User login
What you can do to optimize blood conservation in ObGyn practice
The authors report no financial relationships relevant to this article.
Obstetric hemorrhage is responsible for approximately 17% to 25% of all pregnancy-related deaths.1 Excessive blood loss also is a risk during gynecologic surgery. Iron-deficiency anemia increases the risk of complication and the need for transfusion in both settings. By identifying and treating anemia before childbirth and elective surgery, you can optimize the patient’s condition and usually avert the need for emergency transfusion.
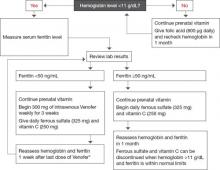
The Geisinger Health System has developed a unique Blood Conservation Program that focuses on the prevention of major blood loss by identifying and treating anemia in antepartum, postpartum, and gynecologic patients. The program’s protocols for treating anemia in antepartum and surgical patients are illustrated in FIGURES 1 AND 2. Geisinger practitioners have found that adherence to these protocols reduces the need for transfusion in many patients and improves their quality of life.
Here, we 1) look at the key data that will help you identify and then treat anemia in gynecologic, obstetric, and postpartum patients and 2) describe a variety of treatment options.
FIGURE 1 The gynecologic surgical patient: Preop diagnosis and treatment of anemia
* If anemia is refractory to iron therapy, consider erythropoietin therapy if benefits outweigh risks.
FIGURE 2 For the antepartum patient: Diagnosis and treatment of anemia
* If anemia is refractory to iron therapy, consider erythropoietin therapy if benefits outweigh risks.
Focus on the baseline hemoglobin level
The key to prevention of emergency transfusion—as well as postpartum anemia—is optimization of the patient’s hemoglobin level before delivery. It also is prudent when elective surgery is planned. In our institution, clinicians whose patients are at risk for hemorrhage or significant blood loss have the option of consulting with the Blood Conservation Program.
When the program began in November 2004, its primary purpose was to reduce the need for blood transfusion in elective surgery, including gynecologic procedures. It later expanded to include obstetric patients who have a hemoglobin level below 11 g/dL and patients who are considered to be at risk of major blood loss.
In addition to obstetric and surgical patients, the Geisinger Blood Conservation Program provides support for patients who will not accept blood or blood products for religious or personal reasons, even in life-threatening situations. The program has provided more than 8,000 consultations to date.
When to evaluate patients for anemia
Anemia in women is most often defined as a hemoglobin level below 12 g/dL or a hematocrit below 36%. In pregnant patients, the cutoff points are lower: 11 g/dL and 33%, respectively. During pregnancy, hemoglobin and hematocrit levels reach their nadir during the second trimester and then begin to rise until term.
Symptoms of anemia include fatigue, depression, shortness of breath, hypotension, and heart palpitations. However, some patients at risk of major blood loss during delivery or surgery do not display typical symptoms associated with anemia, and the condition can be confirmed only by laboratory testing.
At Geisinger, we recommend consultation with the Blood Conservation Program for any patient who exhibits symptoms of anemia or who is at risk of major blood loss. For example, the risk of blood loss during childbirth varies with the method of delivery.1 On average, obstetric patients lose 500 mL of blood during vaginal delivery; 1,000 mL during cesarean delivery; and 1,500 mL when cesarean delivery is followed by hysterectomy.1,2 Hemorrhage is classified as follows:
- Class 1 – Blood loss as high as 750 mL, or 15% of blood volume
- Class 2 – 750 to 1,500 mL, or 15% to 30% of blood volume
- Class 3 – 1,500 to 2,400 mL, or 30% to 40% of blood volume
- Class 4 – more than 2,400 mL, or more than 40% of blood volume.1
Abnormal placentation, such as placenta accreta, percreta, increta, and previa, which can often be diagnosed antepartum, may lead to significant blood loss during and after delivery. Obstetric emergencies, including abruption, trauma, and uterine rupture, may also be associated with major blood loss.
Iron deficiency lies at the root of most cases of anemia
Iron deficiency affects an estimated 2.15 billion people globally, with a prevalence of 12% to 43% worldwide.3,4 The daily iron requirement is 1 mg of elemental iron for nonobstetric patients, 2 mg for pregnant and lactating women. Latent iron deficiency is common in women who have had multiple pregnancies. These and other important facts about iron are described in the Box “Essential facts about iron”.
In iron-deficiency anemia, the following serum levels are reduced:
- Iron. A normal reading is 60 to 170 μg/dL.
- Hemoglobin, a measure of the production and turnover of red blood cells. A normal level is ≥12 g/dL (≥11 g/dL in pregnancy).
- Serum ferritin (a protein that stores iron). A normal reading is 12 to 150 ng/mL.
- Transferrin saturation. Transferrin is a transporting protein that shuttles iron to the bone marrow. The normal transferrin saturation level ranges from 20% to 50%.
Ferritin and hemoglobin levels tend to be the most efficient indicators of iron status.5
Some clinicians may also use:
- Mean corpuscular volume (MCV). Normal is 80 to 96 fL.
- Random distribution of red blood cell weight (RDW). A normal value is 11.5% to 15.5%.
- Reticulocyte count. Normal is 0.4% to 2.3%.
Laboratory tests for iron deficiency
When the Blood Conservation Program is initially consulted, the laboratory studies we recommend are based on the clinical presentation and condition of the patient. During pregnancy, we try to take account of the normal hemodynamic changes that occur during gestation. Therefore, we recommend:
- assessment of the serum ferritin level
- complete blood count (CBC) with differential. (If the hemoglobin/hematocrit is low, a peripheral smear is recommended to further evaluate microcytic anemia.)
Transferrin saturation and serum iron levels have not been shown to be useful markers in pregnant women because they are not specific for iron-restricted erythropoiesis and can be abnormally low during pregnancy.6
In nonpregnant patients, we recommend initial evaluation of:
- serum iron level
- total iron-binding capacity (TIBC). Normal levels are 240 to 450 μg/dL
- transferrin saturation.
A caveat about the ferritin level
Ferritin is both an iron-storage indicator and an acute-phase protein, so the clinician must be careful to exclude inflammatory processes that can elevate the ferritin level, giving a false indicator of iron stability in the maternal system. These inflammatory processes can include preeclampsia and neoplastic or infectious conditions.7 Transferrin saturation, however, is not affected by inflammatory processes and can be used as a confirmatory test for iron deficiency.4
Try oral iron supplementation first
When laboratory testing confirms the presence of iron-deficiency anemia, initial management is oral iron supplementation for 2 weeks, followed by repeat laboratory evaluation.
For patients scheduled for surgery, oral therapy includes a daily dosage of:
- 325 mg of ferrous sulfate
- 250 mg of vitamin C
- 800 μg of folic acid
- a multivitamin.
For perinatal patients, the daily oral regimen is:
- 325 mg of ferrous sulfate
- 250 mg of vitamin C
- a prenatal vitamin.
These medications are the least expensive alternatives for treating anemia.
Advise patients who are taking iron supplements not to ingest the medication with dairy products, coffee, tea, or foods that have a high content of phytic acid (e.g., grains, seeds, and legumes). Foods and prescription drugs that interact with iron supplements are listed in TABLE 1, along with recommendations on optimal timing of iron supplementation and other medications.
When you prescribe oral iron supplementation, bear in mind that some patients experience gastrointestinal side effects—constipation, nausea, diarrhea—so unpleasant that they stop taking their medication. In that scenario, you will need to find alternative formulations or delivery routes. One alternative you can suggest is a daily helping of blackstrap molasses, which supplies 27 mg of elemental iron per tablespoon.
