User login
Which comorbidities most diminish quality of life in patients with MS?
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
DALLAS – (MS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. In addition, comorbidities account for about 18% of the variance in health-related quality of life, and a higher number of comorbidities correlates with lower health-related quality of life in a “clear dose–response” manner, the researchers said.
The “magnitude of effect emphasizes the need for recognition and appropriate management of comorbidities,” said presenting author Lara Marie Pangan Lo, a researcher at Menzies Institute for Medical Research at the University of Tasmania, Australia, and her research colleagues. “The individual effect sizes may assist with the prioritizing of comorbidities that require more or less aggressive treatment in order to minimize” their impact.
Prior studies have found that patients with MS have lower health-related quality of life, compared with the general population, and that comorbidities affect patients’ quality of life, but few studies have looked at the effects of individual comorbidities on quality of life, Ms. Lo and her colleagues said. To examine the total impact and relative importance of comorbidities on psychosocial, physical, and overall health-related quality of life in people with MS, the investigators analyzed survey data from 902 participants in the survey-based Australian MS Longitudinal Study. They used linear regression and dominance analysis to assess relationships between comorbidities and participants’ Assessment of Quality of Life-8 Dimensions scores, which can range from 0 (death) to 1 (perfect health).
The predicted health-related quality of life for patients without comorbidities was 0.74. After the researchers adjusted for age, sex, and education, they found that systemic lupus erythematosus (reported by 1.56% of patients), depression (41.25%), hyperthyroidism (3.01%), and anxiety (38.35%) were associated with the greatest estimated decreases in health-related quality of life (–0.16, –0.15, –0.12, and –0.11, respectively). Depression and anxiety had the largest effect on psychosocial health–related quality of life, whereas systemic lupus erythematosus, rheumatoid arthritis, and hyperthyroidism had the largest impact on physical health–related quality of life. Other comorbidities that significantly correlated with quality of life included osteoporosis, type 2 diabetes, migraine, and inflammatory bowel disease.
The study was supported by Multiple Sclerosis Research Australia. The authors had no relevant disclosures.
SOURCE: Lo LMP et al. ACTRIMS Forum 2019, Abstract 80.
REPORTING FROM ACTRIMS FORUM 2019
Evaluations for possible MS often turn up one of its many mimics
DALLAS – Of 95 patients referred to two multiple sclerosis (MS) centers for a possible diagnosis of MS, 74% did not have MS, according to a study presented at ACTRIMS Forum 2019. A majority had clinical syndromes or imaging findings that are atypical for MS, which “underscores the importance of familiarity with typical MS clinical and imaging findings in avoiding misdiagnosis,” said Marwa Kaisey, MD, and her research colleagues. Dr. Kaisey is a neurologist at Cedars-Sinai Medical Center in Los Angeles.
Physicians often refer patients to academic MS centers to determine whether patients have MS or one of its many mimics. To study the characteristics and final diagnoses of patients referred to MS centers for evaluation of possible MS, the investigators reviewed electronic medical records and MRI from all new patient evaluations at the Cedars-Sinai Medical Center and University of California, Los Angeles MS clinics between July 2016 and June 2017. The researchers excluded patients referred with a previously established diagnosis of MS.
There were 366 new patients evaluated, including 236 patients with previously established MS diagnoses and 35 patients whose evaluations were not related to MS. Of the 95 patients referred for a question of MS diagnosis, 60% had clinical syndromes that were atypical for MS, 22% had normal neurologic exams, and a third had pain or sensory changes that were not localizable to the CNS.
Sixty-seven percent had MRI that was atypical for MS, and nearly half of the patients without MS had nonspecific MRI changes. “Often, these MRI changes alone prompted referral for an MS evaluation,” Dr. Kaisey and colleagues reported. “This suggests that novel, specific imaging tools may increase diagnostic confidence in the clinical setting.”
