User login
Osteoarthritis Treatment in the Veteran Population
Osteoarthritis (OA) is one of the most common diseases affecting the general population and is characterized by progressive, noninflammatory degenerative changes primarily involving the hips, knees, spine, hands, and feet. Among veterans the incidence and prevalence of OA is considerably higher than the incidence found in the general population. A study examining active-duty service members between 1999 and 2008 reported a 19-fold higher incidence in service members aged > 40 years compared with those aged < 20 years.1 In addition, women and African American service members seem to have a higher incidence of OA compared with other populations. Overall, the economic burden of OA is estimated to approach or exceed $60 billion annually and will continue to increase due to longer life expectancies in veterans.2,3 Much of this burden relates to a lack of disease-modifying treatment and inadequacy of analgesic therapy.
Patterns of Osteoarthritis
The strongest risk factor associated with OA is age. Osteoarthritis is the most common cause of pain and disability in the elderly population.4 A heritable component seems to be associated with primary OA as shown by family risk studies.5 Estrogenic effects seem to protect younger women, whereas postmenopausal women are at greater risk after age 50 years. Previous joint trauma and activities have a large impact on the risk of developing OA later, particularly those activities and occupations requiring high-impact joint loading, such as those often seen in veterans. Other modifiable risk factors include smoking and obesity. The risk for knee OA has been found to increase 30-fold in patients with a body mass index > 30.6
Several OA disease patterns exist. The disorder can be characterized as primary or secondary. Primary OA classically presents in the aging male or postmenopausal female involving the apophyseal joints of the lumbar and cervical spine; base of the thumb (first carpometacarpal,[CMC] joint); proximal or distal interphalangeal joints (PIPs and DIPs) of the hand, knee, or hip; or the first metatarsophalangeal joint. The disease may be localized to 1 joint (localized OA) or involve multiple joints (generalized OA). The disease is more common in men aged < 45 years and more common in women aged > 45 years. In either sex, progression with age is a prominent feature.
Rarely, patients may present with inflammatory arthritis in a distribution typical of OA that is not associated with psoriasis or another disease. This form is known as inflammatory or erosive OA. A minority of cases present with rapidly progressive hip or knee degeneration, the cause of which is unknown. Osteoarthritis involving the metacarpophalangeal joints (MCPs), wrists, elbows, shoulders, or ankles is much less common. Patients with radiographic evidence of OA at these sites should be evaluated for a cause of secondary OA.
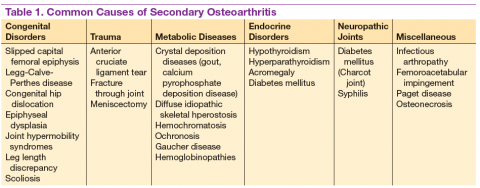
Patients often develop secondary OA in the setting of inflammatory arthritis, crystal-induced arthritis, and other systemic diseases. Causes of secondary OA should be considered when OA manifests in an atypical joint. Common causes of secondary OA are outlined in Table 1. A careful history may undercover a prior diagnosis of gout, calcium pyrophosphate deposition disease, or infectious arthritis in the affected joint. An important metabolic cause of secondary OA is hemochromatosis, which can lead to osteophytic change primarily in the second and third MCPs. Patients with diabetes mellitus-associated neuropathy may develop destructive changes in the foot (Charcot joint).
Symptoms and Examination
Osteoarthritis encompasses a wide spectrum of common conditions with similar pathophysiology. Most of these conditions share similar historic features, including pain during or after use and stiffness after prolonged periods of inactivity. Other common symptoms include swelling, joint locking or “cracking,” instability, and joint fatigue. Patients may perceive OA discomfort in different ways. Whereas one patient with knee OA may describe a sharp, gnawing pain, another may experience painless swelling and instability. Although OA is mainly considered a localized disease, patients may present with multiple areas of pain, suggesting a more generalized pattern. Patients with OA may have short periods of morning stiffness and “gelling,” but prolonged stiffness suggests the presence of inflammatory arthritis.
Examination of the osteoarthritic joint is performed with thorough palpation and range of motion testing. Evidence of joint swelling may be present near the joint line with pain on palpation. Palpable crepitus is commonly noted with restricted range of motion, usually inducing pain at the maximal range. Osteophytes or chondrophytes at the joint line may be tender and are commonly mistaken for joint swelling. In the hands, bony hypertrophy of the PIP and DIP joints may be noted (Bouchard’s and Heberden’s nodes, respectively). Pain at the base of the thumb is a common complaint in patients with OA of the CMC joint.
Most cases of OA can be diagnosed by taking a history and a physical examination without further investigation; however, plain radiographs are frequently obtained to confirm the diagnosis. Joint inflammation, when present, is usually mild. Occasionally, patients may present with evidence of warmth, effusion, and severe pain with restriction of motion. Patients with these symptoms should undergo prompt arthrocentesis to rule out infection, crystal-associated arthritis, hemarthrosis, or other inflammatory causes.
