User login
Discharge Before Noon
It is thought that late afternoon hospital discharges create admission bottlenecks in the emergency department (ED).[1] As hospital occupancy increases, so too does ED boarding time.[2] Increased ED boarding time can result in increased length of stay (LOS)[3] and reduced patient and staff satisfaction.[4] Early in the day discharge programs are intended to improve hospital throughput.[5, 6, 7, 8, 9] Yet, ED admission timing is, in part, determined by external fluctuations in ED volume and acuity that early discharges do not impact.[10] We previously reported that high levels of discharge before noon (DBN) from inpatient medicine units is achievable through a multidisciplinary intervention.[5] We now evaluate the effect of this intervention upon admission patterns and the sustainability of the DBN initiative.
The DBN intervention consisted of afternoon interdisciplinary rounds, a checklist of team members' responsibilities, a standardized electronic communication tool, and daily feedback on the DBN rate.[5] The intervention resulted in an increase in the DBN rate from 11% to 38% in the first 13 months. We previously reported effects upon the discharged patient as measured by the observed to expected length of stay (O:E LOS) and 30‐day readmission rate. We now assess the effect of our DBN initiative on the subsequent patient and hospital throughput. Our objectives for this study were: (1) to determine the effect of DBN on the admission arrival times and admissions per hour to the units, and (2) in a separate data collection and analysis, to determine if the increased DBN rate is sustainable. We hypothesize that DBN results in admissions arriving onto the units earlier in the day. We further hypothesize that because of this redistribution, DBN will level the load of admissions, reducing admissions per hour peaks that can occur late in the day.
METHODS
Study Design, Participants, and Setting
This is a pre‐/postretrospective analysis evaluating the effect of a previously described DBN intervention.[5] Two inpatient acute‐care medicine units at NYU Langone Medical Center's Tisch Hospital, a 725‐bed, urban, academic medical center, were included in the analysis. All patients admitted to the units underwent the intervention.
Intervention
The DBN intervention began with a multidisciplinary kickoff event in which all team members received education on the importance of DBN, a clear description of roles in the DBN process, and a corresponding checklist of responsibilities. The checklist was utilized at new afternoon interdisciplinary rounds intended to identify next‐day DBNs. Patients identified in afternoon interdisciplinary rounds were logged in a DBN website that generated twice‐daily automated emails to communicate the planned DBN list to frontline staff and key stakeholders. Daily, real‐time feedback on the DBN rate was provided to floor staff.
Measures
Admission Arrival Time
The arrival location and time to any hospital area (ED, radiology, inpatient medical unit) is recorded in the electronic medical record (Epic, Madison, WI) at the time the patient arrives by the patient unit assistant or unit clerk. We obtained the arrival time to each hospital unit throughout the patient's hospitalization for all patients arriving to the study units during their hospitalization between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. These time periods and exclusions match those used in our previous DBN article.[5] To match that study's criteria, we excluded patients on the units in the patient class observation, inpatient hospice, and those patients whose discharge disposition was expired or hospice.
ED Admissions
All patients with a first inpatient unit location of ED and no other inpatient unit location prior to arrival on the study units were included in the ED admission analysis. Units that treat but do not provide long‐term boarding/housing of inpatientssuch as radiology, hemodialysis, and cardiac catheterizationwere not considered in determining ED admission status. Even if a patient had recorded arrival to those areas between ED and study unit arrival, these patients were considered ED admissions, as they were never admitted to another inpatient unit.
Transfers and Direct Admissions
All patients whose first inpatient unit location was the study units were included in the transfers and direct admissions analysis. Those patients who were recorded as coming from another inpatient unit (such as another medical, surgical, step‐down, intensive care, or other specialty unit) prior to study unit arrival were included as intrahospital transfers.
Level Load of Admissions
Level loading is a lean methodology term that describes reducing the unevenness in a production line to enhance efficiency.[11] We evaluated this by comparing the admissions per hour (density distribution) to the studied units in the pre‐ and postintervention periods.
Sustainability of the DBN Intervention
The DBN intervention, as described in our original article, continues uninterrupted. Using the same methodology, inclusion criteria, exclusion criteria, and data analysis previously described, we gathered the discharge date and time as recorded by the patient unit assistant for all patients discharged from the study units for the 18 months (July 1, 2013 to December 31, 2014) after our original article to evaluate the sustainability of our improvement in DBN rates.
Statistical Analysis
Median admission time to the floor was compared between the 2 time periods using the Wilcoxon rank sum test. This is a non parametric test of the null hypothesis that the two time periods have the same distributions of admission time to the floor. To evaluate statistical significance, each admission time is arranged in order of magnitude and assigned a rank. The sum of the ranks for each group is calculated and the smaller rank sum (the W statistic) is compared to an expected range of values based on the sample sizes. If this value is out of range then one can reject the null hypothesis. The density distributions of admissions during the 2 time periods were compared using the Kolmogorov‐Smirnov test. The 2‐sided Kolmogorov‐Smirnov test evaluates the maximum distance (D) between the distributions of 2 samples.[12] We chose this test because it evaluates differences between both the position and shape of the distributions of the samples.
RESULTS
Setting Characteristics
The units had an average occupancy rate of 86.8% for the duration of the study. The average number of total discharges per day was 9.8. The average absolute length of stay was 5.6 days.
Admission Arrival Time to the Unit
ED Admissions
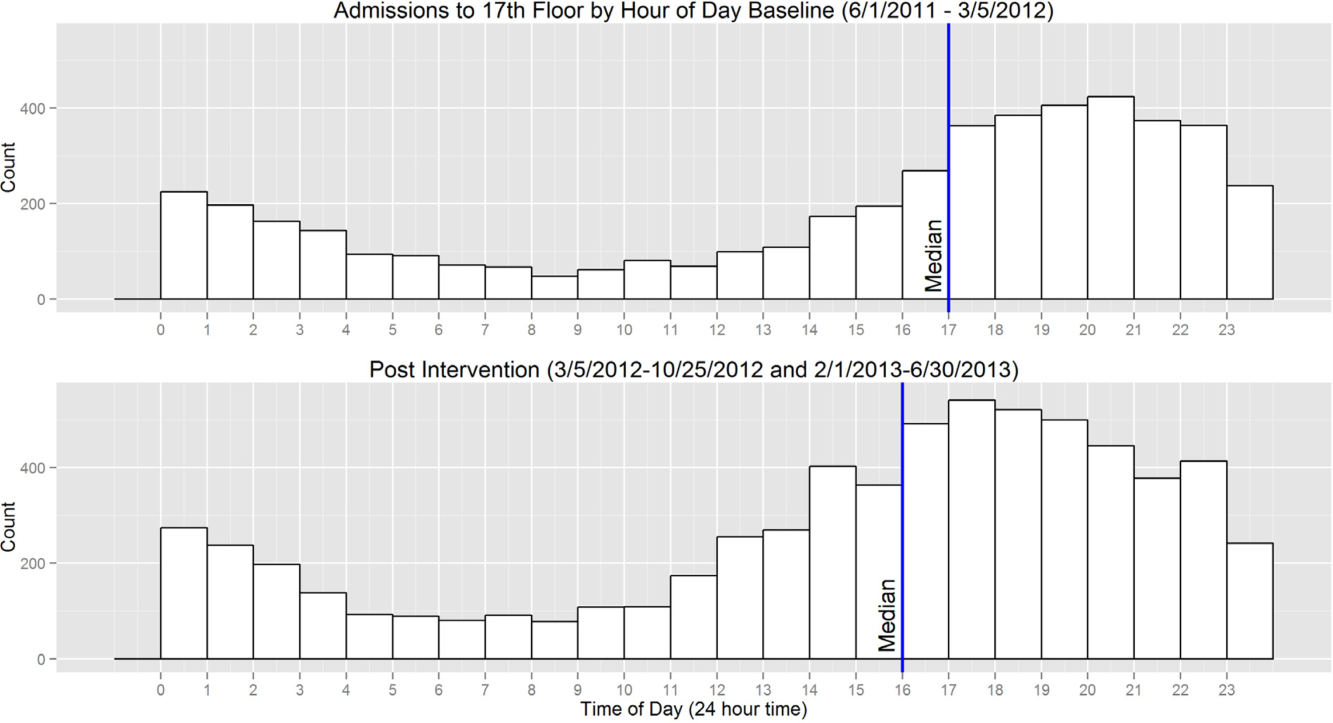
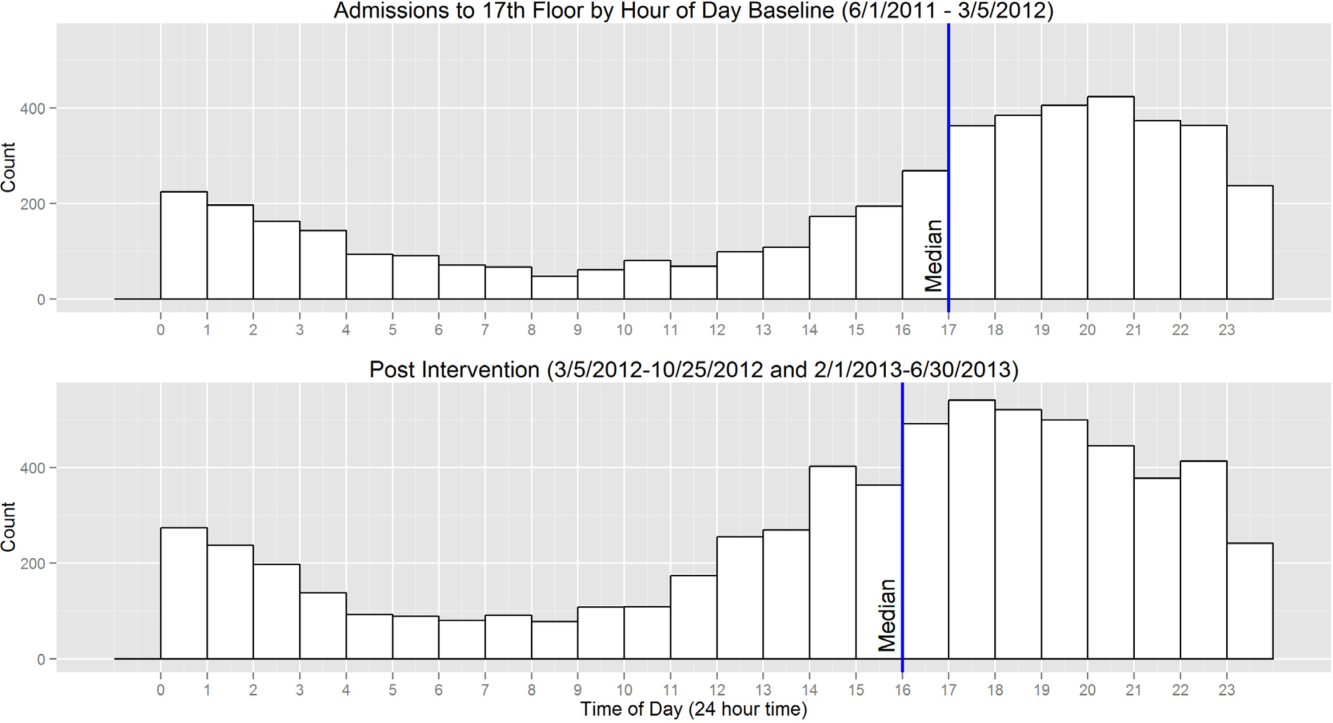
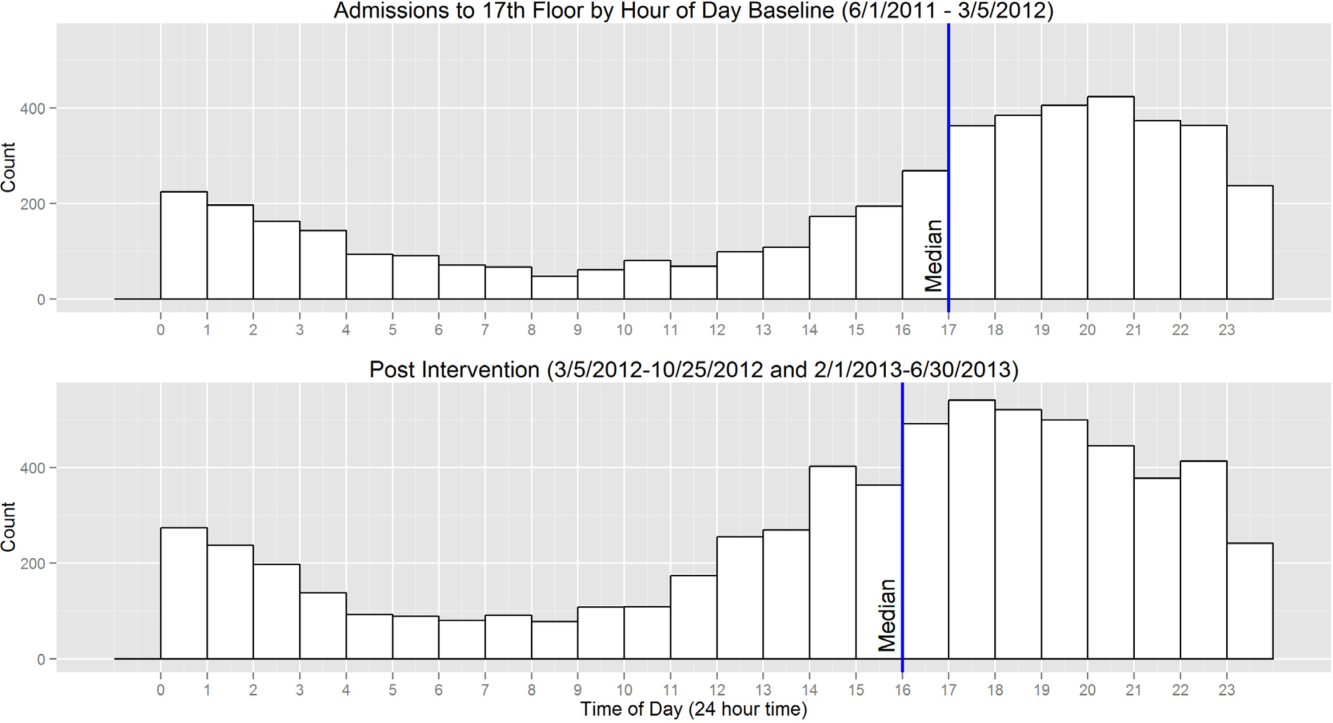
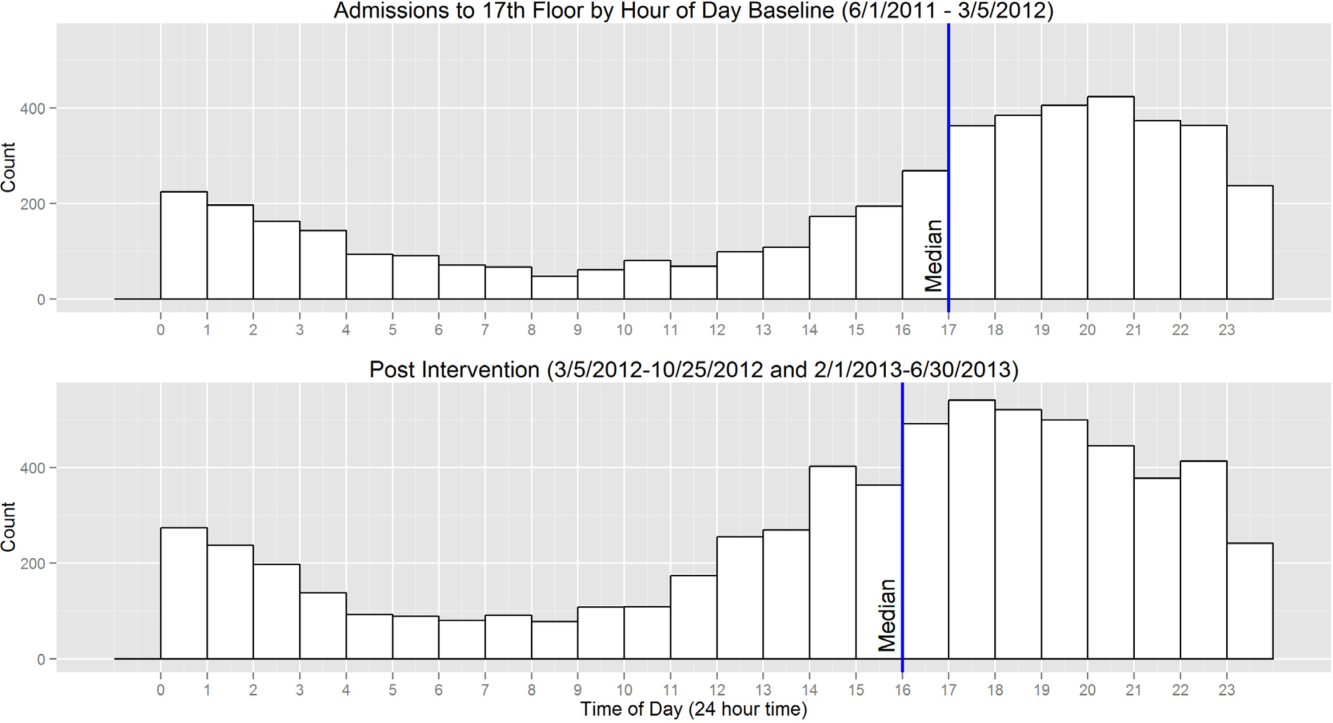
A total of 6566 patients were admitted from the ED to the units, 2756 in the baseline period and 3810 in the intervention period. The median arrival time to the units of ED admissions grouped by hour of the day moved by 1 hour, from 5 pm to 4 pm from the baseline to intervention period, and this change was statistically significant (W=16,211,778, P<0.01) (Figure 1).
