User login
What is the microbiology of liver abscess?
Case
A 29-year-old woman with chronic urticaria, previously on omalizumab, presented with 2 weeks of abdominal pain and fever. She had traveled to Nicaragua within the past 10 months. CT showed a 6 x 5 cm liver abscess. Entamoeba histolytica was detected by stool polymerase chain reaction, and E. histolytica antibody was positive. The abscess was drained, and she completed a 10-day course of metronidazole followed by a 7-day course of paromomycin.
Brief overview
Bacterial, parasitic, and fungal organisms can cause liver abscess. Worldwide, bacteria are the most common cause of liver abscess. Infection is usually polymicrobial, though Klebsiella and the Streptococcus milleri group are the most common organisms identified.
Entamoeba histolytica is the most frequent cause of amoebic liver abscess and should be strongly considered in a returning traveler, visitor from another country, or those on monoclonal antibody therapy directed against IgE such as omalizumab. Candida species are the most common fungal etiology; an example being hepatosplenic candidiasis in hematologic malignancies.
Overview of the data
Pyogenic liver abscess. A variety of bacteria have been isolated from pyogenic liver abscesses (PLA) because of differences in mechanism of infection (such as biliary tract interventions, postoperative complications, and hematogenous spread), immunocompromised states, and geographical variation. The literature is not robust for pyogenic liver abscesses, and the microbiology isolated via epidemiologic studies are confounded by the mechanism of infection and thus difficult to generalize.
Initially, the Enterobacteriaceae including Klebsiella pneumoniae and Escherichia coli were the most common cause of PLA in the United States. The emergence of improved culturing techniques, which has improved the yield of facultative anaerobes such as the Streptococcus milleri (also known as Streptococcus anginosus) group, has led to an increased incidence and wider assortment of bacteria, with a more recent study of 38 patients in the Cleveland Clinic system showing that about half of the PLA were polymicrobial with the predominant organism when monomicrobial being of the Strep milleri group in 9/22 patients (Chemaly et al.).
Biliary tract disease, whether from choledocholithiasis, stricture, or malignant obstruction is the most common etiology of PLA. Much of the PLA-focused literature is from Asia, where Klebsiella is more commonly a cause of liver abscess. In a study of 248 Taiwanese patients with PLA, Klebsiella was responsible for 69% of PLA (Yang et al.). In a study of 79 patients hospitalized in New York, Klebsiella was the most common bacteria isolated, although more than half of the patients studied were Asian, and Klebsiella was more common among Asian patients than the other groups studied. An 8-year analysis of patients admitted to a University Hospital in Taiwan with cryptogenic PLA showed that the etiology was Klebsiella in 46/52 patients (Chen et al.). Most patients with Klebsiella liver abscess have documented bacteremia.
The second most common mechanism is bacterial translocation through the portal venous system. E. coli is commonly isolated and is frequently spread from intra-abdominal infections such as appendicitis leading to pylephlebitis. As the diagnosis and management of appendicitis has improved, the incidence of appendicitis causing a PLA has decreased.
PLA should be cultured to guide therapy and catheter drainage may be required. However, common organisms causing liver abscess should also be considered when selecting initial antibiotic therapy as cultures are frequently affected by previous antibiotic exposure or imprecise culturing techniques. Blood cultures should be obtained, and empiric therapy with a beta-lactam/beta-lactamase inhibitor or third-generation cephalosporin plus metronidazole should be started thereafter.
Entamoeba histolytica. E. histolytica, an anaerobic parasite that can lead to amoebic dysentery and liver abscess, affects upwards of 50 million people worldwide, predominantly in India and sub-Saharan Africa. Travel to an endemic area for longer than 1 month carries a high risk of transmission, though cases have been described with less than a week of exposure.
Infection occurs following consumption of affected food or water and can lead to dysentery within 3 weeks. Fever and right upper quadrant pain develop later, anywhere from 3 months to years following initial exposure. To diagnose, both serologic and stool testing for E. histolytica are recommended owing to the high sensitivity and low specificity of the serologic antibody test and the low sensitivity and high specificity of the stool antigen test. Imaging may reveal a single cyst with surrounding edema, which is characteristic.
Effective treatment is a two-step process. Metronidazole targets trophozoites that cause liver abscesses followed by paromomycin or diloxanide furoate to eradicate luminal oocysts and prevent reinfection. Aspiration and catheter drainage is necessary if the microbiology or etiology of the liver abscess remains uncertain, patients are not responding to antibiotics, or there is concern for impending rupture with cyst size greater than 6 cm (Jun et al.).
