User login
Long-term methimazole therapy improves Graves disease remission rate
VICTORIA, B.C. – In the debate over the optimal duration of methimazole therapy for Graves disease, findings of a new randomized, controlled trial reported at the annual meeting of the American Thyroid Association tip the balance in favor of long-term therapy.
The relapse rate among patients who stayed on the drug long term, for a median of 96 months, was about one-third that among patients who stopped after 18 months, reported lead investigator Fereidoun Azizi, MD, of the Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran. Patients staying on the drug long term did not experience any adverse effects during that time, although only those able to tolerate the drug initially were randomized.
There may be two explanations for this benefit of long-term therapy, according to Dr. Azizi. Long-term therapy may alter immune-related molecular signaling and cell subsets in both the thymus and periphery, ultimately shifting disease course. On the other hand, establishing and maintaining euthyroidism for a prolonged period of time may quell the autoimmune response.
“We are looking at this in depth and also at some of the [molecular factors] in order to elucidate the mechanism behind our striking findings,” he said.
One of the session cochairs, Yaron Tomer, MD, chair of the department of medicine and the Anita and Jack Saltz Chair in Diabetes Research at the Montefiore Medical Center, New York, commented, “There is a move today away from radioactive iodine – many patients do not want radioactive iodine, and we do more surgery now because of that. So this opens up a new option that we didn’t have before.”
The other session cochair, Catherine A. Dinauer, MD, a pediatric endocrinologist and clinician at the Yale Pediatric Thyroid Center, New Haven, Conn., noted that duration of therapy frequently comes up in her practice.
Study details
Relapse of hyperthyroidism after discontinuation of antithyroid drugs remains problematic, Dr. Azizi pointed out when introducing the study.
“Many of the major papers have noted that longer antithyroid drug treatment does not really influence remission rate of Graves, and therefore most of us treat for between 12 and 24 months with antithyroid drugs, and then we stop the medication,” he said. However, recent studies and in particular a meta-analysis (Thyroid. 2017;27:1223-31) suggest there may be an advantage of long-term therapy.
Dr. Azizi and coinvestigators recruited to their trial 302 consecutive patients from a single clinic who had untreated Graves disease and were started on methimazole (Tapazole) therapy.
The 258 patients completing 18 months of therapy were randomized to stop the drug or continue on a maintenance dose long term, for 60-120 months, on a single-blind basis. (The other 44 patients withdrew mainly because of side effects, relapse, and loss to follow-up.)
Patients in the long-term therapy group stayed on the drug for a median of 96 months. The decision about specifically when to stop in this group was guided by thyroid function test results and patients’ clinical status and preferences, according to Dr. Azizi.
The rate of relapse at 48 months after stopping methimazole was 51% among patients in the short-term therapy group but just 16% among patients in the long-term therapy group (P less than or equal to .001). “Definitely, this looks like a cure of the disease if we consider this very low incidence of relapse,” he commented.
Within the group treated long term, patients who did and did not experience relapse were statistically indistinguishable with respect to temporal trends in levels of triiodothyronine (T3), free thyroxine (T4), thyroid-stimulating hormone (TSH), and thyroid-stimulating hormone receptor antibody (TRAb).
Additionally, the daily dose of methimazole therapy required to maintain TSH levels in the normal range fell similarly over time, to about half the initial dose, regardless of whether patients had a relapse or not.
“At the end of treatment, the majority of patients were taking less than 5 mg/day of methimazole,” Dr. Azizi reported. “Some patients needed only two or three pills of 5-mg methimazole per week, and this is very interesting to know, that after you continue, you have definitely more response to methimazole.”
Multivariate analyses showed that in the short-term therapy group, risk factors for relapse were age, sex, and end-of-therapy levels of T3, TSH, and TRAb. In the long-term therapy group, risk factors were end-of-therapy levels of free T4 and TSH.
“We are currently performing more in-depth analysis of genetic markers, including both SNPs [single nucleotide polymorphisms] and HLA [human leukocyte antigen] subtyping on these samples to assess any potential association between relapse rates and genetic background,” Dr. Azizi noted. “However, the problem is the low number of patients who have had a relapse long term.”
During the first 18 months of methimazole therapy, 16 patients had adverse effects in the first 2 months (14 had cutaneous reactions and 2 had elevation of liver enzymes). However, there were no serious complications, such as agranulocytosis.
“It’s very reassuring that after 18 months, in those who had long-term treatment, we did not see any minor or major complications throughout, up to the 120 months of treatment we have had in some of our patients,” Dr. Azizi commented.
Dr. Azizi disclosed that he had no relevant conflicts of interest.
VICTORIA, B.C. – In the debate over the optimal duration of methimazole therapy for Graves disease, findings of a new randomized, controlled trial reported at the annual meeting of the American Thyroid Association tip the balance in favor of long-term therapy.
The relapse rate among patients who stayed on the drug long term, for a median of 96 months, was about one-third that among patients who stopped after 18 months, reported lead investigator Fereidoun Azizi, MD, of the Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran. Patients staying on the drug long term did not experience any adverse effects during that time, although only those able to tolerate the drug initially were randomized.
There may be two explanations for this benefit of long-term therapy, according to Dr. Azizi. Long-term therapy may alter immune-related molecular signaling and cell subsets in both the thymus and periphery, ultimately shifting disease course. On the other hand, establishing and maintaining euthyroidism for a prolonged period of time may quell the autoimmune response.
“We are looking at this in depth and also at some of the [molecular factors] in order to elucidate the mechanism behind our striking findings,” he said.
One of the session cochairs, Yaron Tomer, MD, chair of the department of medicine and the Anita and Jack Saltz Chair in Diabetes Research at the Montefiore Medical Center, New York, commented, “There is a move today away from radioactive iodine – many patients do not want radioactive iodine, and we do more surgery now because of that. So this opens up a new option that we didn’t have before.”
The other session cochair, Catherine A. Dinauer, MD, a pediatric endocrinologist and clinician at the Yale Pediatric Thyroid Center, New Haven, Conn., noted that duration of therapy frequently comes up in her practice.
Study details
Relapse of hyperthyroidism after discontinuation of antithyroid drugs remains problematic, Dr. Azizi pointed out when introducing the study.
“Many of the major papers have noted that longer antithyroid drug treatment does not really influence remission rate of Graves, and therefore most of us treat for between 12 and 24 months with antithyroid drugs, and then we stop the medication,” he said. However, recent studies and in particular a meta-analysis (Thyroid. 2017;27:1223-31) suggest there may be an advantage of long-term therapy.
Dr. Azizi and coinvestigators recruited to their trial 302 consecutive patients from a single clinic who had untreated Graves disease and were started on methimazole (Tapazole) therapy.
The 258 patients completing 18 months of therapy were randomized to stop the drug or continue on a maintenance dose long term, for 60-120 months, on a single-blind basis. (The other 44 patients withdrew mainly because of side effects, relapse, and loss to follow-up.)
Patients in the long-term therapy group stayed on the drug for a median of 96 months. The decision about specifically when to stop in this group was guided by thyroid function test results and patients’ clinical status and preferences, according to Dr. Azizi.
The rate of relapse at 48 months after stopping methimazole was 51% among patients in the short-term therapy group but just 16% among patients in the long-term therapy group (P less than or equal to .001). “Definitely, this looks like a cure of the disease if we consider this very low incidence of relapse,” he commented.
Within the group treated long term, patients who did and did not experience relapse were statistically indistinguishable with respect to temporal trends in levels of triiodothyronine (T3), free thyroxine (T4), thyroid-stimulating hormone (TSH), and thyroid-stimulating hormone receptor antibody (TRAb).
Additionally, the daily dose of methimazole therapy required to maintain TSH levels in the normal range fell similarly over time, to about half the initial dose, regardless of whether patients had a relapse or not.
“At the end of treatment, the majority of patients were taking less than 5 mg/day of methimazole,” Dr. Azizi reported. “Some patients needed only two or three pills of 5-mg methimazole per week, and this is very interesting to know, that after you continue, you have definitely more response to methimazole.”
Multivariate analyses showed that in the short-term therapy group, risk factors for relapse were age, sex, and end-of-therapy levels of T3, TSH, and TRAb. In the long-term therapy group, risk factors were end-of-therapy levels of free T4 and TSH.
“We are currently performing more in-depth analysis of genetic markers, including both SNPs [single nucleotide polymorphisms] and HLA [human leukocyte antigen] subtyping on these samples to assess any potential association between relapse rates and genetic background,” Dr. Azizi noted. “However, the problem is the low number of patients who have had a relapse long term.”
During the first 18 months of methimazole therapy, 16 patients had adverse effects in the first 2 months (14 had cutaneous reactions and 2 had elevation of liver enzymes). However, there were no serious complications, such as agranulocytosis.
“It’s very reassuring that after 18 months, in those who had long-term treatment, we did not see any minor or major complications throughout, up to the 120 months of treatment we have had in some of our patients,” Dr. Azizi commented.
Dr. Azizi disclosed that he had no relevant conflicts of interest.
VICTORIA, B.C. – In the debate over the optimal duration of methimazole therapy for Graves disease, findings of a new randomized, controlled trial reported at the annual meeting of the American Thyroid Association tip the balance in favor of long-term therapy.
The relapse rate among patients who stayed on the drug long term, for a median of 96 months, was about one-third that among patients who stopped after 18 months, reported lead investigator Fereidoun Azizi, MD, of the Endocrine Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran. Patients staying on the drug long term did not experience any adverse effects during that time, although only those able to tolerate the drug initially were randomized.
There may be two explanations for this benefit of long-term therapy, according to Dr. Azizi. Long-term therapy may alter immune-related molecular signaling and cell subsets in both the thymus and periphery, ultimately shifting disease course. On the other hand, establishing and maintaining euthyroidism for a prolonged period of time may quell the autoimmune response.
“We are looking at this in depth and also at some of the [molecular factors] in order to elucidate the mechanism behind our striking findings,” he said.
One of the session cochairs, Yaron Tomer, MD, chair of the department of medicine and the Anita and Jack Saltz Chair in Diabetes Research at the Montefiore Medical Center, New York, commented, “There is a move today away from radioactive iodine – many patients do not want radioactive iodine, and we do more surgery now because of that. So this opens up a new option that we didn’t have before.”
The other session cochair, Catherine A. Dinauer, MD, a pediatric endocrinologist and clinician at the Yale Pediatric Thyroid Center, New Haven, Conn., noted that duration of therapy frequently comes up in her practice.
Study details
Relapse of hyperthyroidism after discontinuation of antithyroid drugs remains problematic, Dr. Azizi pointed out when introducing the study.
“Many of the major papers have noted that longer antithyroid drug treatment does not really influence remission rate of Graves, and therefore most of us treat for between 12 and 24 months with antithyroid drugs, and then we stop the medication,” he said. However, recent studies and in particular a meta-analysis (Thyroid. 2017;27:1223-31) suggest there may be an advantage of long-term therapy.
Dr. Azizi and coinvestigators recruited to their trial 302 consecutive patients from a single clinic who had untreated Graves disease and were started on methimazole (Tapazole) therapy.
The 258 patients completing 18 months of therapy were randomized to stop the drug or continue on a maintenance dose long term, for 60-120 months, on a single-blind basis. (The other 44 patients withdrew mainly because of side effects, relapse, and loss to follow-up.)
Patients in the long-term therapy group stayed on the drug for a median of 96 months. The decision about specifically when to stop in this group was guided by thyroid function test results and patients’ clinical status and preferences, according to Dr. Azizi.
The rate of relapse at 48 months after stopping methimazole was 51% among patients in the short-term therapy group but just 16% among patients in the long-term therapy group (P less than or equal to .001). “Definitely, this looks like a cure of the disease if we consider this very low incidence of relapse,” he commented.
Within the group treated long term, patients who did and did not experience relapse were statistically indistinguishable with respect to temporal trends in levels of triiodothyronine (T3), free thyroxine (T4), thyroid-stimulating hormone (TSH), and thyroid-stimulating hormone receptor antibody (TRAb).
Additionally, the daily dose of methimazole therapy required to maintain TSH levels in the normal range fell similarly over time, to about half the initial dose, regardless of whether patients had a relapse or not.
“At the end of treatment, the majority of patients were taking less than 5 mg/day of methimazole,” Dr. Azizi reported. “Some patients needed only two or three pills of 5-mg methimazole per week, and this is very interesting to know, that after you continue, you have definitely more response to methimazole.”
Multivariate analyses showed that in the short-term therapy group, risk factors for relapse were age, sex, and end-of-therapy levels of T3, TSH, and TRAb. In the long-term therapy group, risk factors were end-of-therapy levels of free T4 and TSH.
“We are currently performing more in-depth analysis of genetic markers, including both SNPs [single nucleotide polymorphisms] and HLA [human leukocyte antigen] subtyping on these samples to assess any potential association between relapse rates and genetic background,” Dr. Azizi noted. “However, the problem is the low number of patients who have had a relapse long term.”
During the first 18 months of methimazole therapy, 16 patients had adverse effects in the first 2 months (14 had cutaneous reactions and 2 had elevation of liver enzymes). However, there were no serious complications, such as agranulocytosis.
“It’s very reassuring that after 18 months, in those who had long-term treatment, we did not see any minor or major complications throughout, up to the 120 months of treatment we have had in some of our patients,” Dr. Azizi commented.
Dr. Azizi disclosed that he had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: Relative to peers who stopped methimazole after 18 months, patients who continued on the drug for a median of 96 months had a lower rate of relapse after discontinuation (51% vs. 16%; P less than or equal to .001).
Data source: A randomized controlled trial among 258 patients with Graves disease who were relapse free after 18 months on methimazole.
Disclosures: Dr. Azizi disclosed that he had no relevant conflicts of interest.
Add-on mycophenolate boosts efficacy of steroids for Graves’ orbitopathy
VICTORIA, B.C. – Adding a nonsteroidal immunosuppressant to steroid therapy improves control of active, moderate-to-severe Graves’ orbitopathy, according to findings from a randomized controlled trial reported at the annual meeting of the American Thyroid Association.
Relative to counterparts given pulsed intravenous methylprednisolone alone, patients also given oral mycophenolate were twice as likely to achieve reduction of their ophthalmic signs and symptoms, first author George J. Kahaly, MD, PhD, reported in a session on behalf of the European Group on Graves’ Orbitopathy (EUGOGO). And the combination was generally safe and well tolerated.

“Since there is a clear advantage of combination treatment in response rate, in the absence of contraindication to mycophenolate, patients with active and severe orbitopathy may be considered for combination treatment,” he proposed.
A session attendee noted that a similar recent study from China suggests that mycophenolate monotherapy achieves a very high remission rate in this patient population (Clin Endocrinol (Oxf). 2017;86[2]:247-55). “Why don’t we just go for [mycophenolate] alone? Why keep pushing steroids?” he asked.
Methodology of that study was less rigorous, maintained Dr. Kahaly, who is professor of medicine and endocrinology/metabolism, chief physician of the endocrine outpatient clinic, and director of the thyroid research lab at Gutenberg University Medical Center in Mainz, Germany.
“I would say mycophenolate alone is not a powerful enough treatment to observe a response rate of 70%, 80%, 90%,” he stated. “You need more time. This is a lymphocyte-inhibiting agent, so you need the acute effect of the intravenous steroids at the beginning.”
Session cochair Angela M. Leung, MD, assistant professor of medicine at the University of California, Los Angeles, and an endocrinologist at both UCLA and the VA Greater Los Angeles Healthcare System, commented, “This is an intriguing study with very promising data from an active group of investigators.”

At the same time, benefit of add-on mycophenolate remains uncertain, in her opinion. “Clearly, more studies, perhaps longer-duration ones, are needed to assess the true effect and clinical efficacy,” she said.
Introducing the EUGOGO trial, Dr. Kahaly noted that European guidelines recommend intravenous methylprednisolone as first-line therapy for Graves’ orbitopathy that is moderate to severe or sight threatening (Eur Thyroid J. 2016;5:9-26). Some patients, however, do not achieve response on this therapy, and others who do achieve response then go on to experience relapse, underscoring the need for better therapies.
The combination the investigators selected pairs the anti-inflammatory activity of methylprednisolone with the antiproliferative activity of mycophenolate (CellCept), which is mainly used in the transplantation field.
The trial, funded in part by Novartis, was open to patients with Graves’ disease who had been euthyroid for at least 2 months but had untreated, active, moderate-to-severe orbitopathy with involvement of soft tissues and eye muscles. Those with optic neuropathy were excluded.
Patients were randomized to 12 weeks of once-weekly intravenous methylprednisolone either alone or with the addition of 24 weeks of twice-daily oral mycophenolate initiated at the same time.
Blinded observers assessed patients for orbitopathy response, defined as improvement in two or more of six outcome measures (eyelid swelling, clinical activity score, proptosis, lid width, diplopia, and motility) in at least one eye, without deterioration in any of the same measures in either eye.
Results showed that the 24-week rate of response was 71% with methylprednisolone plus mycophenolate and 53% with methylprednisolone alone (odds ratio, 2.16; P = .026).
Dr. Kahaly acknowledged that the rate in the monotherapy group was lower than that in some in past studies and proposed this was due to both a tightening of response criteria and more conservative steroid dosing in recent years.
Benefit was similar across patient subgroups stratified by sex, smoking history, clinical activity score, duration of orbitopathy, and level of antibodies to the thyroid-stimulating hormone receptor.
The group given combination therapy also had a lower 36-week relapse rate, although this difference was not significant (4% vs. 8%; odds ratio, 0.65; P = .613). Quality-of-life scores improved in both the monotherapy group (P = .009) and the combination therapy group (P = .002).
The difference between groups in extent of proptosis was just 1 mm. “This is not enough,” he asserted, noting that teprotumumab, an investigational antibody that inhibits insulin-like growth factor I receptor, was recently found to decrease proptosis in this population by 2.7 mm (N Engl J Med. 2017;376:1748-61). “This is the only drug that has led to a significant decrease of proptosis,” he noted.
“The drugs were well tolerated, and the treatment went smoothly. We didn’t have one single dropout because of drug side effects,” Dr. Kahaly reported.
The incidence of drug-related side effects was 20% with methylprednisolone and 25% with methylprednisolone plus mycophenolate, a nonsignificant difference. In both groups, most side effects were rated as mild or moderate.
Trial limitations included the lack of a placebo control, short duration of follow-up, and missing information about subsequent surgical procedures, such as orbital decompression and squint and lid surgery, acknowledged Dr. Kahaly, who disclosed that he had no relevant conflicts of interest.
VICTORIA, B.C. – Adding a nonsteroidal immunosuppressant to steroid therapy improves control of active, moderate-to-severe Graves’ orbitopathy, according to findings from a randomized controlled trial reported at the annual meeting of the American Thyroid Association.
Relative to counterparts given pulsed intravenous methylprednisolone alone, patients also given oral mycophenolate were twice as likely to achieve reduction of their ophthalmic signs and symptoms, first author George J. Kahaly, MD, PhD, reported in a session on behalf of the European Group on Graves’ Orbitopathy (EUGOGO). And the combination was generally safe and well tolerated.

“Since there is a clear advantage of combination treatment in response rate, in the absence of contraindication to mycophenolate, patients with active and severe orbitopathy may be considered for combination treatment,” he proposed.
A session attendee noted that a similar recent study from China suggests that mycophenolate monotherapy achieves a very high remission rate in this patient population (Clin Endocrinol (Oxf). 2017;86[2]:247-55). “Why don’t we just go for [mycophenolate] alone? Why keep pushing steroids?” he asked.
Methodology of that study was less rigorous, maintained Dr. Kahaly, who is professor of medicine and endocrinology/metabolism, chief physician of the endocrine outpatient clinic, and director of the thyroid research lab at Gutenberg University Medical Center in Mainz, Germany.
“I would say mycophenolate alone is not a powerful enough treatment to observe a response rate of 70%, 80%, 90%,” he stated. “You need more time. This is a lymphocyte-inhibiting agent, so you need the acute effect of the intravenous steroids at the beginning.”
Session cochair Angela M. Leung, MD, assistant professor of medicine at the University of California, Los Angeles, and an endocrinologist at both UCLA and the VA Greater Los Angeles Healthcare System, commented, “This is an intriguing study with very promising data from an active group of investigators.”

At the same time, benefit of add-on mycophenolate remains uncertain, in her opinion. “Clearly, more studies, perhaps longer-duration ones, are needed to assess the true effect and clinical efficacy,” she said.
Introducing the EUGOGO trial, Dr. Kahaly noted that European guidelines recommend intravenous methylprednisolone as first-line therapy for Graves’ orbitopathy that is moderate to severe or sight threatening (Eur Thyroid J. 2016;5:9-26). Some patients, however, do not achieve response on this therapy, and others who do achieve response then go on to experience relapse, underscoring the need for better therapies.
The combination the investigators selected pairs the anti-inflammatory activity of methylprednisolone with the antiproliferative activity of mycophenolate (CellCept), which is mainly used in the transplantation field.
The trial, funded in part by Novartis, was open to patients with Graves’ disease who had been euthyroid for at least 2 months but had untreated, active, moderate-to-severe orbitopathy with involvement of soft tissues and eye muscles. Those with optic neuropathy were excluded.
Patients were randomized to 12 weeks of once-weekly intravenous methylprednisolone either alone or with the addition of 24 weeks of twice-daily oral mycophenolate initiated at the same time.
Blinded observers assessed patients for orbitopathy response, defined as improvement in two or more of six outcome measures (eyelid swelling, clinical activity score, proptosis, lid width, diplopia, and motility) in at least one eye, without deterioration in any of the same measures in either eye.
Results showed that the 24-week rate of response was 71% with methylprednisolone plus mycophenolate and 53% with methylprednisolone alone (odds ratio, 2.16; P = .026).
Dr. Kahaly acknowledged that the rate in the monotherapy group was lower than that in some in past studies and proposed this was due to both a tightening of response criteria and more conservative steroid dosing in recent years.