Transfers and Direct Admissions
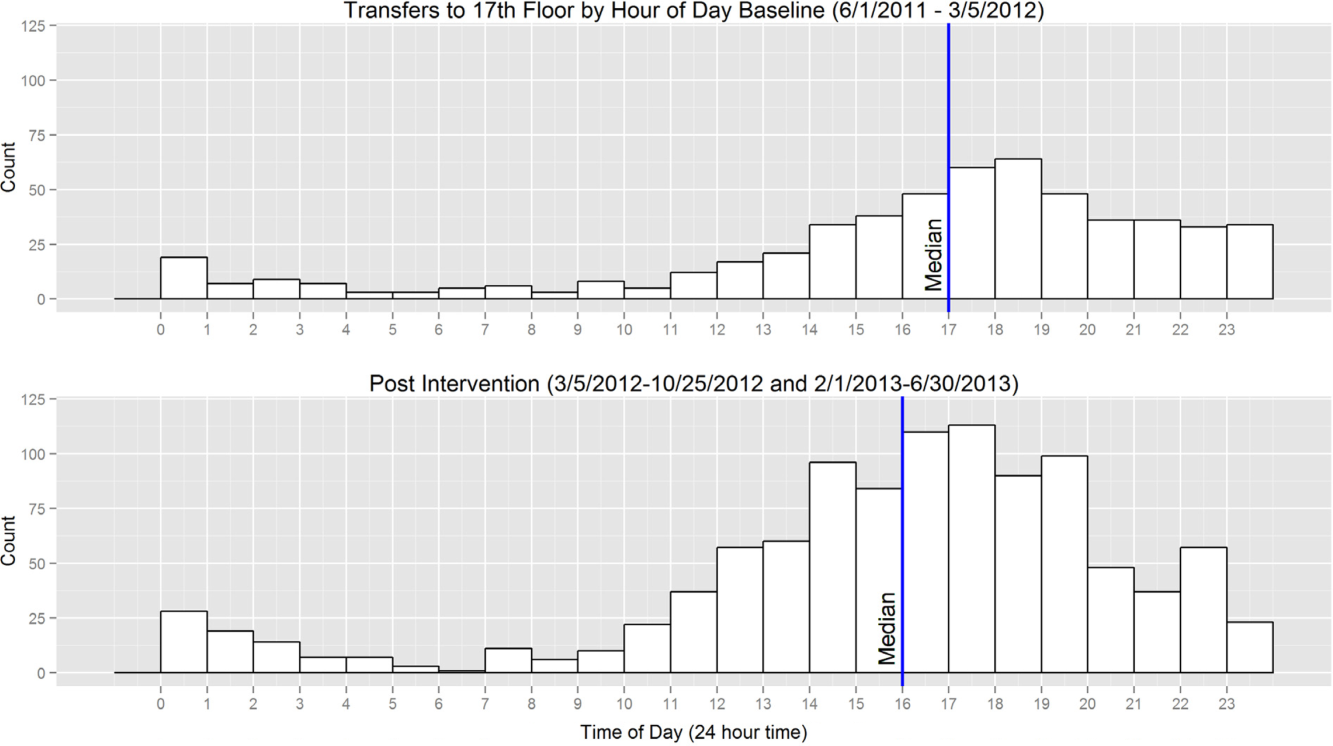
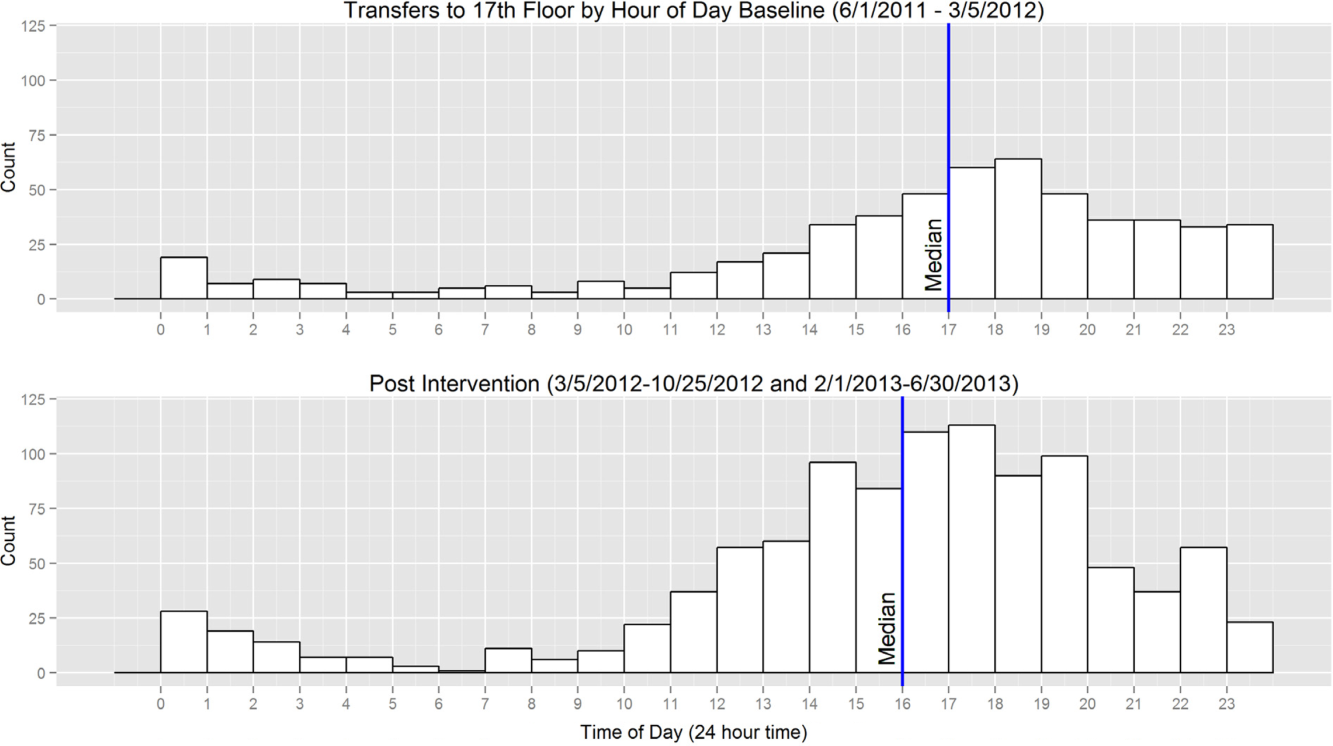
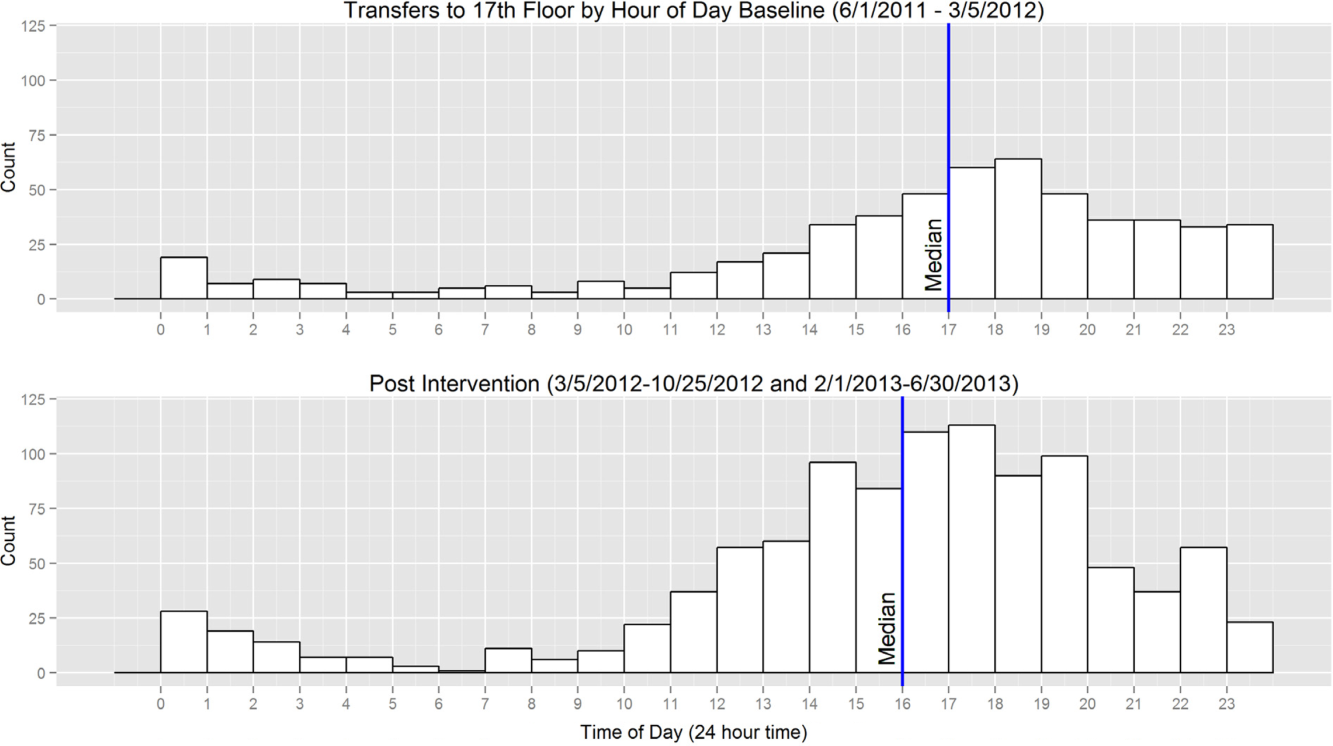
A total of 823 patients were transferred or directly admitted to the units, 310 in the baseline period and 513 in the intervention period. The median arrival time to the units grouped by hour of the day moved 1 hour from 5 pm to 4 pm, and this change was statistically significant (W=324,532, P<0.01) (Figure 2).
Level Load of Admissions
In the baseline period, the highest density of ED admissions occurred during the 5‐hour period from 5 pm to 10 pm, when 42.3% of daily admissions arrived (Figure 3). In the intervention period, the highest density of admissions occurred during the 5‐hour period from 3 pm to 8 pm, when 40.0% of daily admissions arrived. The difference between the density distributions for the 2 time periods was found to be statistically significant using the Kolmogorov‐Smirnov test (D=0.03, P<0.01).
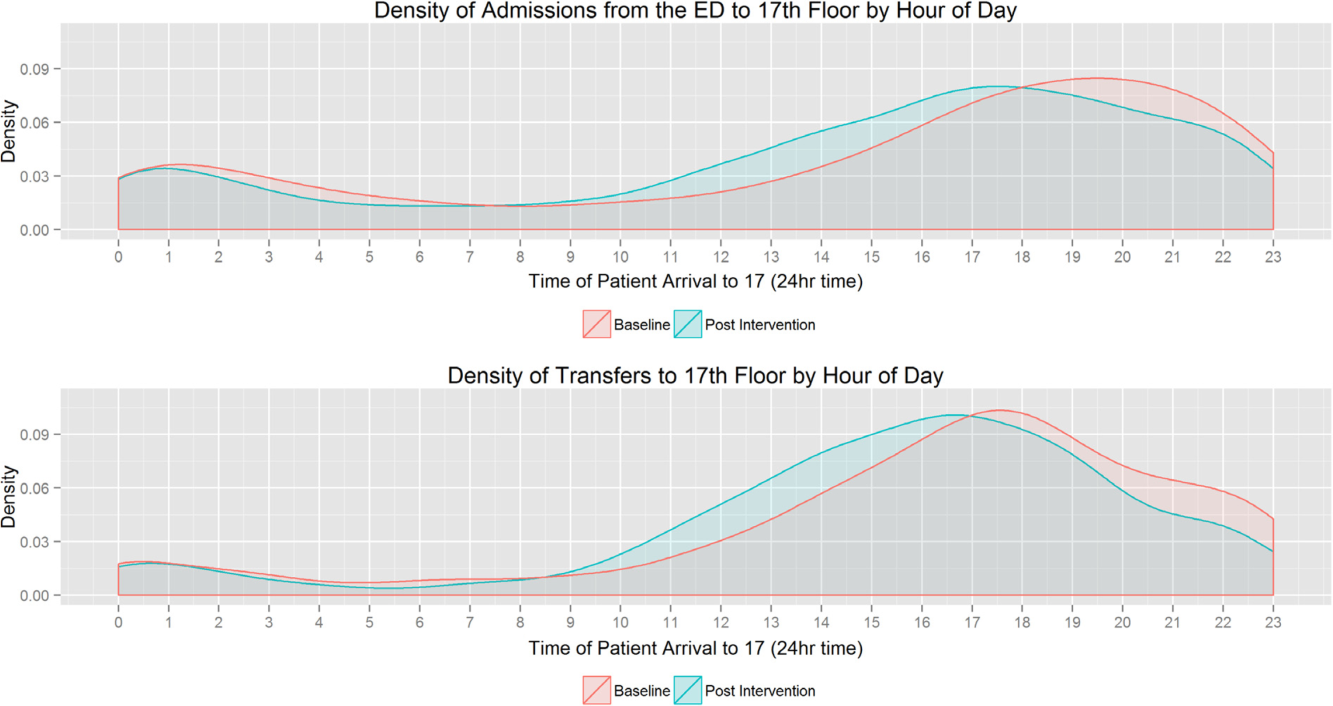
In the baseline period, the highest density of transfers and direct admissions occurred during the 5‐hour period from 3 pm to 8 pm, when 51.7% of daily admissions arrived (Figure 3). In the intervention time period, the highest density of transfers and direct admissions occurred during the 5‐hour time period from 2 pm to 7 pm, when 50.3% of daily admissions arrived. The difference between the density distributions of transfers and direct admissions for the 2 time periods was not statistically significant using the Kolmogorov‐Smirnov test (D=0.04, P=0.3).
