User login
Concurrent Treatment of a Middle-Third Clavicle Fracture and Type IV Acromioclavicular Dislocation
Acromioclavicular (AC) dislocations and displaced fractures of the middle third of the clavicle rarely occur together. Isolated AC joint separation is often treated nonoperatively with internal coracoclavicular (CC) fixation or reconstruction considered for type IV-VI AC dislocations and some type III injuries.1 Isolated clavicle fractures traditionally have been treated nonoperatively. The current trend is toward internal fixation for displaced and shortened fractures.2 There have been only a handful of reports of concomitant AC dislocation and midshaft clavicle fracture.3-6 Previous treatments have included nonoperative treatment, AC fixation, or internal fixation of the clavicle with ligamentous reconstruction.
We present a previously undescribed technique for internal fixation of this rare shoulder injury. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
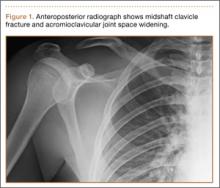
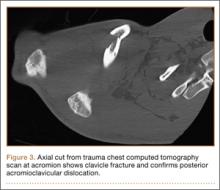
While driving an all-terrain vehicle, a healthy 19-year-old right-hand–dominant man hit a bridge and sustained direct impact to his right shoulder. He presented to the emergency department complaining of right shoulder pain and deformity without skin disruption, vascular insufficiency, or neurologic symptoms. Anteroposterior (AP) radiograph showed an oblique, displaced, middle-third clavicle shaft fracture (Figure 1). An associated type IV AC dislocation was confirmed on axillary radiograph (Figure 2) and on an axial cut from a trauma chest computed tomography (CT) scan (Figure 3). The patient was discharged home from the trauma service the next day with a sling for comfort and plans for delayed, elective operative fixation 1 week later.
The patient was placed in a beach-chair position. Through a longitudinal incision extending laterally over the AC joint, the clavicle was exposed for fracture reduction, with care taken to retain soft-tissue attachments. The distal clavicle was buttonholed posteriorly through the trapezius muscle and fascia. The distal fracture fragment was devoid of any remaining CC ligamentous attachment. After satisfactory reduction, a low-profile precontoured clavicle plate (Superior Midshaft Clavicle Plate; Acumed, Hillsboro, Oregon) was placed superiorly; the fracture was compressed through the plate and internally fixed with three 3.5-mm bicortical screws on both sides of the fracture. Approximately 5 mm of the distal clavicle was resected at the AC joint to facilitate adequate AC and CC reduction without disruption of the clavicle fracture. With an adequate CC reduction, a 3.5-mm fully threaded cortical screw was placed through the most distal hole in the clavicle plate, clavicle, and coracoid.
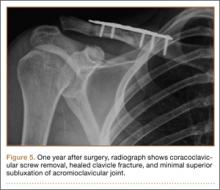
After surgery, the patient was placed into an ARC shoulder immobilizer (Bledsoe, Grand Prairie, Texas) for 6 weeks, removing the immobilizer only for elbow and wrist range of motion (ROM) exercises. Radiographs at 3-month follow-up (Figure 4) showed a healed fracture with no loss of AC or CC reduction. Three months after surgery, another procedure was performed to remove the CC screw. One year after the initial surgery, the patient complained of intermittent soreness over the lateral shoulder but was not limited in his activities and was back to performing manual labor without difficulty. He had full ROM in forward flexion, abduction, internal rotation, and external rotation without weakness, tenderness, or any neurovascular deficit. After CC screw removal, no deformity returned at the shoulder. Radiographs showed a healed fracture with minimal superior subluxation at the AC joint without significant change from the 3-month follow-up (Figure 5).
Discussion
The combined injury pattern of a type IV AC dislocation and a displaced middle-third clavicle shaft fracture is rare. The usual mechanism of injury, as seen in the present case, is a direct blow to the shoulder at the tip of the acromion, though indirect forces from a fall on an outstretched hand are also described.7 Disruption of the CC ligaments with AC separation likely dissipates the stress necessary to create a clavicle fracture in most cases,1 explaining the rarity of this injury. It is imperative to evaluate patients for injury to both the osseous and ligamentous structures.
