User login
First in utero cerebrovascular surgery success
The team from Boston Children’s Hospital and Brigham and Women’s Hospital used ultrasound guidance to repair the vein of Galen malformation, which causes excessively high blood flow, resulting in both neurologic and cardiac complications.
The surgery was performed in a fetus at 34 weeks’ gestational age, with remarkable results. Since birth, the baby girl, who was identified in utero as being at high risk of suffering serious complications of the malformation, has required no medication to treat heart failure and no postnatal surgery.
Repeated echocardiograms after birth displayed marked improvement in cardiac output, and brain MRI showed no brain injury and a normal neurologic exam.
“This is incredibly exciting. The hope is that this baby, and others with this condition who receive this in utero surgery in future, will go on to have a normal life,” lead researcher Darren B. Orbach, MD, PhD, said in an interview.
“We were thrilled to see that the aggressive decline usually seen after birth simply did not appear. We are pleased to report that at 6 weeks, the infant is progressing remarkably well, on no medications, eating normally, gaining weight and is back home. There are no signs of any negative effects on the brain,” he added.
Dr. Orbach, codirector of the Cerebrovascular Surgery & Interventions Center at Boston Children’s Hospital, and colleagues described this first case report of the in utero vein of Galen malformation repair in a research letter, published online in the journal Stroke.
Vein of Galen malformation
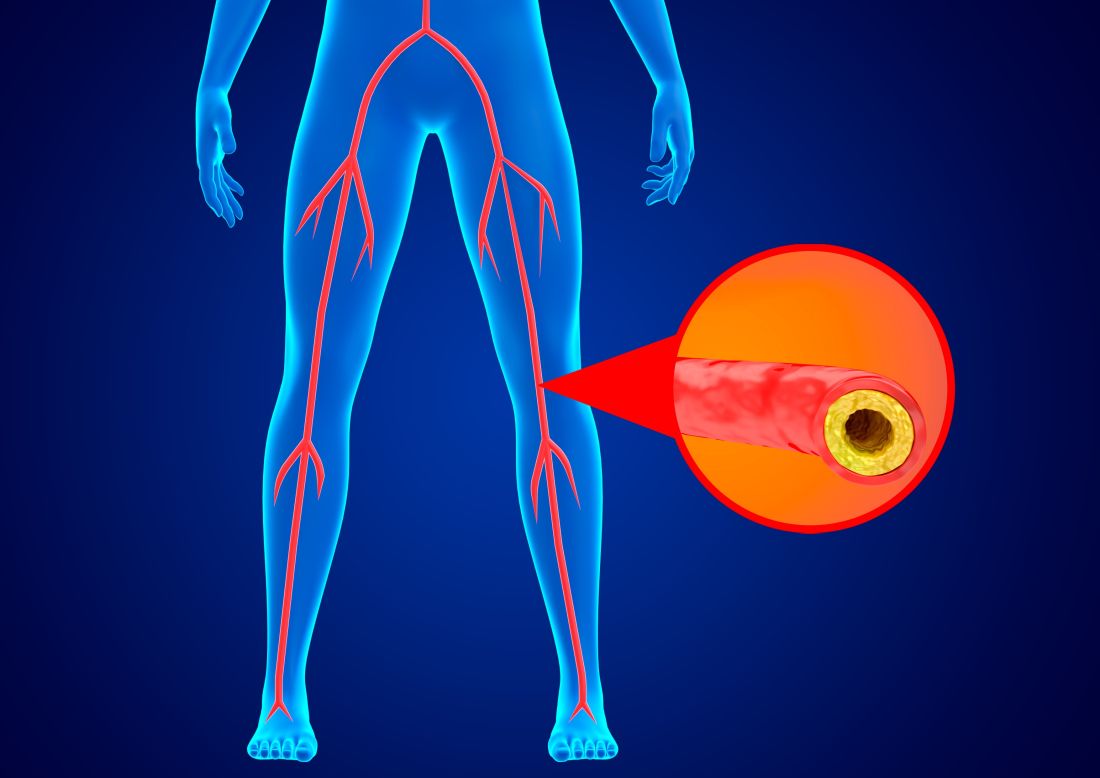
Dr. Orbach explained that vein of Galen malformation, which occurs in around 1 in every 60,000 births, is a cerebrovascular anomaly in which the arterial system is directly connected to the venous system rather than to capillaries that are necessary to slow blood flow and deliver oxygen to surrounding brain tissue.
“The arterial and venous systems are fundamentally very different. The arterial system is high pressure, high flow; while the venous system is low pressure, low flow. They shouldn’t be directly connected,” he noted.
The vein of Galen malformation is the most extreme version of such an anomaly. Developing in early gestation, it is associated with a large increase in blood flow through the brain which grows over time and can sometimes result in twice the total cardiac output of the body or even more, Dr. Orbach said.
The placenta is believed to be protective as most babies don’t have overt physiologic problems in utero, but they can run into crisis after birth, with the abnormally high blood flow causing an immense stress to the heart.
Babies typically present with heart failure as their first major symptom soon after birth, Dr. Orbach said. “Although the anatomical problem is in the brain, the clinical manifestation is high-output heart failure. The heart is trying to do double its normal work, pumping the blood to the malformation and immediately back to the heart and that blood is not performing any useful function.
“These newborns can get very sick. They need multiple medications to support their cardiovascular system and we need to do procedures to try and reduce the blood flow,” he explained.
Brain injury is also a common problem. “The brain circulation is very abnormal. The blood is being shunted through the malformation rather than circulating through the brain tissue which can become ischemic,” Dr. Orbach commented.
“The babies who get sick would have a very high mortality (up to 90%) without expert care. Even those who do receive expert care at a specialty center have a mortality rate of 30% to 40% and those who survive have a high risk of neurologic and cognitive impairment,” he added.
The current treatment for babies born with the condition involves transarterial embolization, by which a catheter is inserted into the arterial system to enable the malformation to be occluded by various techniques.
But Dr. Orbach pointed out that some babies are born too sick to have the postnatal intervention. “The heart failure and brain injury is so overwhelming that no matter what we do, we cannot reverse it, and these babies normally do not survive. What we are doing with the fetal surgery is trying to help those babies who cannot be treated with the current postnatal approach,” he said.
The first stage of this research involved trying to identify these very-high-risk babies in utero, and the researchers found that on fetal MRI a particular measurement of one of the venous sinuses that drains the main malformation was a good predictor of how the baby would fare after birth. The babies predicted to do poorly from this test are the targets for the fetal surgery.
The technique used for the postnatal intervention is too technically challenging to perform in utero. “So we have developed a different approach for the in utero surgery that involves navigating into the accepting vein in the malformation with a needle under ultrasound guidance, and then packing the vein with metal coils to dramatically reduce the blood flow,” Dr. Orbach explained.
This procedure was performed in this first patient on March 15. The surgery was part of a clinical trial that is planned to include 20 cases in total.
“The immediate goal is to see whether we can transform those fetuses who are at very high risk of getting sick after birth into babies who do well in the [neonatal] ICU and are able to be sent home for elective treatment at a few months of age,” Dr. Orbach noted. “The study is continuing as it is vital that we continue and show efficacy and safety in other patients as well,” he added.
Dr. Orbach said the results of this first case were extremely encouraging. “Each stage was exciting – the technical success of the procedure, and then seeing the [blood] flow diminish on the ultrasound right there during the procedure; then the next day we did a fetal echocardiogram, and we could see that the abnormal cardiac output was dramatically reduced, and a fetal MRI scan also showed the malformation was already coming down in size.”
The baby was born prematurely 2 days after the procedure because of ruptured membranes with a birth weight of 1.9 kg (4.2 lb). She has not required any cardiovascular support or postnatal embolization.
“We were waiting with bated breath until the baby was born to see how she did clinically. I was trying to be conservative in my expectations, but it was quickly apparent that she was going to do great,” he said. Now at home, she has some oxygen treatment for the first few weeks, “but right now her neurological status is completely intact and essentially she looks like any other baby,” Dr. Orbach commented.
It is not yet known whether the infant will need any additional procedures. “We will follow her closely and make a decision on whether further treatment is needed based on whether the malformation is growing or not,” Dr. Orbach said. Longer term follow-up will also assess secondary problems sometimes seen, such as learning problems and seizures.
Although other fetal surgeries are now routinely performed, this is believed to be the first in utero surgery aimed at the cerebrovascular system.
“There were a lot of uncertainties,” Dr. Orbach said. “We didn’t even know if we would be able to see our instruments on ultrasound.” To model the procedure, the researchers had a phantom fetal skull and brain constructed with a vein of Galen malformation, which was key to obtaining Food and Drug Administration approval for the study.
If the study shows success in the other patients too, the technique could be rolled out to other centers. “There definitely needs to be fetal surgery and neurointerventional teams familiar with vein of Galen malformation in place, and ready to manage complications after delivery regardless of outcome. But we are not the only center with those capabilities, so if our trial pans out, yes, the hope is that other teams in specialist children’s hospitals around the world could do this too,” he added.
Pioneering work
Commenting on the case report in an American Heart Association press release, Colin Derdeyn, MD, a neurointerventional radiologist at University of Iowa Health Care, Iowa City, who performs vein of Galen malformation embolizations on neonates, said: “The key advance here is to intervene before the physiologic events of birth can cause life-threatening heart failure.”
Dr. Derdeyn, who is a past chair of the American Heart Association’s Stroke Council, cautioned that one successful case is not enough experience to conclude that the risks of this procedure are worth the benefits.
But, he added: “The positive hemodynamic changes that they observed in utero and after birth – reduction in flow, reduction in size of the draining vein, reversal of the abnormal reversed flow in the aorta – are really encouraging. These are some of the most exciting and surprising aspects of this case report. This is pioneering work being done in a very careful and responsible way.”
The study was funded by a grant from the Sage Schermerhorn Chair for Image-Guided Therapy.
A version of this article first appeared on Medscape.com.
The team from Boston Children’s Hospital and Brigham and Women’s Hospital used ultrasound guidance to repair the vein of Galen malformation, which causes excessively high blood flow, resulting in both neurologic and cardiac complications.
The surgery was performed in a fetus at 34 weeks’ gestational age, with remarkable results. Since birth, the baby girl, who was identified in utero as being at high risk of suffering serious complications of the malformation, has required no medication to treat heart failure and no postnatal surgery.
Repeated echocardiograms after birth displayed marked improvement in cardiac output, and brain MRI showed no brain injury and a normal neurologic exam.
“This is incredibly exciting. The hope is that this baby, and others with this condition who receive this in utero surgery in future, will go on to have a normal life,” lead researcher Darren B. Orbach, MD, PhD, said in an interview.
“We were thrilled to see that the aggressive decline usually seen after birth simply did not appear. We are pleased to report that at 6 weeks, the infant is progressing remarkably well, on no medications, eating normally, gaining weight and is back home. There are no signs of any negative effects on the brain,” he added.
Dr. Orbach, codirector of the Cerebrovascular Surgery & Interventions Center at Boston Children’s Hospital, and colleagues described this first case report of the in utero vein of Galen malformation repair in a research letter, published online in the journal Stroke.
Vein of Galen malformation
Dr. Orbach explained that vein of Galen malformation, which occurs in around 1 in every 60,000 births, is a cerebrovascular anomaly in which the arterial system is directly connected to the venous system rather than to capillaries that are necessary to slow blood flow and deliver oxygen to surrounding brain tissue.
“The arterial and venous systems are fundamentally very different. The arterial system is high pressure, high flow; while the venous system is low pressure, low flow. They shouldn’t be directly connected,” he noted.
The vein of Galen malformation is the most extreme version of such an anomaly. Developing in early gestation, it is associated with a large increase in blood flow through the brain which grows over time and can sometimes result in twice the total cardiac output of the body or even more, Dr. Orbach said.
The placenta is believed to be protective as most babies don’t have overt physiologic problems in utero, but they can run into crisis after birth, with the abnormally high blood flow causing an immense stress to the heart.
Babies typically present with heart failure as their first major symptom soon after birth, Dr. Orbach said. “Although the anatomical problem is in the brain, the clinical manifestation is high-output heart failure. The heart is trying to do double its normal work, pumping the blood to the malformation and immediately back to the heart and that blood is not performing any useful function.
“These newborns can get very sick. They need multiple medications to support their cardiovascular system and we need to do procedures to try and reduce the blood flow,” he explained.
Brain injury is also a common problem. “The brain circulation is very abnormal. The blood is being shunted through the malformation rather than circulating through the brain tissue which can become ischemic,” Dr. Orbach commented.
“The babies who get sick would have a very high mortality (up to 90%) without expert care. Even those who do receive expert care at a specialty center have a mortality rate of 30% to 40% and those who survive have a high risk of neurologic and cognitive impairment,” he added.
The current treatment for babies born with the condition involves transarterial embolization, by which a catheter is inserted into the arterial system to enable the malformation to be occluded by various techniques.
But Dr. Orbach pointed out that some babies are born too sick to have the postnatal intervention. “The heart failure and brain injury is so overwhelming that no matter what we do, we cannot reverse it, and these babies normally do not survive. What we are doing with the fetal surgery is trying to help those babies who cannot be treated with the current postnatal approach,” he said.
The first stage of this research involved trying to identify these very-high-risk babies in utero, and the researchers found that on fetal MRI a particular measurement of one of the venous sinuses that drains the main malformation was a good predictor of how the baby would fare after birth. The babies predicted to do poorly from this test are the targets for the fetal surgery.
The technique used for the postnatal intervention is too technically challenging to perform in utero. “So we have developed a different approach for the in utero surgery that involves navigating into the accepting vein in the malformation with a needle under ultrasound guidance, and then packing the vein with metal coils to dramatically reduce the blood flow,” Dr. Orbach explained.
This procedure was performed in this first patient on March 15. The surgery was part of a clinical trial that is planned to include 20 cases in total.
“The immediate goal is to see whether we can transform those fetuses who are at very high risk of getting sick after birth into babies who do well in the [neonatal] ICU and are able to be sent home for elective treatment at a few months of age,” Dr. Orbach noted. “The study is continuing as it is vital that we continue and show efficacy and safety in other patients as well,” he added.
Dr. Orbach said the results of this first case were extremely encouraging. “Each stage was exciting – the technical success of the procedure, and then seeing the [blood] flow diminish on the ultrasound right there during the procedure; then the next day we did a fetal echocardiogram, and we could see that the abnormal cardiac output was dramatically reduced, and a fetal MRI scan also showed the malformation was already coming down in size.”
The baby was born prematurely 2 days after the procedure because of ruptured membranes with a birth weight of 1.9 kg (4.2 lb). She has not required any cardiovascular support or postnatal embolization.
“We were waiting with bated breath until the baby was born to see how she did clinically. I was trying to be conservative in my expectations, but it was quickly apparent that she was going to do great,” he said. Now at home, she has some oxygen treatment for the first few weeks, “but right now her neurological status is completely intact and essentially she looks like any other baby,” Dr. Orbach commented.
It is not yet known whether the infant will need any additional procedures. “We will follow her closely and make a decision on whether further treatment is needed based on whether the malformation is growing or not,” Dr. Orbach said. Longer term follow-up will also assess secondary problems sometimes seen, such as learning problems and seizures.
Although other fetal surgeries are now routinely performed, this is believed to be the first in utero surgery aimed at the cerebrovascular system.
“There were a lot of uncertainties,” Dr. Orbach said. “We didn’t even know if we would be able to see our instruments on ultrasound.” To model the procedure, the researchers had a phantom fetal skull and brain constructed with a vein of Galen malformation, which was key to obtaining Food and Drug Administration approval for the study.
If the study shows success in the other patients too, the technique could be rolled out to other centers. “There definitely needs to be fetal surgery and neurointerventional teams familiar with vein of Galen malformation in place, and ready to manage complications after delivery regardless of outcome. But we are not the only center with those capabilities, so if our trial pans out, yes, the hope is that other teams in specialist children’s hospitals around the world could do this too,” he added.
Pioneering work
Commenting on the case report in an American Heart Association press release, Colin Derdeyn, MD, a neurointerventional radiologist at University of Iowa Health Care, Iowa City, who performs vein of Galen malformation embolizations on neonates, said: “The key advance here is to intervene before the physiologic events of birth can cause life-threatening heart failure.”
Dr. Derdeyn, who is a past chair of the American Heart Association’s Stroke Council, cautioned that one successful case is not enough experience to conclude that the risks of this procedure are worth the benefits.
But, he added: “The positive hemodynamic changes that they observed in utero and after birth – reduction in flow, reduction in size of the draining vein, reversal of the abnormal reversed flow in the aorta – are really encouraging. These are some of the most exciting and surprising aspects of this case report. This is pioneering work being done in a very careful and responsible way.”
The study was funded by a grant from the Sage Schermerhorn Chair for Image-Guided Therapy.
A version of this article first appeared on Medscape.com.
The team from Boston Children’s Hospital and Brigham and Women’s Hospital used ultrasound guidance to repair the vein of Galen malformation, which causes excessively high blood flow, resulting in both neurologic and cardiac complications.
The surgery was performed in a fetus at 34 weeks’ gestational age, with remarkable results. Since birth, the baby girl, who was identified in utero as being at high risk of suffering serious complications of the malformation, has required no medication to treat heart failure and no postnatal surgery.
Repeated echocardiograms after birth displayed marked improvement in cardiac output, and brain MRI showed no brain injury and a normal neurologic exam.
“This is incredibly exciting. The hope is that this baby, and others with this condition who receive this in utero surgery in future, will go on to have a normal life,” lead researcher Darren B. Orbach, MD, PhD, said in an interview.
“We were thrilled to see that the aggressive decline usually seen after birth simply did not appear. We are pleased to report that at 6 weeks, the infant is progressing remarkably well, on no medications, eating normally, gaining weight and is back home. There are no signs of any negative effects on the brain,” he added.
Dr. Orbach, codirector of the Cerebrovascular Surgery & Interventions Center at Boston Children’s Hospital, and colleagues described this first case report of the in utero vein of Galen malformation repair in a research letter, published online in the journal Stroke.
Vein of Galen malformation
Dr. Orbach explained that vein of Galen malformation, which occurs in around 1 in every 60,000 births, is a cerebrovascular anomaly in which the arterial system is directly connected to the venous system rather than to capillaries that are necessary to slow blood flow and deliver oxygen to surrounding brain tissue.
“The arterial and venous systems are fundamentally very different. The arterial system is high pressure, high flow; while the venous system is low pressure, low flow. They shouldn’t be directly connected,” he noted.
The vein of Galen malformation is the most extreme version of such an anomaly. Developing in early gestation, it is associated with a large increase in blood flow through the brain which grows over time and can sometimes result in twice the total cardiac output of the body or even more, Dr. Orbach said.
The placenta is believed to be protective as most babies don’t have overt physiologic problems in utero, but they can run into crisis after birth, with the abnormally high blood flow causing an immense stress to the heart.
Babies typically present with heart failure as their first major symptom soon after birth, Dr. Orbach said. “Although the anatomical problem is in the brain, the clinical manifestation is high-output heart failure. The heart is trying to do double its normal work, pumping the blood to the malformation and immediately back to the heart and that blood is not performing any useful function.
