User login
Left-sided back pain that won’t go away
A 68-year-old man came to the emergency department complaining of left-side thoracic back pain, after 5 days of outpatient treatment with analgesics did not help him. His pain started after physical labor, but he did not recall any trauma. A review of his medical history revealed only coronary artery disease, with coronary stent placement several years before this event. He had not been hospitalized recently, undergone an invasive procedure, or taken antibiotics.
On examination, a left thoracic paraspinal muscle was tender without fluctuance, overlying skin redness, or a lesion. An elevated white blood cell count of 12,300/mcL was the only laboratory test with abnormal results. The patient did not have fever, and results of urinalysis, chest radiograph, and abdominal sonogram were normal. Computed tomography (CT) images of the abdomen and pelvis showed inflammation of a left thoracic paraspinal muscle.
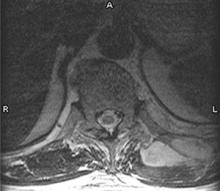
Thirty-six hours after admission, the patient developed fever (38.8°C). His physicians obtained a blood culture. The fever recurred (at 38.9°C) the following day, and 2 more blood cultures were done. His back pain did not improve despite analgesics, intravenous antibiotics, and physical therapy; therefore, on the eighth day in the hospital, magnetic resonance imaging (MRI) was performed (FIGURE).
FIGURE
MRI of the back
What is the diagnosis?
Diagnosis: Methicillin-resistant Staphylococcus aureus pyomyositis
Reports of the 3 blood cultures, acquired on the seventh day in the hospital, showed growth of methicillin-resistant Staphylococcus aureus (MRSA) with antibiotic susceptibility patterns common to community-acquired MRSA.1 A purulent aspirate was obtained from the lesion in the FIGURE with CT-guided drainage. Community-acquired MRSA grew in the aspirate culture. The final diagnosis was a primary skeletal muscle abscess without contiguous spread from an adjacent site, or pyomyositis.
Epidemiology of pyomyositis
Pyomyositis is uncommon in immunocompetent individuals living outside of the tropics. It is usually caused by S aureus. In the United States between 1981 and 2002, 330 cases were identified in a literature review,2 which noted an increasing incidence. Of these cases, 70% were caused by S aureus and 61.5% of patients were immunocompromised; 1 involved MRSA.
In 2003, 2 of 3 MRSA cases were reported in patients with hematologic disorders.3 In 2005, 4 community-acquired MRSA cases were reported;1 2 had other illnesses leading to increased risk. MRSA pyomyositis is now being reported in immunocompetent individuals, but most cases arise in patients with cancer, diabetes mellitus, rheumatologic disorders, hematologic disorders, renal failure, liver cirrhosis, intravenous drug use, or HIV infection.2,4,5 With staphylococcal infections increasing,6 including MRSA and community-acquired MRSA, the incidence of pyomyositis may increase correspondingly.
Consider the possibility of pyomyositis in patients with localized muscle pain and tenderness and who have risk factors for acquiring MRSA—living in a community with prevalent MRSA, recent hospitalization, antibiotic use, invasive procedures, or chronic venous catheters.
Most commonly, pyomyositis occurs in a leg or arm.2 In the 330 cases mentioned above, the sites of infection, in descending order of frequency, were lower extremity, upper extremity, buttocks, chest wall, paraspinal, and psoas.
Diagnostic evaluation: Know the stages
Making the correct diagnosis at the initial presentation is difficult because nonspecific symptoms resemble a muscle strain. But this infection progresses to bacteremia, making early identification important. To recognize pyomyositis before bacteremia develops, rely on clinical suspicion and familiarity with the 3 stages of the disease.
Stage 1 (invasive) is characterized by muscle pain and tenderness without systemic evidence of illness. Stage 2 (suppurative) is the formation of an abscess. At this time systemic symptoms such as fever may occur; otherwise physical exam findings remain vague with tenderness and induration without overlying skin redness or palpable fluctuance common to skin abscesses. Stage 3 is bacteremia or sepsis. Awareness of the risks and the stages of pyomyositis will aid in quicker diagnosis.
