User login
Assessment of Medical School Musculoskeletal Education
A basic understanding of the clinical components of musculoskeletal medicine is necessary in many medical fields. Musculoskeletal injuries represent the second most common presentation in US emergency departments, account for 49 million visits to orthopedic surgeon offices, and cost the United States an estimated $950 billion annually.1-3 Despite the staggering need for competency in musculoskeletal medicine, Freedman and Bernstein4 in 1998 demonstrated that musculoskeletal knowledge is inadequate among medical school graduates.
In 2005, the United States Bone and Joint Decade (now the United States Bone and Joint Initiative) announced Project 100, which recommended that 100% of US medical schools begin requiring a musculoskeletal course by the end of the decade.5 This project was intended to increase musculoskeletal understanding among medical students. Optimal curriculum reform, however, remains controversial. Many studies have found that medical schools continue to provide inadequate musculoskeletal education.4,6-9 For example, an integrated musculoskeletal curriculum with increased lecture time was found to improve clinical confidence but not musculoskeletal knowledge.6 In contrast, a 2-week intensive musculoskeletal module and a 6-week course involving orthopedic resident and faculty education has been shown to improve understanding.10,11
We conducted a study to determine the adequacy of musculoskeletal knowledge in medical school students, to determine musculoskeletal competency after curriculum reform through increased lecture and laboratory time, and to draw conclusions about factors leading to increased musculoskeletal competency to guide future curriculum reforms. We hypothesized that musculoskeletal knowledge would increase as a result of increased lecture and laboratory time.
Materials and Methods
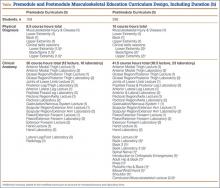
The Tufts University School of Medicine Institutional Review Board approved this study. The medical school curriculum at our institution was redesigned to include a dedicated musculoskeletal module to improve medical student education (Table). The study compared medical students given the old musculoskeletal module (premodule group) and those given the new musculoskeletal module (postmodule group). The premodule group received 8.5 hours of physical diagnosis skills training and 30 hours of clinical anatomy training (12 lecture hours, 18 laboratory hours), and the postmodule group received 10 hours of physical diagnosis training and 41.5 hours of clinical anatomy training (18.5 lecture hours, 23 laboratory hours).
The lecture material for the postmodule group covered all topics/questions addressed on the validated musculoskeletal adequacy assessment. The new module specifically added 6 hours of dedicated clinically based musculoskeletal lecture time during the anatomy course and concurrent with the physical diagnosis course. The topics covered with case-based scenarios were orthopedic emergencies, adult hip and back, knee, pediatric hip and back, elbow/wrist/hand, and shoulder. A validated musculoskeletal competency examination was given to the premodule group at the end of the musculoskeletal anatomy and physical diagnosis lectures. The postmodule group took the competency examination at the end of the “new” 6 hours of musculoskeletal education.
We used the Freedman and Bernstein4 basic competency examination for musculoskeletal education assessment to assess knowledge. This examination is the only validated tool for assessing basic clinical musculoskeletal knowledge. All students were also asked whether they had experience rotating in orthopedic surgery or in a related musculoskeletal field (rheumatology, physiatry, neurology) during the medical school “selective” period that allowed 1 afternoon per week of elective time. Duration of exposure was assessed. The examination was given to 109 students in the premodule group 1 year before the curriculum changes. The examination was then given to the students for the first 2 years after the curriculum changes were implemented, with 296 students in the postmodule group. All questions on the examination were addressed within the 6 lecture hours in the new module. A single reviewer anonymously scored the examinations according to the validated scoring system over a 2-week period.4 Independent t tests were used to compare examination scores between the premodule and postmodule groups. Statistical significance was set at P < .05. Equal variance between groups was not assumed.
