User login
Student Care Transitions Curriculum
There is increasing evidence that the transfer of medically complex patients across different settings can be associated with poor communication and patient dissatisfaction with the care received, potentially leading to negative clinical outcomes. While medical schools are beginning to introduce curricula on these transitions of care, few have been evaluated and subjected to peer review with the purpose of finding the most effective teaching and training methods.
Older adults and those with multiple chronic diseases frequently require medical care that spans multiple locations, and thus are most at risk for poor clinical outcomes during care transitions.1, 2 Medication errors and adverse drug reactions after hospital discharge are common.3, 4 Unsuccessful care transitions may also result in nonelective readmission after discharge, and there is evidence that readmissions may be a quality indicator for hospital care.57 Poor communication between patients and their healthcare providers is another element of poorly executed care transitions. Qualitative studies show that patients are frequently dissatisfied with the discharge process and are often unprepared to assume responsibility for their own care when they leave the hospital.8 Communication among providers can also be suboptimal. One meta‐analysis found that hospital physicians and primary care providers communicated infrequently and the availability of discharge summaries at the postdischarge visit was low, which may have affected the quality of care.9
Knowing that these gaps are common, there have been signs of increased emphasis on improving communication and working in teams as part of health professions training. The Institute of Medicine, in its 2003 report Health Professions Education: A Bridge to Quality,10 stressed education on management of chronic diseases, working in interdisciplinary teams, as well as a focus on quality improvement. In addition, the American Association of Medical Colleges (AAMC) encouraged training medical students on preparing safe discharge plans in its 2007 geriatrics competencies.11
Some medical schools have introduced care transitions curricula, though few have published data on their effectiveness. A search for teaching products using care transitions or transitional care on the online educational portals POGOe (Portal of Geriatric Online Education) and MedEdPortal yielded a total of 7 unique sets of teaching materials on care transitions for medical students.1218 However, a search on PubMed in July 2010 for peer‐reviewed articles on care transitions curricula developed for medical students which contained evaluation data only yielded 3 articles.1921 These 3 curricula, written by Bray‐Hall et al., Lai et al., and Ouchida et al., respectively, all trained third‐year medical students on diverse aspects of the discharge process using methods such as lectures, workshops, and patient visits, and showed favorable skill and knowledge outcomes.
Recognizing the importance of care transitions in medical education, a new curriculum addressing this topic was developed and introduced for fourth‐year medical students at the Emory University School of Medicine in 2009. The broad goal for this module was to develop a course concentrating on concrete skills that would train students to perform better care transitions while minimizing the time they had to spend away from a busy Internal Medicine sub‐internship. This curriculum used a mixed approach that included face‐to‐face teaching with faculty, online didactic instruction and interaction, and direct patient care. The course objectives were for students to develop a working fund of knowledge on care transitions, to learn to write a complete discharge summary, and to communicate the elements of a safe discharge plan. This article will describe the implementation of this curriculum and its evaluation.
METHODS
The Emory Care Transitions Curriculum started in August 2009 with fourth‐year medical students at the Emory University School of Medicine. This section will describe the details of the implementation of this curriculum, as well as the evaluation methodology and results.
Overview
This module was offered to Emory medical students participating in a required Senior Medicine rotation during their fourth year. The study population consisted of the 121 fourth‐year Emory medical students who participated in this rotation during the academic year that started in August 2009 and ended in April 2010. Students participated in the rotation at 1 of 3 teaching sites: Grady Memorial Hospital (GMH), Emory University Hospital (EUH), and the Atlanta VA Medical Center (AVAMC); 98 students completed their rotation at GMH, 12 at EUH, and 11 at AVAMC. For all online activities, students used the Blackboard platform software, available to them at
Course Description
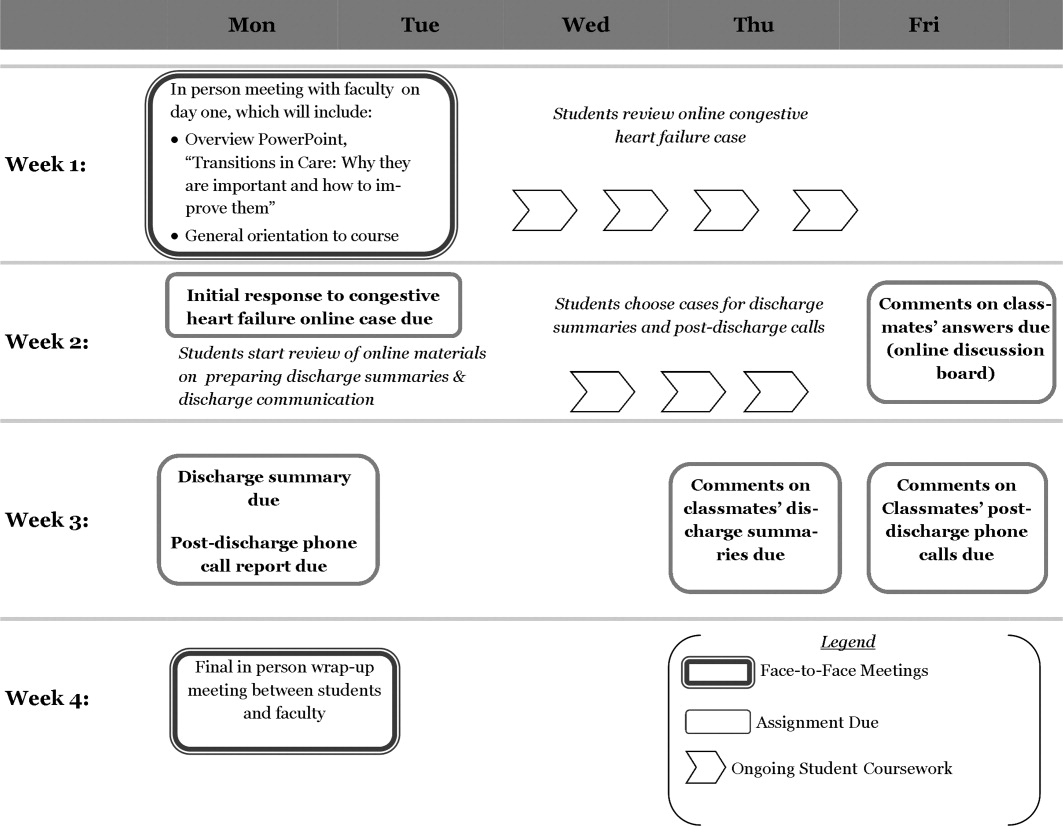
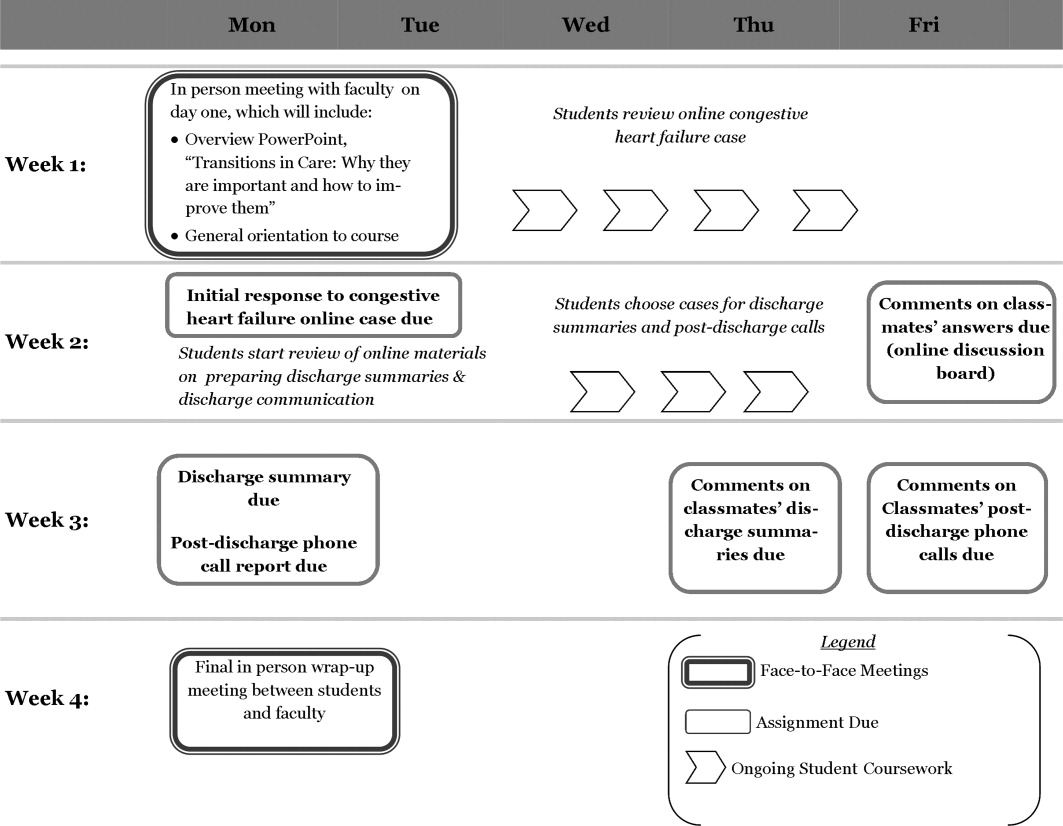
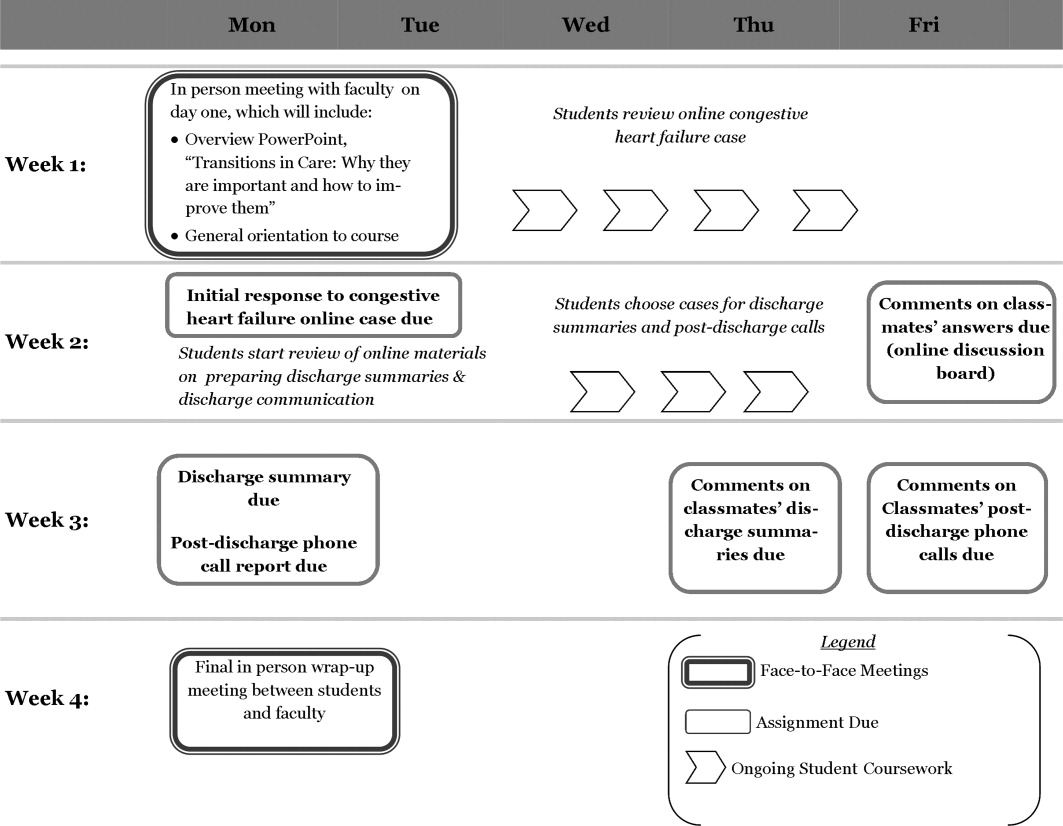
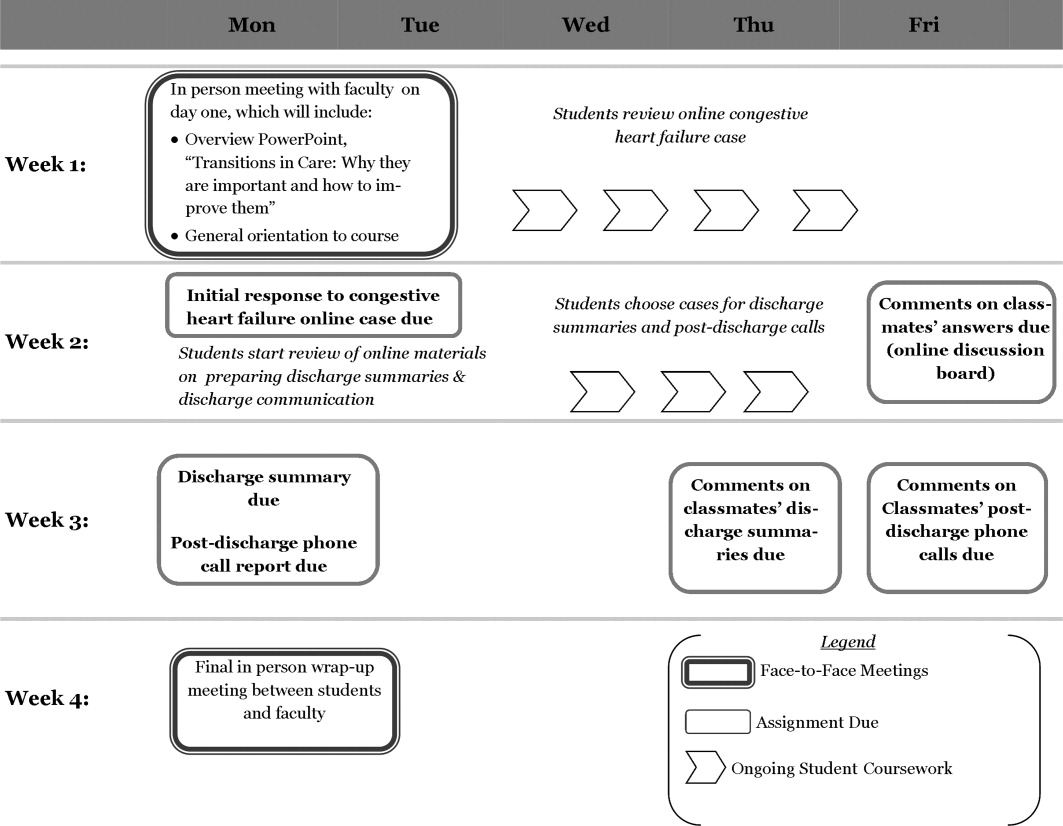
The course consisted of 3 components, each associated with specific student assignments: a slide presentation on care transitions with an associated case discussion, training on discharge summaries, and the execution of a postdischarge phone call. Figure 1 describes the course delivery schedule.
Slide Presentation and Case Discussion
This section started on day 2 of the clerkship, with a face‐to‐face lecture titled Transitions of Care: Why They Are Important, and How to Improve Them. It included the following components: definition of the different posthospital discharge options, explanation of the reasons for the complexity of care transitions in high‐risk patient populations, and an enumeration of methods to improve the safety of care transitions. Students also read a review article on the topic to further add to their fund of knowledge.23
The second part of the section involved discussion of a case posted on Blackboard (a discussion board) designed to highlight some of the challenges associated with care transitions. The case included 2 successive discharge summaries for an elderly patient with congestive heart failure: 1 for the initial exacerbation, and the other for a readmission. Using an online discussion board, students were asked to report the strong points and shortcomings of the patient's management, as well as those of the discharge summaries. Then the students were asked to post responses to at least 2 of their classmates' reports on the discussion board.
Training on Discharge Summaries
During the module, students received training on how to prepare a complete and informative discharge summary. This online training consisted of a lecture prepared by a faculty member (M.A.E.) and the use of a discharge summary template based on a guide prepared by the Boston Association of Academic Hospitalists (BAAHM), which is part of a toolkit available from the Society of Hospital Medicine.24 After reading the lecture, each student selected 1 of the patients they cared for during their rotation, and wrote a discharge summary. They posted it to a Blackboard discussion board, and were then asked to comment on one of their classmates' reports on the same forum. Faculty (M.A.E. and R.C.) also gave online feedback to each student about their discharge summary.