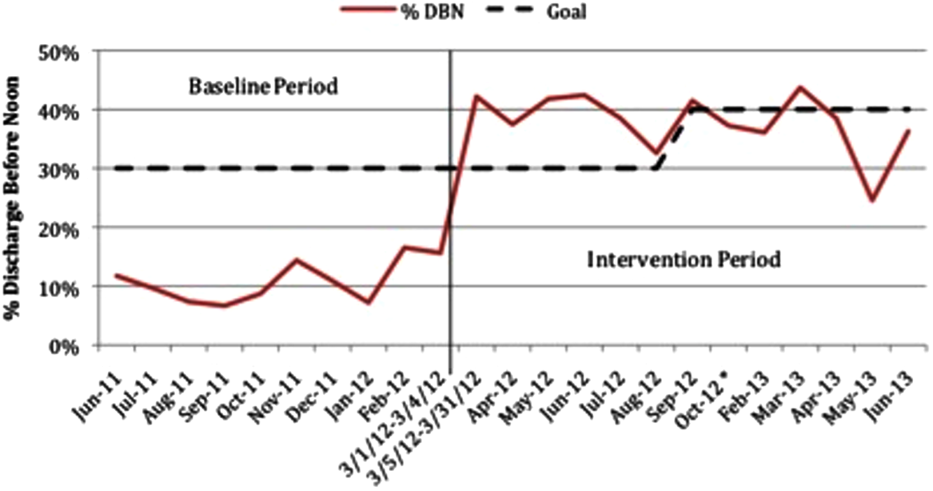
Sustainability of the DBN Intervention
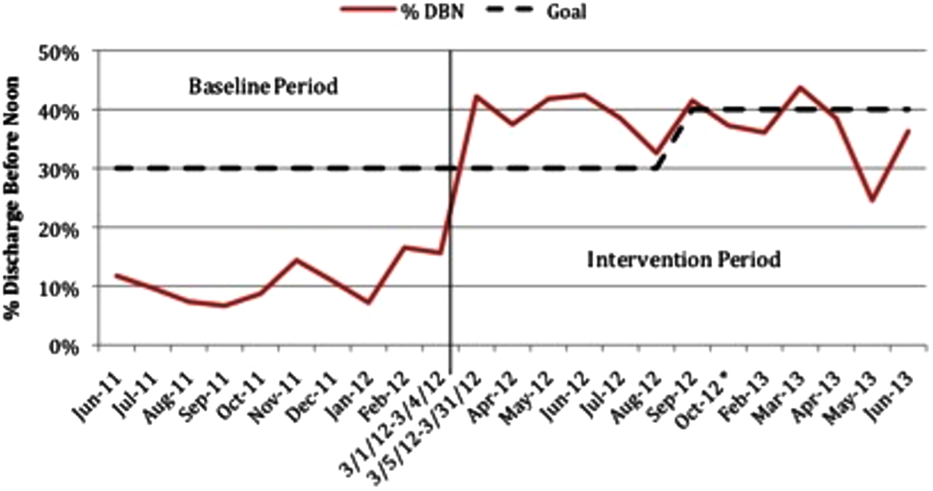
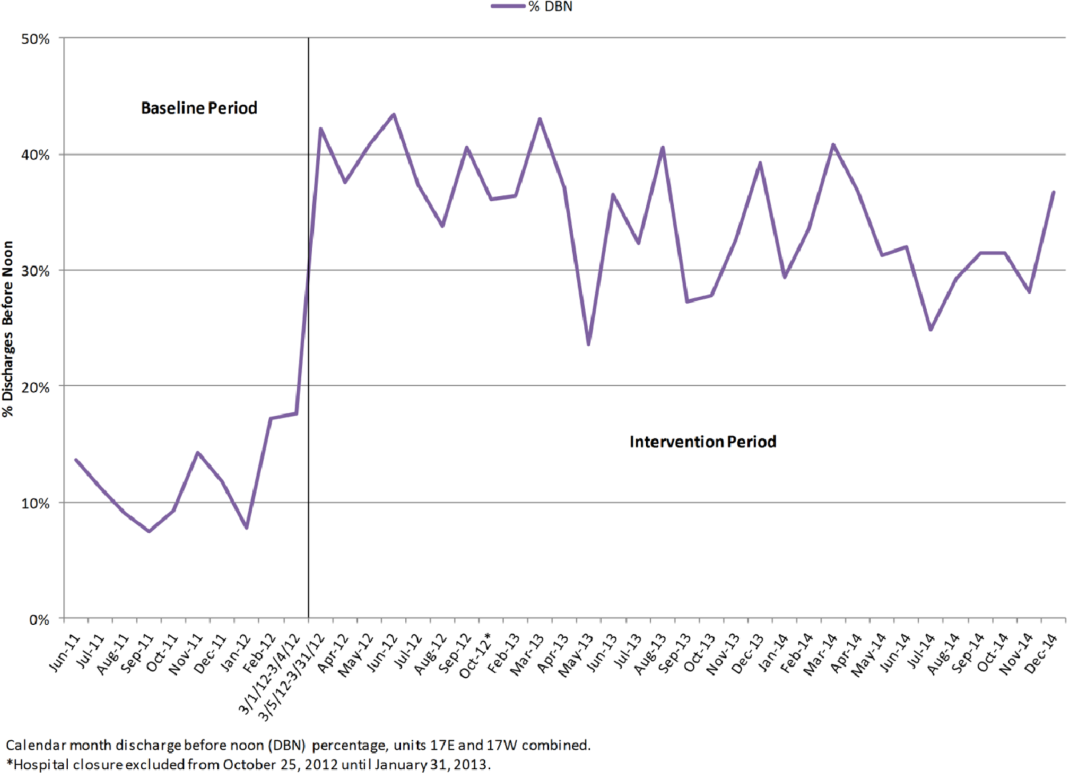
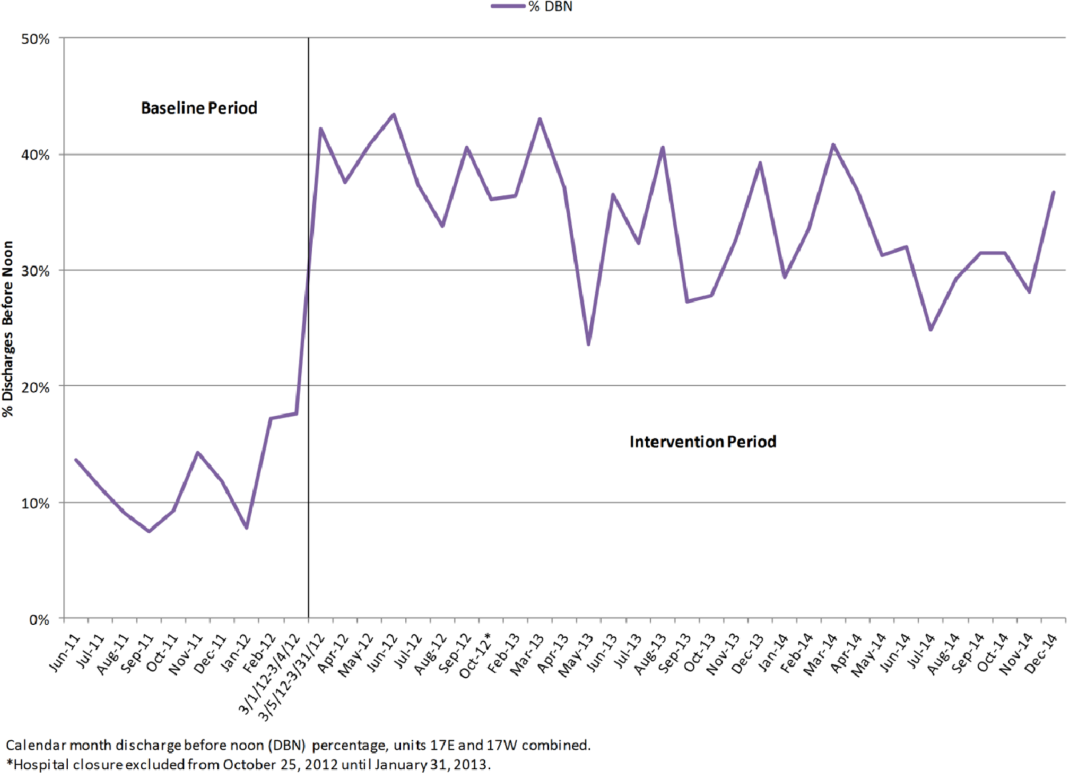
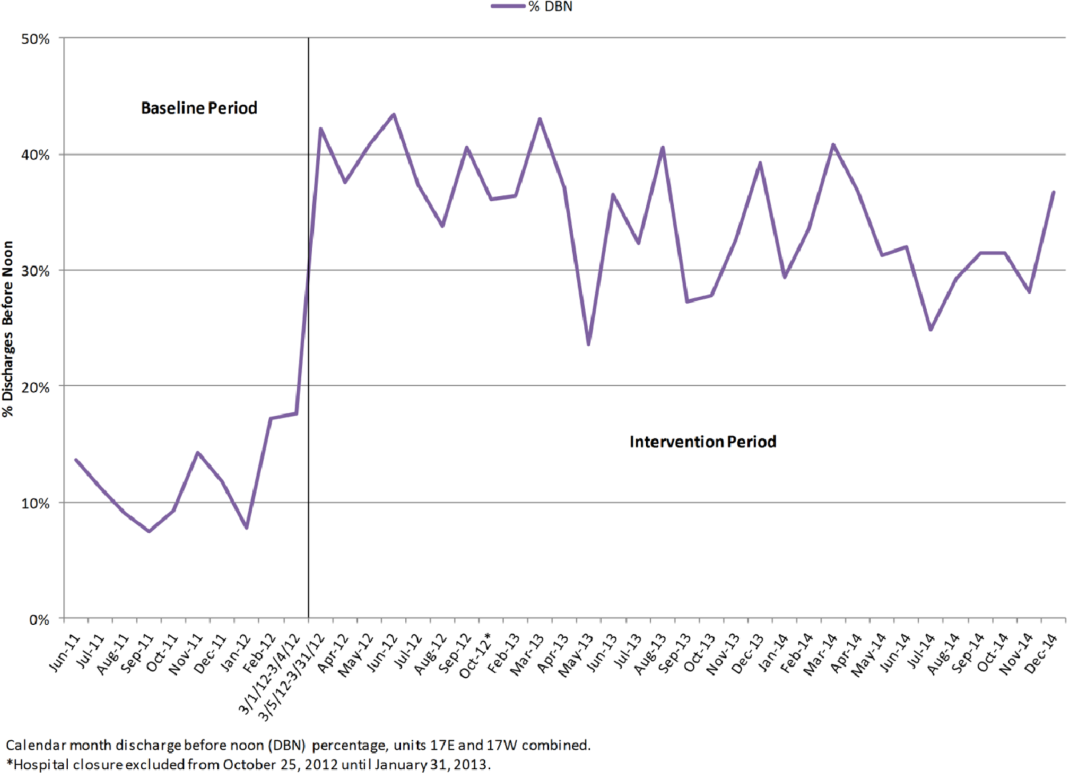
For the 18 months after the prior reported DBN intervention period, an additional 5505 total discharges were included for analysis. Of these, 1796 were DBN. The average DBN rate for the study units from March 5, 2012 until December 31, 2014 (the original intervention period plus the additional 18 months of new data) is 35% (Figure 4).
DISCUSSION
The potential effects of DBN are multiple. By reducing the O:E LOS and allowing patients the time to acquire their medications, make follow‐up appointments, and ask questions while providers are still in the hospital, our DBN initiative impacts the discharged patient's quality, safety, and efficiency of care.[5] We now report how the DBN initiative potentially impacts the subsequent patient's efficiency of care and hospital throughput. In addition, we show that the DBN initiative is sustainable over years.
Over the same time course as our initial DBN intervention, we found a statistically significant change in the time when admitted patients arrive on the floor. This was true of those patients admitted through the ED and those directly admitted to the floor. In a complex hospital system with many factors both internal (bed cleaning, patient transportation) and external (natural variations in ED volume and acuity) affecting the timing of admissions, it is important to note that increasing the DBN rate correlates with a change in median admission arrival time. From a patient safety standpoint, any initiative that moves admissions away from evening and night hours and takes advantage of (usually more robust) day staffing is a potentially favorable intervention.[13]
We observed a statistically significant reduction of highest frequency peaks of ED admissions. It appears that opening beds up earlier in the day through DBN may help level the load of admissions from the ED. There was no effect on highest frequency peaks of transfer admissions to the floor. This may be due to the timing of transfers being dependent on factors other than bed availability, such as timing of transportation to the hospital or the timing of planned treatment.
We also found that the DBN intervention has created sustainable increases in the DBN rate. Since our initial publication, we have received direct communication from physicians, administrators and managers in 6 different states and 2 foreign countries asking for additional information or reporting that their hospitals are pursuing similar goals. Some of the most common questions asked include: Are your results sustained? and What do you think is a reasonable DBN goal? We have attempted to answer both of these questions. We previously reported improvement to an average DBN rate of 38% over the first 13 intervention months. With more time, we now see an absolute DBN rate of 35%. In November 2014, we restructured our medicine service to become geographic, so that the same group of doctors, trainees, nurses, care managers, and social workers care for patients on a single ward. Since this initiative, our DBN rate has climbed to greater than 40%. We hope to report further on this new intervention in the future. Similar hospital centers can consider using our experience on an inpatient acute‐care medical unit in an urban environment as a benchmark for setting hospital metric goals for early‐in‐the‐day discharge.
Several studies have previously reported on early‐in‐the‐day discharge initiatives. These were smaller studies that focused on descriptions of the type of intervention, including a discharge brunch on an obstetrics floor,[8] scheduled discharges,[6] in‐room displays of expected day and time of discharge,[9] and a physician‐centered discharge process.[7] Our study is substantially larger, focused on inpatient medicine units, and reports the effect of significant changes in DBN on patient and hospital metrics.
Our study had several limitations. The study is based in a single site, potentially limiting the generalizability of our findings. The hospital underwent tremendous change during the course of the intervention, including its temporary closure due to Hurricane Sandy. We cannot exclude effects related to shifts in volume and possible differences in the pre‐ and post‐time period patient populations. The prior study evaluated the population of discharged patients, but the admission analysis in this study involves the population of admitted patients. There may be slight differences in the populations due to the inclusion of patients who were admitted but not discharged from the units (for instance due to transfer after admission). Though the findings on admission arrival time correlate well with the increasing DBN rates, as they occur during the same time and in the same direction (earlier in the day), we are unable to conclude if the effect is causative. There were many interventions ongoing throughout the hospital to improve throughput, and these programs could have created local trends that confound our data. We are also unable to evaluate the clinical significance of a 1‐hour shift in median admission arrival time. Each hospital system must determine for itself if the time and resource investment in DBN is worth the change in admission timing described. We completed this analysis with the perspective of the inpatient medical unit experience, including the timing and number of admissions arriving to the units. We cannot exclude the possibility that changes in arrival times or boarding trends in the ED contribute to our findings.