Results
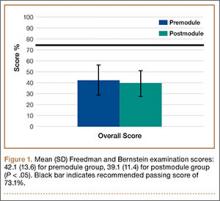
The examination was given to 405 medical students (109 premodule, 296 postmodule) Mean examination score was 40%, significantly below the recommended mean passing score of 73.1%.4 Only 1 student achieved a passing score. Independent t tests were used to compare examination scores of the premodule and postmodule groups. Mean (SD) scores were higher (P < .05) for the premodule group, 42.1 (13.6), than the postmodule group, 39.1 (11.4) (Figure 1).
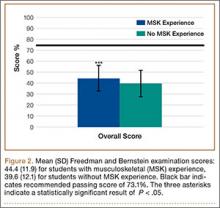
Independent t tests were used to compare examination scores of students with either orthopedics or rheumatology experience and students without this experience. Mean (SD) scores were higher (P < .05) for students with experience, 44.4 (11.9), than students without experience, 39.6 (12.1) (Figure 2). Students with neurology or physiatry experience did not score significantly higher than students without this experience. Statistical significance was set as P < .05. SAS 9.0 software (SAS Institute, Cary, North Carolina) was used for statistical analysis.
Discussion
Our students’ mean examination score was significantly lower than the passing (competency) score of 73.1%. Although Project 100 acknowledged many medical schools for implementing a required musculoskeletal course, our study results showed that adequate competency as indicated by a passing score on the Freedman and Bernstein examination was not achieved in medical school despite devoted musculoskeletal lecture time. Our postmodule group had lower scores than our premodule group despite being exposed to more lecture and laboratory material that systematically addressed every examination question. Similarly, Day and colleagues6 found that medical students scored a mean of 45% on the Freedman and Bernstein examination despite increased lecture and laboratory time.6 Lecture and laboratory exposure does not result in long-term information retention. Medical school competency is not significantly higher than what Freedman and Bernstein4 found for musculoskeletal education almost a decade earlier.
Musculoskeletal medicine typically is not revisited during medical school unless a student opts for an elective with a musculoskeletal basis. This specialty differs from others, such as neurology, which requires a 1-month clinical rotation before graduation. As increasing lecture and laboratory time did little to increase competency, adding a required clinical rotation in a musculoskeletal field or integrated musculoskeletal modules for anatomy and clinical training may be the best option for educational reform.
Our study found significantly higher Freedman and Bernstein examination scores for students with orthopedic surgery or rheumatology experience than for students without this experience. First- and second-year medical students are allowed to do a “selective” rotation—1 afternoon a week in an elective rotation of their choice. Students with orthopedics or rheumatology experience in this setting tended to score higher on the examination, possibly a result of both exposure to and interest in musculoskeletal issues. Many other studies have found that clinical exposure within a musculoskeletal field resulted in significantly higher musculoskeletal knowledge.8,12-16 Skelley and colleagues12 found that musculoskeletal clinical exposure of as short as 15 days significantly increased understanding among medical students. Grunfeld and colleagues15 found that students interested in orthopedics also had significantly more musculoskeletal knowledge. Musculoskeletal clinical exposure should be considered in medical school reform. As coordinating a curriculum with orthopedic resident and faculty involvement can set up educational barriers at some medical schools, dedicated musculoskeletal modules with a mock clinical skills component may be a useful consideration, and these have been shown to improve musculoskeletal knowledge.10,11
There are limitations to our study. The musculoskeletal examination was not given to an equal number of medical students in each group. The study also did not control for attendance, and therefore some students who took the musculoskeletal examination may not have attended all musculoskeletal module lectures. The validated examination used for basic competency is another possible limitation. The Freedman and Bernstein examination is the only validated examination used for basic competency, but it may not accurately assess meaningful development of clinical skills applicable to a patient musculoskeletal setting. No studies have assessed the correlation between musculoskeletal competency based on the Freedman and Bernstein examination and patient outcomes.
We conclude that increasing dedicated musculoskeletal lecture hours does not improve musculoskeletal knowledge. Future considerations should include incorporating further hands-on training through clinical skills workshops or rotations in orthopedic surgery or rheumatology.
