User login
Development of a VA Clinician Resource to Facilitate Care Among Veterans Experiencing Homelessness
Development of a VA Clinician Resource to Facilitate Care Among Veterans Experiencing Homelessness
Veterans experiencing homelessness are at an elevated risk for adverse health outcomes, including suicide. This population also experiences chronic health conditions (eg, cardiovascular disease and sexually transmitted infections) and psychiatric conditions (eg, substance use disorders and posttraumatic stress disorder) with a greater propensity than veterans without history of homelessness.1,2 Similarly, veterans experiencing homelessness often report concurrent stressors, such as justice involvement and unemployment, which further impact social functioning.3
The US Department of Veterans Affairs (VA) offers a range of health and social services to veterans experiencing homelessness. These programs are designed to respond to the multifactorial challenges faced by this population and are aimed at achieving sustained, permanent housing.4 To facilitate this effort, these programs provide targeted and tailored health (eg, primary care) and social (eg, case management and vocational rehabilitation) services to address barriers to housing stability (eg, substance use, serious mental illness, interacting with the criminal legal system, and unemployment).
Despite the availability of these programs, engaging veterans in VA services—whether in general or tailored for those experiencing or at risk for homelessness—remains challenging. Many veterans at risk for or experiencing homelessness overuse service settings that provide immediate care, such as urgent care or emergency departments (EDs).5,6 These individuals often visit an ED to augment or complement medical care they received in an outpatient setting, which can result in an elevated health care burden as well as impacted provision of treatment, especially surrounding care for chronic conditions (eg, cardiovascular health or serious mental illness).7-9
VA EDs offer urgent care and emergency services and often serve as a point of entry for veterans experiencing homelessness.10 They offer veterans expedient access to care that can address immediate needs (eg, substance use withdrawal, pain management, and suicide risk). EDs may be easier to access given they have longer hours of operation and patients can present without a scheduled appointment. VA EDs are an important point to identify homelessness and connect individuals to social service resources and outpatient health care referrals (eg, primary care and mental health).4,11
Some clinicians experience uncertainty in navigating or providing care for veterans experiencing or at risk for homelessness. A qualitative study conducted outside the VA found many clinicians did not know how to approach clinical conversations among unstably housed individuals, particularly when they discussed how to manage care for complex health conditions in the context of ongoing case management challenges, such as discharge planning.12 Another study found that clinicians working with individuals experiencing homelessness may have limited prior training or experience treating these patients.13 As a result, these clinicians may be unaware of available social services or unknowingly have biases that negatively impact care. Research remains limited surrounding beliefs about and methods of enhancing care among VA clinicians working with veterans experiencing homelessness in the ED.
This multiphase pilot study sought to understand service delivery processes and gaps in VA ED settings. Phase 1 examined ED clinician perceptions of care, facilitators, and barriers to providing care (including suicide risk assessments) and making postdischarge outpatient referrals among VA ED clinicians who regularly work with veterans experiencing homelessness. Phase 2 used this information to develop a clinical psychoeducational resource to enhance post-ED access to care for veterans experiencing or at risk for homelessness.
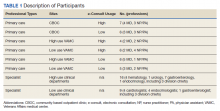
QUALITATIVE INTERVIEWS
Semistructured qualitative interviews were conducted with 11 VA ED clinicians from 6 Veteran Integrated Service Networks between August 2022 and February 2023. Clinicians were eligible if they currently worked within a VA ED setting (including urgent care) and indicated that some of their patients were veterans experiencing homelessness. All health care practitioners (HCPs) participated in an interview and a postinterview self-report survey that assessed demographic and job-related characteristics. Eight HCPs identified as female and 3 identified as male. All clinicians identified as White and 3 as Hispanic or Latino. Eight clinicians were licensed clinical social workers, 2 were ED nurses, and 1 was an ED physician.
After each clinician provided informed consent, they were invited to complete a telephone or Microsoft Teams interview. All interviews were recorded and subsequently transcribed. Interviews explored clinicians’ experiences caring for veterans experiencing homelessness, with a focus on services provided within the ED, as well as mandated ED screenings such as a suicide risk assessment. Interview questions also addressed postdischarge knowledge and experiences with referrals to VA health services (eg, primary care, mental health) and social services (eg, housing programs). Interviews lasted 30 to 90 minutes.
Recruitment ended after attaining sufficient thematic data, accomplished via an information power approach to sampling. This occurred when the study aims, sample characteristics, existing theory, and depth and quality of interviews dynamically informed the decision to cease recruitment of additional participants.14,15 Given the scope of study (examining service delivery and knowledge gaps), the specificity of the targeted sample (VA ED clinicians providing care to veterans experiencing homelessness), the level of pre-existing theoretical background informing the study aims, and depth and quality of interview dialogue, this information power approach provides justification for attaining small sample sizes. Following the interview, HCPs completed a demographic questionnaire. Participants were not compensated.
Data Analysis
Directed content analysis was used to analyze qualitative data, with the framework method employed as an analytic instrument to facilitate analysis.16-18 Analysts engaged in bracketing and discussed reflexivity before data analysis to reflect on personal subjectivities and reduce potential bias.19,20
A prototype coding framework was developed that enabled coders to meaningfully summarize and condense data within transcripts into varying domains, categories, or topics found within the interview guide. Domain examples included clinical backgrounds, suicide risk and assessment protocols among veterans experiencing homelessness, beliefs about service delivery for veterans experiencing homelessness, and barriers and facilitators that may impact their ability to provide post-ED discharge care. Coders discussed the findings and if there was a need to modify templates. All transcripts were double coded. Once complete, individual templates were merged into a unified Microsoft Excel sheet, which allowed for more discrete analyses, enabling analysts to examine trends across content areas within the dataset.
Clinical Resource Development
HCPs were queried regarding available outpatient resources for post-ED care (eg, printed discharge paperwork and best practice alerts or automated workflows within the electronic health record). Resources used by participants were examined, as well as which resources clinicians thought would help them care for veterans experiencing homelessness. Noted gaps were used to develop a tailored resource for clinicians who treat veterans experiencing homelessness in the ED. This resource was created with the intention it could inform all ED clinicians, with the option for personalization to align with the needs of local services, based on needed content areas identified (eg, emergency shelters and suicide prevention resources).
Resource development followed an information systems research (ISR) framework that used a 3-pronged process of identifying circumstances for how a tool is developed, the problems it aims to address, and the knowledge that informs its development, implementation, and evaluation.21,22 Initial wireframes of the resource were provided via email to 10 subject matter experts (SMEs) in veteran suicide prevention, emergency medicine, and homeless programs. SMEs were identified via professional listservs, VA program office leadership, literature searches of similar research, and snowball sampling. Solicited feedback on the resource from the SMEs included its design, language, tone, flow, format, and content (ideation and prototyping). The feedback was collated and used to revise the resource. SMEs then reviewed and provided feedback on the revised resource. This iterative cycle (prototype review, commentary, ideation, prototype review) continued until the SMEs offered no additional edits to the resource. In total, 7 iterations of the resource were developed, critiqued, and revised.
INTERVIEW RESULTS
Compassion Fatigue
Many participants expressed concerns about compassion fatigue among VA ED clinicians. Those interviewed indicated that treating veterans experiencing homelessness sometimes led to the development of what they described as a “callus,” a “sixth sense,” or an inherent sense of “suspicion” or distrust. These feelings resulted from concerns about an individual’s secondary gain or potential hidden agenda (eg, a veteran reporting suicidal ideation to attain shelter on a cold night), with clinicians not wanting to feel as if they were taken advantage of or deceived.
Many clinicians noted that compassion fatigue resulted from witnessing the same veterans experiencing homelessness routinely use emergency services for nonemergent or nonmedical needs. Some also expressed that over time this may result in them becoming less empathetic when caring for veterans experiencing homelessness. They hypothesized that clinicians may experience burnout, which could potentially result in a lack of curiosity and concern about a veteran’s risk for suicide or need for social services. Others may “take things for granted,” leading them to discount stressors that are “very real to the patient, this person.”
Clinicians indicated that such sentiments may impact overall care. Potential negative consequences included stigmatization of veterans experiencing homelessness, incomplete or partial suicide risk screenings with this population, inattentive or impersonal care, and expedited discharge from the ED without appropriate safety planning or social service referrals. Clinicians interviewed intended to find ways to combat compassion fatigue and maintain a commitment to provide comprehensive care to all veterans, including those experiencing homelessness. They felt conflict between a lack of empathy for individuals experiencing homelessness and becoming numb to the problem due to overexposure. However, these clinicians remained committed to providing care to these veterans and fighting to maintain the purpose of recovery-focused care.
Knowledge Gaps on Available Services
While many clinicians knew of general resources available to veterans experiencing homelessness, few had detailed information on where to seek consults for other homeless programs, who to contact regarding these services, when they were available, or how to refer to them. Many reported feeling uneasy when discharging veterans experiencing homelessness from care, often being unable to provide local, comprehensive referrals to support their needs and ensure their well-being. These sentiments were compounded when the veteran reported suicidal thoughts or recent suicidal behavior; clinicians felt concerned about the methods to engage these individuals into evidence-based mental health care within the context of unstable housing arrangements.
Some clinicians appeared to lack awareness of the wide array of VA homeless programming. Most could acknowledge at least some aspects of available programming (eg, the US Department of Housing and Urban Development– VA Supportive Housing program), while others were unaware of services tailored to the needs of those experiencing homelessness (eg, homeless patient aligned care teams), or of services targeting concurrent psychosocial stressors (eg, Veterans Justice Programs). Interviewees hypothesized this as being particularly notable among clinicians who are new to the VA or those who work in VA settings as part of their graduate or medical school training. Those aware of the services were uncertain of the referral process, relying on a single social worker or nurse to connect individuals experiencing homelessness to health and social services.
Interviewed clinicians noted that suicide risk screening of veterans experiencing homelessness was only performed by a limited number of individuals within the ED. Some did not feel sufficiently trained, comfortable, or knowledgeable about how to navigate care for veterans experiencing homelessness and at risk of suicide. Clinicians described “an uncomfortableness about suicidal ideation, where people just freeze up” and “don’t know what to do and don’t know what to say.”
Lack of Tangible Resources, Trainings, and Referrals
HCPs reported occasionally lacking the necessary clinical resources and information in the ED to properly support veterans experiencing homelessness and suicidal ideation. Common concerns included case management and discharge planning, as well as navigating health factors, such as elevated suicide risk. Some HCPs felt the local resources they do have access to—discharge packets or other forms of patient information—were not always tailored for the needs (eg, transportation) or abilities of veterans experiencing homelessness. One noted: “We give them a sheet of paper with some resources, which they don’t have the skills to follow up [with] anyway.”
Many interviewees wished for additional training in working with veterans experiencing homelessness. They reported that prior training from the VA Talent Management System or through unit-based programming could assist in educating clinicians on homeless services and suicide risk assessment. When queried on what training they had received, many noted there was “no formal training on what the VA offers homeless vets,” leading many to describe it as on-the-job training. This appeared especially among newer clinicians, who reported they were reliant upon learning from other, more senior staff within the ED.
The absence of training further illustrates the issue of institutional knowledge on these services and referrals, which was often confined to a single individual or team. Not having readily accessible resources, training, or information appropriate for all skill levels and positions within the ED hindered the ability of HCPs to connect veterans experiencing homelessness with social services to ensure their health and safety postdischarge: “If we had a better knowledge base of what the VA offers and the steps to go through in order to get the veteran set up for those things, it would be helpful.”
CLINICAL RESOURCE
A psychoeducational resource was developed for HCPs treating veterans experiencing homelessness (Figure). The resource was designed to mitigate compassion fatigue and recenter attention on the VA commitment to care while emphasizing the need to be responsive to the concerns of these individuals. Initial wireframes of the resource were developed by a small group of authors in review and appraisal of qualitative findings (EP, RH). These wireframes were developed to broadly illustrate the arrangement/structure of content, range of resources to potentially include (eg, available VA homeless programs or consultation resources), and to draft initial wording and phrasing. Subject matter expert feedback refined these wireframes, providing commentary on specific programs to include or exclude, changes and alterations to the design and flow of the resource, and edits to language, word choice, and tone over numerous iterations.
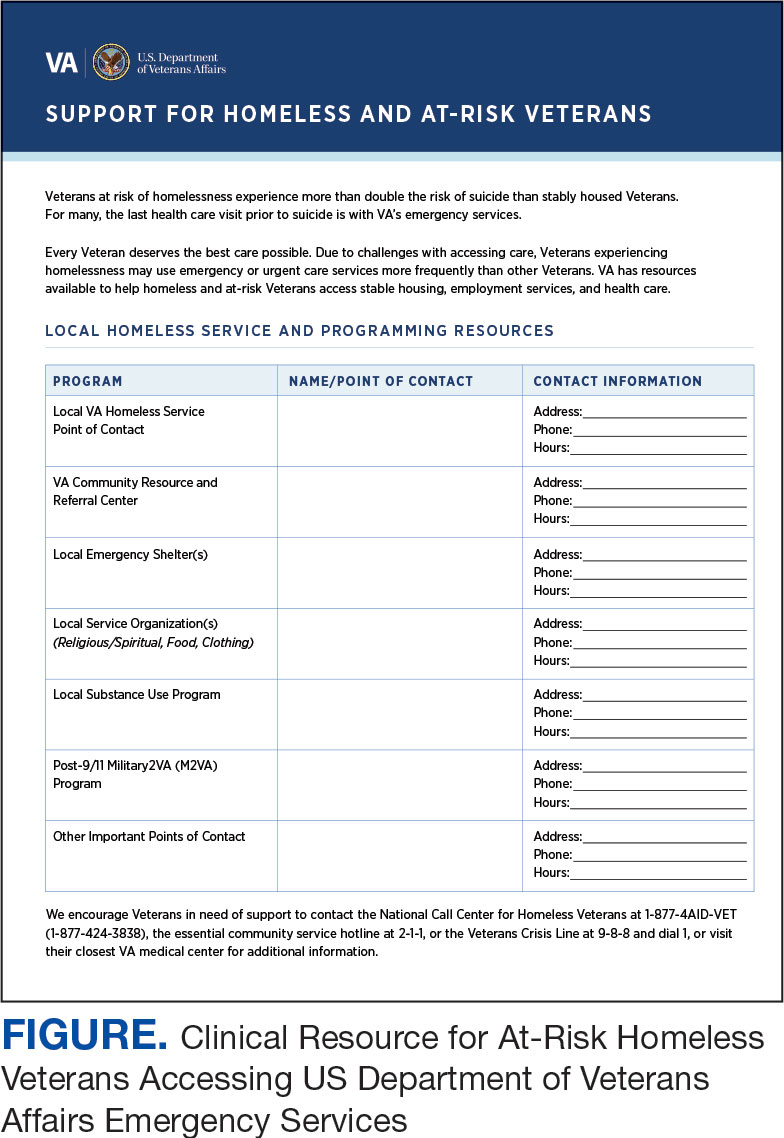
Given that many ED HCPs presented concerns surrounding secondary gain in the context of suicide risk, this resource focused on suicide risk. At the top of the resource, it states “Veterans at risk for homelessness experience more than double the risk for suicide than stably housed veterans.”23 Also at the top, the resource states: “For many, the last health care visit prior to suicide is often with VA emergency services."24 The goal of these statements was to educate users on the elevated risk for suicide in veterans experiencing homelessness and their role in preventing such deaths.
Text in this section emphasizes that every veteran deserves the best care possible and recenters HCP attention on providing quality, comprehensive care regardless of housing status. The inclusion of this material was prioritized given the concerns expressed regarding compassion fatigue and suspicions of secondary gain (eg, a veteran reporting suicidal ideation to attain shelter or respite from outside conditions).
