1016/S2352-3026(18)30175-3.
Checkpoint inhibitors can cause rare, but serious, hematological immune-related adverse events (hem-irAEs), which require early detection and intervention, according to a recent French study.
Immune thrombocytopenia, hemolytic anemia, and neutropenia were the most common hem-irAEs in the population, reported lead author, Nicolas Delanoy, MD, of Gustave Roussy, Université Paris-Saclay, Villejuif, France, and his colleagues.
“About 71% of patients treated have any-grade irAEs and 10% have grade 3-4 irAEs after anti-PD-1 immunotherapy,” the investigators wrote. The report is in The Lancet Haematology. “In most cases, they involve the skin, gastrointestinal tract, thyroid or endocrine glands, liver, lungs, or joints. However, all organs can potentially be affected, including the hemopoietic system.”
Despite this possibility, few reports detail the frequency or character of hematological toxicities from immunotherapy.
The present study involved 948 patients who entered into three French registries between 2014 and 2018. The first registry, consisting of 745 patients, was observed prospectively during checkpoint inhibitor therapy. The other two registries provided retrospective data on confirmed irAEs or hem-irAEs.
Among 745 patients followed during checkpoint inhibitor therapy, four developed hem-irAEs, providing an incidence rate of 0.5%. The other two databases added 31 patients with confirmed hem-irAEs, allowing for characterization of 35 total cases.
The group of 35 patients had a median age of 65 years, with more men (n = 21) than women (n = 14). Melanoma was the most common type of malignancy (43%), followed by non–small-cell lung cancer (34%), lymphoma (11%), and others. The majority of patients received nivolumab (57%), slightly fewer received pembrolizumab (40%), and a small minority received atezolizumab (3%).
Immune thrombocytopenia, hemolytic anemia, and neutropenia were the most common hem-irAEs, each occurring in nine patients (26%). Five patients (14%) had aplastic anemia or pancytopenia, two patients had bicytopenia (6%; neutropenia and anemia or thrombocytopenia and anemia), and one patient had pure red cell aplasia (3%).
Hem-irAEs resolved in 60% of patients, but two patients (6%) died due to febrile neutropenia. Overall, 71% of hem-irAEs were grade 4.
These findings suggest that hem-irAEs are rare, but they are often serious, and potentially life-threatening, the researchers noted.
In 7 of 35 patients (20%) who were rechallenged with checkpoint inhibitor therapy, 3 (43%) had recurrence of hem-irAEs. This finding should elicit caution and close monitoring if rechallenge is elected.
“This observational study encourages further, in-depth investigations of hematological immune toxicities, to search for biomarkers that can be helpful for earlier detection,” the investigators concluded.
This study was funded by Gustave Roussy and the Gustave Roussy Immunotherapy Program. Dr. Delanoy reported nonfinancial support from Sanofi and other authors reported financial relationships with pharmaceutical companies.
SOURCE: Delanoy N et al. Lancet Haematol. 2018 Dec 4. doi: 10.1016/S2352-3026(18)30175-3.
Checkpoint inhibitors can cause rare, but serious, hematological immune-related adverse events (hem-irAEs), which require early detection and intervention, according to a recent French study.
Immune thrombocytopenia, hemolytic anemia, and neutropenia were the most common hem-irAEs in the population, reported lead author, Nicolas Delanoy, MD, of Gustave Roussy, Université Paris-Saclay, Villejuif, France, and his colleagues.
“About 71% of patients treated have any-grade irAEs and 10% have grade 3-4 irAEs after anti-PD-1 immunotherapy,” the investigators wrote. The report is in The Lancet Haematology. “In most cases, they involve the skin, gastrointestinal tract, thyroid or endocrine glands, liver, lungs, or joints. However, all organs can potentially be affected, including the hemopoietic system.”
Despite this possibility, few reports detail the frequency or character of hematological toxicities from immunotherapy.
The present study involved 948 patients who entered into three French registries between 2014 and 2018. The first registry, consisting of 745 patients, was observed prospectively during checkpoint inhibitor therapy. The other two registries provided retrospective data on confirmed irAEs or hem-irAEs.
Among 745 patients followed during checkpoint inhibitor therapy, four developed hem-irAEs, providing an incidence rate of 0.5%. The other two databases added 31 patients with confirmed hem-irAEs, allowing for characterization of 35 total cases.
The group of 35 patients had a median age of 65 years, with more men (n = 21) than women (n = 14). Melanoma was the most common type of malignancy (43%), followed by non–small-cell lung cancer (34%), lymphoma (11%), and others. The majority of patients received nivolumab (57%), slightly fewer received pembrolizumab (40%), and a small minority received atezolizumab (3%).
Immune thrombocytopenia, hemolytic anemia, and neutropenia were the most common hem-irAEs, each occurring in nine patients (26%). Five patients (14%) had aplastic anemia or pancytopenia, two patients had bicytopenia (6%; neutropenia and anemia or thrombocytopenia and anemia), and one patient had pure red cell aplasia (3%).
Hem-irAEs resolved in 60% of patients, but two patients (6%) died due to febrile neutropenia. Overall, 71% of hem-irAEs were grade 4.
These findings suggest that hem-irAEs are rare, but they are often serious, and potentially life-threatening, the researchers noted.
In 7 of 35 patients (20%) who were rechallenged with checkpoint inhibitor therapy, 3 (43%) had recurrence of hem-irAEs. This finding should elicit caution and close monitoring if rechallenge is elected.
“This observational study encourages further, in-depth investigations of hematological immune toxicities, to search for biomarkers that can be helpful for earlier detection,” the investigators concluded.
This study was funded by Gustave Roussy and the Gustave Roussy Immunotherapy Program. Dr. Delanoy reported nonfinancial support from Sanofi and other authors reported financial relationships with pharmaceutical companies.
SOURCE: Delanoy N et al. Lancet Haematol. 2018 Dec 4. doi: 10.1016/S2352-3026(18)30175-3.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: Checkpoint inhibitor therapy led to hematological toxicity in 0.5% of patients.
Study details: A study of 948 patients in French registries who were observed prospectively or retrospectively, including a case series of 35 patients treated with checkpoint inhibitor therapy who developed hematologic, immune-related adverse events.
Disclosures: This study was funded by Gustave Roussy and the Gustave Roussy Immunotherapy Program. Dr. Delanoy reported nonfinancial support from Sanofi and other authors reported financial relationships with pharmaceutical companies.
Source: Delanoy N et al. Lancet Haematol. 2018 Dec 4. doi: 10.1016/S2352-3026(18)30175-3.
CRS/HIPEC safety concerns may be outdated
, according to a retrospective study involving more than 34,000 cases.
Compared with four other surgical oncology procedures considered high risk, CRS/HIPEC had the lowest 30-day mortality rate, reported lead author Jason M. Foster, MD, of the University of Nebraska Medical Center in Omaha, and his colleagues.
“The perception of high morbidity, high mortality, and poor surgical outcomes remains a barrier to CRS/HIPEC patient referral as well as clinical trial development in the United States, despite the published noncomparative data establishing contemporary safety,” the investigators wrote in JAMA Network Open.
The study involved 34,114 patients from the American College of Surgeons National Surgical Quality Improvement Project (NSQIP) database who underwent CRS/HIPEC (n = 1,822), trisegmental hepatectomy (n = 2,449), right lobe hepatectomy (n = 5,109), pancreaticoduodenectomy (Whipple; n = 16,793), or esophagectomy (n = 7,941) during 2005-2015. The investigators rates of overall 30-day postoperative mortality, superficial incisional infection, deep incisional infection, organ space infection, return to operating room, and length of hospital stay.
Analysis revealed that CRS/HIPEC had a 30-day mortality rate of 1.1%, which was lower than rates of 2.5%-3.9% for the comparative procedures. Similarly, organ space infection rate was lowest for CRS/HIPEC (7.2%). Superficial and deep incisional infection rates were 5.4% and 1.7%, respectively, for CRS/HIPEC, lower than all procedures except right lobe hepatectomy, with rates of 4.6% and 1.5%. Return to OR was necessary for 6.8% of CRS/HIPEC patients, a rate similar to the other procedures except esophagectomy, in which return to OR was necessary 14.4% of the time. Finally, CRS/HIPEC had a median length of stay of 8 days, which was slightly longer than right lobe or trisegmental hepatectomy (7 days), but shorter than Whipple procedure or esophagectomy (10 days.)
