User login
VQI-VVR registry data eyed for guiding development of ethical standards
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
NEW YORK – Registry data can be used to craft guidance for determining the appropriateness of procedures at vein centers, based on data presented by Thomas W. Wakefield, MD at the 2018 Veith Symposium.
The Vascular Quality Initiative Varicose Vein Registry (VQI-VVR), initiated in 2014 by the Society for Vascular Surgery in conjunction with the American Venous Forum, captures procedures that are performed in vein centers, office-based practices, and ambulatory or inpatient settings. The VVR looks at ablation and phlebectomy techniques and captures data including patient demographics, history, procedure data, plus early and late office-based and patient-reported follow-up in order to benchmark and improve outcomes and develop best practices and to help meet vein center certification requirements. The VVR includes 39 centers and more than 23,000 procedures.
Dr. Wakefield, who heads the VVR, used this registry as a means to illustrate how VQIs could be used to establish whether “the expected health benefit exceeds the expected negative consequences by a sufficiently wide margin that the procedure is worth doing.” This can be considered to be “appropriateness, which is part of ethical treatment.” Dr. Wakefield is the Stanley Professor of Vascular Surgery at the University of Michigan and section head, vascular surgery, University of Michigan Cardiovascular Center, Ann Arbor.
Data from the VQI registry (of which the VVR is a component) are now being used to generate appropriateness reports, said Dr. Wakefield.
The VQI represents a large comprehensive database of long-term data to define appropriate care. In addition, the VQI infrastructure is already geared to producing these reports both at a center and at a surgeon level. One disadvantage of the VVR registry, however, is low participation – only the 39 centers – and that it doesn’t capture cosmetic procedures and lesser (C1) disease. Further, it’s “likely the VQI participants are the ‘good actors,’ ” he added.
Targets for appropriateness include the proportion of patients undergoing ablation C2 or C4 disease or greater, the mean number of ablations per patient, the mean number of ablations per limb, and the proportion of perforated ablations for greater than C4 disease. Plotting out the data for these procedures at the center level can be assessed against current thinking on best practices in the various areas. For example, “the mean number of ablations per patient has been suggested at 1.8 to be about the right number,” and he used the graph of the center performance in this area to show that most of the centers were below this objective.
In an even more appropriate example of how this kind of data could be used to determine appropriateness, Dr. Wakefield described how perforated ablations should be performed for greater than C4 disease, but not for C2 disease. He described how, according to the actual data in the registry, there have been 870 total perforated treatments recorded, 38% for C2 disease, and of these 332 procedures, almost half of these were performed at one center only, with two other centers reporting 30 such procedures. “So clearly there are three centers that are doing perforated ablations for patients that are outside the guidelines,” Dr. Wakefield pointed out.
In future, payer demand is likely to demand that each treating physician provide evidence of the appropriateness of procedures performed, as well as appropriate patient selection and adherence to best practices, and good outcomes, which is part of what a society-based registry such as the VVR can provide.
“I believe the VQI-VVR is well-positioned to meet these needs. And if we ask the question ‘can VQI be used as a benchmark for setting ethical standards,’ I think it can certainly be used to help set appropriate standards, and since appropriateness is one part of ethical standards, I believe it has a role,” he concluded.
Dr. Wakefield reported that he had no disclosures.
REPORTING FROM THE 2018 VEITH SYMPOSIUM
Don’t just work hard; work hard at living
NEW YORK – “A physician falls overboard on a large cruise ship and passengers gather at the guard rail. The first passenger at the guardrail shakes his finger down at the drowning physician and says, ‘You need to learn how to swim!’ Another passenger says, ‘No, man, throw him a life preserver.’ ... Finally, a passenger says, ‘We need better guard rails.’ ”
That’s the analogy Cynthia K. Shortell, MD used to kick off her presentation on physician burnout and the need for resilience at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
“Which of these is right? Well, of course, the answer is they all are,” said Dr. Shortell, who is a professor of surgery at Duke University Durham, N.C. But certainly, only the life preserver answer was appropriate at that time for the drowning physician, she added.
Continuing the analogy, Dr. Shortell pointed out that surely there is a man overboard, with 1 in 20 surgeons reporting suicidal ideation. That rate jumps threefold if the surgeon has had a recent medical error. In addition, vascular surgeons in particular are within the top tier of specialties at risk for burnout.
“We do need better guardrails,” she said, and described the need to actively engage with the health care system to help solve these issues, including those involving electronic medical records and operating room inefficiency and use. In addition, there is a great need for additional services that are provided to other high-end professionals, including food, concierge service, gym access, and other services that help with tasks of daily life when physicians need to spend most of their time at the hospital.
But, in the end, Dr. Shortell said, “We do need to learn to swim. Ultimately, we do need to take a role in having responsibility to solve this problem on our own. We need to change the way we think about our work, and the way we think about our health, and the way our culture values working hard instead of working hard at living.”
Dr. Shortell also highlighted the need to deal with musculoskeletal issues arising from the way that surgeons operate. This, along with good leadership, are key factors in preventing and remediating burnout.
Dr. Shortell had no disclosures relevant to her talk.
NEW YORK – “A physician falls overboard on a large cruise ship and passengers gather at the guard rail. The first passenger at the guardrail shakes his finger down at the drowning physician and says, ‘You need to learn how to swim!’ Another passenger says, ‘No, man, throw him a life preserver.’ ... Finally, a passenger says, ‘We need better guard rails.’ ”
That’s the analogy Cynthia K. Shortell, MD used to kick off her presentation on physician burnout and the need for resilience at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
“Which of these is right? Well, of course, the answer is they all are,” said Dr. Shortell, who is a professor of surgery at Duke University Durham, N.C. But certainly, only the life preserver answer was appropriate at that time for the drowning physician, she added.
Continuing the analogy, Dr. Shortell pointed out that surely there is a man overboard, with 1 in 20 surgeons reporting suicidal ideation. That rate jumps threefold if the surgeon has had a recent medical error. In addition, vascular surgeons in particular are within the top tier of specialties at risk for burnout.