Radiographic Features
Plain radiographs are extremely helpful in denoting the extent of OA in a particular joint. Radiographic features of OA include narrowing of the joint space, osteophyte formation, and subchondral bone abnormalities. Narrowing of the joint space and alignment abnormalities occur due to loss of articular cartilage. Changes in the subchondral bone include sclerosis and cystic lesions. Erosive changes, ankylosis, and calcification of the articular cartilage are typically absent.
In the hands, a particular pattern is noted involving the PIP and DIP joints with characteristic sparing of the MCPs (Figure 1A). The first CMC joint is also commonly involved, with bony osteophyte formation and joint space loss. In the knee and hip, loss of joint space with subchondral bone cyst and osteophyte formation is common (Figure 1B).
The cervical and/or lumbar spine may reveal spondylosis, disc space narrowing, and osteophytes. More than 50% of people aged > 65 years have radiologic evidence of OA. However, radiographic evidence of OA is at least twice as common as symptomatic OA, warranting careful consideration when contemplating treatment.7
Pathogenesis
Normal articular cartilage is a complex tissue composed of extracellular matrix and chondrocytes. Under ideal conditions, hemostasis is maintained with balance between degradation and synthesis of extracellular matrix proteins. In the aging cartilage, a reduction of total proteoglycan synthesis occurs, decreasing its capacity to retain water. Matrix proteins are modified, leading to the accumulation of advanced glycation end products (AGEs). This process is irreversible, and AGEs cannot be removed from the articular cartilage. Chondrocytes respond to AGEs with increased catabolic activity and cytokine release. Initial chondral edema and matrix degradation leads to stress fractures in the collagen network and fissuring of the cartilage. Eventually, the microfractures lead to fragmenting of the cartilage, formation of loose bodies, and synovial inflammation. Sclerosis occurs in the subchondral bone, with accelerated bone turnover leading to osteophyte formation.8
Treatment
Unfortunately, no pharmacologic or nonpharmacologic therapy has been shown to reverse or halt the progression of OA. A comprehensive approach to the treatment of patients with OA is imperative for reducing disability and improving quality of life. Several sources have published guidelines for the management of OA.9-11 More recently, comprehensive clinical practice guidelines have been published regarding nonsurgical management of hip and knee OA in the veteran population.12
Initially, a conservative approach is generally recommended with reduction of modifiable risk factors and patient education. Weight loss, aerobic conditioning, and physical therapy can improve function and stability. Notably, a weight reduction of 5% has been associated with an 18% to 24% improvement in knee OA.6 A supervised walking exercise program can be extremely beneficial for patients, with several studies showing improvement in pain, ambulatory function, and psychological well-being. Bracing devices and orthotic footwear can be helpful for compartmental unloading of the knee. The use of ambulatory assist devices (eg, canes, walkers) and splinting may also be of benefit. Topical lidocaine, capsaicin, and topical nonsteroidal anti-inflammatory drugs (NSAIDs) therapy can be useful adjuncts.
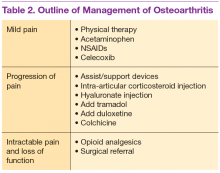
Medications are used mainly to provide analgesia and improve function while causing the fewest adverse effects (AEs) (Table 2). Contrary to conventional teaching, acetaminophen may not be as effective in the treatment of OA as previously thought. A recently published metaanalysis comparing treatments for knee OA revealed acetaminophen to be the least effective agent.13 Another meta-analysis showed that acetaminophen provided clinically insignificant pain relief in OA of the hip and knee.14 However, acetaminophen may be useful in the treatment of mild OA or in patients with contraindications to other oral therapies. Nonsteroidal anti-inflammatory drug therapy is more effective in a patient with inflammatory OA symptoms (eg, effusion, erosive OA) and can be added to acetaminophen if ineffective alone. Gastrointestinal protection against ulceration may be warranted, and use of NSAIDs may be contraindicated in the patient with high bleeding risk, renal insufficiency, or cardiovascular disease. In patients with low cardiac risk, celecoxib can be effective. Patients who have a contraindication to NSAIDs may find benefit from other analgesic agents, such as tramadol or duloxetine. Intra-articular corticosteroid injections can be particularly helpful for patients with a single osteoarthritic joint that has been unresponsive to oral or topical analgesics. Opioid analgesics may be used as a last resort when all other agents and therapies have failed. Most patients who require opioid therapy are awaiting surgical repair or are not surgical candidates.
Use of nutritional supplements such as glucosamine and chondroitin sulfate in the treatment of primary knee OA is controversial. These agents are not regulated by the FDA and their potency, purity, and safety are not guaranteed. Furthermore, the bioavailability of oral glucosamine and chondroitin sulfate is particularly poor, and studies have revealed conflicting evidence on their ability to reduce pain in patients with OA. Nonetheless, some evidence exists for cartilage proteoglycan integration and synthesis with glucosamine and chondroitin compounds. Most patients taking these supplements experience few AEs, and some report good responses to therapy. Some patients allergic to shellfish may experience a reaction to glucosamine products.