“This study found that CRS/HIPEC had the lowest mortality risk, almost 50%-75% lower than other advanced oncology surgical procedures,” the investigators noted. “These findings provide objective data to dispel the misperception of morbidity and mortality concerns surrounding CRS/HIPEC, and surgical risk should no longer remain a deterrent to patient referral or development of clinical trials for CRS/HIPEC.”
The study was funded by the Platon Foundation and the Hill Foundation. The authors reported no conflicts of interest.
SOURCE: Foster JM et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.6847.
The recent study by Foster et al. provides insight into the national safety of reductive surgery combined with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC); however, more detailed safety and efficacy data are needed to influence current practices, according to Margaret Smith, MD, and Hari Nathan, MD, PhD.
A closer look at the Foster et al. study reveals three key limitations: First, “cytoreductive surgery encompasses a wide range of procedures, from resection of one peritoneal nodule to multivisceral resection with peritoneal stripping, and, thus, reflects a wide range of possible morbidity,” the authors wrote in an editorial for JAMA Network Open. Therefore, the findings may not represent certain patient populations.
Second, “comparison with other procedures for different indications constructs a straw man.” In contrast with some candidates for CRS/HIPEC, “a patient with pancreatic cancer has no other curative option besides a Whipple procedure.” This imperfect comparison should be considered as such.
Third, the safety of CRS/HIPEC may not be the procedure’s primary limitation. “A more salient concern may be its oncologic effectiveness,” the authors wrote.
Although a clinical randomized trial from 2003 involving patients with colorectal peritoneal carcinomatosis showed a near doubling of overall survival with CRS/HIPEC, compared with systemic chemotherapy alone (22 vs. 12.5 months), a comprehensive understanding of safety and efficacy is lacking, particularly regarding the inclusion of HIPEC. For example, the recent phase 3 Prodige 7 trial showed that addition of HIPEC to CRS added morbidity without survival advantage in patients with colorectal peritoneal carcinomatosis; in contrast, a separate phase 3 trial in epithelial ovarian cancer showed that adding HIPEC to CRS did extend survival.
“…Others have cautioned against changing practice based on these results given concerns over small sample size, imbalances in effects seen across centers, and overall survival with CRS/HIPEC that was similar to other studies’ reported survival following interval debulking alone. Legitimate concerns regarding the efficacy of CRS/HIPEC exist, and appropriate patient selection for this aggressive treatment remains a challenge. Foster et al. demonstrates acceptable morbidity and mortality rates for CRS/HIPEC in this highly selected patient cohort. However, until the benefit for individual patients is more thoroughly understood, clinician referral and treatment practices will remain difficult to transform,” the authors wrote.
Dr. Smith and Dr. Nathan are affiliated with Michigan Medicine at the University of Michigan in Ann Arbor. These comments are adapted from the accompanying editorial (JAMA Netw Open 2019 Jan 11. doi:10.1001/jamanetworkopen.2018.6839).
The recent study by Foster et al. provides insight into the national safety of reductive surgery combined with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC); however, more detailed safety and efficacy data are needed to influence current practices, according to Margaret Smith, MD, and Hari Nathan, MD, PhD.
A closer look at the Foster et al. study reveals three key limitations: First, “cytoreductive surgery encompasses a wide range of procedures, from resection of one peritoneal nodule to multivisceral resection with peritoneal stripping, and, thus, reflects a wide range of possible morbidity,” the authors wrote in an editorial for JAMA Network Open. Therefore, the findings may not represent certain patient populations.
Second, “comparison with other procedures for different indications constructs a straw man.” In contrast with some candidates for CRS/HIPEC, “a patient with pancreatic cancer has no other curative option besides a Whipple procedure.” This imperfect comparison should be considered as such.
Third, the safety of CRS/HIPEC may not be the procedure’s primary limitation. “A more salient concern may be its oncologic effectiveness,” the authors wrote.
Although a clinical randomized trial from 2003 involving patients with colorectal peritoneal carcinomatosis showed a near doubling of overall survival with CRS/HIPEC, compared with systemic chemotherapy alone (22 vs. 12.5 months), a comprehensive understanding of safety and efficacy is lacking, particularly regarding the inclusion of HIPEC. For example, the recent phase 3 Prodige 7 trial showed that addition of HIPEC to CRS added morbidity without survival advantage in patients with colorectal peritoneal carcinomatosis; in contrast, a separate phase 3 trial in epithelial ovarian cancer showed that adding HIPEC to CRS did extend survival.
“…Others have cautioned against changing practice based on these results given concerns over small sample size, imbalances in effects seen across centers, and overall survival with CRS/HIPEC that was similar to other studies’ reported survival following interval debulking alone. Legitimate concerns regarding the efficacy of CRS/HIPEC exist, and appropriate patient selection for this aggressive treatment remains a challenge. Foster et al. demonstrates acceptable morbidity and mortality rates for CRS/HIPEC in this highly selected patient cohort. However, until the benefit for individual patients is more thoroughly understood, clinician referral and treatment practices will remain difficult to transform,” the authors wrote.
Dr. Smith and Dr. Nathan are affiliated with Michigan Medicine at the University of Michigan in Ann Arbor. These comments are adapted from the accompanying editorial (JAMA Netw Open 2019 Jan 11. doi:10.1001/jamanetworkopen.2018.6839).
The recent study by Foster et al. provides insight into the national safety of reductive surgery combined with hyperthermic intraperitoneal chemotherapy (CRS/HIPEC); however, more detailed safety and efficacy data are needed to influence current practices, according to Margaret Smith, MD, and Hari Nathan, MD, PhD.
A closer look at the Foster et al. study reveals three key limitations: First, “cytoreductive surgery encompasses a wide range of procedures, from resection of one peritoneal nodule to multivisceral resection with peritoneal stripping, and, thus, reflects a wide range of possible morbidity,” the authors wrote in an editorial for JAMA Network Open. Therefore, the findings may not represent certain patient populations.
Second, “comparison with other procedures for different indications constructs a straw man.” In contrast with some candidates for CRS/HIPEC, “a patient with pancreatic cancer has no other curative option besides a Whipple procedure.” This imperfect comparison should be considered as such.
Third, the safety of CRS/HIPEC may not be the procedure’s primary limitation. “A more salient concern may be its oncologic effectiveness,” the authors wrote.
Although a clinical randomized trial from 2003 involving patients with colorectal peritoneal carcinomatosis showed a near doubling of overall survival with CRS/HIPEC, compared with systemic chemotherapy alone (22 vs. 12.5 months), a comprehensive understanding of safety and efficacy is lacking, particularly regarding the inclusion of HIPEC. For example, the recent phase 3 Prodige 7 trial showed that addition of HIPEC to CRS added morbidity without survival advantage in patients with colorectal peritoneal carcinomatosis; in contrast, a separate phase 3 trial in epithelial ovarian cancer showed that adding HIPEC to CRS did extend survival.
“…Others have cautioned against changing practice based on these results given concerns over small sample size, imbalances in effects seen across centers, and overall survival with CRS/HIPEC that was similar to other studies’ reported survival following interval debulking alone. Legitimate concerns regarding the efficacy of CRS/HIPEC exist, and appropriate patient selection for this aggressive treatment remains a challenge. Foster et al. demonstrates acceptable morbidity and mortality rates for CRS/HIPEC in this highly selected patient cohort. However, until the benefit for individual patients is more thoroughly understood, clinician referral and treatment practices will remain difficult to transform,” the authors wrote.
Dr. Smith and Dr. Nathan are affiliated with Michigan Medicine at the University of Michigan in Ann Arbor. These comments are adapted from the accompanying editorial (JAMA Netw Open 2019 Jan 11. doi:10.1001/jamanetworkopen.2018.6839).
, according to a retrospective study involving more than 34,000 cases.
Compared with four other surgical oncology procedures considered high risk, CRS/HIPEC had the lowest 30-day mortality rate, reported lead author Jason M. Foster, MD, of the University of Nebraska Medical Center in Omaha, and his colleagues.
“The perception of high morbidity, high mortality, and poor surgical outcomes remains a barrier to CRS/HIPEC patient referral as well as clinical trial development in the United States, despite the published noncomparative data establishing contemporary safety,” the investigators wrote in JAMA Network Open.