Benefit was similar across patient subgroups stratified by sex, smoking history, clinical activity score, duration of orbitopathy, and level of antibodies to the thyroid-stimulating hormone receptor.
The group given combination therapy also had a lower 36-week relapse rate, although this difference was not significant (4% vs. 8%; odds ratio, 0.65; P = .613). Quality-of-life scores improved in both the monotherapy group (P = .009) and the combination therapy group (P = .002).
The difference between groups in extent of proptosis was just 1 mm. “This is not enough,” he asserted, noting that teprotumumab, an investigational antibody that inhibits insulin-like growth factor I receptor, was recently found to decrease proptosis in this population by 2.7 mm (N Engl J Med. 2017;376:1748-61). “This is the only drug that has led to a significant decrease of proptosis,” he noted.
“The drugs were well tolerated, and the treatment went smoothly. We didn’t have one single dropout because of drug side effects,” Dr. Kahaly reported.
The incidence of drug-related side effects was 20% with methylprednisolone and 25% with methylprednisolone plus mycophenolate, a nonsignificant difference. In both groups, most side effects were rated as mild or moderate.
Trial limitations included the lack of a placebo control, short duration of follow-up, and missing information about subsequent surgical procedures, such as orbital decompression and squint and lid surgery, acknowledged Dr. Kahaly, who disclosed that he had no relevant conflicts of interest.
VICTORIA, B.C. – Adding a nonsteroidal immunosuppressant to steroid therapy improves control of active, moderate-to-severe Graves’ orbitopathy, according to findings from a randomized controlled trial reported at the annual meeting of the American Thyroid Association.
Relative to counterparts given pulsed intravenous methylprednisolone alone, patients also given oral mycophenolate were twice as likely to achieve reduction of their ophthalmic signs and symptoms, first author George J. Kahaly, MD, PhD, reported in a session on behalf of the European Group on Graves’ Orbitopathy (EUGOGO). And the combination was generally safe and well tolerated.

“Since there is a clear advantage of combination treatment in response rate, in the absence of contraindication to mycophenolate, patients with active and severe orbitopathy may be considered for combination treatment,” he proposed.
A session attendee noted that a similar recent study from China suggests that mycophenolate monotherapy achieves a very high remission rate in this patient population (Clin Endocrinol (Oxf). 2017;86[2]:247-55). “Why don’t we just go for [mycophenolate] alone? Why keep pushing steroids?” he asked.
Methodology of that study was less rigorous, maintained Dr. Kahaly, who is professor of medicine and endocrinology/metabolism, chief physician of the endocrine outpatient clinic, and director of the thyroid research lab at Gutenberg University Medical Center in Mainz, Germany.
“I would say mycophenolate alone is not a powerful enough treatment to observe a response rate of 70%, 80%, 90%,” he stated. “You need more time. This is a lymphocyte-inhibiting agent, so you need the acute effect of the intravenous steroids at the beginning.”
Session cochair Angela M. Leung, MD, assistant professor of medicine at the University of California, Los Angeles, and an endocrinologist at both UCLA and the VA Greater Los Angeles Healthcare System, commented, “This is an intriguing study with very promising data from an active group of investigators.”

At the same time, benefit of add-on mycophenolate remains uncertain, in her opinion. “Clearly, more studies, perhaps longer-duration ones, are needed to assess the true effect and clinical efficacy,” she said.
Introducing the EUGOGO trial, Dr. Kahaly noted that European guidelines recommend intravenous methylprednisolone as first-line therapy for Graves’ orbitopathy that is moderate to severe or sight threatening (Eur Thyroid J. 2016;5:9-26). Some patients, however, do not achieve response on this therapy, and others who do achieve response then go on to experience relapse, underscoring the need for better therapies.
The combination the investigators selected pairs the anti-inflammatory activity of methylprednisolone with the antiproliferative activity of mycophenolate (CellCept), which is mainly used in the transplantation field.
The trial, funded in part by Novartis, was open to patients with Graves’ disease who had been euthyroid for at least 2 months but had untreated, active, moderate-to-severe orbitopathy with involvement of soft tissues and eye muscles. Those with optic neuropathy were excluded.
Patients were randomized to 12 weeks of once-weekly intravenous methylprednisolone either alone or with the addition of 24 weeks of twice-daily oral mycophenolate initiated at the same time.
Blinded observers assessed patients for orbitopathy response, defined as improvement in two or more of six outcome measures (eyelid swelling, clinical activity score, proptosis, lid width, diplopia, and motility) in at least one eye, without deterioration in any of the same measures in either eye.
Results showed that the 24-week rate of response was 71% with methylprednisolone plus mycophenolate and 53% with methylprednisolone alone (odds ratio, 2.16; P = .026).
Dr. Kahaly acknowledged that the rate in the monotherapy group was lower than that in some in past studies and proposed this was due to both a tightening of response criteria and more conservative steroid dosing in recent years.
Benefit was similar across patient subgroups stratified by sex, smoking history, clinical activity score, duration of orbitopathy, and level of antibodies to the thyroid-stimulating hormone receptor.
The group given combination therapy also had a lower 36-week relapse rate, although this difference was not significant (4% vs. 8%; odds ratio, 0.65; P = .613). Quality-of-life scores improved in both the monotherapy group (P = .009) and the combination therapy group (P = .002).
The difference between groups in extent of proptosis was just 1 mm. “This is not enough,” he asserted, noting that teprotumumab, an investigational antibody that inhibits insulin-like growth factor I receptor, was recently found to decrease proptosis in this population by 2.7 mm (N Engl J Med. 2017;376:1748-61). “This is the only drug that has led to a significant decrease of proptosis,” he noted.
“The drugs were well tolerated, and the treatment went smoothly. We didn’t have one single dropout because of drug side effects,” Dr. Kahaly reported.
The incidence of drug-related side effects was 20% with methylprednisolone and 25% with methylprednisolone plus mycophenolate, a nonsignificant difference. In both groups, most side effects were rated as mild or moderate.
Trial limitations included the lack of a placebo control, short duration of follow-up, and missing information about subsequent surgical procedures, such as orbital decompression and squint and lid surgery, acknowledged Dr. Kahaly, who disclosed that he had no relevant conflicts of interest.
AT ATA 2017
Key clinical point:
Major finding: Relative to peers given methylprednisolone alone, patients given methylprednisolone plus mycophenolate were twice as likely to achieve response (odds ratio, 2.16).
Data source: A multicenter randomized controlled trial in 164 patients with Graves’ disease who had active, moderate-to-severe orbitopathy.
Disclosures: Dr. Kahaly disclosed that he had no relevant conflicts of interest. The trial was partly funded by Novartis.
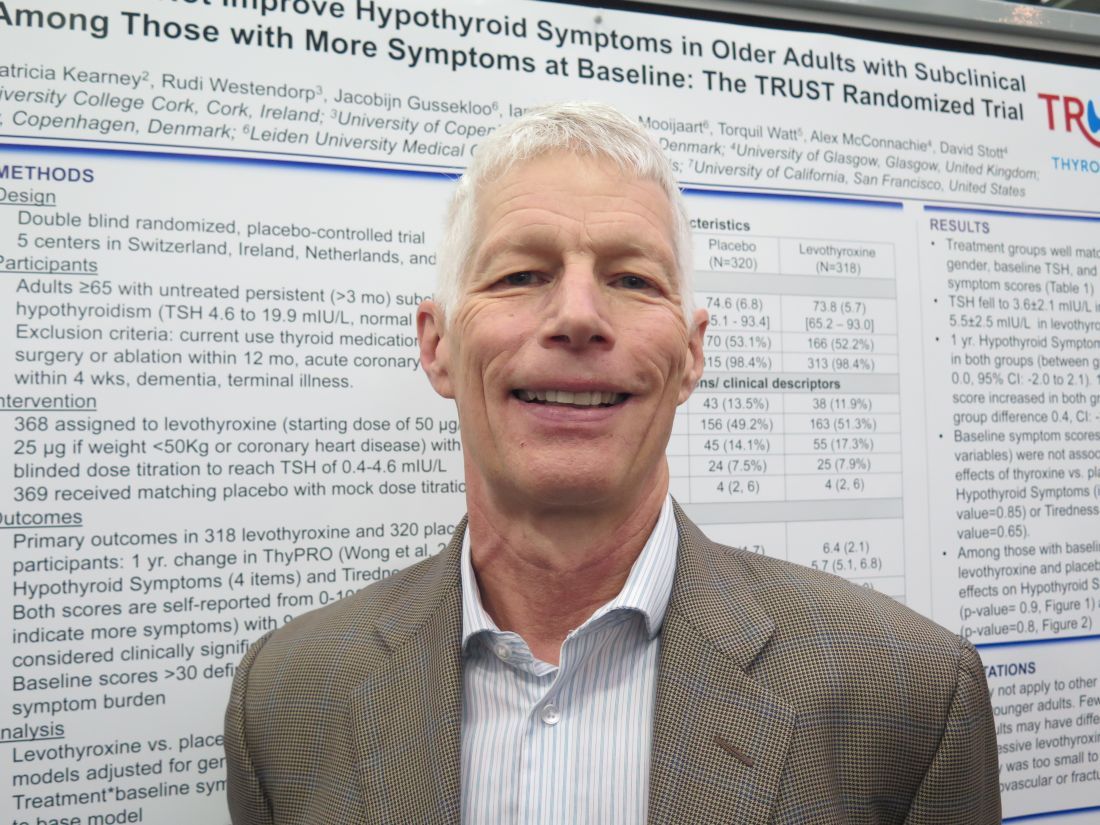
Symptoms fail to predict benefit of hormone therapy in older adults with subclinical hypothyroidism
VICTORIA, B.C. – , according to findings from a study reported at the annual meeting of the American Thyroid Association.
“In the U.S., individuals are frequently treated either for just a number – just because their thyroid-stimulating hormone (TSH) is elevated – or for nonspecific hypothyroid-type symptoms, such as weight gain, cold intolerance, and such. It’s extremely common,” lead investigator Douglas Bauer, MD, professor and internist at the University of California, San Francisco, commented in an interview.
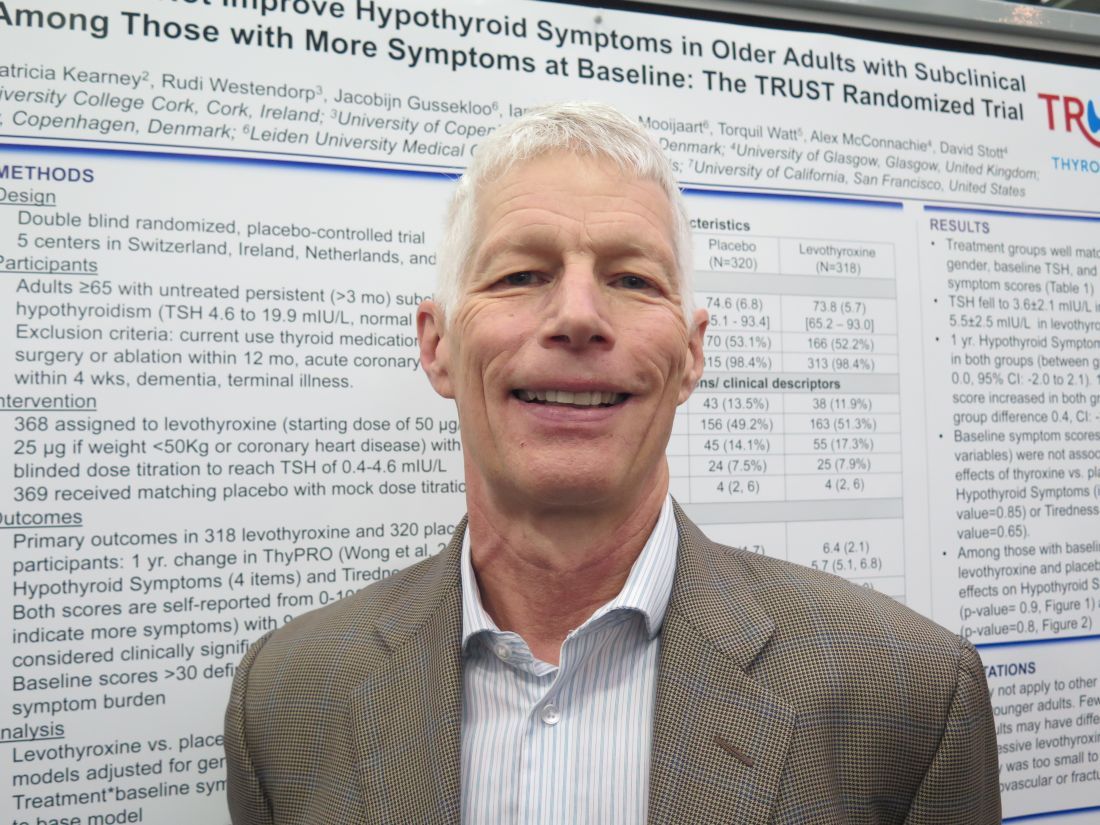
“On average, this study suggests that you shouldn’t be using hypothyroid-type symptomatology to treat subclinical hypothyroidism,” he said, while also acknowledging that not writing that prescription can be challenging. “It’s hard to do nothing, I know.”
Dr. Bauer and his coinvestigators performed a subgroup analysis of the randomized controlled TRUST trial (Thyroid Hormone Replacement for Subclinical Hypothyroidism), conducted in Switzerland, Ireland, the Netherlands, and the United Kingdom. In the trial, 737 adults aged 65 years or older with persistent subclinical hypothyroidism (TSH level, 4.60-19.99 mIU/L, with normal free thyroxine level) were given either levothyroxine or placebo on a double-blind basis.
Results for the entire trial population, previously reported, showed that at 1 year, patient-reported symptoms on a thyroid-specific quality-of-life questionnaire had improved by a similar extent in both groups, with no significant differences between them (N Engl J Med. 2017;376:2534-44).
The new analysis focused on two subgroups that might be especially expected to benefit: 132 patients with a hypothyroid symptoms score greater than 30 on a 100-point scale and 209 patients with a tiredness score greater than 30 on a 100-point scale.
Results reported in a poster session showed that at 1 year, scores had improved by about 10 points with levothyroxine and placebo alike, with no significant difference, in both the group with higher hypothyroid symptoms scores (P = .90) and the group with higher tiredness scores (P = .80).
“This provides additional evidence that it’s unlikely that the treatment of subclinical hypothyroidism, at least in this population, is going to lead to symptomatic improvement,” Dr. Bauer commented.
“I would speculate that we’ve overestimated the benefit [of thyroid hormone therapy] on symptoms based on the fact that previous studies haven’t been blinded,” he said, noting that the TRUST trial used a rigorous blinding protocol, even going so far as to change the appearance of placebo pills to convince patients in the placebo group that their dose was being titrated.
A potential criticism is that the treatment was not aggressive enough, with patients in the levothyroxine group achieving a mean TSH level of 3.6 mIU/L, according to Dr. Bauer. “I think many people treating with thyroxine would like to see this TSH fall into the 2 mIU/L to 3 mIU/L range,” he acknowledged.
Taken together, the trial’s overall and subgroup findings do not rule out potential benefit for certain patients, he cautioned. For example, patients with very high symptom burden and patients with baseline TSH levels greater than 10 mIU/L were too few for separate analysis, and younger adults were not included at all.
Additionally, treatment impact on other important clinical outcomes – cardiovascular events and fractures – could not be assessed in TRUST because of insufficient enrollment.
Dr. Bauer disclosed that he had no relevant conflicts of interest. The trial was funded by the European Union, Swiss National Science Foundation, Swiss Heart Foundation, and Velux Stiftung. Merck supplied study drug.
VICTORIA, B.C. – , according to findings from a study reported at the annual meeting of the American Thyroid Association.
“In the U.S., individuals are frequently treated either for just a number – just because their thyroid-stimulating hormone (TSH) is elevated – or for nonspecific hypothyroid-type symptoms, such as weight gain, cold intolerance, and such. It’s extremely common,” lead investigator Douglas Bauer, MD, professor and internist at the University of California, San Francisco, commented in an interview.
“On average, this study suggests that you shouldn’t be using hypothyroid-type symptomatology to treat subclinical hypothyroidism,” he said, while also acknowledging that not writing that prescription can be challenging. “It’s hard to do nothing, I know.”
Dr. Bauer and his coinvestigators performed a subgroup analysis of the randomized controlled TRUST trial (Thyroid Hormone Replacement for Subclinical Hypothyroidism), conducted in Switzerland, Ireland, the Netherlands, and the United Kingdom. In the trial, 737 adults aged 65 years or older with persistent subclinical hypothyroidism (TSH level, 4.60-19.99 mIU/L, with normal free thyroxine level) were given either levothyroxine or placebo on a double-blind basis.
Results for the entire trial population, previously reported, showed that at 1 year, patient-reported symptoms on a thyroid-specific quality-of-life questionnaire had improved by a similar extent in both groups, with no significant differences between them (N Engl J Med. 2017;376:2534-44).
The new analysis focused on two subgroups that might be especially expected to benefit: 132 patients with a hypothyroid symptoms score greater than 30 on a 100-point scale and 209 patients with a tiredness score greater than 30 on a 100-point scale.
Results reported in a poster session showed that at 1 year, scores had improved by about 10 points with levothyroxine and placebo alike, with no significant difference, in both the group with higher hypothyroid symptoms scores (P = .90) and the group with higher tiredness scores (P = .80).
“This provides additional evidence that it’s unlikely that the treatment of subclinical hypothyroidism, at least in this population, is going to lead to symptomatic improvement,” Dr. Bauer commented.
“I would speculate that we’ve overestimated the benefit [of thyroid hormone therapy] on symptoms based on the fact that previous studies haven’t been blinded,” he said, noting that the TRUST trial used a rigorous blinding protocol, even going so far as to change the appearance of placebo pills to convince patients in the placebo group that their dose was being titrated.
A potential criticism is that the treatment was not aggressive enough, with patients in the levothyroxine group achieving a mean TSH level of 3.6 mIU/L, according to Dr. Bauer. “I think many people treating with thyroxine would like to see this TSH fall into the 2 mIU/L to 3 mIU/L range,” he acknowledged.
Taken together, the trial’s overall and subgroup findings do not rule out potential benefit for certain patients, he cautioned. For example, patients with very high symptom burden and patients with baseline TSH levels greater than 10 mIU/L were too few for separate analysis, and younger adults were not included at all.
Additionally, treatment impact on other important clinical outcomes – cardiovascular events and fractures – could not be assessed in TRUST because of insufficient enrollment.
Dr. Bauer disclosed that he had no relevant conflicts of interest. The trial was funded by the European Union, Swiss National Science Foundation, Swiss Heart Foundation, and Velux Stiftung. Merck supplied study drug.
VICTORIA, B.C. – , according to findings from a study reported at the annual meeting of the American Thyroid Association.
“In the U.S., individuals are frequently treated either for just a number – just because their thyroid-stimulating hormone (TSH) is elevated – or for nonspecific hypothyroid-type symptoms, such as weight gain, cold intolerance, and such. It’s extremely common,” lead investigator Douglas Bauer, MD, professor and internist at the University of California, San Francisco, commented in an interview.
“On average, this study suggests that you shouldn’t be using hypothyroid-type symptomatology to treat subclinical hypothyroidism,” he said, while also acknowledging that not writing that prescription can be challenging. “It’s hard to do nothing, I know.”
Dr. Bauer and his coinvestigators performed a subgroup analysis of the randomized controlled TRUST trial (Thyroid Hormone Replacement for Subclinical Hypothyroidism), conducted in Switzerland, Ireland, the Netherlands, and the United Kingdom. In the trial, 737 adults aged 65 years or older with persistent subclinical hypothyroidism (TSH level, 4.60-19.99 mIU/L, with normal free thyroxine level) were given either levothyroxine or placebo on a double-blind basis.
Results for the entire trial population, previously reported, showed that at 1 year, patient-reported symptoms on a thyroid-specific quality-of-life questionnaire had improved by a similar extent in both groups, with no significant differences between them (N Engl J Med. 2017;376:2534-44).
The new analysis focused on two subgroups that might be especially expected to benefit: 132 patients with a hypothyroid symptoms score greater than 30 on a 100-point scale and 209 patients with a tiredness score greater than 30 on a 100-point scale.
Results reported in a poster session showed that at 1 year, scores had improved by about 10 points with levothyroxine and placebo alike, with no significant difference, in both the group with higher hypothyroid symptoms scores (P = .90) and the group with higher tiredness scores (P = .80).
“This provides additional evidence that it’s unlikely that the treatment of subclinical hypothyroidism, at least in this population, is going to lead to symptomatic improvement,” Dr. Bauer commented.
“I would speculate that we’ve overestimated the benefit [of thyroid hormone therapy] on symptoms based on the fact that previous studies haven’t been blinded,” he said, noting that the TRUST trial used a rigorous blinding protocol, even going so far as to change the appearance of placebo pills to convince patients in the placebo group that their dose was being titrated.
A potential criticism is that the treatment was not aggressive enough, with patients in the levothyroxine group achieving a mean TSH level of 3.6 mIU/L, according to Dr. Bauer. “I think many people treating with thyroxine would like to see this TSH fall into the 2 mIU/L to 3 mIU/L range,” he acknowledged.
Taken together, the trial’s overall and subgroup findings do not rule out potential benefit for certain patients, he cautioned. For example, patients with very high symptom burden and patients with baseline TSH levels greater than 10 mIU/L were too few for separate analysis, and younger adults were not included at all.
Additionally, treatment impact on other important clinical outcomes – cardiovascular events and fractures – could not be assessed in TRUST because of insufficient enrollment.
Dr. Bauer disclosed that he had no relevant conflicts of interest. The trial was funded by the European Union, Swiss National Science Foundation, Swiss Heart Foundation, and Velux Stiftung. Merck supplied study drug.