Postdischarge Phone Call
Students were also assigned to communicate with the patient for whom they prepared a discharge summary by performing a postdischarge phone call within a week of the patient's departure from the hospital. They reviewed a discharge checklist adapted from Ideal Discharge for an Elderly Patient: A Hospitalist Checklist, issued by the Society of Hospital Medicine.25 This document contains the necessary elements of a safe discharge plan, and used these points as the basis of the patient phone interview. The goal of the call and the use of the checklist was to reinforce the main elements of communication with patients that need to occur before they leave the hospital.
Students then used the checklist as the basis for a short (<400 words) report discussing the strong points and shortcomings of their patient's discharge, and posted it on a Blackboard discussion board. They were also asked to comment on at least one of their classmates' reports on the board. Faculty (M.A.E. and R.C.) also participated in the discussion board, commenting at least once on all students' reports.
Evaluation
The course was evaluated in order to assess changes in skills, knowledge and attitudes, as well as satisfaction with the course.
Evaluation Components
In order to assess the outcomes described above, questionnaires were utilized, and objective criteria were used to evaluate students' work. Students completed a pretest before the first face‐to‐face session, and a posttest after the second in‐person discussion. Pretest items were identical to those in the posttest, except that the posttest also contained 6 satisfaction questions. The components that were included in both pre‐ and posttests were:
Five multiple choice questions measuring students' confidence in their own skills regarding discharge summaries and transitional care (pre‐ and postsurvey). These 5 questions were adapted from the questionnaire developed by Lai et al.20 Confidence questionnaire items are detailed in Table 1.
Five multiple choice questions assessing students' attitudes regarding the importance of different components of the care transitions process (pre‐ and postsurvey). Attitude questionnaire items are detailed in Table 1.
Ten multiple choice questions in which each had one right answer, assessing students' knowledge base on transitional care issues (pre‐and postsurvey). Knowledge questions and their correct answers are detailed in Table 2.
| Mean Likert Scores* | P Value | ||
|---|---|---|---|
| Pre‐Course | Post‐Course | ||
| |||
| Confidence items | |||
| 1. I am confident in my ability to involve patients in making a plan for their care. | 3.8 | 4.2 | <0.001 |
| 2. I am confident in my ability to review patients' medications and side effects. | 3.4 | 4.1 | <0.001 |
| 3. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.4 | 4.3 | <0.001 |
| 4. I am confident in my ability to prepare a complete discharge summary. | 3.0 | 4.2 | <0.001 |
| 5. I can identify the different types of places that may serve as a setting for discharge from the inpatient setting. | 3.1 | 3.9 | <0.001 |
| Total confidence score (out of 25) | 16.7 | 20.7 | <0.001 |
| Attitude items | |||
| 1. A hospital physician should always communicate with a patient's primary care physician before that patient is discharged from the hospital, in order to ensure a smooth transition of care. | 4.0 | 4.1 | 0.78 |
| 2. Before a patient is discharged from the hospital, a physician (not just the nurse or case manager) should always meet with the patient to discuss his medications, and goals of care. | 4.4 | 4.4 | 0.50 |
| 3. It is critical for a primary care physician to have access to a discharge summary when seeing a patient for the first time after leaving the hospital. | 4.6 | 4.7 | 0.25 |
| 4. The main reason patients often don't take their medications properly after discharge is that they are confused by the instructions given to them at the hospital. | 3.7 | 3.8 | 0.65 |
| 5. Avoiding rehospitalization should be a top priority for physicians in the process of discharge from the hospital. | 4.1 | 4.3 | 0.95 |
| Total attitude score (out of 25) | 20.8 | 21.3 | 0.07 |
| Percent Correct | |||
|---|---|---|---|
| Question (Correct Answer in Parenthesis) | Pre‐Course | Post‐Course | P Value |
| |||
| 1. When a patient is discharged with home health care, which of the following services is usually not part of the package? (A caregiver to sit with the patient and supervise them most of the day.) | 70 | 83 | 0.020* |
| 2. When a patient is discharged from the hospital to a skilled nursing facility (SNF) for further care, which of these is a service that is typically provided? (Physical therapy.) | 78 | 75 | 0.649 |
| 3. Which of the following rehabilitation activities is more likely to be in the job description of an occupational therapist? (Training of strength in upper extremities.) | 24 | 51 | <0.001* |
| 4. Which of these is least likely to be a cause of poor patient outcomes after hospital discharge? (The discharging of patients to skilled nursing facilities.) | 93 | 97 | 0.166 |
| 5. Which of these is more likely to be an indicator of poor outcomes after hospital discharge? (Having had 3 hospitalizations in the last 6 months.) | 93 | 96 | 0.287 |
| 6. Which of these data is the least likely to be an indicator that the patient is too sick to be discharged from the hospital? (Hemoglobin concentration of 9.5 g/dl.) | 45 | 74 | <0.001* |
| 7. Which of the following medications would merit the most time spent on communication with patients, family members, and receiving physicians? (Furosemide.) | 58 | 96 | <0.001* |
| 8. You are caring for an 89‐year‐old man who is being treated in the hospital for an exacerbation of his congestive heart failure (CHF). He is doing well, ambulating 100 feet without shortness of breath, and is showing understanding of the need for all his different medications. However, he is not yet back to his functional baseline. Which of the following is the LEAST appropriate setting for discharge? (Hospice care.) | 74 | 70 | 0.458 |
| 9. Which of the following is true about skilled nursing facility (SNF) care? (Patients can be admitted for treatment with IV antibiotics for several weeks.) | 52 | 79 | <0.001* |
| 10. Educating patients at discharge about their illness and medication has been found to help decrease readmission rates. (True.) | 97 | 100 | 0.045 |
| Percentage of total questions correct | 68 | 82 | <0.001* |
The questionnaire items were developed by study faculty (M.A.E. and J.M.F.) and were edited in consultation with clinical faculty members from outside Emory with experience developing care transitions curricula: Dr. Karin Ouchida of Montefiore Medical Center in New York City, and Dr. William Lyons of the University of Nebraska Medical Center.
The 6 posttest items addressed student satisfaction with individual course components, which were: the heart failure online case, training on preparing discharge summaries, initial in‐person slide presentation, postdischarge phone call, overall online discussion across all items, and finally, satisfaction with the overall course. Questionnaire items on comfort, attitudes, and satisfaction all used a five‐point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The 10 multiple‐choice questions on knowledge each had one right answer.