Previous case reports of concomitant AC separation and midshaft clavicle fracture have described a variety of treatment options, but to date our case represents the only episode in which both the clavicle fracture and the AC joint were treated with open reduction and internal fixation (ORIF). Wurtz and colleagues5 reported on a series of 4 patients with AC disruption and middle-third clavicle fracture. Three of the 4 patients had type IV AC separation; all 3 were treated, 2 acutely and 1 chronically, with open reduction of the AC and CC joints; 2 of these patients had CC screw fixation only after reduction, and the third had 2 Steinmann pins placed across the AC joint without CC screw fixation. All hardware was removed after 12 weeks. The fourth patient had a type II AC dislocation and was treated with closed reduction of the clavicle with no intervention for the AC joint. None of the clavicle fractures in this series were treated with internal fixation. All patients had full and pain-free ROM at 1- to 3-year follow-up.
Juhn and Simonian3 reported on a case of type VI separation with greenstick midshaft clavicle fracture in a hockey player seen 7 days after injury. The patient described some tingling in the upper extremity and had shoulder pain on initial presentation but was noted to have minimal displacement of both the AC joint and the midshaft clavicle fracture. Both injuries were treated nonsurgically with good outcome, and the patient returned to full activity (including hockey) within 14 weeks after injury.
Lancourt4 described the case of a patient with a type V AC dislocation and a displaced midshaft clavicle fracture. The AC joint was treated with Steinmann pin fixation, and the clavicle fracture was treated nonoperatively. The author cited high complication rates of plate fixation for clavicle fractures as the reason for not performing the additional procedure. The pins were removed 8 weeks after surgery. At 3-year follow-up, the patient had good radiographic and clinical outcome.
Yeh and colleagues6 described a patient who sustained a displaced midshaft clavicle fracture and a type IV AC dislocation in a fall from a horse. The patient underwent ORIF of the clavicle fracture with plate fixation. After the procedure, the AC joint was still unstable intraoperatively, and the AC and CC ligaments were reconstructed with semitendinosus allograft. The patient had full and painless ROM at 1-year follow-up.
The present case report serves as a reminder to obtain adequate shoulder radiographs when evaluating “just another clavicle fracture.” The radiographs should include a good axillary view to ensure there is not an associated AC dislocation. Increasingly, some authors have been advocating internal fixation for clavicle fractures, with reports of improved functional outcomes, improved cosmesis, and increased union rates.2 Indications for operative fixation include shortening and 100% displacement,8 and relative indications include open fractures.1 Operative fixation is perhaps more important for younger, athletic, and manual-labor populations. The trend in treatment of clavicle fractures toward operative fixation lends itself well to ORIF of the AC and CC joints; hence, a modern treatment for this rarely described combination injury should include internal plate fixation of the clavicle in addition to CC fixation. This additional procedure requires little extra time and energy in an operative scenario already requiring anesthesia, with easy insertion of the CC screw through the clavicle plate. Use of a CC screw obviates any potential risks associated with use of allograft tissue, and there is no anticipated difficulty with screw removal at 12 weeks.
Alternative options for AC stability include CC reconstruction with ligamentous allograft, ligamentous autograft, or suture/tightrope techniques. A noted advantage of these alternative techniques is less need to return to the operating room for the hardware removal that is recommended with CC screw fixation. However, these procedures potentially increase surgical exposure and operating time. In addition, screw fixation minimizes the possibility of donor-site morbidity from autograft transfers and potential complications from allograft tissue.
Hook plate fixation of the AC joint has also been described. In a recent case report of a similar injury pattern, plate fixation of the clavicle with simultaneous hook plate fixation of the AC joint was described.9 The patient did well but required removal of hardware of the hook plate and the clavicle plate 1 and 3 years after surgery, respectively. Although screw fixation is biomechanically stronger, debate persists about the clinical importance of this increase in strength.1 In the setting of plate fixation for the clavicle, these alternative AC fixations would require technique adjustments, including length of grafts and/or sutures, and raise concerns regarding interaction of the metal with the fixation material.
Critical evaluation of our technique revealed a lucency larger than the screw (Figure 5). However, the screw was not clinically loose at removal. This potential complication, in combination with the bent screw (Figure 4) before removal, highlights the concern for screw breakage with this technique, given the increased construct stiffness caused by the added plate.
