User login
ONLINE EXCLUSIVE: PEERist Program Provides Rural Nebraska Hospital 24/7 HM Coverage
Hospitalist programs take many shapes, and the organizational flowchart typically depends on the number and makeup of the physicians, the hospital, the patients, and the community. Adequately covering the needs of inpatient units can be especially frustrating in rural communities, some hospitalists say.
“There are only five physicians total in our town,” says Gary Ensz, MD, a partner in the Auburn Family Health Center in Auburn, Neb. “In addition to being family practitioners, we are our own hospitalists. Covering the emergency room, seeing patients in clinic, and following hospitalized patients is a big burden.”
To address these issues, Dr. Ensz and his partners developed the Physician Extender Emergency Room Hospitalist (PEERist) program. They utilize physician assistants (PAs) to serve many hospitalist functions under their supervision.
“We hired PAs to work in the hospital and the emergency room,” Dr. Ensz explains. “They do not work in the clinic and then take call. Their only responsibilities are to the hospital and ER.”

—Gary Ensz, MD, partner, Auburn (Neb.) Family Health Center
PEERists work under protocols addressing treatment concerns and give guidance on when physicians should be called. On-call doctors round in the morning with the PA. The physicians like this approach, Dr. Ensz says, because they see the PEERist when it is convenient for them; before, they would leave clinic patients to attend to concerns at the hospital.
Impact of ER Call
“For most of us practicing in rural situations, the demands of ER call force people to retire,” Dr. Ensz says. “Now we have someone at the hospital highly trained and, as they get more experience, actually do some work better simply because they are there all the time. At worst, you now have two sets of hands working on the patient.”
PAs work a rotating schedule of up to 72 hours with as many as nine days off in a row. PAs can be recruited from a much larger area; in fact, one commutes four hours each way. PEERists say the time off makes it easier to do things with their families or work another job.
Other Benefits
In addition to pluses associated with the practice, Dr. Ensz is seeing other benefits, such as closer working relationships with the nurses. He also stresses that his hospital now has 24/7 in-house coverage, something almost unheard of in small rural hospitals.
One of the more subtle improvements might have been in getting people to the hospital quicker. “It wasn’t unusual for someone to come to clinic with symptoms they had for a while,” Dr. Ensz says. “The PEERists being in-house all the time have done away with these concerns.”
Hospitalist programs take many shapes, and the organizational flowchart typically depends on the number and makeup of the physicians, the hospital, the patients, and the community. Adequately covering the needs of inpatient units can be especially frustrating in rural communities, some hospitalists say.
“There are only five physicians total in our town,” says Gary Ensz, MD, a partner in the Auburn Family Health Center in Auburn, Neb. “In addition to being family practitioners, we are our own hospitalists. Covering the emergency room, seeing patients in clinic, and following hospitalized patients is a big burden.”
To address these issues, Dr. Ensz and his partners developed the Physician Extender Emergency Room Hospitalist (PEERist) program. They utilize physician assistants (PAs) to serve many hospitalist functions under their supervision.
“We hired PAs to work in the hospital and the emergency room,” Dr. Ensz explains. “They do not work in the clinic and then take call. Their only responsibilities are to the hospital and ER.”

—Gary Ensz, MD, partner, Auburn (Neb.) Family Health Center
PEERists work under protocols addressing treatment concerns and give guidance on when physicians should be called. On-call doctors round in the morning with the PA. The physicians like this approach, Dr. Ensz says, because they see the PEERist when it is convenient for them; before, they would leave clinic patients to attend to concerns at the hospital.
Impact of ER Call
“For most of us practicing in rural situations, the demands of ER call force people to retire,” Dr. Ensz says. “Now we have someone at the hospital highly trained and, as they get more experience, actually do some work better simply because they are there all the time. At worst, you now have two sets of hands working on the patient.”
PAs work a rotating schedule of up to 72 hours with as many as nine days off in a row. PAs can be recruited from a much larger area; in fact, one commutes four hours each way. PEERists say the time off makes it easier to do things with their families or work another job.
Other Benefits
In addition to pluses associated with the practice, Dr. Ensz is seeing other benefits, such as closer working relationships with the nurses. He also stresses that his hospital now has 24/7 in-house coverage, something almost unheard of in small rural hospitals.
One of the more subtle improvements might have been in getting people to the hospital quicker. “It wasn’t unusual for someone to come to clinic with symptoms they had for a while,” Dr. Ensz says. “The PEERists being in-house all the time have done away with these concerns.”
Hospitalist programs take many shapes, and the organizational flowchart typically depends on the number and makeup of the physicians, the hospital, the patients, and the community. Adequately covering the needs of inpatient units can be especially frustrating in rural communities, some hospitalists say.
“There are only five physicians total in our town,” says Gary Ensz, MD, a partner in the Auburn Family Health Center in Auburn, Neb. “In addition to being family practitioners, we are our own hospitalists. Covering the emergency room, seeing patients in clinic, and following hospitalized patients is a big burden.”
To address these issues, Dr. Ensz and his partners developed the Physician Extender Emergency Room Hospitalist (PEERist) program. They utilize physician assistants (PAs) to serve many hospitalist functions under their supervision.
“We hired PAs to work in the hospital and the emergency room,” Dr. Ensz explains. “They do not work in the clinic and then take call. Their only responsibilities are to the hospital and ER.”

—Gary Ensz, MD, partner, Auburn (Neb.) Family Health Center
PEERists work under protocols addressing treatment concerns and give guidance on when physicians should be called. On-call doctors round in the morning with the PA. The physicians like this approach, Dr. Ensz says, because they see the PEERist when it is convenient for them; before, they would leave clinic patients to attend to concerns at the hospital.
Impact of ER Call
“For most of us practicing in rural situations, the demands of ER call force people to retire,” Dr. Ensz says. “Now we have someone at the hospital highly trained and, as they get more experience, actually do some work better simply because they are there all the time. At worst, you now have two sets of hands working on the patient.”
PAs work a rotating schedule of up to 72 hours with as many as nine days off in a row. PAs can be recruited from a much larger area; in fact, one commutes four hours each way. PEERists say the time off makes it easier to do things with their families or work another job.
Other Benefits
In addition to pluses associated with the practice, Dr. Ensz is seeing other benefits, such as closer working relationships with the nurses. He also stresses that his hospital now has 24/7 in-house coverage, something almost unheard of in small rural hospitals.
One of the more subtle improvements might have been in getting people to the hospital quicker. “It wasn’t unusual for someone to come to clinic with symptoms they had for a while,” Dr. Ensz says. “The PEERists being in-house all the time have done away with these concerns.”
Nurse Practitioners, Physician Assistants to the Rescue
In 2004, the hospitalist group at the University of Michigan Health System in Ann Arbor faced a manpower problem: In a refrain common to hospitalist groups around the country, changes in duty-hour regulations were making it harder for medical residents to continue to provide inpatient coverage at the same levels as before.
Addressing the issue was difficult for the HM group and hospital administrators; they were going to need a significant number of new providers, and qualified physicians were in short supply. To address these issues, the HM group chose to add nonphysician providers (NPP) to their service.
“NPPs had worked at UM for a long time in other areas,” says Vikas Parekh, MD, SFHM, associate director of hospitalist management. “We had just created a new service that was hiring new people and thought NPPs would help in providing services.”
Hiring NPPs helped solve the University of Michigan’s problem, and the tactic has helped solve manpower issues at numerous HM groups around the country. But deciding whether your HM group should hire physicians, NPPs—usually nurse practitioners (NPs) and physician assistants (PAs)—or some combination of the two will not be easy. It is a complex decision, one that requires following state-level licensing and practice laws as well as local hospital bylaws and federal and private insurance payment rules. Such decisions also mean HM group directors need to keep in mind case mixes and the personalities of the physicians in the practice.
“There is no one-size-fits-all solution,” says Mitchell Wilson, MD, SFHM, corporate medical director for Eagle Hospital Physicians in Atlanta. “Not all environments are well-suited to NPP practice. Even when it is, you can’t just throw an NPP into the mix on their own with the expectation they will be successful.”
Whether it’s covering admissions, streamlining discharges, or working as an integral part of a care team, NPPs can be the solution expanding HM groups are looking for.

“Our physicians depend on NPPs to help them complete patient care in a more efficient manner and work to enhance continuity of care,” says Mary Whitehead, RN, APRN-BC, FNP, of Hospital Medicine Associates in Fort Worth, Texas. “We lower physician rounding time so patients are seen sooner and tests are requested sooner. In addition, the patients really appreciate the extra time we can spend with them.”
Trained, Licensed, Available
NPs must be registered nurses with clinical experience before they can enroll in an advanced degree program, which usually results in a master’s degree or doctorate. Generally, a state board of nursing, or a state board jointly with the state medical board, regulates NPs.
PAs are trained in more of a traditional medical model. They have a variable education level all the way up to a PhD, although more states are requiring at least a master’s degree. Practice and other legal parameters most often come under the authority of state medical boards.
NPPs can provide additional medical expertise to patients, says Ryan Genzink, PA, a physician assistant with Hospitalists of Western Michigan in Grand Rapids and the American Academy of Physician Assistants’ medical liaison to SHM. “One of the challenges faced by physicians is that they often have to be in two places at once,” he says. “There is a recognition that teams provide better care for complicated patients.”
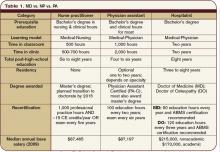
NPPs generally practice under the supervision of a physician hospitalist. Some states allow a greater degree of independence for NPs. However, most NPs and PAs are required to have a practice agreement outlining their responsibilities and the amount of oversight required (see Table 1, p. 39). There is no such thing as a “fire and forget” NPP.
“The practice needs to thoroughly understand the legal environment early in the process,” says John Nelson, MD, MHM, hospitalist director at Bellevue (Wash.) Medical Center, partner in Nelson Flores Hospital Medicine Consultants, and SHM cofounder. “NPPs are not a ‘hospitalist lite’ that can function entirely like a hospitalist.”
Hospital bylaws, which can vary greatly by city, county, or state, are another important consideration before you hire an NPP.
“In some areas, NPPs may not be able to practice in the ICU,” Dr. Wilson says. “In others, the physician may be required to see the patient instead of consulting with the NPP. The idiosyncrasies of the individual hospital’s bylaws may impact the efficiency of the NPP/MD team.”
Physician Characteristics
Environmental variables—namely, the personality of the physicians within the practice—should be considered before you head down the NPP path. It makes little practical or financial sense to spend the time and effort of hiring an NPP if the physicians still insist on doing all the work.
“[It’s] one of the most significant factors in successfully integrating an NPP program,” Dr. Wilson says. “Will [physicians] be able to tolerate some degree of uncertainty when letting others see their patients? Are they open to adapting to different practice styles? The thing we see most often in practices that use NPPs to their advantage is the recognition that there is an important role for the nonphysician at the bedside.”
Some physicians hesitate to work with NPPs, while others welcome the extra help and unique experience NPPs offer. Experts agree that forcing NPPs on a physician is not a good idea. They also agree that, especially when beginning a new program, group directors should let physicians who are interested in working with NPPs take the lead. As NPP use in the group matures, many of those who were at first unwilling can decide that there is a place for NPPs in their practice.
Case Mix Is Key
The types and kinds of patient seen might limit the use of NPPs in hospitalist practice. “Our experience is that acuity and complexity of the care, especially as it relates to diagnostic and therapeutic decision-making, makes it difficult for NPPs to function independently,” Dr. Parekh says.
Dr. Wilson agrees. “Depending on the specific attributes of the setting, a service with both high-complexity and high-acuity patients may be a more challenging environment to realize the efficiencies of NPPs,” he says. “There is a relationship between complexity, acuity, and physician involvement.”
Even so, a continuum of NPP use in HM practice is achievable. For example, as a patient improves, an NPP might be able to take on a larger role in treatment by participating in discharge planning. In more acute patients, the NPP can save valuable physician time by coordinating with consultants, staying on top of treatments, and consolidating clinically important data for the physician.
Many Models in Use
Historically, the widespread use of alternative providers began in 2004 as a result of the changes to resident duty-hours. The restrictions created a workforce gap, which led to a large number of new positions in hospitals nationwide. Many of HM’s early adopters essentially went with what they knew.
“We work in teams where the physician, NPP, and nurse see a group of patients similar in function to an attending, resident, and RN,” Genzink says. “We see ‘our’ patients in a collaborative fashion.”
There are other models that have proven successful in the correct setting. Some HM groups use specialist NPPs to cover specific clinical areas, such as orthopedics or oncology. This not only develops a cadre of providers with excellent understanding of their patients, but it also frees up physician time for more acute and complicated patients.
“Our physicians depend on us helping them get patient care completed more efficiently, so that length of stay is acceptable, and to enhance continuity of care,” says Whitehead, the American Academy of Nurse Practitioners’ liaison to SHM. “Having an NPP visit the patient daily, documenting progress, greatly enhances communications between physicians and consultants.”
Other groups have NPPs specialize by function—for example, they cover all admissions or work mainly with discharging a patient. Some groups have the physician see the patient on admission, work out a care plan, then turn over management to the NPP. Many agree that most NPPs are best utilized by having them cover specific shifts, such as overnight call or on a swing shift, to help during peak demand.
Monetary and Time Commitments
The financial impact of NPPs on a hospitalist practice depends on many factors. Groups will need to look not only at the salary and benefit costs associated with the position, but also how best to fit that person into the billing system.
Salary and benefit comparisons are fairly straightforward: The State of Hospital Medicine: 2010 Report Based on 2009 Data, produced by SHM and the Medical Group Management Association, shows median total compensation for adult hospitalists at $215,000 per year; NPP compensation is around $87,000.1
The general cost of benefits (health insurance, retirement, etc.) is fairly typical throughout a hospitalist practice, so there should be little difference between a new FTE hospitalist or NPP. Other considerations, including office space and support staff, would be roughly the same if the group hired a physician. The cost of continuing education and malpractice insurance likely will be less with an NPP, but it is best to check before making a new hire.
After the outgo has been established, the next step is to look at the differences in reimbursement for NPPs vs. physicians. Here, again, the math gets tricky. The Centers for Medicare & Medicaid Services (CMS) pay NPPs at 85% of the physician rate for a specific diagnosis. However, if there is direct physician involvement, the claim can be filed as “shared billing” and reimbursed at 100%.
For some hospitalist practices, adding NPPs is an easy decision to make. Dr. Parekh says his group already has policies in place that require a physician to see the patient every day. In that case, no extra physician time is necessary, so shared billing makes sense. Other hospitals’ bylaws might have similar requirements.
For practices in which the NPP is able to work with less oversight, it might be better to bill at 85% rather than use the physician time to meet shared-billing criteria. Even in practices with greater NPP autonomy, such variables as case mix and patient acuity might enter into the equation. If the patient is sick enough that the physician is involved for a significant amount of time, then shared billing probably is best.
Experts say group directors and hiring managers should look carefully at contracts with private insurers, too. There most likely will be considerable variation in how each plan handles NPP claims.
Managing performance expectations can have an impact on the successful use of NPPs in a hospitalist practice. Setting realistic goals and groupwide understanding of what the NPPs’ roles will be is crucial. The practice should look at the work that needs to be done and decide if that work provides a genuinely valuable role for an NPP.
Hire for Need, Not Desperation
“The mistake I see most often is hiring an NPP because a practice is desperate for help,” says Martin Buser, MPH, FACHE, a partner in Hospitalist Management Resources, LLC, in San Diego. “Smart practices are looking at NPPs, evaluating where they do the most good, and then setting out their role and expectations based on these needs and the practice environment.”
Hiring mistakes can be compounded if the NPP is not a good match to the job description or group expectations. If the practice hires an NPP fresh out of school, the group will need to establish training and have the new hire work more closely with physicians. If, on the other hand, an NP has 10 years of experience in an ICU, or a PA has worked in the ED for the past five years, a higher level of autonomy can be granted sooner. However, NPPs with established backgrounds are almost as rare as experienced hospitalists (see “Integrating NPPs Into HM Practice,” p. 38).
Inevitably, there will be changes in the interactions between patients and the hospitalists, as both physicians and NPPs become more comfortable with the other’s practice style, as well as each other’s strengths and weaknesses.
MD-to-NPP Ratio Varies
The practice structure and optimal mix of NPPs to MDs is something that will be specific to the hospitalist group. “We don’t really have good studies on this subject,” Buser says. “I usually get worried when we exceed two NPPs to one MD.”
Others disagree. Dr. Parekh, who works in an academic center, says his group has been successful having one MD work with as many as three NPPs. At the other end, Dr. Wilson says his 10 years of experience suggest 1:1 is the most efficient ratio.