1. Centers for Disease Control and Prevention, National Center for Health Statistics, Ambulatory and Hospital Care Statistics Branch. National Hospital Ambulatory Medical Care Survey: 2009 outpatient department summary tables. http://www.cdc.gov/nchs/data/ahcd/nhamcs_outpatient/2009_opd_web_tables.pdf. Accessed January 8, 2015.
2. Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008 Aug 6;(7):1-38.
3. United States Bone and Joint Initiative. The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal and Economic Costs. Rosemont, IL: United States Bone and Joint Initiative; 2008. http://www.boneandjointburden.org. Accessed January 9, 2015.
4. Freedman KB, Bernstein J. The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am. 1998;80(10):1421-1427.
5. United States Bone and Joint Initiative. Project 100—Undergraduate Musculoskeletal Education. Rosemont, IL: United States Bone and Joint Initiative; 2005. www.usbjd.org/projects/project_op.cfm?dirID=127. Accessed January 9, 2015.
6. Day CS, Ahn CS, Yeh AC, Tabrizi S. Early assessment of a new integrated preclinical musculoskeletal curriculum at a medical school. Am J Orthop. 2011;40(1):14-18.
7. Day CS, Yeh AC, Franko O, Ramirez M, Krupat E. Musculoskeletal medicine: an assessment of the attitudes and knowledge of medical students at Harvard Medical School. Acad Med. 2007;82(5):452-457.
8. Matzkin E, Smith EL, Freccero D, Richardson AB. Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am. 2005;87(2):310-314.
9. Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84(4):604-608.
10. Bilderback K, Eggerstedt J, Sadasivan KK, et al. Design and implementation of a system-based course in musculoskeletal medicine for medical students. J Bone Joint Surg Am. 2008;90(10):2292-2300.
11. Queally JM, Cummins F, Brennan SA, Shelly MJ, O’Byrne JM. Assessment of a new undergraduate module in musculoskeletal medicine. J Bone Joint Surg Am. 2011;93(3):e9.
12. Skelley NW, Tanaka MJ, Skelley LM, LaPorte DM. Medical student musculoskeletal education: an institutional survey. J Bone Joint Surg Am. 2012;94(19):e146(1-7).
13. DiGiovanni BF, Chu JY, Mooney CJ, Lambert DR. Maturation of medical student musculoskeletal medicine knowledge and clinical confidence. Med Educ Online. 2012;17. doi:10.3402/meo.v17i0.17092. Epub 2012 Jul 23.
14. Schmale GA. More evidence of educational inadequacies in musculoskeletal medicine. Clin Orthop. 2005;(437):251-259.
15. Grunfeld R, Banks S, Fox E, Levy BA, Craig C, Black K. An assessment of musculoskeletal knowledge in graduating medical and physician assistant students and implications for musculoskeletal care providers. J Bone Joint Surg Am. 2012;94(4):343-348.
16. Yeh AC, Franko O, Day CS. Impact of clinical electives and residency interest on medical students’ education in musculoskeletal medicine. J Bone Joint Surg Am. 2008;90(2):307-315.
A basic understanding of the clinical components of musculoskeletal medicine is necessary in many medical fields. Musculoskeletal injuries represent the second most common presentation in US emergency departments, account for 49 million visits to orthopedic surgeon offices, and cost the United States an estimated $950 billion annually.1-3 Despite the staggering need for competency in musculoskeletal medicine, Freedman and Bernstein4 in 1998 demonstrated that musculoskeletal knowledge is inadequate among medical school graduates.
In 2005, the United States Bone and Joint Decade (now the United States Bone and Joint Initiative) announced Project 100, which recommended that 100% of US medical schools begin requiring a musculoskeletal course by the end of the decade.5 This project was intended to increase musculoskeletal understanding among medical students. Optimal curriculum reform, however, remains controversial. Many studies have found that medical schools continue to provide inadequate musculoskeletal education.4,6-9 For example, an integrated musculoskeletal curriculum with increased lecture time was found to improve clinical confidence but not musculoskeletal knowledge.6 In contrast, a 2-week intensive musculoskeletal module and a 6-week course involving orthopedic resident and faculty education has been shown to improve understanding.10,11
We conducted a study to determine the adequacy of musculoskeletal knowledge in medical school students, to determine musculoskeletal competency after curriculum reform through increased lecture and laboratory time, and to draw conclusions about factors leading to increased musculoskeletal competency to guide future curriculum reforms. We hypothesized that musculoskeletal knowledge would increase as a result of increased lecture and laboratory time.