“These newborns can get very sick. They need multiple medications to support their cardiovascular system and we need to do procedures to try and reduce the blood flow,” he explained.
Brain injury is also a common problem. “The brain circulation is very abnormal. The blood is being shunted through the malformation rather than circulating through the brain tissue which can become ischemic,” Dr. Orbach commented.
“The babies who get sick would have a very high mortality (up to 90%) without expert care. Even those who do receive expert care at a specialty center have a mortality rate of 30% to 40% and those who survive have a high risk of neurologic and cognitive impairment,” he added.
The current treatment for babies born with the condition involves transarterial embolization, by which a catheter is inserted into the arterial system to enable the malformation to be occluded by various techniques.
But Dr. Orbach pointed out that some babies are born too sick to have the postnatal intervention. “The heart failure and brain injury is so overwhelming that no matter what we do, we cannot reverse it, and these babies normally do not survive. What we are doing with the fetal surgery is trying to help those babies who cannot be treated with the current postnatal approach,” he said.
The first stage of this research involved trying to identify these very-high-risk babies in utero, and the researchers found that on fetal MRI a particular measurement of one of the venous sinuses that drains the main malformation was a good predictor of how the baby would fare after birth. The babies predicted to do poorly from this test are the targets for the fetal surgery.
The technique used for the postnatal intervention is too technically challenging to perform in utero. “So we have developed a different approach for the in utero surgery that involves navigating into the accepting vein in the malformation with a needle under ultrasound guidance, and then packing the vein with metal coils to dramatically reduce the blood flow,” Dr. Orbach explained.
This procedure was performed in this first patient on March 15. The surgery was part of a clinical trial that is planned to include 20 cases in total.
“The immediate goal is to see whether we can transform those fetuses who are at very high risk of getting sick after birth into babies who do well in the [neonatal] ICU and are able to be sent home for elective treatment at a few months of age,” Dr. Orbach noted. “The study is continuing as it is vital that we continue and show efficacy and safety in other patients as well,” he added.
Dr. Orbach said the results of this first case were extremely encouraging. “Each stage was exciting – the technical success of the procedure, and then seeing the [blood] flow diminish on the ultrasound right there during the procedure; then the next day we did a fetal echocardiogram, and we could see that the abnormal cardiac output was dramatically reduced, and a fetal MRI scan also showed the malformation was already coming down in size.”
The baby was born prematurely 2 days after the procedure because of ruptured membranes with a birth weight of 1.9 kg (4.2 lb). She has not required any cardiovascular support or postnatal embolization.
“We were waiting with bated breath until the baby was born to see how she did clinically. I was trying to be conservative in my expectations, but it was quickly apparent that she was going to do great,” he said. Now at home, she has some oxygen treatment for the first few weeks, “but right now her neurological status is completely intact and essentially she looks like any other baby,” Dr. Orbach commented.
It is not yet known whether the infant will need any additional procedures. “We will follow her closely and make a decision on whether further treatment is needed based on whether the malformation is growing or not,” Dr. Orbach said. Longer term follow-up will also assess secondary problems sometimes seen, such as learning problems and seizures.
Although other fetal surgeries are now routinely performed, this is believed to be the first in utero surgery aimed at the cerebrovascular system.
“There were a lot of uncertainties,” Dr. Orbach said. “We didn’t even know if we would be able to see our instruments on ultrasound.” To model the procedure, the researchers had a phantom fetal skull and brain constructed with a vein of Galen malformation, which was key to obtaining Food and Drug Administration approval for the study.
If the study shows success in the other patients too, the technique could be rolled out to other centers. “There definitely needs to be fetal surgery and neurointerventional teams familiar with vein of Galen malformation in place, and ready to manage complications after delivery regardless of outcome. But we are not the only center with those capabilities, so if our trial pans out, yes, the hope is that other teams in specialist children’s hospitals around the world could do this too,” he added.
Pioneering work
Commenting on the case report in an American Heart Association press release, Colin Derdeyn, MD, a neurointerventional radiologist at University of Iowa Health Care, Iowa City, who performs vein of Galen malformation embolizations on neonates, said: “The key advance here is to intervene before the physiologic events of birth can cause life-threatening heart failure.”
Dr. Derdeyn, who is a past chair of the American Heart Association’s Stroke Council, cautioned that one successful case is not enough experience to conclude that the risks of this procedure are worth the benefits.
But, he added: “The positive hemodynamic changes that they observed in utero and after birth – reduction in flow, reduction in size of the draining vein, reversal of the abnormal reversed flow in the aorta – are really encouraging. These are some of the most exciting and surprising aspects of this case report. This is pioneering work being done in a very careful and responsible way.”
The study was funded by a grant from the Sage Schermerhorn Chair for Image-Guided Therapy.
A version of this article first appeared on Medscape.com.
FROM STROKE
Machine-learning model improves MI diagnosis
Use of a machine-learning model that incorporates information from a single troponin test as well as other clinical data was superior to current practice as an aid to the diagnosis of myocardial infarction in the emergency department in a new study.
“Our results suggest that and free up space in the emergency department,” senior author Nicholas L. Mills, MD, University of Edinburgh, Scotland, said in an interview.
“And, perhaps even more importantly, use of this model could also increase the proportion of patients who are correctly identified as at a high probability of having an MI,” he added.
The study was published online in Nature Medicine.
The authors explained that at present, the likelihood of an MI diagnosis for patients presenting to the emergency department with chest pain is based on a fixed troponin threshold in serial tests at specific time points, but there are several problems with this approach.
First, a fixed troponin threshold is generally used for all patients, which does not account for age, sex, or comorbidities that are known to influence cardiac troponin concentrations. Second, the need to perform tests at specific time points for serial testing can be challenging in busy emergency departments.
And third, patients are categorized as being at low, intermediate, or high risk of MI on the basis of troponin thresholds alone, and the test does not take into account other important factors, such as the time of symptom onset or findings on the electrocardiogram.
“Our current practice of using the same threshold to rule in and rule out an MI for everyone, regardless of whether they are an 18-year-old female without a history of heart disease or an 85-year-old male with known heart failure, doesn’t perform well, and there’s a significant risk of misdiagnosis. There is also a high likelihood for inequalities in care, particularly between men and women,” Dr. Mills said.
The current study evaluated whether use of a machine learning model known as CoDE-ACS to guide decision-making could overcome some of these challenges.
The machine learning model assesses the whole spectrum of troponin levels as a continuous variable (rather than use of a single threshold) and turns this measurement into a probability that an individual patient is having an MI after accounting for other factors, including age, sex, comorbidities, and time from symptom onset.
For the current study, the CoDE-ACS model was trained in 10,000 patients with suspected acute coronary syndrome (ACS) who presented to 10 hospitals in Scotland as part of the High-STEACS trial evaluating the implementation of a high-sensitivity cardiac troponin I assay. The results were then validated in another 10,000 patients from six countries around the world.
“Using this model, the patient can have a troponin test on arrival at the emergency department. The other information on age, sex, clinical history, and time since symptom onset is keyed in, and it gives a probability on a scale of 0–100 as to whether the patient is having an MI,” Dr. Mills noted.
“It also has the capacity to incorporate more information over time. So, if there is a second troponin measurement made, then the model automatically refines the probability score,” he added.
The current study showed that use of the CoDE-ACS model identified more patients at presentation as having a low probability of having an MI than fixed cardiac troponin thresholds (61% vs. 27%) with a similar negative predictive value.
It also identified fewer patients as having a high probability of having an MI (10% vs. 16%) with a greater positive predictive value.
Among patients who were identified as having a low probability of MI, the rate of cardiac death was lower than the rate among those with intermediate or high probability at 30 days (0.1% vs. 0.5% and 1.8%) and 1 year (0.3% vs. 2.8% and 4.2%).
“The results show that the machine learning model doubles the proportion of patients who can be discharged with a single test compared to the current practice of using the threshold approach. It really is a game changer in terms of its potential to improve health efficiency,” Dr. Mills said.
In terms of ruling patients in as possibly having an MI, he pointed out that troponin levels are increased in patients with a wide range of other conditions, including heart failure, kidney failure, and atrial fibrillation.
“When using the threshold approach, only one in four patients with an elevated troponin level will actually be having an MI, and that leads to confusion,” he said. “This model takes into consideration these other conditions and so it can correctly identify three out of four patients with a high probability of having an MI. We can therefore be more confident that it is appropriate to refer those patients to cardiology and save a lot of potentially unnecessary investigations and treatments in the others.”
Dr. Mills said the model also seems to work when assessing patients early on.
“Around one-third of patients present within 3 hours of symptom onset, and actually these are a high-risk group because people who have genuine cardiac pain are normally extremely uncomfortable and tend to present quickly. Current guidelines require that we do two tests in all these individuals, but this new model incorporates the time of symptom onset into its estimates of probability and therefore allows us to rule out patients even when they present very early.”
He reported that a second test is required in only one in five patients – those whose first test indicated intermediate probability.
“The second test allows us to refine the probability further, allowing us to rule another half of those patients out. We are then left with a small proportion of patients – about 1 in 10 – who remain of intermediate probability and will require additional clinical judgment.”
Should improve inequities in MI diagnosis
Dr. Mills said the CoDE-ACS model will improve current inequities in MI diagnosis, because of which MI is underrecognized in women and younger people.
“Women have troponin concentrations that are half those of men, and although sex-specific troponin thresholds are recommended in the guidelines, they are not widely used. This automatically leads to underrecognition of heart disease in women. But this new machine learning model performs identically in men and women because it has been trained to recognize the different normal levels in men and women,” he explained.
“It will also help us not to underdiagnose MI in younger people who often have a less classical presentation of MI, and they also generally have very low concentrations of troponin, so any increase in troponin way below the current diagnostic threshold may be very relevant to their risk,” he added.
The researchers are planning a randomized trial of the new model to demonstrate the impact it could have on equality of care and overcrowding in the emergency department. In the trial, patients will be randomly assigned to undergo decision-making on the basis of troponin thresholds (current practice) or to undergo decision-making through the CoDE-ACS model.
“The hope is that this trial will show reductions in unnecessary hospital admissions and length of stay in the emergency department,” Dr. Mills said. Results are expected sometime next year.
“This algorithm is very well trained. It has learned on 20,000 patients, so it has a lot more experience than I have, and I have been a professor of cardiology for 20 years,” Dr. Mills said.
He said he believes these models will get even smarter in the future as more data are added.
“I think the future for good decision-making in emergency care will be informed by clinical decision support from well-trained machine learning algorithms and they will help us guide not just the diagnosis of MI but also heart failure and other important cardiac conditions,” he said.
‘Elegant and exciting’ data
Commenting on the study, John W. McEvoy, MB, University of Galway, Ireland, said: “These are elegant and exciting data; however, the inputs into the machine learning algorithm include all the necessary information to actually diagnose MI. So why predict MI, when a human diagnosis can just be made directly? The answer to this question may depend on whether we trust machines more than humans.”
Dr. Mills noted that clinical judgment will always be an important part of MI diagnosis.
“Currently, using the troponin threshold approach, experienced clinicians will be able to nuance the results, but invariably, there is disagreement on this, and this can be a major source of tension within clinical care. By providing more individualized information, this will help enormously in the decision-making process,” he said.
“This model is not about replacing clinical decision-making. It’s more about augmenting decision-making and giving clinicians guidance to be able to improve efficiency and reduce inequality,” he added.
The study was funded with support from the National Institute for Health Research and NHSX, the British Heart Foundation, and Wellcome Leap. Dr. Mills has received honoraria or consultancy from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. He is employed by the University of Edinburgh, which has filed a patent on the Collaboration for the Diagnosis and Evaluation of Acute Coronary Syndrome score.
A version of this article first appeared on Medscape.com.
Use of a machine-learning model that incorporates information from a single troponin test as well as other clinical data was superior to current practice as an aid to the diagnosis of myocardial infarction in the emergency department in a new study.
“Our results suggest that and free up space in the emergency department,” senior author Nicholas L. Mills, MD, University of Edinburgh, Scotland, said in an interview.
“And, perhaps even more importantly, use of this model could also increase the proportion of patients who are correctly identified as at a high probability of having an MI,” he added.
The study was published online in Nature Medicine.
The authors explained that at present, the likelihood of an MI diagnosis for patients presenting to the emergency department with chest pain is based on a fixed troponin threshold in serial tests at specific time points, but there are several problems with this approach.
First, a fixed troponin threshold is generally used for all patients, which does not account for age, sex, or comorbidities that are known to influence cardiac troponin concentrations. Second, the need to perform tests at specific time points for serial testing can be challenging in busy emergency departments.
And third, patients are categorized as being at low, intermediate, or high risk of MI on the basis of troponin thresholds alone, and the test does not take into account other important factors, such as the time of symptom onset or findings on the electrocardiogram.
“Our current practice of using the same threshold to rule in and rule out an MI for everyone, regardless of whether they are an 18-year-old female without a history of heart disease or an 85-year-old male with known heart failure, doesn’t perform well, and there’s a significant risk of misdiagnosis. There is also a high likelihood for inequalities in care, particularly between men and women,” Dr. Mills said.
The current study evaluated whether use of a machine learning model known as CoDE-ACS to guide decision-making could overcome some of these challenges.
The machine learning model assesses the whole spectrum of troponin levels as a continuous variable (rather than use of a single threshold) and turns this measurement into a probability that an individual patient is having an MI after accounting for other factors, including age, sex, comorbidities, and time from symptom onset.
For the current study, the CoDE-ACS model was trained in 10,000 patients with suspected acute coronary syndrome (ACS) who presented to 10 hospitals in Scotland as part of the High-STEACS trial evaluating the implementation of a high-sensitivity cardiac troponin I assay. The results were then validated in another 10,000 patients from six countries around the world.
“Using this model, the patient can have a troponin test on arrival at the emergency department. The other information on age, sex, clinical history, and time since symptom onset is keyed in, and it gives a probability on a scale of 0–100 as to whether the patient is having an MI,” Dr. Mills noted.
“It also has the capacity to incorporate more information over time. So, if there is a second troponin measurement made, then the model automatically refines the probability score,” he added.
The current study showed that use of the CoDE-ACS model identified more patients at presentation as having a low probability of having an MI than fixed cardiac troponin thresholds (61% vs. 27%) with a similar negative predictive value.
It also identified fewer patients as having a high probability of having an MI (10% vs. 16%) with a greater positive predictive value.
Among patients who were identified as having a low probability of MI, the rate of cardiac death was lower than the rate among those with intermediate or high probability at 30 days (0.1% vs. 0.5% and 1.8%) and 1 year (0.3% vs. 2.8% and 4.2%).
“The results show that the machine learning model doubles the proportion of patients who can be discharged with a single test compared to the current practice of using the threshold approach. It really is a game changer in terms of its potential to improve health efficiency,” Dr. Mills said.
In terms of ruling patients in as possibly having an MI, he pointed out that troponin levels are increased in patients with a wide range of other conditions, including heart failure, kidney failure, and atrial fibrillation.
“When using the threshold approach, only one in four patients with an elevated troponin level will actually be having an MI, and that leads to confusion,” he said. “This model takes into consideration these other conditions and so it can correctly identify three out of four patients with a high probability of having an MI. We can therefore be more confident that it is appropriate to refer those patients to cardiology and save a lot of potentially unnecessary investigations and treatments in the others.”
Dr. Mills said the model also seems to work when assessing patients early on.
“Around one-third of patients present within 3 hours of symptom onset, and actually these are a high-risk group because people who have genuine cardiac pain are normally extremely uncomfortable and tend to present quickly. Current guidelines require that we do two tests in all these individuals, but this new model incorporates the time of symptom onset into its estimates of probability and therefore allows us to rule out patients even when they present very early.”
He reported that a second test is required in only one in five patients – those whose first test indicated intermediate probability.
“The second test allows us to refine the probability further, allowing us to rule another half of those patients out. We are then left with a small proportion of patients – about 1 in 10 – who remain of intermediate probability and will require additional clinical judgment.”
Should improve inequities in MI diagnosis
Dr. Mills said the CoDE-ACS model will improve current inequities in MI diagnosis, because of which MI is underrecognized in women and younger people.
“Women have troponin concentrations that are half those of men, and although sex-specific troponin thresholds are recommended in the guidelines, they are not widely used. This automatically leads to underrecognition of heart disease in women. But this new machine learning model performs identically in men and women because it has been trained to recognize the different normal levels in men and women,” he explained.
“It will also help us not to underdiagnose MI in younger people who often have a less classical presentation of MI, and they also generally have very low concentrations of troponin, so any increase in troponin way below the current diagnostic threshold may be very relevant to their risk,” he added.
The researchers are planning a randomized trial of the new model to demonstrate the impact it could have on equality of care and overcrowding in the emergency department. In the trial, patients will be randomly assigned to undergo decision-making on the basis of troponin thresholds (current practice) or to undergo decision-making through the CoDE-ACS model.
“The hope is that this trial will show reductions in unnecessary hospital admissions and length of stay in the emergency department,” Dr. Mills said. Results are expected sometime next year.
“This algorithm is very well trained. It has learned on 20,000 patients, so it has a lot more experience than I have, and I have been a professor of cardiology for 20 years,” Dr. Mills said.
He said he believes these models will get even smarter in the future as more data are added.
“I think the future for good decision-making in emergency care will be informed by clinical decision support from well-trained machine learning algorithms and they will help us guide not just the diagnosis of MI but also heart failure and other important cardiac conditions,” he said.
‘Elegant and exciting’ data
Commenting on the study, John W. McEvoy, MB, University of Galway, Ireland, said: “These are elegant and exciting data; however, the inputs into the machine learning algorithm include all the necessary information to actually diagnose MI. So why predict MI, when a human diagnosis can just be made directly? The answer to this question may depend on whether we trust machines more than humans.”
Dr. Mills noted that clinical judgment will always be an important part of MI diagnosis.
“Currently, using the troponin threshold approach, experienced clinicians will be able to nuance the results, but invariably, there is disagreement on this, and this can be a major source of tension within clinical care. By providing more individualized information, this will help enormously in the decision-making process,” he said.
“This model is not about replacing clinical decision-making. It’s more about augmenting decision-making and giving clinicians guidance to be able to improve efficiency and reduce inequality,” he added.
The study was funded with support from the National Institute for Health Research and NHSX, the British Heart Foundation, and Wellcome Leap. Dr. Mills has received honoraria or consultancy from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. He is employed by the University of Edinburgh, which has filed a patent on the Collaboration for the Diagnosis and Evaluation of Acute Coronary Syndrome score.
A version of this article first appeared on Medscape.com.
Use of a machine-learning model that incorporates information from a single troponin test as well as other clinical data was superior to current practice as an aid to the diagnosis of myocardial infarction in the emergency department in a new study.
“Our results suggest that and free up space in the emergency department,” senior author Nicholas L. Mills, MD, University of Edinburgh, Scotland, said in an interview.
“And, perhaps even more importantly, use of this model could also increase the proportion of patients who are correctly identified as at a high probability of having an MI,” he added.
The study was published online in Nature Medicine.
The authors explained that at present, the likelihood of an MI diagnosis for patients presenting to the emergency department with chest pain is based on a fixed troponin threshold in serial tests at specific time points, but there are several problems with this approach.
