User login
Risks and remedies when your surgical patient is obese
The authors report no financial relationships relevant to this article.
The adverse consequences of obesity go far beyond aesthetic and psychosocial concerns. Patients who are markedly overweight face a real risk of developing severe health conditions—not just cardiac disease, diabetes mellitus, and hypertension, but also sleep apnea, venous thromboembolism, certain cancers (particularly breast and uterine), and biliary tract disease. Obesity also contributes to menstrual abnormalities and infertility and may complicate pregnancy.
Surgery in these patients poses a number of challenges. Not only does obesity frequently compromise the technical aspects of a procedure, it requires the surgeon to use certain measures in the preoperative and postoperative phases of management, such as counseling the patient extensively about the risks and potential complications she faces, initiating antibiotic prophylaxis, and ensuring early ambulation. These and other measures are especially important when uncontrolled, coexisting disease is present.
Not every obese patient is a significant surgical risk, so care should be individualized and use a team approach involving the gynecologist, anesthesiologist, primary care physician, and other appropriate subspecialists.
This article outlines the parameters of good surgical care in the obese patient, defined here as having a body mass index (BMI) of 30 kg/m2 or above, or 35 kg/m2 or above for morbid obesity. Whenever possible, we draw our recommendations from the published literature. In the absence of data, we base them on our surgical experience in the obese population.
Risks of surgery
It is imperative for the gynecologic surgeon to discuss the special risks of surgery with the obese patient well in advance of the operation and to formulate a systematic plan for evaluation, utilizing other members of the team when necessary. If the surgeon keeps the following risks in mind and is proactive, complications can be kept to a minimum.
Poor wound healing
Wound healing is a complex process involving several concurrent phases; an abnormality in any phase may impair healing. Those phases are:
- inflammatory phase, in which fluid and cells are released to clean the wound and prepare for the next phase of healing
- fibroplastic (proliferative) phase, in which fibroblasts accumulate and form collagen, the building block of connective tissue. This stage is marked by neovascularization and increased formation of granulation tissue
- wound contraction
- remodeling/maturation, in which new collagen is laid down as old collagen is broken down, resulting in scar formation.
- Obtain a chemistry panel: complete blood count, prothrombin time, activated partial thromboplastin time, and arterial blood gas studies. Type and cross-match if significant blood loss is expected
- Order a chest radiograph and electrocardiogram
- Test pulmonary function only if the patient has a history or suspected history of obstructive lung disease
- Order echocardiography only if the electrocardiogram or history suggests compromised cardiac function
- Instruct the patient on the use of incentive spirometry
- Prescribe a mechanical bowel-cleansing regimen if inadvertent injury is likely
- Notify anesthesiology and operating room personnel before the patient’s arrival
- Give 1 g of cefoxitin or another cephalosporin 60 minutes before the start of the procedure3
- Give 5,000 U of subcutaneous unfractionated heparin at least 2 hours before the start of surgery, and administer it every 8 hours until discharge.6 Alternative regimens: 5,000 U of dalteparin, a low-molecular-weight heparin, 12 hours before beginning the procedure and every 12 hours until discharge, or 40 mg of enoxaparin 12 hours before beginning surgery and every 12 hours until discharge
- Apply a pneumatic calf-compression apparatus in the operating room
Obese patients possess a thick layer of adipose tissue, which by its nature and location is minimally vascularized. This tissue essentially becomes dead space, an ideal medium for bacterial growth. Many obese patients also have diabetes mellitus, malignancy, or other comorbidity that further impairs healing.
As a result, obese patients are at increased risk of wound complications, breakdown, and subsequent dehiscence and evisceration. This translates into increased febrile morbidity, prolonged hospitalization, and higher cost.
What the data show. A number of studies have documented a higher incidence of wound complications in obese patients. In one retrospective review, Gallup1 observed an increased risk of wound complications in obese patients, but the incidence diminished after implementation of a protocol of meticulous cleansing, subcutaneous heparin, and modified incision and closure techniques. In a similar retrospective study of 300 obese patients, Pitkin2 reported wound complications among approximately one third of patients and postoperative fever among more than three quarters. Surgical-site infections are thought to occur in as many as 5% of patients.
Prophylaxis may be effective in some patients, but can be challenging. It entails meticulous skin cleansing and careful consideration of where the incision is placed, type of closure, use of a drain, and antibiotic administration.
Antibiotic prophylaxis is based on the theory that its presence in host tissues will alter natural defense mechanisms and kill bacteria that inoculate the wound. Because the window of efficacy is narrow, antibiotics should be administered shortly before the time of inoculation (ie, shortly before the time of incision, vaginal entry, etc.). Current guidelines suggest the use of broad-spectrum agents, including a cephalosporin, approximately 60 minutes before the incision. Redosing is recommended for procedures that last longer than 3 hours, as well as for those that involve significant blood loss (>1,500 mL).
For surgical procedures other than hysterectomy and laparotomy, prophylaxis may not be warranted.3 However, when the patient is markedly obese, many surgeons, including me (Dr. Perkins), sometimes opt to give antibiotics anyway—except for laparoscopic procedures—primarily for wound healing.
Compromised operative exposure
One of the main challenges of surgery in the obese is achieving adequate exposure; when it is inadequate, inadvertent injury may occur.
In addition to a thick abdominal wall composed largely of adipose tissue, these patients frequently have significant accumulations of fat in the mesenteries of the bowel, omentum, and pelvic peritoneum. These accumulations make it difficult to navigate around what becomes a narrow operative field.
Exposure can also be limited in vaginal surgery, because many obese women have very large thighs, buttocks, and accumulations of perineal fat.
Because exposure is a key element of successful surgery, modification of the procedure often becomes necessary—eg, focusing on a single area of the operative field at a time.
Use of a special retractor may help. A self-retaining retractor can be extremely useful. The Bookwalter retractor, first described in 1980, is a commonly used, table-fixed system that attaches to the side rail and can be assembled in minutes (FIGURE 1).4 The variety of rings and blades allows for excellent exposure. Although several complications have been associated with use of the Bookwalter retractor (primarily colon perforation and neuropathy5), they are infrequent and can be minimized by selecting the appropriate blade size and periodically repositioning the blades.
When this or other table-fixed retractors are unavailable, two Balfour retractors, placed at opposite poles of the field to obtain satisfactory exposure, may suffice. With a morbidly obese patient, multiple assistants may still be required to facilitate optimal exposure.
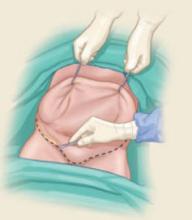
FIGURE 1 A tool to increase exposure
This self-retaining Bookwalter retractor is fixed to the surgical table and features a variety of rings and blades to facilitate exposure.
Thromboembolism
Venous thromboembolism is a major cause of mortality and morbidity in hospitalized patients, causing approximately 60,000 deaths every year.6 Obesity increases the risk of deep venous thrombosis in patients undergoing pelvic surgery. Because of their weight—and, often, coexisting conditions such as cardiorespiratory disease—many obese women are inactive or minimally active postoperatively, increasing the risk of thromboembolism, which remains heightened as long as 3 weeks after discharge. Older women are also at high risk, as are those with a malignancy.
Current guidelines call for the application of a pneumatic calf-compression device in the operating room, with removal after the patient is fully ambulatory. I (Dr. Perkins) also advocate simultaneous use of low-dose heparin, which should be given before surgery and continued until discharge.
Although the use of unfractionated heparin in conjunction with spinal or epidural anesthesia is not a major concern, the use of low-molecular-weight heparin warrants consultation with the anesthesiologist. Unfractionated heparin is preferred because it is metabolized much more rapidly than low-molecular weight heparin.7 The main concern with use of heparin in this setting (regardless of the patient’s weight) is spinal hematoma formation.
Inadvertent injury
Because exposure tends to be limited in obese patients, there is an ever-present risk of injury to bowel, bladder, ureter, and vascular structures. In obese women with a history of abdominal surgery, adhesions are likely, and the risk of bowel injury is increased. Similarly, in obese patients undergoing a laparoscopic procedure, many surface landmarks and vessels may be hard to discern.
Consider preoperative bowel preparation when there is a high risk of intestinal injury.8
Use a scalpel to incise the skin and delineate the area to be excised. That area typically consists of a large wedge of abdominal skin and subcutaneous fat.
Although the addition of panniculectomy to gynecologic surgery in the morbidly obese patient is a fairly recent strategy to increase exposure, the procedure itself has roots in the 19th century. In 1910, Howard Kelly of The Johns Hopkins Hospital reported a lipectomy that involved excision of a large wedge of abdominal skin and fat,21 although indications for that lipectomy appear to have been grounded in cosmesis and personal comfort for the patient.
Technique
Panniculectomy involves excision of a large portion of abdominal skin and subcutaneous fat down to, but not including, the rectus fascia, to gain much greater exposure to the lower abdominal cavity and pelvis.
Once the segment to be excised is delineated, it is mobilized using electrocautery to achieve meticulous hemostasis. After all surgical procedures are completed, the abdominal wall is closed in multiple layers, and drains are placed in the subcutaneous layer. Surgeons who have performed this procedure report significantly increased exposure and access to pelvic structures.
Once the skin is incised, the wedge is mobilized using electrocautery, down to, but not including, the rectus fascia.