CONCLUSION
In our hospital, a successful DBN initiative correlates with movement of ED admissions and transfers onto the inpatient units earlier in the day. There was a leveling of the load for ED admissions over the same time period. DBN continues to be an achievable hospital goal, and we provide a potential benchmark for similar hospitals.
Disclosure
Nothing to report.
- , , , Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , et al. Time series analysis of emergency department length of stay per 8‐hour shift. West J Emerg Med. 2012;13(2):163–168.
- , , , , , Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , , et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014;9(4):210–214.
- , , All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , , , , , Emergency department crowding: factors influencing flow. West J Emerg Med. 2010;11(1):10–15.
- The Toyota Way: 14 Management Principles From the World's Greatest Manufacturer. New York, NY: McGraw‐Hill; 2004.
- Comparing Distributions. New York, NY: Springer; 2010.
- , , , et al. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792.
It is thought that late afternoon hospital discharges create admission bottlenecks in the emergency department (ED).[1] As hospital occupancy increases, so too does ED boarding time.[2] Increased ED boarding time can result in increased length of stay (LOS)[3] and reduced patient and staff satisfaction.[4] Early in the day discharge programs are intended to improve hospital throughput.[5, 6, 7, 8, 9] Yet, ED admission timing is, in part, determined by external fluctuations in ED volume and acuity that early discharges do not impact.[10] We previously reported that high levels of discharge before noon (DBN) from inpatient medicine units is achievable through a multidisciplinary intervention.[5] We now evaluate the effect of this intervention upon admission patterns and the sustainability of the DBN initiative.
The DBN intervention consisted of afternoon interdisciplinary rounds, a checklist of team members' responsibilities, a standardized electronic communication tool, and daily feedback on the DBN rate.[5] The intervention resulted in an increase in the DBN rate from 11% to 38% in the first 13 months. We previously reported effects upon the discharged patient as measured by the observed to expected length of stay (O:E LOS) and 30‐day readmission rate. We now assess the effect of our DBN initiative on the subsequent patient and hospital throughput. Our objectives for this study were: (1) to determine the effect of DBN on the admission arrival times and admissions per hour to the units, and (2) in a separate data collection and analysis, to determine if the increased DBN rate is sustainable. We hypothesize that DBN results in admissions arriving onto the units earlier in the day. We further hypothesize that because of this redistribution, DBN will level the load of admissions, reducing admissions per hour peaks that can occur late in the day.
METHODS
Study Design, Participants, and Setting
This is a pre‐/postretrospective analysis evaluating the effect of a previously described DBN intervention.[5] Two inpatient acute‐care medicine units at NYU Langone Medical Center's Tisch Hospital, a 725‐bed, urban, academic medical center, were included in the analysis. All patients admitted to the units underwent the intervention.
Intervention
The DBN intervention began with a multidisciplinary kickoff event in which all team members received education on the importance of DBN, a clear description of roles in the DBN process, and a corresponding checklist of responsibilities. The checklist was utilized at new afternoon interdisciplinary rounds intended to identify next‐day DBNs. Patients identified in afternoon interdisciplinary rounds were logged in a DBN website that generated twice‐daily automated emails to communicate the planned DBN list to frontline staff and key stakeholders. Daily, real‐time feedback on the DBN rate was provided to floor staff.
Measures
Admission Arrival Time
The arrival location and time to any hospital area (ED, radiology, inpatient medical unit) is recorded in the electronic medical record (Epic, Madison, WI) at the time the patient arrives by the patient unit assistant or unit clerk. We obtained the arrival time to each hospital unit throughout the patient's hospitalization for all patients arriving to the study units during their hospitalization between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. These time periods and exclusions match those used in our previous DBN article.[5] To match that study's criteria, we excluded patients on the units in the patient class observation, inpatient hospice, and those patients whose discharge disposition was expired or hospice.
ED Admissions
All patients with a first inpatient unit location of ED and no other inpatient unit location prior to arrival on the study units were included in the ED admission analysis. Units that treat but do not provide long‐term boarding/housing of inpatientssuch as radiology, hemodialysis, and cardiac catheterizationwere not considered in determining ED admission status. Even if a patient had recorded arrival to those areas between ED and study unit arrival, these patients were considered ED admissions, as they were never admitted to another inpatient unit.
Transfers and Direct Admissions
All patients whose first inpatient unit location was the study units were included in the transfers and direct admissions analysis. Those patients who were recorded as coming from another inpatient unit (such as another medical, surgical, step‐down, intensive care, or other specialty unit) prior to study unit arrival were included as intrahospital transfers.
Level Load of Admissions
Level loading is a lean methodology term that describes reducing the unevenness in a production line to enhance efficiency.[11] We evaluated this by comparing the admissions per hour (density distribution) to the studied units in the pre‐ and postintervention periods.
Sustainability of the DBN Intervention
The DBN intervention, as described in our original article, continues uninterrupted. Using the same methodology, inclusion criteria, exclusion criteria, and data analysis previously described, we gathered the discharge date and time as recorded by the patient unit assistant for all patients discharged from the study units for the 18 months (July 1, 2013 to December 31, 2014) after our original article to evaluate the sustainability of our improvement in DBN rates.
Statistical Analysis
Median admission time to the floor was compared between the 2 time periods using the Wilcoxon rank sum test. This is a non parametric test of the null hypothesis that the two time periods have the same distributions of admission time to the floor. To evaluate statistical significance, each admission time is arranged in order of magnitude and assigned a rank. The sum of the ranks for each group is calculated and the smaller rank sum (the W statistic) is compared to an expected range of values based on the sample sizes. If this value is out of range then one can reject the null hypothesis. The density distributions of admissions during the 2 time periods were compared using the Kolmogorov‐Smirnov test. The 2‐sided Kolmogorov‐Smirnov test evaluates the maximum distance (D) between the distributions of 2 samples.[12] We chose this test because it evaluates differences between both the position and shape of the distributions of the samples.
RESULTS
Setting Characteristics
The units had an average occupancy rate of 86.8% for the duration of the study. The average number of total discharges per day was 9.8. The average absolute length of stay was 5.6 days.
Admission Arrival Time to the Unit
ED Admissions
A total of 6566 patients were admitted from the ED to the units, 2756 in the baseline period and 3810 in the intervention period. The median arrival time to the units of ED admissions grouped by hour of the day moved by 1 hour, from 5 pm to 4 pm from the baseline to intervention period, and this change was statistically significant (W=16,211,778, P<0.01) (Figure 1).
Transfers and Direct Admissions
A total of 823 patients were transferred or directly admitted to the units, 310 in the baseline period and 513 in the intervention period. The median arrival time to the units grouped by hour of the day moved 1 hour from 5 pm to 4 pm, and this change was statistically significant (W=324,532, P<0.01) (Figure 2).
Level Load of Admissions
In the baseline period, the highest density of ED admissions occurred during the 5‐hour period from 5 pm to 10 pm, when 42.3% of daily admissions arrived (Figure 3). In the intervention period, the highest density of admissions occurred during the 5‐hour period from 3 pm to 8 pm, when 40.0% of daily admissions arrived. The difference between the density distributions for the 2 time periods was found to be statistically significant using the Kolmogorov‐Smirnov test (D=0.03, P<0.01).
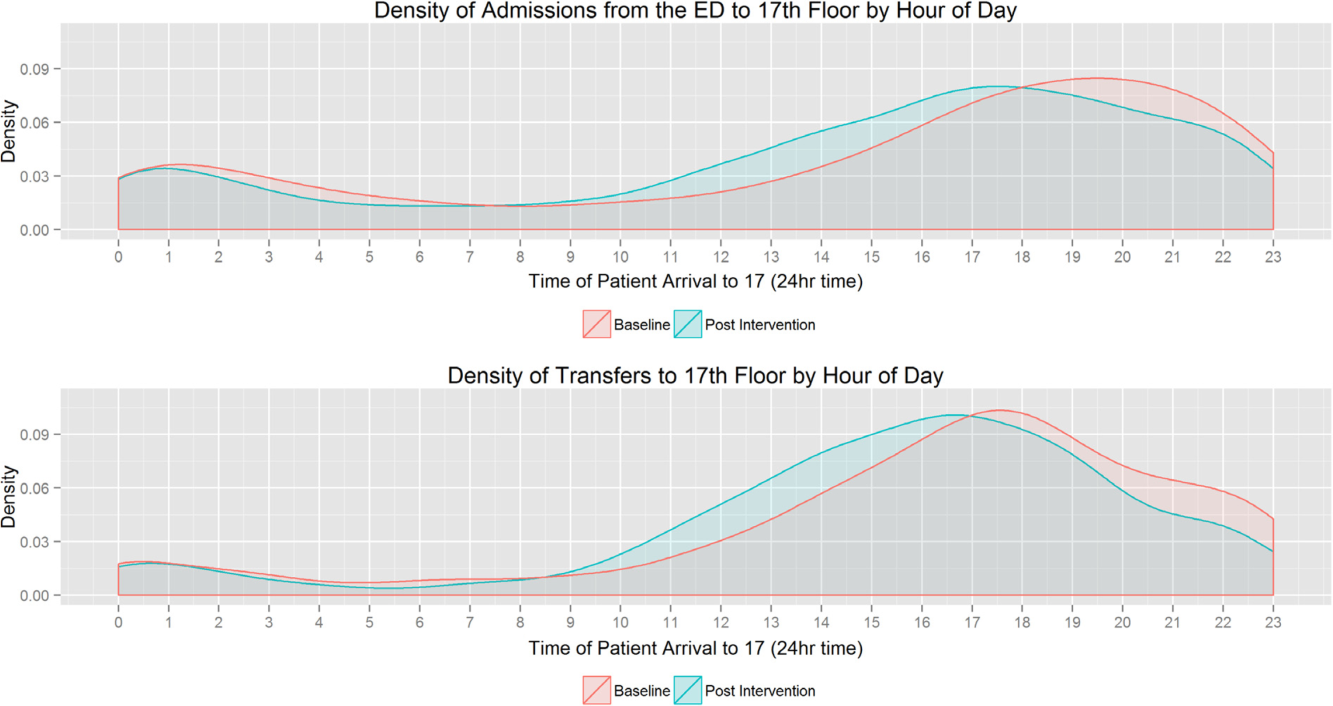
In the baseline period, the highest density of transfers and direct admissions occurred during the 5‐hour period from 3 pm to 8 pm, when 51.7% of daily admissions arrived (Figure 3). In the intervention time period, the highest density of transfers and direct admissions occurred during the 5‐hour time period from 2 pm to 7 pm, when 50.3% of daily admissions arrived. The difference between the density distributions of transfers and direct admissions for the 2 time periods was not statistically significant using the Kolmogorov‐Smirnov test (D=0.04, P=0.3).
Sustainability of the DBN Intervention
For the 18 months after the prior reported DBN intervention period, an additional 5505 total discharges were included for analysis. Of these, 1796 were DBN. The average DBN rate for the study units from March 5, 2012 until December 31, 2014 (the original intervention period plus the additional 18 months of new data) is 35% (Figure 4).
DISCUSSION
The potential effects of DBN are multiple. By reducing the O:E LOS and allowing patients the time to acquire their medications, make follow‐up appointments, and ask questions while providers are still in the hospital, our DBN initiative impacts the discharged patient's quality, safety, and efficiency of care.[5] We now report how the DBN initiative potentially impacts the subsequent patient's efficiency of care and hospital throughput. In addition, we show that the DBN initiative is sustainable over years.
Over the same time course as our initial DBN intervention, we found a statistically significant change in the time when admitted patients arrive on the floor. This was true of those patients admitted through the ED and those directly admitted to the floor. In a complex hospital system with many factors both internal (bed cleaning, patient transportation) and external (natural variations in ED volume and acuity) affecting the timing of admissions, it is important to note that increasing the DBN rate correlates with a change in median admission arrival time. From a patient safety standpoint, any initiative that moves admissions away from evening and night hours and takes advantage of (usually more robust) day staffing is a potentially favorable intervention.[13]
We observed a statistically significant reduction of highest frequency peaks of ED admissions. It appears that opening beds up earlier in the day through DBN may help level the load of admissions from the ED. There was no effect on highest frequency peaks of transfer admissions to the floor. This may be due to the timing of transfers being dependent on factors other than bed availability, such as timing of transportation to the hospital or the timing of planned treatment.
We also found that the DBN intervention has created sustainable increases in the DBN rate. Since our initial publication, we have received direct communication from physicians, administrators and managers in 6 different states and 2 foreign countries asking for additional information or reporting that their hospitals are pursuing similar goals. Some of the most common questions asked include: Are your results sustained? and What do you think is a reasonable DBN goal? We have attempted to answer both of these questions. We previously reported improvement to an average DBN rate of 38% over the first 13 intervention months. With more time, we now see an absolute DBN rate of 35%. In November 2014, we restructured our medicine service to become geographic, so that the same group of doctors, trainees, nurses, care managers, and social workers care for patients on a single ward. Since this initiative, our DBN rate has climbed to greater than 40%. We hope to report further on this new intervention in the future. Similar hospital centers can consider using our experience on an inpatient acute‐care medical unit in an urban environment as a benchmark for setting hospital metric goals for early‐in‐the‐day discharge.
Several studies have previously reported on early‐in‐the‐day discharge initiatives. These were smaller studies that focused on descriptions of the type of intervention, including a discharge brunch on an obstetrics floor,[8] scheduled discharges,[6] in‐room displays of expected day and time of discharge,[9] and a physician‐centered discharge process.[7] Our study is substantially larger, focused on inpatient medicine units, and reports the effect of significant changes in DBN on patient and hospital metrics.
Our study had several limitations. The study is based in a single site, potentially limiting the generalizability of our findings. The hospital underwent tremendous change during the course of the intervention, including its temporary closure due to Hurricane Sandy. We cannot exclude effects related to shifts in volume and possible differences in the pre‐ and post‐time period patient populations. The prior study evaluated the population of discharged patients, but the admission analysis in this study involves the population of admitted patients. There may be slight differences in the populations due to the inclusion of patients who were admitted but not discharged from the units (for instance due to transfer after admission). Though the findings on admission arrival time correlate well with the increasing DBN rates, as they occur during the same time and in the same direction (earlier in the day), we are unable to conclude if the effect is causative. There were many interventions ongoing throughout the hospital to improve throughput, and these programs could have created local trends that confound our data. We are also unable to evaluate the clinical significance of a 1‐hour shift in median admission arrival time. Each hospital system must determine for itself if the time and resource investment in DBN is worth the change in admission timing described. We completed this analysis with the perspective of the inpatient medical unit experience, including the timing and number of admissions arriving to the units. We cannot exclude the possibility that changes in arrival times or boarding trends in the ED contribute to our findings.
CONCLUSION
In our hospital, a successful DBN initiative correlates with movement of ED admissions and transfers onto the inpatient units earlier in the day. There was a leveling of the load for ED admissions over the same time period. DBN continues to be an achievable hospital goal, and we provide a potential benchmark for similar hospitals.
Disclosure
Nothing to report.