First, a fixed troponin threshold is generally used for all patients, which does not account for age, sex, or comorbidities that are known to influence cardiac troponin concentrations. Second, the need to perform tests at specific time points for serial testing can be challenging in busy emergency departments.
And third, patients are categorized as being at low, intermediate, or high risk of MI on the basis of troponin thresholds alone, and the test does not take into account other important factors, such as the time of symptom onset or findings on the electrocardiogram.
“Our current practice of using the same threshold to rule in and rule out an MI for everyone, regardless of whether they are an 18-year-old female without a history of heart disease or an 85-year-old male with known heart failure, doesn’t perform well, and there’s a significant risk of misdiagnosis. There is also a high likelihood for inequalities in care, particularly between men and women,” Dr. Mills said.
The current study evaluated whether use of a machine learning model known as CoDE-ACS to guide decision-making could overcome some of these challenges.
The machine learning model assesses the whole spectrum of troponin levels as a continuous variable (rather than use of a single threshold) and turns this measurement into a probability that an individual patient is having an MI after accounting for other factors, including age, sex, comorbidities, and time from symptom onset.
For the current study, the CoDE-ACS model was trained in 10,000 patients with suspected acute coronary syndrome (ACS) who presented to 10 hospitals in Scotland as part of the High-STEACS trial evaluating the implementation of a high-sensitivity cardiac troponin I assay. The results were then validated in another 10,000 patients from six countries around the world.
“Using this model, the patient can have a troponin test on arrival at the emergency department. The other information on age, sex, clinical history, and time since symptom onset is keyed in, and it gives a probability on a scale of 0–100 as to whether the patient is having an MI,” Dr. Mills noted.
“It also has the capacity to incorporate more information over time. So, if there is a second troponin measurement made, then the model automatically refines the probability score,” he added.
The current study showed that use of the CoDE-ACS model identified more patients at presentation as having a low probability of having an MI than fixed cardiac troponin thresholds (61% vs. 27%) with a similar negative predictive value.
It also identified fewer patients as having a high probability of having an MI (10% vs. 16%) with a greater positive predictive value.
Among patients who were identified as having a low probability of MI, the rate of cardiac death was lower than the rate among those with intermediate or high probability at 30 days (0.1% vs. 0.5% and 1.8%) and 1 year (0.3% vs. 2.8% and 4.2%).
“The results show that the machine learning model doubles the proportion of patients who can be discharged with a single test compared to the current practice of using the threshold approach. It really is a game changer in terms of its potential to improve health efficiency,” Dr. Mills said.
In terms of ruling patients in as possibly having an MI, he pointed out that troponin levels are increased in patients with a wide range of other conditions, including heart failure, kidney failure, and atrial fibrillation.
“When using the threshold approach, only one in four patients with an elevated troponin level will actually be having an MI, and that leads to confusion,” he said. “This model takes into consideration these other conditions and so it can correctly identify three out of four patients with a high probability of having an MI. We can therefore be more confident that it is appropriate to refer those patients to cardiology and save a lot of potentially unnecessary investigations and treatments in the others.”
Dr. Mills said the model also seems to work when assessing patients early on.
“Around one-third of patients present within 3 hours of symptom onset, and actually these are a high-risk group because people who have genuine cardiac pain are normally extremely uncomfortable and tend to present quickly. Current guidelines require that we do two tests in all these individuals, but this new model incorporates the time of symptom onset into its estimates of probability and therefore allows us to rule out patients even when they present very early.”
He reported that a second test is required in only one in five patients – those whose first test indicated intermediate probability.
“The second test allows us to refine the probability further, allowing us to rule another half of those patients out. We are then left with a small proportion of patients – about 1 in 10 – who remain of intermediate probability and will require additional clinical judgment.”
Should improve inequities in MI diagnosis
Dr. Mills said the CoDE-ACS model will improve current inequities in MI diagnosis, because of which MI is underrecognized in women and younger people.
“Women have troponin concentrations that are half those of men, and although sex-specific troponin thresholds are recommended in the guidelines, they are not widely used. This automatically leads to underrecognition of heart disease in women. But this new machine learning model performs identically in men and women because it has been trained to recognize the different normal levels in men and women,” he explained.
“It will also help us not to underdiagnose MI in younger people who often have a less classical presentation of MI, and they also generally have very low concentrations of troponin, so any increase in troponin way below the current diagnostic threshold may be very relevant to their risk,” he added.
The researchers are planning a randomized trial of the new model to demonstrate the impact it could have on equality of care and overcrowding in the emergency department. In the trial, patients will be randomly assigned to undergo decision-making on the basis of troponin thresholds (current practice) or to undergo decision-making through the CoDE-ACS model.
“The hope is that this trial will show reductions in unnecessary hospital admissions and length of stay in the emergency department,” Dr. Mills said. Results are expected sometime next year.
“This algorithm is very well trained. It has learned on 20,000 patients, so it has a lot more experience than I have, and I have been a professor of cardiology for 20 years,” Dr. Mills said.
He said he believes these models will get even smarter in the future as more data are added.
“I think the future for good decision-making in emergency care will be informed by clinical decision support from well-trained machine learning algorithms and they will help us guide not just the diagnosis of MI but also heart failure and other important cardiac conditions,” he said.
‘Elegant and exciting’ data
Commenting on the study, John W. McEvoy, MB, University of Galway, Ireland, said: “These are elegant and exciting data; however, the inputs into the machine learning algorithm include all the necessary information to actually diagnose MI. So why predict MI, when a human diagnosis can just be made directly? The answer to this question may depend on whether we trust machines more than humans.”
Dr. Mills noted that clinical judgment will always be an important part of MI diagnosis.
“Currently, using the troponin threshold approach, experienced clinicians will be able to nuance the results, but invariably, there is disagreement on this, and this can be a major source of tension within clinical care. By providing more individualized information, this will help enormously in the decision-making process,” he said.
“This model is not about replacing clinical decision-making. It’s more about augmenting decision-making and giving clinicians guidance to be able to improve efficiency and reduce inequality,” he added.
The study was funded with support from the National Institute for Health Research and NHSX, the British Heart Foundation, and Wellcome Leap. Dr. Mills has received honoraria or consultancy from Abbott Diagnostics, Roche Diagnostics, Siemens Healthineers, and LumiraDx. He is employed by the University of Edinburgh, which has filed a patent on the Collaboration for the Diagnosis and Evaluation of Acute Coronary Syndrome score.
A version of this article first appeared on Medscape.com.
FROM NATURE MEDICINE
Age-specific cut-offs needed for cardiac troponin tests?
The study shows that the 99th percentile for the upper reference limit (used to define myocardial injury) for high-sensitivity (hs)–troponin T in the new analysis matched those reported by manufacturers. However, the same threshold for hs–troponin I was lower than was manufacturer-reported levels when considering the whole population.
And for both hs–troponin T and hs–troponin I, there were significant differences in 99th percentile levels by age.
“Our data suggest that some cases of myocardial injury may be missed in the whole population by using current non–age specific thresholds of troponin I,” lead author, John McEvoy, MB, University of Galway (Ireland), said in an interview. “If the non–age specific threshold was lowered to that in our cohort, then we would pick up more people with myocardial injury.”
“However,” Dr. McEvoy added, “if age-specific thresholds were deployed, then our data suggest that thresholds used to diagnose myocardial injury would need to be higher in older adults, somewhat lower in middle-aged individuals and much lower in younger people.”
The study was published online in the Journal of the American College of Cardiology.
The authors explain that the 99th percentile upper–reference limit threshold is the common benchmark of abnormality for all troponin assays. Five high-sensitivity cardiac troponin assays have been cleared by the Food and Drug Administration for clinical use and allow for earlier diagnosis of MI.
However, there has been variability in the approach used to define the 99th percentile upper reference limits for these assays, with definitions of healthy reference populations differing and the various assays available are not standardized or harmonized. So troponin concentrations at 99th percentiles do not align across assays, and the generalizability of manufacturer-reported reference upper reference limits for hs-troponin assays to the U.S. adult population is unknown.
They note that though sex-specific 99th percentile upper reference limits for hs-troponin have been recommended since 2018, age-specific thresholds are not yet endorsed, and whether thresholds differ by race or ethnicity is also controversial.
They aimed to investigate these issues using stored serum samples from adults aged 18 or older who participated in the 1999-2004 National Health and Nutrition Examination Survey (NHANES).
Dr. McEvoy described the NHANES database as “the gold standard cohort for representation of the U.S. adult population,” noting that other studies conducted by the manufacturers of the troponin tests have often used convenience samples from patients attending hospital clinics and blood donors, which he said were not representative of the whole population.
For the study, the researchers estimated that the 99th percentile upper reference limit for four hs-troponin assays (one troponin T and three troponin I) in a strictly defined healthy reference subgroup of 2,746 individuals from the NHANES cohort.
Results showed that the NHANES 99th percentile upper reference limit for hs–troponin T (19 ng/L) matched the manufacturer-reported level (19 ng/L). But, the NHANES upper reference levels for three troponin I assays were lower than were levels stated by the manufacturers.
The NHANES levels were 13 ng/L for the Abbott hs–troponin I assay (manufacturer: 28 ng/L); 5 ng/L for the Ortho hs–troponin I assay (manufacturer: 11 ng/L); and 37 ng/L for the Siemens hs–troponin I assay (manufacturer: 46.5 ng/L).
Furthermore, the 99th percentile upper reference limits for all four hs-troponin assays were statistically significantly lower in healthy adults younger than 40 years, compared with healthy adults older than 60 years.
There were also significant differences in upper reference limits by sex, but none by race/ethnicity.
Dr. McEvoy explained that NHANES is a very well phenotyped database with information on individuals’ health, body mass index, and other biomarkers. “This allows us to define a completely healthy subgroup of people, which could explain why the 99th percentile threshold for hs–troponin I was lower than previously reported from other cohorts,” he added.
Though there may be concern that such a healthy subgroup would mean the sample is enriched with younger people, whereas the typical person having their troponin measured would be older, Dr. McEvoy pointed out that there were more than 400 people older than 60 years in the healthy group. “This is probably the biggest cohort of super healthy older U.S. adults ever sampled in this regard,” he commented.
Dr. McEvoy said that the overall results from the study suggested that different thresholds might need to be considered for troponin I. “This could lead to threshold levels used to diagnose myocardial injury being cut in the population as a whole.”
But, he said a more important message was the need for age-specific thresholds.
“We found that troponin levels track with age. Even in individuals who age in a very healthy way, their troponin levels are greater than in younger people. This is the first time this has been shown with such clear statistical significance,” Dr. McEvoy said. “We think this data provides a compelling case for the use of age-specific cut-offs.”
He explained that, if age-specific thresholds were used to diagnose myocardial injury, the cut point from the current data would be higher than it would be from current manufacturers’ recommendations in those older than 60 years, so fewer people in this age group would be labeled as having myocardial injury.
“Our results suggest that, at present, we are seeing more false positives in older people leading to more unnecessary tests.” Using age-specific cut off points will reduce the number of false positives in older people. Dr. McEvoy noted a similar change in the way D-Dimer blood tests have been used to diagnose pulmonary embolism in recent years.
Using age-specific cut-offs for hs-troponin would also reduce the number of false negatives in younger people, Dr. McEvoy added.
Further studies needed?
In an accompanying editorial, Cian McCarthy, MB, Austin Vyas, and James Januzzi, MD, of Massachusetts General Hospital, Boston, note that though there are substantial shortcomings to using the 99th percentile upper reference limit of troponins for the diagnosis of cardiac injury, they believe this measurement should persist as a central component of the MI diagnostic criteria, with the caveat that this is only one component of the definition of MI and does not alone define it.
“Cardiac troponin measurement is one of the most commonly utilized blood tests in hospital-based settings, and yet important questions remain about what exactly is a normal value for this test,” the editorialists comment.
They say this new study emphasizes the importance of age and sex in interpretation of troponin levels.
“Although the use of such cut-offs may further complicate MI diagnostic criteria, this is superseded by the benefits of improved diagnostic accuracy in younger and female patients (a critical health equity step) while reducing MI overdiagnosis in the elderly, with the resultant harms that might follow, adverse psychosocial patient impact, and unnecessary health care expenditure from cascade testing,” they write.
They conclude that further large studies derived from healthy cohorts should be conducted to answer this question in a definitive fashion.
A version of this article first appeared on Medscape.com.
The study shows that the 99th percentile for the upper reference limit (used to define myocardial injury) for high-sensitivity (hs)–troponin T in the new analysis matched those reported by manufacturers. However, the same threshold for hs–troponin I was lower than was manufacturer-reported levels when considering the whole population.
And for both hs–troponin T and hs–troponin I, there were significant differences in 99th percentile levels by age.
“Our data suggest that some cases of myocardial injury may be missed in the whole population by using current non–age specific thresholds of troponin I,” lead author, John McEvoy, MB, University of Galway (Ireland), said in an interview. “If the non–age specific threshold was lowered to that in our cohort, then we would pick up more people with myocardial injury.”
“However,” Dr. McEvoy added, “if age-specific thresholds were deployed, then our data suggest that thresholds used to diagnose myocardial injury would need to be higher in older adults, somewhat lower in middle-aged individuals and much lower in younger people.”
The study was published online in the Journal of the American College of Cardiology.
The authors explain that the 99th percentile upper–reference limit threshold is the common benchmark of abnormality for all troponin assays. Five high-sensitivity cardiac troponin assays have been cleared by the Food and Drug Administration for clinical use and allow for earlier diagnosis of MI.
However, there has been variability in the approach used to define the 99th percentile upper reference limits for these assays, with definitions of healthy reference populations differing and the various assays available are not standardized or harmonized. So troponin concentrations at 99th percentiles do not align across assays, and the generalizability of manufacturer-reported reference upper reference limits for hs-troponin assays to the U.S. adult population is unknown.
They note that though sex-specific 99th percentile upper reference limits for hs-troponin have been recommended since 2018, age-specific thresholds are not yet endorsed, and whether thresholds differ by race or ethnicity is also controversial.
They aimed to investigate these issues using stored serum samples from adults aged 18 or older who participated in the 1999-2004 National Health and Nutrition Examination Survey (NHANES).
Dr. McEvoy described the NHANES database as “the gold standard cohort for representation of the U.S. adult population,” noting that other studies conducted by the manufacturers of the troponin tests have often used convenience samples from patients attending hospital clinics and blood donors, which he said were not representative of the whole population.
For the study, the researchers estimated that the 99th percentile upper reference limit for four hs-troponin assays (one troponin T and three troponin I) in a strictly defined healthy reference subgroup of 2,746 individuals from the NHANES cohort.
Results showed that the NHANES 99th percentile upper reference limit for hs–troponin T (19 ng/L) matched the manufacturer-reported level (19 ng/L). But, the NHANES upper reference levels for three troponin I assays were lower than were levels stated by the manufacturers.
The NHANES levels were 13 ng/L for the Abbott hs–troponin I assay (manufacturer: 28 ng/L); 5 ng/L for the Ortho hs–troponin I assay (manufacturer: 11 ng/L); and 37 ng/L for the Siemens hs–troponin I assay (manufacturer: 46.5 ng/L).
Furthermore, the 99th percentile upper reference limits for all four hs-troponin assays were statistically significantly lower in healthy adults younger than 40 years, compared with healthy adults older than 60 years.
There were also significant differences in upper reference limits by sex, but none by race/ethnicity.
Dr. McEvoy explained that NHANES is a very well phenotyped database with information on individuals’ health, body mass index, and other biomarkers. “This allows us to define a completely healthy subgroup of people, which could explain why the 99th percentile threshold for hs–troponin I was lower than previously reported from other cohorts,” he added.
Though there may be concern that such a healthy subgroup would mean the sample is enriched with younger people, whereas the typical person having their troponin measured would be older, Dr. McEvoy pointed out that there were more than 400 people older than 60 years in the healthy group. “This is probably the biggest cohort of super healthy older U.S. adults ever sampled in this regard,” he commented.
Dr. McEvoy said that the overall results from the study suggested that different thresholds might need to be considered for troponin I. “This could lead to threshold levels used to diagnose myocardial injury being cut in the population as a whole.”
But, he said a more important message was the need for age-specific thresholds.
“We found that troponin levels track with age. Even in individuals who age in a very healthy way, their troponin levels are greater than in younger people. This is the first time this has been shown with such clear statistical significance,” Dr. McEvoy said. “We think this data provides a compelling case for the use of age-specific cut-offs.”
He explained that, if age-specific thresholds were used to diagnose myocardial injury, the cut point from the current data would be higher than it would be from current manufacturers’ recommendations in those older than 60 years, so fewer people in this age group would be labeled as having myocardial injury.
“Our results suggest that, at present, we are seeing more false positives in older people leading to more unnecessary tests.” Using age-specific cut off points will reduce the number of false positives in older people. Dr. McEvoy noted a similar change in the way D-Dimer blood tests have been used to diagnose pulmonary embolism in recent years.
Using age-specific cut-offs for hs-troponin would also reduce the number of false negatives in younger people, Dr. McEvoy added.
Further studies needed?
In an accompanying editorial, Cian McCarthy, MB, Austin Vyas, and James Januzzi, MD, of Massachusetts General Hospital, Boston, note that though there are substantial shortcomings to using the 99th percentile upper reference limit of troponins for the diagnosis of cardiac injury, they believe this measurement should persist as a central component of the MI diagnostic criteria, with the caveat that this is only one component of the definition of MI and does not alone define it.
“Cardiac troponin measurement is one of the most commonly utilized blood tests in hospital-based settings, and yet important questions remain about what exactly is a normal value for this test,” the editorialists comment.
They say this new study emphasizes the importance of age and sex in interpretation of troponin levels.
“Although the use of such cut-offs may further complicate MI diagnostic criteria, this is superseded by the benefits of improved diagnostic accuracy in younger and female patients (a critical health equity step) while reducing MI overdiagnosis in the elderly, with the resultant harms that might follow, adverse psychosocial patient impact, and unnecessary health care expenditure from cascade testing,” they write.
They conclude that further large studies derived from healthy cohorts should be conducted to answer this question in a definitive fashion.
A version of this article first appeared on Medscape.com.
The study shows that the 99th percentile for the upper reference limit (used to define myocardial injury) for high-sensitivity (hs)–troponin T in the new analysis matched those reported by manufacturers. However, the same threshold for hs–troponin I was lower than was manufacturer-reported levels when considering the whole population.
And for both hs–troponin T and hs–troponin I, there were significant differences in 99th percentile levels by age.
“Our data suggest that some cases of myocardial injury may be missed in the whole population by using current non–age specific thresholds of troponin I,” lead author, John McEvoy, MB, University of Galway (Ireland), said in an interview. “If the non–age specific threshold was lowered to that in our cohort, then we would pick up more people with myocardial injury.”
“However,” Dr. McEvoy added, “if age-specific thresholds were deployed, then our data suggest that thresholds used to diagnose myocardial injury would need to be higher in older adults, somewhat lower in middle-aged individuals and much lower in younger people.”
The study was published online in the Journal of the American College of Cardiology.
The authors explain that the 99th percentile upper–reference limit threshold is the common benchmark of abnormality for all troponin assays. Five high-sensitivity cardiac troponin assays have been cleared by the Food and Drug Administration for clinical use and allow for earlier diagnosis of MI.
