User login
Progress still needed for pregnant and postpartum gastroenterologists
Despite increasing numbers joining the field, women remain a minority group in gastroenterology, where they constitute only 18% of these physicians.1 Additionally, women continue to be underrepresented among senior faculty and in leadership roles in both academic and private practice settings.2 While women now make up a majority of medical school matriculants3,4 women trainees are frequently dissuaded from pursuing specialty fellowships following residency, particularly in procedurally based fields like gastroenterology, because of perceived incompatibility with childbearing and child-rearing.5-8 For many who choose to enter the field despite these challenges, gastroenterology training and early practice often coincide with childbearing years.910 These structural impediments may contribute to the “leaky pipeline” and female physician attrition during the first decade of independent practice after fellowship.11-13 Urgent changes are needed in order to retain and support clinicians and physician-scientists through this period so that they, their offspring, their patients, and the field are able to thrive.
Fertility and pregnancy
The decision to have a child is a major milestone for many physicians and often occurs during gastroenterology training or early practice.10 Medical-training and early-career environments are not yet optimized to support women who become pregnant. At baseline, the formative years of a career are challenging ones, punctuated by long hours and both intellectually and emotionally demanding work. They are also often physically grueling, particularly while one is learning and becoming efficient in endoscopy. The ergonomics in the endoscopy suite (as in other areas of medicine) are not optimized for physicians of shorter stature, smaller hand sizes, and those who may have difficulty pushing a several-hundred-pound endoscopy cart bedside, all of which contribute to increased injury risk for female proceduralists.7,14-16 Methods to reduce endoscopic injuries in pregnant endoscopists have not yet been studied. Additionally, the existence of maternity and gender bias has been well-documented, in our field and beyond.17-20 Not surprisingly, women in gastroenterology commonly report delayed childbearing, with expected consequences, including increased infertility rates, compared with nonphysician peers.21 After 5 and 10 years as attendings, female gastroenterologists continue to report fewer children than male colleagues.22,23 Once pregnant, there are a number of field-specific challenges to navigate. These include decisions about the safety of performing procedures involving fluoroscopy or high infectious risk, particularly early in pregnancy when organogenesis occurs.7,24 Additionally, engaging in appropriate obstetric care can be challenging given the need for regular physician and ultrasound appointments.
Simple, cost-efficient interventions may be effective in decreasing infertility rates, pregnancy loss, and poor physician experiences during pregnancy. For one, all gastroenterology divisions could craft written policies that include a no-tolerance approach to expressions of maternity bias against pregnant or postpartum trainees and faculty.12,25 Additionally, ergonomic improvements, such as standing pads, dial extenders, and adjusted screen heights may decrease injury rates and increase comfort for female endoscopists.26,27 There should also be a no-penalty, no-questions-asked approach for any female endoscopist who defers performance of an obstetrically high-risk procedure to a nonpregnant colleague. Additionally, pregnant gastroenterologists should be supported in obtaining high-quality obstetric care. At an individual level, nonpregnant gastroenterologists, and particularly male allies, can support pregnant colleagues by agreeing to perform higher-risk procedures, stepping in if a fellow is unable to perform endoscopy because of pregnancy, and by offering to push the endoscopy cart on behalf of a pregnant colleague to bedside, if necessary.10,28
Parental leave
Following delivery, parental leave presents an additional challenge for the physician parent. Paid maternal leave has been associated with improved child and maternal outcomes and is widely available to physicians outside the United States.29,30 At present, duration of leave varies significantly by career stage (fellows versus attending), practice setting (academic center versus private practice), and geographic location. The American Academy of Pediatrics recommends a minimum of 12 weeks of leave.31 This length has been associated with lower rates of postpartum depression and higher rates of sustained breastfeeding, with subsequent improved health outcomes for mother and child.32-34 An increasing number of states have passed laws mandating minimum paid and unpaid parental leave time (for example, in Massachusetts, gastroenterology trainees and faculty are afforded 12 weeks of leave, in accordance with state law).35 Recent changes to board eligibility and training requirements via the American Board of Medical Specialties and the American Council for Graduate Medical Education now provide 6 weeks for parental leave. This is an improvement over prior policies which rendered many physician-parents board-ineligible if they took more than 4 weeks of leave, although it must be noted that even the revised policies allow for less time than either that of Obstetricians and Gynecologists or than the American Academy of Pediatrics recommends.
Our data, presented at the 2021 ACG conference, suggest that many trainees report receiving 4 weeks or less of parental leave, despite the ACGME and ABMS policies described above. We also found that physicians were frequently not aware of their institution or division leave policies.10 Ideally, all gastroenterology divisions in the United States would follow the recommended leave duration set forth by the medical societies of specialties that care for pregnant and postpartum mothers and their infants. Additionally, the impact of leave time on graduation and board eligibility, as well as academic and practice promotion, should be made clear at the time of leave and should minimize adverse consequences for the careers of pregnant and postpartum gastroenterologists. Gastroenterology trainees and faculty should be educated in the existence and details of their institution or practice policies, and these policies should be made readily available to all physicians and administrators.
Postpartum period
The transition back to work is a challenging one for mothers in all fields of medicine, particularly for those returning to procedurally based subspecialties such as gastroenterology. This is especially true for trainees and faculty who have returned to work sooner than the recommended 12 weeks and for those who are post cesarean section, for whom physical healing may not be complete. Long days performing endoscopy may be physically challenging or impossible for some women during the postpartum period. Additionally, expressing breast milk, a metabolically intensive activity, also necessitates time, space, and privacy to perform and is frequently made more difficult by insufficient lactation accommodations. The COVID-19 pandemic has increased logistic challenges for lactating mothers, because of the need for well-ventilated lactation spaces to minimize infectious risk.19 Our colleagues have reported pumping in their vehicles, in supply closets, and in spaces that require so much travel time (in addition to time required to express milk, store milk, and clean pump equipment) that the practice was unsustainable, and the physician stopped breastfeeding prematurely.36
The benefits of breastfeeding for mother and infant are well-established, and exclusive breastfeeding for the first 6 months of life is supported by the American College of Obstetricians and Gynecologists, whose position statement reads as follows: “Policies that protect the right of a woman and her child to breastfeed ... and that accommodate milk expression, such as ... paid maternity leave, on-site childcare, break time for expressing milk, and a clean, private location for expressing milk, are essential to sustaining breastfeeding.”37 We would add to these recommendations provision of dedicated milk storage space and establishment of clear, supportive policies that allow lactating physicians to breastfeed and express breast milk if they choose without career penalty. Several institutions offer scheduled protected clinical time and modified work relative value units (RVU) for lactating physicians, such that returning parents can have protected time for expressing breast milk and still meet RVU targets.38 Additionally, many academic institutions offer productivity adjustments for tenure-track faculty who have recently had children.
