User login
Unexpected skin necrosis of the thighs
A 62-YEAR-OLD WOMAN sought care at our clinic for painful skin lesions that had developed on her thighs 5 days earlier. She had received ongoing treatment at our clinic over the past few years for diabetes, hyperlipidemia, hypertension, and sarcoidosis. In the last 2 years, she’d had 2 hospitalizations for acute renal failure, with a creatinine value as high as 3.8 mg/dL and a persistent glomerular filtration rate consistent with stage 3 chronic kidney disease.
The medications she was taking included glyburide, pravastatin, and lisinopril. During the 2 years prior to her recent clinic visit, she’d had some intermittently elevated calcium readings. Repeat calcium levels each time were normal. In addition, her parathyroid hormone levels fluctuated between low, high, and normal. Her technetium sestamibi scan was negative for hyperparathyroidism. The patient was unemployed and gave no history of recent travel, injuries, or exposure to animals.
On examination, we noted large, poorly demarcated, warm, indurated erythematous lesions on her lateral thighs. She was given a diagnosis of cellulitis and treated with trimethoprim/sulfa-methoxazole 160/800 mg twice daily for 10 days. During follow-up visits 3 and 7 days later, she indicated that the lesions were less painful and they appeared to be less swollen.
Three weeks later, the patient returned to the clinic with skin sloughing that had produced necrotic lesions with black es-char on the bases (FIGURE 1). In addition, new lesions appeared on her anterior thighs. An initial punch biopsy of the lesions revealed no significant pathologic abnormality.
FIGURE 1
What started as indurated plaques…
The patient initially came in for the treatment of indurated plaques, which developed into ulcerative skin lesions with erythematous edges and eschar on the bases.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Calciphylaxis
Calciphylaxis is an uncommon disorder of vascular calcification and thrombosis resulting in skin necrosis.1 It most commonly occurs in people with end-stage renal disease (ESRD) on hemodialysis, but in nonuremic patients the most frequent cause is primary hyperparathyroidism.2,3 Similar vascular calcifications may be observed in milk alkali syndrome, rickets, collagen diseases, and hypervitaminosis D. Progression to necrosis in these cases is extremely rare.1 There are only a few documented cases of calciphylaxis associated with sarcoidosis, hypercalcemia, and non-ESRD.4
Female sex and diabetes appear to be risk factors.2 The presence of autoimmune disorders is a major feature in patients without ESRD.2,5 Although this patient did not have a previously diagnosed autoimmune disorder, an antinuclear antibody (ANA) test and lupus anticoagulant values were later found to be positive. In patients with autoimmune disorders, prednisone administration is associated with an increased risk of calciphylaxis.5 A hypercoagulable state can also underlie development of calciphylaxis. Our patient did have a mild protein C and S deficiency.
The prognosis of patients diagnosed with calciphylaxis is very poor. The mortality rate is reported to be as high as 60% to 80%.6
4 other possibilities comprise the differential diagnosis
Several conditions may present with erythema or necrosis similar to that of calciphylaxis (TABLE).
Warfarin-induced skin necrosis may produce hemorrhagic bullae and necrotic eschar, but generally presents within 3 to 10 days of initiating warfarin therapy.7 Severe dermatologic manifestations tend to affect the breasts, buttocks, and thighs.
Cutaneous anthrax causes painless necrotic lesions with black eschar, but is linked to bioterrorism or contact with infected animals. Constitutional symptoms such as fever, chills, and malaise are often present. Skin lesions are located primarily on the face, neck, and upper extremities.
Cholesterol embolization results from cholesterol crystals detaching and obstructing smaller arteries. Skin involvement includes livedo reticularis, petechiae, purpura, and ulcerations.
Vasculitis can affect all sizes of blood vessels. It can occur as a complication of connective tissue disorders, viral infections such as hepatitis B and C, or hypersensitivity reactions to medications such as penicillins and cephalosporins. Systemic symptoms are common, as is palpable purpura. Tissue biopsy is important for diagnosis and reveals blood vessel inflammation, not vessel wall calcification.