However, there has been variability in the approach used to define the 99th percentile upper reference limits for these assays, with definitions of healthy reference populations differing and the various assays available are not standardized or harmonized. So troponin concentrations at 99th percentiles do not align across assays, and the generalizability of manufacturer-reported reference upper reference limits for hs-troponin assays to the U.S. adult population is unknown.
They note that though sex-specific 99th percentile upper reference limits for hs-troponin have been recommended since 2018, age-specific thresholds are not yet endorsed, and whether thresholds differ by race or ethnicity is also controversial.
They aimed to investigate these issues using stored serum samples from adults aged 18 or older who participated in the 1999-2004 National Health and Nutrition Examination Survey (NHANES).
Dr. McEvoy described the NHANES database as “the gold standard cohort for representation of the U.S. adult population,” noting that other studies conducted by the manufacturers of the troponin tests have often used convenience samples from patients attending hospital clinics and blood donors, which he said were not representative of the whole population.
For the study, the researchers estimated that the 99th percentile upper reference limit for four hs-troponin assays (one troponin T and three troponin I) in a strictly defined healthy reference subgroup of 2,746 individuals from the NHANES cohort.
Results showed that the NHANES 99th percentile upper reference limit for hs–troponin T (19 ng/L) matched the manufacturer-reported level (19 ng/L). But, the NHANES upper reference levels for three troponin I assays were lower than were levels stated by the manufacturers.
The NHANES levels were 13 ng/L for the Abbott hs–troponin I assay (manufacturer: 28 ng/L); 5 ng/L for the Ortho hs–troponin I assay (manufacturer: 11 ng/L); and 37 ng/L for the Siemens hs–troponin I assay (manufacturer: 46.5 ng/L).
Furthermore, the 99th percentile upper reference limits for all four hs-troponin assays were statistically significantly lower in healthy adults younger than 40 years, compared with healthy adults older than 60 years.
There were also significant differences in upper reference limits by sex, but none by race/ethnicity.
Dr. McEvoy explained that NHANES is a very well phenotyped database with information on individuals’ health, body mass index, and other biomarkers. “This allows us to define a completely healthy subgroup of people, which could explain why the 99th percentile threshold for hs–troponin I was lower than previously reported from other cohorts,” he added.
Though there may be concern that such a healthy subgroup would mean the sample is enriched with younger people, whereas the typical person having their troponin measured would be older, Dr. McEvoy pointed out that there were more than 400 people older than 60 years in the healthy group. “This is probably the biggest cohort of super healthy older U.S. adults ever sampled in this regard,” he commented.
Dr. McEvoy said that the overall results from the study suggested that different thresholds might need to be considered for troponin I. “This could lead to threshold levels used to diagnose myocardial injury being cut in the population as a whole.”
But, he said a more important message was the need for age-specific thresholds.
“We found that troponin levels track with age. Even in individuals who age in a very healthy way, their troponin levels are greater than in younger people. This is the first time this has been shown with such clear statistical significance,” Dr. McEvoy said. “We think this data provides a compelling case for the use of age-specific cut-offs.”
He explained that, if age-specific thresholds were used to diagnose myocardial injury, the cut point from the current data would be higher than it would be from current manufacturers’ recommendations in those older than 60 years, so fewer people in this age group would be labeled as having myocardial injury.
“Our results suggest that, at present, we are seeing more false positives in older people leading to more unnecessary tests.” Using age-specific cut off points will reduce the number of false positives in older people. Dr. McEvoy noted a similar change in the way D-Dimer blood tests have been used to diagnose pulmonary embolism in recent years.
Using age-specific cut-offs for hs-troponin would also reduce the number of false negatives in younger people, Dr. McEvoy added.
Further studies needed?
In an accompanying editorial, Cian McCarthy, MB, Austin Vyas, and James Januzzi, MD, of Massachusetts General Hospital, Boston, note that though there are substantial shortcomings to using the 99th percentile upper reference limit of troponins for the diagnosis of cardiac injury, they believe this measurement should persist as a central component of the MI diagnostic criteria, with the caveat that this is only one component of the definition of MI and does not alone define it.
“Cardiac troponin measurement is one of the most commonly utilized blood tests in hospital-based settings, and yet important questions remain about what exactly is a normal value for this test,” the editorialists comment.
They say this new study emphasizes the importance of age and sex in interpretation of troponin levels.
“Although the use of such cut-offs may further complicate MI diagnostic criteria, this is superseded by the benefits of improved diagnostic accuracy in younger and female patients (a critical health equity step) while reducing MI overdiagnosis in the elderly, with the resultant harms that might follow, adverse psychosocial patient impact, and unnecessary health care expenditure from cascade testing,” they write.
They conclude that further large studies derived from healthy cohorts should be conducted to answer this question in a definitive fashion.
A version of this article first appeared on Medscape.com.
FROM JACC
Novel insights on Takotsubo syndrome could lead to new therapies
Takotsubo syndrome is a form of acute heart failure that mimics acute coronary syndromes, with troponin elevation and symptoms including chest pain and dyspnea, but without a culprit lesion on coronary angiography.
However, echocardiography shows the heart to be massively enlarged. The condition was named by Japanese researchers as the shape of the left ventricle resembles the Takotsubo fishing pot used to trap octopi.
The condition affects mainly older women and accounts for about 6% of female patients presenting with acute coronary syndrome symptoms. In around two-thirds of cases there is a triggering stress event which can be physical, such as an acute disease, or emotional, such as an argument or the sudden death of someone close, hence the term “broken heart syndrome.” The emotional stress triggering the syndrome can also be positive such as a birthday party or the birth of a grandchild.
“The mechanisms involved in Takotsubo syndrome are unknown. Because there is often a stress trigger it is believed that sympathetic activation causes a surge of catecholamine release, but that is not fully understood,” lead author of the current study, Thomas Stiermaier, MD, University Heart Center Lübeck (Germany), explained in an interview.
“We wanted to look more closely at the hemodynamic effects in the hearts of patients with Takotsubo syndrome to see if we could identify novel mechanisms contributing to the condition,” he added.
The aptly named Optimized Characterization of Takotsubo Syndrome by Obtaining Pressure Volume Loops (OCTOPUS) study was published online in the Journal of the American College of Cardiology.
For the study, the researchers used a conductance catheter inserted into the left ventricle of the heart to analyze pressure-volume relationships in 24 consecutive patients with Takotsubo syndrome and a control population of 20 participants without cardiovascular disease.
These pressure-volume loops are “the gold standard for direct, real-time assessment of systolic and diastolic cardiac function independent of loading conditions,” and “provide in-depth information regarding ventricular-arterial coupling and cardiac energetics and efficiency,” the authors wrote.
“These parameters comprise a considerable amount of information on cardiac performance and help to advance our understanding of cardiac physiology and its pathophysiological role in various conditions,” they noted, adding that this is believed to be the first comprehensive hemodynamic analysis in patients with Takotsubo syndrome using such invasive tracing of pressure-volume loops.
Results showed that Takotsubo syndrome is associated with a severely impaired cardiac contractility and a shortened systolic period. In response, the heart compensates by increasing left ventricular end diastolic volume to preserve the stroke volume.
Diastolic function is characterized by prolonged active relaxation but unaltered passive elastic properties. The analysis of myocardial energetics revealed an inefficient system with increased potential and decreased kinetic energy (stroke work).
“These are new and important findings,” Dr. Stiermaier said, adding that these hemodynamic changes give clues as to the underlying mechanisms at play in Takotsubo syndrome, as well as possible treatment strategies that could be investigated.
“Taking all this information together, we believe that it is likely that decreased phosphorylation of myofilament proteins – which may be caused by some kind of disturbance in calcium metabolism – may partially account for the impaired contractility and shortened systolic period seen in Takotsubo syndrome,” he commented.
The researchers suggested that Takotsubo syndrome may therefore be treated with medications such as omecamtiv (a drug that increases systolic duration) or the calcium sensitizer levosimendan, which improves contractility, possibly in combination with beta-blockers to protect against the intense adrenergic activation.
They noted that several studies have reported the use of levosimendan in Takotsubo syndrome and have suggested positive effects by accelerating recovery of ventricular function. But they added that prospective data are lacking, and, to their knowledge, omecamtiv has not been tested in Takotsubo syndrome.
“We need to clearly identify the mechanism involved in these changes at the cellular level, and then test these medications to see if they can help prevent or reverse the hemodynamic changes seen in Takotsubo syndrome,” Dr. Stiermaier said.
He explained that the contractile abnormalities in Takotsubo syndrome are transient and generally normalize after a few weeks or months, but while systolic function may appear normal in the long term there are other more subtle changes that can persist, and these patients have an increased rate of cardiovascular events, compared with the healthy population over the long term.
However, because Takotsubo syndrome patients generally have a high rate of other comorbidities, it is not known whether their increased event rate is caused by the syndrome or by these other comorbidities.
While some patients with Takotsubo syndrome have a mild disease course and a good prognosis, others have more complications, with around 10%-15% going on to develop severe disease with cardiogenic shock or pleural effusion, Dr. Stiermaier noted.
“These patients have a bad prognosis. Our aim is to try to identify the patients who are at high risk of these complications and treat them early to prevent cardiogenic shock and pleural effusion from developing,” he said. “We are hopeful that by identifying the hemodynamic changes occurring in Takotsubo syndrome we can figure out the mechanisms involved and give medications in the acute setting to prevent the complications that can arise down the road.”
Mechanisms ‘appealing but speculative’
In an editorial (J Am Coll Cardiol. 2023 May;81[20]:1992-5), Jorge Salamanca, MD, and Fernando Alfonso, MD, Hospital Universitario de La Princesa, Madrid, described this new study as “an important piece of research, providing a careful, systematic, and comprehensive set of sophisticated invasive hemodynamic data that shed new light on our understanding of this unique clinical entity.”
They said the researchers have provided “robust data on the acute hemodynamic behavior of the left ventricle in patients with Takotsubo syndrome that clearly advance the field but also raise new questions.”
But the editorialists cautioned that the hypotheses of the potential mechanisms linking a molecular basis for the metabolic dysregulation, resulting in increased potential energy coupled with a decreased kinetic energy, “are appealing but largely speculative.”
“Whether these hemodynamic findings could be the foundation and would support the use of novel and attractive drugs in Takotsubo syndrome, remains unsettled and can only be considered as hypothesis generating,” they wrote.
“Further studies are required to elucidate factors associated with a more severe hemodynamic derangement and to devise therapeutic strategies helping to rapidly restore an efficient left ventricular function in these challenging patients,” they concluded.
The study authors and the editorialists reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Takotsubo syndrome is a form of acute heart failure that mimics acute coronary syndromes, with troponin elevation and symptoms including chest pain and dyspnea, but without a culprit lesion on coronary angiography.
However, echocardiography shows the heart to be massively enlarged. The condition was named by Japanese researchers as the shape of the left ventricle resembles the Takotsubo fishing pot used to trap octopi.
The condition affects mainly older women and accounts for about 6% of female patients presenting with acute coronary syndrome symptoms. In around two-thirds of cases there is a triggering stress event which can be physical, such as an acute disease, or emotional, such as an argument or the sudden death of someone close, hence the term “broken heart syndrome.” The emotional stress triggering the syndrome can also be positive such as a birthday party or the birth of a grandchild.
“The mechanisms involved in Takotsubo syndrome are unknown. Because there is often a stress trigger it is believed that sympathetic activation causes a surge of catecholamine release, but that is not fully understood,” lead author of the current study, Thomas Stiermaier, MD, University Heart Center Lübeck (Germany), explained in an interview.
“We wanted to look more closely at the hemodynamic effects in the hearts of patients with Takotsubo syndrome to see if we could identify novel mechanisms contributing to the condition,” he added.
The aptly named Optimized Characterization of Takotsubo Syndrome by Obtaining Pressure Volume Loops (OCTOPUS) study was published online in the Journal of the American College of Cardiology.
For the study, the researchers used a conductance catheter inserted into the left ventricle of the heart to analyze pressure-volume relationships in 24 consecutive patients with Takotsubo syndrome and a control population of 20 participants without cardiovascular disease.
These pressure-volume loops are “the gold standard for direct, real-time assessment of systolic and diastolic cardiac function independent of loading conditions,” and “provide in-depth information regarding ventricular-arterial coupling and cardiac energetics and efficiency,” the authors wrote.
“These parameters comprise a considerable amount of information on cardiac performance and help to advance our understanding of cardiac physiology and its pathophysiological role in various conditions,” they noted, adding that this is believed to be the first comprehensive hemodynamic analysis in patients with Takotsubo syndrome using such invasive tracing of pressure-volume loops.
Results showed that Takotsubo syndrome is associated with a severely impaired cardiac contractility and a shortened systolic period. In response, the heart compensates by increasing left ventricular end diastolic volume to preserve the stroke volume.
Diastolic function is characterized by prolonged active relaxation but unaltered passive elastic properties. The analysis of myocardial energetics revealed an inefficient system with increased potential and decreased kinetic energy (stroke work).
“These are new and important findings,” Dr. Stiermaier said, adding that these hemodynamic changes give clues as to the underlying mechanisms at play in Takotsubo syndrome, as well as possible treatment strategies that could be investigated.
“Taking all this information together, we believe that it is likely that decreased phosphorylation of myofilament proteins – which may be caused by some kind of disturbance in calcium metabolism – may partially account for the impaired contractility and shortened systolic period seen in Takotsubo syndrome,” he commented.
The researchers suggested that Takotsubo syndrome may therefore be treated with medications such as omecamtiv (a drug that increases systolic duration) or the calcium sensitizer levosimendan, which improves contractility, possibly in combination with beta-blockers to protect against the intense adrenergic activation.
They noted that several studies have reported the use of levosimendan in Takotsubo syndrome and have suggested positive effects by accelerating recovery of ventricular function. But they added that prospective data are lacking, and, to their knowledge, omecamtiv has not been tested in Takotsubo syndrome.
“We need to clearly identify the mechanism involved in these changes at the cellular level, and then test these medications to see if they can help prevent or reverse the hemodynamic changes seen in Takotsubo syndrome,” Dr. Stiermaier said.
He explained that the contractile abnormalities in Takotsubo syndrome are transient and generally normalize after a few weeks or months, but while systolic function may appear normal in the long term there are other more subtle changes that can persist, and these patients have an increased rate of cardiovascular events, compared with the healthy population over the long term.
However, because Takotsubo syndrome patients generally have a high rate of other comorbidities, it is not known whether their increased event rate is caused by the syndrome or by these other comorbidities.
While some patients with Takotsubo syndrome have a mild disease course and a good prognosis, others have more complications, with around 10%-15% going on to develop severe disease with cardiogenic shock or pleural effusion, Dr. Stiermaier noted.
“These patients have a bad prognosis. Our aim is to try to identify the patients who are at high risk of these complications and treat them early to prevent cardiogenic shock and pleural effusion from developing,” he said. “We are hopeful that by identifying the hemodynamic changes occurring in Takotsubo syndrome we can figure out the mechanisms involved and give medications in the acute setting to prevent the complications that can arise down the road.”
Mechanisms ‘appealing but speculative’
In an editorial (J Am Coll Cardiol. 2023 May;81[20]:1992-5), Jorge Salamanca, MD, and Fernando Alfonso, MD, Hospital Universitario de La Princesa, Madrid, described this new study as “an important piece of research, providing a careful, systematic, and comprehensive set of sophisticated invasive hemodynamic data that shed new light on our understanding of this unique clinical entity.”
They said the researchers have provided “robust data on the acute hemodynamic behavior of the left ventricle in patients with Takotsubo syndrome that clearly advance the field but also raise new questions.”
But the editorialists cautioned that the hypotheses of the potential mechanisms linking a molecular basis for the metabolic dysregulation, resulting in increased potential energy coupled with a decreased kinetic energy, “are appealing but largely speculative.”
“Whether these hemodynamic findings could be the foundation and would support the use of novel and attractive drugs in Takotsubo syndrome, remains unsettled and can only be considered as hypothesis generating,” they wrote.
“Further studies are required to elucidate factors associated with a more severe hemodynamic derangement and to devise therapeutic strategies helping to rapidly restore an efficient left ventricular function in these challenging patients,” they concluded.
The study authors and the editorialists reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Takotsubo syndrome is a form of acute heart failure that mimics acute coronary syndromes, with troponin elevation and symptoms including chest pain and dyspnea, but without a culprit lesion on coronary angiography.
However, echocardiography shows the heart to be massively enlarged. The condition was named by Japanese researchers as the shape of the left ventricle resembles the Takotsubo fishing pot used to trap octopi.
The condition affects mainly older women and accounts for about 6% of female patients presenting with acute coronary syndrome symptoms. In around two-thirds of cases there is a triggering stress event which can be physical, such as an acute disease, or emotional, such as an argument or the sudden death of someone close, hence the term “broken heart syndrome.” The emotional stress triggering the syndrome can also be positive such as a birthday party or the birth of a grandchild.
“The mechanisms involved in Takotsubo syndrome are unknown. Because there is often a stress trigger it is believed that sympathetic activation causes a surge of catecholamine release, but that is not fully understood,” lead author of the current study, Thomas Stiermaier, MD, University Heart Center Lübeck (Germany), explained in an interview.
“We wanted to look more closely at the hemodynamic effects in the hearts of patients with Takotsubo syndrome to see if we could identify novel mechanisms contributing to the condition,” he added.
The aptly named Optimized Characterization of Takotsubo Syndrome by Obtaining Pressure Volume Loops (OCTOPUS) study was published online in the Journal of the American College of Cardiology.
For the study, the researchers used a conductance catheter inserted into the left ventricle of the heart to analyze pressure-volume relationships in 24 consecutive patients with Takotsubo syndrome and a control population of 20 participants without cardiovascular disease.
These pressure-volume loops are “the gold standard for direct, real-time assessment of systolic and diastolic cardiac function independent of loading conditions,” and “provide in-depth information regarding ventricular-arterial coupling and cardiac energetics and efficiency,” the authors wrote.
“These parameters comprise a considerable amount of information on cardiac performance and help to advance our understanding of cardiac physiology and its pathophysiological role in various conditions,” they noted, adding that this is believed to be the first comprehensive hemodynamic analysis in patients with Takotsubo syndrome using such invasive tracing of pressure-volume loops.
Results showed that Takotsubo syndrome is associated with a severely impaired cardiac contractility and a shortened systolic period. In response, the heart compensates by increasing left ventricular end diastolic volume to preserve the stroke volume.
Diastolic function is characterized by prolonged active relaxation but unaltered passive elastic properties. The analysis of myocardial energetics revealed an inefficient system with increased potential and decreased kinetic energy (stroke work).
“These are new and important findings,” Dr. Stiermaier said, adding that these hemodynamic changes give clues as to the underlying mechanisms at play in Takotsubo syndrome, as well as possible treatment strategies that could be investigated.
“Taking all this information together, we believe that it is likely that decreased phosphorylation of myofilament proteins – which may be caused by some kind of disturbance in calcium metabolism – may partially account for the impaired contractility and shortened systolic period seen in Takotsubo syndrome,” he commented.