Each student completed one discharge summary during the course. For it to be deemed satisfactory, it had to have the 5 following components, all present in the BAAHM template24:
A documented discharge medication list with specific dosing schedules.
Lists of admission medications and/or a list of medication changes during hospitalization.
A discharge plan that specifies the next setting of care, as well as the planned follow‐up.
A hospital course organized by system and/or specific chronology.
A physical exam, laboratory tests, and diagnostic studies performed on admission.
Student reports of their postdischarge phone call were also evaluated by study faculty (M.A.E. and R.C.). For the report of the interview to be considered satisfactory, it had to contain at least the following 2 elements:
A discussion of the patient's medication list, including documentation of a discussion of hazardous medications (e.g., furosemide, warfarin, digoxin, insulin) if applicable.
Documentation of a discussion on follow‐up plans with a primary physician or specialist.
Data Analysis
Outcomes were evaluated based on the results of pre‐ and posttest questionnaires, in addition to the satisfactoriness of discharge summaries and postdischarge phone call reports. As for the questionnaires, 4 types of scores were analyzed based on students' questionnaire responses:
Skills Confidence Score: The sum of Likert scores for confidence items on the pre‐ and posttest was the confidence score, with a highest possible score of 25, in which the highest scores were associated with the most confidence in executing the discharge process.
Attitude Score: The sum of Likert scores for attitude items on the pre‐ and posttest was the attitude score, with a highest possible score of 25, in which the highest scores were associated with student attitudes ascribing the most importance to a safe discharge process.
Knowledge Score: The percentage of total correct answers on knowledge questions on the pre‐ and posttest were used to obtain the knowledge score, in which a score of 100 was highest.
Satisfaction Score: Satisfaction questions on the posttest questionnaire were analyzed separately to assess satisfaction with each component of the curriculum, ranging from poor (score = 1) to excellent (score = 5). We also determined the percentage of students who rated each portion of the course good or better.
In addition to questionnaire scores, students' performance in the preparation of discharge summaries and the postdischarge phone interview were evaluated. Discharge summaries and postdischarge phone interviews were classified as satisfactory or unsatisfactory based on the criteria outlined in the previous section on outcome evaluation.
Quantitative and Qualitative Analysis
Skills confidence, attitude, and knowledge scores were compared between pre‐ and posttest. Paired t tests were used to calculate statistical significance. A P value below 0.05 was considered statistically significant, using two‐tailed tests.
We also analyzed whether there were any differences in changes in confidence, attitude, and knowledge scores according to the time of year in which the course was taken by students. For this, we divided the nine‐month course into 3 trimesters (AugustOctober, NovemberJanuary, and FebruaryApril). In order to determine whether 3 were any differences in score changes among the different periods, we used a one‐way analysis of variance (ANOVA), in which a P value below 0.05 would indicate a statistically significant difference among the periods. All statistical analyses were performed using SPSS 17.0 for Windows.
Statistical tests were not utilized for the satisfaction scores, but the overall goal was for their mean to be 3 (good) or above. Also, the percentages of satisfactory discharge summaries and postdischarge phone interviews were measured. The goal was for both tasks to have a percentage of satisfactory evaluations of 80% or above.
RESULTS
The 121 students who took the module completed both the pre‐ and posttests. Table 1 details the mean pre‐ and posttest Likert scores for all confidence and attitude questions, as well as the changes in the 25‐point total confidence and attitude score from pre‐ to posttest. The change in confidence scores among survey participants was statistically significant (P < 0.001), while the change in attitude score was not (P = 0.07). Table 2 compares the percentage of correct answers before and after the course for individual knowledge questions, as well as for the entire knowledge quiz. Changes in total knowledge scores were statistically significant: the mean percentage of correct answers out of 10 questions was 68% on the pretest, and 82% on the posttest (P < 0.001).
Table 3 measures the changes in confidence, attitude, and knowledge scores by the period of the year in which students took the course. One‐way ANOVA tests for each of the 3 domains did not find statistically significant changes in confidence, attitude, or knowledge scores among the 3 trimesters in which we divided the module's calendar.
| Section of Questionnaire | Total for Year | Period of Year | F Value | P Value | ||
|---|---|---|---|---|---|---|
| AugustOctober | NovemberJanuary | FebruaryApril | ||||
| Confidence | ||||||
| Mean pre‐course score | 16.7 | 16.5 | 16.5 | 17.0 | ||
| Mean post‐course score | 20.7 | 21.0 | 19.9 | 21.0 | ||
| Mean change in score | 4.0 | 4.5 | 3.4 | 4.0 | 0.92 | 0.40 |
| Attitude | ||||||
| Mean pre‐course score | 20.8 | 20.9 | 20.5 | 20.6 | ||
| Mean post‐course score | 21.3 | 21.3 | 21.3 | 21.1 | ||
| Mean change in score | 0.5 | 0.4 | 0.8 | 0.5 | 0.13 | 0.88 |
| Knowledge | ||||||
| Mean pre‐course percentage correct | 68 | 71.3 | 67.4 | 66.4 | ||
| Mean post‐course percentage correct | 82 | 82.5 | 80.9 | 82.1 | ||
| Mean change in score | 14 | 11.2 | 13.5 | 15.7 | 0.60 | 0.55 |
| No. of participants | 121 | 40 | 34 | 47 | ||
Table 4 shows satisfaction scores on the posttest. The overall Likert rating for the course was 3.9, with 97.5% of students rating it good or better. The highest‐rated individual component of the course by Likert score was the training on discharge summaries, with a rating of 4.1. The lowest‐rated by this parameter was the congestive heart failure case, with a rating of 3.6. The online discussion across all topics had the lowest percentage of students rating it good or above, at 83.5%.
| Curriculum Section | Mean Likert Rating (Out of 5) | Percentage Rated Good or Above |
|---|---|---|
| Congestive heart failure case | 3.6 | 95.0 |
| Discharge summaries | 4.1 | 96.7 |
| Initial in‐person slide presentation | 4.0 | 97.5 |
| Postdischarge phone call | 3.7 | 95.0 |
| Online discussion for all topics | 3.7 | 83.5 |
| Overall curriculum rating | 3.9 | 97.5 |
As for student discharge summaries, 109 out of 121 (90.1%) met all the criteria in order to be deemed satisfactory; 109 out of 121 (90.1%) of postdischarge phone call reports met both required components. Both these results exceeded the goal of 80% set before the course started.
DISCUSSION
The Emory Care Transitions Curriculum for fourth‐year medical students started in the 20092010 academic year with the main goal of teaching students transferable skills that would ultimately lead to their participating in safer hospital discharges in their future practice as physicians. At the end of this course, students exhibited greater confidence in managing the discharge process, improved overall fund of knowledge relating to care transitions, and a demonstration of appropriate skills related to preparing discharge summaries and communicating with patients at discharge. This was all executed with a delivery method that students found engaging.
Analyzing the results, it is noteworthy that confidence improved, while attitudes did not. Even though confidence in performing a task does not necessarily reflect one's ability to perform it, our students' confidence scores may serve as a proxy for their ability to manage tasks related to the discharge process, like managing medications and preparing discharge summaries. Thus, while some studies suggest that self‐assessment among physicians may not always relate well to competence,26, 27 in our study, students did demonstrate skills in discharge summary preparation and in identifying the most relevant aspects of patient communication at hospital discharge. As for the absence of attitude change, this may have partly been a function of the fact that students in our group started with attitude scores that were already quite high, with a mean pretest attitude score of 20.7 out of 25.
Changes in student confidence, attitudes, and knowledge from pre‐ to posttest did not vary significantly across the academic year. Thus, one could interpret from our findings that more experienced students who took the module close to graduation benefited similarly from the course to those who completed it earlier, at least according to those rubrics. Another possible source of variation in student experience was the hospital in which students rotated: the demographics of GMH, with its large uninsured population; AVAMC, with more elderly patients; and EUH, with a more affluent profile, are certainly different. However, the number of students rotating at EUH and AVAMC were comparatively too small to attempt to draw any conclusions about how rotation site affected student experiences.
The use of a blended approach that integrated face‐to‐face didactics, patient care, and online learning offered some advantages. Curricular goals were achieved through a course that required only 2 hours of in‐person faculty time with students. This is significant, considering the time demands that academic medical faculty usually face. This approach also permitted students who were participating in a busy clinical rotation, and had limited opportunities to meet as a group, the ability to do coursework at their own pace. Another strength of the study is that all students who participated in the rotation were able to complete their surveys.
As for limitations, it is worth noting that in a course with a blended curriculum, the online discussion had the lowest percentage of students rating it good or better. Part of the perceived difficulty may have resulted from the fact that there are no other courses in the Emory medical curriculum that utilize discussion boards or distance learning methods as teaching tools. Despite this generation of students' technological savvy, this new mode of discussion may have proven difficult to pick up when they were in the midst of a busy clinical rotation. This serves as a reminder that while online curricula have proven successful in this and other settings, each element needs to be tailored to the audience. One other factor to be considered while interpreting this study's results is that this study utilized some survey instruments that have not been previously validated, even though they were developed in consultation with experts in the field of care transitions education.
We used a dichotomous, criteria‐based system to rate students' discharge summaries and reports of postdischarge phone calls. While this quantitative approach allowed us to more objectively define the quality of students' work, it did offer some disadvantages. First, even though we based the rating system for discharge summaries on a BAAHM template, it was not subjected to more extensive validation. Moreover, the quantitative approach diverted us from finding themes and other qualitative data from students' write‐ups, which could potentially have given us a fuller picture of their work.
This study contributes to the small, but growing, literature on care transitions education. The studies by Bray‐Hall et al., Lai et al., and Ouchida et al.,1921 used different methodologies, but all were directed at third‐year students using curricula with classroom and clinical learning, and showed favorable outcomes in knowledge and skills. The present study also showed positive results in students' knowledge and skills, but targeted it toward graduating medical students and included a focus on concrete skills, such as discharge summary preparation. It also utilized a nontraditional delivery approach which reached its objectives while also limiting the demands on faculty and students' face time during busy clinical rotations, which is especially important when considering that students were dispersed at multiple sites.
It is likely that medical schools will implement more care transitions curricula in coming years, as organizations like the AAMC11 and the Institute of Medicine10 increase the pressure to train future doctors to better address the needs of older and chronically ill patients, who require care from professionals of multiple disciplines, in disparate care settings. Moreover, the 2010 Patient Protection and Affordable Care Act28 contains provisions with financial incentives for hospitals to decrease readmissions. Once these become widely implemented, there will be a greater impetus to train medical practitioners to discharge patients more safely. When that occurs, medical schools will have additional compelling reasons to offer courses that teach students skills to execute better care transitions. The hoped‐for outcome of these curricula will ultimately be safer and more effective patient care.
Acknowledgements
The authors thank Dr. Ted Johnson at the Emory University School of Medicine for editorial review. They also express their gratitude to Dr. Karin Ouchida at Montefiore Medical Center and Dr. William Lyons at University of Nebraska Medical Center for their technical support in preparation of the curriculum. Disclosures: None of the authors has any relevant conflicts of interest. All coauthors have seen and agree with the contents of this manuscript. The authors are responsible for the integrity of the data described in this study. The research in this manuscript has not been submitted or accepted for publication in another journal.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,.Adverse drug events in elderly patients receiving home health services following hospital discharge.Ann Pharmacother.1999;33:1147–1153.