TABLE
Is it calciphylaxis or something else?1,3,7-9
| Condition | Characteristics |
|---|---|
| Warfarin-induced skin necrosis | Painful, erythematous, edematous lesions; rapidly progressive; petechiae, hemorrhagic bullae, then necrotic eschar |
| Cutaneous anthrax | Small painless, pruritic papules; advances to bullae; finally erodes to painless necrotic lesions with black eschar |
| Cholesterol embolization | Majority with livedo reticularis, cyanosis, or gangrene; smaller percentage with cutaneous ulceration, purpura, petechiae, or painful, firm erythematous nodules |
| Vasculitis | Palpable purpura; biopsy of most affected area is necessary for diagnosis |
| Calciphylaxis | Painful erythematous papules, plaques, nodules, or ulcerations in areas with high adiposity; may progress to necrosis |
What to do when the biopsy isn’t helpful
This case points out an important pathologic rule: If the biopsy doesn’t correlate with the observed disease, additional biopsies are indicated. Calciphylaxis is diagnosed on tissue microscopy, but the initial punch biopsy of the lesion revealed no significant pathologic abnormality. However, a subsequent deep-tissue biopsy showed extensive vascular wall calcification and septal fibrosis with subcutaneous fat necrosis.
Repeating abnormal laboratory testing is often appropriate, too. However, in this patient’s case, it probably would not have been helpful because she had intermittently elevated calcium levels over the years.
Wound cultures are often inaccurate in identifying a causative agent and this patient did not appear to have acute infection.
Management is mainly supportive
If you have a patient with calciphylaxis, address predisposing conditions such as hyperparathyroidism, hypercalcemia, and renal dysfunction5 (strength of recommendation [SOR]: C). In addition, discontinue calcium and vitamin D supplementation6 (SOR: C).
Finally, the patient will need meticulous wound care with adequate pain control; special attention to prevention of secondary infection is essential1,6 (SOR: C).
Our patient was one of the lucky ones
We treated this patient’s hypercalcemia, which was noted on admission to the hospital, with zoledronate and corrected her hypophosphatemia. Her renal function significantly improved with aggressive hydration.
With correction of electrolytes and normalization of kidney function, lesion progression was arrested. Granulation tissue developed in the lesions and split-thickness expanded skin grafts were performed on the large lesions (FIGURE 2). Fortunately, this patient survived despite the usual high rate of mortality. JFP
FIGURE 2
Good granulation beds, followed by closure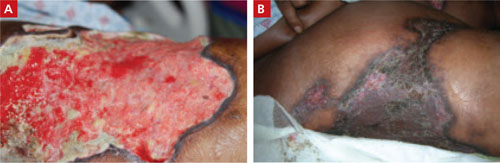
After aggressive treatment of renal dysfunction, correction of electrolyte abnormalities, and meticulous wound care, the patient’s lesions developed good granulation beds and showed signs of healing (A). The second image (B), taken 9 months after the patient first sought treatment for the lesions, shows the wounds after skin grafting.
CORRESPONDENCE
E.J. Mayeaux, Jr, MD, DABFP, FAAFP, Louisiana State University Health Sciences Center, 1501 Kings Highway, Shreveport, LA 71130; [email protected]
1. Kent RB 3rd, Lylerly RT. Systemic calciphylaxis. South Med J. 1994;87:278-281.
2. Nigwekar SU, Wolf M, Sterns RH, et al. Calciphylaxis from nonuremic causes. Clin J Am Soc Nephrol. 2008;3:1139-1143.
3. Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating. Kidney Int. 2002;61:2210-2217.
4. Swanson AM, Desai SR, Jackson JD, et al. Calciphylaxis associated with chronic inflammatory conditions, immunosuppression therapy, and normal renal function: a report of 2 cases. Arch Dermatol. 2009;145:723-725.
5. Weenig RH, Sewell LD, Davis MD, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-579.
6. Al-Hwiesh AK. Calciphylaxis of both proximal and distal distribution. Saudi J Kidney Dis Transpl. 2008;19:82-86.
7. Renick AM Jr. Anticoagulant-induced necrosis of skin and sub-cutaneous tissues. South Med J. 1976;69:775-778, 804.
8. Wenner KA, Kenner JR. Anthrax. Dermatol Clin. 2004;22:247-256.
9. Falanga V, Fine MJ, Kapoor WN. The cutaneous manifestations of cholesterol crystal embolization. Arch Dermatol. 1986;122:1194-1198.
