User login
Reduction in Iatrogenic Pneumothorax
Iatrogenic pneumothorax (IAP) is a complication of invasive procedures that is associated with substantial morbidity and some mortality.[1] IAP is often avoidable, and in many cases can be prevented through adherence to evidence‐based guidelines and procedural techniques known to reduce the incidence of IAP.[2] IAP may occur with a subclavian (SC) or internal jugular (IJ) central venous catheter (CVC) insertion, but is more frequently associated with the SC approach.[3] Ultrasound guidance during IJ CVC insertion is associated with a lower risk as compared to guidance by anatomical landmarks.[4, 5] Other bedside procedures that are known to cause IAP include thoracentesis. This risk can also be reduced with the use of ultrasound guidance.[6]
Including simulation in training for CVC insertion has been demonstrated in meta‐analyses to improve both learner outcomes, including simulator performance and perceived confidence, and patient outcomes, including fewer failed CVC attempts and reduced incidence of IAP.[7] Even brief simulation workshops lasting less than two hours can improve patient safety during CVC insertion.[8]
The implementation of ultrasound‐based simulation and improved adherence to the actual use of ultrasound at the bedside can be motivated by tying competency‐based educational objectives (eg, CVC insertion) to clinical outcomes (ie, rates of IAP) and tracking both as part of a continuous quality‐improvement cycle.[9] Adherence to best practices for CVC insertion can also be improved through standardizing hospital‐wide policies and hands‐on training.[10] Involving many stakeholders, including nurses, physicians, nurse practioners and physician assistants, in a multidisciplinary team has been shown to help alter entrenched behaviors and reduce the incidence of central‐line associated bloodstream infections through long‐term adherence to evidence‐based interventions.[11]
LOCAL PROBLEM
The Agency for Healthcare Research and Quality (AHRQ) has designed Patient Safety Indicators (PSIs) (
Our hospital is a member of the University HealthSystem Consortium (UHC) (
Despite this, the PSI can highlight areas where quality‐improvement efforts might be best directed. In 2005 and 2006, our hospital was ranked within the lowest UHC performance quartile for all‐cause IAP PSI.
During FY 2006 (September 2005August 2006), root‐cause analysis on cases of IAP at our hospital found that CVC insertion (40%) was the most common procedure associated with IAP, with SC insertion causing 69% of CVC‐associated IAP. Other common procedures associated with IAP were operative/pacemaker (30%), thoracentesis (25%), and ventilator associated (5%). Ultrasound was not used in 2/5 cases of IJ CVC placement and 3/5 thoracentesis cases. Only 44% of CVC insertions had a procedure note.
Intended Improvement/Study Question
Our team set out to plan and implement a set of multifaceted interventions within 90 days. The short‐term goal was a 50% reduction in the CVC IAP and all‐cause IAP rate within 18 months, and the long‐term goal was sustained reduction of CVC IAP and all‐cause IAP rate.
METHODS
The format of this article is based on the standards for quality‐improvement reporting excellence guidelines for the reporting of studies on the effectiveness of quality‐improvement interventions.[14]
Setting
Stanford University Medical Center is an academic medical center with 465 beds and over 25,000 inpatient admissions per year, providing both general acute care services and tertiary medical care. Residents perform CVC bedside procedures when central venous access is needed, in the intensive care unit (ICU), operating room (OR), and inpatient units. Prior to this project, ultrasound equipment was only available in the emergency department (ED) and ICUs. There was no formal CVC procedure supervision policy, CVC training curriculum, and procedure note templates for documentation of CVC insertion.
Planning the Interventions
A multidisciplinary quality‐improvement team met weekly during the 90‐day design period from January 2007 to March 2007. Our team included representatives from the departments of medicine, anesthesia and critical care, surgery, nursing, and emergency medicine. We also partnered with our institution's clinical and administrative leaders, experts in simulation, and the hospital quality department.
We hypothesized that a standardized set of education and training interventions promoting ultrasound‐guided IJ CVC insertion as the method of choice at our hospital would significantly reduce our rate of CVC‐associated IAP. Our multifaceted intervention included: (1) clinical and documentation standards based on evidence, (2) cognitive aids, (3) simulation training, (4) purchase and deployment of ultrasound equipment, and (5) feedback to clinical services.
Our team followed the define, measure, analyze, improve, control (DMAIC) framework.[15] We set interval goals with target completion dates throughout the 90‐day period, identified owners of each goal, and tracked progress with a shared spreadsheet.
In the 90‐day intervention, we accomplished the following: (1) conducted root‐cause analysis of IAP cases for fiscal year 2006, (2) created clinical and documentation standards around CVC placement, (3) created cognitive aids and procedure note templates, (4) developed simulation training courses, and (5) requested purchase of additional ultrasound equipment.
Data Collection
To evaluate our progress in reducing the rates of IAP, we tracked the incidence of IAP using UHC and AHRQ PSI methodology. In collaboration with our hospital's quality department, we manually reviewed every PSI‐identified case of IAP. This review has focused on identifying whether or not pneumothorax actually occurred, and whether it was associated with CVC insertion. For those associated with CVC, data were collected for patient location and service, the procedure site, whether ultrasound was used, whether a chest tube was required, and the final disposition of the patient.
Demographic data (age, gender, case mix index [CMI]) shown in Table 1 were obtained through MIDAS+ Solutions (Tucson, Arizona), a proprietary database that contains healthcare management coded data. Total hospital CVC insertion rates were calculated using International Classification of Diseases, Ninth Revision (ICD‐9) coding for 38.93 and 38.97. ICU central lineassociated blood stream infections (CLABSI) data were obtained from internal collection by our infection control team. Number and location of CVCs placed in the ICU data were obtained from nursing flow sheets in our electronic medical record (EMR). Cost information was provided by our finance department using internal accounting.
| Patients With CVC Insertion | Year | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| |||||||||
| Age, y (mean) | 55.0 | 55.5 | 55.0 | 57.0 | 56.5 | 58.5 | 57.5 | 59.0 | 58.5 |
| % female | 47.0 | 49.5 | 47.0 | 48.8 | 46.2 | 46.1 | 45.7 | 46.2 | 45.7 |
| Case‐mix index | 3.08 | 3.35 | 3.21 | 3.40 | 3.71 | 3.91 | 3.92 | 3.92 | 4.08 |
| Total no. of CVCs/year* | 1,593 | 1,141 | 1,589 | 2,250 | 2,441 | 2,774 | 2,754 | 2,722 | 2,845 |
| No. of CVCs/year in ICU | NA | NA | NA | 1,502 | 1,357 | 1,345 | 1,316 | 1,421 | 1,590 |
| No. of subclavians/year in ICU | NA | NA | NA | 167 | 75 | 70 | 83 | 75 | 97 |
| No. of IJs/year in ICU | NA | NA | NA | 898 | 773 | 681 | 677 | 713 | 876 |
| No. of femorals/year in ICU | NA | NA | NA | 212 | 152 | 203 | 171 | 198 | 206 |
| No. of PICCs/year in ICU | NA | NA | NA | 225 | 357 | 391 | 385 | 435 | 411 |
| Preintervention (2006) | Postintervention (20082014) | P Value | |||||||
| Age, y (mean) | 55.2 | 58.7 | <0.0001 | ||||||
| % female | 47.0% | 46.4% | 0.642 | ||||||
| Case‐mix index | 3.08 | 3.73 | <0.0001 | ||||||
| CVC insertion rate | 8.1% | 11.4% | <0.0001 | ||||||
| All Inpatients | Year | ||||||||
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Age, y (mean) | 57.1 | 57.2 | 56.8 | 57.2 | 57.5 | 58.0 | 58.0 | 57.9 | 58.3 |
| % female | 51.6 | 51.2 | 52.4 | 51.7 | 51.1 | 51.5 | 50.3 | 49.9 | 50.1 |
| Case‐mix index | 1.86 | 1.98 | 1.96 | 1.99 | 1.96 | 2.02 | 2.03 | 2.07 | 2.23 |
| Preintervention (2006) | Postintervention (20082014) | P Value | |||||||
| Age, y (mean) | 57.1 | 57.6 | <0.01 | ||||||
| % female | 51.6% | 50.9% | 0.07 | ||||||
| Case‐mix index | 1.86 | 2.03 | 0.13 | ||||||
| Central Line‐Associated Bloodstream Infections per 1,000 Central Line Days | |||||||||
| Preintervention | Postintervention | P Value | |||||||
| Short term (2006 vs 2008) | 1.8 | 0.60 | 0.004 | ||||||
| Long term (2006 vs 20082014) | 1.8 | 0.68 | <0.0001 | ||||||
The project granted a Notice of Determination of Approval from the Stanford Administrative Panels for the Protection of Human Subjects (institutional review board).
Methods of Evaluation/Analysis
For the purpose of this analysis, the preintervention period was defined as January 1, 2006 through December 31, 2006, our first year of IAP case review. We defined the intervention period as January 1, 2007 through December 31, 2007, during which we planned and implemented hospital‐wide standardization of CVC insertion practices and incorporated CVC insertion training simulation into resident orientation in July 2007. The postintervention period was defined as January 1, 2008 through December 31, 2014.
All statistical analyses were performed using Stata version 12.1 (StataCorp, College Station, TX). [2] tests were used to determine statistical differences in pre‐ versus postintervention patient demographic data (age, gender, CMI), CVC insertion rates, and CLABSI rates. Because IAP is a rare event, a statistical process control g‐chart was created using QI Macros (KnowWare International, Inc., Denver, CO) to show the number of CVC procedures between IAP. [2] and Fisher exact tests were used to determine statistical differences in CVC anatomic location and use of ultrasound pre‐ and postintervention. A 2‐sided Z test to show a difference in proportions was used to determine statistical differences in CVC‐related IAP rate and all‐cause IAP rate pre‐ and postintervention.
Measuring Adherence to Intervention
Location of CVC Placement and Ultrasound Guidance Pre‐ Versus Postintervention
We utilized the Stanford Clinical Informatics Center (SCCI) services for obtaining counts of patients. Custom queries were performed on SCCI's Stanford Translational Research Integrated Database Environment (STRIDE) platform[16] to search Stanford Hospital electronic heath records for patients. This search primarily involved getting counts for the number of patients with clinical notes that contained the keywords of interest. To identify documentation for placement of CVC from 2006 to 2014, procedure or operative notes containing the words central line or CVC were counted. Further subcounts were obtained by searching for additional keywords such as PICC [peripherally inserted central catheters], femoral, jugular, subclavian, and ultrasound.
Adherence to Intervention in the ICU in 2014
A total of 100 charts were reviewed from patients in our medical and surgical ICU with a CVC in 2014 to evaluate the current trend of central line placement and sustainability of our intervention. Fifty charts were initially randomly selected from the ICU cohort. For those who had multiple lines placed, only the first line was reviewed. Because the initial audit did not provide enough SC lines and we wanted to review more IJ lines, we randomly selected an additional 25 patients who had SC and 25 patients who had IJ to review. The following was collected during chart review: primary team, location of line placement, usage of ultrasound, usage of standard procedure template, supervision, level of training for supervisor, and level of training for staff who performed procedure.
Outcomes
The rate of CVC‐associated IAP was calculated as the total number of IAPs attributed to CVCs divided by the total number of CVCs inserted determined by ICD‐9 coding for 38.93 and 38.97. The total IAP rate was calculated as the total number of IAP/1000 discharges.
RESULTS
Interventions
Our team began the intervention in early 2007 with promotion of ultrasound‐guided IJ catheterization. Clinical exceptions included: (1) trauma or code situations where access to the neck is limited, (2) suspected or confirmed neck injuries, (3) presence of a tracheostomy, and (4) bilateral internal jugular sites unsuitable for catheterization.
Our hospital adopted new formal CVC insertion policies consistent with the above training and education efforts. All physicians were required to document CVC insertions using the template available in the EMR. To be certified to perform CVC insertion independently, trainee physicians were required to complete the simulation training and successfully place a minimum of 5 CVCs directly supervised by an already‐certified physician. This was consistent with the Accreditation Council for Graduate Medical Education suggested minimum requirement in 2007. In our critical care units, all CVC insertions must be supervised by an ICU fellow or attending.
To reinforce the on‐the‐ground work by our physician leaders, we created 2 education tools to embed best practices into our CVC insertion workflow. A checklist with best practices for CVC insertion that was distributed throughout the hospital via central line kits and educational flyers, and a CVC insertion procedure note template consistent with California Department of Public Health documentation requirements was made available in our EMR.
In June 2007, we integrated CVC insertion simulation training into procedure workshops required for all medicine, surgery, anesthesia, and emergency medicine trainees during their intern year. These workshops promoted ultrasound‐guided IJ catheterization and supporting evidence for the new IJ site preference. Training sessions were 2 to 3 hours, and included a demonstration of best‐practice CVC insertion, as well as training with simulation models supervised by an instructor using a standardized CVC checklist. These trainings used both the Blue Phantom human torso model (
Hospital administration provided funds to purchase ultrasound machines for patient units such as medicine, cardiology, ED, and ICU). A total of 4 Site‐Rite (Bard Access Systems, Inc., Salt Lake City, UT) ultrasounds were purchased in 2007. The hospital has continued to purchase ultrasound units yearly, and had 53 ultrasound units in 2014
Cases of IAP were continuously reviewed throughout the intervention period. Based on their higher CVC‐associated IAP rates, the ORs and catheterization lab were identified as having opportunities for improvement. In 2008, Hospital quality‐improvement leadership met with physician leaders in these areas to review their CVC‐related IAP data and to discuss strategies to reduce their IAP rates. These strategies included lessons learned from other services that had successfully decreased their IAP rates.
To sustain our gains, we continue to review all IAP through our coding quality, clinical documentation, quality reporting departments, and peer review. We have implemented other strategies to decrease IAP, such as the use of ultrasound guidance for bedside thoracentesis procedures, which became possible after the availability of more ultrasound devices. Training for ultrasound‐guided thoracentesis was done by our procedure‐team attending during supervision of residents.
Outcomes
Preintervention (January 1, 2006 to December 31, 2006)
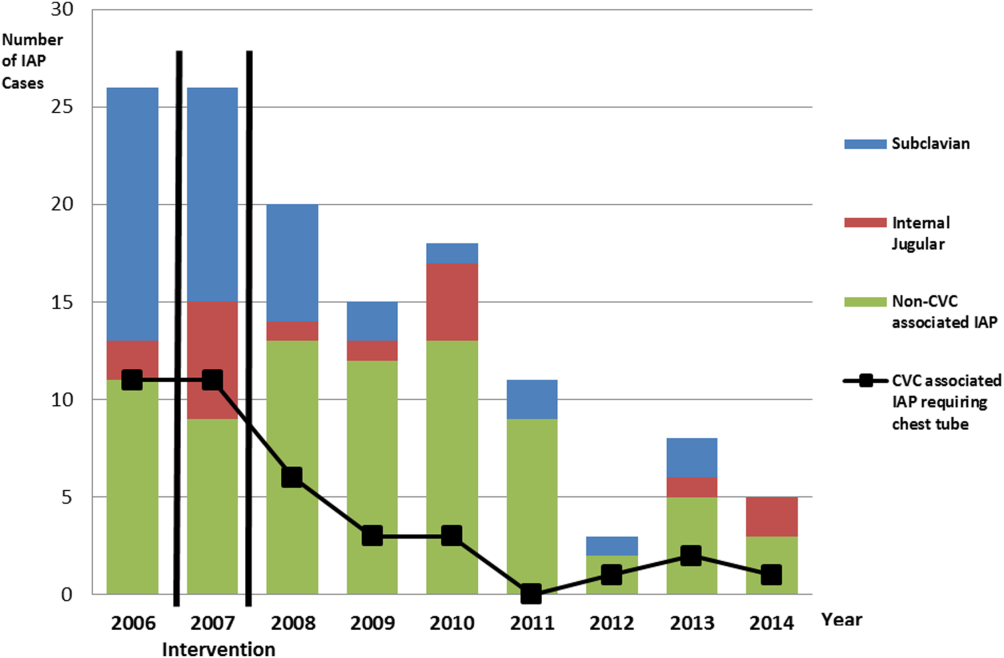
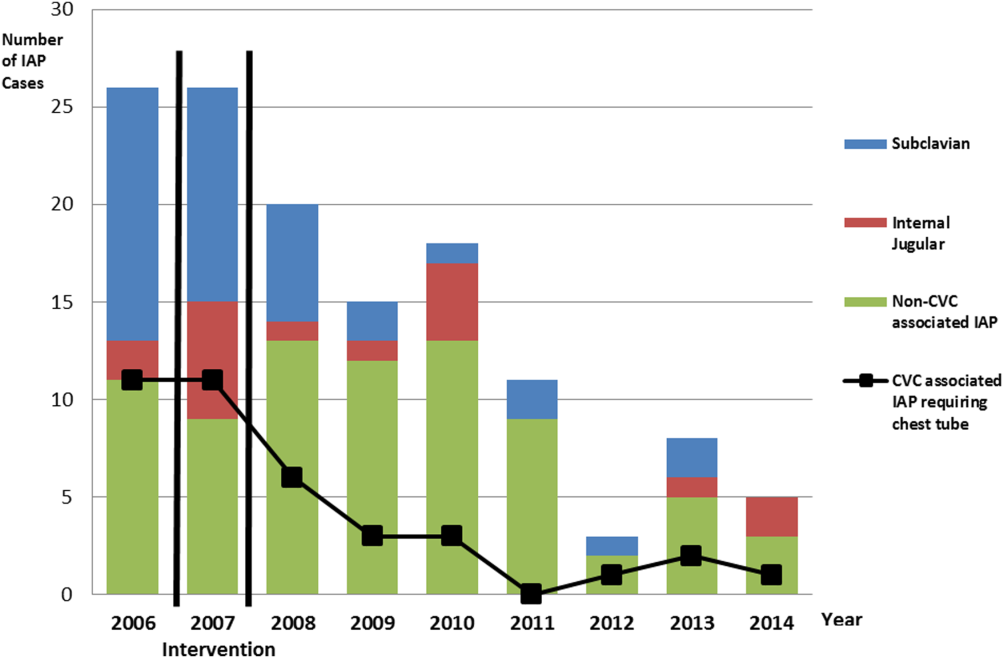
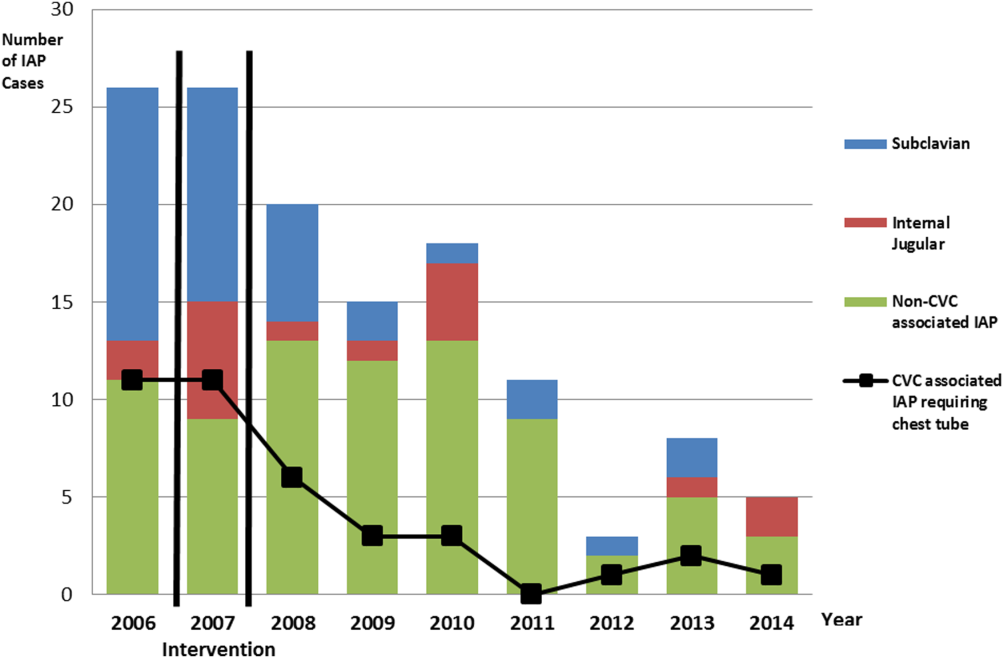
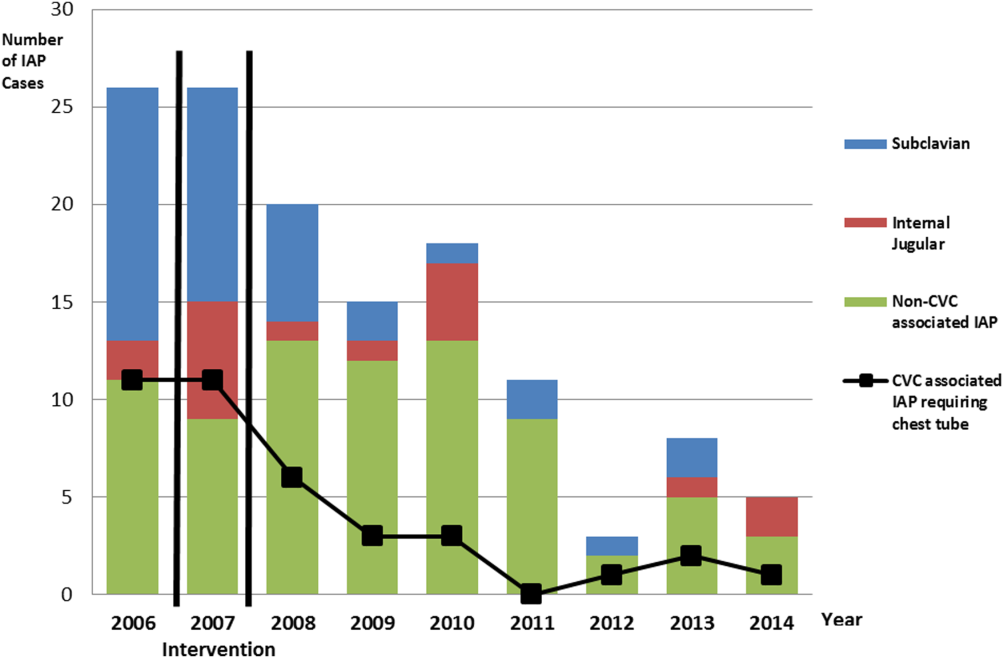
There were a total of 26 cases of IAP in 2006. Of these, 15 (58%) were associated with CVC insertion (Figure 1). The single procedure associated with the largest proportion of IAP was SC CVC insertion (11 cases, 42% of all IAP cases). Eleven CVC‐associated IAPs were significant enough to require chest tube placement. Our hospital recorded a total of 1593 CVC insertions (ICD‐9 codes 38.93 and 38.97) in 2006.
