User login
The time is now for physicians to ride the digital disruption wave
CHICAGO – “The health care milieu is ripe for digital disruption,” said Anton Decker, MD. Speaking at the American Gastroenterological Association Partners in Value meeting, which was developed in partnership with the Digestive Health Physicians Association, he said that physicians need to become part of the disruption before it’s too late.
There’s no sign of improvement in worrisome trends in reimbursement, said Dr. Decker, president, international, at the Mayo Clinic, Rochester, Minn. The megamerger trend that is bringing together ever-larger payers, pharmacy benefit managers, and hospital groups is just one manifestation of the trend toward consolidation that’s also seen in the airline industry, in financial services, and in telecommunications, he said.
“The math is not good on the payer and health systems side,” but for physicians, “There are ways to survive trends like this if we can move ourselves higher in the food chain.”
Other players in the health care space are figuring it out, he said. For example, the state of Ohio has five Medicaid plans; in 2018, aggregate profits for these plans were approximately 400 million dollars. Laying this profit figure against the backdrop of Medicare reimbursement rates for physician services makes it clear that “we have to figure out ways to survive this game,” he said.
“Health systems keep their lights on because of the hospital reimbursements – that pays for everything else,” said Dr. Decker, adding that payments from commercial insurers fill the coffers that, in turn, pay physicians who are employed by health systems. However, there’s a sea change underway in the sites in which care is delivered: “There’s enormous pressure to get people out of the hospital and out of the emergency rooms,” said Dr. Decker, “And that’s not always better for patients.”
That shift to delivering care outside of the four walls of the hospital represents an opportunity for digitally savvy companies, many of whom may actually have little experience with health care delivery.
“Digital disruption is a sleeping giant that is easy to ignore, but you do that at your own peril. It’s happening in front of your eyes. My message today is: Figure out how you can move yourself further down the line.”
Chronic diseases, said Dr. Decker, “represent an opportunity for providers and health systems to leverage digital disruption.”
Overall, health care services contribute only to 10% of a patient’s health, said Dr. Decker, and are far overshadowed by individual health behaviors and social determinants of health. Is there a role for physicians to move beyond the clinic and hospital as partners in the digital disruption of health care? Yes, said Dr. Decker: “We’re not part of that aspect of a person’s life, and we need to be. ... I believe that providers have the right to be involved in other aspects of peoples’ lives to make them better, and yes, also to survive financially.”
said Dr. Decker. “Sixty percent of this country has a chronic disease. We as health care providers need to think differently about that.”
Changes are already well underway, with score upon score of startup companies developing apps that utilize smartphones and wearable devices to offer coaching, health education, and remote monitoring to consumers. “The barrier to entry is really low,” said Dr. Decker, with Silicon Valley already partnering with patients and payers to achieve digital monitoring and care delivery. But relatively few of these partnerships have actually involved physicians in building and executing the solutions they offer. “And that’s our fault, for not making sure we are part of this disruption,” he said.
Further, the evidence base for much of this monitoring and intervention is low. “There are some scathing articles on the level of evidence that these apps have – or don’t have,” said Dr. Becker. Physicians who get on board at the early stages of technology development could make a real difference, he said. “We could help them build the real evidence.”
Looping back to the current payer model, Dr. Decker asked, “Which pool of money is this coming from?” From the same pool of money that pays physicians, he said: “It’s coming off our backs.”
This isn’t a time when physicians can afford to wait and see how the digital health care landscape evolves, stressed Dr. Decker, making the subtle but important point that it’s hard to discern when you’re in the middle of disruptive change. Though the curve may appear relatively flat at the moment, he assured attendees that exponential growth in digital health care is already well underway.
Here is where early entry and user adoption are key: “Why do you think Facebook bought WhatsApp?” he asked. Though the messaging app, which has more than a billion users worldwide, is free now, eventual plans to charge WhatsApp users a dollar – or even less – per year will net Facebook staggering sums in the end, he said. Companies like Facebook “have figured out...the strength of exponential growth in a digital world,” he said.
All the building blocks are in place for physicians to begin contributing to health care’s digital disruption, said Dr. Decker. The Centers for Medicare and Medicaid already have reimbursement codes for remote patient monitoring, for example. “Providers are being left out, and I think it’s our own fault.”
Dr. Decker reported that he had no relevant conflicts of interest.
CHICAGO – “The health care milieu is ripe for digital disruption,” said Anton Decker, MD. Speaking at the American Gastroenterological Association Partners in Value meeting, which was developed in partnership with the Digestive Health Physicians Association, he said that physicians need to become part of the disruption before it’s too late.
There’s no sign of improvement in worrisome trends in reimbursement, said Dr. Decker, president, international, at the Mayo Clinic, Rochester, Minn. The megamerger trend that is bringing together ever-larger payers, pharmacy benefit managers, and hospital groups is just one manifestation of the trend toward consolidation that’s also seen in the airline industry, in financial services, and in telecommunications, he said.
“The math is not good on the payer and health systems side,” but for physicians, “There are ways to survive trends like this if we can move ourselves higher in the food chain.”
Other players in the health care space are figuring it out, he said. For example, the state of Ohio has five Medicaid plans; in 2018, aggregate profits for these plans were approximately 400 million dollars. Laying this profit figure against the backdrop of Medicare reimbursement rates for physician services makes it clear that “we have to figure out ways to survive this game,” he said.
“Health systems keep their lights on because of the hospital reimbursements – that pays for everything else,” said Dr. Decker, adding that payments from commercial insurers fill the coffers that, in turn, pay physicians who are employed by health systems. However, there’s a sea change underway in the sites in which care is delivered: “There’s enormous pressure to get people out of the hospital and out of the emergency rooms,” said Dr. Decker, “And that’s not always better for patients.”
That shift to delivering care outside of the four walls of the hospital represents an opportunity for digitally savvy companies, many of whom may actually have little experience with health care delivery.
“Digital disruption is a sleeping giant that is easy to ignore, but you do that at your own peril. It’s happening in front of your eyes. My message today is: Figure out how you can move yourself further down the line.”
Chronic diseases, said Dr. Decker, “represent an opportunity for providers and health systems to leverage digital disruption.”
Overall, health care services contribute only to 10% of a patient’s health, said Dr. Decker, and are far overshadowed by individual health behaviors and social determinants of health. Is there a role for physicians to move beyond the clinic and hospital as partners in the digital disruption of health care? Yes, said Dr. Decker: “We’re not part of that aspect of a person’s life, and we need to be. ... I believe that providers have the right to be involved in other aspects of peoples’ lives to make them better, and yes, also to survive financially.”
said Dr. Decker. “Sixty percent of this country has a chronic disease. We as health care providers need to think differently about that.”
Changes are already well underway, with score upon score of startup companies developing apps that utilize smartphones and wearable devices to offer coaching, health education, and remote monitoring to consumers. “The barrier to entry is really low,” said Dr. Decker, with Silicon Valley already partnering with patients and payers to achieve digital monitoring and care delivery. But relatively few of these partnerships have actually involved physicians in building and executing the solutions they offer. “And that’s our fault, for not making sure we are part of this disruption,” he said.
Further, the evidence base for much of this monitoring and intervention is low. “There are some scathing articles on the level of evidence that these apps have – or don’t have,” said Dr. Becker. Physicians who get on board at the early stages of technology development could make a real difference, he said. “We could help them build the real evidence.”
Looping back to the current payer model, Dr. Decker asked, “Which pool of money is this coming from?” From the same pool of money that pays physicians, he said: “It’s coming off our backs.”
This isn’t a time when physicians can afford to wait and see how the digital health care landscape evolves, stressed Dr. Decker, making the subtle but important point that it’s hard to discern when you’re in the middle of disruptive change. Though the curve may appear relatively flat at the moment, he assured attendees that exponential growth in digital health care is already well underway.
Here is where early entry and user adoption are key: “Why do you think Facebook bought WhatsApp?” he asked. Though the messaging app, which has more than a billion users worldwide, is free now, eventual plans to charge WhatsApp users a dollar – or even less – per year will net Facebook staggering sums in the end, he said. Companies like Facebook “have figured out...the strength of exponential growth in a digital world,” he said.
All the building blocks are in place for physicians to begin contributing to health care’s digital disruption, said Dr. Decker. The Centers for Medicare and Medicaid already have reimbursement codes for remote patient monitoring, for example. “Providers are being left out, and I think it’s our own fault.”
Dr. Decker reported that he had no relevant conflicts of interest.
CHICAGO – “The health care milieu is ripe for digital disruption,” said Anton Decker, MD. Speaking at the American Gastroenterological Association Partners in Value meeting, which was developed in partnership with the Digestive Health Physicians Association, he said that physicians need to become part of the disruption before it’s too late.
There’s no sign of improvement in worrisome trends in reimbursement, said Dr. Decker, president, international, at the Mayo Clinic, Rochester, Minn. The megamerger trend that is bringing together ever-larger payers, pharmacy benefit managers, and hospital groups is just one manifestation of the trend toward consolidation that’s also seen in the airline industry, in financial services, and in telecommunications, he said.
“The math is not good on the payer and health systems side,” but for physicians, “There are ways to survive trends like this if we can move ourselves higher in the food chain.”
Other players in the health care space are figuring it out, he said. For example, the state of Ohio has five Medicaid plans; in 2018, aggregate profits for these plans were approximately 400 million dollars. Laying this profit figure against the backdrop of Medicare reimbursement rates for physician services makes it clear that “we have to figure out ways to survive this game,” he said.
“Health systems keep their lights on because of the hospital reimbursements – that pays for everything else,” said Dr. Decker, adding that payments from commercial insurers fill the coffers that, in turn, pay physicians who are employed by health systems. However, there’s a sea change underway in the sites in which care is delivered: “There’s enormous pressure to get people out of the hospital and out of the emergency rooms,” said Dr. Decker, “And that’s not always better for patients.”
That shift to delivering care outside of the four walls of the hospital represents an opportunity for digitally savvy companies, many of whom may actually have little experience with health care delivery.
“Digital disruption is a sleeping giant that is easy to ignore, but you do that at your own peril. It’s happening in front of your eyes. My message today is: Figure out how you can move yourself further down the line.”
Chronic diseases, said Dr. Decker, “represent an opportunity for providers and health systems to leverage digital disruption.”
Overall, health care services contribute only to 10% of a patient’s health, said Dr. Decker, and are far overshadowed by individual health behaviors and social determinants of health. Is there a role for physicians to move beyond the clinic and hospital as partners in the digital disruption of health care? Yes, said Dr. Decker: “We’re not part of that aspect of a person’s life, and we need to be. ... I believe that providers have the right to be involved in other aspects of peoples’ lives to make them better, and yes, also to survive financially.”
said Dr. Decker. “Sixty percent of this country has a chronic disease. We as health care providers need to think differently about that.”
Changes are already well underway, with score upon score of startup companies developing apps that utilize smartphones and wearable devices to offer coaching, health education, and remote monitoring to consumers. “The barrier to entry is really low,” said Dr. Decker, with Silicon Valley already partnering with patients and payers to achieve digital monitoring and care delivery. But relatively few of these partnerships have actually involved physicians in building and executing the solutions they offer. “And that’s our fault, for not making sure we are part of this disruption,” he said.
Further, the evidence base for much of this monitoring and intervention is low. “There are some scathing articles on the level of evidence that these apps have – or don’t have,” said Dr. Becker. Physicians who get on board at the early stages of technology development could make a real difference, he said. “We could help them build the real evidence.”
Looping back to the current payer model, Dr. Decker asked, “Which pool of money is this coming from?” From the same pool of money that pays physicians, he said: “It’s coming off our backs.”
This isn’t a time when physicians can afford to wait and see how the digital health care landscape evolves, stressed Dr. Decker, making the subtle but important point that it’s hard to discern when you’re in the middle of disruptive change. Though the curve may appear relatively flat at the moment, he assured attendees that exponential growth in digital health care is already well underway.
Here is where early entry and user adoption are key: “Why do you think Facebook bought WhatsApp?” he asked. Though the messaging app, which has more than a billion users worldwide, is free now, eventual plans to charge WhatsApp users a dollar – or even less – per year will net Facebook staggering sums in the end, he said. Companies like Facebook “have figured out...the strength of exponential growth in a digital world,” he said.
All the building blocks are in place for physicians to begin contributing to health care’s digital disruption, said Dr. Decker. The Centers for Medicare and Medicaid already have reimbursement codes for remote patient monitoring, for example. “Providers are being left out, and I think it’s our own fault.”
Dr. Decker reported that he had no relevant conflicts of interest.
EXPERT ANALYSIS FROM AGA PARTNERS IN VALUE MEETING
Patients frequently drive too soon after ICD implantation
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
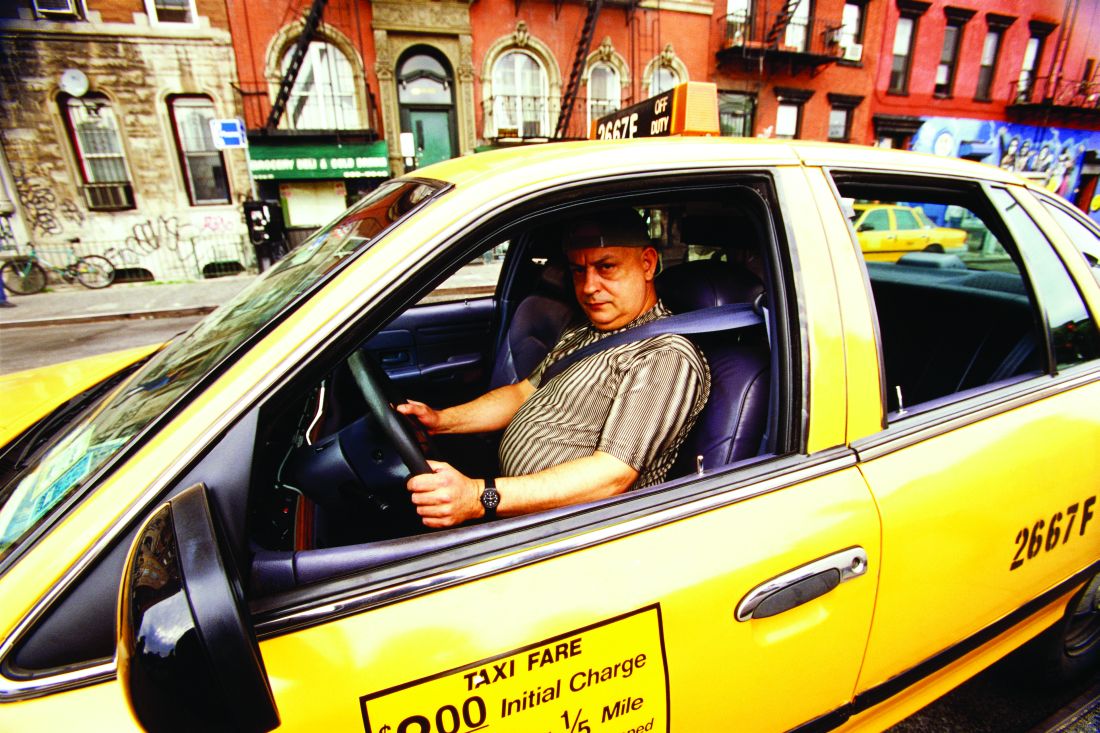
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
PARIS – Fewer than half of commercial drivers who received implantable cardioverter-defibrillators (ICDs) recalled being told they should never drive professionally again, according to a recent Danish survey. Further, about a third of patients overall reported that they began driving soon after they received an ICD, during the period when guidelines recommend refraining from driving.
“These devices, they save lives – so what’s not to like?” lead investigator Jenny Bjerre, MD, asked at the annual congress of the European Society of Cardiology. “Well, if you are a patient qualifying for an ICD, you also automatically qualify for some driving restrictions.” These are put in place because of the concern for an arrhythmia causing a loss of consciousness behind the wheel, she said.
A European consensus statement calls for a 3-month driving moratorium when an ICD is implanted for secondary prevention or after an appropriate ICD shock, and a 4-week restriction when an ICD is placed for primary prevention. All these restrictions apply to personal driver’s licenses; anyone with an ICD is permanently restricted from commercial driving according to the consensus statement, said Dr. Bjerre, of the University Hospital, Copenhagen.