The study involved 34,114 patients from the American College of Surgeons National Surgical Quality Improvement Project (NSQIP) database who underwent CRS/HIPEC (n = 1,822), trisegmental hepatectomy (n = 2,449), right lobe hepatectomy (n = 5,109), pancreaticoduodenectomy (Whipple; n = 16,793), or esophagectomy (n = 7,941) during 2005-2015. The investigators rates of overall 30-day postoperative mortality, superficial incisional infection, deep incisional infection, organ space infection, return to operating room, and length of hospital stay.
Analysis revealed that CRS/HIPEC had a 30-day mortality rate of 1.1%, which was lower than rates of 2.5%-3.9% for the comparative procedures. Similarly, organ space infection rate was lowest for CRS/HIPEC (7.2%). Superficial and deep incisional infection rates were 5.4% and 1.7%, respectively, for CRS/HIPEC, lower than all procedures except right lobe hepatectomy, with rates of 4.6% and 1.5%. Return to OR was necessary for 6.8% of CRS/HIPEC patients, a rate similar to the other procedures except esophagectomy, in which return to OR was necessary 14.4% of the time. Finally, CRS/HIPEC had a median length of stay of 8 days, which was slightly longer than right lobe or trisegmental hepatectomy (7 days), but shorter than Whipple procedure or esophagectomy (10 days.)
“This study found that CRS/HIPEC had the lowest mortality risk, almost 50%-75% lower than other advanced oncology surgical procedures,” the investigators noted. “These findings provide objective data to dispel the misperception of morbidity and mortality concerns surrounding CRS/HIPEC, and surgical risk should no longer remain a deterrent to patient referral or development of clinical trials for CRS/HIPEC.”
The study was funded by the Platon Foundation and the Hill Foundation. The authors reported no conflicts of interest.
SOURCE: Foster JM et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.6847.
, according to a retrospective study involving more than 34,000 cases.
Compared with four other surgical oncology procedures considered high risk, CRS/HIPEC had the lowest 30-day mortality rate, reported lead author Jason M. Foster, MD, of the University of Nebraska Medical Center in Omaha, and his colleagues.
“The perception of high morbidity, high mortality, and poor surgical outcomes remains a barrier to CRS/HIPEC patient referral as well as clinical trial development in the United States, despite the published noncomparative data establishing contemporary safety,” the investigators wrote in JAMA Network Open.
The study involved 34,114 patients from the American College of Surgeons National Surgical Quality Improvement Project (NSQIP) database who underwent CRS/HIPEC (n = 1,822), trisegmental hepatectomy (n = 2,449), right lobe hepatectomy (n = 5,109), pancreaticoduodenectomy (Whipple; n = 16,793), or esophagectomy (n = 7,941) during 2005-2015. The investigators rates of overall 30-day postoperative mortality, superficial incisional infection, deep incisional infection, organ space infection, return to operating room, and length of hospital stay.
Analysis revealed that CRS/HIPEC had a 30-day mortality rate of 1.1%, which was lower than rates of 2.5%-3.9% for the comparative procedures. Similarly, organ space infection rate was lowest for CRS/HIPEC (7.2%). Superficial and deep incisional infection rates were 5.4% and 1.7%, respectively, for CRS/HIPEC, lower than all procedures except right lobe hepatectomy, with rates of 4.6% and 1.5%. Return to OR was necessary for 6.8% of CRS/HIPEC patients, a rate similar to the other procedures except esophagectomy, in which return to OR was necessary 14.4% of the time. Finally, CRS/HIPEC had a median length of stay of 8 days, which was slightly longer than right lobe or trisegmental hepatectomy (7 days), but shorter than Whipple procedure or esophagectomy (10 days.)
“This study found that CRS/HIPEC had the lowest mortality risk, almost 50%-75% lower than other advanced oncology surgical procedures,” the investigators noted. “These findings provide objective data to dispel the misperception of morbidity and mortality concerns surrounding CRS/HIPEC, and surgical risk should no longer remain a deterrent to patient referral or development of clinical trials for CRS/HIPEC.”
The study was funded by the Platon Foundation and the Hill Foundation. The authors reported no conflicts of interest.
SOURCE: Foster JM et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.6847.
FROM JAMA NETWORK OPEN
Key clinical point: Cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) appears safe, and concerns about high complication rates may be outdated.
Major finding: CRS/HIPEC had a 30-day mortality rate of 1.1%, which was lower than rates of 2.5%-3.9% for comparative high-risk surgical oncology procedures.
Study details: A retrospective study of 34,114 patients from the American College of Surgeons National Surgical Quality Improvement Project (NSQIP) database who underwent CRS/HIPEC (n = 1,822), trisegmental hepatectomy (n = 2,449), right lobe hepatectomy (n = 5,109), pancreaticoduodenectomy (Whipple; n = 16,793), or esophagectomy (n = 7,941) during 2005-2015.
Disclosures: The study was funded by the Platon Foundation and the Hill Foundation. The authors reported no conflicts of interest.
Source: Foster JM et al. JAMA Netw Open. 2019 Jan 11. doi: 10.1001/jamanetworkopen.2018.6847.
Dietary aluminum may trigger IBS
Aluminum ingested in small amounts causes visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may trigger irritable bowel syndrome (IBS) in humans, according to a study published in Cellular and Molecular Gastroenterology and Hepatology.
Rats given oral aluminum exhibited dose-dependent visceral pain along with activation of proteinase-activated receptor-2 (PAR2) and mast cell degranulation, a combination of events that mirror clinical signs and molecular mechanisms of IBS in humans, reported lead author, Nicolas Esquerre, PhD, of Lille Inflammation Research International Center at Université Lille in France, and his colleagues. The study contributes to ongoing research surrounding causes and mechanisms of IBS, which may vary among patients because of disease subsets. These findings suggest that some patients with IBS may benefit from dietary aluminum restriction or chelation therapy.
“[T]he question of the initial trigger [of IBS] still remains unresolved,” the investigators wrote. “A more precise link between food and IBS has been demonstrated for gluten and other wheat proteins, lactose, and nickel, highlighting particular subsets of IBS patients now diagnosed as nonceliac gluten/wheat sensitivity, lactose intolerance, and nickel-allergic contact mucositis,” they added. “Here, we evaluated the effect of aluminum, a common contaminant of food and water, on abdominal pain.”
Aluminum may enter the diet as a food additive, or it may contaminate foods grown in aluminum-rich soil. Other sources of oral exposure include packaging and kitchenware. A previous study showed that most Americans ingest 0.01-1.4 mg/kg of aluminum daily, and 5% ingest 1.58 mg/kg daily (i.e., 95 mg per day for a 60-kg person).
Based on these statistics, rats in the present study received oral aluminum citrate (AlCi) corresponding with three doses of aluminum: 0.5 mg/kg, 1.5 mg/kg, or 3.0 mg/kg. Treatment continued for 30 days, with colorectal distension (CRD) measured on days 2, 4, 8, 15, and 30.
Results showed a dose-dependent relationship between aluminum ingestion and visceral hypersensitivity. Within 2 days, rats receiving 3.0 mg/kg of aluminum exhibited a significantly lower pain threshold, and within 8 days, rats receiving 0.5 mg/kg and 1.5 mg/kg also showed increased visceral hypersensitivity.
After 1 month of treatment, rats receiving 1.5 mg/kg per day demonstrated a 30% increase in pain compared with control animals. In the same group, visceral hypersensitivity began to wane 7 days after cessation of treatment; 4 more weeks were needed to return to baseline. When treatment was restarted, visceral hypersensitivity occurred within 2 days, compared with 8 days upon initial administration. These findings are particularly relevant to some people, as the 1.5-mg/kg dose corresponds with the daily amount of aluminum ingested by 5% of Americans. Similar patterns of response and sensitization were observed in rats ingesting 0.5 mg/kg and 3.0 mg/kg. Female rats were more sensitive to aluminum than were male rats, a sex pattern that mimics human IBS.
Further testing showed that rats treated with zinc citrate (ZnCi) did not exhibit changes to pain threshold, thereby excluding citrate as an aggravating factor. Rat models of noninflammatory and inflammatory colonic hypersensitivity (butyrate enema or intrathecal injection of 25%-50% ethanol in combination with 2,4,6-trinitrobenzenesulfonic acid, respectively) had visceral hypersensitivity similar to that of rats in the 1.5-mg/kg AlCi group.
Testing of colonic tissue from AlCi-treated rats did not reveal inflammatory changes according to a variety of qualifiers, including histology, myeloperoxidase activity, mRNA expression of several inflammatory cytokines, or infiltration of eosinophils or macrophages. Noninflammatory effects of aluminum, however, were found. For instance, treated rats had lower serotonin levels in enteroendocrine cells.