In all, the referred patients received 28 diagnoses other than MS, most commonly migraine (10 patients), anxiety or conversion disorder (9), postinfectious or idiopathic transverse myelitis (8), compression myelopathy or spondylopathy (8), and peripheral neuropathy or radiculopathy (7).
The researchers did not have any relevant disclosures.
SOURCE: Kaisey M et al. ACTRIMS Forum 2019, Abstract 90.
DALLAS – Of 95 patients referred to two multiple sclerosis (MS) centers for a possible diagnosis of MS, 74% did not have MS, according to a study presented at ACTRIMS Forum 2019. A majority had clinical syndromes or imaging findings that are atypical for MS, which “underscores the importance of familiarity with typical MS clinical and imaging findings in avoiding misdiagnosis,” said Marwa Kaisey, MD, and her research colleagues. Dr. Kaisey is a neurologist at Cedars-Sinai Medical Center in Los Angeles.
Physicians often refer patients to academic MS centers to determine whether patients have MS or one of its many mimics. To study the characteristics and final diagnoses of patients referred to MS centers for evaluation of possible MS, the investigators reviewed electronic medical records and MRI from all new patient evaluations at the Cedars-Sinai Medical Center and University of California, Los Angeles MS clinics between July 2016 and June 2017. The researchers excluded patients referred with a previously established diagnosis of MS.
There were 366 new patients evaluated, including 236 patients with previously established MS diagnoses and 35 patients whose evaluations were not related to MS. Of the 95 patients referred for a question of MS diagnosis, 60% had clinical syndromes that were atypical for MS, 22% had normal neurologic exams, and a third had pain or sensory changes that were not localizable to the CNS.
Sixty-seven percent had MRI that was atypical for MS, and nearly half of the patients without MS had nonspecific MRI changes. “Often, these MRI changes alone prompted referral for an MS evaluation,” Dr. Kaisey and colleagues reported. “This suggests that novel, specific imaging tools may increase diagnostic confidence in the clinical setting.”
In all, the referred patients received 28 diagnoses other than MS, most commonly migraine (10 patients), anxiety or conversion disorder (9), postinfectious or idiopathic transverse myelitis (8), compression myelopathy or spondylopathy (8), and peripheral neuropathy or radiculopathy (7).
The researchers did not have any relevant disclosures.
SOURCE: Kaisey M et al. ACTRIMS Forum 2019, Abstract 90.
DALLAS – Of 95 patients referred to two multiple sclerosis (MS) centers for a possible diagnosis of MS, 74% did not have MS, according to a study presented at ACTRIMS Forum 2019. A majority had clinical syndromes or imaging findings that are atypical for MS, which “underscores the importance of familiarity with typical MS clinical and imaging findings in avoiding misdiagnosis,” said Marwa Kaisey, MD, and her research colleagues. Dr. Kaisey is a neurologist at Cedars-Sinai Medical Center in Los Angeles.
Physicians often refer patients to academic MS centers to determine whether patients have MS or one of its many mimics. To study the characteristics and final diagnoses of patients referred to MS centers for evaluation of possible MS, the investigators reviewed electronic medical records and MRI from all new patient evaluations at the Cedars-Sinai Medical Center and University of California, Los Angeles MS clinics between July 2016 and June 2017. The researchers excluded patients referred with a previously established diagnosis of MS.
There were 366 new patients evaluated, including 236 patients with previously established MS diagnoses and 35 patients whose evaluations were not related to MS. Of the 95 patients referred for a question of MS diagnosis, 60% had clinical syndromes that were atypical for MS, 22% had normal neurologic exams, and a third had pain or sensory changes that were not localizable to the CNS.
Sixty-seven percent had MRI that was atypical for MS, and nearly half of the patients without MS had nonspecific MRI changes. “Often, these MRI changes alone prompted referral for an MS evaluation,” Dr. Kaisey and colleagues reported. “This suggests that novel, specific imaging tools may increase diagnostic confidence in the clinical setting.”