Hyaluronate injections can be recommended for patients with moderate OA who have failed standard medical treatment. Most clinical trials of hyaluronate suggest an analgesic benefit comparable with NSAID therapy and corticosteroid injections, but high-quality studies are lacking.
Colchicine may be effective in patients with inflammatory or noninflammatory OA. Two small studies showed colchicine to be beneficial in the treatment of primary OA of the knee.15,16 Hydroxychloroquine may be helpful in the treatment of inflammatory OA.
Loss of joint function or severe pain refractory to medical treatment in a patient with OA likely requires surgical intervention. Patients who have difficulty ambulating more than a reasonable distance (ie, 1 block) or cannot stand in place for more than several minutes due to severe pain should be considered for total joint replacement. Patients often report awaking with severe pain at night or pain that significantly impedes their activities of daily living. In these patients, total joint replacement can be extremely beneficial and life altering.
Conclusion
Osteoarthritis is the most common arthritic disease and has a very high prevalence in the veteran population. Aging, obesity, prior trauma, and activity level are the common risk factors for the development of OA. Patterns of disease are recognizable by history, examination, and prominent radiographic features. Causes of secondary OA are important to recognize and treat. The pathogenesis of OA involves a disrupted homeostatic process leading to cartilage degradation, microfracture, subchondral sclerosis, and osteophyte formation. Treatment is unique to the individual and should include a comprehensive strategy involving patient education, exercise or physical therapy, and analgesia. Patients with severe osteoarthritis that significantly impacts activities of daily living may benefit from surgery.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cameron KL, Hsiao MS, Owens BD, Burks R, Svoboda SJ. Incidence of physician diagnosed osteoarthritis among active duty United States military service members. Arthritis Rheum. 2011;63(10):2974-2982.
2. Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56(5):1397-1407.
3. Oliviero F, Ramonda R, Punzi L. New horizons in osteoarthritis. Swiss Med Wkly. 2010;140:w13098.
4. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115-2126.
5. Kraus VB, Jordan JM, Doherty M, et al. The Genetics of Generalized Osteoarthritis (GOGO) study: study design and evaluation of osteoarthritis phenotypes. Osteoarthritis Cartilage. 2007;15(2):120-127.
6. Lementowski PW, Zelicof SB. Obesity and osteoarthritis. Am J Orthop (Belle Mead NJ). 2008;37(3):148-151.
7. Anandacoomarasamy A, March L. Current evidence for osteoarthritis treatments. Ther Adv Musculoskelet Dis. 2010;2(1):17-28.
8. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskel Dis. 2013;5(2):77-94.
9. Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4);465-474.
10. Fernandes L, Hagen KB, Bijlsma JW, et al; European League Against Rheumatism (EULAR). EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125-1135.
11. Katz JN, Earp BE, Gomoll AH. Surgical management of osteoarthritis. Arthritis Care Res (Hoboken). 2010;62(9):1220-1228.
12. U.S. Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Non-Surgical Management of Hip & Knee Osteoarthritis, Version 1.0. U.S. Department of Veterans Affairs Website. http://www.healthquality.va.gov/guidelines/CD/OA. Published 2014. Accessed February 9, 2015.
13. Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, McAlindon TE. Comparative
effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162(1):46-54.
14. Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
15. Das SK, Mishra K, Ramakrishnan S, et al. A randomized controlled trial to evaluate the slow-acting symptom modifying effects of a regimen containing colchicine in a subset of patients with osteoarthritis of the knee. Osteoarthritis Cartilage. 2002;10(4):247-252.
16. Aran S, Malekzadeh S, Seifirad S. A double-blind randomized controlled trial appraising the symptom-modifying effects of colchicine on osteoarthritis of the knee. Clin Exp Rheumatol. 2011;29(3):513-518.
Osteoarthritis (OA) is one of the most common diseases affecting the general population and is characterized by progressive, noninflammatory degenerative changes primarily involving the hips, knees, spine, hands, and feet. Among veterans the incidence and prevalence of OA is considerably higher than the incidence found in the general population. A study examining active-duty service members between 1999 and 2008 reported a 19-fold higher incidence in service members aged > 40 years compared with those aged < 20 years.1 In addition, women and African American service members seem to have a higher incidence of OA compared with other populations. Overall, the economic burden of OA is estimated to approach or exceed $60 billion annually and will continue to increase due to longer life expectancies in veterans.2,3 Much of this burden relates to a lack of disease-modifying treatment and inadequacy of analgesic therapy.
Patterns of Osteoarthritis
The strongest risk factor associated with OA is age. Osteoarthritis is the most common cause of pain and disability in the elderly population.4 A heritable component seems to be associated with primary OA as shown by family risk studies.5 Estrogenic effects seem to protect younger women, whereas postmenopausal women are at greater risk after age 50 years. Previous joint trauma and activities have a large impact on the risk of developing OA later, particularly those activities and occupations requiring high-impact joint loading, such as those often seen in veterans. Other modifiable risk factors include smoking and obesity. The risk for knee OA has been found to increase 30-fold in patients with a body mass index > 30.6
Several OA disease patterns exist. The disorder can be characterized as primary or secondary. Primary OA classically presents in the aging male or postmenopausal female involving the apophyseal joints of the lumbar and cervical spine; base of the thumb (first carpometacarpal,[CMC] joint); proximal or distal interphalangeal joints (PIPs and DIPs) of the hand, knee, or hip; or the first metatarsophalangeal joint. The disease may be localized to 1 joint (localized OA) or involve multiple joints (generalized OA). The disease is more common in men aged < 45 years and more common in women aged > 45 years. In either sex, progression with age is a prominent feature.