Oral therapy should be continued even after hemoglobin and ferritin levels normalize. If laboratory values remain low after 2 weeks of oral therapy, parenteral therapy can be added to the oral regimen.
Therapy may be discontinued 2 months after delivery of the infant or surgery as long as the cause of the blood loss has been remedied. If the mother is breastfeeding, she should continue taking a prenatal vitamin until nursing has stopped.
TABLE 1
Some foods and drugs don’t mix well with iron
| Food or drug | Interaction | Recommendations |
|---|---|---|
| Foods high in phytic acid (grains, seeds, legumes) | Decreased absorption of iron | Do not take iron within 2 hours of eating foods high in phytic acid |
| Dairy products | Decreased bioavailability of iron | Do not take iron supplements within 1 hour of consuming dairy products, which can significantly decrease iron absorption |
| Levothyroxine | Iron reduces levothyroxine serum levels and efficacy | Take levothyroxine and iron at least 4 hours apart |
| Methyldopa | Oral iron reduces the efficacy of methyldopa | Consider IV iron or take oral iron and methyldopa as far apart as possible |
| Proton pump inhibitors (PPIs) | Absorption of oral iron is enhanced by gastric acid. PPIs decrease gastric acid production, thereby reducing the bioavailability of iron | Consider IV iron preparations |
| Ofloxacin | Iron reduces efficacy of ofloxacin | Administer ofloxacin and iron 2 hours apart |
| Cholestyramine | Decreased efficacy of iron | Administer iron and cholestyramine at least 4 hours apart |
| Calcium, aluminum, magnesium | Decreased absorption of iron | Iron should be taken at least 1 hour before or 2 hours after products that contain calcium, aluminum, or magnesium |
| Note: This table is not a comprehensive summary of all medications used in practice, but a list of those used commonly in obstetric and gynecologic populations | ||
IV iron isn’t as risky as you think
Historically, clinicians have avoided using parenteral iron sucrose (Venofer) because they have been taught that it can cause an anaphylactic reaction. In fact, although anaphylaxis may have been associated with older intravenous (IV) iron preparations, clinical trials have demonstrated the safety of IV iron sucrose and low-molecular-weight iron dextran. In a study involving 800 patients, Breymann and colleagues demonstrated that parenteral iron preparations containing dextran or iron dextrin could be safely given to pregnant women.4 Only 1.5% of the patients in the study experienced side effects from the therapy, and no anaphylactic reactions were observed.
In another study, 25 pregnant patients were given IV iron sucrose, and the only adverse reaction reported was a “not-unpleasant taste” during the injection.8
In an additional study, Breymann and colleagues found no adverse outcomes in 20 postpartum patients who received IV iron sucrose in addition to erythropoietin therapy.9
- The daily iron requirement is 2 mg of elemental iron in pregnancy and lactation, 1 mg at all other times
- The typical US diet contains about 18 mg of iron a day, of which only about 1 mg is absorbed
- Iron absorption occurs primarily in the second portion of the duodenum
- Iron absorption increases with iron deficiency
- One unit of blood contains 250 mg of iron
- Total body iron store is between 1,000 and 3,000 mg, depending on body size
- Each pregnancy depletes maternal iron stores by about 750 mg
- Latent iron deficiency is common in women who have had many pregnancies and in women who have menorrhagia.
Our preference for parenteral therapy is iron sucrose, classified by the Food and Drug Administration (FDA) as Pregnancy Category B. Iron sucrose is contraindicated in patients who have iron overload, hypersensitivity to inactive components of iron sucrose, or anemia that is not caused by iron deficiency. Adverse reactions to iron sucrose include, but are not limited to, anaphylaxis, hypotension, cramping, nausea, headache, vomiting, diarrhea, and chest pain. Adverse reactions are very rare, occurring in fewer than 1% of patients.
To determine whether the patient has an allergy to iron sucrose, give a test dosage of 25 mg via slow IV push and wait 20 minutes. If a reaction occurs, hold the remainder of the dose and consider alternative therapies. If no allergic reaction occurs, administer the remaining 275 mg in 50 mL to 100 mL of saline.
You may need to add erythropoietin to the regimen
Erythropoietin is a hormone made by the kidneys to promote formation of red blood cells in the bone marrow. A deficiency in this hormone causes anemia in patients who have renal disease, and nephrologists use a synthetic form of epoetin alfa (Epogen) to increase the hemoglobin level in dialysis patients.10 Epoetin alfa falls into FDA Pregnancy Category C.
In rare instances, erythropoietin-stimulating agents (ESAs), such as epoetin alfa, in addition to both IV and oral iron supplementation, are needed to increase the patient’s hemoglobin level and hematocrit before delivery or surgery. Before beginning ESA therapy, the patient’s platelet count and activity level need to be considered. ESAs have been linked to thrombolytic events and, therefore, should not be used in patients who have an elevated platelet count. The risk of thrombolytic events is a particular danger for antepartum patients on bed rest, and ESAs may be contraindicated for that reason.
Obstetric and surgical patients whose anemia has proven refractory to iron therapy may be considered for an ESA, as long as the benefits of this choice outweigh the risks. At an approximate cost of $400 for every 40,000 U, ESA therapy is by far the most expensive alternative to blood transfusion for patients who have iron-deficiency anemia. The patient typically receives one to two doses of an ESA.
Cost comparisons for alternative treatment modalities in iron-deficiency anemia can be found in TABLE 2.
TABLE 2
Estimated cost of treatment of anemia*
| Therapy | Dosage | Cost per dose |
|---|---|---|
| ORAL THERAPY | ||
| Ferrous sulfate | 325 mg | $0.05–$0.09 |
| Vitamin C | 500 mg | $0.04 |
| Vitron C | 1 tablet | $0.20 |
| Folic acid | 800 μg | $0.02 |
| INTRAVENOUS THERAPY | ||
| Iron sucrose | 100 mg | $80.00 |
| OTHER INTERVENTIONS | ||
| Transfusion | 1 U | $500.00–$600.00 |
| Erythropoietin | 40,000 U | $400.00 |
| * Local averages in central Pennsylvania | ||
TABLE 3
How safe are iron compounds in pregnancy and lactation?
| Compound | FDA pregnancy category | World Health Organization lactation recommendation | Thompson lactation rating |
|---|---|---|---|
| Parenteral iron dextran | C | Compatible with breastfeeding | Risk to infant cannot be ruled out |
| Parenteral iron sucrose | B | ||
| Oral iron | A | Unavailable | |
| Oral sodium ferric gluconate | A | Compatible with breastfeeding |
Erythropoietin-stimulating agents carry serious risks
The FDA issued the first of a series of letters to health-care professionals warning of adverse events associated with the use of ESAs in March 2007, after several randomized, controlled trials found an increased risk of stroke, blood clots, myocardial infarction, and death with high dosages. In November 2008, the FDA approved a black-box warning for the labels of Procrit and Aranesp, the two ESAs in general use in the United States. The new labels advise clinicians to modify dosages for patients who are in renal failure to maintain a target hemoglobin level between 11 and 12 g/dL, rather than the higher targets that had been in use.11,12
Transfusion is the last resort
Blood transfusion must also be considered as prophylaxis for blood loss in patients who have critically low hemoglobin levels, with due consideration of the procedure’s risks and benefits. Because the definition of “critically low” varies from patient to patient, other variables should be taken into consideration, including blood pressure; heart rate; urine output; tolerance for performing activities of daily living without dizziness, chest discomfort, or shortness of breath; and medical history. Potential drawbacks are considerable.
