User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Children and COVID: Many parents see vaccine as the greater risk
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
Charcoal could be the cure for the common high-fat diet
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Charcoal won’t let high-fat diet weigh you down
Do you want to be the funniest person alive? Of course you do. It’s really simple too, just one joke can make you the greatest comedian of all time. All you have to do is go camping and cook food over a roaring campfire. When someone drops food into the fire (which they always will), get ready. Once they fish out the offending food, which is almost certainly coated in hot coals, tell them: “Ah, eat it anyway. A little texture never hurt!” Trust us, most hilarious and original gag of all time.
But before your hapless friend brushes off his hot dog and forces a laugh, consider this: Japanese researchers have found that a charcoal supplement can prevent weight gain in mice consuming a high-fat diet. Charcoal is actually quite the helpful substance, and not just for grilling. It’s been used as medicine for hundreds of years and even today is used as a treatment for drug overdose and excess gas and flatulence.
The study involved two groups of mice: One was fed a normal diet, the other a high-fat diet. After 12 weeks, the high-fat diet mice had gained weight. At that point, edible activated charcoal was added to their diet. From that point, weight gain was similar between the two groups, and the amount of bile acid, cholesterol, triglyceride, and fatty acid excreted by the high-fat mice increased by two to four times.
The researchers supported the notion that consuming an activated charcoal supplement before or while eating fatty food could prevent weight gain from said fatty food. Which works out well for the classic American barbecue, which is traditionally both high in fat and charcoal. All you have to do is buy some extra charcoal briquettes to pass around and munch on with your friends. Now that’s a party we can get behind.
There’s awake, and then there’s neurologically awake
Time to toss another urban legend onto the trash heap of history. Say goodbye to the benefits of uninterrupted sleep. It’s a fraud, a fake, a myth, a hit or myth, a swing and a myth, an old wives’ tale. You can stuff it and put it on a shelf next to Bigfoot, the Slender Man, and Twinkies.
We all thought we needed 8 hours of uninterrupted sleep every night, but guess who we forgot to tell? Our brains. They’ve been doing exactly the opposite all along, laughing at us the whole time. Smug SOBs.
To straighten out this mess, let’s bring in a scientist, Celia Kjaerby of the Center for Translational Neuromedicine at the University of Copenhagen: “You may think that sleep is a constant state that you are in, and then you wake up. But there is a lot more to sleep than meets the eye. We have learned that noradrenaline causes you to wake up more than 100 times a night. And that is during perfectly normal sleep.”
Those 100 or so sleep interruptions are so brief that we don’t even notice, but they are very important, according to a study conducted at the university. Those tiny little wake-up calls are “the essence for the part of sleep that makes us wake up rested and which enables us to remember what we learned the day before. ... The very short awakenings are created by waves of norepinephrine [and they] reset the brain so that it is ready to store memory when you dive back into sleep,” lead author Maiken Nedergaard, MD, explained.
The investigators compared the level of noradrenaline in sleeping mice with their electrical activity and found that the hormone constantly increased and decreased in a wavelike pattern. A high level meant that the animal was neurologically awake. Deeper valleys between the high points meant better sleep, and the mice with the “highest number of deep noradrenaline valleys were also the ones with the best memory,” the team said in their written statement.
Not just the best memory, they said, but “super memory.” That, of course, was enough to get the attention of Marvel Comics, so the next Disney superhero blockbuster will feature Nocturna, the queen of the night. Her power? Never forgets. Her archnemesis? The Insomniac. Her catchphrase? “Let me sleep on it.”
Words can hurt, literally
Growing up, we’re sure you heard the “sticks and stones” rhyme. Maybe you’ve even recited it once or twice to defend yourself. Well, forget it, because words can hurt and your brain knows it.
In a new study published in Frontiers in Communication, Marijn Struiksma, PhD, of Utrecht University, and colleagues incorporated the use of electroencephalography (EEG) and skin conductance on 79 women to see how words (specifically insults) actually affect the human body.
Each subject was asked to read three different types of statements: an insult, a compliment, and something factual but neutral. Half of the statements contained the subject’s name and half used somebody else’s. The participants were told that these statements were collected from three men.
Nobody interacted with each other, and the setting was completely clinical, yet the results were unmistakable. The EEG showed an effect in P2 amplitude with repetitive insults, no matter who it was about. Even though the insults weren’t real and the participants were aware of it, the brain still recognized them as hurtful, coming across as “mini slaps in the face,” Dr. Struiksma noted in a written statement.
The researchers noted that more needs to be done to better understand the long-term effects that insults can have and create a deeper understanding between words and emotion, but studying the effects of insults in a real-life setting is ethically tricky. This study is a start.
So, yeah, sticks and stones can break your bones, but words will actually hurt you.
This article was updated 7/21/22.
Children and COVID: Does latest rise in new cases point toward stabilization?
New COVID-19 cases rose for the second time in 3 weeks, as the effort to vaccinate the youngest children continued to slow after just 3 full weeks.
Nationally, over 75,000 children under age 5 years received their first dose of COVID-19 vaccine during the week of July 7-13. That number is down from the previous week – 118,000 from June 30 to July 6 – which, in turn, was lower than the 206,000 doses administered through the first 10 days after approval, based on data from the Centers for Disease Control and Prevention. That all adds up to just under 400,000 vaccinated children, or 2% of the eligible population under age 5, as of July 13.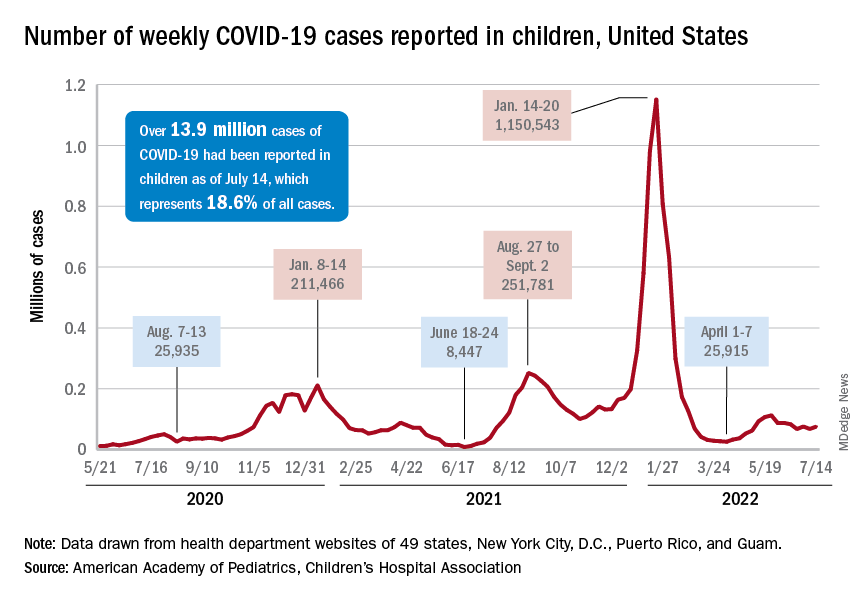
State-level data, meanwhile, show considerable variation, the American Academy of Pediatrics noted in its weekly analysis of the CDC vaccine data. Vermont has already vaccinated 10.0% of children under age 5 years, and Massachusetts is at 9.5%, while Mississippi (0.3%), Alabama (0.5%), and Louisiana (0.8%) are still below 1%, the AAP said.
New cases show signs of steadying
The national count was up by 11.1% for the week of July 8-14, rising to 75,000 new cases, compared with 68,000 the previous week, but the recent trend seems to be leaning toward steadiness. The overall number has been between 67,000 and 76,000 over the past 4 weeks, alternating between rising and falling in that time span, according to data gathered by the AAP and the Children’s Hospital Association from state and territorial health departments.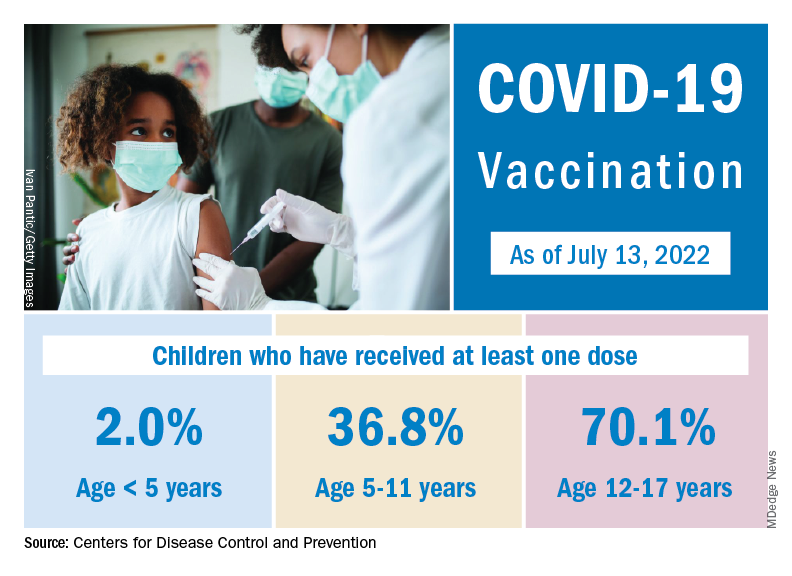
the two groups said, also noting that several states have stopped updating their online dashboards over the past year, making the current total artificially low in comparison.
Taken with that grain of salt, the cumulative number of child cases since the start of the pandemic is just over 13.9 million, which represents 18.6% of all cases in the United States. That proportion has been declining in recent weeks and was as high as 19.0% as late as mid-May. “While COVID-19 cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases,” the AAP and CHA said.
New COVID-19 cases rose for the second time in 3 weeks, as the effort to vaccinate the youngest children continued to slow after just 3 full weeks.