The researchers suggested that Takotsubo syndrome may therefore be treated with medications such as omecamtiv (a drug that increases systolic duration) or the calcium sensitizer levosimendan, which improves contractility, possibly in combination with beta-blockers to protect against the intense adrenergic activation.
They noted that several studies have reported the use of levosimendan in Takotsubo syndrome and have suggested positive effects by accelerating recovery of ventricular function. But they added that prospective data are lacking, and, to their knowledge, omecamtiv has not been tested in Takotsubo syndrome.
“We need to clearly identify the mechanism involved in these changes at the cellular level, and then test these medications to see if they can help prevent or reverse the hemodynamic changes seen in Takotsubo syndrome,” Dr. Stiermaier said.
He explained that the contractile abnormalities in Takotsubo syndrome are transient and generally normalize after a few weeks or months, but while systolic function may appear normal in the long term there are other more subtle changes that can persist, and these patients have an increased rate of cardiovascular events, compared with the healthy population over the long term.
However, because Takotsubo syndrome patients generally have a high rate of other comorbidities, it is not known whether their increased event rate is caused by the syndrome or by these other comorbidities.
While some patients with Takotsubo syndrome have a mild disease course and a good prognosis, others have more complications, with around 10%-15% going on to develop severe disease with cardiogenic shock or pleural effusion, Dr. Stiermaier noted.
“These patients have a bad prognosis. Our aim is to try to identify the patients who are at high risk of these complications and treat them early to prevent cardiogenic shock and pleural effusion from developing,” he said. “We are hopeful that by identifying the hemodynamic changes occurring in Takotsubo syndrome we can figure out the mechanisms involved and give medications in the acute setting to prevent the complications that can arise down the road.”
Mechanisms ‘appealing but speculative’
In an editorial (J Am Coll Cardiol. 2023 May;81[20]:1992-5), Jorge Salamanca, MD, and Fernando Alfonso, MD, Hospital Universitario de La Princesa, Madrid, described this new study as “an important piece of research, providing a careful, systematic, and comprehensive set of sophisticated invasive hemodynamic data that shed new light on our understanding of this unique clinical entity.”
They said the researchers have provided “robust data on the acute hemodynamic behavior of the left ventricle in patients with Takotsubo syndrome that clearly advance the field but also raise new questions.”
But the editorialists cautioned that the hypotheses of the potential mechanisms linking a molecular basis for the metabolic dysregulation, resulting in increased potential energy coupled with a decreased kinetic energy, “are appealing but largely speculative.”
“Whether these hemodynamic findings could be the foundation and would support the use of novel and attractive drugs in Takotsubo syndrome, remains unsettled and can only be considered as hypothesis generating,” they wrote.
“Further studies are required to elucidate factors associated with a more severe hemodynamic derangement and to devise therapeutic strategies helping to rapidly restore an efficient left ventricular function in these challenging patients,” they concluded.
The study authors and the editorialists reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN JOURNAL OF CARDIOLOGY
Endovascular approach best for below-knee limb-threatening ischemia?
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Statin misinformation on social media flagged by AI
Using artificial intelligence to analyze large amounts of information from social media platforms generated some novel insights into public perceptions about statins, results of a new study show.
The study, which used AI to analyze discussions about statins on the social media platform Reddit, corroborated previously documented reasons for statin hesitancy, including adverse effect profiles and general disenfranchisement with health care.
But it also found novel points of discourse, including linking statins to COVID-19 outcomes and the role of cholesterol, statins, and the ketogenic diet.
“We used AI to tell us what is being discussed about statins on social media and to quantify the information in topics that people think are important,” senior study author Fatima Rodriguez, MD, MPH, Stanford (Calif.) University School of Medicine, said in an interview.
“Some of the themes were surprising to us. While we expected discussion on side effects, we were surprised to see so much discussion refuting the idea that increased levels of LDL were detrimental. There were also a large amount of posts on statin use being correlated to COVID outcomes. Our findings show how widespread this misinformation is,” she said.
“As a preventative cardiologist, I spend a lot of my time trying to get patients to take statins, but patients often rely on social media for information, and this can contain a lot of misinformation. People tend to be more honest on online forums than they are in the doctor’s office, so they are probably asking the questions and having discussions on subjects they really care about. So, understanding what is being discussed on social media is very valuable information for us as clinicians.”
The study was published online in JAMA Network Open.
The researchers analyzed all statin-related discussions on Reddit that were dated between Jan. 1, 2009, and July 12, 2022. Statin- and cholesterol-focused communities were identified to create a list of statin-related discussions. An AI pipeline was developed to cluster these discussions into specific topics and overarching thematic groups.
A total of 10,233 unique statin-related discussions and 5,188 unique authors were identified. A total of 100 discussion topics were identified and classified into six overarching thematic groups: (1) ketogenic diets, diabetes, supplements, and statins; (2) statin adverse effects; (3) statin hesitancy; (4) clinical trial appraisals; (5) pharmaceutical industry bias and statins; and (6) red yeast rice and statins.
Several examples of statin-related misinformation were identified, including distrust of the hypothesis that LDL-C has a causal association with heart disease. Discussions included quotes such as, “I think LDL is pretty much irrelevant. Your HDL and triglycerides are far more important.”
Other topics suggested that certain natural supplements would be an acceptable alternative to statins. Quotes included: “Red yeast rice is a statin basically, by the way,” and “statins are basically mycotoxins and deplete you of fat-soluble nutrients, like coQ10, vit D, K, A and E, and in all likelihood through these depletions worsen cardiovascular health.”
The researchers also looked at temporal trends and found that these sorts of discussions have increased over time.
One of the common themes identified was using the ketogenic diet phenomenon as an argument against increased cholesterol levels being bad for health.
Dr. Rodriguez elaborated: “People think the ketogenic diet is healthy as they lose weight on it. And as it can be associated with a small increase in LDL cholesterol, there was a lot of opinion that this meant increasing LDL was a good thing.”
The researchers also conducted a sentiment analysis, which designated topics as positive, negative, or neutral with regard to statins.
“We found that almost no topic was positive. Everything was either neutral or negative. This is pretty consistent with what we are seeing around hesitancy in clinical practice, but you would think that maybe a few people may have a positive view on statins,” Dr. Rodriguez commented.
“One of the problems with statins and lowering cholesterol is that it takes a long time to see a benefit, but this misinformation will result in some people not taking their medication,” she added.
Dr. Rodriguez noted that in this study AI is augmenting, not replacing, what clinicians and researchers do. “But it is a valuable tool to scan a large volume of information, and we have shown here it can generate new insights that we may not have thought of. It’s important to know what’s out there so we can try and combat it.”
She pointed out that patients don’t read the medical literature showing the benefits of statins but rather rely on social media for their information.
“We need to understand all sorts of patient engagement and use the same tools to combat this misinformation. We have a responsibility to try and stop dangerous and false information from being propagated,” she commented.
“These drugs are clearly not dangerous when used in line with clinical guidelines, and they have been proven to have multiple benefits again and again, but we don’t see those kinds of discussions in the community at all. We as clinicians need to use social media and AI to give out the right information. This could start to combat all the misinformation out there.”
A version of this article first appeared on Medscape.com.
Using artificial intelligence to analyze large amounts of information from social media platforms generated some novel insights into public perceptions about statins, results of a new study show.
The study, which used AI to analyze discussions about statins on the social media platform Reddit, corroborated previously documented reasons for statin hesitancy, including adverse effect profiles and general disenfranchisement with health care.
But it also found novel points of discourse, including linking statins to COVID-19 outcomes and the role of cholesterol, statins, and the ketogenic diet.
“We used AI to tell us what is being discussed about statins on social media and to quantify the information in topics that people think are important,” senior study author Fatima Rodriguez, MD, MPH, Stanford (Calif.) University School of Medicine, said in an interview.
“Some of the themes were surprising to us. While we expected discussion on side effects, we were surprised to see so much discussion refuting the idea that increased levels of LDL were detrimental. There were also a large amount of posts on statin use being correlated to COVID outcomes. Our findings show how widespread this misinformation is,” she said.
“As a preventative cardiologist, I spend a lot of my time trying to get patients to take statins, but patients often rely on social media for information, and this can contain a lot of misinformation. People tend to be more honest on online forums than they are in the doctor’s office, so they are probably asking the questions and having discussions on subjects they really care about. So, understanding what is being discussed on social media is very valuable information for us as clinicians.”
The study was published online in JAMA Network Open.
The researchers analyzed all statin-related discussions on Reddit that were dated between Jan. 1, 2009, and July 12, 2022. Statin- and cholesterol-focused communities were identified to create a list of statin-related discussions. An AI pipeline was developed to cluster these discussions into specific topics and overarching thematic groups.
A total of 10,233 unique statin-related discussions and 5,188 unique authors were identified. A total of 100 discussion topics were identified and classified into six overarching thematic groups: (1) ketogenic diets, diabetes, supplements, and statins; (2) statin adverse effects; (3) statin hesitancy; (4) clinical trial appraisals; (5) pharmaceutical industry bias and statins; and (6) red yeast rice and statins.
Several examples of statin-related misinformation were identified, including distrust of the hypothesis that LDL-C has a causal association with heart disease. Discussions included quotes such as, “I think LDL is pretty much irrelevant. Your HDL and triglycerides are far more important.”
Other topics suggested that certain natural supplements would be an acceptable alternative to statins. Quotes included: “Red yeast rice is a statin basically, by the way,” and “statins are basically mycotoxins and deplete you of fat-soluble nutrients, like coQ10, vit D, K, A and E, and in all likelihood through these depletions worsen cardiovascular health.”
The researchers also looked at temporal trends and found that these sorts of discussions have increased over time.
One of the common themes identified was using the ketogenic diet phenomenon as an argument against increased cholesterol levels being bad for health.
Dr. Rodriguez elaborated: “People think the ketogenic diet is healthy as they lose weight on it. And as it can be associated with a small increase in LDL cholesterol, there was a lot of opinion that this meant increasing LDL was a good thing.”
The researchers also conducted a sentiment analysis, which designated topics as positive, negative, or neutral with regard to statins.
“We found that almost no topic was positive. Everything was either neutral or negative. This is pretty consistent with what we are seeing around hesitancy in clinical practice, but you would think that maybe a few people may have a positive view on statins,” Dr. Rodriguez commented.
“One of the problems with statins and lowering cholesterol is that it takes a long time to see a benefit, but this misinformation will result in some people not taking their medication,” she added.
Dr. Rodriguez noted that in this study AI is augmenting, not replacing, what clinicians and researchers do. “But it is a valuable tool to scan a large volume of information, and we have shown here it can generate new insights that we may not have thought of. It’s important to know what’s out there so we can try and combat it.”
She pointed out that patients don’t read the medical literature showing the benefits of statins but rather rely on social media for their information.
“We need to understand all sorts of patient engagement and use the same tools to combat this misinformation. We have a responsibility to try and stop dangerous and false information from being propagated,” she commented.
“These drugs are clearly not dangerous when used in line with clinical guidelines, and they have been proven to have multiple benefits again and again, but we don’t see those kinds of discussions in the community at all. We as clinicians need to use social media and AI to give out the right information. This could start to combat all the misinformation out there.”
A version of this article first appeared on Medscape.com.
Using artificial intelligence to analyze large amounts of information from social media platforms generated some novel insights into public perceptions about statins, results of a new study show.
The study, which used AI to analyze discussions about statins on the social media platform Reddit, corroborated previously documented reasons for statin hesitancy, including adverse effect profiles and general disenfranchisement with health care.
But it also found novel points of discourse, including linking statins to COVID-19 outcomes and the role of cholesterol, statins, and the ketogenic diet.
“We used AI to tell us what is being discussed about statins on social media and to quantify the information in topics that people think are important,” senior study author Fatima Rodriguez, MD, MPH, Stanford (Calif.) University School of Medicine, said in an interview.
“Some of the themes were surprising to us. While we expected discussion on side effects, we were surprised to see so much discussion refuting the idea that increased levels of LDL were detrimental. There were also a large amount of posts on statin use being correlated to COVID outcomes. Our findings show how widespread this misinformation is,” she said.
“As a preventative cardiologist, I spend a lot of my time trying to get patients to take statins, but patients often rely on social media for information, and this can contain a lot of misinformation. People tend to be more honest on online forums than they are in the doctor’s office, so they are probably asking the questions and having discussions on subjects they really care about. So, understanding what is being discussed on social media is very valuable information for us as clinicians.”
The study was published online in JAMA Network Open.
The researchers analyzed all statin-related discussions on Reddit that were dated between Jan. 1, 2009, and July 12, 2022. Statin- and cholesterol-focused communities were identified to create a list of statin-related discussions. An AI pipeline was developed to cluster these discussions into specific topics and overarching thematic groups.
A total of 10,233 unique statin-related discussions and 5,188 unique authors were identified. A total of 100 discussion topics were identified and classified into six overarching thematic groups: (1) ketogenic diets, diabetes, supplements, and statins; (2) statin adverse effects; (3) statin hesitancy; (4) clinical trial appraisals; (5) pharmaceutical industry bias and statins; and (6) red yeast rice and statins.
Several examples of statin-related misinformation were identified, including distrust of the hypothesis that LDL-C has a causal association with heart disease. Discussions included quotes such as, “I think LDL is pretty much irrelevant. Your HDL and triglycerides are far more important.”
Other topics suggested that certain natural supplements would be an acceptable alternative to statins. Quotes included: “Red yeast rice is a statin basically, by the way,” and “statins are basically mycotoxins and deplete you of fat-soluble nutrients, like coQ10, vit D, K, A and E, and in all likelihood through these depletions worsen cardiovascular health.”
The researchers also looked at temporal trends and found that these sorts of discussions have increased over time.
One of the common themes identified was using the ketogenic diet phenomenon as an argument against increased cholesterol levels being bad for health.
Dr. Rodriguez elaborated: “People think the ketogenic diet is healthy as they lose weight on it. And as it can be associated with a small increase in LDL cholesterol, there was a lot of opinion that this meant increasing LDL was a good thing.”
The researchers also conducted a sentiment analysis, which designated topics as positive, negative, or neutral with regard to statins.
“We found that almost no topic was positive. Everything was either neutral or negative. This is pretty consistent with what we are seeing around hesitancy in clinical practice, but you would think that maybe a few people may have a positive view on statins,” Dr. Rodriguez commented.
“One of the problems with statins and lowering cholesterol is that it takes a long time to see a benefit, but this misinformation will result in some people not taking their medication,” she added.
Dr. Rodriguez noted that in this study AI is augmenting, not replacing, what clinicians and researchers do. “But it is a valuable tool to scan a large volume of information, and we have shown here it can generate new insights that we may not have thought of. It’s important to know what’s out there so we can try and combat it.”
She pointed out that patients don’t read the medical literature showing the benefits of statins but rather rely on social media for their information.
“We need to understand all sorts of patient engagement and use the same tools to combat this misinformation. We have a responsibility to try and stop dangerous and false information from being propagated,” she commented.
“These drugs are clearly not dangerous when used in line with clinical guidelines, and they have been proven to have multiple benefits again and again, but we don’t see those kinds of discussions in the community at all. We as clinicians need to use social media and AI to give out the right information. This could start to combat all the misinformation out there.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Gut microbiome may guide personalized heart failure therapy
Understanding more about the gut microbiome and how it may affect the development and treatment of heart failure could lead to a more personalized approach to managing the condition, a new review article suggests.
the authors note. “Interactions among the gut microbiome, diet, and medications offer potentially innovative modalities for management of patients with heart failure,” they add.
The review was published online in the Journal of the American College of Cardiology.
“Over the past years we have gathered more understanding about how important the gut microbiome is in relation to how our bodies function overall and even though the cardiovascular system and the heart itself may appear to be quite distant from the gut, we know the gut microbiome affects the cardiovascular system and the physiology of heart failure,” lead author Petra Mamic, MD, Stanford (Calif.) University, told this news organization.
“We’ve also learnt that the microbiome is very personalized. It seems to be affected by a lot of intrinsic and as well as extrinsic factors. For cardiovascular diseases in particular, we always knew that diet and lifestyle were part of the environmental risk, and we now believe that the gut microbiome may be one of the factors that mediates that risk,” she said.
“Studies on the gut microbiome are difficult to do and we are right at the beginning of this type of research. But we have learned that the microbiome is altered or dysregulated in many diseases including many cardiovascular diseases, and many of the changes in the microbiome we see in different cardiovascular diseases seem to overlap,” she added.
Dr. Mamic explained that patients with heart failure have a microbiome that appears different and dysregulated, compared with the microbiome in healthy individuals.
“The difficulty is teasing out whether the microbiome changes are causing heart failure or if they are a consequence of the heart failure and all the medications and comorbidities associated with heart failure,” she commented.
Animal studies have shown that many microbial products, small molecules made by the microbiome, seem to affect how the heart recovers from injury, for example after a myocardial infarction, and how much the heart scars and hypertrophies after an injury, Dr. Mamic reported. These microbiome-derived small molecules can also affect blood pressure, which is dysregulated in heart failure.
Other products of the microbiome can be pro-inflammatory or anti-inflammatory, which can again affect the cardiovascular physiology and the heart, she noted.
High-fiber diet may be beneficial
One area of particular interest at present involves the role of short-chain fatty acids, which are a byproduct of microbes in the gut that digest fiber.
“These short chain fatty acids seem to have positive effects on the host physiology. They are anti-inflammatory; they lower blood pressure; and they seem to protect the heart from scarring and hypertrophy after injury. In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted,” Dr. Mamic explained.
They are an obvious focus of interest because these short-chain fatty acids are produced when gut bacteria break down dietary fiber, raising the possibility of beneficial effects from eating a high-fiber diet.
Another product of the gut microbiome of interest is trimethylamine N-oxide, formed when gut bacteria break down nutrients such as L-carnitine and phosphatidyl choline, nutrients abundant in foods of animal origin, especially red meat. This metabolite has proatherogenic and prothrombotic effects, and negatively affected cardiac remodeling in a mouse heart failure model, the review notes.
However, though it is too early to make specific dietary recommendations based on these findings, Dr. Mamic points out that a high-fiber diet is thought to be beneficial.
“Nutritional research is very hard to do and the data is limited, but as best as we can summarize things, we know that plant-based diets such as the Mediterranean and DASH diets seem to prevent some of the risk factors for the development of heart failure and seem to slow the progression of heart failure,” she added.
One of the major recommendations in these diets is a high intake of fiber, including whole foods, vegetables, fruits, legumes, and nuts, and less intake of processed food and red meat. “In general, I think everyone should eat like that, but I specifically recommend a plant-based diet with a high amount of fiber to my heart failure patients,” Dr. Mamic said.
Large variation in microbiome composition
The review also explores the idea of personalization of diet or specific treatments dependent on an individual’s gut microbiome composition.
Dr. Mamic explains: “When we look at the microbiome composition between individuals, it is very different. There is very little overlap between individuals, even in people who are related. It seems to be more to do with the environment – people who are living together are more likely to have similarities in their microbiome. We are still trying to understand what drives these differences.”
It is thought that these differences may affect the response to a specific diet or medication. Dr. Mamic gives the example of fiber. “Not all bacteria can digest the same types of fiber, so not everyone responds in the same way to a high-fiber diet. That’s probably because of differences in their microbiome.”