Hydatid cysts. Serologic testing via enzyme-linked immunoassay and radiographic characteristics are used to diagnose cysts caused by Echinococcus, of which there are many species. Imaging typically shows a well-defined cyst with calcifications and budding daughter cysts. Aspiration of an echinococcal cyst carries a risk of anaphylaxis and spread of infection and should only be undertaken if there is serologic and radiographic uncertainty.
Fungal abscesses. Fungal abscesses are most commonly caused by Candida species. The typical patient presentation includes high fever and elevated alkaline phosphatase, usually during the count recovery phase of patients with hematologic malignancies undergoing chemotherapy.
Fungal abscesses are frequently too small to aspirate. Fortunately, serum and radiographic results, as well as the clinical setting, make diagnosis more straightforward. Serum fungal markers can be checked and empiric treatment with amphotericin B or an echinocandin is recommended, followed by narrowing to oral fluconazole. Treatment should continue until abscesses resolve.
Interestingly, if patients become neutropenic during their antifungal course, the microabscesses may disappear on CT or MRI, only to reappear once neutrophils return. Once patients have a stable neutrophil count and imaging shows no abscesses, antifungal treatment can be discontinued, but must be restarted if patients are to undergo additional chemotherapy with expected neutropenia.
Back to the case
While impossible to state with certainty, infection with E. histolytica while in Nicaragua was thought most likely in this case. This patient was on omalizumab for chronic urticaria immediately prior to acquiring the infection and this anti-IgE monoclonal antibody likely predisposed her to a parasitic infection. Knowing this epidemiology, she may not have required catheter drainage, however, the cyst was causing pain and drainage provided decompression. She was treated with antibiotics followed by paromomycin.
Bottom line
Entamoeba histolytica is the most common cause of liver abscess worldwide, but identifying risk factors and mechanism of infection can lead to the most likely infecting organism.
Dr. Mehra is assistant professor of medicine in the Section of Hospital Medicine at the University of Virginia Medical Center and School of Medicine, Charlottesville. Dr. Parsons is also assistant professor of medicine in the Section of Hospital Medicine at the University of Virginia Medical Center and School of Medicine.
References
Chemaly RF. Microbiology of liver abscesses and the predictive value of abscess gram stain and associated blood cultures. Diagn Microbiol Infect Dis. 2003;46(4):245-8.
Yang CC. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect. 2004;37(3):176.
Chen SC. Comparison of pyogenic liver abscesses of biliary and cryptogenic origin. An eight-year analysis in a University Hospital. Swiss Med Wkly. 2005;135(23-24):344-51.
Yang CC. Pyogenic liver abscess in Taiwan: emphasis on gas-forming liver abscess in diabetics. Am J Gastroenterol. 1993;88:1911-15.
Jun CH. Risk factors and clinical outcomes for spontaneous rupture of pyogenic liver abscess. J Dig Dis. 2015;16(1):31-6.
Smego RA Jr. Treatment options for hepatic cystic echinococcosis. Int J Infect Dis. 2005;9(2):69-76.
Additional reading
Huang CJ et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg. 1996;223(5):600-7.
Meddings L et al. A population-based study of pyogenic liver abscesses in the United States: incidence, mortality, and temporal trends. Am J Gastroenterol. 2010;105(1):117-24..
Petri WA, Singh U. Diagnosis and management of amoebiasis. Clin Infect Dis. 1999 Nov;29(5):1117-25.
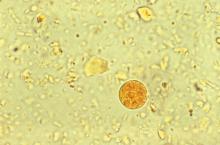
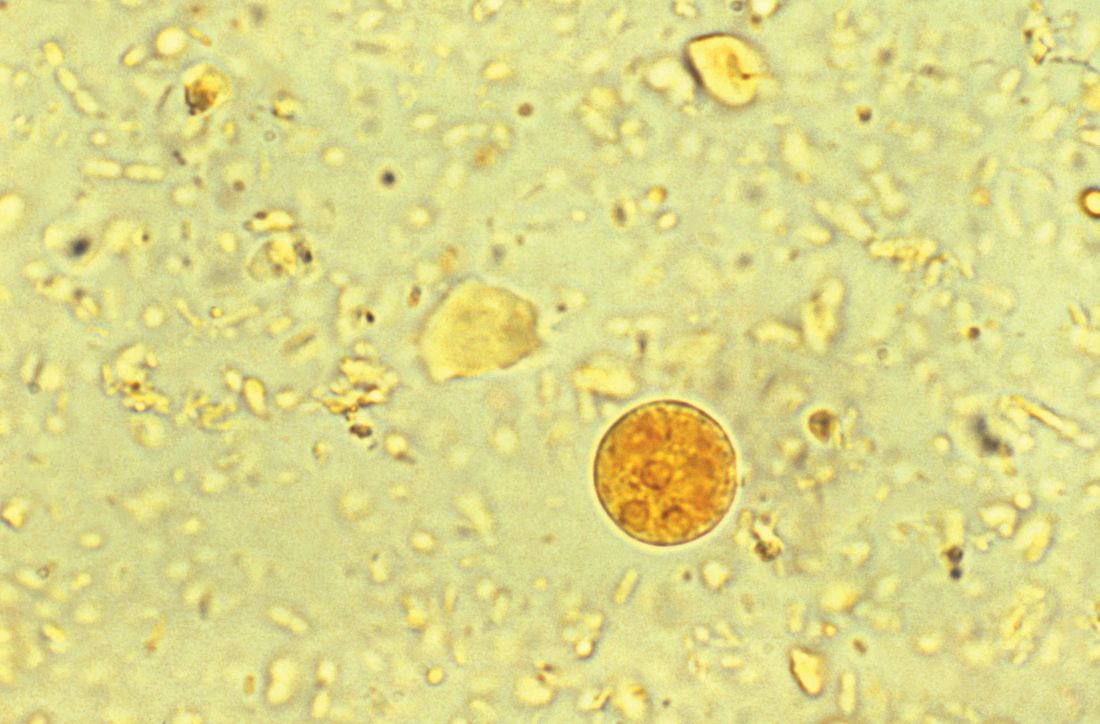
Accompanying Photo caption: CT scan showing E. histolytica liver abscess. RELATED PHOTO IS PHOTOMICROGRAPH, NOT CT SCAN. G