Nationally, over 75,000 children under age 5 years received their first dose of COVID-19 vaccine during the week of July 7-13. That number is down from the previous week – 118,000 from June 30 to July 6 – which, in turn, was lower than the 206,000 doses administered through the first 10 days after approval, based on data from the Centers for Disease Control and Prevention. That all adds up to just under 400,000 vaccinated children, or 2% of the eligible population under age 5, as of July 13.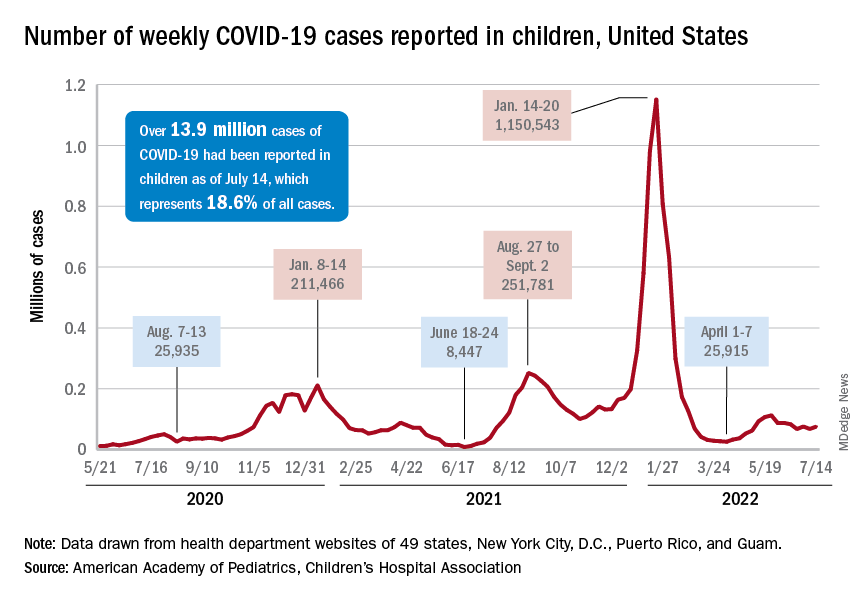
State-level data, meanwhile, show considerable variation, the American Academy of Pediatrics noted in its weekly analysis of the CDC vaccine data. Vermont has already vaccinated 10.0% of children under age 5 years, and Massachusetts is at 9.5%, while Mississippi (0.3%), Alabama (0.5%), and Louisiana (0.8%) are still below 1%, the AAP said.
New cases show signs of steadying
The national count was up by 11.1% for the week of July 8-14, rising to 75,000 new cases, compared with 68,000 the previous week, but the recent trend seems to be leaning toward steadiness. The overall number has been between 67,000 and 76,000 over the past 4 weeks, alternating between rising and falling in that time span, according to data gathered by the AAP and the Children’s Hospital Association from state and territorial health departments.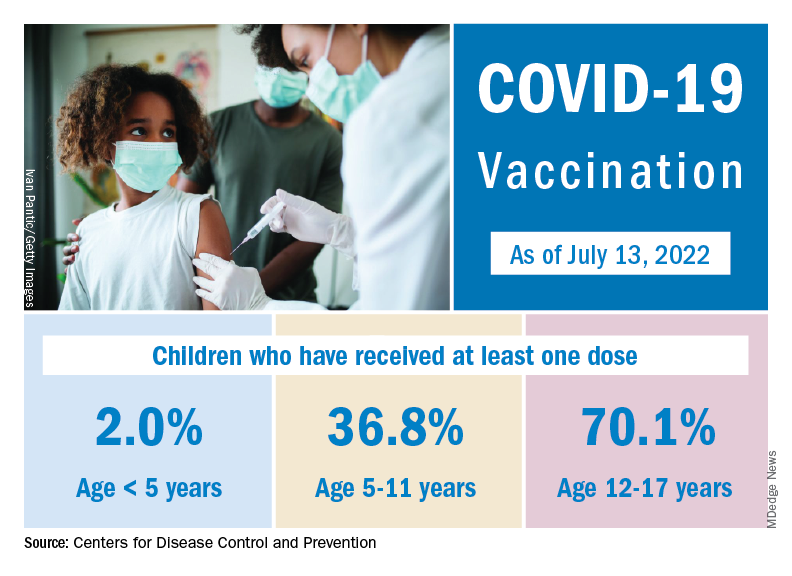
the two groups said, also noting that several states have stopped updating their online dashboards over the past year, making the current total artificially low in comparison.
Taken with that grain of salt, the cumulative number of child cases since the start of the pandemic is just over 13.9 million, which represents 18.6% of all cases in the United States. That proportion has been declining in recent weeks and was as high as 19.0% as late as mid-May. “While COVID-19 cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases,” the AAP and CHA said.
New COVID-19 cases rose for the second time in 3 weeks, as the effort to vaccinate the youngest children continued to slow after just 3 full weeks.
Nationally, over 75,000 children under age 5 years received their first dose of COVID-19 vaccine during the week of July 7-13. That number is down from the previous week – 118,000 from June 30 to July 6 – which, in turn, was lower than the 206,000 doses administered through the first 10 days after approval, based on data from the Centers for Disease Control and Prevention. That all adds up to just under 400,000 vaccinated children, or 2% of the eligible population under age 5, as of July 13.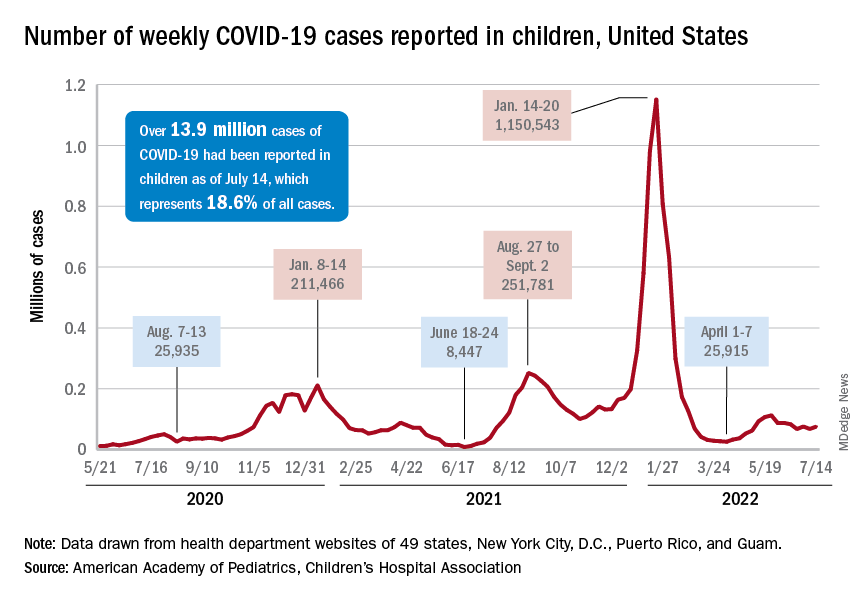
State-level data, meanwhile, show considerable variation, the American Academy of Pediatrics noted in its weekly analysis of the CDC vaccine data. Vermont has already vaccinated 10.0% of children under age 5 years, and Massachusetts is at 9.5%, while Mississippi (0.3%), Alabama (0.5%), and Louisiana (0.8%) are still below 1%, the AAP said.
New cases show signs of steadying
The national count was up by 11.1% for the week of July 8-14, rising to 75,000 new cases, compared with 68,000 the previous week, but the recent trend seems to be leaning toward steadiness. The overall number has been between 67,000 and 76,000 over the past 4 weeks, alternating between rising and falling in that time span, according to data gathered by the AAP and the Children’s Hospital Association from state and territorial health departments.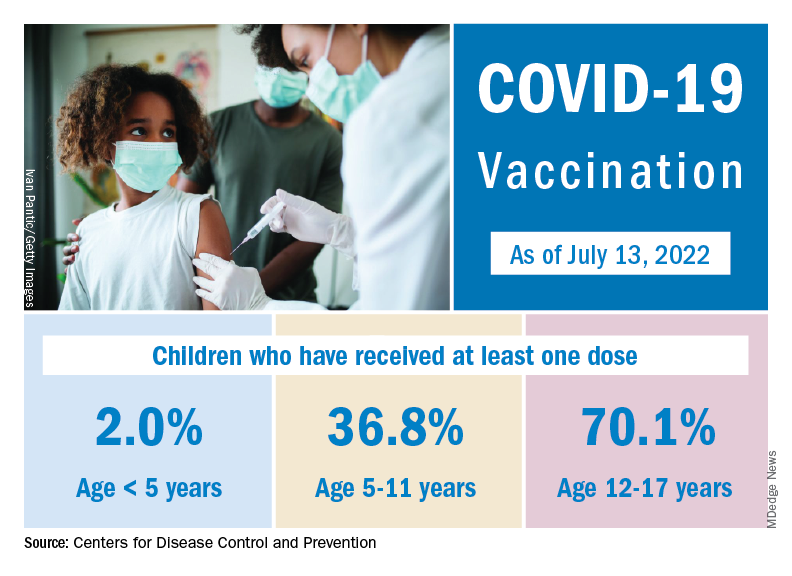
the two groups said, also noting that several states have stopped updating their online dashboards over the past year, making the current total artificially low in comparison.
Taken with that grain of salt, the cumulative number of child cases since the start of the pandemic is just over 13.9 million, which represents 18.6% of all cases in the United States. That proportion has been declining in recent weeks and was as high as 19.0% as late as mid-May. “While COVID-19 cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases,” the AAP and CHA said.
Shift schedule today could worsen that stroke tomorrow
Body clocks and the shifting risks of stroke
Health care professionals, we’re sure, are no strangers to rotating shifts. And, as practitioners of the shiftly arts, you should know new research shows that working those kinds of hours can have lasting effects on your health. And it’s all based on your sleep-wake cycle.
In a study published in Neurobiology of Sleep and Circadian Rhythms, investigators at Texas A&M University looked at the effects of working these kinds of shifts for a long period of time and then returning to a regular 24-hour cycle later in life. The study piggybacks on a previous study, which showed that rats on shift schedules had more severe stroke outcomes than those who were on a 24-hour cycle.
The current study demonstrates that working rotating shifts does have a lasting effect, by way of messing with the sleep-wake cycle. Based on the research, the rats that performed those kinds of shifts never got back to a normal schedule. When strokes occurred, outcomes were much worse, and the females had a higher mortality rate and more severe functional deficits than the males.
Now for the “good” news: Even if you’re among those who haven’t worked a rotating shift, you may not be safe either.
People who have regular working hours have a tendency to take work home and stay up late, especially with so many moving to a remote-work model. And if you’re staying up late on the weekends you’re producing what lead author David J. Earnest, PhD, called “social jet lag,” which messes with your circadian rhythm to wind you down for sleep. All of these things can lead to the same kind of effects that working rotating shifts has on your health, he said in a written statement.
How do you combat this? Dr. Earnest recommended creating a sleep schedule and setting regular mealtimes. Also ease up on high-fat foods, drinking, and smoking. The connection between your brain and gut also could play a part in how severe a stroke can be.
So continue to work hard, but not too hard.
Got 3 minutes? You got time for culture
Much like a Krabby Patty, art is good for your soul. Seriously, staring at a 500-year-old painting may not seem like much, but research has proven time and again that going to a museum and looking at paintings by long-dead artists you probably know better as pizza-eating superhero turtles improves mood, stress, and well-being.
A couple of years ago, however, museums and art galleries ran into a big virus-shaped problem. You may have heard of it. All of a sudden it became a very bad idea for people to gather together in one building and huddle around the Mona Lisa, which, by the way, is a lot smaller in person than you might expect. But, rather than sit around with a bunch of priceless art for an indeterminate amount of time, museums brought their exhibits to the Internet so that people from all over the world could see great works from their couches.