Risks
The most important risk is impaired healing of the abdominal wound. One study of this procedure in patients on a gynecologic oncology service noted wound complications in 35% of patients, as well as significant blood loss (up to 1,800 mL in one case).22 Another study by Hopkins and associates,23 however, reported minimal blood loss and wound complications.
Caveats
The procedure requires an experienced surgeon, particularly if no plastic surgeon is readily available. Also, when counseling the patient about this procedure, it is important to emphasize that its primary indication is to maximize exposure; cosmetic benefits are secondary.
Impaired cardiorespiratory function
Pulmonary function typically is compromised in the markedly obese, with restrictive lung disease and reduced functional residual capacity. If the patient smokes or has chronic obstructive lung disease, her pulmonary function is compromised even further, and her condition should be relayed to the anesthesiologist.
In addition, many obese patients have preexisting heart disease or conditions such as hyperlipidemia that put them at risk for heart disease. When evaluating an obese surgical patient, also ask about less apparent disorders, such as sleep apnea, which, if not addressed, may have grave postoperative consequences.
Preoperative evaluation and preparation
Goal: Assess and minimize risks
This process begins in the office or clinic with a discussion with the patient of any concerns and risks. The importance of early mobilization and ambulation after surgery should be emphasized. Any patient with uncontrolled diabetes or hypertension should continue to be monitored by her primary care physician. A patient who has not seen a physician recently should be assessed by an internist to ensure that no conditions go undetected before surgery.
Routine testing to start, but additional assessment may be justified. An obese patient should undergo the same routine testing as a woman of normal weight, but further testing may be warranted for any coexisting disorder. Because the obese patient may have a restrictive lung pattern by virtue of her body habitus, pulmonary-function testing is unlikely to yield new information and is probably not indicated—unless she smokes or has a history of chronic obstructive pulmonary disease. In that case, tests will clarify the obstructive component and bronchodilator response and are useful in postoperative management. Measurement of arterial blood gases is useful, however, because levels reflect respiratory function on a day-to-day basis.
Additional tests of cardiac status probably are not indicated on the basis of obesity alone. However, if initial tests (eg, the electrocardiogram) and the history suggest compromised cardiac function, two-dimensional echocardiography should be performed to determine the ejection fraction. Any concerns regarding cardiac function should be discussed with the anesthesiologist and cardiologist.
Because compromised pulmonary function is likely, I (Dr. Perkins) instruct each patient on the use of incentive spirometry before she undergoes anesthesia so that she has realistic expectations about the postoperative course. I also administer heparin at least 2 hours before induction (8 hours before induction if unfractionated heparin is used).6
If a hysterectomy or prolonged laparotomy is planned, prophylactic antibiotics are recommended.3 Thigh-high compression stockings or a pneumatic calf-compression device should be applied upon arrival in the operating room.
Anesthesia-related issues
Anticipate challenges involving the airway
The anesthesiologist’s primary concern in regard to the obese patient is establishment and maintenance of an airway to promote oxygenation. In morbidly and extremely morbidly obese patients, anatomic factors such as large breasts; a short, thick neck; large tongue; decreased mobility of the cervical spine; limited mouth opening; and greater amount of adipose tissue in the face and cheeks can render mask ventilation and intubation extremely difficult or impossible. Decreased functional residual capacity and tidal volume in the range of closing capacity may lead to extremely rapid oxygen desaturation when the patient is apneic.9
If the patient is pregnant, factors such as excess adipose tissue in the face become even more pronounced and increase the potential for catastrophe.
Appreciate mechanical concerns
The morbidly obese patient may exceed the weight limit of the operating table. In addition, placing her in a steep Trendelenburg position or rotating her laterally may compromise the integrity of the bed.
Coexisting disease, such as sleep apnea and acid reflux disease, should also be kept in mind. Compromised respiratory mechanics (eg, restrictive lung pattern) may cause further deterioration and make mechanical ventilation more difficult.
It also may be hard to establish vascular access, necessitating central venous line placement and introducing its associated risks.
Keep the anesthesiologist in the loop
In the postoperative period, obese patients face a heightened risk of complications related to diminished pulmonary function, such as oxygen desaturation, hypoventilation, and airway obstruction, which may lead to atelectasis, pneumonia, and pulmonary edema.10,11 For these reasons, early consultation with the anesthesiologist is recommended, especially if the initial evaluation suggests potential difficulties in securing the airway. In turn, the anesthesiologist should understand that, in some obese patients, even establishing a surgical airway may be difficult. Regional anesthesia should be considered when feasible.
Antacids and drugs that increase gastric motility have proved to be useful in minimizing aspiration-related risks.12,13
Surgical technique
Begin abdominal procedures by carefully choosing an incision
Do not base the decision solely on the degree of obesity, but also consider any additional procedures that are planned, such as lymph-node sampling. A vertical incision does permit greater exposure than is afforded by a transverse incision, but in some cases the latter may be more appropriate—even if the patient is morbidly obese.
Do not place the incision below the panniculus, in the crease just above the suprapubic mound, though it may be tempting to do so when the panniculus is large and thick. This area is a warm, moist, anaerobic environment that promotes the proliferation of numerous micro-organisms, creating a bacterial cesspool. It is the worst place to make an incision.
If a transverse incision is selected, place caudal traction on the panniculus (which may be facilitated by applying two towel clips to the tissue fold), and incise through the fold at a point approximately three to four fingerbreadths above the symphysis (FIGURE 2).
If a midline incision is selected, a similar technique is appropriate, with downward traction applied to the panniculus and the incision begun at the lower pole of this fold up to the umbilicus—or through it and above, should more room be required.14
After incising the superficial fascia, greater exposure may be gained by incising the rectus sheath beneath the pannicular fold and extending it down to the symphysis. After entering the abdominal cavity, the surgeon may encounter a redundant, fat-laden layer of peritoneum. The edges of this tissue may be temporarily sutured to the edges of the skin incision to remove it from the operative field and obtain better visualization.
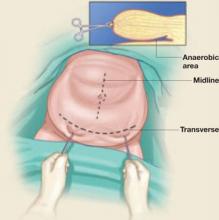
FIGURE 2 Incision placement can be counterintuitive
Avoid placing the skin incision beneath the panniculus, an anaerobic area ripe for infection. Instead, retract the panniculus caudally and incise the skin above the fold, as shown.
A few remedies can help when exposure is limited
Exposure is one of the most important elements of successful surgery, but it is often restricted when marked obesity is present. Fortunately, numerous adjuncts are available to address this problem, such as the table-fixed retractor systems described earlier in this article, or one or more of the following tactics:
- Do not try to expose the entire pelvic basin. One technique to ease exploration—especially when more than one procedure is planned—is to refrain from exposing the entire pelvic basin at one time. Instead, focus on obtaining adequate visualization in the immediate area and, once work in that area is finished, concentrate on the next.
- Use extra-long instruments in an extremely large patient, especially if she has a “deep” pelvis.
- Abbreviate the procedure, if possible. Because these cases are technically more difficult and frequently involve excessive blood loss, it may be wiser to perform an “incomplete” procedure, such as supracervical hysterectomy instead of total hysterectomy, depending on the indication.14
- Use a cell-saver blood-collection system if significant blood loss is anticipated. Also remember to give a second dose of prophylactic antibiotic.
Strategies for effective wound closure
The best method of abdominal wound closure has been a subject of debate among both gynecologic and general surgeons. In the obese patient, the key variables are the rather thick subcutaneous fat layer within the abdominal wall and the impact of intra-abdominal pressure on the incision.
What the data show. A number of studies, including one by Montz and colleagues,15 have demonstrated that the running mass-closure technique using delayed-absorbable or permanent suture is just as effective as interrupted suture placement (eg, Smead-Jones closure) but is faster, with less suture deposited in the wound.
The following considerations may also be helpful:
- Approximate the subcutaneous fascia? There has been some debate about whether the subcutaneous fascia must be approximated. My (Dr. Perkins) personal preference in morbidly obese patients is to place several interrupted sutures to obliterate much of the dead space, facilitate skin closure, and minimize tension on the wound; I have noted no significant increase in wound complications using this technique. Placement of a closed-suction drain (eg, Jackson Pratt, Hemovac) is a good alternative.
- Is a drain useful? Some have questioned whether use of a drain increases the likelihood of wound complications,16 but this concern is irrelevant because, in most—if not all—cases, the drainage tubing is exteriorized via a separate stab wound remote from the incision.
- Consider retention sutures. A morbidly obese patient may benefit from through-and-through retention sutures using 0 or #1 permanent material along with rubber bolsters to minimize cutting of the suture into the skin, especially if increased intra-abdominal pressure is likely (FIGURE 3).17 These sutures can be removed on the 10th to 12th postoperative day.
FIGURE 3 Minimize tension on the wound
A morbidly obese patient may benefit from through-and-through retention sutures along with rubber bolsters to minimize cutting of the suture into the skin.
Vaginal surgery does not increase complication rate in the obese
The vaginal approach can be extremely challenging in the morbidly obese patient, especially when hysterectomy is performed. Exposure is often compromised by the large folds about the thighs and buttocks, limiting access to the perineum and vaginal vault. If the patient also has a narrow, contracted pelvis, the difficulty is compounded. Because of these and other concerns about morbidity, many gynecologists hesitate to perform hysterectomy via the vaginal route when the patient is obese.