Quiz
Microbiology of liver abscesses
Bacterial, parasitic, and fungal organisms can all cause liver abscesses. History, including travel history, is very important in deciphering which organisms are present.
Question 1: What is the most common cause of an amoebic liver abscess worldwide?
A. Echinococcus
B. Klebsiella pneumoniae
C. Entamoeba histolytica
D. Escherichia coli
The best answer is choice C. E. histolytica causes amoebic dysentery and liver abscess. This anaerobic parasite affects 50 million people worldwide, with the highest prevalence in India, sub-Saharan Africa, Mexico, and parts of Central and South America. Travelers spending a month or more in endemic areas are at highest risk, but cases have been reported with less than one week of exposure.
Question 2: Which type of parasitic cyst should not be aspirated?
A. Echinococcus
B. Entamoeba histolytica
C. Schistosomiasis
D. Paramoeba
The best answer is choice A. Aspiration of an echinococcal cyst carries a risk of anaphylaxis and spread of infection and should only be done if there is serologic and radiographic uncertainty. Imaging typically shows a well-defined cyst with calcifications and budding daughter cysts.
Key Points
- Risk factors and mechanism of action will suggest the most likely organisms and guide antibiotic choice.
- Entamoeba histolytica is the most common cause of liver abscess worldwide.
- Stool PCR and antibody testing for E. histolytica should both be ordered in the work-up of a liver abscess.
- Calcifications and daughter cysts budding off the main cyst can distinguish echinococcal cyst from E. histolytica abscess radiographically.
Case
A 29-year-old woman with chronic urticaria, previously on omalizumab, presented with 2 weeks of abdominal pain and fever. She had traveled to Nicaragua within the past 10 months. CT showed a 6 x 5 cm liver abscess. Entamoeba histolytica was detected by stool polymerase chain reaction, and E. histolytica antibody was positive. The abscess was drained, and she completed a 10-day course of metronidazole followed by a 7-day course of paromomycin.
Brief overview
Bacterial, parasitic, and fungal organisms can cause liver abscess. Worldwide, bacteria are the most common cause of liver abscess. Infection is usually polymicrobial, though Klebsiella and the Streptococcus milleri group are the most common organisms identified.
Entamoeba histolytica is the most frequent cause of amoebic liver abscess and should be strongly considered in a returning traveler, visitor from another country, or those on monoclonal antibody therapy directed against IgE such as omalizumab. Candida species are the most common fungal etiology; an example being hepatosplenic candidiasis in hematologic malignancies.
Overview of the data
Pyogenic liver abscess. A variety of bacteria have been isolated from pyogenic liver abscesses (PLA) because of differences in mechanism of infection (such as biliary tract interventions, postoperative complications, and hematogenous spread), immunocompromised states, and geographical variation. The literature is not robust for pyogenic liver abscesses, and the microbiology isolated via epidemiologic studies are confounded by the mechanism of infection and thus difficult to generalize.
Initially, the Enterobacteriaceae including Klebsiella pneumoniae and Escherichia coli were the most common cause of PLA in the United States. The emergence of improved culturing techniques, which has improved the yield of facultative anaerobes such as the Streptococcus milleri (also known as Streptococcus anginosus) group, has led to an increased incidence and wider assortment of bacteria, with a more recent study of 38 patients in the Cleveland Clinic system showing that about half of the PLA were polymicrobial with the predominant organism when monomicrobial being of the Strep milleri group in 9/22 patients (Chemaly et al.).