“Enteroendocrine cells are specialized epithelial cells that respond to luminal stimuli by releasing various biologically active compounds,” the investigators wrote. “They regulate several physiological and homeostatic functions of the gastrointestinal tract, such as postprandial secretion, motility, immune responses, and sensory functions. A reduced number of enteroendocrine cells has been observed in the duodenum, ileum, and colon of some patients with IBS.”
In addition to changes in enteroendocrine cells, AlCi-treated rats had greater colonic mast cell degranulation and histamine with upregulation of histidine decarboxylase transcripts, suggesting that aluminum activated mast cells.
To determine the role of mast cell activation in visceral hypersensitivity, rats were given AlCi with cromoglycate, an inhibitor of mast cell degranulation. This treatment reduced mast cell degranulation and visceral pain threshold, compared with AlCi-treated rats not receiving cromoglycate, suggesting that mast cell degranulation is a primary driver of visceral hypersensitivity. This observation was confirmed by a mast cell–deficient mouse strain (Kit W-sh/W-sh), that had a normal number of mast cells incapable of degranulation. Treating the mast cell–deficient mice with AlCi did not induce visceral hypersensitivity, thereby confirming the role of mast cell degranulation.
Along with mast cell degranulation, AlCi treatment led to PAR2 activation. Investigators explored the significance of this finding with PAR2 knockout mice. When treated with AlCi, PAR2 knockout mice showed no increase in visceral hypersensitivity, suggesting that hypersensitivity is dependent on PAR2 activation. Further testing revealed that mast cell–deficient mice (Kit W-sh/W-sh) did not have PAR2 upregulation either, connecting a sequence in which aluminum triggers mast cell degranulation, mast cell degranulation drives PAR2 upregulation, and PAR2 upregulation causes visceral hypersensitivity. The latter two events in this chain – mast cell degranulation and PAR2 upregulation – mirror molecular mechanisms of IBS in humans.
“We speculate that aluminum activates mast cells to release mediators that can increase excitability of nociceptive afferences contributing to the visceral pain phenotype,” the investigators wrote. “Taken together, our results linked aluminum to several mechanisms implicated in IBS pathophysiology, highlighting a possible role for aluminum as a triggering factor in IBS development.”
The investigators suggested that these findings could influence preventive or therapeutic strategies: “Aluminum might be the first identified dietary risk factor for IBS, implying that measures to limit aluminum dietary consumption or to chelate aluminum may represent novel pathways of prevention and treatment of IBS in some susceptible patients,” they wrote.
The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
SOURCE: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
Irritable bowel syndrome is a chronic functional gastrointestinal disorder, characterized by relapsing/remitting diarrhea, constipation, and visceral pain. IBS afflicts 10%-25% of the population in developed countries.
Despite histologically normal intestinal biopsy specimens, biological signatures of IBS include alterations in intestinal gene expression, increased gut permeability, and changes in gut microbiota composition. Thus, although the cause or causes of IBS are not defined, these and other data highlight the enormous breadth of factors that might play a role in this disorder. Similar alterations also are associated with inflammatory bowel disease (IBD), although the magnitude of changes is typically greater in IBD. Nevertheless, these data suggest that IBS and IBD may share triggers and pathogenetic mechanisms. That prevalence of both IBS and IBD have shown marked increases in incidence, roughly paralleling the modernization of society that accelerated in the mid-20th century, raises the possibility that environmental factors associated with human activity may be a driver of both diseases. Recent findings suggest that aluminum may be one such trigger. While humans have always been exposed to aluminum, the most abundant metal on earth, industrialization has increased the magnitude of exposure owing to the use of aluminum salts as stabilizers in processed foods and the concentration of ground water aluminum in agricultural products. Mimicking estimated average human ingestion of aluminum via administering it orally to rats increases their perception of visceral pain. These results suggest a possible role for increased exposure to aluminum in driving the post–mid-20th-century increased incidence of IBS. Unfortunately, only broad societal estimates of aluminum exposure are available, and aluminum levels are difficult to measure in individuals, making it difficult to epidemiologically investigate the role of aluminum in promoting GI disease in humans. Hence, I submit that levels of aluminum ingestion by humans should be more closely monitored and the potential of aluminum to promote GI disease carefully scrutinized.
Andrew Ted Gewirtz, PhD, distinguished university center professor, Georgia State University’s Institute for Biomedical Sciences’ Center for Inflammation, Immunity and Infection, Atlanta.
Irritable bowel syndrome is a chronic functional gastrointestinal disorder, characterized by relapsing/remitting diarrhea, constipation, and visceral pain. IBS afflicts 10%-25% of the population in developed countries.
Despite histologically normal intestinal biopsy specimens, biological signatures of IBS include alterations in intestinal gene expression, increased gut permeability, and changes in gut microbiota composition. Thus, although the cause or causes of IBS are not defined, these and other data highlight the enormous breadth of factors that might play a role in this disorder. Similar alterations also are associated with inflammatory bowel disease (IBD), although the magnitude of changes is typically greater in IBD. Nevertheless, these data suggest that IBS and IBD may share triggers and pathogenetic mechanisms. That prevalence of both IBS and IBD have shown marked increases in incidence, roughly paralleling the modernization of society that accelerated in the mid-20th century, raises the possibility that environmental factors associated with human activity may be a driver of both diseases. Recent findings suggest that aluminum may be one such trigger. While humans have always been exposed to aluminum, the most abundant metal on earth, industrialization has increased the magnitude of exposure owing to the use of aluminum salts as stabilizers in processed foods and the concentration of ground water aluminum in agricultural products. Mimicking estimated average human ingestion of aluminum via administering it orally to rats increases their perception of visceral pain. These results suggest a possible role for increased exposure to aluminum in driving the post–mid-20th-century increased incidence of IBS. Unfortunately, only broad societal estimates of aluminum exposure are available, and aluminum levels are difficult to measure in individuals, making it difficult to epidemiologically investigate the role of aluminum in promoting GI disease in humans. Hence, I submit that levels of aluminum ingestion by humans should be more closely monitored and the potential of aluminum to promote GI disease carefully scrutinized.
Andrew Ted Gewirtz, PhD, distinguished university center professor, Georgia State University’s Institute for Biomedical Sciences’ Center for Inflammation, Immunity and Infection, Atlanta.
Irritable bowel syndrome is a chronic functional gastrointestinal disorder, characterized by relapsing/remitting diarrhea, constipation, and visceral pain. IBS afflicts 10%-25% of the population in developed countries.
Despite histologically normal intestinal biopsy specimens, biological signatures of IBS include alterations in intestinal gene expression, increased gut permeability, and changes in gut microbiota composition. Thus, although the cause or causes of IBS are not defined, these and other data highlight the enormous breadth of factors that might play a role in this disorder. Similar alterations also are associated with inflammatory bowel disease (IBD), although the magnitude of changes is typically greater in IBD. Nevertheless, these data suggest that IBS and IBD may share triggers and pathogenetic mechanisms. That prevalence of both IBS and IBD have shown marked increases in incidence, roughly paralleling the modernization of society that accelerated in the mid-20th century, raises the possibility that environmental factors associated with human activity may be a driver of both diseases. Recent findings suggest that aluminum may be one such trigger. While humans have always been exposed to aluminum, the most abundant metal on earth, industrialization has increased the magnitude of exposure owing to the use of aluminum salts as stabilizers in processed foods and the concentration of ground water aluminum in agricultural products. Mimicking estimated average human ingestion of aluminum via administering it orally to rats increases their perception of visceral pain. These results suggest a possible role for increased exposure to aluminum in driving the post–mid-20th-century increased incidence of IBS. Unfortunately, only broad societal estimates of aluminum exposure are available, and aluminum levels are difficult to measure in individuals, making it difficult to epidemiologically investigate the role of aluminum in promoting GI disease in humans. Hence, I submit that levels of aluminum ingestion by humans should be more closely monitored and the potential of aluminum to promote GI disease carefully scrutinized.
Andrew Ted Gewirtz, PhD, distinguished university center professor, Georgia State University’s Institute for Biomedical Sciences’ Center for Inflammation, Immunity and Infection, Atlanta.
Aluminum ingested in small amounts causes visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may trigger irritable bowel syndrome (IBS) in humans, according to a study published in Cellular and Molecular Gastroenterology and Hepatology.