Creating a more supportive environment for women gastroenterologists who desire children allows the field to be more representative of our patient population and has been shown to positively impact outcomes from improved colorectal cancer screening rates to more guideline-directed informed consent conversations.39-41 Gastroenterology should comprise a physician workforce predicated on clinical and research excellence alone and should not require its practitioners to delay or abstain from pregnancy and child rearing. Robust, clear, and generous parental leave and postpartum accommodations will allow the field to retain and promote talented physicians, who will then contribute to the betterment of patients and the field over decades.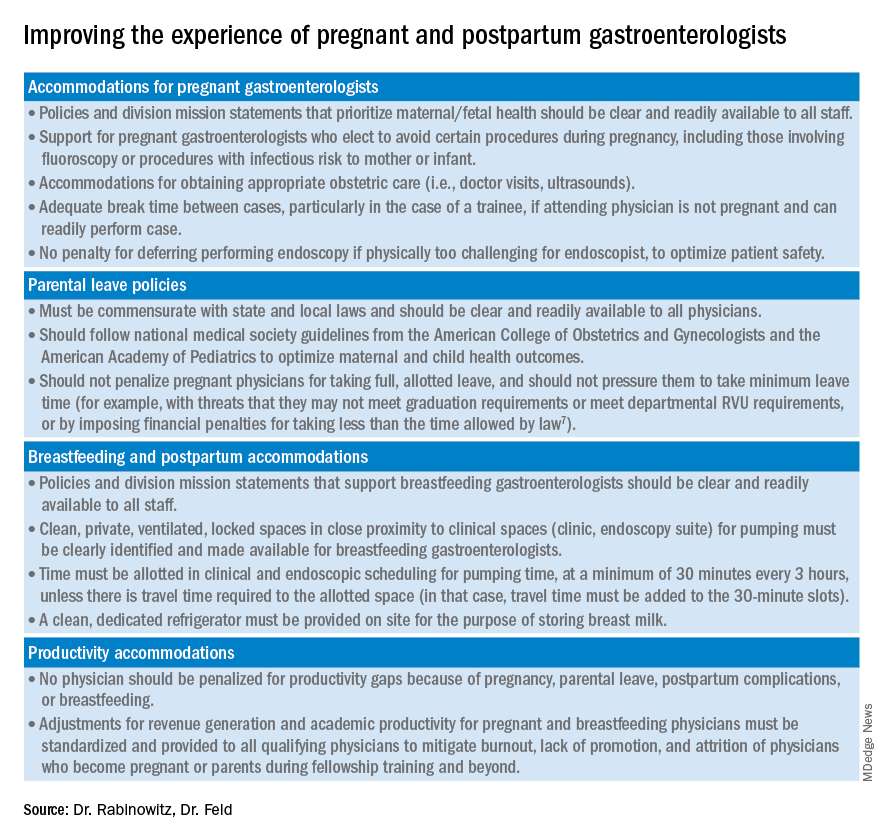
Dr. Rabinowitz is a faculty member in the department of medicine and division of gastroenterology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston. Dr. Feld is a transplant hepatology fellow, division of gastroenterology, department of medicine, University of Washington, Seattle. Dr. Rabinowitz and Dr. Feld have no conflicts of interest to disclose.
References
1. AAMC. Diversity in Medicine: Facts and Figures 2019. 2018.
2. Colleges AoAM. The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership, 2015-2016. 2016. www.aamc.org/download/481206/data/2015table11.pdf.
3. AAMC. Table B-3: Total U.S. Medical School Enrollment by Race/Ethnicity and Sex, 2014-2015 through 2018-2019, 2019.
4. Rabinowitz LG. Recognizing blind spots – a remedy for gender bias in medicine? (N Engl. J Med. 2018; 378[24]: 2253-5).
5. Douglas PS et al. Career preferences and perceptions of cardiology among US internal medicine trainees: Factors influencing cardiology career choice. JAMA Cardiol 2018; 3(8):682-91.
6. Stack SW et al. Childbearing decisions in residency: A multicenter survey of female residents. Acad Med 2020;95(10):1550-7.
7. David YN et al. Pregnancy and the working gastroenterologist: Perceptions, realities, and systemic challenges. Gastroenterology 2021;161(3):756-60.
8. Rembacken BJ et al. Barriers and bias standing in the way of female trainees wanting to learn advanced endoscopy. United European Gastroenterol J. 2019;7(8):1141-5.
9. Arlow FL et al. Gastroenterology training and career choices: A prospective longitudinal study of the impact of gender and of managed care. Am J Gastroenterol. 2002;97(2):459-69.
10. Feld L et al. Parental leave for gastroenterology fellows: A national survey of current fellows. Am J Gastroenterol. 2021;116:S611-2.
11. Rabinowitz LG et al. Addressing gender in gastroenterology: opportunities for change. Gastrointest Endosc. 2020;91(1):155-61.
12. Feld LD. Baby steps in the right direction: Toward a parental leave policy for gastroenterology fellows. Am J Gastroenterol. 2021;116(3):505-8.
13. Feld LD. Interviewing for two. Am J Gastroenterol. 2020;116(3):445-6
14. Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93(5):1047-56.e5.
15. Harvin G. Review of musculoskeletal injuries and prevention in the endoscopy practitioner. J Clin Gastroenterol. 2014;48(7):590-4.