This is absolutely a good thing for public access, but do these virtual art exhibits provide the same health benefits as going to a museum in person? That’s what a group of European researchers aimed to find out, and in a study published in Frontiers of Psychology, that’s exactly what they found.
Their directive to the 84 study participants was simple: Take a well-being survey, engage with either of a pair of online exhibits (a Monet painting and a display of Japanese culinary traditions) for just 3 minutes, then take another well-being assessment. The results were quite clear: Even just a couple of minutes of viewing art online improved all the well-being categories on the survey, such as lowering anxiety, negative mood, and loneliness, as well as increasing subjective well-being. Also, the more beautiful or meaningful a person found the art, the more their mood and well-being improved.
The researchers noted that these results could help access in places where access to art is limited, such as waiting rooms, hospitals, and rural areas. Let’s just hope it sticks to that, and that big businesses don’t take notice. Just imagine them plastering ads with classic Renaissance artworks. After all, art makes you feel good, and you know what else feels good on a hot summer day? An ice-cold Coca-Cola! By the way, we’re taking offers, advertising agencies. The LOTME staff can absolutely be bought.
Appetite for etymology
Today on “It’s a Thing,” we examine various states of hunger and what they should be called. Our first guest is that historically hungry royal person, King Henry VIII of England. Your majesty, have you ever been “hangry?”
KH8: First, let me thank you for inviting me on the show, Maurice. I’m a huge fan. A recent study done in the United Kingdom and Austria showed that “hunger is associated with greater levels of anger and irritability, as well as lower levels of pleasure,” according to a Eurekalert statement. So, yes, I have been “hangry.”
Maurice: Now to our next guest. Martha Stewart, can you add anything about that study?
Martha: Happy to, Maurice. The 64 participants used a smartphone app to record their hunger levels and emotional states five times a day for 21 days. It’s the first time that “hanger” was studied outside a lab, and it showed that hunger “was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants,” the investigators said in that statement.
Maurice: It’s official, then. Hangry is a thing, and we don’t need to put it in quotes anymore. Now let’s meet our third and final guest, Betty Crocker. Betty, I’m told you have a study to plug.
Betty: That’s right, Mo. Researchers at Tel Aviv University looked at survey data from almost 3,000 men and women and found that men ate 17% more food during the warmer months (March to September) than they did the rest of the year. Among women, however, caloric intake did not change.
KH8: I saw that study. Didn’t they put 27 people out in the sun and then take blood samples?
Betty: Indeed they did, Hank. After 25 minutes of sun exposure, the 13 men felt hungrier than before, but the 14 women did not. The men also had higher levels of ghrelin, an appetite-stimulating hormone, than the women.
Maurice: To sum all this up, then, we’ve got angry and hungry officially combining to make hangry, and now it looks like the sun is causing hunger in men, which makes them … sungry?
Martha: It’s a thing.
Chicken cutlets with a side of COVID
You stopped at the drive through at McDonald’s on the way home from work, and while you’re looking for something sweet in the refrigerator for dessert, you see that chicken breast that expires today.
Freezing meat that’s about to expire might be your go-to so it doesn’t go to waste, but it’s been found that SARS-CoV-2 can live in meat that’s been in the refrigerator or freezer for more than a month.
Researchers exposed chicken, beef, pork, and salmon to surrogate viruses that are similar to COVID but not as harmful and stored them in freezers at –4° F and in the refrigerator at 39.2° F. “We even found that the viruses could be cultured after [being frozen for] that length of time,” lead author Emily Bailey, PhD, of Campbell University in Buies Creek, N.C., said in Study Finds.
The team began its research after hearing of COVID-19 outbreaks where there were no reports of community transmission, such as in Southeast Asia. Tracing eventually led to packaged meats as the culprits in those cases. SARS-CoV-2 is able to replicate in the gut, as well as the respiratory tract, so it could affect the gut before respiratory symptoms start. It is crucial to ensure cross contamination doesn’t occur, and inadequate sanitation prior to packaging needs to be addressed, the investigators said.
Honestly, we didn’t think anything could survive in a freezer for that long, but SARS-CoV-2 is a fighter.
Body clocks and the shifting risks of stroke
Health care professionals, we’re sure, are no strangers to rotating shifts. And, as practitioners of the shiftly arts, you should know new research shows that working those kinds of hours can have lasting effects on your health. And it’s all based on your sleep-wake cycle.
In a study published in Neurobiology of Sleep and Circadian Rhythms, investigators at Texas A&M University looked at the effects of working these kinds of shifts for a long period of time and then returning to a regular 24-hour cycle later in life. The study piggybacks on a previous study, which showed that rats on shift schedules had more severe stroke outcomes than those who were on a 24-hour cycle.
The current study demonstrates that working rotating shifts does have a lasting effect, by way of messing with the sleep-wake cycle. Based on the research, the rats that performed those kinds of shifts never got back to a normal schedule. When strokes occurred, outcomes were much worse, and the females had a higher mortality rate and more severe functional deficits than the males.
Now for the “good” news: Even if you’re among those who haven’t worked a rotating shift, you may not be safe either.
People who have regular working hours have a tendency to take work home and stay up late, especially with so many moving to a remote-work model. And if you’re staying up late on the weekends you’re producing what lead author David J. Earnest, PhD, called “social jet lag,” which messes with your circadian rhythm to wind you down for sleep. All of these things can lead to the same kind of effects that working rotating shifts has on your health, he said in a written statement.
How do you combat this? Dr. Earnest recommended creating a sleep schedule and setting regular mealtimes. Also ease up on high-fat foods, drinking, and smoking. The connection between your brain and gut also could play a part in how severe a stroke can be.
So continue to work hard, but not too hard.
Got 3 minutes? You got time for culture
Much like a Krabby Patty, art is good for your soul. Seriously, staring at a 500-year-old painting may not seem like much, but research has proven time and again that going to a museum and looking at paintings by long-dead artists you probably know better as pizza-eating superhero turtles improves mood, stress, and well-being.
A couple of years ago, however, museums and art galleries ran into a big virus-shaped problem. You may have heard of it. All of a sudden it became a very bad idea for people to gather together in one building and huddle around the Mona Lisa, which, by the way, is a lot smaller in person than you might expect. But, rather than sit around with a bunch of priceless art for an indeterminate amount of time, museums brought their exhibits to the Internet so that people from all over the world could see great works from their couches.
This is absolutely a good thing for public access, but do these virtual art exhibits provide the same health benefits as going to a museum in person? That’s what a group of European researchers aimed to find out, and in a study published in Frontiers of Psychology, that’s exactly what they found.
Their directive to the 84 study participants was simple: Take a well-being survey, engage with either of a pair of online exhibits (a Monet painting and a display of Japanese culinary traditions) for just 3 minutes, then take another well-being assessment. The results were quite clear: Even just a couple of minutes of viewing art online improved all the well-being categories on the survey, such as lowering anxiety, negative mood, and loneliness, as well as increasing subjective well-being. Also, the more beautiful or meaningful a person found the art, the more their mood and well-being improved.
The researchers noted that these results could help access in places where access to art is limited, such as waiting rooms, hospitals, and rural areas. Let’s just hope it sticks to that, and that big businesses don’t take notice. Just imagine them plastering ads with classic Renaissance artworks. After all, art makes you feel good, and you know what else feels good on a hot summer day? An ice-cold Coca-Cola! By the way, we’re taking offers, advertising agencies. The LOTME staff can absolutely be bought.
Appetite for etymology
Today on “It’s a Thing,” we examine various states of hunger and what they should be called. Our first guest is that historically hungry royal person, King Henry VIII of England. Your majesty, have you ever been “hangry?”
KH8: First, let me thank you for inviting me on the show, Maurice. I’m a huge fan. A recent study done in the United Kingdom and Austria showed that “hunger is associated with greater levels of anger and irritability, as well as lower levels of pleasure,” according to a Eurekalert statement. So, yes, I have been “hangry.”
Maurice: Now to our next guest. Martha Stewart, can you add anything about that study?
Martha: Happy to, Maurice. The 64 participants used a smartphone app to record their hunger levels and emotional states five times a day for 21 days. It’s the first time that “hanger” was studied outside a lab, and it showed that hunger “was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants,” the investigators said in that statement.
Maurice: It’s official, then. Hangry is a thing, and we don’t need to put it in quotes anymore. Now let’s meet our third and final guest, Betty Crocker. Betty, I’m told you have a study to plug.
Betty: That’s right, Mo. Researchers at Tel Aviv University looked at survey data from almost 3,000 men and women and found that men ate 17% more food during the warmer months (March to September) than they did the rest of the year. Among women, however, caloric intake did not change.
KH8: I saw that study. Didn’t they put 27 people out in the sun and then take blood samples?
Betty: Indeed they did, Hank. After 25 minutes of sun exposure, the 13 men felt hungrier than before, but the 14 women did not. The men also had higher levels of ghrelin, an appetite-stimulating hormone, than the women.
Maurice: To sum all this up, then, we’ve got angry and hungry officially combining to make hangry, and now it looks like the sun is causing hunger in men, which makes them … sungry?
Martha: It’s a thing.
Chicken cutlets with a side of COVID
You stopped at the drive through at McDonald’s on the way home from work, and while you’re looking for something sweet in the refrigerator for dessert, you see that chicken breast that expires today.
Freezing meat that’s about to expire might be your go-to so it doesn’t go to waste, but it’s been found that SARS-CoV-2 can live in meat that’s been in the refrigerator or freezer for more than a month.
Researchers exposed chicken, beef, pork, and salmon to surrogate viruses that are similar to COVID but not as harmful and stored them in freezers at –4° F and in the refrigerator at 39.2° F. “We even found that the viruses could be cultured after [being frozen for] that length of time,” lead author Emily Bailey, PhD, of Campbell University in Buies Creek, N.C., said in Study Finds.
The team began its research after hearing of COVID-19 outbreaks where there were no reports of community transmission, such as in Southeast Asia. Tracing eventually led to packaged meats as the culprits in those cases. SARS-CoV-2 is able to replicate in the gut, as well as the respiratory tract, so it could affect the gut before respiratory symptoms start. It is crucial to ensure cross contamination doesn’t occur, and inadequate sanitation prior to packaging needs to be addressed, the investigators said.
Honestly, we didn’t think anything could survive in a freezer for that long, but SARS-CoV-2 is a fighter.
Body clocks and the shifting risks of stroke
Health care professionals, we’re sure, are no strangers to rotating shifts. And, as practitioners of the shiftly arts, you should know new research shows that working those kinds of hours can have lasting effects on your health. And it’s all based on your sleep-wake cycle.