What the data show. Several studies have addressed these issues, including one by Pratt and Daikoku18 and another by Rafii and colleagues,19 both of which demonstrated that obese patients have a complication rate roughly equivalent to that observed in patients of normal weight, although obese patients have a greater decrease in hemoglobin level and a slightly higher incidence of postoperative fever.
Similarly, in a retrospective study, Pitkin20 found no significant difference between the complication rates of obese and nonobese patients.
Another argument for the self-retaining retractor. From a technical standpoint, achieving good exposure is the primary challenge of vaginal surgery and usually requires two or more assistants—who themselves have limited or no direct view of the field—who must stand for long periods. Again, a viable alternative is use of a self-retaining retractor. One in particular, the MiniOmni retractor, is a small, uncumbersome, table-fixed system that can be maneuvered so that vaginal and perineal structures are readily accessible.
Choice of stirrups is also relevant. Exposure can be affected by the type of stirrups used. “Candy cane” stirrups facilitate exposure more than fixed stirrups (eg, Allen stirrups) do. Regardless of the stirrups selected, however, it is important to avoid excessive or prolonged hip flexion, or nerve injury may result.
How to minimize postoperative complications
After surgery, an obese patient requires close and continuous monitoring to avert complications and detect any that occur. Consider the following measures:
- A stint in the intensive care unit. In the morbidly obese patient, massive fluid shift (eg, extensive blood loss, prolonged surgery with losses from the peritoneum, etc.) or concern about sleep apnea may justify close monitoring in an intensive care unit or similar setting—at least briefly. Later, as the patient recovers, sleep studies may indicate whether apnea is present.
- Document fluid intake and output, especially in the elderly and in women with cardiorespiratory disease.
- Give analgesics in an amount sufficient to control pain and minimize activity that might place excessive tension on the abdominal incision, but also allows the patient to remain alert enough to ambulate effectively and perform pulmonary toileting.
- Begin ambulation on the first postoperative day—or on the evening after surgery, if circumstances permit. This helps clear secretions from the respiratory tract, reduces the risk of thromboembolism, and speeds the return of normal bowel function. Hourly incentive spirometry is also recommended for the first few days after surgery.
- Continue heparin. In patients at moderate or high risk of thromboembolism, continue low-dose heparin until discharge or for 7 days, whichever comes first.
- Keep other physicians involved. If the patient has a significant comorbidity, such as cardiorespiratory disease or uncontrolled diabetes, she should remain under the care of her internist or other primary care provider.
- Closely monitor the surgical wound for early signs of infection, which include inflammation and collections of serous fluid, blood, pus, or a mixture of these. If retention sutures were placed, check them frequently to ensure that they are not cutting into the skin of the abdomen.
- Strongly recommend weight loss. At the time of the last postoperative visit, tell the patient in clear language that obesity is extremely bad for her health and strongly encourage her to lose weight under the supervision of her primary care provider. If she has no such provider, make the appropriate referral.
1. Gallup DG. Modifications of celiotomy techniques to decrease morbidity in obese gynecologic patients. Am J Obstet Gynecol. 1984;150:171-178.
2. Pitkin RM. Abdominal hysterectomy in obese women. Surg Gynecol Obstet. 1976;142:532-536.
3. Antibiotic prophylaxis for gynecologic procedures. ACOG Practice Bulletin No. 74. Washington, DC: American College of Obstetricians and Gynecologists; July 2006.
4. Bookwalter JR. A new table-fixed retractor. Surg Clin North Am. 1980;60:399-405.
5. Noldus J, Graefen M, Huland H. Major postoperative complications secondary to use of the Bookwalter self-retaining retractor. Urology. 2002;60:964-967.
6. Prevention of deep vein thrombosis and pulmonary embolism. ACOG Practice Bulletin No. 21. Washington, DC: American College of Obstetricians and Gynecologists; October 2000.
7. Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165-1177.
8. Perkins JD, Dent LL. Avoiding and repairing bowel injury in gynecologic surgery. OBG Management. 2004;16(8):15-28.
9. Cressey DM, Berthoud MC, Reilly CS. Effectiveness of continuous airway pressure to enhance preoxygenation in morbidly obese women. Anesthesia. 2001;56:670-689.
10. Jordan H, Perlow MD, Mark A, Morgan MD. Massive maternal obesity and perioperative cesarean morbidity. Am J Obstet Gynecol. 1994;170:560-565.
11. Hood DD, Dewan DN. Anesthetic and obstetric outcome in morbidly obese parturients. Anesthesiology. 1993;79:1210-1218.
12. James CF, Gibbs CP, Banner T. Postpartum perioperative risk of aspiration pneumonia. Anesthesiology. 1984;61:756-759.
13. Manchikanti L, Colliver JA, Marrero TC, Roush JR. Ranitidine and metoclopramide for prophylaxis of aspiration pneumonitis in elective surgery. Anesth Analg. 1984;63:903-910.
14. Morrow CP, Hernandez WL, Townsend DE, DiSaia PJ. Pelvic celiotomy in the obese patient. Am J Obstet Gynecol. 1977;127:335-339.
15. Montz FJ, Creasman WT, Eddy G, DiSaia PJ. Running mass closure of abdominal wounds using absorbable looped suture. J Gynecol Surg. 1991;7:107-110.
16. Ramsey PS, White AM, Guinn DA, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967-973.
17. Soisson AP, Olt G, Soper JT, Berchuck A, Rodriguez G, Clarke-Pearson DL. Prevention of superficial wound separation with subcutaneous retention sutures. Gynecol Oncol. 1993;51:330-334.
18. Pratt JH, Daikoku NH. Obesity and vaginal hysterectomy. J Reprod Med. 1990;35:945-949.
19. Rafii A, Samain E, Levardon M, Darai E, Deval B. Vaginal hysterectomy for benign disorders in obese women: a prospective study. Br J Obstet Gynaecol. 2005;111:223-227.
20. Pitkin RM. Vaginal hysterectomy in obese women. Obstet Gynecol. 1977;49:567-569.
21. Kelly HA. Excision of the fat of the abdominal wall—lipectomy. Surg Gynecol Obstet. 1910;10:229-231.
22. Wright JD, Rosenbush EJ, Powell MA, et al. Longterm outcome of women who undergo panniculectomy at the time of gynecologic surgery. Gynecol Oncol. 2006;102:86-91.
23. Hopkins MP, Shriner AM, Parker MG, Scott L. Panniculectomy at the time of gynecologic surgery in morbidly obese patients. Am J Obstet Gynecol. 2000;182:1502-1505.
The authors report no financial relationships relevant to this article.
The adverse consequences of obesity go far beyond aesthetic and psychosocial concerns. Patients who are markedly overweight face a real risk of developing severe health conditions—not just cardiac disease, diabetes mellitus, and hypertension, but also sleep apnea, venous thromboembolism, certain cancers (particularly breast and uterine), and biliary tract disease. Obesity also contributes to menstrual abnormalities and infertility and may complicate pregnancy.
Surgery in these patients poses a number of challenges. Not only does obesity frequently compromise the technical aspects of a procedure, it requires the surgeon to use certain measures in the preoperative and postoperative phases of management, such as counseling the patient extensively about the risks and potential complications she faces, initiating antibiotic prophylaxis, and ensuring early ambulation. These and other measures are especially important when uncontrolled, coexisting disease is present.
Not every obese patient is a significant surgical risk, so care should be individualized and use a team approach involving the gynecologist, anesthesiologist, primary care physician, and other appropriate subspecialists.
This article outlines the parameters of good surgical care in the obese patient, defined here as having a body mass index (BMI) of 30 kg/m2 or above, or 35 kg/m2 or above for morbid obesity. Whenever possible, we draw our recommendations from the published literature. In the absence of data, we base them on our surgical experience in the obese population.
Risks of surgery
It is imperative for the gynecologic surgeon to discuss the special risks of surgery with the obese patient well in advance of the operation and to formulate a systematic plan for evaluation, utilizing other members of the team when necessary. If the surgeon keeps the following risks in mind and is proactive, complications can be kept to a minimum.
Poor wound healing
Wound healing is a complex process involving several concurrent phases; an abnormality in any phase may impair healing. Those phases are:
- inflammatory phase, in which fluid and cells are released to clean the wound and prepare for the next phase of healing
- fibroplastic (proliferative) phase, in which fibroblasts accumulate and form collagen, the building block of connective tissue. This stage is marked by neovascularization and increased formation of granulation tissue
- wound contraction
- remodeling/maturation, in which new collagen is laid down as old collagen is broken down, resulting in scar formation.
- Obtain a chemistry panel: complete blood count, prothrombin time, activated partial thromboplastin time, and arterial blood gas studies. Type and cross-match if significant blood loss is expected
- Order a chest radiograph and electrocardiogram
- Test pulmonary function only if the patient has a history or suspected history of obstructive lung disease
- Order echocardiography only if the electrocardiogram or history suggests compromised cardiac function
- Instruct the patient on the use of incentive spirometry
- Prescribe a mechanical bowel-cleansing regimen if inadvertent injury is likely
- Notify anesthesiology and operating room personnel before the patient’s arrival
- Give 1 g of cefoxitin or another cephalosporin 60 minutes before the start of the procedure3
- Give 5,000 U of subcutaneous unfractionated heparin at least 2 hours before the start of surgery, and administer it every 8 hours until discharge.6 Alternative regimens: 5,000 U of dalteparin, a low-molecular-weight heparin, 12 hours before beginning the procedure and every 12 hours until discharge, or 40 mg of enoxaparin 12 hours before beginning surgery and every 12 hours until discharge
- Apply a pneumatic calf-compression apparatus in the operating room
Obese patients possess a thick layer of adipose tissue, which by its nature and location is minimally vascularized. This tissue essentially becomes dead space, an ideal medium for bacterial growth. Many obese patients also have diabetes mellitus, malignancy, or other comorbidity that further impairs healing.