Materials and Methods
The Tufts University School of Medicine Institutional Review Board approved this study. The medical school curriculum at our institution was redesigned to include a dedicated musculoskeletal module to improve medical student education (Table). The study compared medical students given the old musculoskeletal module (premodule group) and those given the new musculoskeletal module (postmodule group). The premodule group received 8.5 hours of physical diagnosis skills training and 30 hours of clinical anatomy training (12 lecture hours, 18 laboratory hours), and the postmodule group received 10 hours of physical diagnosis training and 41.5 hours of clinical anatomy training (18.5 lecture hours, 23 laboratory hours).
The lecture material for the postmodule group covered all topics/questions addressed on the validated musculoskeletal adequacy assessment. The new module specifically added 6 hours of dedicated clinically based musculoskeletal lecture time during the anatomy course and concurrent with the physical diagnosis course. The topics covered with case-based scenarios were orthopedic emergencies, adult hip and back, knee, pediatric hip and back, elbow/wrist/hand, and shoulder. A validated musculoskeletal competency examination was given to the premodule group at the end of the musculoskeletal anatomy and physical diagnosis lectures. The postmodule group took the competency examination at the end of the “new” 6 hours of musculoskeletal education.
We used the Freedman and Bernstein4 basic competency examination for musculoskeletal education assessment to assess knowledge. This examination is the only validated tool for assessing basic clinical musculoskeletal knowledge. All students were also asked whether they had experience rotating in orthopedic surgery or in a related musculoskeletal field (rheumatology, physiatry, neurology) during the medical school “selective” period that allowed 1 afternoon per week of elective time. Duration of exposure was assessed. The examination was given to 109 students in the premodule group 1 year before the curriculum changes. The examination was then given to the students for the first 2 years after the curriculum changes were implemented, with 296 students in the postmodule group. All questions on the examination were addressed within the 6 lecture hours in the new module. A single reviewer anonymously scored the examinations according to the validated scoring system over a 2-week period.4 Independent t tests were used to compare examination scores between the premodule and postmodule groups. Statistical significance was set at P < .05. Equal variance between groups was not assumed.
Results
The examination was given to 405 medical students (109 premodule, 296 postmodule) Mean examination score was 40%, significantly below the recommended mean passing score of 73.1%.4 Only 1 student achieved a passing score. Independent t tests were used to compare examination scores of the premodule and postmodule groups. Mean (SD) scores were higher (P < .05) for the premodule group, 42.1 (13.6), than the postmodule group, 39.1 (11.4) (Figure 1).
Independent t tests were used to compare examination scores of students with either orthopedics or rheumatology experience and students without this experience. Mean (SD) scores were higher (P < .05) for students with experience, 44.4 (11.9), than students without experience, 39.6 (12.1) (Figure 2). Students with neurology or physiatry experience did not score significantly higher than students without this experience. Statistical significance was set as P < .05. SAS 9.0 software (SAS Institute, Cary, North Carolina) was used for statistical analysis.
Discussion
Our students’ mean examination score was significantly lower than the passing (competency) score of 73.1%. Although Project 100 acknowledged many medical schools for implementing a required musculoskeletal course, our study results showed that adequate competency as indicated by a passing score on the Freedman and Bernstein examination was not achieved in medical school despite devoted musculoskeletal lecture time. Our postmodule group had lower scores than our premodule group despite being exposed to more lecture and laboratory material that systematically addressed every examination question. Similarly, Day and colleagues6 found that medical students scored a mean of 45% on the Freedman and Bernstein examination despite increased lecture and laboratory time.6 Lecture and laboratory exposure does not result in long-term information retention. Medical school competency is not significantly higher than what Freedman and Bernstein4 found for musculoskeletal education almost a decade earlier.
