User login
Blood group O linked to decreased risk of SARS-CoV-2 infection
Blood group O was associated with a decreased risk for contracting SARS-CoV-2 infection, according to the results of large retrospective analysis of the Danish population.
Researchers Mike Bogetofte Barnkob, MD, of the Department of Clinical Immunology, Odense (Denmark) University Hospital, and colleagues performed a retrospective cohort analysis of all Danish individuals with a known ABO blood group who were tested for SARS-CoV-2 between Feb. 27, 2020, and July 30, 2020.
Of the 841,327 people tested, ABO and RhD blood groups could be identified for 473,654 individuals. ABO and RhD data from 2,204,742 (38% of the entire Danish population) were used as a reference, according to the online report in Blood Advances.
The primary outcome was status of ABO and RhD blood groups and test results for SARS-CoV-2. The secondary outcomes followed were hospitalization and death from COVID-19.
Reduced prevalence
The study found that ABO blood groups varied significantly between patients and the reference group, with only 38.41% (95% confidence interval, 37.30%-39.50%) of the patients belonging to blood group O, compared with 41.70% (95% CI, 41.60%-41.80%) in the controls, corresponding to a relative risk of 0.87 (95% CI, 0.83-0.91) for acquiring COVID-19.
There was a slight, but statistically significant, difference in blood group distribution between the SARS-CoV-22 individuals and the reference population (P < .001), according to the authors.
Among the SARS-CoV-2 individuals, fewer group O individuals were found (P < .001); while more A, B, and AB individuals were seen (P < .001, P = .011, and P = .091, respectively). There was no significant difference seen among A, B, and AB blood groups (P = .30). The RR for contracting SARS-CoV-2 were 1.09 (95% CI, 1.04-1.14) for A group individuals; 1.06 (95% CI, 0.99-1.14) for B group; and 1.15 (95% CI, 1.03-1.27) for AB group, respectively.
There was no difference found in the RhD group between positive test cases and the reference population (P = .15). In addition, there was no statistical difference (all P > .40) between ABO blood groups and clinical severity of COVID-19 for nonhospitalized patients versus hospitalized patients or for deceased patients versus living patients, the researchers added.
Possible causes
The authors speculated on two possible causes of the lower prevalence of SARS-CoV-2 infection in the blood group O population. The first is that anti-A and anti-B antibodies may have an effect on neutralizing SARS-CoV viruses and that anti-A and anti-B are present on mucosal surfaces in some individuals lacking the corresponding ABO blood group. The second is that the association between ABO blood groups and levels of von Willebrand factor, which is higher in non-O individuals and is tied to an increased likelihood of arterial and venous thrombosis, could have an indirect or unknown impact on susceptibility to infection, according to the authors.
“Given the known increased risk of thrombosis in non-O individuals and the evolving central role for thrombosis in the pathogenesis of COVID-19, it is important to explore this aspect more closely in larger patient cohorts (e.g., by examining ABO blood type and viral load, the severity of symptoms, and the long-term effects following COVID-19),” the researchers concluded.
One author reported receiving fees from Bristol Myers Squibb, Novartis, and Roche. The remaining authors reported they had no competing financial interests.
SOURCE: Barnkob MB et al. Blood Adv. 2020 Oct 14. doi: 10.1182/bloodadvances.2020002657.
Blood group O was associated with a decreased risk for contracting SARS-CoV-2 infection, according to the results of large retrospective analysis of the Danish population.
Researchers Mike Bogetofte Barnkob, MD, of the Department of Clinical Immunology, Odense (Denmark) University Hospital, and colleagues performed a retrospective cohort analysis of all Danish individuals with a known ABO blood group who were tested for SARS-CoV-2 between Feb. 27, 2020, and July 30, 2020.
Of the 841,327 people tested, ABO and RhD blood groups could be identified for 473,654 individuals. ABO and RhD data from 2,204,742 (38% of the entire Danish population) were used as a reference, according to the online report in Blood Advances.
The primary outcome was status of ABO and RhD blood groups and test results for SARS-CoV-2. The secondary outcomes followed were hospitalization and death from COVID-19.
Reduced prevalence
The study found that ABO blood groups varied significantly between patients and the reference group, with only 38.41% (95% confidence interval, 37.30%-39.50%) of the patients belonging to blood group O, compared with 41.70% (95% CI, 41.60%-41.80%) in the controls, corresponding to a relative risk of 0.87 (95% CI, 0.83-0.91) for acquiring COVID-19.
There was a slight, but statistically significant, difference in blood group distribution between the SARS-CoV-22 individuals and the reference population (P < .001), according to the authors.
Among the SARS-CoV-2 individuals, fewer group O individuals were found (P < .001); while more A, B, and AB individuals were seen (P < .001, P = .011, and P = .091, respectively). There was no significant difference seen among A, B, and AB blood groups (P = .30). The RR for contracting SARS-CoV-2 were 1.09 (95% CI, 1.04-1.14) for A group individuals; 1.06 (95% CI, 0.99-1.14) for B group; and 1.15 (95% CI, 1.03-1.27) for AB group, respectively.
There was no difference found in the RhD group between positive test cases and the reference population (P = .15). In addition, there was no statistical difference (all P > .40) between ABO blood groups and clinical severity of COVID-19 for nonhospitalized patients versus hospitalized patients or for deceased patients versus living patients, the researchers added.
Possible causes
The authors speculated on two possible causes of the lower prevalence of SARS-CoV-2 infection in the blood group O population. The first is that anti-A and anti-B antibodies may have an effect on neutralizing SARS-CoV viruses and that anti-A and anti-B are present on mucosal surfaces in some individuals lacking the corresponding ABO blood group. The second is that the association between ABO blood groups and levels of von Willebrand factor, which is higher in non-O individuals and is tied to an increased likelihood of arterial and venous thrombosis, could have an indirect or unknown impact on susceptibility to infection, according to the authors.
“Given the known increased risk of thrombosis in non-O individuals and the evolving central role for thrombosis in the pathogenesis of COVID-19, it is important to explore this aspect more closely in larger patient cohorts (e.g., by examining ABO blood type and viral load, the severity of symptoms, and the long-term effects following COVID-19),” the researchers concluded.
One author reported receiving fees from Bristol Myers Squibb, Novartis, and Roche. The remaining authors reported they had no competing financial interests.
SOURCE: Barnkob MB et al. Blood Adv. 2020 Oct 14. doi: 10.1182/bloodadvances.2020002657.
Blood group O was associated with a decreased risk for contracting SARS-CoV-2 infection, according to the results of large retrospective analysis of the Danish population.
Researchers Mike Bogetofte Barnkob, MD, of the Department of Clinical Immunology, Odense (Denmark) University Hospital, and colleagues performed a retrospective cohort analysis of all Danish individuals with a known ABO blood group who were tested for SARS-CoV-2 between Feb. 27, 2020, and July 30, 2020.
Of the 841,327 people tested, ABO and RhD blood groups could be identified for 473,654 individuals. ABO and RhD data from 2,204,742 (38% of the entire Danish population) were used as a reference, according to the online report in Blood Advances.
The primary outcome was status of ABO and RhD blood groups and test results for SARS-CoV-2. The secondary outcomes followed were hospitalization and death from COVID-19.
Reduced prevalence
The study found that ABO blood groups varied significantly between patients and the reference group, with only 38.41% (95% confidence interval, 37.30%-39.50%) of the patients belonging to blood group O, compared with 41.70% (95% CI, 41.60%-41.80%) in the controls, corresponding to a relative risk of 0.87 (95% CI, 0.83-0.91) for acquiring COVID-19.