However, all of them agree that having one NPP work with more than one physician is not sustainable. The NPP will be less familiar with each doctor’s practice style, what kind of information they need, and how things should be presented. If two or more hospitalists share an NPP, there can be internal friction over division of the NPP’s time, as well as extending the time before the MDs have a good feel for the NPP’s strengths and weaknesses.
In the final analysis, the HM group has to look at the amount and type of work available. In some cases, it will make financial and clinical sense to bring on an NPP. Under other circumstances, an FTE hospitalist is the best fit.
“Sustainability, quality, and efficiency are the drivers for NPP/MD teams. Increasing pressure to offset program costs is not,” Dr. Wilson says. “You do it because it helps sustain the program, helps with recruiting, and effects your efficiency.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- Medical Group Management Association and the Society of Hospital Medicine. State of Hospital Medicine: 2010 Report Based on 2009 Data. 2010. Philadelphia and Englewood, Colo.
In 2004, the hospitalist group at the University of Michigan Health System in Ann Arbor faced a manpower problem: In a refrain common to hospitalist groups around the country, changes in duty-hour regulations were making it harder for medical residents to continue to provide inpatient coverage at the same levels as before.
Addressing the issue was difficult for the HM group and hospital administrators; they were going to need a significant number of new providers, and qualified physicians were in short supply. To address these issues, the HM group chose to add nonphysician providers (NPP) to their service.
“NPPs had worked at UM for a long time in other areas,” says Vikas Parekh, MD, SFHM, associate director of hospitalist management. “We had just created a new service that was hiring new people and thought NPPs would help in providing services.”
Hiring NPPs helped solve the University of Michigan’s problem, and the tactic has helped solve manpower issues at numerous HM groups around the country. But deciding whether your HM group should hire physicians, NPPs—usually nurse practitioners (NPs) and physician assistants (PAs)—or some combination of the two will not be easy. It is a complex decision, one that requires following state-level licensing and practice laws as well as local hospital bylaws and federal and private insurance payment rules. Such decisions also mean HM group directors need to keep in mind case mixes and the personalities of the physicians in the practice.
“There is no one-size-fits-all solution,” says Mitchell Wilson, MD, SFHM, corporate medical director for Eagle Hospital Physicians in Atlanta. “Not all environments are well-suited to NPP practice. Even when it is, you can’t just throw an NPP into the mix on their own with the expectation they will be successful.”
Whether it’s covering admissions, streamlining discharges, or working as an integral part of a care team, NPPs can be the solution expanding HM groups are looking for.

“Our physicians depend on NPPs to help them complete patient care in a more efficient manner and work to enhance continuity of care,” says Mary Whitehead, RN, APRN-BC, FNP, of Hospital Medicine Associates in Fort Worth, Texas. “We lower physician rounding time so patients are seen sooner and tests are requested sooner. In addition, the patients really appreciate the extra time we can spend with them.”
Trained, Licensed, Available
NPs must be registered nurses with clinical experience before they can enroll in an advanced degree program, which usually results in a master’s degree or doctorate. Generally, a state board of nursing, or a state board jointly with the state medical board, regulates NPs.
PAs are trained in more of a traditional medical model. They have a variable education level all the way up to a PhD, although more states are requiring at least a master’s degree. Practice and other legal parameters most often come under the authority of state medical boards.
NPPs can provide additional medical expertise to patients, says Ryan Genzink, PA, a physician assistant with Hospitalists of Western Michigan in Grand Rapids and the American Academy of Physician Assistants’ medical liaison to SHM. “One of the challenges faced by physicians is that they often have to be in two places at once,” he says. “There is a recognition that teams provide better care for complicated patients.”
NPPs generally practice under the supervision of a physician hospitalist. Some states allow a greater degree of independence for NPs. However, most NPs and PAs are required to have a practice agreement outlining their responsibilities and the amount of oversight required (see Table 1, p. 39). There is no such thing as a “fire and forget” NPP.
“The practice needs to thoroughly understand the legal environment early in the process,” says John Nelson, MD, MHM, hospitalist director at Bellevue (Wash.) Medical Center, partner in Nelson Flores Hospital Medicine Consultants, and SHM cofounder. “NPPs are not a ‘hospitalist lite’ that can function entirely like a hospitalist.”
Hospital bylaws, which can vary greatly by city, county, or state, are another important consideration before you hire an NPP.
“In some areas, NPPs may not be able to practice in the ICU,” Dr. Wilson says. “In others, the physician may be required to see the patient instead of consulting with the NPP. The idiosyncrasies of the individual hospital’s bylaws may impact the efficiency of the NPP/MD team.”
Physician Characteristics
Environmental variables—namely, the personality of the physicians within the practice—should be considered before you head down the NPP path. It makes little practical or financial sense to spend the time and effort of hiring an NPP if the physicians still insist on doing all the work.
“[It’s] one of the most significant factors in successfully integrating an NPP program,” Dr. Wilson says. “Will [physicians] be able to tolerate some degree of uncertainty when letting others see their patients? Are they open to adapting to different practice styles? The thing we see most often in practices that use NPPs to their advantage is the recognition that there is an important role for the nonphysician at the bedside.”
Some physicians hesitate to work with NPPs, while others welcome the extra help and unique experience NPPs offer. Experts agree that forcing NPPs on a physician is not a good idea. They also agree that, especially when beginning a new program, group directors should let physicians who are interested in working with NPPs take the lead. As NPP use in the group matures, many of those who were at first unwilling can decide that there is a place for NPPs in their practice.
Case Mix Is Key
The types and kinds of patient seen might limit the use of NPPs in hospitalist practice. “Our experience is that acuity and complexity of the care, especially as it relates to diagnostic and therapeutic decision-making, makes it difficult for NPPs to function independently,” Dr. Parekh says.
Dr. Wilson agrees. “Depending on the specific attributes of the setting, a service with both high-complexity and high-acuity patients may be a more challenging environment to realize the efficiencies of NPPs,” he says. “There is a relationship between complexity, acuity, and physician involvement.”
Even so, a continuum of NPP use in HM practice is achievable. For example, as a patient improves, an NPP might be able to take on a larger role in treatment by participating in discharge planning. In more acute patients, the NPP can save valuable physician time by coordinating with consultants, staying on top of treatments, and consolidating clinically important data for the physician.
Many Models in Use
Historically, the widespread use of alternative providers began in 2004 as a result of the changes to resident duty-hours. The restrictions created a workforce gap, which led to a large number of new positions in hospitals nationwide. Many of HM’s early adopters essentially went with what they knew.
“We work in teams where the physician, NPP, and nurse see a group of patients similar in function to an attending, resident, and RN,” Genzink says. “We see ‘our’ patients in a collaborative fashion.”
There are other models that have proven successful in the correct setting. Some HM groups use specialist NPPs to cover specific clinical areas, such as orthopedics or oncology. This not only develops a cadre of providers with excellent understanding of their patients, but it also frees up physician time for more acute and complicated patients.
“Our physicians depend on us helping them get patient care completed more efficiently, so that length of stay is acceptable, and to enhance continuity of care,” says Whitehead, the American Academy of Nurse Practitioners’ liaison to SHM. “Having an NPP visit the patient daily, documenting progress, greatly enhances communications between physicians and consultants.”
Other groups have NPPs specialize by function—for example, they cover all admissions or work mainly with discharging a patient. Some groups have the physician see the patient on admission, work out a care plan, then turn over management to the NPP. Many agree that most NPPs are best utilized by having them cover specific shifts, such as overnight call or on a swing shift, to help during peak demand.
Monetary and Time Commitments
The financial impact of NPPs on a hospitalist practice depends on many factors. Groups will need to look not only at the salary and benefit costs associated with the position, but also how best to fit that person into the billing system.
Salary and benefit comparisons are fairly straightforward: The State of Hospital Medicine: 2010 Report Based on 2009 Data, produced by SHM and the Medical Group Management Association, shows median total compensation for adult hospitalists at $215,000 per year; NPP compensation is around $87,000.1
The general cost of benefits (health insurance, retirement, etc.) is fairly typical throughout a hospitalist practice, so there should be little difference between a new FTE hospitalist or NPP. Other considerations, including office space and support staff, would be roughly the same if the group hired a physician. The cost of continuing education and malpractice insurance likely will be less with an NPP, but it is best to check before making a new hire.
After the outgo has been established, the next step is to look at the differences in reimbursement for NPPs vs. physicians. Here, again, the math gets tricky. The Centers for Medicare & Medicaid Services (CMS) pay NPPs at 85% of the physician rate for a specific diagnosis. However, if there is direct physician involvement, the claim can be filed as “shared billing” and reimbursed at 100%.
For some hospitalist practices, adding NPPs is an easy decision to make. Dr. Parekh says his group already has policies in place that require a physician to see the patient every day. In that case, no extra physician time is necessary, so shared billing makes sense. Other hospitals’ bylaws might have similar requirements.
For practices in which the NPP is able to work with less oversight, it might be better to bill at 85% rather than use the physician time to meet shared-billing criteria. Even in practices with greater NPP autonomy, such variables as case mix and patient acuity might enter into the equation. If the patient is sick enough that the physician is involved for a significant amount of time, then shared billing probably is best.
Experts say group directors and hiring managers should look carefully at contracts with private insurers, too. There most likely will be considerable variation in how each plan handles NPP claims.
Managing performance expectations can have an impact on the successful use of NPPs in a hospitalist practice. Setting realistic goals and groupwide understanding of what the NPPs’ roles will be is crucial. The practice should look at the work that needs to be done and decide if that work provides a genuinely valuable role for an NPP.
Hire for Need, Not Desperation
“The mistake I see most often is hiring an NPP because a practice is desperate for help,” says Martin Buser, MPH, FACHE, a partner in Hospitalist Management Resources, LLC, in San Diego. “Smart practices are looking at NPPs, evaluating where they do the most good, and then setting out their role and expectations based on these needs and the practice environment.”
Hiring mistakes can be compounded if the NPP is not a good match to the job description or group expectations. If the practice hires an NPP fresh out of school, the group will need to establish training and have the new hire work more closely with physicians. If, on the other hand, an NP has 10 years of experience in an ICU, or a PA has worked in the ED for the past five years, a higher level of autonomy can be granted sooner. However, NPPs with established backgrounds are almost as rare as experienced hospitalists (see “Integrating NPPs Into HM Practice,” p. 38).
Inevitably, there will be changes in the interactions between patients and the hospitalists, as both physicians and NPPs become more comfortable with the other’s practice style, as well as each other’s strengths and weaknesses.
MD-to-NPP Ratio Varies
The practice structure and optimal mix of NPPs to MDs is something that will be specific to the hospitalist group. “We don’t really have good studies on this subject,” Buser says. “I usually get worried when we exceed two NPPs to one MD.”
Others disagree. Dr. Parekh, who works in an academic center, says his group has been successful having one MD work with as many as three NPPs. At the other end, Dr. Wilson says his 10 years of experience suggest 1:1 is the most efficient ratio.
However, all of them agree that having one NPP work with more than one physician is not sustainable. The NPP will be less familiar with each doctor’s practice style, what kind of information they need, and how things should be presented. If two or more hospitalists share an NPP, there can be internal friction over division of the NPP’s time, as well as extending the time before the MDs have a good feel for the NPP’s strengths and weaknesses.
In the final analysis, the HM group has to look at the amount and type of work available. In some cases, it will make financial and clinical sense to bring on an NPP. Under other circumstances, an FTE hospitalist is the best fit.
“Sustainability, quality, and efficiency are the drivers for NPP/MD teams. Increasing pressure to offset program costs is not,” Dr. Wilson says. “You do it because it helps sustain the program, helps with recruiting, and effects your efficiency.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- Medical Group Management Association and the Society of Hospital Medicine. State of Hospital Medicine: 2010 Report Based on 2009 Data. 2010. Philadelphia and Englewood, Colo.
In 2004, the hospitalist group at the University of Michigan Health System in Ann Arbor faced a manpower problem: In a refrain common to hospitalist groups around the country, changes in duty-hour regulations were making it harder for medical residents to continue to provide inpatient coverage at the same levels as before.
Addressing the issue was difficult for the HM group and hospital administrators; they were going to need a significant number of new providers, and qualified physicians were in short supply. To address these issues, the HM group chose to add nonphysician providers (NPP) to their service.
“NPPs had worked at UM for a long time in other areas,” says Vikas Parekh, MD, SFHM, associate director of hospitalist management. “We had just created a new service that was hiring new people and thought NPPs would help in providing services.”
Hiring NPPs helped solve the University of Michigan’s problem, and the tactic has helped solve manpower issues at numerous HM groups around the country. But deciding whether your HM group should hire physicians, NPPs—usually nurse practitioners (NPs) and physician assistants (PAs)—or some combination of the two will not be easy. It is a complex decision, one that requires following state-level licensing and practice laws as well as local hospital bylaws and federal and private insurance payment rules. Such decisions also mean HM group directors need to keep in mind case mixes and the personalities of the physicians in the practice.
“There is no one-size-fits-all solution,” says Mitchell Wilson, MD, SFHM, corporate medical director for Eagle Hospital Physicians in Atlanta. “Not all environments are well-suited to NPP practice. Even when it is, you can’t just throw an NPP into the mix on their own with the expectation they will be successful.”
Whether it’s covering admissions, streamlining discharges, or working as an integral part of a care team, NPPs can be the solution expanding HM groups are looking for.

“Our physicians depend on NPPs to help them complete patient care in a more efficient manner and work to enhance continuity of care,” says Mary Whitehead, RN, APRN-BC, FNP, of Hospital Medicine Associates in Fort Worth, Texas. “We lower physician rounding time so patients are seen sooner and tests are requested sooner. In addition, the patients really appreciate the extra time we can spend with them.”
Trained, Licensed, Available
NPs must be registered nurses with clinical experience before they can enroll in an advanced degree program, which usually results in a master’s degree or doctorate. Generally, a state board of nursing, or a state board jointly with the state medical board, regulates NPs.
PAs are trained in more of a traditional medical model. They have a variable education level all the way up to a PhD, although more states are requiring at least a master’s degree. Practice and other legal parameters most often come under the authority of state medical boards.
NPPs can provide additional medical expertise to patients, says Ryan Genzink, PA, a physician assistant with Hospitalists of Western Michigan in Grand Rapids and the American Academy of Physician Assistants’ medical liaison to SHM. “One of the challenges faced by physicians is that they often have to be in two places at once,” he says. “There is a recognition that teams provide better care for complicated patients.”
NPPs generally practice under the supervision of a physician hospitalist. Some states allow a greater degree of independence for NPs. However, most NPs and PAs are required to have a practice agreement outlining their responsibilities and the amount of oversight required (see Table 1, p. 39). There is no such thing as a “fire and forget” NPP.
“The practice needs to thoroughly understand the legal environment early in the process,” says John Nelson, MD, MHM, hospitalist director at Bellevue (Wash.) Medical Center, partner in Nelson Flores Hospital Medicine Consultants, and SHM cofounder. “NPPs are not a ‘hospitalist lite’ that can function entirely like a hospitalist.”
Hospital bylaws, which can vary greatly by city, county, or state, are another important consideration before you hire an NPP.
“In some areas, NPPs may not be able to practice in the ICU,” Dr. Wilson says. “In others, the physician may be required to see the patient instead of consulting with the NPP. The idiosyncrasies of the individual hospital’s bylaws may impact the efficiency of the NPP/MD team.”
Physician Characteristics
Environmental variables—namely, the personality of the physicians within the practice—should be considered before you head down the NPP path. It makes little practical or financial sense to spend the time and effort of hiring an NPP if the physicians still insist on doing all the work.
“[It’s] one of the most significant factors in successfully integrating an NPP program,” Dr. Wilson says. “Will [physicians] be able to tolerate some degree of uncertainty when letting others see their patients? Are they open to adapting to different practice styles? The thing we see most often in practices that use NPPs to their advantage is the recognition that there is an important role for the nonphysician at the bedside.”
Some physicians hesitate to work with NPPs, while others welcome the extra help and unique experience NPPs offer. Experts agree that forcing NPPs on a physician is not a good idea. They also agree that, especially when beginning a new program, group directors should let physicians who are interested in working with NPPs take the lead. As NPP use in the group matures, many of those who were at first unwilling can decide that there is a place for NPPs in their practice.
Case Mix Is Key
The types and kinds of patient seen might limit the use of NPPs in hospitalist practice. “Our experience is that acuity and complexity of the care, especially as it relates to diagnostic and therapeutic decision-making, makes it difficult for NPPs to function independently,” Dr. Parekh says.