Conclusion
As in the other reports mentioned, our patient had an excellent clinical and radiographic outcome. It could be inferred that, if fixation for isolated clavicle fractures demonstrates improved function, better outcomes would be seen for higher-energy fractures associated with AC dislocation. Given the current trend toward surgical fixation for certain clavicle fractures, we recommend that clavicle fractures associated with type IV AC dislocation be treated with ORIF of both injuries.
1. Ring D, Jupiter J. Injuries to the shoulder girdle. In: Browner, BD. Skeletal Trauma. Philadelphia, PA: Elsevier Health Sciences; 2008:1755-1778.
2. Altamimi SA, McKee MD; Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):1-8.
3. Juhn MS, Simonian PT. Type VI acromioclavicular separation with middle-third clavicle fracture in an ice hockey player. Clin J Sports Med. 2002;12(5):315-317.
4. Lancourt JE. Acromioclavicular dislocation with adjacent clavicular fracture in a horseback rider. A case report. Am J Sports Med. 1990;18(3):321-322.
5. Wurtz LD, Lyons FA, Rockwood CA Jr. Fracture of the middle third of the clavicle and dislocation of the acromioclavicular joint. A report of four cases. J Bone Joint Surg Am. 1992;74(1):133-137.
6. Yeh PC, Miller SR, Cunningham JG, Sethi PM. Midshaft clavicle fracture and acromioclavicular dislocation: a case report of a rare injury. J Shoulder Elbow Surg. 2009;18(5):e1-e4.
7. Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br. 1988;70(3):461-464.
8. Kim W, McKee MD. Management of acute clavicle fractures. Orthop Clin North Am. 2008;39(4):491-505.
9. Woolf SK, Valentine BJ, Barfield WR, Hartsock LA. Middle-third clavicle fracture with associated type IV acromioclavicular separation: case report and literature review. J Surg Orthop Adv. 2013;22(2):183-186.
Acromioclavicular (AC) dislocations and displaced fractures of the middle third of the clavicle rarely occur together. Isolated AC joint separation is often treated nonoperatively with internal coracoclavicular (CC) fixation or reconstruction considered for type IV-VI AC dislocations and some type III injuries.1 Isolated clavicle fractures traditionally have been treated nonoperatively. The current trend is toward internal fixation for displaced and shortened fractures.2 There have been only a handful of reports of concomitant AC dislocation and midshaft clavicle fracture.3-6 Previous treatments have included nonoperative treatment, AC fixation, or internal fixation of the clavicle with ligamentous reconstruction.
We present a previously undescribed technique for internal fixation of this rare shoulder injury. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
While driving an all-terrain vehicle, a healthy 19-year-old right-hand–dominant man hit a bridge and sustained direct impact to his right shoulder. He presented to the emergency department complaining of right shoulder pain and deformity without skin disruption, vascular insufficiency, or neurologic symptoms. Anteroposterior (AP) radiograph showed an oblique, displaced, middle-third clavicle shaft fracture (Figure 1). An associated type IV AC dislocation was confirmed on axillary radiograph (Figure 2) and on an axial cut from a trauma chest computed tomography (CT) scan (Figure 3). The patient was discharged home from the trauma service the next day with a sling for comfort and plans for delayed, elective operative fixation 1 week later.
The patient was placed in a beach-chair position. Through a longitudinal incision extending laterally over the AC joint, the clavicle was exposed for fracture reduction, with care taken to retain soft-tissue attachments. The distal clavicle was buttonholed posteriorly through the trapezius muscle and fascia. The distal fracture fragment was devoid of any remaining CC ligamentous attachment. After satisfactory reduction, a low-profile precontoured clavicle plate (Superior Midshaft Clavicle Plate; Acumed, Hillsboro, Oregon) was placed superiorly; the fracture was compressed through the plate and internally fixed with three 3.5-mm bicortical screws on both sides of the fracture. Approximately 5 mm of the distal clavicle was resected at the AC joint to facilitate adequate AC and CC reduction without disruption of the clavicle fracture. With an adequate CC reduction, a 3.5-mm fully threaded cortical screw was placed through the most distal hole in the clavicle plate, clavicle, and coracoid.