Biliary tract disease, whether from choledocholithiasis, stricture, or malignant obstruction is the most common etiology of PLA. Much of the PLA-focused literature is from Asia, where Klebsiella is more commonly a cause of liver abscess. In a study of 248 Taiwanese patients with PLA, Klebsiella was responsible for 69% of PLA (Yang et al.). In a study of 79 patients hospitalized in New York, Klebsiella was the most common bacteria isolated, although more than half of the patients studied were Asian, and Klebsiella was more common among Asian patients than the other groups studied. An 8-year analysis of patients admitted to a University Hospital in Taiwan with cryptogenic PLA showed that the etiology was Klebsiella in 46/52 patients (Chen et al.). Most patients with Klebsiella liver abscess have documented bacteremia.
The second most common mechanism is bacterial translocation through the portal venous system. E. coli is commonly isolated and is frequently spread from intra-abdominal infections such as appendicitis leading to pylephlebitis. As the diagnosis and management of appendicitis has improved, the incidence of appendicitis causing a PLA has decreased.
PLA should be cultured to guide therapy and catheter drainage may be required. However, common organisms causing liver abscess should also be considered when selecting initial antibiotic therapy as cultures are frequently affected by previous antibiotic exposure or imprecise culturing techniques. Blood cultures should be obtained, and empiric therapy with a beta-lactam/beta-lactamase inhibitor or third-generation cephalosporin plus metronidazole should be started thereafter.
Entamoeba histolytica. E. histolytica, an anaerobic parasite that can lead to amoebic dysentery and liver abscess, affects upwards of 50 million people worldwide, predominantly in India and sub-Saharan Africa. Travel to an endemic area for longer than 1 month carries a high risk of transmission, though cases have been described with less than a week of exposure.
Infection occurs following consumption of affected food or water and can lead to dysentery within 3 weeks. Fever and right upper quadrant pain develop later, anywhere from 3 months to years following initial exposure. To diagnose, both serologic and stool testing for E. histolytica are recommended owing to the high sensitivity and low specificity of the serologic antibody test and the low sensitivity and high specificity of the stool antigen test. Imaging may reveal a single cyst with surrounding edema, which is characteristic.
Effective treatment is a two-step process. Metronidazole targets trophozoites that cause liver abscesses followed by paromomycin or diloxanide furoate to eradicate luminal oocysts and prevent reinfection. Aspiration and catheter drainage is necessary if the microbiology or etiology of the liver abscess remains uncertain, patients are not responding to antibiotics, or there is concern for impending rupture with cyst size greater than 6 cm (Jun et al.).
Hydatid cysts. Serologic testing via enzyme-linked immunoassay and radiographic characteristics are used to diagnose cysts caused by Echinococcus, of which there are many species. Imaging typically shows a well-defined cyst with calcifications and budding daughter cysts. Aspiration of an echinococcal cyst carries a risk of anaphylaxis and spread of infection and should only be undertaken if there is serologic and radiographic uncertainty.
Fungal abscesses. Fungal abscesses are most commonly caused by Candida species. The typical patient presentation includes high fever and elevated alkaline phosphatase, usually during the count recovery phase of patients with hematologic malignancies undergoing chemotherapy.
Fungal abscesses are frequently too small to aspirate. Fortunately, serum and radiographic results, as well as the clinical setting, make diagnosis more straightforward. Serum fungal markers can be checked and empiric treatment with amphotericin B or an echinocandin is recommended, followed by narrowing to oral fluconazole. Treatment should continue until abscesses resolve.
Interestingly, if patients become neutropenic during their antifungal course, the microabscesses may disappear on CT or MRI, only to reappear once neutrophils return. Once patients have a stable neutrophil count and imaging shows no abscesses, antifungal treatment can be discontinued, but must be restarted if patients are to undergo additional chemotherapy with expected neutropenia.
Back to the case
While impossible to state with certainty, infection with E. histolytica while in Nicaragua was thought most likely in this case. This patient was on omalizumab for chronic urticaria immediately prior to acquiring the infection and this anti-IgE monoclonal antibody likely predisposed her to a parasitic infection. Knowing this epidemiology, she may not have required catheter drainage, however, the cyst was causing pain and drainage provided decompression. She was treated with antibiotics followed by paromomycin.
Bottom line
Entamoeba histolytica is the most common cause of liver abscess worldwide, but identifying risk factors and mechanism of infection can lead to the most likely infecting organism.