Another example is the response to the heart failure drug digoxin, which is metabolized by one particular strain of bacteria in the gut. The toxicity or effectiveness of digoxin seems to be influenced by levels of this bacterial strain, and this again can be influenced by diet, Dr. Mamic says.
Manipulating the microbiome as a therapeutic strategy
Microbiome-targeting therapies may also become part of future treatment strategies for many conditions, including heart failure, the review authors say.
Probiotics (foods and dietary supplements that contain live microbes) interact with the gut microbiota to alter host physiology beneficially. Certain probiotics may specifically modulate processes dysregulated in heart failure, as was suggested in a rodent heart failure model in which supplementation with Lactobacillus-containing and Bifidobacterium-containing probiotics resulted in markedly improved cardiac function, the authors report.
However, a randomized trial (GutHeart) of probiotic yeast Saccharomyces boulardii in patients with heart failure found no improvement in cardiac function, compared with standard care.
Commenting on this, Dr. Mamic suggested that a more specific approach may be needed.
“Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria,” Dr. Mamic said. These bacteria are commercially available as a probiotic, and the researchers are planning a study to give patients with heart failure these specific probiotics. “We are trying to find practical ways forward and to be guided by the data. These people have very little Bifidobacteria, and we know that probiotics seem to be accepted best by the host where there is a specific need for them, so this seems like a sensible approach.”
Dr. Mamic does not recommend that heart failure patients take general probiotic products at present, but she tells her patients about the study she is doing. “Probiotics are quite different from each other. It is a very unregulated market. A general probiotic product may not contain the specific bacteria needed.”
Include microbiome data in biobanks
The review calls for more research on the subject and a more systematic approach to collecting data on the microbiome.
“At present for medical research, blood samples are collected, stored, and analyzed routinely. I think we should also be collecting stool samples in the same way to analyze the microbiome,” Dr. Mamic suggests.
“If we can combine that with data from blood tests on various metabolites/cytokines and look at how the microbiome changes over time or with medication, or with diet, and how the host responds including clinically relevant data, that would be really important. Given how quickly the field is growing I would think there would be biobanks including the microbiome in a few years’ time.”
“We need to gather this data. We would be looking for which bacteria are there, what their functionality is, how it changes over time, with diet or medication, and even whether we can use the microbiome data to predict who will respond to a specific drug.”
Dr. Mamic believes that in the future, analysis of the microbiome could be a routine part of deciding what people eat for good health and to characterize patients for personalized therapies.
“It is clear that the microbiome can influence health, and a dysregulated microbiome negatively affects the host, but there is lot of work to do. We need to learn a lot more about it, but we shouldn’t miss the opportunity to do this,” she concluded.
Dr. Mamic reported no disclosures.
A version of this article first appeared on Medscape.com.
Understanding more about the gut microbiome and how it may affect the development and treatment of heart failure could lead to a more personalized approach to managing the condition, a new review article suggests.
the authors note. “Interactions among the gut microbiome, diet, and medications offer potentially innovative modalities for management of patients with heart failure,” they add.
The review was published online in the Journal of the American College of Cardiology.
“Over the past years we have gathered more understanding about how important the gut microbiome is in relation to how our bodies function overall and even though the cardiovascular system and the heart itself may appear to be quite distant from the gut, we know the gut microbiome affects the cardiovascular system and the physiology of heart failure,” lead author Petra Mamic, MD, Stanford (Calif.) University, told this news organization.
“We’ve also learnt that the microbiome is very personalized. It seems to be affected by a lot of intrinsic and as well as extrinsic factors. For cardiovascular diseases in particular, we always knew that diet and lifestyle were part of the environmental risk, and we now believe that the gut microbiome may be one of the factors that mediates that risk,” she said.
“Studies on the gut microbiome are difficult to do and we are right at the beginning of this type of research. But we have learned that the microbiome is altered or dysregulated in many diseases including many cardiovascular diseases, and many of the changes in the microbiome we see in different cardiovascular diseases seem to overlap,” she added.
Dr. Mamic explained that patients with heart failure have a microbiome that appears different and dysregulated, compared with the microbiome in healthy individuals.
“The difficulty is teasing out whether the microbiome changes are causing heart failure or if they are a consequence of the heart failure and all the medications and comorbidities associated with heart failure,” she commented.
Animal studies have shown that many microbial products, small molecules made by the microbiome, seem to affect how the heart recovers from injury, for example after a myocardial infarction, and how much the heart scars and hypertrophies after an injury, Dr. Mamic reported. These microbiome-derived small molecules can also affect blood pressure, which is dysregulated in heart failure.
Other products of the microbiome can be pro-inflammatory or anti-inflammatory, which can again affect the cardiovascular physiology and the heart, she noted.
High-fiber diet may be beneficial
One area of particular interest at present involves the role of short-chain fatty acids, which are a byproduct of microbes in the gut that digest fiber.
“These short chain fatty acids seem to have positive effects on the host physiology. They are anti-inflammatory; they lower blood pressure; and they seem to protect the heart from scarring and hypertrophy after injury. In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted,” Dr. Mamic explained.
They are an obvious focus of interest because these short-chain fatty acids are produced when gut bacteria break down dietary fiber, raising the possibility of beneficial effects from eating a high-fiber diet.
Another product of the gut microbiome of interest is trimethylamine N-oxide, formed when gut bacteria break down nutrients such as L-carnitine and phosphatidyl choline, nutrients abundant in foods of animal origin, especially red meat. This metabolite has proatherogenic and prothrombotic effects, and negatively affected cardiac remodeling in a mouse heart failure model, the review notes.
However, though it is too early to make specific dietary recommendations based on these findings, Dr. Mamic points out that a high-fiber diet is thought to be beneficial.
“Nutritional research is very hard to do and the data is limited, but as best as we can summarize things, we know that plant-based diets such as the Mediterranean and DASH diets seem to prevent some of the risk factors for the development of heart failure and seem to slow the progression of heart failure,” she added.
One of the major recommendations in these diets is a high intake of fiber, including whole foods, vegetables, fruits, legumes, and nuts, and less intake of processed food and red meat. “In general, I think everyone should eat like that, but I specifically recommend a plant-based diet with a high amount of fiber to my heart failure patients,” Dr. Mamic said.
Large variation in microbiome composition
The review also explores the idea of personalization of diet or specific treatments dependent on an individual’s gut microbiome composition.
Dr. Mamic explains: “When we look at the microbiome composition between individuals, it is very different. There is very little overlap between individuals, even in people who are related. It seems to be more to do with the environment – people who are living together are more likely to have similarities in their microbiome. We are still trying to understand what drives these differences.”
It is thought that these differences may affect the response to a specific diet or medication. Dr. Mamic gives the example of fiber. “Not all bacteria can digest the same types of fiber, so not everyone responds in the same way to a high-fiber diet. That’s probably because of differences in their microbiome.”
Another example is the response to the heart failure drug digoxin, which is metabolized by one particular strain of bacteria in the gut. The toxicity or effectiveness of digoxin seems to be influenced by levels of this bacterial strain, and this again can be influenced by diet, Dr. Mamic says.
Manipulating the microbiome as a therapeutic strategy
Microbiome-targeting therapies may also become part of future treatment strategies for many conditions, including heart failure, the review authors say.
Probiotics (foods and dietary supplements that contain live microbes) interact with the gut microbiota to alter host physiology beneficially. Certain probiotics may specifically modulate processes dysregulated in heart failure, as was suggested in a rodent heart failure model in which supplementation with Lactobacillus-containing and Bifidobacterium-containing probiotics resulted in markedly improved cardiac function, the authors report.
However, a randomized trial (GutHeart) of probiotic yeast Saccharomyces boulardii in patients with heart failure found no improvement in cardiac function, compared with standard care.
Commenting on this, Dr. Mamic suggested that a more specific approach may be needed.
“Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria,” Dr. Mamic said. These bacteria are commercially available as a probiotic, and the researchers are planning a study to give patients with heart failure these specific probiotics. “We are trying to find practical ways forward and to be guided by the data. These people have very little Bifidobacteria, and we know that probiotics seem to be accepted best by the host where there is a specific need for them, so this seems like a sensible approach.”
Dr. Mamic does not recommend that heart failure patients take general probiotic products at present, but she tells her patients about the study she is doing. “Probiotics are quite different from each other. It is a very unregulated market. A general probiotic product may not contain the specific bacteria needed.”
Include microbiome data in biobanks
The review calls for more research on the subject and a more systematic approach to collecting data on the microbiome.
“At present for medical research, blood samples are collected, stored, and analyzed routinely. I think we should also be collecting stool samples in the same way to analyze the microbiome,” Dr. Mamic suggests.
“If we can combine that with data from blood tests on various metabolites/cytokines and look at how the microbiome changes over time or with medication, or with diet, and how the host responds including clinically relevant data, that would be really important. Given how quickly the field is growing I would think there would be biobanks including the microbiome in a few years’ time.”
“We need to gather this data. We would be looking for which bacteria are there, what their functionality is, how it changes over time, with diet or medication, and even whether we can use the microbiome data to predict who will respond to a specific drug.”
Dr. Mamic believes that in the future, analysis of the microbiome could be a routine part of deciding what people eat for good health and to characterize patients for personalized therapies.
“It is clear that the microbiome can influence health, and a dysregulated microbiome negatively affects the host, but there is lot of work to do. We need to learn a lot more about it, but we shouldn’t miss the opportunity to do this,” she concluded.
Dr. Mamic reported no disclosures.
A version of this article first appeared on Medscape.com.
Understanding more about the gut microbiome and how it may affect the development and treatment of heart failure could lead to a more personalized approach to managing the condition, a new review article suggests.
the authors note. “Interactions among the gut microbiome, diet, and medications offer potentially innovative modalities for management of patients with heart failure,” they add.
The review was published online in the Journal of the American College of Cardiology.
“Over the past years we have gathered more understanding about how important the gut microbiome is in relation to how our bodies function overall and even though the cardiovascular system and the heart itself may appear to be quite distant from the gut, we know the gut microbiome affects the cardiovascular system and the physiology of heart failure,” lead author Petra Mamic, MD, Stanford (Calif.) University, told this news organization.
“We’ve also learnt that the microbiome is very personalized. It seems to be affected by a lot of intrinsic and as well as extrinsic factors. For cardiovascular diseases in particular, we always knew that diet and lifestyle were part of the environmental risk, and we now believe that the gut microbiome may be one of the factors that mediates that risk,” she said.
“Studies on the gut microbiome are difficult to do and we are right at the beginning of this type of research. But we have learned that the microbiome is altered or dysregulated in many diseases including many cardiovascular diseases, and many of the changes in the microbiome we see in different cardiovascular diseases seem to overlap,” she added.
Dr. Mamic explained that patients with heart failure have a microbiome that appears different and dysregulated, compared with the microbiome in healthy individuals.
“The difficulty is teasing out whether the microbiome changes are causing heart failure or if they are a consequence of the heart failure and all the medications and comorbidities associated with heart failure,” she commented.
Animal studies have shown that many microbial products, small molecules made by the microbiome, seem to affect how the heart recovers from injury, for example after a myocardial infarction, and how much the heart scars and hypertrophies after an injury, Dr. Mamic reported. These microbiome-derived small molecules can also affect blood pressure, which is dysregulated in heart failure.
Other products of the microbiome can be pro-inflammatory or anti-inflammatory, which can again affect the cardiovascular physiology and the heart, she noted.
High-fiber diet may be beneficial
One area of particular interest at present involves the role of short-chain fatty acids, which are a byproduct of microbes in the gut that digest fiber.
“These short chain fatty acids seem to have positive effects on the host physiology. They are anti-inflammatory; they lower blood pressure; and they seem to protect the heart from scarring and hypertrophy after injury. In heart failure, the gut microbes that make these short-chain fatty acids are significantly depleted,” Dr. Mamic explained.
They are an obvious focus of interest because these short-chain fatty acids are produced when gut bacteria break down dietary fiber, raising the possibility of beneficial effects from eating a high-fiber diet.
Another product of the gut microbiome of interest is trimethylamine N-oxide, formed when gut bacteria break down nutrients such as L-carnitine and phosphatidyl choline, nutrients abundant in foods of animal origin, especially red meat. This metabolite has proatherogenic and prothrombotic effects, and negatively affected cardiac remodeling in a mouse heart failure model, the review notes.
However, though it is too early to make specific dietary recommendations based on these findings, Dr. Mamic points out that a high-fiber diet is thought to be beneficial.
“Nutritional research is very hard to do and the data is limited, but as best as we can summarize things, we know that plant-based diets such as the Mediterranean and DASH diets seem to prevent some of the risk factors for the development of heart failure and seem to slow the progression of heart failure,” she added.
One of the major recommendations in these diets is a high intake of fiber, including whole foods, vegetables, fruits, legumes, and nuts, and less intake of processed food and red meat. “In general, I think everyone should eat like that, but I specifically recommend a plant-based diet with a high amount of fiber to my heart failure patients,” Dr. Mamic said.
Large variation in microbiome composition
The review also explores the idea of personalization of diet or specific treatments dependent on an individual’s gut microbiome composition.
Dr. Mamic explains: “When we look at the microbiome composition between individuals, it is very different. There is very little overlap between individuals, even in people who are related. It seems to be more to do with the environment – people who are living together are more likely to have similarities in their microbiome. We are still trying to understand what drives these differences.”
It is thought that these differences may affect the response to a specific diet or medication. Dr. Mamic gives the example of fiber. “Not all bacteria can digest the same types of fiber, so not everyone responds in the same way to a high-fiber diet. That’s probably because of differences in their microbiome.”
Another example is the response to the heart failure drug digoxin, which is metabolized by one particular strain of bacteria in the gut. The toxicity or effectiveness of digoxin seems to be influenced by levels of this bacterial strain, and this again can be influenced by diet, Dr. Mamic says.
Manipulating the microbiome as a therapeutic strategy
Microbiome-targeting therapies may also become part of future treatment strategies for many conditions, including heart failure, the review authors say.
Probiotics (foods and dietary supplements that contain live microbes) interact with the gut microbiota to alter host physiology beneficially. Certain probiotics may specifically modulate processes dysregulated in heart failure, as was suggested in a rodent heart failure model in which supplementation with Lactobacillus-containing and Bifidobacterium-containing probiotics resulted in markedly improved cardiac function, the authors report.
However, a randomized trial (GutHeart) of probiotic yeast Saccharomyces boulardii in patients with heart failure found no improvement in cardiac function, compared with standard care.
Commenting on this, Dr. Mamic suggested that a more specific approach may be needed.
“Some of our preliminary data have shown people who have heart failure have severely depleted Bifidobacteria,” Dr. Mamic said. These bacteria are commercially available as a probiotic, and the researchers are planning a study to give patients with heart failure these specific probiotics. “We are trying to find practical ways forward and to be guided by the data. These people have very little Bifidobacteria, and we know that probiotics seem to be accepted best by the host where there is a specific need for them, so this seems like a sensible approach.”
Dr. Mamic does not recommend that heart failure patients take general probiotic products at present, but she tells her patients about the study she is doing. “Probiotics are quite different from each other. It is a very unregulated market. A general probiotic product may not contain the specific bacteria needed.”
Include microbiome data in biobanks
The review calls for more research on the subject and a more systematic approach to collecting data on the microbiome.
“At present for medical research, blood samples are collected, stored, and analyzed routinely. I think we should also be collecting stool samples in the same way to analyze the microbiome,” Dr. Mamic suggests.
“If we can combine that with data from blood tests on various metabolites/cytokines and look at how the microbiome changes over time or with medication, or with diet, and how the host responds including clinically relevant data, that would be really important. Given how quickly the field is growing I would think there would be biobanks including the microbiome in a few years’ time.”
“We need to gather this data. We would be looking for which bacteria are there, what their functionality is, how it changes over time, with diet or medication, and even whether we can use the microbiome data to predict who will respond to a specific drug.”
Dr. Mamic believes that in the future, analysis of the microbiome could be a routine part of deciding what people eat for good health and to characterize patients for personalized therapies.
“It is clear that the microbiome can influence health, and a dysregulated microbiome negatively affects the host, but there is lot of work to do. We need to learn a lot more about it, but we shouldn’t miss the opportunity to do this,” she concluded.
Dr. Mamic reported no disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
‘Bony’ stroke: Bone defects can cause recurrent stroke
These so-called “bony” strokes constitute a possible cause of recurrent ischemia in the same vascular territory as previous episodes, note the authors, led by Johanna Haertl, MD, Technical University of Munich.
“In patients with recurrent strokes in one vascular territory the presence of a symptomatic anatomic bone or cartilage anomaly may be considered as a differential diagnosis after sufficient exclusion of competing etiologies of an ischemic stroke,” they conclude.
“Due to the possibly high risk of stroke recurrence and potentially causative treatment options, bony strokes seem to be highly relevant for clinical practice,” they add.
The study was published online in the journal Stroke.
In their report, investigators explain that diagnosis of a bony stroke is based on a combination of imaging devices including CT, MRI, angiography, and sonography of brain-supplying vessels.
In addition to conventional static imaging, dynamic imaging modalities with the patients’ head in a fixed rotation or reclination has been shown to be useful as this enables the detection of a compressive effect on brain-supplying arteries caused by head movement.
They note that these bony strokes have been described previously – mainly as single case reports or small case series – but a systematic evaluation of each anatomical type of bony stroke is currently lacking.
For the current paper, the authors describe the identification and therapeutic workup of six patients with a bony stroke among 4,200 patients with ischemic stroke treated from January 2017 to March 2022 at their comprehensive stroke care center, constituting an incidence of 0.14%.
But they caution, “Given our retrospective study design, the method of patient acquisition, and the lack of systematic evaluation of bony strokes during acute stroke treatment, epidemiologic conclusions can be drawn only very carefully.”
In each of these six cases, the recurrent stroke was found to be caused by large-artery embolism from mechanical stress by bone or cartilage anomalies on arteries supplying the brain.
“Our case series aims to raise awareness for the rare entity of bony strokes, emphasizing the necessity to evaluate structural bone or cartilage lesions as a possible cause of ischemic stroke in patients with stroke recurrence of unknown cause in one vascular territory. We further aim on highlighting individual diagnostic and therapeutic options,” they state.
They note that it has previously been suggested that ischemic strokes based on bone or cartilage anomalies are more common in the relatively young patients with stroke, which is in line with their current patient data (mean age, 55 years), but this may reflect a selection bias.
A medical history with an association between changes in the head position and the occurrence of ischemic stroke may also raise awareness of the possibility of a bony stroke.
The authors outline treatment options for bony stroke, which they describe as diverse: They include conservative treatment, endovascular stenting, occlusion of the affected vessel, surgical bypass, and bone/cartilage removal.
From a pathophysiologic point of view, it seems reasonable to eliminate a causative lesion by surgical removal of the mechanical stressor, they note.
In cases of vascular stenting, they caution that the remainder of the mechanical stressor may provoke stent fracture and recurrent stroke, which occurred in two of their patients, a situation that may be observed more often in the future with the increasing use of vascular stenting.