Musculoskeletal medicine typically is not revisited during medical school unless a student opts for an elective with a musculoskeletal basis. This specialty differs from others, such as neurology, which requires a 1-month clinical rotation before graduation. As increasing lecture and laboratory time did little to increase competency, adding a required clinical rotation in a musculoskeletal field or integrated musculoskeletal modules for anatomy and clinical training may be the best option for educational reform.
Our study found significantly higher Freedman and Bernstein examination scores for students with orthopedic surgery or rheumatology experience than for students without this experience. First- and second-year medical students are allowed to do a “selective” rotation—1 afternoon a week in an elective rotation of their choice. Students with orthopedics or rheumatology experience in this setting tended to score higher on the examination, possibly a result of both exposure to and interest in musculoskeletal issues. Many other studies have found that clinical exposure within a musculoskeletal field resulted in significantly higher musculoskeletal knowledge.8,12-16 Skelley and colleagues12 found that musculoskeletal clinical exposure of as short as 15 days significantly increased understanding among medical students. Grunfeld and colleagues15 found that students interested in orthopedics also had significantly more musculoskeletal knowledge. Musculoskeletal clinical exposure should be considered in medical school reform. As coordinating a curriculum with orthopedic resident and faculty involvement can set up educational barriers at some medical schools, dedicated musculoskeletal modules with a mock clinical skills component may be a useful consideration, and these have been shown to improve musculoskeletal knowledge.10,11
There are limitations to our study. The musculoskeletal examination was not given to an equal number of medical students in each group. The study also did not control for attendance, and therefore some students who took the musculoskeletal examination may not have attended all musculoskeletal module lectures. The validated examination used for basic competency is another possible limitation. The Freedman and Bernstein examination is the only validated examination used for basic competency, but it may not accurately assess meaningful development of clinical skills applicable to a patient musculoskeletal setting. No studies have assessed the correlation between musculoskeletal competency based on the Freedman and Bernstein examination and patient outcomes.
We conclude that increasing dedicated musculoskeletal lecture hours does not improve musculoskeletal knowledge. Future considerations should include incorporating further hands-on training through clinical skills workshops or rotations in orthopedic surgery or rheumatology.
A basic understanding of the clinical components of musculoskeletal medicine is necessary in many medical fields. Musculoskeletal injuries represent the second most common presentation in US emergency departments, account for 49 million visits to orthopedic surgeon offices, and cost the United States an estimated $950 billion annually.1-3 Despite the staggering need for competency in musculoskeletal medicine, Freedman and Bernstein4 in 1998 demonstrated that musculoskeletal knowledge is inadequate among medical school graduates.
In 2005, the United States Bone and Joint Decade (now the United States Bone and Joint Initiative) announced Project 100, which recommended that 100% of US medical schools begin requiring a musculoskeletal course by the end of the decade.5 This project was intended to increase musculoskeletal understanding among medical students. Optimal curriculum reform, however, remains controversial. Many studies have found that medical schools continue to provide inadequate musculoskeletal education.4,6-9 For example, an integrated musculoskeletal curriculum with increased lecture time was found to improve clinical confidence but not musculoskeletal knowledge.6 In contrast, a 2-week intensive musculoskeletal module and a 6-week course involving orthopedic resident and faculty education has been shown to improve understanding.10,11
We conducted a study to determine the adequacy of musculoskeletal knowledge in medical school students, to determine musculoskeletal competency after curriculum reform through increased lecture and laboratory time, and to draw conclusions about factors leading to increased musculoskeletal competency to guide future curriculum reforms. We hypothesized that musculoskeletal knowledge would increase as a result of increased lecture and laboratory time.