There was a slight, but statistically significant, difference in blood group distribution between the SARS-CoV-22 individuals and the reference population (P < .001), according to the authors.
Among the SARS-CoV-2 individuals, fewer group O individuals were found (P < .001); while more A, B, and AB individuals were seen (P < .001, P = .011, and P = .091, respectively). There was no significant difference seen among A, B, and AB blood groups (P = .30). The RR for contracting SARS-CoV-2 were 1.09 (95% CI, 1.04-1.14) for A group individuals; 1.06 (95% CI, 0.99-1.14) for B group; and 1.15 (95% CI, 1.03-1.27) for AB group, respectively.
There was no difference found in the RhD group between positive test cases and the reference population (P = .15). In addition, there was no statistical difference (all P > .40) between ABO blood groups and clinical severity of COVID-19 for nonhospitalized patients versus hospitalized patients or for deceased patients versus living patients, the researchers added.
Possible causes
The authors speculated on two possible causes of the lower prevalence of SARS-CoV-2 infection in the blood group O population. The first is that anti-A and anti-B antibodies may have an effect on neutralizing SARS-CoV viruses and that anti-A and anti-B are present on mucosal surfaces in some individuals lacking the corresponding ABO blood group. The second is that the association between ABO blood groups and levels of von Willebrand factor, which is higher in non-O individuals and is tied to an increased likelihood of arterial and venous thrombosis, could have an indirect or unknown impact on susceptibility to infection, according to the authors.
“Given the known increased risk of thrombosis in non-O individuals and the evolving central role for thrombosis in the pathogenesis of COVID-19, it is important to explore this aspect more closely in larger patient cohorts (e.g., by examining ABO blood type and viral load, the severity of symptoms, and the long-term effects following COVID-19),” the researchers concluded.
One author reported receiving fees from Bristol Myers Squibb, Novartis, and Roche. The remaining authors reported they had no competing financial interests.
SOURCE: Barnkob MB et al. Blood Adv. 2020 Oct 14. doi: 10.1182/bloodadvances.2020002657.
FROM BLOOD ADVANCES
Study: Complications from childhood ALL and its treatment are common, but can be managed
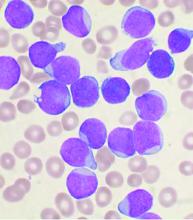
Despite survival after treatment of acute lymphoblastic leukemia (ALL), a high percentage of children suffered acute complications, even without relapse, according to a report published online in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study of 110 children with acute lymphoblastic leukemia (ALL), Ayse Pınar Öztürk, MD, and colleagues at Istanbul University, Cerrahpasa Faculty of Medicine, evaluated the acute complications that occurred during the treatment of childhood ALL and documented their survival rates. The 110 patients, comprising 65 boys and 45 girls, were all treated with the Children’s Oncology Group protocol from 1999 to 2014.
The mean age at admission was 8.3 years and 97 patients (88.2%) were diagnosed with pre–B-cell ALL, 11 (10%) with T-cell ALL, 1 (0.9%) with mixed phenotype acute leukemia, and 1 (0.9%) with mature B-cell acute leukemia. A total of 36.3% were evaluated to be in the standard-risk group and the rest were in the high-risk group. Regular follow-up and evaluation for acute complications was available for 105 of the patients.
Survival and complications
Of the 110 patients, 98 were assessed in the survival analyses. The 5- and 10-year overall survival rates were both 85.9%, while the relapse-free survival rates at 1, 3, and 5 years were 97.9%, 91.3%, and 86.3%, respectively. These results are favorable and in line with good results reported in the literature, according to the researchers.
In terms of acute complications, infection was the most common (88.5%), followed by gastrointestinal (27.6%), neurologic (26.6%), metabolic/endocrine (15.2%), drug-related hypersensitivity (15.2%), avascular necrosis (12.3%), thrombotic (10.4%), severe psychiatric (1.9%), and various other complications (11.4%).
In the present study, 13 of the 98 patients (13.3%) died. All 13 patients had been in the high-risk group and 9 had had relapsed ALL. Of the 13 deaths, 8 (8.2%) had resulted from treatment resistance and toxicity and 5 (5.1%) from severe infection (sepsis).
During ALL treatment, various complications can occur related to the disease itself or the treatment, according to the authors. However, they added that in regularly and closely monitored patients, complications can be effectively prevented, treated, and eliminated by aggressive observation and prompt intervention.
“In our study, the short hospitalization period, prompt implementation of protocol updates, rapid analysis of laboratory tests, continuous supportive care, efficient education given to the parents of children, and consistently undertaking patient care and treatment management by the same expert team increased the success of the therapy and ensured low complication rates,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Öztürk AP et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 17. doi: 10.1016/j.clml.2020.08.025.
Despite survival after treatment of acute lymphoblastic leukemia (ALL), a high percentage of children suffered acute complications, even without relapse, according to a report published online in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study of 110 children with acute lymphoblastic leukemia (ALL), Ayse Pınar Öztürk, MD, and colleagues at Istanbul University, Cerrahpasa Faculty of Medicine, evaluated the acute complications that occurred during the treatment of childhood ALL and documented their survival rates. The 110 patients, comprising 65 boys and 45 girls, were all treated with the Children’s Oncology Group protocol from 1999 to 2014.
The mean age at admission was 8.3 years and 97 patients (88.2%) were diagnosed with pre–B-cell ALL, 11 (10%) with T-cell ALL, 1 (0.9%) with mixed phenotype acute leukemia, and 1 (0.9%) with mature B-cell acute leukemia. A total of 36.3% were evaluated to be in the standard-risk group and the rest were in the high-risk group. Regular follow-up and evaluation for acute complications was available for 105 of the patients.
Survival and complications
Of the 110 patients, 98 were assessed in the survival analyses. The 5- and 10-year overall survival rates were both 85.9%, while the relapse-free survival rates at 1, 3, and 5 years were 97.9%, 91.3%, and 86.3%, respectively. These results are favorable and in line with good results reported in the literature, according to the researchers.
In terms of acute complications, infection was the most common (88.5%), followed by gastrointestinal (27.6%), neurologic (26.6%), metabolic/endocrine (15.2%), drug-related hypersensitivity (15.2%), avascular necrosis (12.3%), thrombotic (10.4%), severe psychiatric (1.9%), and various other complications (11.4%).
In the present study, 13 of the 98 patients (13.3%) died. All 13 patients had been in the high-risk group and 9 had had relapsed ALL. Of the 13 deaths, 8 (8.2%) had resulted from treatment resistance and toxicity and 5 (5.1%) from severe infection (sepsis).
During ALL treatment, various complications can occur related to the disease itself or the treatment, according to the authors. However, they added that in regularly and closely monitored patients, complications can be effectively prevented, treated, and eliminated by aggressive observation and prompt intervention.
“In our study, the short hospitalization period, prompt implementation of protocol updates, rapid analysis of laboratory tests, continuous supportive care, efficient education given to the parents of children, and consistently undertaking patient care and treatment management by the same expert team increased the success of the therapy and ensured low complication rates,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Öztürk AP et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 17. doi: 10.1016/j.clml.2020.08.025.
Despite survival after treatment of acute lymphoblastic leukemia (ALL), a high percentage of children suffered acute complications, even without relapse, according to a report published online in Clinical Lymphoma, Myeloma & Leukemia.
In a retrospective study of 110 children with acute lymphoblastic leukemia (ALL), Ayse Pınar Öztürk, MD, and colleagues at Istanbul University, Cerrahpasa Faculty of Medicine, evaluated the acute complications that occurred during the treatment of childhood ALL and documented their survival rates. The 110 patients, comprising 65 boys and 45 girls, were all treated with the Children’s Oncology Group protocol from 1999 to 2014.