The resource also attempts to address high rates of emergency service by veterans experiencing homelessness: “Due to challenges with accessing care, Veterans experiencing homelessness may use emergency or urgent care services more frequently than other Veterans.”25 The resource also indicates that VA resources are available to help homeless and at-risk veterans to acquire stable housing, employment, and engage in healthcare, which are outlined with specific contact information. Given the breadth of local and VA services, a portion of the resource is dedicated to local health and social services available for veterans experiencing homelessness. HCPs complete the first page, which is devoted to local homeless service and program resources.
Following SME consultation, the list of programs provided underwent a series of iterations. The program types listed are deemed to be of greatest benefit to veterans experiencing homelessness and most consulted by HCPs. Including VA and non-VA emergency shelters allows clinicians flexible options if a particular shelter is full, closed, or would not meet the veteran’s needs or preference (eg, lack of childcare or does not allow pets). The second column of this section is left intentionally blank; here, the HCP is to list a local point-of- contact at each program. This encourages clinical teams to seek out and make direct contact with these programs and establish (in)formal relationships with them. The HCP then completes the third column with contact information.
Once completed, the resource acts as a living document. Clinicians and SMEs consulted for this study expressed the desire to have an easily accessible resource that can be updated based on necessary changes (eg, emergency shelter address or hours of operation). The resource can be housed within each local VA emergency or urgent care service setting alongside other available clinical tools.
While local resources are the primary focus, interviewees also suggested that some HCPs are not aware of the available VA services . This material, found on the back of the resource, provides a general overview of services available through VA homeless programs. SME consultation and discussion led to selecting the 5 listed categories: housing services, health care services, case management, employment services, and justice-related programming, each with a brief description.
Information for the National Call Center for Homeless Veterans, community service hotline, and Veterans Crisis Line are included on the front page. These hotlines and phone numbers are always available for veterans experiencing homelessness, enabling them to make these connections themselves, if desired. Additionally, given the challenges noted by some HCPs in performing suicide risk screening, evaluation, and intervention, a prompt for the VA Suicide Risk Management Consultation service was also included on the back page.
Creating a Shared and Local Resource
This clinical resource was developed to establish a centralized, shared, local resource available to VA ED HCPs who lacked knowledge of available services or reported discomfort conducting suicide risk screening for veterans experiencing homelessness. In many cases, ED referrals to homeless programs and suicide prevention care was assigned to a single individual, often a nurse or social worker. As a result, an undue amount of work and strain was placed on these individuals, as this forced them to act as the sole bridge between care in the ED and postdischarge social (eg, homeless programs) and mental health (eg, suicide prevention) services. The creation of a unified, easily accessible document aimed to distribute this responsibility more equitably across ED staff.
DISCUSSION
This project intended to develop a clinician resource to support VA ED clinicians caring for veterans experiencing homelessness and their access to services postdischarge. Qualitative interviews provided insights into the burnout and compassion fatigue present in these settings, as well as the challenges and needs regarding knowledge of local and VA services. Emphasis was placed on leveraging extant resources and subject matter expertise to develop a resource capable of providing brief and informative guidance.
This resource is particularly relevant for HCPs new to the VA, including trainees and new hires, who may be less aware of VA and local social services. It has the potential to reduce the burden on VA ED staff to provide guidance and recommendations surrounding postdischarge social services. The resource acknowledges homeless programming focused on social determinants of health that can destabilize housing (eg, legal or occupational challenges). This can incentivize clinicians to discuss these programs with veterans to facilitate their ability to navigate complex health and psychosocial challenges.
HCPs interviewed for this study indicated their apprehension regarding suicide risk screening and evaluation, a process currently mandated within VA ED settings.26 This may be compounded among HCPs with minimal mental health training or those who have worked in community-based settings where such screening and evaluation efforts are not required. The resource reminds clinicians of available VA consultation services, which can provide additional training, clinical guidance, and review of existing local ED processes.
While the resource was directly informed by qualitative interviews conducted with VA emergency service HCPs and developed through an iterative process with SMEs, further research is necessary to determine its effectiveness at increasing access to health and social services among veterans experiencing homelessness. The resource has not been used by HCPs working in these settings to examine uptake or sustained use, nor clinicians’ perceptions of its utility, including acceptability and feasibility; these are important next steps to understand if the resource is functioning as intended.
Compassion fatigue, as well as associated sequelae (eg, burnout, distress, and psychiatric symptoms), is well-documented among individuals working with individuals experiencing homelessness, including VA HCPs.27-30 Such experiences are likely driven by several factors, including the clinical complexity and service needs of this veteran population. Although compassion fatigue was noted by many clinicians interviewed for this study, it is unclear if the resource alone would address factors driving compassion fatigue, or if additional programming or services may be necessary.
Limitations
The resource requires local HCPs to routinely update its content (eg, establishment of a new emergency shelter in the community or change in hours or contact information of an existing one), which may be challenging. This is especially true as it relates to community resources, which may be more likely to change than national VA programming.
This resource was initially developed following qualitative interviews with a small sample of VA HCPs (explicitly those working within ED settings) and may not be representative of all HCPs engaged in VA care with veterans experiencing homelessness. The perspectives and experiences of those interviewed do not represent the views of all VA ED HCPs and may differ from the perspectives of those in regions with unique cultural and regional considerations.31
Given that most of the interviewees were social workers in EDs engaged in care for veterans experiencing homelessness, these findings and informational needs may differ among other types of HCPs who provide services for veterans experiencing homelessness in other settings. Content in the resource was included based on clinician input, and may not reflect the perspectives of veterans, who may perceive some resources as more important (eg, access to primary care or dental services).28
CONCLUSIONS
This project represents the culmination of qualitative interviews and SME input to develop a free-to-use clinician resource to facilitate service delivery and connection to services following discharge from VA EDs for veterans experiencing homelessness. Serving as a template, this resource can be customized to increase knowledge of local VA and community resources to support these individuals. Continued refinement and piloting of this resource to evaluate acceptability, implementation barriers, and use remains warranted.
- Holliday R, Kinney AR, Smith AA, et al. A latent class analysis to identify subgroups of VHA using homeless veterans at greater risk for suicide mortality. J Affect Disord. 2022;315:162-167. doi:10.1016/j.jad.2022.07.062
- Weber J, Lee RC, Martsolf D. Understanding the health of veterans who are homeless: a review of the literature. Public Health Nurs. 2017;34(5):505-511. doi:10.1111/phn.12338
- Holliday R, Desai A, Stimmel M, Liu S, Monteith LL, Stewart KE. Meeting the health and social service needs of veterans who interact with the criminal justice system and experience homelessness: a holistic conceptualization and recommendations for tailoring care. Curr Treat Options Psychiatry. 2022;9(3):174-185. doi:10.1007/s40501-022-00275-1
- Holliday R, Desai A, Gerard G, Liu S, Stimmel M. Understanding the intersection of homelessness and justice involvement: enhancing veteran suicide prevention through VA programming. Fed Pract. 2022;39(1):8-11. doi:10.12788/fp.0216
- Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778-784. doi:10.2105/ajph.92.5.778
- Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(Suppl 2):S225-S231. doi:10.2105/AJPH.2013.301307
- Doran KM, Raven MC, Rosenheck RA. What drives frequent emergency department use in an integrated health system? National data from the Veterans Health Administration. Ann Emerg Med. 2013;62(2):151-159. doi:10.1016/j.annemergmed.2013.02.016
- Tsai J, Rosenheck RA. Risk factors for ED use among homeless veterans. Am J Emerg Med. 2013;31(5):855-858. doi:10.1016/j.ajem.2013.02.046
- Nelson RE, Suo Y, Pettey W, et al. Costs associated with health care services accessed through VA and in the community through Medicare for veterans experiencing homelessness. Health Serv Res. 2018;53(Suppl 3):5352-5374. doi:10.1111/1475-6773.13054
- Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi:10.1097/MLR.0000000000000112
- Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1- 6. doi:10.1027/0227-5910/a000001
- Decker H, Raguram M, Kanzaria HK, Duke M, Wick E. Provider perceptions of challenges and facilitators to surgical care in unhoused patients: a qualitative analysis. Surgery. 2024;175(4):1095-1102. doi:10.1016/j.surg.2023.11.009
- Panushka KA, Kozlowski Z, Dalessandro C, Sanders JN, Millar MM, Gawron LM. “It’s not a top priority”: a qualitative analysis of provider views on barriers to reproductive healthcare provision for homeless women in the United States. Soc Work Public Health. 2023;38(5 -8):428-436. doi:10.1080/19371918.2024.2315180
- Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893-1907. doi:10.1007/s11135-017-0574-8
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753-1760. doi:10.1177/1049732315617444
- Assarroudi A, Heshmati Nabavi F, Armat MR, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J Res Nurs. 2018;23(1):42-55. doi:10.1177/1744987117741667
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288.
- Goldsmith LJ. Using Framework Analysis in Applied Qualitative Research. Qual Rep. 2021;26(6):2061-2076. doi:10.46743/2160-3715/2021.5011
- Tufford L, Newman P. Bracketing in qualitative research. Qual Soc Work. 2012;11(1):80-96.
- Dodgson JE. Reflexivity in Qualitative Research. J Hum Lact. 2019;35(2):220-222. doi:10.1177/0890334419830990
- Hevner AR. A three cycle view of design science research. Scand J Inf Syst. 2007;19(2):4.
- Farao J, Malila B, Conrad N, Mutsvangwa T, Rangaka MX, Douglas TS. A user-centred design frame work for mHealth. PLOS ONE. 2020;15(8):e0237910. doi:10.1371/journal.pone.0237910
- Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481-498. doi:10.1111/sltb.12369
- Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1- 6. doi:10.1027/0227-5910/a000001
- Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and lowincome Veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi:10.1097/MLR.0000000000000112
- Holliday R, Hostetter T, Brenner LA, Bahraini N, Tsai J. Suicide risk screening and evaluation among patients accessing VHA services and identified as being newly homeless. Health Serv Res. 2024;59(5):e14301. doi:10.1111/1475-6773.14301
- Waegemakers Schiff J, Lane AM. PTSD symptoms, vicarious traumatization, and burnout in front line workers in the homeless sector. Community Ment Health J. 2019;55(3):454-462. doi:10.1007/s10597-018-00364-7
- Steenekamp BL, Barker SL. Exploring the experiences of compassion fatigue amongst peer support workers in homelessness services. Community Ment Health J. 2024;60(4):772-783. doi:10.1007/s10597-024-01234-1
- Perez S, Kerman N, Dej E, et al. When I can’t help, I suffer: a scoping review of moral distress in service providers working with persons experiencing homelessness. J Ment Health. Published online 2024:1-16. doi:10.1080/09638237.2024.2426986
- Monteith LL, Holliday R, Christe’An DI, Sherrill A, Brenner LA, Hoffmire CA. Suicide risk and prevention in Guam: clinical and research considerations and a call to action. Asian J Psychiatry. 2023;83:103546. doi:10.1016/j.ajp.2023.103546
- Surís A, Holliday R, Hooshyar D, et al. Development and implementation of a homeless mobile medical/mental veteran intervention. Fed Pract. 2017;34(9):18.
Veterans experiencing homelessness are at an elevated risk for adverse health outcomes, including suicide. This population also experiences chronic health conditions (eg, cardiovascular disease and sexually transmitted infections) and psychiatric conditions (eg, substance use disorders and posttraumatic stress disorder) with a greater propensity than veterans without history of homelessness.1,2 Similarly, veterans experiencing homelessness often report concurrent stressors, such as justice involvement and unemployment, which further impact social functioning.3
The US Department of Veterans Affairs (VA) offers a range of health and social services to veterans experiencing homelessness. These programs are designed to respond to the multifactorial challenges faced by this population and are aimed at achieving sustained, permanent housing.4 To facilitate this effort, these programs provide targeted and tailored health (eg, primary care) and social (eg, case management and vocational rehabilitation) services to address barriers to housing stability (eg, substance use, serious mental illness, interacting with the criminal legal system, and unemployment).
Despite the availability of these programs, engaging veterans in VA services—whether in general or tailored for those experiencing or at risk for homelessness—remains challenging. Many veterans at risk for or experiencing homelessness overuse service settings that provide immediate care, such as urgent care or emergency departments (EDs).5,6 These individuals often visit an ED to augment or complement medical care they received in an outpatient setting, which can result in an elevated health care burden as well as impacted provision of treatment, especially surrounding care for chronic conditions (eg, cardiovascular health or serious mental illness).7-9
VA EDs offer urgent care and emergency services and often serve as a point of entry for veterans experiencing homelessness.10 They offer veterans expedient access to care that can address immediate needs (eg, substance use withdrawal, pain management, and suicide risk). EDs may be easier to access given they have longer hours of operation and patients can present without a scheduled appointment. VA EDs are an important point to identify homelessness and connect individuals to social service resources and outpatient health care referrals (eg, primary care and mental health).4,11
Some clinicians experience uncertainty in navigating or providing care for veterans experiencing or at risk for homelessness. A qualitative study conducted outside the VA found many clinicians did not know how to approach clinical conversations among unstably housed individuals, particularly when they discussed how to manage care for complex health conditions in the context of ongoing case management challenges, such as discharge planning.12 Another study found that clinicians working with individuals experiencing homelessness may have limited prior training or experience treating these patients.13 As a result, these clinicians may be unaware of available social services or unknowingly have biases that negatively impact care. Research remains limited surrounding beliefs about and methods of enhancing care among VA clinicians working with veterans experiencing homelessness in the ED.
This multiphase pilot study sought to understand service delivery processes and gaps in VA ED settings. Phase 1 examined ED clinician perceptions of care, facilitators, and barriers to providing care (including suicide risk assessments) and making postdischarge outpatient referrals among VA ED clinicians who regularly work with veterans experiencing homelessness. Phase 2 used this information to develop a clinical psychoeducational resource to enhance post-ED access to care for veterans experiencing or at risk for homelessness.
QUALITATIVE INTERVIEWS
Semistructured qualitative interviews were conducted with 11 VA ED clinicians from 6 Veteran Integrated Service Networks between August 2022 and February 2023. Clinicians were eligible if they currently worked within a VA ED setting (including urgent care) and indicated that some of their patients were veterans experiencing homelessness. All health care practitioners (HCPs) participated in an interview and a postinterview self-report survey that assessed demographic and job-related characteristics. Eight HCPs identified as female and 3 identified as male. All clinicians identified as White and 3 as Hispanic or Latino. Eight clinicians were licensed clinical social workers, 2 were ED nurses, and 1 was an ED physician.
After each clinician provided informed consent, they were invited to complete a telephone or Microsoft Teams interview. All interviews were recorded and subsequently transcribed. Interviews explored clinicians’ experiences caring for veterans experiencing homelessness, with a focus on services provided within the ED, as well as mandated ED screenings such as a suicide risk assessment. Interview questions also addressed postdischarge knowledge and experiences with referrals to VA health services (eg, primary care, mental health) and social services (eg, housing programs). Interviews lasted 30 to 90 minutes.
Recruitment ended after attaining sufficient thematic data, accomplished via an information power approach to sampling. This occurred when the study aims, sample characteristics, existing theory, and depth and quality of interviews dynamically informed the decision to cease recruitment of additional participants.14,15 Given the scope of study (examining service delivery and knowledge gaps), the specificity of the targeted sample (VA ED clinicians providing care to veterans experiencing homelessness), the level of pre-existing theoretical background informing the study aims, and depth and quality of interview dialogue, this information power approach provides justification for attaining small sample sizes. Following the interview, HCPs completed a demographic questionnaire. Participants were not compensated.