Materials and Methods
The Tufts University School of Medicine Institutional Review Board approved this study. The medical school curriculum at our institution was redesigned to include a dedicated musculoskeletal module to improve medical student education (Table). The study compared medical students given the old musculoskeletal module (premodule group) and those given the new musculoskeletal module (postmodule group). The premodule group received 8.5 hours of physical diagnosis skills training and 30 hours of clinical anatomy training (12 lecture hours, 18 laboratory hours), and the postmodule group received 10 hours of physical diagnosis training and 41.5 hours of clinical anatomy training (18.5 lecture hours, 23 laboratory hours).
The lecture material for the postmodule group covered all topics/questions addressed on the validated musculoskeletal adequacy assessment. The new module specifically added 6 hours of dedicated clinically based musculoskeletal lecture time during the anatomy course and concurrent with the physical diagnosis course. The topics covered with case-based scenarios were orthopedic emergencies, adult hip and back, knee, pediatric hip and back, elbow/wrist/hand, and shoulder. A validated musculoskeletal competency examination was given to the premodule group at the end of the musculoskeletal anatomy and physical diagnosis lectures. The postmodule group took the competency examination at the end of the “new” 6 hours of musculoskeletal education.
We used the Freedman and Bernstein4 basic competency examination for musculoskeletal education assessment to assess knowledge. This examination is the only validated tool for assessing basic clinical musculoskeletal knowledge. All students were also asked whether they had experience rotating in orthopedic surgery or in a related musculoskeletal field (rheumatology, physiatry, neurology) during the medical school “selective” period that allowed 1 afternoon per week of elective time. Duration of exposure was assessed. The examination was given to 109 students in the premodule group 1 year before the curriculum changes. The examination was then given to the students for the first 2 years after the curriculum changes were implemented, with 296 students in the postmodule group. All questions on the examination were addressed within the 6 lecture hours in the new module. A single reviewer anonymously scored the examinations according to the validated scoring system over a 2-week period.4 Independent t tests were used to compare examination scores between the premodule and postmodule groups. Statistical significance was set at P < .05. Equal variance between groups was not assumed.
Results
The examination was given to 405 medical students (109 premodule, 296 postmodule) Mean examination score was 40%, significantly below the recommended mean passing score of 73.1%.4 Only 1 student achieved a passing score. Independent t tests were used to compare examination scores of the premodule and postmodule groups. Mean (SD) scores were higher (P < .05) for the premodule group, 42.1 (13.6), than the postmodule group, 39.1 (11.4) (Figure 1).
Independent t tests were used to compare examination scores of students with either orthopedics or rheumatology experience and students without this experience. Mean (SD) scores were higher (P < .05) for students with experience, 44.4 (11.9), than students without experience, 39.6 (12.1) (Figure 2). Students with neurology or physiatry experience did not score significantly higher than students without this experience. Statistical significance was set as P < .05. SAS 9.0 software (SAS Institute, Cary, North Carolina) was used for statistical analysis.
Discussion
Our students’ mean examination score was significantly lower than the passing (competency) score of 73.1%. Although Project 100 acknowledged many medical schools for implementing a required musculoskeletal course, our study results showed that adequate competency as indicated by a passing score on the Freedman and Bernstein examination was not achieved in medical school despite devoted musculoskeletal lecture time. Our postmodule group had lower scores than our premodule group despite being exposed to more lecture and laboratory material that systematically addressed every examination question. Similarly, Day and colleagues6 found that medical students scored a mean of 45% on the Freedman and Bernstein examination despite increased lecture and laboratory time.6 Lecture and laboratory exposure does not result in long-term information retention. Medical school competency is not significantly higher than what Freedman and Bernstein4 found for musculoskeletal education almost a decade earlier.
Musculoskeletal medicine typically is not revisited during medical school unless a student opts for an elective with a musculoskeletal basis. This specialty differs from others, such as neurology, which requires a 1-month clinical rotation before graduation. As increasing lecture and laboratory time did little to increase competency, adding a required clinical rotation in a musculoskeletal field or integrated musculoskeletal modules for anatomy and clinical training may be the best option for educational reform.