As a result, obese patients are at increased risk of wound complications, breakdown, and subsequent dehiscence and evisceration. This translates into increased febrile morbidity, prolonged hospitalization, and higher cost.
What the data show. A number of studies have documented a higher incidence of wound complications in obese patients. In one retrospective review, Gallup1 observed an increased risk of wound complications in obese patients, but the incidence diminished after implementation of a protocol of meticulous cleansing, subcutaneous heparin, and modified incision and closure techniques. In a similar retrospective study of 300 obese patients, Pitkin2 reported wound complications among approximately one third of patients and postoperative fever among more than three quarters. Surgical-site infections are thought to occur in as many as 5% of patients.
Prophylaxis may be effective in some patients, but can be challenging. It entails meticulous skin cleansing and careful consideration of where the incision is placed, type of closure, use of a drain, and antibiotic administration.
Antibiotic prophylaxis is based on the theory that its presence in host tissues will alter natural defense mechanisms and kill bacteria that inoculate the wound. Because the window of efficacy is narrow, antibiotics should be administered shortly before the time of inoculation (ie, shortly before the time of incision, vaginal entry, etc.). Current guidelines suggest the use of broad-spectrum agents, including a cephalosporin, approximately 60 minutes before the incision. Redosing is recommended for procedures that last longer than 3 hours, as well as for those that involve significant blood loss (>1,500 mL).
For surgical procedures other than hysterectomy and laparotomy, prophylaxis may not be warranted.3 However, when the patient is markedly obese, many surgeons, including me (Dr. Perkins), sometimes opt to give antibiotics anyway—except for laparoscopic procedures—primarily for wound healing.
Compromised operative exposure
One of the main challenges of surgery in the obese is achieving adequate exposure; when it is inadequate, inadvertent injury may occur.
In addition to a thick abdominal wall composed largely of adipose tissue, these patients frequently have significant accumulations of fat in the mesenteries of the bowel, omentum, and pelvic peritoneum. These accumulations make it difficult to navigate around what becomes a narrow operative field.
Exposure can also be limited in vaginal surgery, because many obese women have very large thighs, buttocks, and accumulations of perineal fat.
Because exposure is a key element of successful surgery, modification of the procedure often becomes necessary—eg, focusing on a single area of the operative field at a time.
Use of a special retractor may help. A self-retaining retractor can be extremely useful. The Bookwalter retractor, first described in 1980, is a commonly used, table-fixed system that attaches to the side rail and can be assembled in minutes (FIGURE 1).4 The variety of rings and blades allows for excellent exposure. Although several complications have been associated with use of the Bookwalter retractor (primarily colon perforation and neuropathy5), they are infrequent and can be minimized by selecting the appropriate blade size and periodically repositioning the blades.
When this or other table-fixed retractors are unavailable, two Balfour retractors, placed at opposite poles of the field to obtain satisfactory exposure, may suffice. With a morbidly obese patient, multiple assistants may still be required to facilitate optimal exposure.
FIGURE 1 A tool to increase exposure
This self-retaining Bookwalter retractor is fixed to the surgical table and features a variety of rings and blades to facilitate exposure.
Thromboembolism
Venous thromboembolism is a major cause of mortality and morbidity in hospitalized patients, causing approximately 60,000 deaths every year.6 Obesity increases the risk of deep venous thrombosis in patients undergoing pelvic surgery. Because of their weight—and, often, coexisting conditions such as cardiorespiratory disease—many obese women are inactive or minimally active postoperatively, increasing the risk of thromboembolism, which remains heightened as long as 3 weeks after discharge. Older women are also at high risk, as are those with a malignancy.
Current guidelines call for the application of a pneumatic calf-compression device in the operating room, with removal after the patient is fully ambulatory. I (Dr. Perkins) also advocate simultaneous use of low-dose heparin, which should be given before surgery and continued until discharge.
Although the use of unfractionated heparin in conjunction with spinal or epidural anesthesia is not a major concern, the use of low-molecular-weight heparin warrants consultation with the anesthesiologist. Unfractionated heparin is preferred because it is metabolized much more rapidly than low-molecular weight heparin.7 The main concern with use of heparin in this setting (regardless of the patient’s weight) is spinal hematoma formation.
Inadvertent injury
Because exposure tends to be limited in obese patients, there is an ever-present risk of injury to bowel, bladder, ureter, and vascular structures. In obese women with a history of abdominal surgery, adhesions are likely, and the risk of bowel injury is increased. Similarly, in obese patients undergoing a laparoscopic procedure, many surface landmarks and vessels may be hard to discern.
Consider preoperative bowel preparation when there is a high risk of intestinal injury.8
Use a scalpel to incise the skin and delineate the area to be excised. That area typically consists of a large wedge of abdominal skin and subcutaneous fat.
Although the addition of panniculectomy to gynecologic surgery in the morbidly obese patient is a fairly recent strategy to increase exposure, the procedure itself has roots in the 19th century. In 1910, Howard Kelly of The Johns Hopkins Hospital reported a lipectomy that involved excision of a large wedge of abdominal skin and fat,21 although indications for that lipectomy appear to have been grounded in cosmesis and personal comfort for the patient.
Technique
Panniculectomy involves excision of a large portion of abdominal skin and subcutaneous fat down to, but not including, the rectus fascia, to gain much greater exposure to the lower abdominal cavity and pelvis.
Once the segment to be excised is delineated, it is mobilized using electrocautery to achieve meticulous hemostasis. After all surgical procedures are completed, the abdominal wall is closed in multiple layers, and drains are placed in the subcutaneous layer. Surgeons who have performed this procedure report significantly increased exposure and access to pelvic structures.
Once the skin is incised, the wedge is mobilized using electrocautery, down to, but not including, the rectus fascia.
Risks
The most important risk is impaired healing of the abdominal wound. One study of this procedure in patients on a gynecologic oncology service noted wound complications in 35% of patients, as well as significant blood loss (up to 1,800 mL in one case).22 Another study by Hopkins and associates,23 however, reported minimal blood loss and wound complications.
Caveats
The procedure requires an experienced surgeon, particularly if no plastic surgeon is readily available. Also, when counseling the patient about this procedure, it is important to emphasize that its primary indication is to maximize exposure; cosmetic benefits are secondary.
Impaired cardiorespiratory function
Pulmonary function typically is compromised in the markedly obese, with restrictive lung disease and reduced functional residual capacity. If the patient smokes or has chronic obstructive lung disease, her pulmonary function is compromised even further, and her condition should be relayed to the anesthesiologist.
In addition, many obese patients have preexisting heart disease or conditions such as hyperlipidemia that put them at risk for heart disease. When evaluating an obese surgical patient, also ask about less apparent disorders, such as sleep apnea, which, if not addressed, may have grave postoperative consequences.
Preoperative evaluation and preparation
Goal: Assess and minimize risks
This process begins in the office or clinic with a discussion with the patient of any concerns and risks. The importance of early mobilization and ambulation after surgery should be emphasized. Any patient with uncontrolled diabetes or hypertension should continue to be monitored by her primary care physician. A patient who has not seen a physician recently should be assessed by an internist to ensure that no conditions go undetected before surgery.
Routine testing to start, but additional assessment may be justified. An obese patient should undergo the same routine testing as a woman of normal weight, but further testing may be warranted for any coexisting disorder. Because the obese patient may have a restrictive lung pattern by virtue of her body habitus, pulmonary-function testing is unlikely to yield new information and is probably not indicated—unless she smokes or has a history of chronic obstructive pulmonary disease. In that case, tests will clarify the obstructive component and bronchodilator response and are useful in postoperative management. Measurement of arterial blood gases is useful, however, because levels reflect respiratory function on a day-to-day basis.
Additional tests of cardiac status probably are not indicated on the basis of obesity alone. However, if initial tests (eg, the electrocardiogram) and the history suggest compromised cardiac function, two-dimensional echocardiography should be performed to determine the ejection fraction. Any concerns regarding cardiac function should be discussed with the anesthesiologist and cardiologist.
Because compromised pulmonary function is likely, I (Dr. Perkins) instruct each patient on the use of incentive spirometry before she undergoes anesthesia so that she has realistic expectations about the postoperative course. I also administer heparin at least 2 hours before induction (8 hours before induction if unfractionated heparin is used).6
If a hysterectomy or prolonged laparotomy is planned, prophylactic antibiotics are recommended.3 Thigh-high compression stockings or a pneumatic calf-compression device should be applied upon arrival in the operating room.
Anesthesia-related issues
Anticipate challenges involving the airway
The anesthesiologist’s primary concern in regard to the obese patient is establishment and maintenance of an airway to promote oxygenation. In morbidly and extremely morbidly obese patients, anatomic factors such as large breasts; a short, thick neck; large tongue; decreased mobility of the cervical spine; limited mouth opening; and greater amount of adipose tissue in the face and cheeks can render mask ventilation and intubation extremely difficult or impossible. Decreased functional residual capacity and tidal volume in the range of closing capacity may lead to extremely rapid oxygen desaturation when the patient is apneic.9
If the patient is pregnant, factors such as excess adipose tissue in the face become even more pronounced and increase the potential for catastrophe.