It is thought that late afternoon hospital discharges create admission bottlenecks in the emergency department (ED).[1] As hospital occupancy increases, so too does ED boarding time.[2] Increased ED boarding time can result in increased length of stay (LOS)[3] and reduced patient and staff satisfaction.[4] Early in the day discharge programs are intended to improve hospital throughput.[5, 6, 7, 8, 9] Yet, ED admission timing is, in part, determined by external fluctuations in ED volume and acuity that early discharges do not impact.[10] We previously reported that high levels of discharge before noon (DBN) from inpatient medicine units is achievable through a multidisciplinary intervention.[5] We now evaluate the effect of this intervention upon admission patterns and the sustainability of the DBN initiative.
The DBN intervention consisted of afternoon interdisciplinary rounds, a checklist of team members' responsibilities, a standardized electronic communication tool, and daily feedback on the DBN rate.[5] The intervention resulted in an increase in the DBN rate from 11% to 38% in the first 13 months. We previously reported effects upon the discharged patient as measured by the observed to expected length of stay (O:E LOS) and 30‐day readmission rate. We now assess the effect of our DBN initiative on the subsequent patient and hospital throughput. Our objectives for this study were: (1) to determine the effect of DBN on the admission arrival times and admissions per hour to the units, and (2) in a separate data collection and analysis, to determine if the increased DBN rate is sustainable. We hypothesize that DBN results in admissions arriving onto the units earlier in the day. We further hypothesize that because of this redistribution, DBN will level the load of admissions, reducing admissions per hour peaks that can occur late in the day.
METHODS
Study Design, Participants, and Setting
This is a pre‐/postretrospective analysis evaluating the effect of a previously described DBN intervention.[5] Two inpatient acute‐care medicine units at NYU Langone Medical Center's Tisch Hospital, a 725‐bed, urban, academic medical center, were included in the analysis. All patients admitted to the units underwent the intervention.
Intervention
The DBN intervention began with a multidisciplinary kickoff event in which all team members received education on the importance of DBN, a clear description of roles in the DBN process, and a corresponding checklist of responsibilities. The checklist was utilized at new afternoon interdisciplinary rounds intended to identify next‐day DBNs. Patients identified in afternoon interdisciplinary rounds were logged in a DBN website that generated twice‐daily automated emails to communicate the planned DBN list to frontline staff and key stakeholders. Daily, real‐time feedback on the DBN rate was provided to floor staff.
Measures
Admission Arrival Time
The arrival location and time to any hospital area (ED, radiology, inpatient medical unit) is recorded in the electronic medical record (Epic, Madison, WI) at the time the patient arrives by the patient unit assistant or unit clerk. We obtained the arrival time to each hospital unit throughout the patient's hospitalization for all patients arriving to the study units during their hospitalization between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. These time periods and exclusions match those used in our previous DBN article.[5] To match that study's criteria, we excluded patients on the units in the patient class observation, inpatient hospice, and those patients whose discharge disposition was expired or hospice.
ED Admissions
All patients with a first inpatient unit location of ED and no other inpatient unit location prior to arrival on the study units were included in the ED admission analysis. Units that treat but do not provide long‐term boarding/housing of inpatientssuch as radiology, hemodialysis, and cardiac catheterizationwere not considered in determining ED admission status. Even if a patient had recorded arrival to those areas between ED and study unit arrival, these patients were considered ED admissions, as they were never admitted to another inpatient unit.
Transfers and Direct Admissions
All patients whose first inpatient unit location was the study units were included in the transfers and direct admissions analysis. Those patients who were recorded as coming from another inpatient unit (such as another medical, surgical, step‐down, intensive care, or other specialty unit) prior to study unit arrival were included as intrahospital transfers.
Level Load of Admissions
Level loading is a lean methodology term that describes reducing the unevenness in a production line to enhance efficiency.[11] We evaluated this by comparing the admissions per hour (density distribution) to the studied units in the pre‐ and postintervention periods.
Sustainability of the DBN Intervention
The DBN intervention, as described in our original article, continues uninterrupted. Using the same methodology, inclusion criteria, exclusion criteria, and data analysis previously described, we gathered the discharge date and time as recorded by the patient unit assistant for all patients discharged from the study units for the 18 months (July 1, 2013 to December 31, 2014) after our original article to evaluate the sustainability of our improvement in DBN rates.
Statistical Analysis
Median admission time to the floor was compared between the 2 time periods using the Wilcoxon rank sum test. This is a non parametric test of the null hypothesis that the two time periods have the same distributions of admission time to the floor. To evaluate statistical significance, each admission time is arranged in order of magnitude and assigned a rank. The sum of the ranks for each group is calculated and the smaller rank sum (the W statistic) is compared to an expected range of values based on the sample sizes. If this value is out of range then one can reject the null hypothesis. The density distributions of admissions during the 2 time periods were compared using the Kolmogorov‐Smirnov test. The 2‐sided Kolmogorov‐Smirnov test evaluates the maximum distance (D) between the distributions of 2 samples.[12] We chose this test because it evaluates differences between both the position and shape of the distributions of the samples.
RESULTS
Setting Characteristics
The units had an average occupancy rate of 86.8% for the duration of the study. The average number of total discharges per day was 9.8. The average absolute length of stay was 5.6 days.
Admission Arrival Time to the Unit
ED Admissions
A total of 6566 patients were admitted from the ED to the units, 2756 in the baseline period and 3810 in the intervention period. The median arrival time to the units of ED admissions grouped by hour of the day moved by 1 hour, from 5 pm to 4 pm from the baseline to intervention period, and this change was statistically significant (W=16,211,778, P<0.01) (Figure 1).
Transfers and Direct Admissions
A total of 823 patients were transferred or directly admitted to the units, 310 in the baseline period and 513 in the intervention period. The median arrival time to the units grouped by hour of the day moved 1 hour from 5 pm to 4 pm, and this change was statistically significant (W=324,532, P<0.01) (Figure 2).
Level Load of Admissions
In the baseline period, the highest density of ED admissions occurred during the 5‐hour period from 5 pm to 10 pm, when 42.3% of daily admissions arrived (Figure 3). In the intervention period, the highest density of admissions occurred during the 5‐hour period from 3 pm to 8 pm, when 40.0% of daily admissions arrived. The difference between the density distributions for the 2 time periods was found to be statistically significant using the Kolmogorov‐Smirnov test (D=0.03, P<0.01).
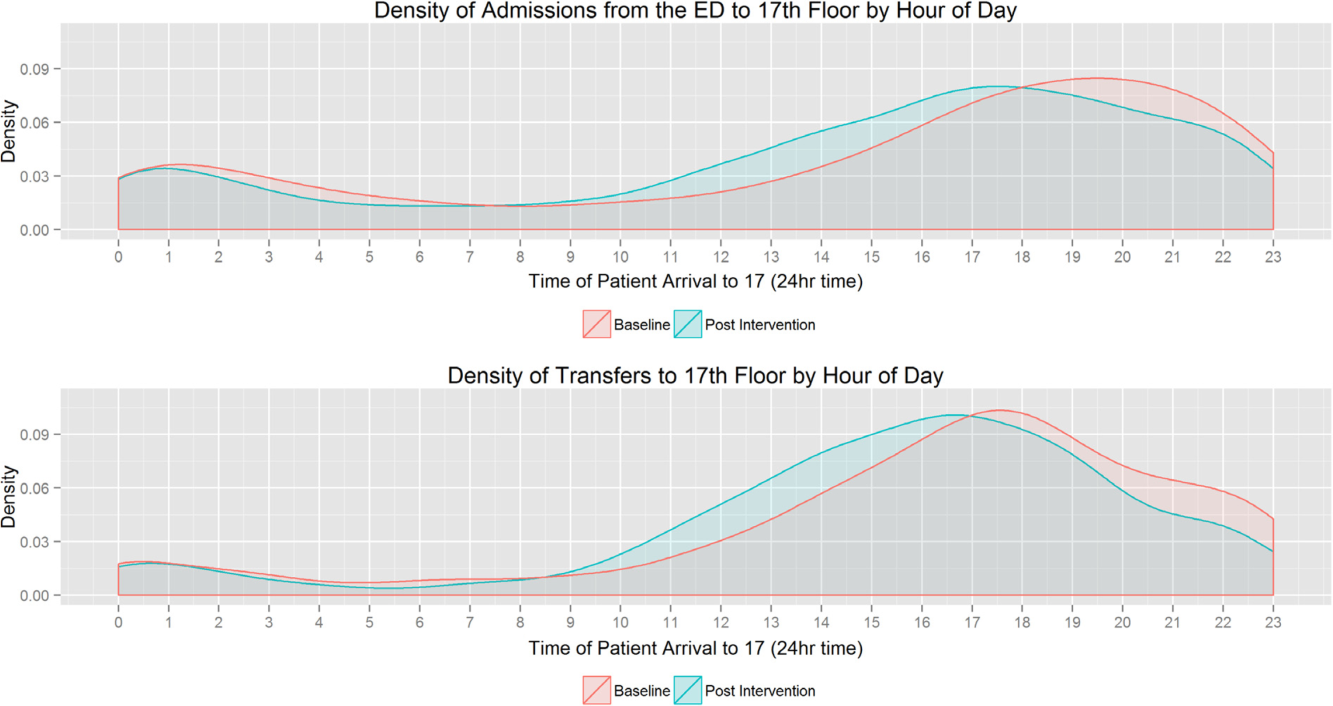
In the baseline period, the highest density of transfers and direct admissions occurred during the 5‐hour period from 3 pm to 8 pm, when 51.7% of daily admissions arrived (Figure 3). In the intervention time period, the highest density of transfers and direct admissions occurred during the 5‐hour time period from 2 pm to 7 pm, when 50.3% of daily admissions arrived. The difference between the density distributions of transfers and direct admissions for the 2 time periods was not statistically significant using the Kolmogorov‐Smirnov test (D=0.04, P=0.3).
Sustainability of the DBN Intervention
For the 18 months after the prior reported DBN intervention period, an additional 5505 total discharges were included for analysis. Of these, 1796 were DBN. The average DBN rate for the study units from March 5, 2012 until December 31, 2014 (the original intervention period plus the additional 18 months of new data) is 35% (Figure 4).
DISCUSSION
The potential effects of DBN are multiple. By reducing the O:E LOS and allowing patients the time to acquire their medications, make follow‐up appointments, and ask questions while providers are still in the hospital, our DBN initiative impacts the discharged patient's quality, safety, and efficiency of care.[5] We now report how the DBN initiative potentially impacts the subsequent patient's efficiency of care and hospital throughput. In addition, we show that the DBN initiative is sustainable over years.
Over the same time course as our initial DBN intervention, we found a statistically significant change in the time when admitted patients arrive on the floor. This was true of those patients admitted through the ED and those directly admitted to the floor. In a complex hospital system with many factors both internal (bed cleaning, patient transportation) and external (natural variations in ED volume and acuity) affecting the timing of admissions, it is important to note that increasing the DBN rate correlates with a change in median admission arrival time. From a patient safety standpoint, any initiative that moves admissions away from evening and night hours and takes advantage of (usually more robust) day staffing is a potentially favorable intervention.[13]
We observed a statistically significant reduction of highest frequency peaks of ED admissions. It appears that opening beds up earlier in the day through DBN may help level the load of admissions from the ED. There was no effect on highest frequency peaks of transfer admissions to the floor. This may be due to the timing of transfers being dependent on factors other than bed availability, such as timing of transportation to the hospital or the timing of planned treatment.
We also found that the DBN intervention has created sustainable increases in the DBN rate. Since our initial publication, we have received direct communication from physicians, administrators and managers in 6 different states and 2 foreign countries asking for additional information or reporting that their hospitals are pursuing similar goals. Some of the most common questions asked include: Are your results sustained? and What do you think is a reasonable DBN goal? We have attempted to answer both of these questions. We previously reported improvement to an average DBN rate of 38% over the first 13 intervention months. With more time, we now see an absolute DBN rate of 35%. In November 2014, we restructured our medicine service to become geographic, so that the same group of doctors, trainees, nurses, care managers, and social workers care for patients on a single ward. Since this initiative, our DBN rate has climbed to greater than 40%. We hope to report further on this new intervention in the future. Similar hospital centers can consider using our experience on an inpatient acute‐care medical unit in an urban environment as a benchmark for setting hospital metric goals for early‐in‐the‐day discharge.
Several studies have previously reported on early‐in‐the‐day discharge initiatives. These were smaller studies that focused on descriptions of the type of intervention, including a discharge brunch on an obstetrics floor,[8] scheduled discharges,[6] in‐room displays of expected day and time of discharge,[9] and a physician‐centered discharge process.[7] Our study is substantially larger, focused on inpatient medicine units, and reports the effect of significant changes in DBN on patient and hospital metrics.
Our study had several limitations. The study is based in a single site, potentially limiting the generalizability of our findings. The hospital underwent tremendous change during the course of the intervention, including its temporary closure due to Hurricane Sandy. We cannot exclude effects related to shifts in volume and possible differences in the pre‐ and post‐time period patient populations. The prior study evaluated the population of discharged patients, but the admission analysis in this study involves the population of admitted patients. There may be slight differences in the populations due to the inclusion of patients who were admitted but not discharged from the units (for instance due to transfer after admission). Though the findings on admission arrival time correlate well with the increasing DBN rates, as they occur during the same time and in the same direction (earlier in the day), we are unable to conclude if the effect is causative. There were many interventions ongoing throughout the hospital to improve throughput, and these programs could have created local trends that confound our data. We are also unable to evaluate the clinical significance of a 1‐hour shift in median admission arrival time. Each hospital system must determine for itself if the time and resource investment in DBN is worth the change in admission timing described. We completed this analysis with the perspective of the inpatient medical unit experience, including the timing and number of admissions arriving to the units. We cannot exclude the possibility that changes in arrival times or boarding trends in the ED contribute to our findings.
CONCLUSION
In our hospital, a successful DBN initiative correlates with movement of ED admissions and transfers onto the inpatient units earlier in the day. There was a leveling of the load for ED admissions over the same time period. DBN continues to be an achievable hospital goal, and we provide a potential benchmark for similar hospitals.
Disclosure
Nothing to report.
- , , , Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , et al. Time series analysis of emergency department length of stay per 8‐hour shift. West J Emerg Med. 2012;13(2):163–168.
- , , , , , Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , , et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014;9(4):210–214.
- , , All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , , , , , Emergency department crowding: factors influencing flow. West J Emerg Med. 2010;11(1):10–15.
- The Toyota Way: 14 Management Principles From the World's Greatest Manufacturer. New York, NY: McGraw‐Hill; 2004.
- Comparing Distributions. New York, NY: Springer; 2010.
- , , , et al. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792.
- , , , Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , et al. Time series analysis of emergency department length of stay per 8‐hour shift. West J Emerg Med. 2012;13(2):163–168.
- , , , , , Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , , et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014;9(4):210–214.
- , , All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , , , , , Emergency department crowding: factors influencing flow. West J Emerg Med. 2010;11(1):10–15.
- The Toyota Way: 14 Management Principles From the World's Greatest Manufacturer. New York, NY: McGraw‐Hill; 2004.
- Comparing Distributions. New York, NY: Springer; 2010.
- , , , et al. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792.
© 2015 Society of Hospital Medicine
Discharge Before Noon
Late afternoon hospital discharges are thought to create admission bottlenecks in the emergency department (ED).[1] ED overcrowding increases the length of stay (LOS) of patients[2] and is a major dissatisfier for both patients and staff.[3] In our medical center, ED patients who are admitted after 1:00 pm have a 0.6‐day longer risk‐adjusted LOS than those admitted before 1:00 pm (M. Radford, MD, written communication, March 2012).