Rats given oral aluminum exhibited dose-dependent visceral pain along with activation of proteinase-activated receptor-2 (PAR2) and mast cell degranulation, a combination of events that mirror clinical signs and molecular mechanisms of IBS in humans, reported lead author, Nicolas Esquerre, PhD, of Lille Inflammation Research International Center at Université Lille in France, and his colleagues. The study contributes to ongoing research surrounding causes and mechanisms of IBS, which may vary among patients because of disease subsets. These findings suggest that some patients with IBS may benefit from dietary aluminum restriction or chelation therapy.
“[T]he question of the initial trigger [of IBS] still remains unresolved,” the investigators wrote. “A more precise link between food and IBS has been demonstrated for gluten and other wheat proteins, lactose, and nickel, highlighting particular subsets of IBS patients now diagnosed as nonceliac gluten/wheat sensitivity, lactose intolerance, and nickel-allergic contact mucositis,” they added. “Here, we evaluated the effect of aluminum, a common contaminant of food and water, on abdominal pain.”
Aluminum may enter the diet as a food additive, or it may contaminate foods grown in aluminum-rich soil. Other sources of oral exposure include packaging and kitchenware. A previous study showed that most Americans ingest 0.01-1.4 mg/kg of aluminum daily, and 5% ingest 1.58 mg/kg daily (i.e., 95 mg per day for a 60-kg person).
Based on these statistics, rats in the present study received oral aluminum citrate (AlCi) corresponding with three doses of aluminum: 0.5 mg/kg, 1.5 mg/kg, or 3.0 mg/kg. Treatment continued for 30 days, with colorectal distension (CRD) measured on days 2, 4, 8, 15, and 30.
Results showed a dose-dependent relationship between aluminum ingestion and visceral hypersensitivity. Within 2 days, rats receiving 3.0 mg/kg of aluminum exhibited a significantly lower pain threshold, and within 8 days, rats receiving 0.5 mg/kg and 1.5 mg/kg also showed increased visceral hypersensitivity.
After 1 month of treatment, rats receiving 1.5 mg/kg per day demonstrated a 30% increase in pain compared with control animals. In the same group, visceral hypersensitivity began to wane 7 days after cessation of treatment; 4 more weeks were needed to return to baseline. When treatment was restarted, visceral hypersensitivity occurred within 2 days, compared with 8 days upon initial administration. These findings are particularly relevant to some people, as the 1.5-mg/kg dose corresponds with the daily amount of aluminum ingested by 5% of Americans. Similar patterns of response and sensitization were observed in rats ingesting 0.5 mg/kg and 3.0 mg/kg. Female rats were more sensitive to aluminum than were male rats, a sex pattern that mimics human IBS.
Further testing showed that rats treated with zinc citrate (ZnCi) did not exhibit changes to pain threshold, thereby excluding citrate as an aggravating factor. Rat models of noninflammatory and inflammatory colonic hypersensitivity (butyrate enema or intrathecal injection of 25%-50% ethanol in combination with 2,4,6-trinitrobenzenesulfonic acid, respectively) had visceral hypersensitivity similar to that of rats in the 1.5-mg/kg AlCi group.
Testing of colonic tissue from AlCi-treated rats did not reveal inflammatory changes according to a variety of qualifiers, including histology, myeloperoxidase activity, mRNA expression of several inflammatory cytokines, or infiltration of eosinophils or macrophages. Noninflammatory effects of aluminum, however, were found. For instance, treated rats had lower serotonin levels in enteroendocrine cells.
“Enteroendocrine cells are specialized epithelial cells that respond to luminal stimuli by releasing various biologically active compounds,” the investigators wrote. “They regulate several physiological and homeostatic functions of the gastrointestinal tract, such as postprandial secretion, motility, immune responses, and sensory functions. A reduced number of enteroendocrine cells has been observed in the duodenum, ileum, and colon of some patients with IBS.”
In addition to changes in enteroendocrine cells, AlCi-treated rats had greater colonic mast cell degranulation and histamine with upregulation of histidine decarboxylase transcripts, suggesting that aluminum activated mast cells.
To determine the role of mast cell activation in visceral hypersensitivity, rats were given AlCi with cromoglycate, an inhibitor of mast cell degranulation. This treatment reduced mast cell degranulation and visceral pain threshold, compared with AlCi-treated rats not receiving cromoglycate, suggesting that mast cell degranulation is a primary driver of visceral hypersensitivity. This observation was confirmed by a mast cell–deficient mouse strain (Kit W-sh/W-sh), that had a normal number of mast cells incapable of degranulation. Treating the mast cell–deficient mice with AlCi did not induce visceral hypersensitivity, thereby confirming the role of mast cell degranulation.
Along with mast cell degranulation, AlCi treatment led to PAR2 activation. Investigators explored the significance of this finding with PAR2 knockout mice. When treated with AlCi, PAR2 knockout mice showed no increase in visceral hypersensitivity, suggesting that hypersensitivity is dependent on PAR2 activation. Further testing revealed that mast cell–deficient mice (Kit W-sh/W-sh) did not have PAR2 upregulation either, connecting a sequence in which aluminum triggers mast cell degranulation, mast cell degranulation drives PAR2 upregulation, and PAR2 upregulation causes visceral hypersensitivity. The latter two events in this chain – mast cell degranulation and PAR2 upregulation – mirror molecular mechanisms of IBS in humans.
“We speculate that aluminum activates mast cells to release mediators that can increase excitability of nociceptive afferences contributing to the visceral pain phenotype,” the investigators wrote. “Taken together, our results linked aluminum to several mechanisms implicated in IBS pathophysiology, highlighting a possible role for aluminum as a triggering factor in IBS development.”
The investigators suggested that these findings could influence preventive or therapeutic strategies: “Aluminum might be the first identified dietary risk factor for IBS, implying that measures to limit aluminum dietary consumption or to chelate aluminum may represent novel pathways of prevention and treatment of IBS in some susceptible patients,” they wrote.
The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
SOURCE: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
Aluminum ingested in small amounts causes visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may trigger irritable bowel syndrome (IBS) in humans, according to a study published in Cellular and Molecular Gastroenterology and Hepatology.
Rats given oral aluminum exhibited dose-dependent visceral pain along with activation of proteinase-activated receptor-2 (PAR2) and mast cell degranulation, a combination of events that mirror clinical signs and molecular mechanisms of IBS in humans, reported lead author, Nicolas Esquerre, PhD, of Lille Inflammation Research International Center at Université Lille in France, and his colleagues. The study contributes to ongoing research surrounding causes and mechanisms of IBS, which may vary among patients because of disease subsets. These findings suggest that some patients with IBS may benefit from dietary aluminum restriction or chelation therapy.
“[T]he question of the initial trigger [of IBS] still remains unresolved,” the investigators wrote. “A more precise link between food and IBS has been demonstrated for gluten and other wheat proteins, lactose, and nickel, highlighting particular subsets of IBS patients now diagnosed as nonceliac gluten/wheat sensitivity, lactose intolerance, and nickel-allergic contact mucositis,” they added. “Here, we evaluated the effect of aluminum, a common contaminant of food and water, on abdominal pain.”
Aluminum may enter the diet as a food additive, or it may contaminate foods grown in aluminum-rich soil. Other sources of oral exposure include packaging and kitchenware. A previous study showed that most Americans ingest 0.01-1.4 mg/kg of aluminum daily, and 5% ingest 1.58 mg/kg daily (i.e., 95 mg per day for a 60-kg person).
Based on these statistics, rats in the present study received oral aluminum citrate (AlCi) corresponding with three doses of aluminum: 0.5 mg/kg, 1.5 mg/kg, or 3.0 mg/kg. Treatment continued for 30 days, with colorectal distension (CRD) measured on days 2, 4, 8, 15, and 30.
Results showed a dose-dependent relationship between aluminum ingestion and visceral hypersensitivity. Within 2 days, rats receiving 3.0 mg/kg of aluminum exhibited a significantly lower pain threshold, and within 8 days, rats receiving 0.5 mg/kg and 1.5 mg/kg also showed increased visceral hypersensitivity.
After 1 month of treatment, rats receiving 1.5 mg/kg per day demonstrated a 30% increase in pain compared with control animals. In the same group, visceral hypersensitivity began to wane 7 days after cessation of treatment; 4 more weeks were needed to return to baseline. When treatment was restarted, visceral hypersensitivity occurred within 2 days, compared with 8 days upon initial administration. These findings are particularly relevant to some people, as the 1.5-mg/kg dose corresponds with the daily amount of aluminum ingested by 5% of Americans. Similar patterns of response and sensitization were observed in rats ingesting 0.5 mg/kg and 3.0 mg/kg. Female rats were more sensitive to aluminum than were male rats, a sex pattern that mimics human IBS.