Diagnostic delay occurs because the first stage presents with nonspecific symptoms and examination findings, and also because initial laboratory and radiographic testing are inconclusive. Elevation of the white blood cell count and the erythrocyte sedimentation rate occur early, while serum muscle enzymes remain normal.2,4,5
Imaging studies performed during the first stage may not be productive; however, in the second stage imaging identifies the abscess. Although limited data exist regarding the best imaging modality, MRI and CT appear most useful.1,3,4,7 In 1 retrospective analysis, ultrasound identified 5 of 8 cases correctly, while MRI and CT were diagnostic in 5 of 6 and 9 of 9, respectively.7
Treatment: Antibiotics, drainage
Choose an antibiotic empirically that covers S aureus and is also appropriate for MRSA. Pyomyositis discovered in the first stage may resolve with antibiotics alone.4 In addition, early intervention may be especially important with MRSA, since MRSA bacteremia is associated with increased mortality compared with methicillin-sensitive S aureus bacteremia.6
If the condition progresses to the second stage with abscess development, surgical or percutaneous drainage will be necessary. Identification and removal of the site of infection in patients with community-acquired staphylococcal bacteremia results in improved outcomes,8 and pyomyositis can be an overlooked source.
Patient outcome
The day following drainage of the abscess, the patient was discharged from the hospital. He was treated for 6 weeks with intravenous antibiotics because of staphylococcal bacteremia, and he has fully recovered.
Acknowledgments
The authors would like to thank Robert Martin, Lead Operator, Information Technology, Texas Tech University Health Sciences Center at Amarillo for assistance in computer image enhancement and development.
CORRESPONDENCE
Timothy J. Benton, MD, Texas Tech University Health Sciences Center at Amarillo, Department of Family and Community Medicine, 1600 Wallace Boulevard, Amarillo, TX 79106. E-mail: [email protected]
1. Ruiz M, Yohannes S, Wladyka CG. Pyomyositis caused by methicillin-resistant Staphylococcus aureus. N Engl J Med 2005;352:1488-1489.
2. Crum NF. Bacterial pyomyositis in the United States. Am J Med 2004;117:420-428.
3. Hayashi T. Pyomyositis as a focus of infection in hematological disorders: a report of 3 cases. Int J Hematol 2003;77:171-174.
4. Ebright JR, Pieper B. Skin and soft tissue infections in injection drug users. Infect Dis Clin North Am 2002;16:697-712.
5. Hossain A, Reis ED, Soundararajan K, Kerstain MD, Hollier LH. Nontropical pyomyositis: analysis of eight patients in an urban center. Am Surg 2000;66:1064-1066.
6. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53-59.
7. Boniotti V. Contribution of imaging to the evaluation of pyomyositis. Radiol Med 2005;109:404-13.
8. Jensen AG. Importance of focus identification in the treatment of Staphylococcus aureus bacteremia. J Hosp Infect 2002;52:29-36.
A 68-year-old man came to the emergency department complaining of left-side thoracic back pain, after 5 days of outpatient treatment with analgesics did not help him. His pain started after physical labor, but he did not recall any trauma. A review of his medical history revealed only coronary artery disease, with coronary stent placement several years before this event. He had not been hospitalized recently, undergone an invasive procedure, or taken antibiotics.
On examination, a left thoracic paraspinal muscle was tender without fluctuance, overlying skin redness, or a lesion. An elevated white blood cell count of 12,300/mcL was the only laboratory test with abnormal results. The patient did not have fever, and results of urinalysis, chest radiograph, and abdominal sonogram were normal. Computed tomography (CT) images of the abdomen and pelvis showed inflammation of a left thoracic paraspinal muscle.
Thirty-six hours after admission, the patient developed fever (38.8°C). His physicians obtained a blood culture. The fever recurred (at 38.9°C) the following day, and 2 more blood cultures were done. His back pain did not improve despite analgesics, intravenous antibiotics, and physical therapy; therefore, on the eighth day in the hospital, magnetic resonance imaging (MRI) was performed (FIGURE).
FIGURE
MRI of the back
What is the diagnosis?