Appreciate mechanical concerns
The morbidly obese patient may exceed the weight limit of the operating table. In addition, placing her in a steep Trendelenburg position or rotating her laterally may compromise the integrity of the bed.
Coexisting disease, such as sleep apnea and acid reflux disease, should also be kept in mind. Compromised respiratory mechanics (eg, restrictive lung pattern) may cause further deterioration and make mechanical ventilation more difficult.
It also may be hard to establish vascular access, necessitating central venous line placement and introducing its associated risks.
Keep the anesthesiologist in the loop
In the postoperative period, obese patients face a heightened risk of complications related to diminished pulmonary function, such as oxygen desaturation, hypoventilation, and airway obstruction, which may lead to atelectasis, pneumonia, and pulmonary edema.10,11 For these reasons, early consultation with the anesthesiologist is recommended, especially if the initial evaluation suggests potential difficulties in securing the airway. In turn, the anesthesiologist should understand that, in some obese patients, even establishing a surgical airway may be difficult. Regional anesthesia should be considered when feasible.
Antacids and drugs that increase gastric motility have proved to be useful in minimizing aspiration-related risks.12,13
Surgical technique
Begin abdominal procedures by carefully choosing an incision
Do not base the decision solely on the degree of obesity, but also consider any additional procedures that are planned, such as lymph-node sampling. A vertical incision does permit greater exposure than is afforded by a transverse incision, but in some cases the latter may be more appropriate—even if the patient is morbidly obese.
Do not place the incision below the panniculus, in the crease just above the suprapubic mound, though it may be tempting to do so when the panniculus is large and thick. This area is a warm, moist, anaerobic environment that promotes the proliferation of numerous micro-organisms, creating a bacterial cesspool. It is the worst place to make an incision.
If a transverse incision is selected, place caudal traction on the panniculus (which may be facilitated by applying two towel clips to the tissue fold), and incise through the fold at a point approximately three to four fingerbreadths above the symphysis (FIGURE 2).
If a midline incision is selected, a similar technique is appropriate, with downward traction applied to the panniculus and the incision begun at the lower pole of this fold up to the umbilicus—or through it and above, should more room be required.14
After incising the superficial fascia, greater exposure may be gained by incising the rectus sheath beneath the pannicular fold and extending it down to the symphysis. After entering the abdominal cavity, the surgeon may encounter a redundant, fat-laden layer of peritoneum. The edges of this tissue may be temporarily sutured to the edges of the skin incision to remove it from the operative field and obtain better visualization.
FIGURE 2 Incision placement can be counterintuitive
Avoid placing the skin incision beneath the panniculus, an anaerobic area ripe for infection. Instead, retract the panniculus caudally and incise the skin above the fold, as shown.
A few remedies can help when exposure is limited
Exposure is one of the most important elements of successful surgery, but it is often restricted when marked obesity is present. Fortunately, numerous adjuncts are available to address this problem, such as the table-fixed retractor systems described earlier in this article, or one or more of the following tactics:
- Do not try to expose the entire pelvic basin. One technique to ease exploration—especially when more than one procedure is planned—is to refrain from exposing the entire pelvic basin at one time. Instead, focus on obtaining adequate visualization in the immediate area and, once work in that area is finished, concentrate on the next.
- Use extra-long instruments in an extremely large patient, especially if she has a “deep” pelvis.
- Abbreviate the procedure, if possible. Because these cases are technically more difficult and frequently involve excessive blood loss, it may be wiser to perform an “incomplete” procedure, such as supracervical hysterectomy instead of total hysterectomy, depending on the indication.14
- Use a cell-saver blood-collection system if significant blood loss is anticipated. Also remember to give a second dose of prophylactic antibiotic.
Strategies for effective wound closure
The best method of abdominal wound closure has been a subject of debate among both gynecologic and general surgeons. In the obese patient, the key variables are the rather thick subcutaneous fat layer within the abdominal wall and the impact of intra-abdominal pressure on the incision.
What the data show. A number of studies, including one by Montz and colleagues,15 have demonstrated that the running mass-closure technique using delayed-absorbable or permanent suture is just as effective as interrupted suture placement (eg, Smead-Jones closure) but is faster, with less suture deposited in the wound.
The following considerations may also be helpful:
- Approximate the subcutaneous fascia? There has been some debate about whether the subcutaneous fascia must be approximated. My (Dr. Perkins) personal preference in morbidly obese patients is to place several interrupted sutures to obliterate much of the dead space, facilitate skin closure, and minimize tension on the wound; I have noted no significant increase in wound complications using this technique. Placement of a closed-suction drain (eg, Jackson Pratt, Hemovac) is a good alternative.
- Is a drain useful? Some have questioned whether use of a drain increases the likelihood of wound complications,16 but this concern is irrelevant because, in most—if not all—cases, the drainage tubing is exteriorized via a separate stab wound remote from the incision.
- Consider retention sutures. A morbidly obese patient may benefit from through-and-through retention sutures using 0 or #1 permanent material along with rubber bolsters to minimize cutting of the suture into the skin, especially if increased intra-abdominal pressure is likely (FIGURE 3).17 These sutures can be removed on the 10th to 12th postoperative day.
FIGURE 3 Minimize tension on the wound
A morbidly obese patient may benefit from through-and-through retention sutures along with rubber bolsters to minimize cutting of the suture into the skin.
Vaginal surgery does not increase complication rate in the obese
The vaginal approach can be extremely challenging in the morbidly obese patient, especially when hysterectomy is performed. Exposure is often compromised by the large folds about the thighs and buttocks, limiting access to the perineum and vaginal vault. If the patient also has a narrow, contracted pelvis, the difficulty is compounded. Because of these and other concerns about morbidity, many gynecologists hesitate to perform hysterectomy via the vaginal route when the patient is obese.
What the data show. Several studies have addressed these issues, including one by Pratt and Daikoku18 and another by Rafii and colleagues,19 both of which demonstrated that obese patients have a complication rate roughly equivalent to that observed in patients of normal weight, although obese patients have a greater decrease in hemoglobin level and a slightly higher incidence of postoperative fever.
Similarly, in a retrospective study, Pitkin20 found no significant difference between the complication rates of obese and nonobese patients.
Another argument for the self-retaining retractor. From a technical standpoint, achieving good exposure is the primary challenge of vaginal surgery and usually requires two or more assistants—who themselves have limited or no direct view of the field—who must stand for long periods. Again, a viable alternative is use of a self-retaining retractor. One in particular, the MiniOmni retractor, is a small, uncumbersome, table-fixed system that can be maneuvered so that vaginal and perineal structures are readily accessible.
Choice of stirrups is also relevant. Exposure can be affected by the type of stirrups used. “Candy cane” stirrups facilitate exposure more than fixed stirrups (eg, Allen stirrups) do. Regardless of the stirrups selected, however, it is important to avoid excessive or prolonged hip flexion, or nerve injury may result.
How to minimize postoperative complications
After surgery, an obese patient requires close and continuous monitoring to avert complications and detect any that occur. Consider the following measures:
- A stint in the intensive care unit. In the morbidly obese patient, massive fluid shift (eg, extensive blood loss, prolonged surgery with losses from the peritoneum, etc.) or concern about sleep apnea may justify close monitoring in an intensive care unit or similar setting—at least briefly. Later, as the patient recovers, sleep studies may indicate whether apnea is present.
- Document fluid intake and output, especially in the elderly and in women with cardiorespiratory disease.
- Give analgesics in an amount sufficient to control pain and minimize activity that might place excessive tension on the abdominal incision, but also allows the patient to remain alert enough to ambulate effectively and perform pulmonary toileting.
- Begin ambulation on the first postoperative day—or on the evening after surgery, if circumstances permit. This helps clear secretions from the respiratory tract, reduces the risk of thromboembolism, and speeds the return of normal bowel function. Hourly incentive spirometry is also recommended for the first few days after surgery.
- Continue heparin. In patients at moderate or high risk of thromboembolism, continue low-dose heparin until discharge or for 7 days, whichever comes first.
- Keep other physicians involved. If the patient has a significant comorbidity, such as cardiorespiratory disease or uncontrolled diabetes, she should remain under the care of her internist or other primary care provider.
- Closely monitor the surgical wound for early signs of infection, which include inflammation and collections of serous fluid, blood, pus, or a mixture of these. If retention sutures were placed, check them frequently to ensure that they are not cutting into the skin of the abdomen.
- Strongly recommend weight loss. At the time of the last postoperative visit, tell the patient in clear language that obesity is extremely bad for her health and strongly encourage her to lose weight under the supervision of her primary care provider. If she has no such provider, make the appropriate referral.
The authors report no financial relationships relevant to this article.
The adverse consequences of obesity go far beyond aesthetic and psychosocial concerns. Patients who are markedly overweight face a real risk of developing severe health conditions—not just cardiac disease, diabetes mellitus, and hypertension, but also sleep apnea, venous thromboembolism, certain cancers (particularly breast and uterine), and biliary tract disease. Obesity also contributes to menstrual abnormalities and infertility and may complicate pregnancy.