In a study published in Neurobiology of Sleep and Circadian Rhythms, investigators at Texas A&M University looked at the effects of working these kinds of shifts for a long period of time and then returning to a regular 24-hour cycle later in life. The study piggybacks on a previous study, which showed that rats on shift schedules had more severe stroke outcomes than those who were on a 24-hour cycle.
The current study demonstrates that working rotating shifts does have a lasting effect, by way of messing with the sleep-wake cycle. Based on the research, the rats that performed those kinds of shifts never got back to a normal schedule. When strokes occurred, outcomes were much worse, and the females had a higher mortality rate and more severe functional deficits than the males.
Now for the “good” news: Even if you’re among those who haven’t worked a rotating shift, you may not be safe either.
People who have regular working hours have a tendency to take work home and stay up late, especially with so many moving to a remote-work model. And if you’re staying up late on the weekends you’re producing what lead author David J. Earnest, PhD, called “social jet lag,” which messes with your circadian rhythm to wind you down for sleep. All of these things can lead to the same kind of effects that working rotating shifts has on your health, he said in a written statement.
How do you combat this? Dr. Earnest recommended creating a sleep schedule and setting regular mealtimes. Also ease up on high-fat foods, drinking, and smoking. The connection between your brain and gut also could play a part in how severe a stroke can be.
So continue to work hard, but not too hard.
Got 3 minutes? You got time for culture
Much like a Krabby Patty, art is good for your soul. Seriously, staring at a 500-year-old painting may not seem like much, but research has proven time and again that going to a museum and looking at paintings by long-dead artists you probably know better as pizza-eating superhero turtles improves mood, stress, and well-being.
A couple of years ago, however, museums and art galleries ran into a big virus-shaped problem. You may have heard of it. All of a sudden it became a very bad idea for people to gather together in one building and huddle around the Mona Lisa, which, by the way, is a lot smaller in person than you might expect. But, rather than sit around with a bunch of priceless art for an indeterminate amount of time, museums brought their exhibits to the Internet so that people from all over the world could see great works from their couches.
This is absolutely a good thing for public access, but do these virtual art exhibits provide the same health benefits as going to a museum in person? That’s what a group of European researchers aimed to find out, and in a study published in Frontiers of Psychology, that’s exactly what they found.
Their directive to the 84 study participants was simple: Take a well-being survey, engage with either of a pair of online exhibits (a Monet painting and a display of Japanese culinary traditions) for just 3 minutes, then take another well-being assessment. The results were quite clear: Even just a couple of minutes of viewing art online improved all the well-being categories on the survey, such as lowering anxiety, negative mood, and loneliness, as well as increasing subjective well-being. Also, the more beautiful or meaningful a person found the art, the more their mood and well-being improved.
The researchers noted that these results could help access in places where access to art is limited, such as waiting rooms, hospitals, and rural areas. Let’s just hope it sticks to that, and that big businesses don’t take notice. Just imagine them plastering ads with classic Renaissance artworks. After all, art makes you feel good, and you know what else feels good on a hot summer day? An ice-cold Coca-Cola! By the way, we’re taking offers, advertising agencies. The LOTME staff can absolutely be bought.
Appetite for etymology
Today on “It’s a Thing,” we examine various states of hunger and what they should be called. Our first guest is that historically hungry royal person, King Henry VIII of England. Your majesty, have you ever been “hangry?”
KH8: First, let me thank you for inviting me on the show, Maurice. I’m a huge fan. A recent study done in the United Kingdom and Austria showed that “hunger is associated with greater levels of anger and irritability, as well as lower levels of pleasure,” according to a Eurekalert statement. So, yes, I have been “hangry.”
Maurice: Now to our next guest. Martha Stewart, can you add anything about that study?
Martha: Happy to, Maurice. The 64 participants used a smartphone app to record their hunger levels and emotional states five times a day for 21 days. It’s the first time that “hanger” was studied outside a lab, and it showed that hunger “was associated with 37% of the variance in irritability, 34% of the variance in anger, and 38% of the variance in pleasure recorded by the participants,” the investigators said in that statement.
Maurice: It’s official, then. Hangry is a thing, and we don’t need to put it in quotes anymore. Now let’s meet our third and final guest, Betty Crocker. Betty, I’m told you have a study to plug.
Betty: That’s right, Mo. Researchers at Tel Aviv University looked at survey data from almost 3,000 men and women and found that men ate 17% more food during the warmer months (March to September) than they did the rest of the year. Among women, however, caloric intake did not change.
KH8: I saw that study. Didn’t they put 27 people out in the sun and then take blood samples?
Betty: Indeed they did, Hank. After 25 minutes of sun exposure, the 13 men felt hungrier than before, but the 14 women did not. The men also had higher levels of ghrelin, an appetite-stimulating hormone, than the women.
Maurice: To sum all this up, then, we’ve got angry and hungry officially combining to make hangry, and now it looks like the sun is causing hunger in men, which makes them … sungry?
Martha: It’s a thing.
Chicken cutlets with a side of COVID
You stopped at the drive through at McDonald’s on the way home from work, and while you’re looking for something sweet in the refrigerator for dessert, you see that chicken breast that expires today.
Freezing meat that’s about to expire might be your go-to so it doesn’t go to waste, but it’s been found that SARS-CoV-2 can live in meat that’s been in the refrigerator or freezer for more than a month.
Researchers exposed chicken, beef, pork, and salmon to surrogate viruses that are similar to COVID but not as harmful and stored them in freezers at –4° F and in the refrigerator at 39.2° F. “We even found that the viruses could be cultured after [being frozen for] that length of time,” lead author Emily Bailey, PhD, of Campbell University in Buies Creek, N.C., said in Study Finds.
The team began its research after hearing of COVID-19 outbreaks where there were no reports of community transmission, such as in Southeast Asia. Tracing eventually led to packaged meats as the culprits in those cases. SARS-CoV-2 is able to replicate in the gut, as well as the respiratory tract, so it could affect the gut before respiratory symptoms start. It is crucial to ensure cross contamination doesn’t occur, and inadequate sanitation prior to packaging needs to be addressed, the investigators said.
Honestly, we didn’t think anything could survive in a freezer for that long, but SARS-CoV-2 is a fighter.
Children and COVID: Vaccination a harder sell in the summer
The COVID-19 vaccination effort in the youngest children has begun much more slowly than the most recent rollout for older children, according to the Centers for Disease Control and Prevention.
in early November of 2021, based on CDC data last updated on July 7.
That approval, of course, came between the Delta and Omicron surges, when awareness was higher. The low initial uptake among those under age 5, however, was not unexpected by the Biden administration. “That number in and of itself is very much in line with our expectation, and we’re eager to continue working closely with partners to build on this start,” a senior administration official told ABC News.
With approval of the vaccine occurring after the school year was over, parents’ thoughts have been focused more on vacations and less on vaccinations. “Even before these vaccines officially became available, this was going to be a different rollout; it was going to take more time,” the official explained.
Incidence measures continue on different paths
New COVID-19 cases dropped during the latest reporting week (July 1-7), returning to the downward trend that began in late May and then stopped for 1 week (June 24-30), when cases were up by 12.4%, according to the American Academy of Pediatrics and the Children’s Hospital Association.

Children also represent a smaller share of cases, probably because of underreporting. “There has been a notable decline in the portion of reported weekly COVID-19 cases that are children,” the two groups said in their weekly COVID report. Although “cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases.”
Other measures, however, have been rising slowly but steadily since the spring. New admissions of patients aged 0-17 years with confirmed COVID, which were down to 0.13 per 100,000 population in early April, had climbed to 0.39 per 100,000 by July 7, the CDC said on its COVID Data Tracker.
Emergency department visits continue to show the same upward trend, despite a small decline in early June. A COVID diagnosis was involved in just 0.5% of ED visits in children aged 0-11 years on March 26, but by July 6 the rate was 4.7%. Increases were not as high among older children: From 0.3% on March 26 to 2.5% on July 6 for those aged 12-15 and from 0.3% to 2.4% for 16- and 17-year-olds, according to the CDC.
The COVID-19 vaccination effort in the youngest children has begun much more slowly than the most recent rollout for older children, according to the Centers for Disease Control and Prevention.
in early November of 2021, based on CDC data last updated on July 7.
That approval, of course, came between the Delta and Omicron surges, when awareness was higher. The low initial uptake among those under age 5, however, was not unexpected by the Biden administration. “That number in and of itself is very much in line with our expectation, and we’re eager to continue working closely with partners to build on this start,” a senior administration official told ABC News.
With approval of the vaccine occurring after the school year was over, parents’ thoughts have been focused more on vacations and less on vaccinations. “Even before these vaccines officially became available, this was going to be a different rollout; it was going to take more time,” the official explained.
Incidence measures continue on different paths
New COVID-19 cases dropped during the latest reporting week (July 1-7), returning to the downward trend that began in late May and then stopped for 1 week (June 24-30), when cases were up by 12.4%, according to the American Academy of Pediatrics and the Children’s Hospital Association.

Children also represent a smaller share of cases, probably because of underreporting. “There has been a notable decline in the portion of reported weekly COVID-19 cases that are children,” the two groups said in their weekly COVID report. Although “cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases.”
Other measures, however, have been rising slowly but steadily since the spring. New admissions of patients aged 0-17 years with confirmed COVID, which were down to 0.13 per 100,000 population in early April, had climbed to 0.39 per 100,000 by July 7, the CDC said on its COVID Data Tracker.
Emergency department visits continue to show the same upward trend, despite a small decline in early June. A COVID diagnosis was involved in just 0.5% of ED visits in children aged 0-11 years on March 26, but by July 6 the rate was 4.7%. Increases were not as high among older children: From 0.3% on March 26 to 2.5% on July 6 for those aged 12-15 and from 0.3% to 2.4% for 16- and 17-year-olds, according to the CDC.
The COVID-19 vaccination effort in the youngest children has begun much more slowly than the most recent rollout for older children, according to the Centers for Disease Control and Prevention.
in early November of 2021, based on CDC data last updated on July 7.
That approval, of course, came between the Delta and Omicron surges, when awareness was higher. The low initial uptake among those under age 5, however, was not unexpected by the Biden administration. “That number in and of itself is very much in line with our expectation, and we’re eager to continue working closely with partners to build on this start,” a senior administration official told ABC News.
With approval of the vaccine occurring after the school year was over, parents’ thoughts have been focused more on vacations and less on vaccinations. “Even before these vaccines officially became available, this was going to be a different rollout; it was going to take more time,” the official explained.
Incidence measures continue on different paths
New COVID-19 cases dropped during the latest reporting week (July 1-7), returning to the downward trend that began in late May and then stopped for 1 week (June 24-30), when cases were up by 12.4%, according to the American Academy of Pediatrics and the Children’s Hospital Association.