Postintervention (January 1, 2008 to December 31, 2014)
There were a total of 80 cases of IAP over 7 years, of which 24 (30%) were associated with CVC insertion. Of these, 16 required chest tube placement. In the last 4 years of the postintervention period (20112014), there were only 5 cases of CVC‐associated IAP requiring chest tube placement (Figure 1). There were a total of 12,000 CVC insertions recorded over the same period.
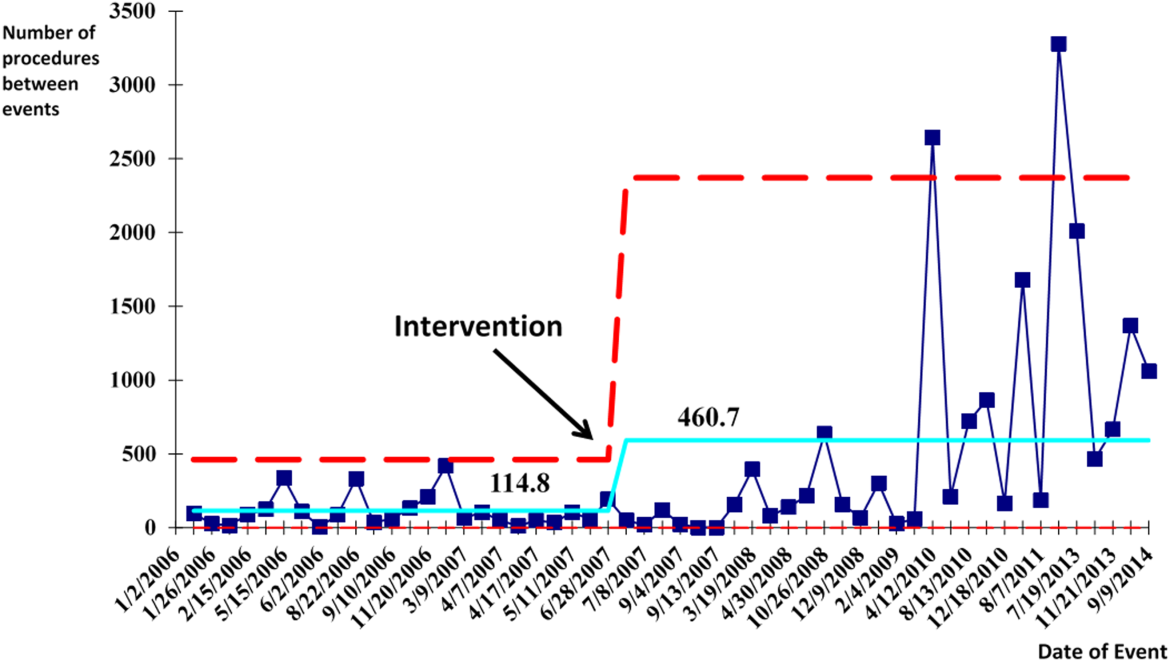
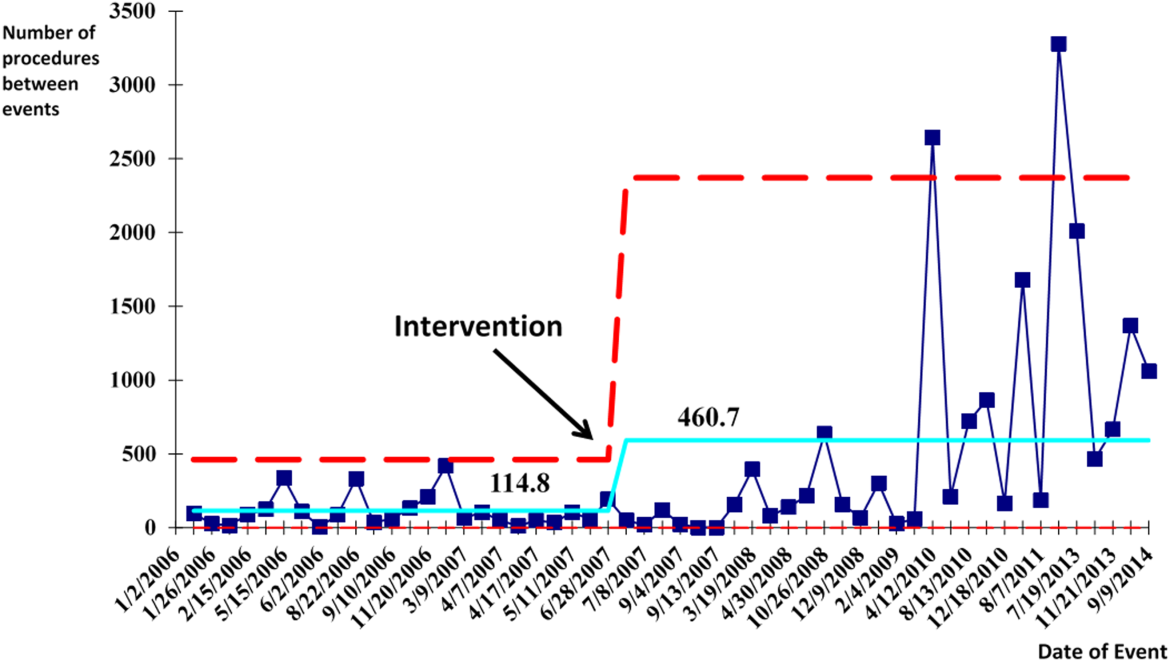
We successfully met both our short‐ and long‐term goals. Our preintervention CVC‐associated IAP rate was 0.94%, and our post‐intervention rate during 2008 was 0.44%, a short‐term reduction of 53% (P=0.088). Our average postintervention CVC‐associated IAP rate for the years 2008 through 2014 was 0.13%, a significant long‐term reduction of 86% (P<0.0001) (Table 2). The decrease in CVC‐associated IAP rates occurred despite an older patient population (P<0.001) and a higher CMI (P<0.001) in postintervention patients who received a CVC (Table 1). Special cause variation corresponding to a change in our process is demonstrated in Figure 2. The preintervention average number of procedures between IAP was 114.8 and increased to 460.7 in the postintervention period.
| Total CVC (n=95) | Subclavian (n=29) | Internal Jugular (n=58) | Femoral (n=8) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||
| Compliance to intervention | |||||||||||||
| US guided | 68.1% | 20.7% | 86.2% | 100.0% | |||||||||
| Procedure note completion | 90.4% | 93.1% | 86.2% | 100.0% | |||||||||
| Supervision | 70.2% | 77.8% | 73.1% | 87.5% | |||||||||
| Level of training | |||||||||||||
| Resident | 61.1% | 58.6% | 60.3% | 75.0% | |||||||||
| Fellow | 25.3% | 27.6% | 24.1% | 25.0% | |||||||||
| Attending | 4.2% | 6.9% | 3.4% | 0.0% | |||||||||
| Advance practitioner | 3.2% | 3.4% | 3.4% | 0.0% | |||||||||
| Unknown | 6.3% | 3.4% | 8.6% | 0.0% | |||||||||
| Supervisor type | |||||||||||||
| Resident | 3.0% | 4.8% | 2.6% | 0.0% | |||||||||
| Fellow | 54.5% | 33.3% | 57.9% | 100.0% | |||||||||
| Attending | 42.4% | 61.9% | 39.5% | 0.0% | |||||||||
| Location of CVC Placement | Internal Jugular (n=25) | Subclavian (n=25) | |||||||||||
| MICU | 32.0% | 32.0% | |||||||||||
| SICU* | 40.0% | 52.0% | |||||||||||
| Operating room | 28.0% | 16.0% | |||||||||||
| Average no. of attempts/procedure | 1.4 | 1.5 | |||||||||||
| Indications for subclavian insertion (n=25) | |||||||||||||
| Trauma/surgical site | 60.0% | ||||||||||||
| Need for additional access | 16.0% | ||||||||||||
| Unsuccessful IJ placement | 4.0% | ||||||||||||
| Unclear | 20.0% | ||||||||||||
| Iatrogenic Pneumothorax Rate (20062014) | Year | ||||||||||||
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||
| % of CVC insertions associated with IAP | 0.94 | 1.49 | 0.44 | 0.13 | 0.20 | 0.07 | 0.04 | 0.11 | 0.07 | ||||
| All‐cause IAP per 1,000 discharges | 1.32 | 1.29 | 0.98 | 0.71 | 0.83 | 0.49 | 0.13 | 0.35 | 0.23 | ||||
| Preintervention | Postintervention | P Value | |||||||||||
| CVC‐ associated IAP short term (2006 vs 2008) | 0.94% | 0.44% | 0.088 | ||||||||||
| CVC‐associated IAP long term (2006 vs 20082014) | 0.94% | 0.13% | <0.0001 | ||||||||||
| All‐cause IAP per 1,000 discharges short term (2006 vs 2008) | 1.32 | 0.98 | <0.0001 | ||||||||||
| All‐cause IAP per 1,000 discharges long term (2006 vs 2008‐14) | 1.32 | 0.52 | <0.0001 | ||||||||||
With the decrease in CVC‐associated IAP, we also saw a decrease in our all‐cause IAP rate per 1000 discharges from 1.32 in 2006 to 0.98 in 2008. This represents a 26% short‐term reduction (P<0.0001). We also saw a decrease in our all‐cause IAP rate per 1000 discharges to 0.52 from 2008 to 2014, representing a 61% long‐term reduction (P<0.0001). This decrease in all‐cause IAP postintervention occurred despite an older patient population (P<0.01) for all discharges. Our hospital is now in the highest performance UHC quartile for all‐cause IAP in 2012 to 2014.
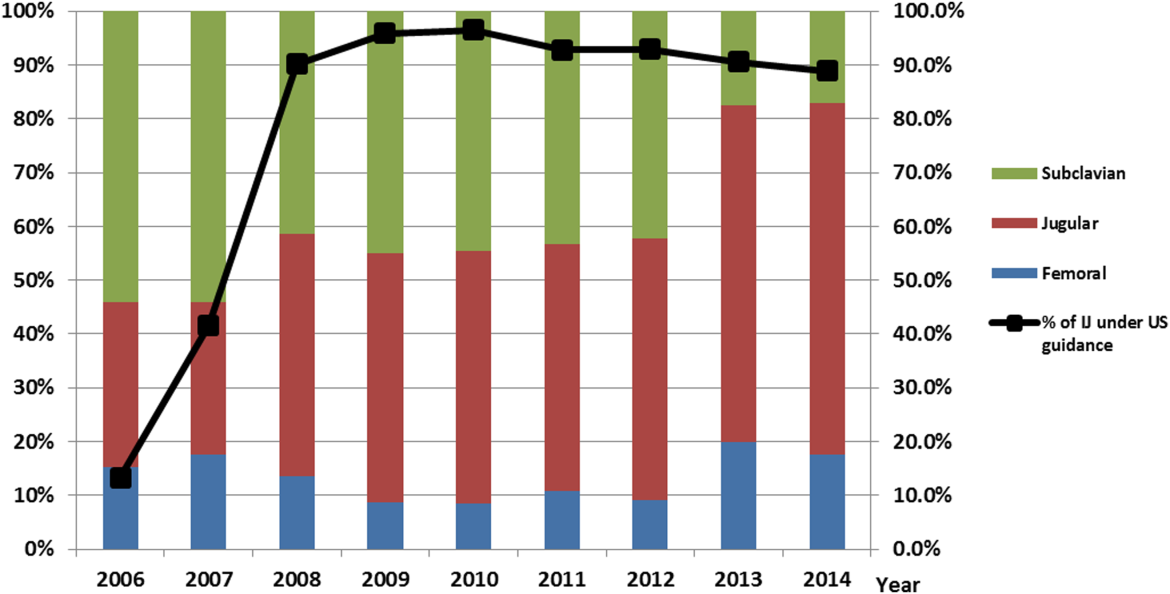
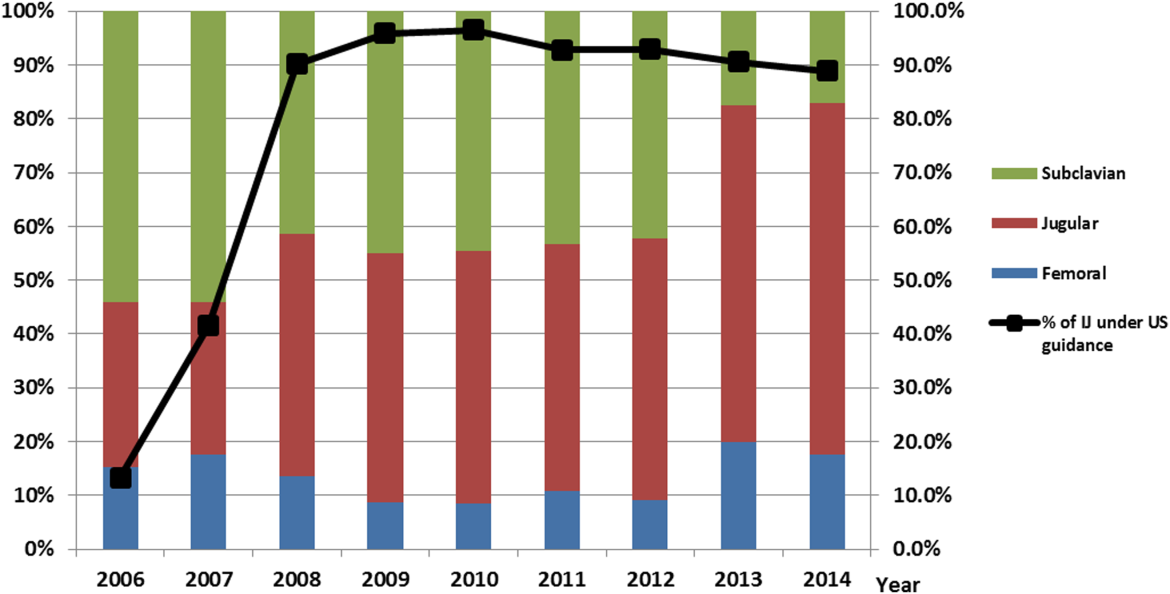
After our multifaceted intervention in 2007, there was substantially more and consistent documentation of CVC procedure notes from less than 500 in 2006 to greater than 2000 in 2009. The distribution of CVC procedure notes in the pre‐ (2006) versus postintervention (20082014) period showed a decrease in the proportion of femoral lines from 15% to 11%, increase in IJ lines from 31% to 49%, and a decrease in SC from 54% to 40% (P=0.001). The distribution of IJ CVC procedure notes in the pre‐ (2006) versus postintervention (20082014) period showed an increase in the proportion of procedures with ultrasound documentation from 13% to 93% (P<0.001) (Figure 3).
In our ICU 2014 audit, the majority of CVC lines were placed by residents under supervision (>70%), and most used the standard CVC note template to document the procedure (90%). Of the total CVC approach, 66% were IJ and 4% were SC. Eighty‐six percent used ultrasound during IJ placement. The majority of SC insertions were placed in the surgical ICU and had clear indications (80%) for placement. Of those, 75% were due to trauma (limited access to neck) or surgery (interfering with surgical site) (Table 2).
DISCUSSION
Summary
This quality‐improvement intervention demonstrates that a multidisciplinary team can successfully implement a multifaceted intervention that sustainably reduces the rate of IAP complications from CVC placement and improves patient safety over 7 years. We found high compliance with our intervention, which included an increase in CVC notes and documentation of ultrasound guidance. There was also an increase in the IJ approach in our postintervention period. We showed statistically significant long‐term reductions in both CVC‐associated and all‐cause IAP rates. From 2011 to 2014, there were only 5 cases of CVC‐associated IAP requiring chest tube placement. Post hoc analysis showed a statistically significant decrease in CLABSI rates (P<0.0001) from a preintervention rate of 1.6 infections per 1000 central line days to postintervention average rate of 0.68 infections per 1000 central line days. This decrease may be related to the incorporation of wide sterile barrier techniques in our CVC training workshops, checklists, and template procedure notes.
A strength of this study is the sustained significant long‐term reduction in IAP. There are few data that exist to describe sustained interventions in this area. Sustainability was achieved by integrating our interventions into ongoing programs that already existed in the hospital; we incorporated our simulation training into the existing new resident orientation, increased the availability of existing ultrasound equipment, and continued our IAP chart review through coding quality with feedback to involved services. The procedure note template continues to be easily available in our EMR, and the SC approach to CVC placement is limited to select cases.
Based on a post hoc cost‐benefit analysis, the financial benefits of decreasing the rate of IAP outweigh the costs associated with implementation of this initiative. The purchase cost for a Site‐Rite (Bard Access Systems) ultrasound machine was $18,000. The cost of materials for 1 workshop is $5000 annually. Cases from the Nationwide Inpatient Sample that were flagged by this PSI had 7.0% excess mortality, 4.4 days of excess hospitalization, and approximately $18,000 in excess hospital charges.[17, 18] Based on these data, if we had continued at our preintervention rate of CVC‐associated IAP requiring chest tube placement, we would estimate 9 additional CVC‐associated IAPs requiring chest tube insertion per year. This would result in over $180,000 of additional costs annually. Based on an initial cost of $100,000 for 4 workshops and the necessary equipment, we would have realized our cost savings in less than 1 year postintervention. These are all approximate costs, and further detailed analysis is needed.
One challenge with this intervention is the culture change away from using the SC approach, and the concern from trainees of how they would learn to perform SC CVC if needed. We would suggest dedicated SC CVC ultrasound training for those services who may need to use this approach (eg, neuroanesthesia and trauma).
Interpretation/Relation to Other Evidence
The field of implementation science can help explain why some projects are successful and others fail. We can further dissect the success of this project using an implementation science model similar to that described by French et al.[19] French et al. describe 4 behavior‐change techniques. These steps include (1) who needs to do what differently, (2) which barriers and enablers need to be addressed, (3) which intervention component could overcome the barriers and enhance enablers, and (4) how can behavior change be measured and understood. Barriers included suboptimal skills of residents, low awareness of evidence‐based guidelines, and entrenched practices inconsistent with best evidence. There was also a belief that IJ lines were more likely to become infected. Targeted behaviors needing to be done differently were the choice of CVC placement site and insertion technique. Barriers to change were assessed by asking members of the project team to explore with members of their service what led them to do CVC lines without ultrasound guidance. Enhancements focused on information provision, simulation practice, and persuasive communication. Behavior change was measured by tracking the number of IAPs, site of CVC, and documentation of technique. Continuation of these interventions based on this theoretical framework drove maintenance of gains.
We completed our main intervention planning in 90 days, and met our short‐term goal on schedule. The Institute for Healthcare Improvement (IHI) advocates that such short timelines are efficient mechanisms for developing and acting on projects. Other institutions have reported on similar rapid‐cycle planning and short‐term goal setting[20]
Limitations
Our study captures the experience of a quality‐improvement team at a single academic center, and our results may not be generalizable to other institutions. Our chart review process only occurred once a case had been identified through AHRQ PSI methodology. It is possible that the PSI does not capture all cases of IAP, although we believe our coding department has a very rigorous process to look for all IAP evidence in the patient's record. We used administrative data to determine the number of hospital‐wide CVC procedures.
Our compliance data with interventions from STRIDE are based on looking for key words in procedure note documentation (so undocumented notes are not captured). To validate this, we performed a manual audit of our adherence to our intervention in 2014, and those data are consistent with the results from our STRIDE data.
Our study's observational design also cannot control for exogenous effects on physician practice relating to CVC insertion or the overall risk of IAP. Some of our decrease in complications may be from the increase in PICC line use. Nevertheless, our CVC‐associated IAP rate has decreased despite >6000 non‐PICC CVCs in our ICU over the past 5 years, and a rising CMI (18% increase in postintervention period) and older population of patients with CVC insertion (P<0.0001)
CONCLUSIONS
We are the first, to our knowledge, to report a measurable improvement in reducing IAP patient outcomes that has been sustained for over 7 years. Our hospital is in the highest performance UHC quartile for all‐cause IAP in 2012 to 2014. A multidisciplinary quality‐improvement team, focused on evidence, patient safety, and standardization, can use a multifaceted intervention to sustainably improve patient outcomes. Promoting ultrasound‐guided IJ catheterization as the CVC insertion method of choice significantly reduced our hospital's rate of CVC‐associated IAP.
Acknowledgements
The authors acknowledge many who have contributed to this quality‐improvement project:
Irina Tokareva, Jay Lee, Kourt Bowes, and Gomathi Krishnan for data analysis; Laura Meinke for significant website curriculum; Fred Mihm, Sarah Williams, and John Kugler for leadership in ultrasound training; Kevin Tabb and Norm Rizk for hospital financial support of simulation workshops and ultrasound machines; Pooja Loftus and Helene Grossman for statistical analysis; Eric Hadhazy for data support; Joan Hendershott for cost information; Nancy Szaflarski for project management and manuscript review; and Isabella Chu for manuscript review.
Disclosures: STRIDE (Stanford Translational Research Integrated Database Environment) is a research and development project at Stanford University to create a standards‐based informatics platform supporting clinical and translational research. This STRIDE project was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
- , , . Significance of iatrogenic pneumothoraces. Chest. 1994;105(4):1147–1150.
- , , , , , . How to avoid and manage a pneumothorax. J Vasc Access. 2006;7(1):7–14.
- , , , . Iatrogenic pneumothorax: etiology, incidence and risk factors. Thorac Cardiovasc Surg. 2009;57(5):286–290.