Our study found significantly higher Freedman and Bernstein examination scores for students with orthopedic surgery or rheumatology experience than for students without this experience. First- and second-year medical students are allowed to do a “selective” rotation—1 afternoon a week in an elective rotation of their choice. Students with orthopedics or rheumatology experience in this setting tended to score higher on the examination, possibly a result of both exposure to and interest in musculoskeletal issues. Many other studies have found that clinical exposure within a musculoskeletal field resulted in significantly higher musculoskeletal knowledge.8,12-16 Skelley and colleagues12 found that musculoskeletal clinical exposure of as short as 15 days significantly increased understanding among medical students. Grunfeld and colleagues15 found that students interested in orthopedics also had significantly more musculoskeletal knowledge. Musculoskeletal clinical exposure should be considered in medical school reform. As coordinating a curriculum with orthopedic resident and faculty involvement can set up educational barriers at some medical schools, dedicated musculoskeletal modules with a mock clinical skills component may be a useful consideration, and these have been shown to improve musculoskeletal knowledge.10,11
There are limitations to our study. The musculoskeletal examination was not given to an equal number of medical students in each group. The study also did not control for attendance, and therefore some students who took the musculoskeletal examination may not have attended all musculoskeletal module lectures. The validated examination used for basic competency is another possible limitation. The Freedman and Bernstein examination is the only validated examination used for basic competency, but it may not accurately assess meaningful development of clinical skills applicable to a patient musculoskeletal setting. No studies have assessed the correlation between musculoskeletal competency based on the Freedman and Bernstein examination and patient outcomes.
We conclude that increasing dedicated musculoskeletal lecture hours does not improve musculoskeletal knowledge. Future considerations should include incorporating further hands-on training through clinical skills workshops or rotations in orthopedic surgery or rheumatology.
1. Centers for Disease Control and Prevention, National Center for Health Statistics, Ambulatory and Hospital Care Statistics Branch. National Hospital Ambulatory Medical Care Survey: 2009 outpatient department summary tables. http://www.cdc.gov/nchs/data/ahcd/nhamcs_outpatient/2009_opd_web_tables.pdf. Accessed January 8, 2015.
2. Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008 Aug 6;(7):1-38.
3. United States Bone and Joint Initiative. The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal and Economic Costs. Rosemont, IL: United States Bone and Joint Initiative; 2008. http://www.boneandjointburden.org. Accessed January 9, 2015.
4. Freedman KB, Bernstein J. The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am. 1998;80(10):1421-1427.
5. United States Bone and Joint Initiative. Project 100—Undergraduate Musculoskeletal Education. Rosemont, IL: United States Bone and Joint Initiative; 2005. www.usbjd.org/projects/project_op.cfm?dirID=127. Accessed January 9, 2015.
6. Day CS, Ahn CS, Yeh AC, Tabrizi S. Early assessment of a new integrated preclinical musculoskeletal curriculum at a medical school. Am J Orthop. 2011;40(1):14-18.
7. Day CS, Yeh AC, Franko O, Ramirez M, Krupat E. Musculoskeletal medicine: an assessment of the attitudes and knowledge of medical students at Harvard Medical School. Acad Med. 2007;82(5):452-457.
8. Matzkin E, Smith EL, Freccero D, Richardson AB. Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am. 2005;87(2):310-314.
9. Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84(4):604-608.
10. Bilderback K, Eggerstedt J, Sadasivan KK, et al. Design and implementation of a system-based course in musculoskeletal medicine for medical students. J Bone Joint Surg Am. 2008;90(10):2292-2300.
11. Queally JM, Cummins F, Brennan SA, Shelly MJ, O’Byrne JM. Assessment of a new undergraduate module in musculoskeletal medicine. J Bone Joint Surg Am. 2011;93(3):e9.
12. Skelley NW, Tanaka MJ, Skelley LM, LaPorte DM. Medical student musculoskeletal education: an institutional survey. J Bone Joint Surg Am. 2012;94(19):e146(1-7).
