User login
MRI Improved Breast Cancer Detection in Average-Risk Women
SAN FRANCISCO – MRI-screening may improve the detection of biologically relevant breast cancer in women who are at average-risk, and reduce the interval-cancer rate down to 0%, at a low false-positive rate, say the authors of a new study presented at the 2015 Breast Cancer Symposium.
In this cohort of heavily pre-screened women at average risk, the additional cancer yield achieved through MRI was high, at 15.8 cases per 1,000 women screened, and the added cancers diagnosed by MRI tended to be of high nuclear grade.
“MRI improves the detection of small high grade cancers in women at average risk, to the extent that the interval cancer rate was zero,” said Dr. Christiane Kuhl, of the University of Aachen, Germany.
“Between 30% and 50% of cancers identified in women who undergo screening mammography are not detected by mammography,” she said during her presentation.
Breast cancer continues to be the main or second most important cause of cancer death in women, and is the main cause of life years lost in women. “Which tells you that the main problem with mammography screening is not overdiagnosis,” she said. “The main problem is actually underdiagnois of disease.”
Breast MRI is currently recommended for screening women who are at a high-risk of breast-cancer, but despite decades of mammographic screening, breast cancer continues to cause high mortality for women who are deemed to be at an average risk of the disease. These data suggest that there is a need for improved methods of early diagnosis in this population.
Dr. Kuhl and her colleagues investigated the utility of supplemental MRI-screening of women who carry an average-risk of breast-cancer, and they conducted a prospective observational cohort-study that assessed the use of MRI screening in this population. The participants were in the usual age range for screening-mammography (40-70 years).
The women underwent dynamic contrast-enhanced MRI of the breast in addition to mammography every 12, 24, or 36 months, plus follow-up of 2 years to establish a standard-of-reference. The cohort included 2,120 women who underwent a total 3,861 MRI screenings.
Breast-cancer was diagnosed in 61 women (DCIS: 20, invasive: 41), and the rate of interval cancers was 0%, irrespective of screening interval. Of these women, 48 were diagnosed at prevalence-screening by MRI alone (supplemental cancer detection rate: 22.6 cases per 1,000 women screened. In addition, 13 women were diagnosed with breast-cancer in 1,741 incidence-screening-rounds collected over 4,887 women-years. A total 12 of these 13 incident cancers were diagnosed by screening-MRI alone (supplemental cancer detection rate was 6.9 per 1,000), one by MRI and mammography, and none were by mammography alone.
The authors also found that the supplemental cancer detection rate was independent of mammographic breast density. Invasive cancers were small, with a mean size of 8mm. They were node-negative in 93.4%, ER/PR-negative in 32.8%, and de-differentiated in 41.7% at prevalence, and 46% at incidence-screening. The specificity of MRI-screening was 97.1%, while false positive rate was 2.9%.
In a discussion of the paper, Dr. A. Marilyn Leitch, of the University of Texas Southwestern Medical Center, Dallas, pointed out that this was a selected population with negative mammograms. But is it possible to “apply MRI at longer intervals, say every 3 years, without initial mammography as a screening tool, in average risk women?” she asked
One of her concerns, however, is that “we hear all the time about the high false positive rates with MRI,” and they are generally higher than was reported in this study. “MRI also detects lesions that might drive patients to avoid breast conserving surgery, and there can be unreasonable costs for screening and work up of false positives.”
Screening guidelines from the USPSTF say that evidence for replacing mammography with MRI is lacking and the balance of benefit versus harms cannot be determined. “Even more ‘liberal’ guidelines from the American Cancer Society reserve MRI for high risk patients.”
What is needed is a clinical trial, she summarized, that will compare screening MRI at 3 year intervals to tomosynthesis mammogram annually in average risk women.
SAN FRANCISCO – MRI-screening may improve the detection of biologically relevant breast cancer in women who are at average-risk, and reduce the interval-cancer rate down to 0%, at a low false-positive rate, say the authors of a new study presented at the 2015 Breast Cancer Symposium.
In this cohort of heavily pre-screened women at average risk, the additional cancer yield achieved through MRI was high, at 15.8 cases per 1,000 women screened, and the added cancers diagnosed by MRI tended to be of high nuclear grade.
“MRI improves the detection of small high grade cancers in women at average risk, to the extent that the interval cancer rate was zero,” said Dr. Christiane Kuhl, of the University of Aachen, Germany.
“Between 30% and 50% of cancers identified in women who undergo screening mammography are not detected by mammography,” she said during her presentation.
Breast cancer continues to be the main or second most important cause of cancer death in women, and is the main cause of life years lost in women. “Which tells you that the main problem with mammography screening is not overdiagnosis,” she said. “The main problem is actually underdiagnois of disease.”
Breast MRI is currently recommended for screening women who are at a high-risk of breast-cancer, but despite decades of mammographic screening, breast cancer continues to cause high mortality for women who are deemed to be at an average risk of the disease. These data suggest that there is a need for improved methods of early diagnosis in this population.
Dr. Kuhl and her colleagues investigated the utility of supplemental MRI-screening of women who carry an average-risk of breast-cancer, and they conducted a prospective observational cohort-study that assessed the use of MRI screening in this population. The participants were in the usual age range for screening-mammography (40-70 years).
The women underwent dynamic contrast-enhanced MRI of the breast in addition to mammography every 12, 24, or 36 months, plus follow-up of 2 years to establish a standard-of-reference. The cohort included 2,120 women who underwent a total 3,861 MRI screenings.
Breast-cancer was diagnosed in 61 women (DCIS: 20, invasive: 41), and the rate of interval cancers was 0%, irrespective of screening interval. Of these women, 48 were diagnosed at prevalence-screening by MRI alone (supplemental cancer detection rate: 22.6 cases per 1,000 women screened. In addition, 13 women were diagnosed with breast-cancer in 1,741 incidence-screening-rounds collected over 4,887 women-years. A total 12 of these 13 incident cancers were diagnosed by screening-MRI alone (supplemental cancer detection rate was 6.9 per 1,000), one by MRI and mammography, and none were by mammography alone.
The authors also found that the supplemental cancer detection rate was independent of mammographic breast density. Invasive cancers were small, with a mean size of 8mm. They were node-negative in 93.4%, ER/PR-negative in 32.8%, and de-differentiated in 41.7% at prevalence, and 46% at incidence-screening. The specificity of MRI-screening was 97.1%, while false positive rate was 2.9%.
In a discussion of the paper, Dr. A. Marilyn Leitch, of the University of Texas Southwestern Medical Center, Dallas, pointed out that this was a selected population with negative mammograms. But is it possible to “apply MRI at longer intervals, say every 3 years, without initial mammography as a screening tool, in average risk women?” she asked
One of her concerns, however, is that “we hear all the time about the high false positive rates with MRI,” and they are generally higher than was reported in this study. “MRI also detects lesions that might drive patients to avoid breast conserving surgery, and there can be unreasonable costs for screening and work up of false positives.”
Screening guidelines from the USPSTF say that evidence for replacing mammography with MRI is lacking and the balance of benefit versus harms cannot be determined. “Even more ‘liberal’ guidelines from the American Cancer Society reserve MRI for high risk patients.”
What is needed is a clinical trial, she summarized, that will compare screening MRI at 3 year intervals to tomosynthesis mammogram annually in average risk women.
SAN FRANCISCO – MRI-screening may improve the detection of biologically relevant breast cancer in women who are at average-risk, and reduce the interval-cancer rate down to 0%, at a low false-positive rate, say the authors of a new study presented at the 2015 Breast Cancer Symposium.
In this cohort of heavily pre-screened women at average risk, the additional cancer yield achieved through MRI was high, at 15.8 cases per 1,000 women screened, and the added cancers diagnosed by MRI tended to be of high nuclear grade.
“MRI improves the detection of small high grade cancers in women at average risk, to the extent that the interval cancer rate was zero,” said Dr. Christiane Kuhl, of the University of Aachen, Germany.
“Between 30% and 50% of cancers identified in women who undergo screening mammography are not detected by mammography,” she said during her presentation.
Breast cancer continues to be the main or second most important cause of cancer death in women, and is the main cause of life years lost in women. “Which tells you that the main problem with mammography screening is not overdiagnosis,” she said. “The main problem is actually underdiagnois of disease.”
Breast MRI is currently recommended for screening women who are at a high-risk of breast-cancer, but despite decades of mammographic screening, breast cancer continues to cause high mortality for women who are deemed to be at an average risk of the disease. These data suggest that there is a need for improved methods of early diagnosis in this population.
Dr. Kuhl and her colleagues investigated the utility of supplemental MRI-screening of women who carry an average-risk of breast-cancer, and they conducted a prospective observational cohort-study that assessed the use of MRI screening in this population. The participants were in the usual age range for screening-mammography (40-70 years).
The women underwent dynamic contrast-enhanced MRI of the breast in addition to mammography every 12, 24, or 36 months, plus follow-up of 2 years to establish a standard-of-reference. The cohort included 2,120 women who underwent a total 3,861 MRI screenings.
Breast-cancer was diagnosed in 61 women (DCIS: 20, invasive: 41), and the rate of interval cancers was 0%, irrespective of screening interval. Of these women, 48 were diagnosed at prevalence-screening by MRI alone (supplemental cancer detection rate: 22.6 cases per 1,000 women screened. In addition, 13 women were diagnosed with breast-cancer in 1,741 incidence-screening-rounds collected over 4,887 women-years. A total 12 of these 13 incident cancers were diagnosed by screening-MRI alone (supplemental cancer detection rate was 6.9 per 1,000), one by MRI and mammography, and none were by mammography alone.
The authors also found that the supplemental cancer detection rate was independent of mammographic breast density. Invasive cancers were small, with a mean size of 8mm. They were node-negative in 93.4%, ER/PR-negative in 32.8%, and de-differentiated in 41.7% at prevalence, and 46% at incidence-screening. The specificity of MRI-screening was 97.1%, while false positive rate was 2.9%.
In a discussion of the paper, Dr. A. Marilyn Leitch, of the University of Texas Southwestern Medical Center, Dallas, pointed out that this was a selected population with negative mammograms. But is it possible to “apply MRI at longer intervals, say every 3 years, without initial mammography as a screening tool, in average risk women?” she asked
One of her concerns, however, is that “we hear all the time about the high false positive rates with MRI,” and they are generally higher than was reported in this study. “MRI also detects lesions that might drive patients to avoid breast conserving surgery, and there can be unreasonable costs for screening and work up of false positives.”
Screening guidelines from the USPSTF say that evidence for replacing mammography with MRI is lacking and the balance of benefit versus harms cannot be determined. “Even more ‘liberal’ guidelines from the American Cancer Society reserve MRI for high risk patients.”
What is needed is a clinical trial, she summarized, that will compare screening MRI at 3 year intervals to tomosynthesis mammogram annually in average risk women.
2015 BREAST CANCER SYMPOSIUM
ASCO: MRI improved breast cancer detection in average risk women
SAN FRANCISCO – MRI-screening may improve the detection of biologically relevant breast cancer in women who are at average-risk, and reduce the interval-cancer rate down to 0%, at a low false-positive rate, say the authors of a new study presented at the 2015 Breast Cancer Symposium.
In this cohort of heavily pre-screened women at average risk, the additional cancer yield achieved through MRI was high, at 15.8 cases per 1,000 women screened, and the added cancers diagnosed by MRI tended to be of high nuclear grade.
“MRI improves the detection of small high grade cancers in women at average risk, to the extent that the interval cancer rate was zero,” said Dr. Christiane Kuhl, of the University of Aachen, Germany.
“Between 30% and 50% of cancers identified in women who undergo screening mammography are not detected by mammography,” she said during her presentation.
Breast cancer continues to be the main or second most important cause of cancer death in women, and is the main cause of life years lost in women. “Which tells you that the main problem with mammography screening is not overdiagnosis,” she said. “The main problem is actually underdiagnois of disease.”
Breast MRI is currently recommended for screening women who are at a high-risk of breast-cancer, but despite decades of mammographic screening, breast cancer continues to cause high mortality for women who are deemed to be at an average risk of the disease. These data suggest that there is a need for improved methods of early diagnosis in this population.