- , , , et al. Real‐time ultrasound‐guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):R162.
- , , . Safe placement of central venous catheters: a measured approach. J Intens Care Med. 2011;26(6):392–396.
- , , , . Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero‐risk environment. Chest. 2009;135(5):1315–1320.
- , , , , , . Use of simulation‐based education to improve outcomes of central venous catheterization: a systematic review and meta‐analysis. Acad Med. 2011;86(9):1137–1147.
- , , , , , . A prerotational, simulation‐based workshop improves the safety of central venous catheter insertion: results of a successful internal medicine house staff training program. Chest. 2011;140(3):652–658.
- , , , , . Linking residency training effectiveness to clinical outcomes: a quality improvement approach. Jt Comm J Qual Patient Saf. 2010;36(5):203–208.
- , , , et al. Education of physicians‐in‐training can decrease the risk for vascular catheter infection. Ann Intern Med. 2000;132(8):641–648.
- , , , et al. A multidisciplinary approach to reduce central line‐associated bloodstream infections. Jt Comm J Qual Patient Saf. 2013;39(2):61–69.
- , , , et al. Validity of selected Patient Safety Indicators: opportunities and concerns. J Am Coll Surg. 2011;212(6):924–934.
- , , , et al. Cases of iatrogenic pneumothorax can be identified from ICD‐9‐CM coded data. Am J Med Qual. 2010;25(3):218–224.
- , , , , ; SQUIRE development group. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ. 2009;338:a3152.
- . The Quality Toolbox. 2nd ed. Milwaukee, WI: ASQ Quality Press; 2005.
- , , , . STRIDE—an integrated standards‐based translational research informatics platform. AMIA Annu Symp Proc. 2009;2009:391–395.
- , , . Accidental iatrogenic pneumothorax in hospitalized patients. Med Care. 2006;44(2):182–186.
- , . Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290(14):1868–1874.
- , , , et al. Developing theory‐informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38.
- , . Using rapid‐cycle quality improvement methodology to reduce feeding tubes in patients with advanced dementia: before and after study. BMJ. 2004;329(7464):491–494.
Iatrogenic pneumothorax (IAP) is a complication of invasive procedures that is associated with substantial morbidity and some mortality.[1] IAP is often avoidable, and in many cases can be prevented through adherence to evidence‐based guidelines and procedural techniques known to reduce the incidence of IAP.[2] IAP may occur with a subclavian (SC) or internal jugular (IJ) central venous catheter (CVC) insertion, but is more frequently associated with the SC approach.[3] Ultrasound guidance during IJ CVC insertion is associated with a lower risk as compared to guidance by anatomical landmarks.[4, 5] Other bedside procedures that are known to cause IAP include thoracentesis. This risk can also be reduced with the use of ultrasound guidance.[6]
Including simulation in training for CVC insertion has been demonstrated in meta‐analyses to improve both learner outcomes, including simulator performance and perceived confidence, and patient outcomes, including fewer failed CVC attempts and reduced incidence of IAP.[7] Even brief simulation workshops lasting less than two hours can improve patient safety during CVC insertion.[8]
The implementation of ultrasound‐based simulation and improved adherence to the actual use of ultrasound at the bedside can be motivated by tying competency‐based educational objectives (eg, CVC insertion) to clinical outcomes (ie, rates of IAP) and tracking both as part of a continuous quality‐improvement cycle.[9] Adherence to best practices for CVC insertion can also be improved through standardizing hospital‐wide policies and hands‐on training.[10] Involving many stakeholders, including nurses, physicians, nurse practioners and physician assistants, in a multidisciplinary team has been shown to help alter entrenched behaviors and reduce the incidence of central‐line associated bloodstream infections through long‐term adherence to evidence‐based interventions.[11]
LOCAL PROBLEM
The Agency for Healthcare Research and Quality (AHRQ) has designed Patient Safety Indicators (PSIs) (
Our hospital is a member of the University HealthSystem Consortium (UHC) (
Despite this, the PSI can highlight areas where quality‐improvement efforts might be best directed. In 2005 and 2006, our hospital was ranked within the lowest UHC performance quartile for all‐cause IAP PSI.
During FY 2006 (September 2005August 2006), root‐cause analysis on cases of IAP at our hospital found that CVC insertion (40%) was the most common procedure associated with IAP, with SC insertion causing 69% of CVC‐associated IAP. Other common procedures associated with IAP were operative/pacemaker (30%), thoracentesis (25%), and ventilator associated (5%). Ultrasound was not used in 2/5 cases of IJ CVC placement and 3/5 thoracentesis cases. Only 44% of CVC insertions had a procedure note.
Intended Improvement/Study Question
Our team set out to plan and implement a set of multifaceted interventions within 90 days. The short‐term goal was a 50% reduction in the CVC IAP and all‐cause IAP rate within 18 months, and the long‐term goal was sustained reduction of CVC IAP and all‐cause IAP rate.
METHODS
The format of this article is based on the standards for quality‐improvement reporting excellence guidelines for the reporting of studies on the effectiveness of quality‐improvement interventions.[14]
Setting
Stanford University Medical Center is an academic medical center with 465 beds and over 25,000 inpatient admissions per year, providing both general acute care services and tertiary medical care. Residents perform CVC bedside procedures when central venous access is needed, in the intensive care unit (ICU), operating room (OR), and inpatient units. Prior to this project, ultrasound equipment was only available in the emergency department (ED) and ICUs. There was no formal CVC procedure supervision policy, CVC training curriculum, and procedure note templates for documentation of CVC insertion.
Planning the Interventions
A multidisciplinary quality‐improvement team met weekly during the 90‐day design period from January 2007 to March 2007. Our team included representatives from the departments of medicine, anesthesia and critical care, surgery, nursing, and emergency medicine. We also partnered with our institution's clinical and administrative leaders, experts in simulation, and the hospital quality department.
We hypothesized that a standardized set of education and training interventions promoting ultrasound‐guided IJ CVC insertion as the method of choice at our hospital would significantly reduce our rate of CVC‐associated IAP. Our multifaceted intervention included: (1) clinical and documentation standards based on evidence, (2) cognitive aids, (3) simulation training, (4) purchase and deployment of ultrasound equipment, and (5) feedback to clinical services.
Our team followed the define, measure, analyze, improve, control (DMAIC) framework.[15] We set interval goals with target completion dates throughout the 90‐day period, identified owners of each goal, and tracked progress with a shared spreadsheet.
In the 90‐day intervention, we accomplished the following: (1) conducted root‐cause analysis of IAP cases for fiscal year 2006, (2) created clinical and documentation standards around CVC placement, (3) created cognitive aids and procedure note templates, (4) developed simulation training courses, and (5) requested purchase of additional ultrasound equipment.
Data Collection
To evaluate our progress in reducing the rates of IAP, we tracked the incidence of IAP using UHC and AHRQ PSI methodology. In collaboration with our hospital's quality department, we manually reviewed every PSI‐identified case of IAP. This review has focused on identifying whether or not pneumothorax actually occurred, and whether it was associated with CVC insertion. For those associated with CVC, data were collected for patient location and service, the procedure site, whether ultrasound was used, whether a chest tube was required, and the final disposition of the patient.
Demographic data (age, gender, case mix index [CMI]) shown in Table 1 were obtained through MIDAS+ Solutions (Tucson, Arizona), a proprietary database that contains healthcare management coded data. Total hospital CVC insertion rates were calculated using International Classification of Diseases, Ninth Revision (ICD‐9) coding for 38.93 and 38.97. ICU central lineassociated blood stream infections (CLABSI) data were obtained from internal collection by our infection control team. Number and location of CVCs placed in the ICU data were obtained from nursing flow sheets in our electronic medical record (EMR). Cost information was provided by our finance department using internal accounting.
| Patients With CVC Insertion | Year | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| |||||||||
| Age, y (mean) | 55.0 | 55.5 | 55.0 | 57.0 | 56.5 | 58.5 | 57.5 | 59.0 | 58.5 |
| % female | 47.0 | 49.5 | 47.0 | 48.8 | 46.2 | 46.1 | 45.7 | 46.2 | 45.7 |
| Case‐mix index | 3.08 | 3.35 | 3.21 | 3.40 | 3.71 | 3.91 | 3.92 | 3.92 | 4.08 |
| Total no. of CVCs/year* | 1,593 | 1,141 | 1,589 | 2,250 | 2,441 | 2,774 | 2,754 | 2,722 | 2,845 |
| No. of CVCs/year in ICU | NA | NA | NA | 1,502 | 1,357 | 1,345 | 1,316 | 1,421 | 1,590 |
| No. of subclavians/year in ICU | NA | NA | NA | 167 | 75 | 70 | 83 | 75 | 97 |
| No. of IJs/year in ICU | NA | NA | NA | 898 | 773 | 681 | 677 | 713 | 876 |
| No. of femorals/year in ICU | NA | NA | NA | 212 | 152 | 203 | 171 | 198 | 206 |
| No. of PICCs/year in ICU | NA | NA | NA | 225 | 357 | 391 | 385 | 435 | 411 |
| Preintervention (2006) | Postintervention (20082014) | P Value | |||||||
| Age, y (mean) | 55.2 | 58.7 | <0.0001 | ||||||
| % female | 47.0% | 46.4% | 0.642 | ||||||
| Case‐mix index | 3.08 | 3.73 | <0.0001 | ||||||
| CVC insertion rate | 8.1% | 11.4% | <0.0001 | ||||||
| All Inpatients | Year | ||||||||
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Age, y (mean) | 57.1 | 57.2 | 56.8 | 57.2 | 57.5 | 58.0 | 58.0 | 57.9 | 58.3 |
| % female | 51.6 | 51.2 | 52.4 | 51.7 | 51.1 | 51.5 | 50.3 | 49.9 | 50.1 |
| Case‐mix index | 1.86 | 1.98 | 1.96 | 1.99 | 1.96 | 2.02 | 2.03 | 2.07 | 2.23 |
| Preintervention (2006) | Postintervention (20082014) | P Value | |||||||
| Age, y (mean) | 57.1 | 57.6 | <0.01 | ||||||
| % female | 51.6% | 50.9% | 0.07 | ||||||
| Case‐mix index | 1.86 | 2.03 | 0.13 | ||||||
| Central Line‐Associated Bloodstream Infections per 1,000 Central Line Days | |||||||||
| Preintervention | Postintervention | P Value | |||||||
| Short term (2006 vs 2008) | 1.8 | 0.60 | 0.004 | ||||||
| Long term (2006 vs 20082014) | 1.8 | 0.68 | <0.0001 | ||||||
The project granted a Notice of Determination of Approval from the Stanford Administrative Panels for the Protection of Human Subjects (institutional review board).
Methods of Evaluation/Analysis
For the purpose of this analysis, the preintervention period was defined as January 1, 2006 through December 31, 2006, our first year of IAP case review. We defined the intervention period as January 1, 2007 through December 31, 2007, during which we planned and implemented hospital‐wide standardization of CVC insertion practices and incorporated CVC insertion training simulation into resident orientation in July 2007. The postintervention period was defined as January 1, 2008 through December 31, 2014.
All statistical analyses were performed using Stata version 12.1 (StataCorp, College Station, TX). [2] tests were used to determine statistical differences in pre‐ versus postintervention patient demographic data (age, gender, CMI), CVC insertion rates, and CLABSI rates. Because IAP is a rare event, a statistical process control g‐chart was created using QI Macros (KnowWare International, Inc., Denver, CO) to show the number of CVC procedures between IAP. [2] and Fisher exact tests were used to determine statistical differences in CVC anatomic location and use of ultrasound pre‐ and postintervention. A 2‐sided Z test to show a difference in proportions was used to determine statistical differences in CVC‐related IAP rate and all‐cause IAP rate pre‐ and postintervention.
Measuring Adherence to Intervention
Location of CVC Placement and Ultrasound Guidance Pre‐ Versus Postintervention
We utilized the Stanford Clinical Informatics Center (SCCI) services for obtaining counts of patients. Custom queries were performed on SCCI's Stanford Translational Research Integrated Database Environment (STRIDE) platform[16] to search Stanford Hospital electronic heath records for patients. This search primarily involved getting counts for the number of patients with clinical notes that contained the keywords of interest. To identify documentation for placement of CVC from 2006 to 2014, procedure or operative notes containing the words central line or CVC were counted. Further subcounts were obtained by searching for additional keywords such as PICC [peripherally inserted central catheters], femoral, jugular, subclavian, and ultrasound.
Adherence to Intervention in the ICU in 2014
A total of 100 charts were reviewed from patients in our medical and surgical ICU with a CVC in 2014 to evaluate the current trend of central line placement and sustainability of our intervention. Fifty charts were initially randomly selected from the ICU cohort. For those who had multiple lines placed, only the first line was reviewed. Because the initial audit did not provide enough SC lines and we wanted to review more IJ lines, we randomly selected an additional 25 patients who had SC and 25 patients who had IJ to review. The following was collected during chart review: primary team, location of line placement, usage of ultrasound, usage of standard procedure template, supervision, level of training for supervisor, and level of training for staff who performed procedure.
Outcomes
The rate of CVC‐associated IAP was calculated as the total number of IAPs attributed to CVCs divided by the total number of CVCs inserted determined by ICD‐9 coding for 38.93 and 38.97. The total IAP rate was calculated as the total number of IAP/1000 discharges.
RESULTS
Interventions
Our team began the intervention in early 2007 with promotion of ultrasound‐guided IJ catheterization. Clinical exceptions included: (1) trauma or code situations where access to the neck is limited, (2) suspected or confirmed neck injuries, (3) presence of a tracheostomy, and (4) bilateral internal jugular sites unsuitable for catheterization.
Our hospital adopted new formal CVC insertion policies consistent with the above training and education efforts. All physicians were required to document CVC insertions using the template available in the EMR. To be certified to perform CVC insertion independently, trainee physicians were required to complete the simulation training and successfully place a minimum of 5 CVCs directly supervised by an already‐certified physician. This was consistent with the Accreditation Council for Graduate Medical Education suggested minimum requirement in 2007. In our critical care units, all CVC insertions must be supervised by an ICU fellow or attending.
To reinforce the on‐the‐ground work by our physician leaders, we created 2 education tools to embed best practices into our CVC insertion workflow. A checklist with best practices for CVC insertion that was distributed throughout the hospital via central line kits and educational flyers, and a CVC insertion procedure note template consistent with California Department of Public Health documentation requirements was made available in our EMR.
In June 2007, we integrated CVC insertion simulation training into procedure workshops required for all medicine, surgery, anesthesia, and emergency medicine trainees during their intern year. These workshops promoted ultrasound‐guided IJ catheterization and supporting evidence for the new IJ site preference. Training sessions were 2 to 3 hours, and included a demonstration of best‐practice CVC insertion, as well as training with simulation models supervised by an instructor using a standardized CVC checklist. These trainings used both the Blue Phantom human torso model (
Hospital administration provided funds to purchase ultrasound machines for patient units such as medicine, cardiology, ED, and ICU). A total of 4 Site‐Rite (Bard Access Systems, Inc., Salt Lake City, UT) ultrasounds were purchased in 2007. The hospital has continued to purchase ultrasound units yearly, and had 53 ultrasound units in 2014
Cases of IAP were continuously reviewed throughout the intervention period. Based on their higher CVC‐associated IAP rates, the ORs and catheterization lab were identified as having opportunities for improvement. In 2008, Hospital quality‐improvement leadership met with physician leaders in these areas to review their CVC‐related IAP data and to discuss strategies to reduce their IAP rates. These strategies included lessons learned from other services that had successfully decreased their IAP rates.
To sustain our gains, we continue to review all IAP through our coding quality, clinical documentation, quality reporting departments, and peer review. We have implemented other strategies to decrease IAP, such as the use of ultrasound guidance for bedside thoracentesis procedures, which became possible after the availability of more ultrasound devices. Training for ultrasound‐guided thoracentesis was done by our procedure‐team attending during supervision of residents.
Outcomes
Preintervention (January 1, 2006 to December 31, 2006)
There were a total of 26 cases of IAP in 2006. Of these, 15 (58%) were associated with CVC insertion (Figure 1). The single procedure associated with the largest proportion of IAP was SC CVC insertion (11 cases, 42% of all IAP cases). Eleven CVC‐associated IAPs were significant enough to require chest tube placement. Our hospital recorded a total of 1593 CVC insertions (ICD‐9 codes 38.93 and 38.97) in 2006.
Postintervention (January 1, 2008 to December 31, 2014)
There were a total of 80 cases of IAP over 7 years, of which 24 (30%) were associated with CVC insertion. Of these, 16 required chest tube placement. In the last 4 years of the postintervention period (20112014), there were only 5 cases of CVC‐associated IAP requiring chest tube placement (Figure 1). There were a total of 12,000 CVC insertions recorded over the same period.
We successfully met both our short‐ and long‐term goals. Our preintervention CVC‐associated IAP rate was 0.94%, and our post‐intervention rate during 2008 was 0.44%, a short‐term reduction of 53% (P=0.088). Our average postintervention CVC‐associated IAP rate for the years 2008 through 2014 was 0.13%, a significant long‐term reduction of 86% (P<0.0001) (Table 2). The decrease in CVC‐associated IAP rates occurred despite an older patient population (P<0.001) and a higher CMI (P<0.001) in postintervention patients who received a CVC (Table 1). Special cause variation corresponding to a change in our process is demonstrated in Figure 2. The preintervention average number of procedures between IAP was 114.8 and increased to 460.7 in the postintervention period.
| Total CVC (n=95) | Subclavian (n=29) | Internal Jugular (n=58) | Femoral (n=8) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||
| Compliance to intervention | |||||||||||||
| US guided | 68.1% | 20.7% | 86.2% | 100.0% | |||||||||
| Procedure note completion | 90.4% | 93.1% | 86.2% | 100.0% | |||||||||
| Supervision | 70.2% | 77.8% | 73.1% | 87.5% | |||||||||
| Level of training | |||||||||||||
| Resident | 61.1% | 58.6% | 60.3% | 75.0% | |||||||||
| Fellow | 25.3% | 27.6% | 24.1% | 25.0% | |||||||||
| Attending | 4.2% | 6.9% | 3.4% | 0.0% | |||||||||
| Advance practitioner | 3.2% | 3.4% | 3.4% | 0.0% | |||||||||
| Unknown | 6.3% | 3.4% | 8.6% | 0.0% | |||||||||
| Supervisor type | |||||||||||||
| Resident | 3.0% | 4.8% | 2.6% | 0.0% | |||||||||
| Fellow | 54.5% | 33.3% | 57.9% | 100.0% | |||||||||
| Attending | 42.4% | 61.9% | 39.5% | 0.0% | |||||||||
| Location of CVC Placement | Internal Jugular (n=25) | Subclavian (n=25) | |||||||||||
| MICU | 32.0% | 32.0% | |||||||||||
| SICU* | 40.0% | 52.0% | |||||||||||
| Operating room | 28.0% | 16.0% | |||||||||||
| Average no. of attempts/procedure | 1.4 | 1.5 | |||||||||||
| Indications for subclavian insertion (n=25) | |||||||||||||
| Trauma/surgical site | 60.0% | ||||||||||||
| Need for additional access | 16.0% | ||||||||||||
| Unsuccessful IJ placement | 4.0% | ||||||||||||
| Unclear | 20.0% | ||||||||||||
| Iatrogenic Pneumothorax Rate (20062014) | Year | ||||||||||||
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||
| % of CVC insertions associated with IAP | 0.94 | 1.49 | 0.44 | 0.13 | 0.20 | 0.07 | 0.04 | 0.11 | 0.07 | ||||
| All‐cause IAP per 1,000 discharges | 1.32 | 1.29 | 0.98 | 0.71 | 0.83 | 0.49 | 0.13 | 0.35 | 0.23 | ||||
| Preintervention | Postintervention | P Value | |||||||||||
| CVC‐ associated IAP short term (2006 vs 2008) | 0.94% | 0.44% | 0.088 | ||||||||||
| CVC‐associated IAP long term (2006 vs 20082014) | 0.94% | 0.13% | <0.0001 | ||||||||||
| All‐cause IAP per 1,000 discharges short term (2006 vs 2008) | 1.32 | 0.98 | <0.0001 | ||||||||||
| All‐cause IAP per 1,000 discharges long term (2006 vs 2008‐14) | 1.32 | 0.52 | <0.0001 | ||||||||||
With the decrease in CVC‐associated IAP, we also saw a decrease in our all‐cause IAP rate per 1000 discharges from 1.32 in 2006 to 0.98 in 2008. This represents a 26% short‐term reduction (P<0.0001). We also saw a decrease in our all‐cause IAP rate per 1000 discharges to 0.52 from 2008 to 2014, representing a 61% long‐term reduction (P<0.0001). This decrease in all‐cause IAP postintervention occurred despite an older patient population (P<0.01) for all discharges. Our hospital is now in the highest performance UHC quartile for all‐cause IAP in 2012 to 2014.
After our multifaceted intervention in 2007, there was substantially more and consistent documentation of CVC procedure notes from less than 500 in 2006 to greater than 2000 in 2009. The distribution of CVC procedure notes in the pre‐ (2006) versus postintervention (20082014) period showed a decrease in the proportion of femoral lines from 15% to 11%, increase in IJ lines from 31% to 49%, and a decrease in SC from 54% to 40% (P=0.001). The distribution of IJ CVC procedure notes in the pre‐ (2006) versus postintervention (20082014) period showed an increase in the proportion of procedures with ultrasound documentation from 13% to 93% (P<0.001) (Figure 3).
In our ICU 2014 audit, the majority of CVC lines were placed by residents under supervision (>70%), and most used the standard CVC note template to document the procedure (90%). Of the total CVC approach, 66% were IJ and 4% were SC. Eighty‐six percent used ultrasound during IJ placement. The majority of SC insertions were placed in the surgical ICU and had clear indications (80%) for placement. Of those, 75% were due to trauma (limited access to neck) or surgery (interfering with surgical site) (Table 2).