13. DiGiovanni BF, Chu JY, Mooney CJ, Lambert DR. Maturation of medical student musculoskeletal medicine knowledge and clinical confidence. Med Educ Online. 2012;17. doi:10.3402/meo.v17i0.17092. Epub 2012 Jul 23.
14. Schmale GA. More evidence of educational inadequacies in musculoskeletal medicine. Clin Orthop. 2005;(437):251-259.
15. Grunfeld R, Banks S, Fox E, Levy BA, Craig C, Black K. An assessment of musculoskeletal knowledge in graduating medical and physician assistant students and implications for musculoskeletal care providers. J Bone Joint Surg Am. 2012;94(4):343-348.
16. Yeh AC, Franko O, Day CS. Impact of clinical electives and residency interest on medical students’ education in musculoskeletal medicine. J Bone Joint Surg Am. 2008;90(2):307-315.
1. Centers for Disease Control and Prevention, National Center for Health Statistics, Ambulatory and Hospital Care Statistics Branch. National Hospital Ambulatory Medical Care Survey: 2009 outpatient department summary tables. http://www.cdc.gov/nchs/data/ahcd/nhamcs_outpatient/2009_opd_web_tables.pdf. Accessed January 8, 2015.
2. Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008 Aug 6;(7):1-38.
3. United States Bone and Joint Initiative. The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal and Economic Costs. Rosemont, IL: United States Bone and Joint Initiative; 2008. http://www.boneandjointburden.org. Accessed January 9, 2015.
4. Freedman KB, Bernstein J. The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am. 1998;80(10):1421-1427.
5. United States Bone and Joint Initiative. Project 100—Undergraduate Musculoskeletal Education. Rosemont, IL: United States Bone and Joint Initiative; 2005. www.usbjd.org/projects/project_op.cfm?dirID=127. Accessed January 9, 2015.
6. Day CS, Ahn CS, Yeh AC, Tabrizi S. Early assessment of a new integrated preclinical musculoskeletal curriculum at a medical school. Am J Orthop. 2011;40(1):14-18.
7. Day CS, Yeh AC, Franko O, Ramirez M, Krupat E. Musculoskeletal medicine: an assessment of the attitudes and knowledge of medical students at Harvard Medical School. Acad Med. 2007;82(5):452-457.
8. Matzkin E, Smith EL, Freccero D, Richardson AB. Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am. 2005;87(2):310-314.
9. Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84(4):604-608.
10. Bilderback K, Eggerstedt J, Sadasivan KK, et al. Design and implementation of a system-based course in musculoskeletal medicine for medical students. J Bone Joint Surg Am. 2008;90(10):2292-2300.
11. Queally JM, Cummins F, Brennan SA, Shelly MJ, O’Byrne JM. Assessment of a new undergraduate module in musculoskeletal medicine. J Bone Joint Surg Am. 2011;93(3):e9.
12. Skelley NW, Tanaka MJ, Skelley LM, LaPorte DM. Medical student musculoskeletal education: an institutional survey. J Bone Joint Surg Am. 2012;94(19):e146(1-7).
13. DiGiovanni BF, Chu JY, Mooney CJ, Lambert DR. Maturation of medical student musculoskeletal medicine knowledge and clinical confidence. Med Educ Online. 2012;17. doi:10.3402/meo.v17i0.17092. Epub 2012 Jul 23.
14. Schmale GA. More evidence of educational inadequacies in musculoskeletal medicine. Clin Orthop. 2005;(437):251-259.
15. Grunfeld R, Banks S, Fox E, Levy BA, Craig C, Black K. An assessment of musculoskeletal knowledge in graduating medical and physician assistant students and implications for musculoskeletal care providers. J Bone Joint Surg Am. 2012;94(4):343-348.
16. Yeh AC, Franko O, Day CS. Impact of clinical electives and residency interest on medical students’ education in musculoskeletal medicine. J Bone Joint Surg Am. 2008;90(2):307-315.