The multiple risks associated with transfusion include:
- immunosuppression
- fever
- chills
- urticaria
- hemolytic transfusion reaction
- septic transfusion reaction
- bacterial contamination
- anaphylaxis
- graft-versus-host reactions
- transfer of viral diseases, including hepatitis B and C and human immunodeficiency virus (HIV).
The risk of immunosuppression, in particular, should be weighed heavily for pregnant patients and those who are planning an elective surgical procedure. The possibility of viral transmission is also a deterrent. According to the Red Cross, the transmission rate is one in every 205,000 transfusions for hepatitis B, one in 2 million for hepatitis C, and one in 2,135,000 for HIV. These considerations, as well as the blood shortages that sometimes occur in practice, are sufficient reason to seek safer alternatives, when possible.
When a patient refuses transfusion
Caring for a patient who has an elevated risk of major blood loss can be particularly difficult when she is a member of a religious group such as Jehovah’s Witnesses. These patients generally decline the transfusion of plasma, packed red blood cells, white blood cells, platelets, and whole blood products.
In the Geisinger Health System, consultation with the Blood Conservation Program has been particularly helpful in these circumstances, offering clinicians alternative ways to correct anemia and prepare for the possibility of major blood loss. Patients who will not allow blood transfusion are often willing to accept plasma volume expanders that are not derived from blood, such as perfluorocarbon solutions, hydroxyethyl starch, crystalloid, or dextran.13 ESA therapy may be acceptable to some patients who refuse transfusion. Most are willing to go along with oral or IV iron supplementation to reduce their need for transfusion.
Postpartum patients may need special consideration
Iron supplementation is safe for breastfeeding mothers
Anemia in a breastfeeding woman is not uncommon and should be identified and treated. Iron supplementation with oral or IV compounds is considered safe for pregnant and breastfeeding women.
ESA therapy is a riskier strategy, whose benefits must clearly outweigh risks for all patients.
Anemia and postpartum depression
Studies have demonstrated a correlation between anemia and postpartum depression. Beard and colleagues showed a 25% improvement in cognition and improved scores on stress and depression scales in postpartum women who had iron-deficiency anemia when they were treated with daily iron and vitamin C.14 Other studies have addressed an increased risk of anemia in low-income postpartum women and the deleterious impact of iron-deficiency anemia on the quality of mother–child interactions and subsequent child development. Correcting maternal iron deficiency could prevent adverse outcomes in these mothers and their offspring.15,16
1. Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 5th ed. Philadelphia, Pa: Churchill Livingstone; 2007.
2. Creasy RK, Resnik R, Iams JD. Creasy and Resnik’s Maternal–Fetal Medicine: Principles and Practice. 6th ed. Philadelphia, Pa: Saunders; 2009.
3. Khusun H, Yip R, Schultink W, Dillon DHS. World Health Organization hemoglobin cutoff points for the detection of anemia are valid for an Indonesian population. J Nutr. 1999;129:1669-1674.
4. Breymann C. Intravenous iron in surgery and obstetrics. Transfus Altern Transfus Med. 2002;4(Suppl 2):22-23.
5. Mei Z, Cogswell ME, Parvanta I, et al. Hemoglobin and ferritin are currently the most efficient indicators of population response to iron interventions: an analysis of nine randomized controlled trials. J Nutr. 2005;135:1974-1980.
6. Gronowski AM, ed. Current Clinical Pathology: Handbook of Clinical Laboratory Testing During Pregnancy. Totowa, NJ: Humana Press; 2004:200.
7. Mani S, Duffy TP. Anemia of pregnancy. Clin Perinatol. 1995;22:593-607.
8. Bayoumeu F, Subiran-Buisset C, Baka NE, Legagneur H, Monnier-Barbarino P, Laxenaire MC. Iron therapy in iron deficiency anemia in pregnancy: intravenous route versus oral route. Am J Obstet Gynecol. 2002;186:518-522.
9. Breymann C, Richter C, Hüttner C, Huch R, Huch A. Effectiveness of recombinant erythropoietin and iron sucrose vs. iron therapy only, in patients with postpartum anaemia and blunted erythropoiesis. Eur J Clin Invest. 2000;30:154-161.
10. Bieber E. Erythropoietin, the biology of erythropoiesis and epoetin alfa. An overview. J Reprod Med. 2001;46(5 Suppl):521-530.
11. Patient Information for Procrit. Available at: www.procrit.com. Accessed December 1, 2009.
12. Patient Information for Aranesp. Available at: www.aranesp.com. Accessed December 1, 2009.
13. Baker BW. Blood conservation, obstetrics, and Jehovah’s Witnesses. Anesthesiol Clin North America. 1998;16:375-384.
14. Beard JL, Hendricks MK, Perez EM, et al. Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr. 2005;135:267-272.
15. Bodnar LM, Cogswell ME, Scanlon KS. Low income postpartum women are at risk of iron deficiency. J Nutr. 2002;132:2298-2302.
16. Perez EM, Hendricks MK, Beard JL, et al. Mother–infant interactions and infant development are altered by maternal iron deficiency anemia. J Nutr. 2005;135:850-855.
The authors report no financial relationships relevant to this article.
Obstetric hemorrhage is responsible for approximately 17% to 25% of all pregnancy-related deaths.1 Excessive blood loss also is a risk during gynecologic surgery. Iron-deficiency anemia increases the risk of complication and the need for transfusion in both settings. By identifying and treating anemia before childbirth and elective surgery, you can optimize the patient’s condition and usually avert the need for emergency transfusion.
The Geisinger Health System has developed a unique Blood Conservation Program that focuses on the prevention of major blood loss by identifying and treating anemia in antepartum, postpartum, and gynecologic patients. The program’s protocols for treating anemia in antepartum and surgical patients are illustrated in FIGURES 1 AND 2. Geisinger practitioners have found that adherence to these protocols reduces the need for transfusion in many patients and improves their quality of life.
Here, we 1) look at the key data that will help you identify and then treat anemia in gynecologic, obstetric, and postpartum patients and 2) describe a variety of treatment options.
FIGURE 1 The gynecologic surgical patient: Preop diagnosis and treatment of anemia
* If anemia is refractory to iron therapy, consider erythropoietin therapy if benefits outweigh risks.
FIGURE 2 For the antepartum patient: Diagnosis and treatment of anemia
* If anemia is refractory to iron therapy, consider erythropoietin therapy if benefits outweigh risks.
Focus on the baseline hemoglobin level
The key to prevention of emergency transfusion—as well as postpartum anemia—is optimization of the patient’s hemoglobin level before delivery. It also is prudent when elective surgery is planned. In our institution, clinicians whose patients are at risk for hemorrhage or significant blood loss have the option of consulting with the Blood Conservation Program.
When the program began in November 2004, its primary purpose was to reduce the need for blood transfusion in elective surgery, including gynecologic procedures. It later expanded to include obstetric patients who have a hemoglobin level below 11 g/dL and patients who are considered to be at risk of major blood loss.
In addition to obstetric and surgical patients, the Geisinger Blood Conservation Program provides support for patients who will not accept blood or blood products for religious or personal reasons, even in life-threatening situations. The program has provided more than 8,000 consultations to date.
When to evaluate patients for anemia
Anemia in women is most often defined as a hemoglobin level below 12 g/dL or a hematocrit below 36%. In pregnant patients, the cutoff points are lower: 11 g/dL and 33%, respectively. During pregnancy, hemoglobin and hematocrit levels reach their nadir during the second trimester and then begin to rise until term.