“As you can imagine, these restrictions are not that popular with the patients,” she said. She related the story of a patient, a taxi driver who had returned to a full range of physically taxing activities after his ICD implantation, but whose livelihood had been taken away from him.
Dr. Bjerre said she sought to understand the perspective of this patient, who said, “Sometimes I wish I hadn’t been resuscitated!” She saw that the loss of freedom and a meaningful occupation had profoundly affected the daily life of this patient, and she became curious about adherence to driving restrictions in patients with ICDs.
Using the nationwide Danish medical record database, Dr. Bjerre and her colleagues looked at a nationwide cohort of ICD patients to see they remembered hearing about restrictions on personal and commercial driving activities after ICD implantation. They also investigated adherence to restrictions, and sought to identify what factors were associated with nonadherence.
The questionnaire developed by Dr. Bjerre and her colleagues was made available to the ICD cohort both electronically and in a paper version. Questionnaires received were linked with a variety of nationwide registries through each participant’s unique national identification number, she explained. They obtained information about comorbidities, pharmacotherapies, and socioeconomic status. Not only did this linkage give more precise and complete data than would a questionnaire alone, but it also allowed the investigators to see how responders differed from nonresponders – important in questionnaire research, said Dr. Bjerre.
The investigators were able to locate and distribute questionnaires to a total of 3,913 living adults who had received first-time ICDs during the 3-year study period. In the end, even after excluding 31 responses for missing data, 2,741 responses were used for analysis – a response rate of over 70%.
The median age of respondents was 67, and 83% were male. About half – 46% – of respondents had an ICD implanted for primary prevention. Compared with those who did respond, said Dr. Bjerre, the nonresponders “were younger, sicker, more likely to be female, had lower socioeconomic status, and were less likely to be on guideline-directed therapy.”
Over 90% of respondents held a private driver’s license at the time of their ICD implantation, and just 7% were actively using a commercial license prior to implantation. Participants had a variety of commercial driving occupations, including driving trucks, buses, and taxis.
“Only 43% of primary prevention patients and 64% of secondary prevention patients stated that they had been informed about any driving restrictions,” said Dr. Bjerre. The figure was slightly better for patients after an ICD shock was delivered – 72% of these patients recalled hearing about driving restrictions.
“Among professional drivers – who are never supposed to drive again – only 45% said they had been informed about any professional driving restrictions,” she added.
What did patients report about their actual driving behaviors? Of patients receiving an ICD for primary prevention, 34% resumed driving within one week of ICD implantation. For those receiving an ICD for secondary prevention and those who had received an appropriate ICD shock, 43% and 30%, respectively, began driving before the recommended 3 months had elapsed.
The driving behavior of those with commercial licenses didn’t differ from the cohort as a whole: 35% of this group had resumed commercial driving.
In all the study’s subgroups, nonadherence to driving restrictions was more likely if the participant didn’t recall having been informed of the restrictions, with an odds ratio (OR) of 3.34 for nonadherence. However, noted Dr. Bjerre, at least 20% of patients in all subgroups who said they’d been told not to drive still resumed driving in contravention of restrictions. “So it seems that information can’t explain everything,” she said.
Additional predictors of nonadherence included male sex, with an OR of 1.53, being the only driver in the household (OR 1.29), and being at least 60 years old (OR, 1.20). Those receiving an ICD for secondary prevention had an OR of 2.20 for nonadherence, as well.
The study had a large cohort of real-life ICD patients and the response rate was high, said Dr. Bjerre. However, there was a risk of recall bias; additionally, nonresponders differed from responders, limiting full generalizability of the data. Finally, she observed that participants may have given the answers they thought were socially desirable.
“I want to get back to our friend the taxi driver,” who was adherent to restrictions, but who kept wanting to know what the actual chances were that he’d harm someone if he resumed driving. Realizing she couldn’t give him a very precise answer, Dr. Bjerre concluded, “I do think we owe it to our patients to provide more evidence on the absolute risk of traffic accidents in these patients.”
Dr. Bjerre reported that she had no conflicts of interest.
REPORTING FROM ESC CONGRESS 2019
Cancer overtakes CVD as cause of death in high-income countries
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
PARIS – Though cardiovascular disease still accounts for 40% of deaths around the world, , according to new data from a global prospective study.
“Cancer deaths are becoming more frequent not because the rates of death from cancer are going up, but because we have decreased the deaths from cardiovascular disease,” said the study’s senior author, Salim Yusuf, MD, at the annual congress of the European Society of Cardiology.
A striking pattern emerged when cause of death was stratified by country income level, said fellow investigator Darryl P. Leong, MBBS, in presenting data regarding shifting global mortality patterns. Fully 55% of deaths in high-income nations were caused by cancer, compared with 30% in middle-income countries and 15% in low-income countries. In high-income countries, by contrast, cardiovascular disease (CVD) was the cause of death 23% of the time, while that figure was 42% and 43% for middle- and low-income countries, respectively.
Looking at the data slightly differently, the ratio of cardiovascular deaths to cancer deaths for high-income countries is 0.4; for middle-income countries, the ratio is 1.3, and “One is threefold more likely to die from cardiovascular disease as from cancer” in low-income countries, said Dr. Leong. Although the United States is not included in the PURE study, “recent data shows that some states in the U.S. also have higher cancer mortality than cardiovascular disease. This is a success story,” said Dr. Yusuf, since the shift is largely attributable to decreased mortality from CVD.
Dr. Leong and Dr. Yusuf each presented results from the PURE (Prospective Urban Rural Epidemiology) study, which has enrolled a total of 202,000 individuals from 27 countries on every inhabited continent but Australia. Follow-up data are available for 167,000 individuals in 21 countries. Canada, Russia, China, India, Brazil, and Chile are among the most populous national that are included. Their findings were published simultaneously in the Lancet with the congress presentations (2019 Sep 3; doi: 10.1016/S0140-6736(19)32008-2 and doi: 10.1016/S0140-6736(19)32007-0).
The INTERHEART risk score, an integrated cardiovascular risk score that uses non-laboratory values such as age, smoking status, family history, and comorbidities, was calculated for all participants. “We observed that the highest predicted cardiovascular risk is in high-income countries, and the lowest, in low-income countries,” said Dr. Leong, a cardiologist at McMaster University and the Population Health Research Institute, both in Hamilton, Ont.
Over the study period, 11,307 deaths occurred. Over 9,000 incident cardiovascular events were observed, as were over 5,000 new cancers.
“We have some interesting observations from these data,” said Dr. Leong. “Firstly, there is a gradient in the cardiovascular disease rates, moving from lowest in high-income countries – despite the fact that their INTERHEART risk score was highest – through to highest incident cardiovascular disease in low-income countries, despite their INTERHEART risk score being lowest.” This difference, said Dr. Leong, was driven by higher myocardial infarction rates in low-income countries and higher stroke rates in middle-income countries, when compared to high-income countries.
Once a participant was subject to one of the incident diseases, though, the patterns shifted. For CVD, cancer, chronic obstructive pulmonary disease, pneumonia, and injury, the likelihood of death within 1 year was highest in low-income countries – markedly higher, in the case of CVD. For all conditions, the one-year case-fatality rate after the occurrence of an incident disease was lowest in high-income countries.
“So we are seeing a new transition,” said Dr. Yusuf, the executive director of the Population Health Research Institute and Distinguished University Professor of Medicine, McMaster University, both in Hamilton, Ont. “The old transition was infectious diseases giving way to noncommunicable diseases. Now we are seeing a transition within noncommunicable diseases: In rich countries, cardiovascular disease is going down, perhaps due to better prevention, but I think even more importantly, due to better treatments.
“I want to hasten to add that the difference in risk between high-, middle-, and low-income countries in cardiovascular disease is not due to risk factors,” he went on. “Risk factors, if anything, are lower in the poor countries, compared to the higher-income countries.”
The shift away from cardiovascular disease mortality toward cancer mortality is also occurring in some countries that are in the upper tier of middle-income nations, including Chile, Argentina, Turkey, and Poland, said Dr. Yusuf, who presented data regarding the relative contributions of risk factors to cardiovascular disease and mortality.
Risk factors for cardiovascular disease in the PURE study were expressed by a measure called the population attributable fraction (PAF) that captures both the hazard ratio for a particular risk factor and the prevalence of the risk factor, explained Dr. Yusuf. “Hypertension, by far, was the biggest risk factor of cardiovascular disease globally,” he added, noting that the PAF for hypertension was over 20%. Hypertension far outstripped the next most significant risk factor, high non-HDL cholesterol, which had a PAF of less than 10%.
“This was a big surprise to us: Household pollution was a big factor,” said Dr. Yusuf, who later added that particulate matter from cooking, particularly with solid fuels such as wood or charcoal, was likely the source of much household air pollution, “a big problem in middle- and low-income countries.”
Tobacco usage is decreasing, as is its contribution to cardiovascular deaths, but other commonly cited culprits for cardiovascular disease were not significant contributors to cardiovascular disease in the PURE population.
“Abdominal obesity, and not BMI” contributes to cardiovascular risk. “BMI is not a good indicator of risk,” said Dr. Yusuf in a video interview. These results were presented separately at the congress.
“Grip strength is important; in fact, it is more important than low physical activity. People have focused on physical activity – how much you do. But strength seems to be more important…We haven’t focused on the importance of strength in the past.”
“Salt doesn’t figure in at all; salt has been exaggerated as a risk factor,” said Dr. Yusuf. “Diet needs to be rethought,” and conventional thinking challenged, he added, noting that consumption of full-fat dairy, nuts, and a moderate amount of meat all were protective among the PURE cohort.
Looking next at factors contributing to mortality in the global PURE population, low educational level had the highest attributable fraction of mortality of any single risk factor, at about 12%. “This has been ignored,” said Dr. Yusuf. “In most epidemiological studies, it’s been used as a covariate, or a stratifier,” rather than addressing low education itself as a risk factor, he said.
Tobacco use, low grip strength, and poor diet all had attributable fractions of just over 10%, said Dr. Yusuf, again noting that it wasn’t fat or meat consumption that made for the riskiest diet.
Overall, metabolic risk factors accounted for the largest fraction of risk of cardiovascular disease in the PURE population, with behavioral risk factors such as alcohol and tobacco use coming next. This held true across all income categories. However, in higher income nations where environmental factors and household air pollution are lower contributors to cardiovascular disease, metabolic and behavioral risk factors contributed more to cardiovascular disease risk.
Global differences in cardiovascular disease rates, stressed Dr. Yusuf, are not primarily attributable to metabolic risk factors. “The [World Health Organization] has focused on risk factors and has not focused on improved health care. Health care matters, and it matters in a big way.”
Adults aged 35-70 were recruited from 4 high-, 12 middle- and 5 low-income countries for PURE, and followed for a median 9.5 years. Cardiovascular disease and other health events salient to the study were documented both through direct contact and administrative record review, said Dr. Leong, and data about cardiovascular events and vital status were known for well over 90% of study participants.
Slightly less than half of participants were male, and over 108,000 participants were from middle income countries.
The PURE study was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, the Ontaario Ministry of Health and Long-Term Care, Astra Zeneca, Boehringer Ingelheim, Sanofi-Aentis, Servier Laboratories, and Glaxo Smith Kline. The study also received additional support in individual participating countries. Dr. Yusuf and Dr. Leon reported that they had no relevant conflicts of interest.
REPORTING FROM ESC CONGRESS 2019
GALACTIC: Early vasodilation strategy no help in acute heart failure
PARIS – A practical strategy of early and aggressive vasodilation and optimization of long-term medication for acute heart failure did not budge all-cause mortality or 180-day readmission rates, according to results of a pragmatic trial presented at the annual congress of the European Society of Cardiology.
“To our great disappointment, the curves were superimposable” between intervention and control arms in the GALACTIC (Goal-directed Afterload Reduction in Acute Congestive Cardiac Decompensation) trial, said lead investigator Christian Eugen Mueller, MD. “There was no signal of a benefit” for those receiving the targeted intervention: the adjusted hazard ratio was 1.07 for the composite primary endpoint of all-cause mortality or 6-month readmission for acute heart failure (P = 0.59).
GALACTIC, explained Dr. Mueller, was the largest investigator-initiated, randomized, controlled trial of pharmacologic therapy for acute heart failure (AHF).
“It is different in that it did not investigate a single drug, but a strategy of early, intensive, and sustained vasodilation. It is also unique in that it used individual doses of well-characterized, widely available, and mostly inexpensive drugs,” said Dr. Mueller, director of the Cardiovascular Research Institute at the University Hospital, Basel, Switzerland. “So this would have the beauty that, if it has a positive finding, you – in whatever country you come from – would be immediately able to apply it once you’re back home in your institution.”
The study attempted to address the gap between symptom amelioration and long-term outcomes when patients arrive in the ED with AHF. “Despite symptomatic improvement achieved from loop diuretics, mortality and morbidity remain unacceptably high,” said Dr. Mueller, with 40%-50% of AHF patients experiencing rehospitalization or death within 180 days of discharge.
Much remains unknown about the optimal treatment strategy for AHF. Aggressive vasodilation has been shown to improve outcomes in less-severe AHF, and intravenous nitrates are known to improve outcomes in AHF where severe pulmonary edema is present – “a phenotype representing only about 5% of patients,” noted Dr. Mueller. Still, “it is unknown whether aggressive vasodilation also improves outcomes in the much more common less-severe phenotype.”
Also, previous trials that ran intravenous vasodilators at a fixed dose for 48 hours did not improve AHF outcomes, so a one-size-fits-all strategy was not one the GALACTIC investigators sought to pursue.
In addition to a flexible regimen, “any strategy applied needs to take into consideration that the vast majority of patients with acute heart failure, after initial treatment in the ED, are then treated in a general cardiology ward,” added Dr. Mueller.
This meant that intravenous nitrate infusion was not part of the GALACTIC trial; rather, sublingual and transdermal nitrates were used, explained Dr. Mueller. “Transdermal application has the beauty that if you have an adverse effect – and hypotension is the most dangerous one – you can immediately remove the patch, and thereby avoid any further harm.”
The two-part strategy tested in GALACTIC involved reducing cardiac filling pressures by maintaining or increasing organ perfusion, while also increasing “long-term lifesaving therapy” targeting the renin-angiotensin-aldosterone system during hospitalization, with a goal to continue optimal treatment long term.
ACE inhibitors or angiotensin receptor blockers were added on the second day of hospitalization for the intervention group, said Dr. Mueller, and “in the ideal setting, up-titrated very aggressively from day to day.
“However, as you know, up-titration to target dose is sometimes wishful thinking in this frail population,” he said, so the GALACTIC trial protocol included a scheme to back dosing off for hypotension, hypokalemia, or worsening renal function. Systolic BP guided how aggressively vasodilation and ACE inhibitor/angiotensin receptor blocker therapy were escalated.
In the end, 382 patients randomized to the intervention arm received early, intensive, and sustained vasodilation, and the 399 patients in the control arm received standard-of-care treatment according to ESC guidelines. These figures omit two patients in the standard-of-care arm who withdrew consent, but follow-up was otherwise complete, said Dr. Mueller. Physicians treating patients in both study arms had discretion to use such other therapies as loop diuretics, beta-blockers, aldosterone antagonists, and cardiac devices.
Adult patients coming to the ED with acute dyspnea classified as New York Heart Association class III or IV were eligible if they had brain natriuretic peptide (BNP) levels of at least 500 ng/L, or N-terminal of the prohormone BNP (NT-proBNP) levels of at least 2,000 ng/L.
Overall, patients enrolled in GALACTIC were in their late 70s, and women made up 37% of the population.
The actual median BNP for enrollees was about 1,250 ng/L, and the median NT-proBNP was just under 6,000 ng/L. The median left ventricular ejection fraction was 37%. About a third of patients had diabetes, and 85% had hypertension. Over half had known chronic heart failure, about a third had prior history of MI, and half of patients had atrial fibrillation at baseline.
“Signs of congestion were present in all patients, and over 90% had rales on physical examination,” said Dr. Mueller.
Patients who were destined for the ICU, those who had systolic BP below 100 mm Hg or marked creatinine elevation, or who required cardiopulmonary resuscitation were excluded. Also excluded were patients with known structural defects such as severe valvular stenosis, congenital heart disease, or hypertrophic obstructive cardiomyopathy. GALACTIC also excluded patients with isolated right ventricular failure caused by pulmonary hypertension.