A 62-YEAR-OLD WOMAN sought care at our clinic for painful skin lesions that had developed on her thighs 5 days earlier. She had received ongoing treatment at our clinic over the past few years for diabetes, hyperlipidemia, hypertension, and sarcoidosis. In the last 2 years, she’d had 2 hospitalizations for acute renal failure, with a creatinine value as high as 3.8 mg/dL and a persistent glomerular filtration rate consistent with stage 3 chronic kidney disease.
The medications she was taking included glyburide, pravastatin, and lisinopril. During the 2 years prior to her recent clinic visit, she’d had some intermittently elevated calcium readings. Repeat calcium levels each time were normal. In addition, her parathyroid hormone levels fluctuated between low, high, and normal. Her technetium sestamibi scan was negative for hyperparathyroidism. The patient was unemployed and gave no history of recent travel, injuries, or exposure to animals.
On examination, we noted large, poorly demarcated, warm, indurated erythematous lesions on her lateral thighs. She was given a diagnosis of cellulitis and treated with trimethoprim/sulfa-methoxazole 160/800 mg twice daily for 10 days. During follow-up visits 3 and 7 days later, she indicated that the lesions were less painful and they appeared to be less swollen.
Three weeks later, the patient returned to the clinic with skin sloughing that had produced necrotic lesions with black es-char on the bases (FIGURE 1). In addition, new lesions appeared on her anterior thighs. An initial punch biopsy of the lesions revealed no significant pathologic abnormality.
FIGURE 1
What started as indurated plaques…
The patient initially came in for the treatment of indurated plaques, which developed into ulcerative skin lesions with erythematous edges and eschar on the bases.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Calciphylaxis
Calciphylaxis is an uncommon disorder of vascular calcification and thrombosis resulting in skin necrosis.1 It most commonly occurs in people with end-stage renal disease (ESRD) on hemodialysis, but in nonuremic patients the most frequent cause is primary hyperparathyroidism.2,3 Similar vascular calcifications may be observed in milk alkali syndrome, rickets, collagen diseases, and hypervitaminosis D. Progression to necrosis in these cases is extremely rare.1 There are only a few documented cases of calciphylaxis associated with sarcoidosis, hypercalcemia, and non-ESRD.4
Female sex and diabetes appear to be risk factors.2 The presence of autoimmune disorders is a major feature in patients without ESRD.2,5 Although this patient did not have a previously diagnosed autoimmune disorder, an antinuclear antibody (ANA) test and lupus anticoagulant values were later found to be positive. In patients with autoimmune disorders, prednisone administration is associated with an increased risk of calciphylaxis.5 A hypercoagulable state can also underlie development of calciphylaxis. Our patient did have a mild protein C and S deficiency.
The prognosis of patients diagnosed with calciphylaxis is very poor. The mortality rate is reported to be as high as 60% to 80%.6
4 other possibilities comprise the differential diagnosis
Several conditions may present with erythema or necrosis similar to that of calciphylaxis (TABLE).
Warfarin-induced skin necrosis may produce hemorrhagic bullae and necrotic eschar, but generally presents within 3 to 10 days of initiating warfarin therapy.7 Severe dermatologic manifestations tend to affect the breasts, buttocks, and thighs.
Cutaneous anthrax causes painless necrotic lesions with black eschar, but is linked to bioterrorism or contact with infected animals. Constitutional symptoms such as fever, chills, and malaise are often present. Skin lesions are located primarily on the face, neck, and upper extremities.
Cholesterol embolization results from cholesterol crystals detaching and obstructing smaller arteries. Skin involvement includes livedo reticularis, petechiae, purpura, and ulcerations.
Vasculitis can affect all sizes of blood vessels. It can occur as a complication of connective tissue disorders, viral infections such as hepatitis B and C, or hypersensitivity reactions to medications such as penicillins and cephalosporins. Systemic symptoms are common, as is palpable purpura. Tissue biopsy is important for diagnosis and reveals blood vessel inflammation, not vessel wall calcification.