Symptoms of anemia include fatigue, depression, shortness of breath, hypotension, and heart palpitations. However, some patients at risk of major blood loss during delivery or surgery do not display typical symptoms associated with anemia, and the condition can be confirmed only by laboratory testing.
At Geisinger, we recommend consultation with the Blood Conservation Program for any patient who exhibits symptoms of anemia or who is at risk of major blood loss. For example, the risk of blood loss during childbirth varies with the method of delivery.1 On average, obstetric patients lose 500 mL of blood during vaginal delivery; 1,000 mL during cesarean delivery; and 1,500 mL when cesarean delivery is followed by hysterectomy.1,2 Hemorrhage is classified as follows:
- Class 1 – Blood loss as high as 750 mL, or 15% of blood volume
- Class 2 – 750 to 1,500 mL, or 15% to 30% of blood volume
- Class 3 – 1,500 to 2,400 mL, or 30% to 40% of blood volume
- Class 4 – more than 2,400 mL, or more than 40% of blood volume.1
Abnormal placentation, such as placenta accreta, percreta, increta, and previa, which can often be diagnosed antepartum, may lead to significant blood loss during and after delivery. Obstetric emergencies, including abruption, trauma, and uterine rupture, may also be associated with major blood loss.
Iron deficiency lies at the root of most cases of anemia
Iron deficiency affects an estimated 2.15 billion people globally, with a prevalence of 12% to 43% worldwide.3,4 The daily iron requirement is 1 mg of elemental iron for nonobstetric patients, 2 mg for pregnant and lactating women. Latent iron deficiency is common in women who have had multiple pregnancies. These and other important facts about iron are described in the Box “Essential facts about iron”.
In iron-deficiency anemia, the following serum levels are reduced:
- Iron. A normal reading is 60 to 170 μg/dL.
- Hemoglobin, a measure of the production and turnover of red blood cells. A normal level is ≥12 g/dL (≥11 g/dL in pregnancy).
- Serum ferritin (a protein that stores iron). A normal reading is 12 to 150 ng/mL.
- Transferrin saturation. Transferrin is a transporting protein that shuttles iron to the bone marrow. The normal transferrin saturation level ranges from 20% to 50%.
Ferritin and hemoglobin levels tend to be the most efficient indicators of iron status.5
Some clinicians may also use:
- Mean corpuscular volume (MCV). Normal is 80 to 96 fL.
- Random distribution of red blood cell weight (RDW). A normal value is 11.5% to 15.5%.
- Reticulocyte count. Normal is 0.4% to 2.3%.
Laboratory tests for iron deficiency
When the Blood Conservation Program is initially consulted, the laboratory studies we recommend are based on the clinical presentation and condition of the patient. During pregnancy, we try to take account of the normal hemodynamic changes that occur during gestation. Therefore, we recommend:
- assessment of the serum ferritin level
- complete blood count (CBC) with differential. (If the hemoglobin/hematocrit is low, a peripheral smear is recommended to further evaluate microcytic anemia.)
Transferrin saturation and serum iron levels have not been shown to be useful markers in pregnant women because they are not specific for iron-restricted erythropoiesis and can be abnormally low during pregnancy.6
In nonpregnant patients, we recommend initial evaluation of:
- serum iron level
- total iron-binding capacity (TIBC). Normal levels are 240 to 450 μg/dL
- transferrin saturation.
A caveat about the ferritin level
Ferritin is both an iron-storage indicator and an acute-phase protein, so the clinician must be careful to exclude inflammatory processes that can elevate the ferritin level, giving a false indicator of iron stability in the maternal system. These inflammatory processes can include preeclampsia and neoplastic or infectious conditions.7 Transferrin saturation, however, is not affected by inflammatory processes and can be used as a confirmatory test for iron deficiency.4
Try oral iron supplementation first
When laboratory testing confirms the presence of iron-deficiency anemia, initial management is oral iron supplementation for 2 weeks, followed by repeat laboratory evaluation.
For patients scheduled for surgery, oral therapy includes a daily dosage of:
- 325 mg of ferrous sulfate
- 250 mg of vitamin C
- 800 μg of folic acid
- a multivitamin.
For perinatal patients, the daily oral regimen is:
- 325 mg of ferrous sulfate
- 250 mg of vitamin C
- a prenatal vitamin.
These medications are the least expensive alternatives for treating anemia.
Advise patients who are taking iron supplements not to ingest the medication with dairy products, coffee, tea, or foods that have a high content of phytic acid (e.g., grains, seeds, and legumes). Foods and prescription drugs that interact with iron supplements are listed in TABLE 1, along with recommendations on optimal timing of iron supplementation and other medications.
When you prescribe oral iron supplementation, bear in mind that some patients experience gastrointestinal side effects—constipation, nausea, diarrhea—so unpleasant that they stop taking their medication. In that scenario, you will need to find alternative formulations or delivery routes. One alternative you can suggest is a daily helping of blackstrap molasses, which supplies 27 mg of elemental iron per tablespoon.
Oral therapy should be continued even after hemoglobin and ferritin levels normalize. If laboratory values remain low after 2 weeks of oral therapy, parenteral therapy can be added to the oral regimen.
Therapy may be discontinued 2 months after delivery of the infant or surgery as long as the cause of the blood loss has been remedied. If the mother is breastfeeding, she should continue taking a prenatal vitamin until nursing has stopped.
TABLE 1
Some foods and drugs don’t mix well with iron
| Food or drug | Interaction | Recommendations |
|---|---|---|
| Foods high in phytic acid (grains, seeds, legumes) | Decreased absorption of iron | Do not take iron within 2 hours of eating foods high in phytic acid |
| Dairy products | Decreased bioavailability of iron | Do not take iron supplements within 1 hour of consuming dairy products, which can significantly decrease iron absorption |
| Levothyroxine | Iron reduces levothyroxine serum levels and efficacy | Take levothyroxine and iron at least 4 hours apart |
| Methyldopa | Oral iron reduces the efficacy of methyldopa | Consider IV iron or take oral iron and methyldopa as far apart as possible |
| Proton pump inhibitors (PPIs) | Absorption of oral iron is enhanced by gastric acid. PPIs decrease gastric acid production, thereby reducing the bioavailability of iron | Consider IV iron preparations |
| Ofloxacin | Iron reduces efficacy of ofloxacin | Administer ofloxacin and iron 2 hours apart |
| Cholestyramine | Decreased efficacy of iron | Administer iron and cholestyramine at least 4 hours apart |
| Calcium, aluminum, magnesium | Decreased absorption of iron | Iron should be taken at least 1 hour before or 2 hours after products that contain calcium, aluminum, or magnesium |
| Note: This table is not a comprehensive summary of all medications used in practice, but a list of those used commonly in obstetric and gynecologic populations | ||
IV iron isn’t as risky as you think
Historically, clinicians have avoided using parenteral iron sucrose (Venofer) because they have been taught that it can cause an anaphylactic reaction. In fact, although anaphylaxis may have been associated with older intravenous (IV) iron preparations, clinical trials have demonstrated the safety of IV iron sucrose and low-molecular-weight iron dextran. In a study involving 800 patients, Breymann and colleagues demonstrated that parenteral iron preparations containing dextran or iron dextrin could be safely given to pregnant women.4 Only 1.5% of the patients in the study experienced side effects from the therapy, and no anaphylactic reactions were observed.