Dr. Kuhl and her colleagues investigated the utility of supplemental MRI-screening of women who carry an average-risk of breast-cancer, and they conducted a prospective observational cohort-study that assessed the use of MRI screening in this population. The participants were in the usual age range for screening-mammography (40-70 years).
The women underwent dynamic contrast-enhanced MRI of the breast in addition to mammography every 12, 24, or 36 months, plus follow-up of 2 years to establish a standard-of-reference. The cohort included 2,120 women who underwent a total 3,861 MRI screenings.
Breast-cancer was diagnosed in 61 women (DCIS: 20, invasive: 41), and the rate of interval cancers was 0%, irrespective of screening interval. Of these women, 48 were diagnosed at prevalence-screening by MRI alone (supplemental cancer detection rate: 22.6 cases per 1,000 women screened. In addition, 13 women were diagnosed with breast-cancer in 1,741 incidence-screening-rounds collected over 4,887 women-years. A total 12 of these 13 incident cancers were diagnosed by screening-MRI alone (supplemental cancer detection rate was 6.9 per 1,000), one by MRI and mammography, and none were by mammography alone.
The authors also found that the supplemental cancer detection rate was independent of mammographic breast density. Invasive cancers were small, with a mean size of 8mm. They were node-negative in 93.4%, ER/PR-negative in 32.8%, and de-differentiated in 41.7% at prevalence, and 46% at incidence-screening. The specificity of MRI-screening was 97.1%, while false positive rate was 2.9%.
In a discussion of the paper, Dr. A. Marilyn Leitch, of the University of Texas Southwestern Medical Center, Dallas, pointed out that this was a selected population with negative mammograms. But is it possible to “apply MRI at longer intervals, say every 3 years, without initial mammography as a screening tool, in average risk women?” she asked
One of her concerns, however, is that “we hear all the time about the high false positive rates with MRI,” and they are generally higher than was reported in this study. “MRI also detects lesions that might drive patients to avoid breast conserving surgery, and there can be unreasonable costs for screening and work up of false positives.”
Screening guidelines from the USPSTF say that evidence for replacing mammography with MRI is lacking and the balance of benefit versus harms cannot be determined. “Even more ‘liberal’ guidelines from the American Cancer Society reserve MRI for high risk patients.”
What is needed is a clinical trial, she summarized, that will compare screening MRI at 3 year intervals to tomosynthesis mammogram annually in average risk women.
SAN FRANCISCO – MRI-screening may improve the detection of biologically relevant breast cancer in women who are at average-risk, and reduce the interval-cancer rate down to 0%, at a low false-positive rate, say the authors of a new study presented at the 2015 Breast Cancer Symposium.
In this cohort of heavily pre-screened women at average risk, the additional cancer yield achieved through MRI was high, at 15.8 cases per 1,000 women screened, and the added cancers diagnosed by MRI tended to be of high nuclear grade.
“MRI improves the detection of small high grade cancers in women at average risk, to the extent that the interval cancer rate was zero,” said Dr. Christiane Kuhl, of the University of Aachen, Germany.
“Between 30% and 50% of cancers identified in women who undergo screening mammography are not detected by mammography,” she said during her presentation.
Breast cancer continues to be the main or second most important cause of cancer death in women, and is the main cause of life years lost in women. “Which tells you that the main problem with mammography screening is not overdiagnosis,” she said. “The main problem is actually underdiagnois of disease.”
Breast MRI is currently recommended for screening women who are at a high-risk of breast-cancer, but despite decades of mammographic screening, breast cancer continues to cause high mortality for women who are deemed to be at an average risk of the disease. These data suggest that there is a need for improved methods of early diagnosis in this population.
Dr. Kuhl and her colleagues investigated the utility of supplemental MRI-screening of women who carry an average-risk of breast-cancer, and they conducted a prospective observational cohort-study that assessed the use of MRI screening in this population. The participants were in the usual age range for screening-mammography (40-70 years).
The women underwent dynamic contrast-enhanced MRI of the breast in addition to mammography every 12, 24, or 36 months, plus follow-up of 2 years to establish a standard-of-reference. The cohort included 2,120 women who underwent a total 3,861 MRI screenings.
Breast-cancer was diagnosed in 61 women (DCIS: 20, invasive: 41), and the rate of interval cancers was 0%, irrespective of screening interval. Of these women, 48 were diagnosed at prevalence-screening by MRI alone (supplemental cancer detection rate: 22.6 cases per 1,000 women screened. In addition, 13 women were diagnosed with breast-cancer in 1,741 incidence-screening-rounds collected over 4,887 women-years. A total 12 of these 13 incident cancers were diagnosed by screening-MRI alone (supplemental cancer detection rate was 6.9 per 1,000), one by MRI and mammography, and none were by mammography alone.
The authors also found that the supplemental cancer detection rate was independent of mammographic breast density. Invasive cancers were small, with a mean size of 8mm. They were node-negative in 93.4%, ER/PR-negative in 32.8%, and de-differentiated in 41.7% at prevalence, and 46% at incidence-screening. The specificity of MRI-screening was 97.1%, while false positive rate was 2.9%.
In a discussion of the paper, Dr. A. Marilyn Leitch, of the University of Texas Southwestern Medical Center, Dallas, pointed out that this was a selected population with negative mammograms. But is it possible to “apply MRI at longer intervals, say every 3 years, without initial mammography as a screening tool, in average risk women?” she asked
One of her concerns, however, is that “we hear all the time about the high false positive rates with MRI,” and they are generally higher than was reported in this study. “MRI also detects lesions that might drive patients to avoid breast conserving surgery, and there can be unreasonable costs for screening and work up of false positives.”
Screening guidelines from the USPSTF say that evidence for replacing mammography with MRI is lacking and the balance of benefit versus harms cannot be determined. “Even more ‘liberal’ guidelines from the American Cancer Society reserve MRI for high risk patients.”
What is needed is a clinical trial, she summarized, that will compare screening MRI at 3 year intervals to tomosynthesis mammogram annually in average risk women.
SAN FRANCISCO – MRI-screening may improve the detection of biologically relevant breast cancer in women who are at average-risk, and reduce the interval-cancer rate down to 0%, at a low false-positive rate, say the authors of a new study presented at the 2015 Breast Cancer Symposium.
In this cohort of heavily pre-screened women at average risk, the additional cancer yield achieved through MRI was high, at 15.8 cases per 1,000 women screened, and the added cancers diagnosed by MRI tended to be of high nuclear grade.
“MRI improves the detection of small high grade cancers in women at average risk, to the extent that the interval cancer rate was zero,” said Dr. Christiane Kuhl, of the University of Aachen, Germany.
“Between 30% and 50% of cancers identified in women who undergo screening mammography are not detected by mammography,” she said during her presentation.
Breast cancer continues to be the main or second most important cause of cancer death in women, and is the main cause of life years lost in women. “Which tells you that the main problem with mammography screening is not overdiagnosis,” she said. “The main problem is actually underdiagnois of disease.”
Breast MRI is currently recommended for screening women who are at a high-risk of breast-cancer, but despite decades of mammographic screening, breast cancer continues to cause high mortality for women who are deemed to be at an average risk of the disease. These data suggest that there is a need for improved methods of early diagnosis in this population.
Dr. Kuhl and her colleagues investigated the utility of supplemental MRI-screening of women who carry an average-risk of breast-cancer, and they conducted a prospective observational cohort-study that assessed the use of MRI screening in this population. The participants were in the usual age range for screening-mammography (40-70 years).
The women underwent dynamic contrast-enhanced MRI of the breast in addition to mammography every 12, 24, or 36 months, plus follow-up of 2 years to establish a standard-of-reference. The cohort included 2,120 women who underwent a total 3,861 MRI screenings.
Breast-cancer was diagnosed in 61 women (DCIS: 20, invasive: 41), and the rate of interval cancers was 0%, irrespective of screening interval. Of these women, 48 were diagnosed at prevalence-screening by MRI alone (supplemental cancer detection rate: 22.6 cases per 1,000 women screened. In addition, 13 women were diagnosed with breast-cancer in 1,741 incidence-screening-rounds collected over 4,887 women-years. A total 12 of these 13 incident cancers were diagnosed by screening-MRI alone (supplemental cancer detection rate was 6.9 per 1,000), one by MRI and mammography, and none were by mammography alone.
The authors also found that the supplemental cancer detection rate was independent of mammographic breast density. Invasive cancers were small, with a mean size of 8mm. They were node-negative in 93.4%, ER/PR-negative in 32.8%, and de-differentiated in 41.7% at prevalence, and 46% at incidence-screening. The specificity of MRI-screening was 97.1%, while false positive rate was 2.9%.
In a discussion of the paper, Dr. A. Marilyn Leitch, of the University of Texas Southwestern Medical Center, Dallas, pointed out that this was a selected population with negative mammograms. But is it possible to “apply MRI at longer intervals, say every 3 years, without initial mammography as a screening tool, in average risk women?” she asked
One of her concerns, however, is that “we hear all the time about the high false positive rates with MRI,” and they are generally higher than was reported in this study. “MRI also detects lesions that might drive patients to avoid breast conserving surgery, and there can be unreasonable costs for screening and work up of false positives.”
Screening guidelines from the USPSTF say that evidence for replacing mammography with MRI is lacking and the balance of benefit versus harms cannot be determined. “Even more ‘liberal’ guidelines from the American Cancer Society reserve MRI for high risk patients.”
What is needed is a clinical trial, she summarized, that will compare screening MRI at 3 year intervals to tomosynthesis mammogram annually in average risk women.
2015 BREAST CANCER SYMPOSIUM
Key clinical point: MRI-screening improved the detection of biologically relevant breast-cancer in women at average risk.
Major finding: The additional cancer yield achieved through MRI was 15.8 cases per 1,000 women screened.
Data source: A prospective observational cohort-study that was conducted in two centers on 2,120 asymptomatic women, for a total of 3,861 MRI-studies, covering 7,007 women-years.
Disclosures: The authors have no disclosures.
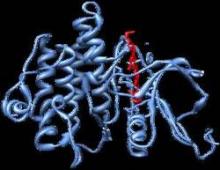
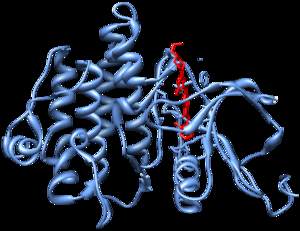
ASCO: AIs reduce risk of contralateral breast cancer in patients with BRCA mutation
SAN FRANCISCO – The use of aromatase inhibitors (AIs) in the adjuvant setting appears to delay the development of contralateral breast cancer, and this effect was particularly prevalent among breast cancer patients who were BRCA positive, according to findings presented here at the 2015 Breast Cancer Symposium.
“AI use was suggestive of a decreased risk in all patients with a P value of .08, which was not statistically significant,” said Dr. Maryam Nemati Shafaee, from the University of Texas M.D. Anderson Cancer Center, Houston, who presented the results of her study. “However among patients with BRCA mutation, AI use was significantly associated with a smaller hazard of developing contralateral breast cancer with a P value of .04.”
“This may give these patients an option other than prophylactic mastectomy,” she said.
The risk of contralateral breast cancer in women who are carriers of BRCA1 and 2 mutations is up to 64%. Those with estrogen receptor positive (ER+) disease are offered tamoxifen or AIs adjuvantly. Some studies have suggested that tamoxifen might be able to reduce the risk of contralateral breast cancer in this population, but results have been conflicting.
“There is no final conclusion on the use of tamoxifen in preventing contralateral breast cancer in BRCA mutation carriers,” said Dr. Shafee, “And there are no such data on the effect of AIs.”
Dr. Shafee and her colleagues identified 2,520 patients known to carry a BRCA mutation from a prospectively maintained database, and, of that number, 486 breast cancer patients with known BRCA status were included in the final analysis.
Of these patients, the majority were diagnosed under the age of 50 years, and the majority had not undergone prophylactic mastectomy. Most patients had received tamoxifen only (60%), 21% had received tamoxifen and AIs sequentially, and 16% had received AIs only.