Further testing showed that rats treated with zinc citrate (ZnCi) did not exhibit changes to pain threshold, thereby excluding citrate as an aggravating factor. Rat models of noninflammatory and inflammatory colonic hypersensitivity (butyrate enema or intrathecal injection of 25%-50% ethanol in combination with 2,4,6-trinitrobenzenesulfonic acid, respectively) had visceral hypersensitivity similar to that of rats in the 1.5-mg/kg AlCi group.
Testing of colonic tissue from AlCi-treated rats did not reveal inflammatory changes according to a variety of qualifiers, including histology, myeloperoxidase activity, mRNA expression of several inflammatory cytokines, or infiltration of eosinophils or macrophages. Noninflammatory effects of aluminum, however, were found. For instance, treated rats had lower serotonin levels in enteroendocrine cells.
“Enteroendocrine cells are specialized epithelial cells that respond to luminal stimuli by releasing various biologically active compounds,” the investigators wrote. “They regulate several physiological and homeostatic functions of the gastrointestinal tract, such as postprandial secretion, motility, immune responses, and sensory functions. A reduced number of enteroendocrine cells has been observed in the duodenum, ileum, and colon of some patients with IBS.”
In addition to changes in enteroendocrine cells, AlCi-treated rats had greater colonic mast cell degranulation and histamine with upregulation of histidine decarboxylase transcripts, suggesting that aluminum activated mast cells.
To determine the role of mast cell activation in visceral hypersensitivity, rats were given AlCi with cromoglycate, an inhibitor of mast cell degranulation. This treatment reduced mast cell degranulation and visceral pain threshold, compared with AlCi-treated rats not receiving cromoglycate, suggesting that mast cell degranulation is a primary driver of visceral hypersensitivity. This observation was confirmed by a mast cell–deficient mouse strain (Kit W-sh/W-sh), that had a normal number of mast cells incapable of degranulation. Treating the mast cell–deficient mice with AlCi did not induce visceral hypersensitivity, thereby confirming the role of mast cell degranulation.
Along with mast cell degranulation, AlCi treatment led to PAR2 activation. Investigators explored the significance of this finding with PAR2 knockout mice. When treated with AlCi, PAR2 knockout mice showed no increase in visceral hypersensitivity, suggesting that hypersensitivity is dependent on PAR2 activation. Further testing revealed that mast cell–deficient mice (Kit W-sh/W-sh) did not have PAR2 upregulation either, connecting a sequence in which aluminum triggers mast cell degranulation, mast cell degranulation drives PAR2 upregulation, and PAR2 upregulation causes visceral hypersensitivity. The latter two events in this chain – mast cell degranulation and PAR2 upregulation – mirror molecular mechanisms of IBS in humans.
“We speculate that aluminum activates mast cells to release mediators that can increase excitability of nociceptive afferences contributing to the visceral pain phenotype,” the investigators wrote. “Taken together, our results linked aluminum to several mechanisms implicated in IBS pathophysiology, highlighting a possible role for aluminum as a triggering factor in IBS development.”
The investigators suggested that these findings could influence preventive or therapeutic strategies: “Aluminum might be the first identified dietary risk factor for IBS, implying that measures to limit aluminum dietary consumption or to chelate aluminum may represent novel pathways of prevention and treatment of IBS in some susceptible patients,” they wrote.
The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
SOURCE: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Aluminum ingestion triggers visceral hypersensitivity in rats, suggesting that dietary levels of aluminum may contribute to development of irritable bowel syndrome in humans.
Major finding: In rodents, 1 month of oral aluminum administration led to a 30% increase in pain during colorectal distension, compared with control subjects.
Study details: A rodent study including noninflammatory and inflammatory IBS rat models, mast cell–deficient mice, and PAR2 knockout mice.
Disclosures: The study was funded by the European Fund for Regional Economic Development; the Hauts de France Region, Ministère de l’Enseignement Supérieur et de la Recherche (CPER IRENI); and Digestscience (European Research Foundation on Intestinal Diseases and Nutrition).
Source: Esquerre N et al. Cell Mol Gastroenterol Hepatol. 2019 Sep 20. doi: 10.1016/j.jcmgh.2018.09.012.
HPV-16/-18 dramatically increases risk of high-grade CIN in young women
Young women with HPV-16/-18 are significantly more likely to develop high-grade cervical intraepithelial neoplasia (CIN), compared with young women who do not have HPV-16/-18, and therefore require close monitoring, according to a 9-year study of more than 500 women.
Specific strain of HPV had less effect on risk in women aged 30 years or older, compared with younger women, reported lead author Maria Fröberg, MD, PhD, of Karolinska University Hospital and Institute in Stockholm and her colleagues.
“With today’s introduction of HPV primary screening into several organized screening programs and with many triage algorithms available, further research is needed to ensure safe follow-up management and prevent the unnecessary treatment of transient positive HPV findings associated with regressive high-grade CIN,” the investigators wrote in Cancer.
To better understand risk associated with HPV, the investigators drew from a database of 9,464 Swedish women who were cytologically negative for cervical intraepithelial lesions or malignancy (NILM) at baseline during 2005-2007. These baseline-negative women were followed for 9 years; during this time, 96 women developed histologically confirmed, high-grade CIN (CIN2, CIN3, cervical cancer, or adenocarcinoma in situ [AIS]). For each case, five age-matched women were selected who did not develop high-grade CIN to make a control cohort of 480 women.
Approximately half of the cases had CIN2 (45.8%), and half had CIN3 or worse histopathology (CIN3+, 54.2%). HPV-16/-18 was more often associated with CIN3+, compared with CIN2 (Pearson x2, 6.12; P less than .02 [2-sided]). Women with high-grade CIN were significantly more likely to have HPV of any strain, compared with controls (odds ratio, 6.78). Women aged younger than 30 years who had HPV-16/-18 at baseline were far more likely to develop high-grade CIN (OR, 9.44) but showed less impact from other strains of HPV (OR, 2.24). In contrast, women aged 30 years or older showed similar increases in high-grade CIN risk when comparing HPV-16/-18 with other strains (OR, 8.16 vs. 9.04).
“These latter findings suggest that genotyping for HPV-16/-18 might be useful for risk stratification among younger women,” the investigators suggested, noting that “further prospective study on this topic is warranted.”
The study was funded by the Swedish Cancer Foundation, the Stockholm County Council, the Swedish Research Council, and the King Gustaf V Jubilee Fund, and the Karolinska Institute. During the study, one investigator received grants from VALGENT and the 7th Framework Programme of DG Research and Innovation (European Commission).
SOURCE: Fröberg M et al. Cancer. 2018 Dec 10. doi: 10.1002/cncr.31788.
Young women with HPV-16/-18 are significantly more likely to develop high-grade cervical intraepithelial neoplasia (CIN), compared with young women who do not have HPV-16/-18, and therefore require close monitoring, according to a 9-year study of more than 500 women.
Specific strain of HPV had less effect on risk in women aged 30 years or older, compared with younger women, reported lead author Maria Fröberg, MD, PhD, of Karolinska University Hospital and Institute in Stockholm and her colleagues.
“With today’s introduction of HPV primary screening into several organized screening programs and with many triage algorithms available, further research is needed to ensure safe follow-up management and prevent the unnecessary treatment of transient positive HPV findings associated with regressive high-grade CIN,” the investigators wrote in Cancer.
To better understand risk associated with HPV, the investigators drew from a database of 9,464 Swedish women who were cytologically negative for cervical intraepithelial lesions or malignancy (NILM) at baseline during 2005-2007. These baseline-negative women were followed for 9 years; during this time, 96 women developed histologically confirmed, high-grade CIN (CIN2, CIN3, cervical cancer, or adenocarcinoma in situ [AIS]). For each case, five age-matched women were selected who did not develop high-grade CIN to make a control cohort of 480 women.