Prespecified subgroup analyses compared women with men, and those younger than 75 years with older participants. Women saw a significantly higher hazard ratio for readmission or death, indicating a potential harm from the intervention, said Dr. Mueller. An additional analysis stratified patients by left ventricular ejection fraction. Aside from the intervention’s negative effect on women participating in the trial, no other subgroups benefited or were harmed by an early vasodilation strategy.
Alexandre Mebazaa, MD, the designated discussant for the presentation, said that, although the GALACTIC trial was neutral, it represents “an important step forward in acute heart failure.
“Congratulations: First, because we know that in the critically ill condition it’s very difficult to do trials,” and the GALACTIC investigators succeeded in enrolling patients within the first 5 hours of presentation to EDs, noted Dr. Mebazaa, professor of anesthesiology and critical care medicine at the Paris Diderot School of Medicine.
He added that GALACTIC succeeded in continuing vasodilator use beyond the 48-hour mark. “For the first time, you had the courage to go a little bit further down, and we see that patients got the drug with vasodilator properties for 2 days or more.”
However, the long recruitment period for GALACTIC – first enrollment began in 2007 – meant that the study design reflected a thought process about AHF that doesn’t necessarily reflect current practice, noted Dr. Mebazaa. “The trial was designed many years ago, and at that time, we were still thinking that giving very aggressive treatment in the first hours could have an impact.
“Now, when we will be treating patients with vasodilators with acute heart failure – at least myself and my group – I would really wonder whether there is still evidence in the world to support the use of those agents.”
Dr. Mueller noted limitations of the GALACTIC trial, including the lack of generalizability to patients with systolic hypotension or severe renal dysfunction, since these populations were excluded. Also, “the open-label design, which was mandated by the aim to test a strategy, not a single drug, may have introduced a bias in the unblinded assessment of dyspnea” during inpatient stay.
The study was funded by several Swiss research institutions and had no industry support. Dr. Mueller reported no relevant conflicts of interest. Dr. Mebazaa reported financial relationships with Roche, Service, Novartis, AstraZeneca, S-Form Pharma, 4Teen$4, Adrenomed, and Sphingotec.
SOURCE: Mueller C. ESC 2019, Hot Line Session 3.
PARIS – A practical strategy of early and aggressive vasodilation and optimization of long-term medication for acute heart failure did not budge all-cause mortality or 180-day readmission rates, according to results of a pragmatic trial presented at the annual congress of the European Society of Cardiology.
“To our great disappointment, the curves were superimposable” between intervention and control arms in the GALACTIC (Goal-directed Afterload Reduction in Acute Congestive Cardiac Decompensation) trial, said lead investigator Christian Eugen Mueller, MD. “There was no signal of a benefit” for those receiving the targeted intervention: the adjusted hazard ratio was 1.07 for the composite primary endpoint of all-cause mortality or 6-month readmission for acute heart failure (P = 0.59).
GALACTIC, explained Dr. Mueller, was the largest investigator-initiated, randomized, controlled trial of pharmacologic therapy for acute heart failure (AHF).
“It is different in that it did not investigate a single drug, but a strategy of early, intensive, and sustained vasodilation. It is also unique in that it used individual doses of well-characterized, widely available, and mostly inexpensive drugs,” said Dr. Mueller, director of the Cardiovascular Research Institute at the University Hospital, Basel, Switzerland. “So this would have the beauty that, if it has a positive finding, you – in whatever country you come from – would be immediately able to apply it once you’re back home in your institution.”
The study attempted to address the gap between symptom amelioration and long-term outcomes when patients arrive in the ED with AHF. “Despite symptomatic improvement achieved from loop diuretics, mortality and morbidity remain unacceptably high,” said Dr. Mueller, with 40%-50% of AHF patients experiencing rehospitalization or death within 180 days of discharge.
Much remains unknown about the optimal treatment strategy for AHF. Aggressive vasodilation has been shown to improve outcomes in less-severe AHF, and intravenous nitrates are known to improve outcomes in AHF where severe pulmonary edema is present – “a phenotype representing only about 5% of patients,” noted Dr. Mueller. Still, “it is unknown whether aggressive vasodilation also improves outcomes in the much more common less-severe phenotype.”
Also, previous trials that ran intravenous vasodilators at a fixed dose for 48 hours did not improve AHF outcomes, so a one-size-fits-all strategy was not one the GALACTIC investigators sought to pursue.
In addition to a flexible regimen, “any strategy applied needs to take into consideration that the vast majority of patients with acute heart failure, after initial treatment in the ED, are then treated in a general cardiology ward,” added Dr. Mueller.
This meant that intravenous nitrate infusion was not part of the GALACTIC trial; rather, sublingual and transdermal nitrates were used, explained Dr. Mueller. “Transdermal application has the beauty that if you have an adverse effect – and hypotension is the most dangerous one – you can immediately remove the patch, and thereby avoid any further harm.”
The two-part strategy tested in GALACTIC involved reducing cardiac filling pressures by maintaining or increasing organ perfusion, while also increasing “long-term lifesaving therapy” targeting the renin-angiotensin-aldosterone system during hospitalization, with a goal to continue optimal treatment long term.
ACE inhibitors or angiotensin receptor blockers were added on the second day of hospitalization for the intervention group, said Dr. Mueller, and “in the ideal setting, up-titrated very aggressively from day to day.
“However, as you know, up-titration to target dose is sometimes wishful thinking in this frail population,” he said, so the GALACTIC trial protocol included a scheme to back dosing off for hypotension, hypokalemia, or worsening renal function. Systolic BP guided how aggressively vasodilation and ACE inhibitor/angiotensin receptor blocker therapy were escalated.
In the end, 382 patients randomized to the intervention arm received early, intensive, and sustained vasodilation, and the 399 patients in the control arm received standard-of-care treatment according to ESC guidelines. These figures omit two patients in the standard-of-care arm who withdrew consent, but follow-up was otherwise complete, said Dr. Mueller. Physicians treating patients in both study arms had discretion to use such other therapies as loop diuretics, beta-blockers, aldosterone antagonists, and cardiac devices.
Adult patients coming to the ED with acute dyspnea classified as New York Heart Association class III or IV were eligible if they had brain natriuretic peptide (BNP) levels of at least 500 ng/L, or N-terminal of the prohormone BNP (NT-proBNP) levels of at least 2,000 ng/L.
Overall, patients enrolled in GALACTIC were in their late 70s, and women made up 37% of the population.
The actual median BNP for enrollees was about 1,250 ng/L, and the median NT-proBNP was just under 6,000 ng/L. The median left ventricular ejection fraction was 37%. About a third of patients had diabetes, and 85% had hypertension. Over half had known chronic heart failure, about a third had prior history of MI, and half of patients had atrial fibrillation at baseline.
“Signs of congestion were present in all patients, and over 90% had rales on physical examination,” said Dr. Mueller.
Patients who were destined for the ICU, those who had systolic BP below 100 mm Hg or marked creatinine elevation, or who required cardiopulmonary resuscitation were excluded. Also excluded were patients with known structural defects such as severe valvular stenosis, congenital heart disease, or hypertrophic obstructive cardiomyopathy. GALACTIC also excluded patients with isolated right ventricular failure caused by pulmonary hypertension.
Prespecified subgroup analyses compared women with men, and those younger than 75 years with older participants. Women saw a significantly higher hazard ratio for readmission or death, indicating a potential harm from the intervention, said Dr. Mueller. An additional analysis stratified patients by left ventricular ejection fraction. Aside from the intervention’s negative effect on women participating in the trial, no other subgroups benefited or were harmed by an early vasodilation strategy.
Alexandre Mebazaa, MD, the designated discussant for the presentation, said that, although the GALACTIC trial was neutral, it represents “an important step forward in acute heart failure.
“Congratulations: First, because we know that in the critically ill condition it’s very difficult to do trials,” and the GALACTIC investigators succeeded in enrolling patients within the first 5 hours of presentation to EDs, noted Dr. Mebazaa, professor of anesthesiology and critical care medicine at the Paris Diderot School of Medicine.
He added that GALACTIC succeeded in continuing vasodilator use beyond the 48-hour mark. “For the first time, you had the courage to go a little bit further down, and we see that patients got the drug with vasodilator properties for 2 days or more.”
However, the long recruitment period for GALACTIC – first enrollment began in 2007 – meant that the study design reflected a thought process about AHF that doesn’t necessarily reflect current practice, noted Dr. Mebazaa. “The trial was designed many years ago, and at that time, we were still thinking that giving very aggressive treatment in the first hours could have an impact.
“Now, when we will be treating patients with vasodilators with acute heart failure – at least myself and my group – I would really wonder whether there is still evidence in the world to support the use of those agents.”
Dr. Mueller noted limitations of the GALACTIC trial, including the lack of generalizability to patients with systolic hypotension or severe renal dysfunction, since these populations were excluded. Also, “the open-label design, which was mandated by the aim to test a strategy, not a single drug, may have introduced a bias in the unblinded assessment of dyspnea” during inpatient stay.
The study was funded by several Swiss research institutions and had no industry support. Dr. Mueller reported no relevant conflicts of interest. Dr. Mebazaa reported financial relationships with Roche, Service, Novartis, AstraZeneca, S-Form Pharma, 4Teen$4, Adrenomed, and Sphingotec.
SOURCE: Mueller C. ESC 2019, Hot Line Session 3.
PARIS – A practical strategy of early and aggressive vasodilation and optimization of long-term medication for acute heart failure did not budge all-cause mortality or 180-day readmission rates, according to results of a pragmatic trial presented at the annual congress of the European Society of Cardiology.
“To our great disappointment, the curves were superimposable” between intervention and control arms in the GALACTIC (Goal-directed Afterload Reduction in Acute Congestive Cardiac Decompensation) trial, said lead investigator Christian Eugen Mueller, MD. “There was no signal of a benefit” for those receiving the targeted intervention: the adjusted hazard ratio was 1.07 for the composite primary endpoint of all-cause mortality or 6-month readmission for acute heart failure (P = 0.59).
GALACTIC, explained Dr. Mueller, was the largest investigator-initiated, randomized, controlled trial of pharmacologic therapy for acute heart failure (AHF).
“It is different in that it did not investigate a single drug, but a strategy of early, intensive, and sustained vasodilation. It is also unique in that it used individual doses of well-characterized, widely available, and mostly inexpensive drugs,” said Dr. Mueller, director of the Cardiovascular Research Institute at the University Hospital, Basel, Switzerland. “So this would have the beauty that, if it has a positive finding, you – in whatever country you come from – would be immediately able to apply it once you’re back home in your institution.”
The study attempted to address the gap between symptom amelioration and long-term outcomes when patients arrive in the ED with AHF. “Despite symptomatic improvement achieved from loop diuretics, mortality and morbidity remain unacceptably high,” said Dr. Mueller, with 40%-50% of AHF patients experiencing rehospitalization or death within 180 days of discharge.
Much remains unknown about the optimal treatment strategy for AHF. Aggressive vasodilation has been shown to improve outcomes in less-severe AHF, and intravenous nitrates are known to improve outcomes in AHF where severe pulmonary edema is present – “a phenotype representing only about 5% of patients,” noted Dr. Mueller. Still, “it is unknown whether aggressive vasodilation also improves outcomes in the much more common less-severe phenotype.”
Also, previous trials that ran intravenous vasodilators at a fixed dose for 48 hours did not improve AHF outcomes, so a one-size-fits-all strategy was not one the GALACTIC investigators sought to pursue.
In addition to a flexible regimen, “any strategy applied needs to take into consideration that the vast majority of patients with acute heart failure, after initial treatment in the ED, are then treated in a general cardiology ward,” added Dr. Mueller.
This meant that intravenous nitrate infusion was not part of the GALACTIC trial; rather, sublingual and transdermal nitrates were used, explained Dr. Mueller. “Transdermal application has the beauty that if you have an adverse effect – and hypotension is the most dangerous one – you can immediately remove the patch, and thereby avoid any further harm.”
The two-part strategy tested in GALACTIC involved reducing cardiac filling pressures by maintaining or increasing organ perfusion, while also increasing “long-term lifesaving therapy” targeting the renin-angiotensin-aldosterone system during hospitalization, with a goal to continue optimal treatment long term.
ACE inhibitors or angiotensin receptor blockers were added on the second day of hospitalization for the intervention group, said Dr. Mueller, and “in the ideal setting, up-titrated very aggressively from day to day.
“However, as you know, up-titration to target dose is sometimes wishful thinking in this frail population,” he said, so the GALACTIC trial protocol included a scheme to back dosing off for hypotension, hypokalemia, or worsening renal function. Systolic BP guided how aggressively vasodilation and ACE inhibitor/angiotensin receptor blocker therapy were escalated.
In the end, 382 patients randomized to the intervention arm received early, intensive, and sustained vasodilation, and the 399 patients in the control arm received standard-of-care treatment according to ESC guidelines. These figures omit two patients in the standard-of-care arm who withdrew consent, but follow-up was otherwise complete, said Dr. Mueller. Physicians treating patients in both study arms had discretion to use such other therapies as loop diuretics, beta-blockers, aldosterone antagonists, and cardiac devices.
Adult patients coming to the ED with acute dyspnea classified as New York Heart Association class III or IV were eligible if they had brain natriuretic peptide (BNP) levels of at least 500 ng/L, or N-terminal of the prohormone BNP (NT-proBNP) levels of at least 2,000 ng/L.
Overall, patients enrolled in GALACTIC were in their late 70s, and women made up 37% of the population.
The actual median BNP for enrollees was about 1,250 ng/L, and the median NT-proBNP was just under 6,000 ng/L. The median left ventricular ejection fraction was 37%. About a third of patients had diabetes, and 85% had hypertension. Over half had known chronic heart failure, about a third had prior history of MI, and half of patients had atrial fibrillation at baseline.
“Signs of congestion were present in all patients, and over 90% had rales on physical examination,” said Dr. Mueller.
Patients who were destined for the ICU, those who had systolic BP below 100 mm Hg or marked creatinine elevation, or who required cardiopulmonary resuscitation were excluded. Also excluded were patients with known structural defects such as severe valvular stenosis, congenital heart disease, or hypertrophic obstructive cardiomyopathy. GALACTIC also excluded patients with isolated right ventricular failure caused by pulmonary hypertension.
Prespecified subgroup analyses compared women with men, and those younger than 75 years with older participants. Women saw a significantly higher hazard ratio for readmission or death, indicating a potential harm from the intervention, said Dr. Mueller. An additional analysis stratified patients by left ventricular ejection fraction. Aside from the intervention’s negative effect on women participating in the trial, no other subgroups benefited or were harmed by an early vasodilation strategy.
Alexandre Mebazaa, MD, the designated discussant for the presentation, said that, although the GALACTIC trial was neutral, it represents “an important step forward in acute heart failure.
“Congratulations: First, because we know that in the critically ill condition it’s very difficult to do trials,” and the GALACTIC investigators succeeded in enrolling patients within the first 5 hours of presentation to EDs, noted Dr. Mebazaa, professor of anesthesiology and critical care medicine at the Paris Diderot School of Medicine.
He added that GALACTIC succeeded in continuing vasodilator use beyond the 48-hour mark. “For the first time, you had the courage to go a little bit further down, and we see that patients got the drug with vasodilator properties for 2 days or more.”
However, the long recruitment period for GALACTIC – first enrollment began in 2007 – meant that the study design reflected a thought process about AHF that doesn’t necessarily reflect current practice, noted Dr. Mebazaa. “The trial was designed many years ago, and at that time, we were still thinking that giving very aggressive treatment in the first hours could have an impact.
“Now, when we will be treating patients with vasodilators with acute heart failure – at least myself and my group – I would really wonder whether there is still evidence in the world to support the use of those agents.”
Dr. Mueller noted limitations of the GALACTIC trial, including the lack of generalizability to patients with systolic hypotension or severe renal dysfunction, since these populations were excluded. Also, “the open-label design, which was mandated by the aim to test a strategy, not a single drug, may have introduced a bias in the unblinded assessment of dyspnea” during inpatient stay.