AT ATA 2017
Key clinical point: Hypothyroid-type symptoms do not predict treatment benefit in older adults with subclinical hypothyroidism.
Major finding: Patients had statistically indistinguishable improvements at 1 year in hypothyroid symptoms scores (P = .90) and Tiredness scores (P = .80) whether given levothyroxine or placebo.
Data source: A subgroup analysis of older adults with subclinical hypothyroidism having higher baseline levels of overall hypothyroid symptoms (n = 132) or tiredness (n = 209) (TRUST trial).
Disclosures: Dr. Bauer disclosed that he had no relevant conflicts of interest. The trial was funded by the European Union, Swiss National Science Foundation, Swiss Heart Foundation, and Velux Stiftung. Merck supplied study drug.
Too few RA patients get timely adjustment of DMARDs
Adjustment of disease-modifying antirheumatic drug (DMARD) therapy is not happening quickly enough for a substantial minority of rheumatoid arthritis patients with moderate to high disease activity, according to the findings of a registry study that is the first to evaluate this association.
Investigators led by Yomei Shaw, PhD, a research fellow with the National Data Bank for Rheumatic Diseases, retrospectively analyzed data from 538 patients in the university’s Rheumatoid Arthritis Comparative Effectiveness Research (RACER) registry who had moderate to high disease activity. Dr. Shaw conducted the study as a doctoral student in the department of health policy and management at the University of Pittsburgh.
In 40% of patients who had persistent disease activity of this severity, clinicians waited more than the 90 days recommended by treat-to-target (T2T) guidelines to adjust DMARDs, according to published results (Arthritis Care Res. 2017 Sep 21. doi: 10.1002/acr.23418). Such delay was more common for certain groups, including those on biologics and those who had rheumatoid arthritis (RA) for longer.
Compared with peers whose therapy was adjusted sooner, patients with such delayed adjustment were about one-quarter less likely to achieve low disease activity or remission during follow-up.
“The results of our survival analyses suggest that delays in DMARD adjustment of more than 3 months are common among RA patients with [moderate to high disease activity], highlighting an important potential gap in quality of care for these patients,” Dr. Shaw and her colleagues wrote.
They acknowledge that some of the delays in adjustment may have been unavoidable. For example, patients on biologic DMARDs may have needed insurance approval to start a new biologic, and patients with long-standing disease may have had fewer options remaining or symptoms that clinicians attributed to irreversible joint damage.
The study’s findings provide additional evidence of the importance of timely, guideline-adherent DMARD adjustment in reducing the amount of time patients spend in moderate to high disease activity, the investigators further contend.
“Promoting T2T in clinical practice requires coordinated change at the system, rheumatology practice, and individual levels,” such as consistently documenting the treatment target, assessing disease activity at every visit, and mandating a minimum visit frequency, they conclude.
Dr. Shaw and her colleagues studied patients having moderate to high disease activity, defined according to the 28-joint Disease Activity Score with C-reactive protein criteria (score of greater than 3.2).
The investigators reported a median time to adjustment of DMARD therapy of 154 days during 943.5 patient-years of follow-up. These adjustments could be adding, switching, or increasing the dose of a DMARD medication (excluding corticosteroids).
In multivariate analysis, patients had a longer time to DMARD adjustment if they were aged 75 years or older (subdistribution hazard ratio, 0.61; P = .02), had lower baseline disease activity (0.72; P less than .01), had longer duration of rheumatoid arthritis (0.98; P less than .01), or were receiving a biologic DMARD at baseline (0.71; P less than .01).
The median time to achieving low disease activity or remission was 301 days for the entire cohort. Patients had a longer time to achieve this goal if their DMARD therapy was not adjusted within 90 days (hazard ratio, 0.76; P = .01) or if they were African American (0.63; P = .01) or had higher baseline disease activity (0.75; P less than .01). They had a shorter time if they had better mental health (1.01; P = .03) or physical health (1.01; P = .02) as assessed with the 12-item Short Form Health Survey.
One of the study authors received research funding from Genentech and is currently employed by AbbVie. The registry used was funded by the National Institutes of Health and Genentech.
Randomized controlled trials demonstrate that statin lipid–lowering drugs reduce repeat cardiovascular events. Based on this evidence, clinicians agree that the vast majority of patients should receive statin lipid-lowering drugs after a CV event, and that providers not prescribing statins to these patients are providing suboptimal care.
By analogy, the data provided in this new analysis by Shaw and her colleagues suggests that many rheumatologists are providing suboptimal care. Many randomized, controlled trials testing a treat-to-target (T2T) paradigm demonstrate the clinical benefits of changing treatments for patients with rheumatoid arthritis who are in moderate or high disease activity. Yet, this analysis found many patients do not change treatments despite poor disease control. While the current study does not examine the reasons for suboptimal care, some correlates include:
• Patient preference to not change treatment;
• Provider desire to give treatments more time to work; and
• Health system issues such as drug payment complexities.
Continuing medical education may be necessary, but it is not a sufficient lever to push providers to implement T2T. Audit and feedback – providing individual providers with their performance metrics – alerts rheumatic disease providers when improvement is necessary. Yet, most providers need specific strategies within their practice to implement T2T. Collaborative learning between providers with a common purpose and coaches that understand the complexities of implementing T2T have been shown in the recently published TRACTION trial to produce improvements (Arthritis Rheumatol. 2017;69[7]:1374-80). The article by Shaw and her colleagues should sound the alarm to rheumatic disease providers: Care for RA needs improving if we want to produce optimal outcomes.
Daniel H. Solomon, MD, is a professor of medicine at Harvard University, and chief of the section of clinical sciences in the division of rheumatology at Brigham and Women’s Hospital, both in Boston. He has no relevant disclosures.
Randomized controlled trials demonstrate that statin lipid–lowering drugs reduce repeat cardiovascular events. Based on this evidence, clinicians agree that the vast majority of patients should receive statin lipid-lowering drugs after a CV event, and that providers not prescribing statins to these patients are providing suboptimal care.
By analogy, the data provided in this new analysis by Shaw and her colleagues suggests that many rheumatologists are providing suboptimal care. Many randomized, controlled trials testing a treat-to-target (T2T) paradigm demonstrate the clinical benefits of changing treatments for patients with rheumatoid arthritis who are in moderate or high disease activity. Yet, this analysis found many patients do not change treatments despite poor disease control. While the current study does not examine the reasons for suboptimal care, some correlates include:
• Patient preference to not change treatment;
• Provider desire to give treatments more time to work; and
• Health system issues such as drug payment complexities.
Continuing medical education may be necessary, but it is not a sufficient lever to push providers to implement T2T. Audit and feedback – providing individual providers with their performance metrics – alerts rheumatic disease providers when improvement is necessary. Yet, most providers need specific strategies within their practice to implement T2T. Collaborative learning between providers with a common purpose and coaches that understand the complexities of implementing T2T have been shown in the recently published TRACTION trial to produce improvements (Arthritis Rheumatol. 2017;69[7]:1374-80). The article by Shaw and her colleagues should sound the alarm to rheumatic disease providers: Care for RA needs improving if we want to produce optimal outcomes.
Daniel H. Solomon, MD, is a professor of medicine at Harvard University, and chief of the section of clinical sciences in the division of rheumatology at Brigham and Women’s Hospital, both in Boston. He has no relevant disclosures.
Randomized controlled trials demonstrate that statin lipid–lowering drugs reduce repeat cardiovascular events. Based on this evidence, clinicians agree that the vast majority of patients should receive statin lipid-lowering drugs after a CV event, and that providers not prescribing statins to these patients are providing suboptimal care.
By analogy, the data provided in this new analysis by Shaw and her colleagues suggests that many rheumatologists are providing suboptimal care. Many randomized, controlled trials testing a treat-to-target (T2T) paradigm demonstrate the clinical benefits of changing treatments for patients with rheumatoid arthritis who are in moderate or high disease activity. Yet, this analysis found many patients do not change treatments despite poor disease control. While the current study does not examine the reasons for suboptimal care, some correlates include:
• Patient preference to not change treatment;
• Provider desire to give treatments more time to work; and
• Health system issues such as drug payment complexities.
Continuing medical education may be necessary, but it is not a sufficient lever to push providers to implement T2T. Audit and feedback – providing individual providers with their performance metrics – alerts rheumatic disease providers when improvement is necessary. Yet, most providers need specific strategies within their practice to implement T2T. Collaborative learning between providers with a common purpose and coaches that understand the complexities of implementing T2T have been shown in the recently published TRACTION trial to produce improvements (Arthritis Rheumatol. 2017;69[7]:1374-80). The article by Shaw and her colleagues should sound the alarm to rheumatic disease providers: Care for RA needs improving if we want to produce optimal outcomes.
Daniel H. Solomon, MD, is a professor of medicine at Harvard University, and chief of the section of clinical sciences in the division of rheumatology at Brigham and Women’s Hospital, both in Boston. He has no relevant disclosures.
Adjustment of disease-modifying antirheumatic drug (DMARD) therapy is not happening quickly enough for a substantial minority of rheumatoid arthritis patients with moderate to high disease activity, according to the findings of a registry study that is the first to evaluate this association.
Investigators led by Yomei Shaw, PhD, a research fellow with the National Data Bank for Rheumatic Diseases, retrospectively analyzed data from 538 patients in the university’s Rheumatoid Arthritis Comparative Effectiveness Research (RACER) registry who had moderate to high disease activity. Dr. Shaw conducted the study as a doctoral student in the department of health policy and management at the University of Pittsburgh.
In 40% of patients who had persistent disease activity of this severity, clinicians waited more than the 90 days recommended by treat-to-target (T2T) guidelines to adjust DMARDs, according to published results (Arthritis Care Res. 2017 Sep 21. doi: 10.1002/acr.23418). Such delay was more common for certain groups, including those on biologics and those who had rheumatoid arthritis (RA) for longer.
Compared with peers whose therapy was adjusted sooner, patients with such delayed adjustment were about one-quarter less likely to achieve low disease activity or remission during follow-up.
“The results of our survival analyses suggest that delays in DMARD adjustment of more than 3 months are common among RA patients with [moderate to high disease activity], highlighting an important potential gap in quality of care for these patients,” Dr. Shaw and her colleagues wrote.
They acknowledge that some of the delays in adjustment may have been unavoidable. For example, patients on biologic DMARDs may have needed insurance approval to start a new biologic, and patients with long-standing disease may have had fewer options remaining or symptoms that clinicians attributed to irreversible joint damage.
The study’s findings provide additional evidence of the importance of timely, guideline-adherent DMARD adjustment in reducing the amount of time patients spend in moderate to high disease activity, the investigators further contend.
“Promoting T2T in clinical practice requires coordinated change at the system, rheumatology practice, and individual levels,” such as consistently documenting the treatment target, assessing disease activity at every visit, and mandating a minimum visit frequency, they conclude.
Dr. Shaw and her colleagues studied patients having moderate to high disease activity, defined according to the 28-joint Disease Activity Score with C-reactive protein criteria (score of greater than 3.2).
The investigators reported a median time to adjustment of DMARD therapy of 154 days during 943.5 patient-years of follow-up. These adjustments could be adding, switching, or increasing the dose of a DMARD medication (excluding corticosteroids).
In multivariate analysis, patients had a longer time to DMARD adjustment if they were aged 75 years or older (subdistribution hazard ratio, 0.61; P = .02), had lower baseline disease activity (0.72; P less than .01), had longer duration of rheumatoid arthritis (0.98; P less than .01), or were receiving a biologic DMARD at baseline (0.71; P less than .01).
The median time to achieving low disease activity or remission was 301 days for the entire cohort. Patients had a longer time to achieve this goal if their DMARD therapy was not adjusted within 90 days (hazard ratio, 0.76; P = .01) or if they were African American (0.63; P = .01) or had higher baseline disease activity (0.75; P less than .01). They had a shorter time if they had better mental health (1.01; P = .03) or physical health (1.01; P = .02) as assessed with the 12-item Short Form Health Survey.
One of the study authors received research funding from Genentech and is currently employed by AbbVie. The registry used was funded by the National Institutes of Health and Genentech.
Adjustment of disease-modifying antirheumatic drug (DMARD) therapy is not happening quickly enough for a substantial minority of rheumatoid arthritis patients with moderate to high disease activity, according to the findings of a registry study that is the first to evaluate this association.
Investigators led by Yomei Shaw, PhD, a research fellow with the National Data Bank for Rheumatic Diseases, retrospectively analyzed data from 538 patients in the university’s Rheumatoid Arthritis Comparative Effectiveness Research (RACER) registry who had moderate to high disease activity. Dr. Shaw conducted the study as a doctoral student in the department of health policy and management at the University of Pittsburgh.
In 40% of patients who had persistent disease activity of this severity, clinicians waited more than the 90 days recommended by treat-to-target (T2T) guidelines to adjust DMARDs, according to published results (Arthritis Care Res. 2017 Sep 21. doi: 10.1002/acr.23418). Such delay was more common for certain groups, including those on biologics and those who had rheumatoid arthritis (RA) for longer.
Compared with peers whose therapy was adjusted sooner, patients with such delayed adjustment were about one-quarter less likely to achieve low disease activity or remission during follow-up.
“The results of our survival analyses suggest that delays in DMARD adjustment of more than 3 months are common among RA patients with [moderate to high disease activity], highlighting an important potential gap in quality of care for these patients,” Dr. Shaw and her colleagues wrote.
They acknowledge that some of the delays in adjustment may have been unavoidable. For example, patients on biologic DMARDs may have needed insurance approval to start a new biologic, and patients with long-standing disease may have had fewer options remaining or symptoms that clinicians attributed to irreversible joint damage.
The study’s findings provide additional evidence of the importance of timely, guideline-adherent DMARD adjustment in reducing the amount of time patients spend in moderate to high disease activity, the investigators further contend.
“Promoting T2T in clinical practice requires coordinated change at the system, rheumatology practice, and individual levels,” such as consistently documenting the treatment target, assessing disease activity at every visit, and mandating a minimum visit frequency, they conclude.
Dr. Shaw and her colleagues studied patients having moderate to high disease activity, defined according to the 28-joint Disease Activity Score with C-reactive protein criteria (score of greater than 3.2).
The investigators reported a median time to adjustment of DMARD therapy of 154 days during 943.5 patient-years of follow-up. These adjustments could be adding, switching, or increasing the dose of a DMARD medication (excluding corticosteroids).
In multivariate analysis, patients had a longer time to DMARD adjustment if they were aged 75 years or older (subdistribution hazard ratio, 0.61; P = .02), had lower baseline disease activity (0.72; P less than .01), had longer duration of rheumatoid arthritis (0.98; P less than .01), or were receiving a biologic DMARD at baseline (0.71; P less than .01).
The median time to achieving low disease activity or remission was 301 days for the entire cohort. Patients had a longer time to achieve this goal if their DMARD therapy was not adjusted within 90 days (hazard ratio, 0.76; P = .01) or if they were African American (0.63; P = .01) or had higher baseline disease activity (0.75; P less than .01). They had a shorter time if they had better mental health (1.01; P = .03) or physical health (1.01; P = .02) as assessed with the 12-item Short Form Health Survey.
One of the study authors received research funding from Genentech and is currently employed by AbbVie. The registry used was funded by the National Institutes of Health and Genentech.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: In 40% of patients who had persistent disease activity of this severity, clinicians waited more than the 90 days recommended by treat-to-target guidelines to adjust DMARDs.
Data source: A retrospective cohort study of 538 patients with RA having moderate to high disease activity.
Disclosures: One of the study authors received research funding from Genentech and is currently employed by AbbVie. The study registry used was funded by the National Institutes of Health and Genentech.
‘Making a difference in cancer care’
Survival improves when patients with cancer self-report symptoms
Key clinical point Patients with metastatic cancer who self-reported symptoms experienced significant improvement in overall survival. Major finding Median overall survival with self-reporting of symptoms compared with usual care was 31.2 and 26 months, respectively. Data source A randomized controlled clinical trial of 766 patients. Funding and disclosures This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr Basch and Dr Burstein each reported having no disclosures.
Patients with metastatic cancer who self-reported symptoms during routine cancer treatment experienced a number of benefits, including a statistically significant improvement in overall survival, according to findings from a randomized, controlled clinical trial (see p. e184). The median overall survival in 441 patients receiving treatment for metastatic breast, lung, genitourinary, or gynecologic cancer who were randomized to the self-reporting intervention arm was more than 5 months longer (a nearly 20% increase) than in 325 patients receiving standard care (31.2 vs. 26 months), Ethan Basch, MD, of the Lineberger Comprehensive Cancer Center at the University of North Carolina, Chapel Hill, said at the meeting. “Another way to think of this is [in terms of] 5-year survival. At 5 years, 8% more patients were alive in the self-reporting group,” he said.
In addition, 31% of patients in the intervention arm had better quality of life/physical functioning, compared with those in the control arm, and 7% fewer patients in the intervention arm visited an emergency room during the study. The duration of potentially life-prolonging chemotherapy was increased by an average of 2 months in the intervention arm, he said (JAMA. 2017 Jun 4. doi: 10.1001/jama.2017.7156).
Symptoms such as nausea, pain, and fatigue are common among patients with metastatic cancer and can often go undetected by doctors and nurses until they become severe and physically debilitating, Dr Basch added, noting that patients are often hesitant to call the office between visits to report symptoms.
Dr Basch and his colleagues hypothesized that self-reporting of patient symptoms between visits or before a visit while the patient was in the clinic waiting area would prompt earlier intervention and improve symptom control and outcomes.
Study participants were patients at Memorial Sloan Kettering Cancer Center who had advanced solid genitourinary, gynecologic, breast, or lung tumors and who were receiving outpatient chemotherapy. Those assigned to the intervention group used tablet computers and an online web survey system to report on 12 symptoms commonly experienced during chemotherapy. The system triggers an alert to a nurse when a severe or worsening symptom is reported. Patients in the usual care group discussed symptoms during office visits and were encouraged to call the office between visits if they were concerned about symptoms.
Patients remained on the study until discontinuation of all cancer treatment, hospice, or death.
One possible explanation for the findings is that this self-reporting approach prompts clinicians to manage symptoms before they cause serious downstream complications, Dr Basch said.
The approach may also keep patients more physically functional, which is known from previous studies to have a strong association with better survival, and it may also improve management of chemotherapy side effects, enabling longer duration of beneficial cancer treatment. “In oncology, we often are limited in our ability to give life-prolonging treatment because people don’t tolerate it well,” Dr Basch explained.
“This approach should be considered for inclusion in standard symptoms management as a component of high-quality cancer care,” he concluded, noting that efforts are underway to test the next generation of systems to improve communication between patients and care teams and to figure out how best to integrate these tools into oncology practice.
The system used in the this study was designed for research, but a number of companies have tools currently available for patient-reported outcomes, and others are being developed, Dr Basch said. A National Cancer Institute questionnaire, the PRO-CTCAE, is publicly available and can be loaded into patients’ electronic health records for this purpose as well.
Harold J Burstein, MD, of Dana-Farber Cancer Institute, Boston, said the study findings validate the feeling among many clinicians that patient-focused, team-based care can improve outcomes in a meaningful way for patients. If this were a drug … it would be worth tens, if not hundreds of thousands, of dollars per year … We don’t have those same kinds of dollars to help implement these into our electronic health records or our systems. We need to find ways to support that and make it happen,” he said.
— Sharon Worcester
TRK inhibitor shows ‘striking’ activity and durability across diverse cancers
Key clinical point Larotrectinib has good, durable efficacy when used to treat advanced cancers harboring TRK fusions. Major finding The overall response rate was 76%, and 79% of responses were still ongoing at 12 months. Data source An integrated analysis of phase 1 and 2 trials among 55 children and adults having 17 discrete types of advanced cancer with TRK fusions. Funding and disclosures Loxo Oncology funded the study. Dr Hyman disclosed that he has a consulting or advisory role with Atara Biotherapeutics, Chugai Pharma, and CytomX Therapeutics, and that he receives research funding from AstraZeneca and Puma Biotechnology.
Larotrectinib, an oral inhibitor of tropomyosin receptor kinase (TRK), has durable efficacy across diverse adult and pediatric cancers that harbor a genetic aberration known as TRK fusion, according to findings from an analysis of 3 trials reported at the meeting (see p. e184). Fusion of a TRK gene with an unrelated gene leads to uncontrolled signaling in the TRK pathway, potentially causing tumor growth and addiction to this input, David Hyman, MD, chief of early drug development at Memorial Sloan Kettering Cancer Center in New York, explained in a press briefing.
“One of the defining features of TRK fusions is that they are not just found in one cancer type, but in dozens of different cancer types, and not just in adults, but children as well, spanning the entire lifetime of the person,” he noted. They are rare in common cancers and nearly universal in certain uncommon cancers; collectively, they are present in possibly 5,000 cancers diagnosed each year in the United States.
Dr Hyman and his colleagues analyzed data from 55 patients having 17 discrete types of advanced cancer harboring TRK fusions who were treated with larotrectinib in phase 1 and 2 trials. Results showed an overall response rate of 76%, and the majority of responses were still ongoing at 12 months. “I believe these data support larotrectinib as a potential new standard of care for these patients,” he said. “However, I want to emphasize that really recognizing this benefit in the community will require that we test patients more universally for the presence of TRK fusions or other tumor-agnostic biomarkers, such as microsatellite instability.”
Study details
The investigators analyzed data from 3 trials in which patients with advanced TRK fusion-positive solid cancers received larotrectinib (LOXO-101): a phase 1 trial among 8 adult patients, a phase 1/2 trial among 12 pediatric patients (SCOUT), and a phase 2 “basket” trial among 35 adult and adolescent patients (NAVIGATE).
“These patients were identified by local testing,” Dr Hyman noted. “We did not perform central screening to find the TRK fusions, and in fact, 50 different laboratories identified the 55 patients. So in a sense, this really represents the real-world identification of these patients.”