16. LabX Oecs. www.labx.com/product/endoscopy-cart (accessed 2021 Nov 19.
17. Heilman ME and Okimoto TG. Motherhood: A potential source of bias in employment decisions. J Appl Psychol. 2008;93(1):189-98.
18. Robinson K et al. Racism, bias, and discrimination as modifiable barriers to breastfeeding for African American women: A scoping review of the literature. J Midwifery Womens Health. 2019;64(6):734-42.
19. Rabinowitz LG and Rabinowitz DG. Women on the Frontline: A Changed Workforce and the Fight Against COVID-19. Acad Med. 2021 Jun 1;96(6):808-12.
20. Rabinowitz LG et al. Gender in the endoscopy suite. Lancet Gastroenterol Hepatol. 2020 Dec;5(12):1032-4.
21. Stentz NC et al. Fertility and childbearing among American female physicians. J Womens Health. 2016; 25(10):1059-65.
22. Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol. 2005;100(2):259-64.
23. Singh A et al. Women in gastroenterology committee of American College of G. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol. 2008;103(7):1589-95.
24. Krueger KJ and Hoffman BJ. Radiation exposure during gastroenterologic fluoroscopy: Risk assessment for pregnant workers. Am J Gastroenterol. 1992;87(4):429-31.
25. Krause ML et al. Impact of pregnancy and gender on internal medicine resident evaluations: A retrospective cohort study. J Gen Intern Med. 2017;32(6):648-53.
26. Pawa S et al. Are all endoscopy-related musculoskeletal injuries created equal? Results of a national gender-based survey. Am J Gastroenterol. 2021;116(3):530-8.
27. David YN et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Am J Gastroenterol. 2021;116(3):539-50.
28. Bilal M et al. The need for allyship in achieving gender equity in gastroenterology. Am J Gastroenterol. 2021 Oct 19. doi: 10.14309/ajg.0000000000001508. Online ahead of print.
29. Jou J et al. Paid maternity leave in the United States: Associations with maternal and infant health. Matern Child Health J. 2018;22(2):216-25.
30. Aitken Z et al. The maternal health outcomes of paid maternity leave: A systematic review. Soc Sci Med. 2015;130:32-41.
31. Dodson NA and Talib HJ. Paid parental leave for mothers and fathers can improve physician wellness. AAP News. 2020 Jul 1. https://publications.aap.org/aapnews/news/12432.
32. Kornfeind KR and Sipsma HL. Exploring the link between maternity leave and postpartum depression. Womens Health Issues 2018;28(4):321-6.
33. Navarro-Rosenblatt D and Garmendia ML. Maternity leave and its impact on breastfeeding: A review of the literature. Breastfeed Med 2018;13(9):589-97.
34. Stack SW et al. Maternity leave in residency: A multicenter study of determinants and wellness outcomes. Acad Med. 2019;94(11):1738-45.
35. Mass.gov. Paid Family and Medical Leave Information for Massachusetts Employers. 2020.
36. Ares Segura S et al. en representacion del Comite de Lactancia Materna de la Asociacion Espanola de P. [The importance of maternal nutrition during breastfeeding: Do breastfeeding mothers need nutritional supplements?]. An Pediatr. (Barc) 2016;84(6):347 e1-7.
37. American College of Obstetricians and Gynecologists, Committee on Obstetric Practice. Committee Opinion No. 658: Optimizing Support for Breastfeeding as Part of Obstetric Practice. Obstet Gynecol. 2016;127(2):e86-92.
38. Porter KK et al. A lactation credit model to support breastfeeding in radiology: The new gold standard to support “liquid gold.” Clin Imaging 2021;80:16-8.
39. Davis J et al. Clinical practice patterns suggest female patients prefer female endoscopists. Dig Dis Sci. 2015;60(10):3149-50.
40. Menees SB et al. Women patients’ preference for women physicians is a barrier to colon cancer screening. Gastrointest Endosc. 2005;62(2):219-23.
41. Feld LD et al. Management of code status in the periendoscopic period: A national survey of current practices and beliefs of U.S. gastroenterologists. Gastrointest Endosc. 2021;94(1):172-7.e2.
Despite increasing numbers joining the field, women remain a minority group in gastroenterology, where they constitute only 18% of these physicians.1 Additionally, women continue to be underrepresented among senior faculty and in leadership roles in both academic and private practice settings.2 While women now make up a majority of medical school matriculants3,4 women trainees are frequently dissuaded from pursuing specialty fellowships following residency, particularly in procedurally based fields like gastroenterology, because of perceived incompatibility with childbearing and child-rearing.5-8 For many who choose to enter the field despite these challenges, gastroenterology training and early practice often coincide with childbearing years.910 These structural impediments may contribute to the “leaky pipeline” and female physician attrition during the first decade of independent practice after fellowship.11-13 Urgent changes are needed in order to retain and support clinicians and physician-scientists through this period so that they, their offspring, their patients, and the field are able to thrive.
Fertility and pregnancy
The decision to have a child is a major milestone for many physicians and often occurs during gastroenterology training or early practice.10 Medical-training and early-career environments are not yet optimized to support women who become pregnant. At baseline, the formative years of a career are challenging ones, punctuated by long hours and both intellectually and emotionally demanding work. They are also often physically grueling, particularly while one is learning and becoming efficient in endoscopy. The ergonomics in the endoscopy suite (as in other areas of medicine) are not optimized for physicians of shorter stature, smaller hand sizes, and those who may have difficulty pushing a several-hundred-pound endoscopy cart bedside, all of which contribute to increased injury risk for female proceduralists.7,14-16 Methods to reduce endoscopic injuries in pregnant endoscopists have not yet been studied. Additionally, the existence of maternity and gender bias has been well-documented, in our field and beyond.17-20 Not surprisingly, women in gastroenterology commonly report delayed childbearing, with expected consequences, including increased infertility rates, compared with nonphysician peers.21 After 5 and 10 years as attendings, female gastroenterologists continue to report fewer children than male colleagues.22,23 Once pregnant, there are a number of field-specific challenges to navigate. These include decisions about the safety of performing procedures involving fluoroscopy or high infectious risk, particularly early in pregnancy when organogenesis occurs.7,24 Additionally, engaging in appropriate obstetric care can be challenging given the need for regular physician and ultrasound appointments.