- ,,,,.The association between the quality of inpatient care and early readmission: A meta‐analysis of the evidence.Med Care.1997;35(10):1044–1059.
- ,,,,.The association between the quality of inpatient care and early readmission.Ann Intern Med.1995;122(6):415–421.
- ,.Hospital readmissions as a measure of quality of health care: Advantages and limitations.Arch Intern Med.2000;160(8):1074–1081.
- ,.Lost in transition: Challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;140:533–536.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians.JAMA.2007;297:831–841.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington, DC:National Academy Press;2003.
- American Association of Medical Colleges. Geriatric Competencies for Medical Students: Recommendations of the July 2007 Geriatrics Consensus Conference.2008. Available at: http://www.aamc.org/newsroom/press kits/competencies.pdf. Accessed February 25, 2009.
- Eskildsen M, Price T, Tenover JL. Computer‐based geriatrics workbooks for resident teaching. MedEdPortal. 2007. Available at http://services. aamc.org/30/mededportal/servlet/s/segment/mededportal/ find_resources/ browse/?subid=640.
- .Care transitions in the older adult.MedEdPortal.2008. Available at http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/find_resources/browse/?subid=678. Accessed March 19, 2011.
- ,,, et al.Web‐based module to train and assess competency in systems‐based practice.Portal of Online Geriatric Education.2009. Product ID #20002. Available at: http://www. pogoe.org/node/407. Accessed March 19, 2011.
- .CHAMP (Curriculum for the Hospitalized Aging Medical Patient): The ideal hospital discharge.Portal of Online Geriatric Education.2009. Product ID #18995. Available at: http://www. pogoe.org/productid/18995. Accessed March 19, 2011.
- .M1 care transitions.Portal of Online Geriatric Education.2009. Product ID #20450. Available at: http://www. pogoe.org/node/660. Accessed March 19, 2011.
- .Transitional care.Portal of Online Geriatric Education.2007. Product ID #18991. Available at: http://www.pogoe.org/node/262. Accessed March 19, 2011.
- .Discharge summary feedback.Portal of Online Geriatric Education.2009. Product ID #20546. Available at: http://www.pogoe.org/node/788. Accessed March 19, 2011.
- ,,.Toward safe hospital discharge: A transitions in care curriculum for medical students.J Gen Intern Med.25(8):878–881.
- ,,,,.Postdischarge follow‐up visits for medical and pharmacy students on an inpatient medicine clerkship.J Hosp Med.2008;3(1):20–27.
- ,,,,.Fast forward rounds: An effective method for teaching medical students to transition patients safely across care settings.J Am Geriatr Soc.2009;57:910–917.
- .Fourth‐year medical student care transitions curriculum (free login required).Portal of Online Geriatric Education.2010. Available at: http://www.pogoe.org/node/867. Accessed July 16, 2010.
- .Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- Society of Hospital Medicine. Quality initiatives for patient care—BOOSTing care transitions resource room.2010. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_Care Transitions/html_CC/12Clinical Tools/01_Toolkits.cfm. Accessed November 16, 2010.
- Society of Hospital Medicine. Ideal discharge for an elderly patient: A hospitalist checklist.2005. Available at: http://www.hospitalmedicine. org/AM/Template.cfm?Section=QI_Clinical_Tools8(2):105–110.
- ,,.Difficulties in recognizing one's own incompetence: Novice physicians who are unskilled and unaware of it.Acad Med.2001;76(10 suppl):S87–S89.
- Patient Protection and Affordable Care Act, H.R. 3590.ENR, 111th Congress, 2010.
There is increasing evidence that the transfer of medically complex patients across different settings can be associated with poor communication and patient dissatisfaction with the care received, potentially leading to negative clinical outcomes. While medical schools are beginning to introduce curricula on these transitions of care, few have been evaluated and subjected to peer review with the purpose of finding the most effective teaching and training methods.
Older adults and those with multiple chronic diseases frequently require medical care that spans multiple locations, and thus are most at risk for poor clinical outcomes during care transitions.1, 2 Medication errors and adverse drug reactions after hospital discharge are common.3, 4 Unsuccessful care transitions may also result in nonelective readmission after discharge, and there is evidence that readmissions may be a quality indicator for hospital care.57 Poor communication between patients and their healthcare providers is another element of poorly executed care transitions. Qualitative studies show that patients are frequently dissatisfied with the discharge process and are often unprepared to assume responsibility for their own care when they leave the hospital.8 Communication among providers can also be suboptimal. One meta‐analysis found that hospital physicians and primary care providers communicated infrequently and the availability of discharge summaries at the postdischarge visit was low, which may have affected the quality of care.9
Knowing that these gaps are common, there have been signs of increased emphasis on improving communication and working in teams as part of health professions training. The Institute of Medicine, in its 2003 report Health Professions Education: A Bridge to Quality,10 stressed education on management of chronic diseases, working in interdisciplinary teams, as well as a focus on quality improvement. In addition, the American Association of Medical Colleges (AAMC) encouraged training medical students on preparing safe discharge plans in its 2007 geriatrics competencies.11
Some medical schools have introduced care transitions curricula, though few have published data on their effectiveness. A search for teaching products using care transitions or transitional care on the online educational portals POGOe (Portal of Geriatric Online Education) and MedEdPortal yielded a total of 7 unique sets of teaching materials on care transitions for medical students.1218 However, a search on PubMed in July 2010 for peer‐reviewed articles on care transitions curricula developed for medical students which contained evaluation data only yielded 3 articles.1921 These 3 curricula, written by Bray‐Hall et al., Lai et al., and Ouchida et al., respectively, all trained third‐year medical students on diverse aspects of the discharge process using methods such as lectures, workshops, and patient visits, and showed favorable skill and knowledge outcomes.
Recognizing the importance of care transitions in medical education, a new curriculum addressing this topic was developed and introduced for fourth‐year medical students at the Emory University School of Medicine in 2009. The broad goal for this module was to develop a course concentrating on concrete skills that would train students to perform better care transitions while minimizing the time they had to spend away from a busy Internal Medicine sub‐internship. This curriculum used a mixed approach that included face‐to‐face teaching with faculty, online didactic instruction and interaction, and direct patient care. The course objectives were for students to develop a working fund of knowledge on care transitions, to learn to write a complete discharge summary, and to communicate the elements of a safe discharge plan. This article will describe the implementation of this curriculum and its evaluation.
METHODS
The Emory Care Transitions Curriculum started in August 2009 with fourth‐year medical students at the Emory University School of Medicine. This section will describe the details of the implementation of this curriculum, as well as the evaluation methodology and results.
Overview
This module was offered to Emory medical students participating in a required Senior Medicine rotation during their fourth year. The study population consisted of the 121 fourth‐year Emory medical students who participated in this rotation during the academic year that started in August 2009 and ended in April 2010. Students participated in the rotation at 1 of 3 teaching sites: Grady Memorial Hospital (GMH), Emory University Hospital (EUH), and the Atlanta VA Medical Center (AVAMC); 98 students completed their rotation at GMH, 12 at EUH, and 11 at AVAMC. For all online activities, students used the Blackboard platform software, available to them at
Course Description
The course consisted of 3 components, each associated with specific student assignments: a slide presentation on care transitions with an associated case discussion, training on discharge summaries, and the execution of a postdischarge phone call. Figure 1 describes the course delivery schedule.
Slide Presentation and Case Discussion
This section started on day 2 of the clerkship, with a face‐to‐face lecture titled Transitions of Care: Why They Are Important, and How to Improve Them. It included the following components: definition of the different posthospital discharge options, explanation of the reasons for the complexity of care transitions in high‐risk patient populations, and an enumeration of methods to improve the safety of care transitions. Students also read a review article on the topic to further add to their fund of knowledge.23
The second part of the section involved discussion of a case posted on Blackboard (a discussion board) designed to highlight some of the challenges associated with care transitions. The case included 2 successive discharge summaries for an elderly patient with congestive heart failure: 1 for the initial exacerbation, and the other for a readmission. Using an online discussion board, students were asked to report the strong points and shortcomings of the patient's management, as well as those of the discharge summaries. Then the students were asked to post responses to at least 2 of their classmates' reports on the discussion board.
Training on Discharge Summaries
During the module, students received training on how to prepare a complete and informative discharge summary. This online training consisted of a lecture prepared by a faculty member (M.A.E.) and the use of a discharge summary template based on a guide prepared by the Boston Association of Academic Hospitalists (BAAHM), which is part of a toolkit available from the Society of Hospital Medicine.24 After reading the lecture, each student selected 1 of the patients they cared for during their rotation, and wrote a discharge summary. They posted it to a Blackboard discussion board, and were then asked to comment on one of their classmates' reports on the same forum. Faculty (M.A.E. and R.C.) also gave online feedback to each student about their discharge summary.
Postdischarge Phone Call
Students were also assigned to communicate with the patient for whom they prepared a discharge summary by performing a postdischarge phone call within a week of the patient's departure from the hospital. They reviewed a discharge checklist adapted from Ideal Discharge for an Elderly Patient: A Hospitalist Checklist, issued by the Society of Hospital Medicine.25 This document contains the necessary elements of a safe discharge plan, and used these points as the basis of the patient phone interview. The goal of the call and the use of the checklist was to reinforce the main elements of communication with patients that need to occur before they leave the hospital.
Students then used the checklist as the basis for a short (<400 words) report discussing the strong points and shortcomings of their patient's discharge, and posted it on a Blackboard discussion board. They were also asked to comment on at least one of their classmates' reports on the board. Faculty (M.A.E. and R.C.) also participated in the discussion board, commenting at least once on all students' reports.
Evaluation
The course was evaluated in order to assess changes in skills, knowledge and attitudes, as well as satisfaction with the course.
Evaluation Components
In order to assess the outcomes described above, questionnaires were utilized, and objective criteria were used to evaluate students' work. Students completed a pretest before the first face‐to‐face session, and a posttest after the second in‐person discussion. Pretest items were identical to those in the posttest, except that the posttest also contained 6 satisfaction questions. The components that were included in both pre‐ and posttests were:
Five multiple choice questions measuring students' confidence in their own skills regarding discharge summaries and transitional care (pre‐ and postsurvey). These 5 questions were adapted from the questionnaire developed by Lai et al.20 Confidence questionnaire items are detailed in Table 1.
Five multiple choice questions assessing students' attitudes regarding the importance of different components of the care transitions process (pre‐ and postsurvey). Attitude questionnaire items are detailed in Table 1.