Children also represent a smaller share of cases, probably because of underreporting. “There has been a notable decline in the portion of reported weekly COVID-19 cases that are children,” the two groups said in their weekly COVID report. Although “cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases.”
Other measures, however, have been rising slowly but steadily since the spring. New admissions of patients aged 0-17 years with confirmed COVID, which were down to 0.13 per 100,000 population in early April, had climbed to 0.39 per 100,000 by July 7, the CDC said on its COVID Data Tracker.
Emergency department visits continue to show the same upward trend, despite a small decline in early June. A COVID diagnosis was involved in just 0.5% of ED visits in children aged 0-11 years on March 26, but by July 6 the rate was 4.7%. Increases were not as high among older children: From 0.3% on March 26 to 2.5% on July 6 for those aged 12-15 and from 0.3% to 2.4% for 16- and 17-year-olds, according to the CDC.
Mosquitoes and the vicious circle that’s gone viral
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
These viruses want mosquitoes with good taste
Taste can be a pretty subjective sense. Not everyone agrees on what tastes good and what tastes bad. Most people would agree that freshly baked cookies taste good, but what about lima beans? And what about mosquitoes? What tastes good to a mosquito?
The answer? Blood. Blood tastes good to a mosquito. That really wasn’t a very hard question, was it? You did know the answer, didn’t you? They don’t care about cookies, and they certainly don’t care about lima beans. It’s blood that they love.
That brings us back to subjectivity, because it is possible for blood to taste even better. The secret ingredient is dengue … and Zika.
A study just published in Cell demonstrates that mice infected with dengue and Zika viruses release a volatile compound called acetophenone. “We found that flavivirus [like dengue and Zika] can utilize the increased release of acetophenone to help itself achieve its lifecycles more effectively by making their hosts more attractive to mosquito vectors,” senior author Gong Cheng of Tsinghua University, Beijing, said in a written statement.
How do they do it? The viruses, he explained, promote the proliferation of acetophenone-producing skin bacteria. “As a result, some bacteria overreplicate and produce more acetophenone. Suddenly, these sick individuals smell as delicious to mosquitoes as a tray of freshly baked cookies to a group of five-year-old children,” the statement said.
And how do you stop a group of tiny, flying 5-year-olds? That’s right, with acne medication. Really? You knew that one but not the blood one before? The investigators fed isotretinoin to the infected mice, which led to reduced acetophenone release from skin bacteria and made the animals no more attractive to the mosquitoes than their uninfected counterparts.
The investigators are planning to take the next step – feeding isotretinoin to people with dengue and Zika – having gotten the official fictional taste-test approval of celebrity chef Gordon Ramsay, who said, “You’re going to feed this #$^% to sick people? ARE YOU &%*$@#& KIDDING ME?”
Okay, so maybe approval isn’t quite the right word.
Welcome to bladders of the rich and famous!
Don’t you hate it when you’re driving out to your multimillion-dollar second home in the Hamptons and traffic is so bad you absolutely have to find a place to “rest” along the way? But wouldn’t you know it, there just isn’t anywhere to stop! Geez, how do we live?
That’s where David Shusterman, MD, a urologist in New York City and a true American hero, comes in. He’s identified a market and positioned himself as the king of both bladder surgery and “bladder Botox” for the wealthy New Yorkers who regularly make long journeys from the city out to their second homes in the Hamptons. Traffic has increased dramatically on Long Island roads in recent years, and the journey can now taking upward of 4 hours. Some people just can’t make it that long without a bathroom break, and there are very few places to stop along the way.
Dr. Shusterman understands the plight of the Hamptons vacationer, as he told Insider.com: “I can’t tell you how many arguments I personally get into – I’ve lost three friends because I’m the driver and refuse to stop for them.” A tragedy worthy of Shakespeare himself.
During the summer season, Dr. Shusterman performs about 10 prostate artery embolizations a week, an hour-long procedure that shrinks the prostate, which is great for 50- to 60-year-old men with enlarged prostates that cause more frequent bathroom trips. He also performs Botox injections into the bladder once or twice a week for women, which reduces the need to urinate for roughly 6 months. The perfect amount of time to get them through the summer season.
These procedures are sometimes covered by insurance but can cost as much as $20,000 if paid out of pocket. That’s a lot of money to us, but if you’re the sort of person who has a second home in the Hamptons, $20,000 is chump change, especially if it means you won’t have to go 2 entire minutes out of your way to use a gas-station bathroom. Then again, having seen a more than a few gas-station bathrooms in our time, maybe they have a point.
Ditch the apples. Go for the avocados
We’ve all heard about “an apple a day,” but instead of apples you might want to go with avocados.
Avocados are generally thought to be a healthy fat. A study just published in the Journal of the American Heart Association proves that they actually don’t do anything for your waistline but will work wonders on your cholesterol level. The study involved 923 participants who were considered overweight/obese split into two groups: One was asked to consume an avocado a day, and the other continued their usual diets and were asked to consume fewer than two avocados a month.
At the end of the 6 months, the researchers found total cholesterol decreased by an additional 2.9 mg/dL and LDL cholesterol by 2.5 mg/dL in those who ate one avocado every day, compared with the usual-diet group. And even though avocados have a lot of calories, there was no clinical evidence that it impacted weight gain or any cardiometabolic risk factors, according to a statement from Penn State University.
Avocados, then, can be considered a guilt-free food. The findings from this study suggest it can give a substantial boost to your overall quality of diet, in turn lessening your risk of developing type 2 diabetes and some cancers, Kristina Peterson, PhD, assistant professor of nutritional sciences at Texas Tech University, said in the statement.
So get creative with your avocado recipes. You can only eat so much guacamole.
Your nose knows a good friend for you
You’ve probably noticed how dogs sniff other dogs and people before becoming friends. It would be pretty comical if people did the same thing, right? Just walked up to strangers and started sniffing them like dogs?
Well, apparently humans do go by smell when it comes to making friends, and they prefer people who smell like them. Maybe you’ve noticed that your friends look like you, share your values, and think the same way as you. You’re probably right, seeing as previous research has pointed to this.
For the current study, done to show how smell affects human behavior, researchers recruited people who befriended each other quickly, before knowing much about each other. They assumed that the relationships between these same-sex, nonromantic “click friends” relied more on physiological traits, including smell. After collecting samples from the click friends, researchers used an eNose to scan chemical signatures. In another experiment, human volunteers sniffed samples to determine if any were similar. Both experiments showed that click friends had more similar smells than pairs of random people.
“This is not to say that we act like goats or shrews – humans likely rely on other, far more dominant cues in their social decision-making. Nevertheless, our study’s results do suggest that our nose plays a bigger role than previously thought in our choice of friends,” said senior author Noam Sobel, PhD, of the Weizmann Institute of Science in Rehovot, Israel.