Diagnosis: Methicillin-resistant Staphylococcus aureus pyomyositis
Reports of the 3 blood cultures, acquired on the seventh day in the hospital, showed growth of methicillin-resistant Staphylococcus aureus (MRSA) with antibiotic susceptibility patterns common to community-acquired MRSA.1 A purulent aspirate was obtained from the lesion in the FIGURE with CT-guided drainage. Community-acquired MRSA grew in the aspirate culture. The final diagnosis was a primary skeletal muscle abscess without contiguous spread from an adjacent site, or pyomyositis.
Epidemiology of pyomyositis
Pyomyositis is uncommon in immunocompetent individuals living outside of the tropics. It is usually caused by S aureus. In the United States between 1981 and 2002, 330 cases were identified in a literature review,2 which noted an increasing incidence. Of these cases, 70% were caused by S aureus and 61.5% of patients were immunocompromised; 1 involved MRSA.
In 2003, 2 of 3 MRSA cases were reported in patients with hematologic disorders.3 In 2005, 4 community-acquired MRSA cases were reported;1 2 had other illnesses leading to increased risk. MRSA pyomyositis is now being reported in immunocompetent individuals, but most cases arise in patients with cancer, diabetes mellitus, rheumatologic disorders, hematologic disorders, renal failure, liver cirrhosis, intravenous drug use, or HIV infection.2,4,5 With staphylococcal infections increasing,6 including MRSA and community-acquired MRSA, the incidence of pyomyositis may increase correspondingly.
Consider the possibility of pyomyositis in patients with localized muscle pain and tenderness and who have risk factors for acquiring MRSA—living in a community with prevalent MRSA, recent hospitalization, antibiotic use, invasive procedures, or chronic venous catheters.
Most commonly, pyomyositis occurs in a leg or arm.2 In the 330 cases mentioned above, the sites of infection, in descending order of frequency, were lower extremity, upper extremity, buttocks, chest wall, paraspinal, and psoas.
Diagnostic evaluation: Know the stages
Making the correct diagnosis at the initial presentation is difficult because nonspecific symptoms resemble a muscle strain. But this infection progresses to bacteremia, making early identification important. To recognize pyomyositis before bacteremia develops, rely on clinical suspicion and familiarity with the 3 stages of the disease.
Stage 1 (invasive) is characterized by muscle pain and tenderness without systemic evidence of illness. Stage 2 (suppurative) is the formation of an abscess. At this time systemic symptoms such as fever may occur; otherwise physical exam findings remain vague with tenderness and induration without overlying skin redness or palpable fluctuance common to skin abscesses. Stage 3 is bacteremia or sepsis. Awareness of the risks and the stages of pyomyositis will aid in quicker diagnosis.
Diagnostic delay occurs because the first stage presents with nonspecific symptoms and examination findings, and also because initial laboratory and radiographic testing are inconclusive. Elevation of the white blood cell count and the erythrocyte sedimentation rate occur early, while serum muscle enzymes remain normal.2,4,5
Imaging studies performed during the first stage may not be productive; however, in the second stage imaging identifies the abscess. Although limited data exist regarding the best imaging modality, MRI and CT appear most useful.1,3,4,7 In 1 retrospective analysis, ultrasound identified 5 of 8 cases correctly, while MRI and CT were diagnostic in 5 of 6 and 9 of 9, respectively.7
Treatment: Antibiotics, drainage
Choose an antibiotic empirically that covers S aureus and is also appropriate for MRSA. Pyomyositis discovered in the first stage may resolve with antibiotics alone.4 In addition, early intervention may be especially important with MRSA, since MRSA bacteremia is associated with increased mortality compared with methicillin-sensitive S aureus bacteremia.6
If the condition progresses to the second stage with abscess development, surgical or percutaneous drainage will be necessary. Identification and removal of the site of infection in patients with community-acquired staphylococcal bacteremia results in improved outcomes,8 and pyomyositis can be an overlooked source.
Patient outcome
The day following drainage of the abscess, the patient was discharged from the hospital. He was treated for 6 weeks with intravenous antibiotics because of staphylococcal bacteremia, and he has fully recovered.