Ten multiple choice questions in which each had one right answer, assessing students' knowledge base on transitional care issues (pre‐and postsurvey). Knowledge questions and their correct answers are detailed in Table 2.
| Mean Likert Scores* | P Value | ||
|---|---|---|---|
| Pre‐Course | Post‐Course | ||
| |||
| Confidence items | |||
| 1. I am confident in my ability to involve patients in making a plan for their care. | 3.8 | 4.2 | <0.001 |
| 2. I am confident in my ability to review patients' medications and side effects. | 3.4 | 4.1 | <0.001 |
| 3. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.4 | 4.3 | <0.001 |
| 4. I am confident in my ability to prepare a complete discharge summary. | 3.0 | 4.2 | <0.001 |
| 5. I can identify the different types of places that may serve as a setting for discharge from the inpatient setting. | 3.1 | 3.9 | <0.001 |
| Total confidence score (out of 25) | 16.7 | 20.7 | <0.001 |
| Attitude items | |||
| 1. A hospital physician should always communicate with a patient's primary care physician before that patient is discharged from the hospital, in order to ensure a smooth transition of care. | 4.0 | 4.1 | 0.78 |
| 2. Before a patient is discharged from the hospital, a physician (not just the nurse or case manager) should always meet with the patient to discuss his medications, and goals of care. | 4.4 | 4.4 | 0.50 |
| 3. It is critical for a primary care physician to have access to a discharge summary when seeing a patient for the first time after leaving the hospital. | 4.6 | 4.7 | 0.25 |
| 4. The main reason patients often don't take their medications properly after discharge is that they are confused by the instructions given to them at the hospital. | 3.7 | 3.8 | 0.65 |
| 5. Avoiding rehospitalization should be a top priority for physicians in the process of discharge from the hospital. | 4.1 | 4.3 | 0.95 |
| Total attitude score (out of 25) | 20.8 | 21.3 | 0.07 |
| Percent Correct | |||
|---|---|---|---|
| Question (Correct Answer in Parenthesis) | Pre‐Course | Post‐Course | P Value |
| |||
| 1. When a patient is discharged with home health care, which of the following services is usually not part of the package? (A caregiver to sit with the patient and supervise them most of the day.) | 70 | 83 | 0.020* |
| 2. When a patient is discharged from the hospital to a skilled nursing facility (SNF) for further care, which of these is a service that is typically provided? (Physical therapy.) | 78 | 75 | 0.649 |
| 3. Which of the following rehabilitation activities is more likely to be in the job description of an occupational therapist? (Training of strength in upper extremities.) | 24 | 51 | <0.001* |
| 4. Which of these is least likely to be a cause of poor patient outcomes after hospital discharge? (The discharging of patients to skilled nursing facilities.) | 93 | 97 | 0.166 |
| 5. Which of these is more likely to be an indicator of poor outcomes after hospital discharge? (Having had 3 hospitalizations in the last 6 months.) | 93 | 96 | 0.287 |
| 6. Which of these data is the least likely to be an indicator that the patient is too sick to be discharged from the hospital? (Hemoglobin concentration of 9.5 g/dl.) | 45 | 74 | <0.001* |
| 7. Which of the following medications would merit the most time spent on communication with patients, family members, and receiving physicians? (Furosemide.) | 58 | 96 | <0.001* |
| 8. You are caring for an 89‐year‐old man who is being treated in the hospital for an exacerbation of his congestive heart failure (CHF). He is doing well, ambulating 100 feet without shortness of breath, and is showing understanding of the need for all his different medications. However, he is not yet back to his functional baseline. Which of the following is the LEAST appropriate setting for discharge? (Hospice care.) | 74 | 70 | 0.458 |
| 9. Which of the following is true about skilled nursing facility (SNF) care? (Patients can be admitted for treatment with IV antibiotics for several weeks.) | 52 | 79 | <0.001* |
| 10. Educating patients at discharge about their illness and medication has been found to help decrease readmission rates. (True.) | 97 | 100 | 0.045 |
| Percentage of total questions correct | 68 | 82 | <0.001* |
The questionnaire items were developed by study faculty (M.A.E. and J.M.F.) and were edited in consultation with clinical faculty members from outside Emory with experience developing care transitions curricula: Dr. Karin Ouchida of Montefiore Medical Center in New York City, and Dr. William Lyons of the University of Nebraska Medical Center.
The 6 posttest items addressed student satisfaction with individual course components, which were: the heart failure online case, training on preparing discharge summaries, initial in‐person slide presentation, postdischarge phone call, overall online discussion across all items, and finally, satisfaction with the overall course. Questionnaire items on comfort, attitudes, and satisfaction all used a five‐point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The 10 multiple‐choice questions on knowledge each had one right answer.
Each student completed one discharge summary during the course. For it to be deemed satisfactory, it had to have the 5 following components, all present in the BAAHM template24:
A documented discharge medication list with specific dosing schedules.
Lists of admission medications and/or a list of medication changes during hospitalization.
A discharge plan that specifies the next setting of care, as well as the planned follow‐up.
A hospital course organized by system and/or specific chronology.
A physical exam, laboratory tests, and diagnostic studies performed on admission.
Student reports of their postdischarge phone call were also evaluated by study faculty (M.A.E. and R.C.). For the report of the interview to be considered satisfactory, it had to contain at least the following 2 elements:
A discussion of the patient's medication list, including documentation of a discussion of hazardous medications (e.g., furosemide, warfarin, digoxin, insulin) if applicable.
Documentation of a discussion on follow‐up plans with a primary physician or specialist.
Data Analysis
Outcomes were evaluated based on the results of pre‐ and posttest questionnaires, in addition to the satisfactoriness of discharge summaries and postdischarge phone call reports. As for the questionnaires, 4 types of scores were analyzed based on students' questionnaire responses:
Skills Confidence Score: The sum of Likert scores for confidence items on the pre‐ and posttest was the confidence score, with a highest possible score of 25, in which the highest scores were associated with the most confidence in executing the discharge process.
Attitude Score: The sum of Likert scores for attitude items on the pre‐ and posttest was the attitude score, with a highest possible score of 25, in which the highest scores were associated with student attitudes ascribing the most importance to a safe discharge process.
Knowledge Score: The percentage of total correct answers on knowledge questions on the pre‐ and posttest were used to obtain the knowledge score, in which a score of 100 was highest.
Satisfaction Score: Satisfaction questions on the posttest questionnaire were analyzed separately to assess satisfaction with each component of the curriculum, ranging from poor (score = 1) to excellent (score = 5). We also determined the percentage of students who rated each portion of the course good or better.
In addition to questionnaire scores, students' performance in the preparation of discharge summaries and the postdischarge phone interview were evaluated. Discharge summaries and postdischarge phone interviews were classified as satisfactory or unsatisfactory based on the criteria outlined in the previous section on outcome evaluation.
Quantitative and Qualitative Analysis
Skills confidence, attitude, and knowledge scores were compared between pre‐ and posttest. Paired t tests were used to calculate statistical significance. A P value below 0.05 was considered statistically significant, using two‐tailed tests.
We also analyzed whether there were any differences in changes in confidence, attitude, and knowledge scores according to the time of year in which the course was taken by students. For this, we divided the nine‐month course into 3 trimesters (AugustOctober, NovemberJanuary, and FebruaryApril). In order to determine whether 3 were any differences in score changes among the different periods, we used a one‐way analysis of variance (ANOVA), in which a P value below 0.05 would indicate a statistically significant difference among the periods. All statistical analyses were performed using SPSS 17.0 for Windows.
Statistical tests were not utilized for the satisfaction scores, but the overall goal was for their mean to be 3 (good) or above. Also, the percentages of satisfactory discharge summaries and postdischarge phone interviews were measured. The goal was for both tasks to have a percentage of satisfactory evaluations of 80% or above.
RESULTS
The 121 students who took the module completed both the pre‐ and posttests. Table 1 details the mean pre‐ and posttest Likert scores for all confidence and attitude questions, as well as the changes in the 25‐point total confidence and attitude score from pre‐ to posttest. The change in confidence scores among survey participants was statistically significant (P < 0.001), while the change in attitude score was not (P = 0.07). Table 2 compares the percentage of correct answers before and after the course for individual knowledge questions, as well as for the entire knowledge quiz. Changes in total knowledge scores were statistically significant: the mean percentage of correct answers out of 10 questions was 68% on the pretest, and 82% on the posttest (P < 0.001).
Table 3 measures the changes in confidence, attitude, and knowledge scores by the period of the year in which students took the course. One‐way ANOVA tests for each of the 3 domains did not find statistically significant changes in confidence, attitude, or knowledge scores among the 3 trimesters in which we divided the module's calendar.
| Section of Questionnaire | Total for Year | Period of Year | F Value | P Value | ||
|---|---|---|---|---|---|---|
| AugustOctober | NovemberJanuary | FebruaryApril | ||||
| Confidence | ||||||
| Mean pre‐course score | 16.7 | 16.5 | 16.5 | 17.0 | ||
| Mean post‐course score | 20.7 | 21.0 | 19.9 | 21.0 | ||
| Mean change in score | 4.0 | 4.5 | 3.4 | 4.0 | 0.92 | 0.40 |
| Attitude | ||||||
| Mean pre‐course score | 20.8 | 20.9 | 20.5 | 20.6 | ||
| Mean post‐course score | 21.3 | 21.3 | 21.3 | 21.1 | ||
| Mean change in score | 0.5 | 0.4 | 0.8 | 0.5 | 0.13 | 0.88 |
| Knowledge | ||||||
| Mean pre‐course percentage correct | 68 | 71.3 | 67.4 | 66.4 | ||
| Mean post‐course percentage correct | 82 | 82.5 | 80.9 | 82.1 | ||
| Mean change in score | 14 | 11.2 | 13.5 | 15.7 | 0.60 | 0.55 |
| No. of participants | 121 | 40 | 34 | 47 | ||
Table 4 shows satisfaction scores on the posttest. The overall Likert rating for the course was 3.9, with 97.5% of students rating it good or better. The highest‐rated individual component of the course by Likert score was the training on discharge summaries, with a rating of 4.1. The lowest‐rated by this parameter was the congestive heart failure case, with a rating of 3.6. The online discussion across all topics had the lowest percentage of students rating it good or above, at 83.5%.
| Curriculum Section | Mean Likert Rating (Out of 5) | Percentage Rated Good or Above |
|---|---|---|
| Congestive heart failure case | 3.6 | 95.0 |
| Discharge summaries | 4.1 | 96.7 |
| Initial in‐person slide presentation | 4.0 | 97.5 |
| Postdischarge phone call | 3.7 | 95.0 |
| Online discussion for all topics | 3.7 | 83.5 |
| Overall curriculum rating | 3.9 | 97.5 |
As for student discharge summaries, 109 out of 121 (90.1%) met all the criteria in order to be deemed satisfactory; 109 out of 121 (90.1%) of postdischarge phone call reports met both required components. Both these results exceeded the goal of 80% set before the course started.
DISCUSSION
The Emory Care Transitions Curriculum for fourth‐year medical students started in the 20092010 academic year with the main goal of teaching students transferable skills that would ultimately lead to their participating in safer hospital discharges in their future practice as physicians. At the end of this course, students exhibited greater confidence in managing the discharge process, improved overall fund of knowledge relating to care transitions, and a demonstration of appropriate skills related to preparing discharge summaries and communicating with patients at discharge. This was all executed with a delivery method that students found engaging.
Analyzing the results, it is noteworthy that confidence improved, while attitudes did not. Even though confidence in performing a task does not necessarily reflect one's ability to perform it, our students' confidence scores may serve as a proxy for their ability to manage tasks related to the discharge process, like managing medications and preparing discharge summaries. Thus, while some studies suggest that self‐assessment among physicians may not always relate well to competence,26, 27 in our study, students did demonstrate skills in discharge summary preparation and in identifying the most relevant aspects of patient communication at hospital discharge. As for the absence of attitude change, this may have partly been a function of the fact that students in our group started with attitude scores that were already quite high, with a mean pretest attitude score of 20.7 out of 25.