After surgery, the patient was placed into an ARC shoulder immobilizer (Bledsoe, Grand Prairie, Texas) for 6 weeks, removing the immobilizer only for elbow and wrist range of motion (ROM) exercises. Radiographs at 3-month follow-up (Figure 4) showed a healed fracture with no loss of AC or CC reduction. Three months after surgery, another procedure was performed to remove the CC screw. One year after the initial surgery, the patient complained of intermittent soreness over the lateral shoulder but was not limited in his activities and was back to performing manual labor without difficulty. He had full ROM in forward flexion, abduction, internal rotation, and external rotation without weakness, tenderness, or any neurovascular deficit. After CC screw removal, no deformity returned at the shoulder. Radiographs showed a healed fracture with minimal superior subluxation at the AC joint without significant change from the 3-month follow-up (Figure 5).
Discussion
The combined injury pattern of a type IV AC dislocation and a displaced middle-third clavicle shaft fracture is rare. The usual mechanism of injury, as seen in the present case, is a direct blow to the shoulder at the tip of the acromion, though indirect forces from a fall on an outstretched hand are also described.7 Disruption of the CC ligaments with AC separation likely dissipates the stress necessary to create a clavicle fracture in most cases,1 explaining the rarity of this injury. It is imperative to evaluate patients for injury to both the osseous and ligamentous structures.
Previous case reports of concomitant AC separation and midshaft clavicle fracture have described a variety of treatment options, but to date our case represents the only episode in which both the clavicle fracture and the AC joint were treated with open reduction and internal fixation (ORIF). Wurtz and colleagues5 reported on a series of 4 patients with AC disruption and middle-third clavicle fracture. Three of the 4 patients had type IV AC separation; all 3 were treated, 2 acutely and 1 chronically, with open reduction of the AC and CC joints; 2 of these patients had CC screw fixation only after reduction, and the third had 2 Steinmann pins placed across the AC joint without CC screw fixation. All hardware was removed after 12 weeks. The fourth patient had a type II AC dislocation and was treated with closed reduction of the clavicle with no intervention for the AC joint. None of the clavicle fractures in this series were treated with internal fixation. All patients had full and pain-free ROM at 1- to 3-year follow-up.
Juhn and Simonian3 reported on a case of type VI separation with greenstick midshaft clavicle fracture in a hockey player seen 7 days after injury. The patient described some tingling in the upper extremity and had shoulder pain on initial presentation but was noted to have minimal displacement of both the AC joint and the midshaft clavicle fracture. Both injuries were treated nonsurgically with good outcome, and the patient returned to full activity (including hockey) within 14 weeks after injury.
Lancourt4 described the case of a patient with a type V AC dislocation and a displaced midshaft clavicle fracture. The AC joint was treated with Steinmann pin fixation, and the clavicle fracture was treated nonoperatively. The author cited high complication rates of plate fixation for clavicle fractures as the reason for not performing the additional procedure. The pins were removed 8 weeks after surgery. At 3-year follow-up, the patient had good radiographic and clinical outcome.
Yeh and colleagues6 described a patient who sustained a displaced midshaft clavicle fracture and a type IV AC dislocation in a fall from a horse. The patient underwent ORIF of the clavicle fracture with plate fixation. After the procedure, the AC joint was still unstable intraoperatively, and the AC and CC ligaments were reconstructed with semitendinosus allograft. The patient had full and painless ROM at 1-year follow-up.
The present case report serves as a reminder to obtain adequate shoulder radiographs when evaluating “just another clavicle fracture.” The radiographs should include a good axillary view to ensure there is not an associated AC dislocation. Increasingly, some authors have been advocating internal fixation for clavicle fractures, with reports of improved functional outcomes, improved cosmesis, and increased union rates.2 Indications for operative fixation include shortening and 100% displacement,8 and relative indications include open fractures.1 Operative fixation is perhaps more important for younger, athletic, and manual-labor populations. The trend in treatment of clavicle fractures toward operative fixation lends itself well to ORIF of the AC and CC joints; hence, a modern treatment for this rarely described combination injury should include internal plate fixation of the clavicle in addition to CC fixation. This additional procedure requires little extra time and energy in an operative scenario already requiring anesthesia, with easy insertion of the CC screw through the clavicle plate. Use of a CC screw obviates any potential risks associated with use of allograft tissue, and there is no anticipated difficulty with screw removal at 12 weeks.