The study was funded by several Swiss research institutions and had no industry support. Dr. Mueller reported no relevant conflicts of interest. Dr. Mebazaa reported financial relationships with Roche, Service, Novartis, AstraZeneca, S-Form Pharma, 4Teen$4, Adrenomed, and Sphingotec.
SOURCE: Mueller C. ESC 2019, Hot Line Session 3.
REPORTING FROM THE ESC CONGRESS 2019
Bringing focus to the issue: Dr. Elizabeth Loder on gender in medicine
The recently published “Eleven Things Not to Say to Your Female Colleagues,” has sparked debate on medical Twitter. Senior author Elizabeth Loder, MD, developed the content collaboratively with members of the Migraine Mavens, a private Facebook group of North American headache practitioners and researchers.
In an interview, Dr. Loder, chief of the headache division in the neurology department at Brigham and Women’s Hospital, Boston, and professor of neurology at Harvard Medical School, Boston, shared the background and context for the article.
Q: Could you explain the impetus for putting this together? How did you arrive at the chart that is the center of the article?
A: In June, I gave the Seymour Solomon lecture at the American Headache Society annual scientific meeting. Because it was an award lecture, I was able to choose the topic. I decided to talk about gender-based problems faced by women in medicine, with a focus on the headache field.
These problems include sexual harassment, hurtful sex-based comments, gender-based barriers to career advancement, as well as the difficulties women face in getting institutions or professional societies to pay attention to these problems.
I wanted to provide real, recent examples of troubling behavior or comments, so I appealed to the Migraine Mavens group to describe their own experiences. I was not expecting the response I got. Not only did people post many examples of such behavior in the group, but I also received many private messages describing things that were so hurtful or private that the woman involved did not even feel comfortable posting them in our group.
I ended up with plenty of real-life vignettes. The title of my talk was “Time’s Up: Headache Medicine in the #MeToo Era.” Shortly after the talk, a member of the group posted this:
“Oh, Dr. Elizabeth Loder, how timely was your talk yesterday, and we have so much further to progress. ...
“Just now, I had this experience: I have been recently selected for a leadership position within AHS and I was talking to one of our male colleagues about it. ... He expressed his doubt in my ability to serve this role well.
“I thought it was because I am early in my career, and as I was reassuring him that I would reach out to him and others for mentorship, he then said ‘AND you have two small children. ... You don’t have time for this.’ ”
There was lively discussion in the group about how this poster could have responded and what bystanders could have said. One of the group members, Clarimar Borrero-Mejias, MD, a pediatric neurologist at Phoenix Children’s Hospital, pointed out that many men and women might benefit from knowing what kinds of things not to say to other colleagues. I suggested that we should take some of the problems we had discussed and write a paper, and that she should be the first author. We then crowdsourced the scenarios to be included.
The grid format came immediately to mind because I know that tables and charts and boxes are good ways to organize and present information. We also wanted to keep the article short and accessible, and thus the idea of “Ten Things” was born. At the end of our work, though, someone posted the vignette about the salary discussion. It was amazing to me how many women, even in this day and age, are still told that men deserve more money because of their family or other responsibilities. We thus decided that it had to be 11, not 10, things.
The article was possible only because of the supportive reaction of the editor of Headache, Thomas Ward, MD. He not only published the piece rapidly, but also agreed to make it free so that anyone who wanted to could access the entire article without hitting a paywall (Headache. 2019 Sep 26. doi: 10.1111/head.13647).
Q: Could you share some of the reactions you’ve gotten? I did see that Esther Choo, MD – an emergency medicine physician and prominent proponent for gender equity in medicine – highlighted the article on Twitter; are there other highlights, or surprising reactions, or pushback, that you’d like to share?
A: We were thrilled to be the subject of a “tweetorial” by Dr. Choo. It’s impossible to overestimate the boost this gave to the paper. She has over 75,000 Twitter followers, and it was quite impressive to watch the exponential increase in the article’s Altmetrics score after her tweetorial. This brought the article to the attention of people outside our own subspecialty. The experiences we described seem to be familiar to women doctors in every specialty and subspecialty, and also relevant outside medicine. I saw tweets from women lawyers, engineers, and others, many of whom said this sort of behavior is a problem in their own fields.
It’s probably not surprising that the vast majority of reactions came from women. A number of men tweeted the article, though, and recommended it to other men. This sort of #HeForShe support is gratifying. We did get some negative reactions, but there are Migraine Mavens on Twitter and we’ve taken them on.
Q: You offer suggestions for reframing many behaviors that reflect implicit bias. You also offer suggestions for bystanders to challenge these biases and support women who are on the receiving end of the behaviors you call out. Do you think exhibiting more of this kind of solidarity can help change the culture of medicine?
A: I believe many people who witness the behaviors are uncomfortable and would like to help but just don’t know what to say. Often, they are caught off guard. Some of our suggested responses are all-purpose lines that can be effective simply by calling attention to the behavior, for example, “What did you just say?” or “Why would you say something like that?” As Dr. Choo said, “Learn them, say them often.”
It’s critical to remember that problems like this are not in the past. This article gave real examples of things that have happened to real women recently. The sheer number of women who retweeted the article with statements such as, “How many of these have been said to you? Straw poll. I got 9,” demonstrates that behavior like this is common.
I recently received an email that forwarded a message written by a medical assistant. I’ve changed the names, but it otherwise read “Dr. Smith wants this patient to have a nerve block. ... You can schedule them with Abigail or Nancy.” Guess what? Abigail and Nancy are doctors. Not only that, they are Dr. Smith’s true peers in every way imaginable, having been hired at exactly the same time and having exactly the same titles and duties. There seems to be only one reason they are not addressed as doctor while their male colleague is, and that is their gender. So the struggle highlighted by #MyFirstNameIsDoctor is real. Women doctors live it every day.
The recently published “Eleven Things Not to Say to Your Female Colleagues,” has sparked debate on medical Twitter. Senior author Elizabeth Loder, MD, developed the content collaboratively with members of the Migraine Mavens, a private Facebook group of North American headache practitioners and researchers.
In an interview, Dr. Loder, chief of the headache division in the neurology department at Brigham and Women’s Hospital, Boston, and professor of neurology at Harvard Medical School, Boston, shared the background and context for the article.
Q: Could you explain the impetus for putting this together? How did you arrive at the chart that is the center of the article?
A: In June, I gave the Seymour Solomon lecture at the American Headache Society annual scientific meeting. Because it was an award lecture, I was able to choose the topic. I decided to talk about gender-based problems faced by women in medicine, with a focus on the headache field.
These problems include sexual harassment, hurtful sex-based comments, gender-based barriers to career advancement, as well as the difficulties women face in getting institutions or professional societies to pay attention to these problems.
I wanted to provide real, recent examples of troubling behavior or comments, so I appealed to the Migraine Mavens group to describe their own experiences. I was not expecting the response I got. Not only did people post many examples of such behavior in the group, but I also received many private messages describing things that were so hurtful or private that the woman involved did not even feel comfortable posting them in our group.
I ended up with plenty of real-life vignettes. The title of my talk was “Time’s Up: Headache Medicine in the #MeToo Era.” Shortly after the talk, a member of the group posted this:
“Oh, Dr. Elizabeth Loder, how timely was your talk yesterday, and we have so much further to progress. ...
“Just now, I had this experience: I have been recently selected for a leadership position within AHS and I was talking to one of our male colleagues about it. ... He expressed his doubt in my ability to serve this role well.
“I thought it was because I am early in my career, and as I was reassuring him that I would reach out to him and others for mentorship, he then said ‘AND you have two small children. ... You don’t have time for this.’ ”
There was lively discussion in the group about how this poster could have responded and what bystanders could have said. One of the group members, Clarimar Borrero-Mejias, MD, a pediatric neurologist at Phoenix Children’s Hospital, pointed out that many men and women might benefit from knowing what kinds of things not to say to other colleagues. I suggested that we should take some of the problems we had discussed and write a paper, and that she should be the first author. We then crowdsourced the scenarios to be included.
The grid format came immediately to mind because I know that tables and charts and boxes are good ways to organize and present information. We also wanted to keep the article short and accessible, and thus the idea of “Ten Things” was born. At the end of our work, though, someone posted the vignette about the salary discussion. It was amazing to me how many women, even in this day and age, are still told that men deserve more money because of their family or other responsibilities. We thus decided that it had to be 11, not 10, things.
The article was possible only because of the supportive reaction of the editor of Headache, Thomas Ward, MD. He not only published the piece rapidly, but also agreed to make it free so that anyone who wanted to could access the entire article without hitting a paywall (Headache. 2019 Sep 26. doi: 10.1111/head.13647).
Q: Could you share some of the reactions you’ve gotten? I did see that Esther Choo, MD – an emergency medicine physician and prominent proponent for gender equity in medicine – highlighted the article on Twitter; are there other highlights, or surprising reactions, or pushback, that you’d like to share?
A: We were thrilled to be the subject of a “tweetorial” by Dr. Choo. It’s impossible to overestimate the boost this gave to the paper. She has over 75,000 Twitter followers, and it was quite impressive to watch the exponential increase in the article’s Altmetrics score after her tweetorial. This brought the article to the attention of people outside our own subspecialty. The experiences we described seem to be familiar to women doctors in every specialty and subspecialty, and also relevant outside medicine. I saw tweets from women lawyers, engineers, and others, many of whom said this sort of behavior is a problem in their own fields.
It’s probably not surprising that the vast majority of reactions came from women. A number of men tweeted the article, though, and recommended it to other men. This sort of #HeForShe support is gratifying. We did get some negative reactions, but there are Migraine Mavens on Twitter and we’ve taken them on.
Q: You offer suggestions for reframing many behaviors that reflect implicit bias. You also offer suggestions for bystanders to challenge these biases and support women who are on the receiving end of the behaviors you call out. Do you think exhibiting more of this kind of solidarity can help change the culture of medicine?
A: I believe many people who witness the behaviors are uncomfortable and would like to help but just don’t know what to say. Often, they are caught off guard. Some of our suggested responses are all-purpose lines that can be effective simply by calling attention to the behavior, for example, “What did you just say?” or “Why would you say something like that?” As Dr. Choo said, “Learn them, say them often.”
It’s critical to remember that problems like this are not in the past. This article gave real examples of things that have happened to real women recently. The sheer number of women who retweeted the article with statements such as, “How many of these have been said to you? Straw poll. I got 9,” demonstrates that behavior like this is common.
I recently received an email that forwarded a message written by a medical assistant. I’ve changed the names, but it otherwise read “Dr. Smith wants this patient to have a nerve block. ... You can schedule them with Abigail or Nancy.” Guess what? Abigail and Nancy are doctors. Not only that, they are Dr. Smith’s true peers in every way imaginable, having been hired at exactly the same time and having exactly the same titles and duties. There seems to be only one reason they are not addressed as doctor while their male colleague is, and that is their gender. So the struggle highlighted by #MyFirstNameIsDoctor is real. Women doctors live it every day.
The recently published “Eleven Things Not to Say to Your Female Colleagues,” has sparked debate on medical Twitter. Senior author Elizabeth Loder, MD, developed the content collaboratively with members of the Migraine Mavens, a private Facebook group of North American headache practitioners and researchers.
In an interview, Dr. Loder, chief of the headache division in the neurology department at Brigham and Women’s Hospital, Boston, and professor of neurology at Harvard Medical School, Boston, shared the background and context for the article.
Q: Could you explain the impetus for putting this together? How did you arrive at the chart that is the center of the article?
A: In June, I gave the Seymour Solomon lecture at the American Headache Society annual scientific meeting. Because it was an award lecture, I was able to choose the topic. I decided to talk about gender-based problems faced by women in medicine, with a focus on the headache field.
These problems include sexual harassment, hurtful sex-based comments, gender-based barriers to career advancement, as well as the difficulties women face in getting institutions or professional societies to pay attention to these problems.
I wanted to provide real, recent examples of troubling behavior or comments, so I appealed to the Migraine Mavens group to describe their own experiences. I was not expecting the response I got. Not only did people post many examples of such behavior in the group, but I also received many private messages describing things that were so hurtful or private that the woman involved did not even feel comfortable posting them in our group.
I ended up with plenty of real-life vignettes. The title of my talk was “Time’s Up: Headache Medicine in the #MeToo Era.” Shortly after the talk, a member of the group posted this:
“Oh, Dr. Elizabeth Loder, how timely was your talk yesterday, and we have so much further to progress. ...
“Just now, I had this experience: I have been recently selected for a leadership position within AHS and I was talking to one of our male colleagues about it. ... He expressed his doubt in my ability to serve this role well.
“I thought it was because I am early in my career, and as I was reassuring him that I would reach out to him and others for mentorship, he then said ‘AND you have two small children. ... You don’t have time for this.’ ”
There was lively discussion in the group about how this poster could have responded and what bystanders could have said. One of the group members, Clarimar Borrero-Mejias, MD, a pediatric neurologist at Phoenix Children’s Hospital, pointed out that many men and women might benefit from knowing what kinds of things not to say to other colleagues. I suggested that we should take some of the problems we had discussed and write a paper, and that she should be the first author. We then crowdsourced the scenarios to be included.
The grid format came immediately to mind because I know that tables and charts and boxes are good ways to organize and present information. We also wanted to keep the article short and accessible, and thus the idea of “Ten Things” was born. At the end of our work, though, someone posted the vignette about the salary discussion. It was amazing to me how many women, even in this day and age, are still told that men deserve more money because of their family or other responsibilities. We thus decided that it had to be 11, not 10, things.
The article was possible only because of the supportive reaction of the editor of Headache, Thomas Ward, MD. He not only published the piece rapidly, but also agreed to make it free so that anyone who wanted to could access the entire article without hitting a paywall (Headache. 2019 Sep 26. doi: 10.1111/head.13647).
Q: Could you share some of the reactions you’ve gotten? I did see that Esther Choo, MD – an emergency medicine physician and prominent proponent for gender equity in medicine – highlighted the article on Twitter; are there other highlights, or surprising reactions, or pushback, that you’d like to share?
A: We were thrilled to be the subject of a “tweetorial” by Dr. Choo. It’s impossible to overestimate the boost this gave to the paper. She has over 75,000 Twitter followers, and it was quite impressive to watch the exponential increase in the article’s Altmetrics score after her tweetorial. This brought the article to the attention of people outside our own subspecialty. The experiences we described seem to be familiar to women doctors in every specialty and subspecialty, and also relevant outside medicine. I saw tweets from women lawyers, engineers, and others, many of whom said this sort of behavior is a problem in their own fields.
It’s probably not surprising that the vast majority of reactions came from women. A number of men tweeted the article, though, and recommended it to other men. This sort of #HeForShe support is gratifying. We did get some negative reactions, but there are Migraine Mavens on Twitter and we’ve taken them on.
Q: You offer suggestions for reframing many behaviors that reflect implicit bias. You also offer suggestions for bystanders to challenge these biases and support women who are on the receiving end of the behaviors you call out. Do you think exhibiting more of this kind of solidarity can help change the culture of medicine?
A: I believe many people who witness the behaviors are uncomfortable and would like to help but just don’t know what to say. Often, they are caught off guard. Some of our suggested responses are all-purpose lines that can be effective simply by calling attention to the behavior, for example, “What did you just say?” or “Why would you say something like that?” As Dr. Choo said, “Learn them, say them often.”
It’s critical to remember that problems like this are not in the past. This article gave real examples of things that have happened to real women recently. The sheer number of women who retweeted the article with statements such as, “How many of these have been said to you? Straw poll. I got 9,” demonstrates that behavior like this is common.
I recently received an email that forwarded a message written by a medical assistant. I’ve changed the names, but it otherwise read “Dr. Smith wants this patient to have a nerve block. ... You can schedule them with Abigail or Nancy.” Guess what? Abigail and Nancy are doctors. Not only that, they are Dr. Smith’s true peers in every way imaginable, having been hired at exactly the same time and having exactly the same titles and duties. There seems to be only one reason they are not addressed as doctor while their male colleague is, and that is their gender. So the struggle highlighted by #MyFirstNameIsDoctor is real. Women doctors live it every day.
#MyFirstNameIsDoctor: Why it matters, and what you can do
When Shawnté James, MD, picked up the phone at work recently, a male physician on the other end was calling for a peer-to-peer review of a patient’s insurance issue.