DISCUSSION
Summary
This quality‐improvement intervention demonstrates that a multidisciplinary team can successfully implement a multifaceted intervention that sustainably reduces the rate of IAP complications from CVC placement and improves patient safety over 7 years. We found high compliance with our intervention, which included an increase in CVC notes and documentation of ultrasound guidance. There was also an increase in the IJ approach in our postintervention period. We showed statistically significant long‐term reductions in both CVC‐associated and all‐cause IAP rates. From 2011 to 2014, there were only 5 cases of CVC‐associated IAP requiring chest tube placement. Post hoc analysis showed a statistically significant decrease in CLABSI rates (P<0.0001) from a preintervention rate of 1.6 infections per 1000 central line days to postintervention average rate of 0.68 infections per 1000 central line days. This decrease may be related to the incorporation of wide sterile barrier techniques in our CVC training workshops, checklists, and template procedure notes.
A strength of this study is the sustained significant long‐term reduction in IAP. There are few data that exist to describe sustained interventions in this area. Sustainability was achieved by integrating our interventions into ongoing programs that already existed in the hospital; we incorporated our simulation training into the existing new resident orientation, increased the availability of existing ultrasound equipment, and continued our IAP chart review through coding quality with feedback to involved services. The procedure note template continues to be easily available in our EMR, and the SC approach to CVC placement is limited to select cases.
Based on a post hoc cost‐benefit analysis, the financial benefits of decreasing the rate of IAP outweigh the costs associated with implementation of this initiative. The purchase cost for a Site‐Rite (Bard Access Systems) ultrasound machine was $18,000. The cost of materials for 1 workshop is $5000 annually. Cases from the Nationwide Inpatient Sample that were flagged by this PSI had 7.0% excess mortality, 4.4 days of excess hospitalization, and approximately $18,000 in excess hospital charges.[17, 18] Based on these data, if we had continued at our preintervention rate of CVC‐associated IAP requiring chest tube placement, we would estimate 9 additional CVC‐associated IAPs requiring chest tube insertion per year. This would result in over $180,000 of additional costs annually. Based on an initial cost of $100,000 for 4 workshops and the necessary equipment, we would have realized our cost savings in less than 1 year postintervention. These are all approximate costs, and further detailed analysis is needed.
One challenge with this intervention is the culture change away from using the SC approach, and the concern from trainees of how they would learn to perform SC CVC if needed. We would suggest dedicated SC CVC ultrasound training for those services who may need to use this approach (eg, neuroanesthesia and trauma).
Interpretation/Relation to Other Evidence
The field of implementation science can help explain why some projects are successful and others fail. We can further dissect the success of this project using an implementation science model similar to that described by French et al.[19] French et al. describe 4 behavior‐change techniques. These steps include (1) who needs to do what differently, (2) which barriers and enablers need to be addressed, (3) which intervention component could overcome the barriers and enhance enablers, and (4) how can behavior change be measured and understood. Barriers included suboptimal skills of residents, low awareness of evidence‐based guidelines, and entrenched practices inconsistent with best evidence. There was also a belief that IJ lines were more likely to become infected. Targeted behaviors needing to be done differently were the choice of CVC placement site and insertion technique. Barriers to change were assessed by asking members of the project team to explore with members of their service what led them to do CVC lines without ultrasound guidance. Enhancements focused on information provision, simulation practice, and persuasive communication. Behavior change was measured by tracking the number of IAPs, site of CVC, and documentation of technique. Continuation of these interventions based on this theoretical framework drove maintenance of gains.
We completed our main intervention planning in 90 days, and met our short‐term goal on schedule. The Institute for Healthcare Improvement (IHI) advocates that such short timelines are efficient mechanisms for developing and acting on projects. Other institutions have reported on similar rapid‐cycle planning and short‐term goal setting[20]
Limitations
Our study captures the experience of a quality‐improvement team at a single academic center, and our results may not be generalizable to other institutions. Our chart review process only occurred once a case had been identified through AHRQ PSI methodology. It is possible that the PSI does not capture all cases of IAP, although we believe our coding department has a very rigorous process to look for all IAP evidence in the patient's record. We used administrative data to determine the number of hospital‐wide CVC procedures.
Our compliance data with interventions from STRIDE are based on looking for key words in procedure note documentation (so undocumented notes are not captured). To validate this, we performed a manual audit of our adherence to our intervention in 2014, and those data are consistent with the results from our STRIDE data.
Our study's observational design also cannot control for exogenous effects on physician practice relating to CVC insertion or the overall risk of IAP. Some of our decrease in complications may be from the increase in PICC line use. Nevertheless, our CVC‐associated IAP rate has decreased despite >6000 non‐PICC CVCs in our ICU over the past 5 years, and a rising CMI (18% increase in postintervention period) and older population of patients with CVC insertion (P<0.0001)
CONCLUSIONS
We are the first, to our knowledge, to report a measurable improvement in reducing IAP patient outcomes that has been sustained for over 7 years. Our hospital is in the highest performance UHC quartile for all‐cause IAP in 2012 to 2014. A multidisciplinary quality‐improvement team, focused on evidence, patient safety, and standardization, can use a multifaceted intervention to sustainably improve patient outcomes. Promoting ultrasound‐guided IJ catheterization as the CVC insertion method of choice significantly reduced our hospital's rate of CVC‐associated IAP.
Acknowledgements
The authors acknowledge many who have contributed to this quality‐improvement project:
Irina Tokareva, Jay Lee, Kourt Bowes, and Gomathi Krishnan for data analysis; Laura Meinke for significant website curriculum; Fred Mihm, Sarah Williams, and John Kugler for leadership in ultrasound training; Kevin Tabb and Norm Rizk for hospital financial support of simulation workshops and ultrasound machines; Pooja Loftus and Helene Grossman for statistical analysis; Eric Hadhazy for data support; Joan Hendershott for cost information; Nancy Szaflarski for project management and manuscript review; and Isabella Chu for manuscript review.
Disclosures: STRIDE (Stanford Translational Research Integrated Database Environment) is a research and development project at Stanford University to create a standards‐based informatics platform supporting clinical and translational research. This STRIDE project was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
Iatrogenic pneumothorax (IAP) is a complication of invasive procedures that is associated with substantial morbidity and some mortality.[1] IAP is often avoidable, and in many cases can be prevented through adherence to evidence‐based guidelines and procedural techniques known to reduce the incidence of IAP.[2] IAP may occur with a subclavian (SC) or internal jugular (IJ) central venous catheter (CVC) insertion, but is more frequently associated with the SC approach.[3] Ultrasound guidance during IJ CVC insertion is associated with a lower risk as compared to guidance by anatomical landmarks.[4, 5] Other bedside procedures that are known to cause IAP include thoracentesis. This risk can also be reduced with the use of ultrasound guidance.[6]
Including simulation in training for CVC insertion has been demonstrated in meta‐analyses to improve both learner outcomes, including simulator performance and perceived confidence, and patient outcomes, including fewer failed CVC attempts and reduced incidence of IAP.[7] Even brief simulation workshops lasting less than two hours can improve patient safety during CVC insertion.[8]
The implementation of ultrasound‐based simulation and improved adherence to the actual use of ultrasound at the bedside can be motivated by tying competency‐based educational objectives (eg, CVC insertion) to clinical outcomes (ie, rates of IAP) and tracking both as part of a continuous quality‐improvement cycle.[9] Adherence to best practices for CVC insertion can also be improved through standardizing hospital‐wide policies and hands‐on training.[10] Involving many stakeholders, including nurses, physicians, nurse practioners and physician assistants, in a multidisciplinary team has been shown to help alter entrenched behaviors and reduce the incidence of central‐line associated bloodstream infections through long‐term adherence to evidence‐based interventions.[11]
LOCAL PROBLEM
The Agency for Healthcare Research and Quality (AHRQ) has designed Patient Safety Indicators (PSIs) (
Our hospital is a member of the University HealthSystem Consortium (UHC) (
Despite this, the PSI can highlight areas where quality‐improvement efforts might be best directed. In 2005 and 2006, our hospital was ranked within the lowest UHC performance quartile for all‐cause IAP PSI.
During FY 2006 (September 2005August 2006), root‐cause analysis on cases of IAP at our hospital found that CVC insertion (40%) was the most common procedure associated with IAP, with SC insertion causing 69% of CVC‐associated IAP. Other common procedures associated with IAP were operative/pacemaker (30%), thoracentesis (25%), and ventilator associated (5%). Ultrasound was not used in 2/5 cases of IJ CVC placement and 3/5 thoracentesis cases. Only 44% of CVC insertions had a procedure note.
Intended Improvement/Study Question
Our team set out to plan and implement a set of multifaceted interventions within 90 days. The short‐term goal was a 50% reduction in the CVC IAP and all‐cause IAP rate within 18 months, and the long‐term goal was sustained reduction of CVC IAP and all‐cause IAP rate.
METHODS
The format of this article is based on the standards for quality‐improvement reporting excellence guidelines for the reporting of studies on the effectiveness of quality‐improvement interventions.[14]
Setting
Stanford University Medical Center is an academic medical center with 465 beds and over 25,000 inpatient admissions per year, providing both general acute care services and tertiary medical care. Residents perform CVC bedside procedures when central venous access is needed, in the intensive care unit (ICU), operating room (OR), and inpatient units. Prior to this project, ultrasound equipment was only available in the emergency department (ED) and ICUs. There was no formal CVC procedure supervision policy, CVC training curriculum, and procedure note templates for documentation of CVC insertion.
Planning the Interventions
A multidisciplinary quality‐improvement team met weekly during the 90‐day design period from January 2007 to March 2007. Our team included representatives from the departments of medicine, anesthesia and critical care, surgery, nursing, and emergency medicine. We also partnered with our institution's clinical and administrative leaders, experts in simulation, and the hospital quality department.
We hypothesized that a standardized set of education and training interventions promoting ultrasound‐guided IJ CVC insertion as the method of choice at our hospital would significantly reduce our rate of CVC‐associated IAP. Our multifaceted intervention included: (1) clinical and documentation standards based on evidence, (2) cognitive aids, (3) simulation training, (4) purchase and deployment of ultrasound equipment, and (5) feedback to clinical services.
Our team followed the define, measure, analyze, improve, control (DMAIC) framework.[15] We set interval goals with target completion dates throughout the 90‐day period, identified owners of each goal, and tracked progress with a shared spreadsheet.
In the 90‐day intervention, we accomplished the following: (1) conducted root‐cause analysis of IAP cases for fiscal year 2006, (2) created clinical and documentation standards around CVC placement, (3) created cognitive aids and procedure note templates, (4) developed simulation training courses, and (5) requested purchase of additional ultrasound equipment.
Data Collection
To evaluate our progress in reducing the rates of IAP, we tracked the incidence of IAP using UHC and AHRQ PSI methodology. In collaboration with our hospital's quality department, we manually reviewed every PSI‐identified case of IAP. This review has focused on identifying whether or not pneumothorax actually occurred, and whether it was associated with CVC insertion. For those associated with CVC, data were collected for patient location and service, the procedure site, whether ultrasound was used, whether a chest tube was required, and the final disposition of the patient.
Demographic data (age, gender, case mix index [CMI]) shown in Table 1 were obtained through MIDAS+ Solutions (Tucson, Arizona), a proprietary database that contains healthcare management coded data. Total hospital CVC insertion rates were calculated using International Classification of Diseases, Ninth Revision (ICD‐9) coding for 38.93 and 38.97. ICU central lineassociated blood stream infections (CLABSI) data were obtained from internal collection by our infection control team. Number and location of CVCs placed in the ICU data were obtained from nursing flow sheets in our electronic medical record (EMR). Cost information was provided by our finance department using internal accounting.
| Patients With CVC Insertion | Year | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| |||||||||
| Age, y (mean) | 55.0 | 55.5 | 55.0 | 57.0 | 56.5 | 58.5 | 57.5 | 59.0 | 58.5 |
| % female | 47.0 | 49.5 | 47.0 | 48.8 | 46.2 | 46.1 | 45.7 | 46.2 | 45.7 |
| Case‐mix index | 3.08 | 3.35 | 3.21 | 3.40 | 3.71 | 3.91 | 3.92 | 3.92 | 4.08 |
| Total no. of CVCs/year* | 1,593 | 1,141 | 1,589 | 2,250 | 2,441 | 2,774 | 2,754 | 2,722 | 2,845 |
| No. of CVCs/year in ICU | NA | NA | NA | 1,502 | 1,357 | 1,345 | 1,316 | 1,421 | 1,590 |
| No. of subclavians/year in ICU | NA | NA | NA | 167 | 75 | 70 | 83 | 75 | 97 |
| No. of IJs/year in ICU | NA | NA | NA | 898 | 773 | 681 | 677 | 713 | 876 |
| No. of femorals/year in ICU | NA | NA | NA | 212 | 152 | 203 | 171 | 198 | 206 |
| No. of PICCs/year in ICU | NA | NA | NA | 225 | 357 | 391 | 385 | 435 | 411 |
| Preintervention (2006) | Postintervention (20082014) | P Value | |||||||
| Age, y (mean) | 55.2 | 58.7 | <0.0001 | ||||||
| % female | 47.0% | 46.4% | 0.642 | ||||||
| Case‐mix index | 3.08 | 3.73 | <0.0001 | ||||||
| CVC insertion rate | 8.1% | 11.4% | <0.0001 | ||||||
| All Inpatients | Year | ||||||||
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Age, y (mean) | 57.1 | 57.2 | 56.8 | 57.2 | 57.5 | 58.0 | 58.0 | 57.9 | 58.3 |
| % female | 51.6 | 51.2 | 52.4 | 51.7 | 51.1 | 51.5 | 50.3 | 49.9 | 50.1 |
| Case‐mix index | 1.86 | 1.98 | 1.96 | 1.99 | 1.96 | 2.02 | 2.03 | 2.07 | 2.23 |
| Preintervention (2006) | Postintervention (20082014) | P Value | |||||||
| Age, y (mean) | 57.1 | 57.6 | <0.01 | ||||||
| % female | 51.6% | 50.9% | 0.07 | ||||||
| Case‐mix index | 1.86 | 2.03 | 0.13 | ||||||
| Central Line‐Associated Bloodstream Infections per 1,000 Central Line Days | |||||||||
| Preintervention | Postintervention | P Value | |||||||
| Short term (2006 vs 2008) | 1.8 | 0.60 | 0.004 | ||||||
| Long term (2006 vs 20082014) | 1.8 | 0.68 | <0.0001 | ||||||
The project granted a Notice of Determination of Approval from the Stanford Administrative Panels for the Protection of Human Subjects (institutional review board).
Methods of Evaluation/Analysis
For the purpose of this analysis, the preintervention period was defined as January 1, 2006 through December 31, 2006, our first year of IAP case review. We defined the intervention period as January 1, 2007 through December 31, 2007, during which we planned and implemented hospital‐wide standardization of CVC insertion practices and incorporated CVC insertion training simulation into resident orientation in July 2007. The postintervention period was defined as January 1, 2008 through December 31, 2014.
All statistical analyses were performed using Stata version 12.1 (StataCorp, College Station, TX). [2] tests were used to determine statistical differences in pre‐ versus postintervention patient demographic data (age, gender, CMI), CVC insertion rates, and CLABSI rates. Because IAP is a rare event, a statistical process control g‐chart was created using QI Macros (KnowWare International, Inc., Denver, CO) to show the number of CVC procedures between IAP. [2] and Fisher exact tests were used to determine statistical differences in CVC anatomic location and use of ultrasound pre‐ and postintervention. A 2‐sided Z test to show a difference in proportions was used to determine statistical differences in CVC‐related IAP rate and all‐cause IAP rate pre‐ and postintervention.
Measuring Adherence to Intervention
Location of CVC Placement and Ultrasound Guidance Pre‐ Versus Postintervention
We utilized the Stanford Clinical Informatics Center (SCCI) services for obtaining counts of patients. Custom queries were performed on SCCI's Stanford Translational Research Integrated Database Environment (STRIDE) platform[16] to search Stanford Hospital electronic heath records for patients. This search primarily involved getting counts for the number of patients with clinical notes that contained the keywords of interest. To identify documentation for placement of CVC from 2006 to 2014, procedure or operative notes containing the words central line or CVC were counted. Further subcounts were obtained by searching for additional keywords such as PICC [peripherally inserted central catheters], femoral, jugular, subclavian, and ultrasound.
Adherence to Intervention in the ICU in 2014
A total of 100 charts were reviewed from patients in our medical and surgical ICU with a CVC in 2014 to evaluate the current trend of central line placement and sustainability of our intervention. Fifty charts were initially randomly selected from the ICU cohort. For those who had multiple lines placed, only the first line was reviewed. Because the initial audit did not provide enough SC lines and we wanted to review more IJ lines, we randomly selected an additional 25 patients who had SC and 25 patients who had IJ to review. The following was collected during chart review: primary team, location of line placement, usage of ultrasound, usage of standard procedure template, supervision, level of training for supervisor, and level of training for staff who performed procedure.
Outcomes
The rate of CVC‐associated IAP was calculated as the total number of IAPs attributed to CVCs divided by the total number of CVCs inserted determined by ICD‐9 coding for 38.93 and 38.97. The total IAP rate was calculated as the total number of IAP/1000 discharges.
RESULTS
Interventions
Our team began the intervention in early 2007 with promotion of ultrasound‐guided IJ catheterization. Clinical exceptions included: (1) trauma or code situations where access to the neck is limited, (2) suspected or confirmed neck injuries, (3) presence of a tracheostomy, and (4) bilateral internal jugular sites unsuitable for catheterization.
Our hospital adopted new formal CVC insertion policies consistent with the above training and education efforts. All physicians were required to document CVC insertions using the template available in the EMR. To be certified to perform CVC insertion independently, trainee physicians were required to complete the simulation training and successfully place a minimum of 5 CVCs directly supervised by an already‐certified physician. This was consistent with the Accreditation Council for Graduate Medical Education suggested minimum requirement in 2007. In our critical care units, all CVC insertions must be supervised by an ICU fellow or attending.
To reinforce the on‐the‐ground work by our physician leaders, we created 2 education tools to embed best practices into our CVC insertion workflow. A checklist with best practices for CVC insertion that was distributed throughout the hospital via central line kits and educational flyers, and a CVC insertion procedure note template consistent with California Department of Public Health documentation requirements was made available in our EMR.
In June 2007, we integrated CVC insertion simulation training into procedure workshops required for all medicine, surgery, anesthesia, and emergency medicine trainees during their intern year. These workshops promoted ultrasound‐guided IJ catheterization and supporting evidence for the new IJ site preference. Training sessions were 2 to 3 hours, and included a demonstration of best‐practice CVC insertion, as well as training with simulation models supervised by an instructor using a standardized CVC checklist. These trainings used both the Blue Phantom human torso model (
Hospital administration provided funds to purchase ultrasound machines for patient units such as medicine, cardiology, ED, and ICU). A total of 4 Site‐Rite (Bard Access Systems, Inc., Salt Lake City, UT) ultrasounds were purchased in 2007. The hospital has continued to purchase ultrasound units yearly, and had 53 ultrasound units in 2014
Cases of IAP were continuously reviewed throughout the intervention period. Based on their higher CVC‐associated IAP rates, the ORs and catheterization lab were identified as having opportunities for improvement. In 2008, Hospital quality‐improvement leadership met with physician leaders in these areas to review their CVC‐related IAP data and to discuss strategies to reduce their IAP rates. These strategies included lessons learned from other services that had successfully decreased their IAP rates.
To sustain our gains, we continue to review all IAP through our coding quality, clinical documentation, quality reporting departments, and peer review. We have implemented other strategies to decrease IAP, such as the use of ultrasound guidance for bedside thoracentesis procedures, which became possible after the availability of more ultrasound devices. Training for ultrasound‐guided thoracentesis was done by our procedure‐team attending during supervision of residents.
Outcomes
Preintervention (January 1, 2006 to December 31, 2006)
There were a total of 26 cases of IAP in 2006. Of these, 15 (58%) were associated with CVC insertion (Figure 1). The single procedure associated with the largest proportion of IAP was SC CVC insertion (11 cases, 42% of all IAP cases). Eleven CVC‐associated IAPs were significant enough to require chest tube placement. Our hospital recorded a total of 1593 CVC insertions (ICD‐9 codes 38.93 and 38.97) in 2006.
Postintervention (January 1, 2008 to December 31, 2014)
There were a total of 80 cases of IAP over 7 years, of which 24 (30%) were associated with CVC insertion. Of these, 16 required chest tube placement. In the last 4 years of the postintervention period (20112014), there were only 5 cases of CVC‐associated IAP requiring chest tube placement (Figure 1). There were a total of 12,000 CVC insertions recorded over the same period.