Dr. Mehra is assistant professor of medicine in the Section of Hospital Medicine at the University of Virginia Medical Center and School of Medicine, Charlottesville. Dr. Parsons is also assistant professor of medicine in the Section of Hospital Medicine at the University of Virginia Medical Center and School of Medicine.
References
Chemaly RF. Microbiology of liver abscesses and the predictive value of abscess gram stain and associated blood cultures. Diagn Microbiol Infect Dis. 2003;46(4):245-8.
Yang CC. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect. 2004;37(3):176.
Chen SC. Comparison of pyogenic liver abscesses of biliary and cryptogenic origin. An eight-year analysis in a University Hospital. Swiss Med Wkly. 2005;135(23-24):344-51.
Yang CC. Pyogenic liver abscess in Taiwan: emphasis on gas-forming liver abscess in diabetics. Am J Gastroenterol. 1993;88:1911-15.
Jun CH. Risk factors and clinical outcomes for spontaneous rupture of pyogenic liver abscess. J Dig Dis. 2015;16(1):31-6.
Smego RA Jr. Treatment options for hepatic cystic echinococcosis. Int J Infect Dis. 2005;9(2):69-76.
Additional reading
Huang CJ et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg. 1996;223(5):600-7.
Meddings L et al. A population-based study of pyogenic liver abscesses in the United States: incidence, mortality, and temporal trends. Am J Gastroenterol. 2010;105(1):117-24..
Petri WA, Singh U. Diagnosis and management of amoebiasis. Clin Infect Dis. 1999 Nov;29(5):1117-25.
Accompanying Photo caption: CT scan showing E. histolytica liver abscess. RELATED PHOTO IS PHOTOMICROGRAPH, NOT CT SCAN. G
Quiz
Microbiology of liver abscesses
Bacterial, parasitic, and fungal organisms can all cause liver abscesses. History, including travel history, is very important in deciphering which organisms are present.
Question 1: What is the most common cause of an amoebic liver abscess worldwide?
A. Echinococcus
B. Klebsiella pneumoniae
C. Entamoeba histolytica
D. Escherichia coli
The best answer is choice C. E. histolytica causes amoebic dysentery and liver abscess. This anaerobic parasite affects 50 million people worldwide, with the highest prevalence in India, sub-Saharan Africa, Mexico, and parts of Central and South America. Travelers spending a month or more in endemic areas are at highest risk, but cases have been reported with less than one week of exposure.
Question 2: Which type of parasitic cyst should not be aspirated?
A. Echinococcus
B. Entamoeba histolytica
C. Schistosomiasis
D. Paramoeba
The best answer is choice A. Aspiration of an echinococcal cyst carries a risk of anaphylaxis and spread of infection and should only be done if there is serologic and radiographic uncertainty. Imaging typically shows a well-defined cyst with calcifications and budding daughter cysts.
Key Points
- Risk factors and mechanism of action will suggest the most likely organisms and guide antibiotic choice.
- Entamoeba histolytica is the most common cause of liver abscess worldwide.
- Stool PCR and antibody testing for E. histolytica should both be ordered in the work-up of a liver abscess.
- Calcifications and daughter cysts budding off the main cyst can distinguish echinococcal cyst from E. histolytica abscess radiographically.
Case
A 29-year-old woman with chronic urticaria, previously on omalizumab, presented with 2 weeks of abdominal pain and fever. She had traveled to Nicaragua within the past 10 months. CT showed a 6 x 5 cm liver abscess. Entamoeba histolytica was detected by stool polymerase chain reaction, and E. histolytica antibody was positive. The abscess was drained, and she completed a 10-day course of metronidazole followed by a 7-day course of paromomycin.
Brief overview
Bacterial, parasitic, and fungal organisms can cause liver abscess. Worldwide, bacteria are the most common cause of liver abscess. Infection is usually polymicrobial, though Klebsiella and the Streptococcus milleri group are the most common organisms identified.
Entamoeba histolytica is the most frequent cause of amoebic liver abscess and should be strongly considered in a returning traveler, visitor from another country, or those on monoclonal antibody therapy directed against IgE such as omalizumab. Candida species are the most common fungal etiology; an example being hepatosplenic candidiasis in hematologic malignancies.
Overview of the data
Pyogenic liver abscess. A variety of bacteria have been isolated from pyogenic liver abscesses (PLA) because of differences in mechanism of infection (such as biliary tract interventions, postoperative complications, and hematogenous spread), immunocompromised states, and geographical variation. The literature is not robust for pyogenic liver abscesses, and the microbiology isolated via epidemiologic studies are confounded by the mechanism of infection and thus difficult to generalize.