“Hi, this is Dr. Y, calling to speak with Shawnté about patient X. Is she available?” asked the physician. “No,” replied Dr. James, an assistant professor of pediatrics at MedStar Georgetown University Hospital, Washington.
She related the rest of the interaction in a recent tweet:
“I’m Dr. XY calling a peer-to-peer review of a denial. Is Shawnté available?”
— Shawnté James (@ShawnteJamesMD) October 10, 2019
Me: “No.”
Him: “Is she in today?”
Me: “There’s no Shawnté here.”
Him: “Oh this is the number I have for Dr. Shawnté James”
Me: “Oh, DR. JAMES. Yes, that’s me. How can I help?”#MyFirstNameIsDoctor
The tweet, along with many others that used the hashtag #MyFirstNameIsDoctor, struck a chord among female physicians on Twitter. In tweets of their own, they related instance after instance of peers, coworkers, and patients assuming first-name familiarity with them – but not their male colleagues.
“This time it’s a peer-to-peer review. Last time it was being introduced to new hospital leadership as, ‘Shawnté, one of our pediatricians,’ ” Dr. James said in an interview. “The truth is, for physician women – particularly women of color – this is a regular occurrence.”
Data show an ongoing problem
Objective evidence that female physicians and scientists are significantly less likely than their male peers to be addressed by their titles came in a just-published study of presentations at the annual meeting of the American Society for Clinical Oncology in 2017 and 2018.
Narjust Duma, MD, the study’s first author, described her growing awareness of the problem.
Dr. Duma recalled a session on the last day of the ASCO 2018 meeting. Five presenters were speaking – four men and a woman. “The woman is the one who knows the most about this subject. She’s the only one at the table who’s a full professor,” Dr. Duma, assistant professor of hematology/oncology at the University of Wisconsin–Madison, said in an interview. “And then everybody is introduced as ‘Dr. So-and-so,’ and when they come to her, they introduce her as ‘Julie.’ ”
“Is it just me?” Dr. Duma asked herself. The same day, she began a Twitter poll to ask whether her female peers were experiencing this phenomenon, and got an “overwhelming” response.
“We need data to learn the extent of the problem,” she said she realized.
The ASCO annual meeting afforded an ideal opportunity for data gathering, said Dr. Duma, because presentations are recorded and written transcripts generated. Dr. Duma assembled a research team that had a 50-50 gender balance and racial and ethnic diversity. The team combed ASCO transcripts to code introductions according to whether title and surname were used or whether speakers were addressed by first name only.
After excluding videos that did not capture speaker introductions, Dr. Duma and collaborators were left with 781 videos to watch and code.
Female speakers overall were less likely to be addressed by their professional title (62% vs. 81% for males, P less than .001). Male introducers used professional titles 53% of the time when introducing female speakers, and 80% of the time when introducing male speakers (P less than .01). No gender differences were seen when females were the introducers (J Clin Oncol. 2019 Oct 11. doi: 10.1200/JCO.19.01608).
Looking further, male introducers addressed female speakers by first name only in 24% of the cases. Female introducers used first names only with female speakers 7% of the time, a statistically significant difference. “This is the part that is really sad,” said Dr. Duma.
She and her coauthors also performed multivariable analysis to adjust for factors such as seniority and geographic location; after adjustment, males were still over 2.5 times as likely as females to be introduced with their professional title, and females were nearly six times as likely as males to be introduced by their first names only. When the introducer was male, a female speaker was over three times more likely to be introduced by her first name only.
Dr. Duma and colleagues are working with the ASCO 2020 planning team to develop a template that standardizes presenter introductions. They’re also planning for prospective data collection at that meeting, and will include self-reported race and ethnicity data for presenters and introducers who choose to provide it.
“We do not plan to create a ‘her versus him’ battle,” said Dr. Duma. “The goal is to use this hardcore data to bring attention to the problem.” She pointed out that, though fewer females introduced other females by first name only, the problem wasn’t limited only to male introducers at ASCO.
“The problem is unconscious bias. Nobody’s exempt,” said Dr. Duma. She related that she herself had just sent a work-related email to a female colleague that addressed her by her first name, and had copied many of their mutual colleagues. Realizing her gaffe, she held herself to her own standard by apologizing to her colleague and copying everyone who saw the first email. “The goal is to bring attention to the difference, so we can improve gender bias in medicine together.”
Patient interactions: Sometimes, a delicate balance
What’s the right approach when a patient, uninvited, addresses you by your first name? Natalie Strand, MD, had been thinking about the best way to handle this sticky situation for some time. Recently, she tried it out on a patient and shared her approach in a tweet:
So proud of myself!
— Natalie Strand (@DrNatStrand) October 11, 2019
After introducing myself as Dr. Strand to a patient, he looked at my name badge and said- oh, so Natalie.
Usually I’m stuck feeling afraid to rock the boat...
Not today!
“Yes, but I go by Dr. Strand at work! “
I finally said it!!!
There was an awkward moment with the patient, Dr. Strand acknowledged, “but we moved past it.”
Asserting one’s hard-earned status despite a societally ingrained desire to please or to avoid confrontation can be difficult, she acknowledged, but it’s worth it. Put simply, she said, “I want to be called Dr. Strand.”
The importance of this issue can sometimes be hard for male colleagues to understand, said Dr. Strand, who practices outpatient interventional pain medicine at the Mayo Clinic, Scottsdale, Ariz. “The people that have privilege – they don’t see it as privilege. And that’s not anybody’s fault. That’s just the reality of it, because that’s the norm. … That’s why putting a name to microaggression and microinsults is so powerful, because once you name it, then you can respond to it.”
Beginning from a point of mutual professionalism is a good place to start, Dr. Strand said in an interview. She always begins by addressing her patients by their surname and waits for patients to invite her to call them by their first names. “The most professional approach is the best first step,” she said. When she has a longstanding relationship with patients and she knows that trust and mutual respect have been established, she may also invite first-name familiarity.
“Patients don’t do this to be mean,” emphasized Dr. Strand, adding that, particularly with older patients, “they are trying to be sweet.” That’s part of the difficulty in finding a gentle but firm way to bring the relationship back to a professional footing.
Judging by the responses she’s gotten from other female physicians, this delicate situation, and the best way to ask for professionalism with patients, is a common struggle. Many of her female peers have said they’ll consider adopting her approach, she said.
“Male physicians are our allies,” said Dr. Strand. “The needs of the patients come first. This isn’t about power; it’s not about holding a power differential against the patient. It’s about having a culture of mutual respect, and being seen as a physician. Not as a female physician, not as a male physician. Just being seen as a physician, so you can act as a physician.”
Whether they come from patients or peers, said Dr. James, who adroitly called out the physician reviewer who asked for her by first name, “These microaggressions are uncomfortable to address at the time they occur – but they are teachable moments that we should all take advantage of. Usually, a gentle correction, such as, ‘I prefer to be addressed as Dr. James while at work,’ is sufficient.” However, she added, “sometimes, a firmer ‘I feel disrespected when you address me by my first name to colleagues and patients’ is needed.”
This article was updated 10/15/19.
When Shawnté James, MD, picked up the phone at work recently, a male physician on the other end was calling for a peer-to-peer review of a patient’s insurance issue.
“Hi, this is Dr. Y, calling to speak with Shawnté about patient X. Is she available?” asked the physician. “No,” replied Dr. James, an assistant professor of pediatrics at MedStar Georgetown University Hospital, Washington.
She related the rest of the interaction in a recent tweet:
“I’m Dr. XY calling a peer-to-peer review of a denial. Is Shawnté available?”
— Shawnté James (@ShawnteJamesMD) October 10, 2019
Me: “No.”
Him: “Is she in today?”
Me: “There’s no Shawnté here.”
Him: “Oh this is the number I have for Dr. Shawnté James”
Me: “Oh, DR. JAMES. Yes, that’s me. How can I help?”#MyFirstNameIsDoctor
The tweet, along with many others that used the hashtag #MyFirstNameIsDoctor, struck a chord among female physicians on Twitter. In tweets of their own, they related instance after instance of peers, coworkers, and patients assuming first-name familiarity with them – but not their male colleagues.
“This time it’s a peer-to-peer review. Last time it was being introduced to new hospital leadership as, ‘Shawnté, one of our pediatricians,’ ” Dr. James said in an interview. “The truth is, for physician women – particularly women of color – this is a regular occurrence.”
Data show an ongoing problem
Objective evidence that female physicians and scientists are significantly less likely than their male peers to be addressed by their titles came in a just-published study of presentations at the annual meeting of the American Society for Clinical Oncology in 2017 and 2018.
Narjust Duma, MD, the study’s first author, described her growing awareness of the problem.
Dr. Duma recalled a session on the last day of the ASCO 2018 meeting. Five presenters were speaking – four men and a woman. “The woman is the one who knows the most about this subject. She’s the only one at the table who’s a full professor,” Dr. Duma, assistant professor of hematology/oncology at the University of Wisconsin–Madison, said in an interview. “And then everybody is introduced as ‘Dr. So-and-so,’ and when they come to her, they introduce her as ‘Julie.’ ”
“Is it just me?” Dr. Duma asked herself. The same day, she began a Twitter poll to ask whether her female peers were experiencing this phenomenon, and got an “overwhelming” response.
“We need data to learn the extent of the problem,” she said she realized.
The ASCO annual meeting afforded an ideal opportunity for data gathering, said Dr. Duma, because presentations are recorded and written transcripts generated. Dr. Duma assembled a research team that had a 50-50 gender balance and racial and ethnic diversity. The team combed ASCO transcripts to code introductions according to whether title and surname were used or whether speakers were addressed by first name only.
After excluding videos that did not capture speaker introductions, Dr. Duma and collaborators were left with 781 videos to watch and code.
Female speakers overall were less likely to be addressed by their professional title (62% vs. 81% for males, P less than .001). Male introducers used professional titles 53% of the time when introducing female speakers, and 80% of the time when introducing male speakers (P less than .01). No gender differences were seen when females were the introducers (J Clin Oncol. 2019 Oct 11. doi: 10.1200/JCO.19.01608).
Looking further, male introducers addressed female speakers by first name only in 24% of the cases. Female introducers used first names only with female speakers 7% of the time, a statistically significant difference. “This is the part that is really sad,” said Dr. Duma.
She and her coauthors also performed multivariable analysis to adjust for factors such as seniority and geographic location; after adjustment, males were still over 2.5 times as likely as females to be introduced with their professional title, and females were nearly six times as likely as males to be introduced by their first names only. When the introducer was male, a female speaker was over three times more likely to be introduced by her first name only.
Dr. Duma and colleagues are working with the ASCO 2020 planning team to develop a template that standardizes presenter introductions. They’re also planning for prospective data collection at that meeting, and will include self-reported race and ethnicity data for presenters and introducers who choose to provide it.
“We do not plan to create a ‘her versus him’ battle,” said Dr. Duma. “The goal is to use this hardcore data to bring attention to the problem.” She pointed out that, though fewer females introduced other females by first name only, the problem wasn’t limited only to male introducers at ASCO.
“The problem is unconscious bias. Nobody’s exempt,” said Dr. Duma. She related that she herself had just sent a work-related email to a female colleague that addressed her by her first name, and had copied many of their mutual colleagues. Realizing her gaffe, she held herself to her own standard by apologizing to her colleague and copying everyone who saw the first email. “The goal is to bring attention to the difference, so we can improve gender bias in medicine together.”
Patient interactions: Sometimes, a delicate balance
What’s the right approach when a patient, uninvited, addresses you by your first name? Natalie Strand, MD, had been thinking about the best way to handle this sticky situation for some time. Recently, she tried it out on a patient and shared her approach in a tweet:
So proud of myself!
— Natalie Strand (@DrNatStrand) October 11, 2019
After introducing myself as Dr. Strand to a patient, he looked at my name badge and said- oh, so Natalie.
Usually I’m stuck feeling afraid to rock the boat...
Not today!
“Yes, but I go by Dr. Strand at work! “
I finally said it!!!
There was an awkward moment with the patient, Dr. Strand acknowledged, “but we moved past it.”
Asserting one’s hard-earned status despite a societally ingrained desire to please or to avoid confrontation can be difficult, she acknowledged, but it’s worth it. Put simply, she said, “I want to be called Dr. Strand.”
The importance of this issue can sometimes be hard for male colleagues to understand, said Dr. Strand, who practices outpatient interventional pain medicine at the Mayo Clinic, Scottsdale, Ariz. “The people that have privilege – they don’t see it as privilege. And that’s not anybody’s fault. That’s just the reality of it, because that’s the norm. … That’s why putting a name to microaggression and microinsults is so powerful, because once you name it, then you can respond to it.”
Beginning from a point of mutual professionalism is a good place to start, Dr. Strand said in an interview. She always begins by addressing her patients by their surname and waits for patients to invite her to call them by their first names. “The most professional approach is the best first step,” she said. When she has a longstanding relationship with patients and she knows that trust and mutual respect have been established, she may also invite first-name familiarity.
“Patients don’t do this to be mean,” emphasized Dr. Strand, adding that, particularly with older patients, “they are trying to be sweet.” That’s part of the difficulty in finding a gentle but firm way to bring the relationship back to a professional footing.
Judging by the responses she’s gotten from other female physicians, this delicate situation, and the best way to ask for professionalism with patients, is a common struggle. Many of her female peers have said they’ll consider adopting her approach, she said.
“Male physicians are our allies,” said Dr. Strand. “The needs of the patients come first. This isn’t about power; it’s not about holding a power differential against the patient. It’s about having a culture of mutual respect, and being seen as a physician. Not as a female physician, not as a male physician. Just being seen as a physician, so you can act as a physician.”
Whether they come from patients or peers, said Dr. James, who adroitly called out the physician reviewer who asked for her by first name, “These microaggressions are uncomfortable to address at the time they occur – but they are teachable moments that we should all take advantage of. Usually, a gentle correction, such as, ‘I prefer to be addressed as Dr. James while at work,’ is sufficient.” However, she added, “sometimes, a firmer ‘I feel disrespected when you address me by my first name to colleagues and patients’ is needed.”
This article was updated 10/15/19.
When Shawnté James, MD, picked up the phone at work recently, a male physician on the other end was calling for a peer-to-peer review of a patient’s insurance issue.
“Hi, this is Dr. Y, calling to speak with Shawnté about patient X. Is she available?” asked the physician. “No,” replied Dr. James, an assistant professor of pediatrics at MedStar Georgetown University Hospital, Washington.
She related the rest of the interaction in a recent tweet:
“I’m Dr. XY calling a peer-to-peer review of a denial. Is Shawnté available?”
— Shawnté James (@ShawnteJamesMD) October 10, 2019
Me: “No.”
Him: “Is she in today?”
Me: “There’s no Shawnté here.”
Him: “Oh this is the number I have for Dr. Shawnté James”
Me: “Oh, DR. JAMES. Yes, that’s me. How can I help?”#MyFirstNameIsDoctor
The tweet, along with many others that used the hashtag #MyFirstNameIsDoctor, struck a chord among female physicians on Twitter. In tweets of their own, they related instance after instance of peers, coworkers, and patients assuming first-name familiarity with them – but not their male colleagues.
“This time it’s a peer-to-peer review. Last time it was being introduced to new hospital leadership as, ‘Shawnté, one of our pediatricians,’ ” Dr. James said in an interview. “The truth is, for physician women – particularly women of color – this is a regular occurrence.”
Data show an ongoing problem
Objective evidence that female physicians and scientists are significantly less likely than their male peers to be addressed by their titles came in a just-published study of presentations at the annual meeting of the American Society for Clinical Oncology in 2017 and 2018.
Narjust Duma, MD, the study’s first author, described her growing awareness of the problem.
Dr. Duma recalled a session on the last day of the ASCO 2018 meeting. Five presenters were speaking – four men and a woman. “The woman is the one who knows the most about this subject. She’s the only one at the table who’s a full professor,” Dr. Duma, assistant professor of hematology/oncology at the University of Wisconsin–Madison, said in an interview. “And then everybody is introduced as ‘Dr. So-and-so,’ and when they come to her, they introduce her as ‘Julie.’ ”
“Is it just me?” Dr. Duma asked herself. The same day, she began a Twitter poll to ask whether her female peers were experiencing this phenomenon, and got an “overwhelming” response.
“We need data to learn the extent of the problem,” she said she realized.