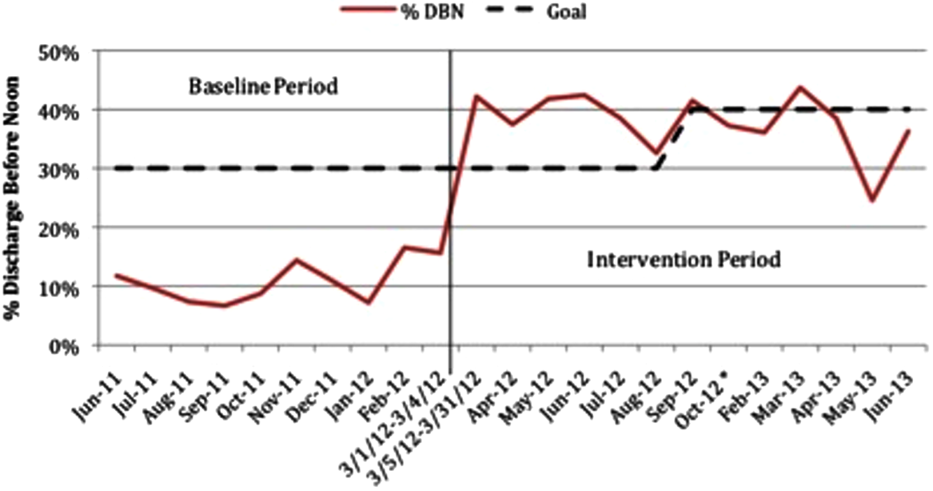
Many potential barriers to discharging patients early in the day exist.[4] However, comprehensive discharge planning favorably impacts discharge times.[5] There are limited published data regarding discharging patients early in the day. Studies have focused on improved discharge care coordination,[6, 7] in‐room display of planned discharge time,[8] and a discharge brunch.[9] In January 2012, the calendar month discharge before noon (DBN) percentage for 2 inpatient medicine units in our institution was approximately 7%, well below the organizational goal of 30%. We describe an intervention to sustainably increase the DBN percentage.
METHODS
Setting
The intervention took place on the 17th floor of New York University (NYU) Langone Medical Center's Tisch Hospital, an urban, academic medical center. All patients on the 17th floor received the intervention.
The 17th floor is composed of 2 acute care inpatient medical units17E and 17W. Each unit has 35 medical beds including a 16‐bed medical step down unit (SDU). Medical teams on the floor consist of 4 housestaff teams, a nurse practitioner (NP) team, and an SDU team. Each housestaff and NP team is led by a hospitalist, who is the attending of record for the majority of patients, though some patients on these teams are cared for by private attendings. Medical teams admit patients to any unit based upon bed availability. Nurses are assigned patients by acuity, not by medical team.
Intervention
Kick‐Off Event, Definition of Responsibilities, and Checklist
All stakeholders and front‐line staff were invited to a kickoff event on March 5, 2012. This event included education and discussion about the importance of a safe and early discharge from the patient and staff perspective. Roles in the discharge process were clearly defined and a corresponding checklist was created (Table 1). The checklist was used at least once per day during afternoon interdisciplinary in preparation for next‐day DBNs. Discharge date and time are communicated by the medical team to individual patients and families on the day a patient is identified for DBN. Patients and families did not receive additional orientation to the DBN initiative.
| Discharge Task | Responsible Team Member |
|---|---|
| |
| MD discharge summary and medication reconciliation | Resident or NP |
| Discharge order | Resident or NP |
| Prescription(s) | Resident or NP |
| Communicate discharge date and time to patient/family | Resident/hospitalist/NP |
| Patient education | Nurse |
| RN discharge summary | Nurse |
| Patient belongings/clothing | Nurse |
| Patient education/teaching | Nurse |
| Final labs/tests | Nurse |
| Assess Foley catheter need and remove | Nurse |
| Transportation | Social worker and care manager |
| At‐home services (HHA/HA/private hire) | Social worker and care manager |
| Equipment/supplies (DME, O2, ostomy supplies) | Social worker and care manager |
Interdisciplinary Rounds and DBN Website
In the past, interdisciplinary rounds, attended by each unit's charge nurse (CN), the medical resident or NP, the hospitalist, the team‐based social work (SW), and care management (CM) occurred in the morning between 9:00 am and 10:00 am. With the DBN initiative, additional afternoon interdisciplinary rounds were held at 3:00 pm. These rounds were designed to identify the next day's DBNs. Multidisciplinary team members were asked to complete the checklist responsibilities the same day that DBNs were identified rather than waiting until the day of discharge. A DBN website was created, and CMs were asked to log anticipated DBNs on this site after 3:00 pm rounds. The website generates a daily automated email at 4:30 pm to the DBN listserv with a list of the next day's anticipated DBNs. The listserv includes all hospitalists, residents, NPs, CNs, nurse managers (NM), medical directors, bed management, building services, SWs, and CMs. Additional departments were subsequently added as the DBN initiative became standard of care.
Assistant NMs update the DBN website overnight, adding patients identified by nursing staff as a possible DBN and highlighting changes in the condition of previously identified patients. At 7:00 am, an automated update email is sent by the website to the listserv. The automated emails include the DBN checklist, key phone numbers, and useful links.
Daily Leadership Meeting, Ongoing Process Improvement, and Real‐Time Feedback
Weekdays at 11:00 am, an interdisciplinary leadership meeting occurs with the medical directors, assistant NMs, CNs, and representatives from SW, CM, and hospital administration. At this meeting, all discharges from the previous day are reviewed to identify areas for improvement and trends in barriers to DBN. The current day's expected DBNs are also reviewed to address discharge bottlenecks in real time. Daily feedback was provided via a poster displayed in staff areas with daily DBN statistics.
Reward and Recognition
At the kickoff, a prize system was announced for the conclusion of the first month of the intervention if DBN thresholds were met. Rewards included a pizza party and raffle gift certificates. To hardwire the process, these rewards were repeated at the conclusion of each of the first 3 months of the intervention.
Changes to the Floor
There were notable changes to the floor during the time of this intervention. From October 25, 2012 until January 1, 2013, the hospital was closed after evacuation due to Hurricane Sandy. Units 17E and 17W reopened on January 14, 2013. The NP team was not restarted with the reopening. All other floor processes, including the DBN interventions, were restarted. The time period of floor closure was excluded in this analysis. The initial medical center goal was 30% DBNs. During the intervention period, the goal increased to 40%.
Data Collection and Analysis
Primary Outcome: Calendar Month DBN Percentage
The date and time of discharge are recorded by the discharging nurse or patient unit assistant in our electronic medical record (Epic, Madison WI) at the time the patient leaves the unit. Utilizing NYU's cost accounting system (Enterprise Performance Systems Inc., Chicago, IL), we obtained discharge date and time among inpatients discharged from units 17E and 17W between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. The analysis includes 8 months of baseline data and 13 months of intervention data (not counting the excluded months from hospital closure), measuring the extent to which improvement was sustained. To match organizational criteria for DBN, we excluded patients on the units in the patient class observation, deaths, and inpatient hospice.
Patients were identified as DBNs if the discharge time was before 12:01 pm, in accordance with our medical center administration's definition of DBN. Calendar month DBN percentage was calculated by dividing the number of DBN patients during the calendar month by the total number of discharged patients during the calendar month. The proportion of DBNs in the baseline population was compared to the proportion of DBNs in the intervention population. Statistical significance for the change in DBN was evaluated by use of a 2‐tailed z test.
Secondary Outcomes: Observed‐to‐Expected LOS and 30‐Day Readmission Rate
Expected LOS was provided by the University Health Consortium (UHC). UHC calculates a risk‐adjusted LOS for each patient by assigning a severity of illness, selection of a patient population to serve as a basis of the model, and use of statistical regression to assign an expected LOS in days. Observed‐to‐expected (O/E) LOS for each patient is calculated by dividing the expected LOS in days by the observed (actual) LOS in days. The average of the O/E LOS for all patients in the baseline period was compared to the average O/E LOS for all patients in the intervention period. This average was calculated by summing the O/E LOS of all patients in each time period and dividing by the total number of patients. In accordance with our medical center administration's reporting standards, we report the mean of the O/E LOS. For statistical evaluation of this non‐normally distributed continuous variable, we also report the median of the O/E LOS for the baseline and intervention time period and use the Wilcoxon rank sum test to evaluate for statistical significance.
Readmission cases are identified by the clinical quality and effectiveness department at our medical center using the UHC definition of all patients who are readmitted to a hospital within 30 days of discharge from the index admission. The 30‐day readmission rate is calculated by dividing the total number of cases identified as readmissions within 30 days by the total number of admissions over the same time period. This rate was obtained on a calendar‐month basis for patients discharged from the index admission before noon, after noon, and in total. These rates were averaged over the baseline and intervention period. The proportion of 30‐day readmissions in the baseline population was compared to the proportion of 30‐day readmissions in the intervention population. Statistical significance for the change in 30‐day readmissions was evaluated by use of a 2‐tailed z test.
RESULTS
Primary Outcome: Calendar Month DBN Percentage
The calendar month DBN percentage increased in the first month of the intervention, from 16% to 42% (Figure 1). This improvement was sustained throughout the intervention, with an average calendar month DBN percentage of 38% over the 13‐month intervention period. Use of a 2‐tailed z test to compare the pre‐intervention proportion (11%) of patients who were DBN with the post‐intervention proportion (38%) who were DBN showed a statistically significant change (z score 23.6, P = 0.0002). Units 17E and 17W had a combined 2536 total discharges in the baseline period, with 265 patients discharged before noon. In the intervention period, 3277 total discharges occurred, with 1236 patients discharged before noon. The average time of discharge moved 1 hour and 31 minutes, from 3:43 pm in the baseline period to 2:13 pm in the intervention period.
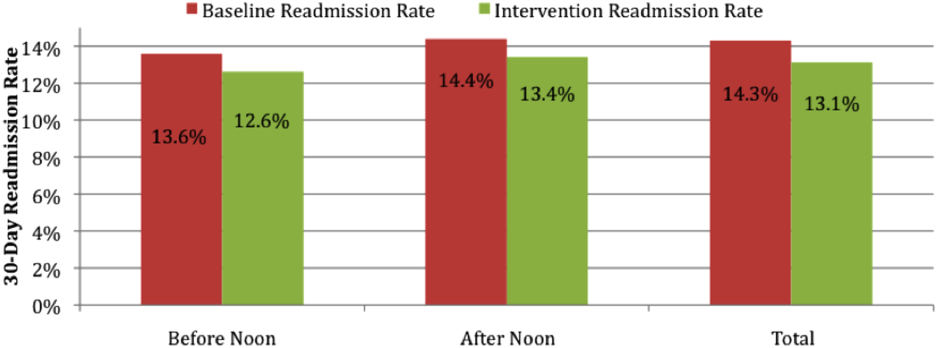
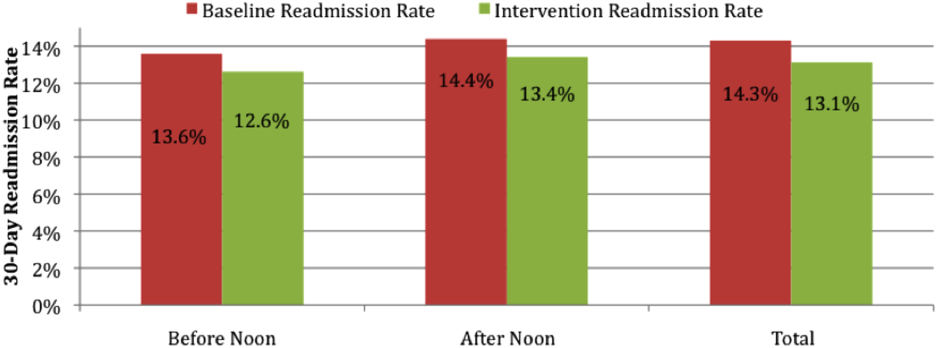
Secondary Outcomes: O/E LOS and 30‐Day Readmission Rate
The average O/E LOS during the baseline period was 1.06, and this declined during the intervention period to 0.96 [Table 2]. Using the Wilcoxon rank sum test, we found a statistically significant difference between the O/E LOS in the baseline (median 0.82) and intervention (median 0.76) periods (P = 0.0001). The average 30‐day readmission rate declined from 14.3% during the baseline to 13.1% during the intervention period. The change in 30‐day readmission rate was not statistically significant (z score=1.3132, P=0.1902). The change in readmission rate was similar and not statistically significant whether the patient was discharged before (13.6% baseline vs 12.6% intervention, P=0.66) or after noon (14.4% baseline vs 13.4% intervention, P=0.35) (Figure 2).
| Units 17E and 17W | Baseline Period | Intervention Period | Change | P Value |
|---|---|---|---|---|
| ||||
| O/E LOS, mean (median) | 1.06 (0.82) | 0.96 (0.76) | 10% | 0.0001a |
| 30‐day readmission rate | 14.3 | 13.1 | 1.2% | 0.1902 |
DISCUSSION
Throughput and discharges late in the day are challenges that face all medical centers. We demonstrate that successful and sustainable improvements in DBN are possible. We were able to increase the DBN percentage from 11% in the baseline period to an average of 38% in the 13 months after our intervention. Our success allowed us to surpass our medical center's initial goal of 30% DBN.
The intervention took place on 2 inpatient medical units at an urban, academic medical center. This intervention is likely generalizable to comparable medical centers. The study is limited by the implementation of multiple interventions as part of the DBN initiative at the same time. We are unable to isolate the effect of individual changes. If other medical centers wish to use a similar intervention, we believe the 3 most important parts of our intervention are: (1) kickoff event to engage all staff with a clear definition of roles; (2) daily real‐time feedback, utilizing tools such as unit boards tracking the DBN percentage; and (3) a standardized form of communication for expected DBNs. In our experience, for a DBN to be successful, the team, patient, and family members must be alerted, and discharge plans must be initiated at least 1 day prior to the expected discharge. Attempting to discharge a patient before noon when they have been identified on the day of discharge is a losing proposition, both to achieve a coordinated, safe discharge and for staff and patient satisfaction.
The O/E LOS and 30‐day readmission rate declined over the intervention period, suggesting that there is no negative effect on these metrics. There was concern that staff would choose to keep patients an extra night to allow for an extra DBN the following day. This was actively discouraged during the kickoff event and throughout the intervention period at interdisciplinary rounds and through informal communications. Based upon the decline in O/E LOS, this did not occur. There was also concern that the 30‐day readmission rate may increase if patients are discharged earlier in the day than usual. We observed an actual but not statistically significant decline in 30‐day readmission rate, potentially due to improved communication between team members and earlier identification of expected discharges at the prior day's afternoon DBN rounds. It is unknown if the decline in O/E LOS and 30‐day readmission rate was effected by the DBN initiative. Many other initiatives were ongoing within the medical center that could be effecting these variables. More research is required to better understand the true effect of DBN on LOS and 30‐day readmission rate.
There is limited literature on discharge early in the day. One previous study showed improvement in the DBN percentage on an obstetric floor through the institution of a discharge brunch.[9] Another report showed a modest increase (from 19.6% to 26%) in DBNs with the use of scheduled discharges.[6] This study was of unclear duration and was not specific to medical units. Another study focused on the use of in‐room display boards to document the expected day and time of patient discharge.[8] That report focused on the ability to schedule and achieve the scheduled discharge date and time. The authors describe a trend toward more discharges early in the day but provide no specific data on this effect. The only study looking specifically at discharge early in the day on a medical unit showed improvement in the discharge before 1:00 pm percentage, but was of small size (81 total patients) and short duration (1 month).[7] Our study is of larger size and longer duration, is focused on implementation of a medical service, and provides a comprehensive system that should be reproducible.