The median follow up 8.6 years.
Upon univariate analysis, only BRCA status was associated with a risk of contralateral breast cancer (P= .04). “Interestingly AI use was suggestive to lead to decreased risk (P value of .08) but did not reach statistical significance,” said Dr. Shafee.
In multivariate analysis, BRCA status was significantly associated with an increased risk of contralateral breast cancer. AI was again suggestive of a decreased risk (P= .08).
BRCA mutation status was also significantly associated with shorter time to the development of contralateral breast cancer (P= .047), compared with patients who were BRCA negative. AI treatment was marginally significantly associated with time to the development of contralateral breast cancer (P= .088), as compared with patients who didn’t receive this treatment. Those who received AI therapy had a smaller hazard of cancer development in the other breast.
The effect on risk of cancer in the second breast was not statistically associated with age, HER2 status, TNM stage, and tamoxifen use.
Dr. Shafee noted that the study had several limitations, one being the relatively small sample size of BRCA 1&2 mutation carriers with hormone positive tumors. “Validation of our findings based on a larger cohort of BRCA mutation carriers who have received endocrine therapy in adjuvant setting is recommended,” she said.
Dr. William J. Gradishar, of the Lurie COmprehensive Cancer Center of Northwestern University, Chicago, noted that while the data are impressive, he agreed with Dr. Shafee that the “numbers are simply too small to make any sweeping recommendations based on these data.”
In his discussion of the popular, he also posed the question if these patients are really a reflection of BRCA mutation carriers, being that they are largely ER+. “The conclusions are intriguing and value further evaluation, and I would caution the use of this broadly in this use of individuals,” noted Dr. Gradishar.
SAN FRANCISCO – The use of aromatase inhibitors (AIs) in the adjuvant setting appears to delay the development of contralateral breast cancer, and this effect was particularly prevalent among breast cancer patients who were BRCA positive, according to findings presented here at the 2015 Breast Cancer Symposium.
“AI use was suggestive of a decreased risk in all patients with a P value of .08, which was not statistically significant,” said Dr. Maryam Nemati Shafaee, from the University of Texas M.D. Anderson Cancer Center, Houston, who presented the results of her study. “However among patients with BRCA mutation, AI use was significantly associated with a smaller hazard of developing contralateral breast cancer with a P value of .04.”
“This may give these patients an option other than prophylactic mastectomy,” she said.
The risk of contralateral breast cancer in women who are carriers of BRCA1 and 2 mutations is up to 64%. Those with estrogen receptor positive (ER+) disease are offered tamoxifen or AIs adjuvantly. Some studies have suggested that tamoxifen might be able to reduce the risk of contralateral breast cancer in this population, but results have been conflicting.
“There is no final conclusion on the use of tamoxifen in preventing contralateral breast cancer in BRCA mutation carriers,” said Dr. Shafee, “And there are no such data on the effect of AIs.”
Dr. Shafee and her colleagues identified 2,520 patients known to carry a BRCA mutation from a prospectively maintained database, and, of that number, 486 breast cancer patients with known BRCA status were included in the final analysis.
Of these patients, the majority were diagnosed under the age of 50 years, and the majority had not undergone prophylactic mastectomy. Most patients had received tamoxifen only (60%), 21% had received tamoxifen and AIs sequentially, and 16% had received AIs only.
The median follow up 8.6 years.
Upon univariate analysis, only BRCA status was associated with a risk of contralateral breast cancer (P= .04). “Interestingly AI use was suggestive to lead to decreased risk (P value of .08) but did not reach statistical significance,” said Dr. Shafee.
In multivariate analysis, BRCA status was significantly associated with an increased risk of contralateral breast cancer. AI was again suggestive of a decreased risk (P= .08).
BRCA mutation status was also significantly associated with shorter time to the development of contralateral breast cancer (P= .047), compared with patients who were BRCA negative. AI treatment was marginally significantly associated with time to the development of contralateral breast cancer (P= .088), as compared with patients who didn’t receive this treatment. Those who received AI therapy had a smaller hazard of cancer development in the other breast.
The effect on risk of cancer in the second breast was not statistically associated with age, HER2 status, TNM stage, and tamoxifen use.
Dr. Shafee noted that the study had several limitations, one being the relatively small sample size of BRCA 1&2 mutation carriers with hormone positive tumors. “Validation of our findings based on a larger cohort of BRCA mutation carriers who have received endocrine therapy in adjuvant setting is recommended,” she said.
Dr. William J. Gradishar, of the Lurie COmprehensive Cancer Center of Northwestern University, Chicago, noted that while the data are impressive, he agreed with Dr. Shafee that the “numbers are simply too small to make any sweeping recommendations based on these data.”
In his discussion of the popular, he also posed the question if these patients are really a reflection of BRCA mutation carriers, being that they are largely ER+. “The conclusions are intriguing and value further evaluation, and I would caution the use of this broadly in this use of individuals,” noted Dr. Gradishar.
SAN FRANCISCO – The use of aromatase inhibitors (AIs) in the adjuvant setting appears to delay the development of contralateral breast cancer, and this effect was particularly prevalent among breast cancer patients who were BRCA positive, according to findings presented here at the 2015 Breast Cancer Symposium.
“AI use was suggestive of a decreased risk in all patients with a P value of .08, which was not statistically significant,” said Dr. Maryam Nemati Shafaee, from the University of Texas M.D. Anderson Cancer Center, Houston, who presented the results of her study. “However among patients with BRCA mutation, AI use was significantly associated with a smaller hazard of developing contralateral breast cancer with a P value of .04.”
“This may give these patients an option other than prophylactic mastectomy,” she said.
The risk of contralateral breast cancer in women who are carriers of BRCA1 and 2 mutations is up to 64%. Those with estrogen receptor positive (ER+) disease are offered tamoxifen or AIs adjuvantly. Some studies have suggested that tamoxifen might be able to reduce the risk of contralateral breast cancer in this population, but results have been conflicting.
“There is no final conclusion on the use of tamoxifen in preventing contralateral breast cancer in BRCA mutation carriers,” said Dr. Shafee, “And there are no such data on the effect of AIs.”
Dr. Shafee and her colleagues identified 2,520 patients known to carry a BRCA mutation from a prospectively maintained database, and, of that number, 486 breast cancer patients with known BRCA status were included in the final analysis.
Of these patients, the majority were diagnosed under the age of 50 years, and the majority had not undergone prophylactic mastectomy. Most patients had received tamoxifen only (60%), 21% had received tamoxifen and AIs sequentially, and 16% had received AIs only.
The median follow up 8.6 years.
Upon univariate analysis, only BRCA status was associated with a risk of contralateral breast cancer (P= .04). “Interestingly AI use was suggestive to lead to decreased risk (P value of .08) but did not reach statistical significance,” said Dr. Shafee.
In multivariate analysis, BRCA status was significantly associated with an increased risk of contralateral breast cancer. AI was again suggestive of a decreased risk (P= .08).
BRCA mutation status was also significantly associated with shorter time to the development of contralateral breast cancer (P= .047), compared with patients who were BRCA negative. AI treatment was marginally significantly associated with time to the development of contralateral breast cancer (P= .088), as compared with patients who didn’t receive this treatment. Those who received AI therapy had a smaller hazard of cancer development in the other breast.
The effect on risk of cancer in the second breast was not statistically associated with age, HER2 status, TNM stage, and tamoxifen use.
Dr. Shafee noted that the study had several limitations, one being the relatively small sample size of BRCA 1&2 mutation carriers with hormone positive tumors. “Validation of our findings based on a larger cohort of BRCA mutation carriers who have received endocrine therapy in adjuvant setting is recommended,” she said.
Dr. William J. Gradishar, of the Lurie COmprehensive Cancer Center of Northwestern University, Chicago, noted that while the data are impressive, he agreed with Dr. Shafee that the “numbers are simply too small to make any sweeping recommendations based on these data.”
In his discussion of the popular, he also posed the question if these patients are really a reflection of BRCA mutation carriers, being that they are largely ER+. “The conclusions are intriguing and value further evaluation, and I would caution the use of this broadly in this use of individuals,” noted Dr. Gradishar.
Key clinical point: Aromase inhibitors (AIs) may reduce the rate of contralateral breast cancer in women who already have the disease and are positive for BRCA mutations.
Major finding: Compared with patients who did not receive AI therapy, those given an AI had a smaller likelihood of developing contralateral breast cancer (HR = 0.42; 95% CI, 0.22-0.81; P= .01).
Data source: A retrospective study of a prospectively maintained database from which 486 breast cancer patients with known BRCA status were included.
Disclosures: Dr. Shafee had no disclosures. Co-author Banu Arun had done consulting or had an advisory role with Abbvie and received research funding from Avon Foundation and Susan G. Komen. Dr Gradishar had no disclosures.
ASCO: Radiotherapy not needed for all women post mastectomy
Postmastectomy radiotherapy should not be routinely recommended for breast cancer patients with microscopic nodal metastases (N1mic) and T1-2 tumors, according to new findings presented at the symposium.
In patients with T1-2, N1 disease who were treated with standard therapies, the study authors found that overall, there were low rates of locoregional failure. Dr. Lonika Majithia of Ohio State University, Columbus, and colleagues, reported that “patients with N1mic disease had no locoregional failure events and improved overall survival, compared with patients with macrometastases.”
The indications for postmastectomy radiotherapy have expanded to include patients with one to three axillary nodal metastases, note the authors, and with improvements in diagnostic evaluation, an increasing number of N1mic are being detected. Therefore, the challenge facing oncologists now is if the risk posed by N1mic warrants routine delivery of postmastectomy radiotherapy.
The authors identified 550 eligible patients from a prospectively maintained cancer registry, who had a 5-year median follow-up. All patients had pathologic T1-2N1 breast cancer and were treated with an initial mastectomy and adjuvant systemic therapy from 2000 to 2013.
The primary endpoint of the study was locoregional failure, defined as a recurrence in either the ipsilateral chest wall or regional lymphatics (axillary, internal mammary, or supraclavicular). Secondary endpoints included disease-free survival and overall survival.
The majority of patients in the cohort had received chemotherapy (78%; n = 428) and antiendocrine therapy (70%; n = 385), while 15% (n = 82) had received postmastectomy radiation. Among the patients with N1mic disease, 81 had 1+ node, 13 had 2+ nodes, and 1 had 3+ nodes.
The 5-year rate of locoregional failure was 0% for patients with N1mic disease, as compared with 4.6% for those with macrometastases (P = .84). For the entire patient cohort, the 5-year locoregional failure rate was 3.9%. For patients with 1+, 2+, and 3+ nodes, the 5-year rate was 2.6%, 4.7%, and 6.4%, respectively (P = .79).
The authors observed that patients with N1mic disease had a trend towards improved disease-free survival (91.6% vs. 82.3%; P = .07) as well as significantly improved overall survival (96.9% vs. 87.6%; P = .03), as compared with patients with macrometastases.
Postmastectomy radiotherapy should not be routinely recommended for breast cancer patients with microscopic nodal metastases (N1mic) and T1-2 tumors, according to new findings presented at the symposium.
In patients with T1-2, N1 disease who were treated with standard therapies, the study authors found that overall, there were low rates of locoregional failure. Dr. Lonika Majithia of Ohio State University, Columbus, and colleagues, reported that “patients with N1mic disease had no locoregional failure events and improved overall survival, compared with patients with macrometastases.”
The indications for postmastectomy radiotherapy have expanded to include patients with one to three axillary nodal metastases, note the authors, and with improvements in diagnostic evaluation, an increasing number of N1mic are being detected. Therefore, the challenge facing oncologists now is if the risk posed by N1mic warrants routine delivery of postmastectomy radiotherapy.
The authors identified 550 eligible patients from a prospectively maintained cancer registry, who had a 5-year median follow-up. All patients had pathologic T1-2N1 breast cancer and were treated with an initial mastectomy and adjuvant systemic therapy from 2000 to 2013.