In all, the referred patients received 28 diagnoses other than MS, most commonly migraine (10 patients), anxiety or conversion disorder (9), postinfectious or idiopathic transverse myelitis (8), compression myelopathy or spondylopathy (8), and peripheral neuropathy or radiculopathy (7).
The researchers did not have any relevant disclosures.
SOURCE: Kaisey M et al. ACTRIMS Forum 2019, Abstract 90.
REPORTING FROM ACTRIMS FORUM 2019
Migraine associated with more severe disability in patients with MS
DALLAS – researchers reported at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Traditional migraine risk factors such as obesity, anxiety, and depression were also overrepresented in our cohort” of patients with multiple sclerosis (MS) and migraine, said Anne M. Damian, MD, of Johns Hopkins University, Baltimore, and her research colleagues.
Migraine is common in patients with MS, but whether migraine plays a role in MS disease course or MS symptom severity is unknown. Dr. Damian and her colleagues conducted an observational study to examine the associations between migraine history, disability, and neurologic function in patients with MS and whether migraine tends to occur with other comorbid conditions in MS.
They analyzed data from 289 patients (79% female; mean age, 49.2 years) patients with MS who completed the Multiple Sclerosis Performance Test (MSPT), an iPad version of the MS Functional Composite. MS outcome measures included disability (such as the Patient Determined Disease Steps) and objective neurologic outcomes (such as walking speed, manual dexterity, and processing speed). Patients also completed a questionnaire about comorbidities, including history of physician-diagnosed migraine, diabetes, hypertension, hypercholesterolemia, heart disease, sleep apnea, depression, and anxiety.
The researchers used generalized linear models adjusted for age, sex, MS subtype, MS duration, years of education, and body mass index to evaluate the association between history of migraine and MS outcomes.
Compared with patients with MS without migraine, migraineurs (n = 65) tended to be younger (mean age, 44.3 years vs. 50.4 years) and were more likely to be overweight or obese (73.9% vs. 51.6%). In addition, patients with MS and migraine were more likely to have a history of depression (46.2% vs. 24.2%), anxiety (30.8% vs. 18.8%), and severe rather than mild disability (odds ratio, 3.08; 95% confidence, 1.04-9.20). Migraine also was associated with significantly slower walking speeds (9.08% slower; 95% CI, 0.82%-18.77%). Migraine was not associated with processing speed or manual dexterity, however.
If an association between migraine history and worse MS disability is confirmed, migraine history may be a factor that neurologists could consider when making MS treatment decisions, Dr. Damian said. The researchers noted that migraine was reported by patients and not detected using a validated questionnaire. Future studies should investigate whether MS lesions on MRI differ in migraineurs and whether migraine predicts future neurologic disability in patients with MS.
Collection of the MSPT outcomes was sponsored by Biogen.
SOURCE: Damian AM et al. ACTRIMS Forum 2019, Abstract 78.
DALLAS – researchers reported at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Traditional migraine risk factors such as obesity, anxiety, and depression were also overrepresented in our cohort” of patients with multiple sclerosis (MS) and migraine, said Anne M. Damian, MD, of Johns Hopkins University, Baltimore, and her research colleagues.
Migraine is common in patients with MS, but whether migraine plays a role in MS disease course or MS symptom severity is unknown. Dr. Damian and her colleagues conducted an observational study to examine the associations between migraine history, disability, and neurologic function in patients with MS and whether migraine tends to occur with other comorbid conditions in MS.
They analyzed data from 289 patients (79% female; mean age, 49.2 years) patients with MS who completed the Multiple Sclerosis Performance Test (MSPT), an iPad version of the MS Functional Composite. MS outcome measures included disability (such as the Patient Determined Disease Steps) and objective neurologic outcomes (such as walking speed, manual dexterity, and processing speed). Patients also completed a questionnaire about comorbidities, including history of physician-diagnosed migraine, diabetes, hypertension, hypercholesterolemia, heart disease, sleep apnea, depression, and anxiety.