Initially, the Enterobacteriaceae including Klebsiella pneumoniae and Escherichia coli were the most common cause of PLA in the United States. The emergence of improved culturing techniques, which has improved the yield of facultative anaerobes such as the Streptococcus milleri (also known as Streptococcus anginosus) group, has led to an increased incidence and wider assortment of bacteria, with a more recent study of 38 patients in the Cleveland Clinic system showing that about half of the PLA were polymicrobial with the predominant organism when monomicrobial being of the Strep milleri group in 9/22 patients (Chemaly et al.).
Biliary tract disease, whether from choledocholithiasis, stricture, or malignant obstruction is the most common etiology of PLA. Much of the PLA-focused literature is from Asia, where Klebsiella is more commonly a cause of liver abscess. In a study of 248 Taiwanese patients with PLA, Klebsiella was responsible for 69% of PLA (Yang et al.). In a study of 79 patients hospitalized in New York, Klebsiella was the most common bacteria isolated, although more than half of the patients studied were Asian, and Klebsiella was more common among Asian patients than the other groups studied. An 8-year analysis of patients admitted to a University Hospital in Taiwan with cryptogenic PLA showed that the etiology was Klebsiella in 46/52 patients (Chen et al.). Most patients with Klebsiella liver abscess have documented bacteremia.
The second most common mechanism is bacterial translocation through the portal venous system. E. coli is commonly isolated and is frequently spread from intra-abdominal infections such as appendicitis leading to pylephlebitis. As the diagnosis and management of appendicitis has improved, the incidence of appendicitis causing a PLA has decreased.
PLA should be cultured to guide therapy and catheter drainage may be required. However, common organisms causing liver abscess should also be considered when selecting initial antibiotic therapy as cultures are frequently affected by previous antibiotic exposure or imprecise culturing techniques. Blood cultures should be obtained, and empiric therapy with a beta-lactam/beta-lactamase inhibitor or third-generation cephalosporin plus metronidazole should be started thereafter.
Entamoeba histolytica. E. histolytica, an anaerobic parasite that can lead to amoebic dysentery and liver abscess, affects upwards of 50 million people worldwide, predominantly in India and sub-Saharan Africa. Travel to an endemic area for longer than 1 month carries a high risk of transmission, though cases have been described with less than a week of exposure.
Infection occurs following consumption of affected food or water and can lead to dysentery within 3 weeks. Fever and right upper quadrant pain develop later, anywhere from 3 months to years following initial exposure. To diagnose, both serologic and stool testing for E. histolytica are recommended owing to the high sensitivity and low specificity of the serologic antibody test and the low sensitivity and high specificity of the stool antigen test. Imaging may reveal a single cyst with surrounding edema, which is characteristic.
Effective treatment is a two-step process. Metronidazole targets trophozoites that cause liver abscesses followed by paromomycin or diloxanide furoate to eradicate luminal oocysts and prevent reinfection. Aspiration and catheter drainage is necessary if the microbiology or etiology of the liver abscess remains uncertain, patients are not responding to antibiotics, or there is concern for impending rupture with cyst size greater than 6 cm (Jun et al.).
Hydatid cysts. Serologic testing via enzyme-linked immunoassay and radiographic characteristics are used to diagnose cysts caused by Echinococcus, of which there are many species. Imaging typically shows a well-defined cyst with calcifications and budding daughter cysts. Aspiration of an echinococcal cyst carries a risk of anaphylaxis and spread of infection and should only be undertaken if there is serologic and radiographic uncertainty.
Fungal abscesses. Fungal abscesses are most commonly caused by Candida species. The typical patient presentation includes high fever and elevated alkaline phosphatase, usually during the count recovery phase of patients with hematologic malignancies undergoing chemotherapy.
Fungal abscesses are frequently too small to aspirate. Fortunately, serum and radiographic results, as well as the clinical setting, make diagnosis more straightforward. Serum fungal markers can be checked and empiric treatment with amphotericin B or an echinocandin is recommended, followed by narrowing to oral fluconazole. Treatment should continue until abscesses resolve.
Interestingly, if patients become neutropenic during their antifungal course, the microabscesses may disappear on CT or MRI, only to reappear once neutrophils return. Once patients have a stable neutrophil count and imaging shows no abscesses, antifungal treatment can be discontinued, but must be restarted if patients are to undergo additional chemotherapy with expected neutropenia.
Back to the case
While impossible to state with certainty, infection with E. histolytica while in Nicaragua was thought most likely in this case. This patient was on omalizumab for chronic urticaria immediately prior to acquiring the infection and this anti-IgE monoclonal antibody likely predisposed her to a parasitic infection. Knowing this epidemiology, she may not have required catheter drainage, however, the cyst was causing pain and drainage provided decompression. She was treated with antibiotics followed by paromomycin.