“We do need better guardrails,” she said, and described the need to actively engage with the health care system to help solve these issues, including those involving electronic medical records and operating room inefficiency and use. In addition, there is a great need for additional services that are provided to other high-end professionals, including food, concierge service, gym access, and other services that help with tasks of daily life when physicians need to spend most of their time at the hospital.
But, in the end, Dr. Shortell said, “We do need to learn to swim. Ultimately, we do need to take a role in having responsibility to solve this problem on our own. We need to change the way we think about our work, and the way we think about our health, and the way our culture values working hard instead of working hard at living.”
Dr. Shortell also highlighted the need to deal with musculoskeletal issues arising from the way that surgeons operate. This, along with good leadership, are key factors in preventing and remediating burnout.
Dr. Shortell had no disclosures relevant to her talk.
NEW YORK – “A physician falls overboard on a large cruise ship and passengers gather at the guard rail. The first passenger at the guardrail shakes his finger down at the drowning physician and says, ‘You need to learn how to swim!’ Another passenger says, ‘No, man, throw him a life preserver.’ ... Finally, a passenger says, ‘We need better guard rails.’ ”
That’s the analogy Cynthia K. Shortell, MD used to kick off her presentation on physician burnout and the need for resilience at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
“Which of these is right? Well, of course, the answer is they all are,” said Dr. Shortell, who is a professor of surgery at Duke University Durham, N.C. But certainly, only the life preserver answer was appropriate at that time for the drowning physician, she added.
Continuing the analogy, Dr. Shortell pointed out that surely there is a man overboard, with 1 in 20 surgeons reporting suicidal ideation. That rate jumps threefold if the surgeon has had a recent medical error. In addition, vascular surgeons in particular are within the top tier of specialties at risk for burnout.
“We do need better guardrails,” she said, and described the need to actively engage with the health care system to help solve these issues, including those involving electronic medical records and operating room inefficiency and use. In addition, there is a great need for additional services that are provided to other high-end professionals, including food, concierge service, gym access, and other services that help with tasks of daily life when physicians need to spend most of their time at the hospital.
But, in the end, Dr. Shortell said, “We do need to learn to swim. Ultimately, we do need to take a role in having responsibility to solve this problem on our own. We need to change the way we think about our work, and the way we think about our health, and the way our culture values working hard instead of working hard at living.”
Dr. Shortell also highlighted the need to deal with musculoskeletal issues arising from the way that surgeons operate. This, along with good leadership, are key factors in preventing and remediating burnout.
Dr. Shortell had no disclosures relevant to her talk.
REPORTING FROM THE VEITHSYMPOSIUM
What’s new with the SVS VQI?
NEW YORK – The Vascular Quality Initiative (VQI) is designed to improve the quality, safety, and effectiveness of vascular health care, but also reduce costs through the collection and exchange of information, according to Larry W. Kraiss, MD, professor of surgery, University of Utah, Salt Lake City.
The VQI consists of three major components: a federally accredited patient safety organization (PSO), a registry, and a distributed network of quality groups, which can also serve as a platform for internal quality improvement efforts.
Even though registries are considered less reliable than the venerated randomized clinical trial models are, registries have some unique advantages, according to Dr. Kraiss, who spoke at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. Randomized clinical trials (RCTs) are very expensive to conduct and are criticized for potentially not being generalizable because of their rigidly defined inclusion/exclusion criteria. Despite inherent problems with registry data, especially bias, there are now statistical methods to help account for the biases. Registry-controlled trials are going to be important to answer many questions that cannot be answered by RCTs. Such trials can be too costly or actually unethical to randomize under certain circumstances. Registries, however, provide real-world patient populations in greater numbers than RCTs can manage, including access to rare events that would otherwise not be detected.
The VQI holds an important place in this second tier and is an important source of information for clinical care.
The VQI has grown steadily since its inception, and there are more than 500 centers now participating, including 6 international centers, and 18 regional groups, according to Dr. Kraiss. There are more than 530,000 procedures contained within the VQI’s 12 registries, with more than half of them involving peripheral vascular interventions and carotid endarterectomies. “But there [are] a healthy number of cases in all of the other registries, which provide a very rich resource and evidence base,” he added.
The VQI is becoming very important in the regulatory framework, with the Food and Drug Administration embracing “real-world evidence” as a way to justify some of its decisions, and the VQI has been involved in this process. The VQI has coordinated several post-market surveillance programs, the two most important being in the areas of thoracic endovascular aortic repair (TEVAR) and transcarotid artery revascularization (TCAR), said Dr. Kraiss.
One of the important values of the VQI is the ability to examine benchmarks and to compare performance across centers. For example, looking at aortic abdominal aneurysm (AAA) repair data, the results showed that a number of centers were not following established Society for Vascular Society guidelines and that there were a substantial number of AAAs reported in the VQI that were treated when they were below the threshold for intervention and should have received routine observation only.
So, ultimately two of the greatest values of the VQI are the ability to use it as a means of local quality improvement, and to provide an avenue for important clinical research, Dr. Kraiss concluded.
Dr. Kraiss reported that they had no disclosures.
NEW YORK – The Vascular Quality Initiative (VQI) is designed to improve the quality, safety, and effectiveness of vascular health care, but also reduce costs through the collection and exchange of information, according to Larry W. Kraiss, MD, professor of surgery, University of Utah, Salt Lake City.
The VQI consists of three major components: a federally accredited patient safety organization (PSO), a registry, and a distributed network of quality groups, which can also serve as a platform for internal quality improvement efforts.
Even though registries are considered less reliable than the venerated randomized clinical trial models are, registries have some unique advantages, according to Dr. Kraiss, who spoke at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. Randomized clinical trials (RCTs) are very expensive to conduct and are criticized for potentially not being generalizable because of their rigidly defined inclusion/exclusion criteria. Despite inherent problems with registry data, especially bias, there are now statistical methods to help account for the biases. Registry-controlled trials are going to be important to answer many questions that cannot be answered by RCTs. Such trials can be too costly or actually unethical to randomize under certain circumstances. Registries, however, provide real-world patient populations in greater numbers than RCTs can manage, including access to rare events that would otherwise not be detected.