The primary endpoint of the study was locoregional failure, defined as a recurrence in either the ipsilateral chest wall or regional lymphatics (axillary, internal mammary, or supraclavicular). Secondary endpoints included disease-free survival and overall survival.
The majority of patients in the cohort had received chemotherapy (78%; n = 428) and antiendocrine therapy (70%; n = 385), while 15% (n = 82) had received postmastectomy radiation. Among the patients with N1mic disease, 81 had 1+ node, 13 had 2+ nodes, and 1 had 3+ nodes.
The 5-year rate of locoregional failure was 0% for patients with N1mic disease, as compared with 4.6% for those with macrometastases (P = .84). For the entire patient cohort, the 5-year locoregional failure rate was 3.9%. For patients with 1+, 2+, and 3+ nodes, the 5-year rate was 2.6%, 4.7%, and 6.4%, respectively (P = .79).
The authors observed that patients with N1mic disease had a trend towards improved disease-free survival (91.6% vs. 82.3%; P = .07) as well as significantly improved overall survival (96.9% vs. 87.6%; P = .03), as compared with patients with macrometastases.
Postmastectomy radiotherapy should not be routinely recommended for breast cancer patients with microscopic nodal metastases (N1mic) and T1-2 tumors, according to new findings presented at the symposium.
In patients with T1-2, N1 disease who were treated with standard therapies, the study authors found that overall, there were low rates of locoregional failure. Dr. Lonika Majithia of Ohio State University, Columbus, and colleagues, reported that “patients with N1mic disease had no locoregional failure events and improved overall survival, compared with patients with macrometastases.”
The indications for postmastectomy radiotherapy have expanded to include patients with one to three axillary nodal metastases, note the authors, and with improvements in diagnostic evaluation, an increasing number of N1mic are being detected. Therefore, the challenge facing oncologists now is if the risk posed by N1mic warrants routine delivery of postmastectomy radiotherapy.
The authors identified 550 eligible patients from a prospectively maintained cancer registry, who had a 5-year median follow-up. All patients had pathologic T1-2N1 breast cancer and were treated with an initial mastectomy and adjuvant systemic therapy from 2000 to 2013.
The primary endpoint of the study was locoregional failure, defined as a recurrence in either the ipsilateral chest wall or regional lymphatics (axillary, internal mammary, or supraclavicular). Secondary endpoints included disease-free survival and overall survival.
The majority of patients in the cohort had received chemotherapy (78%; n = 428) and antiendocrine therapy (70%; n = 385), while 15% (n = 82) had received postmastectomy radiation. Among the patients with N1mic disease, 81 had 1+ node, 13 had 2+ nodes, and 1 had 3+ nodes.
The 5-year rate of locoregional failure was 0% for patients with N1mic disease, as compared with 4.6% for those with macrometastases (P = .84). For the entire patient cohort, the 5-year locoregional failure rate was 3.9%. For patients with 1+, 2+, and 3+ nodes, the 5-year rate was 2.6%, 4.7%, and 6.4%, respectively (P = .79).
The authors observed that patients with N1mic disease had a trend towards improved disease-free survival (91.6% vs. 82.3%; P = .07) as well as significantly improved overall survival (96.9% vs. 87.6%; P = .03), as compared with patients with macrometastases.
FROM THE 2015 ASCO BREAST CANCER SYMPOSIUM
Key clinical point: Radiotherapy following mastectomy should not be routinely recommended for breast cancer patients with microscopic nodal metastases (N1mic) and T1-2 tumors.
Major finding: The 5-year rate of locoregional failure was 0% for patients with N1mic disease vs. 4.6% in those with macrometastases (P = .84).
Data source: 550 eligible patients who met the inclusion criteria were identified from a prospectively maintained cancer registry.
Disclosures: No conflicts of interest were disclosed.
Treating women with metastatic breast cancer takes toll
Medical oncologists empathize with their patients and feel responsible for providing them emotional/psychological support, but many experience the negative emotional impact of their work when treating women with metastatic breast cancer, according to survey results presented at the symposium.
Medical oncologists with less experience appeared to be more impacted by their emotions as compared to physicians with more experience, and the study authors noted that “acknowledging medical oncologists’ emotions is important and underscores their own need for psychological/emotional support.”
Dr. Adam M. Brufsky, associate chief, division of hematology/oncology and codirector, Comprehensive Breast Cancer Center at the University of Pittsburgh, and his colleagues surveyed medical oncologists who treat five or more women per month with metastatic breast cancer, and surveys were also completed by patients with the disease. The goal of the study was to evaluate the emotional impact on the oncologist. The surveys were conducted from June to August 2014.
A total of 359 patients (median age 53 years) and 252 medical oncologists (median age 49 years and a median of 15 years in practice) completed the survey.
At the initial diagnosis of metastatic breast cancer, a larger proportion of oncologists as compared with patients reported that showing care and compassion (81% vs. 72%) and helping patients cope with their diagnosis (63% vs. 51%) were very important. A smaller percentage of respondents felt that referring patients to support services (24% vs. 38%) was very important, but a greater number of oncologists who were practicing less than 15 years, as compared to those in practice longer, stated that referrals to support services were very important at first diagnosis (30% vs. 19%). Dr. Brufsky and his team also found that a slightly higher number of more experienced oncologists perceived emotions like anxiety, commitment, hopefulness, and determination in their patients at their initial diagnosis.
A large proportion of medical oncologists (42%) reported that treating women with this diagnosis generated a great deal of negative emotion, but a majority (81% strongly/somewhat) agreed that it is unprofessional to let emotions impact treatment recommendations. However, nearly a quarter (23%) reported that emotions kept them from providing some information to patients.
The vast majority of respondents (93%) said that they did not want to give their patients false hope, but yet 27% reported that in certain situations, they do not discuss the fact that metastatic breast cancer is incurable with their patients.
Medical oncologists empathize with their patients and feel responsible for providing them emotional/psychological support, but many experience the negative emotional impact of their work when treating women with metastatic breast cancer, according to survey results presented at the symposium.
Medical oncologists with less experience appeared to be more impacted by their emotions as compared to physicians with more experience, and the study authors noted that “acknowledging medical oncologists’ emotions is important and underscores their own need for psychological/emotional support.”
Dr. Adam M. Brufsky, associate chief, division of hematology/oncology and codirector, Comprehensive Breast Cancer Center at the University of Pittsburgh, and his colleagues surveyed medical oncologists who treat five or more women per month with metastatic breast cancer, and surveys were also completed by patients with the disease. The goal of the study was to evaluate the emotional impact on the oncologist. The surveys were conducted from June to August 2014.
A total of 359 patients (median age 53 years) and 252 medical oncologists (median age 49 years and a median of 15 years in practice) completed the survey.
At the initial diagnosis of metastatic breast cancer, a larger proportion of oncologists as compared with patients reported that showing care and compassion (81% vs. 72%) and helping patients cope with their diagnosis (63% vs. 51%) were very important. A smaller percentage of respondents felt that referring patients to support services (24% vs. 38%) was very important, but a greater number of oncologists who were practicing less than 15 years, as compared to those in practice longer, stated that referrals to support services were very important at first diagnosis (30% vs. 19%). Dr. Brufsky and his team also found that a slightly higher number of more experienced oncologists perceived emotions like anxiety, commitment, hopefulness, and determination in their patients at their initial diagnosis.
A large proportion of medical oncologists (42%) reported that treating women with this diagnosis generated a great deal of negative emotion, but a majority (81% strongly/somewhat) agreed that it is unprofessional to let emotions impact treatment recommendations. However, nearly a quarter (23%) reported that emotions kept them from providing some information to patients.
The vast majority of respondents (93%) said that they did not want to give their patients false hope, but yet 27% reported that in certain situations, they do not discuss the fact that metastatic breast cancer is incurable with their patients.
Medical oncologists empathize with their patients and feel responsible for providing them emotional/psychological support, but many experience the negative emotional impact of their work when treating women with metastatic breast cancer, according to survey results presented at the symposium.
Medical oncologists with less experience appeared to be more impacted by their emotions as compared to physicians with more experience, and the study authors noted that “acknowledging medical oncologists’ emotions is important and underscores their own need for psychological/emotional support.”
Dr. Adam M. Brufsky, associate chief, division of hematology/oncology and codirector, Comprehensive Breast Cancer Center at the University of Pittsburgh, and his colleagues surveyed medical oncologists who treat five or more women per month with metastatic breast cancer, and surveys were also completed by patients with the disease. The goal of the study was to evaluate the emotional impact on the oncologist. The surveys were conducted from June to August 2014.
A total of 359 patients (median age 53 years) and 252 medical oncologists (median age 49 years and a median of 15 years in practice) completed the survey.
At the initial diagnosis of metastatic breast cancer, a larger proportion of oncologists as compared with patients reported that showing care and compassion (81% vs. 72%) and helping patients cope with their diagnosis (63% vs. 51%) were very important. A smaller percentage of respondents felt that referring patients to support services (24% vs. 38%) was very important, but a greater number of oncologists who were practicing less than 15 years, as compared to those in practice longer, stated that referrals to support services were very important at first diagnosis (30% vs. 19%). Dr. Brufsky and his team also found that a slightly higher number of more experienced oncologists perceived emotions like anxiety, commitment, hopefulness, and determination in their patients at their initial diagnosis.
A large proportion of medical oncologists (42%) reported that treating women with this diagnosis generated a great deal of negative emotion, but a majority (81% strongly/somewhat) agreed that it is unprofessional to let emotions impact treatment recommendations. However, nearly a quarter (23%) reported that emotions kept them from providing some information to patients.
The vast majority of respondents (93%) said that they did not want to give their patients false hope, but yet 27% reported that in certain situations, they do not discuss the fact that metastatic breast cancer is incurable with their patients.
FROM THE ASCO BREAST CANCER SYMPOSIUM
Key clinical point: Many medical oncologists experience the negative emotional impact of their work when treating patients with metastatic breast cancer.
Major finding: Medical oncologists’ emotions are important and these practitioners should acknowledge their own need for psychological/emotional support.
Data source: A survey was conducted of 359 patients and 252 medical oncologists.
Disclosures: The investigators had no relevant disclosures.
NLR correlates with survival in advanced breast cancer
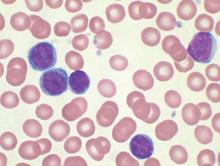
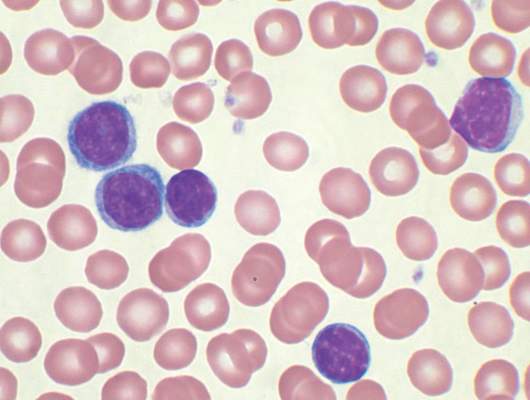
After treatment begins, an increased neutrophil lymphocyte ratio (NLR) can be correlated with poor disease-specific survival in stage IV breast cancer, according to research presented at the symposium. In addition, the change in NLR might be an index of response to systemic treatment.
Inflammatory response exacerbates mechanisms linked to tumor growth and dissemination, note the study authors, led by Dr. Hae-na Shin of the University of Ulsan, Seoul, South Korea. Used as an index of systemic inflammatory status, the NLR could be a predictive biomarker for both prognosis and treatment response.
To test their hypothesis, Dr. Shin and his colleagues evaluated the baseline NLR prior to beginning treatment, and then the change in posttreatment NLR, to assess if the initial NLR and its change after therapy would be predictive of disease outcome in stage IV breast cancer patients.
The study cohort included 250 women with stage IV breast cancer who were diagnosed at the Asan Medical Center between 1997 and 2012. The NLR was evaluated at their first visit to the center, and a posttreatment NLR was obtained during the first follow-up appointment after patients received their first treatment.