The researchers used generalized linear models adjusted for age, sex, MS subtype, MS duration, years of education, and body mass index to evaluate the association between history of migraine and MS outcomes.
Compared with patients with MS without migraine, migraineurs (n = 65) tended to be younger (mean age, 44.3 years vs. 50.4 years) and were more likely to be overweight or obese (73.9% vs. 51.6%). In addition, patients with MS and migraine were more likely to have a history of depression (46.2% vs. 24.2%), anxiety (30.8% vs. 18.8%), and severe rather than mild disability (odds ratio, 3.08; 95% confidence, 1.04-9.20). Migraine also was associated with significantly slower walking speeds (9.08% slower; 95% CI, 0.82%-18.77%). Migraine was not associated with processing speed or manual dexterity, however.
If an association between migraine history and worse MS disability is confirmed, migraine history may be a factor that neurologists could consider when making MS treatment decisions, Dr. Damian said. The researchers noted that migraine was reported by patients and not detected using a validated questionnaire. Future studies should investigate whether MS lesions on MRI differ in migraineurs and whether migraine predicts future neurologic disability in patients with MS.
Collection of the MSPT outcomes was sponsored by Biogen.
SOURCE: Damian AM et al. ACTRIMS Forum 2019, Abstract 78.
DALLAS – researchers reported at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
“Traditional migraine risk factors such as obesity, anxiety, and depression were also overrepresented in our cohort” of patients with multiple sclerosis (MS) and migraine, said Anne M. Damian, MD, of Johns Hopkins University, Baltimore, and her research colleagues.
Migraine is common in patients with MS, but whether migraine plays a role in MS disease course or MS symptom severity is unknown. Dr. Damian and her colleagues conducted an observational study to examine the associations between migraine history, disability, and neurologic function in patients with MS and whether migraine tends to occur with other comorbid conditions in MS.
They analyzed data from 289 patients (79% female; mean age, 49.2 years) patients with MS who completed the Multiple Sclerosis Performance Test (MSPT), an iPad version of the MS Functional Composite. MS outcome measures included disability (such as the Patient Determined Disease Steps) and objective neurologic outcomes (such as walking speed, manual dexterity, and processing speed). Patients also completed a questionnaire about comorbidities, including history of physician-diagnosed migraine, diabetes, hypertension, hypercholesterolemia, heart disease, sleep apnea, depression, and anxiety.
The researchers used generalized linear models adjusted for age, sex, MS subtype, MS duration, years of education, and body mass index to evaluate the association between history of migraine and MS outcomes.
Compared with patients with MS without migraine, migraineurs (n = 65) tended to be younger (mean age, 44.3 years vs. 50.4 years) and were more likely to be overweight or obese (73.9% vs. 51.6%). In addition, patients with MS and migraine were more likely to have a history of depression (46.2% vs. 24.2%), anxiety (30.8% vs. 18.8%), and severe rather than mild disability (odds ratio, 3.08; 95% confidence, 1.04-9.20). Migraine also was associated with significantly slower walking speeds (9.08% slower; 95% CI, 0.82%-18.77%). Migraine was not associated with processing speed or manual dexterity, however.
If an association between migraine history and worse MS disability is confirmed, migraine history may be a factor that neurologists could consider when making MS treatment decisions, Dr. Damian said. The researchers noted that migraine was reported by patients and not detected using a validated questionnaire. Future studies should investigate whether MS lesions on MRI differ in migraineurs and whether migraine predicts future neurologic disability in patients with MS.
Collection of the MSPT outcomes was sponsored by Biogen.
SOURCE: Damian AM et al. ACTRIMS Forum 2019, Abstract 78.