The mean age at admission was 8.3 years and 97 patients (88.2%) were diagnosed with pre–B-cell ALL, 11 (10%) with T-cell ALL, 1 (0.9%) with mixed phenotype acute leukemia, and 1 (0.9%) with mature B-cell acute leukemia. A total of 36.3% were evaluated to be in the standard-risk group and the rest were in the high-risk group. Regular follow-up and evaluation for acute complications was available for 105 of the patients.
Survival and complications
Of the 110 patients, 98 were assessed in the survival analyses. The 5- and 10-year overall survival rates were both 85.9%, while the relapse-free survival rates at 1, 3, and 5 years were 97.9%, 91.3%, and 86.3%, respectively. These results are favorable and in line with good results reported in the literature, according to the researchers.
In terms of acute complications, infection was the most common (88.5%), followed by gastrointestinal (27.6%), neurologic (26.6%), metabolic/endocrine (15.2%), drug-related hypersensitivity (15.2%), avascular necrosis (12.3%), thrombotic (10.4%), severe psychiatric (1.9%), and various other complications (11.4%).
In the present study, 13 of the 98 patients (13.3%) died. All 13 patients had been in the high-risk group and 9 had had relapsed ALL. Of the 13 deaths, 8 (8.2%) had resulted from treatment resistance and toxicity and 5 (5.1%) from severe infection (sepsis).
During ALL treatment, various complications can occur related to the disease itself or the treatment, according to the authors. However, they added that in regularly and closely monitored patients, complications can be effectively prevented, treated, and eliminated by aggressive observation and prompt intervention.
“In our study, the short hospitalization period, prompt implementation of protocol updates, rapid analysis of laboratory tests, continuous supportive care, efficient education given to the parents of children, and consistently undertaking patient care and treatment management by the same expert team increased the success of the therapy and ensured low complication rates,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Öztürk AP et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 17. doi: 10.1016/j.clml.2020.08.025.
FROM Clinical Lymphoma, Myeloma & Leukemia
Older adults with multiple myeloma face heavy burden of care
A substantial cumulative burden of treatment in the first year is borne by patients newly diagnosed with multiple myeloma (MM), according to a report published online in Clinical Lymphoma, Myeloma and Leukemia.
MM is a disease of aging, with a median age at diagnosis of 69 years, and the burden of treatment and not just possible outcomes should be considered in decision-making discussions with patients, according to researchers Hira S. Mian, MD, of McMaster University, Hamilton, Ont., and colleagues.
They performed a retrospective study of a Medicare-linked database of 3,065 adults newly diagnosed with multiple myeloma (MM) between 2007-2013. The treatment burden among the patients was assessed to determine those factors associated with high treatment burden.
Heavy burden
Treatment burden was defined as the number of total days with a health care encounter (including acute care and outpatient visits), oncology and nononcology physician visits, and the number of new prescriptions within the first year following diagnosis, according to the researchers.
The study found that there was a substantial burden of treatment, including a median of more than 2 months of cumulative interactions with health care, within the first year following diagnosis. This burden was highest during the first 3 months.
Those patients who had multiple comorbidities (adjusted odds ratio [aOR] 1.27 per 1-point increase in Charlson comorbidity index, P < .001), poor performance status (aOR 1.85, P < .001), myeloma-related end-organ damage, especially bone disease (aOR 2.28, P < .001), and those who received autologous stem cell transplant (aOR 2.41, P < .001) were more likely to have a higher treatment burden, they reported.
“Decision-making regarding treatment modalities should not just emphasize traditional parameters such as response rates and progression-free survival but should also include a discussion regarding the workload burden placed on the patient and the care partner, in order to ensure informed and patient-centered decision-making is prioritized. This may be particularly relevant among certain subgroups such as older patients with cancer who may prioritize quality of life over aggressive disease control and overall survival,” the researchers concluded.
The study was funded by the National Cancer Institute at the U.S. National Institutes of Health. The authors reported funding from a variety of pharmaceutical and biotechnology companies.
SOURCE: Mian HS et al. Clin Lymphoma Myeloma Leuk. 2020 Oct 1. doi: 10.1016/j.clml.2020.09.010.
A substantial cumulative burden of treatment in the first year is borne by patients newly diagnosed with multiple myeloma (MM), according to a report published online in Clinical Lymphoma, Myeloma and Leukemia.
MM is a disease of aging, with a median age at diagnosis of 69 years, and the burden of treatment and not just possible outcomes should be considered in decision-making discussions with patients, according to researchers Hira S. Mian, MD, of McMaster University, Hamilton, Ont., and colleagues.
They performed a retrospective study of a Medicare-linked database of 3,065 adults newly diagnosed with multiple myeloma (MM) between 2007-2013. The treatment burden among the patients was assessed to determine those factors associated with high treatment burden.
Heavy burden
Treatment burden was defined as the number of total days with a health care encounter (including acute care and outpatient visits), oncology and nononcology physician visits, and the number of new prescriptions within the first year following diagnosis, according to the researchers.
The study found that there was a substantial burden of treatment, including a median of more than 2 months of cumulative interactions with health care, within the first year following diagnosis. This burden was highest during the first 3 months.
Those patients who had multiple comorbidities (adjusted odds ratio [aOR] 1.27 per 1-point increase in Charlson comorbidity index, P < .001), poor performance status (aOR 1.85, P < .001), myeloma-related end-organ damage, especially bone disease (aOR 2.28, P < .001), and those who received autologous stem cell transplant (aOR 2.41, P < .001) were more likely to have a higher treatment burden, they reported.
“Decision-making regarding treatment modalities should not just emphasize traditional parameters such as response rates and progression-free survival but should also include a discussion regarding the workload burden placed on the patient and the care partner, in order to ensure informed and patient-centered decision-making is prioritized. This may be particularly relevant among certain subgroups such as older patients with cancer who may prioritize quality of life over aggressive disease control and overall survival,” the researchers concluded.
The study was funded by the National Cancer Institute at the U.S. National Institutes of Health. The authors reported funding from a variety of pharmaceutical and biotechnology companies.
SOURCE: Mian HS et al. Clin Lymphoma Myeloma Leuk. 2020 Oct 1. doi: 10.1016/j.clml.2020.09.010.
A substantial cumulative burden of treatment in the first year is borne by patients newly diagnosed with multiple myeloma (MM), according to a report published online in Clinical Lymphoma, Myeloma and Leukemia.
MM is a disease of aging, with a median age at diagnosis of 69 years, and the burden of treatment and not just possible outcomes should be considered in decision-making discussions with patients, according to researchers Hira S. Mian, MD, of McMaster University, Hamilton, Ont., and colleagues.
They performed a retrospective study of a Medicare-linked database of 3,065 adults newly diagnosed with multiple myeloma (MM) between 2007-2013. The treatment burden among the patients was assessed to determine those factors associated with high treatment burden.
Heavy burden
Treatment burden was defined as the number of total days with a health care encounter (including acute care and outpatient visits), oncology and nononcology physician visits, and the number of new prescriptions within the first year following diagnosis, according to the researchers.
The study found that there was a substantial burden of treatment, including a median of more than 2 months of cumulative interactions with health care, within the first year following diagnosis. This burden was highest during the first 3 months.