Data Analysis
Directed content analysis was used to analyze qualitative data, with the framework method employed as an analytic instrument to facilitate analysis.16-18 Analysts engaged in bracketing and discussed reflexivity before data analysis to reflect on personal subjectivities and reduce potential bias.19,20
A prototype coding framework was developed that enabled coders to meaningfully summarize and condense data within transcripts into varying domains, categories, or topics found within the interview guide. Domain examples included clinical backgrounds, suicide risk and assessment protocols among veterans experiencing homelessness, beliefs about service delivery for veterans experiencing homelessness, and barriers and facilitators that may impact their ability to provide post-ED discharge care. Coders discussed the findings and if there was a need to modify templates. All transcripts were double coded. Once complete, individual templates were merged into a unified Microsoft Excel sheet, which allowed for more discrete analyses, enabling analysts to examine trends across content areas within the dataset.
Clinical Resource Development
HCPs were queried regarding available outpatient resources for post-ED care (eg, printed discharge paperwork and best practice alerts or automated workflows within the electronic health record). Resources used by participants were examined, as well as which resources clinicians thought would help them care for veterans experiencing homelessness. Noted gaps were used to develop a tailored resource for clinicians who treat veterans experiencing homelessness in the ED. This resource was created with the intention it could inform all ED clinicians, with the option for personalization to align with the needs of local services, based on needed content areas identified (eg, emergency shelters and suicide prevention resources).
Resource development followed an information systems research (ISR) framework that used a 3-pronged process of identifying circumstances for how a tool is developed, the problems it aims to address, and the knowledge that informs its development, implementation, and evaluation.21,22 Initial wireframes of the resource were provided via email to 10 subject matter experts (SMEs) in veteran suicide prevention, emergency medicine, and homeless programs. SMEs were identified via professional listservs, VA program office leadership, literature searches of similar research, and snowball sampling. Solicited feedback on the resource from the SMEs included its design, language, tone, flow, format, and content (ideation and prototyping). The feedback was collated and used to revise the resource. SMEs then reviewed and provided feedback on the revised resource. This iterative cycle (prototype review, commentary, ideation, prototype review) continued until the SMEs offered no additional edits to the resource. In total, 7 iterations of the resource were developed, critiqued, and revised.
INTERVIEW RESULTS
Compassion Fatigue
Many participants expressed concerns about compassion fatigue among VA ED clinicians. Those interviewed indicated that treating veterans experiencing homelessness sometimes led to the development of what they described as a “callus,” a “sixth sense,” or an inherent sense of “suspicion” or distrust. These feelings resulted from concerns about an individual’s secondary gain or potential hidden agenda (eg, a veteran reporting suicidal ideation to attain shelter on a cold night), with clinicians not wanting to feel as if they were taken advantage of or deceived.
Many clinicians noted that compassion fatigue resulted from witnessing the same veterans experiencing homelessness routinely use emergency services for nonemergent or nonmedical needs. Some also expressed that over time this may result in them becoming less empathetic when caring for veterans experiencing homelessness. They hypothesized that clinicians may experience burnout, which could potentially result in a lack of curiosity and concern about a veteran’s risk for suicide or need for social services. Others may “take things for granted,” leading them to discount stressors that are “very real to the patient, this person.”
Clinicians indicated that such sentiments may impact overall care. Potential negative consequences included stigmatization of veterans experiencing homelessness, incomplete or partial suicide risk screenings with this population, inattentive or impersonal care, and expedited discharge from the ED without appropriate safety planning or social service referrals. Clinicians interviewed intended to find ways to combat compassion fatigue and maintain a commitment to provide comprehensive care to all veterans, including those experiencing homelessness. They felt conflict between a lack of empathy for individuals experiencing homelessness and becoming numb to the problem due to overexposure. However, these clinicians remained committed to providing care to these veterans and fighting to maintain the purpose of recovery-focused care.
Knowledge Gaps on Available Services
While many clinicians knew of general resources available to veterans experiencing homelessness, few had detailed information on where to seek consults for other homeless programs, who to contact regarding these services, when they were available, or how to refer to them. Many reported feeling uneasy when discharging veterans experiencing homelessness from care, often being unable to provide local, comprehensive referrals to support their needs and ensure their well-being. These sentiments were compounded when the veteran reported suicidal thoughts or recent suicidal behavior; clinicians felt concerned about the methods to engage these individuals into evidence-based mental health care within the context of unstable housing arrangements.
Some clinicians appeared to lack awareness of the wide array of VA homeless programming. Most could acknowledge at least some aspects of available programming (eg, the US Department of Housing and Urban Development– VA Supportive Housing program), while others were unaware of services tailored to the needs of those experiencing homelessness (eg, homeless patient aligned care teams), or of services targeting concurrent psychosocial stressors (eg, Veterans Justice Programs). Interviewees hypothesized this as being particularly notable among clinicians who are new to the VA or those who work in VA settings as part of their graduate or medical school training. Those aware of the services were uncertain of the referral process, relying on a single social worker or nurse to connect individuals experiencing homelessness to health and social services.
Interviewed clinicians noted that suicide risk screening of veterans experiencing homelessness was only performed by a limited number of individuals within the ED. Some did not feel sufficiently trained, comfortable, or knowledgeable about how to navigate care for veterans experiencing homelessness and at risk of suicide. Clinicians described “an uncomfortableness about suicidal ideation, where people just freeze up” and “don’t know what to do and don’t know what to say.”
Lack of Tangible Resources, Trainings, and Referrals
HCPs reported occasionally lacking the necessary clinical resources and information in the ED to properly support veterans experiencing homelessness and suicidal ideation. Common concerns included case management and discharge planning, as well as navigating health factors, such as elevated suicide risk. Some HCPs felt the local resources they do have access to—discharge packets or other forms of patient information—were not always tailored for the needs (eg, transportation) or abilities of veterans experiencing homelessness. One noted: “We give them a sheet of paper with some resources, which they don’t have the skills to follow up [with] anyway.”
Many interviewees wished for additional training in working with veterans experiencing homelessness. They reported that prior training from the VA Talent Management System or through unit-based programming could assist in educating clinicians on homeless services and suicide risk assessment. When queried on what training they had received, many noted there was “no formal training on what the VA offers homeless vets,” leading many to describe it as on-the-job training. This appeared especially among newer clinicians, who reported they were reliant upon learning from other, more senior staff within the ED.
The absence of training further illustrates the issue of institutional knowledge on these services and referrals, which was often confined to a single individual or team. Not having readily accessible resources, training, or information appropriate for all skill levels and positions within the ED hindered the ability of HCPs to connect veterans experiencing homelessness with social services to ensure their health and safety postdischarge: “If we had a better knowledge base of what the VA offers and the steps to go through in order to get the veteran set up for those things, it would be helpful.”
CLINICAL RESOURCE
A psychoeducational resource was developed for HCPs treating veterans experiencing homelessness (Figure). The resource was designed to mitigate compassion fatigue and recenter attention on the VA commitment to care while emphasizing the need to be responsive to the concerns of these individuals. Initial wireframes of the resource were developed by a small group of authors in review and appraisal of qualitative findings (EP, RH). These wireframes were developed to broadly illustrate the arrangement/structure of content, range of resources to potentially include (eg, available VA homeless programs or consultation resources), and to draft initial wording and phrasing. Subject matter expert feedback refined these wireframes, providing commentary on specific programs to include or exclude, changes and alterations to the design and flow of the resource, and edits to language, word choice, and tone over numerous iterations.
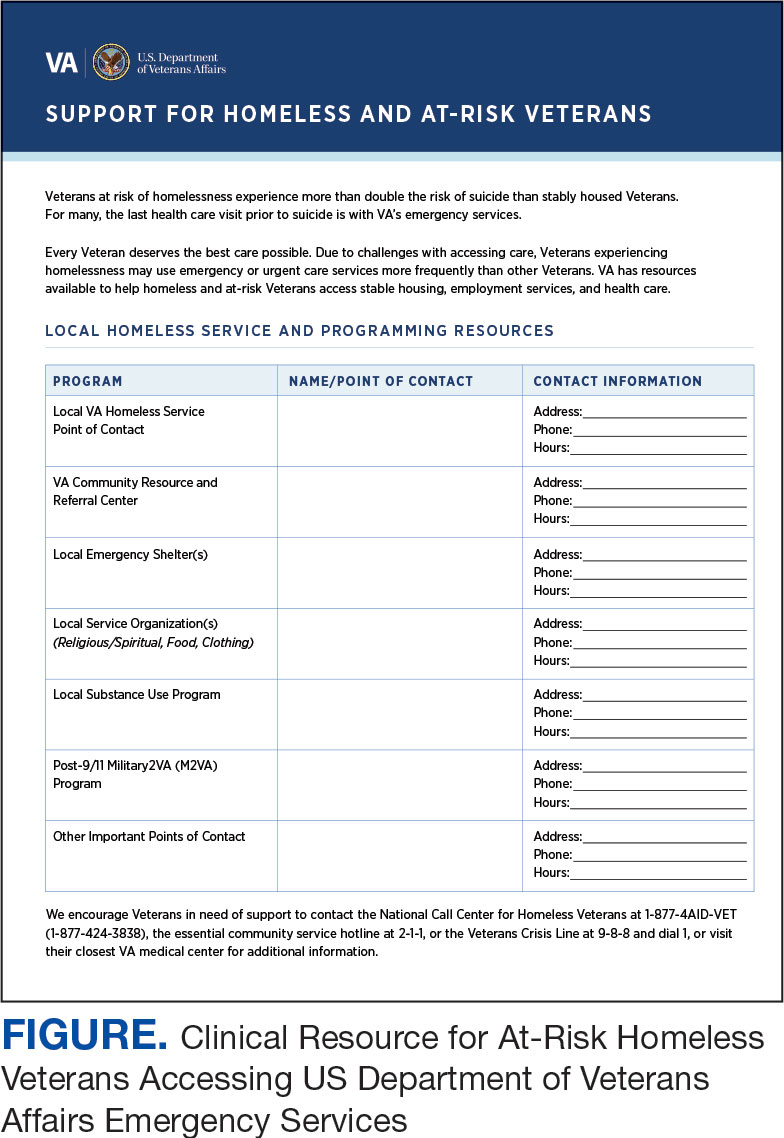
Given that many ED HCPs presented concerns surrounding secondary gain in the context of suicide risk, this resource focused on suicide risk. At the top of the resource, it states “Veterans at risk for homelessness experience more than double the risk for suicide than stably housed veterans.”23 Also at the top, the resource states: “For many, the last health care visit prior to suicide is often with VA emergency services."24 The goal of these statements was to educate users on the elevated risk for suicide in veterans experiencing homelessness and their role in preventing such deaths.
Text in this section emphasizes that every veteran deserves the best care possible and recenters HCP attention on providing quality, comprehensive care regardless of housing status. The inclusion of this material was prioritized given the concerns expressed regarding compassion fatigue and suspicions of secondary gain (eg, a veteran reporting suicidal ideation to attain shelter or respite from outside conditions).
The resource also attempts to address high rates of emergency service by veterans experiencing homelessness: “Due to challenges with accessing care, Veterans experiencing homelessness may use emergency or urgent care services more frequently than other Veterans.”25 The resource also indicates that VA resources are available to help homeless and at-risk veterans to acquire stable housing, employment, and engage in healthcare, which are outlined with specific contact information. Given the breadth of local and VA services, a portion of the resource is dedicated to local health and social services available for veterans experiencing homelessness. HCPs complete the first page, which is devoted to local homeless service and program resources.
Following SME consultation, the list of programs provided underwent a series of iterations. The program types listed are deemed to be of greatest benefit to veterans experiencing homelessness and most consulted by HCPs. Including VA and non-VA emergency shelters allows clinicians flexible options if a particular shelter is full, closed, or would not meet the veteran’s needs or preference (eg, lack of childcare or does not allow pets). The second column of this section is left intentionally blank; here, the HCP is to list a local point-of- contact at each program. This encourages clinical teams to seek out and make direct contact with these programs and establish (in)formal relationships with them. The HCP then completes the third column with contact information.
Once completed, the resource acts as a living document. Clinicians and SMEs consulted for this study expressed the desire to have an easily accessible resource that can be updated based on necessary changes (eg, emergency shelter address or hours of operation). The resource can be housed within each local VA emergency or urgent care service setting alongside other available clinical tools.
While local resources are the primary focus, interviewees also suggested that some HCPs are not aware of the available VA services . This material, found on the back of the resource, provides a general overview of services available through VA homeless programs. SME consultation and discussion led to selecting the 5 listed categories: housing services, health care services, case management, employment services, and justice-related programming, each with a brief description.
Information for the National Call Center for Homeless Veterans, community service hotline, and Veterans Crisis Line are included on the front page. These hotlines and phone numbers are always available for veterans experiencing homelessness, enabling them to make these connections themselves, if desired. Additionally, given the challenges noted by some HCPs in performing suicide risk screening, evaluation, and intervention, a prompt for the VA Suicide Risk Management Consultation service was also included on the back page.
Creating a Shared and Local Resource
This clinical resource was developed to establish a centralized, shared, local resource available to VA ED HCPs who lacked knowledge of available services or reported discomfort conducting suicide risk screening for veterans experiencing homelessness. In many cases, ED referrals to homeless programs and suicide prevention care was assigned to a single individual, often a nurse or social worker. As a result, an undue amount of work and strain was placed on these individuals, as this forced them to act as the sole bridge between care in the ED and postdischarge social (eg, homeless programs) and mental health (eg, suicide prevention) services. The creation of a unified, easily accessible document aimed to distribute this responsibility more equitably across ED staff.
DISCUSSION
This project intended to develop a clinician resource to support VA ED clinicians caring for veterans experiencing homelessness and their access to services postdischarge. Qualitative interviews provided insights into the burnout and compassion fatigue present in these settings, as well as the challenges and needs regarding knowledge of local and VA services. Emphasis was placed on leveraging extant resources and subject matter expertise to develop a resource capable of providing brief and informative guidance.
This resource is particularly relevant for HCPs new to the VA, including trainees and new hires, who may be less aware of VA and local social services. It has the potential to reduce the burden on VA ED staff to provide guidance and recommendations surrounding postdischarge social services. The resource acknowledges homeless programming focused on social determinants of health that can destabilize housing (eg, legal or occupational challenges). This can incentivize clinicians to discuss these programs with veterans to facilitate their ability to navigate complex health and psychosocial challenges.
HCPs interviewed for this study indicated their apprehension regarding suicide risk screening and evaluation, a process currently mandated within VA ED settings.26 This may be compounded among HCPs with minimal mental health training or those who have worked in community-based settings where such screening and evaluation efforts are not required. The resource reminds clinicians of available VA consultation services, which can provide additional training, clinical guidance, and review of existing local ED processes.
While the resource was directly informed by qualitative interviews conducted with VA emergency service HCPs and developed through an iterative process with SMEs, further research is necessary to determine its effectiveness at increasing access to health and social services among veterans experiencing homelessness. The resource has not been used by HCPs working in these settings to examine uptake or sustained use, nor clinicians’ perceptions of its utility, including acceptability and feasibility; these are important next steps to understand if the resource is functioning as intended.
Compassion fatigue, as well as associated sequelae (eg, burnout, distress, and psychiatric symptoms), is well-documented among individuals working with individuals experiencing homelessness, including VA HCPs.27-30 Such experiences are likely driven by several factors, including the clinical complexity and service needs of this veteran population. Although compassion fatigue was noted by many clinicians interviewed for this study, it is unclear if the resource alone would address factors driving compassion fatigue, or if additional programming or services may be necessary.
Limitations
The resource requires local HCPs to routinely update its content (eg, establishment of a new emergency shelter in the community or change in hours or contact information of an existing one), which may be challenging. This is especially true as it relates to community resources, which may be more likely to change than national VA programming.