REPORTING FROM ACTRIMS FORUM 2019
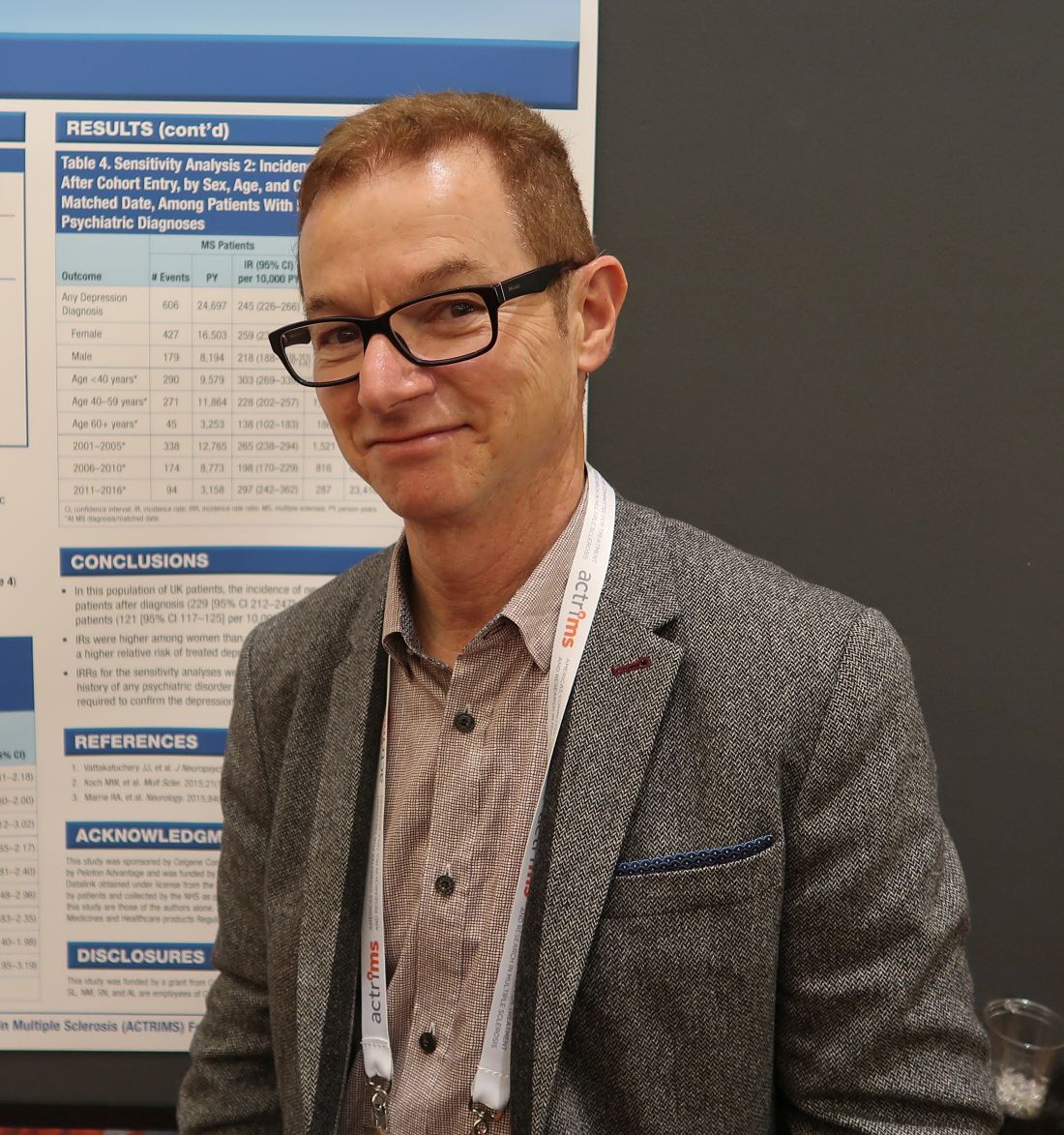
Incidence of treated depression nearly 100% higher in patients with MS
DALLAS – according to an analysis of data from patients in the United Kingdom.