Lead author Inbal Ravreby, a graduate student at the institute, put it this way: “These results imply that, as the saying goes, there is chemistry in social chemistry.”
Pediatricians’ incomes rose faster than most specialties in 2021: Survey
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”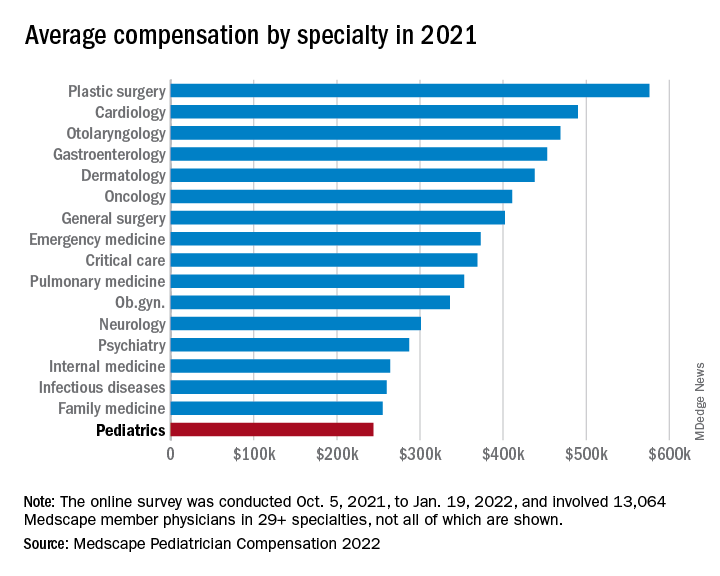
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
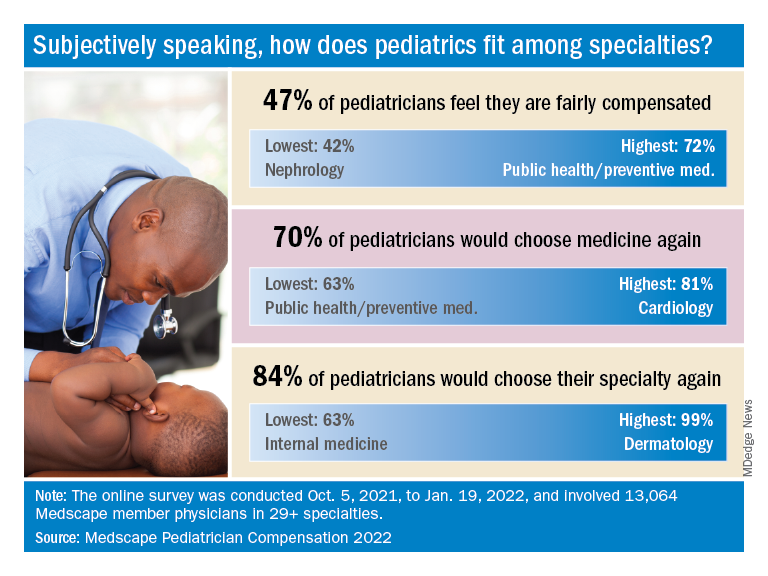
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”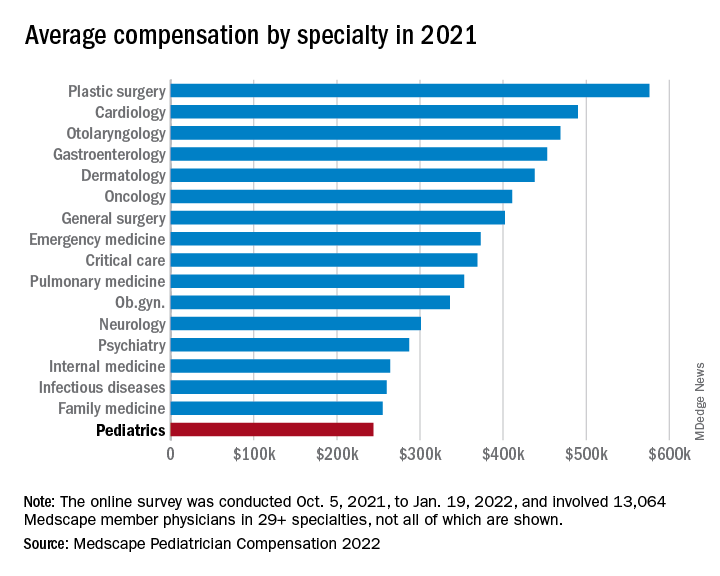
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
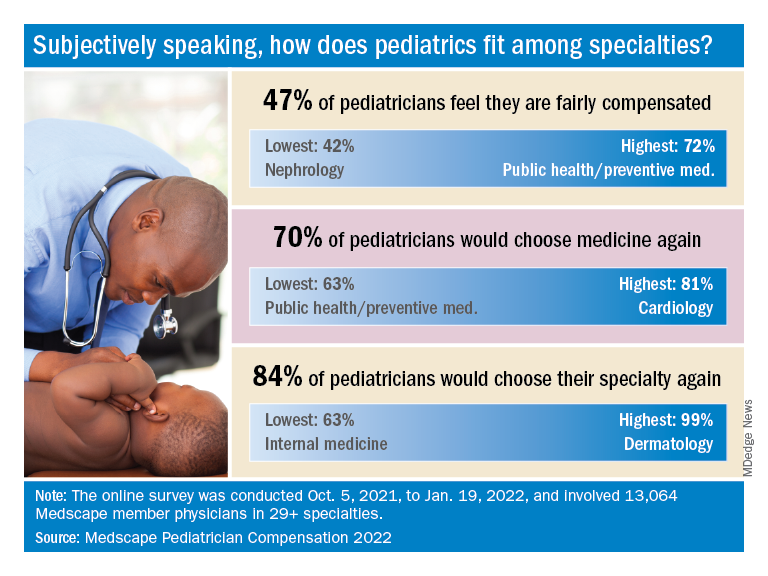
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”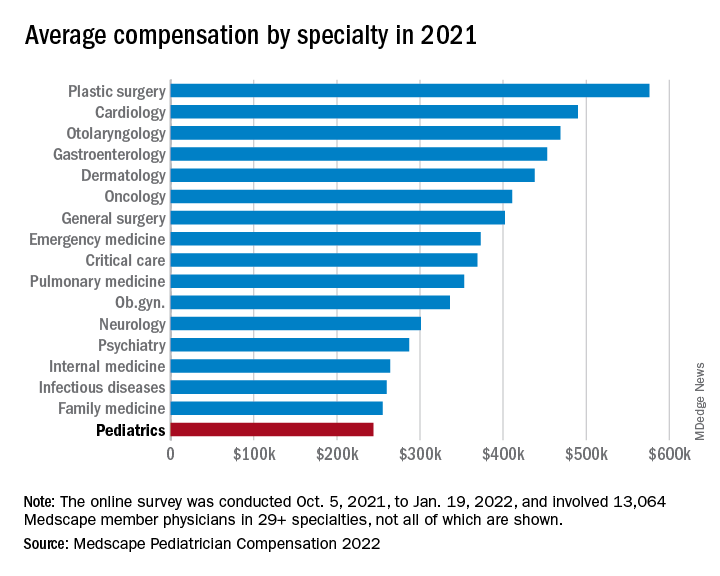
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
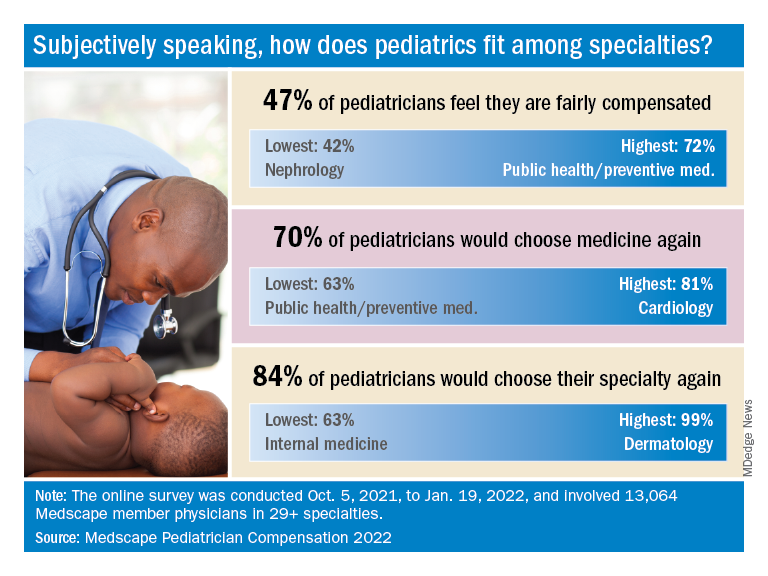
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In the Grand Canyon, norovirus gives new meaning to ‘leave no trace’
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Ain’t gastroenteritis grand?
The Grand Canyon is perhaps America’s greatest natural wonder. The mile-deep gorge of epic proportions, carved over eons by the Colorado River, elicits superlatives of the highest order from those seeing it for the first time. In the past few months, though, visitors to the Grand Canyon have been experiencing a rather more unpleasant sort of reaction: Involuntary bowel evacuation.
Since April, more than 150 river rafters and backcountry campers have fallen ill with bouts of acute gastroenteritis, likely caused by norovirus. Hey, a viral outbreak and our old friend SARS-CoV-2 isn’t involved! Hopefully it won’t get jealous. Whatever the culprit is, however, it got everywhere, as clusters of illness have popped up in unconnected parts of the park and some hikers have been restricted to a smaller portion of the park to avoid further disease spread. The majority of cases occurred in May, so it’s hoped that the outbreak is dying down, but the park remains on alert.
Now, acute gastroenteritis is certainly an unpleasant disease, but it isn’t typically a life-threatening one. There are, however, a couple of unique factors complicating this outbreak. For one, the Grand Canyon is in Arizona (duh), which can get rather hot in the summer months. Expelling waste from both ends becomes rather more dangerous when the thermometer reads over a hundred degrees, and there have been reports of multiple helicopter rescues.
That’s pretty bad, but in a way, they’re the lucky ones. How can we explain this … see, when you visit the Grand Canyon, you’re expected to follow the general rules of Leave No Trace. That means several things, but essentially, if you bring it in, you have to bring it out. Yes, that includes the various consequences of an acute gastroenteritis attack.
Forget spooky campfire stories and hungry wildlife lurking in the night, because true horror is scraping your friend’s diarrhea off the walls of the Grand Canyon into a plastic bag and stuffing it into your backpack. Probably not the sublime one-on-one Grand Canyon experience that people are expecting.
Give us a pee! ... for stem cell retrieval
Getting cells for regenerative stem cell treatment has traditionally been painful and difficult – usually they are retrieved by surgical means from bone marrow or fat tissue – but there may be an easier way.
Just pee in a cup.
Apparently, human urine contains stem cells with the potential to be used for regenerative effects. The magic ingredient? The enzyme telomerase, which “is essential for the self-renewal and potential of different types of stem cells” and is related to longevity, according to researchers at Wake Forest Institute for Regenerative Medicine.
They looked into how regenerative telomerase activity is for various capabilities beyond chromosomal stability, and whether these stem cells can become other kinds of cells for optimal tissue repair. Turns out they could, acting as a “distinct subpopulation” that has the ability not only to grow cells but also to morph into other cells, they said in a written statement.
Safety is also an issue. “Being able to use a patient’s own stem cells for therapy is considered advantageous because they do not induce immune responses or rejection,” said Anthony Atala, MD, a coauthor of the study published in Frontiers in Cell and Developmental Biology.
So less risk, easier retrieval, and great regenerative results. If this takes off, the other methods of retrieval could get flushed down the toilet.
Politicians playing the long game, literally
Before we get started with actual information, here’s a joke about politicians:
What do you call a lawyer with an IQ of 100? Your Honor.
What do you call a lawyer with an IQ of 50? Senator.
Politics is a dirty business, no doubt, so why do people do it? Is it for the prestige? Seems like everyone hates politicians, so it’s probably not that. Is it their selfless concern for the well-being of others? Probably not that either. Is it for the money? Most members of Congress have more corporate sponsors than a NASCAR driver, but we’re going to pass on that one as well.
Once again, science gives us the real answer: Longevity. Politicians live longer than the rest of us, and that longevity gap is getting wider.
Investigators looked at data from 11 industrialized countries, some of it going back to 1817, and found that politicians in the United States can expect to live about 7 years longer than the national average. The difference is around 3 years in Switzerland, 4.5 years in Germany, and 6 years in France.
“For almost all countries, politicians had similar rates of mortality to the general population in the late 19th and early 20th centuries. Throughout the 20th century, differences in mortality rates widened significantly across all countries, so that politicians had an increasing survival advantage over the general population,” they said in a written statement.
Income inequality could be a factor, but the longevity gains made by politicians, which started before the 1940s, predate the rise of their earnings relative to the rest of the population, which didn’t really get going until the 1980s, the investigators noted.
Whatever the reason, we have this closing thought regarding our long-lived lawmakers: What’s the difference between a politician and a snail? One is a slimy pest that leaves a trail everywhere. The other is a snail.
Land of the free, home of obesity
In the United States, it seems, people are becoming more comfortable with obesity. TikTok and Instagram trends often try to show the world that all sizes are beautiful. There’s also the growing popularity of the dad bod.
America, it has been said, is the land of the free. We love our freedom, and we value our individualism. If an obese man orders three meals from McDonald’s just for himself, no one is going to stop him. Many Americans also have more access to the food they want at any given time, even while they are moving around a lot less because of their sedentary lifestyles.
According to a recent study cited by the New York Post, however, America is not the only country battling obesity. Egypt and Mexico, for example, also have men with higher BMIs who cherish their individualism and the right to eat what they want, Plamen Akaliyski, PhD, of University Carlos III of Madrid, and associates, said in Social Science & Medicine.
Women are not as likely to think the same way. “Men in particular think, ‘I’m an individual, don’t tell me what to do. I’m going to eat what I want,’ ” bariatric surgeon George A. Fielding, MD, said in the Post article. Dr. Fielding also noted that women are three times more likely than men to seek bariatric surgery.
Dr. Akaliyski and associates found that Asian countries such as Japan, Singapore, and South Korea – countries that value thrift, discipline, self control, and delaying gratification – have lower rates of obesity.
So yes, we can go to the drive through of a fast food restaurant whenever we want and order whatever we want, but can doesn’t always mean should.