The ASCO annual meeting afforded an ideal opportunity for data gathering, said Dr. Duma, because presentations are recorded and written transcripts generated. Dr. Duma assembled a research team that had a 50-50 gender balance and racial and ethnic diversity. The team combed ASCO transcripts to code introductions according to whether title and surname were used or whether speakers were addressed by first name only.
After excluding videos that did not capture speaker introductions, Dr. Duma and collaborators were left with 781 videos to watch and code.
Female speakers overall were less likely to be addressed by their professional title (62% vs. 81% for males, P less than .001). Male introducers used professional titles 53% of the time when introducing female speakers, and 80% of the time when introducing male speakers (P less than .01). No gender differences were seen when females were the introducers (J Clin Oncol. 2019 Oct 11. doi: 10.1200/JCO.19.01608).
Looking further, male introducers addressed female speakers by first name only in 24% of the cases. Female introducers used first names only with female speakers 7% of the time, a statistically significant difference. “This is the part that is really sad,” said Dr. Duma.
She and her coauthors also performed multivariable analysis to adjust for factors such as seniority and geographic location; after adjustment, males were still over 2.5 times as likely as females to be introduced with their professional title, and females were nearly six times as likely as males to be introduced by their first names only. When the introducer was male, a female speaker was over three times more likely to be introduced by her first name only.
Dr. Duma and colleagues are working with the ASCO 2020 planning team to develop a template that standardizes presenter introductions. They’re also planning for prospective data collection at that meeting, and will include self-reported race and ethnicity data for presenters and introducers who choose to provide it.
“We do not plan to create a ‘her versus him’ battle,” said Dr. Duma. “The goal is to use this hardcore data to bring attention to the problem.” She pointed out that, though fewer females introduced other females by first name only, the problem wasn’t limited only to male introducers at ASCO.
“The problem is unconscious bias. Nobody’s exempt,” said Dr. Duma. She related that she herself had just sent a work-related email to a female colleague that addressed her by her first name, and had copied many of their mutual colleagues. Realizing her gaffe, she held herself to her own standard by apologizing to her colleague and copying everyone who saw the first email. “The goal is to bring attention to the difference, so we can improve gender bias in medicine together.”
Patient interactions: Sometimes, a delicate balance
What’s the right approach when a patient, uninvited, addresses you by your first name? Natalie Strand, MD, had been thinking about the best way to handle this sticky situation for some time. Recently, she tried it out on a patient and shared her approach in a tweet:
So proud of myself!
— Natalie Strand (@DrNatStrand) October 11, 2019
After introducing myself as Dr. Strand to a patient, he looked at my name badge and said- oh, so Natalie.
Usually I’m stuck feeling afraid to rock the boat...
Not today!
“Yes, but I go by Dr. Strand at work! “
I finally said it!!!
There was an awkward moment with the patient, Dr. Strand acknowledged, “but we moved past it.”
Asserting one’s hard-earned status despite a societally ingrained desire to please or to avoid confrontation can be difficult, she acknowledged, but it’s worth it. Put simply, she said, “I want to be called Dr. Strand.”
The importance of this issue can sometimes be hard for male colleagues to understand, said Dr. Strand, who practices outpatient interventional pain medicine at the Mayo Clinic, Scottsdale, Ariz. “The people that have privilege – they don’t see it as privilege. And that’s not anybody’s fault. That’s just the reality of it, because that’s the norm. … That’s why putting a name to microaggression and microinsults is so powerful, because once you name it, then you can respond to it.”
Beginning from a point of mutual professionalism is a good place to start, Dr. Strand said in an interview. She always begins by addressing her patients by their surname and waits for patients to invite her to call them by their first names. “The most professional approach is the best first step,” she said. When she has a longstanding relationship with patients and she knows that trust and mutual respect have been established, she may also invite first-name familiarity.
“Patients don’t do this to be mean,” emphasized Dr. Strand, adding that, particularly with older patients, “they are trying to be sweet.” That’s part of the difficulty in finding a gentle but firm way to bring the relationship back to a professional footing.
Judging by the responses she’s gotten from other female physicians, this delicate situation, and the best way to ask for professionalism with patients, is a common struggle. Many of her female peers have said they’ll consider adopting her approach, she said.
“Male physicians are our allies,” said Dr. Strand. “The needs of the patients come first. This isn’t about power; it’s not about holding a power differential against the patient. It’s about having a culture of mutual respect, and being seen as a physician. Not as a female physician, not as a male physician. Just being seen as a physician, so you can act as a physician.”
Whether they come from patients or peers, said Dr. James, who adroitly called out the physician reviewer who asked for her by first name, “These microaggressions are uncomfortable to address at the time they occur – but they are teachable moments that we should all take advantage of. Usually, a gentle correction, such as, ‘I prefer to be addressed as Dr. James while at work,’ is sufficient.” However, she added, “sometimes, a firmer ‘I feel disrespected when you address me by my first name to colleagues and patients’ is needed.”
This article was updated 10/15/19.
In patients with CIS, combined omics predicts conversion to clinically definite MS
STOCKHOLM –
Further, “combined omics improves diagnostic accuracy” over oligoclonal band (OCB) status alone in differentiating patients with multiple sclerosis (MS) from a group of normal control patients, said Fay Probert, PhD, speaking at a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Not everyone with clinically isolated syndrome (CIS) converts to clinically definite MS, and there is large variability in the time to progression, explained Dr. Probert, a postdoctoral fellow in the department of pharmacology at Oxford (England) University, and colleagues. Though the revised McDonald criteria now allow earlier diagnosis of MS, individuals who will be early converters cannot be identified by these criteria, they noted, citing earlier work showing that just over half (52%) of CIS patients who are OCB positive will have clinically definite MS at the 3-year mark.
To see whether combining analysis of multiple proteins and metabolites improved diagnostic accuracy, Dr. Probert and colleagues examined cerebrospinal fluid (CSF) samples from 41 patients with clinically definite MS, 71 patients with CIS, and 64 control participants without MS. In their analysis, the investigators used nuclear MR metabolomics and a commercially available proteomics assay that identifies and quantifies more than 5,000 proteins.
The multivariate analysis strategy achieved 10-fold external cross-validation of the samples, repeating training and testing of the analysis model while shuffling data. This, explained Dr. Probert and colleagues, “ensures that any discrimination observed cannot have occurred by chance.” Further analysis “identifies the optimal combination of proteomics and metabolomics features which results in the highest diagnostic accuracy.”
Both the nuclear MR metabolomics and the proteomic analyses were able to discriminate between those with clinically definite MS and the control participants, with accuracy of 71% and 75%, respectively.
The levels of seven metabolites present in CSF were predictive of clinically definite MS, compared with non-MS status, independent of OCB status. In fact, noted Dr. Probert and colleagues, “the CSF myoinositol concentration alone diagnosed [clinically definite] MS in this cohort with a specificity of 74% but did not outperform OCB status overall.”
Using the combined omics approach, though, “significantly improved the discrimination” between the non-MS control CSF samples and those of patients with clinically definite MS, wrote Dr. Probert and colleagues. Using a combination of up to five CSF proteins and metabolites yielded accuracy of 85 plus or minus 2%, sensitivity of 85 plus or minus 3%, and specificity of 85 plus or minus 3%. For comparison, using just OCB status provides accuracy of 74%, sensitivity of 88% and specificity of 63%.
Then, Dr. Probert and colleagues turned to the CSF samples from patients with CIS to look for predictors of “fast” (4 years or less) or “slow” (greater than 4 years) conversion to clinically definite MS. “While important for diagnosis, OCB status was not predictive of early conversion,” the investigators noted. However, baseline CSF proteomics analysis alone did differentiate the fast from the slow converters among the CIS subgroup, with an accuracy of 77%.
For patients with CIS who were OCB positive, their baseline metabolite and proteomic profiles were “indistinguishable” from those with clinically definite MS, wrote Dr. Probert and colleagues. The omics analysis was also able to distinguish between OCB-positive CIS patients and the non-MS control patients.
“These results indicate that combined metabolomics and proteomics analysis could not only be used as an adjunct in diagnosis of [clinically definite] MS but could be used as a prognostic test to identify CIS patients at high risk of a second clinical attack within 4 years of onset,” wrote Dr. Probert and coauthors. They noted that the method reported in the poster is the first to offer this prognostic accuracy, but that more work is needed before routine clinical use.
Dr. Probert reported that she had no financial conflicts of interest. One coauthor reported being a consultant to Novartis. Two coauthors reported financial relationships with multiple pharmaceutical companies, including Merck, which partially funded the study. Numares Health, the U.K. Medical Research Council, and the Multiple Sclerosis Society also provided funding support.
SOURCE: Probert F et al. ECTRIMS 2019, Abstract P586.
STOCKHOLM –
Further, “combined omics improves diagnostic accuracy” over oligoclonal band (OCB) status alone in differentiating patients with multiple sclerosis (MS) from a group of normal control patients, said Fay Probert, PhD, speaking at a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Not everyone with clinically isolated syndrome (CIS) converts to clinically definite MS, and there is large variability in the time to progression, explained Dr. Probert, a postdoctoral fellow in the department of pharmacology at Oxford (England) University, and colleagues. Though the revised McDonald criteria now allow earlier diagnosis of MS, individuals who will be early converters cannot be identified by these criteria, they noted, citing earlier work showing that just over half (52%) of CIS patients who are OCB positive will have clinically definite MS at the 3-year mark.
To see whether combining analysis of multiple proteins and metabolites improved diagnostic accuracy, Dr. Probert and colleagues examined cerebrospinal fluid (CSF) samples from 41 patients with clinically definite MS, 71 patients with CIS, and 64 control participants without MS. In their analysis, the investigators used nuclear MR metabolomics and a commercially available proteomics assay that identifies and quantifies more than 5,000 proteins.
The multivariate analysis strategy achieved 10-fold external cross-validation of the samples, repeating training and testing of the analysis model while shuffling data. This, explained Dr. Probert and colleagues, “ensures that any discrimination observed cannot have occurred by chance.” Further analysis “identifies the optimal combination of proteomics and metabolomics features which results in the highest diagnostic accuracy.”
Both the nuclear MR metabolomics and the proteomic analyses were able to discriminate between those with clinically definite MS and the control participants, with accuracy of 71% and 75%, respectively.
The levels of seven metabolites present in CSF were predictive of clinically definite MS, compared with non-MS status, independent of OCB status. In fact, noted Dr. Probert and colleagues, “the CSF myoinositol concentration alone diagnosed [clinically definite] MS in this cohort with a specificity of 74% but did not outperform OCB status overall.”
Using the combined omics approach, though, “significantly improved the discrimination” between the non-MS control CSF samples and those of patients with clinically definite MS, wrote Dr. Probert and colleagues. Using a combination of up to five CSF proteins and metabolites yielded accuracy of 85 plus or minus 2%, sensitivity of 85 plus or minus 3%, and specificity of 85 plus or minus 3%. For comparison, using just OCB status provides accuracy of 74%, sensitivity of 88% and specificity of 63%.
Then, Dr. Probert and colleagues turned to the CSF samples from patients with CIS to look for predictors of “fast” (4 years or less) or “slow” (greater than 4 years) conversion to clinically definite MS. “While important for diagnosis, OCB status was not predictive of early conversion,” the investigators noted. However, baseline CSF proteomics analysis alone did differentiate the fast from the slow converters among the CIS subgroup, with an accuracy of 77%.
For patients with CIS who were OCB positive, their baseline metabolite and proteomic profiles were “indistinguishable” from those with clinically definite MS, wrote Dr. Probert and colleagues. The omics analysis was also able to distinguish between OCB-positive CIS patients and the non-MS control patients.
“These results indicate that combined metabolomics and proteomics analysis could not only be used as an adjunct in diagnosis of [clinically definite] MS but could be used as a prognostic test to identify CIS patients at high risk of a second clinical attack within 4 years of onset,” wrote Dr. Probert and coauthors. They noted that the method reported in the poster is the first to offer this prognostic accuracy, but that more work is needed before routine clinical use.
Dr. Probert reported that she had no financial conflicts of interest. One coauthor reported being a consultant to Novartis. Two coauthors reported financial relationships with multiple pharmaceutical companies, including Merck, which partially funded the study. Numares Health, the U.K. Medical Research Council, and the Multiple Sclerosis Society also provided funding support.
SOURCE: Probert F et al. ECTRIMS 2019, Abstract P586.
STOCKHOLM –
Further, “combined omics improves diagnostic accuracy” over oligoclonal band (OCB) status alone in differentiating patients with multiple sclerosis (MS) from a group of normal control patients, said Fay Probert, PhD, speaking at a poster session at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Not everyone with clinically isolated syndrome (CIS) converts to clinically definite MS, and there is large variability in the time to progression, explained Dr. Probert, a postdoctoral fellow in the department of pharmacology at Oxford (England) University, and colleagues. Though the revised McDonald criteria now allow earlier diagnosis of MS, individuals who will be early converters cannot be identified by these criteria, they noted, citing earlier work showing that just over half (52%) of CIS patients who are OCB positive will have clinically definite MS at the 3-year mark.
To see whether combining analysis of multiple proteins and metabolites improved diagnostic accuracy, Dr. Probert and colleagues examined cerebrospinal fluid (CSF) samples from 41 patients with clinically definite MS, 71 patients with CIS, and 64 control participants without MS. In their analysis, the investigators used nuclear MR metabolomics and a commercially available proteomics assay that identifies and quantifies more than 5,000 proteins.
The multivariate analysis strategy achieved 10-fold external cross-validation of the samples, repeating training and testing of the analysis model while shuffling data. This, explained Dr. Probert and colleagues, “ensures that any discrimination observed cannot have occurred by chance.” Further analysis “identifies the optimal combination of proteomics and metabolomics features which results in the highest diagnostic accuracy.”
Both the nuclear MR metabolomics and the proteomic analyses were able to discriminate between those with clinically definite MS and the control participants, with accuracy of 71% and 75%, respectively.
The levels of seven metabolites present in CSF were predictive of clinically definite MS, compared with non-MS status, independent of OCB status. In fact, noted Dr. Probert and colleagues, “the CSF myoinositol concentration alone diagnosed [clinically definite] MS in this cohort with a specificity of 74% but did not outperform OCB status overall.”
Using the combined omics approach, though, “significantly improved the discrimination” between the non-MS control CSF samples and those of patients with clinically definite MS, wrote Dr. Probert and colleagues. Using a combination of up to five CSF proteins and metabolites yielded accuracy of 85 plus or minus 2%, sensitivity of 85 plus or minus 3%, and specificity of 85 plus or minus 3%. For comparison, using just OCB status provides accuracy of 74%, sensitivity of 88% and specificity of 63%.
Then, Dr. Probert and colleagues turned to the CSF samples from patients with CIS to look for predictors of “fast” (4 years or less) or “slow” (greater than 4 years) conversion to clinically definite MS. “While important for diagnosis, OCB status was not predictive of early conversion,” the investigators noted. However, baseline CSF proteomics analysis alone did differentiate the fast from the slow converters among the CIS subgroup, with an accuracy of 77%.
For patients with CIS who were OCB positive, their baseline metabolite and proteomic profiles were “indistinguishable” from those with clinically definite MS, wrote Dr. Probert and colleagues. The omics analysis was also able to distinguish between OCB-positive CIS patients and the non-MS control patients.
“These results indicate that combined metabolomics and proteomics analysis could not only be used as an adjunct in diagnosis of [clinically definite] MS but could be used as a prognostic test to identify CIS patients at high risk of a second clinical attack within 4 years of onset,” wrote Dr. Probert and coauthors. They noted that the method reported in the poster is the first to offer this prognostic accuracy, but that more work is needed before routine clinical use.
Dr. Probert reported that she had no financial conflicts of interest. One coauthor reported being a consultant to Novartis. Two coauthors reported financial relationships with multiple pharmaceutical companies, including Merck, which partially funded the study. Numares Health, the U.K. Medical Research Council, and the Multiple Sclerosis Society also provided funding support.
SOURCE: Probert F et al. ECTRIMS 2019, Abstract P586.