Surgery in these patients poses a number of challenges. Not only does obesity frequently compromise the technical aspects of a procedure, it requires the surgeon to use certain measures in the preoperative and postoperative phases of management, such as counseling the patient extensively about the risks and potential complications she faces, initiating antibiotic prophylaxis, and ensuring early ambulation. These and other measures are especially important when uncontrolled, coexisting disease is present.
Not every obese patient is a significant surgical risk, so care should be individualized and use a team approach involving the gynecologist, anesthesiologist, primary care physician, and other appropriate subspecialists.
This article outlines the parameters of good surgical care in the obese patient, defined here as having a body mass index (BMI) of 30 kg/m2 or above, or 35 kg/m2 or above for morbid obesity. Whenever possible, we draw our recommendations from the published literature. In the absence of data, we base them on our surgical experience in the obese population.
Risks of surgery
It is imperative for the gynecologic surgeon to discuss the special risks of surgery with the obese patient well in advance of the operation and to formulate a systematic plan for evaluation, utilizing other members of the team when necessary. If the surgeon keeps the following risks in mind and is proactive, complications can be kept to a minimum.
Poor wound healing
Wound healing is a complex process involving several concurrent phases; an abnormality in any phase may impair healing. Those phases are:
- inflammatory phase, in which fluid and cells are released to clean the wound and prepare for the next phase of healing
- fibroplastic (proliferative) phase, in which fibroblasts accumulate and form collagen, the building block of connective tissue. This stage is marked by neovascularization and increased formation of granulation tissue
- wound contraction
- remodeling/maturation, in which new collagen is laid down as old collagen is broken down, resulting in scar formation.
- Obtain a chemistry panel: complete blood count, prothrombin time, activated partial thromboplastin time, and arterial blood gas studies. Type and cross-match if significant blood loss is expected
- Order a chest radiograph and electrocardiogram
- Test pulmonary function only if the patient has a history or suspected history of obstructive lung disease
- Order echocardiography only if the electrocardiogram or history suggests compromised cardiac function
- Instruct the patient on the use of incentive spirometry
- Prescribe a mechanical bowel-cleansing regimen if inadvertent injury is likely
- Notify anesthesiology and operating room personnel before the patient’s arrival
- Give 1 g of cefoxitin or another cephalosporin 60 minutes before the start of the procedure3
- Give 5,000 U of subcutaneous unfractionated heparin at least 2 hours before the start of surgery, and administer it every 8 hours until discharge.6 Alternative regimens: 5,000 U of dalteparin, a low-molecular-weight heparin, 12 hours before beginning the procedure and every 12 hours until discharge, or 40 mg of enoxaparin 12 hours before beginning surgery and every 12 hours until discharge
- Apply a pneumatic calf-compression apparatus in the operating room
Obese patients possess a thick layer of adipose tissue, which by its nature and location is minimally vascularized. This tissue essentially becomes dead space, an ideal medium for bacterial growth. Many obese patients also have diabetes mellitus, malignancy, or other comorbidity that further impairs healing.
As a result, obese patients are at increased risk of wound complications, breakdown, and subsequent dehiscence and evisceration. This translates into increased febrile morbidity, prolonged hospitalization, and higher cost.
What the data show. A number of studies have documented a higher incidence of wound complications in obese patients. In one retrospective review, Gallup1 observed an increased risk of wound complications in obese patients, but the incidence diminished after implementation of a protocol of meticulous cleansing, subcutaneous heparin, and modified incision and closure techniques. In a similar retrospective study of 300 obese patients, Pitkin2 reported wound complications among approximately one third of patients and postoperative fever among more than three quarters. Surgical-site infections are thought to occur in as many as 5% of patients.
Prophylaxis may be effective in some patients, but can be challenging. It entails meticulous skin cleansing and careful consideration of where the incision is placed, type of closure, use of a drain, and antibiotic administration.
Antibiotic prophylaxis is based on the theory that its presence in host tissues will alter natural defense mechanisms and kill bacteria that inoculate the wound. Because the window of efficacy is narrow, antibiotics should be administered shortly before the time of inoculation (ie, shortly before the time of incision, vaginal entry, etc.). Current guidelines suggest the use of broad-spectrum agents, including a cephalosporin, approximately 60 minutes before the incision. Redosing is recommended for procedures that last longer than 3 hours, as well as for those that involve significant blood loss (>1,500 mL).
For surgical procedures other than hysterectomy and laparotomy, prophylaxis may not be warranted.3 However, when the patient is markedly obese, many surgeons, including me (Dr. Perkins), sometimes opt to give antibiotics anyway—except for laparoscopic procedures—primarily for wound healing.
Compromised operative exposure
One of the main challenges of surgery in the obese is achieving adequate exposure; when it is inadequate, inadvertent injury may occur.
In addition to a thick abdominal wall composed largely of adipose tissue, these patients frequently have significant accumulations of fat in the mesenteries of the bowel, omentum, and pelvic peritoneum. These accumulations make it difficult to navigate around what becomes a narrow operative field.
Exposure can also be limited in vaginal surgery, because many obese women have very large thighs, buttocks, and accumulations of perineal fat.
Because exposure is a key element of successful surgery, modification of the procedure often becomes necessary—eg, focusing on a single area of the operative field at a time.
Use of a special retractor may help. A self-retaining retractor can be extremely useful. The Bookwalter retractor, first described in 1980, is a commonly used, table-fixed system that attaches to the side rail and can be assembled in minutes (FIGURE 1).4 The variety of rings and blades allows for excellent exposure. Although several complications have been associated with use of the Bookwalter retractor (primarily colon perforation and neuropathy5), they are infrequent and can be minimized by selecting the appropriate blade size and periodically repositioning the blades.
When this or other table-fixed retractors are unavailable, two Balfour retractors, placed at opposite poles of the field to obtain satisfactory exposure, may suffice. With a morbidly obese patient, multiple assistants may still be required to facilitate optimal exposure.
FIGURE 1 A tool to increase exposure
This self-retaining Bookwalter retractor is fixed to the surgical table and features a variety of rings and blades to facilitate exposure.
Thromboembolism
Venous thromboembolism is a major cause of mortality and morbidity in hospitalized patients, causing approximately 60,000 deaths every year.6 Obesity increases the risk of deep venous thrombosis in patients undergoing pelvic surgery. Because of their weight—and, often, coexisting conditions such as cardiorespiratory disease—many obese women are inactive or minimally active postoperatively, increasing the risk of thromboembolism, which remains heightened as long as 3 weeks after discharge. Older women are also at high risk, as are those with a malignancy.
Current guidelines call for the application of a pneumatic calf-compression device in the operating room, with removal after the patient is fully ambulatory. I (Dr. Perkins) also advocate simultaneous use of low-dose heparin, which should be given before surgery and continued until discharge.
Although the use of unfractionated heparin in conjunction with spinal or epidural anesthesia is not a major concern, the use of low-molecular-weight heparin warrants consultation with the anesthesiologist. Unfractionated heparin is preferred because it is metabolized much more rapidly than low-molecular weight heparin.7 The main concern with use of heparin in this setting (regardless of the patient’s weight) is spinal hematoma formation.
Inadvertent injury
Because exposure tends to be limited in obese patients, there is an ever-present risk of injury to bowel, bladder, ureter, and vascular structures. In obese women with a history of abdominal surgery, adhesions are likely, and the risk of bowel injury is increased. Similarly, in obese patients undergoing a laparoscopic procedure, many surface landmarks and vessels may be hard to discern.
Consider preoperative bowel preparation when there is a high risk of intestinal injury.8
Use a scalpel to incise the skin and delineate the area to be excised. That area typically consists of a large wedge of abdominal skin and subcutaneous fat.
Although the addition of panniculectomy to gynecologic surgery in the morbidly obese patient is a fairly recent strategy to increase exposure, the procedure itself has roots in the 19th century. In 1910, Howard Kelly of The Johns Hopkins Hospital reported a lipectomy that involved excision of a large wedge of abdominal skin and fat,21 although indications for that lipectomy appear to have been grounded in cosmesis and personal comfort for the patient.
Technique
Panniculectomy involves excision of a large portion of abdominal skin and subcutaneous fat down to, but not including, the rectus fascia, to gain much greater exposure to the lower abdominal cavity and pelvis.
Once the segment to be excised is delineated, it is mobilized using electrocautery to achieve meticulous hemostasis. After all surgical procedures are completed, the abdominal wall is closed in multiple layers, and drains are placed in the subcutaneous layer. Surgeons who have performed this procedure report significantly increased exposure and access to pelvic structures.
Once the skin is incised, the wedge is mobilized using electrocautery, down to, but not including, the rectus fascia.
Risks
The most important risk is impaired healing of the abdominal wound. One study of this procedure in patients on a gynecologic oncology service noted wound complications in 35% of patients, as well as significant blood loss (up to 1,800 mL in one case).22 Another study by Hopkins and associates,23 however, reported minimal blood loss and wound complications.
Caveats
The procedure requires an experienced surgeon, particularly if no plastic surgeon is readily available. Also, when counseling the patient about this procedure, it is important to emphasize that its primary indication is to maximize exposure; cosmetic benefits are secondary.