Alternative options for AC stability include CC reconstruction with ligamentous allograft, ligamentous autograft, or suture/tightrope techniques. A noted advantage of these alternative techniques is less need to return to the operating room for the hardware removal that is recommended with CC screw fixation. However, these procedures potentially increase surgical exposure and operating time. In addition, screw fixation minimizes the possibility of donor-site morbidity from autograft transfers and potential complications from allograft tissue.
Hook plate fixation of the AC joint has also been described. In a recent case report of a similar injury pattern, plate fixation of the clavicle with simultaneous hook plate fixation of the AC joint was described.9 The patient did well but required removal of hardware of the hook plate and the clavicle plate 1 and 3 years after surgery, respectively. Although screw fixation is biomechanically stronger, debate persists about the clinical importance of this increase in strength.1 In the setting of plate fixation for the clavicle, these alternative AC fixations would require technique adjustments, including length of grafts and/or sutures, and raise concerns regarding interaction of the metal with the fixation material.
Critical evaluation of our technique revealed a lucency larger than the screw (Figure 5). However, the screw was not clinically loose at removal. This potential complication, in combination with the bent screw (Figure 4) before removal, highlights the concern for screw breakage with this technique, given the increased construct stiffness caused by the added plate.
Conclusion
As in the other reports mentioned, our patient had an excellent clinical and radiographic outcome. It could be inferred that, if fixation for isolated clavicle fractures demonstrates improved function, better outcomes would be seen for higher-energy fractures associated with AC dislocation. Given the current trend toward surgical fixation for certain clavicle fractures, we recommend that clavicle fractures associated with type IV AC dislocation be treated with ORIF of both injuries.
Acromioclavicular (AC) dislocations and displaced fractures of the middle third of the clavicle rarely occur together. Isolated AC joint separation is often treated nonoperatively with internal coracoclavicular (CC) fixation or reconstruction considered for type IV-VI AC dislocations and some type III injuries.1 Isolated clavicle fractures traditionally have been treated nonoperatively. The current trend is toward internal fixation for displaced and shortened fractures.2 There have been only a handful of reports of concomitant AC dislocation and midshaft clavicle fracture.3-6 Previous treatments have included nonoperative treatment, AC fixation, or internal fixation of the clavicle with ligamentous reconstruction.
We present a previously undescribed technique for internal fixation of this rare shoulder injury. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
While driving an all-terrain vehicle, a healthy 19-year-old right-hand–dominant man hit a bridge and sustained direct impact to his right shoulder. He presented to the emergency department complaining of right shoulder pain and deformity without skin disruption, vascular insufficiency, or neurologic symptoms. Anteroposterior (AP) radiograph showed an oblique, displaced, middle-third clavicle shaft fracture (Figure 1). An associated type IV AC dislocation was confirmed on axillary radiograph (Figure 2) and on an axial cut from a trauma chest computed tomography (CT) scan (Figure 3). The patient was discharged home from the trauma service the next day with a sling for comfort and plans for delayed, elective operative fixation 1 week later.
The patient was placed in a beach-chair position. Through a longitudinal incision extending laterally over the AC joint, the clavicle was exposed for fracture reduction, with care taken to retain soft-tissue attachments. The distal clavicle was buttonholed posteriorly through the trapezius muscle and fascia. The distal fracture fragment was devoid of any remaining CC ligamentous attachment. After satisfactory reduction, a low-profile precontoured clavicle plate (Superior Midshaft Clavicle Plate; Acumed, Hillsboro, Oregon) was placed superiorly; the fracture was compressed through the plate and internally fixed with three 3.5-mm bicortical screws on both sides of the fracture. Approximately 5 mm of the distal clavicle was resected at the AC joint to facilitate adequate AC and CC reduction without disruption of the clavicle fracture. With an adequate CC reduction, a 3.5-mm fully threaded cortical screw was placed through the most distal hole in the clavicle plate, clavicle, and coracoid.
After surgery, the patient was placed into an ARC shoulder immobilizer (Bledsoe, Grand Prairie, Texas) for 6 weeks, removing the immobilizer only for elbow and wrist range of motion (ROM) exercises. Radiographs at 3-month follow-up (Figure 4) showed a healed fracture with no loss of AC or CC reduction. Three months after surgery, another procedure was performed to remove the CC screw. One year after the initial surgery, the patient complained of intermittent soreness over the lateral shoulder but was not limited in his activities and was back to performing manual labor without difficulty. He had full ROM in forward flexion, abduction, internal rotation, and external rotation without weakness, tenderness, or any neurovascular deficit. After CC screw removal, no deformity returned at the shoulder. Radiographs showed a healed fracture with minimal superior subluxation at the AC joint without significant change from the 3-month follow-up (Figure 5).