The VQI holds an important place in this second tier and is an important source of information for clinical care.
The VQI has grown steadily since its inception, and there are more than 500 centers now participating, including 6 international centers, and 18 regional groups, according to Dr. Kraiss. There are more than 530,000 procedures contained within the VQI’s 12 registries, with more than half of them involving peripheral vascular interventions and carotid endarterectomies. “But there [are] a healthy number of cases in all of the other registries, which provide a very rich resource and evidence base,” he added.
The VQI is becoming very important in the regulatory framework, with the Food and Drug Administration embracing “real-world evidence” as a way to justify some of its decisions, and the VQI has been involved in this process. The VQI has coordinated several post-market surveillance programs, the two most important being in the areas of thoracic endovascular aortic repair (TEVAR) and transcarotid artery revascularization (TCAR), said Dr. Kraiss.
One of the important values of the VQI is the ability to examine benchmarks and to compare performance across centers. For example, looking at aortic abdominal aneurysm (AAA) repair data, the results showed that a number of centers were not following established Society for Vascular Society guidelines and that there were a substantial number of AAAs reported in the VQI that were treated when they were below the threshold for intervention and should have received routine observation only.
So, ultimately two of the greatest values of the VQI are the ability to use it as a means of local quality improvement, and to provide an avenue for important clinical research, Dr. Kraiss concluded.
Dr. Kraiss reported that they had no disclosures.
NEW YORK – The Vascular Quality Initiative (VQI) is designed to improve the quality, safety, and effectiveness of vascular health care, but also reduce costs through the collection and exchange of information, according to Larry W. Kraiss, MD, professor of surgery, University of Utah, Salt Lake City.
The VQI consists of three major components: a federally accredited patient safety organization (PSO), a registry, and a distributed network of quality groups, which can also serve as a platform for internal quality improvement efforts.
Even though registries are considered less reliable than the venerated randomized clinical trial models are, registries have some unique advantages, according to Dr. Kraiss, who spoke at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. Randomized clinical trials (RCTs) are very expensive to conduct and are criticized for potentially not being generalizable because of their rigidly defined inclusion/exclusion criteria. Despite inherent problems with registry data, especially bias, there are now statistical methods to help account for the biases. Registry-controlled trials are going to be important to answer many questions that cannot be answered by RCTs. Such trials can be too costly or actually unethical to randomize under certain circumstances. Registries, however, provide real-world patient populations in greater numbers than RCTs can manage, including access to rare events that would otherwise not be detected.
The VQI holds an important place in this second tier and is an important source of information for clinical care.
The VQI has grown steadily since its inception, and there are more than 500 centers now participating, including 6 international centers, and 18 regional groups, according to Dr. Kraiss. There are more than 530,000 procedures contained within the VQI’s 12 registries, with more than half of them involving peripheral vascular interventions and carotid endarterectomies. “But there [are] a healthy number of cases in all of the other registries, which provide a very rich resource and evidence base,” he added.
The VQI is becoming very important in the regulatory framework, with the Food and Drug Administration embracing “real-world evidence” as a way to justify some of its decisions, and the VQI has been involved in this process. The VQI has coordinated several post-market surveillance programs, the two most important being in the areas of thoracic endovascular aortic repair (TEVAR) and transcarotid artery revascularization (TCAR), said Dr. Kraiss.
One of the important values of the VQI is the ability to examine benchmarks and to compare performance across centers. For example, looking at aortic abdominal aneurysm (AAA) repair data, the results showed that a number of centers were not following established Society for Vascular Society guidelines and that there were a substantial number of AAAs reported in the VQI that were treated when they were below the threshold for intervention and should have received routine observation only.
So, ultimately two of the greatest values of the VQI are the ability to use it as a means of local quality improvement, and to provide an avenue for important clinical research, Dr. Kraiss concluded.
Dr. Kraiss reported that they had no disclosures.
REPORTING FROM THE VEITHSYMPOSIUM
Update on integrated vascular surgery residencies
NEW YORK – In March 2005, the Accreditation Council for Graduate Medical Education approved the primary certificate in vascular surgery, and the first integrated vascular surgery residencies (0+5) were approved shortly thereafter. By 2015, there was more than a 900% increase in both the number of programs and positions, which were offered for matriculation in July 2016, according to Murray L. Shames, MD, professor of surgery and radiology at the University of South Florida, Tampa, and chief of the division of vascular surgery at Tampa General Hospital.
In 2009, Dr. Shames and his colleagues first looked at the issue to try to better understand the applicant pool, and they found that there was a 900% increase in demand for the 0+5 residency positions, compared with the traditional 5+2 vascular fellowships, and that there was a 0+5 applicant-to-position ratio of 8:1 that year. “Despite initial concerns regarding the shortened training, studies have demonstrated equivalent case volumes and job opportunities for integrated vascular residents and vascular fellows,” Dr. Shames stated at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
His current presentation was an update of that assessment done for the 2015 data, as integrated vascular surgery residents have begun to enter the workforce. They looked at the current supply and demand for 0+5 training programs (as well as the traditional 5+2 programs), and the quality and attributes of the 0+5 residency applicants. They obtained data for applicants for both types of programs: 2008-2015 for 0+2 and 2007-2016 for 5+2) and comparable match data were queried for 2008-2016. They looked at the number of programs, the number of positions, the total number of applicants, sex of the applicants, applications/program and applications/position, and the U.S. versus international applicant ratios.