Those patients who had multiple comorbidities (adjusted odds ratio [aOR] 1.27 per 1-point increase in Charlson comorbidity index, P < .001), poor performance status (aOR 1.85, P < .001), myeloma-related end-organ damage, especially bone disease (aOR 2.28, P < .001), and those who received autologous stem cell transplant (aOR 2.41, P < .001) were more likely to have a higher treatment burden, they reported.
“Decision-making regarding treatment modalities should not just emphasize traditional parameters such as response rates and progression-free survival but should also include a discussion regarding the workload burden placed on the patient and the care partner, in order to ensure informed and patient-centered decision-making is prioritized. This may be particularly relevant among certain subgroups such as older patients with cancer who may prioritize quality of life over aggressive disease control and overall survival,” the researchers concluded.
The study was funded by the National Cancer Institute at the U.S. National Institutes of Health. The authors reported funding from a variety of pharmaceutical and biotechnology companies.
SOURCE: Mian HS et al. Clin Lymphoma Myeloma Leuk. 2020 Oct 1. doi: 10.1016/j.clml.2020.09.010.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Meta-analysis: Acalabrutinib showed better PFS and OS than other frontline CLL therapies
Acalabrutinib, given alone or in combination with obinutuzumab, showed favorable progression-free survival (PFS) and overall survival (OS), compared with other frontline therapies for chronic lymphocytic leukemia (CLL) in fludarabine-ineligible patients, according to the results of a meta-analysis comparing clinical trial results.
Researchers conducted a systematic literature review for applicable CLL studies that examined frontline treatments in order to compare the results with data on acalabrutinib (monotherapy and in combination with obinutuzumab) from patients in the ELEVATE-TN study (NCT02475681), according to a report published in Clinical Therapeutics.
Matthew S. Davids, MD, MMSc, of the Dana-Farber Cancer Institute in Boston, and colleagues performed a network meta-analysis (NMA) comparing acalabrutinib versus other standard frontline therapies for CLL in patients for whom fludarabine-based treatment is not appropriate.
“In the absence of head-to-head trial data, NMAs allow for simultaneous comparisons of a number of interventions with multiple comparators, by synthesizing direct and indirect evidence,” the authors stated.
Eight randomized controlled trials (RCTs) met the criteria for comparison.
The researchers constructed two evidence networks: Network A comprised solely RCTs that met the inclusion criteria, and Network B comprised seven RCTs and a published cross-trial comparison of ibrutinib from RESONATE-2 and chlorambucil plus obinutuzumab from iLLUMINATE. PFS and OS results were reported by using hazard ratios and 95% credible intervals.
Overall benefit
Both networks showed a significant improvement in PFS for acalabrutinib plus obinutuzumab over all comparators, according to the researchers. Both networks also showed a significant improvement in PFS for acalabrutinib monotherapy versus most comparators, with a significant difference to ibrutinib monotherapy found in Network A but not Network B.
Conversely, a significant difference in PFS was observed for acalabrutinib monotherapy versus venetoclax plus obinutuzumab in Network B but not Network A.
Overall survival hazard ratios ranged from 0.18 to 0.65 in favor of acalabrutinib-based treatment, but not all were significant. Acalabrutinib plus obinutuzumab ranked highest in terms of PFS and OS improvement, followed by acalabrutinib monotherapy.
“Although our NMAs provide useful insights into the relative efficacy of acalabrutinib, compared with other frontline treatments of CLL, the results cannot be considered confirmatory, and head-to-head randomized trials are needed, especially to compare the efficacy of acalabrutinib versus other targeted agents,” the researchers concluded.
AstraZeneca sponsored the study. The authors reported funding from AstraZeneca and numerous other pharmaceutical companies.
SOURCE: Davids MS et al. Clin Ther. 2020 Oct 5. doi: 10.1016/j.clinthera.2020.08.017.
Acalabrutinib, given alone or in combination with obinutuzumab, showed favorable progression-free survival (PFS) and overall survival (OS), compared with other frontline therapies for chronic lymphocytic leukemia (CLL) in fludarabine-ineligible patients, according to the results of a meta-analysis comparing clinical trial results.
Researchers conducted a systematic literature review for applicable CLL studies that examined frontline treatments in order to compare the results with data on acalabrutinib (monotherapy and in combination with obinutuzumab) from patients in the ELEVATE-TN study (NCT02475681), according to a report published in Clinical Therapeutics.
Matthew S. Davids, MD, MMSc, of the Dana-Farber Cancer Institute in Boston, and colleagues performed a network meta-analysis (NMA) comparing acalabrutinib versus other standard frontline therapies for CLL in patients for whom fludarabine-based treatment is not appropriate.
“In the absence of head-to-head trial data, NMAs allow for simultaneous comparisons of a number of interventions with multiple comparators, by synthesizing direct and indirect evidence,” the authors stated.
Eight randomized controlled trials (RCTs) met the criteria for comparison.
The researchers constructed two evidence networks: Network A comprised solely RCTs that met the inclusion criteria, and Network B comprised seven RCTs and a published cross-trial comparison of ibrutinib from RESONATE-2 and chlorambucil plus obinutuzumab from iLLUMINATE. PFS and OS results were reported by using hazard ratios and 95% credible intervals.
Overall benefit
Both networks showed a significant improvement in PFS for acalabrutinib plus obinutuzumab over all comparators, according to the researchers. Both networks also showed a significant improvement in PFS for acalabrutinib monotherapy versus most comparators, with a significant difference to ibrutinib monotherapy found in Network A but not Network B.
Conversely, a significant difference in PFS was observed for acalabrutinib monotherapy versus venetoclax plus obinutuzumab in Network B but not Network A.
Overall survival hazard ratios ranged from 0.18 to 0.65 in favor of acalabrutinib-based treatment, but not all were significant. Acalabrutinib plus obinutuzumab ranked highest in terms of PFS and OS improvement, followed by acalabrutinib monotherapy.
“Although our NMAs provide useful insights into the relative efficacy of acalabrutinib, compared with other frontline treatments of CLL, the results cannot be considered confirmatory, and head-to-head randomized trials are needed, especially to compare the efficacy of acalabrutinib versus other targeted agents,” the researchers concluded.
AstraZeneca sponsored the study. The authors reported funding from AstraZeneca and numerous other pharmaceutical companies.
SOURCE: Davids MS et al. Clin Ther. 2020 Oct 5. doi: 10.1016/j.clinthera.2020.08.017.
Acalabrutinib, given alone or in combination with obinutuzumab, showed favorable progression-free survival (PFS) and overall survival (OS), compared with other frontline therapies for chronic lymphocytic leukemia (CLL) in fludarabine-ineligible patients, according to the results of a meta-analysis comparing clinical trial results.
Researchers conducted a systematic literature review for applicable CLL studies that examined frontline treatments in order to compare the results with data on acalabrutinib (monotherapy and in combination with obinutuzumab) from patients in the ELEVATE-TN study (NCT02475681), according to a report published in Clinical Therapeutics.
Matthew S. Davids, MD, MMSc, of the Dana-Farber Cancer Institute in Boston, and colleagues performed a network meta-analysis (NMA) comparing acalabrutinib versus other standard frontline therapies for CLL in patients for whom fludarabine-based treatment is not appropriate.
“In the absence of head-to-head trial data, NMAs allow for simultaneous comparisons of a number of interventions with multiple comparators, by synthesizing direct and indirect evidence,” the authors stated.
Eight randomized controlled trials (RCTs) met the criteria for comparison.
The researchers constructed two evidence networks: Network A comprised solely RCTs that met the inclusion criteria, and Network B comprised seven RCTs and a published cross-trial comparison of ibrutinib from RESONATE-2 and chlorambucil plus obinutuzumab from iLLUMINATE. PFS and OS results were reported by using hazard ratios and 95% credible intervals.