Rarely, patients may present with inflammatory arthritis in a distribution typical of OA that is not associated with psoriasis or another disease. This form is known as inflammatory or erosive OA. A minority of cases present with rapidly progressive hip or knee degeneration, the cause of which is unknown. Osteoarthritis involving the metacarpophalangeal joints (MCPs), wrists, elbows, shoulders, or ankles is much less common. Patients with radiographic evidence of OA at these sites should be evaluated for a cause of secondary OA.
Patients often develop secondary OA in the setting of inflammatory arthritis, crystal-induced arthritis, and other systemic diseases. Causes of secondary OA should be considered when OA manifests in an atypical joint. Common causes of secondary OA are outlined in Table 1. A careful history may undercover a prior diagnosis of gout, calcium pyrophosphate deposition disease, or infectious arthritis in the affected joint. An important metabolic cause of secondary OA is hemochromatosis, which can lead to osteophytic change primarily in the second and third MCPs. Patients with diabetes mellitus-associated neuropathy may develop destructive changes in the foot (Charcot joint).
Symptoms and Examination
Osteoarthritis encompasses a wide spectrum of common conditions with similar pathophysiology. Most of these conditions share similar historic features, including pain during or after use and stiffness after prolonged periods of inactivity. Other common symptoms include swelling, joint locking or “cracking,” instability, and joint fatigue. Patients may perceive OA discomfort in different ways. Whereas one patient with knee OA may describe a sharp, gnawing pain, another may experience painless swelling and instability. Although OA is mainly considered a localized disease, patients may present with multiple areas of pain, suggesting a more generalized pattern. Patients with OA may have short periods of morning stiffness and “gelling,” but prolonged stiffness suggests the presence of inflammatory arthritis.
Examination of the osteoarthritic joint is performed with thorough palpation and range of motion testing. Evidence of joint swelling may be present near the joint line with pain on palpation. Palpable crepitus is commonly noted with restricted range of motion, usually inducing pain at the maximal range. Osteophytes or chondrophytes at the joint line may be tender and are commonly mistaken for joint swelling. In the hands, bony hypertrophy of the PIP and DIP joints may be noted (Bouchard’s and Heberden’s nodes, respectively). Pain at the base of the thumb is a common complaint in patients with OA of the CMC joint.
Most cases of OA can be diagnosed by taking a history and a physical examination without further investigation; however, plain radiographs are frequently obtained to confirm the diagnosis. Joint inflammation, when present, is usually mild. Occasionally, patients may present with evidence of warmth, effusion, and severe pain with restriction of motion. Patients with these symptoms should undergo prompt arthrocentesis to rule out infection, crystal-associated arthritis, hemarthrosis, or other inflammatory causes.
Radiographic Features
Plain radiographs are extremely helpful in denoting the extent of OA in a particular joint. Radiographic features of OA include narrowing of the joint space, osteophyte formation, and subchondral bone abnormalities. Narrowing of the joint space and alignment abnormalities occur due to loss of articular cartilage. Changes in the subchondral bone include sclerosis and cystic lesions. Erosive changes, ankylosis, and calcification of the articular cartilage are typically absent.
In the hands, a particular pattern is noted involving the PIP and DIP joints with characteristic sparing of the MCPs (Figure 1A). The first CMC joint is also commonly involved, with bony osteophyte formation and joint space loss. In the knee and hip, loss of joint space with subchondral bone cyst and osteophyte formation is common (Figure 1B).