They found that the number of integrated programs increased from 4 to 48, with an increase from 4 to 56 positions, during the study period, said Dr. Shames. Demand for integrated vascular residencies has increased nearly 300%, from 112 applicants in 2008 to 434 in 2015. The total number of U.S. medical school graduate applicants to these programs has increased from 40 in 2008 to 2,030 in 2015, with the increase in program applicants driven primarily by these U.S. medical school graduates; the number of international applicants per program decrease over this time period from 57 to 37. The percentage of women applicants has steadily increased, from 16% to 27%, and currently women constitute 41% of all integrated vascular surgery residents.
“Overall, the supply for integrated vascular surgery residency positions continues to be outnumbered by the number of applicants, with increasing applicant to position ratios at 7.8:1 in 2015, while the total number for vascular surgery fellowships has remained stable at about 1:1,” Dr. Shames concluded.
Dr. Shames reported having no relevant disclosures for his presentation.
NEW YORK – In March 2005, the Accreditation Council for Graduate Medical Education approved the primary certificate in vascular surgery, and the first integrated vascular surgery residencies (0+5) were approved shortly thereafter. By 2015, there was more than a 900% increase in both the number of programs and positions, which were offered for matriculation in July 2016, according to Murray L. Shames, MD, professor of surgery and radiology at the University of South Florida, Tampa, and chief of the division of vascular surgery at Tampa General Hospital.
In 2009, Dr. Shames and his colleagues first looked at the issue to try to better understand the applicant pool, and they found that there was a 900% increase in demand for the 0+5 residency positions, compared with the traditional 5+2 vascular fellowships, and that there was a 0+5 applicant-to-position ratio of 8:1 that year. “Despite initial concerns regarding the shortened training, studies have demonstrated equivalent case volumes and job opportunities for integrated vascular residents and vascular fellows,” Dr. Shames stated at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
His current presentation was an update of that assessment done for the 2015 data, as integrated vascular surgery residents have begun to enter the workforce. They looked at the current supply and demand for 0+5 training programs (as well as the traditional 5+2 programs), and the quality and attributes of the 0+5 residency applicants. They obtained data for applicants for both types of programs: 2008-2015 for 0+2 and 2007-2016 for 5+2) and comparable match data were queried for 2008-2016. They looked at the number of programs, the number of positions, the total number of applicants, sex of the applicants, applications/program and applications/position, and the U.S. versus international applicant ratios.
They found that the number of integrated programs increased from 4 to 48, with an increase from 4 to 56 positions, during the study period, said Dr. Shames. Demand for integrated vascular residencies has increased nearly 300%, from 112 applicants in 2008 to 434 in 2015. The total number of U.S. medical school graduate applicants to these programs has increased from 40 in 2008 to 2,030 in 2015, with the increase in program applicants driven primarily by these U.S. medical school graduates; the number of international applicants per program decrease over this time period from 57 to 37. The percentage of women applicants has steadily increased, from 16% to 27%, and currently women constitute 41% of all integrated vascular surgery residents.
“Overall, the supply for integrated vascular surgery residency positions continues to be outnumbered by the number of applicants, with increasing applicant to position ratios at 7.8:1 in 2015, while the total number for vascular surgery fellowships has remained stable at about 1:1,” Dr. Shames concluded.
Dr. Shames reported having no relevant disclosures for his presentation.
NEW YORK – In March 2005, the Accreditation Council for Graduate Medical Education approved the primary certificate in vascular surgery, and the first integrated vascular surgery residencies (0+5) were approved shortly thereafter. By 2015, there was more than a 900% increase in both the number of programs and positions, which were offered for matriculation in July 2016, according to Murray L. Shames, MD, professor of surgery and radiology at the University of South Florida, Tampa, and chief of the division of vascular surgery at Tampa General Hospital.
In 2009, Dr. Shames and his colleagues first looked at the issue to try to better understand the applicant pool, and they found that there was a 900% increase in demand for the 0+5 residency positions, compared with the traditional 5+2 vascular fellowships, and that there was a 0+5 applicant-to-position ratio of 8:1 that year. “Despite initial concerns regarding the shortened training, studies have demonstrated equivalent case volumes and job opportunities for integrated vascular residents and vascular fellows,” Dr. Shames stated at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
His current presentation was an update of that assessment done for the 2015 data, as integrated vascular surgery residents have begun to enter the workforce. They looked at the current supply and demand for 0+5 training programs (as well as the traditional 5+2 programs), and the quality and attributes of the 0+5 residency applicants. They obtained data for applicants for both types of programs: 2008-2015 for 0+2 and 2007-2016 for 5+2) and comparable match data were queried for 2008-2016. They looked at the number of programs, the number of positions, the total number of applicants, sex of the applicants, applications/program and applications/position, and the U.S. versus international applicant ratios.
They found that the number of integrated programs increased from 4 to 48, with an increase from 4 to 56 positions, during the study period, said Dr. Shames. Demand for integrated vascular residencies has increased nearly 300%, from 112 applicants in 2008 to 434 in 2015. The total number of U.S. medical school graduate applicants to these programs has increased from 40 in 2008 to 2,030 in 2015, with the increase in program applicants driven primarily by these U.S. medical school graduates; the number of international applicants per program decrease over this time period from 57 to 37. The percentage of women applicants has steadily increased, from 16% to 27%, and currently women constitute 41% of all integrated vascular surgery residents.
“Overall, the supply for integrated vascular surgery residency positions continues to be outnumbered by the number of applicants, with increasing applicant to position ratios at 7.8:1 in 2015, while the total number for vascular surgery fellowships has remained stable at about 1:1,” Dr. Shames concluded.
Dr. Shames reported having no relevant disclosures for his presentation.
REPORTING FROM THE VEITHSYMPOSIUM
What are the barriers to solving the upcoming vascular surgeon shortage?
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
REPORTING FROM THE VEITHSYMPOSIUM
A bovine arch predicts worse outcomes with type B aortic dissections
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
REPORTING FROM VEITHSYMPOSIUM
Quality of life with PAD follows function, not clinical markers
Focus on ability to perform functional tasks when designing interventions aimed at improving health-related quality of life for patients with symptomatic peripheral arterial disease (PAD), advise the authors of a study published in the Journal of Vascular Surgery.