Impaired cardiorespiratory function
Pulmonary function typically is compromised in the markedly obese, with restrictive lung disease and reduced functional residual capacity. If the patient smokes or has chronic obstructive lung disease, her pulmonary function is compromised even further, and her condition should be relayed to the anesthesiologist.
In addition, many obese patients have preexisting heart disease or conditions such as hyperlipidemia that put them at risk for heart disease. When evaluating an obese surgical patient, also ask about less apparent disorders, such as sleep apnea, which, if not addressed, may have grave postoperative consequences.
Preoperative evaluation and preparation
Goal: Assess and minimize risks
This process begins in the office or clinic with a discussion with the patient of any concerns and risks. The importance of early mobilization and ambulation after surgery should be emphasized. Any patient with uncontrolled diabetes or hypertension should continue to be monitored by her primary care physician. A patient who has not seen a physician recently should be assessed by an internist to ensure that no conditions go undetected before surgery.
Routine testing to start, but additional assessment may be justified. An obese patient should undergo the same routine testing as a woman of normal weight, but further testing may be warranted for any coexisting disorder. Because the obese patient may have a restrictive lung pattern by virtue of her body habitus, pulmonary-function testing is unlikely to yield new information and is probably not indicated—unless she smokes or has a history of chronic obstructive pulmonary disease. In that case, tests will clarify the obstructive component and bronchodilator response and are useful in postoperative management. Measurement of arterial blood gases is useful, however, because levels reflect respiratory function on a day-to-day basis.
Additional tests of cardiac status probably are not indicated on the basis of obesity alone. However, if initial tests (eg, the electrocardiogram) and the history suggest compromised cardiac function, two-dimensional echocardiography should be performed to determine the ejection fraction. Any concerns regarding cardiac function should be discussed with the anesthesiologist and cardiologist.
Because compromised pulmonary function is likely, I (Dr. Perkins) instruct each patient on the use of incentive spirometry before she undergoes anesthesia so that she has realistic expectations about the postoperative course. I also administer heparin at least 2 hours before induction (8 hours before induction if unfractionated heparin is used).6
If a hysterectomy or prolonged laparotomy is planned, prophylactic antibiotics are recommended.3 Thigh-high compression stockings or a pneumatic calf-compression device should be applied upon arrival in the operating room.
Anesthesia-related issues
Anticipate challenges involving the airway
The anesthesiologist’s primary concern in regard to the obese patient is establishment and maintenance of an airway to promote oxygenation. In morbidly and extremely morbidly obese patients, anatomic factors such as large breasts; a short, thick neck; large tongue; decreased mobility of the cervical spine; limited mouth opening; and greater amount of adipose tissue in the face and cheeks can render mask ventilation and intubation extremely difficult or impossible. Decreased functional residual capacity and tidal volume in the range of closing capacity may lead to extremely rapid oxygen desaturation when the patient is apneic.9
If the patient is pregnant, factors such as excess adipose tissue in the face become even more pronounced and increase the potential for catastrophe.
Appreciate mechanical concerns
The morbidly obese patient may exceed the weight limit of the operating table. In addition, placing her in a steep Trendelenburg position or rotating her laterally may compromise the integrity of the bed.
Coexisting disease, such as sleep apnea and acid reflux disease, should also be kept in mind. Compromised respiratory mechanics (eg, restrictive lung pattern) may cause further deterioration and make mechanical ventilation more difficult.
It also may be hard to establish vascular access, necessitating central venous line placement and introducing its associated risks.
Keep the anesthesiologist in the loop
In the postoperative period, obese patients face a heightened risk of complications related to diminished pulmonary function, such as oxygen desaturation, hypoventilation, and airway obstruction, which may lead to atelectasis, pneumonia, and pulmonary edema.10,11 For these reasons, early consultation with the anesthesiologist is recommended, especially if the initial evaluation suggests potential difficulties in securing the airway. In turn, the anesthesiologist should understand that, in some obese patients, even establishing a surgical airway may be difficult. Regional anesthesia should be considered when feasible.
Antacids and drugs that increase gastric motility have proved to be useful in minimizing aspiration-related risks.12,13
Surgical technique
Begin abdominal procedures by carefully choosing an incision
Do not base the decision solely on the degree of obesity, but also consider any additional procedures that are planned, such as lymph-node sampling. A vertical incision does permit greater exposure than is afforded by a transverse incision, but in some cases the latter may be more appropriate—even if the patient is morbidly obese.
Do not place the incision below the panniculus, in the crease just above the suprapubic mound, though it may be tempting to do so when the panniculus is large and thick. This area is a warm, moist, anaerobic environment that promotes the proliferation of numerous micro-organisms, creating a bacterial cesspool. It is the worst place to make an incision.
If a transverse incision is selected, place caudal traction on the panniculus (which may be facilitated by applying two towel clips to the tissue fold), and incise through the fold at a point approximately three to four fingerbreadths above the symphysis (FIGURE 2).
If a midline incision is selected, a similar technique is appropriate, with downward traction applied to the panniculus and the incision begun at the lower pole of this fold up to the umbilicus—or through it and above, should more room be required.14
After incising the superficial fascia, greater exposure may be gained by incising the rectus sheath beneath the pannicular fold and extending it down to the symphysis. After entering the abdominal cavity, the surgeon may encounter a redundant, fat-laden layer of peritoneum. The edges of this tissue may be temporarily sutured to the edges of the skin incision to remove it from the operative field and obtain better visualization.
FIGURE 2 Incision placement can be counterintuitive
Avoid placing the skin incision beneath the panniculus, an anaerobic area ripe for infection. Instead, retract the panniculus caudally and incise the skin above the fold, as shown.
A few remedies can help when exposure is limited
Exposure is one of the most important elements of successful surgery, but it is often restricted when marked obesity is present. Fortunately, numerous adjuncts are available to address this problem, such as the table-fixed retractor systems described earlier in this article, or one or more of the following tactics:
- Do not try to expose the entire pelvic basin. One technique to ease exploration—especially when more than one procedure is planned—is to refrain from exposing the entire pelvic basin at one time. Instead, focus on obtaining adequate visualization in the immediate area and, once work in that area is finished, concentrate on the next.
- Use extra-long instruments in an extremely large patient, especially if she has a “deep” pelvis.
- Abbreviate the procedure, if possible. Because these cases are technically more difficult and frequently involve excessive blood loss, it may be wiser to perform an “incomplete” procedure, such as supracervical hysterectomy instead of total hysterectomy, depending on the indication.14
- Use a cell-saver blood-collection system if significant blood loss is anticipated. Also remember to give a second dose of prophylactic antibiotic.
Strategies for effective wound closure
The best method of abdominal wound closure has been a subject of debate among both gynecologic and general surgeons. In the obese patient, the key variables are the rather thick subcutaneous fat layer within the abdominal wall and the impact of intra-abdominal pressure on the incision.
What the data show. A number of studies, including one by Montz and colleagues,15 have demonstrated that the running mass-closure technique using delayed-absorbable or permanent suture is just as effective as interrupted suture placement (eg, Smead-Jones closure) but is faster, with less suture deposited in the wound.
The following considerations may also be helpful:
- Approximate the subcutaneous fascia? There has been some debate about whether the subcutaneous fascia must be approximated. My (Dr. Perkins) personal preference in morbidly obese patients is to place several interrupted sutures to obliterate much of the dead space, facilitate skin closure, and minimize tension on the wound; I have noted no significant increase in wound complications using this technique. Placement of a closed-suction drain (eg, Jackson Pratt, Hemovac) is a good alternative.
- Is a drain useful? Some have questioned whether use of a drain increases the likelihood of wound complications,16 but this concern is irrelevant because, in most—if not all—cases, the drainage tubing is exteriorized via a separate stab wound remote from the incision.
- Consider retention sutures. A morbidly obese patient may benefit from through-and-through retention sutures using 0 or #1 permanent material along with rubber bolsters to minimize cutting of the suture into the skin, especially if increased intra-abdominal pressure is likely (FIGURE 3).17 These sutures can be removed on the 10th to 12th postoperative day.
FIGURE 3 Minimize tension on the wound
A morbidly obese patient may benefit from through-and-through retention sutures along with rubber bolsters to minimize cutting of the suture into the skin.
Vaginal surgery does not increase complication rate in the obese
The vaginal approach can be extremely challenging in the morbidly obese patient, especially when hysterectomy is performed. Exposure is often compromised by the large folds about the thighs and buttocks, limiting access to the perineum and vaginal vault. If the patient also has a narrow, contracted pelvis, the difficulty is compounded. Because of these and other concerns about morbidity, many gynecologists hesitate to perform hysterectomy via the vaginal route when the patient is obese.
What the data show. Several studies have addressed these issues, including one by Pratt and Daikoku18 and another by Rafii and colleagues,19 both of which demonstrated that obese patients have a complication rate roughly equivalent to that observed in patients of normal weight, although obese patients have a greater decrease in hemoglobin level and a slightly higher incidence of postoperative fever.
Similarly, in a retrospective study, Pitkin20 found no significant difference between the complication rates of obese and nonobese patients.
Another argument for the self-retaining retractor. From a technical standpoint, achieving good exposure is the primary challenge of vaginal surgery and usually requires two or more assistants—who themselves have limited or no direct view of the field—who must stand for long periods. Again, a viable alternative is use of a self-retaining retractor. One in particular, the MiniOmni retractor, is a small, uncumbersome, table-fixed system that can be maneuvered so that vaginal and perineal structures are readily accessible.