Discussion
The combined injury pattern of a type IV AC dislocation and a displaced middle-third clavicle shaft fracture is rare. The usual mechanism of injury, as seen in the present case, is a direct blow to the shoulder at the tip of the acromion, though indirect forces from a fall on an outstretched hand are also described.7 Disruption of the CC ligaments with AC separation likely dissipates the stress necessary to create a clavicle fracture in most cases,1 explaining the rarity of this injury. It is imperative to evaluate patients for injury to both the osseous and ligamentous structures.
Previous case reports of concomitant AC separation and midshaft clavicle fracture have described a variety of treatment options, but to date our case represents the only episode in which both the clavicle fracture and the AC joint were treated with open reduction and internal fixation (ORIF). Wurtz and colleagues5 reported on a series of 4 patients with AC disruption and middle-third clavicle fracture. Three of the 4 patients had type IV AC separation; all 3 were treated, 2 acutely and 1 chronically, with open reduction of the AC and CC joints; 2 of these patients had CC screw fixation only after reduction, and the third had 2 Steinmann pins placed across the AC joint without CC screw fixation. All hardware was removed after 12 weeks. The fourth patient had a type II AC dislocation and was treated with closed reduction of the clavicle with no intervention for the AC joint. None of the clavicle fractures in this series were treated with internal fixation. All patients had full and pain-free ROM at 1- to 3-year follow-up.
Juhn and Simonian3 reported on a case of type VI separation with greenstick midshaft clavicle fracture in a hockey player seen 7 days after injury. The patient described some tingling in the upper extremity and had shoulder pain on initial presentation but was noted to have minimal displacement of both the AC joint and the midshaft clavicle fracture. Both injuries were treated nonsurgically with good outcome, and the patient returned to full activity (including hockey) within 14 weeks after injury.
Lancourt4 described the case of a patient with a type V AC dislocation and a displaced midshaft clavicle fracture. The AC joint was treated with Steinmann pin fixation, and the clavicle fracture was treated nonoperatively. The author cited high complication rates of plate fixation for clavicle fractures as the reason for not performing the additional procedure. The pins were removed 8 weeks after surgery. At 3-year follow-up, the patient had good radiographic and clinical outcome.
Yeh and colleagues6 described a patient who sustained a displaced midshaft clavicle fracture and a type IV AC dislocation in a fall from a horse. The patient underwent ORIF of the clavicle fracture with plate fixation. After the procedure, the AC joint was still unstable intraoperatively, and the AC and CC ligaments were reconstructed with semitendinosus allograft. The patient had full and painless ROM at 1-year follow-up.
The present case report serves as a reminder to obtain adequate shoulder radiographs when evaluating “just another clavicle fracture.” The radiographs should include a good axillary view to ensure there is not an associated AC dislocation. Increasingly, some authors have been advocating internal fixation for clavicle fractures, with reports of improved functional outcomes, improved cosmesis, and increased union rates.2 Indications for operative fixation include shortening and 100% displacement,8 and relative indications include open fractures.1 Operative fixation is perhaps more important for younger, athletic, and manual-labor populations. The trend in treatment of clavicle fractures toward operative fixation lends itself well to ORIF of the AC and CC joints; hence, a modern treatment for this rarely described combination injury should include internal plate fixation of the clavicle in addition to CC fixation. This additional procedure requires little extra time and energy in an operative scenario already requiring anesthesia, with easy insertion of the CC screw through the clavicle plate. Use of a CC screw obviates any potential risks associated with use of allograft tissue, and there is no anticipated difficulty with screw removal at 12 weeks.
Alternative options for AC stability include CC reconstruction with ligamentous allograft, ligamentous autograft, or suture/tightrope techniques. A noted advantage of these alternative techniques is less need to return to the operating room for the hardware removal that is recommended with CC screw fixation. However, these procedures potentially increase surgical exposure and operating time. In addition, screw fixation minimizes the possibility of donor-site morbidity from autograft transfers and potential complications from allograft tissue.