This resource was initially developed following qualitative interviews with a small sample of VA HCPs (explicitly those working within ED settings) and may not be representative of all HCPs engaged in VA care with veterans experiencing homelessness. The perspectives and experiences of those interviewed do not represent the views of all VA ED HCPs and may differ from the perspectives of those in regions with unique cultural and regional considerations.31
Given that most of the interviewees were social workers in EDs engaged in care for veterans experiencing homelessness, these findings and informational needs may differ among other types of HCPs who provide services for veterans experiencing homelessness in other settings. Content in the resource was included based on clinician input, and may not reflect the perspectives of veterans, who may perceive some resources as more important (eg, access to primary care or dental services).28
CONCLUSIONS
This project represents the culmination of qualitative interviews and SME input to develop a free-to-use clinician resource to facilitate service delivery and connection to services following discharge from VA EDs for veterans experiencing homelessness. Serving as a template, this resource can be customized to increase knowledge of local VA and community resources to support these individuals. Continued refinement and piloting of this resource to evaluate acceptability, implementation barriers, and use remains warranted.
Veterans experiencing homelessness are at an elevated risk for adverse health outcomes, including suicide. This population also experiences chronic health conditions (eg, cardiovascular disease and sexually transmitted infections) and psychiatric conditions (eg, substance use disorders and posttraumatic stress disorder) with a greater propensity than veterans without history of homelessness.1,2 Similarly, veterans experiencing homelessness often report concurrent stressors, such as justice involvement and unemployment, which further impact social functioning.3
The US Department of Veterans Affairs (VA) offers a range of health and social services to veterans experiencing homelessness. These programs are designed to respond to the multifactorial challenges faced by this population and are aimed at achieving sustained, permanent housing.4 To facilitate this effort, these programs provide targeted and tailored health (eg, primary care) and social (eg, case management and vocational rehabilitation) services to address barriers to housing stability (eg, substance use, serious mental illness, interacting with the criminal legal system, and unemployment).
Despite the availability of these programs, engaging veterans in VA services—whether in general or tailored for those experiencing or at risk for homelessness—remains challenging. Many veterans at risk for or experiencing homelessness overuse service settings that provide immediate care, such as urgent care or emergency departments (EDs).5,6 These individuals often visit an ED to augment or complement medical care they received in an outpatient setting, which can result in an elevated health care burden as well as impacted provision of treatment, especially surrounding care for chronic conditions (eg, cardiovascular health or serious mental illness).7-9
VA EDs offer urgent care and emergency services and often serve as a point of entry for veterans experiencing homelessness.10 They offer veterans expedient access to care that can address immediate needs (eg, substance use withdrawal, pain management, and suicide risk). EDs may be easier to access given they have longer hours of operation and patients can present without a scheduled appointment. VA EDs are an important point to identify homelessness and connect individuals to social service resources and outpatient health care referrals (eg, primary care and mental health).4,11
Some clinicians experience uncertainty in navigating or providing care for veterans experiencing or at risk for homelessness. A qualitative study conducted outside the VA found many clinicians did not know how to approach clinical conversations among unstably housed individuals, particularly when they discussed how to manage care for complex health conditions in the context of ongoing case management challenges, such as discharge planning.12 Another study found that clinicians working with individuals experiencing homelessness may have limited prior training or experience treating these patients.13 As a result, these clinicians may be unaware of available social services or unknowingly have biases that negatively impact care. Research remains limited surrounding beliefs about and methods of enhancing care among VA clinicians working with veterans experiencing homelessness in the ED.
This multiphase pilot study sought to understand service delivery processes and gaps in VA ED settings. Phase 1 examined ED clinician perceptions of care, facilitators, and barriers to providing care (including suicide risk assessments) and making postdischarge outpatient referrals among VA ED clinicians who regularly work with veterans experiencing homelessness. Phase 2 used this information to develop a clinical psychoeducational resource to enhance post-ED access to care for veterans experiencing or at risk for homelessness.
QUALITATIVE INTERVIEWS
Semistructured qualitative interviews were conducted with 11 VA ED clinicians from 6 Veteran Integrated Service Networks between August 2022 and February 2023. Clinicians were eligible if they currently worked within a VA ED setting (including urgent care) and indicated that some of their patients were veterans experiencing homelessness. All health care practitioners (HCPs) participated in an interview and a postinterview self-report survey that assessed demographic and job-related characteristics. Eight HCPs identified as female and 3 identified as male. All clinicians identified as White and 3 as Hispanic or Latino. Eight clinicians were licensed clinical social workers, 2 were ED nurses, and 1 was an ED physician.
After each clinician provided informed consent, they were invited to complete a telephone or Microsoft Teams interview. All interviews were recorded and subsequently transcribed. Interviews explored clinicians’ experiences caring for veterans experiencing homelessness, with a focus on services provided within the ED, as well as mandated ED screenings such as a suicide risk assessment. Interview questions also addressed postdischarge knowledge and experiences with referrals to VA health services (eg, primary care, mental health) and social services (eg, housing programs). Interviews lasted 30 to 90 minutes.
Recruitment ended after attaining sufficient thematic data, accomplished via an information power approach to sampling. This occurred when the study aims, sample characteristics, existing theory, and depth and quality of interviews dynamically informed the decision to cease recruitment of additional participants.14,15 Given the scope of study (examining service delivery and knowledge gaps), the specificity of the targeted sample (VA ED clinicians providing care to veterans experiencing homelessness), the level of pre-existing theoretical background informing the study aims, and depth and quality of interview dialogue, this information power approach provides justification for attaining small sample sizes. Following the interview, HCPs completed a demographic questionnaire. Participants were not compensated.
Data Analysis
Directed content analysis was used to analyze qualitative data, with the framework method employed as an analytic instrument to facilitate analysis.16-18 Analysts engaged in bracketing and discussed reflexivity before data analysis to reflect on personal subjectivities and reduce potential bias.19,20
A prototype coding framework was developed that enabled coders to meaningfully summarize and condense data within transcripts into varying domains, categories, or topics found within the interview guide. Domain examples included clinical backgrounds, suicide risk and assessment protocols among veterans experiencing homelessness, beliefs about service delivery for veterans experiencing homelessness, and barriers and facilitators that may impact their ability to provide post-ED discharge care. Coders discussed the findings and if there was a need to modify templates. All transcripts were double coded. Once complete, individual templates were merged into a unified Microsoft Excel sheet, which allowed for more discrete analyses, enabling analysts to examine trends across content areas within the dataset.
Clinical Resource Development
HCPs were queried regarding available outpatient resources for post-ED care (eg, printed discharge paperwork and best practice alerts or automated workflows within the electronic health record). Resources used by participants were examined, as well as which resources clinicians thought would help them care for veterans experiencing homelessness. Noted gaps were used to develop a tailored resource for clinicians who treat veterans experiencing homelessness in the ED. This resource was created with the intention it could inform all ED clinicians, with the option for personalization to align with the needs of local services, based on needed content areas identified (eg, emergency shelters and suicide prevention resources).
Resource development followed an information systems research (ISR) framework that used a 3-pronged process of identifying circumstances for how a tool is developed, the problems it aims to address, and the knowledge that informs its development, implementation, and evaluation.21,22 Initial wireframes of the resource were provided via email to 10 subject matter experts (SMEs) in veteran suicide prevention, emergency medicine, and homeless programs. SMEs were identified via professional listservs, VA program office leadership, literature searches of similar research, and snowball sampling. Solicited feedback on the resource from the SMEs included its design, language, tone, flow, format, and content (ideation and prototyping). The feedback was collated and used to revise the resource. SMEs then reviewed and provided feedback on the revised resource. This iterative cycle (prototype review, commentary, ideation, prototype review) continued until the SMEs offered no additional edits to the resource. In total, 7 iterations of the resource were developed, critiqued, and revised.
INTERVIEW RESULTS
Compassion Fatigue
Many participants expressed concerns about compassion fatigue among VA ED clinicians. Those interviewed indicated that treating veterans experiencing homelessness sometimes led to the development of what they described as a “callus,” a “sixth sense,” or an inherent sense of “suspicion” or distrust. These feelings resulted from concerns about an individual’s secondary gain or potential hidden agenda (eg, a veteran reporting suicidal ideation to attain shelter on a cold night), with clinicians not wanting to feel as if they were taken advantage of or deceived.
Many clinicians noted that compassion fatigue resulted from witnessing the same veterans experiencing homelessness routinely use emergency services for nonemergent or nonmedical needs. Some also expressed that over time this may result in them becoming less empathetic when caring for veterans experiencing homelessness. They hypothesized that clinicians may experience burnout, which could potentially result in a lack of curiosity and concern about a veteran’s risk for suicide or need for social services. Others may “take things for granted,” leading them to discount stressors that are “very real to the patient, this person.”
Clinicians indicated that such sentiments may impact overall care. Potential negative consequences included stigmatization of veterans experiencing homelessness, incomplete or partial suicide risk screenings with this population, inattentive or impersonal care, and expedited discharge from the ED without appropriate safety planning or social service referrals. Clinicians interviewed intended to find ways to combat compassion fatigue and maintain a commitment to provide comprehensive care to all veterans, including those experiencing homelessness. They felt conflict between a lack of empathy for individuals experiencing homelessness and becoming numb to the problem due to overexposure. However, these clinicians remained committed to providing care to these veterans and fighting to maintain the purpose of recovery-focused care.
Knowledge Gaps on Available Services
While many clinicians knew of general resources available to veterans experiencing homelessness, few had detailed information on where to seek consults for other homeless programs, who to contact regarding these services, when they were available, or how to refer to them. Many reported feeling uneasy when discharging veterans experiencing homelessness from care, often being unable to provide local, comprehensive referrals to support their needs and ensure their well-being. These sentiments were compounded when the veteran reported suicidal thoughts or recent suicidal behavior; clinicians felt concerned about the methods to engage these individuals into evidence-based mental health care within the context of unstable housing arrangements.
Some clinicians appeared to lack awareness of the wide array of VA homeless programming. Most could acknowledge at least some aspects of available programming (eg, the US Department of Housing and Urban Development– VA Supportive Housing program), while others were unaware of services tailored to the needs of those experiencing homelessness (eg, homeless patient aligned care teams), or of services targeting concurrent psychosocial stressors (eg, Veterans Justice Programs). Interviewees hypothesized this as being particularly notable among clinicians who are new to the VA or those who work in VA settings as part of their graduate or medical school training. Those aware of the services were uncertain of the referral process, relying on a single social worker or nurse to connect individuals experiencing homelessness to health and social services.
Interviewed clinicians noted that suicide risk screening of veterans experiencing homelessness was only performed by a limited number of individuals within the ED. Some did not feel sufficiently trained, comfortable, or knowledgeable about how to navigate care for veterans experiencing homelessness and at risk of suicide. Clinicians described “an uncomfortableness about suicidal ideation, where people just freeze up” and “don’t know what to do and don’t know what to say.”
Lack of Tangible Resources, Trainings, and Referrals
HCPs reported occasionally lacking the necessary clinical resources and information in the ED to properly support veterans experiencing homelessness and suicidal ideation. Common concerns included case management and discharge planning, as well as navigating health factors, such as elevated suicide risk. Some HCPs felt the local resources they do have access to—discharge packets or other forms of patient information—were not always tailored for the needs (eg, transportation) or abilities of veterans experiencing homelessness. One noted: “We give them a sheet of paper with some resources, which they don’t have the skills to follow up [with] anyway.”
Many interviewees wished for additional training in working with veterans experiencing homelessness. They reported that prior training from the VA Talent Management System or through unit-based programming could assist in educating clinicians on homeless services and suicide risk assessment. When queried on what training they had received, many noted there was “no formal training on what the VA offers homeless vets,” leading many to describe it as on-the-job training. This appeared especially among newer clinicians, who reported they were reliant upon learning from other, more senior staff within the ED.
The absence of training further illustrates the issue of institutional knowledge on these services and referrals, which was often confined to a single individual or team. Not having readily accessible resources, training, or information appropriate for all skill levels and positions within the ED hindered the ability of HCPs to connect veterans experiencing homelessness with social services to ensure their health and safety postdischarge: “If we had a better knowledge base of what the VA offers and the steps to go through in order to get the veteran set up for those things, it would be helpful.”
CLINICAL RESOURCE
A psychoeducational resource was developed for HCPs treating veterans experiencing homelessness (Figure). The resource was designed to mitigate compassion fatigue and recenter attention on the VA commitment to care while emphasizing the need to be responsive to the concerns of these individuals. Initial wireframes of the resource were developed by a small group of authors in review and appraisal of qualitative findings (EP, RH). These wireframes were developed to broadly illustrate the arrangement/structure of content, range of resources to potentially include (eg, available VA homeless programs or consultation resources), and to draft initial wording and phrasing. Subject matter expert feedback refined these wireframes, providing commentary on specific programs to include or exclude, changes and alterations to the design and flow of the resource, and edits to language, word choice, and tone over numerous iterations.
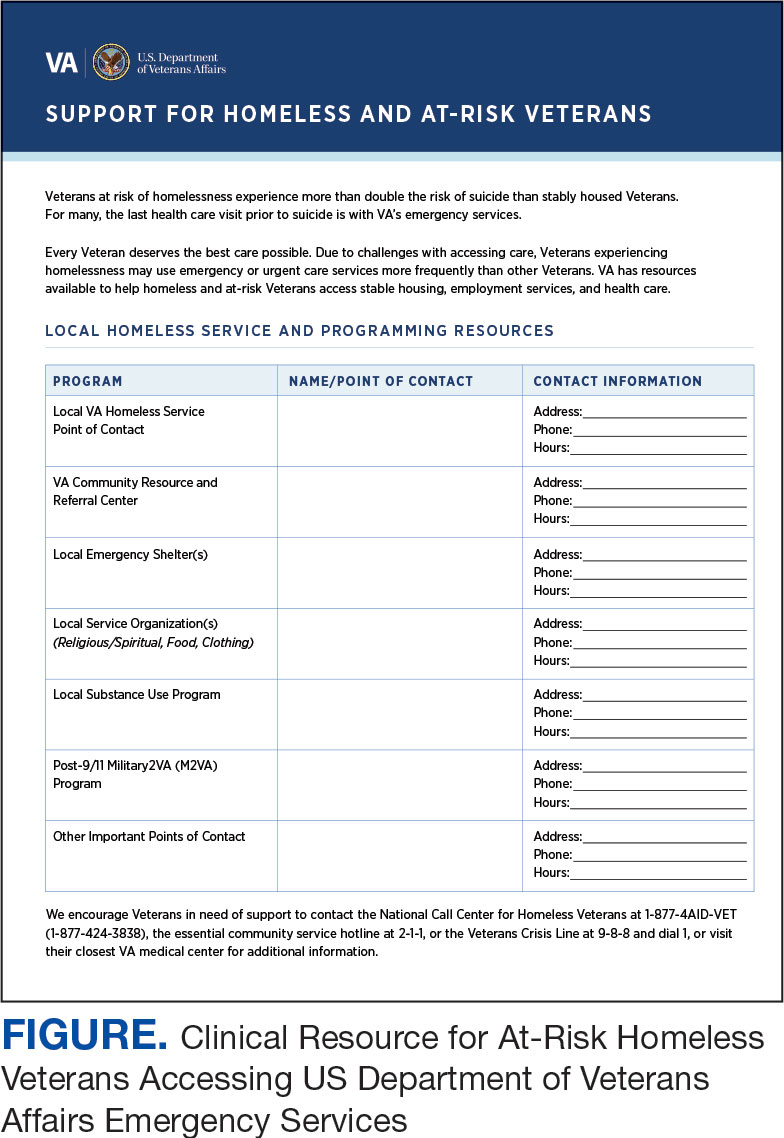
Given that many ED HCPs presented concerns surrounding secondary gain in the context of suicide risk, this resource focused on suicide risk. At the top of the resource, it states “Veterans at risk for homelessness experience more than double the risk for suicide than stably housed veterans.”23 Also at the top, the resource states: “For many, the last health care visit prior to suicide is often with VA emergency services."24 The goal of these statements was to educate users on the elevated risk for suicide in veterans experiencing homelessness and their role in preventing such deaths.