The cervical and/or lumbar spine may reveal spondylosis, disc space narrowing, and osteophytes. More than 50% of people aged > 65 years have radiologic evidence of OA. However, radiographic evidence of OA is at least twice as common as symptomatic OA, warranting careful consideration when contemplating treatment.7
Pathogenesis
Normal articular cartilage is a complex tissue composed of extracellular matrix and chondrocytes. Under ideal conditions, hemostasis is maintained with balance between degradation and synthesis of extracellular matrix proteins. In the aging cartilage, a reduction of total proteoglycan synthesis occurs, decreasing its capacity to retain water. Matrix proteins are modified, leading to the accumulation of advanced glycation end products (AGEs). This process is irreversible, and AGEs cannot be removed from the articular cartilage. Chondrocytes respond to AGEs with increased catabolic activity and cytokine release. Initial chondral edema and matrix degradation leads to stress fractures in the collagen network and fissuring of the cartilage. Eventually, the microfractures lead to fragmenting of the cartilage, formation of loose bodies, and synovial inflammation. Sclerosis occurs in the subchondral bone, with accelerated bone turnover leading to osteophyte formation.8
Treatment
Unfortunately, no pharmacologic or nonpharmacologic therapy has been shown to reverse or halt the progression of OA. A comprehensive approach to the treatment of patients with OA is imperative for reducing disability and improving quality of life. Several sources have published guidelines for the management of OA.9-11 More recently, comprehensive clinical practice guidelines have been published regarding nonsurgical management of hip and knee OA in the veteran population.12
Initially, a conservative approach is generally recommended with reduction of modifiable risk factors and patient education. Weight loss, aerobic conditioning, and physical therapy can improve function and stability. Notably, a weight reduction of 5% has been associated with an 18% to 24% improvement in knee OA.6 A supervised walking exercise program can be extremely beneficial for patients, with several studies showing improvement in pain, ambulatory function, and psychological well-being. Bracing devices and orthotic footwear can be helpful for compartmental unloading of the knee. The use of ambulatory assist devices (eg, canes, walkers) and splinting may also be of benefit. Topical lidocaine, capsaicin, and topical nonsteroidal anti-inflammatory drugs (NSAIDs) therapy can be useful adjuncts.
Medications are used mainly to provide analgesia and improve function while causing the fewest adverse effects (AEs) (Table 2). Contrary to conventional teaching, acetaminophen may not be as effective in the treatment of OA as previously thought. A recently published metaanalysis comparing treatments for knee OA revealed acetaminophen to be the least effective agent.13 Another meta-analysis showed that acetaminophen provided clinically insignificant pain relief in OA of the hip and knee.14 However, acetaminophen may be useful in the treatment of mild OA or in patients with contraindications to other oral therapies. Nonsteroidal anti-inflammatory drug therapy is more effective in a patient with inflammatory OA symptoms (eg, effusion, erosive OA) and can be added to acetaminophen if ineffective alone. Gastrointestinal protection against ulceration may be warranted, and use of NSAIDs may be contraindicated in the patient with high bleeding risk, renal insufficiency, or cardiovascular disease. In patients with low cardiac risk, celecoxib can be effective. Patients who have a contraindication to NSAIDs may find benefit from other analgesic agents, such as tramadol or duloxetine. Intra-articular corticosteroid injections can be particularly helpful for patients with a single osteoarthritic joint that has been unresponsive to oral or topical analgesics. Opioid analgesics may be used as a last resort when all other agents and therapies have failed. Most patients who require opioid therapy are awaiting surgical repair or are not surgical candidates.
Use of nutritional supplements such as glucosamine and chondroitin sulfate in the treatment of primary knee OA is controversial. These agents are not regulated by the FDA and their potency, purity, and safety are not guaranteed. Furthermore, the bioavailability of oral glucosamine and chondroitin sulfate is particularly poor, and studies have revealed conflicting evidence on their ability to reduce pain in patients with OA. Nonetheless, some evidence exists for cartilage proteoglycan integration and synthesis with glucosamine and chondroitin compounds. Most patients taking these supplements experience few AEs, and some report good responses to therapy. Some patients allergic to shellfish may experience a reaction to glucosamine products.
Hyaluronate injections can be recommended for patients with moderate OA who have failed standard medical treatment. Most clinical trials of hyaluronate suggest an analgesic benefit comparable with NSAID therapy and corticosteroid injections, but high-quality studies are lacking.
Colchicine may be effective in patients with inflammatory or noninflammatory OA. Two small studies showed colchicine to be beneficial in the treatment of primary OA of the knee.15,16 Hydroxychloroquine may be helpful in the treatment of inflammatory OA.
Loss of joint function or severe pain refractory to medical treatment in a patient with OA likely requires surgical intervention. Patients who have difficulty ambulating more than a reasonable distance (ie, 1 block) or cannot stand in place for more than several minutes due to severe pain should be considered for total joint replacement. Patients often report awaking with severe pain at night or pain that significantly impedes their activities of daily living. In these patients, total joint replacement can be extremely beneficial and life altering.
Conclusion
Osteoarthritis is the most common arthritic disease and has a very high prevalence in the veteran population. Aging, obesity, prior trauma, and activity level are the common risk factors for the development of OA. Patterns of disease are recognizable by history, examination, and prominent radiographic features. Causes of secondary OA are important to recognize and treat. The pathogenesis of OA involves a disrupted homeostatic process leading to cartilage degradation, microfracture, subchondral sclerosis, and osteophyte formation. Treatment is unique to the individual and should include a comprehensive strategy involving patient education, exercise or physical therapy, and analgesia. Patients with severe osteoarthritis that significantly impacts activities of daily living may benefit from surgery.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Osteoarthritis (OA) is one of the most common diseases affecting the general population and is characterized by progressive, noninflammatory degenerative changes primarily involving the hips, knees, spine, hands, and feet. Among veterans the incidence and prevalence of OA is considerably higher than the incidence found in the general population. A study examining active-duty service members between 1999 and 2008 reported a 19-fold higher incidence in service members aged > 40 years compared with those aged < 20 years.1 In addition, women and African American service members seem to have a higher incidence of OA compared with other populations. Overall, the economic burden of OA is estimated to approach or exceed $60 billion annually and will continue to increase due to longer life expectancies in veterans.2,3 Much of this burden relates to a lack of disease-modifying treatment and inadequacy of analgesic therapy.