We successfully met both our short‐ and long‐term goals. Our preintervention CVC‐associated IAP rate was 0.94%, and our post‐intervention rate during 2008 was 0.44%, a short‐term reduction of 53% (P=0.088). Our average postintervention CVC‐associated IAP rate for the years 2008 through 2014 was 0.13%, a significant long‐term reduction of 86% (P<0.0001) (Table 2). The decrease in CVC‐associated IAP rates occurred despite an older patient population (P<0.001) and a higher CMI (P<0.001) in postintervention patients who received a CVC (Table 1). Special cause variation corresponding to a change in our process is demonstrated in Figure 2. The preintervention average number of procedures between IAP was 114.8 and increased to 460.7 in the postintervention period.
| Total CVC (n=95) | Subclavian (n=29) | Internal Jugular (n=58) | Femoral (n=8) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||
| Compliance to intervention | |||||||||||||
| US guided | 68.1% | 20.7% | 86.2% | 100.0% | |||||||||
| Procedure note completion | 90.4% | 93.1% | 86.2% | 100.0% | |||||||||
| Supervision | 70.2% | 77.8% | 73.1% | 87.5% | |||||||||
| Level of training | |||||||||||||
| Resident | 61.1% | 58.6% | 60.3% | 75.0% | |||||||||
| Fellow | 25.3% | 27.6% | 24.1% | 25.0% | |||||||||
| Attending | 4.2% | 6.9% | 3.4% | 0.0% | |||||||||
| Advance practitioner | 3.2% | 3.4% | 3.4% | 0.0% | |||||||||
| Unknown | 6.3% | 3.4% | 8.6% | 0.0% | |||||||||
| Supervisor type | |||||||||||||
| Resident | 3.0% | 4.8% | 2.6% | 0.0% | |||||||||
| Fellow | 54.5% | 33.3% | 57.9% | 100.0% | |||||||||
| Attending | 42.4% | 61.9% | 39.5% | 0.0% | |||||||||
| Location of CVC Placement | Internal Jugular (n=25) | Subclavian (n=25) | |||||||||||
| MICU | 32.0% | 32.0% | |||||||||||
| SICU* | 40.0% | 52.0% | |||||||||||
| Operating room | 28.0% | 16.0% | |||||||||||
| Average no. of attempts/procedure | 1.4 | 1.5 | |||||||||||
| Indications for subclavian insertion (n=25) | |||||||||||||
| Trauma/surgical site | 60.0% | ||||||||||||
| Need for additional access | 16.0% | ||||||||||||
| Unsuccessful IJ placement | 4.0% | ||||||||||||
| Unclear | 20.0% | ||||||||||||
| Iatrogenic Pneumothorax Rate (20062014) | Year | ||||||||||||
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||
| % of CVC insertions associated with IAP | 0.94 | 1.49 | 0.44 | 0.13 | 0.20 | 0.07 | 0.04 | 0.11 | 0.07 | ||||
| All‐cause IAP per 1,000 discharges | 1.32 | 1.29 | 0.98 | 0.71 | 0.83 | 0.49 | 0.13 | 0.35 | 0.23 | ||||
| Preintervention | Postintervention | P Value | |||||||||||
| CVC‐ associated IAP short term (2006 vs 2008) | 0.94% | 0.44% | 0.088 | ||||||||||
| CVC‐associated IAP long term (2006 vs 20082014) | 0.94% | 0.13% | <0.0001 | ||||||||||
| All‐cause IAP per 1,000 discharges short term (2006 vs 2008) | 1.32 | 0.98 | <0.0001 | ||||||||||
| All‐cause IAP per 1,000 discharges long term (2006 vs 2008‐14) | 1.32 | 0.52 | <0.0001 | ||||||||||
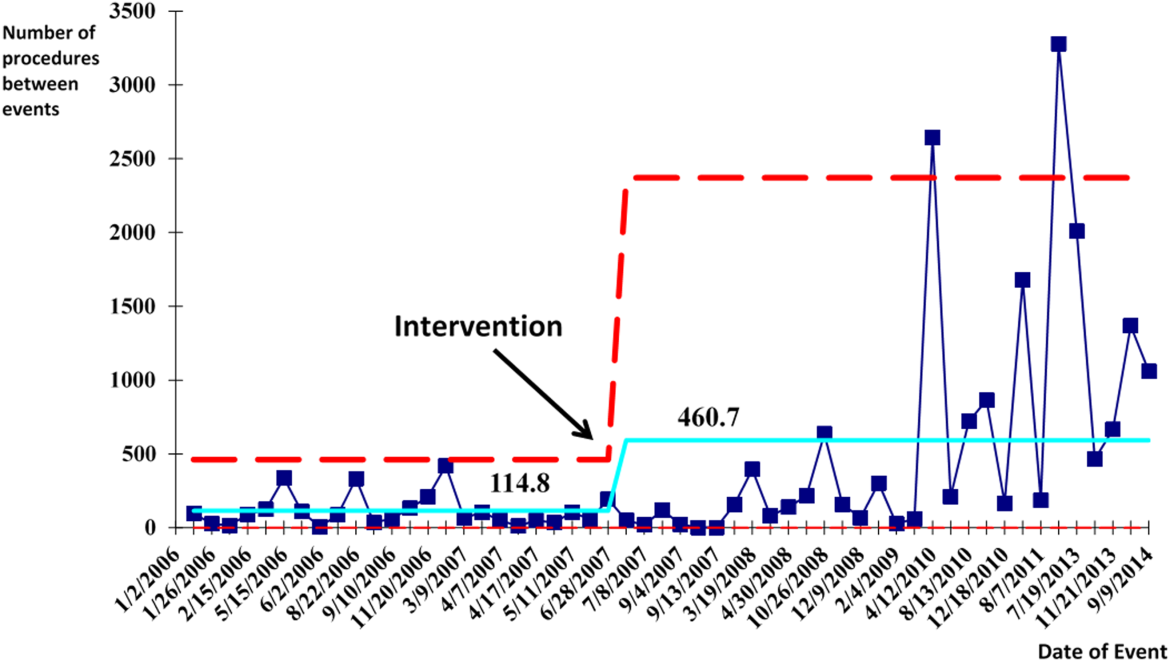
With the decrease in CVC‐associated IAP, we also saw a decrease in our all‐cause IAP rate per 1000 discharges from 1.32 in 2006 to 0.98 in 2008. This represents a 26% short‐term reduction (P<0.0001). We also saw a decrease in our all‐cause IAP rate per 1000 discharges to 0.52 from 2008 to 2014, representing a 61% long‐term reduction (P<0.0001). This decrease in all‐cause IAP postintervention occurred despite an older patient population (P<0.01) for all discharges. Our hospital is now in the highest performance UHC quartile for all‐cause IAP in 2012 to 2014.
After our multifaceted intervention in 2007, there was substantially more and consistent documentation of CVC procedure notes from less than 500 in 2006 to greater than 2000 in 2009. The distribution of CVC procedure notes in the pre‐ (2006) versus postintervention (20082014) period showed a decrease in the proportion of femoral lines from 15% to 11%, increase in IJ lines from 31% to 49%, and a decrease in SC from 54% to 40% (P=0.001). The distribution of IJ CVC procedure notes in the pre‐ (2006) versus postintervention (20082014) period showed an increase in the proportion of procedures with ultrasound documentation from 13% to 93% (P<0.001) (Figure 3).
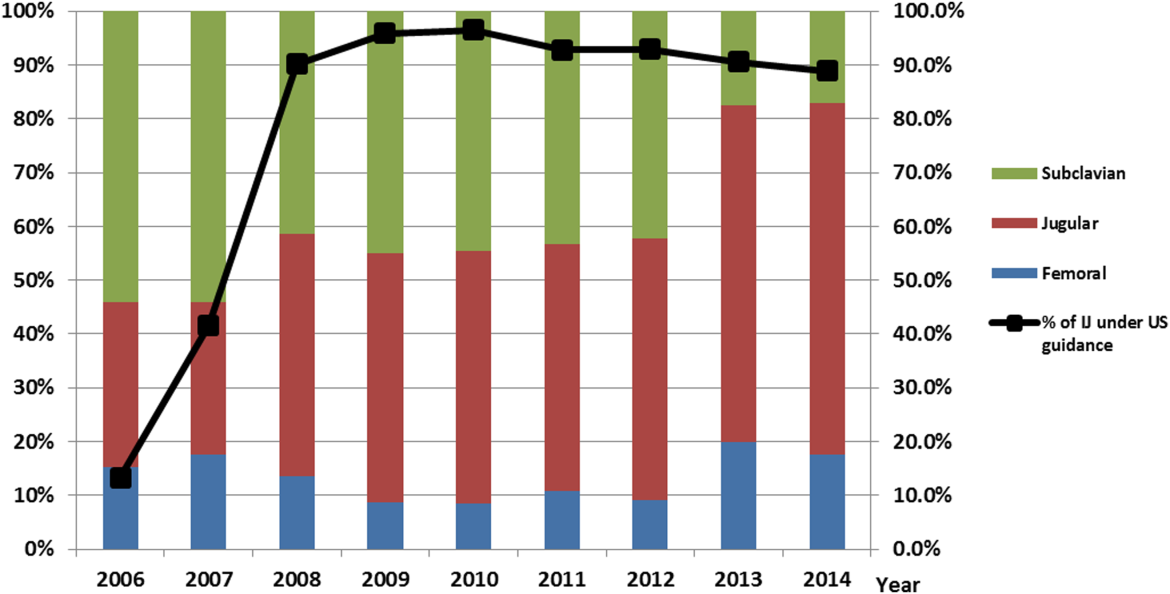
In our ICU 2014 audit, the majority of CVC lines were placed by residents under supervision (>70%), and most used the standard CVC note template to document the procedure (90%). Of the total CVC approach, 66% were IJ and 4% were SC. Eighty‐six percent used ultrasound during IJ placement. The majority of SC insertions were placed in the surgical ICU and had clear indications (80%) for placement. Of those, 75% were due to trauma (limited access to neck) or surgery (interfering with surgical site) (Table 2).
DISCUSSION
Summary
This quality‐improvement intervention demonstrates that a multidisciplinary team can successfully implement a multifaceted intervention that sustainably reduces the rate of IAP complications from CVC placement and improves patient safety over 7 years. We found high compliance with our intervention, which included an increase in CVC notes and documentation of ultrasound guidance. There was also an increase in the IJ approach in our postintervention period. We showed statistically significant long‐term reductions in both CVC‐associated and all‐cause IAP rates. From 2011 to 2014, there were only 5 cases of CVC‐associated IAP requiring chest tube placement. Post hoc analysis showed a statistically significant decrease in CLABSI rates (P<0.0001) from a preintervention rate of 1.6 infections per 1000 central line days to postintervention average rate of 0.68 infections per 1000 central line days. This decrease may be related to the incorporation of wide sterile barrier techniques in our CVC training workshops, checklists, and template procedure notes.
A strength of this study is the sustained significant long‐term reduction in IAP. There are few data that exist to describe sustained interventions in this area. Sustainability was achieved by integrating our interventions into ongoing programs that already existed in the hospital; we incorporated our simulation training into the existing new resident orientation, increased the availability of existing ultrasound equipment, and continued our IAP chart review through coding quality with feedback to involved services. The procedure note template continues to be easily available in our EMR, and the SC approach to CVC placement is limited to select cases.
Based on a post hoc cost‐benefit analysis, the financial benefits of decreasing the rate of IAP outweigh the costs associated with implementation of this initiative. The purchase cost for a Site‐Rite (Bard Access Systems) ultrasound machine was $18,000. The cost of materials for 1 workshop is $5000 annually. Cases from the Nationwide Inpatient Sample that were flagged by this PSI had 7.0% excess mortality, 4.4 days of excess hospitalization, and approximately $18,000 in excess hospital charges.[17, 18] Based on these data, if we had continued at our preintervention rate of CVC‐associated IAP requiring chest tube placement, we would estimate 9 additional CVC‐associated IAPs requiring chest tube insertion per year. This would result in over $180,000 of additional costs annually. Based on an initial cost of $100,000 for 4 workshops and the necessary equipment, we would have realized our cost savings in less than 1 year postintervention. These are all approximate costs, and further detailed analysis is needed.
One challenge with this intervention is the culture change away from using the SC approach, and the concern from trainees of how they would learn to perform SC CVC if needed. We would suggest dedicated SC CVC ultrasound training for those services who may need to use this approach (eg, neuroanesthesia and trauma).
Interpretation/Relation to Other Evidence
The field of implementation science can help explain why some projects are successful and others fail. We can further dissect the success of this project using an implementation science model similar to that described by French et al.[19] French et al. describe 4 behavior‐change techniques. These steps include (1) who needs to do what differently, (2) which barriers and enablers need to be addressed, (3) which intervention component could overcome the barriers and enhance enablers, and (4) how can behavior change be measured and understood. Barriers included suboptimal skills of residents, low awareness of evidence‐based guidelines, and entrenched practices inconsistent with best evidence. There was also a belief that IJ lines were more likely to become infected. Targeted behaviors needing to be done differently were the choice of CVC placement site and insertion technique. Barriers to change were assessed by asking members of the project team to explore with members of their service what led them to do CVC lines without ultrasound guidance. Enhancements focused on information provision, simulation practice, and persuasive communication. Behavior change was measured by tracking the number of IAPs, site of CVC, and documentation of technique. Continuation of these interventions based on this theoretical framework drove maintenance of gains.
We completed our main intervention planning in 90 days, and met our short‐term goal on schedule. The Institute for Healthcare Improvement (IHI) advocates that such short timelines are efficient mechanisms for developing and acting on projects. Other institutions have reported on similar rapid‐cycle planning and short‐term goal setting[20]
Limitations
Our study captures the experience of a quality‐improvement team at a single academic center, and our results may not be generalizable to other institutions. Our chart review process only occurred once a case had been identified through AHRQ PSI methodology. It is possible that the PSI does not capture all cases of IAP, although we believe our coding department has a very rigorous process to look for all IAP evidence in the patient's record. We used administrative data to determine the number of hospital‐wide CVC procedures.
Our compliance data with interventions from STRIDE are based on looking for key words in procedure note documentation (so undocumented notes are not captured). To validate this, we performed a manual audit of our adherence to our intervention in 2014, and those data are consistent with the results from our STRIDE data.
Our study's observational design also cannot control for exogenous effects on physician practice relating to CVC insertion or the overall risk of IAP. Some of our decrease in complications may be from the increase in PICC line use. Nevertheless, our CVC‐associated IAP rate has decreased despite >6000 non‐PICC CVCs in our ICU over the past 5 years, and a rising CMI (18% increase in postintervention period) and older population of patients with CVC insertion (P<0.0001)
CONCLUSIONS
We are the first, to our knowledge, to report a measurable improvement in reducing IAP patient outcomes that has been sustained for over 7 years. Our hospital is in the highest performance UHC quartile for all‐cause IAP in 2012 to 2014. A multidisciplinary quality‐improvement team, focused on evidence, patient safety, and standardization, can use a multifaceted intervention to sustainably improve patient outcomes. Promoting ultrasound‐guided IJ catheterization as the CVC insertion method of choice significantly reduced our hospital's rate of CVC‐associated IAP.
Acknowledgements
The authors acknowledge many who have contributed to this quality‐improvement project:
Irina Tokareva, Jay Lee, Kourt Bowes, and Gomathi Krishnan for data analysis; Laura Meinke for significant website curriculum; Fred Mihm, Sarah Williams, and John Kugler for leadership in ultrasound training; Kevin Tabb and Norm Rizk for hospital financial support of simulation workshops and ultrasound machines; Pooja Loftus and Helene Grossman for statistical analysis; Eric Hadhazy for data support; Joan Hendershott for cost information; Nancy Szaflarski for project management and manuscript review; and Isabella Chu for manuscript review.
Disclosures: STRIDE (Stanford Translational Research Integrated Database Environment) is a research and development project at Stanford University to create a standards‐based informatics platform supporting clinical and translational research. This STRIDE project was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors report no conflicts of interest.
- , , . Significance of iatrogenic pneumothoraces. Chest. 1994;105(4):1147–1150.
- , , , , , . How to avoid and manage a pneumothorax. J Vasc Access. 2006;7(1):7–14.
- , , , . Iatrogenic pneumothorax: etiology, incidence and risk factors. Thorac Cardiovasc Surg. 2009;57(5):286–290.
- , , , et al. Real‐time ultrasound‐guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):R162.
- , , . Safe placement of central venous catheters: a measured approach. J Intens Care Med. 2011;26(6):392–396.
- , , , . Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero‐risk environment. Chest. 2009;135(5):1315–1320.
- , , , , , . Use of simulation‐based education to improve outcomes of central venous catheterization: a systematic review and meta‐analysis. Acad Med. 2011;86(9):1137–1147.
- , , , , , . A prerotational, simulation‐based workshop improves the safety of central venous catheter insertion: results of a successful internal medicine house staff training program. Chest. 2011;140(3):652–658.
- , , , , . Linking residency training effectiveness to clinical outcomes: a quality improvement approach. Jt Comm J Qual Patient Saf. 2010;36(5):203–208.
- , , , et al. Education of physicians‐in‐training can decrease the risk for vascular catheter infection. Ann Intern Med. 2000;132(8):641–648.
- , , , et al. A multidisciplinary approach to reduce central line‐associated bloodstream infections. Jt Comm J Qual Patient Saf. 2013;39(2):61–69.
- , , , et al. Validity of selected Patient Safety Indicators: opportunities and concerns. J Am Coll Surg. 2011;212(6):924–934.
- , , , et al. Cases of iatrogenic pneumothorax can be identified from ICD‐9‐CM coded data. Am J Med Qual. 2010;25(3):218–224.
- , , , , ; SQUIRE development group. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ. 2009;338:a3152.
- . The Quality Toolbox. 2nd ed. Milwaukee, WI: ASQ Quality Press; 2005.
- , , , . STRIDE—an integrated standards‐based translational research informatics platform. AMIA Annu Symp Proc. 2009;2009:391–395.
- , , . Accidental iatrogenic pneumothorax in hospitalized patients. Med Care. 2006;44(2):182–186.
- , . Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290(14):1868–1874.
- , , , et al. Developing theory‐informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38.
- , . Using rapid‐cycle quality improvement methodology to reduce feeding tubes in patients with advanced dementia: before and after study. BMJ. 2004;329(7464):491–494.
- , , . Significance of iatrogenic pneumothoraces. Chest. 1994;105(4):1147–1150.
- , , , , , . How to avoid and manage a pneumothorax. J Vasc Access. 2006;7(1):7–14.
- , , , . Iatrogenic pneumothorax: etiology, incidence and risk factors. Thorac Cardiovasc Surg. 2009;57(5):286–290.
- , , , et al. Real‐time ultrasound‐guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):R162.
- , , . Safe placement of central venous catheters: a measured approach. J Intens Care Med. 2011;26(6):392–396.
- , , , . Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero‐risk environment. Chest. 2009;135(5):1315–1320.
- , , , , , . Use of simulation‐based education to improve outcomes of central venous catheterization: a systematic review and meta‐analysis. Acad Med. 2011;86(9):1137–1147.
- , , , , , . A prerotational, simulation‐based workshop improves the safety of central venous catheter insertion: results of a successful internal medicine house staff training program. Chest. 2011;140(3):652–658.
- , , , , . Linking residency training effectiveness to clinical outcomes: a quality improvement approach. Jt Comm J Qual Patient Saf. 2010;36(5):203–208.
- , , , et al. Education of physicians‐in‐training can decrease the risk for vascular catheter infection. Ann Intern Med. 2000;132(8):641–648.
- , , , et al. A multidisciplinary approach to reduce central line‐associated bloodstream infections. Jt Comm J Qual Patient Saf. 2013;39(2):61–69.
- , , , et al. Validity of selected Patient Safety Indicators: opportunities and concerns. J Am Coll Surg. 2011;212(6):924–934.
- , , , et al. Cases of iatrogenic pneumothorax can be identified from ICD‐9‐CM coded data. Am J Med Qual. 2010;25(3):218–224.
- , , , , ; SQUIRE development group. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ. 2009;338:a3152.
- . The Quality Toolbox. 2nd ed. Milwaukee, WI: ASQ Quality Press; 2005.
- , , , . STRIDE—an integrated standards‐based translational research informatics platform. AMIA Annu Symp Proc. 2009;2009:391–395.
- , , . Accidental iatrogenic pneumothorax in hospitalized patients. Med Care. 2006;44(2):182–186.
- , . Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA. 2003;290(14):1868–1874.
- , , , et al. Developing theory‐informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci. 2012;7:38.
- , . Using rapid‐cycle quality improvement methodology to reduce feeding tubes in patients with advanced dementia: before and after study. BMJ. 2004;329(7464):491–494.
© 2015 Society of Hospital Medicine
Why Transfusion BPAs Are Overridden
Transfusion of blood products has multiple clinical applications, yet when used outside of recommended guidelines it is associated with increased cost, waste, morbidity, and mortality.[1] Studies reviewing restrictive versus liberal blood transfusion strategies have demonstrated no benefit to liberal strategies over restrictive strategies[2, 3, 4, 5, 6, 7, 8, 9, 10] and possibly even harm.[11] Given the risks and real costs of blood transfusions occurring outside of recommended guidelines, professional societies in hematology, anesthesiology, and hospital medicine each include excessive blood transfusions among their top 5 questionable clinical practices in the American Board of Internal Medicine Foundation's Choosing Wisely initiative.[12] To modify behaviors around blood transfusion practices, hospitals and blood banks may need to provide clinical decision support (CDS) for physicians.
The conventional approach to CDS is direct education and training campaigns, but there is a unique opportunity for intelligent decision support at the point of care through electronic medical record (EMR) systems directly integrated with computerized physician order entry (CPOE).[13, 14, 15] Prior work at Stanford toward reducing unnecessary blood transfusions started with hospital‐wide education campaigns, which brought down the percentage of transfusions ordered for patients with hemoglobin (Hgb) >8 g/dL from 57% to 52%. Further reduction to <30% was achieved after the introduction of an interruptive best practice alert (BPA) integrated into the CPOE transfusion ordering process.[16, 17] Specifically, providers attempting to order a blood transfusion for patients with an EMR‐determined Hgb >7 are presented with a BPA popup reminding them of best practice guidelines and a prompt to either abort the transfusion or provide a reason to override the BPA and proceed.
It remains uncertain why up to 30% of transfusions continue to occur outside of recommended guidelines in spite of interruptive prompts. This study demonstrates a general approach to secondary use of clinical data from the EMR toward understanding provider behavior, specifically by analyzing free‐text comments linked to transfusion override behavior and identifying the type of providers interacting with the BPAs.
MATERIALS AND METHODS
At Stanford University Hospital, a 447‐bed academic tertiary care center servicing adult patients, clinicians order blood transfusions through an EMR+CPOE system. When an order for red blood cell transfusion is attempted, the EMR evaluates the patient chart for specific criteria based on previously published guidelines.[18] Specifically, the BPA will review the last recorded Hgb value and trigger if the Hgb is >8, or if the Hgb is >7 and there is no concurrent EMR problem‐list entry related to acute coronary syndrome or acute hemorrhage. Once the blood transfusion BPA triggers, the ordering provider is presented with an interruptive prompt reminding them of best practice guidelines and the 3 most recent Hgb values for the patient.[16] From there, the provider may either abort the transfusion or override the BPA and proceed. Overrides require the provider to select a reason from a predefined list of institutionally accepted transfusion indications including acute bleeding, acute coronary syndrome and Hgb <8, and postoperative cardiothoracic surgery and Hgb <8. If none of the predefined override reasons are selected, the provider simply selects other, with the option of a free‐text comment to elaborate their rationale.