Clinical markers of disease severity and comorbidities are often the primary targets of interventions in PAD patients, but health-related quality of life (HRQoL) based on their functional capabilities matters more to patients, according to Andrew W. Gardner, PhD, of Penn State University, Hershey, and his colleagues.
“Interventions designed to improve HRQoL should focus on improving the quality of executing functional tasks, such as walking more steadily without stumbling; completing ADLs [activities of daily living] that are not specific to walking, such as bathing and transferring; and improving patient-based ability to walk various distances and speeds and to climb stairs,” the researchers wrote.
They studied 216 PAD patients (mean age, 65 years) with ambulatory leg pain confirmed by treadmill exercise and ankle brachial index less than or equal to 0.90 at rest or less than or equal to 0.73 after exercise. Patient HRQoL was measured using the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). All patients performed a maximal treadmill test, a 6-minute walk test, and gait speed from a 4-meter walk test was measured. Their ambulatory activity was monitored for 7 days using a step monitor. In addition, patients self-assessed their ability to perform four lower-level ADLs, consisting of walking across a small room, bathing, transferring from a bed to a chair, and using the toilet. They also evaluated their ability to perform two higher-level ADLs consisting of walking up and down stairs to the second floor without help and walking a half-mile without help.
Approximately 10%-17% of the patients reported either having some difficulty with or being unable to perform basic ADLs, whereas the majority reported either having some difficulty with or being unable to perform higher-level ADLs consisting of walking up and down stairs (74%) and walking a half-mile without help (85%).
The primary novel finding, according to Dr. Gardner and his colleagues, was that patient-based measurements of physical function were the strongest predictors of both physical and mental subscales of HRQoL.
The significant predictors were Walking Impairment Questionnaire speed score (P less than .001), history of stumbling while walking (P less than .001), stair climbing score (P = .001), bathing (P = .001), 6-minute walking distance (P =.004), and daily walking cadence (P = .043). The significant predictors of the role limitations caused by emotional problems subscale of the SF-36 included a history of stumbling while walking (P less than .001), transferring from a bed to a chair (P less than .001), and the walking distance score (P = .022).
Noticeably, a history of stumbling while walking was considered particularly important to the patients. In contrast, objective measurements of physical function (6-minute walking distance and daily walking cadence) were predictive only of the physical function subscale. Comorbid conditions and objective measures of PAD severity, such as ankle brachial index, claudication onset time, and peak walking time, were not at all predictive of HRQoL, the researchers stated.
The authors reported that they had no conflicts of interest.
SOURCE: Gardner AW et al. J Vasc Surg. 2018;68:1126-34.
Focus on ability to perform functional tasks when designing interventions aimed at improving health-related quality of life for patients with symptomatic peripheral arterial disease (PAD), advise the authors of a study published in the Journal of Vascular Surgery.
Clinical markers of disease severity and comorbidities are often the primary targets of interventions in PAD patients, but health-related quality of life (HRQoL) based on their functional capabilities matters more to patients, according to Andrew W. Gardner, PhD, of Penn State University, Hershey, and his colleagues.
“Interventions designed to improve HRQoL should focus on improving the quality of executing functional tasks, such as walking more steadily without stumbling; completing ADLs [activities of daily living] that are not specific to walking, such as bathing and transferring; and improving patient-based ability to walk various distances and speeds and to climb stairs,” the researchers wrote.
They studied 216 PAD patients (mean age, 65 years) with ambulatory leg pain confirmed by treadmill exercise and ankle brachial index less than or equal to 0.90 at rest or less than or equal to 0.73 after exercise. Patient HRQoL was measured using the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). All patients performed a maximal treadmill test, a 6-minute walk test, and gait speed from a 4-meter walk test was measured. Their ambulatory activity was monitored for 7 days using a step monitor. In addition, patients self-assessed their ability to perform four lower-level ADLs, consisting of walking across a small room, bathing, transferring from a bed to a chair, and using the toilet. They also evaluated their ability to perform two higher-level ADLs consisting of walking up and down stairs to the second floor without help and walking a half-mile without help.
Approximately 10%-17% of the patients reported either having some difficulty with or being unable to perform basic ADLs, whereas the majority reported either having some difficulty with or being unable to perform higher-level ADLs consisting of walking up and down stairs (74%) and walking a half-mile without help (85%).
The primary novel finding, according to Dr. Gardner and his colleagues, was that patient-based measurements of physical function were the strongest predictors of both physical and mental subscales of HRQoL.
The significant predictors were Walking Impairment Questionnaire speed score (P less than .001), history of stumbling while walking (P less than .001), stair climbing score (P = .001), bathing (P = .001), 6-minute walking distance (P =.004), and daily walking cadence (P = .043). The significant predictors of the role limitations caused by emotional problems subscale of the SF-36 included a history of stumbling while walking (P less than .001), transferring from a bed to a chair (P less than .001), and the walking distance score (P = .022).
Noticeably, a history of stumbling while walking was considered particularly important to the patients. In contrast, objective measurements of physical function (6-minute walking distance and daily walking cadence) were predictive only of the physical function subscale. Comorbid conditions and objective measures of PAD severity, such as ankle brachial index, claudication onset time, and peak walking time, were not at all predictive of HRQoL, the researchers stated.
The authors reported that they had no conflicts of interest.
SOURCE: Gardner AW et al. J Vasc Surg. 2018;68:1126-34.
Focus on ability to perform functional tasks when designing interventions aimed at improving health-related quality of life for patients with symptomatic peripheral arterial disease (PAD), advise the authors of a study published in the Journal of Vascular Surgery.
Clinical markers of disease severity and comorbidities are often the primary targets of interventions in PAD patients, but health-related quality of life (HRQoL) based on their functional capabilities matters more to patients, according to Andrew W. Gardner, PhD, of Penn State University, Hershey, and his colleagues.