Overall benefit
Both networks showed a significant improvement in PFS for acalabrutinib plus obinutuzumab over all comparators, according to the researchers. Both networks also showed a significant improvement in PFS for acalabrutinib monotherapy versus most comparators, with a significant difference to ibrutinib monotherapy found in Network A but not Network B.
Conversely, a significant difference in PFS was observed for acalabrutinib monotherapy versus venetoclax plus obinutuzumab in Network B but not Network A.
Overall survival hazard ratios ranged from 0.18 to 0.65 in favor of acalabrutinib-based treatment, but not all were significant. Acalabrutinib plus obinutuzumab ranked highest in terms of PFS and OS improvement, followed by acalabrutinib monotherapy.
“Although our NMAs provide useful insights into the relative efficacy of acalabrutinib, compared with other frontline treatments of CLL, the results cannot be considered confirmatory, and head-to-head randomized trials are needed, especially to compare the efficacy of acalabrutinib versus other targeted agents,” the researchers concluded.
AstraZeneca sponsored the study. The authors reported funding from AstraZeneca and numerous other pharmaceutical companies.
SOURCE: Davids MS et al. Clin Ther. 2020 Oct 5. doi: 10.1016/j.clinthera.2020.08.017.
FROM CLINICAL THERAPEUTICS
Orthopedic problems in children can be the first indication of acute lymphoblastic leukemia
The diagnosis of acute lymphoblastic leukemia (ALL) can be delayed because of vague presentation and normal hematological results. Orthopedic manifestations may be the primary presentation of ALL to physicians, and such symptoms in children should be cause for suspicion, even in the absence of hematological abnormalities, according to a report published in the Journal of Orthopaedics.
The study retrospectively assessed 250 consecutive ALL patients at a single institution to identify the frequency of ALL cases presented to the orthopedic department and to determine the number of these patients presenting with normal hematological results, according to Amrath Raj BK, MD, and colleagues at the Manipal (India) Academy of Higher Education.
Suspicion warranted
Twenty-two of the 250 patients (8.8%) presented primarily to the orthopedic department (4 with vertebral compression fractures, 12 with joint pain, and 6 with bone pain), but were subsequently diagnosed with ALL. These results were comparable to previous studies. The mean patient age at the first visit was 5.6 years; 13 patients were boys, and 9 were girls. Six of these 22 patients (27.3%) had a normal peripheral blood smear, according to the researchers.
“Acute leukemia should be considered strongly as a differential diagnosis in children with severe osteoporosis and vertebral fractures. Initial orthopedic manifestations are not uncommon, and the primary physician should maintain a high index of suspicion as a peripheral smear is not diagnostic in all patients,” the researchers concluded.
The authors reported that there was no outside funding source and that they had no conflicts.
SOURCE: Raj BK A et al. Journal of Orthopaedics. 2020;22:326-330.
The diagnosis of acute lymphoblastic leukemia (ALL) can be delayed because of vague presentation and normal hematological results. Orthopedic manifestations may be the primary presentation of ALL to physicians, and such symptoms in children should be cause for suspicion, even in the absence of hematological abnormalities, according to a report published in the Journal of Orthopaedics.
The study retrospectively assessed 250 consecutive ALL patients at a single institution to identify the frequency of ALL cases presented to the orthopedic department and to determine the number of these patients presenting with normal hematological results, according to Amrath Raj BK, MD, and colleagues at the Manipal (India) Academy of Higher Education.
Suspicion warranted
Twenty-two of the 250 patients (8.8%) presented primarily to the orthopedic department (4 with vertebral compression fractures, 12 with joint pain, and 6 with bone pain), but were subsequently diagnosed with ALL. These results were comparable to previous studies. The mean patient age at the first visit was 5.6 years; 13 patients were boys, and 9 were girls. Six of these 22 patients (27.3%) had a normal peripheral blood smear, according to the researchers.
“Acute leukemia should be considered strongly as a differential diagnosis in children with severe osteoporosis and vertebral fractures. Initial orthopedic manifestations are not uncommon, and the primary physician should maintain a high index of suspicion as a peripheral smear is not diagnostic in all patients,” the researchers concluded.
The authors reported that there was no outside funding source and that they had no conflicts.
SOURCE: Raj BK A et al. Journal of Orthopaedics. 2020;22:326-330.
The diagnosis of acute lymphoblastic leukemia (ALL) can be delayed because of vague presentation and normal hematological results. Orthopedic manifestations may be the primary presentation of ALL to physicians, and such symptoms in children should be cause for suspicion, even in the absence of hematological abnormalities, according to a report published in the Journal of Orthopaedics.
The study retrospectively assessed 250 consecutive ALL patients at a single institution to identify the frequency of ALL cases presented to the orthopedic department and to determine the number of these patients presenting with normal hematological results, according to Amrath Raj BK, MD, and colleagues at the Manipal (India) Academy of Higher Education.
Suspicion warranted
Twenty-two of the 250 patients (8.8%) presented primarily to the orthopedic department (4 with vertebral compression fractures, 12 with joint pain, and 6 with bone pain), but were subsequently diagnosed with ALL. These results were comparable to previous studies. The mean patient age at the first visit was 5.6 years; 13 patients were boys, and 9 were girls. Six of these 22 patients (27.3%) had a normal peripheral blood smear, according to the researchers.
“Acute leukemia should be considered strongly as a differential diagnosis in children with severe osteoporosis and vertebral fractures. Initial orthopedic manifestations are not uncommon, and the primary physician should maintain a high index of suspicion as a peripheral smear is not diagnostic in all patients,” the researchers concluded.
The authors reported that there was no outside funding source and that they had no conflicts.
SOURCE: Raj BK A et al. Journal of Orthopaedics. 2020;22:326-330.
FROM THE JOURNAL OF ORTHOPAEDICS
Initial response to novel agents preps MM patients for favorable transplant outcomes
For patients with multiple myeloma, triplet induction with novel agents beat doublet with regards to early results, according to Lalit Kumar, MD, and colleagues at the All India Institute of Medical sciences Myeloma Group, New Delhi.
The study analyzed 326 multiple myeloma patients who received high-dose, novel agent–based induction therapy prior to autologous stem cell transplant (ASCT) at a single institution, according to a report published in Clinical Lymphoma, Myeloma and Leukemia.
Between January 2005 and December 2018, 326 consecutive patients underwent high-dose chemotherapy and autologous stem cell transplant. The median age of the patients was 52 years; 66% were men, nearly 33% had Revised ISS III disease; almost 16% had high-risk cytogenetics and 23% underwent transplant in second remission after salvage therapy for relapse. A total of 194 patients (59.5%) received induction with two novel agents (thalidomide/dexamethasone, n = 95; lenalidomide/dexamethasone, n = 63; bortezomib/dexamethasone, n = 36) and 132 (40.5%) received three drugs (bortezomib/lenalidomide/dexamethasone, n = 53; bortezomib/liposomal doxorubicin/dexamethasone, n = 42; bortezomib/thalidomide/dexamethasone, n = 31; other n = 3).
Outcomes favorable
After transplant 227 (69.8%) patients achieved a complete response; 48 (14.7%) had a very good partial response, 32 (9.8%) had a partial response, and 9 (2.8%) patients had stable disease. Ten (3.1%) patients died of transplant-related complications (before day 100). Triplet induction beat doublet with regards to early response (95.4% vs. 84.02% [doublets], P < .003), stem cell mobilization (88.6% vs. 76.8%, P < .005) and lower day-100 transplant-related mortality (P < .001), However, at a median follow-up of 62.5 months, the median overall response rate (97.5 months triplet vs. 100.0 months doublet) and the median progression free survival (54.5 months vs. 57 months) were not statistically different between the two induction-treatment groups.