Simple, cost-efficient interventions may be effective in decreasing infertility rates, pregnancy loss, and poor physician experiences during pregnancy. For one, all gastroenterology divisions could craft written policies that include a no-tolerance approach to expressions of maternity bias against pregnant or postpartum trainees and faculty.12,25 Additionally, ergonomic improvements, such as standing pads, dial extenders, and adjusted screen heights may decrease injury rates and increase comfort for female endoscopists.26,27 There should also be a no-penalty, no-questions-asked approach for any female endoscopist who defers performance of an obstetrically high-risk procedure to a nonpregnant colleague. Additionally, pregnant gastroenterologists should be supported in obtaining high-quality obstetric care. At an individual level, nonpregnant gastroenterologists, and particularly male allies, can support pregnant colleagues by agreeing to perform higher-risk procedures, stepping in if a fellow is unable to perform endoscopy because of pregnancy, and by offering to push the endoscopy cart on behalf of a pregnant colleague to bedside, if necessary.10,28
Parental leave
Following delivery, parental leave presents an additional challenge for the physician parent. Paid maternal leave has been associated with improved child and maternal outcomes and is widely available to physicians outside the United States.29,30 At present, duration of leave varies significantly by career stage (fellows versus attending), practice setting (academic center versus private practice), and geographic location. The American Academy of Pediatrics recommends a minimum of 12 weeks of leave.31 This length has been associated with lower rates of postpartum depression and higher rates of sustained breastfeeding, with subsequent improved health outcomes for mother and child.32-34 An increasing number of states have passed laws mandating minimum paid and unpaid parental leave time (for example, in Massachusetts, gastroenterology trainees and faculty are afforded 12 weeks of leave, in accordance with state law).35 Recent changes to board eligibility and training requirements via the American Board of Medical Specialties and the American Council for Graduate Medical Education now provide 6 weeks for parental leave. This is an improvement over prior policies which rendered many physician-parents board-ineligible if they took more than 4 weeks of leave, although it must be noted that even the revised policies allow for less time than either that of Obstetricians and Gynecologists or than the American Academy of Pediatrics recommends.
Our data, presented at the 2021 ACG conference, suggest that many trainees report receiving 4 weeks or less of parental leave, despite the ACGME and ABMS policies described above. We also found that physicians were frequently not aware of their institution or division leave policies.10 Ideally, all gastroenterology divisions in the United States would follow the recommended leave duration set forth by the medical societies of specialties that care for pregnant and postpartum mothers and their infants. Additionally, the impact of leave time on graduation and board eligibility, as well as academic and practice promotion, should be made clear at the time of leave and should minimize adverse consequences for the careers of pregnant and postpartum gastroenterologists. Gastroenterology trainees and faculty should be educated in the existence and details of their institution or practice policies, and these policies should be made readily available to all physicians and administrators.
Postpartum period
The transition back to work is a challenging one for mothers in all fields of medicine, particularly for those returning to procedurally based subspecialties such as gastroenterology. This is especially true for trainees and faculty who have returned to work sooner than the recommended 12 weeks and for those who are post cesarean section, for whom physical healing may not be complete. Long days performing endoscopy may be physically challenging or impossible for some women during the postpartum period. Additionally, expressing breast milk, a metabolically intensive activity, also necessitates time, space, and privacy to perform and is frequently made more difficult by insufficient lactation accommodations. The COVID-19 pandemic has increased logistic challenges for lactating mothers, because of the need for well-ventilated lactation spaces to minimize infectious risk.19 Our colleagues have reported pumping in their vehicles, in supply closets, and in spaces that require so much travel time (in addition to time required to express milk, store milk, and clean pump equipment) that the practice was unsustainable, and the physician stopped breastfeeding prematurely.36
The benefits of breastfeeding for mother and infant are well-established, and exclusive breastfeeding for the first 6 months of life is supported by the American College of Obstetricians and Gynecologists, whose position statement reads as follows: “Policies that protect the right of a woman and her child to breastfeed ... and that accommodate milk expression, such as ... paid maternity leave, on-site childcare, break time for expressing milk, and a clean, private location for expressing milk, are essential to sustaining breastfeeding.”37 We would add to these recommendations provision of dedicated milk storage space and establishment of clear, supportive policies that allow lactating physicians to breastfeed and express breast milk if they choose without career penalty. Several institutions offer scheduled protected clinical time and modified work relative value units (RVU) for lactating physicians, such that returning parents can have protected time for expressing breast milk and still meet RVU targets.38 Additionally, many academic institutions offer productivity adjustments for tenure-track faculty who have recently had children.