TABLE
Is it calciphylaxis or something else?1,3,7-9
| Condition | Characteristics |
|---|---|
| Warfarin-induced skin necrosis | Painful, erythematous, edematous lesions; rapidly progressive; petechiae, hemorrhagic bullae, then necrotic eschar |
| Cutaneous anthrax | Small painless, pruritic papules; advances to bullae; finally erodes to painless necrotic lesions with black eschar |
| Cholesterol embolization | Majority with livedo reticularis, cyanosis, or gangrene; smaller percentage with cutaneous ulceration, purpura, petechiae, or painful, firm erythematous nodules |
| Vasculitis | Palpable purpura; biopsy of most affected area is necessary for diagnosis |
| Calciphylaxis | Painful erythematous papules, plaques, nodules, or ulcerations in areas with high adiposity; may progress to necrosis |
What to do when the biopsy isn’t helpful
This case points out an important pathologic rule: If the biopsy doesn’t correlate with the observed disease, additional biopsies are indicated. Calciphylaxis is diagnosed on tissue microscopy, but the initial punch biopsy of the lesion revealed no significant pathologic abnormality. However, a subsequent deep-tissue biopsy showed extensive vascular wall calcification and septal fibrosis with subcutaneous fat necrosis.
Repeating abnormal laboratory testing is often appropriate, too. However, in this patient’s case, it probably would not have been helpful because she had intermittently elevated calcium levels over the years.
Wound cultures are often inaccurate in identifying a causative agent and this patient did not appear to have acute infection.
Management is mainly supportive
If you have a patient with calciphylaxis, address predisposing conditions such as hyperparathyroidism, hypercalcemia, and renal dysfunction5 (strength of recommendation [SOR]: C). In addition, discontinue calcium and vitamin D supplementation6 (SOR: C).
Finally, the patient will need meticulous wound care with adequate pain control; special attention to prevention of secondary infection is essential1,6 (SOR: C).
Our patient was one of the lucky ones
We treated this patient’s hypercalcemia, which was noted on admission to the hospital, with zoledronate and corrected her hypophosphatemia. Her renal function significantly improved with aggressive hydration.
With correction of electrolytes and normalization of kidney function, lesion progression was arrested. Granulation tissue developed in the lesions and split-thickness expanded skin grafts were performed on the large lesions (FIGURE 2). Fortunately, this patient survived despite the usual high rate of mortality. JFP
FIGURE 2
Good granulation beds, followed by closure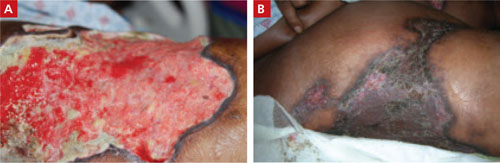
After aggressive treatment of renal dysfunction, correction of electrolyte abnormalities, and meticulous wound care, the patient’s lesions developed good granulation beds and showed signs of healing (A). The second image (B), taken 9 months after the patient first sought treatment for the lesions, shows the wounds after skin grafting.
CORRESPONDENCE
E.J. Mayeaux, Jr, MD, DABFP, FAAFP, Louisiana State University Health Sciences Center, 1501 Kings Highway, Shreveport, LA 71130; [email protected]
A 62-YEAR-OLD WOMAN sought care at our clinic for painful skin lesions that had developed on her thighs 5 days earlier. She had received ongoing treatment at our clinic over the past few years for diabetes, hyperlipidemia, hypertension, and sarcoidosis. In the last 2 years, she’d had 2 hospitalizations for acute renal failure, with a creatinine value as high as 3.8 mg/dL and a persistent glomerular filtration rate consistent with stage 3 chronic kidney disease.
The medications she was taking included glyburide, pravastatin, and lisinopril. During the 2 years prior to her recent clinic visit, she’d had some intermittently elevated calcium readings. Repeat calcium levels each time were normal. In addition, her parathyroid hormone levels fluctuated between low, high, and normal. Her technetium sestamibi scan was negative for hyperparathyroidism. The patient was unemployed and gave no history of recent travel, injuries, or exposure to animals.
On examination, we noted large, poorly demarcated, warm, indurated erythematous lesions on her lateral thighs. She was given a diagnosis of cellulitis and treated with trimethoprim/sulfa-methoxazole 160/800 mg twice daily for 10 days. During follow-up visits 3 and 7 days later, she indicated that the lesions were less painful and they appeared to be less swollen.
Three weeks later, the patient returned to the clinic with skin sloughing that had produced necrotic lesions with black es-char on the bases (FIGURE 1). In addition, new lesions appeared on her anterior thighs. An initial punch biopsy of the lesions revealed no significant pathologic abnormality.