Patients who had undergone transplant in a recent period (2016-18) had a better outcome, compared with initial years, which possibly reflects a combined effect of learning curve, use of triplets, and gradual reduction in day-100 mortality, the authors stated.
“Whether newer regimens incorporating monoclonal antibodies (associated with higher [complete response] rate and [minimal residual disease] negativity) would result in further improvement in survival, needs to be determined in future studies,” the researchers concluded.
The authors reported that they had no conflicts.
SOURCE: Kumar L et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 18. doi: 10.1016/j.clml.2020.08.021.
For patients with multiple myeloma, triplet induction with novel agents beat doublet with regards to early results, according to Lalit Kumar, MD, and colleagues at the All India Institute of Medical sciences Myeloma Group, New Delhi.
The study analyzed 326 multiple myeloma patients who received high-dose, novel agent–based induction therapy prior to autologous stem cell transplant (ASCT) at a single institution, according to a report published in Clinical Lymphoma, Myeloma and Leukemia.
Between January 2005 and December 2018, 326 consecutive patients underwent high-dose chemotherapy and autologous stem cell transplant. The median age of the patients was 52 years; 66% were men, nearly 33% had Revised ISS III disease; almost 16% had high-risk cytogenetics and 23% underwent transplant in second remission after salvage therapy for relapse. A total of 194 patients (59.5%) received induction with two novel agents (thalidomide/dexamethasone, n = 95; lenalidomide/dexamethasone, n = 63; bortezomib/dexamethasone, n = 36) and 132 (40.5%) received three drugs (bortezomib/lenalidomide/dexamethasone, n = 53; bortezomib/liposomal doxorubicin/dexamethasone, n = 42; bortezomib/thalidomide/dexamethasone, n = 31; other n = 3).
Outcomes favorable
After transplant 227 (69.8%) patients achieved a complete response; 48 (14.7%) had a very good partial response, 32 (9.8%) had a partial response, and 9 (2.8%) patients had stable disease. Ten (3.1%) patients died of transplant-related complications (before day 100). Triplet induction beat doublet with regards to early response (95.4% vs. 84.02% [doublets], P < .003), stem cell mobilization (88.6% vs. 76.8%, P < .005) and lower day-100 transplant-related mortality (P < .001), However, at a median follow-up of 62.5 months, the median overall response rate (97.5 months triplet vs. 100.0 months doublet) and the median progression free survival (54.5 months vs. 57 months) were not statistically different between the two induction-treatment groups.
Patients who had undergone transplant in a recent period (2016-18) had a better outcome, compared with initial years, which possibly reflects a combined effect of learning curve, use of triplets, and gradual reduction in day-100 mortality, the authors stated.
“Whether newer regimens incorporating monoclonal antibodies (associated with higher [complete response] rate and [minimal residual disease] negativity) would result in further improvement in survival, needs to be determined in future studies,” the researchers concluded.
The authors reported that they had no conflicts.
SOURCE: Kumar L et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 18. doi: 10.1016/j.clml.2020.08.021.
For patients with multiple myeloma, triplet induction with novel agents beat doublet with regards to early results, according to Lalit Kumar, MD, and colleagues at the All India Institute of Medical sciences Myeloma Group, New Delhi.
The study analyzed 326 multiple myeloma patients who received high-dose, novel agent–based induction therapy prior to autologous stem cell transplant (ASCT) at a single institution, according to a report published in Clinical Lymphoma, Myeloma and Leukemia.
Between January 2005 and December 2018, 326 consecutive patients underwent high-dose chemotherapy and autologous stem cell transplant. The median age of the patients was 52 years; 66% were men, nearly 33% had Revised ISS III disease; almost 16% had high-risk cytogenetics and 23% underwent transplant in second remission after salvage therapy for relapse. A total of 194 patients (59.5%) received induction with two novel agents (thalidomide/dexamethasone, n = 95; lenalidomide/dexamethasone, n = 63; bortezomib/dexamethasone, n = 36) and 132 (40.5%) received three drugs (bortezomib/lenalidomide/dexamethasone, n = 53; bortezomib/liposomal doxorubicin/dexamethasone, n = 42; bortezomib/thalidomide/dexamethasone, n = 31; other n = 3).
Outcomes favorable
After transplant 227 (69.8%) patients achieved a complete response; 48 (14.7%) had a very good partial response, 32 (9.8%) had a partial response, and 9 (2.8%) patients had stable disease. Ten (3.1%) patients died of transplant-related complications (before day 100). Triplet induction beat doublet with regards to early response (95.4% vs. 84.02% [doublets], P < .003), stem cell mobilization (88.6% vs. 76.8%, P < .005) and lower day-100 transplant-related mortality (P < .001), However, at a median follow-up of 62.5 months, the median overall response rate (97.5 months triplet vs. 100.0 months doublet) and the median progression free survival (54.5 months vs. 57 months) were not statistically different between the two induction-treatment groups.
Patients who had undergone transplant in a recent period (2016-18) had a better outcome, compared with initial years, which possibly reflects a combined effect of learning curve, use of triplets, and gradual reduction in day-100 mortality, the authors stated.
“Whether newer regimens incorporating monoclonal antibodies (associated with higher [complete response] rate and [minimal residual disease] negativity) would result in further improvement in survival, needs to be determined in future studies,” the researchers concluded.
The authors reported that they had no conflicts.
SOURCE: Kumar L et al. Clin Lymphoma Myeloma Leuk. 2020 Sep 18. doi: 10.1016/j.clml.2020.08.021.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Two new protein biomarkers may serve as prognostic indicators for outcomes in CLL
Two new protein biomarkers may serve as prognostic indicators for outcomes in chronic lymphocytic leukemia (CLL) patients, according to the results of a proteomic assessment of patients’ serum compared to their event-free survival (EFS).
The results were published in Experimental Hematology.
The study attempted to validate the prognostic ability of known proteomic markers measured pretreatment and to search for new proteomic markers that might be related to treatment response in CLL, according to Fatemeh Saberi Hosnijeh, MD, of Erasmus MC, University Medical Center, Rotterdam, The Netherlands, and colleagues.
Baseline serum samples were taken from 51 CLL patients who were then treated with chemoimmunotherapy. The samples were analyzed for 360 proteomic markers, and those results were compared with patient EFS.
Study subjects were selected from patients enrolled in the HOVON 109 clinical trial, a phase 1/2 trial designed to assess the efficacy and safety of first-line therapy involving chlorambucil, rituximab,and lenalidomide in elderly patients and young frail patients with advanced CLL.
The patients assessed comprised 30 men and 21 women, and the median EFS for all patients was 23 months (ranging from 1.25 to 60.9 months).
Promising biomarkers
The researchers found that patients who had high serum levels of the proteins sCD23 (P = .026), sCD27 (P = .04), the serine peptidase inhibitor SPINT1 (P = .001), and the surface antigen protein LY9 (P = .0003) had a shorter EFS than those with marker levels below the median.
“Taken together, our results validate the prognostic impact of sCD23 and highlight SPINT1 and LY9 as possible promising markers for treatment response in CLL patients,” the researchers stated.
“Despite the relatively small number of available cases, which had an impact on statistical power, our pilot study identified SPINT1 and LY9 as promising independent prognostic proteomic markers next to sCD23 and sCD27 in patients treated for CLL. Further studies with larger sample sizes are required to validate these results,” the researchers concluded.