Changes in student confidence, attitudes, and knowledge from pre‐ to posttest did not vary significantly across the academic year. Thus, one could interpret from our findings that more experienced students who took the module close to graduation benefited similarly from the course to those who completed it earlier, at least according to those rubrics. Another possible source of variation in student experience was the hospital in which students rotated: the demographics of GMH, with its large uninsured population; AVAMC, with more elderly patients; and EUH, with a more affluent profile, are certainly different. However, the number of students rotating at EUH and AVAMC were comparatively too small to attempt to draw any conclusions about how rotation site affected student experiences.
The use of a blended approach that integrated face‐to‐face didactics, patient care, and online learning offered some advantages. Curricular goals were achieved through a course that required only 2 hours of in‐person faculty time with students. This is significant, considering the time demands that academic medical faculty usually face. This approach also permitted students who were participating in a busy clinical rotation, and had limited opportunities to meet as a group, the ability to do coursework at their own pace. Another strength of the study is that all students who participated in the rotation were able to complete their surveys.
As for limitations, it is worth noting that in a course with a blended curriculum, the online discussion had the lowest percentage of students rating it good or better. Part of the perceived difficulty may have resulted from the fact that there are no other courses in the Emory medical curriculum that utilize discussion boards or distance learning methods as teaching tools. Despite this generation of students' technological savvy, this new mode of discussion may have proven difficult to pick up when they were in the midst of a busy clinical rotation. This serves as a reminder that while online curricula have proven successful in this and other settings, each element needs to be tailored to the audience. One other factor to be considered while interpreting this study's results is that this study utilized some survey instruments that have not been previously validated, even though they were developed in consultation with experts in the field of care transitions education.
We used a dichotomous, criteria‐based system to rate students' discharge summaries and reports of postdischarge phone calls. While this quantitative approach allowed us to more objectively define the quality of students' work, it did offer some disadvantages. First, even though we based the rating system for discharge summaries on a BAAHM template, it was not subjected to more extensive validation. Moreover, the quantitative approach diverted us from finding themes and other qualitative data from students' write‐ups, which could potentially have given us a fuller picture of their work.
This study contributes to the small, but growing, literature on care transitions education. The studies by Bray‐Hall et al., Lai et al., and Ouchida et al.,1921 used different methodologies, but all were directed at third‐year students using curricula with classroom and clinical learning, and showed favorable outcomes in knowledge and skills. The present study also showed positive results in students' knowledge and skills, but targeted it toward graduating medical students and included a focus on concrete skills, such as discharge summary preparation. It also utilized a nontraditional delivery approach which reached its objectives while also limiting the demands on faculty and students' face time during busy clinical rotations, which is especially important when considering that students were dispersed at multiple sites.
It is likely that medical schools will implement more care transitions curricula in coming years, as organizations like the AAMC11 and the Institute of Medicine10 increase the pressure to train future doctors to better address the needs of older and chronically ill patients, who require care from professionals of multiple disciplines, in disparate care settings. Moreover, the 2010 Patient Protection and Affordable Care Act28 contains provisions with financial incentives for hospitals to decrease readmissions. Once these become widely implemented, there will be a greater impetus to train medical practitioners to discharge patients more safely. When that occurs, medical schools will have additional compelling reasons to offer courses that teach students skills to execute better care transitions. The hoped‐for outcome of these curricula will ultimately be safer and more effective patient care.
Acknowledgements
The authors thank Dr. Ted Johnson at the Emory University School of Medicine for editorial review. They also express their gratitude to Dr. Karin Ouchida at Montefiore Medical Center and Dr. William Lyons at University of Nebraska Medical Center for their technical support in preparation of the curriculum. Disclosures: None of the authors has any relevant conflicts of interest. All coauthors have seen and agree with the contents of this manuscript. The authors are responsible for the integrity of the data described in this study. The research in this manuscript has not been submitted or accepted for publication in another journal.
There is increasing evidence that the transfer of medically complex patients across different settings can be associated with poor communication and patient dissatisfaction with the care received, potentially leading to negative clinical outcomes. While medical schools are beginning to introduce curricula on these transitions of care, few have been evaluated and subjected to peer review with the purpose of finding the most effective teaching and training methods.
Older adults and those with multiple chronic diseases frequently require medical care that spans multiple locations, and thus are most at risk for poor clinical outcomes during care transitions.1, 2 Medication errors and adverse drug reactions after hospital discharge are common.3, 4 Unsuccessful care transitions may also result in nonelective readmission after discharge, and there is evidence that readmissions may be a quality indicator for hospital care.57 Poor communication between patients and their healthcare providers is another element of poorly executed care transitions. Qualitative studies show that patients are frequently dissatisfied with the discharge process and are often unprepared to assume responsibility for their own care when they leave the hospital.8 Communication among providers can also be suboptimal. One meta‐analysis found that hospital physicians and primary care providers communicated infrequently and the availability of discharge summaries at the postdischarge visit was low, which may have affected the quality of care.9
Knowing that these gaps are common, there have been signs of increased emphasis on improving communication and working in teams as part of health professions training. The Institute of Medicine, in its 2003 report Health Professions Education: A Bridge to Quality,10 stressed education on management of chronic diseases, working in interdisciplinary teams, as well as a focus on quality improvement. In addition, the American Association of Medical Colleges (AAMC) encouraged training medical students on preparing safe discharge plans in its 2007 geriatrics competencies.11
Some medical schools have introduced care transitions curricula, though few have published data on their effectiveness. A search for teaching products using care transitions or transitional care on the online educational portals POGOe (Portal of Geriatric Online Education) and MedEdPortal yielded a total of 7 unique sets of teaching materials on care transitions for medical students.1218 However, a search on PubMed in July 2010 for peer‐reviewed articles on care transitions curricula developed for medical students which contained evaluation data only yielded 3 articles.1921 These 3 curricula, written by Bray‐Hall et al., Lai et al., and Ouchida et al., respectively, all trained third‐year medical students on diverse aspects of the discharge process using methods such as lectures, workshops, and patient visits, and showed favorable skill and knowledge outcomes.
Recognizing the importance of care transitions in medical education, a new curriculum addressing this topic was developed and introduced for fourth‐year medical students at the Emory University School of Medicine in 2009. The broad goal for this module was to develop a course concentrating on concrete skills that would train students to perform better care transitions while minimizing the time they had to spend away from a busy Internal Medicine sub‐internship. This curriculum used a mixed approach that included face‐to‐face teaching with faculty, online didactic instruction and interaction, and direct patient care. The course objectives were for students to develop a working fund of knowledge on care transitions, to learn to write a complete discharge summary, and to communicate the elements of a safe discharge plan. This article will describe the implementation of this curriculum and its evaluation.
METHODS
The Emory Care Transitions Curriculum started in August 2009 with fourth‐year medical students at the Emory University School of Medicine. This section will describe the details of the implementation of this curriculum, as well as the evaluation methodology and results.
Overview
This module was offered to Emory medical students participating in a required Senior Medicine rotation during their fourth year. The study population consisted of the 121 fourth‐year Emory medical students who participated in this rotation during the academic year that started in August 2009 and ended in April 2010. Students participated in the rotation at 1 of 3 teaching sites: Grady Memorial Hospital (GMH), Emory University Hospital (EUH), and the Atlanta VA Medical Center (AVAMC); 98 students completed their rotation at GMH, 12 at EUH, and 11 at AVAMC. For all online activities, students used the Blackboard platform software, available to them at
Course Description
The course consisted of 3 components, each associated with specific student assignments: a slide presentation on care transitions with an associated case discussion, training on discharge summaries, and the execution of a postdischarge phone call. Figure 1 describes the course delivery schedule.
Slide Presentation and Case Discussion
This section started on day 2 of the clerkship, with a face‐to‐face lecture titled Transitions of Care: Why They Are Important, and How to Improve Them. It included the following components: definition of the different posthospital discharge options, explanation of the reasons for the complexity of care transitions in high‐risk patient populations, and an enumeration of methods to improve the safety of care transitions. Students also read a review article on the topic to further add to their fund of knowledge.23
The second part of the section involved discussion of a case posted on Blackboard (a discussion board) designed to highlight some of the challenges associated with care transitions. The case included 2 successive discharge summaries for an elderly patient with congestive heart failure: 1 for the initial exacerbation, and the other for a readmission. Using an online discussion board, students were asked to report the strong points and shortcomings of the patient's management, as well as those of the discharge summaries. Then the students were asked to post responses to at least 2 of their classmates' reports on the discussion board.
Training on Discharge Summaries
During the module, students received training on how to prepare a complete and informative discharge summary. This online training consisted of a lecture prepared by a faculty member (M.A.E.) and the use of a discharge summary template based on a guide prepared by the Boston Association of Academic Hospitalists (BAAHM), which is part of a toolkit available from the Society of Hospital Medicine.24 After reading the lecture, each student selected 1 of the patients they cared for during their rotation, and wrote a discharge summary. They posted it to a Blackboard discussion board, and were then asked to comment on one of their classmates' reports on the same forum. Faculty (M.A.E. and R.C.) also gave online feedback to each student about their discharge summary.
Postdischarge Phone Call
Students were also assigned to communicate with the patient for whom they prepared a discharge summary by performing a postdischarge phone call within a week of the patient's departure from the hospital. They reviewed a discharge checklist adapted from Ideal Discharge for an Elderly Patient: A Hospitalist Checklist, issued by the Society of Hospital Medicine.25 This document contains the necessary elements of a safe discharge plan, and used these points as the basis of the patient phone interview. The goal of the call and the use of the checklist was to reinforce the main elements of communication with patients that need to occur before they leave the hospital.
Students then used the checklist as the basis for a short (<400 words) report discussing the strong points and shortcomings of their patient's discharge, and posted it on a Blackboard discussion board. They were also asked to comment on at least one of their classmates' reports on the board. Faculty (M.A.E. and R.C.) also participated in the discussion board, commenting at least once on all students' reports.
Evaluation
The course was evaluated in order to assess changes in skills, knowledge and attitudes, as well as satisfaction with the course.
Evaluation Components
In order to assess the outcomes described above, questionnaires were utilized, and objective criteria were used to evaluate students' work. Students completed a pretest before the first face‐to‐face session, and a posttest after the second in‐person discussion. Pretest items were identical to those in the posttest, except that the posttest also contained 6 satisfaction questions. The components that were included in both pre‐ and posttests were:
Five multiple choice questions measuring students' confidence in their own skills regarding discharge summaries and transitional care (pre‐ and postsurvey). These 5 questions were adapted from the questionnaire developed by Lai et al.20 Confidence questionnaire items are detailed in Table 1.
Five multiple choice questions assessing students' attitudes regarding the importance of different components of the care transitions process (pre‐ and postsurvey). Attitude questionnaire items are detailed in Table 1.