Creating a more supportive environment for women gastroenterologists who desire children allows the field to be more representative of our patient population and has been shown to positively impact outcomes from improved colorectal cancer screening rates to more guideline-directed informed consent conversations.39-41 Gastroenterology should comprise a physician workforce predicated on clinical and research excellence alone and should not require its practitioners to delay or abstain from pregnancy and child rearing. Robust, clear, and generous parental leave and postpartum accommodations will allow the field to retain and promote talented physicians, who will then contribute to the betterment of patients and the field over decades.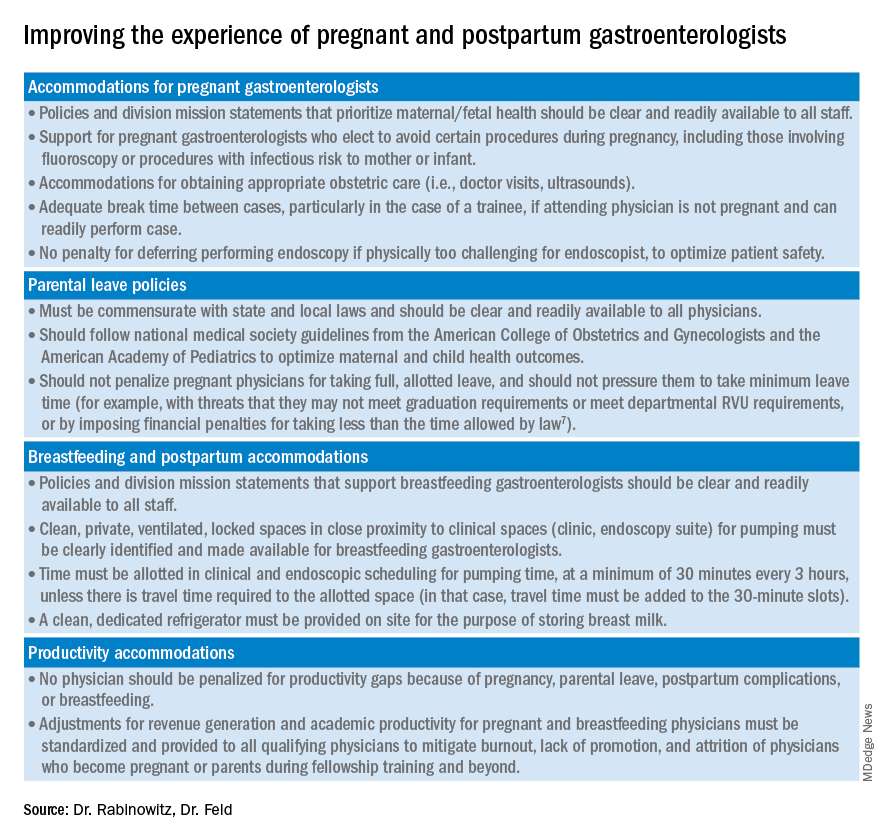
Dr. Rabinowitz is a faculty member in the department of medicine and division of gastroenterology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston. Dr. Feld is a transplant hepatology fellow, division of gastroenterology, department of medicine, University of Washington, Seattle. Dr. Rabinowitz and Dr. Feld have no conflicts of interest to disclose.
References
1. AAMC. Diversity in Medicine: Facts and Figures 2019. 2018.
2. Colleges AoAM. The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership, 2015-2016. 2016. www.aamc.org/download/481206/data/2015table11.pdf.
3. AAMC. Table B-3: Total U.S. Medical School Enrollment by Race/Ethnicity and Sex, 2014-2015 through 2018-2019, 2019.
4. Rabinowitz LG. Recognizing blind spots – a remedy for gender bias in medicine? (N Engl. J Med. 2018; 378[24]: 2253-5).
5. Douglas PS et al. Career preferences and perceptions of cardiology among US internal medicine trainees: Factors influencing cardiology career choice. JAMA Cardiol 2018; 3(8):682-91.
6. Stack SW et al. Childbearing decisions in residency: A multicenter survey of female residents. Acad Med 2020;95(10):1550-7.
7. David YN et al. Pregnancy and the working gastroenterologist: Perceptions, realities, and systemic challenges. Gastroenterology 2021;161(3):756-60.
8. Rembacken BJ et al. Barriers and bias standing in the way of female trainees wanting to learn advanced endoscopy. United European Gastroenterol J. 2019;7(8):1141-5.
9. Arlow FL et al. Gastroenterology training and career choices: A prospective longitudinal study of the impact of gender and of managed care. Am J Gastroenterol. 2002;97(2):459-69.
10. Feld L et al. Parental leave for gastroenterology fellows: A national survey of current fellows. Am J Gastroenterol. 2021;116:S611-2.
11. Rabinowitz LG et al. Addressing gender in gastroenterology: opportunities for change. Gastrointest Endosc. 2020;91(1):155-61.
12. Feld LD. Baby steps in the right direction: Toward a parental leave policy for gastroenterology fellows. Am J Gastroenterol. 2021;116(3):505-8.
13. Feld LD. Interviewing for two. Am J Gastroenterol. 2020;116(3):445-6
14. Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93(5):1047-56.e5.
15. Harvin G. Review of musculoskeletal injuries and prevention in the endoscopy practitioner. J Clin Gastroenterol. 2014;48(7):590-4.
16. LabX Oecs. www.labx.com/product/endoscopy-cart (accessed 2021 Nov 19.
17. Heilman ME and Okimoto TG. Motherhood: A potential source of bias in employment decisions. J Appl Psychol. 2008;93(1):189-98.
18. Robinson K et al. Racism, bias, and discrimination as modifiable barriers to breastfeeding for African American women: A scoping review of the literature. J Midwifery Womens Health. 2019;64(6):734-42.
19. Rabinowitz LG and Rabinowitz DG. Women on the Frontline: A Changed Workforce and the Fight Against COVID-19. Acad Med. 2021 Jun 1;96(6):808-12.
20. Rabinowitz LG et al. Gender in the endoscopy suite. Lancet Gastroenterol Hepatol. 2020 Dec;5(12):1032-4.
21. Stentz NC et al. Fertility and childbearing among American female physicians. J Womens Health. 2016; 25(10):1059-65.
22. Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol. 2005;100(2):259-64.
23. Singh A et al. Women in gastroenterology committee of American College of G. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol. 2008;103(7):1589-95.
24. Krueger KJ and Hoffman BJ. Radiation exposure during gastroenterologic fluoroscopy: Risk assessment for pregnant workers. Am J Gastroenterol. 1992;87(4):429-31.
25. Krause ML et al. Impact of pregnancy and gender on internal medicine resident evaluations: A retrospective cohort study. J Gen Intern Med. 2017;32(6):648-53.
26. Pawa S et al. Are all endoscopy-related musculoskeletal injuries created equal? Results of a national gender-based survey. Am J Gastroenterol. 2021;116(3):530-8.
27. David YN et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Am J Gastroenterol. 2021;116(3):539-50.
28. Bilal M et al. The need for allyship in achieving gender equity in gastroenterology. Am J Gastroenterol. 2021 Oct 19. doi: 10.14309/ajg.0000000000001508. Online ahead of print.
29. Jou J et al. Paid maternity leave in the United States: Associations with maternal and infant health. Matern Child Health J. 2018;22(2):216-25.
30. Aitken Z et al. The maternal health outcomes of paid maternity leave: A systematic review. Soc Sci Med. 2015;130:32-41.
31. Dodson NA and Talib HJ. Paid parental leave for mothers and fathers can improve physician wellness. AAP News. 2020 Jul 1. https://publications.aap.org/aapnews/news/12432.