After a diagnosis of MS, the incidence of new treated depression is 229 per 10,000 person-years. In comparison, the incidence of new treated depression among matched patients without MS is 121 per 10,000 person-years, Neil Minton, MD, drug safety head at Celgene, reported at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
MS causes changes in the CNS that are associated with depression, but “data on rates of incident depression after MS diagnosis ... are limited,” Dr. Minton and his research colleagues said. To examine rates of treated incident depression in patients with MS after an MS diagnosis, compared with rates in a matched population of patients without MS, the researchers analyzed data from the U.K. Clinical Practice Research Datalink.
Their analysis included patients with MS who received a diagnosis of MS between 2001 and 2016, had at least 1 year of history available before the MS diagnosis, and had no history of treated depression. The researchers matched these patients with as many as 10 patients without MS by age, sex, general practice, record history length, and no history of treated depression. Treated depression was defined as a diagnosis code for depression and a prescription for an antidepressant treatment within 90 days. They used Byar’s method to estimate incidence rates and incidence rate ratios, the Kaplan-Meier method to generate cumulative incidence curves, and a log-rank test to compare the curves.
In all, 5,456 patients with MS and 45,712 matched patients without MS were included in the study. Patients’ median age was 42 years; 65% were female. Compared with patients without MS, patients with MS were more likely to have a history of untreated depression (9.6% vs. 7.5%) and to have received an antidepressant treatment for any indication before cohort entry (28.0% vs. 15.5%). Diagnoses for other psychiatric conditions were similar between the groups.
Incidence rates of treated depression were higher among women with MS, compared with men with MS – 241 versus 202 per 10,000 person-years. Compared with patients without MS, however, men with MS had a higher relative risk of treated depression (2.40 vs. 1.73).
The incidence rate ratios were similar in sensitivity analyses that excluded patients with a history of any psychiatric disorder at cohort entry and that did not require treatment to confirm a depression diagnosis.
The study was funded by a grant from Celgene.
SOURCE: Minton N et al. ACTRIMS Forum 2019, Abstract 82.
DALLAS – according to an analysis of data from patients in the United Kingdom.
After a diagnosis of MS, the incidence of new treated depression is 229 per 10,000 person-years. In comparison, the incidence of new treated depression among matched patients without MS is 121 per 10,000 person-years, Neil Minton, MD, drug safety head at Celgene, reported at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
MS causes changes in the CNS that are associated with depression, but “data on rates of incident depression after MS diagnosis ... are limited,” Dr. Minton and his research colleagues said. To examine rates of treated incident depression in patients with MS after an MS diagnosis, compared with rates in a matched population of patients without MS, the researchers analyzed data from the U.K. Clinical Practice Research Datalink.
Their analysis included patients with MS who received a diagnosis of MS between 2001 and 2016, had at least 1 year of history available before the MS diagnosis, and had no history of treated depression. The researchers matched these patients with as many as 10 patients without MS by age, sex, general practice, record history length, and no history of treated depression. Treated depression was defined as a diagnosis code for depression and a prescription for an antidepressant treatment within 90 days. They used Byar’s method to estimate incidence rates and incidence rate ratios, the Kaplan-Meier method to generate cumulative incidence curves, and a log-rank test to compare the curves.
In all, 5,456 patients with MS and 45,712 matched patients without MS were included in the study. Patients’ median age was 42 years; 65% were female. Compared with patients without MS, patients with MS were more likely to have a history of untreated depression (9.6% vs. 7.5%) and to have received an antidepressant treatment for any indication before cohort entry (28.0% vs. 15.5%). Diagnoses for other psychiatric conditions were similar between the groups.
Incidence rates of treated depression were higher among women with MS, compared with men with MS – 241 versus 202 per 10,000 person-years. Compared with patients without MS, however, men with MS had a higher relative risk of treated depression (2.40 vs. 1.73).
The incidence rate ratios were similar in sensitivity analyses that excluded patients with a history of any psychiatric disorder at cohort entry and that did not require treatment to confirm a depression diagnosis.
The study was funded by a grant from Celgene.
SOURCE: Minton N et al. ACTRIMS Forum 2019, Abstract 82.