“Interventions designed to improve HRQoL should focus on improving the quality of executing functional tasks, such as walking more steadily without stumbling; completing ADLs [activities of daily living] that are not specific to walking, such as bathing and transferring; and improving patient-based ability to walk various distances and speeds and to climb stairs,” the researchers wrote.
They studied 216 PAD patients (mean age, 65 years) with ambulatory leg pain confirmed by treadmill exercise and ankle brachial index less than or equal to 0.90 at rest or less than or equal to 0.73 after exercise. Patient HRQoL was measured using the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). All patients performed a maximal treadmill test, a 6-minute walk test, and gait speed from a 4-meter walk test was measured. Their ambulatory activity was monitored for 7 days using a step monitor. In addition, patients self-assessed their ability to perform four lower-level ADLs, consisting of walking across a small room, bathing, transferring from a bed to a chair, and using the toilet. They also evaluated their ability to perform two higher-level ADLs consisting of walking up and down stairs to the second floor without help and walking a half-mile without help.
Approximately 10%-17% of the patients reported either having some difficulty with or being unable to perform basic ADLs, whereas the majority reported either having some difficulty with or being unable to perform higher-level ADLs consisting of walking up and down stairs (74%) and walking a half-mile without help (85%).
The primary novel finding, according to Dr. Gardner and his colleagues, was that patient-based measurements of physical function were the strongest predictors of both physical and mental subscales of HRQoL.
The significant predictors were Walking Impairment Questionnaire speed score (P less than .001), history of stumbling while walking (P less than .001), stair climbing score (P = .001), bathing (P = .001), 6-minute walking distance (P =.004), and daily walking cadence (P = .043). The significant predictors of the role limitations caused by emotional problems subscale of the SF-36 included a history of stumbling while walking (P less than .001), transferring from a bed to a chair (P less than .001), and the walking distance score (P = .022).
Noticeably, a history of stumbling while walking was considered particularly important to the patients. In contrast, objective measurements of physical function (6-minute walking distance and daily walking cadence) were predictive only of the physical function subscale. Comorbid conditions and objective measures of PAD severity, such as ankle brachial index, claudication onset time, and peak walking time, were not at all predictive of HRQoL, the researchers stated.
The authors reported that they had no conflicts of interest.
SOURCE: Gardner AW et al. J Vasc Surg. 2018;68:1126-34.
FROM THE JOURNAL OF VASCULAR SURGERY
Key clinical point: Patient assessment of functional status was the best predictor of health-related quality of life.
Major finding: Objective measures of peripheral arterial disease severity, such as ankle brachial index, claudication onset time, and peak walking time, were not predictive of health-related quality of life.
Study details: A clinical and survey study of 216 patients with peripheral arterial disease.
Disclosures: The authors reported that they had no financial conflicts of interest.
Source: Gardner AW et al. J Vasc Surg. 2018;68:1126-34.
INPACT SFA 5-year results: Drug-coated balloon treatment remains safe, durable
The INPACT SFA trial demonstrated the long-term safety of the IN.PACT Admiral drug-coated balloon (DCB) through 5 years, with no device-, procedure-, or paclitaxel-related deaths seen, coupled with continued low thrombosis rates throughout 5 years, according to John R. Laird, MD, of the Adventist Heart & Vascular Institute, St. Helena, Calif.
Dr. Laird presented the final, 5-year results of the combined INPACT SFA I and II trials at the 2018 Vascular Interventional Vascular Advances meeting.
The combined studies compared 220 patients treated with DCB and 111 treated with standard percutaneous transluminal angioplasty (PTA) who were followed out to 5 years. The patient population was 65% men, had a mean age of about 68 years, and none of the baseline characteristics followed were statistically significant between the treatment groups. The mean total lesion length treated was 8.9 cm for the DCB group and 8.8 cm for the PTA group, also a nonsignificant difference.
The primary efficacy endpoint for the study was primary patency within 12 months, defined as freedom from clinically driven target lesion revascularization (CD-TLR) and duplex ultrasound–derived restenosis. The primary safety endpoint was freedom from device-and procedure-related death through 30 days, and freedom from target limb major amputation and CD-TLR within 12 months.
Although there were no significant differences seen between DCB and placebo for CD-TLR or any TLR, there was a significant difference seen in the time to CD-TLR over 1,800 days: 808 days for DCB versus 475 days for placebo (P less than .001).
There were no significant differences seen between the DCB and placebo for any of the safety endpoint components over 5 years.
INPACT SFA was the “first independently adjudicated, blinded, randomized trial to demonstrate superior effectiveness of a drug-coated balloon through 5 years,” and the “results support DCB as a first-line strategy for the treatment of femoropopliteal disease,” Dr. Laird concluded.
The trial was sponsored by Medtronic Endovascular. Dr. Laird reported that he is a consultant/advisory board member for Abbott Vascular, Bard, Boston Scientific, and Medtronic.
The INPACT SFA trial demonstrated the long-term safety of the IN.PACT Admiral drug-coated balloon (DCB) through 5 years, with no device-, procedure-, or paclitaxel-related deaths seen, coupled with continued low thrombosis rates throughout 5 years, according to John R. Laird, MD, of the Adventist Heart & Vascular Institute, St. Helena, Calif.
Dr. Laird presented the final, 5-year results of the combined INPACT SFA I and II trials at the 2018 Vascular Interventional Vascular Advances meeting.
The combined studies compared 220 patients treated with DCB and 111 treated with standard percutaneous transluminal angioplasty (PTA) who were followed out to 5 years. The patient population was 65% men, had a mean age of about 68 years, and none of the baseline characteristics followed were statistically significant between the treatment groups. The mean total lesion length treated was 8.9 cm for the DCB group and 8.8 cm for the PTA group, also a nonsignificant difference.
The primary efficacy endpoint for the study was primary patency within 12 months, defined as freedom from clinically driven target lesion revascularization (CD-TLR) and duplex ultrasound–derived restenosis. The primary safety endpoint was freedom from device-and procedure-related death through 30 days, and freedom from target limb major amputation and CD-TLR within 12 months.