The authors divided the pretreatment NLR by quartile, and the change in NLR was calculated by dividing posttreatment NLR by pretreatment NLR. If the value was greater than or equal to 1.2, NLR change was increased, and if not, then it was considered to be unchanged or reduced. The prognostic value of NLR was then evaluated by comparison with Cancer Specific Survival (CSS).
When comparing pretreatment NLR and posttreatment NLR, the NLR was elevated in 85 patients (34%) but remained the same or decreased in 165 others (66%). There were no significant differences between these two groups in baseline characteristics. However, in CSS, there were differences between the two groups but they did not reach statistical significance (log rank P = 0.052). The 1-, 3-, 5-year CSS rate was 78.8%, 35.7%, 20.5% in the group with an increased NLR, and 87.1%, 49.3%, 26.9% in the other patient group.
Upon multivariate analysis, the results suggested that an increased NLR change (post/pre NLR greater than or equal to 1.2) had statistical significance as a prognostic factor of stage IV breast cancer patients after treatment (hazard ratio, 1.750; 95% confidence interval, 1.130-2.709; P = 0.012).
After treatment begins, an increased neutrophil lymphocyte ratio (NLR) can be correlated with poor disease-specific survival in stage IV breast cancer, according to research presented at the symposium. In addition, the change in NLR might be an index of response to systemic treatment.
Inflammatory response exacerbates mechanisms linked to tumor growth and dissemination, note the study authors, led by Dr. Hae-na Shin of the University of Ulsan, Seoul, South Korea. Used as an index of systemic inflammatory status, the NLR could be a predictive biomarker for both prognosis and treatment response.
To test their hypothesis, Dr. Shin and his colleagues evaluated the baseline NLR prior to beginning treatment, and then the change in posttreatment NLR, to assess if the initial NLR and its change after therapy would be predictive of disease outcome in stage IV breast cancer patients.
The study cohort included 250 women with stage IV breast cancer who were diagnosed at the Asan Medical Center between 1997 and 2012. The NLR was evaluated at their first visit to the center, and a posttreatment NLR was obtained during the first follow-up appointment after patients received their first treatment.
The authors divided the pretreatment NLR by quartile, and the change in NLR was calculated by dividing posttreatment NLR by pretreatment NLR. If the value was greater than or equal to 1.2, NLR change was increased, and if not, then it was considered to be unchanged or reduced. The prognostic value of NLR was then evaluated by comparison with Cancer Specific Survival (CSS).
When comparing pretreatment NLR and posttreatment NLR, the NLR was elevated in 85 patients (34%) but remained the same or decreased in 165 others (66%). There were no significant differences between these two groups in baseline characteristics. However, in CSS, there were differences between the two groups but they did not reach statistical significance (log rank P = 0.052). The 1-, 3-, 5-year CSS rate was 78.8%, 35.7%, 20.5% in the group with an increased NLR, and 87.1%, 49.3%, 26.9% in the other patient group.
Upon multivariate analysis, the results suggested that an increased NLR change (post/pre NLR greater than or equal to 1.2) had statistical significance as a prognostic factor of stage IV breast cancer patients after treatment (hazard ratio, 1.750; 95% confidence interval, 1.130-2.709; P = 0.012).
After treatment begins, an increased neutrophil lymphocyte ratio (NLR) can be correlated with poor disease-specific survival in stage IV breast cancer, according to research presented at the symposium. In addition, the change in NLR might be an index of response to systemic treatment.
Inflammatory response exacerbates mechanisms linked to tumor growth and dissemination, note the study authors, led by Dr. Hae-na Shin of the University of Ulsan, Seoul, South Korea. Used as an index of systemic inflammatory status, the NLR could be a predictive biomarker for both prognosis and treatment response.
To test their hypothesis, Dr. Shin and his colleagues evaluated the baseline NLR prior to beginning treatment, and then the change in posttreatment NLR, to assess if the initial NLR and its change after therapy would be predictive of disease outcome in stage IV breast cancer patients.
The study cohort included 250 women with stage IV breast cancer who were diagnosed at the Asan Medical Center between 1997 and 2012. The NLR was evaluated at their first visit to the center, and a posttreatment NLR was obtained during the first follow-up appointment after patients received their first treatment.
The authors divided the pretreatment NLR by quartile, and the change in NLR was calculated by dividing posttreatment NLR by pretreatment NLR. If the value was greater than or equal to 1.2, NLR change was increased, and if not, then it was considered to be unchanged or reduced. The prognostic value of NLR was then evaluated by comparison with Cancer Specific Survival (CSS).
When comparing pretreatment NLR and posttreatment NLR, the NLR was elevated in 85 patients (34%) but remained the same or decreased in 165 others (66%). There were no significant differences between these two groups in baseline characteristics. However, in CSS, there were differences between the two groups but they did not reach statistical significance (log rank P = 0.052). The 1-, 3-, 5-year CSS rate was 78.8%, 35.7%, 20.5% in the group with an increased NLR, and 87.1%, 49.3%, 26.9% in the other patient group.
Upon multivariate analysis, the results suggested that an increased NLR change (post/pre NLR greater than or equal to 1.2) had statistical significance as a prognostic factor of stage IV breast cancer patients after treatment (hazard ratio, 1.750; 95% confidence interval, 1.130-2.709; P = 0.012).
AT THE ASCO BREAST CANCER SYMPOSIUM
Key clinical point: Neutrophil lymphocyte ratio (NLR) can be correlated with poor disease-specific survival in stage IV breast cancer and the change in NLR might be an index of response to systemic treatment.
Major finding: The results suggest that an increased NLR change (post/pre NLR greater than or equal to 1.2) had statistical significance as a prognostic factor of stage IV breast cancer patients after treatment (HR, 1.750; 95% CI, 1.130-2.709; P = .012).
Data source: The cohort was comprised of 250 stage IV breast cancer patients diagnosed at a single center and pre and post treatment NLR were evaluated.
Disclosures: The investigators had no relevant disclosures.
No survival difference between continuous and intermittent ADT
Intermittent androgen deprivation is not inferior to continuous therapy in prostate cancer patients, when looking at overall survival, and can be considered an alternative option for patients with recurrent or metastatic disease, according to a new meta-analysis published online Sept. 17 in JAMA Oncology.
Additionally, even though there were no major differences in quality of life observed between groups, some domains seemed to be improved with intermittent therapy.
But the researchers emphasize that it is not yet time to completely give up continuous therapy. “The high risk of bias observed in some trials, the unclear optimal approach to the duration of treatment and off-treatment periods and criteria on which it should be based, and the unknown magnitude of effect according to the disease stage warrant further research before it becomes the mandatory standard of care,” wrote Dr. Sindy Magnan, Université Laval, Quebec City, and colleagues. (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.2895).
Even though intermittent androgen deprivation appears to be an attractive option in this population, evidence for its safety and efficacy is rather limited, and because of that, its use remains somewhat controversial. Recommendations in current guidelines are also variable and not consistent.
However, the importance of assessing this treatment modality is growing, the authors pointed out, given the increase in the number of clinical trials and use of intermittent androgen deprivation therapy (ADT) in clinical practice, and was the impetus for conducting this systematic review and meta-analysis.
A total of 22 articles from 15 trials, for a total of 6,856 patients met their inclusion criteria. All papers were published between 2000 and 2013, and all but one study had an unclear or high risk of bias.
There were only six trials that provided survival data and hazard rations, and two others provided enough information to calculate the hazard ratios. There was no difference between intermittent and continuous therapy based on pooled results of those eight trials (5,352 patients, hazard ratio for death, 1.02; 95% confidence interval, 0.93-1.11; I2 = 23%).
No significant differences were observed between the two treatment groups with respect to cancer-specific survival based on pooled results from five trials (3,613 patients, HR for death, 1.02; 95% CI, 0.87-1.19; I2 = 14%). These results were also consistent across all subgroup and sensitivity analyses.
The same was true for progression-free survival, with no significant differences observed between groups (HR, 0.94; 95% CI, 0.84-1.05; four trials, 1,774 patients).
For quality of life, two trials reported that it was improved with intermittent therapy, while three trials did not observe any difference between the two treatment methods. The other seven trials showed that quality of life was increased with intermittent therapy but only in certain domains, with the most frequently detected differences relating to physical and sexual functioning.
Dr. Magnan is a recipient of a Resident Physician Health Research Career Training Grant from the Fonds de Recherche du Quebec–Santé (FRQS). Dr. Fradet and Dr. Turgeon are recipients of a Clinician-Scientist Award from the FRQS. Dr. Vigneault has received honoraria for consultation for Abvie, Sanofie, Jansen, Astellas, Peladin, and Amgen. None of the other authors have reported disclosures.
The meta-analysis conducted by Magnan et al. is exhaustive, and the team is to be commended for the extensive work and appropriate use of the established methodological guidelines assessing studies comparing intermittent androgen deprivation therapy with continuous ADT for prostate cancer.
The authors have analyzed the data and drawn conclusions based on statistical findings using population science.
However, there is a degree of clinical uncertainty in the data, and this is highlighted by the fact that one of the largest and most robust phase III studies, S9346, that is included in this analysis, begins the “Conclusion” section of its abstract with “Our findings were statistically inconclusive.”
Thus, can population science guide well-informed individual treatment recommendations for who should, and who should not, undergo intermittent ADT? The answer to this question is “No.”
But taking the totality of the data into account and attempting to refine the recommendations for individual patients, there is level I evidence to support intermittent treatment when physician and patient opt to commence androgen deprivation for biochemical recurrence. Notably in this setting, the risk of prostate cancer death is often less than the risk of dying from a comorbidity, a fact supported by the meta-analysis, even with all its limitations, which shows no evidence of a decrement in overall survival.
There is some statistical uncertainty about metastatic disease that is not definitively clarified by the meta-analysis. As such, in the metastatic setting, it is proposed that when a patient is not on a protocol, it is very reasonable to exercise clinical judgment whether to use intermittent ADT based on an individual patient’s response to therapy, adverse event profile, and risk of death from a competing comorbidity.
Dr. Christopher J. Sweeney is from the Lank Center for Genitourinary Oncology, Dana Farber Cancer Institute, Harvard Medical School, Boston. He has no disclosures. These remarks were taken from his editorial accompanying Dr. Magnan’s report (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.3005).
The meta-analysis conducted by Magnan et al. is exhaustive, and the team is to be commended for the extensive work and appropriate use of the established methodological guidelines assessing studies comparing intermittent androgen deprivation therapy with continuous ADT for prostate cancer.
The authors have analyzed the data and drawn conclusions based on statistical findings using population science.
However, there is a degree of clinical uncertainty in the data, and this is highlighted by the fact that one of the largest and most robust phase III studies, S9346, that is included in this analysis, begins the “Conclusion” section of its abstract with “Our findings were statistically inconclusive.”
Thus, can population science guide well-informed individual treatment recommendations for who should, and who should not, undergo intermittent ADT? The answer to this question is “No.”
But taking the totality of the data into account and attempting to refine the recommendations for individual patients, there is level I evidence to support intermittent treatment when physician and patient opt to commence androgen deprivation for biochemical recurrence. Notably in this setting, the risk of prostate cancer death is often less than the risk of dying from a comorbidity, a fact supported by the meta-analysis, even with all its limitations, which shows no evidence of a decrement in overall survival.
There is some statistical uncertainty about metastatic disease that is not definitively clarified by the meta-analysis. As such, in the metastatic setting, it is proposed that when a patient is not on a protocol, it is very reasonable to exercise clinical judgment whether to use intermittent ADT based on an individual patient’s response to therapy, adverse event profile, and risk of death from a competing comorbidity.
Dr. Christopher J. Sweeney is from the Lank Center for Genitourinary Oncology, Dana Farber Cancer Institute, Harvard Medical School, Boston. He has no disclosures. These remarks were taken from his editorial accompanying Dr. Magnan’s report (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.3005).
The meta-analysis conducted by Magnan et al. is exhaustive, and the team is to be commended for the extensive work and appropriate use of the established methodological guidelines assessing studies comparing intermittent androgen deprivation therapy with continuous ADT for prostate cancer.
The authors have analyzed the data and drawn conclusions based on statistical findings using population science.