Children and COVID: Vaccination off to slow start for the newly eligible
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.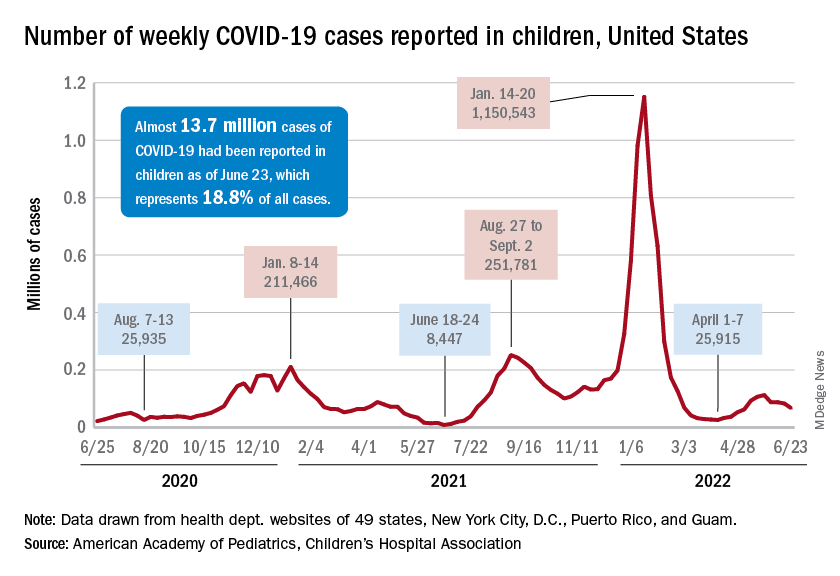
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.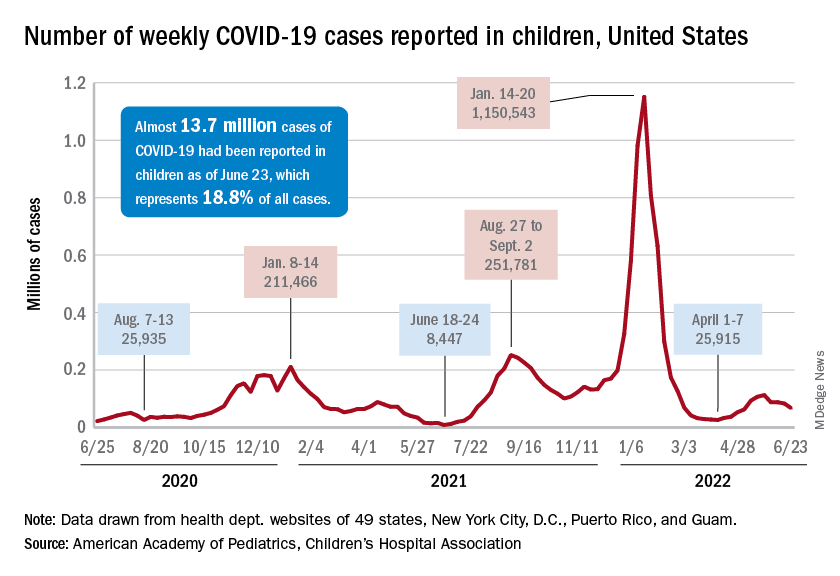
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.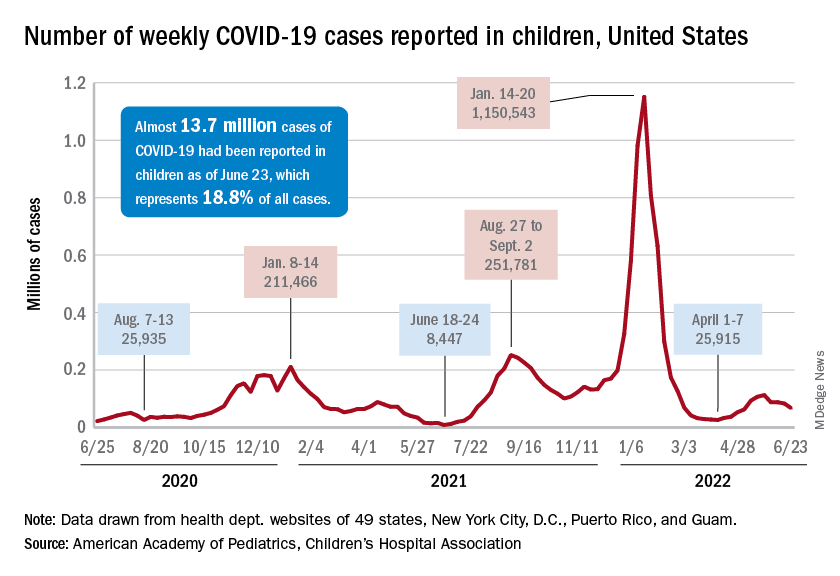
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
Artificial intelligence: The Netflix of cancer treatment
Chemotherapy, now streaming at just $15.99 a month!
It’s a lazy Sunday and you flip on Netflix, looking for something new to watch. There’s an almost-overwhelming number of shows out there, but right at the top of the recommended list is something that strikes your fancy right away. The algorithm behind the scenes is doing its job well, winnowing the universe of content right down to the few things you’ll find relevant, based on what you’ve watched and liked in the past.
Now, the almighty content algorithm is coming for something a little more useful than binge watching obscure 80s sitcoms: cancer treatment.
By plugging the fully sequenced genomes of nearly 10,000 patients with 33 different types of cancer into an algorithm powered by the same sort of artificial intelligence used by Netflix, researchers from London and San Diego found 21 common faults in the chromosomes of tumors, which they called copy number signatures. While cancer is a complex disease, when faults occur in those copy number signatures, the results were similar across the board. If X genetic defect occurs within a tumor, Y result will happen, even across cancer types. For example, tumors whose chromosomes had shattered and reformed had by far the worst disease outcomes.
The eventual hope is that, just as Netflix can predict what you’ll want to watch based on what you’ve already seen, oncologists will be able to predict the course of a cancer, based on the tumor’s early genetic traits, and get ahead of future genetic degradation to prevent the worst outcomes. A sort of “Oh, your tumor has enjoyed The Office. Might we suggest a treatment of 30 Rock” situation. Further research will be required to determine whether or not the cancer algorithm can get us part 2 of “Stranger Things 4” a week early.
Pay criminals, cut crime?
What is the best method for punishing those who commit wrongdoing? Fines? Jail time? Actually, no. A recent study says that financial compensation works best.
In other words, pay them for their actions. Really.
Psychologist Tage S. Rai, PhD, of the University of California, San Diego, Rady School of Management, found that people who hurt others or commit crimes are actually doing it because they think it’s the right thing to do. The results of this study say play at the angle of their morality. When that’s compromised, the offender is less likely to do it again.
Four different experiments were conducted using an online economics game with nearly 1,500 participants. Dr. Rai found that providing a monetary bonus for inflicting a punishment on a third party within the game cut the participants’ willingness to do it again by 50%.
“People punish others to signal their own goodness and receiving compensation might make it seem as though they’re driven by greed rather than justice,” he said.
The big deterrent, though, was negative judgment from peers. People in the study were even more hesitant to inflict harm and gain a profit if they thought they were going to be judged for it.
So maybe the answer to cutting crime isn’t as simple as slapping on a fine. It’s slapping on shame and paying them for it.
A conspiracy of chronobiologic proportions
The Golden State Warriors just won the NBA championship – that much is true – but we’ve got some news that you didn’t get from ESPN. The kind of news that their “partners” from the NBA didn’t want them to report. Unlike most conspiracy theories, however, this one has some science behind it.
In this case, science in the form of a study published in Frontiers in Physiology says that jet lag had a greater effect on the Boston Celtics than it did on the Warriors.
“Eastward travel – where the destination time is later than the origin time – requires the athlete to shorten their day (known as a phase advance). During phase advance, athletes often struggle to fall asleep at an earlier bedtime, leading to sleep loss and, consequently, potential impaired physiological performance and motivation the next day,” senior author Elise Facer-Childs, PhD, of Monash University, Melbourne, said in written statement.
Dr. Facer-Childs and associates took a very close look at 10 seasons’ worth of NBA games – 11,481 games, to be exact – and found “that eastward (but not westward) jet lag was associated with impaired performance for home (but not away) teams.” The existence of a pro-Western bias against teams that traveled eastward for their home games was clear:
- The chance of winning for eastern teams was reduced by 6.0%.
- They grabbed 1.3 fewer rebounds per game.
- Their field goal percentage was 1.2% lower.
And here’s the final nail in the conspiracy coffin: The NBA knew about the jet lag effect and changed the schedule of the finals in 2014 in a way that makes it worse. Before that, the higher-seeded team got two home games, then the lower-seeded team had three at home, followed by two more at the home of the higher seed. Now it’s a 2-2-1-1-1 arrangement that leads to more travel and, of course, more jet lag.
The study was published during the championship series, so the investigators suggested that the Celtics “might benefit from chronobiology-informed strategies designed to mitigate eastward jet lag symptomatology.”
So there you have it, sports fans/conspiracy theorists: You can’t chase Steph Curry around the court for 48 minutes without the right chronobiology-informed strategy. Everyone knows that.
Being hungry can alter your ‘type’
Fasting and being hungry can be a dangerous mix for becoming “hangry” and irritable, but did you know being hungry can also affect your attraction to other people?
Evidence has shown that being hungry can affect important things such as decision-making, memory, cognition, and function. It might affect decision-making in the sense that those six tacos at Taco Bell might win out over grilled chicken breast and veggies at home, but can hunger make you think that the person you just swiped right on isn’t really your type after all?
We’ll leave that up to Valentina Cazzato of Liverpool (England) John Moores University and associates, whose study involved 44 people, of whom 21 were women in their early 20s. The participants were shown computer-generated images of men and women of different sizes. The same background was used for each picture and all the expressions of the models were neutral. Participants were asked to rate each image on how much they liked it. One study was done on participants who had been fasting for 12 hours, and the second was done on those who had just eaten something.
The subjects generally preferred slim models over more rounded ones, but not after fasting. When they were hungry, they found the round human bodies and faces more attractive. So, yes, it’s definitely possible that hunger can alter your attraction to others.
“Future work might seek to elucidate the relationship between physiological states of hunger and shifts in appreciation of the human bodies and whether this relationship might be mediated by individual traits associated with to beholder’s body adiposity,” said researchers.
Chemotherapy, now streaming at just $15.99 a month!
It’s a lazy Sunday and you flip on Netflix, looking for something new to watch. There’s an almost-overwhelming number of shows out there, but right at the top of the recommended list is something that strikes your fancy right away. The algorithm behind the scenes is doing its job well, winnowing the universe of content right down to the few things you’ll find relevant, based on what you’ve watched and liked in the past.
Now, the almighty content algorithm is coming for something a little more useful than binge watching obscure 80s sitcoms: cancer treatment.