FIGURE 1
What started as indurated plaques…
The patient initially came in for the treatment of indurated plaques, which developed into ulcerative skin lesions with erythematous edges and eschar on the bases.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Calciphylaxis
Calciphylaxis is an uncommon disorder of vascular calcification and thrombosis resulting in skin necrosis.1 It most commonly occurs in people with end-stage renal disease (ESRD) on hemodialysis, but in nonuremic patients the most frequent cause is primary hyperparathyroidism.2,3 Similar vascular calcifications may be observed in milk alkali syndrome, rickets, collagen diseases, and hypervitaminosis D. Progression to necrosis in these cases is extremely rare.1 There are only a few documented cases of calciphylaxis associated with sarcoidosis, hypercalcemia, and non-ESRD.4
Female sex and diabetes appear to be risk factors.2 The presence of autoimmune disorders is a major feature in patients without ESRD.2,5 Although this patient did not have a previously diagnosed autoimmune disorder, an antinuclear antibody (ANA) test and lupus anticoagulant values were later found to be positive. In patients with autoimmune disorders, prednisone administration is associated with an increased risk of calciphylaxis.5 A hypercoagulable state can also underlie development of calciphylaxis. Our patient did have a mild protein C and S deficiency.
The prognosis of patients diagnosed with calciphylaxis is very poor. The mortality rate is reported to be as high as 60% to 80%.6
4 other possibilities comprise the differential diagnosis
Several conditions may present with erythema or necrosis similar to that of calciphylaxis (TABLE).
Warfarin-induced skin necrosis may produce hemorrhagic bullae and necrotic eschar, but generally presents within 3 to 10 days of initiating warfarin therapy.7 Severe dermatologic manifestations tend to affect the breasts, buttocks, and thighs.
Cutaneous anthrax causes painless necrotic lesions with black eschar, but is linked to bioterrorism or contact with infected animals. Constitutional symptoms such as fever, chills, and malaise are often present. Skin lesions are located primarily on the face, neck, and upper extremities.
Cholesterol embolization results from cholesterol crystals detaching and obstructing smaller arteries. Skin involvement includes livedo reticularis, petechiae, purpura, and ulcerations.
Vasculitis can affect all sizes of blood vessels. It can occur as a complication of connective tissue disorders, viral infections such as hepatitis B and C, or hypersensitivity reactions to medications such as penicillins and cephalosporins. Systemic symptoms are common, as is palpable purpura. Tissue biopsy is important for diagnosis and reveals blood vessel inflammation, not vessel wall calcification.
TABLE
Is it calciphylaxis or something else?1,3,7-9
| Condition | Characteristics |
|---|---|
| Warfarin-induced skin necrosis | Painful, erythematous, edematous lesions; rapidly progressive; petechiae, hemorrhagic bullae, then necrotic eschar |
| Cutaneous anthrax | Small painless, pruritic papules; advances to bullae; finally erodes to painless necrotic lesions with black eschar |
| Cholesterol embolization | Majority with livedo reticularis, cyanosis, or gangrene; smaller percentage with cutaneous ulceration, purpura, petechiae, or painful, firm erythematous nodules |
| Vasculitis | Palpable purpura; biopsy of most affected area is necessary for diagnosis |
| Calciphylaxis | Painful erythematous papules, plaques, nodules, or ulcerations in areas with high adiposity; may progress to necrosis |
What to do when the biopsy isn’t helpful
This case points out an important pathologic rule: If the biopsy doesn’t correlate with the observed disease, additional biopsies are indicated. Calciphylaxis is diagnosed on tissue microscopy, but the initial punch biopsy of the lesion revealed no significant pathologic abnormality. However, a subsequent deep-tissue biopsy showed extensive vascular wall calcification and septal fibrosis with subcutaneous fat necrosis.
Repeating abnormal laboratory testing is often appropriate, too. However, in this patient’s case, it probably would not have been helpful because she had intermittently elevated calcium levels over the years.
Wound cultures are often inaccurate in identifying a causative agent and this patient did not appear to have acute infection.