Dr. Wilson agrees. “Depending on the specific attributes of the setting, a service with both high-complexity and high-acuity patients may be a more challenging environment to realize the efficiencies of NPPs,” he says. “There is a relationship between complexity, acuity, and physician involvement.”
Even so, a continuum of NPP use in HM practice is achievable. For example, as a patient improves, an NPP might be able to take on a larger role in treatment by participating in discharge planning. In more acute patients, the NPP can save valuable physician time by coordinating with consultants, staying on top of treatments, and consolidating clinically important data for the physician.
Many Models in Use
Historically, the widespread use of alternative providers began in 2004 as a result of the changes to resident duty-hours. The restrictions created a workforce gap, which led to a large number of new positions in hospitals nationwide. Many of HM’s early adopters essentially went with what they knew.
“We work in teams where the physician, NPP, and nurse see a group of patients similar in function to an attending, resident, and RN,” Genzink says. “We see ‘our’ patients in a collaborative fashion.”
There are other models that have proven successful in the correct setting. Some HM groups use specialist NPPs to cover specific clinical areas, such as orthopedics or oncology. This not only develops a cadre of providers with excellent understanding of their patients, but it also frees up physician time for more acute and complicated patients.
“Our physicians depend on us helping them get patient care completed more efficiently, so that length of stay is acceptable, and to enhance continuity of care,” says Whitehead, the American Academy of Nurse Practitioners’ liaison to SHM. “Having an NPP visit the patient daily, documenting progress, greatly enhances communications between physicians and consultants.”
Other groups have NPPs specialize by function—for example, they cover all admissions or work mainly with discharging a patient. Some groups have the physician see the patient on admission, work out a care plan, then turn over management to the NPP. Many agree that most NPPs are best utilized by having them cover specific shifts, such as overnight call or on a swing shift, to help during peak demand.
Monetary and Time Commitments
The financial impact of NPPs on a hospitalist practice depends on many factors. Groups will need to look not only at the salary and benefit costs associated with the position, but also how best to fit that person into the billing system.
Salary and benefit comparisons are fairly straightforward: The State of Hospital Medicine: 2010 Report Based on 2009 Data, produced by SHM and the Medical Group Management Association, shows median total compensation for adult hospitalists at $215,000 per year; NPP compensation is around $87,000.1
The general cost of benefits (health insurance, retirement, etc.) is fairly typical throughout a hospitalist practice, so there should be little difference between a new FTE hospitalist or NPP. Other considerations, including office space and support staff, would be roughly the same if the group hired a physician. The cost of continuing education and malpractice insurance likely will be less with an NPP, but it is best to check before making a new hire.
After the outgo has been established, the next step is to look at the differences in reimbursement for NPPs vs. physicians. Here, again, the math gets tricky. The Centers for Medicare & Medicaid Services (CMS) pay NPPs at 85% of the physician rate for a specific diagnosis. However, if there is direct physician involvement, the claim can be filed as “shared billing” and reimbursed at 100%.
For some hospitalist practices, adding NPPs is an easy decision to make. Dr. Parekh says his group already has policies in place that require a physician to see the patient every day. In that case, no extra physician time is necessary, so shared billing makes sense. Other hospitals’ bylaws might have similar requirements.
For practices in which the NPP is able to work with less oversight, it might be better to bill at 85% rather than use the physician time to meet shared-billing criteria. Even in practices with greater NPP autonomy, such variables as case mix and patient acuity might enter into the equation. If the patient is sick enough that the physician is involved for a significant amount of time, then shared billing probably is best.
Experts say group directors and hiring managers should look carefully at contracts with private insurers, too. There most likely will be considerable variation in how each plan handles NPP claims.
Managing performance expectations can have an impact on the successful use of NPPs in a hospitalist practice. Setting realistic goals and groupwide understanding of what the NPPs’ roles will be is crucial. The practice should look at the work that needs to be done and decide if that work provides a genuinely valuable role for an NPP.
Hire for Need, Not Desperation
“The mistake I see most often is hiring an NPP because a practice is desperate for help,” says Martin Buser, MPH, FACHE, a partner in Hospitalist Management Resources, LLC, in San Diego. “Smart practices are looking at NPPs, evaluating where they do the most good, and then setting out their role and expectations based on these needs and the practice environment.”
Hiring mistakes can be compounded if the NPP is not a good match to the job description or group expectations. If the practice hires an NPP fresh out of school, the group will need to establish training and have the new hire work more closely with physicians. If, on the other hand, an NP has 10 years of experience in an ICU, or a PA has worked in the ED for the past five years, a higher level of autonomy can be granted sooner. However, NPPs with established backgrounds are almost as rare as experienced hospitalists (see “Integrating NPPs Into HM Practice,” p. 38).
Inevitably, there will be changes in the interactions between patients and the hospitalists, as both physicians and NPPs become more comfortable with the other’s practice style, as well as each other’s strengths and weaknesses.
MD-to-NPP Ratio Varies
The practice structure and optimal mix of NPPs to MDs is something that will be specific to the hospitalist group. “We don’t really have good studies on this subject,” Buser says. “I usually get worried when we exceed two NPPs to one MD.”
Others disagree. Dr. Parekh, who works in an academic center, says his group has been successful having one MD work with as many as three NPPs. At the other end, Dr. Wilson says his 10 years of experience suggest 1:1 is the most efficient ratio.
However, all of them agree that having one NPP work with more than one physician is not sustainable. The NPP will be less familiar with each doctor’s practice style, what kind of information they need, and how things should be presented. If two or more hospitalists share an NPP, there can be internal friction over division of the NPP’s time, as well as extending the time before the MDs have a good feel for the NPP’s strengths and weaknesses.
In the final analysis, the HM group has to look at the amount and type of work available. In some cases, it will make financial and clinical sense to bring on an NPP. Under other circumstances, an FTE hospitalist is the best fit.
“Sustainability, quality, and efficiency are the drivers for NPP/MD teams. Increasing pressure to offset program costs is not,” Dr. Wilson says. “You do it because it helps sustain the program, helps with recruiting, and effects your efficiency.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- Medical Group Management Association and the Society of Hospital Medicine. State of Hospital Medicine: 2010 Report Based on 2009 Data. 2010. Philadelphia and Englewood, Colo.
Hospital-Acquired Conditions & The Hospitalist
Hospitalist Neal Axon, MD, first became aware of an important change in his hospital’s policies last year while attending to an elderly patient the morning after admission to the community hospital where he works part time.
“This new form appeared in the chart requesting a urinalysis for my patient, who’d had a Foley catheter placed,” says Dr. Axon, an assistant professor of medicine at the Medical University of South Carolina in Charleston. “I didn’t know why, so I asked. I was told that it was now necessary to document that there was no UTI present on admission.” He asked the charge nurse, “So what do I do now that the catheter has been in place for 12 hours and has colonization without a true infection?”
The next thing he heard: silence.
The new form Dr. Axon encountered was an outgrowth of the requirements of the Deficit Reduction Act (DRA) of 2005, which ordered Medicare to withhold additional hospital payments for hospital-acquired complications (HAC) developed during a hospital stay. One result of the new rule is that much of a hospital’s response to these initiatives has been placed in the hands of the hospitalist. From accurate documentation of complications already present on admission (POA), to confirming that guidelines for treatment are being followed, to taking the lead on review of staff practices and education, hospitalists are in a position to have a wide-ranging impact on patient care and the financial health of their institutions.
Congress Pushes Reforms
In order for Medicare to not provide a reimbursement, an HAC has to be high-cost and/or high-volume, result in the assignment of the case to a higher payment when present as a secondary diagnosis, and “could reasonably be prevented through the application of evidence-based guidelines,” says Barry Straube, MD, chief medical officer and director of the Office of Clinical Standards and Quality at the Centers for Medicare and Medicaid Services (CMS). “CMS was to implement a process where we would not pay the hospitals additional money for these complications.”
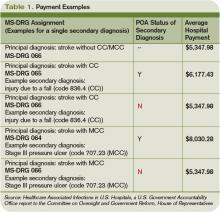
The new rules mean Medicare pays hospitals on the basis of Medicare Severity Diagnostic-Related Groups (MS-DRG), which better reflect the complexity of a patient’s illness. The biggest change was a three-tiered payment schedule: a base level for the diagnosis, a second level adding money to reflect the presence of comorbidities and complications, and a third for major complications and comorbidities (see Table 1, p. 31).
“Instituting HACs means that hospitals would no longer receive the comorbidity and complication payments if the only reason a case qualified for higher payment was the HAC,” Dr. Straube explains. “We did carve out a POA exception for those conditions that were acquired outside of the hospital. HACs only impact additional payments; the hospitals are still paid for the diagnosis that resulted in the hospital admission.”
CMS also identifies three “never events” it won’t reimburse for (see “A Brief History of Never Events,” p. 35): performing the wrong procedure, performing a procedure on the wrong body part, and performing a procedure on the wrong patient. “Neither hospitals nor physicians that are involved in such egregious situations would be paid,” Dr. Straube says.
Preventability: Subject of Controversy
The big questions surrounding HACs: Could they reasonably be prevented through the application of evidence-based guidelines? How preventable are HACs? Who decides if a complication is preventable, and therefore payment for services is withheld?
They’re concerns that are widespread among physicians, hospital administrators, and regulators alike.
“The legislation required the conditions to be ‘reasonably preventable’ using established clinical guidelines,” Dr. Straube says. “We did not have to show 100% prevention. In an imperfect world, they might still take place occasionally, but with good medical care, almost all of these are preventable in this day and age.”
For CMS, the preventable conditions are an either/or situation: Either they existed prior to admission and are subject to payment, or they did not exist at admission and additional payment for the complication will not be made. “HACs do not currently consider a patient’s individual risk for complications,” says Jennifer Meddings, MD, MSc, clinical lecturer and health researcher in the Department of Internal Medicine at the University of Michigan Health System in Ann Arbor. “We know the best strategies to prevent complications in ideal patients, and these are reflected in the HACs. In real life, many of our patients just don’t fit into the guidelines for many reasons—and you have to individualize care.”
Dr. Meddings points to DVT as a prime example. For a certain number of inpatients, the guidelines can be followed to perfection. In other patients (e.g., those with kidney conditions), previous reactions to a medication or an individual’s predisposition to clotting might interfere with treatment. However, CMS doesn’t allow appeals of nonpayment decisions for HACs based on individual circumstances.
Some experts think the rigidness of the payment policy forces physicians to treat patients exactly to guidelines. Even then, payment could be declined if an HAC develops.
“One of the points of most discussion is how preventable some of these are, particularly when choosing those you are no longer going to pay for,” Dr. Meddings says. “Many of the complications currently under review have patients that are at higher risk than others. How much our prevention strategies can alleviate or reduce the risk varies widely among patients.”
Impact on HM Practice
Many of the preventable conditions outlined by CMS do not directly affect hospitalist payment. However, hospitalists often find themselves responsible for properly documenting admission and care.
“The rule changes regarding payment for HACs are only related to hospital payments, and to date, most physicians, including hospitalists, are not directly at financial risk,” says Heidi Wald, MD, MSPH, hospitalist and assistant professor of medicine in the divisions of Health Care Policy Research and General Internal Medicine at the University of Colorado Denver School of Medicine. “Although hospitalists have no financial skin in the game, there are plenty of reasons they would take an interest in addressing HACs in their hospital. In particular, they are often seen as the ‘go-to’ group for quality improvement in their hospitals.”
For example, some HM groups have been active in working with teams of physicians, nurses, and other healthcare providers to address local policies and procedures on prevention of catheter-associated urinary tract infections (UTIs) and DVT.
“This has certainly necessitated a team approach,” says Shaun Frost, MD, FHM, an SHM board member and regional medical director for Cogent Healthcare in St. Paul, Minn. “For many of the HACs that apply to our population of patients, the hospitalist alone cannot be expected to solely execute effective quality improvements. It takes a team effort in that regard, and one that includes many different disciplines.”
The Cogent-affiliated hospitalist group at Temple University Hospital in Philadelphia formed a task force to address issues with catheter-associated UTI. One initiative focused on educating all providers involved in the proper care of the catheters and similar interventions. A secondary focus of the project was an inventory of current practices and procedures.
“It was discovered that we did not have an automatic stop order for Foley catheters, so in some situations, they were likely being left in longer than needed while nursing [staff] tried to contact a physician,” Dr. Frost explains. “We created standardized order sets that include criteria for continuing the catheter. Once the criteria are no longer applicable, nursing will be able to discontinue it.”
Although CMS has only recently turned the spotlight on HACs and never events, hospitalists have been heavily involved in the patient-safety arena for years. “It is not a new phenomenon that hospitalists work for healthcare delivery and healthcare system improvement,” Dr. Meddings says.
Hospital administration at Temple University Hospital recognized the HM group’s quality-improvement (QI) work, and has “specifically charged us with spreading the work we have done in patient safety to the entire house,” Dr. Frost says. “That speaks to the administration’s opinion of the power of the HM program to assist with institution-wide QI initiatives.”
Documentation Is Key
Beyond applying proven methods to avoid HACs, hospitalists can make a difference through documentation. If the hospitalist notes all conditions when the patient first presents to the hospital, additional comorbidity and complication payments should be made.
“The part that probably has the greatest impact on the day-to-day practice of a hospitalist is the increased importance of documentation throughout the hospital episode,” Dr. Meddings says. “If complications are occurring and they are not present in the chart, the coders may not recognize that it has occurred and will not know to include it in the bill. This can have an adverse impact on the hospital and its finances.”
Documentation issues can impact hospital payment in several ways:
- Hospitals might receive additional payment by default if certain HACs are described incorrectly or without sufficient detail (e.g., receiving overpayment because the physician did not indicate a UTI was in fact a catheter-associated UTI);
- As more attention is invested in documenting all conditions POA, hospitals might be coding more comorbidities overall than previously, which also will generate additional payment for hospitals as any POA condition is eligible for increased payment; and
- Hospitals might lose payment when admitting providers fail to adequately document the condition as POA (e.g., a pre-existing decubitus ulcer not detected until the second day of the hospital stay).
The descriptions to be used in coding are very detailed. UTIs, for example, have one code to document the POA assessment, another code to show that a UTI occurred, and a third code to indicate it was catheter-associated. Each code requires appropriate documentation in the chart (see Table 1, above).
The impact hospitalists have on care and payment is not the same across the HAC spectrum. For instance, documenting the presence of pressure ulcers might be easier than distinguishing colonization from infection in those admitted with in-dwelling urinary catheters. Others, such as DVT or vascular catheter-associated infections, are rarely POA unless they are part of the admitting diagnosis.
“This new focus on hospital-acquired conditions may work to the patient’s benefit,” Dr. Meddings says. “The inclusion of pressure ulcers has led to increased attention to skin exams on admission and preventive measures during hospitalizations. In the past, skin exams upon admission may have been given a lower priority, but that has changed.”
Dr. Meddings is concerned that the new rules could force the shifting of resources to areas where the hospital could lose money. If, when, and how many changes will actually take place is still up in the air. “Resource shifting is a concern whenever there is any sort of pay-for-performance attention directed toward one particular complication,” she says. “To balance this, many of the strategies hospitals used to prevent complications are not specific to just the diagnosis that is covered by the HAC.”
Dr. Meddings also hopes the new focus on preventable conditions will have a “halo effect” in the healthcare community. For instance, CMS mandating DVT prevention following orthopedic operations will, hopefully, result in a greater awareness of the problem in other susceptible patients.
POA Indicators
Since hospitalists often perform the initial patient history, physical, and other admission work, they are in the best position to find and document POA indicators (see Table 2, p. below). Proper notes on such things as UTIs present and the state of skin integrity are an important part of making sure the hospital is paid correctly for the care it provides.
Education on the specific definition of each potential HAC is required to help physicians avoid overtreatment of certain conditions, especially UTIs. For example, the Centers for Disease Control and Prevention (CDC) defines all UTIs as symptomatic. Therefore, the screening of all admitted patients, regardless of symptoms, is wasteful and unlikely to help the hospital’s bottom line.
“If you start screening everyone that comes through the door so you don’t miss any pre-existing UTIs, you are going to find a lot of asymptomatic colonization,” Dr. Wald says. “You are also going to spend a lot of money and time on studies and possibly treatments that may not yield many true infections. It is important that physicians know the definition of these HACs to help avoid needless interventions.”