In another study, 25 pregnant patients were given IV iron sucrose, and the only adverse reaction reported was a “not-unpleasant taste” during the injection.8
In an additional study, Breymann and colleagues found no adverse outcomes in 20 postpartum patients who received IV iron sucrose in addition to erythropoietin therapy.9
- The daily iron requirement is 2 mg of elemental iron in pregnancy and lactation, 1 mg at all other times
- The typical US diet contains about 18 mg of iron a day, of which only about 1 mg is absorbed
- Iron absorption occurs primarily in the second portion of the duodenum
- Iron absorption increases with iron deficiency
- One unit of blood contains 250 mg of iron
- Total body iron store is between 1,000 and 3,000 mg, depending on body size
- Each pregnancy depletes maternal iron stores by about 750 mg
- Latent iron deficiency is common in women who have had many pregnancies and in women who have menorrhagia.
Our preference for parenteral therapy is iron sucrose, classified by the Food and Drug Administration (FDA) as Pregnancy Category B. Iron sucrose is contraindicated in patients who have iron overload, hypersensitivity to inactive components of iron sucrose, or anemia that is not caused by iron deficiency. Adverse reactions to iron sucrose include, but are not limited to, anaphylaxis, hypotension, cramping, nausea, headache, vomiting, diarrhea, and chest pain. Adverse reactions are very rare, occurring in fewer than 1% of patients.
To determine whether the patient has an allergy to iron sucrose, give a test dosage of 25 mg via slow IV push and wait 20 minutes. If a reaction occurs, hold the remainder of the dose and consider alternative therapies. If no allergic reaction occurs, administer the remaining 275 mg in 50 mL to 100 mL of saline.
You may need to add erythropoietin to the regimen
Erythropoietin is a hormone made by the kidneys to promote formation of red blood cells in the bone marrow. A deficiency in this hormone causes anemia in patients who have renal disease, and nephrologists use a synthetic form of epoetin alfa (Epogen) to increase the hemoglobin level in dialysis patients.10 Epoetin alfa falls into FDA Pregnancy Category C.
In rare instances, erythropoietin-stimulating agents (ESAs), such as epoetin alfa, in addition to both IV and oral iron supplementation, are needed to increase the patient’s hemoglobin level and hematocrit before delivery or surgery. Before beginning ESA therapy, the patient’s platelet count and activity level need to be considered. ESAs have been linked to thrombolytic events and, therefore, should not be used in patients who have an elevated platelet count. The risk of thrombolytic events is a particular danger for antepartum patients on bed rest, and ESAs may be contraindicated for that reason.
Obstetric and surgical patients whose anemia has proven refractory to iron therapy may be considered for an ESA, as long as the benefits of this choice outweigh the risks. At an approximate cost of $400 for every 40,000 U, ESA therapy is by far the most expensive alternative to blood transfusion for patients who have iron-deficiency anemia. The patient typically receives one to two doses of an ESA.
Cost comparisons for alternative treatment modalities in iron-deficiency anemia can be found in TABLE 2.
TABLE 2
Estimated cost of treatment of anemia*
| Therapy | Dosage | Cost per dose |
|---|---|---|
| ORAL THERAPY | ||
| Ferrous sulfate | 325 mg | $0.05–$0.09 |
| Vitamin C | 500 mg | $0.04 |
| Vitron C | 1 tablet | $0.20 |
| Folic acid | 800 μg | $0.02 |
| INTRAVENOUS THERAPY | ||
| Iron sucrose | 100 mg | $80.00 |
| OTHER INTERVENTIONS | ||
| Transfusion | 1 U | $500.00–$600.00 |
| Erythropoietin | 40,000 U | $400.00 |
| * Local averages in central Pennsylvania | ||
TABLE 3
How safe are iron compounds in pregnancy and lactation?
| Compound | FDA pregnancy category | World Health Organization lactation recommendation | Thompson lactation rating |
|---|---|---|---|
| Parenteral iron dextran | C | Compatible with breastfeeding | Risk to infant cannot be ruled out |
| Parenteral iron sucrose | B | ||
| Oral iron | A | Unavailable | |
| Oral sodium ferric gluconate | A | Compatible with breastfeeding |
Erythropoietin-stimulating agents carry serious risks
The FDA issued the first of a series of letters to health-care professionals warning of adverse events associated with the use of ESAs in March 2007, after several randomized, controlled trials found an increased risk of stroke, blood clots, myocardial infarction, and death with high dosages. In November 2008, the FDA approved a black-box warning for the labels of Procrit and Aranesp, the two ESAs in general use in the United States. The new labels advise clinicians to modify dosages for patients who are in renal failure to maintain a target hemoglobin level between 11 and 12 g/dL, rather than the higher targets that had been in use.11,12
Transfusion is the last resort
Blood transfusion must also be considered as prophylaxis for blood loss in patients who have critically low hemoglobin levels, with due consideration of the procedure’s risks and benefits. Because the definition of “critically low” varies from patient to patient, other variables should be taken into consideration, including blood pressure; heart rate; urine output; tolerance for performing activities of daily living without dizziness, chest discomfort, or shortness of breath; and medical history. Potential drawbacks are considerable.
The multiple risks associated with transfusion include:
- immunosuppression
- fever
- chills
- urticaria
- hemolytic transfusion reaction
- septic transfusion reaction
- bacterial contamination
- anaphylaxis
- graft-versus-host reactions
- transfer of viral diseases, including hepatitis B and C and human immunodeficiency virus (HIV).
The risk of immunosuppression, in particular, should be weighed heavily for pregnant patients and those who are planning an elective surgical procedure. The possibility of viral transmission is also a deterrent. According to the Red Cross, the transmission rate is one in every 205,000 transfusions for hepatitis B, one in 2 million for hepatitis C, and one in 2,135,000 for HIV. These considerations, as well as the blood shortages that sometimes occur in practice, are sufficient reason to seek safer alternatives, when possible.
When a patient refuses transfusion
Caring for a patient who has an elevated risk of major blood loss can be particularly difficult when she is a member of a religious group such as Jehovah’s Witnesses. These patients generally decline the transfusion of plasma, packed red blood cells, white blood cells, platelets, and whole blood products.
In the Geisinger Health System, consultation with the Blood Conservation Program has been particularly helpful in these circumstances, offering clinicians alternative ways to correct anemia and prepare for the possibility of major blood loss. Patients who will not allow blood transfusion are often willing to accept plasma volume expanders that are not derived from blood, such as perfluorocarbon solutions, hydroxyethyl starch, crystalloid, or dextran.13 ESA therapy may be acceptable to some patients who refuse transfusion. Most are willing to go along with oral or IV iron supplementation to reduce their need for transfusion.
Postpartum patients may need special consideration
Iron supplementation is safe for breastfeeding mothers
Anemia in a breastfeeding woman is not uncommon and should be identified and treated. Iron supplementation with oral or IV compounds is considered safe for pregnant and breastfeeding women.
ESA therapy is a riskier strategy, whose benefits must clearly outweigh risks for all patients.
Anemia and postpartum depression
Studies have demonstrated a correlation between anemia and postpartum depression. Beard and colleagues showed a 25% improvement in cognition and improved scores on stress and depression scales in postpartum women who had iron-deficiency anemia when they were treated with daily iron and vitamin C.14 Other studies have addressed an increased risk of anemia in low-income postpartum women and the deleterious impact of iron-deficiency anemia on the quality of mother–child interactions and subsequent child development. Correcting maternal iron deficiency could prevent adverse outcomes in these mothers and their offspring.15,16
The authors report no financial relationships relevant to this article.