Ten multiple choice questions in which each had one right answer, assessing students' knowledge base on transitional care issues (pre‐and postsurvey). Knowledge questions and their correct answers are detailed in Table 2.
| Mean Likert Scores* | P Value | ||
|---|---|---|---|
| Pre‐Course | Post‐Course | ||
| |||
| Confidence items | |||
| 1. I am confident in my ability to involve patients in making a plan for their care. | 3.8 | 4.2 | <0.001 |
| 2. I am confident in my ability to review patients' medications and side effects. | 3.4 | 4.1 | <0.001 |
| 3. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.4 | 4.3 | <0.001 |
| 4. I am confident in my ability to prepare a complete discharge summary. | 3.0 | 4.2 | <0.001 |
| 5. I can identify the different types of places that may serve as a setting for discharge from the inpatient setting. | 3.1 | 3.9 | <0.001 |
| Total confidence score (out of 25) | 16.7 | 20.7 | <0.001 |
| Attitude items | |||
| 1. A hospital physician should always communicate with a patient's primary care physician before that patient is discharged from the hospital, in order to ensure a smooth transition of care. | 4.0 | 4.1 | 0.78 |
| 2. Before a patient is discharged from the hospital, a physician (not just the nurse or case manager) should always meet with the patient to discuss his medications, and goals of care. | 4.4 | 4.4 | 0.50 |
| 3. It is critical for a primary care physician to have access to a discharge summary when seeing a patient for the first time after leaving the hospital. | 4.6 | 4.7 | 0.25 |
| 4. The main reason patients often don't take their medications properly after discharge is that they are confused by the instructions given to them at the hospital. | 3.7 | 3.8 | 0.65 |
| 5. Avoiding rehospitalization should be a top priority for physicians in the process of discharge from the hospital. | 4.1 | 4.3 | 0.95 |
| Total attitude score (out of 25) | 20.8 | 21.3 | 0.07 |
| Percent Correct | |||
|---|---|---|---|
| Question (Correct Answer in Parenthesis) | Pre‐Course | Post‐Course | P Value |
| |||
| 1. When a patient is discharged with home health care, which of the following services is usually not part of the package? (A caregiver to sit with the patient and supervise them most of the day.) | 70 | 83 | 0.020* |
| 2. When a patient is discharged from the hospital to a skilled nursing facility (SNF) for further care, which of these is a service that is typically provided? (Physical therapy.) | 78 | 75 | 0.649 |
| 3. Which of the following rehabilitation activities is more likely to be in the job description of an occupational therapist? (Training of strength in upper extremities.) | 24 | 51 | <0.001* |
| 4. Which of these is least likely to be a cause of poor patient outcomes after hospital discharge? (The discharging of patients to skilled nursing facilities.) | 93 | 97 | 0.166 |
| 5. Which of these is more likely to be an indicator of poor outcomes after hospital discharge? (Having had 3 hospitalizations in the last 6 months.) | 93 | 96 | 0.287 |
| 6. Which of these data is the least likely to be an indicator that the patient is too sick to be discharged from the hospital? (Hemoglobin concentration of 9.5 g/dl.) | 45 | 74 | <0.001* |
| 7. Which of the following medications would merit the most time spent on communication with patients, family members, and receiving physicians? (Furosemide.) | 58 | 96 | <0.001* |
| 8. You are caring for an 89‐year‐old man who is being treated in the hospital for an exacerbation of his congestive heart failure (CHF). He is doing well, ambulating 100 feet without shortness of breath, and is showing understanding of the need for all his different medications. However, he is not yet back to his functional baseline. Which of the following is the LEAST appropriate setting for discharge? (Hospice care.) | 74 | 70 | 0.458 |
| 9. Which of the following is true about skilled nursing facility (SNF) care? (Patients can be admitted for treatment with IV antibiotics for several weeks.) | 52 | 79 | <0.001* |
| 10. Educating patients at discharge about their illness and medication has been found to help decrease readmission rates. (True.) | 97 | 100 | 0.045 |
| Percentage of total questions correct | 68 | 82 | <0.001* |
The questionnaire items were developed by study faculty (M.A.E. and J.M.F.) and were edited in consultation with clinical faculty members from outside Emory with experience developing care transitions curricula: Dr. Karin Ouchida of Montefiore Medical Center in New York City, and Dr. William Lyons of the University of Nebraska Medical Center.
The 6 posttest items addressed student satisfaction with individual course components, which were: the heart failure online case, training on preparing discharge summaries, initial in‐person slide presentation, postdischarge phone call, overall online discussion across all items, and finally, satisfaction with the overall course. Questionnaire items on comfort, attitudes, and satisfaction all used a five‐point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The 10 multiple‐choice questions on knowledge each had one right answer.
Each student completed one discharge summary during the course. For it to be deemed satisfactory, it had to have the 5 following components, all present in the BAAHM template24:
A documented discharge medication list with specific dosing schedules.
Lists of admission medications and/or a list of medication changes during hospitalization.
A discharge plan that specifies the next setting of care, as well as the planned follow‐up.
A hospital course organized by system and/or specific chronology.
A physical exam, laboratory tests, and diagnostic studies performed on admission.
Student reports of their postdischarge phone call were also evaluated by study faculty (M.A.E. and R.C.). For the report of the interview to be considered satisfactory, it had to contain at least the following 2 elements:
A discussion of the patient's medication list, including documentation of a discussion of hazardous medications (e.g., furosemide, warfarin, digoxin, insulin) if applicable.
Documentation of a discussion on follow‐up plans with a primary physician or specialist.
Data Analysis
Outcomes were evaluated based on the results of pre‐ and posttest questionnaires, in addition to the satisfactoriness of discharge summaries and postdischarge phone call reports. As for the questionnaires, 4 types of scores were analyzed based on students' questionnaire responses:
Skills Confidence Score: The sum of Likert scores for confidence items on the pre‐ and posttest was the confidence score, with a highest possible score of 25, in which the highest scores were associated with the most confidence in executing the discharge process.
Attitude Score: The sum of Likert scores for attitude items on the pre‐ and posttest was the attitude score, with a highest possible score of 25, in which the highest scores were associated with student attitudes ascribing the most importance to a safe discharge process.
Knowledge Score: The percentage of total correct answers on knowledge questions on the pre‐ and posttest were used to obtain the knowledge score, in which a score of 100 was highest.
Satisfaction Score: Satisfaction questions on the posttest questionnaire were analyzed separately to assess satisfaction with each component of the curriculum, ranging from poor (score = 1) to excellent (score = 5). We also determined the percentage of students who rated each portion of the course good or better.
In addition to questionnaire scores, students' performance in the preparation of discharge summaries and the postdischarge phone interview were evaluated. Discharge summaries and postdischarge phone interviews were classified as satisfactory or unsatisfactory based on the criteria outlined in the previous section on outcome evaluation.
Quantitative and Qualitative Analysis
Skills confidence, attitude, and knowledge scores were compared between pre‐ and posttest. Paired t tests were used to calculate statistical significance. A P value below 0.05 was considered statistically significant, using two‐tailed tests.
We also analyzed whether there were any differences in changes in confidence, attitude, and knowledge scores according to the time of year in which the course was taken by students. For this, we divided the nine‐month course into 3 trimesters (AugustOctober, NovemberJanuary, and FebruaryApril). In order to determine whether 3 were any differences in score changes among the different periods, we used a one‐way analysis of variance (ANOVA), in which a P value below 0.05 would indicate a statistically significant difference among the periods. All statistical analyses were performed using SPSS 17.0 for Windows.
Statistical tests were not utilized for the satisfaction scores, but the overall goal was for their mean to be 3 (good) or above. Also, the percentages of satisfactory discharge summaries and postdischarge phone interviews were measured. The goal was for both tasks to have a percentage of satisfactory evaluations of 80% or above.
RESULTS
The 121 students who took the module completed both the pre‐ and posttests. Table 1 details the mean pre‐ and posttest Likert scores for all confidence and attitude questions, as well as the changes in the 25‐point total confidence and attitude score from pre‐ to posttest. The change in confidence scores among survey participants was statistically significant (P < 0.001), while the change in attitude score was not (P = 0.07). Table 2 compares the percentage of correct answers before and after the course for individual knowledge questions, as well as for the entire knowledge quiz. Changes in total knowledge scores were statistically significant: the mean percentage of correct answers out of 10 questions was 68% on the pretest, and 82% on the posttest (P < 0.001).
Table 3 measures the changes in confidence, attitude, and knowledge scores by the period of the year in which students took the course. One‐way ANOVA tests for each of the 3 domains did not find statistically significant changes in confidence, attitude, or knowledge scores among the 3 trimesters in which we divided the module's calendar.
| Section of Questionnaire | Total for Year | Period of Year | F Value | P Value | ||
|---|---|---|---|---|---|---|
| AugustOctober | NovemberJanuary | FebruaryApril | ||||
| Confidence | ||||||
| Mean pre‐course score | 16.7 | 16.5 | 16.5 | 17.0 | ||
| Mean post‐course score | 20.7 | 21.0 | 19.9 | 21.0 | ||
| Mean change in score | 4.0 | 4.5 | 3.4 | 4.0 | 0.92 | 0.40 |
| Attitude | ||||||
| Mean pre‐course score | 20.8 | 20.9 | 20.5 | 20.6 | ||
| Mean post‐course score | 21.3 | 21.3 | 21.3 | 21.1 | ||
| Mean change in score | 0.5 | 0.4 | 0.8 | 0.5 | 0.13 | 0.88 |
| Knowledge | ||||||
| Mean pre‐course percentage correct | 68 | 71.3 | 67.4 | 66.4 | ||
| Mean post‐course percentage correct | 82 | 82.5 | 80.9 | 82.1 | ||
| Mean change in score | 14 | 11.2 | 13.5 | 15.7 | 0.60 | 0.55 |
| No. of participants | 121 | 40 | 34 | 47 | ||
Table 4 shows satisfaction scores on the posttest. The overall Likert rating for the course was 3.9, with 97.5% of students rating it good or better. The highest‐rated individual component of the course by Likert score was the training on discharge summaries, with a rating of 4.1. The lowest‐rated by this parameter was the congestive heart failure case, with a rating of 3.6. The online discussion across all topics had the lowest percentage of students rating it good or above, at 83.5%.
| Curriculum Section | Mean Likert Rating (Out of 5) | Percentage Rated Good or Above |
|---|---|---|
| Congestive heart failure case | 3.6 | 95.0 |
| Discharge summaries | 4.1 | 96.7 |
| Initial in‐person slide presentation | 4.0 | 97.5 |
| Postdischarge phone call | 3.7 | 95.0 |
| Online discussion for all topics | 3.7 | 83.5 |
| Overall curriculum rating | 3.9 | 97.5 |
As for student discharge summaries, 109 out of 121 (90.1%) met all the criteria in order to be deemed satisfactory; 109 out of 121 (90.1%) of postdischarge phone call reports met both required components. Both these results exceeded the goal of 80% set before the course started.
DISCUSSION
The Emory Care Transitions Curriculum for fourth‐year medical students started in the 20092010 academic year with the main goal of teaching students transferable skills that would ultimately lead to their participating in safer hospital discharges in their future practice as physicians. At the end of this course, students exhibited greater confidence in managing the discharge process, improved overall fund of knowledge relating to care transitions, and a demonstration of appropriate skills related to preparing discharge summaries and communicating with patients at discharge. This was all executed with a delivery method that students found engaging.
Analyzing the results, it is noteworthy that confidence improved, while attitudes did not. Even though confidence in performing a task does not necessarily reflect one's ability to perform it, our students' confidence scores may serve as a proxy for their ability to manage tasks related to the discharge process, like managing medications and preparing discharge summaries. Thus, while some studies suggest that self‐assessment among physicians may not always relate well to competence,26, 27 in our study, students did demonstrate skills in discharge summary preparation and in identifying the most relevant aspects of patient communication at hospital discharge. As for the absence of attitude change, this may have partly been a function of the fact that students in our group started with attitude scores that were already quite high, with a mean pretest attitude score of 20.7 out of 25.