Minimal Loss
Many hospital administrators and physicians were worried when the HAC program was first announced. Much of the stress and concern, however, seems to have dissipated. CMS estimated the HAC program would save Medicare $21 million in fiscal year 2009. Others, such as Peter McNair and colleagues writing in Health Affairs, suggest the actual impact is closer to $1.1 million.1 The CMS-projected impact of the HAC provision in fiscal-year 2009 was $21 million, out of more than $100 billion in payments.
“I think the HACs will not have a major impact because of the way payments are made,” says internist Robert Berenson, MD, a fellow at the Urban Institute in Washington, D.C., who has studied Medicare policy issues extensively, and for two years was in charge of Medicare payment policies at the Health Care Finance Administration, the precursor to CMS. “Patients who have HACs often have another comorbidity that would kick them into a higher payment category regardless of the presence of a hospital-acquired complication. In the end, it is probably more symbolic and unlikely to make a major dent in hospital income—at least at this point.”
Another limitation to CMS nonpayment for HACs is the issue of deciding which conditions are truly preventable. Dr. Berenson questions the ability of the current system to identify many additional complications for which this approach will be feasible.
“CMS has laid out its strategy, suggesting that we should be able to continue increasing the number of conditions for which providers would be paid differently based on quality,” he says. “Many observers question whether there will ever be measurement tools that are robust enough, and there will be a wide agreement on the preventability of enough conditions that this initiative will go very far.”
Although hospitalists might not face a direct financial risk, they still have their hospitals’ best interest—and their reputations—on the line. “Hospitalists care about preventing complications,” Dr. Wald says. “We are very engaged in working with our hospitals to improve care, maximize quality, and minimize cost.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- McNair PD, Luft HS, Bindman AB. Medicare’s policy not to pay for treating hospital-acquired conditions: the impact. Health Aff (Millwood). 2009;28(5):1485-1493.
TOP IMAGE SOURCE: KAREEM RIZKHALLA/ISTOCKPHOTO.COM
Hospitalist Neal Axon, MD, first became aware of an important change in his hospital’s policies last year while attending to an elderly patient the morning after admission to the community hospital where he works part time.
“This new form appeared in the chart requesting a urinalysis for my patient, who’d had a Foley catheter placed,” says Dr. Axon, an assistant professor of medicine at the Medical University of South Carolina in Charleston. “I didn’t know why, so I asked. I was told that it was now necessary to document that there was no UTI present on admission.” He asked the charge nurse, “So what do I do now that the catheter has been in place for 12 hours and has colonization without a true infection?”
The next thing he heard: silence.
The new form Dr. Axon encountered was an outgrowth of the requirements of the Deficit Reduction Act (DRA) of 2005, which ordered Medicare to withhold additional hospital payments for hospital-acquired complications (HAC) developed during a hospital stay. One result of the new rule is that much of a hospital’s response to these initiatives has been placed in the hands of the hospitalist. From accurate documentation of complications already present on admission (POA), to confirming that guidelines for treatment are being followed, to taking the lead on review of staff practices and education, hospitalists are in a position to have a wide-ranging impact on patient care and the financial health of their institutions.
Congress Pushes Reforms
In order for Medicare to not provide a reimbursement, an HAC has to be high-cost and/or high-volume, result in the assignment of the case to a higher payment when present as a secondary diagnosis, and “could reasonably be prevented through the application of evidence-based guidelines,” says Barry Straube, MD, chief medical officer and director of the Office of Clinical Standards and Quality at the Centers for Medicare and Medicaid Services (CMS). “CMS was to implement a process where we would not pay the hospitals additional money for these complications.”
The new rules mean Medicare pays hospitals on the basis of Medicare Severity Diagnostic-Related Groups (MS-DRG), which better reflect the complexity of a patient’s illness. The biggest change was a three-tiered payment schedule: a base level for the diagnosis, a second level adding money to reflect the presence of comorbidities and complications, and a third for major complications and comorbidities (see Table 1, p. 31).
“Instituting HACs means that hospitals would no longer receive the comorbidity and complication payments if the only reason a case qualified for higher payment was the HAC,” Dr. Straube explains. “We did carve out a POA exception for those conditions that were acquired outside of the hospital. HACs only impact additional payments; the hospitals are still paid for the diagnosis that resulted in the hospital admission.”
CMS also identifies three “never events” it won’t reimburse for (see “A Brief History of Never Events,” p. 35): performing the wrong procedure, performing a procedure on the wrong body part, and performing a procedure on the wrong patient. “Neither hospitals nor physicians that are involved in such egregious situations would be paid,” Dr. Straube says.
Preventability: Subject of Controversy
The big questions surrounding HACs: Could they reasonably be prevented through the application of evidence-based guidelines? How preventable are HACs? Who decides if a complication is preventable, and therefore payment for services is withheld?
They’re concerns that are widespread among physicians, hospital administrators, and regulators alike.
“The legislation required the conditions to be ‘reasonably preventable’ using established clinical guidelines,” Dr. Straube says. “We did not have to show 100% prevention. In an imperfect world, they might still take place occasionally, but with good medical care, almost all of these are preventable in this day and age.”
For CMS, the preventable conditions are an either/or situation: Either they existed prior to admission and are subject to payment, or they did not exist at admission and additional payment for the complication will not be made. “HACs do not currently consider a patient’s individual risk for complications,” says Jennifer Meddings, MD, MSc, clinical lecturer and health researcher in the Department of Internal Medicine at the University of Michigan Health System in Ann Arbor. “We know the best strategies to prevent complications in ideal patients, and these are reflected in the HACs. In real life, many of our patients just don’t fit into the guidelines for many reasons—and you have to individualize care.”
Dr. Meddings points to DVT as a prime example. For a certain number of inpatients, the guidelines can be followed to perfection. In other patients (e.g., those with kidney conditions), previous reactions to a medication or an individual’s predisposition to clotting might interfere with treatment. However, CMS doesn’t allow appeals of nonpayment decisions for HACs based on individual circumstances.
Some experts think the rigidness of the payment policy forces physicians to treat patients exactly to guidelines. Even then, payment could be declined if an HAC develops.
“One of the points of most discussion is how preventable some of these are, particularly when choosing those you are no longer going to pay for,” Dr. Meddings says. “Many of the complications currently under review have patients that are at higher risk than others. How much our prevention strategies can alleviate or reduce the risk varies widely among patients.”
Impact on HM Practice
Many of the preventable conditions outlined by CMS do not directly affect hospitalist payment. However, hospitalists often find themselves responsible for properly documenting admission and care.
“The rule changes regarding payment for HACs are only related to hospital payments, and to date, most physicians, including hospitalists, are not directly at financial risk,” says Heidi Wald, MD, MSPH, hospitalist and assistant professor of medicine in the divisions of Health Care Policy Research and General Internal Medicine at the University of Colorado Denver School of Medicine. “Although hospitalists have no financial skin in the game, there are plenty of reasons they would take an interest in addressing HACs in their hospital. In particular, they are often seen as the ‘go-to’ group for quality improvement in their hospitals.”
For example, some HM groups have been active in working with teams of physicians, nurses, and other healthcare providers to address local policies and procedures on prevention of catheter-associated urinary tract infections (UTIs) and DVT.
“This has certainly necessitated a team approach,” says Shaun Frost, MD, FHM, an SHM board member and regional medical director for Cogent Healthcare in St. Paul, Minn. “For many of the HACs that apply to our population of patients, the hospitalist alone cannot be expected to solely execute effective quality improvements. It takes a team effort in that regard, and one that includes many different disciplines.”
The Cogent-affiliated hospitalist group at Temple University Hospital in Philadelphia formed a task force to address issues with catheter-associated UTI. One initiative focused on educating all providers involved in the proper care of the catheters and similar interventions. A secondary focus of the project was an inventory of current practices and procedures.
“It was discovered that we did not have an automatic stop order for Foley catheters, so in some situations, they were likely being left in longer than needed while nursing [staff] tried to contact a physician,” Dr. Frost explains. “We created standardized order sets that include criteria for continuing the catheter. Once the criteria are no longer applicable, nursing will be able to discontinue it.”
Although CMS has only recently turned the spotlight on HACs and never events, hospitalists have been heavily involved in the patient-safety arena for years. “It is not a new phenomenon that hospitalists work for healthcare delivery and healthcare system improvement,” Dr. Meddings says.
Hospital administration at Temple University Hospital recognized the HM group’s quality-improvement (QI) work, and has “specifically charged us with spreading the work we have done in patient safety to the entire house,” Dr. Frost says. “That speaks to the administration’s opinion of the power of the HM program to assist with institution-wide QI initiatives.”
Documentation Is Key
Beyond applying proven methods to avoid HACs, hospitalists can make a difference through documentation. If the hospitalist notes all conditions when the patient first presents to the hospital, additional comorbidity and complication payments should be made.
“The part that probably has the greatest impact on the day-to-day practice of a hospitalist is the increased importance of documentation throughout the hospital episode,” Dr. Meddings says. “If complications are occurring and they are not present in the chart, the coders may not recognize that it has occurred and will not know to include it in the bill. This can have an adverse impact on the hospital and its finances.”
Documentation issues can impact hospital payment in several ways:
- Hospitals might receive additional payment by default if certain HACs are described incorrectly or without sufficient detail (e.g., receiving overpayment because the physician did not indicate a UTI was in fact a catheter-associated UTI);
- As more attention is invested in documenting all conditions POA, hospitals might be coding more comorbidities overall than previously, which also will generate additional payment for hospitals as any POA condition is eligible for increased payment; and
- Hospitals might lose payment when admitting providers fail to adequately document the condition as POA (e.g., a pre-existing decubitus ulcer not detected until the second day of the hospital stay).
The descriptions to be used in coding are very detailed. UTIs, for example, have one code to document the POA assessment, another code to show that a UTI occurred, and a third code to indicate it was catheter-associated. Each code requires appropriate documentation in the chart (see Table 1, above).
The impact hospitalists have on care and payment is not the same across the HAC spectrum. For instance, documenting the presence of pressure ulcers might be easier than distinguishing colonization from infection in those admitted with in-dwelling urinary catheters. Others, such as DVT or vascular catheter-associated infections, are rarely POA unless they are part of the admitting diagnosis.
“This new focus on hospital-acquired conditions may work to the patient’s benefit,” Dr. Meddings says. “The inclusion of pressure ulcers has led to increased attention to skin exams on admission and preventive measures during hospitalizations. In the past, skin exams upon admission may have been given a lower priority, but that has changed.”
Dr. Meddings is concerned that the new rules could force the shifting of resources to areas where the hospital could lose money. If, when, and how many changes will actually take place is still up in the air. “Resource shifting is a concern whenever there is any sort of pay-for-performance attention directed toward one particular complication,” she says. “To balance this, many of the strategies hospitals used to prevent complications are not specific to just the diagnosis that is covered by the HAC.”
Dr. Meddings also hopes the new focus on preventable conditions will have a “halo effect” in the healthcare community. For instance, CMS mandating DVT prevention following orthopedic operations will, hopefully, result in a greater awareness of the problem in other susceptible patients.
POA Indicators
Since hospitalists often perform the initial patient history, physical, and other admission work, they are in the best position to find and document POA indicators (see Table 2, p. below). Proper notes on such things as UTIs present and the state of skin integrity are an important part of making sure the hospital is paid correctly for the care it provides.
Education on the specific definition of each potential HAC is required to help physicians avoid overtreatment of certain conditions, especially UTIs. For example, the Centers for Disease Control and Prevention (CDC) defines all UTIs as symptomatic. Therefore, the screening of all admitted patients, regardless of symptoms, is wasteful and unlikely to help the hospital’s bottom line.
“If you start screening everyone that comes through the door so you don’t miss any pre-existing UTIs, you are going to find a lot of asymptomatic colonization,” Dr. Wald says. “You are also going to spend a lot of money and time on studies and possibly treatments that may not yield many true infections. It is important that physicians know the definition of these HACs to help avoid needless interventions.”
Minimal Loss
Many hospital administrators and physicians were worried when the HAC program was first announced. Much of the stress and concern, however, seems to have dissipated. CMS estimated the HAC program would save Medicare $21 million in fiscal year 2009. Others, such as Peter McNair and colleagues writing in Health Affairs, suggest the actual impact is closer to $1.1 million.1 The CMS-projected impact of the HAC provision in fiscal-year 2009 was $21 million, out of more than $100 billion in payments.
“I think the HACs will not have a major impact because of the way payments are made,” says internist Robert Berenson, MD, a fellow at the Urban Institute in Washington, D.C., who has studied Medicare policy issues extensively, and for two years was in charge of Medicare payment policies at the Health Care Finance Administration, the precursor to CMS. “Patients who have HACs often have another comorbidity that would kick them into a higher payment category regardless of the presence of a hospital-acquired complication. In the end, it is probably more symbolic and unlikely to make a major dent in hospital income—at least at this point.”
Another limitation to CMS nonpayment for HACs is the issue of deciding which conditions are truly preventable. Dr. Berenson questions the ability of the current system to identify many additional complications for which this approach will be feasible.
“CMS has laid out its strategy, suggesting that we should be able to continue increasing the number of conditions for which providers would be paid differently based on quality,” he says. “Many observers question whether there will ever be measurement tools that are robust enough, and there will be a wide agreement on the preventability of enough conditions that this initiative will go very far.”
Although hospitalists might not face a direct financial risk, they still have their hospitals’ best interest—and their reputations—on the line. “Hospitalists care about preventing complications,” Dr. Wald says. “We are very engaged in working with our hospitals to improve care, maximize quality, and minimize cost.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- McNair PD, Luft HS, Bindman AB. Medicare’s policy not to pay for treating hospital-acquired conditions: the impact. Health Aff (Millwood). 2009;28(5):1485-1493.
TOP IMAGE SOURCE: KAREEM RIZKHALLA/ISTOCKPHOTO.COM
Hospitalist Neal Axon, MD, first became aware of an important change in his hospital’s policies last year while attending to an elderly patient the morning after admission to the community hospital where he works part time.
“This new form appeared in the chart requesting a urinalysis for my patient, who’d had a Foley catheter placed,” says Dr. Axon, an assistant professor of medicine at the Medical University of South Carolina in Charleston. “I didn’t know why, so I asked. I was told that it was now necessary to document that there was no UTI present on admission.” He asked the charge nurse, “So what do I do now that the catheter has been in place for 12 hours and has colonization without a true infection?”
The next thing he heard: silence.
The new form Dr. Axon encountered was an outgrowth of the requirements of the Deficit Reduction Act (DRA) of 2005, which ordered Medicare to withhold additional hospital payments for hospital-acquired complications (HAC) developed during a hospital stay. One result of the new rule is that much of a hospital’s response to these initiatives has been placed in the hands of the hospitalist. From accurate documentation of complications already present on admission (POA), to confirming that guidelines for treatment are being followed, to taking the lead on review of staff practices and education, hospitalists are in a position to have a wide-ranging impact on patient care and the financial health of their institutions.
Congress Pushes Reforms
In order for Medicare to not provide a reimbursement, an HAC has to be high-cost and/or high-volume, result in the assignment of the case to a higher payment when present as a secondary diagnosis, and “could reasonably be prevented through the application of evidence-based guidelines,” says Barry Straube, MD, chief medical officer and director of the Office of Clinical Standards and Quality at the Centers for Medicare and Medicaid Services (CMS). “CMS was to implement a process where we would not pay the hospitals additional money for these complications.”
The new rules mean Medicare pays hospitals on the basis of Medicare Severity Diagnostic-Related Groups (MS-DRG), which better reflect the complexity of a patient’s illness. The biggest change was a three-tiered payment schedule: a base level for the diagnosis, a second level adding money to reflect the presence of comorbidities and complications, and a third for major complications and comorbidities (see Table 1, p. 31).
“Instituting HACs means that hospitals would no longer receive the comorbidity and complication payments if the only reason a case qualified for higher payment was the HAC,” Dr. Straube explains. “We did carve out a POA exception for those conditions that were acquired outside of the hospital. HACs only impact additional payments; the hospitals are still paid for the diagnosis that resulted in the hospital admission.”
CMS also identifies three “never events” it won’t reimburse for (see “A Brief History of Never Events,” p. 35): performing the wrong procedure, performing a procedure on the wrong body part, and performing a procedure on the wrong patient. “Neither hospitals nor physicians that are involved in such egregious situations would be paid,” Dr. Straube says.
Preventability: Subject of Controversy
The big questions surrounding HACs: Could they reasonably be prevented through the application of evidence-based guidelines? How preventable are HACs? Who decides if a complication is preventable, and therefore payment for services is withheld?
They’re concerns that are widespread among physicians, hospital administrators, and regulators alike.