There are several next steps to our work. We will continue to monitor the DBN percentage and the ongoing sustainability of the project. We plan to investigate the effect of this rapid and notable increase in DBN percentage on a variety of patient outcomes and hospital metrics, including patient satisfaction, timeliness of ED admissions, intensive care unit transfers to the medical floor, and direct admissions.
Our study demonstrates that increased timely discharge is an achievable and sustainable goal for medical centers. Future work will allow for better understanding of the full effects of such an intervention on patient outcomes and hospital metrics.
- , , , . Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , , , . Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , . Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , . Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6):250–255.
- , , , et al. Daily multidisciplinary discharge rounds in a trauma center: a little time, well spent. J Trauma. 2009;66(3):880–887.
- , , , . All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , . Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , . The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
Late afternoon hospital discharges are thought to create admission bottlenecks in the emergency department (ED).[1] ED overcrowding increases the length of stay (LOS) of patients[2] and is a major dissatisfier for both patients and staff.[3] In our medical center, ED patients who are admitted after 1:00 pm have a 0.6‐day longer risk‐adjusted LOS than those admitted before 1:00 pm (M. Radford, MD, written communication, March 2012).
Many potential barriers to discharging patients early in the day exist.[4] However, comprehensive discharge planning favorably impacts discharge times.[5] There are limited published data regarding discharging patients early in the day. Studies have focused on improved discharge care coordination,[6, 7] in‐room display of planned discharge time,[8] and a discharge brunch.[9] In January 2012, the calendar month discharge before noon (DBN) percentage for 2 inpatient medicine units in our institution was approximately 7%, well below the organizational goal of 30%. We describe an intervention to sustainably increase the DBN percentage.
METHODS
Setting
The intervention took place on the 17th floor of New York University (NYU) Langone Medical Center's Tisch Hospital, an urban, academic medical center. All patients on the 17th floor received the intervention.
The 17th floor is composed of 2 acute care inpatient medical units17E and 17W. Each unit has 35 medical beds including a 16‐bed medical step down unit (SDU). Medical teams on the floor consist of 4 housestaff teams, a nurse practitioner (NP) team, and an SDU team. Each housestaff and NP team is led by a hospitalist, who is the attending of record for the majority of patients, though some patients on these teams are cared for by private attendings. Medical teams admit patients to any unit based upon bed availability. Nurses are assigned patients by acuity, not by medical team.
Intervention
Kick‐Off Event, Definition of Responsibilities, and Checklist
All stakeholders and front‐line staff were invited to a kickoff event on March 5, 2012. This event included education and discussion about the importance of a safe and early discharge from the patient and staff perspective. Roles in the discharge process were clearly defined and a corresponding checklist was created (Table 1). The checklist was used at least once per day during afternoon interdisciplinary in preparation for next‐day DBNs. Discharge date and time are communicated by the medical team to individual patients and families on the day a patient is identified for DBN. Patients and families did not receive additional orientation to the DBN initiative.
| Discharge Task | Responsible Team Member |
|---|---|
| |
| MD discharge summary and medication reconciliation | Resident or NP |
| Discharge order | Resident or NP |
| Prescription(s) | Resident or NP |
| Communicate discharge date and time to patient/family | Resident/hospitalist/NP |
| Patient education | Nurse |
| RN discharge summary | Nurse |
| Patient belongings/clothing | Nurse |
| Patient education/teaching | Nurse |
| Final labs/tests | Nurse |
| Assess Foley catheter need and remove | Nurse |
| Transportation | Social worker and care manager |
| At‐home services (HHA/HA/private hire) | Social worker and care manager |
| Equipment/supplies (DME, O2, ostomy supplies) | Social worker and care manager |
Interdisciplinary Rounds and DBN Website
In the past, interdisciplinary rounds, attended by each unit's charge nurse (CN), the medical resident or NP, the hospitalist, the team‐based social work (SW), and care management (CM) occurred in the morning between 9:00 am and 10:00 am. With the DBN initiative, additional afternoon interdisciplinary rounds were held at 3:00 pm. These rounds were designed to identify the next day's DBNs. Multidisciplinary team members were asked to complete the checklist responsibilities the same day that DBNs were identified rather than waiting until the day of discharge. A DBN website was created, and CMs were asked to log anticipated DBNs on this site after 3:00 pm rounds. The website generates a daily automated email at 4:30 pm to the DBN listserv with a list of the next day's anticipated DBNs. The listserv includes all hospitalists, residents, NPs, CNs, nurse managers (NM), medical directors, bed management, building services, SWs, and CMs. Additional departments were subsequently added as the DBN initiative became standard of care.
Assistant NMs update the DBN website overnight, adding patients identified by nursing staff as a possible DBN and highlighting changes in the condition of previously identified patients. At 7:00 am, an automated update email is sent by the website to the listserv. The automated emails include the DBN checklist, key phone numbers, and useful links.
Daily Leadership Meeting, Ongoing Process Improvement, and Real‐Time Feedback
Weekdays at 11:00 am, an interdisciplinary leadership meeting occurs with the medical directors, assistant NMs, CNs, and representatives from SW, CM, and hospital administration. At this meeting, all discharges from the previous day are reviewed to identify areas for improvement and trends in barriers to DBN. The current day's expected DBNs are also reviewed to address discharge bottlenecks in real time. Daily feedback was provided via a poster displayed in staff areas with daily DBN statistics.
Reward and Recognition
At the kickoff, a prize system was announced for the conclusion of the first month of the intervention if DBN thresholds were met. Rewards included a pizza party and raffle gift certificates. To hardwire the process, these rewards were repeated at the conclusion of each of the first 3 months of the intervention.
Changes to the Floor
There were notable changes to the floor during the time of this intervention. From October 25, 2012 until January 1, 2013, the hospital was closed after evacuation due to Hurricane Sandy. Units 17E and 17W reopened on January 14, 2013. The NP team was not restarted with the reopening. All other floor processes, including the DBN interventions, were restarted. The time period of floor closure was excluded in this analysis. The initial medical center goal was 30% DBNs. During the intervention period, the goal increased to 40%.
Data Collection and Analysis
Primary Outcome: Calendar Month DBN Percentage
The date and time of discharge are recorded by the discharging nurse or patient unit assistant in our electronic medical record (Epic, Madison WI) at the time the patient leaves the unit. Utilizing NYU's cost accounting system (Enterprise Performance Systems Inc., Chicago, IL), we obtained discharge date and time among inpatients discharged from units 17E and 17W between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. The analysis includes 8 months of baseline data and 13 months of intervention data (not counting the excluded months from hospital closure), measuring the extent to which improvement was sustained. To match organizational criteria for DBN, we excluded patients on the units in the patient class observation, deaths, and inpatient hospice.
Patients were identified as DBNs if the discharge time was before 12:01 pm, in accordance with our medical center administration's definition of DBN. Calendar month DBN percentage was calculated by dividing the number of DBN patients during the calendar month by the total number of discharged patients during the calendar month. The proportion of DBNs in the baseline population was compared to the proportion of DBNs in the intervention population. Statistical significance for the change in DBN was evaluated by use of a 2‐tailed z test.
Secondary Outcomes: Observed‐to‐Expected LOS and 30‐Day Readmission Rate
Expected LOS was provided by the University Health Consortium (UHC). UHC calculates a risk‐adjusted LOS for each patient by assigning a severity of illness, selection of a patient population to serve as a basis of the model, and use of statistical regression to assign an expected LOS in days. Observed‐to‐expected (O/E) LOS for each patient is calculated by dividing the expected LOS in days by the observed (actual) LOS in days. The average of the O/E LOS for all patients in the baseline period was compared to the average O/E LOS for all patients in the intervention period. This average was calculated by summing the O/E LOS of all patients in each time period and dividing by the total number of patients. In accordance with our medical center administration's reporting standards, we report the mean of the O/E LOS. For statistical evaluation of this non‐normally distributed continuous variable, we also report the median of the O/E LOS for the baseline and intervention time period and use the Wilcoxon rank sum test to evaluate for statistical significance.
Readmission cases are identified by the clinical quality and effectiveness department at our medical center using the UHC definition of all patients who are readmitted to a hospital within 30 days of discharge from the index admission. The 30‐day readmission rate is calculated by dividing the total number of cases identified as readmissions within 30 days by the total number of admissions over the same time period. This rate was obtained on a calendar‐month basis for patients discharged from the index admission before noon, after noon, and in total. These rates were averaged over the baseline and intervention period. The proportion of 30‐day readmissions in the baseline population was compared to the proportion of 30‐day readmissions in the intervention population. Statistical significance for the change in 30‐day readmissions was evaluated by use of a 2‐tailed z test.
RESULTS
Primary Outcome: Calendar Month DBN Percentage
The calendar month DBN percentage increased in the first month of the intervention, from 16% to 42% (Figure 1). This improvement was sustained throughout the intervention, with an average calendar month DBN percentage of 38% over the 13‐month intervention period. Use of a 2‐tailed z test to compare the pre‐intervention proportion (11%) of patients who were DBN with the post‐intervention proportion (38%) who were DBN showed a statistically significant change (z score 23.6, P = 0.0002). Units 17E and 17W had a combined 2536 total discharges in the baseline period, with 265 patients discharged before noon. In the intervention period, 3277 total discharges occurred, with 1236 patients discharged before noon. The average time of discharge moved 1 hour and 31 minutes, from 3:43 pm in the baseline period to 2:13 pm in the intervention period.
Secondary Outcomes: O/E LOS and 30‐Day Readmission Rate
The average O/E LOS during the baseline period was 1.06, and this declined during the intervention period to 0.96 [Table 2]. Using the Wilcoxon rank sum test, we found a statistically significant difference between the O/E LOS in the baseline (median 0.82) and intervention (median 0.76) periods (P = 0.0001). The average 30‐day readmission rate declined from 14.3% during the baseline to 13.1% during the intervention period. The change in 30‐day readmission rate was not statistically significant (z score=1.3132, P=0.1902). The change in readmission rate was similar and not statistically significant whether the patient was discharged before (13.6% baseline vs 12.6% intervention, P=0.66) or after noon (14.4% baseline vs 13.4% intervention, P=0.35) (Figure 2).
| Units 17E and 17W | Baseline Period | Intervention Period | Change | P Value |
|---|---|---|---|---|
| ||||
| O/E LOS, mean (median) | 1.06 (0.82) | 0.96 (0.76) | 10% | 0.0001a |
| 30‐day readmission rate | 14.3 | 13.1 | 1.2% | 0.1902 |
DISCUSSION
Throughput and discharges late in the day are challenges that face all medical centers. We demonstrate that successful and sustainable improvements in DBN are possible. We were able to increase the DBN percentage from 11% in the baseline period to an average of 38% in the 13 months after our intervention. Our success allowed us to surpass our medical center's initial goal of 30% DBN.
The intervention took place on 2 inpatient medical units at an urban, academic medical center. This intervention is likely generalizable to comparable medical centers. The study is limited by the implementation of multiple interventions as part of the DBN initiative at the same time. We are unable to isolate the effect of individual changes. If other medical centers wish to use a similar intervention, we believe the 3 most important parts of our intervention are: (1) kickoff event to engage all staff with a clear definition of roles; (2) daily real‐time feedback, utilizing tools such as unit boards tracking the DBN percentage; and (3) a standardized form of communication for expected DBNs. In our experience, for a DBN to be successful, the team, patient, and family members must be alerted, and discharge plans must be initiated at least 1 day prior to the expected discharge. Attempting to discharge a patient before noon when they have been identified on the day of discharge is a losing proposition, both to achieve a coordinated, safe discharge and for staff and patient satisfaction.
The O/E LOS and 30‐day readmission rate declined over the intervention period, suggesting that there is no negative effect on these metrics. There was concern that staff would choose to keep patients an extra night to allow for an extra DBN the following day. This was actively discouraged during the kickoff event and throughout the intervention period at interdisciplinary rounds and through informal communications. Based upon the decline in O/E LOS, this did not occur. There was also concern that the 30‐day readmission rate may increase if patients are discharged earlier in the day than usual. We observed an actual but not statistically significant decline in 30‐day readmission rate, potentially due to improved communication between team members and earlier identification of expected discharges at the prior day's afternoon DBN rounds. It is unknown if the decline in O/E LOS and 30‐day readmission rate was effected by the DBN initiative. Many other initiatives were ongoing within the medical center that could be effecting these variables. More research is required to better understand the true effect of DBN on LOS and 30‐day readmission rate.
There is limited literature on discharge early in the day. One previous study showed improvement in the DBN percentage on an obstetric floor through the institution of a discharge brunch.[9] Another report showed a modest increase (from 19.6% to 26%) in DBNs with the use of scheduled discharges.[6] This study was of unclear duration and was not specific to medical units. Another study focused on the use of in‐room display boards to document the expected day and time of patient discharge.[8] That report focused on the ability to schedule and achieve the scheduled discharge date and time. The authors describe a trend toward more discharges early in the day but provide no specific data on this effect. The only study looking specifically at discharge early in the day on a medical unit showed improvement in the discharge before 1:00 pm percentage, but was of small size (81 total patients) and short duration (1 month).[7] Our study is of larger size and longer duration, is focused on implementation of a medical service, and provides a comprehensive system that should be reproducible.
There are several next steps to our work. We will continue to monitor the DBN percentage and the ongoing sustainability of the project. We plan to investigate the effect of this rapid and notable increase in DBN percentage on a variety of patient outcomes and hospital metrics, including patient satisfaction, timeliness of ED admissions, intensive care unit transfers to the medical floor, and direct admissions.
Our study demonstrates that increased timely discharge is an achievable and sustainable goal for medical centers. Future work will allow for better understanding of the full effects of such an intervention on patient outcomes and hospital metrics.
Late afternoon hospital discharges are thought to create admission bottlenecks in the emergency department (ED).[1] ED overcrowding increases the length of stay (LOS) of patients[2] and is a major dissatisfier for both patients and staff.[3] In our medical center, ED patients who are admitted after 1:00 pm have a 0.6‐day longer risk‐adjusted LOS than those admitted before 1:00 pm (M. Radford, MD, written communication, March 2012).
Many potential barriers to discharging patients early in the day exist.[4] However, comprehensive discharge planning favorably impacts discharge times.[5] There are limited published data regarding discharging patients early in the day. Studies have focused on improved discharge care coordination,[6, 7] in‐room display of planned discharge time,[8] and a discharge brunch.[9] In January 2012, the calendar month discharge before noon (DBN) percentage for 2 inpatient medicine units in our institution was approximately 7%, well below the organizational goal of 30%. We describe an intervention to sustainably increase the DBN percentage.
METHODS
Setting
The intervention took place on the 17th floor of New York University (NYU) Langone Medical Center's Tisch Hospital, an urban, academic medical center. All patients on the 17th floor received the intervention.
The 17th floor is composed of 2 acute care inpatient medical units17E and 17W. Each unit has 35 medical beds including a 16‐bed medical step down unit (SDU). Medical teams on the floor consist of 4 housestaff teams, a nurse practitioner (NP) team, and an SDU team. Each housestaff and NP team is led by a hospitalist, who is the attending of record for the majority of patients, though some patients on these teams are cared for by private attendings. Medical teams admit patients to any unit based upon bed availability. Nurses are assigned patients by acuity, not by medical team.