Acknowledgments
The authors would like to thank Robert Martin, Lead Operator, Information Technology, Texas Tech University Health Sciences Center at Amarillo for assistance in computer image enhancement and development.
CORRESPONDENCE
Timothy J. Benton, MD, Texas Tech University Health Sciences Center at Amarillo, Department of Family and Community Medicine, 1600 Wallace Boulevard, Amarillo, TX 79106. E-mail: [email protected]
A 68-year-old man came to the emergency department complaining of left-side thoracic back pain, after 5 days of outpatient treatment with analgesics did not help him. His pain started after physical labor, but he did not recall any trauma. A review of his medical history revealed only coronary artery disease, with coronary stent placement several years before this event. He had not been hospitalized recently, undergone an invasive procedure, or taken antibiotics.
On examination, a left thoracic paraspinal muscle was tender without fluctuance, overlying skin redness, or a lesion. An elevated white blood cell count of 12,300/mcL was the only laboratory test with abnormal results. The patient did not have fever, and results of urinalysis, chest radiograph, and abdominal sonogram were normal. Computed tomography (CT) images of the abdomen and pelvis showed inflammation of a left thoracic paraspinal muscle.
Thirty-six hours after admission, the patient developed fever (38.8°C). His physicians obtained a blood culture. The fever recurred (at 38.9°C) the following day, and 2 more blood cultures were done. His back pain did not improve despite analgesics, intravenous antibiotics, and physical therapy; therefore, on the eighth day in the hospital, magnetic resonance imaging (MRI) was performed (FIGURE).
FIGURE
MRI of the back
What is the diagnosis?
Diagnosis: Methicillin-resistant Staphylococcus aureus pyomyositis
Reports of the 3 blood cultures, acquired on the seventh day in the hospital, showed growth of methicillin-resistant Staphylococcus aureus (MRSA) with antibiotic susceptibility patterns common to community-acquired MRSA.1 A purulent aspirate was obtained from the lesion in the FIGURE with CT-guided drainage. Community-acquired MRSA grew in the aspirate culture. The final diagnosis was a primary skeletal muscle abscess without contiguous spread from an adjacent site, or pyomyositis.
Epidemiology of pyomyositis
Pyomyositis is uncommon in immunocompetent individuals living outside of the tropics. It is usually caused by S aureus. In the United States between 1981 and 2002, 330 cases were identified in a literature review,2 which noted an increasing incidence. Of these cases, 70% were caused by S aureus and 61.5% of patients were immunocompromised; 1 involved MRSA.
In 2003, 2 of 3 MRSA cases were reported in patients with hematologic disorders.3 In 2005, 4 community-acquired MRSA cases were reported;1 2 had other illnesses leading to increased risk. MRSA pyomyositis is now being reported in immunocompetent individuals, but most cases arise in patients with cancer, diabetes mellitus, rheumatologic disorders, hematologic disorders, renal failure, liver cirrhosis, intravenous drug use, or HIV infection.2,4,5 With staphylococcal infections increasing,6 including MRSA and community-acquired MRSA, the incidence of pyomyositis may increase correspondingly.
Consider the possibility of pyomyositis in patients with localized muscle pain and tenderness and who have risk factors for acquiring MRSA—living in a community with prevalent MRSA, recent hospitalization, antibiotic use, invasive procedures, or chronic venous catheters.
Most commonly, pyomyositis occurs in a leg or arm.2 In the 330 cases mentioned above, the sites of infection, in descending order of frequency, were lower extremity, upper extremity, buttocks, chest wall, paraspinal, and psoas.
Diagnostic evaluation: Know the stages
Making the correct diagnosis at the initial presentation is difficult because nonspecific symptoms resemble a muscle strain. But this infection progresses to bacteremia, making early identification important. To recognize pyomyositis before bacteremia develops, rely on clinical suspicion and familiarity with the 3 stages of the disease.
Stage 1 (invasive) is characterized by muscle pain and tenderness without systemic evidence of illness. Stage 2 (suppurative) is the formation of an abscess. At this time systemic symptoms such as fever may occur; otherwise physical exam findings remain vague with tenderness and induration without overlying skin redness or palpable fluctuance common to skin abscesses. Stage 3 is bacteremia or sepsis. Awareness of the risks and the stages of pyomyositis will aid in quicker diagnosis.