“The legislation required the conditions to be ‘reasonably preventable’ using established clinical guidelines,” Dr. Straube says. “We did not have to show 100% prevention. In an imperfect world, they might still take place occasionally, but with good medical care, almost all of these are preventable in this day and age.”
For CMS, the preventable conditions are an either/or situation: Either they existed prior to admission and are subject to payment, or they did not exist at admission and additional payment for the complication will not be made. “HACs do not currently consider a patient’s individual risk for complications,” says Jennifer Meddings, MD, MSc, clinical lecturer and health researcher in the Department of Internal Medicine at the University of Michigan Health System in Ann Arbor. “We know the best strategies to prevent complications in ideal patients, and these are reflected in the HACs. In real life, many of our patients just don’t fit into the guidelines for many reasons—and you have to individualize care.”
Dr. Meddings points to DVT as a prime example. For a certain number of inpatients, the guidelines can be followed to perfection. In other patients (e.g., those with kidney conditions), previous reactions to a medication or an individual’s predisposition to clotting might interfere with treatment. However, CMS doesn’t allow appeals of nonpayment decisions for HACs based on individual circumstances.
Some experts think the rigidness of the payment policy forces physicians to treat patients exactly to guidelines. Even then, payment could be declined if an HAC develops.
“One of the points of most discussion is how preventable some of these are, particularly when choosing those you are no longer going to pay for,” Dr. Meddings says. “Many of the complications currently under review have patients that are at higher risk than others. How much our prevention strategies can alleviate or reduce the risk varies widely among patients.”
Impact on HM Practice
Many of the preventable conditions outlined by CMS do not directly affect hospitalist payment. However, hospitalists often find themselves responsible for properly documenting admission and care.
“The rule changes regarding payment for HACs are only related to hospital payments, and to date, most physicians, including hospitalists, are not directly at financial risk,” says Heidi Wald, MD, MSPH, hospitalist and assistant professor of medicine in the divisions of Health Care Policy Research and General Internal Medicine at the University of Colorado Denver School of Medicine. “Although hospitalists have no financial skin in the game, there are plenty of reasons they would take an interest in addressing HACs in their hospital. In particular, they are often seen as the ‘go-to’ group for quality improvement in their hospitals.”
For example, some HM groups have been active in working with teams of physicians, nurses, and other healthcare providers to address local policies and procedures on prevention of catheter-associated urinary tract infections (UTIs) and DVT.
“This has certainly necessitated a team approach,” says Shaun Frost, MD, FHM, an SHM board member and regional medical director for Cogent Healthcare in St. Paul, Minn. “For many of the HACs that apply to our population of patients, the hospitalist alone cannot be expected to solely execute effective quality improvements. It takes a team effort in that regard, and one that includes many different disciplines.”
The Cogent-affiliated hospitalist group at Temple University Hospital in Philadelphia formed a task force to address issues with catheter-associated UTI. One initiative focused on educating all providers involved in the proper care of the catheters and similar interventions. A secondary focus of the project was an inventory of current practices and procedures.
“It was discovered that we did not have an automatic stop order for Foley catheters, so in some situations, they were likely being left in longer than needed while nursing [staff] tried to contact a physician,” Dr. Frost explains. “We created standardized order sets that include criteria for continuing the catheter. Once the criteria are no longer applicable, nursing will be able to discontinue it.”
Although CMS has only recently turned the spotlight on HACs and never events, hospitalists have been heavily involved in the patient-safety arena for years. “It is not a new phenomenon that hospitalists work for healthcare delivery and healthcare system improvement,” Dr. Meddings says.
Hospital administration at Temple University Hospital recognized the HM group’s quality-improvement (QI) work, and has “specifically charged us with spreading the work we have done in patient safety to the entire house,” Dr. Frost says. “That speaks to the administration’s opinion of the power of the HM program to assist with institution-wide QI initiatives.”
Documentation Is Key
Beyond applying proven methods to avoid HACs, hospitalists can make a difference through documentation. If the hospitalist notes all conditions when the patient first presents to the hospital, additional comorbidity and complication payments should be made.
“The part that probably has the greatest impact on the day-to-day practice of a hospitalist is the increased importance of documentation throughout the hospital episode,” Dr. Meddings says. “If complications are occurring and they are not present in the chart, the coders may not recognize that it has occurred and will not know to include it in the bill. This can have an adverse impact on the hospital and its finances.”
Documentation issues can impact hospital payment in several ways:
- Hospitals might receive additional payment by default if certain HACs are described incorrectly or without sufficient detail (e.g., receiving overpayment because the physician did not indicate a UTI was in fact a catheter-associated UTI);
- As more attention is invested in documenting all conditions POA, hospitals might be coding more comorbidities overall than previously, which also will generate additional payment for hospitals as any POA condition is eligible for increased payment; and
- Hospitals might lose payment when admitting providers fail to adequately document the condition as POA (e.g., a pre-existing decubitus ulcer not detected until the second day of the hospital stay).
The descriptions to be used in coding are very detailed. UTIs, for example, have one code to document the POA assessment, another code to show that a UTI occurred, and a third code to indicate it was catheter-associated. Each code requires appropriate documentation in the chart (see Table 1, above).
The impact hospitalists have on care and payment is not the same across the HAC spectrum. For instance, documenting the presence of pressure ulcers might be easier than distinguishing colonization from infection in those admitted with in-dwelling urinary catheters. Others, such as DVT or vascular catheter-associated infections, are rarely POA unless they are part of the admitting diagnosis.
“This new focus on hospital-acquired conditions may work to the patient’s benefit,” Dr. Meddings says. “The inclusion of pressure ulcers has led to increased attention to skin exams on admission and preventive measures during hospitalizations. In the past, skin exams upon admission may have been given a lower priority, but that has changed.”
Dr. Meddings is concerned that the new rules could force the shifting of resources to areas where the hospital could lose money. If, when, and how many changes will actually take place is still up in the air. “Resource shifting is a concern whenever there is any sort of pay-for-performance attention directed toward one particular complication,” she says. “To balance this, many of the strategies hospitals used to prevent complications are not specific to just the diagnosis that is covered by the HAC.”
Dr. Meddings also hopes the new focus on preventable conditions will have a “halo effect” in the healthcare community. For instance, CMS mandating DVT prevention following orthopedic operations will, hopefully, result in a greater awareness of the problem in other susceptible patients.
POA Indicators
Since hospitalists often perform the initial patient history, physical, and other admission work, they are in the best position to find and document POA indicators (see Table 2, p. below). Proper notes on such things as UTIs present and the state of skin integrity are an important part of making sure the hospital is paid correctly for the care it provides.
Education on the specific definition of each potential HAC is required to help physicians avoid overtreatment of certain conditions, especially UTIs. For example, the Centers for Disease Control and Prevention (CDC) defines all UTIs as symptomatic. Therefore, the screening of all admitted patients, regardless of symptoms, is wasteful and unlikely to help the hospital’s bottom line.
“If you start screening everyone that comes through the door so you don’t miss any pre-existing UTIs, you are going to find a lot of asymptomatic colonization,” Dr. Wald says. “You are also going to spend a lot of money and time on studies and possibly treatments that may not yield many true infections. It is important that physicians know the definition of these HACs to help avoid needless interventions.”
Minimal Loss
Many hospital administrators and physicians were worried when the HAC program was first announced. Much of the stress and concern, however, seems to have dissipated. CMS estimated the HAC program would save Medicare $21 million in fiscal year 2009. Others, such as Peter McNair and colleagues writing in Health Affairs, suggest the actual impact is closer to $1.1 million.1 The CMS-projected impact of the HAC provision in fiscal-year 2009 was $21 million, out of more than $100 billion in payments.
“I think the HACs will not have a major impact because of the way payments are made,” says internist Robert Berenson, MD, a fellow at the Urban Institute in Washington, D.C., who has studied Medicare policy issues extensively, and for two years was in charge of Medicare payment policies at the Health Care Finance Administration, the precursor to CMS. “Patients who have HACs often have another comorbidity that would kick them into a higher payment category regardless of the presence of a hospital-acquired complication. In the end, it is probably more symbolic and unlikely to make a major dent in hospital income—at least at this point.”
Another limitation to CMS nonpayment for HACs is the issue of deciding which conditions are truly preventable. Dr. Berenson questions the ability of the current system to identify many additional complications for which this approach will be feasible.
“CMS has laid out its strategy, suggesting that we should be able to continue increasing the number of conditions for which providers would be paid differently based on quality,” he says. “Many observers question whether there will ever be measurement tools that are robust enough, and there will be a wide agreement on the preventability of enough conditions that this initiative will go very far.”
Although hospitalists might not face a direct financial risk, they still have their hospitals’ best interest—and their reputations—on the line. “Hospitalists care about preventing complications,” Dr. Wald says. “We are very engaged in working with our hospitals to improve care, maximize quality, and minimize cost.” TH
Kurt Ullman is a freelance medical writer based in Indiana.
Reference
- McNair PD, Luft HS, Bindman AB. Medicare’s policy not to pay for treating hospital-acquired conditions: the impact. Health Aff (Millwood). 2009;28(5):1485-1493.
TOP IMAGE SOURCE: KAREEM RIZKHALLA/ISTOCKPHOTO.COM
Subcutaneous Rehydration Useful Alternative in Kids
Obtaining intravenous access to treat dehydrated infants and youths can be a challenge for the everyday hospitalist. One alternative is subcutaneous rehydration. Interim results from the Increased Flow Utilizing Subcutaneously-Enabled Pediatric Rehydration I (INFUSE) study presented at the recent American College of Emergency Physicians meeting in Boston suggests subcutaneous rehydration as a viable alternative in children with mild to moderate dehydration.
Complete study results were published in the October issue of Pediatrics (doi:10.1542/peds.2008-3588).
"The study included 51 children admitted to emergency rooms throughout the country who were given Hylenex (hyaluronidase human injection-Baxter)," says Sharon Mace, MD, director of pediatric education and quality improvement at the Cleveland Clinic. Hylenex is a purified preparation of the hyaluronidase enzyme; after being administered subcutaneously, it facilitates the infusion of subcutaneous
fluids. "The majority of the patients were able to be given subcutaneous fluids and then sent home," Dr. Mace adds. "In 86% of patients, the catheter was successfully placed on the first attempt. This contrasts to other studies suggesting that the success rate for IV placement in young children is 50% at best."
Shawn L. Ralston, MD, a pediatric hospitalist at the University of Texas Health Sciences Center in San Antonio, notes that most of the time the question of access already has been addressed in the ED. However, there is a subset of medically complex patients in which subcutaneous rehydration is a useful technique to consider.
"The great thing for the hospitalist is that subcutaneous rehydration is almost always one-stick," Dr. Ralston says. "We also find that after rehydration the kids are able to soon begin taking nutrition and water by mouth again."
According to Dr. Mace, only such minor adverse events as swelling and redness at the injection site were observed. No allergic responses were noticed.
Obtaining intravenous access to treat dehydrated infants and youths can be a challenge for the everyday hospitalist. One alternative is subcutaneous rehydration. Interim results from the Increased Flow Utilizing Subcutaneously-Enabled Pediatric Rehydration I (INFUSE) study presented at the recent American College of Emergency Physicians meeting in Boston suggests subcutaneous rehydration as a viable alternative in children with mild to moderate dehydration.
Complete study results were published in the October issue of Pediatrics (doi:10.1542/peds.2008-3588).
"The study included 51 children admitted to emergency rooms throughout the country who were given Hylenex (hyaluronidase human injection-Baxter)," says Sharon Mace, MD, director of pediatric education and quality improvement at the Cleveland Clinic. Hylenex is a purified preparation of the hyaluronidase enzyme; after being administered subcutaneously, it facilitates the infusion of subcutaneous
fluids. "The majority of the patients were able to be given subcutaneous fluids and then sent home," Dr. Mace adds. "In 86% of patients, the catheter was successfully placed on the first attempt. This contrasts to other studies suggesting that the success rate for IV placement in young children is 50% at best."
Shawn L. Ralston, MD, a pediatric hospitalist at the University of Texas Health Sciences Center in San Antonio, notes that most of the time the question of access already has been addressed in the ED. However, there is a subset of medically complex patients in which subcutaneous rehydration is a useful technique to consider.
"The great thing for the hospitalist is that subcutaneous rehydration is almost always one-stick," Dr. Ralston says. "We also find that after rehydration the kids are able to soon begin taking nutrition and water by mouth again."
According to Dr. Mace, only such minor adverse events as swelling and redness at the injection site were observed. No allergic responses were noticed.
Obtaining intravenous access to treat dehydrated infants and youths can be a challenge for the everyday hospitalist. One alternative is subcutaneous rehydration. Interim results from the Increased Flow Utilizing Subcutaneously-Enabled Pediatric Rehydration I (INFUSE) study presented at the recent American College of Emergency Physicians meeting in Boston suggests subcutaneous rehydration as a viable alternative in children with mild to moderate dehydration.
Complete study results were published in the October issue of Pediatrics (doi:10.1542/peds.2008-3588).
"The study included 51 children admitted to emergency rooms throughout the country who were given Hylenex (hyaluronidase human injection-Baxter)," says Sharon Mace, MD, director of pediatric education and quality improvement at the Cleveland Clinic. Hylenex is a purified preparation of the hyaluronidase enzyme; after being administered subcutaneously, it facilitates the infusion of subcutaneous
fluids. "The majority of the patients were able to be given subcutaneous fluids and then sent home," Dr. Mace adds. "In 86% of patients, the catheter was successfully placed on the first attempt. This contrasts to other studies suggesting that the success rate for IV placement in young children is 50% at best."
Shawn L. Ralston, MD, a pediatric hospitalist at the University of Texas Health Sciences Center in San Antonio, notes that most of the time the question of access already has been addressed in the ED. However, there is a subset of medically complex patients in which subcutaneous rehydration is a useful technique to consider.
"The great thing for the hospitalist is that subcutaneous rehydration is almost always one-stick," Dr. Ralston says. "We also find that after rehydration the kids are able to soon begin taking nutrition and water by mouth again."
According to Dr. Mace, only such minor adverse events as swelling and redness at the injection site were observed. No allergic responses were noticed.
Unclear Expectations
As flu season descends on North America, hospitalists from Boston to the San Francisco Bay are concerned about what might happen when normal seasonal influenza hospital admissions are added to new cases of the novel influenza A (H1N1) virus.
Perhaps the most basic, still-unanswered question is how the addition of novel H1N1 virus affects the severity of the upcoming flu season. From April 15 to July 24 of this year, states reported 43,771 confirmed and probable cases of novel H1N1 infection. Of the cases reported, 5,011 people were hospitalized and 302 died. After July 24, the CDC stopped counting novel H1N1 as separate flu cases.
“We are expecting increased illness during the regular flu season, because we think both the novel H1N1 and seasonal flu strains will cause illness in the population,” says Artealia Gilliard, a spokesperson for the U.S. Centers for Disease Control and Prevention (CDC) in Atlanta. “The biggest problem we are having is that there is no set number we can give for planning purposes. We can’t say go out and prepare for X percent more illness, because there is no scientifically sound way to arrive at a number.”
Another concern is that little guidance is available on how severe the novel virus will be. Gilliard notes that the World Health Organization (WHO) gave novel H1N1 the pandemic designation because of its ease of transmission, not the severity of the disease. Although the CDC expects more illness, it is not yet clear how many people will be made sick enough to be cared for by a hospitalist.
“The epidemiology of this illness and prevention issues related to this newly emerging virus are still being studied, making it very difficult to anticipate the staffing needs for the upcoming flu season,” says Irina Schiopescu, MD, a hospitalist and infectious-disease specialist at Roane Medical Center in Harriman, Tenn. “Hospitalists will be among the many front-line healthcare workers who provide direct, bedside clinical care to patients with suspected or confirmed H1N1 influenza.”
Most of the nation’s hospitals spent the summer preparing for another pandemic. Hospitalists have assessed their needs, too, and HM programs are focusing on a diverse set of concerns: prevention education for hospital-based employees, patient management updates, and expected personnel shortages.
“We have been planning for the worst but hoping for the best,” says Julia Wright, MD, FHM, head of the section of hospital medicine at the University of Wisconsin Hospitals in Madison and a member of Team Hospitalist. “Our task group for the upcoming flu season includes all critical-care services, nursing, supply-chain management, and human resources, as well as other appropriate specialties, such as infection control.”
Another Wild Card
How well the vaccination campaign works will have an impact on the incidence of novel H1N1 influenza. Some have expressed concerns about compliance issues in the community, as individuals will need an extra flu shot in addition to the yearly vaccination for seasonal flu strains. The concerns could double if current ongoing clinical trials suggest that two vaccine administrations are required for full protection from the H1N1 virus.