Choice of stirrups is also relevant. Exposure can be affected by the type of stirrups used. “Candy cane” stirrups facilitate exposure more than fixed stirrups (eg, Allen stirrups) do. Regardless of the stirrups selected, however, it is important to avoid excessive or prolonged hip flexion, or nerve injury may result.
How to minimize postoperative complications
After surgery, an obese patient requires close and continuous monitoring to avert complications and detect any that occur. Consider the following measures:
- A stint in the intensive care unit. In the morbidly obese patient, massive fluid shift (eg, extensive blood loss, prolonged surgery with losses from the peritoneum, etc.) or concern about sleep apnea may justify close monitoring in an intensive care unit or similar setting—at least briefly. Later, as the patient recovers, sleep studies may indicate whether apnea is present.
- Document fluid intake and output, especially in the elderly and in women with cardiorespiratory disease.
- Give analgesics in an amount sufficient to control pain and minimize activity that might place excessive tension on the abdominal incision, but also allows the patient to remain alert enough to ambulate effectively and perform pulmonary toileting.
- Begin ambulation on the first postoperative day—or on the evening after surgery, if circumstances permit. This helps clear secretions from the respiratory tract, reduces the risk of thromboembolism, and speeds the return of normal bowel function. Hourly incentive spirometry is also recommended for the first few days after surgery.
- Continue heparin. In patients at moderate or high risk of thromboembolism, continue low-dose heparin until discharge or for 7 days, whichever comes first.
- Keep other physicians involved. If the patient has a significant comorbidity, such as cardiorespiratory disease or uncontrolled diabetes, she should remain under the care of her internist or other primary care provider.
- Closely monitor the surgical wound for early signs of infection, which include inflammation and collections of serous fluid, blood, pus, or a mixture of these. If retention sutures were placed, check them frequently to ensure that they are not cutting into the skin of the abdomen.
- Strongly recommend weight loss. At the time of the last postoperative visit, tell the patient in clear language that obesity is extremely bad for her health and strongly encourage her to lose weight under the supervision of her primary care provider. If she has no such provider, make the appropriate referral.
1. Gallup DG. Modifications of celiotomy techniques to decrease morbidity in obese gynecologic patients. Am J Obstet Gynecol. 1984;150:171-178.
2. Pitkin RM. Abdominal hysterectomy in obese women. Surg Gynecol Obstet. 1976;142:532-536.
3. Antibiotic prophylaxis for gynecologic procedures. ACOG Practice Bulletin No. 74. Washington, DC: American College of Obstetricians and Gynecologists; July 2006.
4. Bookwalter JR. A new table-fixed retractor. Surg Clin North Am. 1980;60:399-405.
5. Noldus J, Graefen M, Huland H. Major postoperative complications secondary to use of the Bookwalter self-retaining retractor. Urology. 2002;60:964-967.
6. Prevention of deep vein thrombosis and pulmonary embolism. ACOG Practice Bulletin No. 21. Washington, DC: American College of Obstetricians and Gynecologists; October 2000.
7. Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165-1177.
8. Perkins JD, Dent LL. Avoiding and repairing bowel injury in gynecologic surgery. OBG Management. 2004;16(8):15-28.
9. Cressey DM, Berthoud MC, Reilly CS. Effectiveness of continuous airway pressure to enhance preoxygenation in morbidly obese women. Anesthesia. 2001;56:670-689.
10. Jordan H, Perlow MD, Mark A, Morgan MD. Massive maternal obesity and perioperative cesarean morbidity. Am J Obstet Gynecol. 1994;170:560-565.
11. Hood DD, Dewan DN. Anesthetic and obstetric outcome in morbidly obese parturients. Anesthesiology. 1993;79:1210-1218.
12. James CF, Gibbs CP, Banner T. Postpartum perioperative risk of aspiration pneumonia. Anesthesiology. 1984;61:756-759.
13. Manchikanti L, Colliver JA, Marrero TC, Roush JR. Ranitidine and metoclopramide for prophylaxis of aspiration pneumonitis in elective surgery. Anesth Analg. 1984;63:903-910.
14. Morrow CP, Hernandez WL, Townsend DE, DiSaia PJ. Pelvic celiotomy in the obese patient. Am J Obstet Gynecol. 1977;127:335-339.
15. Montz FJ, Creasman WT, Eddy G, DiSaia PJ. Running mass closure of abdominal wounds using absorbable looped suture. J Gynecol Surg. 1991;7:107-110.
16. Ramsey PS, White AM, Guinn DA, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967-973.
17. Soisson AP, Olt G, Soper JT, Berchuck A, Rodriguez G, Clarke-Pearson DL. Prevention of superficial wound separation with subcutaneous retention sutures. Gynecol Oncol. 1993;51:330-334.
18. Pratt JH, Daikoku NH. Obesity and vaginal hysterectomy. J Reprod Med. 1990;35:945-949.
19. Rafii A, Samain E, Levardon M, Darai E, Deval B. Vaginal hysterectomy for benign disorders in obese women: a prospective study. Br J Obstet Gynaecol. 2005;111:223-227.
20. Pitkin RM. Vaginal hysterectomy in obese women. Obstet Gynecol. 1977;49:567-569.
21. Kelly HA. Excision of the fat of the abdominal wall—lipectomy. Surg Gynecol Obstet. 1910;10:229-231.
22. Wright JD, Rosenbush EJ, Powell MA, et al. Longterm outcome of women who undergo panniculectomy at the time of gynecologic surgery. Gynecol Oncol. 2006;102:86-91.
23. Hopkins MP, Shriner AM, Parker MG, Scott L. Panniculectomy at the time of gynecologic surgery in morbidly obese patients. Am J Obstet Gynecol. 2000;182:1502-1505.
1. Gallup DG. Modifications of celiotomy techniques to decrease morbidity in obese gynecologic patients. Am J Obstet Gynecol. 1984;150:171-178.
2. Pitkin RM. Abdominal hysterectomy in obese women. Surg Gynecol Obstet. 1976;142:532-536.
3. Antibiotic prophylaxis for gynecologic procedures. ACOG Practice Bulletin No. 74. Washington, DC: American College of Obstetricians and Gynecologists; July 2006.
4. Bookwalter JR. A new table-fixed retractor. Surg Clin North Am. 1980;60:399-405.
5. Noldus J, Graefen M, Huland H. Major postoperative complications secondary to use of the Bookwalter self-retaining retractor. Urology. 2002;60:964-967.
6. Prevention of deep vein thrombosis and pulmonary embolism. ACOG Practice Bulletin No. 21. Washington, DC: American College of Obstetricians and Gynecologists; October 2000.
7. Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165-1177.
8. Perkins JD, Dent LL. Avoiding and repairing bowel injury in gynecologic surgery. OBG Management. 2004;16(8):15-28.
9. Cressey DM, Berthoud MC, Reilly CS. Effectiveness of continuous airway pressure to enhance preoxygenation in morbidly obese women. Anesthesia. 2001;56:670-689.
10. Jordan H, Perlow MD, Mark A, Morgan MD. Massive maternal obesity and perioperative cesarean morbidity. Am J Obstet Gynecol. 1994;170:560-565.
11. Hood DD, Dewan DN. Anesthetic and obstetric outcome in morbidly obese parturients. Anesthesiology. 1993;79:1210-1218.
12. James CF, Gibbs CP, Banner T. Postpartum perioperative risk of aspiration pneumonia. Anesthesiology. 1984;61:756-759.
13. Manchikanti L, Colliver JA, Marrero TC, Roush JR. Ranitidine and metoclopramide for prophylaxis of aspiration pneumonitis in elective surgery. Anesth Analg. 1984;63:903-910.
14. Morrow CP, Hernandez WL, Townsend DE, DiSaia PJ. Pelvic celiotomy in the obese patient. Am J Obstet Gynecol. 1977;127:335-339.
15. Montz FJ, Creasman WT, Eddy G, DiSaia PJ. Running mass closure of abdominal wounds using absorbable looped suture. J Gynecol Surg. 1991;7:107-110.
16. Ramsey PS, White AM, Guinn DA, et al. Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol. 2005;105:967-973.
17. Soisson AP, Olt G, Soper JT, Berchuck A, Rodriguez G, Clarke-Pearson DL. Prevention of superficial wound separation with subcutaneous retention sutures. Gynecol Oncol. 1993;51:330-334.
18. Pratt JH, Daikoku NH. Obesity and vaginal hysterectomy. J Reprod Med. 1990;35:945-949.
19. Rafii A, Samain E, Levardon M, Darai E, Deval B. Vaginal hysterectomy for benign disorders in obese women: a prospective study. Br J Obstet Gynaecol. 2005;111:223-227.
20. Pitkin RM. Vaginal hysterectomy in obese women. Obstet Gynecol. 1977;49:567-569.
21. Kelly HA. Excision of the fat of the abdominal wall—lipectomy. Surg Gynecol Obstet. 1910;10:229-231.
22. Wright JD, Rosenbush EJ, Powell MA, et al. Longterm outcome of women who undergo panniculectomy at the time of gynecologic surgery. Gynecol Oncol. 2006;102:86-91.
23. Hopkins MP, Shriner AM, Parker MG, Scott L. Panniculectomy at the time of gynecologic surgery in morbidly obese patients. Am J Obstet Gynecol. 2000;182:1502-1505.