Diagnostic delay occurs because the first stage presents with nonspecific symptoms and examination findings, and also because initial laboratory and radiographic testing are inconclusive. Elevation of the white blood cell count and the erythrocyte sedimentation rate occur early, while serum muscle enzymes remain normal.2,4,5
Imaging studies performed during the first stage may not be productive; however, in the second stage imaging identifies the abscess. Although limited data exist regarding the best imaging modality, MRI and CT appear most useful.1,3,4,7 In 1 retrospective analysis, ultrasound identified 5 of 8 cases correctly, while MRI and CT were diagnostic in 5 of 6 and 9 of 9, respectively.7
Treatment: Antibiotics, drainage
Choose an antibiotic empirically that covers S aureus and is also appropriate for MRSA. Pyomyositis discovered in the first stage may resolve with antibiotics alone.4 In addition, early intervention may be especially important with MRSA, since MRSA bacteremia is associated with increased mortality compared with methicillin-sensitive S aureus bacteremia.6
If the condition progresses to the second stage with abscess development, surgical or percutaneous drainage will be necessary. Identification and removal of the site of infection in patients with community-acquired staphylococcal bacteremia results in improved outcomes,8 and pyomyositis can be an overlooked source.
Patient outcome
The day following drainage of the abscess, the patient was discharged from the hospital. He was treated for 6 weeks with intravenous antibiotics because of staphylococcal bacteremia, and he has fully recovered.
Acknowledgments
The authors would like to thank Robert Martin, Lead Operator, Information Technology, Texas Tech University Health Sciences Center at Amarillo for assistance in computer image enhancement and development.
CORRESPONDENCE
Timothy J. Benton, MD, Texas Tech University Health Sciences Center at Amarillo, Department of Family and Community Medicine, 1600 Wallace Boulevard, Amarillo, TX 79106. E-mail: [email protected]
1. Ruiz M, Yohannes S, Wladyka CG. Pyomyositis caused by methicillin-resistant Staphylococcus aureus. N Engl J Med 2005;352:1488-1489.
2. Crum NF. Bacterial pyomyositis in the United States. Am J Med 2004;117:420-428.
3. Hayashi T. Pyomyositis as a focus of infection in hematological disorders: a report of 3 cases. Int J Hematol 2003;77:171-174.
4. Ebright JR, Pieper B. Skin and soft tissue infections in injection drug users. Infect Dis Clin North Am 2002;16:697-712.
5. Hossain A, Reis ED, Soundararajan K, Kerstain MD, Hollier LH. Nontropical pyomyositis: analysis of eight patients in an urban center. Am Surg 2000;66:1064-1066.
6. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53-59.
7. Boniotti V. Contribution of imaging to the evaluation of pyomyositis. Radiol Med 2005;109:404-13.
8. Jensen AG. Importance of focus identification in the treatment of Staphylococcus aureus bacteremia. J Hosp Infect 2002;52:29-36.
1. Ruiz M, Yohannes S, Wladyka CG. Pyomyositis caused by methicillin-resistant Staphylococcus aureus. N Engl J Med 2005;352:1488-1489.
2. Crum NF. Bacterial pyomyositis in the United States. Am J Med 2004;117:420-428.
3. Hayashi T. Pyomyositis as a focus of infection in hematological disorders: a report of 3 cases. Int J Hematol 2003;77:171-174.
4. Ebright JR, Pieper B. Skin and soft tissue infections in injection drug users. Infect Dis Clin North Am 2002;16:697-712.
5. Hossain A, Reis ED, Soundararajan K, Kerstain MD, Hollier LH. Nontropical pyomyositis: analysis of eight patients in an urban center. Am Surg 2000;66:1064-1066.
6. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis 2003;36:53-59.
7. Boniotti V. Contribution of imaging to the evaluation of pyomyositis. Radiol Med 2005;109:404-13.
8. Jensen AG. Importance of focus identification in the treatment of Staphylococcus aureus bacteremia. J Hosp Infect 2002;52:29-36.