There also is concern about the availability of vaccines, especially in the early stages. As of early September, Robin Robinson, PhD, director of the Biological Advanced Research and Development Authority (BARDA) at the U.S. Department of Health and Human Services (HHS), announced that manufacturing problems would mean only 45 million doses would be available by Oct. 15, compared with the 120 million doses originally projected. However, HHS says the 195 million doses the U.S. government ordered should be available by the December deadline for final delivery.1
Nevertheless, physicians should expect large-scale vaccination initiatives at their hospitals this fall. Additionally, hospitals are expected to require that healthcare workers, including hospitalists, receive their shots during the first wave of inoculations. “At our facility, we have the potential to give 100,000 or more vaccinations over a very short period of time,” says Patty Skoglund, RN, administrative director for disaster preparedness at Scripps Health in San Diego. “This is in addition to supporting vaccination efforts in the community.”
Southern Hemisphere
The Southern Hemisphere is wrapping up its flu season, and often, experiences south of the equator are a harbinger of what might come in the Northern Hemisphere. So far, the WHO says the Southern Hemisphere’s flu season has been characterized by normal respiratory disease numbers. The impact and severity is still being
evaluated, but it appeared only slightly worse than normal in most places. Hospitals did see increased admissions (see Figure 1, p. 5) requiring respiratory critical care.2 Yet the lack of firm guidance has made planning difficult for HM groups and the U.S. hospitals they work in.
It will be important for hospitalists to stay up to date with a potentially developing situation, especially in the early stages of the flu season. Many current CDC guidelines for treatment, prevention, and control are in interim stages, with more guidance to come as the science firms up. (see “Vaccination Priorities,” right)
“As we get closer to the flu season, we should be able to make specific suggestions and get a better idea of the probable incidence,” says Gilliard. “Novel H1N1 has caused significant illness outside of the regular season. When the temperature changes, will the incidence increase or decrease? We have to get more experience before we will know.”
Information Hotline
Hospitals are working to ensure that there are open lines of communication with key personnel, an important first step in infectious-disease control. It will be necessary to facilitate the timely dispersal of new information on guidelines and treatment considerations to multiple audiences throughout the hospital as they are released. In addition, flu incidence and severity updates will be vital.
“It is imperative that physicians know what is going on in their community and beyond,” says Dr. Schiopescu. “The CDC and the Infectious Disease Society of America (IDSA) are resources for treatment guidelines and information on the spread and severity of both the novel H1N1 and seasonal virus strains. Closer to home, both state and local health boards can help with a more focused view of what is happening in the community.”
Patient placement will be another concern for hospitalists in the event of a widespread outbreak. The current CDC patient care guidelines say that all patients with confirmed or suspected H1N1 infection must be isolated. Although they can be scattered in rooms throughout the hospital, it is strongly suggested that they be placed together as a cohort, if possible.
“Our hospital is looking into designating special areas of the hospital to accept influenza patients,” Dr. Wright says. “We can then give the staff special training on treatment and prevention, give better access to materials and supplies in a single location, and also minimize the time lost to physicians going from one patient to another.”
Staffing Concerns
One of the biggest concerns to HM groups is keeping their own areas of the hospital properly staffed. In addition to the possibility of higher acuity and admissions affecting coverage needs, most experts are suggesting employee absentee rates upward of 40%. To further complicate the picture, interim CDC guidelines say healthcare workers should be off work 24 hours after a fever subsides or seven days, whichever is longer. This guidance, however, could change as the CDC obtains and reviews more information.
“We are a small group of only four physicians,” says Dr. Schiopescu, whose HM group works a six-day on, six-day off schedule for about 85 encounters per week at her 50-bed hospital. “We may need to work additional shifts and be available to be called in early, should the need arise. We have also done some cross-training so that community physicians can help if needed. At worst, we can pull resources from our sister hospitals in the system.”
—Irina Schiopescu, MD, infectious-disease specialist, Roane Medical Center, Harriman, Tenn.
Some hospitals have been able to flex up and increase staffing levels before the season begins. “In addition to adding three full-time equivalent staff, we have actively looked for other specialties, such as internal medicine or family practice, that have the proper skill sets should the need arise,” says Dr. Wright, whose program covers 75% of the 471 medical beds at UW Hospital. “We have also developed a set of protocols to streamline treatment of these patients, no matter who may be taking care of them.”
Scripps is surveying its employees to identify family and other outside obligations that could lead to call-outs and staffing shortages. Hospital administrators expect that the information will identify physicians who might not be able to come to work. The hospital also implemented systems that will allow them to bring in extra people—and get them deployed quickly—from such state and federal support resources as the Public Health Service and the National Disaster Medical System staffs.
“Balancing the needs of the various areas will be tricky at times,” Dr. Wright says. “We have to move people around while making sure we are not leaving one area dangerously understaffed.”
Education Imperative
Educating health workers is of the utmost importance before and during the flu season. A wide range of staff training will be required: reinforcing cough etiquette and hand-washing requirements through completely new procedures. This will be important for patient treatment and patient safety, two areas that intersect in hospitalists every day. In addition, this flu season will require a heightened level of personal responsibility from health workers. “Teaching needs are adding to the burden,” says Skoglund, the administrative director at Scripps. “Unfortunately, it is not as simple as sending out a memo to the staff and affiliated physicians.”
Training is a moving target, at least initially. Clinical employees will need to be trained on treatment and prevention guidelines as they are released, with special emphasis on keeping up with changes as the season progresses and lessons are learned.
“In the past, the CDC suggested using a N-95 respirator for all patients with novel H1N1,” Dr. Schiopescu says. “Currently, that has changed to approved use of a regular surgical mask, unless performing intubation or bronchoscopy.”
Despite the best efforts of the CDC, WHO, and other health organizations, there is no real clear idea of what to expect during the next flu season.
“What is known is that the hospitalist will be on the front lines, involved in the treatment of the sickest patients,” Dr. Wright says. TH
Kurt Ullman is a freelance writer based in Indiana.
Image Source: MAMMAMAART/ISTOCKPHOTO.COM
References
- Officials lower expectations for size of first novel flu vaccine deliveries. Center for Infectious Disease Research & Policy Web site. Available at: www.cidrap.umn.edu/cidrap/content/influenza/swineflu/news/aug1409vaccine.html. Accessed Aug. 20, 2009.
- Pandemic (H1N1) 2009: update 61. WHO Web site. Available at: www.who.int/csr/don/2009_08_12/en/index.html. Accessed Aug. 24, 2009.
As flu season descends on North America, hospitalists from Boston to the San Francisco Bay are concerned about what might happen when normal seasonal influenza hospital admissions are added to new cases of the novel influenza A (H1N1) virus.
Perhaps the most basic, still-unanswered question is how the addition of novel H1N1 virus affects the severity of the upcoming flu season. From April 15 to July 24 of this year, states reported 43,771 confirmed and probable cases of novel H1N1 infection. Of the cases reported, 5,011 people were hospitalized and 302 died. After July 24, the CDC stopped counting novel H1N1 as separate flu cases.
“We are expecting increased illness during the regular flu season, because we think both the novel H1N1 and seasonal flu strains will cause illness in the population,” says Artealia Gilliard, a spokesperson for the U.S. Centers for Disease Control and Prevention (CDC) in Atlanta. “The biggest problem we are having is that there is no set number we can give for planning purposes. We can’t say go out and prepare for X percent more illness, because there is no scientifically sound way to arrive at a number.”
Another concern is that little guidance is available on how severe the novel virus will be. Gilliard notes that the World Health Organization (WHO) gave novel H1N1 the pandemic designation because of its ease of transmission, not the severity of the disease. Although the CDC expects more illness, it is not yet clear how many people will be made sick enough to be cared for by a hospitalist.
“The epidemiology of this illness and prevention issues related to this newly emerging virus are still being studied, making it very difficult to anticipate the staffing needs for the upcoming flu season,” says Irina Schiopescu, MD, a hospitalist and infectious-disease specialist at Roane Medical Center in Harriman, Tenn. “Hospitalists will be among the many front-line healthcare workers who provide direct, bedside clinical care to patients with suspected or confirmed H1N1 influenza.”
Most of the nation’s hospitals spent the summer preparing for another pandemic. Hospitalists have assessed their needs, too, and HM programs are focusing on a diverse set of concerns: prevention education for hospital-based employees, patient management updates, and expected personnel shortages.
“We have been planning for the worst but hoping for the best,” says Julia Wright, MD, FHM, head of the section of hospital medicine at the University of Wisconsin Hospitals in Madison and a member of Team Hospitalist. “Our task group for the upcoming flu season includes all critical-care services, nursing, supply-chain management, and human resources, as well as other appropriate specialties, such as infection control.”
Another Wild Card
How well the vaccination campaign works will have an impact on the incidence of novel H1N1 influenza. Some have expressed concerns about compliance issues in the community, as individuals will need an extra flu shot in addition to the yearly vaccination for seasonal flu strains. The concerns could double if current ongoing clinical trials suggest that two vaccine administrations are required for full protection from the H1N1 virus.
There also is concern about the availability of vaccines, especially in the early stages. As of early September, Robin Robinson, PhD, director of the Biological Advanced Research and Development Authority (BARDA) at the U.S. Department of Health and Human Services (HHS), announced that manufacturing problems would mean only 45 million doses would be available by Oct. 15, compared with the 120 million doses originally projected. However, HHS says the 195 million doses the U.S. government ordered should be available by the December deadline for final delivery.1
Nevertheless, physicians should expect large-scale vaccination initiatives at their hospitals this fall. Additionally, hospitals are expected to require that healthcare workers, including hospitalists, receive their shots during the first wave of inoculations. “At our facility, we have the potential to give 100,000 or more vaccinations over a very short period of time,” says Patty Skoglund, RN, administrative director for disaster preparedness at Scripps Health in San Diego. “This is in addition to supporting vaccination efforts in the community.”
Southern Hemisphere
The Southern Hemisphere is wrapping up its flu season, and often, experiences south of the equator are a harbinger of what might come in the Northern Hemisphere. So far, the WHO says the Southern Hemisphere’s flu season has been characterized by normal respiratory disease numbers. The impact and severity is still being
evaluated, but it appeared only slightly worse than normal in most places. Hospitals did see increased admissions (see Figure 1, p. 5) requiring respiratory critical care.2 Yet the lack of firm guidance has made planning difficult for HM groups and the U.S. hospitals they work in.
It will be important for hospitalists to stay up to date with a potentially developing situation, especially in the early stages of the flu season. Many current CDC guidelines for treatment, prevention, and control are in interim stages, with more guidance to come as the science firms up. (see “Vaccination Priorities,” right)
“As we get closer to the flu season, we should be able to make specific suggestions and get a better idea of the probable incidence,” says Gilliard. “Novel H1N1 has caused significant illness outside of the regular season. When the temperature changes, will the incidence increase or decrease? We have to get more experience before we will know.”
Information Hotline
Hospitals are working to ensure that there are open lines of communication with key personnel, an important first step in infectious-disease control. It will be necessary to facilitate the timely dispersal of new information on guidelines and treatment considerations to multiple audiences throughout the hospital as they are released. In addition, flu incidence and severity updates will be vital.
“It is imperative that physicians know what is going on in their community and beyond,” says Dr. Schiopescu. “The CDC and the Infectious Disease Society of America (IDSA) are resources for treatment guidelines and information on the spread and severity of both the novel H1N1 and seasonal virus strains. Closer to home, both state and local health boards can help with a more focused view of what is happening in the community.”
Patient placement will be another concern for hospitalists in the event of a widespread outbreak. The current CDC patient care guidelines say that all patients with confirmed or suspected H1N1 infection must be isolated. Although they can be scattered in rooms throughout the hospital, it is strongly suggested that they be placed together as a cohort, if possible.
“Our hospital is looking into designating special areas of the hospital to accept influenza patients,” Dr. Wright says. “We can then give the staff special training on treatment and prevention, give better access to materials and supplies in a single location, and also minimize the time lost to physicians going from one patient to another.”
Staffing Concerns
One of the biggest concerns to HM groups is keeping their own areas of the hospital properly staffed. In addition to the possibility of higher acuity and admissions affecting coverage needs, most experts are suggesting employee absentee rates upward of 40%. To further complicate the picture, interim CDC guidelines say healthcare workers should be off work 24 hours after a fever subsides or seven days, whichever is longer. This guidance, however, could change as the CDC obtains and reviews more information.
“We are a small group of only four physicians,” says Dr. Schiopescu, whose HM group works a six-day on, six-day off schedule for about 85 encounters per week at her 50-bed hospital. “We may need to work additional shifts and be available to be called in early, should the need arise. We have also done some cross-training so that community physicians can help if needed. At worst, we can pull resources from our sister hospitals in the system.”
—Irina Schiopescu, MD, infectious-disease specialist, Roane Medical Center, Harriman, Tenn.
Some hospitals have been able to flex up and increase staffing levels before the season begins. “In addition to adding three full-time equivalent staff, we have actively looked for other specialties, such as internal medicine or family practice, that have the proper skill sets should the need arise,” says Dr. Wright, whose program covers 75% of the 471 medical beds at UW Hospital. “We have also developed a set of protocols to streamline treatment of these patients, no matter who may be taking care of them.”
Scripps is surveying its employees to identify family and other outside obligations that could lead to call-outs and staffing shortages. Hospital administrators expect that the information will identify physicians who might not be able to come to work. The hospital also implemented systems that will allow them to bring in extra people—and get them deployed quickly—from such state and federal support resources as the Public Health Service and the National Disaster Medical System staffs.
“Balancing the needs of the various areas will be tricky at times,” Dr. Wright says. “We have to move people around while making sure we are not leaving one area dangerously understaffed.”
Education Imperative
Educating health workers is of the utmost importance before and during the flu season. A wide range of staff training will be required: reinforcing cough etiquette and hand-washing requirements through completely new procedures. This will be important for patient treatment and patient safety, two areas that intersect in hospitalists every day. In addition, this flu season will require a heightened level of personal responsibility from health workers. “Teaching needs are adding to the burden,” says Skoglund, the administrative director at Scripps. “Unfortunately, it is not as simple as sending out a memo to the staff and affiliated physicians.”
Training is a moving target, at least initially. Clinical employees will need to be trained on treatment and prevention guidelines as they are released, with special emphasis on keeping up with changes as the season progresses and lessons are learned.
“In the past, the CDC suggested using a N-95 respirator for all patients with novel H1N1,” Dr. Schiopescu says. “Currently, that has changed to approved use of a regular surgical mask, unless performing intubation or bronchoscopy.”
Despite the best efforts of the CDC, WHO, and other health organizations, there is no real clear idea of what to expect during the next flu season.
“What is known is that the hospitalist will be on the front lines, involved in the treatment of the sickest patients,” Dr. Wright says. TH
Kurt Ullman is a freelance writer based in Indiana.
Image Source: MAMMAMAART/ISTOCKPHOTO.COM
References
- Officials lower expectations for size of first novel flu vaccine deliveries. Center for Infectious Disease Research & Policy Web site. Available at: www.cidrap.umn.edu/cidrap/content/influenza/swineflu/news/aug1409vaccine.html. Accessed Aug. 20, 2009.
- Pandemic (H1N1) 2009: update 61. WHO Web site. Available at: www.who.int/csr/don/2009_08_12/en/index.html. Accessed Aug. 24, 2009.
As flu season descends on North America, hospitalists from Boston to the San Francisco Bay are concerned about what might happen when normal seasonal influenza hospital admissions are added to new cases of the novel influenza A (H1N1) virus.
Perhaps the most basic, still-unanswered question is how the addition of novel H1N1 virus affects the severity of the upcoming flu season. From April 15 to July 24 of this year, states reported 43,771 confirmed and probable cases of novel H1N1 infection. Of the cases reported, 5,011 people were hospitalized and 302 died. After July 24, the CDC stopped counting novel H1N1 as separate flu cases.
“We are expecting increased illness during the regular flu season, because we think both the novel H1N1 and seasonal flu strains will cause illness in the population,” says Artealia Gilliard, a spokesperson for the U.S. Centers for Disease Control and Prevention (CDC) in Atlanta. “The biggest problem we are having is that there is no set number we can give for planning purposes. We can’t say go out and prepare for X percent more illness, because there is no scientifically sound way to arrive at a number.”
Another concern is that little guidance is available on how severe the novel virus will be. Gilliard notes that the World Health Organization (WHO) gave novel H1N1 the pandemic designation because of its ease of transmission, not the severity of the disease. Although the CDC expects more illness, it is not yet clear how many people will be made sick enough to be cared for by a hospitalist.