Bottom line
Entamoeba histolytica is the most common cause of liver abscess worldwide, but identifying risk factors and mechanism of infection can lead to the most likely infecting organism.
Dr. Mehra is assistant professor of medicine in the Section of Hospital Medicine at the University of Virginia Medical Center and School of Medicine, Charlottesville. Dr. Parsons is also assistant professor of medicine in the Section of Hospital Medicine at the University of Virginia Medical Center and School of Medicine.
References
Chemaly RF. Microbiology of liver abscesses and the predictive value of abscess gram stain and associated blood cultures. Diagn Microbiol Infect Dis. 2003;46(4):245-8.
Yang CC. Comparison of pyogenic liver abscess caused by non-Klebsiella pneumoniae and Klebsiella pneumoniae. J Microbiol Immunol Infect. 2004;37(3):176.
Chen SC. Comparison of pyogenic liver abscesses of biliary and cryptogenic origin. An eight-year analysis in a University Hospital. Swiss Med Wkly. 2005;135(23-24):344-51.
Yang CC. Pyogenic liver abscess in Taiwan: emphasis on gas-forming liver abscess in diabetics. Am J Gastroenterol. 1993;88:1911-15.
Jun CH. Risk factors and clinical outcomes for spontaneous rupture of pyogenic liver abscess. J Dig Dis. 2015;16(1):31-6.
Smego RA Jr. Treatment options for hepatic cystic echinococcosis. Int J Infect Dis. 2005;9(2):69-76.
Additional reading
Huang CJ et al. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg. 1996;223(5):600-7.
Meddings L et al. A population-based study of pyogenic liver abscesses in the United States: incidence, mortality, and temporal trends. Am J Gastroenterol. 2010;105(1):117-24..
Petri WA, Singh U. Diagnosis and management of amoebiasis. Clin Infect Dis. 1999 Nov;29(5):1117-25.
Accompanying Photo caption: CT scan showing E. histolytica liver abscess. RELATED PHOTO IS PHOTOMICROGRAPH, NOT CT SCAN. G
Quiz
Microbiology of liver abscesses
Bacterial, parasitic, and fungal organisms can all cause liver abscesses. History, including travel history, is very important in deciphering which organisms are present.
Question 1: What is the most common cause of an amoebic liver abscess worldwide?
A. Echinococcus
B. Klebsiella pneumoniae
C. Entamoeba histolytica
D. Escherichia coli
The best answer is choice C. E. histolytica causes amoebic dysentery and liver abscess. This anaerobic parasite affects 50 million people worldwide, with the highest prevalence in India, sub-Saharan Africa, Mexico, and parts of Central and South America. Travelers spending a month or more in endemic areas are at highest risk, but cases have been reported with less than one week of exposure.
Question 2: Which type of parasitic cyst should not be aspirated?
A. Echinococcus
B. Entamoeba histolytica
C. Schistosomiasis
D. Paramoeba
The best answer is choice A. Aspiration of an echinococcal cyst carries a risk of anaphylaxis and spread of infection and should only be done if there is serologic and radiographic uncertainty. Imaging typically shows a well-defined cyst with calcifications and budding daughter cysts.
Key Points
- Risk factors and mechanism of action will suggest the most likely organisms and guide antibiotic choice.
- Entamoeba histolytica is the most common cause of liver abscess worldwide.
- Stool PCR and antibody testing for E. histolytica should both be ordered in the work-up of a liver abscess.
- Calcifications and daughter cysts budding off the main cyst can distinguish echinococcal cyst from E. histolytica abscess radiographically.
Fecal microbiota transplantation by capsule effective in preventing recurrent C. difficile
Clinical question: Is fecal microbiota transplantation (FMT) by oral capsule noninferior to administration via colonoscopy in preventing recurrent Clostridium difficile infection (RCDI)?
Background: Approximately 20% of patients with an initial episode of C. difficile develop recurrent disease. FMT is the most effective treatment for RCDI. Currently, it is believed that there is a higher rate of success with FMT by colonoscopy, but this is based on studies lacking a control group. The cost of administering FMT by colonoscopy is more than double the cost via oral capsule, and efficacy between the two routes has not been studied in a randomized fashion. If oral capsule delivery is noninferior, then wait times, cost, and procedure risk would be reduced.
Study design: Randomized, unblinded, noninferiority trial.
Setting: Three academic medical centers in Alberta, Ca.