Patterns of Osteoarthritis
The strongest risk factor associated with OA is age. Osteoarthritis is the most common cause of pain and disability in the elderly population.4 A heritable component seems to be associated with primary OA as shown by family risk studies.5 Estrogenic effects seem to protect younger women, whereas postmenopausal women are at greater risk after age 50 years. Previous joint trauma and activities have a large impact on the risk of developing OA later, particularly those activities and occupations requiring high-impact joint loading, such as those often seen in veterans. Other modifiable risk factors include smoking and obesity. The risk for knee OA has been found to increase 30-fold in patients with a body mass index > 30.6
Several OA disease patterns exist. The disorder can be characterized as primary or secondary. Primary OA classically presents in the aging male or postmenopausal female involving the apophyseal joints of the lumbar and cervical spine; base of the thumb (first carpometacarpal,[CMC] joint); proximal or distal interphalangeal joints (PIPs and DIPs) of the hand, knee, or hip; or the first metatarsophalangeal joint. The disease may be localized to 1 joint (localized OA) or involve multiple joints (generalized OA). The disease is more common in men aged < 45 years and more common in women aged > 45 years. In either sex, progression with age is a prominent feature.
Rarely, patients may present with inflammatory arthritis in a distribution typical of OA that is not associated with psoriasis or another disease. This form is known as inflammatory or erosive OA. A minority of cases present with rapidly progressive hip or knee degeneration, the cause of which is unknown. Osteoarthritis involving the metacarpophalangeal joints (MCPs), wrists, elbows, shoulders, or ankles is much less common. Patients with radiographic evidence of OA at these sites should be evaluated for a cause of secondary OA.
Patients often develop secondary OA in the setting of inflammatory arthritis, crystal-induced arthritis, and other systemic diseases. Causes of secondary OA should be considered when OA manifests in an atypical joint. Common causes of secondary OA are outlined in Table 1. A careful history may undercover a prior diagnosis of gout, calcium pyrophosphate deposition disease, or infectious arthritis in the affected joint. An important metabolic cause of secondary OA is hemochromatosis, which can lead to osteophytic change primarily in the second and third MCPs. Patients with diabetes mellitus-associated neuropathy may develop destructive changes in the foot (Charcot joint).
Symptoms and Examination
Osteoarthritis encompasses a wide spectrum of common conditions with similar pathophysiology. Most of these conditions share similar historic features, including pain during or after use and stiffness after prolonged periods of inactivity. Other common symptoms include swelling, joint locking or “cracking,” instability, and joint fatigue. Patients may perceive OA discomfort in different ways. Whereas one patient with knee OA may describe a sharp, gnawing pain, another may experience painless swelling and instability. Although OA is mainly considered a localized disease, patients may present with multiple areas of pain, suggesting a more generalized pattern. Patients with OA may have short periods of morning stiffness and “gelling,” but prolonged stiffness suggests the presence of inflammatory arthritis.
Examination of the osteoarthritic joint is performed with thorough palpation and range of motion testing. Evidence of joint swelling may be present near the joint line with pain on palpation. Palpable crepitus is commonly noted with restricted range of motion, usually inducing pain at the maximal range. Osteophytes or chondrophytes at the joint line may be tender and are commonly mistaken for joint swelling. In the hands, bony hypertrophy of the PIP and DIP joints may be noted (Bouchard’s and Heberden’s nodes, respectively). Pain at the base of the thumb is a common complaint in patients with OA of the CMC joint.
Most cases of OA can be diagnosed by taking a history and a physical examination without further investigation; however, plain radiographs are frequently obtained to confirm the diagnosis. Joint inflammation, when present, is usually mild. Occasionally, patients may present with evidence of warmth, effusion, and severe pain with restriction of motion. Patients with these symptoms should undergo prompt arthrocentesis to rule out infection, crystal-associated arthritis, hemarthrosis, or other inflammatory causes.
Radiographic Features
Plain radiographs are extremely helpful in denoting the extent of OA in a particular joint. Radiographic features of OA include narrowing of the joint space, osteophyte formation, and subchondral bone abnormalities. Narrowing of the joint space and alignment abnormalities occur due to loss of articular cartilage. Changes in the subchondral bone include sclerosis and cystic lesions. Erosive changes, ankylosis, and calcification of the articular cartilage are typically absent.
In the hands, a particular pattern is noted involving the PIP and DIP joints with characteristic sparing of the MCPs (Figure 1A). The first CMC joint is also commonly involved, with bony osteophyte formation and joint space loss. In the knee and hip, loss of joint space with subchondral bone cyst and osteophyte formation is common (Figure 1B).