Text in this section emphasizes that every veteran deserves the best care possible and recenters HCP attention on providing quality, comprehensive care regardless of housing status. The inclusion of this material was prioritized given the concerns expressed regarding compassion fatigue and suspicions of secondary gain (eg, a veteran reporting suicidal ideation to attain shelter or respite from outside conditions).
The resource also attempts to address high rates of emergency service by veterans experiencing homelessness: “Due to challenges with accessing care, Veterans experiencing homelessness may use emergency or urgent care services more frequently than other Veterans.”25 The resource also indicates that VA resources are available to help homeless and at-risk veterans to acquire stable housing, employment, and engage in healthcare, which are outlined with specific contact information. Given the breadth of local and VA services, a portion of the resource is dedicated to local health and social services available for veterans experiencing homelessness. HCPs complete the first page, which is devoted to local homeless service and program resources.
Following SME consultation, the list of programs provided underwent a series of iterations. The program types listed are deemed to be of greatest benefit to veterans experiencing homelessness and most consulted by HCPs. Including VA and non-VA emergency shelters allows clinicians flexible options if a particular shelter is full, closed, or would not meet the veteran’s needs or preference (eg, lack of childcare or does not allow pets). The second column of this section is left intentionally blank; here, the HCP is to list a local point-of- contact at each program. This encourages clinical teams to seek out and make direct contact with these programs and establish (in)formal relationships with them. The HCP then completes the third column with contact information.
Once completed, the resource acts as a living document. Clinicians and SMEs consulted for this study expressed the desire to have an easily accessible resource that can be updated based on necessary changes (eg, emergency shelter address or hours of operation). The resource can be housed within each local VA emergency or urgent care service setting alongside other available clinical tools.
While local resources are the primary focus, interviewees also suggested that some HCPs are not aware of the available VA services . This material, found on the back of the resource, provides a general overview of services available through VA homeless programs. SME consultation and discussion led to selecting the 5 listed categories: housing services, health care services, case management, employment services, and justice-related programming, each with a brief description.
Information for the National Call Center for Homeless Veterans, community service hotline, and Veterans Crisis Line are included on the front page. These hotlines and phone numbers are always available for veterans experiencing homelessness, enabling them to make these connections themselves, if desired. Additionally, given the challenges noted by some HCPs in performing suicide risk screening, evaluation, and intervention, a prompt for the VA Suicide Risk Management Consultation service was also included on the back page.
Creating a Shared and Local Resource
This clinical resource was developed to establish a centralized, shared, local resource available to VA ED HCPs who lacked knowledge of available services or reported discomfort conducting suicide risk screening for veterans experiencing homelessness. In many cases, ED referrals to homeless programs and suicide prevention care was assigned to a single individual, often a nurse or social worker. As a result, an undue amount of work and strain was placed on these individuals, as this forced them to act as the sole bridge between care in the ED and postdischarge social (eg, homeless programs) and mental health (eg, suicide prevention) services. The creation of a unified, easily accessible document aimed to distribute this responsibility more equitably across ED staff.
DISCUSSION
This project intended to develop a clinician resource to support VA ED clinicians caring for veterans experiencing homelessness and their access to services postdischarge. Qualitative interviews provided insights into the burnout and compassion fatigue present in these settings, as well as the challenges and needs regarding knowledge of local and VA services. Emphasis was placed on leveraging extant resources and subject matter expertise to develop a resource capable of providing brief and informative guidance.
This resource is particularly relevant for HCPs new to the VA, including trainees and new hires, who may be less aware of VA and local social services. It has the potential to reduce the burden on VA ED staff to provide guidance and recommendations surrounding postdischarge social services. The resource acknowledges homeless programming focused on social determinants of health that can destabilize housing (eg, legal or occupational challenges). This can incentivize clinicians to discuss these programs with veterans to facilitate their ability to navigate complex health and psychosocial challenges.
HCPs interviewed for this study indicated their apprehension regarding suicide risk screening and evaluation, a process currently mandated within VA ED settings.26 This may be compounded among HCPs with minimal mental health training or those who have worked in community-based settings where such screening and evaluation efforts are not required. The resource reminds clinicians of available VA consultation services, which can provide additional training, clinical guidance, and review of existing local ED processes.
While the resource was directly informed by qualitative interviews conducted with VA emergency service HCPs and developed through an iterative process with SMEs, further research is necessary to determine its effectiveness at increasing access to health and social services among veterans experiencing homelessness. The resource has not been used by HCPs working in these settings to examine uptake or sustained use, nor clinicians’ perceptions of its utility, including acceptability and feasibility; these are important next steps to understand if the resource is functioning as intended.
Compassion fatigue, as well as associated sequelae (eg, burnout, distress, and psychiatric symptoms), is well-documented among individuals working with individuals experiencing homelessness, including VA HCPs.27-30 Such experiences are likely driven by several factors, including the clinical complexity and service needs of this veteran population. Although compassion fatigue was noted by many clinicians interviewed for this study, it is unclear if the resource alone would address factors driving compassion fatigue, or if additional programming or services may be necessary.
Limitations
The resource requires local HCPs to routinely update its content (eg, establishment of a new emergency shelter in the community or change in hours or contact information of an existing one), which may be challenging. This is especially true as it relates to community resources, which may be more likely to change than national VA programming.
This resource was initially developed following qualitative interviews with a small sample of VA HCPs (explicitly those working within ED settings) and may not be representative of all HCPs engaged in VA care with veterans experiencing homelessness. The perspectives and experiences of those interviewed do not represent the views of all VA ED HCPs and may differ from the perspectives of those in regions with unique cultural and regional considerations.31
Given that most of the interviewees were social workers in EDs engaged in care for veterans experiencing homelessness, these findings and informational needs may differ among other types of HCPs who provide services for veterans experiencing homelessness in other settings. Content in the resource was included based on clinician input, and may not reflect the perspectives of veterans, who may perceive some resources as more important (eg, access to primary care or dental services).28
CONCLUSIONS
This project represents the culmination of qualitative interviews and SME input to develop a free-to-use clinician resource to facilitate service delivery and connection to services following discharge from VA EDs for veterans experiencing homelessness. Serving as a template, this resource can be customized to increase knowledge of local VA and community resources to support these individuals. Continued refinement and piloting of this resource to evaluate acceptability, implementation barriers, and use remains warranted.
- Holliday R, Kinney AR, Smith AA, et al. A latent class analysis to identify subgroups of VHA using homeless veterans at greater risk for suicide mortality. J Affect Disord. 2022;315:162-167. doi:10.1016/j.jad.2022.07.062
- Weber J, Lee RC, Martsolf D. Understanding the health of veterans who are homeless: a review of the literature. Public Health Nurs. 2017;34(5):505-511. doi:10.1111/phn.12338
- Holliday R, Desai A, Stimmel M, Liu S, Monteith LL, Stewart KE. Meeting the health and social service needs of veterans who interact with the criminal justice system and experience homelessness: a holistic conceptualization and recommendations for tailoring care. Curr Treat Options Psychiatry. 2022;9(3):174-185. doi:10.1007/s40501-022-00275-1
- Holliday R, Desai A, Gerard G, Liu S, Stimmel M. Understanding the intersection of homelessness and justice involvement: enhancing veteran suicide prevention through VA programming. Fed Pract. 2022;39(1):8-11. doi:10.12788/fp.0216
- Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778-784. doi:10.2105/ajph.92.5.778
- Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(Suppl 2):S225-S231. doi:10.2105/AJPH.2013.301307
- Doran KM, Raven MC, Rosenheck RA. What drives frequent emergency department use in an integrated health system? National data from the Veterans Health Administration. Ann Emerg Med. 2013;62(2):151-159. doi:10.1016/j.annemergmed.2013.02.016
- Tsai J, Rosenheck RA. Risk factors for ED use among homeless veterans. Am J Emerg Med. 2013;31(5):855-858. doi:10.1016/j.ajem.2013.02.046
- Nelson RE, Suo Y, Pettey W, et al. Costs associated with health care services accessed through VA and in the community through Medicare for veterans experiencing homelessness. Health Serv Res. 2018;53(Suppl 3):5352-5374. doi:10.1111/1475-6773.13054
- Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi:10.1097/MLR.0000000000000112
- Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1- 6. doi:10.1027/0227-5910/a000001
- Decker H, Raguram M, Kanzaria HK, Duke M, Wick E. Provider perceptions of challenges and facilitators to surgical care in unhoused patients: a qualitative analysis. Surgery. 2024;175(4):1095-1102. doi:10.1016/j.surg.2023.11.009
- Panushka KA, Kozlowski Z, Dalessandro C, Sanders JN, Millar MM, Gawron LM. “It’s not a top priority”: a qualitative analysis of provider views on barriers to reproductive healthcare provision for homeless women in the United States. Soc Work Public Health. 2023;38(5 -8):428-436. doi:10.1080/19371918.2024.2315180
- Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893-1907. doi:10.1007/s11135-017-0574-8
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753-1760. doi:10.1177/1049732315617444
- Assarroudi A, Heshmati Nabavi F, Armat MR, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J Res Nurs. 2018;23(1):42-55. doi:10.1177/1744987117741667
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288.
- Goldsmith LJ. Using Framework Analysis in Applied Qualitative Research. Qual Rep. 2021;26(6):2061-2076. doi:10.46743/2160-3715/2021.5011
- Tufford L, Newman P. Bracketing in qualitative research. Qual Soc Work. 2012;11(1):80-96.
- Dodgson JE. Reflexivity in Qualitative Research. J Hum Lact. 2019;35(2):220-222. doi:10.1177/0890334419830990
- Hevner AR. A three cycle view of design science research. Scand J Inf Syst. 2007;19(2):4.
- Farao J, Malila B, Conrad N, Mutsvangwa T, Rangaka MX, Douglas TS. A user-centred design frame work for mHealth. PLOS ONE. 2020;15(8):e0237910. doi:10.1371/journal.pone.0237910
- Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481-498. doi:10.1111/sltb.12369
- Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1- 6. doi:10.1027/0227-5910/a000001
- Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and lowincome Veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi:10.1097/MLR.0000000000000112
- Holliday R, Hostetter T, Brenner LA, Bahraini N, Tsai J. Suicide risk screening and evaluation among patients accessing VHA services and identified as being newly homeless. Health Serv Res. 2024;59(5):e14301. doi:10.1111/1475-6773.14301
- Waegemakers Schiff J, Lane AM. PTSD symptoms, vicarious traumatization, and burnout in front line workers in the homeless sector. Community Ment Health J. 2019;55(3):454-462. doi:10.1007/s10597-018-00364-7
- Steenekamp BL, Barker SL. Exploring the experiences of compassion fatigue amongst peer support workers in homelessness services. Community Ment Health J. 2024;60(4):772-783. doi:10.1007/s10597-024-01234-1
- Perez S, Kerman N, Dej E, et al. When I can’t help, I suffer: a scoping review of moral distress in service providers working with persons experiencing homelessness. J Ment Health. Published online 2024:1-16. doi:10.1080/09638237.2024.2426986
- Monteith LL, Holliday R, Christe’An DI, Sherrill A, Brenner LA, Hoffmire CA. Suicide risk and prevention in Guam: clinical and research considerations and a call to action. Asian J Psychiatry. 2023;83:103546. doi:10.1016/j.ajp.2023.103546
- Surís A, Holliday R, Hooshyar D, et al. Development and implementation of a homeless mobile medical/mental veteran intervention. Fed Pract. 2017;34(9):18.
- Holliday R, Kinney AR, Smith AA, et al. A latent class analysis to identify subgroups of VHA using homeless veterans at greater risk for suicide mortality. J Affect Disord. 2022;315:162-167. doi:10.1016/j.jad.2022.07.062
- Weber J, Lee RC, Martsolf D. Understanding the health of veterans who are homeless: a review of the literature. Public Health Nurs. 2017;34(5):505-511. doi:10.1111/phn.12338
- Holliday R, Desai A, Stimmel M, Liu S, Monteith LL, Stewart KE. Meeting the health and social service needs of veterans who interact with the criminal justice system and experience homelessness: a holistic conceptualization and recommendations for tailoring care. Curr Treat Options Psychiatry. 2022;9(3):174-185. doi:10.1007/s40501-022-00275-1
- Holliday R, Desai A, Gerard G, Liu S, Stimmel M. Understanding the intersection of homelessness and justice involvement: enhancing veteran suicide prevention through VA programming. Fed Pract. 2022;39(1):8-11. doi:10.12788/fp.0216
- Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92(5):778-784. doi:10.2105/ajph.92.5.778
- Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs emergency departments. Am J Public Health. 2013;103(Suppl 2):S225-S231. doi:10.2105/AJPH.2013.301307
- Doran KM, Raven MC, Rosenheck RA. What drives frequent emergency department use in an integrated health system? National data from the Veterans Health Administration. Ann Emerg Med. 2013;62(2):151-159. doi:10.1016/j.annemergmed.2013.02.016
- Tsai J, Rosenheck RA. Risk factors for ED use among homeless veterans. Am J Emerg Med. 2013;31(5):855-858. doi:10.1016/j.ajem.2013.02.046
- Nelson RE, Suo Y, Pettey W, et al. Costs associated with health care services accessed through VA and in the community through Medicare for veterans experiencing homelessness. Health Serv Res. 2018;53(Suppl 3):5352-5374. doi:10.1111/1475-6773.13054
- Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi:10.1097/MLR.0000000000000112
- Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1- 6. doi:10.1027/0227-5910/a000001
- Decker H, Raguram M, Kanzaria HK, Duke M, Wick E. Provider perceptions of challenges and facilitators to surgical care in unhoused patients: a qualitative analysis. Surgery. 2024;175(4):1095-1102. doi:10.1016/j.surg.2023.11.009
- Panushka KA, Kozlowski Z, Dalessandro C, Sanders JN, Millar MM, Gawron LM. “It’s not a top priority”: a qualitative analysis of provider views on barriers to reproductive healthcare provision for homeless women in the United States. Soc Work Public Health. 2023;38(5 -8):428-436. doi:10.1080/19371918.2024.2315180
- Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893-1907. doi:10.1007/s11135-017-0574-8
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753-1760. doi:10.1177/1049732315617444
- Assarroudi A, Heshmati Nabavi F, Armat MR, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J Res Nurs. 2018;23(1):42-55. doi:10.1177/1744987117741667
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288.
- Goldsmith LJ. Using Framework Analysis in Applied Qualitative Research. Qual Rep. 2021;26(6):2061-2076. doi:10.46743/2160-3715/2021.5011
- Tufford L, Newman P. Bracketing in qualitative research. Qual Soc Work. 2012;11(1):80-96.
- Dodgson JE. Reflexivity in Qualitative Research. J Hum Lact. 2019;35(2):220-222. doi:10.1177/0890334419830990
- Hevner AR. A three cycle view of design science research. Scand J Inf Syst. 2007;19(2):4.