“The epidemiology of this illness and prevention issues related to this newly emerging virus are still being studied, making it very difficult to anticipate the staffing needs for the upcoming flu season,” says Irina Schiopescu, MD, a hospitalist and infectious-disease specialist at Roane Medical Center in Harriman, Tenn. “Hospitalists will be among the many front-line healthcare workers who provide direct, bedside clinical care to patients with suspected or confirmed H1N1 influenza.”
Most of the nation’s hospitals spent the summer preparing for another pandemic. Hospitalists have assessed their needs, too, and HM programs are focusing on a diverse set of concerns: prevention education for hospital-based employees, patient management updates, and expected personnel shortages.
“We have been planning for the worst but hoping for the best,” says Julia Wright, MD, FHM, head of the section of hospital medicine at the University of Wisconsin Hospitals in Madison and a member of Team Hospitalist. “Our task group for the upcoming flu season includes all critical-care services, nursing, supply-chain management, and human resources, as well as other appropriate specialties, such as infection control.”
Another Wild Card
How well the vaccination campaign works will have an impact on the incidence of novel H1N1 influenza. Some have expressed concerns about compliance issues in the community, as individuals will need an extra flu shot in addition to the yearly vaccination for seasonal flu strains. The concerns could double if current ongoing clinical trials suggest that two vaccine administrations are required for full protection from the H1N1 virus.
There also is concern about the availability of vaccines, especially in the early stages. As of early September, Robin Robinson, PhD, director of the Biological Advanced Research and Development Authority (BARDA) at the U.S. Department of Health and Human Services (HHS), announced that manufacturing problems would mean only 45 million doses would be available by Oct. 15, compared with the 120 million doses originally projected. However, HHS says the 195 million doses the U.S. government ordered should be available by the December deadline for final delivery.1
Nevertheless, physicians should expect large-scale vaccination initiatives at their hospitals this fall. Additionally, hospitals are expected to require that healthcare workers, including hospitalists, receive their shots during the first wave of inoculations. “At our facility, we have the potential to give 100,000 or more vaccinations over a very short period of time,” says Patty Skoglund, RN, administrative director for disaster preparedness at Scripps Health in San Diego. “This is in addition to supporting vaccination efforts in the community.”
Southern Hemisphere
The Southern Hemisphere is wrapping up its flu season, and often, experiences south of the equator are a harbinger of what might come in the Northern Hemisphere. So far, the WHO says the Southern Hemisphere’s flu season has been characterized by normal respiratory disease numbers. The impact and severity is still being
evaluated, but it appeared only slightly worse than normal in most places. Hospitals did see increased admissions (see Figure 1, p. 5) requiring respiratory critical care.2 Yet the lack of firm guidance has made planning difficult for HM groups and the U.S. hospitals they work in.
It will be important for hospitalists to stay up to date with a potentially developing situation, especially in the early stages of the flu season. Many current CDC guidelines for treatment, prevention, and control are in interim stages, with more guidance to come as the science firms up. (see “Vaccination Priorities,” right)
“As we get closer to the flu season, we should be able to make specific suggestions and get a better idea of the probable incidence,” says Gilliard. “Novel H1N1 has caused significant illness outside of the regular season. When the temperature changes, will the incidence increase or decrease? We have to get more experience before we will know.”
Information Hotline
Hospitals are working to ensure that there are open lines of communication with key personnel, an important first step in infectious-disease control. It will be necessary to facilitate the timely dispersal of new information on guidelines and treatment considerations to multiple audiences throughout the hospital as they are released. In addition, flu incidence and severity updates will be vital.
“It is imperative that physicians know what is going on in their community and beyond,” says Dr. Schiopescu. “The CDC and the Infectious Disease Society of America (IDSA) are resources for treatment guidelines and information on the spread and severity of both the novel H1N1 and seasonal virus strains. Closer to home, both state and local health boards can help with a more focused view of what is happening in the community.”
Patient placement will be another concern for hospitalists in the event of a widespread outbreak. The current CDC patient care guidelines say that all patients with confirmed or suspected H1N1 infection must be isolated. Although they can be scattered in rooms throughout the hospital, it is strongly suggested that they be placed together as a cohort, if possible.
“Our hospital is looking into designating special areas of the hospital to accept influenza patients,” Dr. Wright says. “We can then give the staff special training on treatment and prevention, give better access to materials and supplies in a single location, and also minimize the time lost to physicians going from one patient to another.”
Staffing Concerns
One of the biggest concerns to HM groups is keeping their own areas of the hospital properly staffed. In addition to the possibility of higher acuity and admissions affecting coverage needs, most experts are suggesting employee absentee rates upward of 40%. To further complicate the picture, interim CDC guidelines say healthcare workers should be off work 24 hours after a fever subsides or seven days, whichever is longer. This guidance, however, could change as the CDC obtains and reviews more information.
“We are a small group of only four physicians,” says Dr. Schiopescu, whose HM group works a six-day on, six-day off schedule for about 85 encounters per week at her 50-bed hospital. “We may need to work additional shifts and be available to be called in early, should the need arise. We have also done some cross-training so that community physicians can help if needed. At worst, we can pull resources from our sister hospitals in the system.”
—Irina Schiopescu, MD, infectious-disease specialist, Roane Medical Center, Harriman, Tenn.
Some hospitals have been able to flex up and increase staffing levels before the season begins. “In addition to adding three full-time equivalent staff, we have actively looked for other specialties, such as internal medicine or family practice, that have the proper skill sets should the need arise,” says Dr. Wright, whose program covers 75% of the 471 medical beds at UW Hospital. “We have also developed a set of protocols to streamline treatment of these patients, no matter who may be taking care of them.”
Scripps is surveying its employees to identify family and other outside obligations that could lead to call-outs and staffing shortages. Hospital administrators expect that the information will identify physicians who might not be able to come to work. The hospital also implemented systems that will allow them to bring in extra people—and get them deployed quickly—from such state and federal support resources as the Public Health Service and the National Disaster Medical System staffs.
“Balancing the needs of the various areas will be tricky at times,” Dr. Wright says. “We have to move people around while making sure we are not leaving one area dangerously understaffed.”
Education Imperative
Educating health workers is of the utmost importance before and during the flu season. A wide range of staff training will be required: reinforcing cough etiquette and hand-washing requirements through completely new procedures. This will be important for patient treatment and patient safety, two areas that intersect in hospitalists every day. In addition, this flu season will require a heightened level of personal responsibility from health workers. “Teaching needs are adding to the burden,” says Skoglund, the administrative director at Scripps. “Unfortunately, it is not as simple as sending out a memo to the staff and affiliated physicians.”
Training is a moving target, at least initially. Clinical employees will need to be trained on treatment and prevention guidelines as they are released, with special emphasis on keeping up with changes as the season progresses and lessons are learned.
“In the past, the CDC suggested using a N-95 respirator for all patients with novel H1N1,” Dr. Schiopescu says. “Currently, that has changed to approved use of a regular surgical mask, unless performing intubation or bronchoscopy.”
Despite the best efforts of the CDC, WHO, and other health organizations, there is no real clear idea of what to expect during the next flu season.
“What is known is that the hospitalist will be on the front lines, involved in the treatment of the sickest patients,” Dr. Wright says. TH
Kurt Ullman is a freelance writer based in Indiana.
Image Source: MAMMAMAART/ISTOCKPHOTO.COM
References
- Officials lower expectations for size of first novel flu vaccine deliveries. Center for Infectious Disease Research & Policy Web site. Available at: www.cidrap.umn.edu/cidrap/content/influenza/swineflu/news/aug1409vaccine.html. Accessed Aug. 20, 2009.
- Pandemic (H1N1) 2009: update 61. WHO Web site. Available at: www.who.int/csr/don/2009_08_12/en/index.html. Accessed Aug. 24, 2009.
Myriad Warnings Blur the Message
A plethora of posters, a load of labels, and a rainbow of colored wristbands confront the average hospitalist every day. They serve as reminders to wash your hands, avoid using an extremity for blood draws, and other warnings both important and not so much. In this day and age, with a multitude of visual and technological reminders confronting physicians, some raise concerns about the consequences of too many reminders, also known as “alert fatigue.”
“The premise of [warning] signs is to improve quality,” says David Grace, MD, FHM, area medical officer for the Schumacher Group in Lafayette, La., and a member of Team Hospitalist. “I am not at all convinced that this is being accomplished. There is so much visual noise [in the hospital] that important messages get lost in the clutter.”
Alert fatigue is most often used to describe a phenomenon seen in computerized decision support systems. It’s the result of a physician receiving so many warnings that they grow numb and stop looking at them. Although it hasn’t been studied to the same extent in the low- or no-tech arena, alert fatigue is an issue in hospital-based signage.
Marilyn Sue Bogner, PhD, chief scientist at the Institute for the Study of Human Error, LLC, in Bethesda, Md., says alert oversaturation can have unintended consequences. “If there are too many signs, you really have no signs because people don’t pay attention,” she says. “I wouldn’t call it information overload, because you have to take information in before you can be overloaded.”
This lack of attention can lead to important information being ignored or misunderstood. It could cause serious disruptions in patient care and adverse outcomes, including the possibility of injury or even death.
Too Much of a Good Thing
One potentially harmful trend of warning signs in the hospital setting is what psychologists call “dilution.” The more warnings there are, the more people tend to lose sight of why the warning is there in the first place, and low-importance warnings “dilute” the strength of important ones.
“I would like to see a system where only truly high-risk patients are the ones who get the warnings,” Dr. Grace says. “If you restricted precautionary signs to those patients at high risk for transmitting something bad, or those at high risk for getting something bad, you would get better adherence than currently, where you seem to have signs for any patient with any risk for transmitting anything.”
For all the visual cues in the hospital setting to warn physicians of potential dangers, there exists no standardized system to help hospitalists sort out the direct patient-threats from the more mundane housekeeping chores.
“Even a warning that is effective by itself may get buried when there are others hanging around it,” Dr. Bogner says. “There is no hierarchy of importance in most hospitals because there is no central authority making sure that red, for instance, is saved only for a warning about the most dangerous incidents.”
Often specialists are responsible for signs relating to their area of expertise without taking into account the addition to the chaos as well as how the warning will fit in with the realities of the hospital unit. Clutter in the ICU and other areas of the hospital can be exacerbated by multiple disciplines putting up their own signs. There is no method for hospitalists to look around and see which warnings pertain to them.
“There is a reason why all stop signs are red and have eight sides,” Dr. Grace says. “[It] makes it easy to for all to recognize at a glance what is being communicated. In hospitals, the same warning may be many different shapes and colors. This can make it hard for hospitalists, especially those who go to more than one hospital, to know what is being said and the response expected.”
Placement of visual warning signs can add to the confusion and limit effectiveness. Information is best placed near where it is to be used. For example, a sign telling staff that a certain extremity should not be used for blood draws is more likely to be seen and acted upon if it is in the form of a wristband attached to the arm instead of a warning sign on the door. It also is important to have easy access to the tools needed to follow the warning sign’s directions.
“Hospitals don’t have the resources to put a fully stocked isolation cart near every door,” Dr. Grace says. “You get a busy doctor down the far end of the hall and they may decide to just pop in and see their patient for a second, instead of taking the long walk back to the cart. Others follow the lead of the physician and, eventually, there will be a real need for the protection and it won’t be worn. The outcome is an increase in cluster outbreaks.”
Regulatory Requirements
Some of what one of the experts called “the metastasis of signage” can be laid at the feet of the various organizations that regulate healthcare in the U.S. For example, many signs and their placement are required by regulators with, as one hospital risk management expert says, little or no understanding of the impact the mandates have on sign pollution.
“There are guidelines from The Joint Commission and others indicating when you have to put signs up, and often mandate both their content and placement,” says Elaine Ziemba, managing director of risk management at the Stanford Hospitals and Clinics in Palo Alto, Calif. “Environmental health and safety people will decide signage related to medical gasses and fire safety, and biomedical engineering will make decisions related to their equipment.”
Warning signs are added according to the perceived needs of the specific discipline involved. Risk managers are not routinely consulted about warning signs and notices put up around her hospital, Ziemba says. There also is little guidance in the literature about the effectiveness of multiple warning signs, especially when compared with the wide range of studies that assess alert fatigue in electronic medical record systems.
Although hardly restricted to the requirements of The Joint Commission or other agencies, complex and wordy signs add to the visual chaos and actually impair compliance. “Too many signs try to communicate too much information out of a fear that they may be leaving something important out,” Dr. Bogner says. “It is a lot easier to put everything in than to distill things down to get to the nugget you want to get across.”
David Yu, MD, FACP, medical director of hospitalist services at Decatur Memorial Hospital in Decatur, Ill., agrees. A member of Team Hospitalist, Dr. Yu’s mantra is “less is better.” Put the fewest words possible on the sign, then educate the staff on how to implement the information.
“We discourage signs that are overly verbose,” he says. “At the end of the day, the efficacy of signs depends largely on the training and attentiveness of those caring for the patient. It is not fail-safe and requires the staff to acknowledge the sign and institute the indicated policies correctly.”
In some cases, the best sign might not even be a sign.
“Color coding is used extensively in the military,” Dr. Yu says. “On an aircraft carrier, all of the people running around the deck are color-coded. Just by looking around, you can see who deals with armament, who is the refueler, and who does traffic control.”
Dr. Yu’s hospital issues red footies to patients who are at high risk for falls. When any staff member sees a red-footed patient wandering around without an escort, they immediately know they should intervene. It conveys the required message anywhere in the hospital.

—David Grace, MD, FHM, area medical officer, Schumacher Group, Lafayette, La.
“Fire and Forget”
Although many visual warnings have the best of intentions, it doesn’t mean they are effective. Few hospitals have systems in place to follow up and make sure the warning actually has an effect on patient care.
“Alerts should be viewed initially as an experiment, requiring tracking to make sure it works as intended,” says Scott A. Flanders, MD, FHM, president of SHM and professor of medicine and director of the hospitalist program at the University of Michigan at Ann Arbor. “Too frequently in healthcare we put up signs in an attempt to fix a problem, but then don’t follow up to see if it is working.”
A similar phenomenon is seen when early warnings follow a patient through subsequent hospitalizations. This is especially true with isolation protocols, as the patient might not require the same warnings as previous admissions.
“It seems as though anyone who has ever had methicillin-resistant Staphylococcus aureus [MRSA] gets one of those things slapped on their door the minute they come in,” Dr. Grace says. “I have personally seen patients who had a boil grow out [of] MRSA 10 years ago still get a sticker on their door after all this time.”
Thus, warning signs that are not serving their intended purpose don’t ever get taken down; they dilute the usefulness of those that are timely and effective. The trend might indicate that defensive signage (a cousin to defensive medicine) is a driver, the theory being it’s safer and “legally defensible” if a hospital posts a multitude of alerts, rather than miss a sign that could have averted a poor outcome.
Effectiveness Questioned
Even though hospitalists have witnessed a marked increase in visual warnings, there is little to suggest they are effective. For example, studies in Asia during the 2003 SARS scare suggest that isolation precautions were followed closely, yet there was no change in MRSA transmission rates.
The other concern is whether the saturation of warnings causes harm. Dr. Grace receives a warning flag on almost every chart requesting DVT prophylaxis—even for patients who are on heparin infusions or already are on prophylaxis. “Doctors get frustrated and start to ignore the [alerts],” he says. “Then, when someone slips through the cracks and doesn’t get needed treatment, we are less likely to catch it because of alert fatigue.”
Although they are the most visual, and perhaps the most frustrating, part of patient safety, warning signs are not the only bullets in the gunfight.
“I don’t think any institution views [warning] signs as the ultimate solution to problems,” Dr. Flanders says. “Signs end up being one part of a multifactorial intervention—a common and easy first piece of the puzzle.”
Warning signs in the hospital can serve an important communication function, alerting providers of key safety concerns. However, too many warnings can dilute the effectiveness of the signage and hinder patient care.
Hospitalists need to recognize the possibility of sign fatigue in their own practice and link warnings to truly high-risk situations. Alerts can be of help, but they should be viewed as a back-up—not a substitute—for good communication between physicians, colleagues, and the hospital staff. TH
Kurt Ullman is a freelance writer based in Indiana.
A plethora of posters, a load of labels, and a rainbow of colored wristbands confront the average hospitalist every day. They serve as reminders to wash your hands, avoid using an extremity for blood draws, and other warnings both important and not so much. In this day and age, with a multitude of visual and technological reminders confronting physicians, some raise concerns about the consequences of too many reminders, also known as “alert fatigue.”