REPORTING FROM ECTRIMS 2019
Intensive cognitive training may be needed for memory gains in MS
STOCKHOLM – Cognitive rehabilitation to address memory deficits in multiple sclerosis (MS) can take a page from efforts to help those with other conditions, but practitioners and patients should realize that more intensive interventions are likely to be of greater benefit in MS.
in addressing the memory problems frequently seen in MS, Piet Bouman reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Hippocampal pathology can underlie the high-impact memory deficits that are seen frequently in patients with MS, noted Mr. Bouman, a doctoral student at Amsterdam University Medical Centers, and his collaborators. However, they observed, which strategies might best ameliorate hippocampal memory loss for those with MS is an open question.
To address this knowledge gap, Mr. Bouman and his coauthors conducted a systematic review and meta-analysis that aimed to determine which memory interventions in current use most help hippocampal memory functioning. The authors did not limit the review to MS, but included other conditions where hippocampal lesions, atrophy, or changes in connection or functioning may affect memory. These include healthy aging, mild cognitive impairment, and Alzheimer’s disease.
Included in the search for studies were those that used either cognitive or exercise interventions and also evaluated both visuospatial and verbal memory using validated measures, such as the Brief Visuospatial Memory Test or the California Verbal Learning Test.
After reviewing an initial 6,697 articles, the authors used Cochrane criteria to eliminate studies that were at high risk of bias. In the end, 141 studies were selected for the final review, and 82 of these were included in the meta-analysis. Eighteen studies involving 895 individuals addressed healthy aging; 39 studies enrolled 2,256 patients with mild cognitive impairment; 8 studies enrolled 223 patients with Alzheimer’s disease; and 26 studies involving 1,174 patients looked at cognitive impairment in the MS population.
To express the efficacy of the interventions across the various studies, Mr. Bouman and collaborators used the ratio of the difference in mean outcomes between groups and the standard deviation in outcome among participants. This ratio, commonly used to harmonize data in meta-analyses, is termed standardized mean difference.
Individuals representing the healthy aging population saw the most benefit from interventions to address memory loss, with a standardized mean difference of 0.48. Patients with mild cognitive impairment saw a standardized mean difference of 0.46, followed by patients with Alzheimer’s disease with a standardized mean difference of 0.43. Patients with MS lagged far behind in their response to interventions to improve memory, with a standardized mean difference of 0.34.
Looking at the different kinds of interventions, exercise interventions showed moderate effectiveness, with a standardized mean difference of 0.46. By contrast, high intensity cognitive training working on memory strategies was the most effective intervention, said Mr. Bouman and his coauthors: This intervention showed a standardized mean difference of 1.03.
Among the varying conditions associated with hippocampal memory loss, MS-related memory problems saw the least response to intervention, “which might be a result of a more widespread pattern of cognitive decline in MS,” noted Mr. Bouman and coauthors.
“Future studies should work from the realization that memory rehabilitation in MS might require a different approach” than that used in healthy aging, mild cognitive impairment, and Alzheimer’s disease, wrote the authors.
Their review revealed “persistent methodological flaws” in the literature, they noted. These included small sample sizes and selection bias.
Mr. Bouman reported that he had no disclosures. One coauthor reported financial relationships with Sanofi Genzyme, Merck-Serono and Biogen Idec. Another reported financial relationships with Merck-Serono, Bogen, Novartis, Genzyme, and Teva Pharmaceuticals.
SOURCE: Bouman P et al. ECTRIMS 2019. Abstract P1439.
STOCKHOLM – Cognitive rehabilitation to address memory deficits in multiple sclerosis (MS) can take a page from efforts to help those with other conditions, but practitioners and patients should realize that more intensive interventions are likely to be of greater benefit in MS.
in addressing the memory problems frequently seen in MS, Piet Bouman reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Hippocampal pathology can underlie the high-impact memory deficits that are seen frequently in patients with MS, noted Mr. Bouman, a doctoral student at Amsterdam University Medical Centers, and his collaborators. However, they observed, which strategies might best ameliorate hippocampal memory loss for those with MS is an open question.
To address this knowledge gap, Mr. Bouman and his coauthors conducted a systematic review and meta-analysis that aimed to determine which memory interventions in current use most help hippocampal memory functioning. The authors did not limit the review to MS, but included other conditions where hippocampal lesions, atrophy, or changes in connection or functioning may affect memory. These include healthy aging, mild cognitive impairment, and Alzheimer’s disease.
Included in the search for studies were those that used either cognitive or exercise interventions and also evaluated both visuospatial and verbal memory using validated measures, such as the Brief Visuospatial Memory Test or the California Verbal Learning Test.
After reviewing an initial 6,697 articles, the authors used Cochrane criteria to eliminate studies that were at high risk of bias. In the end, 141 studies were selected for the final review, and 82 of these were included in the meta-analysis. Eighteen studies involving 895 individuals addressed healthy aging; 39 studies enrolled 2,256 patients with mild cognitive impairment; 8 studies enrolled 223 patients with Alzheimer’s disease; and 26 studies involving 1,174 patients looked at cognitive impairment in the MS population.
To express the efficacy of the interventions across the various studies, Mr. Bouman and collaborators used the ratio of the difference in mean outcomes between groups and the standard deviation in outcome among participants. This ratio, commonly used to harmonize data in meta-analyses, is termed standardized mean difference.
Individuals representing the healthy aging population saw the most benefit from interventions to address memory loss, with a standardized mean difference of 0.48. Patients with mild cognitive impairment saw a standardized mean difference of 0.46, followed by patients with Alzheimer’s disease with a standardized mean difference of 0.43. Patients with MS lagged far behind in their response to interventions to improve memory, with a standardized mean difference of 0.34.
Looking at the different kinds of interventions, exercise interventions showed moderate effectiveness, with a standardized mean difference of 0.46. By contrast, high intensity cognitive training working on memory strategies was the most effective intervention, said Mr. Bouman and his coauthors: This intervention showed a standardized mean difference of 1.03.
Among the varying conditions associated with hippocampal memory loss, MS-related memory problems saw the least response to intervention, “which might be a result of a more widespread pattern of cognitive decline in MS,” noted Mr. Bouman and coauthors.
“Future studies should work from the realization that memory rehabilitation in MS might require a different approach” than that used in healthy aging, mild cognitive impairment, and Alzheimer’s disease, wrote the authors.
Their review revealed “persistent methodological flaws” in the literature, they noted. These included small sample sizes and selection bias.
Mr. Bouman reported that he had no disclosures. One coauthor reported financial relationships with Sanofi Genzyme, Merck-Serono and Biogen Idec. Another reported financial relationships with Merck-Serono, Bogen, Novartis, Genzyme, and Teva Pharmaceuticals.
SOURCE: Bouman P et al. ECTRIMS 2019. Abstract P1439.
STOCKHOLM – Cognitive rehabilitation to address memory deficits in multiple sclerosis (MS) can take a page from efforts to help those with other conditions, but practitioners and patients should realize that more intensive interventions are likely to be of greater benefit in MS.
in addressing the memory problems frequently seen in MS, Piet Bouman reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
Hippocampal pathology can underlie the high-impact memory deficits that are seen frequently in patients with MS, noted Mr. Bouman, a doctoral student at Amsterdam University Medical Centers, and his collaborators. However, they observed, which strategies might best ameliorate hippocampal memory loss for those with MS is an open question.
To address this knowledge gap, Mr. Bouman and his coauthors conducted a systematic review and meta-analysis that aimed to determine which memory interventions in current use most help hippocampal memory functioning. The authors did not limit the review to MS, but included other conditions where hippocampal lesions, atrophy, or changes in connection or functioning may affect memory. These include healthy aging, mild cognitive impairment, and Alzheimer’s disease.
Included in the search for studies were those that used either cognitive or exercise interventions and also evaluated both visuospatial and verbal memory using validated measures, such as the Brief Visuospatial Memory Test or the California Verbal Learning Test.
After reviewing an initial 6,697 articles, the authors used Cochrane criteria to eliminate studies that were at high risk of bias. In the end, 141 studies were selected for the final review, and 82 of these were included in the meta-analysis. Eighteen studies involving 895 individuals addressed healthy aging; 39 studies enrolled 2,256 patients with mild cognitive impairment; 8 studies enrolled 223 patients with Alzheimer’s disease; and 26 studies involving 1,174 patients looked at cognitive impairment in the MS population.
To express the efficacy of the interventions across the various studies, Mr. Bouman and collaborators used the ratio of the difference in mean outcomes between groups and the standard deviation in outcome among participants. This ratio, commonly used to harmonize data in meta-analyses, is termed standardized mean difference.
Individuals representing the healthy aging population saw the most benefit from interventions to address memory loss, with a standardized mean difference of 0.48. Patients with mild cognitive impairment saw a standardized mean difference of 0.46, followed by patients with Alzheimer’s disease with a standardized mean difference of 0.43. Patients with MS lagged far behind in their response to interventions to improve memory, with a standardized mean difference of 0.34.
Looking at the different kinds of interventions, exercise interventions showed moderate effectiveness, with a standardized mean difference of 0.46. By contrast, high intensity cognitive training working on memory strategies was the most effective intervention, said Mr. Bouman and his coauthors: This intervention showed a standardized mean difference of 1.03.
Among the varying conditions associated with hippocampal memory loss, MS-related memory problems saw the least response to intervention, “which might be a result of a more widespread pattern of cognitive decline in MS,” noted Mr. Bouman and coauthors.
“Future studies should work from the realization that memory rehabilitation in MS might require a different approach” than that used in healthy aging, mild cognitive impairment, and Alzheimer’s disease, wrote the authors.
Their review revealed “persistent methodological flaws” in the literature, they noted. These included small sample sizes and selection bias.
Mr. Bouman reported that he had no disclosures. One coauthor reported financial relationships with Sanofi Genzyme, Merck-Serono and Biogen Idec. Another reported financial relationships with Merck-Serono, Bogen, Novartis, Genzyme, and Teva Pharmaceuticals.
SOURCE: Bouman P et al. ECTRIMS 2019. Abstract P1439.
REPORTING FROM ECTRIMS 2019
Baseline neurofilament light levels track with brain volume loss in MS
STOCKHOLM – according to a recent study. The correlation between CSF NfL at baseline and the percent of total brain volume change was statistically significant and persisted over time, said Alok Bhan, MD, in an interview at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“We found a significant correlation between loss of total brain volume with baseline CSF NfL at the 5- and 10-year follow-up,” reported Dr. Bhan. At the 5-year mark, the correlation coefficient (r) was –0.430 (P = .003); at 10 years, the correlation coefficient was –0.395 (P = .042).
Higher CSF levels of the neuropeptide “thereby predicted steeper loss of brain volume over a 10-year disease course, and baseline CSF NfL could thus be a prognostic factor for later MRI-confirmed progression,” reported Dr. Bhan, of the department of neurology at Stavanger (Norway) University Hospital, and his coinvestigators.
Magnetic resonance imaging, the current standard in tracking MS lesions, has limitations, noted the investigators. “MRI pathology is only revealed after the injury has manifested itself, and as it is commonly being conducted no more frequent[ly] than annually, lesions may have developed up to a year” before they are evident on MRI scans, they said.
Concerns about long-term effects of the gadolinium deposition that results from frequent scans are rising as well, said Dr. Bhan. For these reasons, he said, MRI is an imperfect biomarker for MS progression.
NfL is a polypeptide in neurons that has been proposed as prognostic in MS, but “longitudinal data regarding its prognostic value” are still scarce, said Dr. Bhan.
To help fill that knowledge gap, the study aimed to assess how NfL obtained from CSF at the time of MS diagnosis correlated with MRI-determined loss of brain volume over a period of 10 years.
Participants’ brain atrophy was assessed using MRI performed at baseline and at 5 and 10 years using the same protocol on a 1.5 Tesla scanner. The protocol included dual spin echo T2-weighted imaging, 3-D T1-weighted imaging, and dual spin echo T1-weighted imaging. In addition to obtaining both global and regional changes in brain volume, the investigators also calculated regional volumes for subcortical deep gray matter.
Cerebrospinal fluid obtained from the lumbar puncture performed at the time of baseline assessment was the source for the single NfL value, obtained by use of a commercially available enzyme-linked immunosorbent assay.
Looking at volume loss in specific brain regions, significant correlations were seen between volume loss in the deep gray matter at both 5 and 10 years (r = –0.430 and –0.395; P = .006 and .042, respectively). At 10 years, pallidal nuclei and hippocampal volume losses also correlated significantly with baseline CSF NfL (r = –0.445 and –0.472; P = .020 and .013, respectively).
Attrition was substantial in the cohort, with the initial 44 patients dropping to 39 at 5 years and 27 by 10 years. Of those 44 initial enrollees, 30 were female, and the mean age was about 42 years at baseline. Duration of MS was a median 60 months at the time of enrollment, and the mean Extended Disability Status Scale (EDSS) score was 3.5 at baseline. Most patients (n = 35) had relapsing-remitting MS.
Just 16% of enrollees were on disease-modifying therapy at baseline, but this figure climbed to 52% by the end of the study period, said Dr. Bhan, a trend that in part reflected changes in practice patterns over the study period.
“Our study is yet another report that supports the use of CSF NfL in the routine work-up of newly diagnosed MS,” noted Dr. Bhan and his coauthors. Having a baseline CSF NfL level “would give patients an indication of future disease burden 10 years in advance,” thereby adding to the prognostic toolkit, they said.
Dr. Bhan reported receiving research funding from Novartis Norway, and two other coauthors reported several financial relationships with pharmaceutical companies.
SOURCE: Bhan A et al. ECTRIMS 2019, Abstract P592.
STOCKHOLM – according to a recent study. The correlation between CSF NfL at baseline and the percent of total brain volume change was statistically significant and persisted over time, said Alok Bhan, MD, in an interview at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“We found a significant correlation between loss of total brain volume with baseline CSF NfL at the 5- and 10-year follow-up,” reported Dr. Bhan. At the 5-year mark, the correlation coefficient (r) was –0.430 (P = .003); at 10 years, the correlation coefficient was –0.395 (P = .042).
Higher CSF levels of the neuropeptide “thereby predicted steeper loss of brain volume over a 10-year disease course, and baseline CSF NfL could thus be a prognostic factor for later MRI-confirmed progression,” reported Dr. Bhan, of the department of neurology at Stavanger (Norway) University Hospital, and his coinvestigators.
Magnetic resonance imaging, the current standard in tracking MS lesions, has limitations, noted the investigators. “MRI pathology is only revealed after the injury has manifested itself, and as it is commonly being conducted no more frequent[ly] than annually, lesions may have developed up to a year” before they are evident on MRI scans, they said.
Concerns about long-term effects of the gadolinium deposition that results from frequent scans are rising as well, said Dr. Bhan. For these reasons, he said, MRI is an imperfect biomarker for MS progression.
NfL is a polypeptide in neurons that has been proposed as prognostic in MS, but “longitudinal data regarding its prognostic value” are still scarce, said Dr. Bhan.
To help fill that knowledge gap, the study aimed to assess how NfL obtained from CSF at the time of MS diagnosis correlated with MRI-determined loss of brain volume over a period of 10 years.
Participants’ brain atrophy was assessed using MRI performed at baseline and at 5 and 10 years using the same protocol on a 1.5 Tesla scanner. The protocol included dual spin echo T2-weighted imaging, 3-D T1-weighted imaging, and dual spin echo T1-weighted imaging. In addition to obtaining both global and regional changes in brain volume, the investigators also calculated regional volumes for subcortical deep gray matter.
Cerebrospinal fluid obtained from the lumbar puncture performed at the time of baseline assessment was the source for the single NfL value, obtained by use of a commercially available enzyme-linked immunosorbent assay.
Looking at volume loss in specific brain regions, significant correlations were seen between volume loss in the deep gray matter at both 5 and 10 years (r = –0.430 and –0.395; P = .006 and .042, respectively). At 10 years, pallidal nuclei and hippocampal volume losses also correlated significantly with baseline CSF NfL (r = –0.445 and –0.472; P = .020 and .013, respectively).
Attrition was substantial in the cohort, with the initial 44 patients dropping to 39 at 5 years and 27 by 10 years. Of those 44 initial enrollees, 30 were female, and the mean age was about 42 years at baseline. Duration of MS was a median 60 months at the time of enrollment, and the mean Extended Disability Status Scale (EDSS) score was 3.5 at baseline. Most patients (n = 35) had relapsing-remitting MS.