In an integrated analysis, the overall rate of confirmed response as assessed by investigators was 76%, with complete response in 12% of patients and partial response in 64%. Two patients had such deep tumor regression that they experienced downstaging enabling them to undergo potentially curative surgery. Efficacy was consistent regardless of tumor type, which TRK gene was affected, and the fusion partner gene.
Median time to response was 1.8 months. “This is just a reflection of when the first scan was obtained. But in the clinic, patients reported dramatic improvement of their symptoms within days of starting therapy,” Dr Hyman said.
With a median follow-up of 5.8 months, the median duration of response was not yet reached. In all, 79% of responses were still ongoing at 12 months. Median progression-free survival (PFS) was likewise not reached; the 12-month rate was 63%.
The leading treatment-emergent adverse events were fatigue (38%), dizziness (27%), nausea (26%), and anemia (26%). “This is an extremely well tolerated therapy with only 13% of patients requiring any form of dose modification and not a single patient discontinuing due to adverse events,” he said.
It is not clear why some patients had apparent primary resistance to larotrectinib, but their TRK fusion test results may have been incorrect, Dr Hyman speculated. In all, 6 patients developed acquired resistance to larotrectinib; 5 of them were found to have an identical resistance mutation, and 2 went on to receive and have a response to LOXO-195, a next-generation TRK inhibitor that seems to retain activity in the presence of this mutation (Cancer Discov. 2017 June 3. doi: 10.1158/2159-8290.CD-17-0507).
TRK testing
Several next-generation sequencing-based tests already available clinically can pick up TRK fusions, Dr Hyman pointed out. “But it is important for the ordering physician to understand whether the tests they are ordering include fusion detection and, if it’s an option, to select it. Otherwise, they will not find TRK fusions. “The list price for these tests is in the low thousands of dollars,” he noted. In cancers in which sequential single-gene testing is already being done as standard of care, there is “minimal” incremental cost of instead using comprehensive testing that would detect TRK fusions.
Oncologists should be aware that obtaining test results can take weeks, Dr Hyman stressed. “This [testing] should be more broadly adopted and should be adopted at a point in the patient’s treatment [so that they] don’t become too sick, then don’t have an opportunity to be treated even when the test results come back positive.”
— Susan London
QoL preserved with ribociclib-letrozole for advanced breast cancer
Key clinical point Patients who took ribociclib plus letrozole had less pain and no drop in QoL compared with letrozole alone. Major finding QoL was sustained and pain scores decreased when ribociclib was added to letrozole for patients with advanced breast cancer. Data source Double-blind, placebo-controlled phase 3 trial of letrozole plus ribociclib compared with letrozole plus placebo in 668 patients with advanced hormone receptor–positive, HER2-negative breast cancer. Disclosures Dr Verma reported financial relationships with Novartis, which markets ribociclib, and other firms.
Patients with advanced breast cancer whose aromatase inhibitor therapy was supplemented with a cycline-dependent kinase inhibitor had better PFS with no drop in quality of life (QoL). Health-related QoL for patients on the combination therapy was equivalent to that of patients on monotherapy in most aspects, but patients receiving both therapies had a sustained and clinically meaningful decrease in pain.
In addition, the time to definitive deterioration by 10% or more of the global health status/QoL scale score was similar between treatment arms (hazard ratio [HR], 0.944; 95% confidence interval, 0.720-1.237).
The MONALEESA-2 trial had previously shown that the CDK4/6 inhibitor ribociclib, when added to the aromatase inhibitor letrozole, significantly improved PFS for postmenopausal patients with hormone receptor–positive, HER2-negative advanced breast cancer, when compared with letrozole in combination with placebo.
Sunil Verma, MD, reported on health-related QoL and symptoms in the 2 arms of MONALEESA-2, showing change from baseline, time to a definitive 10% deterioration, and the mean scores for on-treatment time compared with end of treatment on the global health-status QoL subscale of the European Organization for Research and Treatment of Cancer's (EORTC's) 30-item core QoL questionnaire.
“During treatment, overall health-related quality of life was maintained from baseline and was similar in both arms,” said Dr Verma, the study’s first author. Changes during treatment were not statistically significant, and did not reach the predetermined threshold for a clinically meaningful difference. The effect of key symptoms such as fatigue, nausea, and vomiting on QoL was similar for patients receiving ribociclib or placebo, he said. Although symptom scores were slightly higher for patients in the active arm of the study, the results were not clinically significant.
Reporting validated, cancer-specific patient-reported outcomes from the trial, Dr Verma, professor and head of the department of oncology at the University of Calgary in Alberta, Canada, sought to “highlight the patient experience with a focus on health-related quality of life and symptoms,” he said during his presentation at the meeting. “A clinically meaningful – more than 5 points – improvement from baseline in pain score was maintained up to and including cycle 15 in the ribociclib plus letrozole arm.” The placebo arm had a mild, clinically insignificant improvement at most assessment points. For both treatment arms, pain scores increased a bit above baseline levels at the time of disease progression or end of therapy, he said.
Patients completed the EORTC 30-item core QoL questionnaire at their screening visit, and then every 8 weeks for the first 18 months. Then, they completed the questionnaires every 12 weeks until they experienced disease progression, died, were lost to follow-up or withdrew from the study, or stopped treatment.
Statistical analysis of the questionnaire results took into account the patients’ baseline scores, treatments received, and how they were stratified. Investigators assessed both statistical significance and the clinical meaningfulness of changes, defined as a change of 5-10 points.
In MONALEESA-2, 334 patients each were allocated to the ribociclib-letrozole arm and the placebo-letrozole arm. Patients in both arms, said Dr Verma, were very compliant with questionnaire completion. More than 90% of patients who were eligible completed questionnaire through cycle 19 of ribociclib or placebo. He explained that the overall numbers completing the questionnaire declined with time, as more patients had disease progression. Dr Verma said it is important to include those measures, because patients and their families care about “the quality of the time gained,” so patient-reported outcomes should be a part of risk-benefit assessments for new cancer therapies. “While delaying disease progression may help maintain patient quality of life, the addition of novel treatments to existing therapies can add toxicities, which may diminish quality of life,” he said.
— Kari Oakes
Ibrutinib and beyond: optimizing therapy in relapsed CLL
Key clinical point Ibrutinib had durable efficacy in relapsed CLL, and combinations with other targeted agents or with CAR-T cells are promising. Major finding Long-term PFS was better with ibrutinib than with ofatumumab (HR, 0.133). The overall response rate with the triplet of ibrutinib, ublituximab, and umbralisib was 100%. In all, 89% of patients achieved no evidence of disease in marrow when anti-CD19 CAR-T cells were added to ibrutinib. Data source An update of a phase 3 randomized trial among 391 patients with previously treated CLL or SLL (RESONATE). A phase 1/1b trial including 19 patients with mainly relapsed or refractory CLL or SLL. A pilot trial among 10 patients with previously treated, mainly higher-risk, CLL or SLL. Disclosures See article text.
Ibrutinib monotherapy
In the phase 3 randomized RESONATE trial, investigators compared ibrutinib with ofatumumab, an anti-CD20 antibody, among 391 patients with CLL or small lymphocytic lymphoma (SLL), with crossover allowed. Initial results favored ibrutinib.
Investigators led by John C Byrd, MD, director of the division of hematology at the Ohio State University Comprehensive Cancer Center in Columbus, reported updated data in a poster session at the meeting, now with a median 44 months of follow-up in the ibrutinib arm.
Median PFS was not reached with ibrutinib, compared with 8.1 months with ofatumumab (HR, 0.133). The 3-year rate of PFS for ibrutinib and ofatumumab was 59% and 3%, respectively.
The pattern was generally similar across patients stratified by cytogenetics (deletion of 17p, deletion of 11q, or neither), IGHV and TP53 mutation status, and previous lines of therapy, reported Dr Byrd. The 3-year overall survival rate for ibrutinib was 74%. In analyses adjusted for crossover, patients given the inhibitor had a markedly lower risk of death than did peers given the antibody (HR, 0.37). The overall response rate with ibrutinib was 91%. Although the rate of complete response increased with follow-up, it was still just 9%.
The most common grade 3 or worse adverse events were neutropenia (23%), pneumonia (17%), and anemia, thrombocytopenia, and hypertension (8% each). Major hemorrhage was reported in 2 patients (1%) in the ibrutinib group, and 3 (2%) in the ofatumumab group.
The investigators emphasized that these long-term results “show that extended treatment with ibrutinib is tolerable and continues to show sustained PFS in previously treated patients with CLL regardless of high-risk cytogenetics, adding that traditional poor prognostic factors for survival with chemoimmunotherapy, including del(17p) and del(11q), were not significant factors predictive of PFS outcomes with ibrutinib.
Funding and disclosures: Pharmacyclics funded the trial. Dr Byrd disclosed that he receives research funding from Pharmacyclics and other companies.
Ibrutinib plus ublituximab and umbralisib
Investigators led by Loretta J Nastoupil, MD, tested a triplet consisting of ibrutinib with ublituximab (another anti-CD20 antibody) and umbralisib (TGR-1202), an oral PI3 kinase-delta inhibitor, in a phase 1/1b trial of 38 patients with generally heavily pretreated leukemias and lymphomas, including 20 with CLL or SLL. Notably, 8 patients with CLL (50%) had a 17p or 11q deletion.
The median time on study was 11.1 months, reported Dr Nastoupil, of the department of lymphoma/myeloma at the University of Texas MD Anderson Cancer Center, Houston. The overall response rate for the 19 evaluable patients with CLL or SLL was 100% (complete response in 32%, partial response in 68%). The main grade 3 or 4 adverse events in the entire trial population were neutropenia (18%) and pyrexia (8%). Only two patients discontinued treatment because of adverse events.
“An expansion cohort is ongoing at the highest dose, and we will clearly need more patients treated and longer follow-up to really know the efficacy,” commented invited discussant Jennifer R Brown, MD, PhD, director of the Chronic Lymphocytic Leukemia Center at the Dana-Farber Cancer Institute in Boston.
Funding and disclosures: TG Therapeutics funded the trial. Dr Nastoupil has received honoraria and research funding from TG Therapeutics, and honoraria from Pharmacyclics.
Ibrutinib plus CAR-T cells
Investigators in a pilot trial led by Saar Gill, MD, PhD, of the hospital of the University of Pennsylvania in Philadelphia, tested the combination of ibrutinib with chimeric antigen receptor-T cells (CAR-T cells) against CD19, on the basis of preclinical evidence of synergy. The trial participants were 10 patients with CLL or SLL who had not achieved complete response with ibrutinib. All had a 17p deletion or a p53 mutation, or a complex karyotype, and some had a known ibrutinib resistance mutation.
At 3 months, 8 of 9 evaluable patients (89%) had no evidence of disease in bone marrow, reported Dr Gill. Seven patients (78%) achieved a complete or partial radiographic response in the spleen and lymph nodes. Overall, the treatment was well tolerated. One patient developed grade 4 tumor lysis syndrome, and two developed grade 3 cytokine release syndrome. But, none required anticytokine therapy.
Most patients remain on ibrutinib and are being monitored. In addition, the researchers plan to treat 25 more patients with the same combination.
Funding and disclosures: Novartis funded the trial. Dr Gill disclosed that he receives research funding from Novartis (institutional) and has patents for CAR-T cells for AML.
— Susan London
Pazopanib falls short as adjuvant therapy for high-risk RCC
Key clinical point Pazopanib is not efficacious for treating resected high-risk locally advanced RCC. Major finding Compared with placebo, pazopanib started at 600 mg daily did not significantly reduce the risk of DFS events (HR, 0.86; P = .16). Data source A phase 3 randomized controlled trial among 1,538 patients who had undergone nephrectomy for high-risk locally advanced RCC (PROTECT trial). Disclosures Novartis Oncology funded the trial. Dr Motzer disclosed that he is a consultant to Novartis and receives research funding from Novartis (institutional).
The antiangiogenic agent pazopanib is not efficacious when used as adjuvant therapy for resected renal cell carcinoma (RCC) with features that confer a high risk of recurrence, investigators in the PROTECT investigators reported at the meeting. “The trial did not meet its primary endpoint,” concluded lead investigator Robert J Motzer, MD, of Memorial Sloan-Kettering Cancer Center in New York. “Pazopanib is not recommended for adjuvant therapy following resection of locally advanced RCC.”
Adjuvant use of other agents in this class has yielded mixed results, Dr Motzer noted, citing the earlier ASSURE trial found that neither sunitinib nor sorafenib improved disease-free survival (DFS) or overall survival (Lancet 2016;387:2008-2016), and the S-TRAC trial that found that sunitinib improved DFS (N Engl J Med. 2016;375:2246-2254).
Pazopanib is an oral multitargeted tyrosine kinase inhibitor active against the vascular endothelial growth factor receptor (VEGFR). The PROTECT trial included 1,538 patients with resected pT2 (high grade), pT3, or greater nonmetastatic clear cell RCC, a highly vascular tumor typically reliant on aberrant signaling in the VEGF pathway. The patients were assigned evenly to receive pazopanib or placebo for 1 year. The starting dose was lowered from 800 mg daily to 600 mg daily (with escalation permitted) after 403 patients had been treated.
In intention-to-treat analysis among patients started on the 600-mg dose and having a median follow-up of about 31 months, DFS was better with pazopanib but not significantly so (HR, 0.86; P = .16). In secondary analyses, pazopanib had a significant DFS benefit in patients started on the 800-mg dose (HR, 0.69; P = .02) and among the entire trial population started on either dose (HR, 0.80; P = .01).
One possible explanation for the differing results seen with the 2 doses was the difference in follow-up, because the 800-mg group was treated earlier in the trial, said Dr Motzer. But with an additional year of blinded follow-up, the benefit in the 600-mg group diminished, but not in the 800-mg group.
Another possibility was the somewhat better performance of the placebo group used for comparison with the lower dose: the 3-year DFS rate with placebo was 64% for the 600-mg comparison but 56% for the 800-mg comparison. “One factor that could explain differences in the outcomes of the placebo groups includes unidentified patient demographic characteristics,” Dr Motzer added.
Overall survival was statistically indistinguishable between the pazopanib and placebo groups, regardless of dose. However, “the results are inconclusive as the data are not yet mature,” he said, with a definitive analysis planned for 2019.
Patients started on the 600-mg dose of pazopanib had a higher rate of grade 3 or 4 adverse events overall compared with those given placebo (60% vs 21%, respectively), driven in part by higher rates of hypertension and increased alanine aminotransferase levels. “Although the intent of modifying the protocol dose of pazopanib from 800 mg to 600 mg was to reduce the rate of discontinuation and improve the safety profile ... both cohorts had similar discontinuation rates and safety profiles,” Dr Motzer noted.
A QoL analysis for the 600-mg group using the 19-item Functional Assessment of Cancer Therapy Kidney Symptom Index showed values were consistently lower with the drug than with placebo during treatment, with a crossing of the threshold for a minimally important difference at week 8. Pharmacokinetic analyses from the trial, reported in a poster at the meeting, showed that in the group starting pazopanib at 600 mg, DFS was longer in patients who achieved higher drug trough concentrations at week 3 or 5.
— Susan London
Survival improves when patients with cancer self-report symptoms
Key clinical point Patients with metastatic cancer who self-reported symptoms experienced significant improvement in overall survival. Major finding Median overall survival with self-reporting of symptoms compared with usual care was 31.2 and 26 months, respectively. Data source A randomized controlled clinical trial of 766 patients. Funding and disclosures This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr Basch and Dr Burstein each reported having no disclosures.
Patients with metastatic cancer who self-reported symptoms during routine cancer treatment experienced a number of benefits, including a statistically significant improvement in overall survival, according to findings from a randomized, controlled clinical trial (see p. e184). The median overall survival in 441 patients receiving treatment for metastatic breast, lung, genitourinary, or gynecologic cancer who were randomized to the self-reporting intervention arm was more than 5 months longer (a nearly 20% increase) than in 325 patients receiving standard care (31.2 vs. 26 months), Ethan Basch, MD, of the Lineberger Comprehensive Cancer Center at the University of North Carolina, Chapel Hill, said at the meeting. “Another way to think of this is [in terms of] 5-year survival. At 5 years, 8% more patients were alive in the self-reporting group,” he said.
In addition, 31% of patients in the intervention arm had better quality of life/physical functioning, compared with those in the control arm, and 7% fewer patients in the intervention arm visited an emergency room during the study. The duration of potentially life-prolonging chemotherapy was increased by an average of 2 months in the intervention arm, he said (JAMA. 2017 Jun 4. doi: 10.1001/jama.2017.7156).
Symptoms such as nausea, pain, and fatigue are common among patients with metastatic cancer and can often go undetected by doctors and nurses until they become severe and physically debilitating, Dr Basch added, noting that patients are often hesitant to call the office between visits to report symptoms.
Dr Basch and his colleagues hypothesized that self-reporting of patient symptoms between visits or before a visit while the patient was in the clinic waiting area would prompt earlier intervention and improve symptom control and outcomes.
Study participants were patients at Memorial Sloan Kettering Cancer Center who had advanced solid genitourinary, gynecologic, breast, or lung tumors and who were receiving outpatient chemotherapy. Those assigned to the intervention group used tablet computers and an online web survey system to report on 12 symptoms commonly experienced during chemotherapy. The system triggers an alert to a nurse when a severe or worsening symptom is reported. Patients in the usual care group discussed symptoms during office visits and were encouraged to call the office between visits if they were concerned about symptoms.
Patients remained on the study until discontinuation of all cancer treatment, hospice, or death.
One possible explanation for the findings is that this self-reporting approach prompts clinicians to manage symptoms before they cause serious downstream complications, Dr Basch said.
The approach may also keep patients more physically functional, which is known from previous studies to have a strong association with better survival, and it may also improve management of chemotherapy side effects, enabling longer duration of beneficial cancer treatment. “In oncology, we often are limited in our ability to give life-prolonging treatment because people don’t tolerate it well,” Dr Basch explained.
“This approach should be considered for inclusion in standard symptoms management as a component of high-quality cancer care,” he concluded, noting that efforts are underway to test the next generation of systems to improve communication between patients and care teams and to figure out how best to integrate these tools into oncology practice.
The system used in the this study was designed for research, but a number of companies have tools currently available for patient-reported outcomes, and others are being developed, Dr Basch said. A National Cancer Institute questionnaire, the PRO-CTCAE, is publicly available and can be loaded into patients’ electronic health records for this purpose as well.
Harold J Burstein, MD, of Dana-Farber Cancer Institute, Boston, said the study findings validate the feeling among many clinicians that patient-focused, team-based care can improve outcomes in a meaningful way for patients. If this were a drug … it would be worth tens, if not hundreds of thousands, of dollars per year … We don’t have those same kinds of dollars to help implement these into our electronic health records or our systems. We need to find ways to support that and make it happen,” he said.
— Sharon Worcester
TRK inhibitor shows ‘striking’ activity and durability across diverse cancers
Key clinical point Larotrectinib has good, durable efficacy when used to treat advanced cancers harboring TRK fusions. Major finding The overall response rate was 76%, and 79% of responses were still ongoing at 12 months. Data source An integrated analysis of phase 1 and 2 trials among 55 children and adults having 17 discrete types of advanced cancer with TRK fusions. Funding and disclosures Loxo Oncology funded the study. Dr Hyman disclosed that he has a consulting or advisory role with Atara Biotherapeutics, Chugai Pharma, and CytomX Therapeutics, and that he receives research funding from AstraZeneca and Puma Biotechnology.
Larotrectinib, an oral inhibitor of tropomyosin receptor kinase (TRK), has durable efficacy across diverse adult and pediatric cancers that harbor a genetic aberration known as TRK fusion, according to findings from an analysis of 3 trials reported at the meeting (see p. e184). Fusion of a TRK gene with an unrelated gene leads to uncontrolled signaling in the TRK pathway, potentially causing tumor growth and addiction to this input, David Hyman, MD, chief of early drug development at Memorial Sloan Kettering Cancer Center in New York, explained in a press briefing.
“One of the defining features of TRK fusions is that they are not just found in one cancer type, but in dozens of different cancer types, and not just in adults, but children as well, spanning the entire lifetime of the person,” he noted. They are rare in common cancers and nearly universal in certain uncommon cancers; collectively, they are present in possibly 5,000 cancers diagnosed each year in the United States.
Dr Hyman and his colleagues analyzed data from 55 patients having 17 discrete types of advanced cancer harboring TRK fusions who were treated with larotrectinib in phase 1 and 2 trials. Results showed an overall response rate of 76%, and the majority of responses were still ongoing at 12 months. “I believe these data support larotrectinib as a potential new standard of care for these patients,” he said. “However, I want to emphasize that really recognizing this benefit in the community will require that we test patients more universally for the presence of TRK fusions or other tumor-agnostic biomarkers, such as microsatellite instability.”
Study details
The investigators analyzed data from 3 trials in which patients with advanced TRK fusion-positive solid cancers received larotrectinib (LOXO-101): a phase 1 trial among 8 adult patients, a phase 1/2 trial among 12 pediatric patients (SCOUT), and a phase 2 “basket” trial among 35 adult and adolescent patients (NAVIGATE).
“These patients were identified by local testing,” Dr Hyman noted. “We did not perform central screening to find the TRK fusions, and in fact, 50 different laboratories identified the 55 patients. So in a sense, this really represents the real-world identification of these patients.”
In an integrated analysis, the overall rate of confirmed response as assessed by investigators was 76%, with complete response in 12% of patients and partial response in 64%. Two patients had such deep tumor regression that they experienced downstaging enabling them to undergo potentially curative surgery. Efficacy was consistent regardless of tumor type, which TRK gene was affected, and the fusion partner gene.
Median time to response was 1.8 months. “This is just a reflection of when the first scan was obtained. But in the clinic, patients reported dramatic improvement of their symptoms within days of starting therapy,” Dr Hyman said.
With a median follow-up of 5.8 months, the median duration of response was not yet reached. In all, 79% of responses were still ongoing at 12 months. Median progression-free survival (PFS) was likewise not reached; the 12-month rate was 63%.