Data from provider interactions with the BPA were collected from the EMR across all inpatient wards for 8 months after the implementation period. Data collected from each interaction included the patient identifier, alert description, action taken, ordering provider identifier, ordering provider type (job title), optional comments for overriding the BPA, and date and time.
The free‐text override comments were independently reviewed by 2 licensed physicians, tagging them into a set of general categories by iterative inductive analysis of the comment content. Individual comments were allowed multiple possible category tags (eg, coronary artery disease and symptomatic). The initial tagging process was expedited by isolating common keywords in the override comments and assigning likely category tags to each, as in Table 2. The 2 physician reviewers then manually inspected all comments with the option to revise the initial category tagging to ensure validity. Many category tags occurred sporadically and were aggregated into more general categories, such as hematologic disorder (includes myelodysplastic syndrome, myelofibrosis, multiple myeloma, sickle cell, thalassemia, Waldenstrom's), symptomatic (includes fatigue, lightheaded, short of breath), and per other medical doctor [MD] (includes any other physician direction, primarily specialty consultation services).
To assess the inter‐rater agreement of this category tagging between the 2 reviewers, a confusion matrix similar to the example in Table 1 was setup for each tag used. Several agreement statistics are calculated based on the confusion matrix, including the positive agreement rate (Pa+) and Cohen's kappa statistic (). Kappa statistic values range from 1 to +1, with values <0 indicating no agreement and values >0.8 indicating near perfect agreement.[19] To reject the null hypothesis that the 2 reviewers could have independently arrived at their similar tagging assignments by chance, a 2 test was applied for each confusion matrix, with Yates' correction to avoid overestimating statistical significance given the low rates of inter‐rater disagreement.[20]
| Reviewer 1 Tags "Surgery" | ||||
|---|---|---|---|---|
| Yes | No | Total | ||
| ||||
| Reviewer 2 Tags "Surgery" | Yes | 143 | 11 | 154 |
| No | 5 | 820 | 825 | |
| Total | 148 | 831 | 979 | |
| Category Tag | Keyword | Keyword Count |
|---|---|---|
| ||
| Hgb 78 | 7.1, 7.2, 7.8, 7.9, 8, <8 | 360 |
| BMT | BMT | 359 |
| Symptomatic | Symptomatic | 187 |
| Surgery | Postop, post‐op, surgery, surgical | 176 |
| Dropping Hgb | Down, drop, dropping | 117 |
| Chemotherapy | Chemo, chemotherapy | 88 |
| Per other MD | Per | 87 |
| Transplant | Transplant | 70 |
| Cardiac | Cardiac | 66 |
| Bleeding | Bleeding | 65 |
| Procedure | Procedure | 65 |
| Hgb <7 | 7 | 58 |
| Hypotension | Hypotension | 51 |
| Protocol | Protocol | 51 |
| Cirrhosis | Liver | 50 |
| Imminent discharge | Discharge | 49 |
| Leukemia, acute | AML | 44 |
| Cancer | Cancer | 37 |
| Sepsis | Sepsis | 32 |
| Tachycardia | Tachycardia | 28 |
RESULTS
During the data collection period from January 1, 2011 to August 31, 2012, the blood transfusion BPA fired in 11,791 instances, of which 10,642 recorded sufficient data for analysis (Figure 1). The ordering provider proceeded to override the BPA and continued with transfusion in 98% of cases (10,442/10,642). Acute bleeding" was the most common structured response (34%). The majority of BPA overrides used the general purpose other structured response option accounting for 56% (5886/10,442) of override responses, of which 37% (2185/5886) entered a free‐text comment elaborating the override reason. With 3701 nonresponders (other overrides with no free‐text comment), the overall response rate was 65% (6941/10,642).
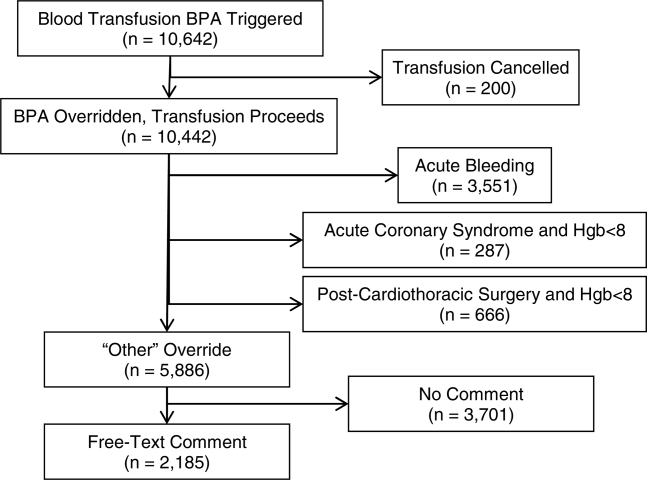
With a handful of free‐text comments included with structured override responses (eg, 28 acute bleeding overrides included additional comment from the provider), a total of 2216 override comments were available for analysis. Using an initial selection of keyword‐tag associations, as in Table 2, 95% (2104/2216) of the override comments had a preliminary category tagging assigned. After manual review and revision by the first physician reviewer, 74% (1633/2216) of the comments retained their automated tags, whereas 26% (583/2216) were updated based on the reviewer's assessment of validity. This included 112 comments lacking automated tags the reviewer manually added, as well as 471 comments with automated tags revised by the reviewer.
The most common override category tags are presented in Figure 2 and Figure 3 for BPAs triggered in response to blood transfusions ordered for patients with Hgb 78 and Hgb >8, respectively. The agreed+ percentages correspond to the number of comments where the 2 physician reviewers both assigned the respective category tag (Pa+), whereas the disagreed percentages correspond to comments where the reviewers differed (Pd=1‐Pa). By Yates' corrected 2 analysis, P was <1010 for independence between reviewer tag assignments for all tags assessed. Kappa statistics are reported in the figures to describe inter‐rater agreement.
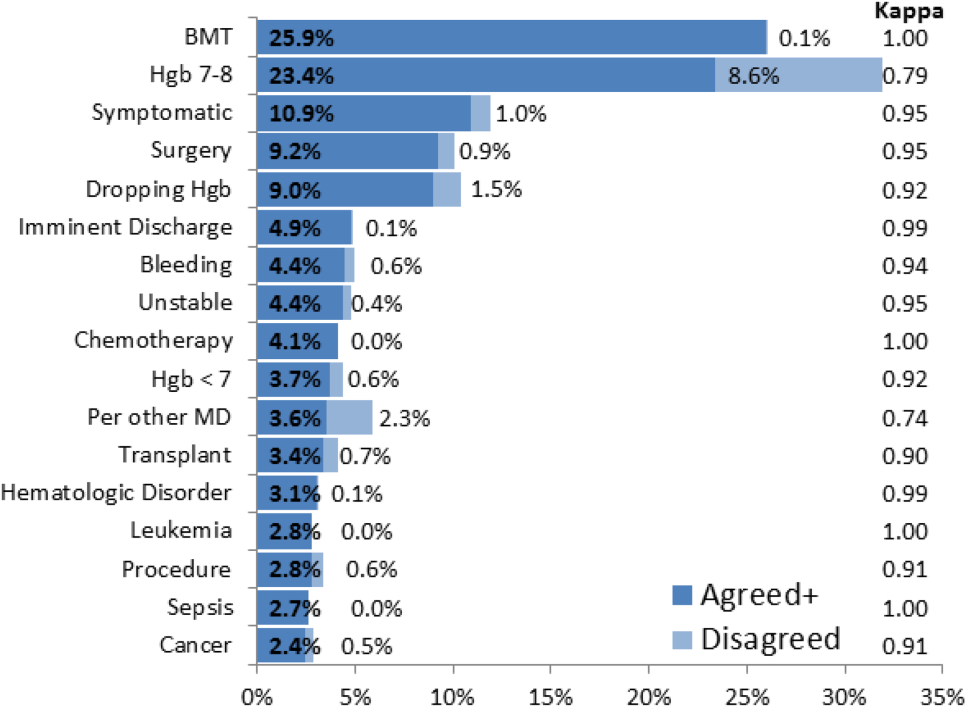
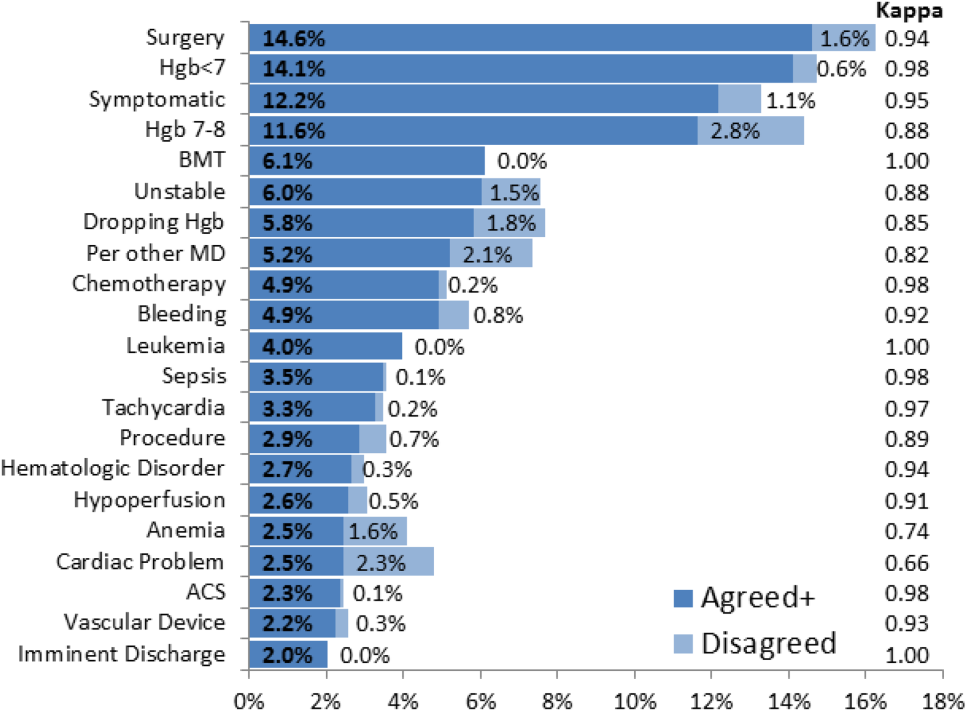
Resident physicians were the primary ordering provider group, accounting for approximately 55% (5863/10,642) of BPA interactions, followed by registered nurses, fellows, and attending physicians.
DISCUSSION
Prior work has established that an interruptive BPA to provide decision support against inappropriate blood transfusions can drive a significant and sustained reduction in unnecessary transfusions,[16] especially when satisfying the primary features of effective decision support.[14] The quantity of transfusions directly aborted by the BPA (only 2% in this case) does not nearly account for the total observed reductions in transfusions, suggesting that the BPA yields an indirect teaching effect over time beyond direct interruption. In other words, once a user has been interrupted by the BPA several times, they will be discouraged from even attempting to order inappropriate blood transfusions in the future.
Despite the improvements above, there remains a substantial fraction (up to 30%) of blood transfusions occurring outside of recommended guidelines where providers specifically override the BPA prompt.[21] This work is the first structured analysis of such BPA override behavior by generalizable methods of EMR data analysis to guide further improvements.
Analysis of the override behavior focused primarily on the free‐text comments explaining provider rationales for overriding the BPA. These comments were categorized by 2 physician reviewers, with P<1010 for all category tags, rejecting the null hypothesis that the 2 reviewers could have independently arrived at their similar category tags by chance. Further assessment of inter‐rater agreement was generally excellent, with >0.8 in the majority of cases. The remaining cases (ie, Hgb 78, per other MD, anemia, cardiac) still had substantial agreement, with >0.6. These disagreements almost universally occurred when a reviewer assigned a subset of the category tags assigned by the other reviewer. For example, 1 reviewer may tag a comment bone marrow transplant (BMT) patient with Hgb 7.2 with BMT and Hgb 78, whereas the other would only cite BMT.
Figure 2 and Figure 3 highlight the varied categories of responses, with most categories comprising <4% of the available responses. Among the most common override reasons are structured protocols for specialty services, as in the stem cell transplant service, whose protocol recommends transfusing blood when Hgb <8 rather than Hgb <7. In these cases, the BPA is unlikely to change protocolized behavior, thus overall workflow would likely be improved by adding a structured BPA override option for these protocols.
Analysis of the override comments did expose some relatively common and questionable transfusion practices, including perioperative and periprocedural transfusions, as well as anticipation of imminent discharge. Prior studies indicate that transfusions in anticipation of surgical or procedural intervention provide no benefit compared to responding to blood requirements intraoperatively as needed,[3, 22, 23] and imminent discharge of a patient is not a well‐recognized reason to transfuse outside of guidelines. The identification of these questionable and relatively common practices identifies opportunities for targeted education and training campaigns.
Symptomatic anemia was 1 of the more commonly cited BPA override reasons with a fraction providing a specific symptom such as fatigue, lightheadedness, or shortness of breath. Although the pervasiveness of this rationale may speak to adding it as a structured BPA override option, the nonspecific, subjective, and nonevidence‐based nature of symptom‐driven blood transfusions suggests that ongoing interruptive BPA prompts can still be useful to remind providers of the risks and guideline‐based approaches to such cases.
Limitations of the analysis are revealed as a fraction of BPA events did not fully record all relevant data, preventing proper analysis. Override comments suggest the BPA was triggering inappropriately for patients appropriately below the recommended transfusion threshold of Hgb <7, assuming provider free‐textentered values were accurate. Review of these cases showed some variability, such as when providers based their transfusion decision on a hematocrit of 20 rather than a Hgb of 7. Many comments also stated nonthreshold Hgb values, such as Hgb 7.2, seeming to imply that the value was close enough to the recommended threshold to justify overriding the transfusion prompt.
The most significant limitation of this study is the substantial fraction of nonresponder BPA transfusion overrides with a nonspecific other reason and no text commentary, comprising 34% (3670/10,642) of all BPA interactions and 62% (3670/5886) of all other overrides. Although the BPA is easily overridden by design to avoid workflow disruption that could compromise the priority of patient care, the nonresponses raise concern for skewed interpretation of the override data. General studies in survey responses provide reassurance that lower response rates do not necessarily indicate response bias,[24] with response rates as low as 25% yielding results statistically indistinguishable from more rigorous methods achieving >50% response rates.[25] In this specific case, response bias is better characterized by comparing ordering provider characteristics for the other overrides with and without free‐text comments. Specifically, Figure 4 shows the distribution of other overrides by provider type (job title) and provider home department (where available from physician department registries), separated by whether a free‐text comment was left. For each sub‐group, a 2 analysis compared the observed versus expected proportion of providers leaving comments based on the null hypothesis that leaving a comment was independent of membership in the subgroup. Similar proportions with nonsignificant P values suggest against significant response bias for most subgroups, but the data do indicate that this work likely under‐represents the opinion of fellows, physician assistants, and neurosurgeons, while slightly over‐representing the opinion of medicine, general surgery, and obstetrics/gynecology practitioners. Given that the under‐represented groups overall constitute a small minority of the total BPA interactions, this work should still be generalizable to the majority of transfusion behavior.
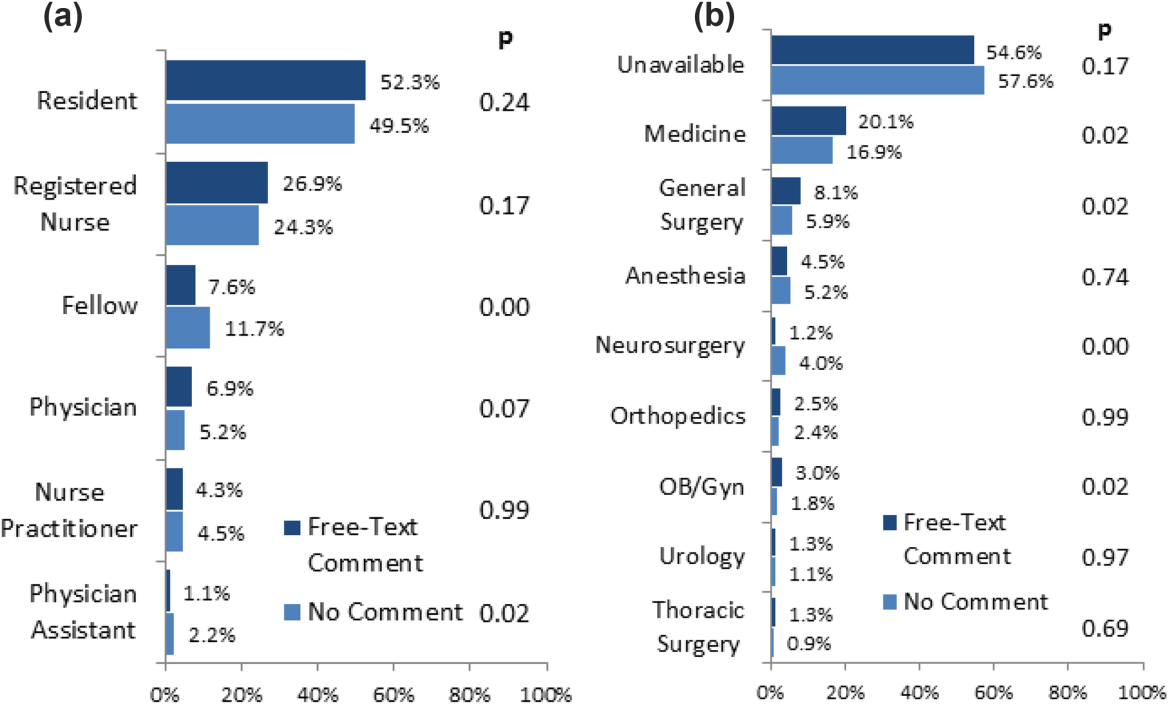
Further review of the ordering provider type (job title) distribution indicates that the vast majority of providers who actually interact with BPAs in this academic hospital are resident physicians. Similarly notable is that 25% of BPAs trigger for registered nurses. Upon review of hospital practices, we confirmed that nurses can enter transfusion orders on behalf of MD cosigners, generally in the context of a verbal order or routine treatment protocol, most notably on the stem cell transplant service. The prevalence of resident, nurse, nurse practitioner, and physician assistant order entry overall indicates that the providers encountering the BPA often do not have the negotiating power to accept or override the prompts, specifically defying the meaningful use goal of decision‐making providers directly interacting with CPOE and decision support prompts.[26]
The theoretical intelligence of the BPA not to trigger in well‐accepted cases of transfusion, where acute bleeding is occurring based on the presence of bleeding related items in the patient's problem list, is demonstrated to be limited. Acute bleeding represented the most common structured override response. This is likely multifactorial, but is largely the result of inconsistent usage of the patient problem lists that the BPA would depend upon. Another commonly cited override explanation was for a dropping Hgb without a specific bleeding source. This could point toward the BPA triggering an algorithm incorporating the last several Hgb values to assess the trajectory. Even then, however, guidelines would advocate holding transfusion and proceeding with serial monitoring of Hgb levels until an accepted transfusion threshold was actually breached.
This analysis demonstrates a general approach to secondary analysis of EMR data, in this case to provide insight into the specific question of why providers continue to order costly, unnecessary, and potentially harmful blood transfusions in spite of an interruptive BPA CDS tool. Limitations of the BPA are now better understood, including technical aspects of accounting for all decision‐making data, the frequency of nonresponse for override rationale, and that the providers interacting with the BPAs often do not have the negotiating power to change ordering behavior. The analysis recognizes protocolized behaviors that should be integrated into the CDS algorithms, and specification of symptomatic anemia as a common albeit subjective indication for blood transfusion. A wide swath of individually uncommon rationales drive transfusion override behavior, motivating further EMR‐based analysis to more efficiently recognize common scenarios (eg, perioperative/procedural, imminent discharge) for directed education and training interventions than can be achieved by conventional chart review.
Acknowledgements
The authors thank Sylvia Bereknyei for consultation on qualitative analysis methods, C.J. Garst for providing the dataset, David Iberri for contributing to early manuscript drafts, Paul Maggio for designing the original BPA, and Debra Green and Brett Toensing for providing staff department registries.
Disclosure: Nothing to report.
Transfusion of blood products has multiple clinical applications, yet when used outside of recommended guidelines it is associated with increased cost, waste, morbidity, and mortality.[1] Studies reviewing restrictive versus liberal blood transfusion strategies have demonstrated no benefit to liberal strategies over restrictive strategies[2, 3, 4, 5, 6, 7, 8, 9, 10] and possibly even harm.[11] Given the risks and real costs of blood transfusions occurring outside of recommended guidelines, professional societies in hematology, anesthesiology, and hospital medicine each include excessive blood transfusions among their top 5 questionable clinical practices in the American Board of Internal Medicine Foundation's Choosing Wisely initiative.[12] To modify behaviors around blood transfusion practices, hospitals and blood banks may need to provide clinical decision support (CDS) for physicians.
The conventional approach to CDS is direct education and training campaigns, but there is a unique opportunity for intelligent decision support at the point of care through electronic medical record (EMR) systems directly integrated with computerized physician order entry (CPOE).[13, 14, 15] Prior work at Stanford toward reducing unnecessary blood transfusions started with hospital‐wide education campaigns, which brought down the percentage of transfusions ordered for patients with hemoglobin (Hgb) >8 g/dL from 57% to 52%. Further reduction to <30% was achieved after the introduction of an interruptive best practice alert (BPA) integrated into the CPOE transfusion ordering process.[16, 17] Specifically, providers attempting to order a blood transfusion for patients with an EMR‐determined Hgb >7 are presented with a BPA popup reminding them of best practice guidelines and a prompt to either abort the transfusion or provide a reason to override the BPA and proceed.
It remains uncertain why up to 30% of transfusions continue to occur outside of recommended guidelines in spite of interruptive prompts. This study demonstrates a general approach to secondary use of clinical data from the EMR toward understanding provider behavior, specifically by analyzing free‐text comments linked to transfusion override behavior and identifying the type of providers interacting with the BPAs.