Approximately half of the cases had CIN2 (45.8%), and half had CIN3 or worse histopathology (CIN3+, 54.2%). HPV-16/-18 was more often associated with CIN3+, compared with CIN2 (Pearson x2, 6.12; P less than .02 [2-sided]). Women with high-grade CIN were significantly more likely to have HPV of any strain, compared with controls (odds ratio, 6.78). Women aged younger than 30 years who had HPV-16/-18 at baseline were far more likely to develop high-grade CIN (OR, 9.44) but showed less impact from other strains of HPV (OR, 2.24). In contrast, women aged 30 years or older showed similar increases in high-grade CIN risk when comparing HPV-16/-18 with other strains (OR, 8.16 vs. 9.04).
“These latter findings suggest that genotyping for HPV-16/-18 might be useful for risk stratification among younger women,” the investigators suggested, noting that “further prospective study on this topic is warranted.”
The study was funded by the Swedish Cancer Foundation, the Stockholm County Council, the Swedish Research Council, and the King Gustaf V Jubilee Fund, and the Karolinska Institute. During the study, one investigator received grants from VALGENT and the 7th Framework Programme of DG Research and Innovation (European Commission).
SOURCE: Fröberg M et al. Cancer. 2018 Dec 10. doi: 10.1002/cncr.31788.
Young women with HPV-16/-18 are significantly more likely to develop high-grade cervical intraepithelial neoplasia (CIN), compared with young women who do not have HPV-16/-18, and therefore require close monitoring, according to a 9-year study of more than 500 women.
Specific strain of HPV had less effect on risk in women aged 30 years or older, compared with younger women, reported lead author Maria Fröberg, MD, PhD, of Karolinska University Hospital and Institute in Stockholm and her colleagues.
“With today’s introduction of HPV primary screening into several organized screening programs and with many triage algorithms available, further research is needed to ensure safe follow-up management and prevent the unnecessary treatment of transient positive HPV findings associated with regressive high-grade CIN,” the investigators wrote in Cancer.
To better understand risk associated with HPV, the investigators drew from a database of 9,464 Swedish women who were cytologically negative for cervical intraepithelial lesions or malignancy (NILM) at baseline during 2005-2007. These baseline-negative women were followed for 9 years; during this time, 96 women developed histologically confirmed, high-grade CIN (CIN2, CIN3, cervical cancer, or adenocarcinoma in situ [AIS]). For each case, five age-matched women were selected who did not develop high-grade CIN to make a control cohort of 480 women.
Approximately half of the cases had CIN2 (45.8%), and half had CIN3 or worse histopathology (CIN3+, 54.2%). HPV-16/-18 was more often associated with CIN3+, compared with CIN2 (Pearson x2, 6.12; P less than .02 [2-sided]). Women with high-grade CIN were significantly more likely to have HPV of any strain, compared with controls (odds ratio, 6.78). Women aged younger than 30 years who had HPV-16/-18 at baseline were far more likely to develop high-grade CIN (OR, 9.44) but showed less impact from other strains of HPV (OR, 2.24). In contrast, women aged 30 years or older showed similar increases in high-grade CIN risk when comparing HPV-16/-18 with other strains (OR, 8.16 vs. 9.04).
“These latter findings suggest that genotyping for HPV-16/-18 might be useful for risk stratification among younger women,” the investigators suggested, noting that “further prospective study on this topic is warranted.”
The study was funded by the Swedish Cancer Foundation, the Stockholm County Council, the Swedish Research Council, and the King Gustaf V Jubilee Fund, and the Karolinska Institute. During the study, one investigator received grants from VALGENT and the 7th Framework Programme of DG Research and Innovation (European Commission).
SOURCE: Fröberg M et al. Cancer. 2018 Dec 10. doi: 10.1002/cncr.31788.
FROM CANCER
Key clinical point: Women with HPV-16/-18 are at significantly higher risk of high-grade cervical intraepithelial neoplasia (CIN), compared with women without HPV-16/-18, and therefore require close monitoring.
Major finding: Women younger than 30 years who test positive for HPV-16/-18 are almost 10 times as likely to develop high-grade CIN, compared with young women negative for HPV-16/-18 (odds ratio, 9.44).
Study details: A nested case-control study involving 96 women who developed high-grade CIN over the 9-year study period, compared with 480 age-matched controls who did not develop cervical lesions.
Disclosures: The study was funded by the Swedish Cancer Foundation, the Stockholm County Council, the Swedish Research Council, and the King Gustaf V Jubilee Fund, and the Karolinska Institute. During the study, one investigator received grants from VALGENT and the 7th Framework Programme of DG Research and Innovation (European Commission).
Source: Fröberg M et al. Cancer. 2018 Dec 10. doi: 10.1002/cncr.31788.
Biomarker algorithm may offer noninvasive look at liver fibrosis
Serum biomarkers may enable a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD), according to results from a recent study.
An algorithm created by the investigators distinguished NAFLD patients with advanced liver fibrosis from those with mild to moderate fibrosis, reported lead author Rohit Loomba, MD, of the University of California at San Diego and his colleagues.
“Liver biopsy is currently the gold standard for diagnosing NASH [nonalcoholic steatohepatitis] and staging liver fibrosis,” the investigators wrote in Clinical Gastroenterology and Hepatology. “However, it is a costly and invasive procedure with an all-cause mortality risk of approximately 0.2%. Liver biopsy typically samples only 1/50,000th of the organ, and it is liable to sampling error with an error rate of 25% for diagnosis of hepatic fibrosis.”
Existing serum-based tests are reliable for diagnosing nonfibrotic NAFLD, but they may misdiagnosis patients with advanced fibrosis. Although imaging-based techniques may provide better diagnostic accuracy, some are available only for subgroups of patients, while others come with a high financial burden. Diagnostic shortcomings may have a major effect on patient outcomes, particularly when risk groups are considered.
“Fibrosis stages F3 and F4 (advanced fibrosis) are primary predictors of liver-related morbidity and mortality, with 11%-22% of NASH patients reported to have advanced fibrosis,” the investigators noted.
The investigators therefore aimed to distinguish such high-risk NAFLD patients from those with mild or moderate liver fibrosis. Three biomarkers were included: hyaluronic acid (HA), TIMP metallopeptidase inhibitor 1 (TIMP-1), and alpha2-macroglobulin (A2M). Each biomarker has documented associations with liver fibrosis. For instance, higher A2M concentrations inhibit fibrinolysis, HA is associated with excessive extracellular matrix and fibrotic tissue, and TIMP-1 is a known liver fibrosis marker and inhibitor of extracellular matrix degradation. The relative strengths of each in detecting advanced liver fibrosis was determined through an algorithm.
The investigators relied on archived serum samples from Duke University, Durham, N.C., (n = 792) and University of California at San Diego (n = 244) that were collected within 11 days of liver biopsy. Biopsies were performed with 15- to 16-gauge needles using at least eight portal tracts, and these samples were used to diagnose NAFLD. Patients with alcoholic liver disease or hepatitis C virus were excluded.
Algorithm training was based on serum measurements from 396 patients treated at Duke University. Samples were divided into mild to moderate (F0-F2) or advanced (F3-F4) fibrosis and split into 10 subsets. The logical regression model was trained on nine subsets and tested on the 10th, with iterations 10 times through this sequence until all 10 samples were tested. This process was repeated 10,000 times. Using the median coefficients from 100,000 logistical regression models, the samples were scored using the algorithm from 0 to 100, with higher numbers representing more advanced fibrosis, and the relative weights of each biomarker measurement were determined.
A noninferiority protocol was used to validate the algorithm, through which the area under the receiver operating characteristic (AUROC) curve was calculated. The AUROC curve of the validation samples was 0.856, with 0.5 being the score for a random algorithm. The algorithm correctly classified 90.0% of F0 cases, 75.0% of F1 cases, 53.8% of F2 cases, 77.4% of F3 cases, and 94.4% of F4 cases. The sensitivity was 79.7% and the specificity was 75.7%.
The algorithm was superior to Fibrosis-4 (FIB-4) and NAFLD Fibrosis Score (NFS) in two validation cohorts. In a combination of validation cohorts, the algorithm correctly identified 79.5% of F3-F4 patients, compared with rates of 25.8% and 28.0% from FIB-4 and NFS, respectively. The investigators noted that the algorithm was unaffected by sex or age. In contrast, FIB-4 is biased toward females, and both FIB-4 and NFS are less accurate with patients aged 35 years or younger.
“Performance of the training and validation sets was robust and well matched, enabling the reliable differentiation of NAFLD patients with and without advanced fibrosis,” the investigators concluded.
The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
SOURCE: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
Serum biomarkers may enable a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD), according to results from a recent study.