The leading treatment-emergent adverse events were fatigue (38%), dizziness (27%), nausea (26%), and anemia (26%). “This is an extremely well tolerated therapy with only 13% of patients requiring any form of dose modification and not a single patient discontinuing due to adverse events,” he said.
It is not clear why some patients had apparent primary resistance to larotrectinib, but their TRK fusion test results may have been incorrect, Dr Hyman speculated. In all, 6 patients developed acquired resistance to larotrectinib; 5 of them were found to have an identical resistance mutation, and 2 went on to receive and have a response to LOXO-195, a next-generation TRK inhibitor that seems to retain activity in the presence of this mutation (Cancer Discov. 2017 June 3. doi: 10.1158/2159-8290.CD-17-0507).
TRK testing
Several next-generation sequencing-based tests already available clinically can pick up TRK fusions, Dr Hyman pointed out. “But it is important for the ordering physician to understand whether the tests they are ordering include fusion detection and, if it’s an option, to select it. Otherwise, they will not find TRK fusions. “The list price for these tests is in the low thousands of dollars,” he noted. In cancers in which sequential single-gene testing is already being done as standard of care, there is “minimal” incremental cost of instead using comprehensive testing that would detect TRK fusions.
Oncologists should be aware that obtaining test results can take weeks, Dr Hyman stressed. “This [testing] should be more broadly adopted and should be adopted at a point in the patient’s treatment [so that they] don’t become too sick, then don’t have an opportunity to be treated even when the test results come back positive.”
— Susan London
QoL preserved with ribociclib-letrozole for advanced breast cancer
Key clinical point Patients who took ribociclib plus letrozole had less pain and no drop in QoL compared with letrozole alone. Major finding QoL was sustained and pain scores decreased when ribociclib was added to letrozole for patients with advanced breast cancer. Data source Double-blind, placebo-controlled phase 3 trial of letrozole plus ribociclib compared with letrozole plus placebo in 668 patients with advanced hormone receptor–positive, HER2-negative breast cancer. Disclosures Dr Verma reported financial relationships with Novartis, which markets ribociclib, and other firms.
Patients with advanced breast cancer whose aromatase inhibitor therapy was supplemented with a cycline-dependent kinase inhibitor had better PFS with no drop in quality of life (QoL). Health-related QoL for patients on the combination therapy was equivalent to that of patients on monotherapy in most aspects, but patients receiving both therapies had a sustained and clinically meaningful decrease in pain.
In addition, the time to definitive deterioration by 10% or more of the global health status/QoL scale score was similar between treatment arms (hazard ratio [HR], 0.944; 95% confidence interval, 0.720-1.237).
The MONALEESA-2 trial had previously shown that the CDK4/6 inhibitor ribociclib, when added to the aromatase inhibitor letrozole, significantly improved PFS for postmenopausal patients with hormone receptor–positive, HER2-negative advanced breast cancer, when compared with letrozole in combination with placebo.
Sunil Verma, MD, reported on health-related QoL and symptoms in the 2 arms of MONALEESA-2, showing change from baseline, time to a definitive 10% deterioration, and the mean scores for on-treatment time compared with end of treatment on the global health-status QoL subscale of the European Organization for Research and Treatment of Cancer's (EORTC's) 30-item core QoL questionnaire.
“During treatment, overall health-related quality of life was maintained from baseline and was similar in both arms,” said Dr Verma, the study’s first author. Changes during treatment were not statistically significant, and did not reach the predetermined threshold for a clinically meaningful difference. The effect of key symptoms such as fatigue, nausea, and vomiting on QoL was similar for patients receiving ribociclib or placebo, he said. Although symptom scores were slightly higher for patients in the active arm of the study, the results were not clinically significant.
Reporting validated, cancer-specific patient-reported outcomes from the trial, Dr Verma, professor and head of the department of oncology at the University of Calgary in Alberta, Canada, sought to “highlight the patient experience with a focus on health-related quality of life and symptoms,” he said during his presentation at the meeting. “A clinically meaningful – more than 5 points – improvement from baseline in pain score was maintained up to and including cycle 15 in the ribociclib plus letrozole arm.” The placebo arm had a mild, clinically insignificant improvement at most assessment points. For both treatment arms, pain scores increased a bit above baseline levels at the time of disease progression or end of therapy, he said.
Patients completed the EORTC 30-item core QoL questionnaire at their screening visit, and then every 8 weeks for the first 18 months. Then, they completed the questionnaires every 12 weeks until they experienced disease progression, died, were lost to follow-up or withdrew from the study, or stopped treatment.
Statistical analysis of the questionnaire results took into account the patients’ baseline scores, treatments received, and how they were stratified. Investigators assessed both statistical significance and the clinical meaningfulness of changes, defined as a change of 5-10 points.
In MONALEESA-2, 334 patients each were allocated to the ribociclib-letrozole arm and the placebo-letrozole arm. Patients in both arms, said Dr Verma, were very compliant with questionnaire completion. More than 90% of patients who were eligible completed questionnaire through cycle 19 of ribociclib or placebo. He explained that the overall numbers completing the questionnaire declined with time, as more patients had disease progression. Dr Verma said it is important to include those measures, because patients and their families care about “the quality of the time gained,” so patient-reported outcomes should be a part of risk-benefit assessments for new cancer therapies. “While delaying disease progression may help maintain patient quality of life, the addition of novel treatments to existing therapies can add toxicities, which may diminish quality of life,” he said.
— Kari Oakes
Ibrutinib and beyond: optimizing therapy in relapsed CLL
Key clinical point Ibrutinib had durable efficacy in relapsed CLL, and combinations with other targeted agents or with CAR-T cells are promising. Major finding Long-term PFS was better with ibrutinib than with ofatumumab (HR, 0.133). The overall response rate with the triplet of ibrutinib, ublituximab, and umbralisib was 100%. In all, 89% of patients achieved no evidence of disease in marrow when anti-CD19 CAR-T cells were added to ibrutinib. Data source An update of a phase 3 randomized trial among 391 patients with previously treated CLL or SLL (RESONATE). A phase 1/1b trial including 19 patients with mainly relapsed or refractory CLL or SLL. A pilot trial among 10 patients with previously treated, mainly higher-risk, CLL or SLL. Disclosures See article text.
Ibrutinib monotherapy
In the phase 3 randomized RESONATE trial, investigators compared ibrutinib with ofatumumab, an anti-CD20 antibody, among 391 patients with CLL or small lymphocytic lymphoma (SLL), with crossover allowed. Initial results favored ibrutinib.
Investigators led by John C Byrd, MD, director of the division of hematology at the Ohio State University Comprehensive Cancer Center in Columbus, reported updated data in a poster session at the meeting, now with a median 44 months of follow-up in the ibrutinib arm.
Median PFS was not reached with ibrutinib, compared with 8.1 months with ofatumumab (HR, 0.133). The 3-year rate of PFS for ibrutinib and ofatumumab was 59% and 3%, respectively.
The pattern was generally similar across patients stratified by cytogenetics (deletion of 17p, deletion of 11q, or neither), IGHV and TP53 mutation status, and previous lines of therapy, reported Dr Byrd. The 3-year overall survival rate for ibrutinib was 74%. In analyses adjusted for crossover, patients given the inhibitor had a markedly lower risk of death than did peers given the antibody (HR, 0.37). The overall response rate with ibrutinib was 91%. Although the rate of complete response increased with follow-up, it was still just 9%.
The most common grade 3 or worse adverse events were neutropenia (23%), pneumonia (17%), and anemia, thrombocytopenia, and hypertension (8% each). Major hemorrhage was reported in 2 patients (1%) in the ibrutinib group, and 3 (2%) in the ofatumumab group.
The investigators emphasized that these long-term results “show that extended treatment with ibrutinib is tolerable and continues to show sustained PFS in previously treated patients with CLL regardless of high-risk cytogenetics, adding that traditional poor prognostic factors for survival with chemoimmunotherapy, including del(17p) and del(11q), were not significant factors predictive of PFS outcomes with ibrutinib.
Funding and disclosures: Pharmacyclics funded the trial. Dr Byrd disclosed that he receives research funding from Pharmacyclics and other companies.
Ibrutinib plus ublituximab and umbralisib
Investigators led by Loretta J Nastoupil, MD, tested a triplet consisting of ibrutinib with ublituximab (another anti-CD20 antibody) and umbralisib (TGR-1202), an oral PI3 kinase-delta inhibitor, in a phase 1/1b trial of 38 patients with generally heavily pretreated leukemias and lymphomas, including 20 with CLL or SLL. Notably, 8 patients with CLL (50%) had a 17p or 11q deletion.
The median time on study was 11.1 months, reported Dr Nastoupil, of the department of lymphoma/myeloma at the University of Texas MD Anderson Cancer Center, Houston. The overall response rate for the 19 evaluable patients with CLL or SLL was 100% (complete response in 32%, partial response in 68%). The main grade 3 or 4 adverse events in the entire trial population were neutropenia (18%) and pyrexia (8%). Only two patients discontinued treatment because of adverse events.
“An expansion cohort is ongoing at the highest dose, and we will clearly need more patients treated and longer follow-up to really know the efficacy,” commented invited discussant Jennifer R Brown, MD, PhD, director of the Chronic Lymphocytic Leukemia Center at the Dana-Farber Cancer Institute in Boston.
Funding and disclosures: TG Therapeutics funded the trial. Dr Nastoupil has received honoraria and research funding from TG Therapeutics, and honoraria from Pharmacyclics.
Ibrutinib plus CAR-T cells
Investigators in a pilot trial led by Saar Gill, MD, PhD, of the hospital of the University of Pennsylvania in Philadelphia, tested the combination of ibrutinib with chimeric antigen receptor-T cells (CAR-T cells) against CD19, on the basis of preclinical evidence of synergy. The trial participants were 10 patients with CLL or SLL who had not achieved complete response with ibrutinib. All had a 17p deletion or a p53 mutation, or a complex karyotype, and some had a known ibrutinib resistance mutation.
At 3 months, 8 of 9 evaluable patients (89%) had no evidence of disease in bone marrow, reported Dr Gill. Seven patients (78%) achieved a complete or partial radiographic response in the spleen and lymph nodes. Overall, the treatment was well tolerated. One patient developed grade 4 tumor lysis syndrome, and two developed grade 3 cytokine release syndrome. But, none required anticytokine therapy.
Most patients remain on ibrutinib and are being monitored. In addition, the researchers plan to treat 25 more patients with the same combination.
Funding and disclosures: Novartis funded the trial. Dr Gill disclosed that he receives research funding from Novartis (institutional) and has patents for CAR-T cells for AML.
— Susan London
Pazopanib falls short as adjuvant therapy for high-risk RCC
Key clinical point Pazopanib is not efficacious for treating resected high-risk locally advanced RCC. Major finding Compared with placebo, pazopanib started at 600 mg daily did not significantly reduce the risk of DFS events (HR, 0.86; P = .16). Data source A phase 3 randomized controlled trial among 1,538 patients who had undergone nephrectomy for high-risk locally advanced RCC (PROTECT trial). Disclosures Novartis Oncology funded the trial. Dr Motzer disclosed that he is a consultant to Novartis and receives research funding from Novartis (institutional).
The antiangiogenic agent pazopanib is not efficacious when used as adjuvant therapy for resected renal cell carcinoma (RCC) with features that confer a high risk of recurrence, investigators in the PROTECT investigators reported at the meeting. “The trial did not meet its primary endpoint,” concluded lead investigator Robert J Motzer, MD, of Memorial Sloan-Kettering Cancer Center in New York. “Pazopanib is not recommended for adjuvant therapy following resection of locally advanced RCC.”
Adjuvant use of other agents in this class has yielded mixed results, Dr Motzer noted, citing the earlier ASSURE trial found that neither sunitinib nor sorafenib improved disease-free survival (DFS) or overall survival (Lancet 2016;387:2008-2016), and the S-TRAC trial that found that sunitinib improved DFS (N Engl J Med. 2016;375:2246-2254).
Pazopanib is an oral multitargeted tyrosine kinase inhibitor active against the vascular endothelial growth factor receptor (VEGFR). The PROTECT trial included 1,538 patients with resected pT2 (high grade), pT3, or greater nonmetastatic clear cell RCC, a highly vascular tumor typically reliant on aberrant signaling in the VEGF pathway. The patients were assigned evenly to receive pazopanib or placebo for 1 year. The starting dose was lowered from 800 mg daily to 600 mg daily (with escalation permitted) after 403 patients had been treated.
In intention-to-treat analysis among patients started on the 600-mg dose and having a median follow-up of about 31 months, DFS was better with pazopanib but not significantly so (HR, 0.86; P = .16). In secondary analyses, pazopanib had a significant DFS benefit in patients started on the 800-mg dose (HR, 0.69; P = .02) and among the entire trial population started on either dose (HR, 0.80; P = .01).
One possible explanation for the differing results seen with the 2 doses was the difference in follow-up, because the 800-mg group was treated earlier in the trial, said Dr Motzer. But with an additional year of blinded follow-up, the benefit in the 600-mg group diminished, but not in the 800-mg group.
Another possibility was the somewhat better performance of the placebo group used for comparison with the lower dose: the 3-year DFS rate with placebo was 64% for the 600-mg comparison but 56% for the 800-mg comparison. “One factor that could explain differences in the outcomes of the placebo groups includes unidentified patient demographic characteristics,” Dr Motzer added.
Overall survival was statistically indistinguishable between the pazopanib and placebo groups, regardless of dose. However, “the results are inconclusive as the data are not yet mature,” he said, with a definitive analysis planned for 2019.
Patients started on the 600-mg dose of pazopanib had a higher rate of grade 3 or 4 adverse events overall compared with those given placebo (60% vs 21%, respectively), driven in part by higher rates of hypertension and increased alanine aminotransferase levels. “Although the intent of modifying the protocol dose of pazopanib from 800 mg to 600 mg was to reduce the rate of discontinuation and improve the safety profile ... both cohorts had similar discontinuation rates and safety profiles,” Dr Motzer noted.
A QoL analysis for the 600-mg group using the 19-item Functional Assessment of Cancer Therapy Kidney Symptom Index showed values were consistently lower with the drug than with placebo during treatment, with a crossing of the threshold for a minimally important difference at week 8. Pharmacokinetic analyses from the trial, reported in a poster at the meeting, showed that in the group starting pazopanib at 600 mg, DFS was longer in patients who achieved higher drug trough concentrations at week 3 or 5.
— Susan London
Survival improves when patients with cancer self-report symptoms
Key clinical point Patients with metastatic cancer who self-reported symptoms experienced significant improvement in overall survival. Major finding Median overall survival with self-reporting of symptoms compared with usual care was 31.2 and 26 months, respectively. Data source A randomized controlled clinical trial of 766 patients. Funding and disclosures This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr Basch and Dr Burstein each reported having no disclosures.
Patients with metastatic cancer who self-reported symptoms during routine cancer treatment experienced a number of benefits, including a statistically significant improvement in overall survival, according to findings from a randomized, controlled clinical trial (see p. e184). The median overall survival in 441 patients receiving treatment for metastatic breast, lung, genitourinary, or gynecologic cancer who were randomized to the self-reporting intervention arm was more than 5 months longer (a nearly 20% increase) than in 325 patients receiving standard care (31.2 vs. 26 months), Ethan Basch, MD, of the Lineberger Comprehensive Cancer Center at the University of North Carolina, Chapel Hill, said at the meeting. “Another way to think of this is [in terms of] 5-year survival. At 5 years, 8% more patients were alive in the self-reporting group,” he said.
In addition, 31% of patients in the intervention arm had better quality of life/physical functioning, compared with those in the control arm, and 7% fewer patients in the intervention arm visited an emergency room during the study. The duration of potentially life-prolonging chemotherapy was increased by an average of 2 months in the intervention arm, he said (JAMA. 2017 Jun 4. doi: 10.1001/jama.2017.7156).
Symptoms such as nausea, pain, and fatigue are common among patients with metastatic cancer and can often go undetected by doctors and nurses until they become severe and physically debilitating, Dr Basch added, noting that patients are often hesitant to call the office between visits to report symptoms.
Dr Basch and his colleagues hypothesized that self-reporting of patient symptoms between visits or before a visit while the patient was in the clinic waiting area would prompt earlier intervention and improve symptom control and outcomes.
Study participants were patients at Memorial Sloan Kettering Cancer Center who had advanced solid genitourinary, gynecologic, breast, or lung tumors and who were receiving outpatient chemotherapy. Those assigned to the intervention group used tablet computers and an online web survey system to report on 12 symptoms commonly experienced during chemotherapy. The system triggers an alert to a nurse when a severe or worsening symptom is reported. Patients in the usual care group discussed symptoms during office visits and were encouraged to call the office between visits if they were concerned about symptoms.
Patients remained on the study until discontinuation of all cancer treatment, hospice, or death.
One possible explanation for the findings is that this self-reporting approach prompts clinicians to manage symptoms before they cause serious downstream complications, Dr Basch said.
The approach may also keep patients more physically functional, which is known from previous studies to have a strong association with better survival, and it may also improve management of chemotherapy side effects, enabling longer duration of beneficial cancer treatment. “In oncology, we often are limited in our ability to give life-prolonging treatment because people don’t tolerate it well,” Dr Basch explained.
“This approach should be considered for inclusion in standard symptoms management as a component of high-quality cancer care,” he concluded, noting that efforts are underway to test the next generation of systems to improve communication between patients and care teams and to figure out how best to integrate these tools into oncology practice.
The system used in the this study was designed for research, but a number of companies have tools currently available for patient-reported outcomes, and others are being developed, Dr Basch said. A National Cancer Institute questionnaire, the PRO-CTCAE, is publicly available and can be loaded into patients’ electronic health records for this purpose as well.
Harold J Burstein, MD, of Dana-Farber Cancer Institute, Boston, said the study findings validate the feeling among many clinicians that patient-focused, team-based care can improve outcomes in a meaningful way for patients. If this were a drug … it would be worth tens, if not hundreds of thousands, of dollars per year … We don’t have those same kinds of dollars to help implement these into our electronic health records or our systems. We need to find ways to support that and make it happen,” he said.
— Sharon Worcester
TRK inhibitor shows ‘striking’ activity and durability across diverse cancers
Key clinical point Larotrectinib has good, durable efficacy when used to treat advanced cancers harboring TRK fusions. Major finding The overall response rate was 76%, and 79% of responses were still ongoing at 12 months. Data source An integrated analysis of phase 1 and 2 trials among 55 children and adults having 17 discrete types of advanced cancer with TRK fusions. Funding and disclosures Loxo Oncology funded the study. Dr Hyman disclosed that he has a consulting or advisory role with Atara Biotherapeutics, Chugai Pharma, and CytomX Therapeutics, and that he receives research funding from AstraZeneca and Puma Biotechnology.
Larotrectinib, an oral inhibitor of tropomyosin receptor kinase (TRK), has durable efficacy across diverse adult and pediatric cancers that harbor a genetic aberration known as TRK fusion, according to findings from an analysis of 3 trials reported at the meeting (see p. e184). Fusion of a TRK gene with an unrelated gene leads to uncontrolled signaling in the TRK pathway, potentially causing tumor growth and addiction to this input, David Hyman, MD, chief of early drug development at Memorial Sloan Kettering Cancer Center in New York, explained in a press briefing.
“One of the defining features of TRK fusions is that they are not just found in one cancer type, but in dozens of different cancer types, and not just in adults, but children as well, spanning the entire lifetime of the person,” he noted. They are rare in common cancers and nearly universal in certain uncommon cancers; collectively, they are present in possibly 5,000 cancers diagnosed each year in the United States.
Dr Hyman and his colleagues analyzed data from 55 patients having 17 discrete types of advanced cancer harboring TRK fusions who were treated with larotrectinib in phase 1 and 2 trials. Results showed an overall response rate of 76%, and the majority of responses were still ongoing at 12 months. “I believe these data support larotrectinib as a potential new standard of care for these patients,” he said. “However, I want to emphasize that really recognizing this benefit in the community will require that we test patients more universally for the presence of TRK fusions or other tumor-agnostic biomarkers, such as microsatellite instability.”
Study details
The investigators analyzed data from 3 trials in which patients with advanced TRK fusion-positive solid cancers received larotrectinib (LOXO-101): a phase 1 trial among 8 adult patients, a phase 1/2 trial among 12 pediatric patients (SCOUT), and a phase 2 “basket” trial among 35 adult and adolescent patients (NAVIGATE).
“These patients were identified by local testing,” Dr Hyman noted. “We did not perform central screening to find the TRK fusions, and in fact, 50 different laboratories identified the 55 patients. So in a sense, this really represents the real-world identification of these patients.”
In an integrated analysis, the overall rate of confirmed response as assessed by investigators was 76%, with complete response in 12% of patients and partial response in 64%. Two patients had such deep tumor regression that they experienced downstaging enabling them to undergo potentially curative surgery. Efficacy was consistent regardless of tumor type, which TRK gene was affected, and the fusion partner gene.
Median time to response was 1.8 months. “This is just a reflection of when the first scan was obtained. But in the clinic, patients reported dramatic improvement of their symptoms within days of starting therapy,” Dr Hyman said.
With a median follow-up of 5.8 months, the median duration of response was not yet reached. In all, 79% of responses were still ongoing at 12 months. Median progression-free survival (PFS) was likewise not reached; the 12-month rate was 63%.
The leading treatment-emergent adverse events were fatigue (38%), dizziness (27%), nausea (26%), and anemia (26%). “This is an extremely well tolerated therapy with only 13% of patients requiring any form of dose modification and not a single patient discontinuing due to adverse events,” he said.