Although there were no significant differences seen between DCB and placebo for CD-TLR or any TLR, there was a significant difference seen in the time to CD-TLR over 1,800 days: 808 days for DCB versus 475 days for placebo (P less than .001).
There were no significant differences seen between the DCB and placebo for any of the safety endpoint components over 5 years.
INPACT SFA was the “first independently adjudicated, blinded, randomized trial to demonstrate superior effectiveness of a drug-coated balloon through 5 years,” and the “results support DCB as a first-line strategy for the treatment of femoropopliteal disease,” Dr. Laird concluded.
The trial was sponsored by Medtronic Endovascular. Dr. Laird reported that he is a consultant/advisory board member for Abbott Vascular, Bard, Boston Scientific, and Medtronic.
The INPACT SFA trial demonstrated the long-term safety of the IN.PACT Admiral drug-coated balloon (DCB) through 5 years, with no device-, procedure-, or paclitaxel-related deaths seen, coupled with continued low thrombosis rates throughout 5 years, according to John R. Laird, MD, of the Adventist Heart & Vascular Institute, St. Helena, Calif.
Dr. Laird presented the final, 5-year results of the combined INPACT SFA I and II trials at the 2018 Vascular Interventional Vascular Advances meeting.
The combined studies compared 220 patients treated with DCB and 111 treated with standard percutaneous transluminal angioplasty (PTA) who were followed out to 5 years. The patient population was 65% men, had a mean age of about 68 years, and none of the baseline characteristics followed were statistically significant between the treatment groups. The mean total lesion length treated was 8.9 cm for the DCB group and 8.8 cm for the PTA group, also a nonsignificant difference.
The primary efficacy endpoint for the study was primary patency within 12 months, defined as freedom from clinically driven target lesion revascularization (CD-TLR) and duplex ultrasound–derived restenosis. The primary safety endpoint was freedom from device-and procedure-related death through 30 days, and freedom from target limb major amputation and CD-TLR within 12 months.
Although there were no significant differences seen between DCB and placebo for CD-TLR or any TLR, there was a significant difference seen in the time to CD-TLR over 1,800 days: 808 days for DCB versus 475 days for placebo (P less than .001).
There were no significant differences seen between the DCB and placebo for any of the safety endpoint components over 5 years.
INPACT SFA was the “first independently adjudicated, blinded, randomized trial to demonstrate superior effectiveness of a drug-coated balloon through 5 years,” and the “results support DCB as a first-line strategy for the treatment of femoropopliteal disease,” Dr. Laird concluded.
The trial was sponsored by Medtronic Endovascular. Dr. Laird reported that he is a consultant/advisory board member for Abbott Vascular, Bard, Boston Scientific, and Medtronic.
FROM VIVA 2018
Key clinical point: Use of a drug-coated balloon was effective and safe over 5 years for the treatment of superficial femoral artery lesions.
Major finding: There was a significant difference seen in the time to clinically driven target lesion revascularization: 808 days for drug-coated balloon versus 475 days for placebo (P less than .001).
Study details: A pair of trials that included 331 patients with superficial femoral artery lesions
Disclosures: The INPACT SFA trial was sponsored by Medtronic Endovascular. Dr. Laird disclosed that he is a consultant/advisory board member for Abbott Vascular, Bard, Boston Scientific, and Medtronic.
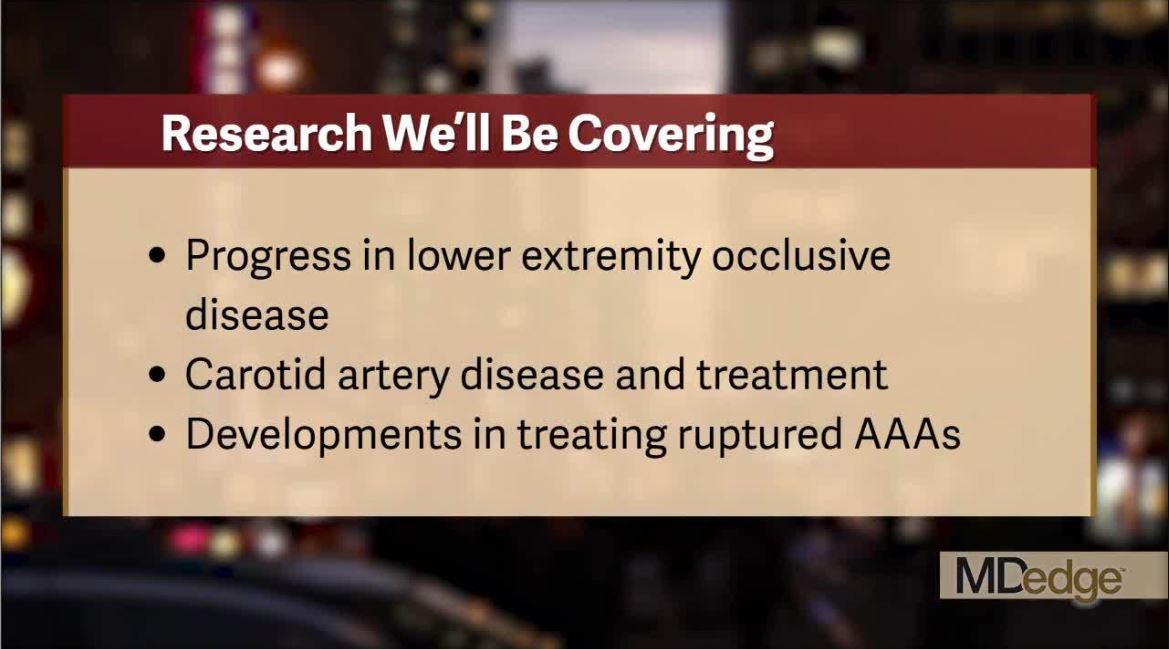
Catch all the action at the VEITHsymposium
The VEITHsymposium, held yearly in New York City, is a world-class meeting that covers the full range of vascular surgery and treatment. Frontline Medical Communications on behalf of our publication, Vascular Specialist, will be there to cover the newest and the best in devices, drugs, and surgical treatments for arterial and venous disease and the biological systems they impact.