Just 16% of enrollees were on disease-modifying therapy at baseline, but this figure climbed to 52% by the end of the study period, said Dr. Bhan, a trend that in part reflected changes in practice patterns over the study period.
“Our study is yet another report that supports the use of CSF NfL in the routine work-up of newly diagnosed MS,” noted Dr. Bhan and his coauthors. Having a baseline CSF NfL level “would give patients an indication of future disease burden 10 years in advance,” thereby adding to the prognostic toolkit, they said.
Dr. Bhan reported receiving research funding from Novartis Norway, and two other coauthors reported several financial relationships with pharmaceutical companies.
SOURCE: Bhan A et al. ECTRIMS 2019, Abstract P592.
STOCKHOLM – according to a recent study. The correlation between CSF NfL at baseline and the percent of total brain volume change was statistically significant and persisted over time, said Alok Bhan, MD, in an interview at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
“We found a significant correlation between loss of total brain volume with baseline CSF NfL at the 5- and 10-year follow-up,” reported Dr. Bhan. At the 5-year mark, the correlation coefficient (r) was –0.430 (P = .003); at 10 years, the correlation coefficient was –0.395 (P = .042).
Higher CSF levels of the neuropeptide “thereby predicted steeper loss of brain volume over a 10-year disease course, and baseline CSF NfL could thus be a prognostic factor for later MRI-confirmed progression,” reported Dr. Bhan, of the department of neurology at Stavanger (Norway) University Hospital, and his coinvestigators.
Magnetic resonance imaging, the current standard in tracking MS lesions, has limitations, noted the investigators. “MRI pathology is only revealed after the injury has manifested itself, and as it is commonly being conducted no more frequent[ly] than annually, lesions may have developed up to a year” before they are evident on MRI scans, they said.
Concerns about long-term effects of the gadolinium deposition that results from frequent scans are rising as well, said Dr. Bhan. For these reasons, he said, MRI is an imperfect biomarker for MS progression.
NfL is a polypeptide in neurons that has been proposed as prognostic in MS, but “longitudinal data regarding its prognostic value” are still scarce, said Dr. Bhan.
To help fill that knowledge gap, the study aimed to assess how NfL obtained from CSF at the time of MS diagnosis correlated with MRI-determined loss of brain volume over a period of 10 years.
Participants’ brain atrophy was assessed using MRI performed at baseline and at 5 and 10 years using the same protocol on a 1.5 Tesla scanner. The protocol included dual spin echo T2-weighted imaging, 3-D T1-weighted imaging, and dual spin echo T1-weighted imaging. In addition to obtaining both global and regional changes in brain volume, the investigators also calculated regional volumes for subcortical deep gray matter.
Cerebrospinal fluid obtained from the lumbar puncture performed at the time of baseline assessment was the source for the single NfL value, obtained by use of a commercially available enzyme-linked immunosorbent assay.
Looking at volume loss in specific brain regions, significant correlations were seen between volume loss in the deep gray matter at both 5 and 10 years (r = –0.430 and –0.395; P = .006 and .042, respectively). At 10 years, pallidal nuclei and hippocampal volume losses also correlated significantly with baseline CSF NfL (r = –0.445 and –0.472; P = .020 and .013, respectively).
Attrition was substantial in the cohort, with the initial 44 patients dropping to 39 at 5 years and 27 by 10 years. Of those 44 initial enrollees, 30 were female, and the mean age was about 42 years at baseline. Duration of MS was a median 60 months at the time of enrollment, and the mean Extended Disability Status Scale (EDSS) score was 3.5 at baseline. Most patients (n = 35) had relapsing-remitting MS.
Just 16% of enrollees were on disease-modifying therapy at baseline, but this figure climbed to 52% by the end of the study period, said Dr. Bhan, a trend that in part reflected changes in practice patterns over the study period.
“Our study is yet another report that supports the use of CSF NfL in the routine work-up of newly diagnosed MS,” noted Dr. Bhan and his coauthors. Having a baseline CSF NfL level “would give patients an indication of future disease burden 10 years in advance,” thereby adding to the prognostic toolkit, they said.
Dr. Bhan reported receiving research funding from Novartis Norway, and two other coauthors reported several financial relationships with pharmaceutical companies.
SOURCE: Bhan A et al. ECTRIMS 2019, Abstract P592.
REPORTING FROM ECTRIMS 2019
Tocilizumab beat azathioprine for NMOSD
STOCKHOLM – according to data reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
The tocilizumab versus azathioprine in highly relapsing neuromyelitis optica spectrum disorders (TANGO) trial, explained senior investigator Fu-Dong Shi, MD, PhD, tracked the time to first NMOSD relapse for patients randomized either to tocilizumab or azathioprine. After 60 weeks of participation in the head-to-head trial, 86% of patients receiving tocilizumab remained relapse-free, compared with 56.9% of those on azathioprine. By 90 weeks of therapy, the relapse-free rate held at 86% for those receiving tocilizumab, compared with 48.1% for those on azathioprine, for a 76.4% relative reduction in risk of relapse.
Patients with concomitant autoimmune disease saw particular benefit from tocilizumab compared with azathioprine. On tocilizumab, 78.8% of those with concomitant autoimmune disease remained relapse-free at 90 weeks, a rate that did not differ significantly from that seen in those without other autoimmune disease. However, 22.3% of those with concomitant autoimmune disease who received azathioprine remained relapse-free at 90 weeks, compared with 63.5% of those without autoimmune disease.
Dr. Shi, of the Tianjin (China) Medical University General Hospital, explained that there was limited evidence for the advantage of newer disease-modifying therapies (DMTs) over such older medications as azathioprine to treat NMOSD. Therefore, he said, he and other investigators in the Chinese Medical Network for Neuroinflammation (CMNN), including first author Chao Zhang, MD, initiated a randomized, multicenter, open-label trial that compared tocilizumab to azathioprine for highly relapsing NMOSD.
A total of 118 patients were enrolled. To participate, patients had to meet the 2015 international consensus criteria for NMOSD, and have had at least two relapses in the past year or three relapses within the preceding 2 years.
After a washout period, participants were randomized 1:1 to receive daily oral azathioprine dosed at 2-3 mg/kg or intravenous tocilizumab dosed at 8 mg/kg every 4 weeks. Participants continued on the assigned regimen for at least 60 weeks.
Secondary endpoints included 12-week confirmed disability progression. Here, 35.8% of those on azathioprine saw disability progression, compared with 9.9% on tocilizumab, for a 72.5% relative risk reduction. Serum aquaporin 4-IgG titers fell further for those taking tocilizumab.
In terms of safety, 83% of those on azathioprine and 61% of those receiving tocilizumab had a treatment-related adverse event, as determined by investigator assessment. About half of patients in each group experienced moderate adverse events, and about 90% had mild adverse events in each group. However, there were twice as many severe adverse events among those taking azathioprine. There was one NMOSD-related death in each group.
Subgroup analyses looked at baseline disability scores, number of previous relapses, disease duration, and age at randomization. None of these variables made a difference in the statistically better performance of tocilizumab compared with azathioprine, with hazard ratios ranging from 0.076 to 0.343 in favor of tocilizumab for all subgroups.
Patients were almost all female (92% overall) and about 47 years old at baseline, with a 6-year history of NMOSD.
Overall, 83% of the cohort had experienced optic neuritis over the preceding 2 years, and 94% had experienced acute myelitis. Other manifestations of NMOSD, such as acute brainstem syndrome and symptomatic cerebral syndrome, were much less frequent, occurring in 4%-30% of patients.
Most patients (71%) had been on oral corticosteroids before the washout period, and 34% had been taking mycophenolate mofetil. Azathioprine was taken by 44% of patients at baseline.
Additional data captured during the TANGO trial are being analyzed and will be reported at a later date, said Dr. Shi. These include optical coherence tomography and visual evoked potentials; magnetic resonance imaging of the brain, spinal cord, and optic nerve; and tracking serum B-cell subpopulations. He added that the investigators are continuing long-term, real-world follow-up of the TANGO patient cohort.
Dr. Shi acknowledged that TANGO was limited by the lack of an independent data monitoring committee and the open-label nature of the study.
The study was funded by Tianjin Medical University; Capital Medical University, Beijing; and the National Science Foundation of China. Dr. Shi and coauthors reported no conflicts of interest.
SOURCE: Zhang C et al. ECTRIMS 2019, Abstract 140.
STOCKHOLM – according to data reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
The tocilizumab versus azathioprine in highly relapsing neuromyelitis optica spectrum disorders (TANGO) trial, explained senior investigator Fu-Dong Shi, MD, PhD, tracked the time to first NMOSD relapse for patients randomized either to tocilizumab or azathioprine. After 60 weeks of participation in the head-to-head trial, 86% of patients receiving tocilizumab remained relapse-free, compared with 56.9% of those on azathioprine. By 90 weeks of therapy, the relapse-free rate held at 86% for those receiving tocilizumab, compared with 48.1% for those on azathioprine, for a 76.4% relative reduction in risk of relapse.
Patients with concomitant autoimmune disease saw particular benefit from tocilizumab compared with azathioprine. On tocilizumab, 78.8% of those with concomitant autoimmune disease remained relapse-free at 90 weeks, a rate that did not differ significantly from that seen in those without other autoimmune disease. However, 22.3% of those with concomitant autoimmune disease who received azathioprine remained relapse-free at 90 weeks, compared with 63.5% of those without autoimmune disease.
Dr. Shi, of the Tianjin (China) Medical University General Hospital, explained that there was limited evidence for the advantage of newer disease-modifying therapies (DMTs) over such older medications as azathioprine to treat NMOSD. Therefore, he said, he and other investigators in the Chinese Medical Network for Neuroinflammation (CMNN), including first author Chao Zhang, MD, initiated a randomized, multicenter, open-label trial that compared tocilizumab to azathioprine for highly relapsing NMOSD.
A total of 118 patients were enrolled. To participate, patients had to meet the 2015 international consensus criteria for NMOSD, and have had at least two relapses in the past year or three relapses within the preceding 2 years.
After a washout period, participants were randomized 1:1 to receive daily oral azathioprine dosed at 2-3 mg/kg or intravenous tocilizumab dosed at 8 mg/kg every 4 weeks. Participants continued on the assigned regimen for at least 60 weeks.
Secondary endpoints included 12-week confirmed disability progression. Here, 35.8% of those on azathioprine saw disability progression, compared with 9.9% on tocilizumab, for a 72.5% relative risk reduction. Serum aquaporin 4-IgG titers fell further for those taking tocilizumab.
In terms of safety, 83% of those on azathioprine and 61% of those receiving tocilizumab had a treatment-related adverse event, as determined by investigator assessment. About half of patients in each group experienced moderate adverse events, and about 90% had mild adverse events in each group. However, there were twice as many severe adverse events among those taking azathioprine. There was one NMOSD-related death in each group.
Subgroup analyses looked at baseline disability scores, number of previous relapses, disease duration, and age at randomization. None of these variables made a difference in the statistically better performance of tocilizumab compared with azathioprine, with hazard ratios ranging from 0.076 to 0.343 in favor of tocilizumab for all subgroups.
Patients were almost all female (92% overall) and about 47 years old at baseline, with a 6-year history of NMOSD.
Overall, 83% of the cohort had experienced optic neuritis over the preceding 2 years, and 94% had experienced acute myelitis. Other manifestations of NMOSD, such as acute brainstem syndrome and symptomatic cerebral syndrome, were much less frequent, occurring in 4%-30% of patients.
Most patients (71%) had been on oral corticosteroids before the washout period, and 34% had been taking mycophenolate mofetil. Azathioprine was taken by 44% of patients at baseline.
Additional data captured during the TANGO trial are being analyzed and will be reported at a later date, said Dr. Shi. These include optical coherence tomography and visual evoked potentials; magnetic resonance imaging of the brain, spinal cord, and optic nerve; and tracking serum B-cell subpopulations. He added that the investigators are continuing long-term, real-world follow-up of the TANGO patient cohort.
Dr. Shi acknowledged that TANGO was limited by the lack of an independent data monitoring committee and the open-label nature of the study.
The study was funded by Tianjin Medical University; Capital Medical University, Beijing; and the National Science Foundation of China. Dr. Shi and coauthors reported no conflicts of interest.
SOURCE: Zhang C et al. ECTRIMS 2019, Abstract 140.
STOCKHOLM – according to data reported at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis.
The tocilizumab versus azathioprine in highly relapsing neuromyelitis optica spectrum disorders (TANGO) trial, explained senior investigator Fu-Dong Shi, MD, PhD, tracked the time to first NMOSD relapse for patients randomized either to tocilizumab or azathioprine. After 60 weeks of participation in the head-to-head trial, 86% of patients receiving tocilizumab remained relapse-free, compared with 56.9% of those on azathioprine. By 90 weeks of therapy, the relapse-free rate held at 86% for those receiving tocilizumab, compared with 48.1% for those on azathioprine, for a 76.4% relative reduction in risk of relapse.
Patients with concomitant autoimmune disease saw particular benefit from tocilizumab compared with azathioprine. On tocilizumab, 78.8% of those with concomitant autoimmune disease remained relapse-free at 90 weeks, a rate that did not differ significantly from that seen in those without other autoimmune disease. However, 22.3% of those with concomitant autoimmune disease who received azathioprine remained relapse-free at 90 weeks, compared with 63.5% of those without autoimmune disease.
Dr. Shi, of the Tianjin (China) Medical University General Hospital, explained that there was limited evidence for the advantage of newer disease-modifying therapies (DMTs) over such older medications as azathioprine to treat NMOSD. Therefore, he said, he and other investigators in the Chinese Medical Network for Neuroinflammation (CMNN), including first author Chao Zhang, MD, initiated a randomized, multicenter, open-label trial that compared tocilizumab to azathioprine for highly relapsing NMOSD.
A total of 118 patients were enrolled. To participate, patients had to meet the 2015 international consensus criteria for NMOSD, and have had at least two relapses in the past year or three relapses within the preceding 2 years.
After a washout period, participants were randomized 1:1 to receive daily oral azathioprine dosed at 2-3 mg/kg or intravenous tocilizumab dosed at 8 mg/kg every 4 weeks. Participants continued on the assigned regimen for at least 60 weeks.
Secondary endpoints included 12-week confirmed disability progression. Here, 35.8% of those on azathioprine saw disability progression, compared with 9.9% on tocilizumab, for a 72.5% relative risk reduction. Serum aquaporin 4-IgG titers fell further for those taking tocilizumab.
In terms of safety, 83% of those on azathioprine and 61% of those receiving tocilizumab had a treatment-related adverse event, as determined by investigator assessment. About half of patients in each group experienced moderate adverse events, and about 90% had mild adverse events in each group. However, there were twice as many severe adverse events among those taking azathioprine. There was one NMOSD-related death in each group.
Subgroup analyses looked at baseline disability scores, number of previous relapses, disease duration, and age at randomization. None of these variables made a difference in the statistically better performance of tocilizumab compared with azathioprine, with hazard ratios ranging from 0.076 to 0.343 in favor of tocilizumab for all subgroups.
Patients were almost all female (92% overall) and about 47 years old at baseline, with a 6-year history of NMOSD.
Overall, 83% of the cohort had experienced optic neuritis over the preceding 2 years, and 94% had experienced acute myelitis. Other manifestations of NMOSD, such as acute brainstem syndrome and symptomatic cerebral syndrome, were much less frequent, occurring in 4%-30% of patients.
Most patients (71%) had been on oral corticosteroids before the washout period, and 34% had been taking mycophenolate mofetil. Azathioprine was taken by 44% of patients at baseline.
Additional data captured during the TANGO trial are being analyzed and will be reported at a later date, said Dr. Shi. These include optical coherence tomography and visual evoked potentials; magnetic resonance imaging of the brain, spinal cord, and optic nerve; and tracking serum B-cell subpopulations. He added that the investigators are continuing long-term, real-world follow-up of the TANGO patient cohort.
Dr. Shi acknowledged that TANGO was limited by the lack of an independent data monitoring committee and the open-label nature of the study.
The study was funded by Tianjin Medical University; Capital Medical University, Beijing; and the National Science Foundation of China. Dr. Shi and coauthors reported no conflicts of interest.
SOURCE: Zhang C et al. ECTRIMS 2019, Abstract 140.
REPORTING FROM ECTRIMS 2019