However, there is a degree of clinical uncertainty in the data, and this is highlighted by the fact that one of the largest and most robust phase III studies, S9346, that is included in this analysis, begins the “Conclusion” section of its abstract with “Our findings were statistically inconclusive.”
Thus, can population science guide well-informed individual treatment recommendations for who should, and who should not, undergo intermittent ADT? The answer to this question is “No.”
But taking the totality of the data into account and attempting to refine the recommendations for individual patients, there is level I evidence to support intermittent treatment when physician and patient opt to commence androgen deprivation for biochemical recurrence. Notably in this setting, the risk of prostate cancer death is often less than the risk of dying from a comorbidity, a fact supported by the meta-analysis, even with all its limitations, which shows no evidence of a decrement in overall survival.
There is some statistical uncertainty about metastatic disease that is not definitively clarified by the meta-analysis. As such, in the metastatic setting, it is proposed that when a patient is not on a protocol, it is very reasonable to exercise clinical judgment whether to use intermittent ADT based on an individual patient’s response to therapy, adverse event profile, and risk of death from a competing comorbidity.
Dr. Christopher J. Sweeney is from the Lank Center for Genitourinary Oncology, Dana Farber Cancer Institute, Harvard Medical School, Boston. He has no disclosures. These remarks were taken from his editorial accompanying Dr. Magnan’s report (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.3005).
Intermittent androgen deprivation is not inferior to continuous therapy in prostate cancer patients, when looking at overall survival, and can be considered an alternative option for patients with recurrent or metastatic disease, according to a new meta-analysis published online Sept. 17 in JAMA Oncology.
Additionally, even though there were no major differences in quality of life observed between groups, some domains seemed to be improved with intermittent therapy.
But the researchers emphasize that it is not yet time to completely give up continuous therapy. “The high risk of bias observed in some trials, the unclear optimal approach to the duration of treatment and off-treatment periods and criteria on which it should be based, and the unknown magnitude of effect according to the disease stage warrant further research before it becomes the mandatory standard of care,” wrote Dr. Sindy Magnan, Université Laval, Quebec City, and colleagues. (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.2895).
Even though intermittent androgen deprivation appears to be an attractive option in this population, evidence for its safety and efficacy is rather limited, and because of that, its use remains somewhat controversial. Recommendations in current guidelines are also variable and not consistent.
However, the importance of assessing this treatment modality is growing, the authors pointed out, given the increase in the number of clinical trials and use of intermittent androgen deprivation therapy (ADT) in clinical practice, and was the impetus for conducting this systematic review and meta-analysis.
A total of 22 articles from 15 trials, for a total of 6,856 patients met their inclusion criteria. All papers were published between 2000 and 2013, and all but one study had an unclear or high risk of bias.
There were only six trials that provided survival data and hazard rations, and two others provided enough information to calculate the hazard ratios. There was no difference between intermittent and continuous therapy based on pooled results of those eight trials (5,352 patients, hazard ratio for death, 1.02; 95% confidence interval, 0.93-1.11; I2 = 23%).
No significant differences were observed between the two treatment groups with respect to cancer-specific survival based on pooled results from five trials (3,613 patients, HR for death, 1.02; 95% CI, 0.87-1.19; I2 = 14%). These results were also consistent across all subgroup and sensitivity analyses.
The same was true for progression-free survival, with no significant differences observed between groups (HR, 0.94; 95% CI, 0.84-1.05; four trials, 1,774 patients).
For quality of life, two trials reported that it was improved with intermittent therapy, while three trials did not observe any difference between the two treatment methods. The other seven trials showed that quality of life was increased with intermittent therapy but only in certain domains, with the most frequently detected differences relating to physical and sexual functioning.
Dr. Magnan is a recipient of a Resident Physician Health Research Career Training Grant from the Fonds de Recherche du Quebec–Santé (FRQS). Dr. Fradet and Dr. Turgeon are recipients of a Clinician-Scientist Award from the FRQS. Dr. Vigneault has received honoraria for consultation for Abvie, Sanofie, Jansen, Astellas, Peladin, and Amgen. None of the other authors have reported disclosures.
Intermittent androgen deprivation is not inferior to continuous therapy in prostate cancer patients, when looking at overall survival, and can be considered an alternative option for patients with recurrent or metastatic disease, according to a new meta-analysis published online Sept. 17 in JAMA Oncology.
Additionally, even though there were no major differences in quality of life observed between groups, some domains seemed to be improved with intermittent therapy.
But the researchers emphasize that it is not yet time to completely give up continuous therapy. “The high risk of bias observed in some trials, the unclear optimal approach to the duration of treatment and off-treatment periods and criteria on which it should be based, and the unknown magnitude of effect according to the disease stage warrant further research before it becomes the mandatory standard of care,” wrote Dr. Sindy Magnan, Université Laval, Quebec City, and colleagues. (JAMA Oncol. 2015. doi: 10.1001/jamaoncol.2015.2895).
Even though intermittent androgen deprivation appears to be an attractive option in this population, evidence for its safety and efficacy is rather limited, and because of that, its use remains somewhat controversial. Recommendations in current guidelines are also variable and not consistent.
However, the importance of assessing this treatment modality is growing, the authors pointed out, given the increase in the number of clinical trials and use of intermittent androgen deprivation therapy (ADT) in clinical practice, and was the impetus for conducting this systematic review and meta-analysis.
A total of 22 articles from 15 trials, for a total of 6,856 patients met their inclusion criteria. All papers were published between 2000 and 2013, and all but one study had an unclear or high risk of bias.
There were only six trials that provided survival data and hazard rations, and two others provided enough information to calculate the hazard ratios. There was no difference between intermittent and continuous therapy based on pooled results of those eight trials (5,352 patients, hazard ratio for death, 1.02; 95% confidence interval, 0.93-1.11; I2 = 23%).
No significant differences were observed between the two treatment groups with respect to cancer-specific survival based on pooled results from five trials (3,613 patients, HR for death, 1.02; 95% CI, 0.87-1.19; I2 = 14%). These results were also consistent across all subgroup and sensitivity analyses.
The same was true for progression-free survival, with no significant differences observed between groups (HR, 0.94; 95% CI, 0.84-1.05; four trials, 1,774 patients).
For quality of life, two trials reported that it was improved with intermittent therapy, while three trials did not observe any difference between the two treatment methods. The other seven trials showed that quality of life was increased with intermittent therapy but only in certain domains, with the most frequently detected differences relating to physical and sexual functioning.
Dr. Magnan is a recipient of a Resident Physician Health Research Career Training Grant from the Fonds de Recherche du Quebec–Santé (FRQS). Dr. Fradet and Dr. Turgeon are recipients of a Clinician-Scientist Award from the FRQS. Dr. Vigneault has received honoraria for consultation for Abvie, Sanofie, Jansen, Astellas, Peladin, and Amgen. None of the other authors have reported disclosures.
FROM JAMA ONCOLOGY
Key clinical point: Intermittent androgen deprivation is not inferior to continuous therapy in regards to overall survival.
Major finding: There was no significant difference between intermittent and continuous therapy for overall survival (HR, 1.02; 95% CI, 0.93-1.11) or cancer-specific survival (HR, 1.02;95% CI, 0.87-1.19).
Data source: A meta-analysis that included 22 articles from 15 trials, with a total of 6,856 patients with prostate cancer treated with androgen deprivation therapy
Disclosures: Dr. Magnan is a recipient of a Resident Physician Health Research Career Training Grant from the Fonds de Recherche du Québec–Santé (FRQS). Dr. Fradet and Dr. Turgeon are recipients of a Clinician-Scientist Award from the FRQS. Dr. Vigneault has received honoraria for consultation for Abvie, Sanofie, Jansen, Astellas, Peladin, and Amgen. None of the other authors have reported disclosures.
Reovirus ready for clinical testing in CLL
Reovirus, a naturally occurring oncolytic virus, appears to exert direct cytotoxic activity against chronic lymphocytic leukemia (CLL) and “phenotypically and functionally” activates patient natural killer cells using a monocyte-derived interferon alpha–dependent mechanism, according to preclinical data published in Leukemia.
Reovirus also enhances antibody-dependent cellular cytotoxicity – mediated killing of CLL cells in combination with anti-CD20 antibodies.
“Reovirus together with anti-CD20 antibodies represents a promising combination strategy for the treatment of CLL … and now warrants clinical evaluation,” wrote Christopher Parrish, Ph.D., of the Leeds (England) Institute of Cancer and Pathology and his colleagues (Leukemia. 2015;29:1799-1810. doi: 10.1038/leu.2015.88).Reovirus is a naturally occurring double-stranded RNA virus, and it exerts its effects against cancer cells by direct oncolysis and activation of antitumor immunity. The researchers investigated the efficacy of reovirus for the treatment of CLL, both as a direct cytotoxic agent and as an immunomodulator, using CLL cell lines and primary CLL cells from 24 patients.
Dr. Parrish and his team treated human CLL cells with live or UV-inactivated reovirus for 7 days. They assessed the ability of reovirus to stimulate immune-mediated killing of CLL using peripheral blood mononuclear cells from healthy volunteers and CLL patients. Reovirus activated natural killer (NK) cells from CLL patients, as well as stimulating innate antitumor immunity.
Rituximab, which is believed to act in part via NK cell–mediated antibody-dependent cellular cytotoxicity, was added to peripheral blood mononuclear cells that were treated with reovirus. Compared with rituximab alone, reovirus treatment significantly increased NK-cell CD107a/b degranulation. Reovirus was then paired with ofatumumab and GA101 to see if the effects observed with reovirus/rituximab could be translated to other anti-CD20 antibodies in which NK cells also play a role. The results were similar.
Absolute monocyte count and the type 1 interferon-alpha response could be used to predict the generation of antitumor innate immunity by reovirus. In cells from 24 CLL patients, about 75% responded to reovirus, with NK-cell activation. Further, NK-cell activation correlated with absolute monocyte count. The role of interferon-alpha is further supported by identification of an interferon gene signature within NK cells from reovirus-treated patients, the researchers said.
The study was supported by Yorkshire Cancer Research and Cancer Research UK. One of the investigators is an employee of Oncolytics Biotech and holds company stock and options. All the other authors declared no conflicts of interest.
Reovirus, a naturally occurring oncolytic virus, appears to exert direct cytotoxic activity against chronic lymphocytic leukemia (CLL) and “phenotypically and functionally” activates patient natural killer cells using a monocyte-derived interferon alpha–dependent mechanism, according to preclinical data published in Leukemia.
Reovirus also enhances antibody-dependent cellular cytotoxicity – mediated killing of CLL cells in combination with anti-CD20 antibodies.
“Reovirus together with anti-CD20 antibodies represents a promising combination strategy for the treatment of CLL … and now warrants clinical evaluation,” wrote Christopher Parrish, Ph.D., of the Leeds (England) Institute of Cancer and Pathology and his colleagues (Leukemia. 2015;29:1799-1810. doi: 10.1038/leu.2015.88).Reovirus is a naturally occurring double-stranded RNA virus, and it exerts its effects against cancer cells by direct oncolysis and activation of antitumor immunity. The researchers investigated the efficacy of reovirus for the treatment of CLL, both as a direct cytotoxic agent and as an immunomodulator, using CLL cell lines and primary CLL cells from 24 patients.
Dr. Parrish and his team treated human CLL cells with live or UV-inactivated reovirus for 7 days. They assessed the ability of reovirus to stimulate immune-mediated killing of CLL using peripheral blood mononuclear cells from healthy volunteers and CLL patients. Reovirus activated natural killer (NK) cells from CLL patients, as well as stimulating innate antitumor immunity.
Rituximab, which is believed to act in part via NK cell–mediated antibody-dependent cellular cytotoxicity, was added to peripheral blood mononuclear cells that were treated with reovirus. Compared with rituximab alone, reovirus treatment significantly increased NK-cell CD107a/b degranulation. Reovirus was then paired with ofatumumab and GA101 to see if the effects observed with reovirus/rituximab could be translated to other anti-CD20 antibodies in which NK cells also play a role. The results were similar.