The cervical and/or lumbar spine may reveal spondylosis, disc space narrowing, and osteophytes. More than 50% of people aged > 65 years have radiologic evidence of OA. However, radiographic evidence of OA is at least twice as common as symptomatic OA, warranting careful consideration when contemplating treatment.7
Pathogenesis
Normal articular cartilage is a complex tissue composed of extracellular matrix and chondrocytes. Under ideal conditions, hemostasis is maintained with balance between degradation and synthesis of extracellular matrix proteins. In the aging cartilage, a reduction of total proteoglycan synthesis occurs, decreasing its capacity to retain water. Matrix proteins are modified, leading to the accumulation of advanced glycation end products (AGEs). This process is irreversible, and AGEs cannot be removed from the articular cartilage. Chondrocytes respond to AGEs with increased catabolic activity and cytokine release. Initial chondral edema and matrix degradation leads to stress fractures in the collagen network and fissuring of the cartilage. Eventually, the microfractures lead to fragmenting of the cartilage, formation of loose bodies, and synovial inflammation. Sclerosis occurs in the subchondral bone, with accelerated bone turnover leading to osteophyte formation.8
Treatment
Unfortunately, no pharmacologic or nonpharmacologic therapy has been shown to reverse or halt the progression of OA. A comprehensive approach to the treatment of patients with OA is imperative for reducing disability and improving quality of life. Several sources have published guidelines for the management of OA.9-11 More recently, comprehensive clinical practice guidelines have been published regarding nonsurgical management of hip and knee OA in the veteran population.12
Initially, a conservative approach is generally recommended with reduction of modifiable risk factors and patient education. Weight loss, aerobic conditioning, and physical therapy can improve function and stability. Notably, a weight reduction of 5% has been associated with an 18% to 24% improvement in knee OA.6 A supervised walking exercise program can be extremely beneficial for patients, with several studies showing improvement in pain, ambulatory function, and psychological well-being. Bracing devices and orthotic footwear can be helpful for compartmental unloading of the knee. The use of ambulatory assist devices (eg, canes, walkers) and splinting may also be of benefit. Topical lidocaine, capsaicin, and topical nonsteroidal anti-inflammatory drugs (NSAIDs) therapy can be useful adjuncts.
Medications are used mainly to provide analgesia and improve function while causing the fewest adverse effects (AEs) (Table 2). Contrary to conventional teaching, acetaminophen may not be as effective in the treatment of OA as previously thought. A recently published metaanalysis comparing treatments for knee OA revealed acetaminophen to be the least effective agent.13 Another meta-analysis showed that acetaminophen provided clinically insignificant pain relief in OA of the hip and knee.14 However, acetaminophen may be useful in the treatment of mild OA or in patients with contraindications to other oral therapies. Nonsteroidal anti-inflammatory drug therapy is more effective in a patient with inflammatory OA symptoms (eg, effusion, erosive OA) and can be added to acetaminophen if ineffective alone. Gastrointestinal protection against ulceration may be warranted, and use of NSAIDs may be contraindicated in the patient with high bleeding risk, renal insufficiency, or cardiovascular disease. In patients with low cardiac risk, celecoxib can be effective. Patients who have a contraindication to NSAIDs may find benefit from other analgesic agents, such as tramadol or duloxetine. Intra-articular corticosteroid injections can be particularly helpful for patients with a single osteoarthritic joint that has been unresponsive to oral or topical analgesics. Opioid analgesics may be used as a last resort when all other agents and therapies have failed. Most patients who require opioid therapy are awaiting surgical repair or are not surgical candidates.
Use of nutritional supplements such as glucosamine and chondroitin sulfate in the treatment of primary knee OA is controversial. These agents are not regulated by the FDA and their potency, purity, and safety are not guaranteed. Furthermore, the bioavailability of oral glucosamine and chondroitin sulfate is particularly poor, and studies have revealed conflicting evidence on their ability to reduce pain in patients with OA. Nonetheless, some evidence exists for cartilage proteoglycan integration and synthesis with glucosamine and chondroitin compounds. Most patients taking these supplements experience few AEs, and some report good responses to therapy. Some patients allergic to shellfish may experience a reaction to glucosamine products.
Hyaluronate injections can be recommended for patients with moderate OA who have failed standard medical treatment. Most clinical trials of hyaluronate suggest an analgesic benefit comparable with NSAID therapy and corticosteroid injections, but high-quality studies are lacking.
Colchicine may be effective in patients with inflammatory or noninflammatory OA. Two small studies showed colchicine to be beneficial in the treatment of primary OA of the knee.15,16 Hydroxychloroquine may be helpful in the treatment of inflammatory OA.
Loss of joint function or severe pain refractory to medical treatment in a patient with OA likely requires surgical intervention. Patients who have difficulty ambulating more than a reasonable distance (ie, 1 block) or cannot stand in place for more than several minutes due to severe pain should be considered for total joint replacement. Patients often report awaking with severe pain at night or pain that significantly impedes their activities of daily living. In these patients, total joint replacement can be extremely beneficial and life altering.