Synopsis: Patients with at least three documented episodes of C. difficile infection were randomized to receive FMT by either oral capsule or colonoscopy. Exclusion criteria included complicated C. difficile infections, cancer undergoing therapy, and conditions requiring antibiotics. The primary outcome was RCDI within 12 weeks after FMT. A total of 105 patients completed the trial, with 96.2% (51/53) of patients in the capsule group and 96.2% (50/52) of patients in the colonoscopy group remaining free of RCDI at the 12-week follow-up. This met the –15% noninferiority margin and suggests that oral capsule may be an effective route of delivery for FMT. Limitations of the study are exclusion of complicated RCDI patients, lack of blinding, and no placebo control (which would have been helpful since the prevention rates were so high and recurrent diarrhea was self-reported among participants, leading to a subjective outcome).
Bottom line: FMT by oral capsule may be noninferior to FMT by colonoscopy in preventing RCDI at 12 weeks.
Citation: Kao D et al. Effect of oral capsule- vs. colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection: A randomized clinical trial. JAMA. 2017 Nov 28;318(20):1985-93.
Dr. Mehra is assistant professor of medicine, division of hospital medicine, University of Virginia.
Clinical question: Is fecal microbiota transplantation (FMT) by oral capsule noninferior to administration via colonoscopy in preventing recurrent Clostridium difficile infection (RCDI)?
Background: Approximately 20% of patients with an initial episode of C. difficile develop recurrent disease. FMT is the most effective treatment for RCDI. Currently, it is believed that there is a higher rate of success with FMT by colonoscopy, but this is based on studies lacking a control group. The cost of administering FMT by colonoscopy is more than double the cost via oral capsule, and efficacy between the two routes has not been studied in a randomized fashion. If oral capsule delivery is noninferior, then wait times, cost, and procedure risk would be reduced.
Study design: Randomized, unblinded, noninferiority trial.
Setting: Three academic medical centers in Alberta, Ca.
Synopsis: Patients with at least three documented episodes of C. difficile infection were randomized to receive FMT by either oral capsule or colonoscopy. Exclusion criteria included complicated C. difficile infections, cancer undergoing therapy, and conditions requiring antibiotics. The primary outcome was RCDI within 12 weeks after FMT. A total of 105 patients completed the trial, with 96.2% (51/53) of patients in the capsule group and 96.2% (50/52) of patients in the colonoscopy group remaining free of RCDI at the 12-week follow-up. This met the –15% noninferiority margin and suggests that oral capsule may be an effective route of delivery for FMT. Limitations of the study are exclusion of complicated RCDI patients, lack of blinding, and no placebo control (which would have been helpful since the prevention rates were so high and recurrent diarrhea was self-reported among participants, leading to a subjective outcome).
Bottom line: FMT by oral capsule may be noninferior to FMT by colonoscopy in preventing RCDI at 12 weeks.
Citation: Kao D et al. Effect of oral capsule- vs. colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection: A randomized clinical trial. JAMA. 2017 Nov 28;318(20):1985-93.
Dr. Mehra is assistant professor of medicine, division of hospital medicine, University of Virginia.
Clinical question: Is fecal microbiota transplantation (FMT) by oral capsule noninferior to administration via colonoscopy in preventing recurrent Clostridium difficile infection (RCDI)?
Background: Approximately 20% of patients with an initial episode of C. difficile develop recurrent disease. FMT is the most effective treatment for RCDI. Currently, it is believed that there is a higher rate of success with FMT by colonoscopy, but this is based on studies lacking a control group. The cost of administering FMT by colonoscopy is more than double the cost via oral capsule, and efficacy between the two routes has not been studied in a randomized fashion. If oral capsule delivery is noninferior, then wait times, cost, and procedure risk would be reduced.
Study design: Randomized, unblinded, noninferiority trial.
Setting: Three academic medical centers in Alberta, Ca.
Synopsis: Patients with at least three documented episodes of C. difficile infection were randomized to receive FMT by either oral capsule or colonoscopy. Exclusion criteria included complicated C. difficile infections, cancer undergoing therapy, and conditions requiring antibiotics. The primary outcome was RCDI within 12 weeks after FMT. A total of 105 patients completed the trial, with 96.2% (51/53) of patients in the capsule group and 96.2% (50/52) of patients in the colonoscopy group remaining free of RCDI at the 12-week follow-up. This met the –15% noninferiority margin and suggests that oral capsule may be an effective route of delivery for FMT. Limitations of the study are exclusion of complicated RCDI patients, lack of blinding, and no placebo control (which would have been helpful since the prevention rates were so high and recurrent diarrhea was self-reported among participants, leading to a subjective outcome).
Bottom line: FMT by oral capsule may be noninferior to FMT by colonoscopy in preventing RCDI at 12 weeks.
Citation: Kao D et al. Effect of oral capsule- vs. colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection: A randomized clinical trial. JAMA. 2017 Nov 28;318(20):1985-93.
Dr. Mehra is assistant professor of medicine, division of hospital medicine, University of Virginia.