32. Kornfeind KR and Sipsma HL. Exploring the link between maternity leave and postpartum depression. Womens Health Issues 2018;28(4):321-6.
33. Navarro-Rosenblatt D and Garmendia ML. Maternity leave and its impact on breastfeeding: A review of the literature. Breastfeed Med 2018;13(9):589-97.
34. Stack SW et al. Maternity leave in residency: A multicenter study of determinants and wellness outcomes. Acad Med. 2019;94(11):1738-45.
35. Mass.gov. Paid Family and Medical Leave Information for Massachusetts Employers. 2020.
36. Ares Segura S et al. en representacion del Comite de Lactancia Materna de la Asociacion Espanola de P. [The importance of maternal nutrition during breastfeeding: Do breastfeeding mothers need nutritional supplements?]. An Pediatr. (Barc) 2016;84(6):347 e1-7.
37. American College of Obstetricians and Gynecologists, Committee on Obstetric Practice. Committee Opinion No. 658: Optimizing Support for Breastfeeding as Part of Obstetric Practice. Obstet Gynecol. 2016;127(2):e86-92.
38. Porter KK et al. A lactation credit model to support breastfeeding in radiology: The new gold standard to support “liquid gold.” Clin Imaging 2021;80:16-8.
39. Davis J et al. Clinical practice patterns suggest female patients prefer female endoscopists. Dig Dis Sci. 2015;60(10):3149-50.
40. Menees SB et al. Women patients’ preference for women physicians is a barrier to colon cancer screening. Gastrointest Endosc. 2005;62(2):219-23.
41. Feld LD et al. Management of code status in the periendoscopic period: A national survey of current practices and beliefs of U.S. gastroenterologists. Gastrointest Endosc. 2021;94(1):172-7.e2.
Despite increasing numbers joining the field, women remain a minority group in gastroenterology, where they constitute only 18% of these physicians.1 Additionally, women continue to be underrepresented among senior faculty and in leadership roles in both academic and private practice settings.2 While women now make up a majority of medical school matriculants3,4 women trainees are frequently dissuaded from pursuing specialty fellowships following residency, particularly in procedurally based fields like gastroenterology, because of perceived incompatibility with childbearing and child-rearing.5-8 For many who choose to enter the field despite these challenges, gastroenterology training and early practice often coincide with childbearing years.910 These structural impediments may contribute to the “leaky pipeline” and female physician attrition during the first decade of independent practice after fellowship.11-13 Urgent changes are needed in order to retain and support clinicians and physician-scientists through this period so that they, their offspring, their patients, and the field are able to thrive.
Fertility and pregnancy
The decision to have a child is a major milestone for many physicians and often occurs during gastroenterology training or early practice.10 Medical-training and early-career environments are not yet optimized to support women who become pregnant. At baseline, the formative years of a career are challenging ones, punctuated by long hours and both intellectually and emotionally demanding work. They are also often physically grueling, particularly while one is learning and becoming efficient in endoscopy. The ergonomics in the endoscopy suite (as in other areas of medicine) are not optimized for physicians of shorter stature, smaller hand sizes, and those who may have difficulty pushing a several-hundred-pound endoscopy cart bedside, all of which contribute to increased injury risk for female proceduralists.7,14-16 Methods to reduce endoscopic injuries in pregnant endoscopists have not yet been studied. Additionally, the existence of maternity and gender bias has been well-documented, in our field and beyond.17-20 Not surprisingly, women in gastroenterology commonly report delayed childbearing, with expected consequences, including increased infertility rates, compared with nonphysician peers.21 After 5 and 10 years as attendings, female gastroenterologists continue to report fewer children than male colleagues.22,23 Once pregnant, there are a number of field-specific challenges to navigate. These include decisions about the safety of performing procedures involving fluoroscopy or high infectious risk, particularly early in pregnancy when organogenesis occurs.7,24 Additionally, engaging in appropriate obstetric care can be challenging given the need for regular physician and ultrasound appointments.
Simple, cost-efficient interventions may be effective in decreasing infertility rates, pregnancy loss, and poor physician experiences during pregnancy. For one, all gastroenterology divisions could craft written policies that include a no-tolerance approach to expressions of maternity bias against pregnant or postpartum trainees and faculty.12,25 Additionally, ergonomic improvements, such as standing pads, dial extenders, and adjusted screen heights may decrease injury rates and increase comfort for female endoscopists.26,27 There should also be a no-penalty, no-questions-asked approach for any female endoscopist who defers performance of an obstetrically high-risk procedure to a nonpregnant colleague. Additionally, pregnant gastroenterologists should be supported in obtaining high-quality obstetric care. At an individual level, nonpregnant gastroenterologists, and particularly male allies, can support pregnant colleagues by agreeing to perform higher-risk procedures, stepping in if a fellow is unable to perform endoscopy because of pregnancy, and by offering to push the endoscopy cart on behalf of a pregnant colleague to bedside, if necessary.10,28
Parental leave
Following delivery, parental leave presents an additional challenge for the physician parent. Paid maternal leave has been associated with improved child and maternal outcomes and is widely available to physicians outside the United States.29,30 At present, duration of leave varies significantly by career stage (fellows versus attending), practice setting (academic center versus private practice), and geographic location. The American Academy of Pediatrics recommends a minimum of 12 weeks of leave.31 This length has been associated with lower rates of postpartum depression and higher rates of sustained breastfeeding, with subsequent improved health outcomes for mother and child.32-34 An increasing number of states have passed laws mandating minimum paid and unpaid parental leave time (for example, in Massachusetts, gastroenterology trainees and faculty are afforded 12 weeks of leave, in accordance with state law).35 Recent changes to board eligibility and training requirements via the American Board of Medical Specialties and the American Council for Graduate Medical Education now provide 6 weeks for parental leave. This is an improvement over prior policies which rendered many physician-parents board-ineligible if they took more than 4 weeks of leave, although it must be noted that even the revised policies allow for less time than either that of Obstetricians and Gynecologists or than the American Academy of Pediatrics recommends.