The authors report that, compared with annual stroke rates in atrial fibrillation patients, stroke recurrence in this patient cohort ahead of definite treatment was high (cumulative 2.14 strokes per year). And as no patient had further ischemia after treatment, they argue that diagnosis and appropriate treatment of bony stroke may reduce or even eliminate the risk for future stroke recurrence.
They propose that for the diagnosis an exact medical history, with emphasis on a possible change of head position at the onset of stroke symptoms, is useful.
Furthermore, previously acquired diagnostic scans including CT or MRI may be evaluated for a symptomatic vessel-bone or cartilage contact. Then, the additional application of dynamic imaging modalities, including dynamic ultrasound of brain-supplying vessels and CT-angiography, may be discussed.
“An appropriate diagnosis and the evaluation of individual and interdisciplinary treatment options seem crucial to prevent recurrent ischemic strokes. Future prospective trials seem mandatory to optimize patient care,” they conclude.
The study had no specific funding. Coauthor Jan S. Kirschke, MD, received research support from the German Research Foundation, Bonescreen, H2020 European Research Council, and Philips. The other authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
These so-called “bony” strokes constitute a possible cause of recurrent ischemia in the same vascular territory as previous episodes, note the authors, led by Johanna Haertl, MD, Technical University of Munich.
“In patients with recurrent strokes in one vascular territory the presence of a symptomatic anatomic bone or cartilage anomaly may be considered as a differential diagnosis after sufficient exclusion of competing etiologies of an ischemic stroke,” they conclude.
“Due to the possibly high risk of stroke recurrence and potentially causative treatment options, bony strokes seem to be highly relevant for clinical practice,” they add.
The study was published online in the journal Stroke.
In their report, investigators explain that diagnosis of a bony stroke is based on a combination of imaging devices including CT, MRI, angiography, and sonography of brain-supplying vessels.
In addition to conventional static imaging, dynamic imaging modalities with the patients’ head in a fixed rotation or reclination has been shown to be useful as this enables the detection of a compressive effect on brain-supplying arteries caused by head movement.
They note that these bony strokes have been described previously – mainly as single case reports or small case series – but a systematic evaluation of each anatomical type of bony stroke is currently lacking.
For the current paper, the authors describe the identification and therapeutic workup of six patients with a bony stroke among 4,200 patients with ischemic stroke treated from January 2017 to March 2022 at their comprehensive stroke care center, constituting an incidence of 0.14%.
But they caution, “Given our retrospective study design, the method of patient acquisition, and the lack of systematic evaluation of bony strokes during acute stroke treatment, epidemiologic conclusions can be drawn only very carefully.”
In each of these six cases, the recurrent stroke was found to be caused by large-artery embolism from mechanical stress by bone or cartilage anomalies on arteries supplying the brain.
“Our case series aims to raise awareness for the rare entity of bony strokes, emphasizing the necessity to evaluate structural bone or cartilage lesions as a possible cause of ischemic stroke in patients with stroke recurrence of unknown cause in one vascular territory. We further aim on highlighting individual diagnostic and therapeutic options,” they state.
They note that it has previously been suggested that ischemic strokes based on bone or cartilage anomalies are more common in the relatively young patients with stroke, which is in line with their current patient data (mean age, 55 years), but this may reflect a selection bias.
A medical history with an association between changes in the head position and the occurrence of ischemic stroke may also raise awareness of the possibility of a bony stroke.
The authors outline treatment options for bony stroke, which they describe as diverse: They include conservative treatment, endovascular stenting, occlusion of the affected vessel, surgical bypass, and bone/cartilage removal.
From a pathophysiologic point of view, it seems reasonable to eliminate a causative lesion by surgical removal of the mechanical stressor, they note.
In cases of vascular stenting, they caution that the remainder of the mechanical stressor may provoke stent fracture and recurrent stroke, which occurred in two of their patients, a situation that may be observed more often in the future with the increasing use of vascular stenting.
The authors report that, compared with annual stroke rates in atrial fibrillation patients, stroke recurrence in this patient cohort ahead of definite treatment was high (cumulative 2.14 strokes per year). And as no patient had further ischemia after treatment, they argue that diagnosis and appropriate treatment of bony stroke may reduce or even eliminate the risk for future stroke recurrence.
They propose that for the diagnosis an exact medical history, with emphasis on a possible change of head position at the onset of stroke symptoms, is useful.
Furthermore, previously acquired diagnostic scans including CT or MRI may be evaluated for a symptomatic vessel-bone or cartilage contact. Then, the additional application of dynamic imaging modalities, including dynamic ultrasound of brain-supplying vessels and CT-angiography, may be discussed.
“An appropriate diagnosis and the evaluation of individual and interdisciplinary treatment options seem crucial to prevent recurrent ischemic strokes. Future prospective trials seem mandatory to optimize patient care,” they conclude.
The study had no specific funding. Coauthor Jan S. Kirschke, MD, received research support from the German Research Foundation, Bonescreen, H2020 European Research Council, and Philips. The other authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
These so-called “bony” strokes constitute a possible cause of recurrent ischemia in the same vascular territory as previous episodes, note the authors, led by Johanna Haertl, MD, Technical University of Munich.
“In patients with recurrent strokes in one vascular territory the presence of a symptomatic anatomic bone or cartilage anomaly may be considered as a differential diagnosis after sufficient exclusion of competing etiologies of an ischemic stroke,” they conclude.
“Due to the possibly high risk of stroke recurrence and potentially causative treatment options, bony strokes seem to be highly relevant for clinical practice,” they add.
The study was published online in the journal Stroke.
In their report, investigators explain that diagnosis of a bony stroke is based on a combination of imaging devices including CT, MRI, angiography, and sonography of brain-supplying vessels.
In addition to conventional static imaging, dynamic imaging modalities with the patients’ head in a fixed rotation or reclination has been shown to be useful as this enables the detection of a compressive effect on brain-supplying arteries caused by head movement.
They note that these bony strokes have been described previously – mainly as single case reports or small case series – but a systematic evaluation of each anatomical type of bony stroke is currently lacking.
For the current paper, the authors describe the identification and therapeutic workup of six patients with a bony stroke among 4,200 patients with ischemic stroke treated from January 2017 to March 2022 at their comprehensive stroke care center, constituting an incidence of 0.14%.
But they caution, “Given our retrospective study design, the method of patient acquisition, and the lack of systematic evaluation of bony strokes during acute stroke treatment, epidemiologic conclusions can be drawn only very carefully.”
In each of these six cases, the recurrent stroke was found to be caused by large-artery embolism from mechanical stress by bone or cartilage anomalies on arteries supplying the brain.
“Our case series aims to raise awareness for the rare entity of bony strokes, emphasizing the necessity to evaluate structural bone or cartilage lesions as a possible cause of ischemic stroke in patients with stroke recurrence of unknown cause in one vascular territory. We further aim on highlighting individual diagnostic and therapeutic options,” they state.
They note that it has previously been suggested that ischemic strokes based on bone or cartilage anomalies are more common in the relatively young patients with stroke, which is in line with their current patient data (mean age, 55 years), but this may reflect a selection bias.
A medical history with an association between changes in the head position and the occurrence of ischemic stroke may also raise awareness of the possibility of a bony stroke.
The authors outline treatment options for bony stroke, which they describe as diverse: They include conservative treatment, endovascular stenting, occlusion of the affected vessel, surgical bypass, and bone/cartilage removal.
From a pathophysiologic point of view, it seems reasonable to eliminate a causative lesion by surgical removal of the mechanical stressor, they note.
In cases of vascular stenting, they caution that the remainder of the mechanical stressor may provoke stent fracture and recurrent stroke, which occurred in two of their patients, a situation that may be observed more often in the future with the increasing use of vascular stenting.
The authors report that, compared with annual stroke rates in atrial fibrillation patients, stroke recurrence in this patient cohort ahead of definite treatment was high (cumulative 2.14 strokes per year). And as no patient had further ischemia after treatment, they argue that diagnosis and appropriate treatment of bony stroke may reduce or even eliminate the risk for future stroke recurrence.
They propose that for the diagnosis an exact medical history, with emphasis on a possible change of head position at the onset of stroke symptoms, is useful.
Furthermore, previously acquired diagnostic scans including CT or MRI may be evaluated for a symptomatic vessel-bone or cartilage contact. Then, the additional application of dynamic imaging modalities, including dynamic ultrasound of brain-supplying vessels and CT-angiography, may be discussed.
“An appropriate diagnosis and the evaluation of individual and interdisciplinary treatment options seem crucial to prevent recurrent ischemic strokes. Future prospective trials seem mandatory to optimize patient care,” they conclude.
The study had no specific funding. Coauthor Jan S. Kirschke, MD, received research support from the German Research Foundation, Bonescreen, H2020 European Research Council, and Philips. The other authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM STROKE
‘Substantial’ variation in responses to BP meds
A new study has shown a substantial variation in the blood pressure response to various antihypertensive medications between individuals, raising the possibility of future personalized therapy.
“We found that using the optimal antihypertensive drug for a particular patient resulted in an average of a 4.4 mm Hg greater reduction of blood pressure compared with a random choice of the other drugs. That is quite a substantial difference, and could be equivalent to adding in another drug,” lead author Johan Sundström, MD, Uppsala (Sweden) University Hospital, told this news organization.
“These preliminary findings suggest that some people may be better treated with one antihypertensive drug rather than another. This is opening up the field of hypertension for personalized medicine,” he added.
The study was published online in the Journal of the American Medical Association.
The authors noted that despite global access to multiple classes of highly effective blood pressure-lowering drugs, only one in four women and one in five men with hypertension reach treatment targets. While most hypertension guidelines advocate combination pharmacotherapy, many patients in routine care continue to be treated with monotherapy, with adverse effects and nonadherence being important clinical problems.
“One drug often does not give enough blood pressure reduction, but patients are often reluctant to up-titrate to two drugs,” Dr. Sundström said. “While we know that the four recommended classes of antihypertensives lower blood pressure equally well on average, we don’t know if their efficacy is the same in individual patients.
“We wondered whether there could be different optimal drugs for different people, and if we could identify the optimal drug for each person then maybe more patients could get to target levels with just one drug,” he said.
The researchers conducted a randomized, double-blind, repeated crossover trial at an outpatient research clinic in Sweden, studying 280 men and women with grade 1 hypertension at low risk for cardiovascular events.
Each participant was scheduled for 2 months’ treatment in random order with each of four different classes of antihypertensive drugs: an ACE inhibitor, lisinopril; an angiotensin II blocker, candesartan; a thiazide diuretic, hydrochlorothiazide; a calcium channel blocker, amlodipine.
There were then repeated treatment periods for two drug classes to try to account for any effect of a particular event that might have affected the blood pressure at one point in time. Ambulatory daytime systolic blood pressure was measured at the end of each treatment period.
Results showed that variation in systolic blood pressure was large between treatments on average, between participants on average, within participants taking the same treatment, and between treatments in the same participant.
Overall, personalized treatment using the optimal single-drug therapy led to a 4.4–mm Hg lower systolic blood pressure in the trial population than a random choice of any of the other drug classes.
Taking into consideration that lisinopril was found to be on average the most efficacious of the drugs at the selected doses, personalized treatment compared with lisinopril still led to a 3.1–mm Hg improvement in systolic blood pressure.
The researchers noted that the mean additional blood pressure reduction achievable by using the optimal agent was of a magnitude twice that achieved by doubling the dose of a first drug, and more than half that of adding a second drug on average.
While there were only small differences between certain drugs (e.g., candesartan vs. lisinopril; amlodipine vs. hydrochlorothiazide), for all other comparisons tested, the choice was important, with particularly large gains to be made by personalizing the choice between candesartan vs. amlodipine and between lisinopril vs. amlodipine.
In addition, some people showed very large differences in response to different drugs, whereas others did not have much difference at all.
How to identify the optimal drug?
“The million-dollar question is how we identify the best drug for each individual patient,” Dr. Sundström said. “This study has opened Pandora’s box. We now need to figure out how to go forward and how we tailor treatment in each patient.”
In the study, the researchers suggest that personalizing therapy could be achieved either by identifying the phenotypic characteristics that are associated with enhanced response to one treatment vs. another or by directly measuring the individual’s responses to a series of treatments to ascertain which is most effective.
Addressing the first scenario, Dr. Sundström explained: “We can analyze the characteristics of patients who did best on each drug. There are many variables we can look at here such as age, diet, baseline blood pressure, exercise levels, smoking status, race, body weight, salt intake, and findings from genetic tests. We are going to try to look into these to see if we can find any predictors of response to various different drugs.”
For the second strategy, he suggested that patients starting pharmacologic therapy could try a few different treatments. “For example, we could give patients two different drugs and ask them to alternate treatment periods with each of them and measure their blood pressure with a home monitoring kit and record adverse effects.”
Nonadherence “is such a big problem with antihypertensives,” he added. “This approach may allow patients to be more empowered when choosing the right treatment, which should help adherence in the longer term.”
‘Proof-of-principle’
Commenting on the study in an accompanying editorial, Robert M. Carey, MD, University of Virginia Health System, Charlottesville, wrote: “At this stage, the findings are more theoretical than immediately practical for the implementation of personalized antihypertensive drug therapy, but the study does provide proof-of-principle and the authors suggest a few scenarios in which a personalized approach could be used in the future.”
He said the practical ramifications of personally targeted therapy remain unclear, given that determination of an individual’s response to a series of short test treatments before selecting long-term therapy may be considered too cumbersome, and currently few phenotypic markers are currently available that would be likely to accurately predict the individual response to a particular therapy.
Dr. Carey concluded that the results of this study “encourage the further pursuit of larger randomized trials using similar repeated crossover designs to validate this concept and eventually in trials with longer follow-up data to determine whether there is improvement in long-term clinical outcomes compared with current strategies.”
He added that the results support the possibility that personalized medical treatment of hypertension “may ultimately supplement or even supplant the current method of antihypertensive drug decision-making in the future.”
This study was supported by the Swedish Research Council; Kjell and Märta Beijer Foundation; and Anders Wiklöf. Dr. Sundström reported owning stock in Symptoms Europe AB and Anagram Kommunikation AB. Coauthor Emil Hagström, MD, PhD, reported receiving grants from Pfizer and Amgen and personal fees from Amgen, Novo Nordisk, Bayer, AstraZeneca, Amarin, and Novartis. Coauthor Ollie Östlund, PhD, reported fees from Uppsala University paid to his institution, Uppsala Clinical Research Center, for its participation in the PHYSIC trial during the conduct of the study. Dr. Carey reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study has shown a substantial variation in the blood pressure response to various antihypertensive medications between individuals, raising the possibility of future personalized therapy.
“We found that using the optimal antihypertensive drug for a particular patient resulted in an average of a 4.4 mm Hg greater reduction of blood pressure compared with a random choice of the other drugs. That is quite a substantial difference, and could be equivalent to adding in another drug,” lead author Johan Sundström, MD, Uppsala (Sweden) University Hospital, told this news organization.
“These preliminary findings suggest that some people may be better treated with one antihypertensive drug rather than another. This is opening up the field of hypertension for personalized medicine,” he added.
The study was published online in the Journal of the American Medical Association.
The authors noted that despite global access to multiple classes of highly effective blood pressure-lowering drugs, only one in four women and one in five men with hypertension reach treatment targets. While most hypertension guidelines advocate combination pharmacotherapy, many patients in routine care continue to be treated with monotherapy, with adverse effects and nonadherence being important clinical problems.
“One drug often does not give enough blood pressure reduction, but patients are often reluctant to up-titrate to two drugs,” Dr. Sundström said. “While we know that the four recommended classes of antihypertensives lower blood pressure equally well on average, we don’t know if their efficacy is the same in individual patients.
“We wondered whether there could be different optimal drugs for different people, and if we could identify the optimal drug for each person then maybe more patients could get to target levels with just one drug,” he said.
The researchers conducted a randomized, double-blind, repeated crossover trial at an outpatient research clinic in Sweden, studying 280 men and women with grade 1 hypertension at low risk for cardiovascular events.
Each participant was scheduled for 2 months’ treatment in random order with each of four different classes of antihypertensive drugs: an ACE inhibitor, lisinopril; an angiotensin II blocker, candesartan; a thiazide diuretic, hydrochlorothiazide; a calcium channel blocker, amlodipine.
There were then repeated treatment periods for two drug classes to try to account for any effect of a particular event that might have affected the blood pressure at one point in time. Ambulatory daytime systolic blood pressure was measured at the end of each treatment period.
Results showed that variation in systolic blood pressure was large between treatments on average, between participants on average, within participants taking the same treatment, and between treatments in the same participant.
Overall, personalized treatment using the optimal single-drug therapy led to a 4.4–mm Hg lower systolic blood pressure in the trial population than a random choice of any of the other drug classes.
Taking into consideration that lisinopril was found to be on average the most efficacious of the drugs at the selected doses, personalized treatment compared with lisinopril still led to a 3.1–mm Hg improvement in systolic blood pressure.
The researchers noted that the mean additional blood pressure reduction achievable by using the optimal agent was of a magnitude twice that achieved by doubling the dose of a first drug, and more than half that of adding a second drug on average.
While there were only small differences between certain drugs (e.g., candesartan vs. lisinopril; amlodipine vs. hydrochlorothiazide), for all other comparisons tested, the choice was important, with particularly large gains to be made by personalizing the choice between candesartan vs. amlodipine and between lisinopril vs. amlodipine.
In addition, some people showed very large differences in response to different drugs, whereas others did not have much difference at all.
How to identify the optimal drug?
“The million-dollar question is how we identify the best drug for each individual patient,” Dr. Sundström said. “This study has opened Pandora’s box. We now need to figure out how to go forward and how we tailor treatment in each patient.”
In the study, the researchers suggest that personalizing therapy could be achieved either by identifying the phenotypic characteristics that are associated with enhanced response to one treatment vs. another or by directly measuring the individual’s responses to a series of treatments to ascertain which is most effective.
Addressing the first scenario, Dr. Sundström explained: “We can analyze the characteristics of patients who did best on each drug. There are many variables we can look at here such as age, diet, baseline blood pressure, exercise levels, smoking status, race, body weight, salt intake, and findings from genetic tests. We are going to try to look into these to see if we can find any predictors of response to various different drugs.”
For the second strategy, he suggested that patients starting pharmacologic therapy could try a few different treatments. “For example, we could give patients two different drugs and ask them to alternate treatment periods with each of them and measure their blood pressure with a home monitoring kit and record adverse effects.”
Nonadherence “is such a big problem with antihypertensives,” he added. “This approach may allow patients to be more empowered when choosing the right treatment, which should help adherence in the longer term.”
‘Proof-of-principle’
Commenting on the study in an accompanying editorial, Robert M. Carey, MD, University of Virginia Health System, Charlottesville, wrote: “At this stage, the findings are more theoretical than immediately practical for the implementation of personalized antihypertensive drug therapy, but the study does provide proof-of-principle and the authors suggest a few scenarios in which a personalized approach could be used in the future.”
He said the practical ramifications of personally targeted therapy remain unclear, given that determination of an individual’s response to a series of short test treatments before selecting long-term therapy may be considered too cumbersome, and currently few phenotypic markers are currently available that would be likely to accurately predict the individual response to a particular therapy.