Changes in student confidence, attitudes, and knowledge from pre‐ to posttest did not vary significantly across the academic year. Thus, one could interpret from our findings that more experienced students who took the module close to graduation benefited similarly from the course to those who completed it earlier, at least according to those rubrics. Another possible source of variation in student experience was the hospital in which students rotated: the demographics of GMH, with its large uninsured population; AVAMC, with more elderly patients; and EUH, with a more affluent profile, are certainly different. However, the number of students rotating at EUH and AVAMC were comparatively too small to attempt to draw any conclusions about how rotation site affected student experiences.
The use of a blended approach that integrated face‐to‐face didactics, patient care, and online learning offered some advantages. Curricular goals were achieved through a course that required only 2 hours of in‐person faculty time with students. This is significant, considering the time demands that academic medical faculty usually face. This approach also permitted students who were participating in a busy clinical rotation, and had limited opportunities to meet as a group, the ability to do coursework at their own pace. Another strength of the study is that all students who participated in the rotation were able to complete their surveys.
As for limitations, it is worth noting that in a course with a blended curriculum, the online discussion had the lowest percentage of students rating it good or better. Part of the perceived difficulty may have resulted from the fact that there are no other courses in the Emory medical curriculum that utilize discussion boards or distance learning methods as teaching tools. Despite this generation of students' technological savvy, this new mode of discussion may have proven difficult to pick up when they were in the midst of a busy clinical rotation. This serves as a reminder that while online curricula have proven successful in this and other settings, each element needs to be tailored to the audience. One other factor to be considered while interpreting this study's results is that this study utilized some survey instruments that have not been previously validated, even though they were developed in consultation with experts in the field of care transitions education.
We used a dichotomous, criteria‐based system to rate students' discharge summaries and reports of postdischarge phone calls. While this quantitative approach allowed us to more objectively define the quality of students' work, it did offer some disadvantages. First, even though we based the rating system for discharge summaries on a BAAHM template, it was not subjected to more extensive validation. Moreover, the quantitative approach diverted us from finding themes and other qualitative data from students' write‐ups, which could potentially have given us a fuller picture of their work.
This study contributes to the small, but growing, literature on care transitions education. The studies by Bray‐Hall et al., Lai et al., and Ouchida et al.,1921 used different methodologies, but all were directed at third‐year students using curricula with classroom and clinical learning, and showed favorable outcomes in knowledge and skills. The present study also showed positive results in students' knowledge and skills, but targeted it toward graduating medical students and included a focus on concrete skills, such as discharge summary preparation. It also utilized a nontraditional delivery approach which reached its objectives while also limiting the demands on faculty and students' face time during busy clinical rotations, which is especially important when considering that students were dispersed at multiple sites.
It is likely that medical schools will implement more care transitions curricula in coming years, as organizations like the AAMC11 and the Institute of Medicine10 increase the pressure to train future doctors to better address the needs of older and chronically ill patients, who require care from professionals of multiple disciplines, in disparate care settings. Moreover, the 2010 Patient Protection and Affordable Care Act28 contains provisions with financial incentives for hospitals to decrease readmissions. Once these become widely implemented, there will be a greater impetus to train medical practitioners to discharge patients more safely. When that occurs, medical schools will have additional compelling reasons to offer courses that teach students skills to execute better care transitions. The hoped‐for outcome of these curricula will ultimately be safer and more effective patient care.
Acknowledgements
The authors thank Dr. Ted Johnson at the Emory University School of Medicine for editorial review. They also express their gratitude to Dr. Karin Ouchida at Montefiore Medical Center and Dr. William Lyons at University of Nebraska Medical Center for their technical support in preparation of the curriculum. Disclosures: None of the authors has any relevant conflicts of interest. All coauthors have seen and agree with the contents of this manuscript. The authors are responsible for the integrity of the data described in this study. The research in this manuscript has not been submitted or accepted for publication in another journal.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,.Adverse drug events in elderly patients receiving home health services following hospital discharge.Ann Pharmacother.1999;33:1147–1153.
- ,,,,.The association between the quality of inpatient care and early readmission: A meta‐analysis of the evidence.Med Care.1997;35(10):1044–1059.
- ,,,,.The association between the quality of inpatient care and early readmission.Ann Intern Med.1995;122(6):415–421.
- ,.Hospital readmissions as a measure of quality of health care: Advantages and limitations.Arch Intern Med.2000;160(8):1074–1081.
- ,.Lost in transition: Challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;140:533–536.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians.JAMA.2007;297:831–841.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington, DC:National Academy Press;2003.
- American Association of Medical Colleges. Geriatric Competencies for Medical Students: Recommendations of the July 2007 Geriatrics Consensus Conference.2008. Available at: http://www.aamc.org/newsroom/press kits/competencies.pdf. Accessed February 25, 2009.
- Eskildsen M, Price T, Tenover JL. Computer‐based geriatrics workbooks for resident teaching. MedEdPortal. 2007. Available at http://services. aamc.org/30/mededportal/servlet/s/segment/mededportal/ find_resources/ browse/?subid=640.
- .Care transitions in the older adult.MedEdPortal.2008. Available at http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/find_resources/browse/?subid=678. Accessed March 19, 2011.
- ,,, et al.Web‐based module to train and assess competency in systems‐based practice.Portal of Online Geriatric Education.2009. Product ID #20002. Available at: http://www. pogoe.org/node/407. Accessed March 19, 2011.
- .CHAMP (Curriculum for the Hospitalized Aging Medical Patient): The ideal hospital discharge.Portal of Online Geriatric Education.2009. Product ID #18995. Available at: http://www. pogoe.org/productid/18995. Accessed March 19, 2011.
- .M1 care transitions.Portal of Online Geriatric Education.2009. Product ID #20450. Available at: http://www. pogoe.org/node/660. Accessed March 19, 2011.
- .Transitional care.Portal of Online Geriatric Education.2007. Product ID #18991. Available at: http://www.pogoe.org/node/262. Accessed March 19, 2011.
- .Discharge summary feedback.Portal of Online Geriatric Education.2009. Product ID #20546. Available at: http://www.pogoe.org/node/788. Accessed March 19, 2011.
- ,,.Toward safe hospital discharge: A transitions in care curriculum for medical students.J Gen Intern Med.25(8):878–881.
- ,,,,.Postdischarge follow‐up visits for medical and pharmacy students on an inpatient medicine clerkship.J Hosp Med.2008;3(1):20–27.
- ,,,,.Fast forward rounds: An effective method for teaching medical students to transition patients safely across care settings.J Am Geriatr Soc.2009;57:910–917.
- .Fourth‐year medical student care transitions curriculum (free login required).Portal of Online Geriatric Education.2010. Available at: http://www.pogoe.org/node/867. Accessed July 16, 2010.
- .Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- Society of Hospital Medicine. Quality initiatives for patient care—BOOSTing care transitions resource room.2010. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_Care Transitions/html_CC/12Clinical Tools/01_Toolkits.cfm. Accessed November 16, 2010.
- Society of Hospital Medicine. Ideal discharge for an elderly patient: A hospitalist checklist.2005. Available at: http://www.hospitalmedicine. org/AM/Template.cfm?Section=QI_Clinical_Tools8(2):105–110.
- ,,.Difficulties in recognizing one's own incompetence: Novice physicians who are unskilled and unaware of it.Acad Med.2001;76(10 suppl):S87–S89.
- Patient Protection and Affordable Care Act, H.R. 3590.ENR, 111th Congress, 2010.
- ,,, et al.Adverse events among medical patients after discharge from hospital.Can Med Assoc J.2004;170(3):345–349.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,.Adverse drug events in elderly patients receiving home health services following hospital discharge.Ann Pharmacother.1999;33:1147–1153.
- ,,,,.The association between the quality of inpatient care and early readmission: A meta‐analysis of the evidence.Med Care.1997;35(10):1044–1059.
- ,,,,.The association between the quality of inpatient care and early readmission.Ann Intern Med.1995;122(6):415–421.
- ,.Hospital readmissions as a measure of quality of health care: Advantages and limitations.Arch Intern Med.2000;160(8):1074–1081.
- ,.Lost in transition: Challenges and opportunities for improving the quality of transitional care.Ann Intern Med.2004;140:533–536.
- ,,,,,.Deficits in communication and information transfer between hospital‐based and primary care physicians.JAMA.2007;297:831–841.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington, DC:National Academy Press;2003.
- American Association of Medical Colleges. Geriatric Competencies for Medical Students: Recommendations of the July 2007 Geriatrics Consensus Conference.2008. Available at: http://www.aamc.org/newsroom/press kits/competencies.pdf. Accessed February 25, 2009.
- Eskildsen M, Price T, Tenover JL. Computer‐based geriatrics workbooks for resident teaching. MedEdPortal. 2007. Available at http://services. aamc.org/30/mededportal/servlet/s/segment/mededportal/ find_resources/ browse/?subid=640.
- .Care transitions in the older adult.MedEdPortal.2008. Available at http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/find_resources/browse/?subid=678. Accessed March 19, 2011.
- ,,, et al.Web‐based module to train and assess competency in systems‐based practice.Portal of Online Geriatric Education.2009. Product ID #20002. Available at: http://www. pogoe.org/node/407. Accessed March 19, 2011.
- .CHAMP (Curriculum for the Hospitalized Aging Medical Patient): The ideal hospital discharge.Portal of Online Geriatric Education.2009. Product ID #18995. Available at: http://www. pogoe.org/productid/18995. Accessed March 19, 2011.
- .M1 care transitions.Portal of Online Geriatric Education.2009. Product ID #20450. Available at: http://www. pogoe.org/node/660. Accessed March 19, 2011.
- .Transitional care.Portal of Online Geriatric Education.2007. Product ID #18991. Available at: http://www.pogoe.org/node/262. Accessed March 19, 2011.
- .Discharge summary feedback.Portal of Online Geriatric Education.2009. Product ID #20546. Available at: http://www.pogoe.org/node/788. Accessed March 19, 2011.
- ,,.Toward safe hospital discharge: A transitions in care curriculum for medical students.J Gen Intern Med.25(8):878–881.
- ,,,,.Postdischarge follow‐up visits for medical and pharmacy students on an inpatient medicine clerkship.J Hosp Med.2008;3(1):20–27.
- ,,,,.Fast forward rounds: An effective method for teaching medical students to transition patients safely across care settings.J Am Geriatr Soc.2009;57:910–917.
- .Fourth‐year medical student care transitions curriculum (free login required).Portal of Online Geriatric Education.2010. Available at: http://www.pogoe.org/node/867. Accessed July 16, 2010.
- .Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs.J Am Geriatr Soc.2003;51:549–555.
- Society of Hospital Medicine. Quality initiatives for patient care—BOOSTing care transitions resource room.2010. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_Care Transitions/html_CC/12Clinical Tools/01_Toolkits.cfm. Accessed November 16, 2010.
- Society of Hospital Medicine. Ideal discharge for an elderly patient: A hospitalist checklist.2005. Available at: http://www.hospitalmedicine. org/AM/Template.cfm?Section=QI_Clinical_Tools8(2):105–110.
- ,,.Difficulties in recognizing one's own incompetence: Novice physicians who are unskilled and unaware of it.Acad Med.2001;76(10 suppl):S87–S89.
- Patient Protection and Affordable Care Act, H.R. 3590.ENR, 111th Congress, 2010.
Copyright © 2011 Society of Hospital Medicine