Hook plate fixation of the AC joint has also been described. In a recent case report of a similar injury pattern, plate fixation of the clavicle with simultaneous hook plate fixation of the AC joint was described.9 The patient did well but required removal of hardware of the hook plate and the clavicle plate 1 and 3 years after surgery, respectively. Although screw fixation is biomechanically stronger, debate persists about the clinical importance of this increase in strength.1 In the setting of plate fixation for the clavicle, these alternative AC fixations would require technique adjustments, including length of grafts and/or sutures, and raise concerns regarding interaction of the metal with the fixation material.
Critical evaluation of our technique revealed a lucency larger than the screw (Figure 5). However, the screw was not clinically loose at removal. This potential complication, in combination with the bent screw (Figure 4) before removal, highlights the concern for screw breakage with this technique, given the increased construct stiffness caused by the added plate.
Conclusion
As in the other reports mentioned, our patient had an excellent clinical and radiographic outcome. It could be inferred that, if fixation for isolated clavicle fractures demonstrates improved function, better outcomes would be seen for higher-energy fractures associated with AC dislocation. Given the current trend toward surgical fixation for certain clavicle fractures, we recommend that clavicle fractures associated with type IV AC dislocation be treated with ORIF of both injuries.
1. Ring D, Jupiter J. Injuries to the shoulder girdle. In: Browner, BD. Skeletal Trauma. Philadelphia, PA: Elsevier Health Sciences; 2008:1755-1778.
2. Altamimi SA, McKee MD; Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):1-8.
3. Juhn MS, Simonian PT. Type VI acromioclavicular separation with middle-third clavicle fracture in an ice hockey player. Clin J Sports Med. 2002;12(5):315-317.
4. Lancourt JE. Acromioclavicular dislocation with adjacent clavicular fracture in a horseback rider. A case report. Am J Sports Med. 1990;18(3):321-322.
5. Wurtz LD, Lyons FA, Rockwood CA Jr. Fracture of the middle third of the clavicle and dislocation of the acromioclavicular joint. A report of four cases. J Bone Joint Surg Am. 1992;74(1):133-137.
6. Yeh PC, Miller SR, Cunningham JG, Sethi PM. Midshaft clavicle fracture and acromioclavicular dislocation: a case report of a rare injury. J Shoulder Elbow Surg. 2009;18(5):e1-e4.
7. Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br. 1988;70(3):461-464.
8. Kim W, McKee MD. Management of acute clavicle fractures. Orthop Clin North Am. 2008;39(4):491-505.
9. Woolf SK, Valentine BJ, Barfield WR, Hartsock LA. Middle-third clavicle fracture with associated type IV acromioclavicular separation: case report and literature review. J Surg Orthop Adv. 2013;22(2):183-186.
1. Ring D, Jupiter J. Injuries to the shoulder girdle. In: Browner, BD. Skeletal Trauma. Philadelphia, PA: Elsevier Health Sciences; 2008:1755-1778.
2. Altamimi SA, McKee MD; Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):1-8.
3. Juhn MS, Simonian PT. Type VI acromioclavicular separation with middle-third clavicle fracture in an ice hockey player. Clin J Sports Med. 2002;12(5):315-317.
4. Lancourt JE. Acromioclavicular dislocation with adjacent clavicular fracture in a horseback rider. A case report. Am J Sports Med. 1990;18(3):321-322.
5. Wurtz LD, Lyons FA, Rockwood CA Jr. Fracture of the middle third of the clavicle and dislocation of the acromioclavicular joint. A report of four cases. J Bone Joint Surg Am. 1992;74(1):133-137.
6. Yeh PC, Miller SR, Cunningham JG, Sethi PM. Midshaft clavicle fracture and acromioclavicular dislocation: a case report of a rare injury. J Shoulder Elbow Surg. 2009;18(5):e1-e4.
7. Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br. 1988;70(3):461-464.
8. Kim W, McKee MD. Management of acute clavicle fractures. Orthop Clin North Am. 2008;39(4):491-505.
9. Woolf SK, Valentine BJ, Barfield WR, Hartsock LA. Middle-third clavicle fracture with associated type IV acromioclavicular separation: case report and literature review. J Surg Orthop Adv. 2013;22(2):183-186.