Check out this video and get a flavor of what we will be covering live once the meeting starts. And be sure follow our continuing coverage next week at on our website and @VascularTweets. Also, check out our in depth reporting from the meeting afterward in the upcoming pages of Vascular Specialist.
The VEITHsymposium, held yearly in New York City, is a world-class meeting that covers the full range of vascular surgery and treatment. Frontline Medical Communications on behalf of our publication, Vascular Specialist, will be there to cover the newest and the best in devices, drugs, and surgical treatments for arterial and venous disease and the biological systems they impact.
Check out this video and get a flavor of what we will be covering live once the meeting starts. And be sure follow our continuing coverage next week at on our website and @VascularTweets. Also, check out our in depth reporting from the meeting afterward in the upcoming pages of Vascular Specialist.
The VEITHsymposium, held yearly in New York City, is a world-class meeting that covers the full range of vascular surgery and treatment. Frontline Medical Communications on behalf of our publication, Vascular Specialist, will be there to cover the newest and the best in devices, drugs, and surgical treatments for arterial and venous disease and the biological systems they impact.
Check out this video and get a flavor of what we will be covering live once the meeting starts. And be sure follow our continuing coverage next week at on our website and @VascularTweets. Also, check out our in depth reporting from the meeting afterward in the upcoming pages of Vascular Specialist.
Struggling to reach an HCV vaccine
Currently, there is no effective hepatitis C virus (HCV) vaccine available despite numerous ongoing studies, according to the results of a review published in Gastroenterology.
In their article, Justin R. Bailey, MD, of Johns Hopkins University, Baltimore, and his colleagues reviewed the limited feasibility of applying traditional vaccine design to HCV and the problem of genetic diversity in the virus, as well as trials of vaccines designed to elicit T-cell responses.
One profound difficulty in the development and testing of an HCV vaccine is that the cohort most predictably at risk for high infection levels, people who inject drugs, are notoriously difficult to recruit, maintain consistent treatment, and follow up on – all necessary aspects of an appropriate vaccine trial.
Thus, at present, adjuvant envelope or core protein and virus-vectored nonstructural antigen vaccines have been tested only in healthy volunteers who are not at risk for HCV infection; viral vectors encoding nonstructural proteins remain the only vaccine strategy tested in truly at-risk individuals, according to Dr. Bailey and his colleagues.
“Although pharmaceutical companies invest in drug development, vaccine development requires investment from sources beyond government and charitable foundations. A prophylactic HCV vaccine is an important part of a successful strategy for global control. Although development is not easy, the quest is a worthy challenge,” Dr. Bailey and his colleagues concluded.
The authors reported having no conflicts.
SOURCE: Bailey JR et al. Gastroenterology. 2018 Sep 27. doi: 10.1053/j.gastro.2018.08.060.
Currently, there is no effective hepatitis C virus (HCV) vaccine available despite numerous ongoing studies, according to the results of a review published in Gastroenterology.
In their article, Justin R. Bailey, MD, of Johns Hopkins University, Baltimore, and his colleagues reviewed the limited feasibility of applying traditional vaccine design to HCV and the problem of genetic diversity in the virus, as well as trials of vaccines designed to elicit T-cell responses.
One profound difficulty in the development and testing of an HCV vaccine is that the cohort most predictably at risk for high infection levels, people who inject drugs, are notoriously difficult to recruit, maintain consistent treatment, and follow up on – all necessary aspects of an appropriate vaccine trial.
Thus, at present, adjuvant envelope or core protein and virus-vectored nonstructural antigen vaccines have been tested only in healthy volunteers who are not at risk for HCV infection; viral vectors encoding nonstructural proteins remain the only vaccine strategy tested in truly at-risk individuals, according to Dr. Bailey and his colleagues.
“Although pharmaceutical companies invest in drug development, vaccine development requires investment from sources beyond government and charitable foundations. A prophylactic HCV vaccine is an important part of a successful strategy for global control. Although development is not easy, the quest is a worthy challenge,” Dr. Bailey and his colleagues concluded.
The authors reported having no conflicts.
SOURCE: Bailey JR et al. Gastroenterology. 2018 Sep 27. doi: 10.1053/j.gastro.2018.08.060.
Currently, there is no effective hepatitis C virus (HCV) vaccine available despite numerous ongoing studies, according to the results of a review published in Gastroenterology.
In their article, Justin R. Bailey, MD, of Johns Hopkins University, Baltimore, and his colleagues reviewed the limited feasibility of applying traditional vaccine design to HCV and the problem of genetic diversity in the virus, as well as trials of vaccines designed to elicit T-cell responses.
One profound difficulty in the development and testing of an HCV vaccine is that the cohort most predictably at risk for high infection levels, people who inject drugs, are notoriously difficult to recruit, maintain consistent treatment, and follow up on – all necessary aspects of an appropriate vaccine trial.
Thus, at present, adjuvant envelope or core protein and virus-vectored nonstructural antigen vaccines have been tested only in healthy volunteers who are not at risk for HCV infection; viral vectors encoding nonstructural proteins remain the only vaccine strategy tested in truly at-risk individuals, according to Dr. Bailey and his colleagues.
“Although pharmaceutical companies invest in drug development, vaccine development requires investment from sources beyond government and charitable foundations. A prophylactic HCV vaccine is an important part of a successful strategy for global control. Although development is not easy, the quest is a worthy challenge,” Dr. Bailey and his colleagues concluded.
The authors reported having no conflicts.
SOURCE: Bailey JR et al. Gastroenterology. 2018 Sep 27. doi: 10.1053/j.gastro.2018.08.060.
FROM GASTROENTEROLOGY