By plugging the fully sequenced genomes of nearly 10,000 patients with 33 different types of cancer into an algorithm powered by the same sort of artificial intelligence used by Netflix, researchers from London and San Diego found 21 common faults in the chromosomes of tumors, which they called copy number signatures. While cancer is a complex disease, when faults occur in those copy number signatures, the results were similar across the board. If X genetic defect occurs within a tumor, Y result will happen, even across cancer types. For example, tumors whose chromosomes had shattered and reformed had by far the worst disease outcomes.
The eventual hope is that, just as Netflix can predict what you’ll want to watch based on what you’ve already seen, oncologists will be able to predict the course of a cancer, based on the tumor’s early genetic traits, and get ahead of future genetic degradation to prevent the worst outcomes. A sort of “Oh, your tumor has enjoyed The Office. Might we suggest a treatment of 30 Rock” situation. Further research will be required to determine whether or not the cancer algorithm can get us part 2 of “Stranger Things 4” a week early.
Pay criminals, cut crime?
What is the best method for punishing those who commit wrongdoing? Fines? Jail time? Actually, no. A recent study says that financial compensation works best.
In other words, pay them for their actions. Really.
Psychologist Tage S. Rai, PhD, of the University of California, San Diego, Rady School of Management, found that people who hurt others or commit crimes are actually doing it because they think it’s the right thing to do. The results of this study say play at the angle of their morality. When that’s compromised, the offender is less likely to do it again.
Four different experiments were conducted using an online economics game with nearly 1,500 participants. Dr. Rai found that providing a monetary bonus for inflicting a punishment on a third party within the game cut the participants’ willingness to do it again by 50%.
“People punish others to signal their own goodness and receiving compensation might make it seem as though they’re driven by greed rather than justice,” he said.
The big deterrent, though, was negative judgment from peers. People in the study were even more hesitant to inflict harm and gain a profit if they thought they were going to be judged for it.
So maybe the answer to cutting crime isn’t as simple as slapping on a fine. It’s slapping on shame and paying them for it.
A conspiracy of chronobiologic proportions
The Golden State Warriors just won the NBA championship – that much is true – but we’ve got some news that you didn’t get from ESPN. The kind of news that their “partners” from the NBA didn’t want them to report. Unlike most conspiracy theories, however, this one has some science behind it.
In this case, science in the form of a study published in Frontiers in Physiology says that jet lag had a greater effect on the Boston Celtics than it did on the Warriors.
“Eastward travel – where the destination time is later than the origin time – requires the athlete to shorten their day (known as a phase advance). During phase advance, athletes often struggle to fall asleep at an earlier bedtime, leading to sleep loss and, consequently, potential impaired physiological performance and motivation the next day,” senior author Elise Facer-Childs, PhD, of Monash University, Melbourne, said in written statement.
Dr. Facer-Childs and associates took a very close look at 10 seasons’ worth of NBA games – 11,481 games, to be exact – and found “that eastward (but not westward) jet lag was associated with impaired performance for home (but not away) teams.” The existence of a pro-Western bias against teams that traveled eastward for their home games was clear:
- The chance of winning for eastern teams was reduced by 6.0%.
- They grabbed 1.3 fewer rebounds per game.
- Their field goal percentage was 1.2% lower.
And here’s the final nail in the conspiracy coffin: The NBA knew about the jet lag effect and changed the schedule of the finals in 2014 in a way that makes it worse. Before that, the higher-seeded team got two home games, then the lower-seeded team had three at home, followed by two more at the home of the higher seed. Now it’s a 2-2-1-1-1 arrangement that leads to more travel and, of course, more jet lag.
The study was published during the championship series, so the investigators suggested that the Celtics “might benefit from chronobiology-informed strategies designed to mitigate eastward jet lag symptomatology.”
So there you have it, sports fans/conspiracy theorists: You can’t chase Steph Curry around the court for 48 minutes without the right chronobiology-informed strategy. Everyone knows that.
Being hungry can alter your ‘type’
Fasting and being hungry can be a dangerous mix for becoming “hangry” and irritable, but did you know being hungry can also affect your attraction to other people?
Evidence has shown that being hungry can affect important things such as decision-making, memory, cognition, and function. It might affect decision-making in the sense that those six tacos at Taco Bell might win out over grilled chicken breast and veggies at home, but can hunger make you think that the person you just swiped right on isn’t really your type after all?
We’ll leave that up to Valentina Cazzato of Liverpool (England) John Moores University and associates, whose study involved 44 people, of whom 21 were women in their early 20s. The participants were shown computer-generated images of men and women of different sizes. The same background was used for each picture and all the expressions of the models were neutral. Participants were asked to rate each image on how much they liked it. One study was done on participants who had been fasting for 12 hours, and the second was done on those who had just eaten something.
The subjects generally preferred slim models over more rounded ones, but not after fasting. When they were hungry, they found the round human bodies and faces more attractive. So, yes, it’s definitely possible that hunger can alter your attraction to others.
“Future work might seek to elucidate the relationship between physiological states of hunger and shifts in appreciation of the human bodies and whether this relationship might be mediated by individual traits associated with to beholder’s body adiposity,” said researchers.
Chemotherapy, now streaming at just $15.99 a month!
It’s a lazy Sunday and you flip on Netflix, looking for something new to watch. There’s an almost-overwhelming number of shows out there, but right at the top of the recommended list is something that strikes your fancy right away. The algorithm behind the scenes is doing its job well, winnowing the universe of content right down to the few things you’ll find relevant, based on what you’ve watched and liked in the past.
Now, the almighty content algorithm is coming for something a little more useful than binge watching obscure 80s sitcoms: cancer treatment.
By plugging the fully sequenced genomes of nearly 10,000 patients with 33 different types of cancer into an algorithm powered by the same sort of artificial intelligence used by Netflix, researchers from London and San Diego found 21 common faults in the chromosomes of tumors, which they called copy number signatures. While cancer is a complex disease, when faults occur in those copy number signatures, the results were similar across the board. If X genetic defect occurs within a tumor, Y result will happen, even across cancer types. For example, tumors whose chromosomes had shattered and reformed had by far the worst disease outcomes.
The eventual hope is that, just as Netflix can predict what you’ll want to watch based on what you’ve already seen, oncologists will be able to predict the course of a cancer, based on the tumor’s early genetic traits, and get ahead of future genetic degradation to prevent the worst outcomes. A sort of “Oh, your tumor has enjoyed The Office. Might we suggest a treatment of 30 Rock” situation. Further research will be required to determine whether or not the cancer algorithm can get us part 2 of “Stranger Things 4” a week early.
Pay criminals, cut crime?
What is the best method for punishing those who commit wrongdoing? Fines? Jail time? Actually, no. A recent study says that financial compensation works best.
In other words, pay them for their actions. Really.
Psychologist Tage S. Rai, PhD, of the University of California, San Diego, Rady School of Management, found that people who hurt others or commit crimes are actually doing it because they think it’s the right thing to do. The results of this study say play at the angle of their morality. When that’s compromised, the offender is less likely to do it again.
Four different experiments were conducted using an online economics game with nearly 1,500 participants. Dr. Rai found that providing a monetary bonus for inflicting a punishment on a third party within the game cut the participants’ willingness to do it again by 50%.
“People punish others to signal their own goodness and receiving compensation might make it seem as though they’re driven by greed rather than justice,” he said.
The big deterrent, though, was negative judgment from peers. People in the study were even more hesitant to inflict harm and gain a profit if they thought they were going to be judged for it.
So maybe the answer to cutting crime isn’t as simple as slapping on a fine. It’s slapping on shame and paying them for it.
A conspiracy of chronobiologic proportions
The Golden State Warriors just won the NBA championship – that much is true – but we’ve got some news that you didn’t get from ESPN. The kind of news that their “partners” from the NBA didn’t want them to report. Unlike most conspiracy theories, however, this one has some science behind it.
In this case, science in the form of a study published in Frontiers in Physiology says that jet lag had a greater effect on the Boston Celtics than it did on the Warriors.
“Eastward travel – where the destination time is later than the origin time – requires the athlete to shorten their day (known as a phase advance). During phase advance, athletes often struggle to fall asleep at an earlier bedtime, leading to sleep loss and, consequently, potential impaired physiological performance and motivation the next day,” senior author Elise Facer-Childs, PhD, of Monash University, Melbourne, said in written statement.
Dr. Facer-Childs and associates took a very close look at 10 seasons’ worth of NBA games – 11,481 games, to be exact – and found “that eastward (but not westward) jet lag was associated with impaired performance for home (but not away) teams.” The existence of a pro-Western bias against teams that traveled eastward for their home games was clear:
- The chance of winning for eastern teams was reduced by 6.0%.
- They grabbed 1.3 fewer rebounds per game.
- Their field goal percentage was 1.2% lower.
And here’s the final nail in the conspiracy coffin: The NBA knew about the jet lag effect and changed the schedule of the finals in 2014 in a way that makes it worse. Before that, the higher-seeded team got two home games, then the lower-seeded team had three at home, followed by two more at the home of the higher seed. Now it’s a 2-2-1-1-1 arrangement that leads to more travel and, of course, more jet lag.
The study was published during the championship series, so the investigators suggested that the Celtics “might benefit from chronobiology-informed strategies designed to mitigate eastward jet lag symptomatology.”
So there you have it, sports fans/conspiracy theorists: You can’t chase Steph Curry around the court for 48 minutes without the right chronobiology-informed strategy. Everyone knows that.
Being hungry can alter your ‘type’
Fasting and being hungry can be a dangerous mix for becoming “hangry” and irritable, but did you know being hungry can also affect your attraction to other people?
Evidence has shown that being hungry can affect important things such as decision-making, memory, cognition, and function. It might affect decision-making in the sense that those six tacos at Taco Bell might win out over grilled chicken breast and veggies at home, but can hunger make you think that the person you just swiped right on isn’t really your type after all?
We’ll leave that up to Valentina Cazzato of Liverpool (England) John Moores University and associates, whose study involved 44 people, of whom 21 were women in their early 20s. The participants were shown computer-generated images of men and women of different sizes. The same background was used for each picture and all the expressions of the models were neutral. Participants were asked to rate each image on how much they liked it. One study was done on participants who had been fasting for 12 hours, and the second was done on those who had just eaten something.
The subjects generally preferred slim models over more rounded ones, but not after fasting. When they were hungry, they found the round human bodies and faces more attractive. So, yes, it’s definitely possible that hunger can alter your attraction to others.
“Future work might seek to elucidate the relationship between physiological states of hunger and shifts in appreciation of the human bodies and whether this relationship might be mediated by individual traits associated with to beholder’s body adiposity,” said researchers.