It is not clear why some patients had apparent primary resistance to larotrectinib, but their TRK fusion test results may have been incorrect, Dr Hyman speculated. In all, 6 patients developed acquired resistance to larotrectinib; 5 of them were found to have an identical resistance mutation, and 2 went on to receive and have a response to LOXO-195, a next-generation TRK inhibitor that seems to retain activity in the presence of this mutation (Cancer Discov. 2017 June 3. doi: 10.1158/2159-8290.CD-17-0507).
TRK testing
Several next-generation sequencing-based tests already available clinically can pick up TRK fusions, Dr Hyman pointed out. “But it is important for the ordering physician to understand whether the tests they are ordering include fusion detection and, if it’s an option, to select it. Otherwise, they will not find TRK fusions. “The list price for these tests is in the low thousands of dollars,” he noted. In cancers in which sequential single-gene testing is already being done as standard of care, there is “minimal” incremental cost of instead using comprehensive testing that would detect TRK fusions.
Oncologists should be aware that obtaining test results can take weeks, Dr Hyman stressed. “This [testing] should be more broadly adopted and should be adopted at a point in the patient’s treatment [so that they] don’t become too sick, then don’t have an opportunity to be treated even when the test results come back positive.”
— Susan London
QoL preserved with ribociclib-letrozole for advanced breast cancer
Key clinical point Patients who took ribociclib plus letrozole had less pain and no drop in QoL compared with letrozole alone. Major finding QoL was sustained and pain scores decreased when ribociclib was added to letrozole for patients with advanced breast cancer. Data source Double-blind, placebo-controlled phase 3 trial of letrozole plus ribociclib compared with letrozole plus placebo in 668 patients with advanced hormone receptor–positive, HER2-negative breast cancer. Disclosures Dr Verma reported financial relationships with Novartis, which markets ribociclib, and other firms.
Patients with advanced breast cancer whose aromatase inhibitor therapy was supplemented with a cycline-dependent kinase inhibitor had better PFS with no drop in quality of life (QoL). Health-related QoL for patients on the combination therapy was equivalent to that of patients on monotherapy in most aspects, but patients receiving both therapies had a sustained and clinically meaningful decrease in pain.
In addition, the time to definitive deterioration by 10% or more of the global health status/QoL scale score was similar between treatment arms (hazard ratio [HR], 0.944; 95% confidence interval, 0.720-1.237).
The MONALEESA-2 trial had previously shown that the CDK4/6 inhibitor ribociclib, when added to the aromatase inhibitor letrozole, significantly improved PFS for postmenopausal patients with hormone receptor–positive, HER2-negative advanced breast cancer, when compared with letrozole in combination with placebo.
Sunil Verma, MD, reported on health-related QoL and symptoms in the 2 arms of MONALEESA-2, showing change from baseline, time to a definitive 10% deterioration, and the mean scores for on-treatment time compared with end of treatment on the global health-status QoL subscale of the European Organization for Research and Treatment of Cancer's (EORTC's) 30-item core QoL questionnaire.
“During treatment, overall health-related quality of life was maintained from baseline and was similar in both arms,” said Dr Verma, the study’s first author. Changes during treatment were not statistically significant, and did not reach the predetermined threshold for a clinically meaningful difference. The effect of key symptoms such as fatigue, nausea, and vomiting on QoL was similar for patients receiving ribociclib or placebo, he said. Although symptom scores were slightly higher for patients in the active arm of the study, the results were not clinically significant.
Reporting validated, cancer-specific patient-reported outcomes from the trial, Dr Verma, professor and head of the department of oncology at the University of Calgary in Alberta, Canada, sought to “highlight the patient experience with a focus on health-related quality of life and symptoms,” he said during his presentation at the meeting. “A clinically meaningful – more than 5 points – improvement from baseline in pain score was maintained up to and including cycle 15 in the ribociclib plus letrozole arm.” The placebo arm had a mild, clinically insignificant improvement at most assessment points. For both treatment arms, pain scores increased a bit above baseline levels at the time of disease progression or end of therapy, he said.
Patients completed the EORTC 30-item core QoL questionnaire at their screening visit, and then every 8 weeks for the first 18 months. Then, they completed the questionnaires every 12 weeks until they experienced disease progression, died, were lost to follow-up or withdrew from the study, or stopped treatment.
Statistical analysis of the questionnaire results took into account the patients’ baseline scores, treatments received, and how they were stratified. Investigators assessed both statistical significance and the clinical meaningfulness of changes, defined as a change of 5-10 points.
In MONALEESA-2, 334 patients each were allocated to the ribociclib-letrozole arm and the placebo-letrozole arm. Patients in both arms, said Dr Verma, were very compliant with questionnaire completion. More than 90% of patients who were eligible completed questionnaire through cycle 19 of ribociclib or placebo. He explained that the overall numbers completing the questionnaire declined with time, as more patients had disease progression. Dr Verma said it is important to include those measures, because patients and their families care about “the quality of the time gained,” so patient-reported outcomes should be a part of risk-benefit assessments for new cancer therapies. “While delaying disease progression may help maintain patient quality of life, the addition of novel treatments to existing therapies can add toxicities, which may diminish quality of life,” he said.
— Kari Oakes
Ibrutinib and beyond: optimizing therapy in relapsed CLL
Key clinical point Ibrutinib had durable efficacy in relapsed CLL, and combinations with other targeted agents or with CAR-T cells are promising. Major finding Long-term PFS was better with ibrutinib than with ofatumumab (HR, 0.133). The overall response rate with the triplet of ibrutinib, ublituximab, and umbralisib was 100%. In all, 89% of patients achieved no evidence of disease in marrow when anti-CD19 CAR-T cells were added to ibrutinib. Data source An update of a phase 3 randomized trial among 391 patients with previously treated CLL or SLL (RESONATE). A phase 1/1b trial including 19 patients with mainly relapsed or refractory CLL or SLL. A pilot trial among 10 patients with previously treated, mainly higher-risk, CLL or SLL. Disclosures See article text.
Ibrutinib monotherapy
In the phase 3 randomized RESONATE trial, investigators compared ibrutinib with ofatumumab, an anti-CD20 antibody, among 391 patients with CLL or small lymphocytic lymphoma (SLL), with crossover allowed. Initial results favored ibrutinib.
Investigators led by John C Byrd, MD, director of the division of hematology at the Ohio State University Comprehensive Cancer Center in Columbus, reported updated data in a poster session at the meeting, now with a median 44 months of follow-up in the ibrutinib arm.
Median PFS was not reached with ibrutinib, compared with 8.1 months with ofatumumab (HR, 0.133). The 3-year rate of PFS for ibrutinib and ofatumumab was 59% and 3%, respectively.
The pattern was generally similar across patients stratified by cytogenetics (deletion of 17p, deletion of 11q, or neither), IGHV and TP53 mutation status, and previous lines of therapy, reported Dr Byrd. The 3-year overall survival rate for ibrutinib was 74%. In analyses adjusted for crossover, patients given the inhibitor had a markedly lower risk of death than did peers given the antibody (HR, 0.37). The overall response rate with ibrutinib was 91%. Although the rate of complete response increased with follow-up, it was still just 9%.
The most common grade 3 or worse adverse events were neutropenia (23%), pneumonia (17%), and anemia, thrombocytopenia, and hypertension (8% each). Major hemorrhage was reported in 2 patients (1%) in the ibrutinib group, and 3 (2%) in the ofatumumab group.
The investigators emphasized that these long-term results “show that extended treatment with ibrutinib is tolerable and continues to show sustained PFS in previously treated patients with CLL regardless of high-risk cytogenetics, adding that traditional poor prognostic factors for survival with chemoimmunotherapy, including del(17p) and del(11q), were not significant factors predictive of PFS outcomes with ibrutinib.
Funding and disclosures: Pharmacyclics funded the trial. Dr Byrd disclosed that he receives research funding from Pharmacyclics and other companies.
Ibrutinib plus ublituximab and umbralisib
Investigators led by Loretta J Nastoupil, MD, tested a triplet consisting of ibrutinib with ublituximab (another anti-CD20 antibody) and umbralisib (TGR-1202), an oral PI3 kinase-delta inhibitor, in a phase 1/1b trial of 38 patients with generally heavily pretreated leukemias and lymphomas, including 20 with CLL or SLL. Notably, 8 patients with CLL (50%) had a 17p or 11q deletion.
The median time on study was 11.1 months, reported Dr Nastoupil, of the department of lymphoma/myeloma at the University of Texas MD Anderson Cancer Center, Houston. The overall response rate for the 19 evaluable patients with CLL or SLL was 100% (complete response in 32%, partial response in 68%). The main grade 3 or 4 adverse events in the entire trial population were neutropenia (18%) and pyrexia (8%). Only two patients discontinued treatment because of adverse events.
“An expansion cohort is ongoing at the highest dose, and we will clearly need more patients treated and longer follow-up to really know the efficacy,” commented invited discussant Jennifer R Brown, MD, PhD, director of the Chronic Lymphocytic Leukemia Center at the Dana-Farber Cancer Institute in Boston.
Funding and disclosures: TG Therapeutics funded the trial. Dr Nastoupil has received honoraria and research funding from TG Therapeutics, and honoraria from Pharmacyclics.
Ibrutinib plus CAR-T cells
Investigators in a pilot trial led by Saar Gill, MD, PhD, of the hospital of the University of Pennsylvania in Philadelphia, tested the combination of ibrutinib with chimeric antigen receptor-T cells (CAR-T cells) against CD19, on the basis of preclinical evidence of synergy. The trial participants were 10 patients with CLL or SLL who had not achieved complete response with ibrutinib. All had a 17p deletion or a p53 mutation, or a complex karyotype, and some had a known ibrutinib resistance mutation.
At 3 months, 8 of 9 evaluable patients (89%) had no evidence of disease in bone marrow, reported Dr Gill. Seven patients (78%) achieved a complete or partial radiographic response in the spleen and lymph nodes. Overall, the treatment was well tolerated. One patient developed grade 4 tumor lysis syndrome, and two developed grade 3 cytokine release syndrome. But, none required anticytokine therapy.
Most patients remain on ibrutinib and are being monitored. In addition, the researchers plan to treat 25 more patients with the same combination.
Funding and disclosures: Novartis funded the trial. Dr Gill disclosed that he receives research funding from Novartis (institutional) and has patents for CAR-T cells for AML.
— Susan London
Pazopanib falls short as adjuvant therapy for high-risk RCC
Key clinical point Pazopanib is not efficacious for treating resected high-risk locally advanced RCC. Major finding Compared with placebo, pazopanib started at 600 mg daily did not significantly reduce the risk of DFS events (HR, 0.86; P = .16). Data source A phase 3 randomized controlled trial among 1,538 patients who had undergone nephrectomy for high-risk locally advanced RCC (PROTECT trial). Disclosures Novartis Oncology funded the trial. Dr Motzer disclosed that he is a consultant to Novartis and receives research funding from Novartis (institutional).
The antiangiogenic agent pazopanib is not efficacious when used as adjuvant therapy for resected renal cell carcinoma (RCC) with features that confer a high risk of recurrence, investigators in the PROTECT investigators reported at the meeting. “The trial did not meet its primary endpoint,” concluded lead investigator Robert J Motzer, MD, of Memorial Sloan-Kettering Cancer Center in New York. “Pazopanib is not recommended for adjuvant therapy following resection of locally advanced RCC.”
Adjuvant use of other agents in this class has yielded mixed results, Dr Motzer noted, citing the earlier ASSURE trial found that neither sunitinib nor sorafenib improved disease-free survival (DFS) or overall survival (Lancet 2016;387:2008-2016), and the S-TRAC trial that found that sunitinib improved DFS (N Engl J Med. 2016;375:2246-2254).
Pazopanib is an oral multitargeted tyrosine kinase inhibitor active against the vascular endothelial growth factor receptor (VEGFR). The PROTECT trial included 1,538 patients with resected pT2 (high grade), pT3, or greater nonmetastatic clear cell RCC, a highly vascular tumor typically reliant on aberrant signaling in the VEGF pathway. The patients were assigned evenly to receive pazopanib or placebo for 1 year. The starting dose was lowered from 800 mg daily to 600 mg daily (with escalation permitted) after 403 patients had been treated.
In intention-to-treat analysis among patients started on the 600-mg dose and having a median follow-up of about 31 months, DFS was better with pazopanib but not significantly so (HR, 0.86; P = .16). In secondary analyses, pazopanib had a significant DFS benefit in patients started on the 800-mg dose (HR, 0.69; P = .02) and among the entire trial population started on either dose (HR, 0.80; P = .01).
One possible explanation for the differing results seen with the 2 doses was the difference in follow-up, because the 800-mg group was treated earlier in the trial, said Dr Motzer. But with an additional year of blinded follow-up, the benefit in the 600-mg group diminished, but not in the 800-mg group.
Another possibility was the somewhat better performance of the placebo group used for comparison with the lower dose: the 3-year DFS rate with placebo was 64% for the 600-mg comparison but 56% for the 800-mg comparison. “One factor that could explain differences in the outcomes of the placebo groups includes unidentified patient demographic characteristics,” Dr Motzer added.
Overall survival was statistically indistinguishable between the pazopanib and placebo groups, regardless of dose. However, “the results are inconclusive as the data are not yet mature,” he said, with a definitive analysis planned for 2019.
Patients started on the 600-mg dose of pazopanib had a higher rate of grade 3 or 4 adverse events overall compared with those given placebo (60% vs 21%, respectively), driven in part by higher rates of hypertension and increased alanine aminotransferase levels. “Although the intent of modifying the protocol dose of pazopanib from 800 mg to 600 mg was to reduce the rate of discontinuation and improve the safety profile ... both cohorts had similar discontinuation rates and safety profiles,” Dr Motzer noted.
A QoL analysis for the 600-mg group using the 19-item Functional Assessment of Cancer Therapy Kidney Symptom Index showed values were consistently lower with the drug than with placebo during treatment, with a crossing of the threshold for a minimally important difference at week 8. Pharmacokinetic analyses from the trial, reported in a poster at the meeting, showed that in the group starting pazopanib at 600 mg, DFS was longer in patients who achieved higher drug trough concentrations at week 3 or 5.
— Susan London
Enasidenib data in IDH2-mutated AML are basis for combination therapy trials
Enasidenib was a well-tolerated, efficacious alternative to cytotoxic chemotherapy for patients with IDH2-mutated relapsed or refractory acute myeloid leukemia (AML), the results of a phase 1/2 study showed.
The Food and Drug Administration recently approved enasidenib (Idhifa, formerly AG-221; Celgene) for the treatment of adult patients with relapsed or refractory AML having an IDH2 mutation as detected by a companion diagnostic test (RealTime IDH2 Assay; Abbott Molecular Inc.). The drug was generally safe and well tolerated, according to reported trial results (Blood. 2017 Aug. 10;130[6]:722-31). The main grade 3-4 enasidenib-related adverse events were hyperbilirubinemia (12%) and IDH inhibitor–associated differentiation syndrome (6%).
The drug is an oral selective inhibitor of mutant isocitrate dehydrogenase 2 (IDH2) enzymes that is not myeloablative. Although enasidenib appears to work by inducing myeloblast differentiation, predictors of response to the drug generally remain elusive, according to Eytan M. Stein, MD, a hematologic oncologist at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
About 12% of patients with AML have an IDH2 mutation. This genetic defect leads to accumulation of the metabolite 2-hydroxyglutarate (2-HG), causing DNA and histone hypermethylation. Hypermethylation, in turn, blocks hematopoietic cellular differentiation.
In a phase 1/2 trial sponsored by Celgene and Agios Pharmaceuticals, the investigators tested daily enasidenib monotherapy among 239 patients with IDH2-mutated advanced myeloid malignancies.
Among the 176 patients with relapsed or refractory AML (more than half of whom had already received at least two regimens directed against the disease), the overall response rate was 40.3%, and the complete response/remission rate was 19.3%. The median duration of response was 5.8 months.
Evaluation of serial bone marrow aspirates showed that responses were associated with myeloid cellular differentiation and maturation, generally without evidence of aplasia or hypoplasia.
With a median follow-up of 7.7 months, median overall survival was 9.3 months in the entire AML cohort and 19.7 months in the subset achieving complete response/remission. Ten percent of patients went on to allogeneic stem cell transplantation.
Although nearly all patients had a marked reduction in plasma levels of 2-HG, the extent of reduction did not predict response, suggesting that this metabolite is not a biomarker for benefit, and additional mechanisms are at play.
“Continuous daily enasidenib treatment was generally well tolerated and induced hematologic responses in patients for whom prior AML therapy had failed,” Dr. Stein and his coinvestigators wrote. “Inducing differentiation of myeloblasts, not cytotoxicity, seems to drive the clinical efficacy of enasidenib.”
They noted that an ongoing multicenter, randomized phase 3 trial, called IDHENTIFY (NCT02577406), is testing enasidenib against conventional regimens in older adults with late-stage AML harboring an IDH2 mutation.
In a companion translational study, investigators led by Michael D. Amatangelo, PhD, a scientist with Celgene in Summit, N.J., further explored mechanisms of enasidenib response and sought to identify alternative biomarkers for benefit in the AML cohort. They measured 2-HG levels, mutant IDH2 allele burden, and co-occurring somatic mutations in samples serially collected during the trial, and used flow cytometry to assess inhibition of mutant IDH2 on hematopoietic differentiation.
Enasidenib therapy induced 2-HG suppression regardless of whether patients’ IDH2 mutation affected the R140 or the R172 residue, according to reported results (Blood. 2017 Aug. 10;130[6]:732-41). However, analyses confirmed that 2-HG suppression alone did not predict response, as most nonresponders also had suppression.
In some patients with complete remission, mutant IDH2 persisted, but there was normalization of hematopoietic stem and progenitor compartments, and emergence of functional neutrophils having the IDH2 mutation. And some patients saw a reduction in mutant IDH2 allele burden, with levels remaining undetectable during response.
Analyses failed to identify any single mutation predictive of response to enasidenib. However, patients who did not achieve a response more commonly had mutations in NRAS and other MAPK pathway effectors, suggesting that RAS signaling plays a role in primary resistance to the drug.
“Although this is only a subgroup analysis of a large single-arm experience, taken together, the clinical response and translational data demonstrate that single-agent [mutant IDH2] inhibition by enasidenib in [relapsed or refractory AML] represents a critical and novel differentiation therapy,” Dr. Amatangelo and his coinvestigators wrote.
“Although enasidenib responses are clinically durable, the genetic heterogeneity observed in our patients suggests that combination with other therapies may be required to achieve long-term disease remission in more patients,” they added. “Current clinical studies combining enasidenib with combination chemotherapy or azacitidine (NCT02677922 and NCT02632708) and future orthogonal targeted therapies will address this question.”
Dr. Stein disclosed that he received grants and personal fees from Celgene and Agios Pharmaceuticals. Dr. Amatangelo disclosed that he is employed by and owns equity in Celgene.
Stein et al. provide for the first time answers to the questions of whether IDH inhibitors are tolerated in patients and whether these compounds induce clinical responses and, excitingly, both answers are positive.
Data from the phase 1/2 trial are encouraging, given that the population studied has a notoriously dismal prognosis when treated with conventional modalities.
Findings from the companion translational study suggest heterogeneity in the dynamics of response to enasidenib, with some responding patients retaining mutant alleles in mature cells, and a smaller group of responding patients clearing the mutation.
These findings raise the important question of whether enasidenib can target leukemic stem cells, the holy grail of AML therapy. Additional questions arising from the research pertain to the long-term effects of the drug, whether it will induce clonal selection, and how it affects leukemic cells that lack an IDH2 mutation.
Together, the results of these studies argue for the further clinical exploration of IDH inhibitors. It is expected that for more powerful responses, differentiation-based IDH2 inhibition will need to be combined with orthogonal treatment modalities, such as standard chemotherapy or other types of mechanism-based targeted therapy. Obviously, in the next phase, enasidenib-based regimens should be compared head to head to standard regimens in a randomized controlled fashion. Such studies, and studies with other IDH2 and IDH1 inhibitors, will address the full role of IDH inhibition in AML treatment.
Bas J. Wouters, MD, PhD, a hematologist at Erasmus University Medical Center, Rotterdam, the Netherlands, made his remarks in a related commentary ( Blood. 2017;130:693-4 ). Dr. Wouters reported no competing financial interests.
Stein et al. provide for the first time answers to the questions of whether IDH inhibitors are tolerated in patients and whether these compounds induce clinical responses and, excitingly, both answers are positive.
Data from the phase 1/2 trial are encouraging, given that the population studied has a notoriously dismal prognosis when treated with conventional modalities.
Findings from the companion translational study suggest heterogeneity in the dynamics of response to enasidenib, with some responding patients retaining mutant alleles in mature cells, and a smaller group of responding patients clearing the mutation.
These findings raise the important question of whether enasidenib can target leukemic stem cells, the holy grail of AML therapy. Additional questions arising from the research pertain to the long-term effects of the drug, whether it will induce clonal selection, and how it affects leukemic cells that lack an IDH2 mutation.
Together, the results of these studies argue for the further clinical exploration of IDH inhibitors. It is expected that for more powerful responses, differentiation-based IDH2 inhibition will need to be combined with orthogonal treatment modalities, such as standard chemotherapy or other types of mechanism-based targeted therapy. Obviously, in the next phase, enasidenib-based regimens should be compared head to head to standard regimens in a randomized controlled fashion. Such studies, and studies with other IDH2 and IDH1 inhibitors, will address the full role of IDH inhibition in AML treatment.
Bas J. Wouters, MD, PhD, a hematologist at Erasmus University Medical Center, Rotterdam, the Netherlands, made his remarks in a related commentary ( Blood. 2017;130:693-4 ). Dr. Wouters reported no competing financial interests.
Stein et al. provide for the first time answers to the questions of whether IDH inhibitors are tolerated in patients and whether these compounds induce clinical responses and, excitingly, both answers are positive.
Data from the phase 1/2 trial are encouraging, given that the population studied has a notoriously dismal prognosis when treated with conventional modalities.