Absolute monocyte count and the type 1 interferon-alpha response could be used to predict the generation of antitumor innate immunity by reovirus. In cells from 24 CLL patients, about 75% responded to reovirus, with NK-cell activation. Further, NK-cell activation correlated with absolute monocyte count. The role of interferon-alpha is further supported by identification of an interferon gene signature within NK cells from reovirus-treated patients, the researchers said.
The study was supported by Yorkshire Cancer Research and Cancer Research UK. One of the investigators is an employee of Oncolytics Biotech and holds company stock and options. All the other authors declared no conflicts of interest.
Reovirus, a naturally occurring oncolytic virus, appears to exert direct cytotoxic activity against chronic lymphocytic leukemia (CLL) and “phenotypically and functionally” activates patient natural killer cells using a monocyte-derived interferon alpha–dependent mechanism, according to preclinical data published in Leukemia.
Reovirus also enhances antibody-dependent cellular cytotoxicity – mediated killing of CLL cells in combination with anti-CD20 antibodies.
“Reovirus together with anti-CD20 antibodies represents a promising combination strategy for the treatment of CLL … and now warrants clinical evaluation,” wrote Christopher Parrish, Ph.D., of the Leeds (England) Institute of Cancer and Pathology and his colleagues (Leukemia. 2015;29:1799-1810. doi: 10.1038/leu.2015.88).Reovirus is a naturally occurring double-stranded RNA virus, and it exerts its effects against cancer cells by direct oncolysis and activation of antitumor immunity. The researchers investigated the efficacy of reovirus for the treatment of CLL, both as a direct cytotoxic agent and as an immunomodulator, using CLL cell lines and primary CLL cells from 24 patients.
Dr. Parrish and his team treated human CLL cells with live or UV-inactivated reovirus for 7 days. They assessed the ability of reovirus to stimulate immune-mediated killing of CLL using peripheral blood mononuclear cells from healthy volunteers and CLL patients. Reovirus activated natural killer (NK) cells from CLL patients, as well as stimulating innate antitumor immunity.
Rituximab, which is believed to act in part via NK cell–mediated antibody-dependent cellular cytotoxicity, was added to peripheral blood mononuclear cells that were treated with reovirus. Compared with rituximab alone, reovirus treatment significantly increased NK-cell CD107a/b degranulation. Reovirus was then paired with ofatumumab and GA101 to see if the effects observed with reovirus/rituximab could be translated to other anti-CD20 antibodies in which NK cells also play a role. The results were similar.
Absolute monocyte count and the type 1 interferon-alpha response could be used to predict the generation of antitumor innate immunity by reovirus. In cells from 24 CLL patients, about 75% responded to reovirus, with NK-cell activation. Further, NK-cell activation correlated with absolute monocyte count. The role of interferon-alpha is further supported by identification of an interferon gene signature within NK cells from reovirus-treated patients, the researchers said.
The study was supported by Yorkshire Cancer Research and Cancer Research UK. One of the investigators is an employee of Oncolytics Biotech and holds company stock and options. All the other authors declared no conflicts of interest.
FROM LEUKEMIA
Key clinical point: Reovirus, a naturally occurring oncolytic virus, in combination with anti-CD20 immunotherapy, may have benefit for the treatment of chronic lymphocytic leukemia.
Major finding: In cells from 24 CLL patients, about 75% responded to reovirus, with natural killer cell activation.
Data source: Preclinical trial that used human CLL lines and murine L929 cells.
Disclosures: The study was supported by Yorkshire Cancer Research and Cancer Research UK. One of the investigators is an employee of Oncolytics Biotech and holds company stock and options. All the other authors declared no conflicts of interest.
Mutation testing aids CML treatment decisions
Patients with Ph+ CML-CP (Philadelphia chromosome–positive chronic myeloid leukemia, chronic phase) who fail to achieve and maintain treatment response at key milestones should be considered for mutation screening, based on data from the DASISION trial.
Patients with mutations had poor outcomes and high rates of treatment discontinuation in an extended 4-year minimum follow-up of patients in the trial; 14 of 17 dasatinib-treated patients and 14 of 18 imatinib-treated patients with mutations discontinued treatment. The primary reason for treatment discontinuation was protocol-defined disease progression (dasatinib, n = 11; imatinib, n = 8); patients with mutations accounted for 61% of discontinuations on dasatinib (n = 11/18) and 42% on imatinib (n = 8/19).
“With the introduction of generic imatinib into the market in 2016, choosing the most appropriate second-line tyrosine-kinase inhibitor for patients, based on factors such as mutation status, will become increasingly important,” Dr. Tim Hughes of the South Australian Health and Medical Research Institute in Adelaide and his colleagues wrote. Having the option to choose the most suitable second-line therapy may ensure improved outcomes and decreased health care costs.
In the DASISION (Dasatinib vs. Imatinib Study in Treatment-Naive CML-CP) trial, all participants had newly diagnosed Ph+ CML-CP; they were treated with dasatinib (n = 259) or imatinib (n = 260) and followed for a minimum of 3 years (Leukemia. 2015 Sep;29[9]:1832-8). Dr. Hughes and his colleagues conducted a retrospective study of the patients who were potentially at a higher risk for developing mutations. This included patients on treatment who had at least one clinically relevant event – no confirmed complete cytogenetic response (cCCyR) within 12 months, no major molecular response (MMR) within 12 months; a fivefold increase in BCR-ABL1 transcript levels with loss of MMR; loss of CCyR – and/or who discontinued treatment for any reason.
Screening identified only a small number of patients with mutations (dasatinib, n = 17; imatinib, n = 18). Those on dasatinib had a narrower spectrum of mutations (4 sites for dasatinib vs. 12 sites for imatinib), fewer phosphate-binding loop mutations (1 mutation for dasatinib vs, 9 mutations for imatinib), and fewer multiple mutations (1 patient on dasatinib vs. 6 patients on imatinib).
However, patients on dasatinib had a greater occurrence of T315I mutations (11 patients on dasatinib vs. 0 patients on imatinib). The researchers hypothesized that this finding resulted from differences in competitive advantage between mutant clones. For example, P-loop mutations Y253F, E255K were found to have higher transformation potency and proliferation rates, compared with T315I, even in the absence of BCR-ABL1 inhibitors. If one assumes that imatinib has lower activity than dasatinib against these mutations, then mutant clones with select P-loop mutations might expand more rapidly than clones with the T315I mutation when exposed to imatinib.
Consistent with this idea, T315I is less common than all P-loop mutations in CML-CP patients with imatinib resistance. In addition, dasatinib suppresses P-loop mutations to a greater extent than does T315I; therefore, T315I may be able to develop during dasatinib treatment with relatively little competition from rapidly proliferating clones.
“Dasatinib, nilotinib, bosutinib, and ponatinib have enabled many patients, including those with mutations, to overcome imatinib resistance; however, each lack[s] efficacy against a small number of different leukemic clones, and all except ponatinib lack efficacy against T315I,” the researchers wrote.
The study was sponsored by Bristol-Myers Squibb. Dr. Hughes reported receiving honoraria and research funding from ARIAD, the maker of ponatinib; Bristol-Myers Squibb, the maker of dasatinib; and Novartis, the maker of imatinib.
Patients with Ph+ CML-CP (Philadelphia chromosome–positive chronic myeloid leukemia, chronic phase) who fail to achieve and maintain treatment response at key milestones should be considered for mutation screening, based on data from the DASISION trial.
Patients with mutations had poor outcomes and high rates of treatment discontinuation in an extended 4-year minimum follow-up of patients in the trial; 14 of 17 dasatinib-treated patients and 14 of 18 imatinib-treated patients with mutations discontinued treatment. The primary reason for treatment discontinuation was protocol-defined disease progression (dasatinib, n = 11; imatinib, n = 8); patients with mutations accounted for 61% of discontinuations on dasatinib (n = 11/18) and 42% on imatinib (n = 8/19).
“With the introduction of generic imatinib into the market in 2016, choosing the most appropriate second-line tyrosine-kinase inhibitor for patients, based on factors such as mutation status, will become increasingly important,” Dr. Tim Hughes of the South Australian Health and Medical Research Institute in Adelaide and his colleagues wrote. Having the option to choose the most suitable second-line therapy may ensure improved outcomes and decreased health care costs.
In the DASISION (Dasatinib vs. Imatinib Study in Treatment-Naive CML-CP) trial, all participants had newly diagnosed Ph+ CML-CP; they were treated with dasatinib (n = 259) or imatinib (n = 260) and followed for a minimum of 3 years (Leukemia. 2015 Sep;29[9]:1832-8). Dr. Hughes and his colleagues conducted a retrospective study of the patients who were potentially at a higher risk for developing mutations. This included patients on treatment who had at least one clinically relevant event – no confirmed complete cytogenetic response (cCCyR) within 12 months, no major molecular response (MMR) within 12 months; a fivefold increase in BCR-ABL1 transcript levels with loss of MMR; loss of CCyR – and/or who discontinued treatment for any reason.
Screening identified only a small number of patients with mutations (dasatinib, n = 17; imatinib, n = 18). Those on dasatinib had a narrower spectrum of mutations (4 sites for dasatinib vs. 12 sites for imatinib), fewer phosphate-binding loop mutations (1 mutation for dasatinib vs, 9 mutations for imatinib), and fewer multiple mutations (1 patient on dasatinib vs. 6 patients on imatinib).
However, patients on dasatinib had a greater occurrence of T315I mutations (11 patients on dasatinib vs. 0 patients on imatinib). The researchers hypothesized that this finding resulted from differences in competitive advantage between mutant clones. For example, P-loop mutations Y253F, E255K were found to have higher transformation potency and proliferation rates, compared with T315I, even in the absence of BCR-ABL1 inhibitors. If one assumes that imatinib has lower activity than dasatinib against these mutations, then mutant clones with select P-loop mutations might expand more rapidly than clones with the T315I mutation when exposed to imatinib.
Consistent with this idea, T315I is less common than all P-loop mutations in CML-CP patients with imatinib resistance. In addition, dasatinib suppresses P-loop mutations to a greater extent than does T315I; therefore, T315I may be able to develop during dasatinib treatment with relatively little competition from rapidly proliferating clones.
“Dasatinib, nilotinib, bosutinib, and ponatinib have enabled many patients, including those with mutations, to overcome imatinib resistance; however, each lack[s] efficacy against a small number of different leukemic clones, and all except ponatinib lack efficacy against T315I,” the researchers wrote.
The study was sponsored by Bristol-Myers Squibb. Dr. Hughes reported receiving honoraria and research funding from ARIAD, the maker of ponatinib; Bristol-Myers Squibb, the maker of dasatinib; and Novartis, the maker of imatinib.
Patients with Ph+ CML-CP (Philadelphia chromosome–positive chronic myeloid leukemia, chronic phase) who fail to achieve and maintain treatment response at key milestones should be considered for mutation screening, based on data from the DASISION trial.
Patients with mutations had poor outcomes and high rates of treatment discontinuation in an extended 4-year minimum follow-up of patients in the trial; 14 of 17 dasatinib-treated patients and 14 of 18 imatinib-treated patients with mutations discontinued treatment. The primary reason for treatment discontinuation was protocol-defined disease progression (dasatinib, n = 11; imatinib, n = 8); patients with mutations accounted for 61% of discontinuations on dasatinib (n = 11/18) and 42% on imatinib (n = 8/19).
“With the introduction of generic imatinib into the market in 2016, choosing the most appropriate second-line tyrosine-kinase inhibitor for patients, based on factors such as mutation status, will become increasingly important,” Dr. Tim Hughes of the South Australian Health and Medical Research Institute in Adelaide and his colleagues wrote. Having the option to choose the most suitable second-line therapy may ensure improved outcomes and decreased health care costs.