“The premise of [warning] signs is to improve quality,” says David Grace, MD, FHM, area medical officer for the Schumacher Group in Lafayette, La., and a member of Team Hospitalist. “I am not at all convinced that this is being accomplished. There is so much visual noise [in the hospital] that important messages get lost in the clutter.”
Alert fatigue is most often used to describe a phenomenon seen in computerized decision support systems. It’s the result of a physician receiving so many warnings that they grow numb and stop looking at them. Although it hasn’t been studied to the same extent in the low- or no-tech arena, alert fatigue is an issue in hospital-based signage.
Marilyn Sue Bogner, PhD, chief scientist at the Institute for the Study of Human Error, LLC, in Bethesda, Md., says alert oversaturation can have unintended consequences. “If there are too many signs, you really have no signs because people don’t pay attention,” she says. “I wouldn’t call it information overload, because you have to take information in before you can be overloaded.”
This lack of attention can lead to important information being ignored or misunderstood. It could cause serious disruptions in patient care and adverse outcomes, including the possibility of injury or even death.
Too Much of a Good Thing
One potentially harmful trend of warning signs in the hospital setting is what psychologists call “dilution.” The more warnings there are, the more people tend to lose sight of why the warning is there in the first place, and low-importance warnings “dilute” the strength of important ones.
“I would like to see a system where only truly high-risk patients are the ones who get the warnings,” Dr. Grace says. “If you restricted precautionary signs to those patients at high risk for transmitting something bad, or those at high risk for getting something bad, you would get better adherence than currently, where you seem to have signs for any patient with any risk for transmitting anything.”
For all the visual cues in the hospital setting to warn physicians of potential dangers, there exists no standardized system to help hospitalists sort out the direct patient-threats from the more mundane housekeeping chores.
“Even a warning that is effective by itself may get buried when there are others hanging around it,” Dr. Bogner says. “There is no hierarchy of importance in most hospitals because there is no central authority making sure that red, for instance, is saved only for a warning about the most dangerous incidents.”
Often specialists are responsible for signs relating to their area of expertise without taking into account the addition to the chaos as well as how the warning will fit in with the realities of the hospital unit. Clutter in the ICU and other areas of the hospital can be exacerbated by multiple disciplines putting up their own signs. There is no method for hospitalists to look around and see which warnings pertain to them.
“There is a reason why all stop signs are red and have eight sides,” Dr. Grace says. “[It] makes it easy to for all to recognize at a glance what is being communicated. In hospitals, the same warning may be many different shapes and colors. This can make it hard for hospitalists, especially those who go to more than one hospital, to know what is being said and the response expected.”
Placement of visual warning signs can add to the confusion and limit effectiveness. Information is best placed near where it is to be used. For example, a sign telling staff that a certain extremity should not be used for blood draws is more likely to be seen and acted upon if it is in the form of a wristband attached to the arm instead of a warning sign on the door. It also is important to have easy access to the tools needed to follow the warning sign’s directions.
“Hospitals don’t have the resources to put a fully stocked isolation cart near every door,” Dr. Grace says. “You get a busy doctor down the far end of the hall and they may decide to just pop in and see their patient for a second, instead of taking the long walk back to the cart. Others follow the lead of the physician and, eventually, there will be a real need for the protection and it won’t be worn. The outcome is an increase in cluster outbreaks.”
Regulatory Requirements
Some of what one of the experts called “the metastasis of signage” can be laid at the feet of the various organizations that regulate healthcare in the U.S. For example, many signs and their placement are required by regulators with, as one hospital risk management expert says, little or no understanding of the impact the mandates have on sign pollution.
“There are guidelines from The Joint Commission and others indicating when you have to put signs up, and often mandate both their content and placement,” says Elaine Ziemba, managing director of risk management at the Stanford Hospitals and Clinics in Palo Alto, Calif. “Environmental health and safety people will decide signage related to medical gasses and fire safety, and biomedical engineering will make decisions related to their equipment.”
Warning signs are added according to the perceived needs of the specific discipline involved. Risk managers are not routinely consulted about warning signs and notices put up around her hospital, Ziemba says. There also is little guidance in the literature about the effectiveness of multiple warning signs, especially when compared with the wide range of studies that assess alert fatigue in electronic medical record systems.
Although hardly restricted to the requirements of The Joint Commission or other agencies, complex and wordy signs add to the visual chaos and actually impair compliance. “Too many signs try to communicate too much information out of a fear that they may be leaving something important out,” Dr. Bogner says. “It is a lot easier to put everything in than to distill things down to get to the nugget you want to get across.”
David Yu, MD, FACP, medical director of hospitalist services at Decatur Memorial Hospital in Decatur, Ill., agrees. A member of Team Hospitalist, Dr. Yu’s mantra is “less is better.” Put the fewest words possible on the sign, then educate the staff on how to implement the information.
“We discourage signs that are overly verbose,” he says. “At the end of the day, the efficacy of signs depends largely on the training and attentiveness of those caring for the patient. It is not fail-safe and requires the staff to acknowledge the sign and institute the indicated policies correctly.”
In some cases, the best sign might not even be a sign.
“Color coding is used extensively in the military,” Dr. Yu says. “On an aircraft carrier, all of the people running around the deck are color-coded. Just by looking around, you can see who deals with armament, who is the refueler, and who does traffic control.”
Dr. Yu’s hospital issues red footies to patients who are at high risk for falls. When any staff member sees a red-footed patient wandering around without an escort, they immediately know they should intervene. It conveys the required message anywhere in the hospital.

—David Grace, MD, FHM, area medical officer, Schumacher Group, Lafayette, La.
“Fire and Forget”
Although many visual warnings have the best of intentions, it doesn’t mean they are effective. Few hospitals have systems in place to follow up and make sure the warning actually has an effect on patient care.
“Alerts should be viewed initially as an experiment, requiring tracking to make sure it works as intended,” says Scott A. Flanders, MD, FHM, president of SHM and professor of medicine and director of the hospitalist program at the University of Michigan at Ann Arbor. “Too frequently in healthcare we put up signs in an attempt to fix a problem, but then don’t follow up to see if it is working.”
A similar phenomenon is seen when early warnings follow a patient through subsequent hospitalizations. This is especially true with isolation protocols, as the patient might not require the same warnings as previous admissions.
“It seems as though anyone who has ever had methicillin-resistant Staphylococcus aureus [MRSA] gets one of those things slapped on their door the minute they come in,” Dr. Grace says. “I have personally seen patients who had a boil grow out [of] MRSA 10 years ago still get a sticker on their door after all this time.”
Thus, warning signs that are not serving their intended purpose don’t ever get taken down; they dilute the usefulness of those that are timely and effective. The trend might indicate that defensive signage (a cousin to defensive medicine) is a driver, the theory being it’s safer and “legally defensible” if a hospital posts a multitude of alerts, rather than miss a sign that could have averted a poor outcome.
Effectiveness Questioned
Even though hospitalists have witnessed a marked increase in visual warnings, there is little to suggest they are effective. For example, studies in Asia during the 2003 SARS scare suggest that isolation precautions were followed closely, yet there was no change in MRSA transmission rates.
The other concern is whether the saturation of warnings causes harm. Dr. Grace receives a warning flag on almost every chart requesting DVT prophylaxis—even for patients who are on heparin infusions or already are on prophylaxis. “Doctors get frustrated and start to ignore the [alerts],” he says. “Then, when someone slips through the cracks and doesn’t get needed treatment, we are less likely to catch it because of alert fatigue.”
Although they are the most visual, and perhaps the most frustrating, part of patient safety, warning signs are not the only bullets in the gunfight.
“I don’t think any institution views [warning] signs as the ultimate solution to problems,” Dr. Flanders says. “Signs end up being one part of a multifactorial intervention—a common and easy first piece of the puzzle.”
Warning signs in the hospital can serve an important communication function, alerting providers of key safety concerns. However, too many warnings can dilute the effectiveness of the signage and hinder patient care.
Hospitalists need to recognize the possibility of sign fatigue in their own practice and link warnings to truly high-risk situations. Alerts can be of help, but they should be viewed as a back-up—not a substitute—for good communication between physicians, colleagues, and the hospital staff. TH
Kurt Ullman is a freelance writer based in Indiana.
A plethora of posters, a load of labels, and a rainbow of colored wristbands confront the average hospitalist every day. They serve as reminders to wash your hands, avoid using an extremity for blood draws, and other warnings both important and not so much. In this day and age, with a multitude of visual and technological reminders confronting physicians, some raise concerns about the consequences of too many reminders, also known as “alert fatigue.”
“The premise of [warning] signs is to improve quality,” says David Grace, MD, FHM, area medical officer for the Schumacher Group in Lafayette, La., and a member of Team Hospitalist. “I am not at all convinced that this is being accomplished. There is so much visual noise [in the hospital] that important messages get lost in the clutter.”
Alert fatigue is most often used to describe a phenomenon seen in computerized decision support systems. It’s the result of a physician receiving so many warnings that they grow numb and stop looking at them. Although it hasn’t been studied to the same extent in the low- or no-tech arena, alert fatigue is an issue in hospital-based signage.
Marilyn Sue Bogner, PhD, chief scientist at the Institute for the Study of Human Error, LLC, in Bethesda, Md., says alert oversaturation can have unintended consequences. “If there are too many signs, you really have no signs because people don’t pay attention,” she says. “I wouldn’t call it information overload, because you have to take information in before you can be overloaded.”
This lack of attention can lead to important information being ignored or misunderstood. It could cause serious disruptions in patient care and adverse outcomes, including the possibility of injury or even death.
Too Much of a Good Thing
One potentially harmful trend of warning signs in the hospital setting is what psychologists call “dilution.” The more warnings there are, the more people tend to lose sight of why the warning is there in the first place, and low-importance warnings “dilute” the strength of important ones.
“I would like to see a system where only truly high-risk patients are the ones who get the warnings,” Dr. Grace says. “If you restricted precautionary signs to those patients at high risk for transmitting something bad, or those at high risk for getting something bad, you would get better adherence than currently, where you seem to have signs for any patient with any risk for transmitting anything.”
For all the visual cues in the hospital setting to warn physicians of potential dangers, there exists no standardized system to help hospitalists sort out the direct patient-threats from the more mundane housekeeping chores.
“Even a warning that is effective by itself may get buried when there are others hanging around it,” Dr. Bogner says. “There is no hierarchy of importance in most hospitals because there is no central authority making sure that red, for instance, is saved only for a warning about the most dangerous incidents.”
Often specialists are responsible for signs relating to their area of expertise without taking into account the addition to the chaos as well as how the warning will fit in with the realities of the hospital unit. Clutter in the ICU and other areas of the hospital can be exacerbated by multiple disciplines putting up their own signs. There is no method for hospitalists to look around and see which warnings pertain to them.
“There is a reason why all stop signs are red and have eight sides,” Dr. Grace says. “[It] makes it easy to for all to recognize at a glance what is being communicated. In hospitals, the same warning may be many different shapes and colors. This can make it hard for hospitalists, especially those who go to more than one hospital, to know what is being said and the response expected.”
Placement of visual warning signs can add to the confusion and limit effectiveness. Information is best placed near where it is to be used. For example, a sign telling staff that a certain extremity should not be used for blood draws is more likely to be seen and acted upon if it is in the form of a wristband attached to the arm instead of a warning sign on the door. It also is important to have easy access to the tools needed to follow the warning sign’s directions.
“Hospitals don’t have the resources to put a fully stocked isolation cart near every door,” Dr. Grace says. “You get a busy doctor down the far end of the hall and they may decide to just pop in and see their patient for a second, instead of taking the long walk back to the cart. Others follow the lead of the physician and, eventually, there will be a real need for the protection and it won’t be worn. The outcome is an increase in cluster outbreaks.”
Regulatory Requirements
Some of what one of the experts called “the metastasis of signage” can be laid at the feet of the various organizations that regulate healthcare in the U.S. For example, many signs and their placement are required by regulators with, as one hospital risk management expert says, little or no understanding of the impact the mandates have on sign pollution.
“There are guidelines from The Joint Commission and others indicating when you have to put signs up, and often mandate both their content and placement,” says Elaine Ziemba, managing director of risk management at the Stanford Hospitals and Clinics in Palo Alto, Calif. “Environmental health and safety people will decide signage related to medical gasses and fire safety, and biomedical engineering will make decisions related to their equipment.”
Warning signs are added according to the perceived needs of the specific discipline involved. Risk managers are not routinely consulted about warning signs and notices put up around her hospital, Ziemba says. There also is little guidance in the literature about the effectiveness of multiple warning signs, especially when compared with the wide range of studies that assess alert fatigue in electronic medical record systems.
Although hardly restricted to the requirements of The Joint Commission or other agencies, complex and wordy signs add to the visual chaos and actually impair compliance. “Too many signs try to communicate too much information out of a fear that they may be leaving something important out,” Dr. Bogner says. “It is a lot easier to put everything in than to distill things down to get to the nugget you want to get across.”
David Yu, MD, FACP, medical director of hospitalist services at Decatur Memorial Hospital in Decatur, Ill., agrees. A member of Team Hospitalist, Dr. Yu’s mantra is “less is better.” Put the fewest words possible on the sign, then educate the staff on how to implement the information.
“We discourage signs that are overly verbose,” he says. “At the end of the day, the efficacy of signs depends largely on the training and attentiveness of those caring for the patient. It is not fail-safe and requires the staff to acknowledge the sign and institute the indicated policies correctly.”
In some cases, the best sign might not even be a sign.
“Color coding is used extensively in the military,” Dr. Yu says. “On an aircraft carrier, all of the people running around the deck are color-coded. Just by looking around, you can see who deals with armament, who is the refueler, and who does traffic control.”
Dr. Yu’s hospital issues red footies to patients who are at high risk for falls. When any staff member sees a red-footed patient wandering around without an escort, they immediately know they should intervene. It conveys the required message anywhere in the hospital.

—David Grace, MD, FHM, area medical officer, Schumacher Group, Lafayette, La.
“Fire and Forget”
Although many visual warnings have the best of intentions, it doesn’t mean they are effective. Few hospitals have systems in place to follow up and make sure the warning actually has an effect on patient care.
“Alerts should be viewed initially as an experiment, requiring tracking to make sure it works as intended,” says Scott A. Flanders, MD, FHM, president of SHM and professor of medicine and director of the hospitalist program at the University of Michigan at Ann Arbor. “Too frequently in healthcare we put up signs in an attempt to fix a problem, but then don’t follow up to see if it is working.”
A similar phenomenon is seen when early warnings follow a patient through subsequent hospitalizations. This is especially true with isolation protocols, as the patient might not require the same warnings as previous admissions.
“It seems as though anyone who has ever had methicillin-resistant Staphylococcus aureus [MRSA] gets one of those things slapped on their door the minute they come in,” Dr. Grace says. “I have personally seen patients who had a boil grow out [of] MRSA 10 years ago still get a sticker on their door after all this time.”
Thus, warning signs that are not serving their intended purpose don’t ever get taken down; they dilute the usefulness of those that are timely and effective. The trend might indicate that defensive signage (a cousin to defensive medicine) is a driver, the theory being it’s safer and “legally defensible” if a hospital posts a multitude of alerts, rather than miss a sign that could have averted a poor outcome.
Effectiveness Questioned
Even though hospitalists have witnessed a marked increase in visual warnings, there is little to suggest they are effective. For example, studies in Asia during the 2003 SARS scare suggest that isolation precautions were followed closely, yet there was no change in MRSA transmission rates.
The other concern is whether the saturation of warnings causes harm. Dr. Grace receives a warning flag on almost every chart requesting DVT prophylaxis—even for patients who are on heparin infusions or already are on prophylaxis. “Doctors get frustrated and start to ignore the [alerts],” he says. “Then, when someone slips through the cracks and doesn’t get needed treatment, we are less likely to catch it because of alert fatigue.”
Although they are the most visual, and perhaps the most frustrating, part of patient safety, warning signs are not the only bullets in the gunfight.
“I don’t think any institution views [warning] signs as the ultimate solution to problems,” Dr. Flanders says. “Signs end up being one part of a multifactorial intervention—a common and easy first piece of the puzzle.”
Warning signs in the hospital can serve an important communication function, alerting providers of key safety concerns. However, too many warnings can dilute the effectiveness of the signage and hinder patient care.
Hospitalists need to recognize the possibility of sign fatigue in their own practice and link warnings to truly high-risk situations. Alerts can be of help, but they should be viewed as a back-up—not a substitute—for good communication between physicians, colleagues, and the hospital staff. TH
Kurt Ullman is a freelance writer based in Indiana.