Findings from the companion translational study suggest heterogeneity in the dynamics of response to enasidenib, with some responding patients retaining mutant alleles in mature cells, and a smaller group of responding patients clearing the mutation.
These findings raise the important question of whether enasidenib can target leukemic stem cells, the holy grail of AML therapy. Additional questions arising from the research pertain to the long-term effects of the drug, whether it will induce clonal selection, and how it affects leukemic cells that lack an IDH2 mutation.
Together, the results of these studies argue for the further clinical exploration of IDH inhibitors. It is expected that for more powerful responses, differentiation-based IDH2 inhibition will need to be combined with orthogonal treatment modalities, such as standard chemotherapy or other types of mechanism-based targeted therapy. Obviously, in the next phase, enasidenib-based regimens should be compared head to head to standard regimens in a randomized controlled fashion. Such studies, and studies with other IDH2 and IDH1 inhibitors, will address the full role of IDH inhibition in AML treatment.
Bas J. Wouters, MD, PhD, a hematologist at Erasmus University Medical Center, Rotterdam, the Netherlands, made his remarks in a related commentary ( Blood. 2017;130:693-4 ). Dr. Wouters reported no competing financial interests.
Enasidenib was a well-tolerated, efficacious alternative to cytotoxic chemotherapy for patients with IDH2-mutated relapsed or refractory acute myeloid leukemia (AML), the results of a phase 1/2 study showed.
The Food and Drug Administration recently approved enasidenib (Idhifa, formerly AG-221; Celgene) for the treatment of adult patients with relapsed or refractory AML having an IDH2 mutation as detected by a companion diagnostic test (RealTime IDH2 Assay; Abbott Molecular Inc.). The drug was generally safe and well tolerated, according to reported trial results (Blood. 2017 Aug. 10;130[6]:722-31). The main grade 3-4 enasidenib-related adverse events were hyperbilirubinemia (12%) and IDH inhibitor–associated differentiation syndrome (6%).
The drug is an oral selective inhibitor of mutant isocitrate dehydrogenase 2 (IDH2) enzymes that is not myeloablative. Although enasidenib appears to work by inducing myeloblast differentiation, predictors of response to the drug generally remain elusive, according to Eytan M. Stein, MD, a hematologic oncologist at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
About 12% of patients with AML have an IDH2 mutation. This genetic defect leads to accumulation of the metabolite 2-hydroxyglutarate (2-HG), causing DNA and histone hypermethylation. Hypermethylation, in turn, blocks hematopoietic cellular differentiation.
In a phase 1/2 trial sponsored by Celgene and Agios Pharmaceuticals, the investigators tested daily enasidenib monotherapy among 239 patients with IDH2-mutated advanced myeloid malignancies.
Among the 176 patients with relapsed or refractory AML (more than half of whom had already received at least two regimens directed against the disease), the overall response rate was 40.3%, and the complete response/remission rate was 19.3%. The median duration of response was 5.8 months.
Evaluation of serial bone marrow aspirates showed that responses were associated with myeloid cellular differentiation and maturation, generally without evidence of aplasia or hypoplasia.
With a median follow-up of 7.7 months, median overall survival was 9.3 months in the entire AML cohort and 19.7 months in the subset achieving complete response/remission. Ten percent of patients went on to allogeneic stem cell transplantation.
Although nearly all patients had a marked reduction in plasma levels of 2-HG, the extent of reduction did not predict response, suggesting that this metabolite is not a biomarker for benefit, and additional mechanisms are at play.
“Continuous daily enasidenib treatment was generally well tolerated and induced hematologic responses in patients for whom prior AML therapy had failed,” Dr. Stein and his coinvestigators wrote. “Inducing differentiation of myeloblasts, not cytotoxicity, seems to drive the clinical efficacy of enasidenib.”
They noted that an ongoing multicenter, randomized phase 3 trial, called IDHENTIFY (NCT02577406), is testing enasidenib against conventional regimens in older adults with late-stage AML harboring an IDH2 mutation.
In a companion translational study, investigators led by Michael D. Amatangelo, PhD, a scientist with Celgene in Summit, N.J., further explored mechanisms of enasidenib response and sought to identify alternative biomarkers for benefit in the AML cohort. They measured 2-HG levels, mutant IDH2 allele burden, and co-occurring somatic mutations in samples serially collected during the trial, and used flow cytometry to assess inhibition of mutant IDH2 on hematopoietic differentiation.
Enasidenib therapy induced 2-HG suppression regardless of whether patients’ IDH2 mutation affected the R140 or the R172 residue, according to reported results (Blood. 2017 Aug. 10;130[6]:732-41). However, analyses confirmed that 2-HG suppression alone did not predict response, as most nonresponders also had suppression.
In some patients with complete remission, mutant IDH2 persisted, but there was normalization of hematopoietic stem and progenitor compartments, and emergence of functional neutrophils having the IDH2 mutation. And some patients saw a reduction in mutant IDH2 allele burden, with levels remaining undetectable during response.
Analyses failed to identify any single mutation predictive of response to enasidenib. However, patients who did not achieve a response more commonly had mutations in NRAS and other MAPK pathway effectors, suggesting that RAS signaling plays a role in primary resistance to the drug.
“Although this is only a subgroup analysis of a large single-arm experience, taken together, the clinical response and translational data demonstrate that single-agent [mutant IDH2] inhibition by enasidenib in [relapsed or refractory AML] represents a critical and novel differentiation therapy,” Dr. Amatangelo and his coinvestigators wrote.
“Although enasidenib responses are clinically durable, the genetic heterogeneity observed in our patients suggests that combination with other therapies may be required to achieve long-term disease remission in more patients,” they added. “Current clinical studies combining enasidenib with combination chemotherapy or azacitidine (NCT02677922 and NCT02632708) and future orthogonal targeted therapies will address this question.”
Dr. Stein disclosed that he received grants and personal fees from Celgene and Agios Pharmaceuticals. Dr. Amatangelo disclosed that he is employed by and owns equity in Celgene.
Enasidenib was a well-tolerated, efficacious alternative to cytotoxic chemotherapy for patients with IDH2-mutated relapsed or refractory acute myeloid leukemia (AML), the results of a phase 1/2 study showed.
The Food and Drug Administration recently approved enasidenib (Idhifa, formerly AG-221; Celgene) for the treatment of adult patients with relapsed or refractory AML having an IDH2 mutation as detected by a companion diagnostic test (RealTime IDH2 Assay; Abbott Molecular Inc.). The drug was generally safe and well tolerated, according to reported trial results (Blood. 2017 Aug. 10;130[6]:722-31). The main grade 3-4 enasidenib-related adverse events were hyperbilirubinemia (12%) and IDH inhibitor–associated differentiation syndrome (6%).
The drug is an oral selective inhibitor of mutant isocitrate dehydrogenase 2 (IDH2) enzymes that is not myeloablative. Although enasidenib appears to work by inducing myeloblast differentiation, predictors of response to the drug generally remain elusive, according to Eytan M. Stein, MD, a hematologic oncologist at Memorial Sloan Kettering Cancer Center, New York, and his coauthors.
About 12% of patients with AML have an IDH2 mutation. This genetic defect leads to accumulation of the metabolite 2-hydroxyglutarate (2-HG), causing DNA and histone hypermethylation. Hypermethylation, in turn, blocks hematopoietic cellular differentiation.
In a phase 1/2 trial sponsored by Celgene and Agios Pharmaceuticals, the investigators tested daily enasidenib monotherapy among 239 patients with IDH2-mutated advanced myeloid malignancies.
Among the 176 patients with relapsed or refractory AML (more than half of whom had already received at least two regimens directed against the disease), the overall response rate was 40.3%, and the complete response/remission rate was 19.3%. The median duration of response was 5.8 months.
Evaluation of serial bone marrow aspirates showed that responses were associated with myeloid cellular differentiation and maturation, generally without evidence of aplasia or hypoplasia.
With a median follow-up of 7.7 months, median overall survival was 9.3 months in the entire AML cohort and 19.7 months in the subset achieving complete response/remission. Ten percent of patients went on to allogeneic stem cell transplantation.
Although nearly all patients had a marked reduction in plasma levels of 2-HG, the extent of reduction did not predict response, suggesting that this metabolite is not a biomarker for benefit, and additional mechanisms are at play.
“Continuous daily enasidenib treatment was generally well tolerated and induced hematologic responses in patients for whom prior AML therapy had failed,” Dr. Stein and his coinvestigators wrote. “Inducing differentiation of myeloblasts, not cytotoxicity, seems to drive the clinical efficacy of enasidenib.”
They noted that an ongoing multicenter, randomized phase 3 trial, called IDHENTIFY (NCT02577406), is testing enasidenib against conventional regimens in older adults with late-stage AML harboring an IDH2 mutation.
In a companion translational study, investigators led by Michael D. Amatangelo, PhD, a scientist with Celgene in Summit, N.J., further explored mechanisms of enasidenib response and sought to identify alternative biomarkers for benefit in the AML cohort. They measured 2-HG levels, mutant IDH2 allele burden, and co-occurring somatic mutations in samples serially collected during the trial, and used flow cytometry to assess inhibition of mutant IDH2 on hematopoietic differentiation.
Enasidenib therapy induced 2-HG suppression regardless of whether patients’ IDH2 mutation affected the R140 or the R172 residue, according to reported results (Blood. 2017 Aug. 10;130[6]:732-41). However, analyses confirmed that 2-HG suppression alone did not predict response, as most nonresponders also had suppression.
In some patients with complete remission, mutant IDH2 persisted, but there was normalization of hematopoietic stem and progenitor compartments, and emergence of functional neutrophils having the IDH2 mutation. And some patients saw a reduction in mutant IDH2 allele burden, with levels remaining undetectable during response.
Analyses failed to identify any single mutation predictive of response to enasidenib. However, patients who did not achieve a response more commonly had mutations in NRAS and other MAPK pathway effectors, suggesting that RAS signaling plays a role in primary resistance to the drug.
“Although this is only a subgroup analysis of a large single-arm experience, taken together, the clinical response and translational data demonstrate that single-agent [mutant IDH2] inhibition by enasidenib in [relapsed or refractory AML] represents a critical and novel differentiation therapy,” Dr. Amatangelo and his coinvestigators wrote.
“Although enasidenib responses are clinically durable, the genetic heterogeneity observed in our patients suggests that combination with other therapies may be required to achieve long-term disease remission in more patients,” they added. “Current clinical studies combining enasidenib with combination chemotherapy or azacitidine (NCT02677922 and NCT02632708) and future orthogonal targeted therapies will address this question.”
Dr. Stein disclosed that he received grants and personal fees from Celgene and Agios Pharmaceuticals. Dr. Amatangelo disclosed that he is employed by and owns equity in Celgene.
FROM BLOOD
Key clinical point:
Major finding: The overall response rate was 40.3%; 2-HG levels and co-occurring mutations were not reliable predictors of response.
Data source: A phase 1/2 trial of enasidenib monotherapy including 176 patients with relapsed or refractory IDH2-mutated AML, and a companion translational study of mechanisms and biomarkers of response in the same patients.
Disclosures: Dr. Stein disclosed that he received grants and personal fees from Celgene and Agios Pharmaceuticals, the trial sponsors. Dr. Amatangelo disclosed that he is employed by and owns equity in Celgene. The study was supported by the National Institutes of Health, National Cancer Institute.
Sequential pazopanib and everolimus nets good survival in metastatic RCC
Sequential treatment with pazopanib and everolimus yields a median overall survival exceeding 2 years in predominantly older and sicker patients with metastatic renal cell carcinoma (RCC) treated in real-world settings, according to results of an Italian multicenter cohort study.
“These data confirmed that pazopanib was effective, even in reduced dosing, and well tolerated and suggested that everolimus may represent an opportunity to continue a therapy when patients cannot further tolerate angiogenesis inhibitors or develop a resistance,” wrote Sabrina Rossetti, MD, of the Istituto Nazionale Tumori Fondazione G. Pascale, Naples, and associates (Front Pharmacol. 2017 Jul 20;8:484).
“Overall, the sequential therapy showed favorable clinical outcomes and a good safety profile and may be feasible even for elderly patients or with multiple comorbidities,” they said.
The investigators prospectively enrolled 31 consecutive patients with newly diagnosed metastatic RCC. They had a median age of 68 years. Fully 73.3% underwent nephrectomy before treatment; 87.1% had at least one comorbidity, and 25.8% had at least three of them.
All patients were treated with the antiangiogenic tyrosine kinase inhibitor pazopanib (Votrient) as first-line therapy and, after disease progression on that agent or discontinuation for toxicity, with the mTOR inhibitor everolimus (Afinitor) as second-line therapy.
The median overall survival with the two-drug sequence was 26.5 months. Median progression-free survival was 10.6 months with pazopanib and 5.3 months with everolimus.
Patients were able to continue on pazopanib for a median time of 8.1 months, with 31% requiring dose reduction. They were able to continue on everolimus for a median time of 4.4 months, with 16% requiring dose reduction.
Main adverse events of any grade on pazopanib were hypertension (48.4%), fatigue (32.2%), and thyroid disorders (19.3%). Those on everolimus were anemia (32.2%), hypercholesterolemia (22.6%), and hyperglycemia (22.6%).
“The choice of second-line treatment in the new therapeutic paradigm is dramatically changed with the approval of new drugs, such as nivolumab and cabozantinib,” noted Dr. Rossetti and colleagues. “The next step in optimizing mRCC management would be the identification of new prognostic and predictive factors to detect a personalized sequence for each patient.”
[email protected]
Sequential treatment with pazopanib and everolimus yields a median overall survival exceeding 2 years in predominantly older and sicker patients with metastatic renal cell carcinoma (RCC) treated in real-world settings, according to results of an Italian multicenter cohort study.
“These data confirmed that pazopanib was effective, even in reduced dosing, and well tolerated and suggested that everolimus may represent an opportunity to continue a therapy when patients cannot further tolerate angiogenesis inhibitors or develop a resistance,” wrote Sabrina Rossetti, MD, of the Istituto Nazionale Tumori Fondazione G. Pascale, Naples, and associates (Front Pharmacol. 2017 Jul 20;8:484).
“Overall, the sequential therapy showed favorable clinical outcomes and a good safety profile and may be feasible even for elderly patients or with multiple comorbidities,” they said.
The investigators prospectively enrolled 31 consecutive patients with newly diagnosed metastatic RCC. They had a median age of 68 years. Fully 73.3% underwent nephrectomy before treatment; 87.1% had at least one comorbidity, and 25.8% had at least three of them.
All patients were treated with the antiangiogenic tyrosine kinase inhibitor pazopanib (Votrient) as first-line therapy and, after disease progression on that agent or discontinuation for toxicity, with the mTOR inhibitor everolimus (Afinitor) as second-line therapy.
The median overall survival with the two-drug sequence was 26.5 months. Median progression-free survival was 10.6 months with pazopanib and 5.3 months with everolimus.
Patients were able to continue on pazopanib for a median time of 8.1 months, with 31% requiring dose reduction. They were able to continue on everolimus for a median time of 4.4 months, with 16% requiring dose reduction.
Main adverse events of any grade on pazopanib were hypertension (48.4%), fatigue (32.2%), and thyroid disorders (19.3%). Those on everolimus were anemia (32.2%), hypercholesterolemia (22.6%), and hyperglycemia (22.6%).
“The choice of second-line treatment in the new therapeutic paradigm is dramatically changed with the approval of new drugs, such as nivolumab and cabozantinib,” noted Dr. Rossetti and colleagues. “The next step in optimizing mRCC management would be the identification of new prognostic and predictive factors to detect a personalized sequence for each patient.”
[email protected]
Sequential treatment with pazopanib and everolimus yields a median overall survival exceeding 2 years in predominantly older and sicker patients with metastatic renal cell carcinoma (RCC) treated in real-world settings, according to results of an Italian multicenter cohort study.
“These data confirmed that pazopanib was effective, even in reduced dosing, and well tolerated and suggested that everolimus may represent an opportunity to continue a therapy when patients cannot further tolerate angiogenesis inhibitors or develop a resistance,” wrote Sabrina Rossetti, MD, of the Istituto Nazionale Tumori Fondazione G. Pascale, Naples, and associates (Front Pharmacol. 2017 Jul 20;8:484).
“Overall, the sequential therapy showed favorable clinical outcomes and a good safety profile and may be feasible even for elderly patients or with multiple comorbidities,” they said.
The investigators prospectively enrolled 31 consecutive patients with newly diagnosed metastatic RCC. They had a median age of 68 years. Fully 73.3% underwent nephrectomy before treatment; 87.1% had at least one comorbidity, and 25.8% had at least three of them.
All patients were treated with the antiangiogenic tyrosine kinase inhibitor pazopanib (Votrient) as first-line therapy and, after disease progression on that agent or discontinuation for toxicity, with the mTOR inhibitor everolimus (Afinitor) as second-line therapy.
The median overall survival with the two-drug sequence was 26.5 months. Median progression-free survival was 10.6 months with pazopanib and 5.3 months with everolimus.
Patients were able to continue on pazopanib for a median time of 8.1 months, with 31% requiring dose reduction. They were able to continue on everolimus for a median time of 4.4 months, with 16% requiring dose reduction.
Main adverse events of any grade on pazopanib were hypertension (48.4%), fatigue (32.2%), and thyroid disorders (19.3%). Those on everolimus were anemia (32.2%), hypercholesterolemia (22.6%), and hyperglycemia (22.6%).
“The choice of second-line treatment in the new therapeutic paradigm is dramatically changed with the approval of new drugs, such as nivolumab and cabozantinib,” noted Dr. Rossetti and colleagues. “The next step in optimizing mRCC management would be the identification of new prognostic and predictive factors to detect a personalized sequence for each patient.”
[email protected]
FRONTIERS IN PHARMACOLOGY
Key clinical point:
Major finding: Median overall survival with first-line pazopanib followed by second-line everolimus was 26.5 months.
Data source: A real-world prospective multicenter cohort study of 31 patients with untreated metastatic RCC.
Disclosures: Dr. Rossetti and colleagues disclosed no relevant conflicts of interest. The study was supported by Novartis Farma SpA.
LIFSCREEN data support broader cancer screening in Li-Fraumeni syndrome
Broader cancer screening of individuals with Li-Fraumeni syndrome (LFS), with or without whole-body magnetic resonance imaging, has a good diagnostic yield and identifies a wide range of cancers, according to a preliminary analysis of the ongoing LIFSCREEN phase 3, randomized, controlled trial.
Investigators led by Olivier Caron, MD, chair of the oncogenetics committee, department of medical oncology, at the Gustave Roussy University Hospital in Villejuif, France, enrolled in the trial 107 individuals from 75 families carrying a TP53 mutation, a genetic aberration commonly present in LFS that confers heightened risk of a variety of malignancies.
Participants had a median age at baseline of 32.9 years, with a range from 5 to 67 years. Fully 98% had a family history of cancer, and 48% had a personal history of cancer.
The participants were assigned to 5 years of standard screening – annual clinical examination, abdomen and pelvis ultrasound, brain MRI, complete blood cell count, and, for women older than 20 years, breast ultrasound and MRI – or intensive screening, entailing the addition of diffusion whole-body MRI.
At the time of the preliminary analysis, 15 patients had undergone only one round of screening; 35, two rounds; 19, three rounds; 24, four rounds; and 7, five rounds, Dr. Caron and associates reported in a research letter (JAMA Oncol. 2017; Aug 3 doi: 10.1001/jamaoncol.2017.1358).
Collectively, this amounted to 226.4 person-years of follow-up.
Screening with either trial strategy (with or without whole-body MRI) led to diagnosis of 23 new primary cancers in 20 patients. Nearly half of the total (12 cancers) were detected at the first round. Patients had a median age of 39.8 at the new cancer diagnosis, with a range from 6 to 70 years.
Of the new cancers, 10 belonged to the core LFS spectrum of breast cancer, sarcoma, and brain tumors. However, the other 13 were outside that spectrum, for example, lung adenocarcinomas, all seen in never or light smokers, and leukemias. Screening also detected three relapses of previous cancers.
Analyses further showed that prior cancer diagnosis was not a reliable marker for risk of new primaries. Although 12 of the patients with a screening-detected new primary had a personal cancer history, 8 did not (P = .22).
“The proportion and diversity of off–core LFS spectrum cancers detected in TP53 mutation carriers as reported by others give growing evidence of a broader LFS spectrum, in agreement with the permissive role of TP53 mutations,” write Dr. Caron and colleagues, who report having no relevant disclosures. “Our observations seem to support recent moves toward broader cancer screening in TP53 mutation carriers.”
The investigators continue to collect data in LIFSCREEN and plan to undertake main analysis later this year. “Our final analysis will help to determine the benefits and drawbacks (mostly related to false-positive test results) of whole-body MRI in TP53 mutation carrier surveillance,” they conclude. “Studies focused on TP53 mutation penetrance, using methods limiting selection bias, are required to refine cancer risks to improve TP53 mutation carrier management.”
Broader cancer screening of individuals with Li-Fraumeni syndrome (LFS), with or without whole-body magnetic resonance imaging, has a good diagnostic yield and identifies a wide range of cancers, according to a preliminary analysis of the ongoing LIFSCREEN phase 3, randomized, controlled trial.
Investigators led by Olivier Caron, MD, chair of the oncogenetics committee, department of medical oncology, at the Gustave Roussy University Hospital in Villejuif, France, enrolled in the trial 107 individuals from 75 families carrying a TP53 mutation, a genetic aberration commonly present in LFS that confers heightened risk of a variety of malignancies.
Participants had a median age at baseline of 32.9 years, with a range from 5 to 67 years. Fully 98% had a family history of cancer, and 48% had a personal history of cancer.
The participants were assigned to 5 years of standard screening – annual clinical examination, abdomen and pelvis ultrasound, brain MRI, complete blood cell count, and, for women older than 20 years, breast ultrasound and MRI – or intensive screening, entailing the addition of diffusion whole-body MRI.