Management is mainly supportive
If you have a patient with calciphylaxis, address predisposing conditions such as hyperparathyroidism, hypercalcemia, and renal dysfunction5 (strength of recommendation [SOR]: C). In addition, discontinue calcium and vitamin D supplementation6 (SOR: C).
Finally, the patient will need meticulous wound care with adequate pain control; special attention to prevention of secondary infection is essential1,6 (SOR: C).
Our patient was one of the lucky ones
We treated this patient’s hypercalcemia, which was noted on admission to the hospital, with zoledronate and corrected her hypophosphatemia. Her renal function significantly improved with aggressive hydration.
With correction of electrolytes and normalization of kidney function, lesion progression was arrested. Granulation tissue developed in the lesions and split-thickness expanded skin grafts were performed on the large lesions (FIGURE 2). Fortunately, this patient survived despite the usual high rate of mortality. JFP
FIGURE 2
Good granulation beds, followed by closure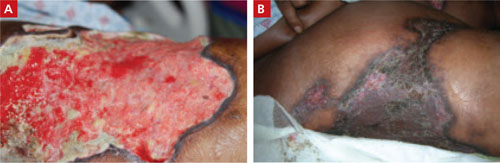
After aggressive treatment of renal dysfunction, correction of electrolyte abnormalities, and meticulous wound care, the patient’s lesions developed good granulation beds and showed signs of healing (A). The second image (B), taken 9 months after the patient first sought treatment for the lesions, shows the wounds after skin grafting.
CORRESPONDENCE
E.J. Mayeaux, Jr, MD, DABFP, FAAFP, Louisiana State University Health Sciences Center, 1501 Kings Highway, Shreveport, LA 71130; [email protected]
1. Kent RB 3rd, Lylerly RT. Systemic calciphylaxis. South Med J. 1994;87:278-281.
2. Nigwekar SU, Wolf M, Sterns RH, et al. Calciphylaxis from nonuremic causes. Clin J Am Soc Nephrol. 2008;3:1139-1143.
3. Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating. Kidney Int. 2002;61:2210-2217.
4. Swanson AM, Desai SR, Jackson JD, et al. Calciphylaxis associated with chronic inflammatory conditions, immunosuppression therapy, and normal renal function: a report of 2 cases. Arch Dermatol. 2009;145:723-725.
5. Weenig RH, Sewell LD, Davis MD, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-579.
6. Al-Hwiesh AK. Calciphylaxis of both proximal and distal distribution. Saudi J Kidney Dis Transpl. 2008;19:82-86.
7. Renick AM Jr. Anticoagulant-induced necrosis of skin and sub-cutaneous tissues. South Med J. 1976;69:775-778, 804.
8. Wenner KA, Kenner JR. Anthrax. Dermatol Clin. 2004;22:247-256.
9. Falanga V, Fine MJ, Kapoor WN. The cutaneous manifestations of cholesterol crystal embolization. Arch Dermatol. 1986;122:1194-1198.
1. Kent RB 3rd, Lylerly RT. Systemic calciphylaxis. South Med J. 1994;87:278-281.
2. Nigwekar SU, Wolf M, Sterns RH, et al. Calciphylaxis from nonuremic causes. Clin J Am Soc Nephrol. 2008;3:1139-1143.
3. Fine A, Zacharias J. Calciphylaxis is usually non-ulcerating. Kidney Int. 2002;61:2210-2217.
4. Swanson AM, Desai SR, Jackson JD, et al. Calciphylaxis associated with chronic inflammatory conditions, immunosuppression therapy, and normal renal function: a report of 2 cases. Arch Dermatol. 2009;145:723-725.
5. Weenig RH, Sewell LD, Davis MD, et al. Calciphylaxis: natural history, risk factor analysis, and outcome. J Am Acad Dermatol. 2007;56:569-579.
6. Al-Hwiesh AK. Calciphylaxis of both proximal and distal distribution. Saudi J Kidney Dis Transpl. 2008;19:82-86.
7. Renick AM Jr. Anticoagulant-induced necrosis of skin and sub-cutaneous tissues. South Med J. 1976;69:775-778, 804.
8. Wenner KA, Kenner JR. Anthrax. Dermatol Clin. 2004;22:247-256.
9. Falanga V, Fine MJ, Kapoor WN. The cutaneous manifestations of cholesterol crystal embolization. Arch Dermatol. 1986;122:1194-1198.