MATERIALS AND METHODS
At Stanford University Hospital, a 447‐bed academic tertiary care center servicing adult patients, clinicians order blood transfusions through an EMR+CPOE system. When an order for red blood cell transfusion is attempted, the EMR evaluates the patient chart for specific criteria based on previously published guidelines.[18] Specifically, the BPA will review the last recorded Hgb value and trigger if the Hgb is >8, or if the Hgb is >7 and there is no concurrent EMR problem‐list entry related to acute coronary syndrome or acute hemorrhage. Once the blood transfusion BPA triggers, the ordering provider is presented with an interruptive prompt reminding them of best practice guidelines and the 3 most recent Hgb values for the patient.[16] From there, the provider may either abort the transfusion or override the BPA and proceed. Overrides require the provider to select a reason from a predefined list of institutionally accepted transfusion indications including acute bleeding, acute coronary syndrome and Hgb <8, and postoperative cardiothoracic surgery and Hgb <8. If none of the predefined override reasons are selected, the provider simply selects other, with the option of a free‐text comment to elaborate their rationale.
Data from provider interactions with the BPA were collected from the EMR across all inpatient wards for 8 months after the implementation period. Data collected from each interaction included the patient identifier, alert description, action taken, ordering provider identifier, ordering provider type (job title), optional comments for overriding the BPA, and date and time.
The free‐text override comments were independently reviewed by 2 licensed physicians, tagging them into a set of general categories by iterative inductive analysis of the comment content. Individual comments were allowed multiple possible category tags (eg, coronary artery disease and symptomatic). The initial tagging process was expedited by isolating common keywords in the override comments and assigning likely category tags to each, as in Table 2. The 2 physician reviewers then manually inspected all comments with the option to revise the initial category tagging to ensure validity. Many category tags occurred sporadically and were aggregated into more general categories, such as hematologic disorder (includes myelodysplastic syndrome, myelofibrosis, multiple myeloma, sickle cell, thalassemia, Waldenstrom's), symptomatic (includes fatigue, lightheaded, short of breath), and per other medical doctor [MD] (includes any other physician direction, primarily specialty consultation services).
To assess the inter‐rater agreement of this category tagging between the 2 reviewers, a confusion matrix similar to the example in Table 1 was setup for each tag used. Several agreement statistics are calculated based on the confusion matrix, including the positive agreement rate (Pa+) and Cohen's kappa statistic (). Kappa statistic values range from 1 to +1, with values <0 indicating no agreement and values >0.8 indicating near perfect agreement.[19] To reject the null hypothesis that the 2 reviewers could have independently arrived at their similar tagging assignments by chance, a 2 test was applied for each confusion matrix, with Yates' correction to avoid overestimating statistical significance given the low rates of inter‐rater disagreement.[20]
| Reviewer 1 Tags "Surgery" | ||||
|---|---|---|---|---|
| Yes | No | Total | ||
| ||||
| Reviewer 2 Tags "Surgery" | Yes | 143 | 11 | 154 |
| No | 5 | 820 | 825 | |
| Total | 148 | 831 | 979 | |
| Category Tag | Keyword | Keyword Count |
|---|---|---|
| ||
| Hgb 78 | 7.1, 7.2, 7.8, 7.9, 8, <8 | 360 |
| BMT | BMT | 359 |
| Symptomatic | Symptomatic | 187 |
| Surgery | Postop, post‐op, surgery, surgical | 176 |
| Dropping Hgb | Down, drop, dropping | 117 |
| Chemotherapy | Chemo, chemotherapy | 88 |
| Per other MD | Per | 87 |
| Transplant | Transplant | 70 |
| Cardiac | Cardiac | 66 |
| Bleeding | Bleeding | 65 |
| Procedure | Procedure | 65 |
| Hgb <7 | 7 | 58 |
| Hypotension | Hypotension | 51 |
| Protocol | Protocol | 51 |
| Cirrhosis | Liver | 50 |
| Imminent discharge | Discharge | 49 |
| Leukemia, acute | AML | 44 |
| Cancer | Cancer | 37 |
| Sepsis | Sepsis | 32 |
| Tachycardia | Tachycardia | 28 |
RESULTS
During the data collection period from January 1, 2011 to August 31, 2012, the blood transfusion BPA fired in 11,791 instances, of which 10,642 recorded sufficient data for analysis (Figure 1). The ordering provider proceeded to override the BPA and continued with transfusion in 98% of cases (10,442/10,642). Acute bleeding" was the most common structured response (34%). The majority of BPA overrides used the general purpose other structured response option accounting for 56% (5886/10,442) of override responses, of which 37% (2185/5886) entered a free‐text comment elaborating the override reason. With 3701 nonresponders (other overrides with no free‐text comment), the overall response rate was 65% (6941/10,642).
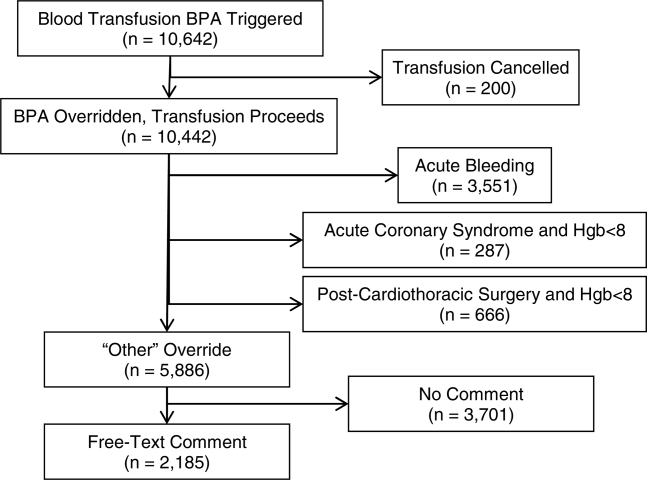
With a handful of free‐text comments included with structured override responses (eg, 28 acute bleeding overrides included additional comment from the provider), a total of 2216 override comments were available for analysis. Using an initial selection of keyword‐tag associations, as in Table 2, 95% (2104/2216) of the override comments had a preliminary category tagging assigned. After manual review and revision by the first physician reviewer, 74% (1633/2216) of the comments retained their automated tags, whereas 26% (583/2216) were updated based on the reviewer's assessment of validity. This included 112 comments lacking automated tags the reviewer manually added, as well as 471 comments with automated tags revised by the reviewer.
The most common override category tags are presented in Figure 2 and Figure 3 for BPAs triggered in response to blood transfusions ordered for patients with Hgb 78 and Hgb >8, respectively. The agreed+ percentages correspond to the number of comments where the 2 physician reviewers both assigned the respective category tag (Pa+), whereas the disagreed percentages correspond to comments where the reviewers differed (Pd=1‐Pa). By Yates' corrected 2 analysis, P was <1010 for independence between reviewer tag assignments for all tags assessed. Kappa statistics are reported in the figures to describe inter‐rater agreement.
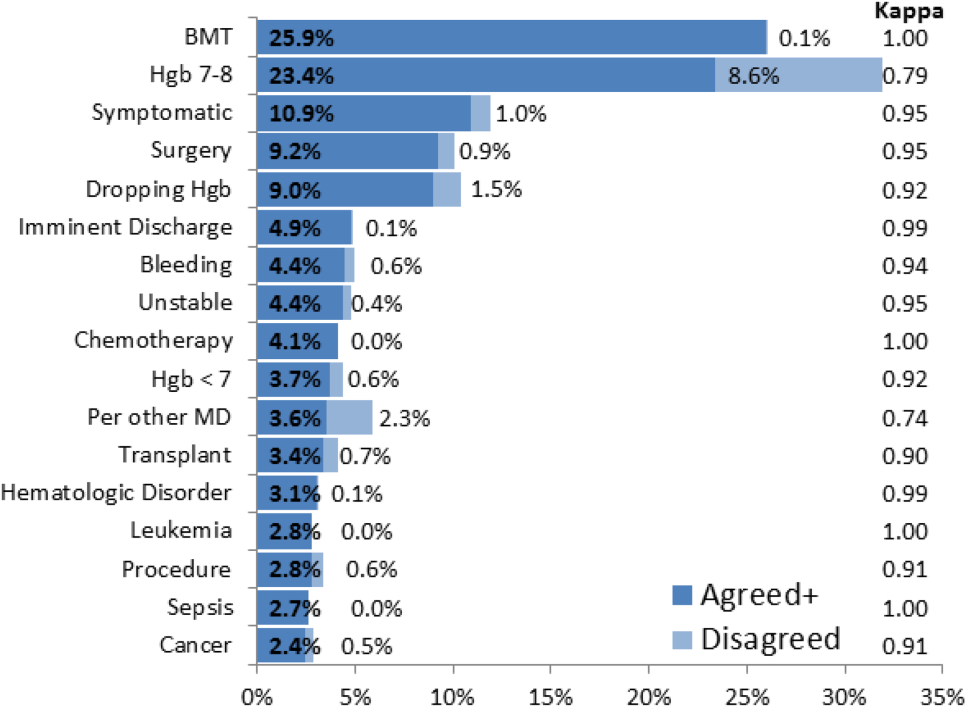
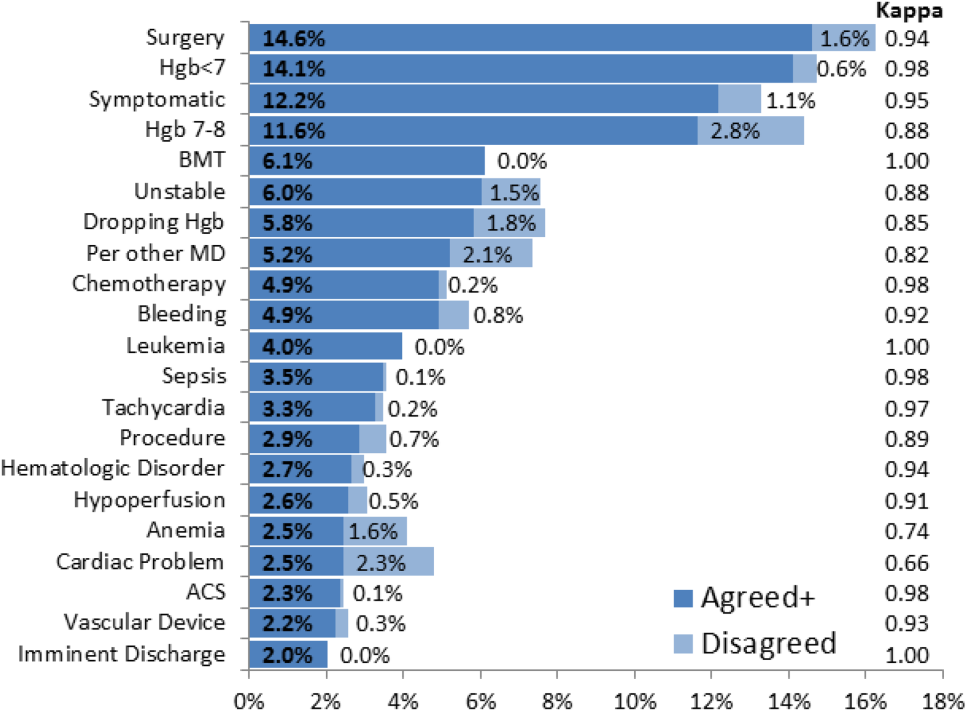
Resident physicians were the primary ordering provider group, accounting for approximately 55% (5863/10,642) of BPA interactions, followed by registered nurses, fellows, and attending physicians.
DISCUSSION
Prior work has established that an interruptive BPA to provide decision support against inappropriate blood transfusions can drive a significant and sustained reduction in unnecessary transfusions,[16] especially when satisfying the primary features of effective decision support.[14] The quantity of transfusions directly aborted by the BPA (only 2% in this case) does not nearly account for the total observed reductions in transfusions, suggesting that the BPA yields an indirect teaching effect over time beyond direct interruption. In other words, once a user has been interrupted by the BPA several times, they will be discouraged from even attempting to order inappropriate blood transfusions in the future.
Despite the improvements above, there remains a substantial fraction (up to 30%) of blood transfusions occurring outside of recommended guidelines where providers specifically override the BPA prompt.[21] This work is the first structured analysis of such BPA override behavior by generalizable methods of EMR data analysis to guide further improvements.
Analysis of the override behavior focused primarily on the free‐text comments explaining provider rationales for overriding the BPA. These comments were categorized by 2 physician reviewers, with P<1010 for all category tags, rejecting the null hypothesis that the 2 reviewers could have independently arrived at their similar category tags by chance. Further assessment of inter‐rater agreement was generally excellent, with >0.8 in the majority of cases. The remaining cases (ie, Hgb 78, per other MD, anemia, cardiac) still had substantial agreement, with >0.6. These disagreements almost universally occurred when a reviewer assigned a subset of the category tags assigned by the other reviewer. For example, 1 reviewer may tag a comment bone marrow transplant (BMT) patient with Hgb 7.2 with BMT and Hgb 78, whereas the other would only cite BMT.
Figure 2 and Figure 3 highlight the varied categories of responses, with most categories comprising <4% of the available responses. Among the most common override reasons are structured protocols for specialty services, as in the stem cell transplant service, whose protocol recommends transfusing blood when Hgb <8 rather than Hgb <7. In these cases, the BPA is unlikely to change protocolized behavior, thus overall workflow would likely be improved by adding a structured BPA override option for these protocols.
Analysis of the override comments did expose some relatively common and questionable transfusion practices, including perioperative and periprocedural transfusions, as well as anticipation of imminent discharge. Prior studies indicate that transfusions in anticipation of surgical or procedural intervention provide no benefit compared to responding to blood requirements intraoperatively as needed,[3, 22, 23] and imminent discharge of a patient is not a well‐recognized reason to transfuse outside of guidelines. The identification of these questionable and relatively common practices identifies opportunities for targeted education and training campaigns.
Symptomatic anemia was 1 of the more commonly cited BPA override reasons with a fraction providing a specific symptom such as fatigue, lightheadedness, or shortness of breath. Although the pervasiveness of this rationale may speak to adding it as a structured BPA override option, the nonspecific, subjective, and nonevidence‐based nature of symptom‐driven blood transfusions suggests that ongoing interruptive BPA prompts can still be useful to remind providers of the risks and guideline‐based approaches to such cases.
Limitations of the analysis are revealed as a fraction of BPA events did not fully record all relevant data, preventing proper analysis. Override comments suggest the BPA was triggering inappropriately for patients appropriately below the recommended transfusion threshold of Hgb <7, assuming provider free‐textentered values were accurate. Review of these cases showed some variability, such as when providers based their transfusion decision on a hematocrit of 20 rather than a Hgb of 7. Many comments also stated nonthreshold Hgb values, such as Hgb 7.2, seeming to imply that the value was close enough to the recommended threshold to justify overriding the transfusion prompt.
The most significant limitation of this study is the substantial fraction of nonresponder BPA transfusion overrides with a nonspecific other reason and no text commentary, comprising 34% (3670/10,642) of all BPA interactions and 62% (3670/5886) of all other overrides. Although the BPA is easily overridden by design to avoid workflow disruption that could compromise the priority of patient care, the nonresponses raise concern for skewed interpretation of the override data. General studies in survey responses provide reassurance that lower response rates do not necessarily indicate response bias,[24] with response rates as low as 25% yielding results statistically indistinguishable from more rigorous methods achieving >50% response rates.[25] In this specific case, response bias is better characterized by comparing ordering provider characteristics for the other overrides with and without free‐text comments. Specifically, Figure 4 shows the distribution of other overrides by provider type (job title) and provider home department (where available from physician department registries), separated by whether a free‐text comment was left. For each sub‐group, a 2 analysis compared the observed versus expected proportion of providers leaving comments based on the null hypothesis that leaving a comment was independent of membership in the subgroup. Similar proportions with nonsignificant P values suggest against significant response bias for most subgroups, but the data do indicate that this work likely under‐represents the opinion of fellows, physician assistants, and neurosurgeons, while slightly over‐representing the opinion of medicine, general surgery, and obstetrics/gynecology practitioners. Given that the under‐represented groups overall constitute a small minority of the total BPA interactions, this work should still be generalizable to the majority of transfusion behavior.
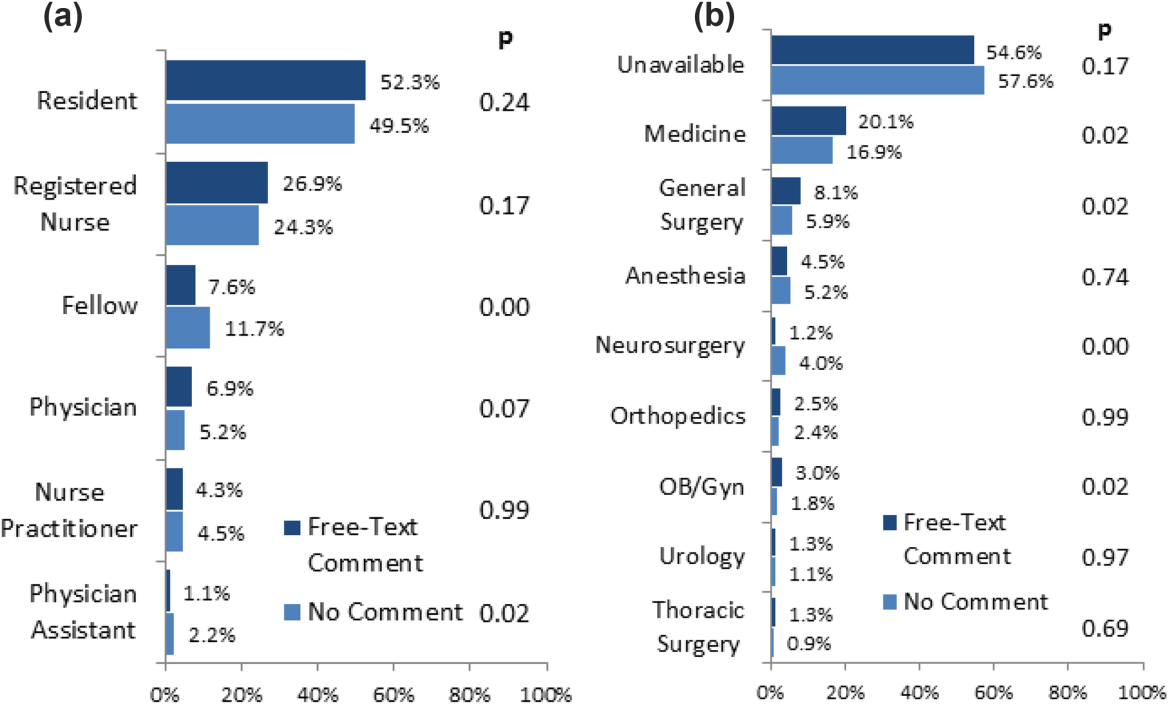
Further review of the ordering provider type (job title) distribution indicates that the vast majority of providers who actually interact with BPAs in this academic hospital are resident physicians. Similarly notable is that 25% of BPAs trigger for registered nurses. Upon review of hospital practices, we confirmed that nurses can enter transfusion orders on behalf of MD cosigners, generally in the context of a verbal order or routine treatment protocol, most notably on the stem cell transplant service. The prevalence of resident, nurse, nurse practitioner, and physician assistant order entry overall indicates that the providers encountering the BPA often do not have the negotiating power to accept or override the prompts, specifically defying the meaningful use goal of decision‐making providers directly interacting with CPOE and decision support prompts.[26]
The theoretical intelligence of the BPA not to trigger in well‐accepted cases of transfusion, where acute bleeding is occurring based on the presence of bleeding related items in the patient's problem list, is demonstrated to be limited. Acute bleeding represented the most common structured override response. This is likely multifactorial, but is largely the result of inconsistent usage of the patient problem lists that the BPA would depend upon. Another commonly cited override explanation was for a dropping Hgb without a specific bleeding source. This could point toward the BPA triggering an algorithm incorporating the last several Hgb values to assess the trajectory. Even then, however, guidelines would advocate holding transfusion and proceeding with serial monitoring of Hgb levels until an accepted transfusion threshold was actually breached.
This analysis demonstrates a general approach to secondary analysis of EMR data, in this case to provide insight into the specific question of why providers continue to order costly, unnecessary, and potentially harmful blood transfusions in spite of an interruptive BPA CDS tool. Limitations of the BPA are now better understood, including technical aspects of accounting for all decision‐making data, the frequency of nonresponse for override rationale, and that the providers interacting with the BPAs often do not have the negotiating power to change ordering behavior. The analysis recognizes protocolized behaviors that should be integrated into the CDS algorithms, and specification of symptomatic anemia as a common albeit subjective indication for blood transfusion. A wide swath of individually uncommon rationales drive transfusion override behavior, motivating further EMR‐based analysis to more efficiently recognize common scenarios (eg, perioperative/procedural, imminent discharge) for directed education and training interventions than can be achieved by conventional chart review.
Acknowledgements
The authors thank Sylvia Bereknyei for consultation on qualitative analysis methods, C.J. Garst for providing the dataset, David Iberri for contributing to early manuscript drafts, Paul Maggio for designing the original BPA, and Debra Green and Brett Toensing for providing staff department registries.
Disclosure: Nothing to report.
Transfusion of blood products has multiple clinical applications, yet when used outside of recommended guidelines it is associated with increased cost, waste, morbidity, and mortality.[1] Studies reviewing restrictive versus liberal blood transfusion strategies have demonstrated no benefit to liberal strategies over restrictive strategies[2, 3, 4, 5, 6, 7, 8, 9, 10] and possibly even harm.[11] Given the risks and real costs of blood transfusions occurring outside of recommended guidelines, professional societies in hematology, anesthesiology, and hospital medicine each include excessive blood transfusions among their top 5 questionable clinical practices in the American Board of Internal Medicine Foundation's Choosing Wisely initiative.[12] To modify behaviors around blood transfusion practices, hospitals and blood banks may need to provide clinical decision support (CDS) for physicians.