Obstetric hemorrhage is responsible for approximately 17% to 25% of all pregnancy-related deaths.1 Excessive blood loss also is a risk during gynecologic surgery. Iron-deficiency anemia increases the risk of complication and the need for transfusion in both settings. By identifying and treating anemia before childbirth and elective surgery, you can optimize the patient’s condition and usually avert the need for emergency transfusion.
The Geisinger Health System has developed a unique Blood Conservation Program that focuses on the prevention of major blood loss by identifying and treating anemia in antepartum, postpartum, and gynecologic patients. The program’s protocols for treating anemia in antepartum and surgical patients are illustrated in FIGURES 1 AND 2. Geisinger practitioners have found that adherence to these protocols reduces the need for transfusion in many patients and improves their quality of life.
Here, we 1) look at the key data that will help you identify and then treat anemia in gynecologic, obstetric, and postpartum patients and 2) describe a variety of treatment options.
FIGURE 1 The gynecologic surgical patient: Preop diagnosis and treatment of anemia
* If anemia is refractory to iron therapy, consider erythropoietin therapy if benefits outweigh risks.
FIGURE 2 For the antepartum patient: Diagnosis and treatment of anemia
* If anemia is refractory to iron therapy, consider erythropoietin therapy if benefits outweigh risks.
Focus on the baseline hemoglobin level
The key to prevention of emergency transfusion—as well as postpartum anemia—is optimization of the patient’s hemoglobin level before delivery. It also is prudent when elective surgery is planned. In our institution, clinicians whose patients are at risk for hemorrhage or significant blood loss have the option of consulting with the Blood Conservation Program.
When the program began in November 2004, its primary purpose was to reduce the need for blood transfusion in elective surgery, including gynecologic procedures. It later expanded to include obstetric patients who have a hemoglobin level below 11 g/dL and patients who are considered to be at risk of major blood loss.
In addition to obstetric and surgical patients, the Geisinger Blood Conservation Program provides support for patients who will not accept blood or blood products for religious or personal reasons, even in life-threatening situations. The program has provided more than 8,000 consultations to date.
When to evaluate patients for anemia
Anemia in women is most often defined as a hemoglobin level below 12 g/dL or a hematocrit below 36%. In pregnant patients, the cutoff points are lower: 11 g/dL and 33%, respectively. During pregnancy, hemoglobin and hematocrit levels reach their nadir during the second trimester and then begin to rise until term.
Symptoms of anemia include fatigue, depression, shortness of breath, hypotension, and heart palpitations. However, some patients at risk of major blood loss during delivery or surgery do not display typical symptoms associated with anemia, and the condition can be confirmed only by laboratory testing.
At Geisinger, we recommend consultation with the Blood Conservation Program for any patient who exhibits symptoms of anemia or who is at risk of major blood loss. For example, the risk of blood loss during childbirth varies with the method of delivery.1 On average, obstetric patients lose 500 mL of blood during vaginal delivery; 1,000 mL during cesarean delivery; and 1,500 mL when cesarean delivery is followed by hysterectomy.1,2 Hemorrhage is classified as follows:
- Class 1 – Blood loss as high as 750 mL, or 15% of blood volume
- Class 2 – 750 to 1,500 mL, or 15% to 30% of blood volume
- Class 3 – 1,500 to 2,400 mL, or 30% to 40% of blood volume
- Class 4 – more than 2,400 mL, or more than 40% of blood volume.1
Abnormal placentation, such as placenta accreta, percreta, increta, and previa, which can often be diagnosed antepartum, may lead to significant blood loss during and after delivery. Obstetric emergencies, including abruption, trauma, and uterine rupture, may also be associated with major blood loss.
Iron deficiency lies at the root of most cases of anemia
Iron deficiency affects an estimated 2.15 billion people globally, with a prevalence of 12% to 43% worldwide.3,4 The daily iron requirement is 1 mg of elemental iron for nonobstetric patients, 2 mg for pregnant and lactating women. Latent iron deficiency is common in women who have had multiple pregnancies. These and other important facts about iron are described in the Box “Essential facts about iron”.
In iron-deficiency anemia, the following serum levels are reduced:
- Iron. A normal reading is 60 to 170 μg/dL.
- Hemoglobin, a measure of the production and turnover of red blood cells. A normal level is ≥12 g/dL (≥11 g/dL in pregnancy).
- Serum ferritin (a protein that stores iron). A normal reading is 12 to 150 ng/mL.
- Transferrin saturation. Transferrin is a transporting protein that shuttles iron to the bone marrow. The normal transferrin saturation level ranges from 20% to 50%.
Ferritin and hemoglobin levels tend to be the most efficient indicators of iron status.5
Some clinicians may also use:
- Mean corpuscular volume (MCV). Normal is 80 to 96 fL.
- Random distribution of red blood cell weight (RDW). A normal value is 11.5% to 15.5%.
- Reticulocyte count. Normal is 0.4% to 2.3%.
Laboratory tests for iron deficiency
When the Blood Conservation Program is initially consulted, the laboratory studies we recommend are based on the clinical presentation and condition of the patient. During pregnancy, we try to take account of the normal hemodynamic changes that occur during gestation. Therefore, we recommend:
- assessment of the serum ferritin level
- complete blood count (CBC) with differential. (If the hemoglobin/hematocrit is low, a peripheral smear is recommended to further evaluate microcytic anemia.)
Transferrin saturation and serum iron levels have not been shown to be useful markers in pregnant women because they are not specific for iron-restricted erythropoiesis and can be abnormally low during pregnancy.6
In nonpregnant patients, we recommend initial evaluation of:
- serum iron level
- total iron-binding capacity (TIBC). Normal levels are 240 to 450 μg/dL
- transferrin saturation.
A caveat about the ferritin level
Ferritin is both an iron-storage indicator and an acute-phase protein, so the clinician must be careful to exclude inflammatory processes that can elevate the ferritin level, giving a false indicator of iron stability in the maternal system. These inflammatory processes can include preeclampsia and neoplastic or infectious conditions.7 Transferrin saturation, however, is not affected by inflammatory processes and can be used as a confirmatory test for iron deficiency.4
Try oral iron supplementation first
When laboratory testing confirms the presence of iron-deficiency anemia, initial management is oral iron supplementation for 2 weeks, followed by repeat laboratory evaluation.
For patients scheduled for surgery, oral therapy includes a daily dosage of:
- 325 mg of ferrous sulfate
- 250 mg of vitamin C
- 800 μg of folic acid
- a multivitamin.
For perinatal patients, the daily oral regimen is:
- 325 mg of ferrous sulfate
- 250 mg of vitamin C
- a prenatal vitamin.
These medications are the least expensive alternatives for treating anemia.
Advise patients who are taking iron supplements not to ingest the medication with dairy products, coffee, tea, or foods that have a high content of phytic acid (e.g., grains, seeds, and legumes). Foods and prescription drugs that interact with iron supplements are listed in TABLE 1, along with recommendations on optimal timing of iron supplementation and other medications.
When you prescribe oral iron supplementation, bear in mind that some patients experience gastrointestinal side effects—constipation, nausea, diarrhea—so unpleasant that they stop taking their medication. In that scenario, you will need to find alternative formulations or delivery routes. One alternative you can suggest is a daily helping of blackstrap molasses, which supplies 27 mg of elemental iron per tablespoon.
Oral therapy should be continued even after hemoglobin and ferritin levels normalize. If laboratory values remain low after 2 weeks of oral therapy, parenteral therapy can be added to the oral regimen.
Therapy may be discontinued 2 months after delivery of the infant or surgery as long as the cause of the blood loss has been remedied. If the mother is breastfeeding, she should continue taking a prenatal vitamin until nursing has stopped.