This research was supported by a grant from Gilead Sciences and an EU TRANSCAN/Dutch Cancer Society grant. The authors declared that they had no conflicts of interest.
SOURCE: Hosnijeh FS et al. Exp Hematol. 2020;89:55-60.
Two new protein biomarkers may serve as prognostic indicators for outcomes in chronic lymphocytic leukemia (CLL) patients, according to the results of a proteomic assessment of patients’ serum compared to their event-free survival (EFS).
The results were published in Experimental Hematology.
The study attempted to validate the prognostic ability of known proteomic markers measured pretreatment and to search for new proteomic markers that might be related to treatment response in CLL, according to Fatemeh Saberi Hosnijeh, MD, of Erasmus MC, University Medical Center, Rotterdam, The Netherlands, and colleagues.
Baseline serum samples were taken from 51 CLL patients who were then treated with chemoimmunotherapy. The samples were analyzed for 360 proteomic markers, and those results were compared with patient EFS.
Study subjects were selected from patients enrolled in the HOVON 109 clinical trial, a phase 1/2 trial designed to assess the efficacy and safety of first-line therapy involving chlorambucil, rituximab,and lenalidomide in elderly patients and young frail patients with advanced CLL.
The patients assessed comprised 30 men and 21 women, and the median EFS for all patients was 23 months (ranging from 1.25 to 60.9 months).
Promising biomarkers
The researchers found that patients who had high serum levels of the proteins sCD23 (P = .026), sCD27 (P = .04), the serine peptidase inhibitor SPINT1 (P = .001), and the surface antigen protein LY9 (P = .0003) had a shorter EFS than those with marker levels below the median.
“Taken together, our results validate the prognostic impact of sCD23 and highlight SPINT1 and LY9 as possible promising markers for treatment response in CLL patients,” the researchers stated.
“Despite the relatively small number of available cases, which had an impact on statistical power, our pilot study identified SPINT1 and LY9 as promising independent prognostic proteomic markers next to sCD23 and sCD27 in patients treated for CLL. Further studies with larger sample sizes are required to validate these results,” the researchers concluded.
This research was supported by a grant from Gilead Sciences and an EU TRANSCAN/Dutch Cancer Society grant. The authors declared that they had no conflicts of interest.
SOURCE: Hosnijeh FS et al. Exp Hematol. 2020;89:55-60.
Two new protein biomarkers may serve as prognostic indicators for outcomes in chronic lymphocytic leukemia (CLL) patients, according to the results of a proteomic assessment of patients’ serum compared to their event-free survival (EFS).
The results were published in Experimental Hematology.
The study attempted to validate the prognostic ability of known proteomic markers measured pretreatment and to search for new proteomic markers that might be related to treatment response in CLL, according to Fatemeh Saberi Hosnijeh, MD, of Erasmus MC, University Medical Center, Rotterdam, The Netherlands, and colleagues.
Baseline serum samples were taken from 51 CLL patients who were then treated with chemoimmunotherapy. The samples were analyzed for 360 proteomic markers, and those results were compared with patient EFS.
Study subjects were selected from patients enrolled in the HOVON 109 clinical trial, a phase 1/2 trial designed to assess the efficacy and safety of first-line therapy involving chlorambucil, rituximab,and lenalidomide in elderly patients and young frail patients with advanced CLL.
The patients assessed comprised 30 men and 21 women, and the median EFS for all patients was 23 months (ranging from 1.25 to 60.9 months).
Promising biomarkers
The researchers found that patients who had high serum levels of the proteins sCD23 (P = .026), sCD27 (P = .04), the serine peptidase inhibitor SPINT1 (P = .001), and the surface antigen protein LY9 (P = .0003) had a shorter EFS than those with marker levels below the median.
“Taken together, our results validate the prognostic impact of sCD23 and highlight SPINT1 and LY9 as possible promising markers for treatment response in CLL patients,” the researchers stated.
“Despite the relatively small number of available cases, which had an impact on statistical power, our pilot study identified SPINT1 and LY9 as promising independent prognostic proteomic markers next to sCD23 and sCD27 in patients treated for CLL. Further studies with larger sample sizes are required to validate these results,” the researchers concluded.
This research was supported by a grant from Gilead Sciences and an EU TRANSCAN/Dutch Cancer Society grant. The authors declared that they had no conflicts of interest.
SOURCE: Hosnijeh FS et al. Exp Hematol. 2020;89:55-60.
FROM EXPERIMENTAL HEMATOLOGY
Low VWF levels or blood group O not linked to intracerebral hemorrhage risk
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
FROM THROMBOSIS RESEARCH
Statins linked to improved survival in multiple myeloma
Statin use was associated with an overall reduction of the risk of death in multiple myeloma (MM) patients, according to a report published in Clinical Lymphoma, Myeloma & Leukemia.
Statins maintained their benefit in patients with multiple myeloma treated with modern-day chemotherapy regimens based on novel agents, but the benefit is less pronounced, reported Amber Afzal, MD, Washington University, St Louis, and colleagues.
Dr. Afzal and colleagues assessed results from 5,922 patients who were diagnosed with multiple myeloma within the study period between 2007 and 2013. The association of statins with mortality in patients with MM was determined using multivariate Cox proportional hazards regression analysis, and a subanalysis was also performed to investigate the effect of statins on mortality in those patients treated with novel agents.
Mortality reduction seen
The study found that the use of statins was associated with a 21% reduction in risk of death (adjusted hazard ratio,] 0.79; 95% confidence interval, 0.74-0.84) among all patients with MM. Among the patents treated with novel agents (n = 3,603), statins reduced mortality by 10% (aHR, 0.90; 95% CI, 0.83-0.98).
“Our current study is the first one to support the survival benefit of statins in patients with myeloma treated with modern-day regimens based on novel agents, although it appears the benefit may not be as pronounced. Therefore, as myeloma regimens become more effective, the benefits of statins may diminish,” the researchers concluded.
The authors reported that they had no relevant disclosures.
SOURCE: Afzal A et al. Clin Lymphoma Myeloma Leuk. 2020 Jul 16. doi: 10.1016/j.clml.2020.07.003.
Statin use was associated with an overall reduction of the risk of death in multiple myeloma (MM) patients, according to a report published in Clinical Lymphoma, Myeloma & Leukemia.
Statins maintained their benefit in patients with multiple myeloma treated with modern-day chemotherapy regimens based on novel agents, but the benefit is less pronounced, reported Amber Afzal, MD, Washington University, St Louis, and colleagues.
Dr. Afzal and colleagues assessed results from 5,922 patients who were diagnosed with multiple myeloma within the study period between 2007 and 2013. The association of statins with mortality in patients with MM was determined using multivariate Cox proportional hazards regression analysis, and a subanalysis was also performed to investigate the effect of statins on mortality in those patients treated with novel agents.
Mortality reduction seen
The study found that the use of statins was associated with a 21% reduction in risk of death (adjusted hazard ratio,] 0.79; 95% confidence interval, 0.74-0.84) among all patients with MM. Among the patents treated with novel agents (n = 3,603), statins reduced mortality by 10% (aHR, 0.90; 95% CI, 0.83-0.98).
“Our current study is the first one to support the survival benefit of statins in patients with myeloma treated with modern-day regimens based on novel agents, although it appears the benefit may not be as pronounced. Therefore, as myeloma regimens become more effective, the benefits of statins may diminish,” the researchers concluded.
The authors reported that they had no relevant disclosures.
SOURCE: Afzal A et al. Clin Lymphoma Myeloma Leuk. 2020 Jul 16. doi: 10.1016/j.clml.2020.07.003.