At the time of the preliminary analysis, 15 patients had undergone only one round of screening; 35, two rounds; 19, three rounds; 24, four rounds; and 7, five rounds, Dr. Caron and associates reported in a research letter (JAMA Oncol. 2017; Aug 3 doi: 10.1001/jamaoncol.2017.1358).
Collectively, this amounted to 226.4 person-years of follow-up.
Screening with either trial strategy (with or without whole-body MRI) led to diagnosis of 23 new primary cancers in 20 patients. Nearly half of the total (12 cancers) were detected at the first round. Patients had a median age of 39.8 at the new cancer diagnosis, with a range from 6 to 70 years.
Of the new cancers, 10 belonged to the core LFS spectrum of breast cancer, sarcoma, and brain tumors. However, the other 13 were outside that spectrum, for example, lung adenocarcinomas, all seen in never or light smokers, and leukemias. Screening also detected three relapses of previous cancers.
Analyses further showed that prior cancer diagnosis was not a reliable marker for risk of new primaries. Although 12 of the patients with a screening-detected new primary had a personal cancer history, 8 did not (P = .22).
“The proportion and diversity of off–core LFS spectrum cancers detected in TP53 mutation carriers as reported by others give growing evidence of a broader LFS spectrum, in agreement with the permissive role of TP53 mutations,” write Dr. Caron and colleagues, who report having no relevant disclosures. “Our observations seem to support recent moves toward broader cancer screening in TP53 mutation carriers.”
The investigators continue to collect data in LIFSCREEN and plan to undertake main analysis later this year. “Our final analysis will help to determine the benefits and drawbacks (mostly related to false-positive test results) of whole-body MRI in TP53 mutation carrier surveillance,” they conclude. “Studies focused on TP53 mutation penetrance, using methods limiting selection bias, are required to refine cancer risks to improve TP53 mutation carrier management.”
Broader cancer screening of individuals with Li-Fraumeni syndrome (LFS), with or without whole-body magnetic resonance imaging, has a good diagnostic yield and identifies a wide range of cancers, according to a preliminary analysis of the ongoing LIFSCREEN phase 3, randomized, controlled trial.
Investigators led by Olivier Caron, MD, chair of the oncogenetics committee, department of medical oncology, at the Gustave Roussy University Hospital in Villejuif, France, enrolled in the trial 107 individuals from 75 families carrying a TP53 mutation, a genetic aberration commonly present in LFS that confers heightened risk of a variety of malignancies.
Participants had a median age at baseline of 32.9 years, with a range from 5 to 67 years. Fully 98% had a family history of cancer, and 48% had a personal history of cancer.
The participants were assigned to 5 years of standard screening – annual clinical examination, abdomen and pelvis ultrasound, brain MRI, complete blood cell count, and, for women older than 20 years, breast ultrasound and MRI – or intensive screening, entailing the addition of diffusion whole-body MRI.
At the time of the preliminary analysis, 15 patients had undergone only one round of screening; 35, two rounds; 19, three rounds; 24, four rounds; and 7, five rounds, Dr. Caron and associates reported in a research letter (JAMA Oncol. 2017; Aug 3 doi: 10.1001/jamaoncol.2017.1358).
Collectively, this amounted to 226.4 person-years of follow-up.
Screening with either trial strategy (with or without whole-body MRI) led to diagnosis of 23 new primary cancers in 20 patients. Nearly half of the total (12 cancers) were detected at the first round. Patients had a median age of 39.8 at the new cancer diagnosis, with a range from 6 to 70 years.
Of the new cancers, 10 belonged to the core LFS spectrum of breast cancer, sarcoma, and brain tumors. However, the other 13 were outside that spectrum, for example, lung adenocarcinomas, all seen in never or light smokers, and leukemias. Screening also detected three relapses of previous cancers.
Analyses further showed that prior cancer diagnosis was not a reliable marker for risk of new primaries. Although 12 of the patients with a screening-detected new primary had a personal cancer history, 8 did not (P = .22).
“The proportion and diversity of off–core LFS spectrum cancers detected in TP53 mutation carriers as reported by others give growing evidence of a broader LFS spectrum, in agreement with the permissive role of TP53 mutations,” write Dr. Caron and colleagues, who report having no relevant disclosures. “Our observations seem to support recent moves toward broader cancer screening in TP53 mutation carriers.”
The investigators continue to collect data in LIFSCREEN and plan to undertake main analysis later this year. “Our final analysis will help to determine the benefits and drawbacks (mostly related to false-positive test results) of whole-body MRI in TP53 mutation carrier surveillance,” they conclude. “Studies focused on TP53 mutation penetrance, using methods limiting selection bias, are required to refine cancer risks to improve TP53 mutation carrier management.”
FROM JAMA ONCOLOGY
Key clinical point:
Major finding: A total of 23 new primary cancers were diagnosed in 20 patients; more than half were outside the core spectrum of Li-Fraumeni syndrome.
Data source: A preliminary analysis of a phase 3, randomized, controlled trial comparing standard and intensive screening among 107 individuals with Li-Fraumeni syndrome carrying a TP53 mutation (LIFSCREEN trial).
Disclosures: The investigators report having no relevant disclosures. The trial was funded by the French Ligue Contre le Cancer.
Immune signature shows good prognostic performance in early-stage NSCLC
A new tumor immune-related gene signature may help take the guesswork out of prognostication in patients with early-stage non–small cell lung cancer (NSCLC), according to a retrospective cohort study.
“Various components of the immune system have been shown to be a determining factor during cancer initiation and progression,” note the investigators, who were led by Bailiang Li, PhD, of Stanford (Calif.) University. “Recent immunotherapies targeting specific immune checkpoints such as programmed death 1 or programmed death ligand 1 have demonstrated a remarkable, durable response in NSCLC. Certain histopathologic patterns, such as intratumoral infiltration by cytotoxic lymphocytes, have also been associated with better prognoses in several cancer types, including NSCLC.”
For the study, the investigators developed and validated an immune-related gene signature using frozen tumors from 2,414 patients with stage I or II nonsquamous NSCLC from 19 public cohorts who underwent resection with negative margins and did not receive any neoadjuvant or adjuvant therapy.
The new signature contained 25 gene pairs consisting of 40 unique immune-related genes, Dr. Li and associates report (JAMA Oncol. 2017 Jul 6. doi: 10.1001/jamaoncol.2017.1609).
Processes such as chemotaxis were enriched among the included genes.
The signature significantly stratified patients into groups that have high and low risks of death during follow-up, both across and within subsets with stage I, IA, IB, or II disease. Relative to counterparts falling into the signature-defined low-risk group, those falling into the signature-defined high-risk group had roughly twice the risk of death after adjustment for clinical and pathologic characteristics, with a hazard ratio range of 1.72 (P less than .001) to 2.36 (P less than .001).
Accuracy of the immune signature exceeded that of two commercialized gene signatures for estimating survival in similar validation cohorts (mean concordance index [C-index], 0.64 vs 0.53 and 0.61).
Moreover, the combination of the immune signature with clinical factors outperformed the signature alone (mean C-index, 0.70 vs 0.63) and another commercialized clinical-molecular combination signature (mean C-index, 0.68 vs 0.65).
“The proposed immune-related gene pair–based signature is a promising prognostic biomarker in nonsquamous NSCLC, including early-stage disease,” concluded the investigators. “Prospective studies are needed to further validate its analytical accuracy for estimating prognoses and to test its clinical utility in individualized management of nonsquamous NSCLC.”
M. Patricia Rivera, MD, FCCP, comments: As lung cancer screening implementation increases, it is expected that the prevalence of early-stage non–small cell lung cancer (NSCLC) will increase.
Currently, adjuvant therapy is reserved for patients with tumors greater than 4 cm or those with N1 disease. Having reliable biomarkers to identify patients at a high risk for recurrence after surgical resection is a significant clinical advantage in order to guide adjuvant therapy. The clinical-immune signature described in this study is an exciting and promising biomarker for estimating overall survival in NSCLC.
M. Patricia Rivera, MD, FCCP, comments: As lung cancer screening implementation increases, it is expected that the prevalence of early-stage non–small cell lung cancer (NSCLC) will increase.
Currently, adjuvant therapy is reserved for patients with tumors greater than 4 cm or those with N1 disease. Having reliable biomarkers to identify patients at a high risk for recurrence after surgical resection is a significant clinical advantage in order to guide adjuvant therapy. The clinical-immune signature described in this study is an exciting and promising biomarker for estimating overall survival in NSCLC.
M. Patricia Rivera, MD, FCCP, comments: As lung cancer screening implementation increases, it is expected that the prevalence of early-stage non–small cell lung cancer (NSCLC) will increase.
Currently, adjuvant therapy is reserved for patients with tumors greater than 4 cm or those with N1 disease. Having reliable biomarkers to identify patients at a high risk for recurrence after surgical resection is a significant clinical advantage in order to guide adjuvant therapy. The clinical-immune signature described in this study is an exciting and promising biomarker for estimating overall survival in NSCLC.
A new tumor immune-related gene signature may help take the guesswork out of prognostication in patients with early-stage non–small cell lung cancer (NSCLC), according to a retrospective cohort study.
“Various components of the immune system have been shown to be a determining factor during cancer initiation and progression,” note the investigators, who were led by Bailiang Li, PhD, of Stanford (Calif.) University. “Recent immunotherapies targeting specific immune checkpoints such as programmed death 1 or programmed death ligand 1 have demonstrated a remarkable, durable response in NSCLC. Certain histopathologic patterns, such as intratumoral infiltration by cytotoxic lymphocytes, have also been associated with better prognoses in several cancer types, including NSCLC.”
For the study, the investigators developed and validated an immune-related gene signature using frozen tumors from 2,414 patients with stage I or II nonsquamous NSCLC from 19 public cohorts who underwent resection with negative margins and did not receive any neoadjuvant or adjuvant therapy.
The new signature contained 25 gene pairs consisting of 40 unique immune-related genes, Dr. Li and associates report (JAMA Oncol. 2017 Jul 6. doi: 10.1001/jamaoncol.2017.1609).
Processes such as chemotaxis were enriched among the included genes.
The signature significantly stratified patients into groups that have high and low risks of death during follow-up, both across and within subsets with stage I, IA, IB, or II disease. Relative to counterparts falling into the signature-defined low-risk group, those falling into the signature-defined high-risk group had roughly twice the risk of death after adjustment for clinical and pathologic characteristics, with a hazard ratio range of 1.72 (P less than .001) to 2.36 (P less than .001).
Accuracy of the immune signature exceeded that of two commercialized gene signatures for estimating survival in similar validation cohorts (mean concordance index [C-index], 0.64 vs 0.53 and 0.61).
Moreover, the combination of the immune signature with clinical factors outperformed the signature alone (mean C-index, 0.70 vs 0.63) and another commercialized clinical-molecular combination signature (mean C-index, 0.68 vs 0.65).
“The proposed immune-related gene pair–based signature is a promising prognostic biomarker in nonsquamous NSCLC, including early-stage disease,” concluded the investigators. “Prospective studies are needed to further validate its analytical accuracy for estimating prognoses and to test its clinical utility in individualized management of nonsquamous NSCLC.”
A new tumor immune-related gene signature may help take the guesswork out of prognostication in patients with early-stage non–small cell lung cancer (NSCLC), according to a retrospective cohort study.
“Various components of the immune system have been shown to be a determining factor during cancer initiation and progression,” note the investigators, who were led by Bailiang Li, PhD, of Stanford (Calif.) University. “Recent immunotherapies targeting specific immune checkpoints such as programmed death 1 or programmed death ligand 1 have demonstrated a remarkable, durable response in NSCLC. Certain histopathologic patterns, such as intratumoral infiltration by cytotoxic lymphocytes, have also been associated with better prognoses in several cancer types, including NSCLC.”
For the study, the investigators developed and validated an immune-related gene signature using frozen tumors from 2,414 patients with stage I or II nonsquamous NSCLC from 19 public cohorts who underwent resection with negative margins and did not receive any neoadjuvant or adjuvant therapy.
The new signature contained 25 gene pairs consisting of 40 unique immune-related genes, Dr. Li and associates report (JAMA Oncol. 2017 Jul 6. doi: 10.1001/jamaoncol.2017.1609).
Processes such as chemotaxis were enriched among the included genes.
The signature significantly stratified patients into groups that have high and low risks of death during follow-up, both across and within subsets with stage I, IA, IB, or II disease. Relative to counterparts falling into the signature-defined low-risk group, those falling into the signature-defined high-risk group had roughly twice the risk of death after adjustment for clinical and pathologic characteristics, with a hazard ratio range of 1.72 (P less than .001) to 2.36 (P less than .001).
Accuracy of the immune signature exceeded that of two commercialized gene signatures for estimating survival in similar validation cohorts (mean concordance index [C-index], 0.64 vs 0.53 and 0.61).
Moreover, the combination of the immune signature with clinical factors outperformed the signature alone (mean C-index, 0.70 vs 0.63) and another commercialized clinical-molecular combination signature (mean C-index, 0.68 vs 0.65).
“The proposed immune-related gene pair–based signature is a promising prognostic biomarker in nonsquamous NSCLC, including early-stage disease,” concluded the investigators. “Prospective studies are needed to further validate its analytical accuracy for estimating prognoses and to test its clinical utility in individualized management of nonsquamous NSCLC.”
FROM JAMA ONCOLOGY
Key clinical point:
Major finding: Compared with peers in the signature-defined low-risk group, patients in the signature-defined high-risk group had roughly twice the adjusted risk of death (hazard ratio range, 1.72-2.36).
Data source: A retrospective cohort study using frozen tumors from 2,414 patients with stage I or II nonsquamous NSCLC who underwent complete resection and did not receive adjuvant or neoadjuvant therapy.
Disclosures: The investigators reported that they had no relevant disclosures. The study was supported in part by the National Institutes of Health.
Some adjuvant endocrine therapies better than others for young breast cancer patients
Young women treated for early hormone receptor–positive, HER2-negative breast cancer fare better if their adjuvant endocrine therapy includes ovarian function suppression (OFS), according to a new analysis published online.
Senior author Gini F. Fleming, MD, director of the medical oncology breast program at the University of Chicago Medical Center, and her colleagues analyzed data from a pair of international phase III randomized adjuvant trials: the Suppression of Ovarian Function Trial (SOFT) and the Tamoxifen and Exemestane Trial (TEXT).
Main analyses were based on a respective 240 and 145 women younger than 35 years who had undergone surgery for early hormone receptor–positive, HER2-negative early breast cancer, received chemotherapy, and were randomly assigned to 5 years of various adjuvant endocrine therapies.
In SOFT, the 5-year breast cancer–free interval was 67.1% (95% CI, 54.6%-76.9%) with tamoxifen (Nolvadex) alone, 75.9% (64.0%-84.4%) with tamoxifen plus OFS, and 83.2% (72.7%-90.0%) with exemestane (Aromasin) plus OFS (J Clin Oncol. 2017 June 27 doi: 10.1200/JCO.2016.72.0946). In TEXT, it was 79.2% (66.2%-87.7%) with tamoxifen plus OFS and 81.6% (69.8%-89.2%) with exemestane plus OFS.
In a quality of life analysis among women receiving OFS, vasomotor symptoms (hot flushes and sweats) showed greatest increase from baseline (roughly 30-40 points) in the first 6 months of therapy. Loss of sexual interest and difficulties in becoming aroused were also noteworthy (8 points or greater). However, scores for global quality of life (physical well-being, mood, coping effort, and health perception) showed little change from baseline and were essentially the same as those seen among premenopausal women aged 35 or older in the same trials.
Overall, 19.8% of the young women in SOFT and TEXT stopped all protocol-assigned endocrine therapy early. The proportion rose with time and was higher than that among the older premenopausal group.
“There was a meaningful clinical benefit in breast cancer outcomes with the addition of OFS to tamoxifen and some additional benefit from use of an aromatase inhibitor with OFS. Longer follow-up is critical to clarify potential survival benefits,” the investigators wrote. “There were substantial adverse effects from these combined endocrine treatments, but they were not different in the younger and older than 35 years populations. Despite this, rates of nonadherence were slightly higher in women younger than 35 years.
“Availability of these age-specific data regarding risks and benefits of combined endocrine therapy will support shared decision making regarding OFS among young women at high risk for recurrence and death from breast cancer and, it is hoped, improve adherence among those who select OFS,” they concluded.
Young women treated for early hormone receptor–positive, HER2-negative breast cancer fare better if their adjuvant endocrine therapy includes ovarian function suppression (OFS), according to a new analysis published online.
Senior author Gini F. Fleming, MD, director of the medical oncology breast program at the University of Chicago Medical Center, and her colleagues analyzed data from a pair of international phase III randomized adjuvant trials: the Suppression of Ovarian Function Trial (SOFT) and the Tamoxifen and Exemestane Trial (TEXT).
Main analyses were based on a respective 240 and 145 women younger than 35 years who had undergone surgery for early hormone receptor–positive, HER2-negative early breast cancer, received chemotherapy, and were randomly assigned to 5 years of various adjuvant endocrine therapies.
In SOFT, the 5-year breast cancer–free interval was 67.1% (95% CI, 54.6%-76.9%) with tamoxifen (Nolvadex) alone, 75.9% (64.0%-84.4%) with tamoxifen plus OFS, and 83.2% (72.7%-90.0%) with exemestane (Aromasin) plus OFS (J Clin Oncol. 2017 June 27 doi: 10.1200/JCO.2016.72.0946). In TEXT, it was 79.2% (66.2%-87.7%) with tamoxifen plus OFS and 81.6% (69.8%-89.2%) with exemestane plus OFS.
In a quality of life analysis among women receiving OFS, vasomotor symptoms (hot flushes and sweats) showed greatest increase from baseline (roughly 30-40 points) in the first 6 months of therapy. Loss of sexual interest and difficulties in becoming aroused were also noteworthy (8 points or greater). However, scores for global quality of life (physical well-being, mood, coping effort, and health perception) showed little change from baseline and were essentially the same as those seen among premenopausal women aged 35 or older in the same trials.
Overall, 19.8% of the young women in SOFT and TEXT stopped all protocol-assigned endocrine therapy early. The proportion rose with time and was higher than that among the older premenopausal group.
“There was a meaningful clinical benefit in breast cancer outcomes with the addition of OFS to tamoxifen and some additional benefit from use of an aromatase inhibitor with OFS. Longer follow-up is critical to clarify potential survival benefits,” the investigators wrote. “There were substantial adverse effects from these combined endocrine treatments, but they were not different in the younger and older than 35 years populations. Despite this, rates of nonadherence were slightly higher in women younger than 35 years.
“Availability of these age-specific data regarding risks and benefits of combined endocrine therapy will support shared decision making regarding OFS among young women at high risk for recurrence and death from breast cancer and, it is hoped, improve adherence among those who select OFS,” they concluded.
Young women treated for early hormone receptor–positive, HER2-negative breast cancer fare better if their adjuvant endocrine therapy includes ovarian function suppression (OFS), according to a new analysis published online.
Senior author Gini F. Fleming, MD, director of the medical oncology breast program at the University of Chicago Medical Center, and her colleagues analyzed data from a pair of international phase III randomized adjuvant trials: the Suppression of Ovarian Function Trial (SOFT) and the Tamoxifen and Exemestane Trial (TEXT).
Main analyses were based on a respective 240 and 145 women younger than 35 years who had undergone surgery for early hormone receptor–positive, HER2-negative early breast cancer, received chemotherapy, and were randomly assigned to 5 years of various adjuvant endocrine therapies.
In SOFT, the 5-year breast cancer–free interval was 67.1% (95% CI, 54.6%-76.9%) with tamoxifen (Nolvadex) alone, 75.9% (64.0%-84.4%) with tamoxifen plus OFS, and 83.2% (72.7%-90.0%) with exemestane (Aromasin) plus OFS (J Clin Oncol. 2017 June 27 doi: 10.1200/JCO.2016.72.0946). In TEXT, it was 79.2% (66.2%-87.7%) with tamoxifen plus OFS and 81.6% (69.8%-89.2%) with exemestane plus OFS.
In a quality of life analysis among women receiving OFS, vasomotor symptoms (hot flushes and sweats) showed greatest increase from baseline (roughly 30-40 points) in the first 6 months of therapy. Loss of sexual interest and difficulties in becoming aroused were also noteworthy (8 points or greater). However, scores for global quality of life (physical well-being, mood, coping effort, and health perception) showed little change from baseline and were essentially the same as those seen among premenopausal women aged 35 or older in the same trials.
Overall, 19.8% of the young women in SOFT and TEXT stopped all protocol-assigned endocrine therapy early. The proportion rose with time and was higher than that among the older premenopausal group.
“There was a meaningful clinical benefit in breast cancer outcomes with the addition of OFS to tamoxifen and some additional benefit from use of an aromatase inhibitor with OFS. Longer follow-up is critical to clarify potential survival benefits,” the investigators wrote. “There were substantial adverse effects from these combined endocrine treatments, but they were not different in the younger and older than 35 years populations. Despite this, rates of nonadherence were slightly higher in women younger than 35 years.
“Availability of these age-specific data regarding risks and benefits of combined endocrine therapy will support shared decision making regarding OFS among young women at high risk for recurrence and death from breast cancer and, it is hoped, improve adherence among those who select OFS,” they concluded.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: In SOFT, the 5-year breast cancer–free interval was 67.1% with tamoxifen alone, 75.9% with tamoxifen plus OFS, and 83.2% with exemestane plus OFS. In TEXT, it was 79.2% with tamoxifen plus OFS and 81.6% with exemestane plus OFS.
Data source: An analysis of women younger than 35 years treated for early hormone receptor–positive, HER2-negative breast cancer and given adjuvant endocrine therapy in the phase III randomized SOFT trial (240 women) or TEXT trial (145 women).
Disclosures: Dr. Fleming disclosed that she receives research funding from Corcept Therapeutics (institutional) and has a relationship with Aeterna Zentaris.