Our data, presented at the 2021 ACG conference, suggest that many trainees report receiving 4 weeks or less of parental leave, despite the ACGME and ABMS policies described above. We also found that physicians were frequently not aware of their institution or division leave policies.10 Ideally, all gastroenterology divisions in the United States would follow the recommended leave duration set forth by the medical societies of specialties that care for pregnant and postpartum mothers and their infants. Additionally, the impact of leave time on graduation and board eligibility, as well as academic and practice promotion, should be made clear at the time of leave and should minimize adverse consequences for the careers of pregnant and postpartum gastroenterologists. Gastroenterology trainees and faculty should be educated in the existence and details of their institution or practice policies, and these policies should be made readily available to all physicians and administrators.
Postpartum period
The transition back to work is a challenging one for mothers in all fields of medicine, particularly for those returning to procedurally based subspecialties such as gastroenterology. This is especially true for trainees and faculty who have returned to work sooner than the recommended 12 weeks and for those who are post cesarean section, for whom physical healing may not be complete. Long days performing endoscopy may be physically challenging or impossible for some women during the postpartum period. Additionally, expressing breast milk, a metabolically intensive activity, also necessitates time, space, and privacy to perform and is frequently made more difficult by insufficient lactation accommodations. The COVID-19 pandemic has increased logistic challenges for lactating mothers, because of the need for well-ventilated lactation spaces to minimize infectious risk.19 Our colleagues have reported pumping in their vehicles, in supply closets, and in spaces that require so much travel time (in addition to time required to express milk, store milk, and clean pump equipment) that the practice was unsustainable, and the physician stopped breastfeeding prematurely.36
The benefits of breastfeeding for mother and infant are well-established, and exclusive breastfeeding for the first 6 months of life is supported by the American College of Obstetricians and Gynecologists, whose position statement reads as follows: “Policies that protect the right of a woman and her child to breastfeed ... and that accommodate milk expression, such as ... paid maternity leave, on-site childcare, break time for expressing milk, and a clean, private location for expressing milk, are essential to sustaining breastfeeding.”37 We would add to these recommendations provision of dedicated milk storage space and establishment of clear, supportive policies that allow lactating physicians to breastfeed and express breast milk if they choose without career penalty. Several institutions offer scheduled protected clinical time and modified work relative value units (RVU) for lactating physicians, such that returning parents can have protected time for expressing breast milk and still meet RVU targets.38 Additionally, many academic institutions offer productivity adjustments for tenure-track faculty who have recently had children.
Creating a more supportive environment for women gastroenterologists who desire children allows the field to be more representative of our patient population and has been shown to positively impact outcomes from improved colorectal cancer screening rates to more guideline-directed informed consent conversations.39-41 Gastroenterology should comprise a physician workforce predicated on clinical and research excellence alone and should not require its practitioners to delay or abstain from pregnancy and child rearing. Robust, clear, and generous parental leave and postpartum accommodations will allow the field to retain and promote talented physicians, who will then contribute to the betterment of patients and the field over decades.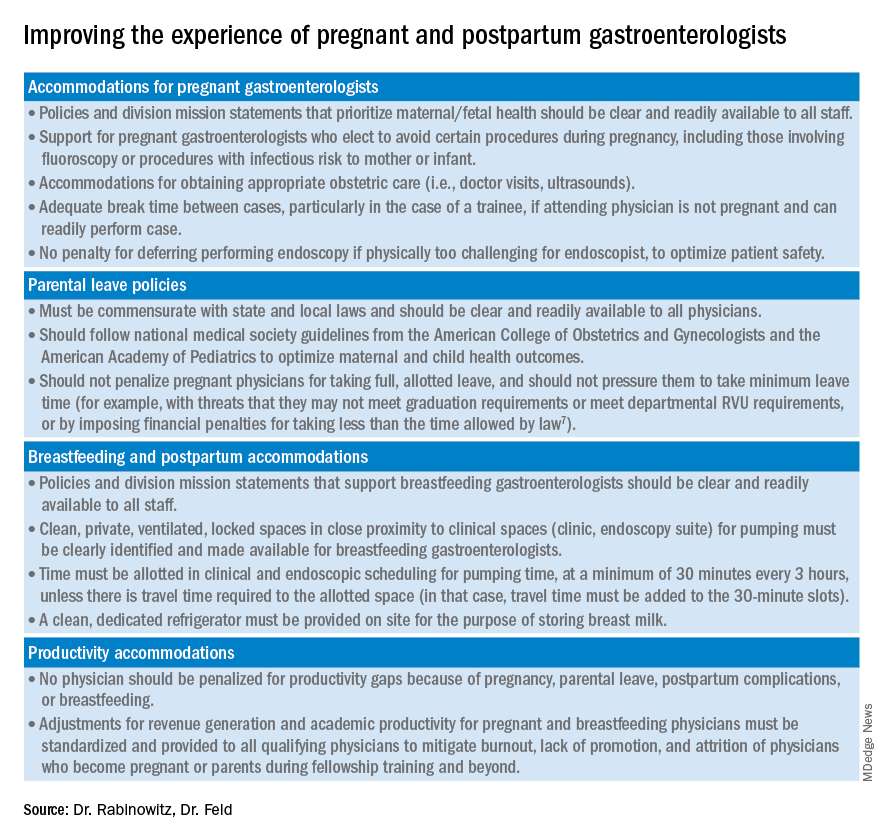
Dr. Rabinowitz is a faculty member in the department of medicine and division of gastroenterology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston. Dr. Feld is a transplant hepatology fellow, division of gastroenterology, department of medicine, University of Washington, Seattle. Dr. Rabinowitz and Dr. Feld have no conflicts of interest to disclose.
References
1. AAMC. Diversity in Medicine: Facts and Figures 2019. 2018.
2. Colleges AoAM. The State of Women in Academic Medicine: The Pipeline and Pathways to Leadership, 2015-2016. 2016. www.aamc.org/download/481206/data/2015table11.pdf.
3. AAMC. Table B-3: Total U.S. Medical School Enrollment by Race/Ethnicity and Sex, 2014-2015 through 2018-2019, 2019.
4. Rabinowitz LG. Recognizing blind spots – a remedy for gender bias in medicine? (N Engl. J Med. 2018; 378[24]: 2253-5).