The conventional approach to CDS is direct education and training campaigns, but there is a unique opportunity for intelligent decision support at the point of care through electronic medical record (EMR) systems directly integrated with computerized physician order entry (CPOE).[13, 14, 15] Prior work at Stanford toward reducing unnecessary blood transfusions started with hospital‐wide education campaigns, which brought down the percentage of transfusions ordered for patients with hemoglobin (Hgb) >8 g/dL from 57% to 52%. Further reduction to <30% was achieved after the introduction of an interruptive best practice alert (BPA) integrated into the CPOE transfusion ordering process.[16, 17] Specifically, providers attempting to order a blood transfusion for patients with an EMR‐determined Hgb >7 are presented with a BPA popup reminding them of best practice guidelines and a prompt to either abort the transfusion or provide a reason to override the BPA and proceed.
It remains uncertain why up to 30% of transfusions continue to occur outside of recommended guidelines in spite of interruptive prompts. This study demonstrates a general approach to secondary use of clinical data from the EMR toward understanding provider behavior, specifically by analyzing free‐text comments linked to transfusion override behavior and identifying the type of providers interacting with the BPAs.
MATERIALS AND METHODS
At Stanford University Hospital, a 447‐bed academic tertiary care center servicing adult patients, clinicians order blood transfusions through an EMR+CPOE system. When an order for red blood cell transfusion is attempted, the EMR evaluates the patient chart for specific criteria based on previously published guidelines.[18] Specifically, the BPA will review the last recorded Hgb value and trigger if the Hgb is >8, or if the Hgb is >7 and there is no concurrent EMR problem‐list entry related to acute coronary syndrome or acute hemorrhage. Once the blood transfusion BPA triggers, the ordering provider is presented with an interruptive prompt reminding them of best practice guidelines and the 3 most recent Hgb values for the patient.[16] From there, the provider may either abort the transfusion or override the BPA and proceed. Overrides require the provider to select a reason from a predefined list of institutionally accepted transfusion indications including acute bleeding, acute coronary syndrome and Hgb <8, and postoperative cardiothoracic surgery and Hgb <8. If none of the predefined override reasons are selected, the provider simply selects other, with the option of a free‐text comment to elaborate their rationale.
Data from provider interactions with the BPA were collected from the EMR across all inpatient wards for 8 months after the implementation period. Data collected from each interaction included the patient identifier, alert description, action taken, ordering provider identifier, ordering provider type (job title), optional comments for overriding the BPA, and date and time.
The free‐text override comments were independently reviewed by 2 licensed physicians, tagging them into a set of general categories by iterative inductive analysis of the comment content. Individual comments were allowed multiple possible category tags (eg, coronary artery disease and symptomatic). The initial tagging process was expedited by isolating common keywords in the override comments and assigning likely category tags to each, as in Table 2. The 2 physician reviewers then manually inspected all comments with the option to revise the initial category tagging to ensure validity. Many category tags occurred sporadically and were aggregated into more general categories, such as hematologic disorder (includes myelodysplastic syndrome, myelofibrosis, multiple myeloma, sickle cell, thalassemia, Waldenstrom's), symptomatic (includes fatigue, lightheaded, short of breath), and per other medical doctor [MD] (includes any other physician direction, primarily specialty consultation services).
To assess the inter‐rater agreement of this category tagging between the 2 reviewers, a confusion matrix similar to the example in Table 1 was setup for each tag used. Several agreement statistics are calculated based on the confusion matrix, including the positive agreement rate (Pa+) and Cohen's kappa statistic (). Kappa statistic values range from 1 to +1, with values <0 indicating no agreement and values >0.8 indicating near perfect agreement.[19] To reject the null hypothesis that the 2 reviewers could have independently arrived at their similar tagging assignments by chance, a 2 test was applied for each confusion matrix, with Yates' correction to avoid overestimating statistical significance given the low rates of inter‐rater disagreement.[20]
| Reviewer 1 Tags "Surgery" | ||||
|---|---|---|---|---|
| Yes | No | Total | ||
| ||||
| Reviewer 2 Tags "Surgery" | Yes | 143 | 11 | 154 |
| No | 5 | 820 | 825 | |
| Total | 148 | 831 | 979 | |
| Category Tag | Keyword | Keyword Count |
|---|---|---|
| ||
| Hgb 78 | 7.1, 7.2, 7.8, 7.9, 8, <8 | 360 |
| BMT | BMT | 359 |
| Symptomatic | Symptomatic | 187 |
| Surgery | Postop, post‐op, surgery, surgical | 176 |
| Dropping Hgb | Down, drop, dropping | 117 |
| Chemotherapy | Chemo, chemotherapy | 88 |
| Per other MD | Per | 87 |
| Transplant | Transplant | 70 |
| Cardiac | Cardiac | 66 |
| Bleeding | Bleeding | 65 |
| Procedure | Procedure | 65 |
| Hgb <7 | 7 | 58 |
| Hypotension | Hypotension | 51 |
| Protocol | Protocol | 51 |
| Cirrhosis | Liver | 50 |
| Imminent discharge | Discharge | 49 |
| Leukemia, acute | AML | 44 |
| Cancer | Cancer | 37 |
| Sepsis | Sepsis | 32 |
| Tachycardia | Tachycardia | 28 |
RESULTS
During the data collection period from January 1, 2011 to August 31, 2012, the blood transfusion BPA fired in 11,791 instances, of which 10,642 recorded sufficient data for analysis (Figure 1). The ordering provider proceeded to override the BPA and continued with transfusion in 98% of cases (10,442/10,642). Acute bleeding" was the most common structured response (34%). The majority of BPA overrides used the general purpose other structured response option accounting for 56% (5886/10,442) of override responses, of which 37% (2185/5886) entered a free‐text comment elaborating the override reason. With 3701 nonresponders (other overrides with no free‐text comment), the overall response rate was 65% (6941/10,642).
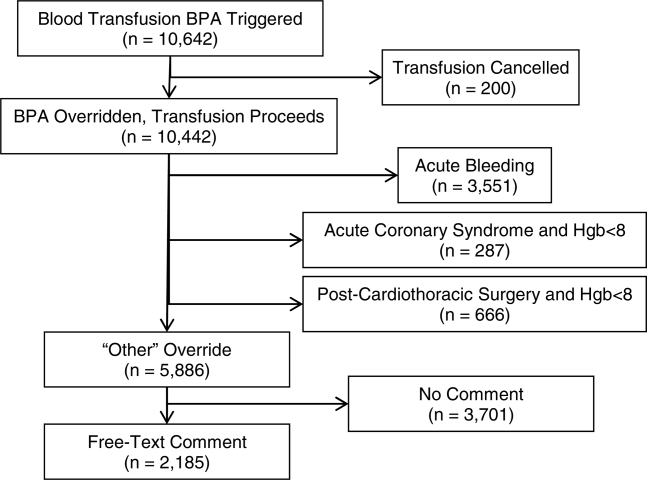
With a handful of free‐text comments included with structured override responses (eg, 28 acute bleeding overrides included additional comment from the provider), a total of 2216 override comments were available for analysis. Using an initial selection of keyword‐tag associations, as in Table 2, 95% (2104/2216) of the override comments had a preliminary category tagging assigned. After manual review and revision by the first physician reviewer, 74% (1633/2216) of the comments retained their automated tags, whereas 26% (583/2216) were updated based on the reviewer's assessment of validity. This included 112 comments lacking automated tags the reviewer manually added, as well as 471 comments with automated tags revised by the reviewer.
The most common override category tags are presented in Figure 2 and Figure 3 for BPAs triggered in response to blood transfusions ordered for patients with Hgb 78 and Hgb >8, respectively. The agreed+ percentages correspond to the number of comments where the 2 physician reviewers both assigned the respective category tag (Pa+), whereas the disagreed percentages correspond to comments where the reviewers differed (Pd=1‐Pa). By Yates' corrected 2 analysis, P was <1010 for independence between reviewer tag assignments for all tags assessed. Kappa statistics are reported in the figures to describe inter‐rater agreement.
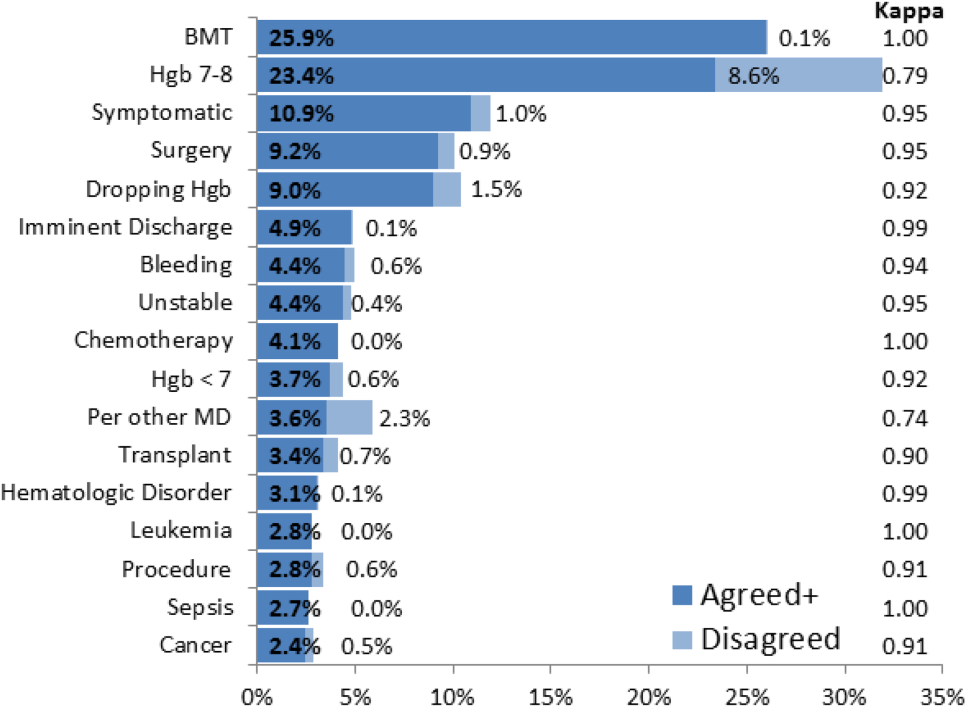
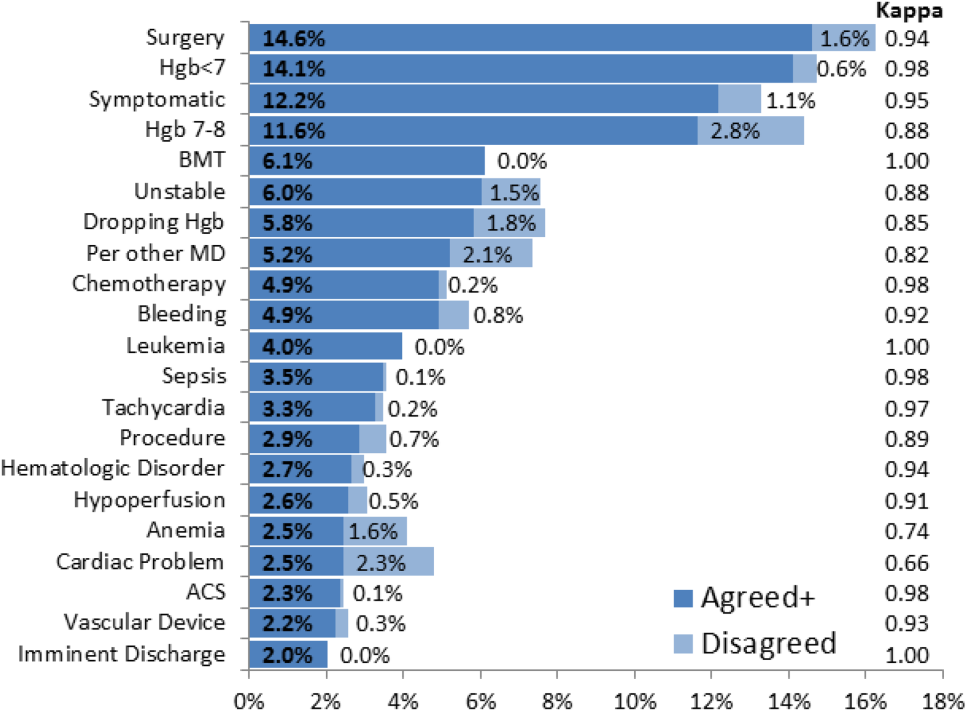
Resident physicians were the primary ordering provider group, accounting for approximately 55% (5863/10,642) of BPA interactions, followed by registered nurses, fellows, and attending physicians.
DISCUSSION
Prior work has established that an interruptive BPA to provide decision support against inappropriate blood transfusions can drive a significant and sustained reduction in unnecessary transfusions,[16] especially when satisfying the primary features of effective decision support.[14] The quantity of transfusions directly aborted by the BPA (only 2% in this case) does not nearly account for the total observed reductions in transfusions, suggesting that the BPA yields an indirect teaching effect over time beyond direct interruption. In other words, once a user has been interrupted by the BPA several times, they will be discouraged from even attempting to order inappropriate blood transfusions in the future.
Despite the improvements above, there remains a substantial fraction (up to 30%) of blood transfusions occurring outside of recommended guidelines where providers specifically override the BPA prompt.[21] This work is the first structured analysis of such BPA override behavior by generalizable methods of EMR data analysis to guide further improvements.
Analysis of the override behavior focused primarily on the free‐text comments explaining provider rationales for overriding the BPA. These comments were categorized by 2 physician reviewers, with P<1010 for all category tags, rejecting the null hypothesis that the 2 reviewers could have independently arrived at their similar category tags by chance. Further assessment of inter‐rater agreement was generally excellent, with >0.8 in the majority of cases. The remaining cases (ie, Hgb 78, per other MD, anemia, cardiac) still had substantial agreement, with >0.6. These disagreements almost universally occurred when a reviewer assigned a subset of the category tags assigned by the other reviewer. For example, 1 reviewer may tag a comment bone marrow transplant (BMT) patient with Hgb 7.2 with BMT and Hgb 78, whereas the other would only cite BMT.
Figure 2 and Figure 3 highlight the varied categories of responses, with most categories comprising <4% of the available responses. Among the most common override reasons are structured protocols for specialty services, as in the stem cell transplant service, whose protocol recommends transfusing blood when Hgb <8 rather than Hgb <7. In these cases, the BPA is unlikely to change protocolized behavior, thus overall workflow would likely be improved by adding a structured BPA override option for these protocols.
Analysis of the override comments did expose some relatively common and questionable transfusion practices, including perioperative and periprocedural transfusions, as well as anticipation of imminent discharge. Prior studies indicate that transfusions in anticipation of surgical or procedural intervention provide no benefit compared to responding to blood requirements intraoperatively as needed,[3, 22, 23] and imminent discharge of a patient is not a well‐recognized reason to transfuse outside of guidelines. The identification of these questionable and relatively common practices identifies opportunities for targeted education and training campaigns.
Symptomatic anemia was 1 of the more commonly cited BPA override reasons with a fraction providing a specific symptom such as fatigue, lightheadedness, or shortness of breath. Although the pervasiveness of this rationale may speak to adding it as a structured BPA override option, the nonspecific, subjective, and nonevidence‐based nature of symptom‐driven blood transfusions suggests that ongoing interruptive BPA prompts can still be useful to remind providers of the risks and guideline‐based approaches to such cases.
Limitations of the analysis are revealed as a fraction of BPA events did not fully record all relevant data, preventing proper analysis. Override comments suggest the BPA was triggering inappropriately for patients appropriately below the recommended transfusion threshold of Hgb <7, assuming provider free‐textentered values were accurate. Review of these cases showed some variability, such as when providers based their transfusion decision on a hematocrit of 20 rather than a Hgb of 7. Many comments also stated nonthreshold Hgb values, such as Hgb 7.2, seeming to imply that the value was close enough to the recommended threshold to justify overriding the transfusion prompt.
The most significant limitation of this study is the substantial fraction of nonresponder BPA transfusion overrides with a nonspecific other reason and no text commentary, comprising 34% (3670/10,642) of all BPA interactions and 62% (3670/5886) of all other overrides. Although the BPA is easily overridden by design to avoid workflow disruption that could compromise the priority of patient care, the nonresponses raise concern for skewed interpretation of the override data. General studies in survey responses provide reassurance that lower response rates do not necessarily indicate response bias,[24] with response rates as low as 25% yielding results statistically indistinguishable from more rigorous methods achieving >50% response rates.[25] In this specific case, response bias is better characterized by comparing ordering provider characteristics for the other overrides with and without free‐text comments. Specifically, Figure 4 shows the distribution of other overrides by provider type (job title) and provider home department (where available from physician department registries), separated by whether a free‐text comment was left. For each sub‐group, a 2 analysis compared the observed versus expected proportion of providers leaving comments based on the null hypothesis that leaving a comment was independent of membership in the subgroup. Similar proportions with nonsignificant P values suggest against significant response bias for most subgroups, but the data do indicate that this work likely under‐represents the opinion of fellows, physician assistants, and neurosurgeons, while slightly over‐representing the opinion of medicine, general surgery, and obstetrics/gynecology practitioners. Given that the under‐represented groups overall constitute a small minority of the total BPA interactions, this work should still be generalizable to the majority of transfusion behavior.
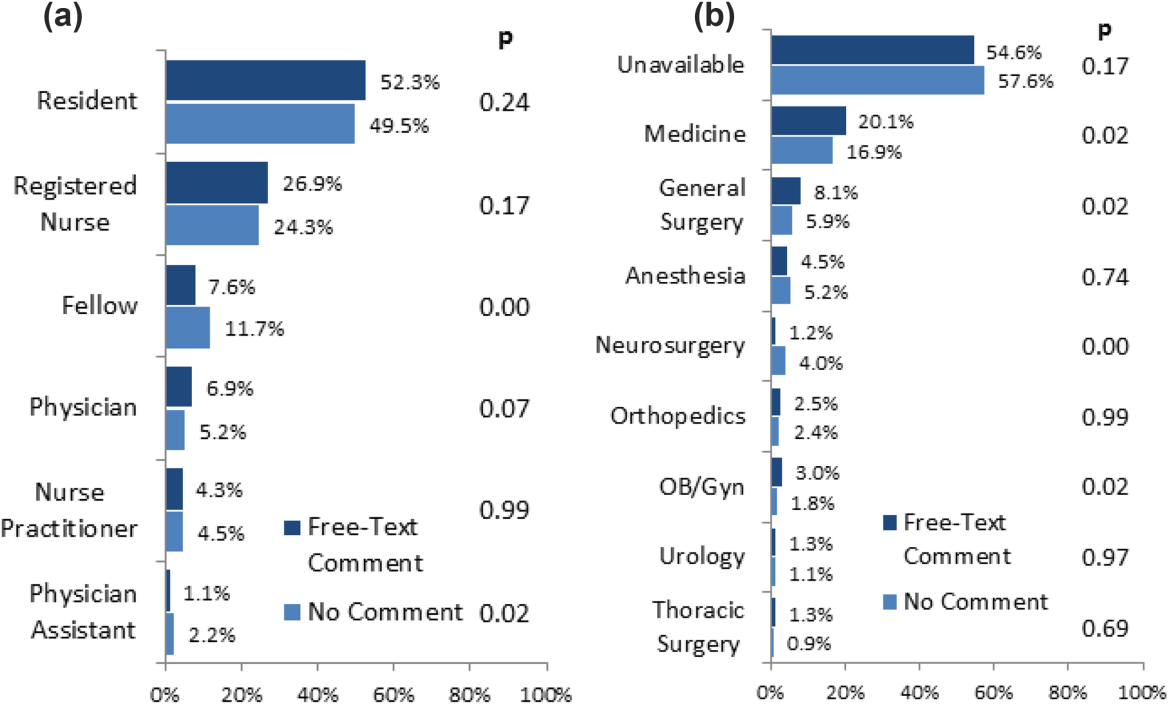
Further review of the ordering provider type (job title) distribution indicates that the vast majority of providers who actually interact with BPAs in this academic hospital are resident physicians. Similarly notable is that 25% of BPAs trigger for registered nurses. Upon review of hospital practices, we confirmed that nurses can enter transfusion orders on behalf of MD cosigners, generally in the context of a verbal order or routine treatment protocol, most notably on the stem cell transplant service. The prevalence of resident, nurse, nurse practitioner, and physician assistant order entry overall indicates that the providers encountering the BPA often do not have the negotiating power to accept or override the prompts, specifically defying the meaningful use goal of decision‐making providers directly interacting with CPOE and decision support prompts.[26]
The theoretical intelligence of the BPA not to trigger in well‐accepted cases of transfusion, where acute bleeding is occurring based on the presence of bleeding related items in the patient's problem list, is demonstrated to be limited. Acute bleeding represented the most common structured override response. This is likely multifactorial, but is largely the result of inconsistent usage of the patient problem lists that the BPA would depend upon. Another commonly cited override explanation was for a dropping Hgb without a specific bleeding source. This could point toward the BPA triggering an algorithm incorporating the last several Hgb values to assess the trajectory. Even then, however, guidelines would advocate holding transfusion and proceeding with serial monitoring of Hgb levels until an accepted transfusion threshold was actually breached.
This analysis demonstrates a general approach to secondary analysis of EMR data, in this case to provide insight into the specific question of why providers continue to order costly, unnecessary, and potentially harmful blood transfusions in spite of an interruptive BPA CDS tool. Limitations of the BPA are now better understood, including technical aspects of accounting for all decision‐making data, the frequency of nonresponse for override rationale, and that the providers interacting with the BPAs often do not have the negotiating power to change ordering behavior. The analysis recognizes protocolized behaviors that should be integrated into the CDS algorithms, and specification of symptomatic anemia as a common albeit subjective indication for blood transfusion. A wide swath of individually uncommon rationales drive transfusion override behavior, motivating further EMR‐based analysis to more efficiently recognize common scenarios (eg, perioperative/procedural, imminent discharge) for directed education and training interventions than can be achieved by conventional chart review.
Acknowledgements
The authors thank Sylvia Bereknyei for consultation on qualitative analysis methods, C.J. Garst for providing the dataset, David Iberri for contributing to early manuscript drafts, Paul Maggio for designing the original BPA, and Debra Green and Brett Toensing for providing staff department registries.
Disclosure: Nothing to report.
© 2014 Society of Hospital Medicine