- Farao J, Malila B, Conrad N, Mutsvangwa T, Rangaka MX, Douglas TS. A user-centred design frame work for mHealth. PLOS ONE. 2020;15(8):e0237910. doi:10.1371/journal.pone.0237910
- Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481-498. doi:10.1111/sltb.12369
- Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1- 6. doi:10.1027/0227-5910/a000001
- Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and lowincome Veterans: a spotlight on the VA Supportive Housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi:10.1097/MLR.0000000000000112
- Holliday R, Hostetter T, Brenner LA, Bahraini N, Tsai J. Suicide risk screening and evaluation among patients accessing VHA services and identified as being newly homeless. Health Serv Res. 2024;59(5):e14301. doi:10.1111/1475-6773.14301
- Waegemakers Schiff J, Lane AM. PTSD symptoms, vicarious traumatization, and burnout in front line workers in the homeless sector. Community Ment Health J. 2019;55(3):454-462. doi:10.1007/s10597-018-00364-7
- Steenekamp BL, Barker SL. Exploring the experiences of compassion fatigue amongst peer support workers in homelessness services. Community Ment Health J. 2024;60(4):772-783. doi:10.1007/s10597-024-01234-1
- Perez S, Kerman N, Dej E, et al. When I can’t help, I suffer: a scoping review of moral distress in service providers working with persons experiencing homelessness. J Ment Health. Published online 2024:1-16. doi:10.1080/09638237.2024.2426986
- Monteith LL, Holliday R, Christe’An DI, Sherrill A, Brenner LA, Hoffmire CA. Suicide risk and prevention in Guam: clinical and research considerations and a call to action. Asian J Psychiatry. 2023;83:103546. doi:10.1016/j.ajp.2023.103546
- Surís A, Holliday R, Hooshyar D, et al. Development and implementation of a homeless mobile medical/mental veteran intervention. Fed Pract. 2017;34(9):18.
Development of a VA Clinician Resource to Facilitate Care Among Veterans Experiencing Homelessness
Development of a VA Clinician Resource to Facilitate Care Among Veterans Experiencing Homelessness
Common Ground: Primary Care and Specialty Clinicians’ Perceptions of E-Consults in the Veterans Health Administration
Electronic consultation (e-consult) is designed to increase access to specialty care by facilitating communication between primary care and specialty clinicians without the need for outpatient face-to-face encounters.1–4 In 2011, the US Department of Veterans Affairs (VA) implemented an e-consult program as a component of its overall strategy to increase access to specialty services, reduce costs of care, and reduce appointment travel burden on patients.
E-consult has substantially increased within the VA since its implementation.5,6 Consistent with limited evaluations from other health care systems, evaluations of the VA e-consult program demonstrated reduced costs, reduced travel time for patients, and improved access to specialty care.2,5–11 However, there is wide variation in e-consult use across VA specialties, facilities, and regions.5,6,12,13 For example, hematology, preoperative evaluation, neurosurgery, endocrinology, and infectious diseases use e-consults more frequently when compared with in-person consults in the VA.6 Reasons for this variation or specific barriers and facilitators of using e-consults have not been described.
Prior qualitative studies report that primary care practitioners (PCPs) describe e-consults as convenient, educational, beneficial for patient care, and useful for improving patient access to specialty care.8,14,15 One study identified limited PCP knowledge of e-consults as a barrier to use.16 Specialists have reported that e-consult improves clinical communication, but increases their workload.1,14,17,18 These studies did not assess perspectives from both clinicians who initiate e-consults and those who respond to them. This is the first qualitative study to assess e-consult perceptions from perspectives of both PCPs and specialists among a large, national sample of VA clinicians who use e-consults. The objective of this study was to understand perspectives of e-consults between PCPs and specialists that may be relevant to increasing adoption in the VA.
Methods
The team (CL, ML, PG, 2 analysts under the guidance of GS and JS and support from RRK, and a biostatistician) conducted semistructured interviews with PCPs, specialists, and specialty division leaders who were employed by VA in 2016 and 2017. Specialties of interest were identified by the VA Office of Specialty Care and included cardiology, endocrinology, gastroenterology, and hematology.
E-Consult Procedures
Within the VA, the specific procedures used to initiate, triage and manage e-consults are coordinated at VA medical centers (VAMCs) and at the Veterans Integrated Service Network (VISN) regional level. E-consult can be requested by any clinician. Generally, e-consults are initiated by PCPs through standardized, specialty-specific templates. Recipients, typically specialists, respond by answering questions, suggesting additional testing and evaluation, or requesting an in-person visit. Communication is documented in the patient’s electronic health record (EHR). Specialists receive different levels of workload credit for responding to e-consults similar to a relative value unit reimbursement model. Training in the use of e-consults is available to practitioners but may vary at local and regional levels.
Recruitment
Our sample included PCPs, specialists, and specialty care division leaders. We first quantified e-consult rates (e-consults per 100 patient visits) between July 2016 and June 2017 at VA facilities within primary care and the 4 priority specialties and identified the 30 sites with the highest e-consult rates and 30 sites with the lowest e-consult rates. Sites with < 500 total visits, < 3 specialties, or without any e-consult visit during the study period were excluded. E-consult rates at community-based outpatient clinics were included with associated VAMCs. We then stratified PCPs by whether they were high or low users of e-consults (determined by the top and bottom users within each site) and credentials (MD vs nurse practitioner [NP] or physician assistant [PA]). Specialists were sampled based on their rate of use relative to colleagues within their site and the use rate of their division. We sampled division chiefs and individuals who had > 300 total visits and 1 e-consult during the study period. To recruit participants, the primary investigator sent an initial email and 2 reminder emails. The team followed up with respondents to schedule an interview.
Interview guides were designed to elicit rich descriptions of barriers and facilitators to e-consult use (eAppendix available at doi:10.12788/fp.0214). The team used the Practical Robust Implementation and Sustainability Model (PRISM), which considers factors along 6 domains for intervention planning, implementation, and sustainment.19 Telephone interviews lasted about 20 minutes and were conducted between September 2017 and March 2018. Interviews were recorded and transcribed verbatim.
Analysis
The team used an iterative, team-based, inductive/deductive approach to conventional content analysis.20,21 Initial code categories were created so that we could identify e-consult best practices—facilitators of e-consult that were recommended by both PCPs and specialists. Inductive codes or labels applied to identify meaningful quotations, phrases, or key terms were used to identify emergent ideas and were added throughout coding after discussion among team members. Consensus was reached using a team-based approach.21 Four analysts independently coded the same 3 transcripts and met to discuss points of divergence and convergence. Analyses continued with emergent themes, categories, and conclusions. Atlas.ti. v.7 was used for coding and data management.22
Results
We conducted 34 interviews with clinicians (Table 1) from 13 VISNs. Four best-practice themes emerged among both PCPs and specialists, including that e-consults (1) are best suited for certain clinical questions and patients; (2) require relevant background information from requesting clinicians and clear recommendations from responding clinicians; (3) are a novel opportunity to provide efficient, transparent care; and (4) may not be fully adopted due to low awareness. Supporting quotations for the following findings are provided in Table 2.
Specific Clinical Questions and Patients
PCPs described specific patients and questions for which they most frequently used e-consults, such as for medication changes (Q1), determining treatment steps (Q2,3), and or clarifying laboratory or imaging findings. PCPs frequently used e-consults for patients who did not require a physical examination or when specialists could make recommendations without seeing patients face-to-face (Q3). An important use of e-consults described by PCPs was for treating conditions they could manage within primary care if additional guidance were available (Q4). Several PCPs and specialists also noted that e-consults were particularly useful for patients who were unable to travel or did not want face-to-face appointments (Q5). Notably, PCPs and specialists mentioned situations for which e-consults were inappropriate, including when a detailed history or physical examination was needed, or if a complex condition was suspected (Q6).
Background Data and Clear Recommendations
Participants described necessary data that should be included in high-quality e-consults. Specialists voiced frustration in time-consuming chart reviews that were often necessary when these data were not provided by the requestor. In some cases, specialists were unable to access necessary EHR data, which delayed responses (Q7). PCPs noted that the most useful responses carefully considered the question, used current patient information to determine treatments, provided clear recommendations, and defined who was responsible for next steps (Q8). PCPs and specialists stated that e-consult templates that required relevant information facilitated high-quality e-consults. Neither wanted to waste the other clinician's time (Q8).
A Novel Opportunity
Many PCPs felt that e-consults improved communication (eg, efficiency, response time), established new communication between clinicians, and reduced patients’ appointment burden (Q10, Q11). Many specialists felt that e-consults improved documentation of communication between clinicians and increased transparency of clinical decisions (Q12). Additionally, many specialists mentioned that e-consults capture previously informal curbside consults, enabling them to receive workload credit (Q13).
Lack of Awareness
Some noted that the biggest barrier to e-consults was not being aware of them generally, or which specialties offer e-consults (Q14). One PCP described e-consults as the best kept secret and found value in sharing the utility of e-consults with colleagues (Q15). All participants, including those who did not frequently use e-consults, felt that e-consults improved the quality of care by providing more timely care or better answers to clinical questions (Q16). Several practitioners also felt that e-consults increased access to specialty care. For example, specialists reported that e-consults enabled them to better manage patient load by using e-consults to answer relatively simple questions, reserving face-to-face consults for more complex patients (Q17).
Discussion
The objective of this study was to identify potential best practices for e-consults that may help increase their quality and use within the VA. We built on prior studies that offered insights on PCP and specialists’ overall satisfaction with e-consult by identifying several themes relevant to the further adoption of e-consults in the VA and elsewhere without a face-to-face visit.8,13,14,16–18 Future work may be beneficial in identifying whether the study themes identified can explain variation in e-consult use or whether addressing these factors might lead to increased or higher quality e-consult use. We are unaware of any qualitative study of comparable scale in a different health care system. Further, this is the first study to assess perspectives on e-consults among those who initiate and respond to them within the same health care system. Perhaps the most important finding from this study is that e-consults are generally viewed favorably, which is a necessary leverage point to increase their adoption within the system.
Clinicians reported several benefits to e-consults, including timely responses to clinical questions, efficient communication, allow for documentation of specialist recommendations, and help capture workload. These benefits are consistent with prior literature that indicates both PCPs and specialists in the VA and other health care systems feel that e-consults improves communication, decreases unnecessary visits, and improves quality of care.1,14,17,18 In particular, clinicians reported that e-consults improve their practice efficiency and efficacy. This is of critical importance given the pressures of providing timely access to primary and specialty care within the VA. Interestingly, many VA practitioners were unaware which specialties offered e-consults within their facilities, reflecting previous work showing that PCPs are often unaware of e-consult options.16 This may partially explain variation in e-consult use. Increasing awareness and educating clinicians on the benefits of e-consults may help promote use among non- and low users.
A common theme reported by both groups was the importance of providing necessary information within e-consult questions and responses. Specialists felt there was a need to ensure that PCPs provide relevant and patient-specific information that would enable them to efficiently and accurately answer questions without the need for extensive EHR review. This reflects previous work showing that specialists are often unable to respond to e-consult requests because they do not contain sufficient information.22 PCPs described a need to ensure that specialists’ responses included information that was detailed enough to make clinical decisions without the need for a reconsult. This highlights a common challenge to medical consultation, in that necessary or relevant information may not be apparent to all clinicians. To address this, there may be a role in developing enhanced, flexible templating that elicits necessary patient-specific information. Such a template may automatically pull relevant data from the EHR and prompt clinicians to provide important information. We did not assess how perspectives of templates varied, and further work could help define precisely what constitutes an effective template, including how it should capture appropriate patient data and how this impacts acceptability or use of e-consults generally. Collaboratively developed service agreements and e-consult templates could help guide PCPs and specialists to engage in efficient communication.
Another theme among both groups was that e-consult is most appropriate within specific clinical scenarios. Examples included review of laboratory results, questions about medication changes, or for patients who were reluctant to travel to appointments. Identifying and promoting specific opportunities for e-consults may help increase their use and align e-consult practices with scenarios that are likely to provide the most benefit to patients. For example, it could be helpful to understand the distance patients must travel for specialty care. Providing that information during clinical encounters could trigger clinicians to consider e-consults as an option. Future work might aim to identify clinical scenarios that clinicians feel are not well suited for e-consults and determine how to adapt them for those scenarios.
Limitations
Generalizability of these findings is limited given the qualitative study design. Participants’ descriptions of experiences with e-consults reflect the experiences of clinicians in the VA and may not reflect clinicians in other settings. We also interviewed a sample of clinicians who were already using e-consults. Important information could be learned from future work with those who have not yet adopted e-consult procedures or adopted and abandoned them.
Conclusions
E-consult is perceived as beneficial by VA PCPs and specialists. Participants suggested using e-consults for appropriate questions or patients and including necessary information and next steps in both the initial e-consult and response. Finding ways to facilitate e-consults with these suggestions in mind may increase delivery of high-quality e-consults. Future work could compare the findings of this work to similar work assessing clinicians perceptions of e-consults outside of the VA.
1. Battaglia C, Lambert-Kerzner A, Aron DC, et al. Evaluation of e-consults in the VHA: provider perspectives. Fed Pract. 2015;32(7):42-48.
2. Haverhals LM, Sayre G, Helfrich CD, et al. E-consult implementation: lessons learned using consolidated framework for implementation research. Am J Manag Care. 2015;21(12):e640-e647. Published 2015 Dec 1.
3. Sewell JL, Telischak KS, Day LW, Kirschner N, Weissman A. Preconsultation exchange in the United States: use, awareness, and attitudes. Am J Manag Care. 2014;20(12):e556-e564. Published 2014 Dec 1.
4. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: early insights. Issue Brief (Commonw Fund). 2011;23:1-14.
5. Kirsh S, Carey E, Aron DC, et al. Impact of a national specialty e-consultation implementation project on access. Am J Manag Care. 2015;21(12):e648-654. Published 2015 Dec 1.
6. Saxon DR, Kaboli PJ, Haraldsson B, Wilson C, Ohl M, Augustine MR. Growth of electronic consultations in the Veterans Health Administration. Am J Manag Care. 2021;27(1):12-19. doi:10.37765/ajmc.2021.88572
7. Olayiwola JN, Anderson D, Jepeal N, et al. Electronic consultations to improve the primary care-specialty care interface for cardiology in the medically underserved: a cluster-randomized controlled trial. Ann Fam Med. 2016;14(2):133-140. doi:10.1370/afm.1869
8. Schettini P, Shah KP, O’Leary CP, et al. Keeping care connected: e-Consultation program improves access to nephrology care. J Telemed Telecare. 2019;25(3):142-150. doi:10.1177/1357633X17748350
9. Whittington MD, Ho PM, Kirsh SR, et al. Cost savings associated with electronic specialty consultations. Am J Manag Care. 2021;27(1):e16-e23. Published 2021 Jan 1. doi:10.37765/ajmc.2021.88579
10. Shipherd JC, Kauth MR, Matza A. Nationwide interdisciplinary e-consultation on transgender care in the Veterans Health Administration. Telemed J E Health. 2016;22(12):1008-1012. doi:10.1089/tmj.2016.0013
11. Strymish J, Gupte G, Afable MK, et al. Electronic consultations (E-consults): advancing infectious disease care in a large Veterans Affairs Healthcare System. Clin Infect Dis. 2017;64(8):1123-1125. doi:10.1093/cid/cix058
12. Williams KM, Kirsh S, Aron D, et al. Evaluation of the Veterans Health Administration’s Specialty Care Transformational Initiatives to promote patient-centered delivery of specialty care: a mixed-methods approach. Telemed J E-Health. 2017;23(7):577-589. doi:10.1089/tmj.2016.0166
13. US Department of Veterans Affairs, Veterans Health Administration, Specialty Care Transformational Initiative Evaluation Center. Evaluation of specialty care initiatives. Published 2013.
14. Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323-330. doi:10.1177/1357633X15582108
15. Lee M, Leonard C, Greene P, et al. Perspectives of VA primary care clinicians toward electronic consultation-related workload burden. JAMA Netw Open. 2020;3(10):e2018104. Published 2020 Oct 1. doi:10.1001/jamanetworkopen.2020.18104
16. Deeds SA, Dowdell KJ, Chew LD, Ackerman SL. Implementing an opt-in eConsult program at seven academic medical centers: a qualitative analysis of primary care provider experiences. J Gen Intern Med. 2019;34(8):1427-1433. doi:10.1007/s11606-019-05067-7
17. Rodriguez KL, Burkitt KH, Bayliss NK, et al. Veteran, primary care provider, and specialist satisfaction with electronic consultation. JMIR Med Inform. 2015;3(1):e5. Published 2015 Jan 14. doi:10.2196/medinform.3725
18. Gupte G, Vimalananda V, Simon SR, DeVito K, Clark J, Orlander JD. Disruptive innovation: implementation of electronic consultations in a Veterans Affairs Health Care System. JMIR Med Inform. 2016;4(1):e6. Published 2016 Feb 12. doi:10.2196/medinform.4801
19. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008;34(4):228-243. doi:10.1016/s1553-7250(08)34030-6
20. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Sage Publications; 2002.
21. Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758-1772. doi:10.1111/j.1475-6773.2006.00684.x
22. Kim EJ, Orlander JD, Afable M, et al. Cardiology electronic consultation (e-consult) use by primary care providers at VA medical centres in New England. J Telemed Telecare. 2019;25(6):370-377. doi:10.1177/1357633X18774468
Electronic consultation (e-consult) is designed to increase access to specialty care by facilitating communication between primary care and specialty clinicians without the need for outpatient face-to-face encounters.1–4 In 2011, the US Department of Veterans Affairs (VA) implemented an e-consult program as a component of its overall strategy to increase access to specialty services, reduce costs of care, and reduce appointment travel burden on patients.
E-consult has substantially increased within the VA since its implementation.5,6 Consistent with limited evaluations from other health care systems, evaluations of the VA e-consult program demonstrated reduced costs, reduced travel time for patients, and improved access to specialty care.2,5–11 However, there is wide variation in e-consult use across VA specialties, facilities, and regions.5,6,12,13 For example, hematology, preoperative evaluation, neurosurgery, endocrinology, and infectious diseases use e-consults more frequently when compared with in-person consults in the VA.6 Reasons for this variation or specific barriers and facilitators of using e-consults have not been described.
Prior qualitative studies report that primary care practitioners (PCPs) describe e-consults as convenient, educational, beneficial for patient care, and useful for improving patient access to specialty care.8,14,15 One study identified limited PCP knowledge of e-consults as a barrier to use.16 Specialists have reported that e-consult improves clinical communication, but increases their workload.1,14,17,18 These studies did not assess perspectives from both clinicians who initiate e-consults and those who respond to them. This is the first qualitative study to assess e-consult perceptions from perspectives of both PCPs and specialists among a large, national sample of VA clinicians who use e-consults. The objective of this study was to understand perspectives of e-consults between PCPs and specialists that may be relevant to increasing adoption in the VA.
Methods
The team (CL, ML, PG, 2 analysts under the guidance of GS and JS and support from RRK, and a biostatistician) conducted semistructured interviews with PCPs, specialists, and specialty division leaders who were employed by VA in 2016 and 2017. Specialties of interest were identified by the VA Office of Specialty Care and included cardiology, endocrinology, gastroenterology, and hematology.
E-Consult Procedures
Within the VA, the specific procedures used to initiate, triage and manage e-consults are coordinated at VA medical centers (VAMCs) and at the Veterans Integrated Service Network (VISN) regional level. E-consult can be requested by any clinician. Generally, e-consults are initiated by PCPs through standardized, specialty-specific templates. Recipients, typically specialists, respond by answering questions, suggesting additional testing and evaluation, or requesting an in-person visit. Communication is documented in the patient’s electronic health record (EHR). Specialists receive different levels of workload credit for responding to e-consults similar to a relative value unit reimbursement model. Training in the use of e-consults is available to practitioners but may vary at local and regional levels.
Recruitment
Our sample included PCPs, specialists, and specialty care division leaders. We first quantified e-consult rates (e-consults per 100 patient visits) between July 2016 and June 2017 at VA facilities within primary care and the 4 priority specialties and identified the 30 sites with the highest e-consult rates and 30 sites with the lowest e-consult rates. Sites with < 500 total visits, < 3 specialties, or without any e-consult visit during the study period were excluded. E-consult rates at community-based outpatient clinics were included with associated VAMCs. We then stratified PCPs by whether they were high or low users of e-consults (determined by the top and bottom users within each site) and credentials (MD vs nurse practitioner [NP] or physician assistant [PA]). Specialists were sampled based on their rate of use relative to colleagues within their site and the use rate of their division. We sampled division chiefs and individuals who had > 300 total visits and 1 e-consult during the study period. To recruit participants, the primary investigator sent an initial email and 2 reminder emails. The team followed up with respondents to schedule an interview.
Interview guides were designed to elicit rich descriptions of barriers and facilitators to e-consult use (eAppendix available at doi:10.12788/fp.0214). The team used the Practical Robust Implementation and Sustainability Model (PRISM), which considers factors along 6 domains for intervention planning, implementation, and sustainment.19 Telephone interviews lasted about 20 minutes and were conducted between September 2017 and March 2018. Interviews were recorded and transcribed verbatim.
Analysis
The team used an iterative, team-based, inductive/deductive approach to conventional content analysis.20,21 Initial code categories were created so that we could identify e-consult best practices—facilitators of e-consult that were recommended by both PCPs and specialists. Inductive codes or labels applied to identify meaningful quotations, phrases, or key terms were used to identify emergent ideas and were added throughout coding after discussion among team members. Consensus was reached using a team-based approach.21 Four analysts independently coded the same 3 transcripts and met to discuss points of divergence and convergence. Analyses continued with emergent themes, categories, and conclusions. Atlas.ti. v.7 was used for coding and data management.22
Results
We conducted 34 interviews with clinicians (Table 1) from 13 VISNs. Four best-practice themes emerged among both PCPs and specialists, including that e-consults (1) are best suited for certain clinical questions and patients; (2) require relevant background information from requesting clinicians and clear recommendations from responding clinicians; (3) are a novel opportunity to provide efficient, transparent care; and (4) may not be fully adopted due to low awareness. Supporting quotations for the following findings are provided in Table 2.
Specific Clinical Questions and Patients
PCPs described specific patients and questions for which they most frequently used e-consults, such as for medication changes (Q1), determining treatment steps (Q2,3), and or clarifying laboratory or imaging findings. PCPs frequently used e-consults for patients who did not require a physical examination or when specialists could make recommendations without seeing patients face-to-face (Q3). An important use of e-consults described by PCPs was for treating conditions they could manage within primary care if additional guidance were available (Q4). Several PCPs and specialists also noted that e-consults were particularly useful for patients who were unable to travel or did not want face-to-face appointments (Q5). Notably, PCPs and specialists mentioned situations for which e-consults were inappropriate, including when a detailed history or physical examination was needed, or if a complex condition was suspected (Q6).
Background Data and Clear Recommendations
Participants described necessary data that should be included in high-quality e-consults. Specialists voiced frustration in time-consuming chart reviews that were often necessary when these data were not provided by the requestor. In some cases, specialists were unable to access necessary EHR data, which delayed responses (Q7). PCPs noted that the most useful responses carefully considered the question, used current patient information to determine treatments, provided clear recommendations, and defined who was responsible for next steps (Q8). PCPs and specialists stated that e-consult templates that required relevant information facilitated high-quality e-consults. Neither wanted to waste the other clinician's time (Q8).
A Novel Opportunity
Many PCPs felt that e-consults improved communication (eg, efficiency, response time), established new communication between clinicians, and reduced patients’ appointment burden (Q10, Q11). Many specialists felt that e-consults improved documentation of communication between clinicians and increased transparency of clinical decisions (Q12). Additionally, many specialists mentioned that e-consults capture previously informal curbside consults, enabling them to receive workload credit (Q13).
Lack of Awareness
Some noted that the biggest barrier to e-consults was not being aware of them generally, or which specialties offer e-consults (Q14). One PCP described e-consults as the best kept secret and found value in sharing the utility of e-consults with colleagues (Q15). All participants, including those who did not frequently use e-consults, felt that e-consults improved the quality of care by providing more timely care or better answers to clinical questions (Q16). Several practitioners also felt that e-consults increased access to specialty care. For example, specialists reported that e-consults enabled them to better manage patient load by using e-consults to answer relatively simple questions, reserving face-to-face consults for more complex patients (Q17).
Discussion
The objective of this study was to identify potential best practices for e-consults that may help increase their quality and use within the VA. We built on prior studies that offered insights on PCP and specialists’ overall satisfaction with e-consult by identifying several themes relevant to the further adoption of e-consults in the VA and elsewhere without a face-to-face visit.8,13,14,16–18 Future work may be beneficial in identifying whether the study themes identified can explain variation in e-consult use or whether addressing these factors might lead to increased or higher quality e-consult use. We are unaware of any qualitative study of comparable scale in a different health care system. Further, this is the first study to assess perspectives on e-consults among those who initiate and respond to them within the same health care system. Perhaps the most important finding from this study is that e-consults are generally viewed favorably, which is a necessary leverage point to increase their adoption within the system.
Clinicians reported several benefits to e-consults, including timely responses to clinical questions, efficient communication, allow for documentation of specialist recommendations, and help capture workload. These benefits are consistent with prior literature that indicates both PCPs and specialists in the VA and other health care systems feel that e-consults improves communication, decreases unnecessary visits, and improves quality of care.1,14,17,18 In particular, clinicians reported that e-consults improve their practice efficiency and efficacy. This is of critical importance given the pressures of providing timely access to primary and specialty care within the VA. Interestingly, many VA practitioners were unaware which specialties offered e-consults within their facilities, reflecting previous work showing that PCPs are often unaware of e-consult options.16 This may partially explain variation in e-consult use. Increasing awareness and educating clinicians on the benefits of e-consults may help promote use among non- and low users.
A common theme reported by both groups was the importance of providing necessary information within e-consult questions and responses. Specialists felt there was a need to ensure that PCPs provide relevant and patient-specific information that would enable them to efficiently and accurately answer questions without the need for extensive EHR review. This reflects previous work showing that specialists are often unable to respond to e-consult requests because they do not contain sufficient information.22 PCPs described a need to ensure that specialists’ responses included information that was detailed enough to make clinical decisions without the need for a reconsult. This highlights a common challenge to medical consultation, in that necessary or relevant information may not be apparent to all clinicians. To address this, there may be a role in developing enhanced, flexible templating that elicits necessary patient-specific information. Such a template may automatically pull relevant data from the EHR and prompt clinicians to provide important information. We did not assess how perspectives of templates varied, and further work could help define precisely what constitutes an effective template, including how it should capture appropriate patient data and how this impacts acceptability or use of e-consults generally. Collaboratively developed service agreements and e-consult templates could help guide PCPs and specialists to engage in efficient communication.
Another theme among both groups was that e-consult is most appropriate within specific clinical scenarios. Examples included review of laboratory results, questions about medication changes, or for patients who were reluctant to travel to appointments. Identifying and promoting specific opportunities for e-consults may help increase their use and align e-consult practices with scenarios that are likely to provide the most benefit to patients. For example, it could be helpful to understand the distance patients must travel for specialty care. Providing that information during clinical encounters could trigger clinicians to consider e-consults as an option. Future work might aim to identify clinical scenarios that clinicians feel are not well suited for e-consults and determine how to adapt them for those scenarios.
Limitations
Generalizability of these findings is limited given the qualitative study design. Participants’ descriptions of experiences with e-consults reflect the experiences of clinicians in the VA and may not reflect clinicians in other settings. We also interviewed a sample of clinicians who were already using e-consults. Important information could be learned from future work with those who have not yet adopted e-consult procedures or adopted and abandoned them.
Conclusions
E-consult is perceived as beneficial by VA PCPs and specialists. Participants suggested using e-consults for appropriate questions or patients and including necessary information and next steps in both the initial e-consult and response. Finding ways to facilitate e-consults with these suggestions in mind may increase delivery of high-quality e-consults. Future work could compare the findings of this work to similar work assessing clinicians perceptions of e-consults outside of the VA.
Electronic consultation (e-consult) is designed to increase access to specialty care by facilitating communication between primary care and specialty clinicians without the need for outpatient face-to-face encounters.1–4 In 2011, the US Department of Veterans Affairs (VA) implemented an e-consult program as a component of its overall strategy to increase access to specialty services, reduce costs of care, and reduce appointment travel burden on patients.
E-consult has substantially increased within the VA since its implementation.5,6 Consistent with limited evaluations from other health care systems, evaluations of the VA e-consult program demonstrated reduced costs, reduced travel time for patients, and improved access to specialty care.2,5–11 However, there is wide variation in e-consult use across VA specialties, facilities, and regions.5,6,12,13 For example, hematology, preoperative evaluation, neurosurgery, endocrinology, and infectious diseases use e-consults more frequently when compared with in-person consults in the VA.6 Reasons for this variation or specific barriers and facilitators of using e-consults have not been described.
Prior qualitative studies report that primary care practitioners (PCPs) describe e-consults as convenient, educational, beneficial for patient care, and useful for improving patient access to specialty care.8,14,15 One study identified limited PCP knowledge of e-consults as a barrier to use.16 Specialists have reported that e-consult improves clinical communication, but increases their workload.1,14,17,18 These studies did not assess perspectives from both clinicians who initiate e-consults and those who respond to them. This is the first qualitative study to assess e-consult perceptions from perspectives of both PCPs and specialists among a large, national sample of VA clinicians who use e-consults. The objective of this study was to understand perspectives of e-consults between PCPs and specialists that may be relevant to increasing adoption in the VA.
Methods
The team (CL, ML, PG, 2 analysts under the guidance of GS and JS and support from RRK, and a biostatistician) conducted semistructured interviews with PCPs, specialists, and specialty division leaders who were employed by VA in 2016 and 2017. Specialties of interest were identified by the VA Office of Specialty Care and included cardiology, endocrinology, gastroenterology, and hematology.
E-Consult Procedures
Within the VA, the specific procedures used to initiate, triage and manage e-consults are coordinated at VA medical centers (VAMCs) and at the Veterans Integrated Service Network (VISN) regional level. E-consult can be requested by any clinician. Generally, e-consults are initiated by PCPs through standardized, specialty-specific templates. Recipients, typically specialists, respond by answering questions, suggesting additional testing and evaluation, or requesting an in-person visit. Communication is documented in the patient’s electronic health record (EHR). Specialists receive different levels of workload credit for responding to e-consults similar to a relative value unit reimbursement model. Training in the use of e-consults is available to practitioners but may vary at local and regional levels.
Recruitment
Our sample included PCPs, specialists, and specialty care division leaders. We first quantified e-consult rates (e-consults per 100 patient visits) between July 2016 and June 2017 at VA facilities within primary care and the 4 priority specialties and identified the 30 sites with the highest e-consult rates and 30 sites with the lowest e-consult rates. Sites with < 500 total visits, < 3 specialties, or without any e-consult visit during the study period were excluded. E-consult rates at community-based outpatient clinics were included with associated VAMCs. We then stratified PCPs by whether they were high or low users of e-consults (determined by the top and bottom users within each site) and credentials (MD vs nurse practitioner [NP] or physician assistant [PA]). Specialists were sampled based on their rate of use relative to colleagues within their site and the use rate of their division. We sampled division chiefs and individuals who had > 300 total visits and 1 e-consult during the study period. To recruit participants, the primary investigator sent an initial email and 2 reminder emails. The team followed up with respondents to schedule an interview.
Interview guides were designed to elicit rich descriptions of barriers and facilitators to e-consult use (eAppendix available at doi:10.12788/fp.0214). The team used the Practical Robust Implementation and Sustainability Model (PRISM), which considers factors along 6 domains for intervention planning, implementation, and sustainment.19 Telephone interviews lasted about 20 minutes and were conducted between September 2017 and March 2018. Interviews were recorded and transcribed verbatim.