Dr. Carey concluded that the results of this study “encourage the further pursuit of larger randomized trials using similar repeated crossover designs to validate this concept and eventually in trials with longer follow-up data to determine whether there is improvement in long-term clinical outcomes compared with current strategies.”
He added that the results support the possibility that personalized medical treatment of hypertension “may ultimately supplement or even supplant the current method of antihypertensive drug decision-making in the future.”
This study was supported by the Swedish Research Council; Kjell and Märta Beijer Foundation; and Anders Wiklöf. Dr. Sundström reported owning stock in Symptoms Europe AB and Anagram Kommunikation AB. Coauthor Emil Hagström, MD, PhD, reported receiving grants from Pfizer and Amgen and personal fees from Amgen, Novo Nordisk, Bayer, AstraZeneca, Amarin, and Novartis. Coauthor Ollie Östlund, PhD, reported fees from Uppsala University paid to his institution, Uppsala Clinical Research Center, for its participation in the PHYSIC trial during the conduct of the study. Dr. Carey reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study has shown a substantial variation in the blood pressure response to various antihypertensive medications between individuals, raising the possibility of future personalized therapy.
“We found that using the optimal antihypertensive drug for a particular patient resulted in an average of a 4.4 mm Hg greater reduction of blood pressure compared with a random choice of the other drugs. That is quite a substantial difference, and could be equivalent to adding in another drug,” lead author Johan Sundström, MD, Uppsala (Sweden) University Hospital, told this news organization.
“These preliminary findings suggest that some people may be better treated with one antihypertensive drug rather than another. This is opening up the field of hypertension for personalized medicine,” he added.
The study was published online in the Journal of the American Medical Association.
The authors noted that despite global access to multiple classes of highly effective blood pressure-lowering drugs, only one in four women and one in five men with hypertension reach treatment targets. While most hypertension guidelines advocate combination pharmacotherapy, many patients in routine care continue to be treated with monotherapy, with adverse effects and nonadherence being important clinical problems.
“One drug often does not give enough blood pressure reduction, but patients are often reluctant to up-titrate to two drugs,” Dr. Sundström said. “While we know that the four recommended classes of antihypertensives lower blood pressure equally well on average, we don’t know if their efficacy is the same in individual patients.
“We wondered whether there could be different optimal drugs for different people, and if we could identify the optimal drug for each person then maybe more patients could get to target levels with just one drug,” he said.
The researchers conducted a randomized, double-blind, repeated crossover trial at an outpatient research clinic in Sweden, studying 280 men and women with grade 1 hypertension at low risk for cardiovascular events.
Each participant was scheduled for 2 months’ treatment in random order with each of four different classes of antihypertensive drugs: an ACE inhibitor, lisinopril; an angiotensin II blocker, candesartan; a thiazide diuretic, hydrochlorothiazide; a calcium channel blocker, amlodipine.
There were then repeated treatment periods for two drug classes to try to account for any effect of a particular event that might have affected the blood pressure at one point in time. Ambulatory daytime systolic blood pressure was measured at the end of each treatment period.
Results showed that variation in systolic blood pressure was large between treatments on average, between participants on average, within participants taking the same treatment, and between treatments in the same participant.
Overall, personalized treatment using the optimal single-drug therapy led to a 4.4–mm Hg lower systolic blood pressure in the trial population than a random choice of any of the other drug classes.
Taking into consideration that lisinopril was found to be on average the most efficacious of the drugs at the selected doses, personalized treatment compared with lisinopril still led to a 3.1–mm Hg improvement in systolic blood pressure.
The researchers noted that the mean additional blood pressure reduction achievable by using the optimal agent was of a magnitude twice that achieved by doubling the dose of a first drug, and more than half that of adding a second drug on average.
While there were only small differences between certain drugs (e.g., candesartan vs. lisinopril; amlodipine vs. hydrochlorothiazide), for all other comparisons tested, the choice was important, with particularly large gains to be made by personalizing the choice between candesartan vs. amlodipine and between lisinopril vs. amlodipine.
In addition, some people showed very large differences in response to different drugs, whereas others did not have much difference at all.
How to identify the optimal drug?
“The million-dollar question is how we identify the best drug for each individual patient,” Dr. Sundström said. “This study has opened Pandora’s box. We now need to figure out how to go forward and how we tailor treatment in each patient.”
In the study, the researchers suggest that personalizing therapy could be achieved either by identifying the phenotypic characteristics that are associated with enhanced response to one treatment vs. another or by directly measuring the individual’s responses to a series of treatments to ascertain which is most effective.
Addressing the first scenario, Dr. Sundström explained: “We can analyze the characteristics of patients who did best on each drug. There are many variables we can look at here such as age, diet, baseline blood pressure, exercise levels, smoking status, race, body weight, salt intake, and findings from genetic tests. We are going to try to look into these to see if we can find any predictors of response to various different drugs.”
For the second strategy, he suggested that patients starting pharmacologic therapy could try a few different treatments. “For example, we could give patients two different drugs and ask them to alternate treatment periods with each of them and measure their blood pressure with a home monitoring kit and record adverse effects.”
Nonadherence “is such a big problem with antihypertensives,” he added. “This approach may allow patients to be more empowered when choosing the right treatment, which should help adherence in the longer term.”
‘Proof-of-principle’
Commenting on the study in an accompanying editorial, Robert M. Carey, MD, University of Virginia Health System, Charlottesville, wrote: “At this stage, the findings are more theoretical than immediately practical for the implementation of personalized antihypertensive drug therapy, but the study does provide proof-of-principle and the authors suggest a few scenarios in which a personalized approach could be used in the future.”
He said the practical ramifications of personally targeted therapy remain unclear, given that determination of an individual’s response to a series of short test treatments before selecting long-term therapy may be considered too cumbersome, and currently few phenotypic markers are currently available that would be likely to accurately predict the individual response to a particular therapy.
Dr. Carey concluded that the results of this study “encourage the further pursuit of larger randomized trials using similar repeated crossover designs to validate this concept and eventually in trials with longer follow-up data to determine whether there is improvement in long-term clinical outcomes compared with current strategies.”
He added that the results support the possibility that personalized medical treatment of hypertension “may ultimately supplement or even supplant the current method of antihypertensive drug decision-making in the future.”
This study was supported by the Swedish Research Council; Kjell and Märta Beijer Foundation; and Anders Wiklöf. Dr. Sundström reported owning stock in Symptoms Europe AB and Anagram Kommunikation AB. Coauthor Emil Hagström, MD, PhD, reported receiving grants from Pfizer and Amgen and personal fees from Amgen, Novo Nordisk, Bayer, AstraZeneca, Amarin, and Novartis. Coauthor Ollie Östlund, PhD, reported fees from Uppsala University paid to his institution, Uppsala Clinical Research Center, for its participation in the PHYSIC trial during the conduct of the study. Dr. Carey reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Antiphospholipid antibodies linked to future CV events
The presence of antiphospholipid antibodies is associated with an increased risk for future cardiovascular events, according to a new study.
The findings point to possible new approaches to risk stratification and the potential for new therapeutic targets in heart disease.
“In this study of the general population, we found that two antiphospholipid antibodies were associated with an increased risk of having a serious cardiovascular event over a follow-up of 8 years,” coauthor Jason Knight, MD, University of Michigan, Ann Arbor, said in an interview.
“If confirmed in further studies, these findings could be used to identify a subgroup of patients who need more careful monitoring and more aggressive risk-factor modification, and if the increased risk linked to these antibodies is high enough, it may also justify preemptive treatments such as the anticoagulants that are routinely used in antiphospholipid syndrome,” Dr. Knight said.
“The long-term vision is that we may identify some people in the general population who would benefit from treating the immune system for the prevention and treatment of cardiovascular disease instead of, or in addition to, using typical cardiovascular medications,” he added.
The study was published online in JAMA Network Open.
Individuals with autoimmune and inflammatory diseases have a greater risk for cardiovascular events than expected based on traditional cardiovascular risk factors, with mechanisms proposed to explain this risk including inflammation-mediated disruption of vascular integrity and activation of platelets and coagulation pathways, the authors explained. However, the role of autoantibodies remains unclear.
They noted that antiphospholipid antibodies can activate endothelial cells, platelets, and neutrophils, and some patients with persistently circulating antiphospholipid antibodies can develop antiphospholipid syndrome – an acquired thromboinflammatory disease characterized by arterial, venous, and microvascular thrombotic events and obstetric complications.
Cross-sectional studies have shown that antiphospholipid antibodies are acutely present in up to 17.4% of patients with stroke or transient ischemic attack, and small cohort studies have suggested that such antibodies may be present in 1%-12% of seemingly healthy individuals. However, the impact of sex, race, and ethnicity on the prevalence of antiphospholipid antibodies and their association with atherosclerotic cardiovascular disease is not known.
The researchers conducted the current study to look at the association between antiphospholipid antibodies and future risk for atherosclerotic cardiovascular events.
They analyzed data from 2,427 participants in the population-based Dallas Heart Study who had no history of atherosclerotic cardiovascular disease or autoimmune diseases requiring immunosuppressive medications at the time of blood sampling at study entry in 2007-2009.
Eight different types of antiphospholipid antibodies were measured, and data on cardiovascular events over the next 8 years was recorded.
Results showed that 14.5% of the cohort tested positive for one of these antiphospholipid antibodies at the start of the study, with approximately one-third of those detected at a moderate or high titer.
The researchers also found that the IgA isotypes of two antiphospholipid antibodies – anticardiolipin and anti-beta-2 glycoprotein – were associated with future atherosclerotic cardiovascular events.
After adjustment for other known risk factors, individuals testing positive for the IgA isotype of anticardiolipin had an almost five times increased risk (hazard ratio, 4.92) of the primary endpoint (myocardial infarction, stroke, coronary revascularization, or cardiovascular death); while those testing positive for anti–beta2-glycoprotein had an almost three times increased risk (HR, 2.91).
Furthermore, there was what appeared to be a dose effect. People with the highest levels of these antibodies also had the highest risk for cardiovascular events, with up to an almost 10-fold increased risk with the higher level of anticardiolipin.
Dr. Knight said that more research into the IgA isotypes of these antiphospholipid antibodies is needed.
“Most of the mechanistic work in the antiphospholipid syndrome field has focused on IgG antiphospholipid antibodies. While we commonly find these IgA antibodies in patients with APS, the extent to which they contribute to disease has not been firmly established,” he said. “The fact that IgA was the primary hit in our unbiased screen suggests that there is more to the story and we need to better understand the implications of having these antibodies in circulation, and what specific problems they may be causing.”
Noting that antiphospholipid antibodies can form transiently after certain situations, such as infections, Dr. Knight said that further studies were needed with repeat blood testing to detect the chronic presence of the antibodies.
He added that information of venous thromboses was not available in this study and “perhaps some of the other antibodies might have stood out if we were able to analyze for different outcomes.”
This study was supported by a Pfizer Aspire Award. Dr. Knight reported receiving research funding and consulting fees from Jazz Pharmaceuticals outside the submitted work.
A version of this article first appeared on Medscape.com.
The presence of antiphospholipid antibodies is associated with an increased risk for future cardiovascular events, according to a new study.
The findings point to possible new approaches to risk stratification and the potential for new therapeutic targets in heart disease.
“In this study of the general population, we found that two antiphospholipid antibodies were associated with an increased risk of having a serious cardiovascular event over a follow-up of 8 years,” coauthor Jason Knight, MD, University of Michigan, Ann Arbor, said in an interview.
“If confirmed in further studies, these findings could be used to identify a subgroup of patients who need more careful monitoring and more aggressive risk-factor modification, and if the increased risk linked to these antibodies is high enough, it may also justify preemptive treatments such as the anticoagulants that are routinely used in antiphospholipid syndrome,” Dr. Knight said.
“The long-term vision is that we may identify some people in the general population who would benefit from treating the immune system for the prevention and treatment of cardiovascular disease instead of, or in addition to, using typical cardiovascular medications,” he added.
The study was published online in JAMA Network Open.
Individuals with autoimmune and inflammatory diseases have a greater risk for cardiovascular events than expected based on traditional cardiovascular risk factors, with mechanisms proposed to explain this risk including inflammation-mediated disruption of vascular integrity and activation of platelets and coagulation pathways, the authors explained. However, the role of autoantibodies remains unclear.
They noted that antiphospholipid antibodies can activate endothelial cells, platelets, and neutrophils, and some patients with persistently circulating antiphospholipid antibodies can develop antiphospholipid syndrome – an acquired thromboinflammatory disease characterized by arterial, venous, and microvascular thrombotic events and obstetric complications.
Cross-sectional studies have shown that antiphospholipid antibodies are acutely present in up to 17.4% of patients with stroke or transient ischemic attack, and small cohort studies have suggested that such antibodies may be present in 1%-12% of seemingly healthy individuals. However, the impact of sex, race, and ethnicity on the prevalence of antiphospholipid antibodies and their association with atherosclerotic cardiovascular disease is not known.
The researchers conducted the current study to look at the association between antiphospholipid antibodies and future risk for atherosclerotic cardiovascular events.
They analyzed data from 2,427 participants in the population-based Dallas Heart Study who had no history of atherosclerotic cardiovascular disease or autoimmune diseases requiring immunosuppressive medications at the time of blood sampling at study entry in 2007-2009.
Eight different types of antiphospholipid antibodies were measured, and data on cardiovascular events over the next 8 years was recorded.
Results showed that 14.5% of the cohort tested positive for one of these antiphospholipid antibodies at the start of the study, with approximately one-third of those detected at a moderate or high titer.
The researchers also found that the IgA isotypes of two antiphospholipid antibodies – anticardiolipin and anti-beta-2 glycoprotein – were associated with future atherosclerotic cardiovascular events.
After adjustment for other known risk factors, individuals testing positive for the IgA isotype of anticardiolipin had an almost five times increased risk (hazard ratio, 4.92) of the primary endpoint (myocardial infarction, stroke, coronary revascularization, or cardiovascular death); while those testing positive for anti–beta2-glycoprotein had an almost three times increased risk (HR, 2.91).
Furthermore, there was what appeared to be a dose effect. People with the highest levels of these antibodies also had the highest risk for cardiovascular events, with up to an almost 10-fold increased risk with the higher level of anticardiolipin.
Dr. Knight said that more research into the IgA isotypes of these antiphospholipid antibodies is needed.
“Most of the mechanistic work in the antiphospholipid syndrome field has focused on IgG antiphospholipid antibodies. While we commonly find these IgA antibodies in patients with APS, the extent to which they contribute to disease has not been firmly established,” he said. “The fact that IgA was the primary hit in our unbiased screen suggests that there is more to the story and we need to better understand the implications of having these antibodies in circulation, and what specific problems they may be causing.”
Noting that antiphospholipid antibodies can form transiently after certain situations, such as infections, Dr. Knight said that further studies were needed with repeat blood testing to detect the chronic presence of the antibodies.
He added that information of venous thromboses was not available in this study and “perhaps some of the other antibodies might have stood out if we were able to analyze for different outcomes.”
This study was supported by a Pfizer Aspire Award. Dr. Knight reported receiving research funding and consulting fees from Jazz Pharmaceuticals outside the submitted work.
A version of this article first appeared on Medscape.com.
The presence of antiphospholipid antibodies is associated with an increased risk for future cardiovascular events, according to a new study.
The findings point to possible new approaches to risk stratification and the potential for new therapeutic targets in heart disease.
“In this study of the general population, we found that two antiphospholipid antibodies were associated with an increased risk of having a serious cardiovascular event over a follow-up of 8 years,” coauthor Jason Knight, MD, University of Michigan, Ann Arbor, said in an interview.
“If confirmed in further studies, these findings could be used to identify a subgroup of patients who need more careful monitoring and more aggressive risk-factor modification, and if the increased risk linked to these antibodies is high enough, it may also justify preemptive treatments such as the anticoagulants that are routinely used in antiphospholipid syndrome,” Dr. Knight said.
“The long-term vision is that we may identify some people in the general population who would benefit from treating the immune system for the prevention and treatment of cardiovascular disease instead of, or in addition to, using typical cardiovascular medications,” he added.
The study was published online in JAMA Network Open.
Individuals with autoimmune and inflammatory diseases have a greater risk for cardiovascular events than expected based on traditional cardiovascular risk factors, with mechanisms proposed to explain this risk including inflammation-mediated disruption of vascular integrity and activation of platelets and coagulation pathways, the authors explained. However, the role of autoantibodies remains unclear.
They noted that antiphospholipid antibodies can activate endothelial cells, platelets, and neutrophils, and some patients with persistently circulating antiphospholipid antibodies can develop antiphospholipid syndrome – an acquired thromboinflammatory disease characterized by arterial, venous, and microvascular thrombotic events and obstetric complications.
Cross-sectional studies have shown that antiphospholipid antibodies are acutely present in up to 17.4% of patients with stroke or transient ischemic attack, and small cohort studies have suggested that such antibodies may be present in 1%-12% of seemingly healthy individuals. However, the impact of sex, race, and ethnicity on the prevalence of antiphospholipid antibodies and their association with atherosclerotic cardiovascular disease is not known.
The researchers conducted the current study to look at the association between antiphospholipid antibodies and future risk for atherosclerotic cardiovascular events.
They analyzed data from 2,427 participants in the population-based Dallas Heart Study who had no history of atherosclerotic cardiovascular disease or autoimmune diseases requiring immunosuppressive medications at the time of blood sampling at study entry in 2007-2009.
Eight different types of antiphospholipid antibodies were measured, and data on cardiovascular events over the next 8 years was recorded.
Results showed that 14.5% of the cohort tested positive for one of these antiphospholipid antibodies at the start of the study, with approximately one-third of those detected at a moderate or high titer.
The researchers also found that the IgA isotypes of two antiphospholipid antibodies – anticardiolipin and anti-beta-2 glycoprotein – were associated with future atherosclerotic cardiovascular events.
After adjustment for other known risk factors, individuals testing positive for the IgA isotype of anticardiolipin had an almost five times increased risk (hazard ratio, 4.92) of the primary endpoint (myocardial infarction, stroke, coronary revascularization, or cardiovascular death); while those testing positive for anti–beta2-glycoprotein had an almost three times increased risk (HR, 2.91).
Furthermore, there was what appeared to be a dose effect. People with the highest levels of these antibodies also had the highest risk for cardiovascular events, with up to an almost 10-fold increased risk with the higher level of anticardiolipin.
Dr. Knight said that more research into the IgA isotypes of these antiphospholipid antibodies is needed.
“Most of the mechanistic work in the antiphospholipid syndrome field has focused on IgG antiphospholipid antibodies. While we commonly find these IgA antibodies in patients with APS, the extent to which they contribute to disease has not been firmly established,” he said. “The fact that IgA was the primary hit in our unbiased screen suggests that there is more to the story and we need to better understand the implications of having these antibodies in circulation, and what specific problems they may be causing.”
Noting that antiphospholipid antibodies can form transiently after certain situations, such as infections, Dr. Knight said that further studies were needed with repeat blood testing to detect the chronic presence of the antibodies.
He added that information of venous thromboses was not available in this study and “perhaps some of the other antibodies might have stood out if we were able to analyze for different outcomes.”
This study was supported by a Pfizer Aspire Award. Dr. Knight reported receiving research funding and consulting fees from Jazz Pharmaceuticals outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN