User login
When Should an Abdominal Aortic Aneurysm Be Treated?
Case
A generally healthy, 74-year-old man presents with sudden-onset abdominal pain due to acute pancreatitis. Computed tomography (CT) of his abdomen shows pancreatic inflammation and an incidental finding of a 4.5-cm abdominal aortic aneurysm. He had never had any imaging of his abdomen prior to this study and described no prior episodes of abdominal pain.
When should his abdominal aortic aneurysm be treated?
Overview
An abdominal aortic aneurysm (AAA) is an abnormal dilation of the abdominal aorta between the diaphragm and the aortic bifurcation of the iliac arteries. An AAA is usually defined as a dilatation with a diameter of >3 cm or 50% greater than the typical diameter. Most AAAs are located in the infrarenal aorta, proximal to the iliac bifurcation.
Population screening programs show a prevalence of AAA of 4% to 8% in men aged 65 to 80 years.1 AAA prevalence is approximately six times greater in men than women, though the prevalence in women might be increasing.1 AAA is most common in white men, with black men and those of Asian heritage having lower risk. A combination of genetic predisposition and environmental and physiologic factors lead to initiation and progression of AAAs; family history, male sex, advanced age, and history of smoking are major risk factors.
Mortality after AAA rupture is high. Approximately 62% of patients die prior to hospital arrival.2 Of those who undergo emergent AAA surgery, 50% will die.1
Aortic repair with a prosthetic vascular graft reduces morbidity and mortality from rupture, but the risks of repair are not trivial.2
Review of the Data
Risk of rupture. An AAA should be repaired when the risk of rupture outweighs the risks of surgical repair. Symptomatic aneurysms—such as those causing back or abdominal pain—have a higher risk of rupture than asymptomatic aneurysms. Most AAAs are asymptomatic and, in the absence of imaging, not identified until the time of rupture. Given the significant mortality associated with rupture, there is benefit to intervening on asymptomatic aneurysms before rupture.
The risk of AAA rupture has been studied in patients who either have been unfit for surgical repair or uninterested in intervention. Risk of rupture increases substantially with aneurysm size. Lederle et al estimated a two-year aneurysm rupture risk of 22.1% for AAA with a diameter of 5.0 to 5.9 cm, 18.9% for 6.0 to 6.9 cm, and 43.4% for a diameter ≥7.0 cm.3 In another study of 476 patients, the average risks of rupture in male and female patients with an AAA of 5.0 to 5.9 cm were 1.0% and 3.9% per year, respectively. For male and female patients with ≥6.0 cm AAAs, risks of rupture were 14.1% and 22.3% per year.4 Women with AAA have been found to have a higher risk of rupture in all studies in which female patients were included.
Because rupture risk increases with size, predicting the rate of growth is clinically important. Powell et al conducted a systematic review of growth rates of small AAAs.5 In 15 studies that examined 7,630 patients, the growth rate for a 3.5-cm aneurysm was estimated at 1.9 mm/year and for a 4.5-cm aneurysm was 3.5 mm/year. Given an exponentially increasing aneurysm diameter, this suggests an elapsed time of 6.2 years for a 3.5-cm aneurysm to grow to 5.5 cm, and 2.3 years for a 4.5-cm AAA to grow to 5.5 cm. This prediction does not account for individual variability in growth rate. Some AAAs grow quickly, others erratically, and others not at all. This growth variability is influenced by individual characteristics including cigarette smoking, sex, age, and other factors.
Medical prevention of progression and rupture. Studies have assessed whether modification of risk factors can delay progression of growth of AAAs. In a small aneurysm trial in the United Kingdom, self-reported smoking status was associated with an incrementally increased growth rate of 0.4 mm per year.5 Each year of smoking increases the relative risk of AAA by 4%, and continued smoking leads to more rapid AAA expansion.6 There is no clear relationship between cholesterol levels and AAA expansion rate. Observational studies suggest that aneurysm expansion decreases with statin use, but there is not sufficient evidence to recommend statin therapy for AAA alone.6
Many patients with AAA, however, are candidates for statins because of concomitant coronary artery or peripheral vascular disease. Small, randomized controlled trials have shown that macrolides and tetracycline antibiotics might inhibit AAA growth, but prescribing them for this purpose is not currently the standard of care.7 Elevated mean blood pressure has been associated with rupture, but there is not good evidence showing delay of progression with treatment of hypertension.6 Early observational studies suggested that beta-blocker use would decrease AAA progression, but further evidence has not supported their benefit in slowing progression of size.8 Likewise, use of angiotensin-converting enzyme inhibitors has also shown no growth inhibition.7 An ongoing Cochrane review is evaluating evidence for these medical treatments of AAA.9
Surgical prevention of rupture. There are two surgical methods of AAA repair: open repair and endovascular aneurysm repair (EVAR). Both involve use of a prosthetic graft to prevent the aneurysm from enlarging. The EVAR procedure typically involves entry at the femoral artery, with use of catheters and guide wires to advance a graft to the desired location and anchor it in place. Because this utilizes an endovascular approach, regional rather than general anesthesia can be used.
Multiple investigators have evaluated for differences in outcomes between the two methods of surgical AAA repair. Studies have shown increased 30-day postoperative mortality with open repair, as well as significantly higher rates of postoperative cardiac, pulmonary, and renal complications. One randomized controlled study found 30-day operative mortality of 1.8% in the EVAR group and 4.3% in the open repair group.10 However, after a median six-year follow-up of patients after EVAR or open repair, there is no difference in total mortality or aneurysm-related mortality.10 Compared with open repair, the need for long-term surveillance and re-intervention post-EVAR is higher, with endoleak and graft migration the most common complications. This accounts for the loss of early survival advantage in post-EVAR patients. By two years post-operation, complication after repair with either technique is not statistically different. De Bruin et al found that six years after randomization for repair type, cumulative survival rates were 69.9% for patients after open repair and 68.9% with EVAR.11
Studies also have focused on subgroups of patients with a higher operative risk and shorter life expectancy, such as the elderly.12 A pooled analysis of 13,419 patients aged ≥80 years from six observational studies showed 8.6% immediate mortality after open repair and 2.3% after EVAR (risk difference 6.2%, 95% CI 5.4-7.0%).13 Pooled analysis of three longer-term studies showed similar overall survival at three years after EVAR and open repair.13 When EVAR is not available, open repair has acceptable short- and long-term survival in patients aged ≥80 years with an AAA at high risk of rupture.14
Screening. A Cochrane review evaluated the effect of ultrasound screening of asymptomatic AAA on mortality. In 127,891 men and 9,342 women aged 65 to 79, researchers found a significant decrease in mortality in men aged 65 to 79 who were screened (odds ratio 0.6, 95% CI 0.47-0.78) but no benefit to screening of women.15 The current U.S. Preventive Services Task Force (USPSTF) guidelines recommend one-time ultrasound-guided (USG) screening for AAA in men aged 65 to 75 who have any history of tobacco use. For men in this age group who have never smoked, the balance between benefits and harms of screening is too close for the USPSTF to make recommendations. Because of the lower prevalence in women, the USPSTF recommends against screening women for AAA.18
Timing of repair. Early repair of small AAAs (4 cm to 5.5 cm) has no long-term survival benefit compared to ultrasound surveillance without repair.16,17 Therefore, AAAs <5.5 cm should be followed with regular ultrasound surveillance every six months, with referral to surgery if the diameter reaches 5.5 cm, or grows >1 cm a year. The size at which surgery should be performed might be lower in women, given that their risk of rupture is higher than men. A thoughtful discussion of individual risks should take place in every case, but in many patients, even the elderly, repair of a large asymptomatic AAA is indicated. 5
Back to the Case
Our patient should have repeat imaging of his AAA in six months and regular surveillance afterward to monitor for growth every six months. When the AAA is >5.5 cm or if it grows >1 cm a year, he should be evaluated for EVAR or open repair.
Bottom Line
The current USPSTF guidelines recommend one-time ultrasound-guided (USG) screening for AAA in men aged 65 to 75 with a history of smoking. If an AAA >3 cm is found, the patient should undergo regular USG screening every six months. The AAA should be repaired if >5.5 cm or symptomatic, via either an endoscopic or open approach.
Dr. Best is a hospitalist at University of Washington Medicine at Harborview and associate program director of the internal-medicine residency program at the University of Washington, Seattle. Dr. Carpenter is a fellow in the division of geriatrics at the University of California at San Franscisco.
References
- Nordon IM, Hinchliffe RJ, Loftus IM, Thompson MM. Pathophysiology and epidemiology of abdominal aortic aneurysms. Nat Rev Cardiol. 2011;8, 92-102.
- Ernst CB. Abdominal aortic aneurysm. N Engl J Med. 1993;328(16):1167-1172.
- Lederle FA, Johnson GR, Wilson SE, et al. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA. 2002;287:2968-2972
- Brown PM, Zelt DT, Sobolev B. The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J Vasc Surg. 2003;37:280-284.
- Powell JT, Sweeting MJ, Brown LC, Gotensparre SM, Fowkes FG, Thompson SG. Systematic review and meta-analysis of growth rates of small abdominal aortic aneurysms. British Journal of Surgery. 2011;98:609-618.
- Brown LC, Powell JT. Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants. Ann Surg. 1999;230(3):289-297.
- Baxter BT, Terrin MC, Dalman RL. Medical management of small abdominal aortic aneurysms. Circulation. 2008;117:1883-1889.
- The Propranolol Aneurysm Trial Investigators. Propranolol for small abdominal aortic aneurysms: results of a randomized trial. J Vasc Surg. 2002:35:72-79.
- Ruhani G, Robertson L, Clarke M. Medical treatment for small abdominal aortic aneurysms. Cochrane Database for Systematic Reviews 2012. Sep 12;9:CD009536. doi: 10.1002/14651858.
- The United Kingdom EVAR Trial Investigators. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010; 362:1863-1871.
- De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1881-1889.
- Jackson RS, Chang DC, Freischlag JA. Comparison of long-term survival after open vs. endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. JAMA. 2012;307(15):1621-1628.
- Biancari F, Catania A, D’Andrea V. Elective endovascular vs. open repair of abdominal aortic aneurysm in patients aged 80 years and older: systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2011;42:571-576.
- Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464-474.
- Cosford PA, Leng GC, Tomas J. Screening for abdominal aortic aneurysm. Cochrane Database for Systematic Reviews 2007, Issue 2. Art. No.: CD002945. DOI: 10.1002/14651858.CD002945.pub2.
- Filardo G, Powell JT, Martinez MA, Ballard DJ. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database for Systematic Reviews 2012, Issue 3. Art. No.:CD001835. DOI: 10.1002/14651858.CD001835.pub3.
- The UK Small Aneurysm Trial Participants. Final 12-year follow-up of surgery versus surveillance in the UK small aneurysm trial. Brit J Surg. 2007;94:702-708.
- U.S. Preventive Services Task Force. Screening for Abdominal Aortic Aneurysm: Recommendation Statement. AHRQ Publication No. 05-0569-A, February 2005.
Case
A generally healthy, 74-year-old man presents with sudden-onset abdominal pain due to acute pancreatitis. Computed tomography (CT) of his abdomen shows pancreatic inflammation and an incidental finding of a 4.5-cm abdominal aortic aneurysm. He had never had any imaging of his abdomen prior to this study and described no prior episodes of abdominal pain.
When should his abdominal aortic aneurysm be treated?
Overview
An abdominal aortic aneurysm (AAA) is an abnormal dilation of the abdominal aorta between the diaphragm and the aortic bifurcation of the iliac arteries. An AAA is usually defined as a dilatation with a diameter of >3 cm or 50% greater than the typical diameter. Most AAAs are located in the infrarenal aorta, proximal to the iliac bifurcation.
Population screening programs show a prevalence of AAA of 4% to 8% in men aged 65 to 80 years.1 AAA prevalence is approximately six times greater in men than women, though the prevalence in women might be increasing.1 AAA is most common in white men, with black men and those of Asian heritage having lower risk. A combination of genetic predisposition and environmental and physiologic factors lead to initiation and progression of AAAs; family history, male sex, advanced age, and history of smoking are major risk factors.
Mortality after AAA rupture is high. Approximately 62% of patients die prior to hospital arrival.2 Of those who undergo emergent AAA surgery, 50% will die.1
Aortic repair with a prosthetic vascular graft reduces morbidity and mortality from rupture, but the risks of repair are not trivial.2
Review of the Data
Risk of rupture. An AAA should be repaired when the risk of rupture outweighs the risks of surgical repair. Symptomatic aneurysms—such as those causing back or abdominal pain—have a higher risk of rupture than asymptomatic aneurysms. Most AAAs are asymptomatic and, in the absence of imaging, not identified until the time of rupture. Given the significant mortality associated with rupture, there is benefit to intervening on asymptomatic aneurysms before rupture.
The risk of AAA rupture has been studied in patients who either have been unfit for surgical repair or uninterested in intervention. Risk of rupture increases substantially with aneurysm size. Lederle et al estimated a two-year aneurysm rupture risk of 22.1% for AAA with a diameter of 5.0 to 5.9 cm, 18.9% for 6.0 to 6.9 cm, and 43.4% for a diameter ≥7.0 cm.3 In another study of 476 patients, the average risks of rupture in male and female patients with an AAA of 5.0 to 5.9 cm were 1.0% and 3.9% per year, respectively. For male and female patients with ≥6.0 cm AAAs, risks of rupture were 14.1% and 22.3% per year.4 Women with AAA have been found to have a higher risk of rupture in all studies in which female patients were included.
Because rupture risk increases with size, predicting the rate of growth is clinically important. Powell et al conducted a systematic review of growth rates of small AAAs.5 In 15 studies that examined 7,630 patients, the growth rate for a 3.5-cm aneurysm was estimated at 1.9 mm/year and for a 4.5-cm aneurysm was 3.5 mm/year. Given an exponentially increasing aneurysm diameter, this suggests an elapsed time of 6.2 years for a 3.5-cm aneurysm to grow to 5.5 cm, and 2.3 years for a 4.5-cm AAA to grow to 5.5 cm. This prediction does not account for individual variability in growth rate. Some AAAs grow quickly, others erratically, and others not at all. This growth variability is influenced by individual characteristics including cigarette smoking, sex, age, and other factors.
Medical prevention of progression and rupture. Studies have assessed whether modification of risk factors can delay progression of growth of AAAs. In a small aneurysm trial in the United Kingdom, self-reported smoking status was associated with an incrementally increased growth rate of 0.4 mm per year.5 Each year of smoking increases the relative risk of AAA by 4%, and continued smoking leads to more rapid AAA expansion.6 There is no clear relationship between cholesterol levels and AAA expansion rate. Observational studies suggest that aneurysm expansion decreases with statin use, but there is not sufficient evidence to recommend statin therapy for AAA alone.6
Many patients with AAA, however, are candidates for statins because of concomitant coronary artery or peripheral vascular disease. Small, randomized controlled trials have shown that macrolides and tetracycline antibiotics might inhibit AAA growth, but prescribing them for this purpose is not currently the standard of care.7 Elevated mean blood pressure has been associated with rupture, but there is not good evidence showing delay of progression with treatment of hypertension.6 Early observational studies suggested that beta-blocker use would decrease AAA progression, but further evidence has not supported their benefit in slowing progression of size.8 Likewise, use of angiotensin-converting enzyme inhibitors has also shown no growth inhibition.7 An ongoing Cochrane review is evaluating evidence for these medical treatments of AAA.9
Surgical prevention of rupture. There are two surgical methods of AAA repair: open repair and endovascular aneurysm repair (EVAR). Both involve use of a prosthetic graft to prevent the aneurysm from enlarging. The EVAR procedure typically involves entry at the femoral artery, with use of catheters and guide wires to advance a graft to the desired location and anchor it in place. Because this utilizes an endovascular approach, regional rather than general anesthesia can be used.
Multiple investigators have evaluated for differences in outcomes between the two methods of surgical AAA repair. Studies have shown increased 30-day postoperative mortality with open repair, as well as significantly higher rates of postoperative cardiac, pulmonary, and renal complications. One randomized controlled study found 30-day operative mortality of 1.8% in the EVAR group and 4.3% in the open repair group.10 However, after a median six-year follow-up of patients after EVAR or open repair, there is no difference in total mortality or aneurysm-related mortality.10 Compared with open repair, the need for long-term surveillance and re-intervention post-EVAR is higher, with endoleak and graft migration the most common complications. This accounts for the loss of early survival advantage in post-EVAR patients. By two years post-operation, complication after repair with either technique is not statistically different. De Bruin et al found that six years after randomization for repair type, cumulative survival rates were 69.9% for patients after open repair and 68.9% with EVAR.11
Studies also have focused on subgroups of patients with a higher operative risk and shorter life expectancy, such as the elderly.12 A pooled analysis of 13,419 patients aged ≥80 years from six observational studies showed 8.6% immediate mortality after open repair and 2.3% after EVAR (risk difference 6.2%, 95% CI 5.4-7.0%).13 Pooled analysis of three longer-term studies showed similar overall survival at three years after EVAR and open repair.13 When EVAR is not available, open repair has acceptable short- and long-term survival in patients aged ≥80 years with an AAA at high risk of rupture.14
Screening. A Cochrane review evaluated the effect of ultrasound screening of asymptomatic AAA on mortality. In 127,891 men and 9,342 women aged 65 to 79, researchers found a significant decrease in mortality in men aged 65 to 79 who were screened (odds ratio 0.6, 95% CI 0.47-0.78) but no benefit to screening of women.15 The current U.S. Preventive Services Task Force (USPSTF) guidelines recommend one-time ultrasound-guided (USG) screening for AAA in men aged 65 to 75 who have any history of tobacco use. For men in this age group who have never smoked, the balance between benefits and harms of screening is too close for the USPSTF to make recommendations. Because of the lower prevalence in women, the USPSTF recommends against screening women for AAA.18
Timing of repair. Early repair of small AAAs (4 cm to 5.5 cm) has no long-term survival benefit compared to ultrasound surveillance without repair.16,17 Therefore, AAAs <5.5 cm should be followed with regular ultrasound surveillance every six months, with referral to surgery if the diameter reaches 5.5 cm, or grows >1 cm a year. The size at which surgery should be performed might be lower in women, given that their risk of rupture is higher than men. A thoughtful discussion of individual risks should take place in every case, but in many patients, even the elderly, repair of a large asymptomatic AAA is indicated. 5
Back to the Case
Our patient should have repeat imaging of his AAA in six months and regular surveillance afterward to monitor for growth every six months. When the AAA is >5.5 cm or if it grows >1 cm a year, he should be evaluated for EVAR or open repair.
Bottom Line
The current USPSTF guidelines recommend one-time ultrasound-guided (USG) screening for AAA in men aged 65 to 75 with a history of smoking. If an AAA >3 cm is found, the patient should undergo regular USG screening every six months. The AAA should be repaired if >5.5 cm or symptomatic, via either an endoscopic or open approach.
Dr. Best is a hospitalist at University of Washington Medicine at Harborview and associate program director of the internal-medicine residency program at the University of Washington, Seattle. Dr. Carpenter is a fellow in the division of geriatrics at the University of California at San Franscisco.
References
- Nordon IM, Hinchliffe RJ, Loftus IM, Thompson MM. Pathophysiology and epidemiology of abdominal aortic aneurysms. Nat Rev Cardiol. 2011;8, 92-102.
- Ernst CB. Abdominal aortic aneurysm. N Engl J Med. 1993;328(16):1167-1172.
- Lederle FA, Johnson GR, Wilson SE, et al. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA. 2002;287:2968-2972
- Brown PM, Zelt DT, Sobolev B. The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J Vasc Surg. 2003;37:280-284.
- Powell JT, Sweeting MJ, Brown LC, Gotensparre SM, Fowkes FG, Thompson SG. Systematic review and meta-analysis of growth rates of small abdominal aortic aneurysms. British Journal of Surgery. 2011;98:609-618.
- Brown LC, Powell JT. Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants. Ann Surg. 1999;230(3):289-297.
- Baxter BT, Terrin MC, Dalman RL. Medical management of small abdominal aortic aneurysms. Circulation. 2008;117:1883-1889.
- The Propranolol Aneurysm Trial Investigators. Propranolol for small abdominal aortic aneurysms: results of a randomized trial. J Vasc Surg. 2002:35:72-79.
- Ruhani G, Robertson L, Clarke M. Medical treatment for small abdominal aortic aneurysms. Cochrane Database for Systematic Reviews 2012. Sep 12;9:CD009536. doi: 10.1002/14651858.
- The United Kingdom EVAR Trial Investigators. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010; 362:1863-1871.
- De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1881-1889.
- Jackson RS, Chang DC, Freischlag JA. Comparison of long-term survival after open vs. endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. JAMA. 2012;307(15):1621-1628.
- Biancari F, Catania A, D’Andrea V. Elective endovascular vs. open repair of abdominal aortic aneurysm in patients aged 80 years and older: systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2011;42:571-576.
- Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464-474.
- Cosford PA, Leng GC, Tomas J. Screening for abdominal aortic aneurysm. Cochrane Database for Systematic Reviews 2007, Issue 2. Art. No.: CD002945. DOI: 10.1002/14651858.CD002945.pub2.
- Filardo G, Powell JT, Martinez MA, Ballard DJ. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database for Systematic Reviews 2012, Issue 3. Art. No.:CD001835. DOI: 10.1002/14651858.CD001835.pub3.
- The UK Small Aneurysm Trial Participants. Final 12-year follow-up of surgery versus surveillance in the UK small aneurysm trial. Brit J Surg. 2007;94:702-708.
- U.S. Preventive Services Task Force. Screening for Abdominal Aortic Aneurysm: Recommendation Statement. AHRQ Publication No. 05-0569-A, February 2005.
Case
A generally healthy, 74-year-old man presents with sudden-onset abdominal pain due to acute pancreatitis. Computed tomography (CT) of his abdomen shows pancreatic inflammation and an incidental finding of a 4.5-cm abdominal aortic aneurysm. He had never had any imaging of his abdomen prior to this study and described no prior episodes of abdominal pain.
When should his abdominal aortic aneurysm be treated?
Overview
An abdominal aortic aneurysm (AAA) is an abnormal dilation of the abdominal aorta between the diaphragm and the aortic bifurcation of the iliac arteries. An AAA is usually defined as a dilatation with a diameter of >3 cm or 50% greater than the typical diameter. Most AAAs are located in the infrarenal aorta, proximal to the iliac bifurcation.
Population screening programs show a prevalence of AAA of 4% to 8% in men aged 65 to 80 years.1 AAA prevalence is approximately six times greater in men than women, though the prevalence in women might be increasing.1 AAA is most common in white men, with black men and those of Asian heritage having lower risk. A combination of genetic predisposition and environmental and physiologic factors lead to initiation and progression of AAAs; family history, male sex, advanced age, and history of smoking are major risk factors.
Mortality after AAA rupture is high. Approximately 62% of patients die prior to hospital arrival.2 Of those who undergo emergent AAA surgery, 50% will die.1
Aortic repair with a prosthetic vascular graft reduces morbidity and mortality from rupture, but the risks of repair are not trivial.2
Review of the Data
Risk of rupture. An AAA should be repaired when the risk of rupture outweighs the risks of surgical repair. Symptomatic aneurysms—such as those causing back or abdominal pain—have a higher risk of rupture than asymptomatic aneurysms. Most AAAs are asymptomatic and, in the absence of imaging, not identified until the time of rupture. Given the significant mortality associated with rupture, there is benefit to intervening on asymptomatic aneurysms before rupture.
The risk of AAA rupture has been studied in patients who either have been unfit for surgical repair or uninterested in intervention. Risk of rupture increases substantially with aneurysm size. Lederle et al estimated a two-year aneurysm rupture risk of 22.1% for AAA with a diameter of 5.0 to 5.9 cm, 18.9% for 6.0 to 6.9 cm, and 43.4% for a diameter ≥7.0 cm.3 In another study of 476 patients, the average risks of rupture in male and female patients with an AAA of 5.0 to 5.9 cm were 1.0% and 3.9% per year, respectively. For male and female patients with ≥6.0 cm AAAs, risks of rupture were 14.1% and 22.3% per year.4 Women with AAA have been found to have a higher risk of rupture in all studies in which female patients were included.
Because rupture risk increases with size, predicting the rate of growth is clinically important. Powell et al conducted a systematic review of growth rates of small AAAs.5 In 15 studies that examined 7,630 patients, the growth rate for a 3.5-cm aneurysm was estimated at 1.9 mm/year and for a 4.5-cm aneurysm was 3.5 mm/year. Given an exponentially increasing aneurysm diameter, this suggests an elapsed time of 6.2 years for a 3.5-cm aneurysm to grow to 5.5 cm, and 2.3 years for a 4.5-cm AAA to grow to 5.5 cm. This prediction does not account for individual variability in growth rate. Some AAAs grow quickly, others erratically, and others not at all. This growth variability is influenced by individual characteristics including cigarette smoking, sex, age, and other factors.
Medical prevention of progression and rupture. Studies have assessed whether modification of risk factors can delay progression of growth of AAAs. In a small aneurysm trial in the United Kingdom, self-reported smoking status was associated with an incrementally increased growth rate of 0.4 mm per year.5 Each year of smoking increases the relative risk of AAA by 4%, and continued smoking leads to more rapid AAA expansion.6 There is no clear relationship between cholesterol levels and AAA expansion rate. Observational studies suggest that aneurysm expansion decreases with statin use, but there is not sufficient evidence to recommend statin therapy for AAA alone.6
Many patients with AAA, however, are candidates for statins because of concomitant coronary artery or peripheral vascular disease. Small, randomized controlled trials have shown that macrolides and tetracycline antibiotics might inhibit AAA growth, but prescribing them for this purpose is not currently the standard of care.7 Elevated mean blood pressure has been associated with rupture, but there is not good evidence showing delay of progression with treatment of hypertension.6 Early observational studies suggested that beta-blocker use would decrease AAA progression, but further evidence has not supported their benefit in slowing progression of size.8 Likewise, use of angiotensin-converting enzyme inhibitors has also shown no growth inhibition.7 An ongoing Cochrane review is evaluating evidence for these medical treatments of AAA.9
Surgical prevention of rupture. There are two surgical methods of AAA repair: open repair and endovascular aneurysm repair (EVAR). Both involve use of a prosthetic graft to prevent the aneurysm from enlarging. The EVAR procedure typically involves entry at the femoral artery, with use of catheters and guide wires to advance a graft to the desired location and anchor it in place. Because this utilizes an endovascular approach, regional rather than general anesthesia can be used.
Multiple investigators have evaluated for differences in outcomes between the two methods of surgical AAA repair. Studies have shown increased 30-day postoperative mortality with open repair, as well as significantly higher rates of postoperative cardiac, pulmonary, and renal complications. One randomized controlled study found 30-day operative mortality of 1.8% in the EVAR group and 4.3% in the open repair group.10 However, after a median six-year follow-up of patients after EVAR or open repair, there is no difference in total mortality or aneurysm-related mortality.10 Compared with open repair, the need for long-term surveillance and re-intervention post-EVAR is higher, with endoleak and graft migration the most common complications. This accounts for the loss of early survival advantage in post-EVAR patients. By two years post-operation, complication after repair with either technique is not statistically different. De Bruin et al found that six years after randomization for repair type, cumulative survival rates were 69.9% for patients after open repair and 68.9% with EVAR.11
Studies also have focused on subgroups of patients with a higher operative risk and shorter life expectancy, such as the elderly.12 A pooled analysis of 13,419 patients aged ≥80 years from six observational studies showed 8.6% immediate mortality after open repair and 2.3% after EVAR (risk difference 6.2%, 95% CI 5.4-7.0%).13 Pooled analysis of three longer-term studies showed similar overall survival at three years after EVAR and open repair.13 When EVAR is not available, open repair has acceptable short- and long-term survival in patients aged ≥80 years with an AAA at high risk of rupture.14
Screening. A Cochrane review evaluated the effect of ultrasound screening of asymptomatic AAA on mortality. In 127,891 men and 9,342 women aged 65 to 79, researchers found a significant decrease in mortality in men aged 65 to 79 who were screened (odds ratio 0.6, 95% CI 0.47-0.78) but no benefit to screening of women.15 The current U.S. Preventive Services Task Force (USPSTF) guidelines recommend one-time ultrasound-guided (USG) screening for AAA in men aged 65 to 75 who have any history of tobacco use. For men in this age group who have never smoked, the balance between benefits and harms of screening is too close for the USPSTF to make recommendations. Because of the lower prevalence in women, the USPSTF recommends against screening women for AAA.18
Timing of repair. Early repair of small AAAs (4 cm to 5.5 cm) has no long-term survival benefit compared to ultrasound surveillance without repair.16,17 Therefore, AAAs <5.5 cm should be followed with regular ultrasound surveillance every six months, with referral to surgery if the diameter reaches 5.5 cm, or grows >1 cm a year. The size at which surgery should be performed might be lower in women, given that their risk of rupture is higher than men. A thoughtful discussion of individual risks should take place in every case, but in many patients, even the elderly, repair of a large asymptomatic AAA is indicated. 5
Back to the Case
Our patient should have repeat imaging of his AAA in six months and regular surveillance afterward to monitor for growth every six months. When the AAA is >5.5 cm or if it grows >1 cm a year, he should be evaluated for EVAR or open repair.
Bottom Line
The current USPSTF guidelines recommend one-time ultrasound-guided (USG) screening for AAA in men aged 65 to 75 with a history of smoking. If an AAA >3 cm is found, the patient should undergo regular USG screening every six months. The AAA should be repaired if >5.5 cm or symptomatic, via either an endoscopic or open approach.
Dr. Best is a hospitalist at University of Washington Medicine at Harborview and associate program director of the internal-medicine residency program at the University of Washington, Seattle. Dr. Carpenter is a fellow in the division of geriatrics at the University of California at San Franscisco.
References
- Nordon IM, Hinchliffe RJ, Loftus IM, Thompson MM. Pathophysiology and epidemiology of abdominal aortic aneurysms. Nat Rev Cardiol. 2011;8, 92-102.
- Ernst CB. Abdominal aortic aneurysm. N Engl J Med. 1993;328(16):1167-1172.
- Lederle FA, Johnson GR, Wilson SE, et al. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA. 2002;287:2968-2972
- Brown PM, Zelt DT, Sobolev B. The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J Vasc Surg. 2003;37:280-284.
- Powell JT, Sweeting MJ, Brown LC, Gotensparre SM, Fowkes FG, Thompson SG. Systematic review and meta-analysis of growth rates of small abdominal aortic aneurysms. British Journal of Surgery. 2011;98:609-618.
- Brown LC, Powell JT. Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants. Ann Surg. 1999;230(3):289-297.
- Baxter BT, Terrin MC, Dalman RL. Medical management of small abdominal aortic aneurysms. Circulation. 2008;117:1883-1889.
- The Propranolol Aneurysm Trial Investigators. Propranolol for small abdominal aortic aneurysms: results of a randomized trial. J Vasc Surg. 2002:35:72-79.
- Ruhani G, Robertson L, Clarke M. Medical treatment for small abdominal aortic aneurysms. Cochrane Database for Systematic Reviews 2012. Sep 12;9:CD009536. doi: 10.1002/14651858.
- The United Kingdom EVAR Trial Investigators. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010; 362:1863-1871.
- De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362:1881-1889.
- Jackson RS, Chang DC, Freischlag JA. Comparison of long-term survival after open vs. endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. JAMA. 2012;307(15):1621-1628.
- Biancari F, Catania A, D’Andrea V. Elective endovascular vs. open repair of abdominal aortic aneurysm in patients aged 80 years and older: systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2011;42:571-576.
- Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464-474.
- Cosford PA, Leng GC, Tomas J. Screening for abdominal aortic aneurysm. Cochrane Database for Systematic Reviews 2007, Issue 2. Art. No.: CD002945. DOI: 10.1002/14651858.CD002945.pub2.
- Filardo G, Powell JT, Martinez MA, Ballard DJ. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database for Systematic Reviews 2012, Issue 3. Art. No.:CD001835. DOI: 10.1002/14651858.CD001835.pub3.
- The UK Small Aneurysm Trial Participants. Final 12-year follow-up of surgery versus surveillance in the UK small aneurysm trial. Brit J Surg. 2007;94:702-708.
- U.S. Preventive Services Task Force. Screening for Abdominal Aortic Aneurysm: Recommendation Statement. AHRQ Publication No. 05-0569-A, February 2005.
What Are the Clinical Indications for Noninvasive Positive Pressure Ventilation?
Case
A 63-year-old man with severe chronic obstructive pulmonary disease (COPD) presents with one week of increasing sputum, cough, and dyspnea. His respiratory rate is 26/minute and oxygen saturation is 86% on room air (RA). He is lethargic and appears mildly uncomfortable, but he responds appropriately to questions in three- to four-word sentences. He is tachypneic with accessory muscle use and has diffuse wheezes throughout his bilateral lung fields. His initial room air arterial blood gas (ABG) is 7.32/68/86/32. Chest radiograph is notable for flattened hemidiaphragms without focal opacity. The patient is placed on oxygen and receives prednisone with nebulized albuterol and ipratropium, but his dyspnea and tachypnea persist. Due to his respiratory distress, bilevel positive airway pressure (BiPAP) is considered.
What are the clinical indications for noninvasive positive pressure ventilation (NPPV)?
Overview
NPPV assists ventilation by delivering positive expiratory and/or inspiratory pressure without the use of an endotracheal tube. Theoretically, NPPV is a preferred method of ventilation as it may eliminate the need for endotracheal intubation and its associated morbidity and mortality, including airway trauma, loss of airway defense mechanisms (ventilator-associated pneumonia), mechanical ventilation (barotrauma), and disruption of speech and swallowing.1
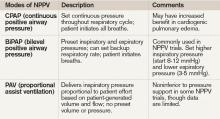
NPPV is generally delivered via full-face mask or nasal mask. Nasal mask is often preferred for patient comfort, though air leaks occur with mouth breathing. There is no difference between nasal and full-face masks in outcomes including intubation rates and mortality.2,3,4 NPPV can be delivered via a portable or standard ventilator using the same modes available for endotracheal intubation, though pressure-cycled ventilators utilizing continuous positive airway pressure (CPAP) and BiPAP are most common. CPAP delivers air at a continuous fixed pressure throughout the respiratory cycle. BiPAP delivers positive pressure at alternating levels—higher for inspiration and lower for expiration. Guidelines suggest choosing a mode based on the etiology and pathophysiology of the respiratory failure and leveraging local comfort and expertise.2,3
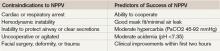
In general, good candidates for NPPV display signs of tachypnea and dyspnea due to hypoxic or hypercapnic respiratory failure but are hemodynamically stable, without excessive secretions, and can protect their airway and achieve a proper seal with the mask.3 Difficulty may arise due to patient intolerance, claustrophobia, gastric distention, and poor fit that leads to air leak or skin erosion. With initiation of NPPV, patients should be followed in a care setting with the capacity for frequent monitoring and, if needed, quick access to invasive airway management. Monitoring should include patient comfort and ability to tolerate the device, vital signs, breathing pattern, oxygen saturation, ABG, and mental status. This initial evaluation may help predict the success of NPPV (see Table 2). Appropriately chosen candidates who do well with NPPV often demonstrate respiratory turnaround in a relatively brief interval.2,3
Review of the Data
NPPV is increasingly utilized in a variety of clinical situations. In 2000, the American Thoracic Society published consensus guidelines on the use of NPPV in acute respiratory failure.2 More recently, the Canadian Medical Association developed clinical guidelines for the use of NPPV in the acute-care setting.4 Clinical scenarios in which there is evidence for the efficacy of NPPV include severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia; it can also be used as a bridge to extubation in COPD patients.1-4
Acute exacerbation of COPD. Several randomized controlled trials (RCT) and meta-analyses have assessed the potential benefits of NPPV in patients with acute exacerbations of COPD. In COPD, NPPV improves gas exchange and facilitates respiratory muscle rest to decrease the work of breathing, which allows for respiratory recovery and time to effectiveness of standard therapies.5 Multiple trials have demonstrated that the addition of NPPV to usual care decreases intubation and mortality rates, as well as hospital lengths of stay (LOS).5-8
A Cochrane review of eight RCTs comparing NPPV with usual care noted a greater than 50% reduction in risk of intubation, and a number needed to treat (NNT) of eight patients to prevent one death.5 Quon and colleagues also compared NPPV to usual care in a meta-analysis of 14 trials.6 Eleven of these trials evaluated hospital mortality, which was decreased by 55% in patients receiving NPPV. Twelve trials assessed need for intubation, which decreased by 65%. In these trials, BiPAP was the most commonly used modality (see Table 3, for a comparison of NPPV modalities). Study patients had an average pH of 7.31 with an average PaCO2 of 68 mmHg. It was noted that the beneficial effects of NPPV increased as pH decreased. An earlier meta-analysis from Keenan and colleagues supported this notion, noting that the subgroup of patients with pH <7.3 benefited most in terms of decreased rates of intubation, hospital LOS, and hospital mortality.7 In this 2003 study, patients with relatively mild exacerbations of COPD did not benefit from the addition of NPPV to usual care. Based on the amount of positive evidence, NPPV is recommended in patients experiencing severe exacerbations of COPD as evidenced by a pH <7.35 and relative hypercarbia.1,2,4,7
Cardiogenic pulmonary edema. In patients with acute cardiogenic pulmonary edema, NPPV has been found to be beneficial, decreasing mortality, rates of intubation, and hospital LOS. Physiologically, NPPV augments cardiac output, improves respiratory mechanics, and decreases afterload.10 Cardiogenic edema is variably defined and has a number of causes elucidated in an analysis of 11 RCTs conducted by Masip and colleagues. These causes included acute coronary syndrome (31%), hypertension (27%), congestive heart failure (14%), and a combination of respiratory infection, arrhythmia, volume overload, and treatment noncompliance (28%).9 In this analysis, CPAP and BiPAP demonstrated a combined 43% reduction in mortality and a 57% reduction in intubation. More recently, Peter and colleagues described a statistically significant reduction in hospital mortality and the need for intubation with CPAP, while BiPAP only demonstrated a statistically significant decrease in need for intubation.10 Thus, there appears to be some evidence that CPAP is the preferred NPPV mode in patients with acute cardiogenic pulmonary edema. Despite inclusion of a recent, large RCT showing no benefit of NPPV versus usual care in cardiogenic pulmonary edema, the overall positive effect of NPPV persisted, particularly when the cause of pulmonary edema was acute coronary syndrome.11
Weaning after intubation. NPPV has been evaluated as a method to facilitate early extubation, as a measure to prevent extubation failure, and as a treatment modality for respiratory failure following extubation, with mixed results.12,13 In 1998, a small trial compared the use of NPPV in COPD patients to facilitate early extubation with a standard weaning protocol. In this population, early NPPV resulted in better weaning rates with shorter times of mechanical ventilation (10 vs. 16 days), fewer days in the ICU, and improved 60-day survival rates (92% vs. 72%).3,14 In another RCT not limited to COPD patients, Grault and colleagues found that NPPV reduced the duration of intubation (4.5 vs. 7.6 days) but was not associated with benefits in ICU length of stay or survival previously described.3,15 Thus, though NPPV may be beneficial in facilitating early extubation in COPD patients, it is not recommended in other patient populations.4
NPPV has also been evaluated as a measure to prevent respiratory failure in patients at high risk for extubation failure. When applied immediately after extubation in patients with COPD and obesity, NPPV reduced reintubation rates and ICU mortality.3,4 In 2004, Esteban and colleagues examined NPPV in patients who had respiratory failure following extubation. In this setting, NPPV was ineffective at preventing reintubation and had no survival benefit.
In summary, NPPV may facilitate early extubation and prevent extubation failure in appropriate patients, such as those with COPD, but is unlikely to be beneficial and is not recommended in patients with existing respiratory failure after extubation.4,15
Immunosuppressed patients. A 2001 single-center, randomized-controlled trial by Holbert and colleagues demonstrated decreased intubation rates and mortality with the application of NPPV in immunosuppressed patients with hypoxemic respiratory failure, fever, and pulmonary infiltrates.16
In this study, immunosuppression occurred most commonly as a result of malignancy. In the group receiving NPPV alternating with oxygen (at least 45 minutes of NPPV alternated every three hours with periods of spontaneous breathing), the rate of subsequent intubation decreased to 46%, compared with 77% in those receiving oxygen alone. The mortality rate was 38% in the NPPV group, as compared with 69% in the standard treatment group.
Though the outcomes in immunocompromised patients with hypoxemia, fever, and pulmonary infiltrates were very poor (38% mortality even with NPPV), this small study and recent guidelines suggest a trial of NPPV in this population.4,16
Other indications. NPPV has been applied in multiple other clinical scenarios, including exacerbation of asthma, community-acquired pneumonia, acute lung injury, and bronchoscopy in hypoxemic patients. It has also been evaluated in the postsurgical period and in chest trauma. There are mixed and less robust data in these various applications, and larger controlled trials are lacking.
In asthma exacerbation, NPPV may improve dyspnea, but data regarding outcomes (intubation, mortality) are lacking. A 2005 Cochrane review concluded that data remain controversial due to insufficient evidence, and guidelines make no recommendations concerning NPPV in asthma exacerbation.4,17 Similarly, in community-acquired pneumonia without prior history of COPD, there is no major role for NPPV.1,3,4 Limited data suggest that NPPV lacks efficacy in preventing post-surgical respiratory failure, though it may be useful in treating existing respiratory failure or preventing intubation in patients following lung resection or abdominal surgery.1,4 In hypoxemic patients undergoing bronchoscopy, NPPV may improve oxygenation (lower respiratory rates and improved PaO2 to FiO2 ratios, compared with oxygen alone) as well as hemodynamics (minimizing the drop in mean arterial pressure). However, outcome data are lacking and the data set is small.4,18 In acute lung injury/acute respiratory distress syndrome, data are also limited, but NPPV appears to have a high failure rate and confers little benefit.1,4
Back to the Case
The patient was admitted to the hospital and placed on BiPAP for approximately 1.5 hours. The patient’s respiratory rate improved to 20/minute and he appeared increasingly comfortable and alert. A repeat ABG revealed improved hypercarbia and acidosis. He was continued on steroids and antibiotics and eventually was weaned from BiPAP and discharged home.
Bottom Line
NPPV is an effective method to decrease mortality, intubation rates, and duration of ICU stay in severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia, and as a bridge to extubation in COPD patients.
Dr. Kraynek is an internal medicine resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is assistant professor of medicine in the Division of General Internal Medicine at the University of Washington School of Medicine.
References
- Ambrosino N, Vagheggini G. Noninvasive positive pressure ventilation in the acute care setting: where are we? Euro Resp J. 2008;31:874-856.
- American Thoracic Society. International Consensus Conferences in Intensive Care Medicine: Noninvasive Positive Pressure Ventilation in Acute Respiratory Failure. Am J Respir Crit Care Med. 2001;163:283-291.
- Liesching T, Kwok H, Hill N. Acute applications of noninvasive positive pressure ventilation. Chest. 2003;124:699-713.
- Keenan S, Sinuff T, Burns K, et al. Clinical practice guidelines for the use of noninvasive positive pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ. 2001;183:E195-E214.
- Lightowler J, Wedzicha J, Elliot M, Ram F. Noninvasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326:185.
- Quon B, Gan W, Sin D. Contemporary management of acute exacerbations of COPD: a systematic review of the metaanalysis. Chest. 2008;133:756-766.
- Keenan S, Sinuff T, Cook D, Hill, N. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive pressure ventilation? Ann Intern Med. 2003;138:861-870.
- Scala R, Naldi M, Archinucci I, Conigilo G, Nava S. Noninvasive positive pressure ventilation in patients with acute exacerbations of COPD and varying levels of consciousness. Chest. 2005;128:1657-1666.
- Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito J. Noninvasive ventilation in acute cardiogenic pulmonary edema. JAMA. 2005;294:3124-3130.
- Peter J, Moran J, Phillips-Hughes J, Graham P, Bersten A. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-anaylsis. Lancet. 2006;367:1155-1163.
- Weng C, Zhao Y, Liu Q, et al. Meta-analysis: noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152:560-600.
- Keenan S, Sinuff T, Cook D, Hill N. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med. 2004;32:2516-2523.
- Esteban A, Frutos-Vivar F, Fergusun N, et al. Noninvasive positive pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004;350:2452-2460.
- Nava S, Ambrosino N, Clinie E, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease: a randomized, controlled trial. Ann Intern Med. 1998;128:721-728.
- Grault C, Daudenthun I, Chevron V, et al. Noninvasive ventilation as a systematic extubation and weaning technique in acute on chronic respiratory failure: a prospective, randomized controlled study. Am J Respir Crit Care Med. 1999;160:86-92.
- Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481-487.
- Ram FSF, Wellington SR, Rowe BH, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database of Systematic Reviews. 2005, Issue 3.
- Antonelli M, Conti G, Rocco M, et al. Noninvasive positive pressure ventilation vs. conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002;121:1149-1154.
Case
A 63-year-old man with severe chronic obstructive pulmonary disease (COPD) presents with one week of increasing sputum, cough, and dyspnea. His respiratory rate is 26/minute and oxygen saturation is 86% on room air (RA). He is lethargic and appears mildly uncomfortable, but he responds appropriately to questions in three- to four-word sentences. He is tachypneic with accessory muscle use and has diffuse wheezes throughout his bilateral lung fields. His initial room air arterial blood gas (ABG) is 7.32/68/86/32. Chest radiograph is notable for flattened hemidiaphragms without focal opacity. The patient is placed on oxygen and receives prednisone with nebulized albuterol and ipratropium, but his dyspnea and tachypnea persist. Due to his respiratory distress, bilevel positive airway pressure (BiPAP) is considered.
What are the clinical indications for noninvasive positive pressure ventilation (NPPV)?
Overview
NPPV assists ventilation by delivering positive expiratory and/or inspiratory pressure without the use of an endotracheal tube. Theoretically, NPPV is a preferred method of ventilation as it may eliminate the need for endotracheal intubation and its associated morbidity and mortality, including airway trauma, loss of airway defense mechanisms (ventilator-associated pneumonia), mechanical ventilation (barotrauma), and disruption of speech and swallowing.1
NPPV is generally delivered via full-face mask or nasal mask. Nasal mask is often preferred for patient comfort, though air leaks occur with mouth breathing. There is no difference between nasal and full-face masks in outcomes including intubation rates and mortality.2,3,4 NPPV can be delivered via a portable or standard ventilator using the same modes available for endotracheal intubation, though pressure-cycled ventilators utilizing continuous positive airway pressure (CPAP) and BiPAP are most common. CPAP delivers air at a continuous fixed pressure throughout the respiratory cycle. BiPAP delivers positive pressure at alternating levels—higher for inspiration and lower for expiration. Guidelines suggest choosing a mode based on the etiology and pathophysiology of the respiratory failure and leveraging local comfort and expertise.2,3
In general, good candidates for NPPV display signs of tachypnea and dyspnea due to hypoxic or hypercapnic respiratory failure but are hemodynamically stable, without excessive secretions, and can protect their airway and achieve a proper seal with the mask.3 Difficulty may arise due to patient intolerance, claustrophobia, gastric distention, and poor fit that leads to air leak or skin erosion. With initiation of NPPV, patients should be followed in a care setting with the capacity for frequent monitoring and, if needed, quick access to invasive airway management. Monitoring should include patient comfort and ability to tolerate the device, vital signs, breathing pattern, oxygen saturation, ABG, and mental status. This initial evaluation may help predict the success of NPPV (see Table 2). Appropriately chosen candidates who do well with NPPV often demonstrate respiratory turnaround in a relatively brief interval.2,3
Review of the Data
NPPV is increasingly utilized in a variety of clinical situations. In 2000, the American Thoracic Society published consensus guidelines on the use of NPPV in acute respiratory failure.2 More recently, the Canadian Medical Association developed clinical guidelines for the use of NPPV in the acute-care setting.4 Clinical scenarios in which there is evidence for the efficacy of NPPV include severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia; it can also be used as a bridge to extubation in COPD patients.1-4
Acute exacerbation of COPD. Several randomized controlled trials (RCT) and meta-analyses have assessed the potential benefits of NPPV in patients with acute exacerbations of COPD. In COPD, NPPV improves gas exchange and facilitates respiratory muscle rest to decrease the work of breathing, which allows for respiratory recovery and time to effectiveness of standard therapies.5 Multiple trials have demonstrated that the addition of NPPV to usual care decreases intubation and mortality rates, as well as hospital lengths of stay (LOS).5-8
A Cochrane review of eight RCTs comparing NPPV with usual care noted a greater than 50% reduction in risk of intubation, and a number needed to treat (NNT) of eight patients to prevent one death.5 Quon and colleagues also compared NPPV to usual care in a meta-analysis of 14 trials.6 Eleven of these trials evaluated hospital mortality, which was decreased by 55% in patients receiving NPPV. Twelve trials assessed need for intubation, which decreased by 65%. In these trials, BiPAP was the most commonly used modality (see Table 3, for a comparison of NPPV modalities). Study patients had an average pH of 7.31 with an average PaCO2 of 68 mmHg. It was noted that the beneficial effects of NPPV increased as pH decreased. An earlier meta-analysis from Keenan and colleagues supported this notion, noting that the subgroup of patients with pH <7.3 benefited most in terms of decreased rates of intubation, hospital LOS, and hospital mortality.7 In this 2003 study, patients with relatively mild exacerbations of COPD did not benefit from the addition of NPPV to usual care. Based on the amount of positive evidence, NPPV is recommended in patients experiencing severe exacerbations of COPD as evidenced by a pH <7.35 and relative hypercarbia.1,2,4,7
Cardiogenic pulmonary edema. In patients with acute cardiogenic pulmonary edema, NPPV has been found to be beneficial, decreasing mortality, rates of intubation, and hospital LOS. Physiologically, NPPV augments cardiac output, improves respiratory mechanics, and decreases afterload.10 Cardiogenic edema is variably defined and has a number of causes elucidated in an analysis of 11 RCTs conducted by Masip and colleagues. These causes included acute coronary syndrome (31%), hypertension (27%), congestive heart failure (14%), and a combination of respiratory infection, arrhythmia, volume overload, and treatment noncompliance (28%).9 In this analysis, CPAP and BiPAP demonstrated a combined 43% reduction in mortality and a 57% reduction in intubation. More recently, Peter and colleagues described a statistically significant reduction in hospital mortality and the need for intubation with CPAP, while BiPAP only demonstrated a statistically significant decrease in need for intubation.10 Thus, there appears to be some evidence that CPAP is the preferred NPPV mode in patients with acute cardiogenic pulmonary edema. Despite inclusion of a recent, large RCT showing no benefit of NPPV versus usual care in cardiogenic pulmonary edema, the overall positive effect of NPPV persisted, particularly when the cause of pulmonary edema was acute coronary syndrome.11
Weaning after intubation. NPPV has been evaluated as a method to facilitate early extubation, as a measure to prevent extubation failure, and as a treatment modality for respiratory failure following extubation, with mixed results.12,13 In 1998, a small trial compared the use of NPPV in COPD patients to facilitate early extubation with a standard weaning protocol. In this population, early NPPV resulted in better weaning rates with shorter times of mechanical ventilation (10 vs. 16 days), fewer days in the ICU, and improved 60-day survival rates (92% vs. 72%).3,14 In another RCT not limited to COPD patients, Grault and colleagues found that NPPV reduced the duration of intubation (4.5 vs. 7.6 days) but was not associated with benefits in ICU length of stay or survival previously described.3,15 Thus, though NPPV may be beneficial in facilitating early extubation in COPD patients, it is not recommended in other patient populations.4
NPPV has also been evaluated as a measure to prevent respiratory failure in patients at high risk for extubation failure. When applied immediately after extubation in patients with COPD and obesity, NPPV reduced reintubation rates and ICU mortality.3,4 In 2004, Esteban and colleagues examined NPPV in patients who had respiratory failure following extubation. In this setting, NPPV was ineffective at preventing reintubation and had no survival benefit.
In summary, NPPV may facilitate early extubation and prevent extubation failure in appropriate patients, such as those with COPD, but is unlikely to be beneficial and is not recommended in patients with existing respiratory failure after extubation.4,15
Immunosuppressed patients. A 2001 single-center, randomized-controlled trial by Holbert and colleagues demonstrated decreased intubation rates and mortality with the application of NPPV in immunosuppressed patients with hypoxemic respiratory failure, fever, and pulmonary infiltrates.16
In this study, immunosuppression occurred most commonly as a result of malignancy. In the group receiving NPPV alternating with oxygen (at least 45 minutes of NPPV alternated every three hours with periods of spontaneous breathing), the rate of subsequent intubation decreased to 46%, compared with 77% in those receiving oxygen alone. The mortality rate was 38% in the NPPV group, as compared with 69% in the standard treatment group.
Though the outcomes in immunocompromised patients with hypoxemia, fever, and pulmonary infiltrates were very poor (38% mortality even with NPPV), this small study and recent guidelines suggest a trial of NPPV in this population.4,16
Other indications. NPPV has been applied in multiple other clinical scenarios, including exacerbation of asthma, community-acquired pneumonia, acute lung injury, and bronchoscopy in hypoxemic patients. It has also been evaluated in the postsurgical period and in chest trauma. There are mixed and less robust data in these various applications, and larger controlled trials are lacking.
In asthma exacerbation, NPPV may improve dyspnea, but data regarding outcomes (intubation, mortality) are lacking. A 2005 Cochrane review concluded that data remain controversial due to insufficient evidence, and guidelines make no recommendations concerning NPPV in asthma exacerbation.4,17 Similarly, in community-acquired pneumonia without prior history of COPD, there is no major role for NPPV.1,3,4 Limited data suggest that NPPV lacks efficacy in preventing post-surgical respiratory failure, though it may be useful in treating existing respiratory failure or preventing intubation in patients following lung resection or abdominal surgery.1,4 In hypoxemic patients undergoing bronchoscopy, NPPV may improve oxygenation (lower respiratory rates and improved PaO2 to FiO2 ratios, compared with oxygen alone) as well as hemodynamics (minimizing the drop in mean arterial pressure). However, outcome data are lacking and the data set is small.4,18 In acute lung injury/acute respiratory distress syndrome, data are also limited, but NPPV appears to have a high failure rate and confers little benefit.1,4
Back to the Case
The patient was admitted to the hospital and placed on BiPAP for approximately 1.5 hours. The patient’s respiratory rate improved to 20/minute and he appeared increasingly comfortable and alert. A repeat ABG revealed improved hypercarbia and acidosis. He was continued on steroids and antibiotics and eventually was weaned from BiPAP and discharged home.
Bottom Line
NPPV is an effective method to decrease mortality, intubation rates, and duration of ICU stay in severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia, and as a bridge to extubation in COPD patients.
Dr. Kraynek is an internal medicine resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is assistant professor of medicine in the Division of General Internal Medicine at the University of Washington School of Medicine.
References
- Ambrosino N, Vagheggini G. Noninvasive positive pressure ventilation in the acute care setting: where are we? Euro Resp J. 2008;31:874-856.
- American Thoracic Society. International Consensus Conferences in Intensive Care Medicine: Noninvasive Positive Pressure Ventilation in Acute Respiratory Failure. Am J Respir Crit Care Med. 2001;163:283-291.
- Liesching T, Kwok H, Hill N. Acute applications of noninvasive positive pressure ventilation. Chest. 2003;124:699-713.
- Keenan S, Sinuff T, Burns K, et al. Clinical practice guidelines for the use of noninvasive positive pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ. 2001;183:E195-E214.
- Lightowler J, Wedzicha J, Elliot M, Ram F. Noninvasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326:185.
- Quon B, Gan W, Sin D. Contemporary management of acute exacerbations of COPD: a systematic review of the metaanalysis. Chest. 2008;133:756-766.
- Keenan S, Sinuff T, Cook D, Hill, N. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive pressure ventilation? Ann Intern Med. 2003;138:861-870.
- Scala R, Naldi M, Archinucci I, Conigilo G, Nava S. Noninvasive positive pressure ventilation in patients with acute exacerbations of COPD and varying levels of consciousness. Chest. 2005;128:1657-1666.
- Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito J. Noninvasive ventilation in acute cardiogenic pulmonary edema. JAMA. 2005;294:3124-3130.
- Peter J, Moran J, Phillips-Hughes J, Graham P, Bersten A. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-anaylsis. Lancet. 2006;367:1155-1163.
- Weng C, Zhao Y, Liu Q, et al. Meta-analysis: noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152:560-600.
- Keenan S, Sinuff T, Cook D, Hill N. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med. 2004;32:2516-2523.
- Esteban A, Frutos-Vivar F, Fergusun N, et al. Noninvasive positive pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004;350:2452-2460.
- Nava S, Ambrosino N, Clinie E, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease: a randomized, controlled trial. Ann Intern Med. 1998;128:721-728.
- Grault C, Daudenthun I, Chevron V, et al. Noninvasive ventilation as a systematic extubation and weaning technique in acute on chronic respiratory failure: a prospective, randomized controlled study. Am J Respir Crit Care Med. 1999;160:86-92.
- Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481-487.
- Ram FSF, Wellington SR, Rowe BH, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database of Systematic Reviews. 2005, Issue 3.
- Antonelli M, Conti G, Rocco M, et al. Noninvasive positive pressure ventilation vs. conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002;121:1149-1154.
Case
A 63-year-old man with severe chronic obstructive pulmonary disease (COPD) presents with one week of increasing sputum, cough, and dyspnea. His respiratory rate is 26/minute and oxygen saturation is 86% on room air (RA). He is lethargic and appears mildly uncomfortable, but he responds appropriately to questions in three- to four-word sentences. He is tachypneic with accessory muscle use and has diffuse wheezes throughout his bilateral lung fields. His initial room air arterial blood gas (ABG) is 7.32/68/86/32. Chest radiograph is notable for flattened hemidiaphragms without focal opacity. The patient is placed on oxygen and receives prednisone with nebulized albuterol and ipratropium, but his dyspnea and tachypnea persist. Due to his respiratory distress, bilevel positive airway pressure (BiPAP) is considered.
What are the clinical indications for noninvasive positive pressure ventilation (NPPV)?
Overview
NPPV assists ventilation by delivering positive expiratory and/or inspiratory pressure without the use of an endotracheal tube. Theoretically, NPPV is a preferred method of ventilation as it may eliminate the need for endotracheal intubation and its associated morbidity and mortality, including airway trauma, loss of airway defense mechanisms (ventilator-associated pneumonia), mechanical ventilation (barotrauma), and disruption of speech and swallowing.1
NPPV is generally delivered via full-face mask or nasal mask. Nasal mask is often preferred for patient comfort, though air leaks occur with mouth breathing. There is no difference between nasal and full-face masks in outcomes including intubation rates and mortality.2,3,4 NPPV can be delivered via a portable or standard ventilator using the same modes available for endotracheal intubation, though pressure-cycled ventilators utilizing continuous positive airway pressure (CPAP) and BiPAP are most common. CPAP delivers air at a continuous fixed pressure throughout the respiratory cycle. BiPAP delivers positive pressure at alternating levels—higher for inspiration and lower for expiration. Guidelines suggest choosing a mode based on the etiology and pathophysiology of the respiratory failure and leveraging local comfort and expertise.2,3
In general, good candidates for NPPV display signs of tachypnea and dyspnea due to hypoxic or hypercapnic respiratory failure but are hemodynamically stable, without excessive secretions, and can protect their airway and achieve a proper seal with the mask.3 Difficulty may arise due to patient intolerance, claustrophobia, gastric distention, and poor fit that leads to air leak or skin erosion. With initiation of NPPV, patients should be followed in a care setting with the capacity for frequent monitoring and, if needed, quick access to invasive airway management. Monitoring should include patient comfort and ability to tolerate the device, vital signs, breathing pattern, oxygen saturation, ABG, and mental status. This initial evaluation may help predict the success of NPPV (see Table 2). Appropriately chosen candidates who do well with NPPV often demonstrate respiratory turnaround in a relatively brief interval.2,3
Review of the Data
NPPV is increasingly utilized in a variety of clinical situations. In 2000, the American Thoracic Society published consensus guidelines on the use of NPPV in acute respiratory failure.2 More recently, the Canadian Medical Association developed clinical guidelines for the use of NPPV in the acute-care setting.4 Clinical scenarios in which there is evidence for the efficacy of NPPV include severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia; it can also be used as a bridge to extubation in COPD patients.1-4
Acute exacerbation of COPD. Several randomized controlled trials (RCT) and meta-analyses have assessed the potential benefits of NPPV in patients with acute exacerbations of COPD. In COPD, NPPV improves gas exchange and facilitates respiratory muscle rest to decrease the work of breathing, which allows for respiratory recovery and time to effectiveness of standard therapies.5 Multiple trials have demonstrated that the addition of NPPV to usual care decreases intubation and mortality rates, as well as hospital lengths of stay (LOS).5-8
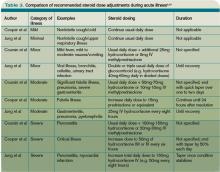
A Cochrane review of eight RCTs comparing NPPV with usual care noted a greater than 50% reduction in risk of intubation, and a number needed to treat (NNT) of eight patients to prevent one death.5 Quon and colleagues also compared NPPV to usual care in a meta-analysis of 14 trials.6 Eleven of these trials evaluated hospital mortality, which was decreased by 55% in patients receiving NPPV. Twelve trials assessed need for intubation, which decreased by 65%. In these trials, BiPAP was the most commonly used modality (see Table 3, for a comparison of NPPV modalities). Study patients had an average pH of 7.31 with an average PaCO2 of 68 mmHg. It was noted that the beneficial effects of NPPV increased as pH decreased. An earlier meta-analysis from Keenan and colleagues supported this notion, noting that the subgroup of patients with pH <7.3 benefited most in terms of decreased rates of intubation, hospital LOS, and hospital mortality.7 In this 2003 study, patients with relatively mild exacerbations of COPD did not benefit from the addition of NPPV to usual care. Based on the amount of positive evidence, NPPV is recommended in patients experiencing severe exacerbations of COPD as evidenced by a pH <7.35 and relative hypercarbia.1,2,4,7
Cardiogenic pulmonary edema. In patients with acute cardiogenic pulmonary edema, NPPV has been found to be beneficial, decreasing mortality, rates of intubation, and hospital LOS. Physiologically, NPPV augments cardiac output, improves respiratory mechanics, and decreases afterload.10 Cardiogenic edema is variably defined and has a number of causes elucidated in an analysis of 11 RCTs conducted by Masip and colleagues. These causes included acute coronary syndrome (31%), hypertension (27%), congestive heart failure (14%), and a combination of respiratory infection, arrhythmia, volume overload, and treatment noncompliance (28%).9 In this analysis, CPAP and BiPAP demonstrated a combined 43% reduction in mortality and a 57% reduction in intubation. More recently, Peter and colleagues described a statistically significant reduction in hospital mortality and the need for intubation with CPAP, while BiPAP only demonstrated a statistically significant decrease in need for intubation.10 Thus, there appears to be some evidence that CPAP is the preferred NPPV mode in patients with acute cardiogenic pulmonary edema. Despite inclusion of a recent, large RCT showing no benefit of NPPV versus usual care in cardiogenic pulmonary edema, the overall positive effect of NPPV persisted, particularly when the cause of pulmonary edema was acute coronary syndrome.11
Weaning after intubation. NPPV has been evaluated as a method to facilitate early extubation, as a measure to prevent extubation failure, and as a treatment modality for respiratory failure following extubation, with mixed results.12,13 In 1998, a small trial compared the use of NPPV in COPD patients to facilitate early extubation with a standard weaning protocol. In this population, early NPPV resulted in better weaning rates with shorter times of mechanical ventilation (10 vs. 16 days), fewer days in the ICU, and improved 60-day survival rates (92% vs. 72%).3,14 In another RCT not limited to COPD patients, Grault and colleagues found that NPPV reduced the duration of intubation (4.5 vs. 7.6 days) but was not associated with benefits in ICU length of stay or survival previously described.3,15 Thus, though NPPV may be beneficial in facilitating early extubation in COPD patients, it is not recommended in other patient populations.4
NPPV has also been evaluated as a measure to prevent respiratory failure in patients at high risk for extubation failure. When applied immediately after extubation in patients with COPD and obesity, NPPV reduced reintubation rates and ICU mortality.3,4 In 2004, Esteban and colleagues examined NPPV in patients who had respiratory failure following extubation. In this setting, NPPV was ineffective at preventing reintubation and had no survival benefit.
In summary, NPPV may facilitate early extubation and prevent extubation failure in appropriate patients, such as those with COPD, but is unlikely to be beneficial and is not recommended in patients with existing respiratory failure after extubation.4,15
Immunosuppressed patients. A 2001 single-center, randomized-controlled trial by Holbert and colleagues demonstrated decreased intubation rates and mortality with the application of NPPV in immunosuppressed patients with hypoxemic respiratory failure, fever, and pulmonary infiltrates.16
In this study, immunosuppression occurred most commonly as a result of malignancy. In the group receiving NPPV alternating with oxygen (at least 45 minutes of NPPV alternated every three hours with periods of spontaneous breathing), the rate of subsequent intubation decreased to 46%, compared with 77% in those receiving oxygen alone. The mortality rate was 38% in the NPPV group, as compared with 69% in the standard treatment group.
Though the outcomes in immunocompromised patients with hypoxemia, fever, and pulmonary infiltrates were very poor (38% mortality even with NPPV), this small study and recent guidelines suggest a trial of NPPV in this population.4,16
Other indications. NPPV has been applied in multiple other clinical scenarios, including exacerbation of asthma, community-acquired pneumonia, acute lung injury, and bronchoscopy in hypoxemic patients. It has also been evaluated in the postsurgical period and in chest trauma. There are mixed and less robust data in these various applications, and larger controlled trials are lacking.
In asthma exacerbation, NPPV may improve dyspnea, but data regarding outcomes (intubation, mortality) are lacking. A 2005 Cochrane review concluded that data remain controversial due to insufficient evidence, and guidelines make no recommendations concerning NPPV in asthma exacerbation.4,17 Similarly, in community-acquired pneumonia without prior history of COPD, there is no major role for NPPV.1,3,4 Limited data suggest that NPPV lacks efficacy in preventing post-surgical respiratory failure, though it may be useful in treating existing respiratory failure or preventing intubation in patients following lung resection or abdominal surgery.1,4 In hypoxemic patients undergoing bronchoscopy, NPPV may improve oxygenation (lower respiratory rates and improved PaO2 to FiO2 ratios, compared with oxygen alone) as well as hemodynamics (minimizing the drop in mean arterial pressure). However, outcome data are lacking and the data set is small.4,18 In acute lung injury/acute respiratory distress syndrome, data are also limited, but NPPV appears to have a high failure rate and confers little benefit.1,4
Back to the Case
The patient was admitted to the hospital and placed on BiPAP for approximately 1.5 hours. The patient’s respiratory rate improved to 20/minute and he appeared increasingly comfortable and alert. A repeat ABG revealed improved hypercarbia and acidosis. He was continued on steroids and antibiotics and eventually was weaned from BiPAP and discharged home.
Bottom Line
NPPV is an effective method to decrease mortality, intubation rates, and duration of ICU stay in severe exacerbations of COPD, cardiogenic pulmonary edema, immunosuppressed patients with pulmonary infiltrates, and hypoxia, and as a bridge to extubation in COPD patients.
Dr. Kraynek is an internal medicine resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is assistant professor of medicine in the Division of General Internal Medicine at the University of Washington School of Medicine.
References
- Ambrosino N, Vagheggini G. Noninvasive positive pressure ventilation in the acute care setting: where are we? Euro Resp J. 2008;31:874-856.
- American Thoracic Society. International Consensus Conferences in Intensive Care Medicine: Noninvasive Positive Pressure Ventilation in Acute Respiratory Failure. Am J Respir Crit Care Med. 2001;163:283-291.
- Liesching T, Kwok H, Hill N. Acute applications of noninvasive positive pressure ventilation. Chest. 2003;124:699-713.
- Keenan S, Sinuff T, Burns K, et al. Clinical practice guidelines for the use of noninvasive positive pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ. 2001;183:E195-E214.
- Lightowler J, Wedzicha J, Elliot M, Ram F. Noninvasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. 2003;326:185.
- Quon B, Gan W, Sin D. Contemporary management of acute exacerbations of COPD: a systematic review of the metaanalysis. Chest. 2008;133:756-766.
- Keenan S, Sinuff T, Cook D, Hill, N. Which patients with acute exacerbation of chronic obstructive pulmonary disease benefit from noninvasive positive pressure ventilation? Ann Intern Med. 2003;138:861-870.
- Scala R, Naldi M, Archinucci I, Conigilo G, Nava S. Noninvasive positive pressure ventilation in patients with acute exacerbations of COPD and varying levels of consciousness. Chest. 2005;128:1657-1666.
- Masip J, Roque M, Sanchez B, Fernandez R, Subirana M, Exposito J. Noninvasive ventilation in acute cardiogenic pulmonary edema. JAMA. 2005;294:3124-3130.
- Peter J, Moran J, Phillips-Hughes J, Graham P, Bersten A. Effect of non-invasive positive pressure ventilation (NIPPV) on mortality in patients with acute cardiogenic pulmonary oedema: a meta-anaylsis. Lancet. 2006;367:1155-1163.
- Weng C, Zhao Y, Liu Q, et al. Meta-analysis: noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152:560-600.
- Keenan S, Sinuff T, Cook D, Hill N. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med. 2004;32:2516-2523.
- Esteban A, Frutos-Vivar F, Fergusun N, et al. Noninvasive positive pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004;350:2452-2460.
- Nava S, Ambrosino N, Clinie E, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease: a randomized, controlled trial. Ann Intern Med. 1998;128:721-728.
- Grault C, Daudenthun I, Chevron V, et al. Noninvasive ventilation as a systematic extubation and weaning technique in acute on chronic respiratory failure: a prospective, randomized controlled study. Am J Respir Crit Care Med. 1999;160:86-92.
- Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481-487.
- Ram FSF, Wellington SR, Rowe BH, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database of Systematic Reviews. 2005, Issue 3.
- Antonelli M, Conti G, Rocco M, et al. Noninvasive positive pressure ventilation vs. conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002;121:1149-1154.
Are Stress-Dose Steroids Indicated in Patients with Adrenal Insufficiency Hospitalized with Noncritical, Nonsurgical Illness?
Case
A 46-year-old woman with Addison’s disease and type II diabetes presents with one day of right leg pain, swelling, and redness. She has had mild nausea and vomiting over the past week, with an episode of diarrhea three days prior. She takes hydrocortisone 30mg in the morning and 10mg at bedtime, as well as fludrocortisone 0.2mg in the morning. She is afebrile with a pulse of 108 beats per minute. Her initial blood pressure was 74/49 mmHg, which improved to 84/45 mmHg following one liter of normal saline. She is mentating appropriately. The physical exam is significant for a large, tender area of erythema and warmth from the right ankle to mid-calf. She is admitted for cellulitis and intravenous antibiotics are initiated.
Does she require an increase in her glucocorticoid dose during her acute illness?
Overview
Adrenal insufficiency occurs in approximately 5 out of every 10,000 people and results from primary failure of the adrenal gland, or secondary impairment of the hypothalamic-pituitary-adrenal (HPA) axis, which regulates cortisol secretion.1 In developed countries, 90% of primary adrenal insufficiency (Addison’s disease) cases are due to autoimmune adrenalitis, which might occur in isolation or as part of an autoimmune polyglandular syndrome.1,2 Secondary adrenal insufficiency is most commonly the result of chronic glucocorticoid therapy, though lesions involving the hypothalamus or pituitary gland might be implicated.2,3
In a healthy individual, cortisol is secreted in a diurnal pattern from the adrenal glands under the control of corticotropin (ACTH) produced by the pituitary gland and corticotropin-releasing hormone (CRH) produced by the hypothalamus (see Figure 1, p. 19). In the normal state, during periods of such systemic stress as illness, trauma, burns, or surgery, cortisol production increases to a degree roughly proportional to the degree of illness (as much as sixfold).4,5 Patients with adrenal insufficiency are unable to mount an appropriate cortisol response and, therefore, are at risk for adrenal crisis—a life-threatening condition characterized by hypotension and hypovolemic shock.
Although recommendations for high-dose intravenous steroids in adrenally insufficient patients who are critically ill or undergoing surgery have been extensively discussed in the literature, there are relatively few data regarding the appropriate management of adrenal insufficiency in patients hospitalized for noncritical illness.
Several recent studies have investigated the patient characteristics, situations, and conditions most likely to provoke adrenal crisis in order to establish guidelines dictating the use of supra-physiologic steroid dosing.
Review of the Data
Studies have estimated the prevalence of adrenal crisis in patients with underlying insufficiency at 3.3 to 6.3 events per 100 patient years, with 42% of patients reporting at least one crisis.2,5,6 A recent survey of 982 patients with Addison’s disease in the United Kingdom reported an 8% annual frequency.7
A retrospective Japanese study reviewed the medical charts of 137 adult patients receiving steroid replacement for established primary or secondary adrenal insufficiency. The authors noted a significant positive association between adrenal crisis and long-term steroid replacement (>4 years), concomitant mental disorder, and sex hormone deficiency. A combination of any of these factors further increased the risk.8
A more recent survey of 444 patients ages 17-81 assessed independent risk factors for adrenal crisis in the setting of primary (N=254) or secondary (N=190) adrenal insufficiency. The incidence of crisis was higher in primary versus secondary insufficiency. In patients with primary insufficiency, concomitant, non-endocrine disorders increased the risk of adrenal crisis, whereas diabetes insipidus and female gender increased risk in patients with secondary insufficiency. This same study also investigated events leading to a crisis and found gastrointestinal infection to be the most frequent factor, followed by other infectious or febrile illnesses. Overall, infection comprised 45% of all identified triggers.6
A similar study conducted by White and Arlt evaluated 841 Addison’s patients in the United Kingdom, Canada, Australia, and New Zealand.7 Again, gastrointestinal illness was the most common provoking factor, responsible for 56% of all reported crises. Flulike illness followed at 11%, followed by infections and surgical procedures at 6% each. This study found a higher risk of crisis in patients with diabetes (type I or II), premature ovarian failure, and asthma; the presence of multiple comorbidities further increased risk.
Medications. Glucocorticoid therapy is known to suppress the HPA axis. Although it was once believed that the duration and dose of therapy correlated directly with the degree of HPA suppression, more recent studies have failed to find any definite relationship.9 Patients taking the equivalent of 5mg of prednisone per day should continue to have an intact HPA axis, as this dose mimics physiologic secretion of cortisol in a healthy individual.3
However, the dose and duration of therapy at which suppression occurs is highly variable between patients. In general, patients on 7.5mg of prednisone or more per day for at least three weeks should be considered to be suppressed.3,9 Additionally, progesterone derivatives (i.e., megestrol) have glucocorticoid activity and might suppress HPA function. Other medications that might have related effects are those that inhibit enzymes involved in cortisol synthesis; ketoconazole and etomidate are common examples. Rifampin and several classes of anti-epileptic drugs induce enzymes, which increase hepatic metabolism of cortisol (see Table 1, p. 18).
Hyperthyroidism. Thyroid hormone is involved in the metabolism of cortisol, thus an increase in T4 correlates with lower levels. Adrenal insufficiency and thyroid disease might coexist within the autoimmune polyglandular syndrome. Initiation or uptitration of thyroid replacement should be avoided if acute adrenal insufficiency is suspected, as this might provoke an adrenal crisis. Conversely, any patient with adrenal insufficiency who has uncontrolled hyperthyroidism should receive two to three times their usual glucocorticoid replacement.1,2
Pregnancy. Levels of cortisol-binding globulin increase throughout pregnancy. In women with intact adrenal function, free cortisol levels also rise during the third trimester. Therefore, glucocorticoid replacement should be increased by 50% during the last three months of pregnancy.2
Acute illness. The cortisol response to stress is highly variable and dependent on a number of factors, including age, underlying health, and genetics. In general, most experts recommend doubling or tripling the daily replacement dose during mild to moderate illness until recovery (often referred to as the “sick-day rules”). What constitutes “recovery” is not clearly defined. When oral intake is compromised, as with vomiting or diarrhea, parenteral administration of steroids is recommended.1-5,9,10 Patients with adrenal insufficiency should be provided an emergency injection kit to use and further counseled to seek medical attention. Injection kits typically consist of 100mg of hydrocortisone or 4mg of dexamethasone, although other glucocorticoids may be used (see Table 2, above left, for conversions).
Limited data are available to support guidelines for glucocorticoid adjustment during acute, non-critical illness. Published guidelines vary both in illness categorization and category-specific recommendations (see Table 3, below).
Coursin and Wood devised a set of guidelines based on a literature review and consultation with experts, categorizing medical illness as minor, moderate, severe, and critical (see Table 3).3 For noncritical illness, they recommended continuation of standard replacement therapy with an additional, once-daily dose, which varied according to illness severity.
Cooper and Stewart conducted a similar review, basing their guidelines on a categorization of mild, moderate, severe/critical, or septic shock. These guidelines recommended a total daily dose of glucocorticoid supplementation, rather than an addition of a single dose to current therapy. They also stated that the least severe category of illness (defined as mild) did not require any change to a patient’s regular therapy.4
Jung et al classified illness as minimal, minor, moderate, severe, and critical.9 Under these guidelines, supplemental therapy was not advised for minimal (nonfebrile) illness. Moderate illness, including cellulitis, warranted a doubling or tripling of the outpatient dose until recovery, which was consistent with prior expert recommendation. More severe illness warranted intravenous administration of steroids.
Back to the Case
The patient had a mild case of cellulitis, classified by most experts as moderate illness, which responded well to vancomycin. Her outpatient glucocorticoid dose was doubled on admission and administered orally for the duration of her hospitalization, as she had no further episodes of vomiting or diarrhea.
Review of the patient’s records from prior hospitalizations and ambulatory visits revealed that her systolic blood pressure typically ran in the 80 mmHg to 100 mmHg range. Following initial volume resuscitation, her systolic blood pressure remained in the 90-100 mmHg range.
She was discharged home in stable condition, with instructions to complete a course of oral trimethoprim/sulfamethoxazole, resume her baseline dose of hydrocortisone the day after discharge, and follow up with her PCP for further monitoring and adjustment of her adrenal replacement therapy.
Bottom Line
For adults with adrenal insufficiency hospitalized with noncritical, nonsurgical illness, the expert recommendation is to double or triple the usual outpatient dose of glucocorticoid; however, data to support this is limited, and each patient should be assessed carefully and monitored to determine the optimal dose adjustment. TH
Dr. Shaw is a resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is an assistant professor of medicine in the division of general internal medicine, University of Washington School of Medicine.
References
- Arlt W. The approach to the adult with newly diagnosed adrenal insufficiency. J Clin Endocrinol Metab. 2009;94(4):1059-1067.
- Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003; 361:1881-1893.
- Coursin DB, Wood KE. Corticosteroid supplementation for adrenal insufficiency. JAMA. 2002;287:236-240.
- Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. N Engl J Med. 2003;348:727-734.
- Hahner S, Allolio B. Therapeutic management of adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23:167-179.
- Hahner S, Loeffler M, Bleicken B, et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies. Eur J Endocrinol. 2010;162:597:602.
- White K, Arlt W. Adrenal crisis in treated Addison’s disease: a predictable but under-managed event. Eur J Endocrinol. 2010;162:115-120.
- Omori K, Nomura K, Shimizu S, Omori N, Takano K. Risk factors for adrenal crises in patients with adrenal insufficiency. Endocr J. 2003;50:745-752.
- Jung C, Inder WJ. Management of adrenal insufficiency during the stress of medical illness and surgery. Med J Aust. 2008;188:409-413.
- Crown A, Lightman S. Why is the management of glucocorticoid deficiency still controversial: a review of the literature. Clin Endocrinol. 2005;63:483-492.
Case
A 46-year-old woman with Addison’s disease and type II diabetes presents with one day of right leg pain, swelling, and redness. She has had mild nausea and vomiting over the past week, with an episode of diarrhea three days prior. She takes hydrocortisone 30mg in the morning and 10mg at bedtime, as well as fludrocortisone 0.2mg in the morning. She is afebrile with a pulse of 108 beats per minute. Her initial blood pressure was 74/49 mmHg, which improved to 84/45 mmHg following one liter of normal saline. She is mentating appropriately. The physical exam is significant for a large, tender area of erythema and warmth from the right ankle to mid-calf. She is admitted for cellulitis and intravenous antibiotics are initiated.
Does she require an increase in her glucocorticoid dose during her acute illness?
Overview
Adrenal insufficiency occurs in approximately 5 out of every 10,000 people and results from primary failure of the adrenal gland, or secondary impairment of the hypothalamic-pituitary-adrenal (HPA) axis, which regulates cortisol secretion.1 In developed countries, 90% of primary adrenal insufficiency (Addison’s disease) cases are due to autoimmune adrenalitis, which might occur in isolation or as part of an autoimmune polyglandular syndrome.1,2 Secondary adrenal insufficiency is most commonly the result of chronic glucocorticoid therapy, though lesions involving the hypothalamus or pituitary gland might be implicated.2,3
In a healthy individual, cortisol is secreted in a diurnal pattern from the adrenal glands under the control of corticotropin (ACTH) produced by the pituitary gland and corticotropin-releasing hormone (CRH) produced by the hypothalamus (see Figure 1, p. 19). In the normal state, during periods of such systemic stress as illness, trauma, burns, or surgery, cortisol production increases to a degree roughly proportional to the degree of illness (as much as sixfold).4,5 Patients with adrenal insufficiency are unable to mount an appropriate cortisol response and, therefore, are at risk for adrenal crisis—a life-threatening condition characterized by hypotension and hypovolemic shock.
Although recommendations for high-dose intravenous steroids in adrenally insufficient patients who are critically ill or undergoing surgery have been extensively discussed in the literature, there are relatively few data regarding the appropriate management of adrenal insufficiency in patients hospitalized for noncritical illness.
Several recent studies have investigated the patient characteristics, situations, and conditions most likely to provoke adrenal crisis in order to establish guidelines dictating the use of supra-physiologic steroid dosing.
Review of the Data
Studies have estimated the prevalence of adrenal crisis in patients with underlying insufficiency at 3.3 to 6.3 events per 100 patient years, with 42% of patients reporting at least one crisis.2,5,6 A recent survey of 982 patients with Addison’s disease in the United Kingdom reported an 8% annual frequency.7
A retrospective Japanese study reviewed the medical charts of 137 adult patients receiving steroid replacement for established primary or secondary adrenal insufficiency. The authors noted a significant positive association between adrenal crisis and long-term steroid replacement (>4 years), concomitant mental disorder, and sex hormone deficiency. A combination of any of these factors further increased the risk.8
A more recent survey of 444 patients ages 17-81 assessed independent risk factors for adrenal crisis in the setting of primary (N=254) or secondary (N=190) adrenal insufficiency. The incidence of crisis was higher in primary versus secondary insufficiency. In patients with primary insufficiency, concomitant, non-endocrine disorders increased the risk of adrenal crisis, whereas diabetes insipidus and female gender increased risk in patients with secondary insufficiency. This same study also investigated events leading to a crisis and found gastrointestinal infection to be the most frequent factor, followed by other infectious or febrile illnesses. Overall, infection comprised 45% of all identified triggers.6
A similar study conducted by White and Arlt evaluated 841 Addison’s patients in the United Kingdom, Canada, Australia, and New Zealand.7 Again, gastrointestinal illness was the most common provoking factor, responsible for 56% of all reported crises. Flulike illness followed at 11%, followed by infections and surgical procedures at 6% each. This study found a higher risk of crisis in patients with diabetes (type I or II), premature ovarian failure, and asthma; the presence of multiple comorbidities further increased risk.
Medications. Glucocorticoid therapy is known to suppress the HPA axis. Although it was once believed that the duration and dose of therapy correlated directly with the degree of HPA suppression, more recent studies have failed to find any definite relationship.9 Patients taking the equivalent of 5mg of prednisone per day should continue to have an intact HPA axis, as this dose mimics physiologic secretion of cortisol in a healthy individual.3
However, the dose and duration of therapy at which suppression occurs is highly variable between patients. In general, patients on 7.5mg of prednisone or more per day for at least three weeks should be considered to be suppressed.3,9 Additionally, progesterone derivatives (i.e., megestrol) have glucocorticoid activity and might suppress HPA function. Other medications that might have related effects are those that inhibit enzymes involved in cortisol synthesis; ketoconazole and etomidate are common examples. Rifampin and several classes of anti-epileptic drugs induce enzymes, which increase hepatic metabolism of cortisol (see Table 1, p. 18).
Hyperthyroidism. Thyroid hormone is involved in the metabolism of cortisol, thus an increase in T4 correlates with lower levels. Adrenal insufficiency and thyroid disease might coexist within the autoimmune polyglandular syndrome. Initiation or uptitration of thyroid replacement should be avoided if acute adrenal insufficiency is suspected, as this might provoke an adrenal crisis. Conversely, any patient with adrenal insufficiency who has uncontrolled hyperthyroidism should receive two to three times their usual glucocorticoid replacement.1,2
Pregnancy. Levels of cortisol-binding globulin increase throughout pregnancy. In women with intact adrenal function, free cortisol levels also rise during the third trimester. Therefore, glucocorticoid replacement should be increased by 50% during the last three months of pregnancy.2
Acute illness. The cortisol response to stress is highly variable and dependent on a number of factors, including age, underlying health, and genetics. In general, most experts recommend doubling or tripling the daily replacement dose during mild to moderate illness until recovery (often referred to as the “sick-day rules”). What constitutes “recovery” is not clearly defined. When oral intake is compromised, as with vomiting or diarrhea, parenteral administration of steroids is recommended.1-5,9,10 Patients with adrenal insufficiency should be provided an emergency injection kit to use and further counseled to seek medical attention. Injection kits typically consist of 100mg of hydrocortisone or 4mg of dexamethasone, although other glucocorticoids may be used (see Table 2, above left, for conversions).
Limited data are available to support guidelines for glucocorticoid adjustment during acute, non-critical illness. Published guidelines vary both in illness categorization and category-specific recommendations (see Table 3, below).
Coursin and Wood devised a set of guidelines based on a literature review and consultation with experts, categorizing medical illness as minor, moderate, severe, and critical (see Table 3).3 For noncritical illness, they recommended continuation of standard replacement therapy with an additional, once-daily dose, which varied according to illness severity.
Cooper and Stewart conducted a similar review, basing their guidelines on a categorization of mild, moderate, severe/critical, or septic shock. These guidelines recommended a total daily dose of glucocorticoid supplementation, rather than an addition of a single dose to current therapy. They also stated that the least severe category of illness (defined as mild) did not require any change to a patient’s regular therapy.4
Jung et al classified illness as minimal, minor, moderate, severe, and critical.9 Under these guidelines, supplemental therapy was not advised for minimal (nonfebrile) illness. Moderate illness, including cellulitis, warranted a doubling or tripling of the outpatient dose until recovery, which was consistent with prior expert recommendation. More severe illness warranted intravenous administration of steroids.
Back to the Case
The patient had a mild case of cellulitis, classified by most experts as moderate illness, which responded well to vancomycin. Her outpatient glucocorticoid dose was doubled on admission and administered orally for the duration of her hospitalization, as she had no further episodes of vomiting or diarrhea.
Review of the patient’s records from prior hospitalizations and ambulatory visits revealed that her systolic blood pressure typically ran in the 80 mmHg to 100 mmHg range. Following initial volume resuscitation, her systolic blood pressure remained in the 90-100 mmHg range.
She was discharged home in stable condition, with instructions to complete a course of oral trimethoprim/sulfamethoxazole, resume her baseline dose of hydrocortisone the day after discharge, and follow up with her PCP for further monitoring and adjustment of her adrenal replacement therapy.
Bottom Line
For adults with adrenal insufficiency hospitalized with noncritical, nonsurgical illness, the expert recommendation is to double or triple the usual outpatient dose of glucocorticoid; however, data to support this is limited, and each patient should be assessed carefully and monitored to determine the optimal dose adjustment. TH
Dr. Shaw is a resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is an assistant professor of medicine in the division of general internal medicine, University of Washington School of Medicine.
References
- Arlt W. The approach to the adult with newly diagnosed adrenal insufficiency. J Clin Endocrinol Metab. 2009;94(4):1059-1067.
- Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003; 361:1881-1893.
- Coursin DB, Wood KE. Corticosteroid supplementation for adrenal insufficiency. JAMA. 2002;287:236-240.
- Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. N Engl J Med. 2003;348:727-734.
- Hahner S, Allolio B. Therapeutic management of adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23:167-179.
- Hahner S, Loeffler M, Bleicken B, et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies. Eur J Endocrinol. 2010;162:597:602.
- White K, Arlt W. Adrenal crisis in treated Addison’s disease: a predictable but under-managed event. Eur J Endocrinol. 2010;162:115-120.
- Omori K, Nomura K, Shimizu S, Omori N, Takano K. Risk factors for adrenal crises in patients with adrenal insufficiency. Endocr J. 2003;50:745-752.
- Jung C, Inder WJ. Management of adrenal insufficiency during the stress of medical illness and surgery. Med J Aust. 2008;188:409-413.
- Crown A, Lightman S. Why is the management of glucocorticoid deficiency still controversial: a review of the literature. Clin Endocrinol. 2005;63:483-492.
Case
A 46-year-old woman with Addison’s disease and type II diabetes presents with one day of right leg pain, swelling, and redness. She has had mild nausea and vomiting over the past week, with an episode of diarrhea three days prior. She takes hydrocortisone 30mg in the morning and 10mg at bedtime, as well as fludrocortisone 0.2mg in the morning. She is afebrile with a pulse of 108 beats per minute. Her initial blood pressure was 74/49 mmHg, which improved to 84/45 mmHg following one liter of normal saline. She is mentating appropriately. The physical exam is significant for a large, tender area of erythema and warmth from the right ankle to mid-calf. She is admitted for cellulitis and intravenous antibiotics are initiated.
Does she require an increase in her glucocorticoid dose during her acute illness?
Overview
Adrenal insufficiency occurs in approximately 5 out of every 10,000 people and results from primary failure of the adrenal gland, or secondary impairment of the hypothalamic-pituitary-adrenal (HPA) axis, which regulates cortisol secretion.1 In developed countries, 90% of primary adrenal insufficiency (Addison’s disease) cases are due to autoimmune adrenalitis, which might occur in isolation or as part of an autoimmune polyglandular syndrome.1,2 Secondary adrenal insufficiency is most commonly the result of chronic glucocorticoid therapy, though lesions involving the hypothalamus or pituitary gland might be implicated.2,3
In a healthy individual, cortisol is secreted in a diurnal pattern from the adrenal glands under the control of corticotropin (ACTH) produced by the pituitary gland and corticotropin-releasing hormone (CRH) produced by the hypothalamus (see Figure 1, p. 19). In the normal state, during periods of such systemic stress as illness, trauma, burns, or surgery, cortisol production increases to a degree roughly proportional to the degree of illness (as much as sixfold).4,5 Patients with adrenal insufficiency are unable to mount an appropriate cortisol response and, therefore, are at risk for adrenal crisis—a life-threatening condition characterized by hypotension and hypovolemic shock.
Although recommendations for high-dose intravenous steroids in adrenally insufficient patients who are critically ill or undergoing surgery have been extensively discussed in the literature, there are relatively few data regarding the appropriate management of adrenal insufficiency in patients hospitalized for noncritical illness.
Several recent studies have investigated the patient characteristics, situations, and conditions most likely to provoke adrenal crisis in order to establish guidelines dictating the use of supra-physiologic steroid dosing.
Review of the Data
Studies have estimated the prevalence of adrenal crisis in patients with underlying insufficiency at 3.3 to 6.3 events per 100 patient years, with 42% of patients reporting at least one crisis.2,5,6 A recent survey of 982 patients with Addison’s disease in the United Kingdom reported an 8% annual frequency.7
A retrospective Japanese study reviewed the medical charts of 137 adult patients receiving steroid replacement for established primary or secondary adrenal insufficiency. The authors noted a significant positive association between adrenal crisis and long-term steroid replacement (>4 years), concomitant mental disorder, and sex hormone deficiency. A combination of any of these factors further increased the risk.8
A more recent survey of 444 patients ages 17-81 assessed independent risk factors for adrenal crisis in the setting of primary (N=254) or secondary (N=190) adrenal insufficiency. The incidence of crisis was higher in primary versus secondary insufficiency. In patients with primary insufficiency, concomitant, non-endocrine disorders increased the risk of adrenal crisis, whereas diabetes insipidus and female gender increased risk in patients with secondary insufficiency. This same study also investigated events leading to a crisis and found gastrointestinal infection to be the most frequent factor, followed by other infectious or febrile illnesses. Overall, infection comprised 45% of all identified triggers.6
A similar study conducted by White and Arlt evaluated 841 Addison’s patients in the United Kingdom, Canada, Australia, and New Zealand.7 Again, gastrointestinal illness was the most common provoking factor, responsible for 56% of all reported crises. Flulike illness followed at 11%, followed by infections and surgical procedures at 6% each. This study found a higher risk of crisis in patients with diabetes (type I or II), premature ovarian failure, and asthma; the presence of multiple comorbidities further increased risk.
Medications. Glucocorticoid therapy is known to suppress the HPA axis. Although it was once believed that the duration and dose of therapy correlated directly with the degree of HPA suppression, more recent studies have failed to find any definite relationship.9 Patients taking the equivalent of 5mg of prednisone per day should continue to have an intact HPA axis, as this dose mimics physiologic secretion of cortisol in a healthy individual.3
However, the dose and duration of therapy at which suppression occurs is highly variable between patients. In general, patients on 7.5mg of prednisone or more per day for at least three weeks should be considered to be suppressed.3,9 Additionally, progesterone derivatives (i.e., megestrol) have glucocorticoid activity and might suppress HPA function. Other medications that might have related effects are those that inhibit enzymes involved in cortisol synthesis; ketoconazole and etomidate are common examples. Rifampin and several classes of anti-epileptic drugs induce enzymes, which increase hepatic metabolism of cortisol (see Table 1, p. 18).
Hyperthyroidism. Thyroid hormone is involved in the metabolism of cortisol, thus an increase in T4 correlates with lower levels. Adrenal insufficiency and thyroid disease might coexist within the autoimmune polyglandular syndrome. Initiation or uptitration of thyroid replacement should be avoided if acute adrenal insufficiency is suspected, as this might provoke an adrenal crisis. Conversely, any patient with adrenal insufficiency who has uncontrolled hyperthyroidism should receive two to three times their usual glucocorticoid replacement.1,2
Pregnancy. Levels of cortisol-binding globulin increase throughout pregnancy. In women with intact adrenal function, free cortisol levels also rise during the third trimester. Therefore, glucocorticoid replacement should be increased by 50% during the last three months of pregnancy.2
Acute illness. The cortisol response to stress is highly variable and dependent on a number of factors, including age, underlying health, and genetics. In general, most experts recommend doubling or tripling the daily replacement dose during mild to moderate illness until recovery (often referred to as the “sick-day rules”). What constitutes “recovery” is not clearly defined. When oral intake is compromised, as with vomiting or diarrhea, parenteral administration of steroids is recommended.1-5,9,10 Patients with adrenal insufficiency should be provided an emergency injection kit to use and further counseled to seek medical attention. Injection kits typically consist of 100mg of hydrocortisone or 4mg of dexamethasone, although other glucocorticoids may be used (see Table 2, above left, for conversions).
Limited data are available to support guidelines for glucocorticoid adjustment during acute, non-critical illness. Published guidelines vary both in illness categorization and category-specific recommendations (see Table 3, below).
Coursin and Wood devised a set of guidelines based on a literature review and consultation with experts, categorizing medical illness as minor, moderate, severe, and critical (see Table 3).3 For noncritical illness, they recommended continuation of standard replacement therapy with an additional, once-daily dose, which varied according to illness severity.
Cooper and Stewart conducted a similar review, basing their guidelines on a categorization of mild, moderate, severe/critical, or septic shock. These guidelines recommended a total daily dose of glucocorticoid supplementation, rather than an addition of a single dose to current therapy. They also stated that the least severe category of illness (defined as mild) did not require any change to a patient’s regular therapy.4
Jung et al classified illness as minimal, minor, moderate, severe, and critical.9 Under these guidelines, supplemental therapy was not advised for minimal (nonfebrile) illness. Moderate illness, including cellulitis, warranted a doubling or tripling of the outpatient dose until recovery, which was consistent with prior expert recommendation. More severe illness warranted intravenous administration of steroids.
Back to the Case
The patient had a mild case of cellulitis, classified by most experts as moderate illness, which responded well to vancomycin. Her outpatient glucocorticoid dose was doubled on admission and administered orally for the duration of her hospitalization, as she had no further episodes of vomiting or diarrhea.
Review of the patient’s records from prior hospitalizations and ambulatory visits revealed that her systolic blood pressure typically ran in the 80 mmHg to 100 mmHg range. Following initial volume resuscitation, her systolic blood pressure remained in the 90-100 mmHg range.
She was discharged home in stable condition, with instructions to complete a course of oral trimethoprim/sulfamethoxazole, resume her baseline dose of hydrocortisone the day after discharge, and follow up with her PCP for further monitoring and adjustment of her adrenal replacement therapy.
Bottom Line
For adults with adrenal insufficiency hospitalized with noncritical, nonsurgical illness, the expert recommendation is to double or triple the usual outpatient dose of glucocorticoid; however, data to support this is limited, and each patient should be assessed carefully and monitored to determine the optimal dose adjustment. TH
Dr. Shaw is a resident in the Department of Medicine at the University of Washington School of Medicine in Seattle. Dr. Best is an assistant professor of medicine in the division of general internal medicine, University of Washington School of Medicine.
References
- Arlt W. The approach to the adult with newly diagnosed adrenal insufficiency. J Clin Endocrinol Metab. 2009;94(4):1059-1067.
- Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003; 361:1881-1893.
- Coursin DB, Wood KE. Corticosteroid supplementation for adrenal insufficiency. JAMA. 2002;287:236-240.
- Cooper MS, Stewart PM. Corticosteroid insufficiency in acutely ill patients. N Engl J Med. 2003;348:727-734.
- Hahner S, Allolio B. Therapeutic management of adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23:167-179.
- Hahner S, Loeffler M, Bleicken B, et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies. Eur J Endocrinol. 2010;162:597:602.
- White K, Arlt W. Adrenal crisis in treated Addison’s disease: a predictable but under-managed event. Eur J Endocrinol. 2010;162:115-120.
- Omori K, Nomura K, Shimizu S, Omori N, Takano K. Risk factors for adrenal crises in patients with adrenal insufficiency. Endocr J. 2003;50:745-752.
- Jung C, Inder WJ. Management of adrenal insufficiency during the stress of medical illness and surgery. Med J Aust. 2008;188:409-413.
- Crown A, Lightman S. Why is the management of glucocorticoid deficiency still controversial: a review of the literature. Clin Endocrinol. 2005;63:483-492.