Analysis
The team used an iterative, team-based, inductive/deductive approach to conventional content analysis.20,21 Initial code categories were created so that we could identify e-consult best practices—facilitators of e-consult that were recommended by both PCPs and specialists. Inductive codes or labels applied to identify meaningful quotations, phrases, or key terms were used to identify emergent ideas and were added throughout coding after discussion among team members. Consensus was reached using a team-based approach.21 Four analysts independently coded the same 3 transcripts and met to discuss points of divergence and convergence. Analyses continued with emergent themes, categories, and conclusions. Atlas.ti. v.7 was used for coding and data management.22
Results
We conducted 34 interviews with clinicians (Table 1) from 13 VISNs. Four best-practice themes emerged among both PCPs and specialists, including that e-consults (1) are best suited for certain clinical questions and patients; (2) require relevant background information from requesting clinicians and clear recommendations from responding clinicians; (3) are a novel opportunity to provide efficient, transparent care; and (4) may not be fully adopted due to low awareness. Supporting quotations for the following findings are provided in Table 2.
Specific Clinical Questions and Patients
PCPs described specific patients and questions for which they most frequently used e-consults, such as for medication changes (Q1), determining treatment steps (Q2,3), and or clarifying laboratory or imaging findings. PCPs frequently used e-consults for patients who did not require a physical examination or when specialists could make recommendations without seeing patients face-to-face (Q3). An important use of e-consults described by PCPs was for treating conditions they could manage within primary care if additional guidance were available (Q4). Several PCPs and specialists also noted that e-consults were particularly useful for patients who were unable to travel or did not want face-to-face appointments (Q5). Notably, PCPs and specialists mentioned situations for which e-consults were inappropriate, including when a detailed history or physical examination was needed, or if a complex condition was suspected (Q6).
Background Data and Clear Recommendations
Participants described necessary data that should be included in high-quality e-consults. Specialists voiced frustration in time-consuming chart reviews that were often necessary when these data were not provided by the requestor. In some cases, specialists were unable to access necessary EHR data, which delayed responses (Q7). PCPs noted that the most useful responses carefully considered the question, used current patient information to determine treatments, provided clear recommendations, and defined who was responsible for next steps (Q8). PCPs and specialists stated that e-consult templates that required relevant information facilitated high-quality e-consults. Neither wanted to waste the other clinician's time (Q8).
A Novel Opportunity
Many PCPs felt that e-consults improved communication (eg, efficiency, response time), established new communication between clinicians, and reduced patients’ appointment burden (Q10, Q11). Many specialists felt that e-consults improved documentation of communication between clinicians and increased transparency of clinical decisions (Q12). Additionally, many specialists mentioned that e-consults capture previously informal curbside consults, enabling them to receive workload credit (Q13).
Lack of Awareness
Some noted that the biggest barrier to e-consults was not being aware of them generally, or which specialties offer e-consults (Q14). One PCP described e-consults as the best kept secret and found value in sharing the utility of e-consults with colleagues (Q15). All participants, including those who did not frequently use e-consults, felt that e-consults improved the quality of care by providing more timely care or better answers to clinical questions (Q16). Several practitioners also felt that e-consults increased access to specialty care. For example, specialists reported that e-consults enabled them to better manage patient load by using e-consults to answer relatively simple questions, reserving face-to-face consults for more complex patients (Q17).
Discussion
The objective of this study was to identify potential best practices for e-consults that may help increase their quality and use within the VA. We built on prior studies that offered insights on PCP and specialists’ overall satisfaction with e-consult by identifying several themes relevant to the further adoption of e-consults in the VA and elsewhere without a face-to-face visit.8,13,14,16–18 Future work may be beneficial in identifying whether the study themes identified can explain variation in e-consult use or whether addressing these factors might lead to increased or higher quality e-consult use. We are unaware of any qualitative study of comparable scale in a different health care system. Further, this is the first study to assess perspectives on e-consults among those who initiate and respond to them within the same health care system. Perhaps the most important finding from this study is that e-consults are generally viewed favorably, which is a necessary leverage point to increase their adoption within the system.
Clinicians reported several benefits to e-consults, including timely responses to clinical questions, efficient communication, allow for documentation of specialist recommendations, and help capture workload. These benefits are consistent with prior literature that indicates both PCPs and specialists in the VA and other health care systems feel that e-consults improves communication, decreases unnecessary visits, and improves quality of care.1,14,17,18 In particular, clinicians reported that e-consults improve their practice efficiency and efficacy. This is of critical importance given the pressures of providing timely access to primary and specialty care within the VA. Interestingly, many VA practitioners were unaware which specialties offered e-consults within their facilities, reflecting previous work showing that PCPs are often unaware of e-consult options.16 This may partially explain variation in e-consult use. Increasing awareness and educating clinicians on the benefits of e-consults may help promote use among non- and low users.
A common theme reported by both groups was the importance of providing necessary information within e-consult questions and responses. Specialists felt there was a need to ensure that PCPs provide relevant and patient-specific information that would enable them to efficiently and accurately answer questions without the need for extensive EHR review. This reflects previous work showing that specialists are often unable to respond to e-consult requests because they do not contain sufficient information.22 PCPs described a need to ensure that specialists’ responses included information that was detailed enough to make clinical decisions without the need for a reconsult. This highlights a common challenge to medical consultation, in that necessary or relevant information may not be apparent to all clinicians. To address this, there may be a role in developing enhanced, flexible templating that elicits necessary patient-specific information. Such a template may automatically pull relevant data from the EHR and prompt clinicians to provide important information. We did not assess how perspectives of templates varied, and further work could help define precisely what constitutes an effective template, including how it should capture appropriate patient data and how this impacts acceptability or use of e-consults generally. Collaboratively developed service agreements and e-consult templates could help guide PCPs and specialists to engage in efficient communication.
Another theme among both groups was that e-consult is most appropriate within specific clinical scenarios. Examples included review of laboratory results, questions about medication changes, or for patients who were reluctant to travel to appointments. Identifying and promoting specific opportunities for e-consults may help increase their use and align e-consult practices with scenarios that are likely to provide the most benefit to patients. For example, it could be helpful to understand the distance patients must travel for specialty care. Providing that information during clinical encounters could trigger clinicians to consider e-consults as an option. Future work might aim to identify clinical scenarios that clinicians feel are not well suited for e-consults and determine how to adapt them for those scenarios.
Limitations
Generalizability of these findings is limited given the qualitative study design. Participants’ descriptions of experiences with e-consults reflect the experiences of clinicians in the VA and may not reflect clinicians in other settings. We also interviewed a sample of clinicians who were already using e-consults. Important information could be learned from future work with those who have not yet adopted e-consult procedures or adopted and abandoned them.
Conclusions
E-consult is perceived as beneficial by VA PCPs and specialists. Participants suggested using e-consults for appropriate questions or patients and including necessary information and next steps in both the initial e-consult and response. Finding ways to facilitate e-consults with these suggestions in mind may increase delivery of high-quality e-consults. Future work could compare the findings of this work to similar work assessing clinicians perceptions of e-consults outside of the VA.
1. Battaglia C, Lambert-Kerzner A, Aron DC, et al. Evaluation of e-consults in the VHA: provider perspectives. Fed Pract. 2015;32(7):42-48.
2. Haverhals LM, Sayre G, Helfrich CD, et al. E-consult implementation: lessons learned using consolidated framework for implementation research. Am J Manag Care. 2015;21(12):e640-e647. Published 2015 Dec 1.
3. Sewell JL, Telischak KS, Day LW, Kirschner N, Weissman A. Preconsultation exchange in the United States: use, awareness, and attitudes. Am J Manag Care. 2014;20(12):e556-e564. Published 2014 Dec 1.
4. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: early insights. Issue Brief (Commonw Fund). 2011;23:1-14.
5. Kirsh S, Carey E, Aron DC, et al. Impact of a national specialty e-consultation implementation project on access. Am J Manag Care. 2015;21(12):e648-654. Published 2015 Dec 1.
6. Saxon DR, Kaboli PJ, Haraldsson B, Wilson C, Ohl M, Augustine MR. Growth of electronic consultations in the Veterans Health Administration. Am J Manag Care. 2021;27(1):12-19. doi:10.37765/ajmc.2021.88572
7. Olayiwola JN, Anderson D, Jepeal N, et al. Electronic consultations to improve the primary care-specialty care interface for cardiology in the medically underserved: a cluster-randomized controlled trial. Ann Fam Med. 2016;14(2):133-140. doi:10.1370/afm.1869
8. Schettini P, Shah KP, O’Leary CP, et al. Keeping care connected: e-Consultation program improves access to nephrology care. J Telemed Telecare. 2019;25(3):142-150. doi:10.1177/1357633X17748350
9. Whittington MD, Ho PM, Kirsh SR, et al. Cost savings associated with electronic specialty consultations. Am J Manag Care. 2021;27(1):e16-e23. Published 2021 Jan 1. doi:10.37765/ajmc.2021.88579
10. Shipherd JC, Kauth MR, Matza A. Nationwide interdisciplinary e-consultation on transgender care in the Veterans Health Administration. Telemed J E Health. 2016;22(12):1008-1012. doi:10.1089/tmj.2016.0013
11. Strymish J, Gupte G, Afable MK, et al. Electronic consultations (E-consults): advancing infectious disease care in a large Veterans Affairs Healthcare System. Clin Infect Dis. 2017;64(8):1123-1125. doi:10.1093/cid/cix058
12. Williams KM, Kirsh S, Aron D, et al. Evaluation of the Veterans Health Administration’s Specialty Care Transformational Initiatives to promote patient-centered delivery of specialty care: a mixed-methods approach. Telemed J E-Health. 2017;23(7):577-589. doi:10.1089/tmj.2016.0166
13. US Department of Veterans Affairs, Veterans Health Administration, Specialty Care Transformational Initiative Evaluation Center. Evaluation of specialty care initiatives. Published 2013.
14. Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323-330. doi:10.1177/1357633X15582108
15. Lee M, Leonard C, Greene P, et al. Perspectives of VA primary care clinicians toward electronic consultation-related workload burden. JAMA Netw Open. 2020;3(10):e2018104. Published 2020 Oct 1. doi:10.1001/jamanetworkopen.2020.18104
16. Deeds SA, Dowdell KJ, Chew LD, Ackerman SL. Implementing an opt-in eConsult program at seven academic medical centers: a qualitative analysis of primary care provider experiences. J Gen Intern Med. 2019;34(8):1427-1433. doi:10.1007/s11606-019-05067-7
17. Rodriguez KL, Burkitt KH, Bayliss NK, et al. Veteran, primary care provider, and specialist satisfaction with electronic consultation. JMIR Med Inform. 2015;3(1):e5. Published 2015 Jan 14. doi:10.2196/medinform.3725
18. Gupte G, Vimalananda V, Simon SR, DeVito K, Clark J, Orlander JD. Disruptive innovation: implementation of electronic consultations in a Veterans Affairs Health Care System. JMIR Med Inform. 2016;4(1):e6. Published 2016 Feb 12. doi:10.2196/medinform.4801
19. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008;34(4):228-243. doi:10.1016/s1553-7250(08)34030-6
20. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Sage Publications; 2002.
21. Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758-1772. doi:10.1111/j.1475-6773.2006.00684.x
22. Kim EJ, Orlander JD, Afable M, et al. Cardiology electronic consultation (e-consult) use by primary care providers at VA medical centres in New England. J Telemed Telecare. 2019;25(6):370-377. doi:10.1177/1357633X18774468
1. Battaglia C, Lambert-Kerzner A, Aron DC, et al. Evaluation of e-consults in the VHA: provider perspectives. Fed Pract. 2015;32(7):42-48.
2. Haverhals LM, Sayre G, Helfrich CD, et al. E-consult implementation: lessons learned using consolidated framework for implementation research. Am J Manag Care. 2015;21(12):e640-e647. Published 2015 Dec 1.
3. Sewell JL, Telischak KS, Day LW, Kirschner N, Weissman A. Preconsultation exchange in the United States: use, awareness, and attitudes. Am J Manag Care. 2014;20(12):e556-e564. Published 2014 Dec 1.
4. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: early insights. Issue Brief (Commonw Fund). 2011;23:1-14.
5. Kirsh S, Carey E, Aron DC, et al. Impact of a national specialty e-consultation implementation project on access. Am J Manag Care. 2015;21(12):e648-654. Published 2015 Dec 1.
6. Saxon DR, Kaboli PJ, Haraldsson B, Wilson C, Ohl M, Augustine MR. Growth of electronic consultations in the Veterans Health Administration. Am J Manag Care. 2021;27(1):12-19. doi:10.37765/ajmc.2021.88572
7. Olayiwola JN, Anderson D, Jepeal N, et al. Electronic consultations to improve the primary care-specialty care interface for cardiology in the medically underserved: a cluster-randomized controlled trial. Ann Fam Med. 2016;14(2):133-140. doi:10.1370/afm.1869
8. Schettini P, Shah KP, O’Leary CP, et al. Keeping care connected: e-Consultation program improves access to nephrology care. J Telemed Telecare. 2019;25(3):142-150. doi:10.1177/1357633X17748350
9. Whittington MD, Ho PM, Kirsh SR, et al. Cost savings associated with electronic specialty consultations. Am J Manag Care. 2021;27(1):e16-e23. Published 2021 Jan 1. doi:10.37765/ajmc.2021.88579
10. Shipherd JC, Kauth MR, Matza A. Nationwide interdisciplinary e-consultation on transgender care in the Veterans Health Administration. Telemed J E Health. 2016;22(12):1008-1012. doi:10.1089/tmj.2016.0013
11. Strymish J, Gupte G, Afable MK, et al. Electronic consultations (E-consults): advancing infectious disease care in a large Veterans Affairs Healthcare System. Clin Infect Dis. 2017;64(8):1123-1125. doi:10.1093/cid/cix058
12. Williams KM, Kirsh S, Aron D, et al. Evaluation of the Veterans Health Administration’s Specialty Care Transformational Initiatives to promote patient-centered delivery of specialty care: a mixed-methods approach. Telemed J E-Health. 2017;23(7):577-589. doi:10.1089/tmj.2016.0166
13. US Department of Veterans Affairs, Veterans Health Administration, Specialty Care Transformational Initiative Evaluation Center. Evaluation of specialty care initiatives. Published 2013.
14. Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323-330. doi:10.1177/1357633X15582108
15. Lee M, Leonard C, Greene P, et al. Perspectives of VA primary care clinicians toward electronic consultation-related workload burden. JAMA Netw Open. 2020;3(10):e2018104. Published 2020 Oct 1. doi:10.1001/jamanetworkopen.2020.18104
16. Deeds SA, Dowdell KJ, Chew LD, Ackerman SL. Implementing an opt-in eConsult program at seven academic medical centers: a qualitative analysis of primary care provider experiences. J Gen Intern Med. 2019;34(8):1427-1433. doi:10.1007/s11606-019-05067-7
17. Rodriguez KL, Burkitt KH, Bayliss NK, et al. Veteran, primary care provider, and specialist satisfaction with electronic consultation. JMIR Med Inform. 2015;3(1):e5. Published 2015 Jan 14. doi:10.2196/medinform.3725
18. Gupte G, Vimalananda V, Simon SR, DeVito K, Clark J, Orlander JD. Disruptive innovation: implementation of electronic consultations in a Veterans Affairs Health Care System. JMIR Med Inform. 2016;4(1):e6. Published 2016 Feb 12. doi:10.2196/medinform.4801
19. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008;34(4):228-243. doi:10.1016/s1553-7250(08)34030-6
20. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Sage Publications; 2002.
21. Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758-1772. doi:10.1111/j.1475-6773.2006.00684.x
22. Kim EJ, Orlander JD, Afable M, et al. Cardiology electronic consultation (e-consult) use by primary care providers at VA medical centres in New England. J Telemed Telecare. 2019;25(6):370-377. doi:10.1177/1357633X18774468