TABLE 1
Some foods and drugs don’t mix well with iron
| Food or drug | Interaction | Recommendations |
|---|---|---|
| Foods high in phytic acid (grains, seeds, legumes) | Decreased absorption of iron | Do not take iron within 2 hours of eating foods high in phytic acid |
| Dairy products | Decreased bioavailability of iron | Do not take iron supplements within 1 hour of consuming dairy products, which can significantly decrease iron absorption |
| Levothyroxine | Iron reduces levothyroxine serum levels and efficacy | Take levothyroxine and iron at least 4 hours apart |
| Methyldopa | Oral iron reduces the efficacy of methyldopa | Consider IV iron or take oral iron and methyldopa as far apart as possible |
| Proton pump inhibitors (PPIs) | Absorption of oral iron is enhanced by gastric acid. PPIs decrease gastric acid production, thereby reducing the bioavailability of iron | Consider IV iron preparations |
| Ofloxacin | Iron reduces efficacy of ofloxacin | Administer ofloxacin and iron 2 hours apart |
| Cholestyramine | Decreased efficacy of iron | Administer iron and cholestyramine at least 4 hours apart |
| Calcium, aluminum, magnesium | Decreased absorption of iron | Iron should be taken at least 1 hour before or 2 hours after products that contain calcium, aluminum, or magnesium |
| Note: This table is not a comprehensive summary of all medications used in practice, but a list of those used commonly in obstetric and gynecologic populations | ||
IV iron isn’t as risky as you think
Historically, clinicians have avoided using parenteral iron sucrose (Venofer) because they have been taught that it can cause an anaphylactic reaction. In fact, although anaphylaxis may have been associated with older intravenous (IV) iron preparations, clinical trials have demonstrated the safety of IV iron sucrose and low-molecular-weight iron dextran. In a study involving 800 patients, Breymann and colleagues demonstrated that parenteral iron preparations containing dextran or iron dextrin could be safely given to pregnant women.4 Only 1.5% of the patients in the study experienced side effects from the therapy, and no anaphylactic reactions were observed.
In another study, 25 pregnant patients were given IV iron sucrose, and the only adverse reaction reported was a “not-unpleasant taste” during the injection.8
In an additional study, Breymann and colleagues found no adverse outcomes in 20 postpartum patients who received IV iron sucrose in addition to erythropoietin therapy.9
- The daily iron requirement is 2 mg of elemental iron in pregnancy and lactation, 1 mg at all other times
- The typical US diet contains about 18 mg of iron a day, of which only about 1 mg is absorbed
- Iron absorption occurs primarily in the second portion of the duodenum
- Iron absorption increases with iron deficiency
- One unit of blood contains 250 mg of iron
- Total body iron store is between 1,000 and 3,000 mg, depending on body size
- Each pregnancy depletes maternal iron stores by about 750 mg
- Latent iron deficiency is common in women who have had many pregnancies and in women who have menorrhagia.
Our preference for parenteral therapy is iron sucrose, classified by the Food and Drug Administration (FDA) as Pregnancy Category B. Iron sucrose is contraindicated in patients who have iron overload, hypersensitivity to inactive components of iron sucrose, or anemia that is not caused by iron deficiency. Adverse reactions to iron sucrose include, but are not limited to, anaphylaxis, hypotension, cramping, nausea, headache, vomiting, diarrhea, and chest pain. Adverse reactions are very rare, occurring in fewer than 1% of patients.
To determine whether the patient has an allergy to iron sucrose, give a test dosage of 25 mg via slow IV push and wait 20 minutes. If a reaction occurs, hold the remainder of the dose and consider alternative therapies. If no allergic reaction occurs, administer the remaining 275 mg in 50 mL to 100 mL of saline.
You may need to add erythropoietin to the regimen
Erythropoietin is a hormone made by the kidneys to promote formation of red blood cells in the bone marrow. A deficiency in this hormone causes anemia in patients who have renal disease, and nephrologists use a synthetic form of epoetin alfa (Epogen) to increase the hemoglobin level in dialysis patients.10 Epoetin alfa falls into FDA Pregnancy Category C.
In rare instances, erythropoietin-stimulating agents (ESAs), such as epoetin alfa, in addition to both IV and oral iron supplementation, are needed to increase the patient’s hemoglobin level and hematocrit before delivery or surgery. Before beginning ESA therapy, the patient’s platelet count and activity level need to be considered. ESAs have been linked to thrombolytic events and, therefore, should not be used in patients who have an elevated platelet count. The risk of thrombolytic events is a particular danger for antepartum patients on bed rest, and ESAs may be contraindicated for that reason.
Obstetric and surgical patients whose anemia has proven refractory to iron therapy may be considered for an ESA, as long as the benefits of this choice outweigh the risks. At an approximate cost of $400 for every 40,000 U, ESA therapy is by far the most expensive alternative to blood transfusion for patients who have iron-deficiency anemia. The patient typically receives one to two doses of an ESA.
Cost comparisons for alternative treatment modalities in iron-deficiency anemia can be found in TABLE 2.
TABLE 2
Estimated cost of treatment of anemia*
| Therapy | Dosage | Cost per dose |
|---|---|---|
| ORAL THERAPY | ||
| Ferrous sulfate | 325 mg | $0.05–$0.09 |
| Vitamin C | 500 mg | $0.04 |
| Vitron C | 1 tablet | $0.20 |
| Folic acid | 800 μg | $0.02 |
| INTRAVENOUS THERAPY | ||
| Iron sucrose | 100 mg | $80.00 |
| OTHER INTERVENTIONS | ||
| Transfusion | 1 U | $500.00–$600.00 |
| Erythropoietin | 40,000 U | $400.00 |
| * Local averages in central Pennsylvania | ||
TABLE 3
How safe are iron compounds in pregnancy and lactation?
| Compound | FDA pregnancy category | World Health Organization lactation recommendation | Thompson lactation rating |
|---|---|---|---|
| Parenteral iron dextran | C | Compatible with breastfeeding | Risk to infant cannot be ruled out |
| Parenteral iron sucrose | B | ||
| Oral iron | A | Unavailable | |
| Oral sodium ferric gluconate | A | Compatible with breastfeeding |
Erythropoietin-stimulating agents carry serious risks
The FDA issued the first of a series of letters to health-care professionals warning of adverse events associated with the use of ESAs in March 2007, after several randomized, controlled trials found an increased risk of stroke, blood clots, myocardial infarction, and death with high dosages. In November 2008, the FDA approved a black-box warning for the labels of Procrit and Aranesp, the two ESAs in general use in the United States. The new labels advise clinicians to modify dosages for patients who are in renal failure to maintain a target hemoglobin level between 11 and 12 g/dL, rather than the higher targets that had been in use.11,12
Transfusion is the last resort
Blood transfusion must also be considered as prophylaxis for blood loss in patients who have critically low hemoglobin levels, with due consideration of the procedure’s risks and benefits. Because the definition of “critically low” varies from patient to patient, other variables should be taken into consideration, including blood pressure; heart rate; urine output; tolerance for performing activities of daily living without dizziness, chest discomfort, or shortness of breath; and medical history. Potential drawbacks are considerable.
The multiple risks associated with transfusion include:
- immunosuppression
- fever
- chills
- urticaria
- hemolytic transfusion reaction
- septic transfusion reaction
- bacterial contamination
- anaphylaxis
- graft-versus-host reactions
- transfer of viral diseases, including hepatitis B and C and human immunodeficiency virus (HIV).