In the DASISION (Dasatinib vs. Imatinib Study in Treatment-Naive CML-CP) trial, all participants had newly diagnosed Ph+ CML-CP; they were treated with dasatinib (n = 259) or imatinib (n = 260) and followed for a minimum of 3 years (Leukemia. 2015 Sep;29[9]:1832-8). Dr. Hughes and his colleagues conducted a retrospective study of the patients who were potentially at a higher risk for developing mutations. This included patients on treatment who had at least one clinically relevant event – no confirmed complete cytogenetic response (cCCyR) within 12 months, no major molecular response (MMR) within 12 months; a fivefold increase in BCR-ABL1 transcript levels with loss of MMR; loss of CCyR – and/or who discontinued treatment for any reason.
Screening identified only a small number of patients with mutations (dasatinib, n = 17; imatinib, n = 18). Those on dasatinib had a narrower spectrum of mutations (4 sites for dasatinib vs. 12 sites for imatinib), fewer phosphate-binding loop mutations (1 mutation for dasatinib vs, 9 mutations for imatinib), and fewer multiple mutations (1 patient on dasatinib vs. 6 patients on imatinib).
However, patients on dasatinib had a greater occurrence of T315I mutations (11 patients on dasatinib vs. 0 patients on imatinib). The researchers hypothesized that this finding resulted from differences in competitive advantage between mutant clones. For example, P-loop mutations Y253F, E255K were found to have higher transformation potency and proliferation rates, compared with T315I, even in the absence of BCR-ABL1 inhibitors. If one assumes that imatinib has lower activity than dasatinib against these mutations, then mutant clones with select P-loop mutations might expand more rapidly than clones with the T315I mutation when exposed to imatinib.
Consistent with this idea, T315I is less common than all P-loop mutations in CML-CP patients with imatinib resistance. In addition, dasatinib suppresses P-loop mutations to a greater extent than does T315I; therefore, T315I may be able to develop during dasatinib treatment with relatively little competition from rapidly proliferating clones.
“Dasatinib, nilotinib, bosutinib, and ponatinib have enabled many patients, including those with mutations, to overcome imatinib resistance; however, each lack[s] efficacy against a small number of different leukemic clones, and all except ponatinib lack efficacy against T315I,” the researchers wrote.
The study was sponsored by Bristol-Myers Squibb. Dr. Hughes reported receiving honoraria and research funding from ARIAD, the maker of ponatinib; Bristol-Myers Squibb, the maker of dasatinib; and Novartis, the maker of imatinib.
FROM LEUKEMIA
Key clinical point:Mutation testing may aid treatment selection in patients with chronic myeloid leukemia (CML) when selecting an alternative therapy because of treatment failure.
Major finding: Patients with mutations accounted for 61% of discontinuations on dasatinib (n = 11/18) and 42% on imatinib (n = 8/19).
Data source: A retrospective analysis of the DASISION trial results of 259 patients treated with dasatinib and 260 treated with imatinib.
Disclosures: The study was sponsored by Bristol-Myers Squibb. Dr. Hughes reported receiving honoraria and research funding from ARIAD, the maker of ponatinib; Bristol-Myers Squibb, the maker of dasatinib; and Novartis, the maker of imatinib.
Whole-exome sequencing reveals important mutations in myeloma
The first comprehensive molecular analysis of patients in a clinical trial with myeloma has identified key copy number and structural abnormalities (CNSAs) and mutations that may help target high risk patients for more appropriate treatments, according to a new study published online in the Journal of Clinical Oncology.
“The detection of mutations can improve our ability to detect high-risk patients who experience relapse and die early, but who may benefit from specific therapeutic interventions,” said Dr. Brian Walker, from the Institute of Cancer Research, London, UK, and his colleagues (J Clin Oncol. 2015 Aug 17. doi:10.1200/JCO.2014.59.1503).
Samples were taken from 463 patients who were newly diagnosed with symptomatic myeloma and enrolled onto the National Cancer Research Institute Myeloma XI trial. This was a phase III, open-label trial in which patients were randomized to triplet immunomodulatory drug induction of either cyclophosphamide, thalidomide, and dexamethasone, or cyclophosphamide, lenalidomide, and dexamethasone.
Whole-exome sequencing of the patients identified 15 significantly mutated genes: IRF4, KRAS, NRAS, MAX, HIST1H1E, RB1, EGR1, TP53, TRAF3, FAM46C, DIS3, BRAF, LTB, CYLD, and FGFR3.
With the exception of NRAS and KRAS, all of the genes are mutated at a low percentage. The finding could be of importance, as it indicates that key pathways are deregulated, instead of mutations arising in single genes.
A number of the mutations appear to have an effect on survival. CCND1 mutations were associated with a negative impact on overall survival (2-year OS, 38%; [95% confidence interval, 14%-100%] vs. 80% [95% CI, 76%-84%]; P = .005). TP53 mutations and deletions were also associated with a significant negative impact on progression-free survival (PFS) and overall survival, as were ATM and ATR mutations.
In contrast, mutations in IRF4 had a positive impact on survival, with a trend toward an improvement in progression free survival (2-year PFS, 71%; [95% CI, 50%-100%] vs. 54% [95% CI, 49%-60%]; P = .09) and a significant impact on overall survival (2-year OS, 100% vs. 79% [95% CI, 75%-83%]; P = .05).
Aside from being prognostic for outcomes, some of these mutations are potential therapeutic targets. The deregulation of the RAS/MAPK pathway with the most common mutations being in NRAS and KRAS is a major therapeutic target, while the other targetable pathway is NF-kappa-B.
“Overall, we identified a set of potential actionable mutations comprising 309 targets applicable to 53% of patients,” the researchers wrote. “In the years to come, we foresee this to increase to 440 targets applicable to 62% of patients.”
The study was supported by several U.K. government grants, as well as funds from the National Institute of Health Biomedical Research Centre at the Royal Marsden Hospital. Coauthor Dr. Boyle was supported by the Fédération Française de Recherche sur le Myélome et les Gammapathies grant. Dr. Walker reports receiving honoraria from Celgene and Onyx Pharmaceuticals.
The first comprehensive molecular analysis of patients in a clinical trial with myeloma has identified key copy number and structural abnormalities (CNSAs) and mutations that may help target high risk patients for more appropriate treatments, according to a new study published online in the Journal of Clinical Oncology.
“The detection of mutations can improve our ability to detect high-risk patients who experience relapse and die early, but who may benefit from specific therapeutic interventions,” said Dr. Brian Walker, from the Institute of Cancer Research, London, UK, and his colleagues (J Clin Oncol. 2015 Aug 17. doi:10.1200/JCO.2014.59.1503).
Samples were taken from 463 patients who were newly diagnosed with symptomatic myeloma and enrolled onto the National Cancer Research Institute Myeloma XI trial. This was a phase III, open-label trial in which patients were randomized to triplet immunomodulatory drug induction of either cyclophosphamide, thalidomide, and dexamethasone, or cyclophosphamide, lenalidomide, and dexamethasone.
Whole-exome sequencing of the patients identified 15 significantly mutated genes: IRF4, KRAS, NRAS, MAX, HIST1H1E, RB1, EGR1, TP53, TRAF3, FAM46C, DIS3, BRAF, LTB, CYLD, and FGFR3.
With the exception of NRAS and KRAS, all of the genes are mutated at a low percentage. The finding could be of importance, as it indicates that key pathways are deregulated, instead of mutations arising in single genes.
A number of the mutations appear to have an effect on survival. CCND1 mutations were associated with a negative impact on overall survival (2-year OS, 38%; [95% confidence interval, 14%-100%] vs. 80% [95% CI, 76%-84%]; P = .005). TP53 mutations and deletions were also associated with a significant negative impact on progression-free survival (PFS) and overall survival, as were ATM and ATR mutations.
In contrast, mutations in IRF4 had a positive impact on survival, with a trend toward an improvement in progression free survival (2-year PFS, 71%; [95% CI, 50%-100%] vs. 54% [95% CI, 49%-60%]; P = .09) and a significant impact on overall survival (2-year OS, 100% vs. 79% [95% CI, 75%-83%]; P = .05).
Aside from being prognostic for outcomes, some of these mutations are potential therapeutic targets. The deregulation of the RAS/MAPK pathway with the most common mutations being in NRAS and KRAS is a major therapeutic target, while the other targetable pathway is NF-kappa-B.
“Overall, we identified a set of potential actionable mutations comprising 309 targets applicable to 53% of patients,” the researchers wrote. “In the years to come, we foresee this to increase to 440 targets applicable to 62% of patients.”
The study was supported by several U.K. government grants, as well as funds from the National Institute of Health Biomedical Research Centre at the Royal Marsden Hospital. Coauthor Dr. Boyle was supported by the Fédération Française de Recherche sur le Myélome et les Gammapathies grant. Dr. Walker reports receiving honoraria from Celgene and Onyx Pharmaceuticals.
The first comprehensive molecular analysis of patients in a clinical trial with myeloma has identified key copy number and structural abnormalities (CNSAs) and mutations that may help target high risk patients for more appropriate treatments, according to a new study published online in the Journal of Clinical Oncology.
“The detection of mutations can improve our ability to detect high-risk patients who experience relapse and die early, but who may benefit from specific therapeutic interventions,” said Dr. Brian Walker, from the Institute of Cancer Research, London, UK, and his colleagues (J Clin Oncol. 2015 Aug 17. doi:10.1200/JCO.2014.59.1503).
Samples were taken from 463 patients who were newly diagnosed with symptomatic myeloma and enrolled onto the National Cancer Research Institute Myeloma XI trial. This was a phase III, open-label trial in which patients were randomized to triplet immunomodulatory drug induction of either cyclophosphamide, thalidomide, and dexamethasone, or cyclophosphamide, lenalidomide, and dexamethasone.
Whole-exome sequencing of the patients identified 15 significantly mutated genes: IRF4, KRAS, NRAS, MAX, HIST1H1E, RB1, EGR1, TP53, TRAF3, FAM46C, DIS3, BRAF, LTB, CYLD, and FGFR3.
With the exception of NRAS and KRAS, all of the genes are mutated at a low percentage. The finding could be of importance, as it indicates that key pathways are deregulated, instead of mutations arising in single genes.
A number of the mutations appear to have an effect on survival. CCND1 mutations were associated with a negative impact on overall survival (2-year OS, 38%; [95% confidence interval, 14%-100%] vs. 80% [95% CI, 76%-84%]; P = .005). TP53 mutations and deletions were also associated with a significant negative impact on progression-free survival (PFS) and overall survival, as were ATM and ATR mutations.
In contrast, mutations in IRF4 had a positive impact on survival, with a trend toward an improvement in progression free survival (2-year PFS, 71%; [95% CI, 50%-100%] vs. 54% [95% CI, 49%-60%]; P = .09) and a significant impact on overall survival (2-year OS, 100% vs. 79% [95% CI, 75%-83%]; P = .05).
Aside from being prognostic for outcomes, some of these mutations are potential therapeutic targets. The deregulation of the RAS/MAPK pathway with the most common mutations being in NRAS and KRAS is a major therapeutic target, while the other targetable pathway is NF-kappa-B.
“Overall, we identified a set of potential actionable mutations comprising 309 targets applicable to 53% of patients,” the researchers wrote. “In the years to come, we foresee this to increase to 440 targets applicable to 62% of patients.”
The study was supported by several U.K. government grants, as well as funds from the National Institute of Health Biomedical Research Centre at the Royal Marsden Hospital. Coauthor Dr. Boyle was supported by the Fédération Française de Recherche sur le Myélome et les Gammapathies grant. Dr. Walker reports receiving honoraria from Celgene and Onyx Pharmaceuticals.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: A comprehensive analysis identified key copy number and structural abnormalities (CNSAs) and mutations in multiple myeloma.
Major finding: Fifteen significantly mutated genes were identified, primarily mutations in the RAS (43%) and nuclear factor kB pathway (17%).
Data source: Whole-exome sequencing for 463 patients who presented with myeloma and were enrolled onto the National Cancer Research Institute Myeloma XI trial.
Disclosures: The study was supported by several U.K. government grants, as well as funds from the National Institute of Health Biomedical Research Centre at the Royal Marsden Hospital, London. Coauthor Dr. Boyle was supported by the Fédération Française de Recherche sur le Myélome et les Gammapathies grant. Dr. Walker reports receiving honoraria from Celgene and Onyx Pharmaceuticals.