Conclusion
Osteoarthritis is the most common arthritic disease and has a very high prevalence in the veteran population. Aging, obesity, prior trauma, and activity level are the common risk factors for the development of OA. Patterns of disease are recognizable by history, examination, and prominent radiographic features. Causes of secondary OA are important to recognize and treat. The pathogenesis of OA involves a disrupted homeostatic process leading to cartilage degradation, microfracture, subchondral sclerosis, and osteophyte formation. Treatment is unique to the individual and should include a comprehensive strategy involving patient education, exercise or physical therapy, and analgesia. Patients with severe osteoarthritis that significantly impacts activities of daily living may benefit from surgery.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cameron KL, Hsiao MS, Owens BD, Burks R, Svoboda SJ. Incidence of physician diagnosed osteoarthritis among active duty United States military service members. Arthritis Rheum. 2011;63(10):2974-2982.
2. Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56(5):1397-1407.
3. Oliviero F, Ramonda R, Punzi L. New horizons in osteoarthritis. Swiss Med Wkly. 2010;140:w13098.
4. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115-2126.
5. Kraus VB, Jordan JM, Doherty M, et al. The Genetics of Generalized Osteoarthritis (GOGO) study: study design and evaluation of osteoarthritis phenotypes. Osteoarthritis Cartilage. 2007;15(2):120-127.
6. Lementowski PW, Zelicof SB. Obesity and osteoarthritis. Am J Orthop (Belle Mead NJ). 2008;37(3):148-151.
7. Anandacoomarasamy A, March L. Current evidence for osteoarthritis treatments. Ther Adv Musculoskelet Dis. 2010;2(1):17-28.
8. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskel Dis. 2013;5(2):77-94.
9. Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4);465-474.
10. Fernandes L, Hagen KB, Bijlsma JW, et al; European League Against Rheumatism (EULAR). EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125-1135.
11. Katz JN, Earp BE, Gomoll AH. Surgical management of osteoarthritis. Arthritis Care Res (Hoboken). 2010;62(9):1220-1228.
12. U.S. Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Non-Surgical Management of Hip & Knee Osteoarthritis, Version 1.0. U.S. Department of Veterans Affairs Website. http://www.healthquality.va.gov/guidelines/CD/OA. Published 2014. Accessed February 9, 2015.
13. Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, McAlindon TE. Comparative
effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162(1):46-54.
14. Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
15. Das SK, Mishra K, Ramakrishnan S, et al. A randomized controlled trial to evaluate the slow-acting symptom modifying effects of a regimen containing colchicine in a subset of patients with osteoarthritis of the knee. Osteoarthritis Cartilage. 2002;10(4):247-252.
16. Aran S, Malekzadeh S, Seifirad S. A double-blind randomized controlled trial appraising the symptom-modifying effects of colchicine on osteoarthritis of the knee. Clin Exp Rheumatol. 2011;29(3):513-518.
1. Cameron KL, Hsiao MS, Owens BD, Burks R, Svoboda SJ. Incidence of physician diagnosed osteoarthritis among active duty United States military service members. Arthritis Rheum. 2011;63(10):2974-2982.
2. Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56(5):1397-1407.
3. Oliviero F, Ramonda R, Punzi L. New horizons in osteoarthritis. Swiss Med Wkly. 2010;140:w13098.
4. Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115-2126.
5. Kraus VB, Jordan JM, Doherty M, et al. The Genetics of Generalized Osteoarthritis (GOGO) study: study design and evaluation of osteoarthritis phenotypes. Osteoarthritis Cartilage. 2007;15(2):120-127.
6. Lementowski PW, Zelicof SB. Obesity and osteoarthritis. Am J Orthop (Belle Mead NJ). 2008;37(3):148-151.
7. Anandacoomarasamy A, March L. Current evidence for osteoarthritis treatments. Ther Adv Musculoskelet Dis. 2010;2(1):17-28.
8. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskel Dis. 2013;5(2):77-94.
9. Hochberg MC, Altman RD, April KT, et al; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4);465-474.
10. Fernandes L, Hagen KB, Bijlsma JW, et al; European League Against Rheumatism (EULAR). EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125-1135.
11. Katz JN, Earp BE, Gomoll AH. Surgical management of osteoarthritis. Arthritis Care Res (Hoboken). 2010;62(9):1220-1228.
12. U.S. Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for the Non-Surgical Management of Hip & Knee Osteoarthritis, Version 1.0. U.S. Department of Veterans Affairs Website. http://www.healthquality.va.gov/guidelines/CD/OA. Published 2014. Accessed February 9, 2015.
13. Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, McAlindon TE. Comparative
effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med. 2015;162(1):46-54.
14. Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225.
15. Das SK, Mishra K, Ramakrishnan S, et al. A randomized controlled trial to evaluate the slow-acting symptom modifying effects of a regimen containing colchicine in a subset of patients with osteoarthritis of the knee. Osteoarthritis Cartilage. 2002;10(4):247-252.
16. Aran S, Malekzadeh S, Seifirad S. A double-blind randomized controlled trial appraising the symptom-modifying effects of colchicine on osteoarthritis of the knee. Clin Exp Rheumatol. 2011;29(3):513-518.