An algorithm created by the investigators distinguished NAFLD patients with advanced liver fibrosis from those with mild to moderate fibrosis, reported lead author Rohit Loomba, MD, of the University of California at San Diego and his colleagues.
“Liver biopsy is currently the gold standard for diagnosing NASH [nonalcoholic steatohepatitis] and staging liver fibrosis,” the investigators wrote in Clinical Gastroenterology and Hepatology. “However, it is a costly and invasive procedure with an all-cause mortality risk of approximately 0.2%. Liver biopsy typically samples only 1/50,000th of the organ, and it is liable to sampling error with an error rate of 25% for diagnosis of hepatic fibrosis.”
Existing serum-based tests are reliable for diagnosing nonfibrotic NAFLD, but they may misdiagnosis patients with advanced fibrosis. Although imaging-based techniques may provide better diagnostic accuracy, some are available only for subgroups of patients, while others come with a high financial burden. Diagnostic shortcomings may have a major effect on patient outcomes, particularly when risk groups are considered.
“Fibrosis stages F3 and F4 (advanced fibrosis) are primary predictors of liver-related morbidity and mortality, with 11%-22% of NASH patients reported to have advanced fibrosis,” the investigators noted.
The investigators therefore aimed to distinguish such high-risk NAFLD patients from those with mild or moderate liver fibrosis. Three biomarkers were included: hyaluronic acid (HA), TIMP metallopeptidase inhibitor 1 (TIMP-1), and alpha2-macroglobulin (A2M). Each biomarker has documented associations with liver fibrosis. For instance, higher A2M concentrations inhibit fibrinolysis, HA is associated with excessive extracellular matrix and fibrotic tissue, and TIMP-1 is a known liver fibrosis marker and inhibitor of extracellular matrix degradation. The relative strengths of each in detecting advanced liver fibrosis was determined through an algorithm.
The investigators relied on archived serum samples from Duke University, Durham, N.C., (n = 792) and University of California at San Diego (n = 244) that were collected within 11 days of liver biopsy. Biopsies were performed with 15- to 16-gauge needles using at least eight portal tracts, and these samples were used to diagnose NAFLD. Patients with alcoholic liver disease or hepatitis C virus were excluded.
Algorithm training was based on serum measurements from 396 patients treated at Duke University. Samples were divided into mild to moderate (F0-F2) or advanced (F3-F4) fibrosis and split into 10 subsets. The logical regression model was trained on nine subsets and tested on the 10th, with iterations 10 times through this sequence until all 10 samples were tested. This process was repeated 10,000 times. Using the median coefficients from 100,000 logistical regression models, the samples were scored using the algorithm from 0 to 100, with higher numbers representing more advanced fibrosis, and the relative weights of each biomarker measurement were determined.
A noninferiority protocol was used to validate the algorithm, through which the area under the receiver operating characteristic (AUROC) curve was calculated. The AUROC curve of the validation samples was 0.856, with 0.5 being the score for a random algorithm. The algorithm correctly classified 90.0% of F0 cases, 75.0% of F1 cases, 53.8% of F2 cases, 77.4% of F3 cases, and 94.4% of F4 cases. The sensitivity was 79.7% and the specificity was 75.7%.
The algorithm was superior to Fibrosis-4 (FIB-4) and NAFLD Fibrosis Score (NFS) in two validation cohorts. In a combination of validation cohorts, the algorithm correctly identified 79.5% of F3-F4 patients, compared with rates of 25.8% and 28.0% from FIB-4 and NFS, respectively. The investigators noted that the algorithm was unaffected by sex or age. In contrast, FIB-4 is biased toward females, and both FIB-4 and NFS are less accurate with patients aged 35 years or younger.
“Performance of the training and validation sets was robust and well matched, enabling the reliable differentiation of NAFLD patients with and without advanced fibrosis,” the investigators concluded.
The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
SOURCE: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
Serum biomarkers may enable a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD), according to results from a recent study.
An algorithm created by the investigators distinguished NAFLD patients with advanced liver fibrosis from those with mild to moderate fibrosis, reported lead author Rohit Loomba, MD, of the University of California at San Diego and his colleagues.
“Liver biopsy is currently the gold standard for diagnosing NASH [nonalcoholic steatohepatitis] and staging liver fibrosis,” the investigators wrote in Clinical Gastroenterology and Hepatology. “However, it is a costly and invasive procedure with an all-cause mortality risk of approximately 0.2%. Liver biopsy typically samples only 1/50,000th of the organ, and it is liable to sampling error with an error rate of 25% for diagnosis of hepatic fibrosis.”
Existing serum-based tests are reliable for diagnosing nonfibrotic NAFLD, but they may misdiagnosis patients with advanced fibrosis. Although imaging-based techniques may provide better diagnostic accuracy, some are available only for subgroups of patients, while others come with a high financial burden. Diagnostic shortcomings may have a major effect on patient outcomes, particularly when risk groups are considered.
“Fibrosis stages F3 and F4 (advanced fibrosis) are primary predictors of liver-related morbidity and mortality, with 11%-22% of NASH patients reported to have advanced fibrosis,” the investigators noted.
The investigators therefore aimed to distinguish such high-risk NAFLD patients from those with mild or moderate liver fibrosis. Three biomarkers were included: hyaluronic acid (HA), TIMP metallopeptidase inhibitor 1 (TIMP-1), and alpha2-macroglobulin (A2M). Each biomarker has documented associations with liver fibrosis. For instance, higher A2M concentrations inhibit fibrinolysis, HA is associated with excessive extracellular matrix and fibrotic tissue, and TIMP-1 is a known liver fibrosis marker and inhibitor of extracellular matrix degradation. The relative strengths of each in detecting advanced liver fibrosis was determined through an algorithm.
The investigators relied on archived serum samples from Duke University, Durham, N.C., (n = 792) and University of California at San Diego (n = 244) that were collected within 11 days of liver biopsy. Biopsies were performed with 15- to 16-gauge needles using at least eight portal tracts, and these samples were used to diagnose NAFLD. Patients with alcoholic liver disease or hepatitis C virus were excluded.
Algorithm training was based on serum measurements from 396 patients treated at Duke University. Samples were divided into mild to moderate (F0-F2) or advanced (F3-F4) fibrosis and split into 10 subsets. The logical regression model was trained on nine subsets and tested on the 10th, with iterations 10 times through this sequence until all 10 samples were tested. This process was repeated 10,000 times. Using the median coefficients from 100,000 logistical regression models, the samples were scored using the algorithm from 0 to 100, with higher numbers representing more advanced fibrosis, and the relative weights of each biomarker measurement were determined.
A noninferiority protocol was used to validate the algorithm, through which the area under the receiver operating characteristic (AUROC) curve was calculated. The AUROC curve of the validation samples was 0.856, with 0.5 being the score for a random algorithm. The algorithm correctly classified 90.0% of F0 cases, 75.0% of F1 cases, 53.8% of F2 cases, 77.4% of F3 cases, and 94.4% of F4 cases. The sensitivity was 79.7% and the specificity was 75.7%.
The algorithm was superior to Fibrosis-4 (FIB-4) and NAFLD Fibrosis Score (NFS) in two validation cohorts. In a combination of validation cohorts, the algorithm correctly identified 79.5% of F3-F4 patients, compared with rates of 25.8% and 28.0% from FIB-4 and NFS, respectively. The investigators noted that the algorithm was unaffected by sex or age. In contrast, FIB-4 is biased toward females, and both FIB-4 and NFS are less accurate with patients aged 35 years or younger.
“Performance of the training and validation sets was robust and well matched, enabling the reliable differentiation of NAFLD patients with and without advanced fibrosis,” the investigators concluded.
The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
SOURCE: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A serum biomarker–based algorithm may provide a noninvasive method of detecting advanced hepatic fibrosis in patients with nonalcoholic fatty liver disease (NAFLD).
Major finding: The area under the receiver operator characteristic (AUROC) curve for a combination of validation samples was 0.856.
Study details: A retrospective study of liver fibrosis serum markers and clinical data from 396 patients with NAFLD and various stages of fibrosis.
Disclosures: The study was supported by Prometheus Laboratories. Authors not employed by Prometheus Laboratories were employed by Duke University or the University of California, San Diego; each institution received funding from Prometheus Laboratories.
Source: Loomba R et al. Clin Gastroenterol Hepatol. 2018 Nov 15. doi: 10.1016/j.cgh.2018.11.004.