Statin use was associated with an overall reduction of the risk of death in multiple myeloma (MM) patients, according to a report published in Clinical Lymphoma, Myeloma & Leukemia.
Statins maintained their benefit in patients with multiple myeloma treated with modern-day chemotherapy regimens based on novel agents, but the benefit is less pronounced, reported Amber Afzal, MD, Washington University, St Louis, and colleagues.
Dr. Afzal and colleagues assessed results from 5,922 patients who were diagnosed with multiple myeloma within the study period between 2007 and 2013. The association of statins with mortality in patients with MM was determined using multivariate Cox proportional hazards regression analysis, and a subanalysis was also performed to investigate the effect of statins on mortality in those patients treated with novel agents.
Mortality reduction seen
The study found that the use of statins was associated with a 21% reduction in risk of death (adjusted hazard ratio,] 0.79; 95% confidence interval, 0.74-0.84) among all patients with MM. Among the patents treated with novel agents (n = 3,603), statins reduced mortality by 10% (aHR, 0.90; 95% CI, 0.83-0.98).
“Our current study is the first one to support the survival benefit of statins in patients with myeloma treated with modern-day regimens based on novel agents, although it appears the benefit may not be as pronounced. Therefore, as myeloma regimens become more effective, the benefits of statins may diminish,” the researchers concluded.
The authors reported that they had no relevant disclosures.
SOURCE: Afzal A et al. Clin Lymphoma Myeloma Leuk. 2020 Jul 16. doi: 10.1016/j.clml.2020.07.003.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Oxidative stress linked to cytogenetic abnormalities in CLL
Oxidative stress may play a role in pathogenesis of B-cell chronic lymphocytic leukemia (B-CLL), according to the results of a biochemical and cytogenetic study of patients published online in Experimental and Molecular Pathology.
The study evaluated the serum levels of oxidative stress biomarkers [conjugated dienes (CD), malondialdehyde (MDA), and nitrite levels] and the levels of antioxidant biomarkers [ceruloplasmin (CP) and glutathione peroxidase (GPx)] in 64 B-CLL patients. The relationship between these biomarkers and the presence of cytogenetic abnormalities was examined, according to Tatiana Zhevak, MD, of Sechenov First Moscow (Russia) State Medical University, and colleagues.
Cytogenetic abnormalities have previously been determined to be linked to a poorer prognosis in CLL patients, and factors that increase the frequency of CA have been shown to increase the risk of rapid tumor progression, Dr. Zhevak and her colleagues stated.
Oxidative stress connection
Enhanced oxidative stress was detected in B-CLL patients as shown by their increased levels of serum CD, MDA, and nitrite, as well as a demonstrated imbalance in the antioxidant defense system as shown by an increased serum CP level and decreased serum GPx activity, according to the researchers.
In addition, these metabolic changes were found to be greater in those patients whose lymphocytes harbored specific cytogenetic abnormalities, and could be predicted by the serum levels of CD. Specifically, the odds of harboring a cytogenetic abnormality increased by a factor of 1.88 (P = .004) for every one-unit increase in serum CD level (mcmol/L), according to the authors.
“Collectively, the results support our hypothesis that oxidative stress and resulting lipid peroxidation play a role in pathogenesis of B-CLL and provide a rational basis for the use of agents regulating the pro-oxidant and antioxidant activity in the treatment of B-CLL patients,” the researchers concluded.
The research was unsponsored and the authors reported having no conflicts.
SOURCE: Zhevak T et al. Exp Mol Patholo. 2020 Oct;16:104524 doi: 10.1016/j.yexmp.2020.104524.
Oxidative stress may play a role in pathogenesis of B-cell chronic lymphocytic leukemia (B-CLL), according to the results of a biochemical and cytogenetic study of patients published online in Experimental and Molecular Pathology.
The study evaluated the serum levels of oxidative stress biomarkers [conjugated dienes (CD), malondialdehyde (MDA), and nitrite levels] and the levels of antioxidant biomarkers [ceruloplasmin (CP) and glutathione peroxidase (GPx)] in 64 B-CLL patients. The relationship between these biomarkers and the presence of cytogenetic abnormalities was examined, according to Tatiana Zhevak, MD, of Sechenov First Moscow (Russia) State Medical University, and colleagues.
Cytogenetic abnormalities have previously been determined to be linked to a poorer prognosis in CLL patients, and factors that increase the frequency of CA have been shown to increase the risk of rapid tumor progression, Dr. Zhevak and her colleagues stated.
Oxidative stress connection
Enhanced oxidative stress was detected in B-CLL patients as shown by their increased levels of serum CD, MDA, and nitrite, as well as a demonstrated imbalance in the antioxidant defense system as shown by an increased serum CP level and decreased serum GPx activity, according to the researchers.
In addition, these metabolic changes were found to be greater in those patients whose lymphocytes harbored specific cytogenetic abnormalities, and could be predicted by the serum levels of CD. Specifically, the odds of harboring a cytogenetic abnormality increased by a factor of 1.88 (P = .004) for every one-unit increase in serum CD level (mcmol/L), according to the authors.
“Collectively, the results support our hypothesis that oxidative stress and resulting lipid peroxidation play a role in pathogenesis of B-CLL and provide a rational basis for the use of agents regulating the pro-oxidant and antioxidant activity in the treatment of B-CLL patients,” the researchers concluded.
The research was unsponsored and the authors reported having no conflicts.
SOURCE: Zhevak T et al. Exp Mol Patholo. 2020 Oct;16:104524 doi: 10.1016/j.yexmp.2020.104524.
Oxidative stress may play a role in pathogenesis of B-cell chronic lymphocytic leukemia (B-CLL), according to the results of a biochemical and cytogenetic study of patients published online in Experimental and Molecular Pathology.
The study evaluated the serum levels of oxidative stress biomarkers [conjugated dienes (CD), malondialdehyde (MDA), and nitrite levels] and the levels of antioxidant biomarkers [ceruloplasmin (CP) and glutathione peroxidase (GPx)] in 64 B-CLL patients. The relationship between these biomarkers and the presence of cytogenetic abnormalities was examined, according to Tatiana Zhevak, MD, of Sechenov First Moscow (Russia) State Medical University, and colleagues.
Cytogenetic abnormalities have previously been determined to be linked to a poorer prognosis in CLL patients, and factors that increase the frequency of CA have been shown to increase the risk of rapid tumor progression, Dr. Zhevak and her colleagues stated.
Oxidative stress connection
Enhanced oxidative stress was detected in B-CLL patients as shown by their increased levels of serum CD, MDA, and nitrite, as well as a demonstrated imbalance in the antioxidant defense system as shown by an increased serum CP level and decreased serum GPx activity, according to the researchers.
In addition, these metabolic changes were found to be greater in those patients whose lymphocytes harbored specific cytogenetic abnormalities, and could be predicted by the serum levels of CD. Specifically, the odds of harboring a cytogenetic abnormality increased by a factor of 1.88 (P = .004) for every one-unit increase in serum CD level (mcmol/L), according to the authors.
“Collectively, the results support our hypothesis that oxidative stress and resulting lipid peroxidation play a role in pathogenesis of B-CLL and provide a rational basis for the use of agents regulating the pro-oxidant and antioxidant activity in the treatment of B-CLL patients,” the researchers concluded.
The research was unsponsored and the authors reported having no conflicts.
SOURCE: Zhevak T et al. Exp Mol Patholo. 2020 Oct;16:104524 doi: 10.1016/j.yexmp.2020.104524.
FROM Experimental and Molecular Pathology