Intervention
Kick‐Off Event, Definition of Responsibilities, and Checklist
All stakeholders and front‐line staff were invited to a kickoff event on March 5, 2012. This event included education and discussion about the importance of a safe and early discharge from the patient and staff perspective. Roles in the discharge process were clearly defined and a corresponding checklist was created (Table 1). The checklist was used at least once per day during afternoon interdisciplinary in preparation for next‐day DBNs. Discharge date and time are communicated by the medical team to individual patients and families on the day a patient is identified for DBN. Patients and families did not receive additional orientation to the DBN initiative.
| Discharge Task | Responsible Team Member |
|---|---|
| |
| MD discharge summary and medication reconciliation | Resident or NP |
| Discharge order | Resident or NP |
| Prescription(s) | Resident or NP |
| Communicate discharge date and time to patient/family | Resident/hospitalist/NP |
| Patient education | Nurse |
| RN discharge summary | Nurse |
| Patient belongings/clothing | Nurse |
| Patient education/teaching | Nurse |
| Final labs/tests | Nurse |
| Assess Foley catheter need and remove | Nurse |
| Transportation | Social worker and care manager |
| At‐home services (HHA/HA/private hire) | Social worker and care manager |
| Equipment/supplies (DME, O2, ostomy supplies) | Social worker and care manager |
Interdisciplinary Rounds and DBN Website
In the past, interdisciplinary rounds, attended by each unit's charge nurse (CN), the medical resident or NP, the hospitalist, the team‐based social work (SW), and care management (CM) occurred in the morning between 9:00 am and 10:00 am. With the DBN initiative, additional afternoon interdisciplinary rounds were held at 3:00 pm. These rounds were designed to identify the next day's DBNs. Multidisciplinary team members were asked to complete the checklist responsibilities the same day that DBNs were identified rather than waiting until the day of discharge. A DBN website was created, and CMs were asked to log anticipated DBNs on this site after 3:00 pm rounds. The website generates a daily automated email at 4:30 pm to the DBN listserv with a list of the next day's anticipated DBNs. The listserv includes all hospitalists, residents, NPs, CNs, nurse managers (NM), medical directors, bed management, building services, SWs, and CMs. Additional departments were subsequently added as the DBN initiative became standard of care.
Assistant NMs update the DBN website overnight, adding patients identified by nursing staff as a possible DBN and highlighting changes in the condition of previously identified patients. At 7:00 am, an automated update email is sent by the website to the listserv. The automated emails include the DBN checklist, key phone numbers, and useful links.
Daily Leadership Meeting, Ongoing Process Improvement, and Real‐Time Feedback
Weekdays at 11:00 am, an interdisciplinary leadership meeting occurs with the medical directors, assistant NMs, CNs, and representatives from SW, CM, and hospital administration. At this meeting, all discharges from the previous day are reviewed to identify areas for improvement and trends in barriers to DBN. The current day's expected DBNs are also reviewed to address discharge bottlenecks in real time. Daily feedback was provided via a poster displayed in staff areas with daily DBN statistics.
Reward and Recognition
At the kickoff, a prize system was announced for the conclusion of the first month of the intervention if DBN thresholds were met. Rewards included a pizza party and raffle gift certificates. To hardwire the process, these rewards were repeated at the conclusion of each of the first 3 months of the intervention.
Changes to the Floor
There were notable changes to the floor during the time of this intervention. From October 25, 2012 until January 1, 2013, the hospital was closed after evacuation due to Hurricane Sandy. Units 17E and 17W reopened on January 14, 2013. The NP team was not restarted with the reopening. All other floor processes, including the DBN interventions, were restarted. The time period of floor closure was excluded in this analysis. The initial medical center goal was 30% DBNs. During the intervention period, the goal increased to 40%.
Data Collection and Analysis
Primary Outcome: Calendar Month DBN Percentage
The date and time of discharge are recorded by the discharging nurse or patient unit assistant in our electronic medical record (Epic, Madison WI) at the time the patient leaves the unit. Utilizing NYU's cost accounting system (Enterprise Performance Systems Inc., Chicago, IL), we obtained discharge date and time among inpatients discharged from units 17E and 17W between June 1, 2011 and March 4, 2012 (the baseline period) and March 5, 2012 and June 31, 2013 (the intervention period). Data from October 25, 2012 to the end of January 2013 were excluded due to hospital closure from Hurricane Sandy. The analysis includes 8 months of baseline data and 13 months of intervention data (not counting the excluded months from hospital closure), measuring the extent to which improvement was sustained. To match organizational criteria for DBN, we excluded patients on the units in the patient class observation, deaths, and inpatient hospice.
Patients were identified as DBNs if the discharge time was before 12:01 pm, in accordance with our medical center administration's definition of DBN. Calendar month DBN percentage was calculated by dividing the number of DBN patients during the calendar month by the total number of discharged patients during the calendar month. The proportion of DBNs in the baseline population was compared to the proportion of DBNs in the intervention population. Statistical significance for the change in DBN was evaluated by use of a 2‐tailed z test.
Secondary Outcomes: Observed‐to‐Expected LOS and 30‐Day Readmission Rate
Expected LOS was provided by the University Health Consortium (UHC). UHC calculates a risk‐adjusted LOS for each patient by assigning a severity of illness, selection of a patient population to serve as a basis of the model, and use of statistical regression to assign an expected LOS in days. Observed‐to‐expected (O/E) LOS for each patient is calculated by dividing the expected LOS in days by the observed (actual) LOS in days. The average of the O/E LOS for all patients in the baseline period was compared to the average O/E LOS for all patients in the intervention period. This average was calculated by summing the O/E LOS of all patients in each time period and dividing by the total number of patients. In accordance with our medical center administration's reporting standards, we report the mean of the O/E LOS. For statistical evaluation of this non‐normally distributed continuous variable, we also report the median of the O/E LOS for the baseline and intervention time period and use the Wilcoxon rank sum test to evaluate for statistical significance.
Readmission cases are identified by the clinical quality and effectiveness department at our medical center using the UHC definition of all patients who are readmitted to a hospital within 30 days of discharge from the index admission. The 30‐day readmission rate is calculated by dividing the total number of cases identified as readmissions within 30 days by the total number of admissions over the same time period. This rate was obtained on a calendar‐month basis for patients discharged from the index admission before noon, after noon, and in total. These rates were averaged over the baseline and intervention period. The proportion of 30‐day readmissions in the baseline population was compared to the proportion of 30‐day readmissions in the intervention population. Statistical significance for the change in 30‐day readmissions was evaluated by use of a 2‐tailed z test.
RESULTS
Primary Outcome: Calendar Month DBN Percentage
The calendar month DBN percentage increased in the first month of the intervention, from 16% to 42% (Figure 1). This improvement was sustained throughout the intervention, with an average calendar month DBN percentage of 38% over the 13‐month intervention period. Use of a 2‐tailed z test to compare the pre‐intervention proportion (11%) of patients who were DBN with the post‐intervention proportion (38%) who were DBN showed a statistically significant change (z score 23.6, P = 0.0002). Units 17E and 17W had a combined 2536 total discharges in the baseline period, with 265 patients discharged before noon. In the intervention period, 3277 total discharges occurred, with 1236 patients discharged before noon. The average time of discharge moved 1 hour and 31 minutes, from 3:43 pm in the baseline period to 2:13 pm in the intervention period.
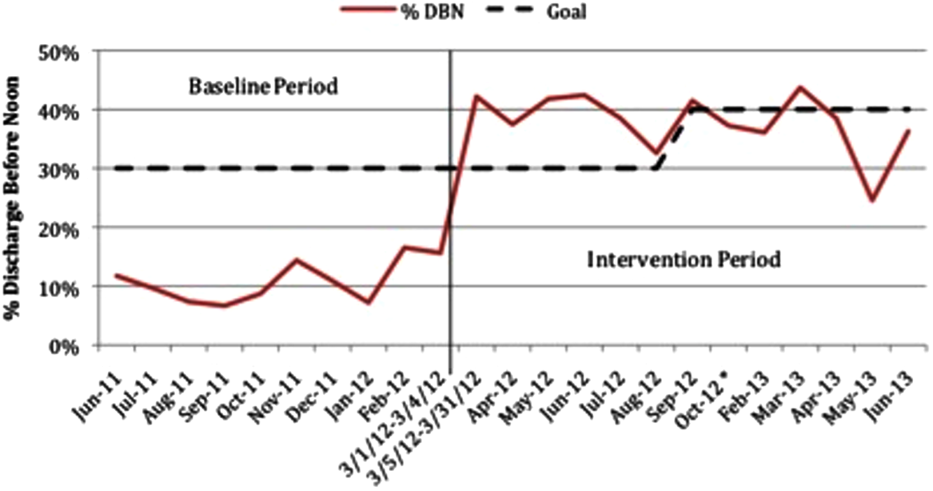
Secondary Outcomes: O/E LOS and 30‐Day Readmission Rate
The average O/E LOS during the baseline period was 1.06, and this declined during the intervention period to 0.96 [Table 2]. Using the Wilcoxon rank sum test, we found a statistically significant difference between the O/E LOS in the baseline (median 0.82) and intervention (median 0.76) periods (P = 0.0001). The average 30‐day readmission rate declined from 14.3% during the baseline to 13.1% during the intervention period. The change in 30‐day readmission rate was not statistically significant (z score=1.3132, P=0.1902). The change in readmission rate was similar and not statistically significant whether the patient was discharged before (13.6% baseline vs 12.6% intervention, P=0.66) or after noon (14.4% baseline vs 13.4% intervention, P=0.35) (Figure 2).
| Units 17E and 17W | Baseline Period | Intervention Period | Change | P Value |
|---|---|---|---|---|
| ||||
| O/E LOS, mean (median) | 1.06 (0.82) | 0.96 (0.76) | 10% | 0.0001a |
| 30‐day readmission rate | 14.3 | 13.1 | 1.2% | 0.1902 |
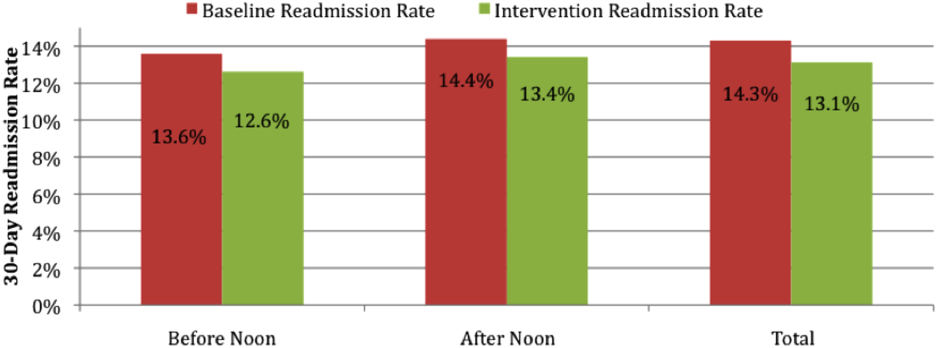
DISCUSSION
Throughput and discharges late in the day are challenges that face all medical centers. We demonstrate that successful and sustainable improvements in DBN are possible. We were able to increase the DBN percentage from 11% in the baseline period to an average of 38% in the 13 months after our intervention. Our success allowed us to surpass our medical center's initial goal of 30% DBN.
The intervention took place on 2 inpatient medical units at an urban, academic medical center. This intervention is likely generalizable to comparable medical centers. The study is limited by the implementation of multiple interventions as part of the DBN initiative at the same time. We are unable to isolate the effect of individual changes. If other medical centers wish to use a similar intervention, we believe the 3 most important parts of our intervention are: (1) kickoff event to engage all staff with a clear definition of roles; (2) daily real‐time feedback, utilizing tools such as unit boards tracking the DBN percentage; and (3) a standardized form of communication for expected DBNs. In our experience, for a DBN to be successful, the team, patient, and family members must be alerted, and discharge plans must be initiated at least 1 day prior to the expected discharge. Attempting to discharge a patient before noon when they have been identified on the day of discharge is a losing proposition, both to achieve a coordinated, safe discharge and for staff and patient satisfaction.
The O/E LOS and 30‐day readmission rate declined over the intervention period, suggesting that there is no negative effect on these metrics. There was concern that staff would choose to keep patients an extra night to allow for an extra DBN the following day. This was actively discouraged during the kickoff event and throughout the intervention period at interdisciplinary rounds and through informal communications. Based upon the decline in O/E LOS, this did not occur. There was also concern that the 30‐day readmission rate may increase if patients are discharged earlier in the day than usual. We observed an actual but not statistically significant decline in 30‐day readmission rate, potentially due to improved communication between team members and earlier identification of expected discharges at the prior day's afternoon DBN rounds. It is unknown if the decline in O/E LOS and 30‐day readmission rate was effected by the DBN initiative. Many other initiatives were ongoing within the medical center that could be effecting these variables. More research is required to better understand the true effect of DBN on LOS and 30‐day readmission rate.
There is limited literature on discharge early in the day. One previous study showed improvement in the DBN percentage on an obstetric floor through the institution of a discharge brunch.[9] Another report showed a modest increase (from 19.6% to 26%) in DBNs with the use of scheduled discharges.[6] This study was of unclear duration and was not specific to medical units. Another study focused on the use of in‐room display boards to document the expected day and time of patient discharge.[8] That report focused on the ability to schedule and achieve the scheduled discharge date and time. The authors describe a trend toward more discharges early in the day but provide no specific data on this effect. The only study looking specifically at discharge early in the day on a medical unit showed improvement in the discharge before 1:00 pm percentage, but was of small size (81 total patients) and short duration (1 month).[7] Our study is of larger size and longer duration, is focused on implementation of a medical service, and provides a comprehensive system that should be reproducible.
There are several next steps to our work. We will continue to monitor the DBN percentage and the ongoing sustainability of the project. We plan to investigate the effect of this rapid and notable increase in DBN percentage on a variety of patient outcomes and hospital metrics, including patient satisfaction, timeliness of ED admissions, intensive care unit transfers to the medical floor, and direct admissions.
Our study demonstrates that increased timely discharge is an achievable and sustainable goal for medical centers. Future work will allow for better understanding of the full effects of such an intervention on patient outcomes and hospital metrics.
- , , , . Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , , , . Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , . Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , . Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6):250–255.
- , , , et al. Daily multidisciplinary discharge rounds in a trauma center: a little time, well spent. J Trauma. 2009;66(3):880–887.
- , , , . All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , . Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , . The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
- , , , . Impact of admission and discharge peak times on hospital overcrowding. Stud Health Technol Inform. 2011;168:82–88.
- , , , , , . Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med. 2013;44(1):230–235.
- , . Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35(1):63–68.
- , , . Caregiver perceptions of the reasons for delayed hospital discharge. Eff Clin Pract. 2001;4(6):250–255.
- , , , et al. Daily multidisciplinary discharge rounds in a trauma center: a little time, well spent. J Trauma. 2009;66(3):880–887.
- , , , . All roads lead to scheduled discharges. Nursing. 2008;38(12):61–63.
- , , , . Discharging patients earlier in the day: a concept worth evaluating. Health Care Manag (Frederick). 2007;26(2):142–146.
- , , , et al. In‐room display of day and time patient is anticipated to leave hospital: a “discharge appointment”. J Hosp Med. 2007;2(1):13–16.
- , . The discharge brunch: reducing chaos and increasing smiles on the OB unit. Nurs Womens Health. 2009;13(5):402–409.
© 2014 Society of Hospital Medicine