5. Douglas PS et al. Career preferences and perceptions of cardiology among US internal medicine trainees: Factors influencing cardiology career choice. JAMA Cardiol 2018; 3(8):682-91.
6. Stack SW et al. Childbearing decisions in residency: A multicenter survey of female residents. Acad Med 2020;95(10):1550-7.
7. David YN et al. Pregnancy and the working gastroenterologist: Perceptions, realities, and systemic challenges. Gastroenterology 2021;161(3):756-60.
8. Rembacken BJ et al. Barriers and bias standing in the way of female trainees wanting to learn advanced endoscopy. United European Gastroenterol J. 2019;7(8):1141-5.
9. Arlow FL et al. Gastroenterology training and career choices: A prospective longitudinal study of the impact of gender and of managed care. Am J Gastroenterol. 2002;97(2):459-69.
10. Feld L et al. Parental leave for gastroenterology fellows: A national survey of current fellows. Am J Gastroenterol. 2021;116:S611-2.
11. Rabinowitz LG et al. Addressing gender in gastroenterology: opportunities for change. Gastrointest Endosc. 2020;91(1):155-61.
12. Feld LD. Baby steps in the right direction: Toward a parental leave policy for gastroenterology fellows. Am J Gastroenterol. 2021;116(3):505-8.
13. Feld LD. Interviewing for two. Am J Gastroenterol. 2020;116(3):445-6
14. Rabinowitz LG et al. Gender dynamics in education and practice of gastroenterology. Gastrointest Endosc. 2021;93(5):1047-56.e5.
15. Harvin G. Review of musculoskeletal injuries and prevention in the endoscopy practitioner. J Clin Gastroenterol. 2014;48(7):590-4.
16. LabX Oecs. www.labx.com/product/endoscopy-cart (accessed 2021 Nov 19.
17. Heilman ME and Okimoto TG. Motherhood: A potential source of bias in employment decisions. J Appl Psychol. 2008;93(1):189-98.
18. Robinson K et al. Racism, bias, and discrimination as modifiable barriers to breastfeeding for African American women: A scoping review of the literature. J Midwifery Womens Health. 2019;64(6):734-42.
19. Rabinowitz LG and Rabinowitz DG. Women on the Frontline: A Changed Workforce and the Fight Against COVID-19. Acad Med. 2021 Jun 1;96(6):808-12.
20. Rabinowitz LG et al. Gender in the endoscopy suite. Lancet Gastroenterol Hepatol. 2020 Dec;5(12):1032-4.
21. Stentz NC et al. Fertility and childbearing among American female physicians. J Womens Health. 2016; 25(10):1059-65.
22. Burke CA et al. Gender disparity in the practice of gastroenterology: The first 5 years of a career. Am J Gastroenterol. 2005;100(2):259-64.
23. Singh A et al. Women in gastroenterology committee of American College of G. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol. 2008;103(7):1589-95.
24. Krueger KJ and Hoffman BJ. Radiation exposure during gastroenterologic fluoroscopy: Risk assessment for pregnant workers. Am J Gastroenterol. 1992;87(4):429-31.
25. Krause ML et al. Impact of pregnancy and gender on internal medicine resident evaluations: A retrospective cohort study. J Gen Intern Med. 2017;32(6):648-53.
26. Pawa S et al. Are all endoscopy-related musculoskeletal injuries created equal? Results of a national gender-based survey. Am J Gastroenterol. 2021;116(3):530-8.
27. David YN et al. Gender-specific factors influencing gastroenterologists to pursue careers in advanced endoscopy: perceptions vs reality. Am J Gastroenterol. 2021;116(3):539-50.
28. Bilal M et al. The need for allyship in achieving gender equity in gastroenterology. Am J Gastroenterol. 2021 Oct 19. doi: 10.14309/ajg.0000000000001508. Online ahead of print.
29. Jou J et al. Paid maternity leave in the United States: Associations with maternal and infant health. Matern Child Health J. 2018;22(2):216-25.
30. Aitken Z et al. The maternal health outcomes of paid maternity leave: A systematic review. Soc Sci Med. 2015;130:32-41.
31. Dodson NA and Talib HJ. Paid parental leave for mothers and fathers can improve physician wellness. AAP News. 2020 Jul 1. https://publications.aap.org/aapnews/news/12432.
32. Kornfeind KR and Sipsma HL. Exploring the link between maternity leave and postpartum depression. Womens Health Issues 2018;28(4):321-6.
33. Navarro-Rosenblatt D and Garmendia ML. Maternity leave and its impact on breastfeeding: A review of the literature. Breastfeed Med 2018;13(9):589-97.
34. Stack SW et al. Maternity leave in residency: A multicenter study of determinants and wellness outcomes. Acad Med. 2019;94(11):1738-45.
35. Mass.gov. Paid Family and Medical Leave Information for Massachusetts Employers. 2020.
36. Ares Segura S et al. en representacion del Comite de Lactancia Materna de la Asociacion Espanola de P. [The importance of maternal nutrition during breastfeeding: Do breastfeeding mothers need nutritional supplements?]. An Pediatr. (Barc) 2016;84(6):347 e1-7.
37. American College of Obstetricians and Gynecologists, Committee on Obstetric Practice. Committee Opinion No. 658: Optimizing Support for Breastfeeding as Part of Obstetric Practice. Obstet Gynecol. 2016;127(2):e86-92.
38. Porter KK et al. A lactation credit model to support breastfeeding in radiology: The new gold standard to support “liquid gold.” Clin Imaging 2021;80:16-8.
39. Davis J et al. Clinical practice patterns suggest female patients prefer female endoscopists. Dig Dis Sci. 2015;60(10):3149-50.
40. Menees SB et al. Women patients’ preference for women physicians is a barrier to colon cancer screening. Gastrointest Endosc. 2005;62(2):219-23.
41. Feld LD et al. Management of code status in the periendoscopic period: A national survey of current practices and beliefs of U.S. gastroenterologists. Gastrointest Endosc. 2021;94(1):172-7.e2.