The risk of immunosuppression, in particular, should be weighed heavily for pregnant patients and those who are planning an elective surgical procedure. The possibility of viral transmission is also a deterrent. According to the Red Cross, the transmission rate is one in every 205,000 transfusions for hepatitis B, one in 2 million for hepatitis C, and one in 2,135,000 for HIV. These considerations, as well as the blood shortages that sometimes occur in practice, are sufficient reason to seek safer alternatives, when possible.
When a patient refuses transfusion
Caring for a patient who has an elevated risk of major blood loss can be particularly difficult when she is a member of a religious group such as Jehovah’s Witnesses. These patients generally decline the transfusion of plasma, packed red blood cells, white blood cells, platelets, and whole blood products.
In the Geisinger Health System, consultation with the Blood Conservation Program has been particularly helpful in these circumstances, offering clinicians alternative ways to correct anemia and prepare for the possibility of major blood loss. Patients who will not allow blood transfusion are often willing to accept plasma volume expanders that are not derived from blood, such as perfluorocarbon solutions, hydroxyethyl starch, crystalloid, or dextran.13 ESA therapy may be acceptable to some patients who refuse transfusion. Most are willing to go along with oral or IV iron supplementation to reduce their need for transfusion.
Postpartum patients may need special consideration
Iron supplementation is safe for breastfeeding mothers
Anemia in a breastfeeding woman is not uncommon and should be identified and treated. Iron supplementation with oral or IV compounds is considered safe for pregnant and breastfeeding women.
ESA therapy is a riskier strategy, whose benefits must clearly outweigh risks for all patients.
Anemia and postpartum depression
Studies have demonstrated a correlation between anemia and postpartum depression. Beard and colleagues showed a 25% improvement in cognition and improved scores on stress and depression scales in postpartum women who had iron-deficiency anemia when they were treated with daily iron and vitamin C.14 Other studies have addressed an increased risk of anemia in low-income postpartum women and the deleterious impact of iron-deficiency anemia on the quality of mother–child interactions and subsequent child development. Correcting maternal iron deficiency could prevent adverse outcomes in these mothers and their offspring.15,16
1. Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 5th ed. Philadelphia, Pa: Churchill Livingstone; 2007.
2. Creasy RK, Resnik R, Iams JD. Creasy and Resnik’s Maternal–Fetal Medicine: Principles and Practice. 6th ed. Philadelphia, Pa: Saunders; 2009.
3. Khusun H, Yip R, Schultink W, Dillon DHS. World Health Organization hemoglobin cutoff points for the detection of anemia are valid for an Indonesian population. J Nutr. 1999;129:1669-1674.
4. Breymann C. Intravenous iron in surgery and obstetrics. Transfus Altern Transfus Med. 2002;4(Suppl 2):22-23.
5. Mei Z, Cogswell ME, Parvanta I, et al. Hemoglobin and ferritin are currently the most efficient indicators of population response to iron interventions: an analysis of nine randomized controlled trials. J Nutr. 2005;135:1974-1980.
6. Gronowski AM, ed. Current Clinical Pathology: Handbook of Clinical Laboratory Testing During Pregnancy. Totowa, NJ: Humana Press; 2004:200.
7. Mani S, Duffy TP. Anemia of pregnancy. Clin Perinatol. 1995;22:593-607.
8. Bayoumeu F, Subiran-Buisset C, Baka NE, Legagneur H, Monnier-Barbarino P, Laxenaire MC. Iron therapy in iron deficiency anemia in pregnancy: intravenous route versus oral route. Am J Obstet Gynecol. 2002;186:518-522.
9. Breymann C, Richter C, Hüttner C, Huch R, Huch A. Effectiveness of recombinant erythropoietin and iron sucrose vs. iron therapy only, in patients with postpartum anaemia and blunted erythropoiesis. Eur J Clin Invest. 2000;30:154-161.
10. Bieber E. Erythropoietin, the biology of erythropoiesis and epoetin alfa. An overview. J Reprod Med. 2001;46(5 Suppl):521-530.
11. Patient Information for Procrit. Available at: www.procrit.com. Accessed December 1, 2009.
12. Patient Information for Aranesp. Available at: www.aranesp.com. Accessed December 1, 2009.
13. Baker BW. Blood conservation, obstetrics, and Jehovah’s Witnesses. Anesthesiol Clin North America. 1998;16:375-384.
14. Beard JL, Hendricks MK, Perez EM, et al. Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr. 2005;135:267-272.
15. Bodnar LM, Cogswell ME, Scanlon KS. Low income postpartum women are at risk of iron deficiency. J Nutr. 2002;132:2298-2302.
16. Perez EM, Hendricks MK, Beard JL, et al. Mother–infant interactions and infant development are altered by maternal iron deficiency anemia. J Nutr. 2005;135:850-855.
1. Gabbe SG, Niebyl JR, Simpson JL. Obstetrics: Normal and Problem Pregnancies. 5th ed. Philadelphia, Pa: Churchill Livingstone; 2007.
2. Creasy RK, Resnik R, Iams JD. Creasy and Resnik’s Maternal–Fetal Medicine: Principles and Practice. 6th ed. Philadelphia, Pa: Saunders; 2009.
3. Khusun H, Yip R, Schultink W, Dillon DHS. World Health Organization hemoglobin cutoff points for the detection of anemia are valid for an Indonesian population. J Nutr. 1999;129:1669-1674.
4. Breymann C. Intravenous iron in surgery and obstetrics. Transfus Altern Transfus Med. 2002;4(Suppl 2):22-23.
5. Mei Z, Cogswell ME, Parvanta I, et al. Hemoglobin and ferritin are currently the most efficient indicators of population response to iron interventions: an analysis of nine randomized controlled trials. J Nutr. 2005;135:1974-1980.
6. Gronowski AM, ed. Current Clinical Pathology: Handbook of Clinical Laboratory Testing During Pregnancy. Totowa, NJ: Humana Press; 2004:200.
7. Mani S, Duffy TP. Anemia of pregnancy. Clin Perinatol. 1995;22:593-607.
8. Bayoumeu F, Subiran-Buisset C, Baka NE, Legagneur H, Monnier-Barbarino P, Laxenaire MC. Iron therapy in iron deficiency anemia in pregnancy: intravenous route versus oral route. Am J Obstet Gynecol. 2002;186:518-522.
9. Breymann C, Richter C, Hüttner C, Huch R, Huch A. Effectiveness of recombinant erythropoietin and iron sucrose vs. iron therapy only, in patients with postpartum anaemia and blunted erythropoiesis. Eur J Clin Invest. 2000;30:154-161.
10. Bieber E. Erythropoietin, the biology of erythropoiesis and epoetin alfa. An overview. J Reprod Med. 2001;46(5 Suppl):521-530.
11. Patient Information for Procrit. Available at: www.procrit.com. Accessed December 1, 2009.
12. Patient Information for Aranesp. Available at: www.aranesp.com. Accessed December 1, 2009.
13. Baker BW. Blood conservation, obstetrics, and Jehovah’s Witnesses. Anesthesiol Clin North America. 1998;16:375-384.
14. Beard JL, Hendricks MK, Perez EM, et al. Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr. 2005;135:267-272.
15. Bodnar LM, Cogswell ME, Scanlon KS. Low income postpartum women are at risk of iron deficiency. J Nutr. 2002;132:2298-2302.
16. Perez EM, Hendricks MK, Beard JL, et al. Mother–infant interactions and infant development are altered by maternal iron deficiency anemia. J Nutr. 2005;135:850-855.