DALLAS – according to an analysis of data from patients in the United Kingdom.
After a diagnosis of MS, the incidence of new treated depression is 229 per 10,000 person-years. In comparison, the incidence of new treated depression among matched patients without MS is 121 per 10,000 person-years, Neil Minton, MD, drug safety head at Celgene, reported at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
MS causes changes in the CNS that are associated with depression, but “data on rates of incident depression after MS diagnosis ... are limited,” Dr. Minton and his research colleagues said. To examine rates of treated incident depression in patients with MS after an MS diagnosis, compared with rates in a matched population of patients without MS, the researchers analyzed data from the U.K. Clinical Practice Research Datalink.
Their analysis included patients with MS who received a diagnosis of MS between 2001 and 2016, had at least 1 year of history available before the MS diagnosis, and had no history of treated depression. The researchers matched these patients with as many as 10 patients without MS by age, sex, general practice, record history length, and no history of treated depression. Treated depression was defined as a diagnosis code for depression and a prescription for an antidepressant treatment within 90 days. They used Byar’s method to estimate incidence rates and incidence rate ratios, the Kaplan-Meier method to generate cumulative incidence curves, and a log-rank test to compare the curves.
In all, 5,456 patients with MS and 45,712 matched patients without MS were included in the study. Patients’ median age was 42 years; 65% were female. Compared with patients without MS, patients with MS were more likely to have a history of untreated depression (9.6% vs. 7.5%) and to have received an antidepressant treatment for any indication before cohort entry (28.0% vs. 15.5%). Diagnoses for other psychiatric conditions were similar between the groups.
Incidence rates of treated depression were higher among women with MS, compared with men with MS – 241 versus 202 per 10,000 person-years. Compared with patients without MS, however, men with MS had a higher relative risk of treated depression (2.40 vs. 1.73).
The incidence rate ratios were similar in sensitivity analyses that excluded patients with a history of any psychiatric disorder at cohort entry and that did not require treatment to confirm a depression diagnosis.
The study was funded by a grant from Celgene.
SOURCE: Minton N et al. ACTRIMS Forum 2019, Abstract 82.
REPORTING FROM ACTRIMS FORUM 2019
Can technology automate assessments of patients with MS in the clinic?
DALLAS – according to research described at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
An analysis of data collected using these methods found that patient-reported outcomes and MRI measures correlate with neuroperformance test results, said Laura Baldassari, MD, a clinical neuroimmunology fellow at the Mellen Center for Multiple Sclerosis at the Cleveland Clinic. Such assessments “could potentially enable us to better tune in to disability worsening and treatment response in our patients.”
The Multiple Sclerosis Performance Test (MSPT) collects patient-reported outcomes and tests patients’ processing speed, contrast sensitivity, manual dexterity, and walking speed. The MSPT is designed for supervised or independent administration with an assistant and has been “incorporated into routine clinical care at the Mellen Center,” Dr. Baldassari said. Before seeing their provider, patients complete the MSPT with a biomedical assistant, which usually takes 30-40 minutes. The data are scored instantly and “integrated into the electronic medical record for use during the clinical encounter.”
Dr. Baldassari and her research colleagues analyzed associations between the neuroperformance metrics, patient-reported outcome measures, and quantitative MRI metrics. The analysis included 976 patients who completed the MSPT between December 2015 and December 2017 and had an MRI within 3 months of a clinical encounter. T2 lesion volume, normalized whole brain volume or whole brain fraction, thalamic volume, and cross-sectional upper cervical spinal cord area at the level of C2 on MRI were calculated using a fully automated method.
Patient-reported outcomes included Quality of Life in Neurological Disorders (Neuro-QoL) upper and lower extremity function, Patient-Reported Outcomes Measurement Information System (PROMIS) physical, and Patient Determined Disease Steps (PDDS).
The researchers used Spearman correlation coefficients to examine the relationships between each neuroperformance test, patient-reported outcome, and MRI measure. Linear regression models determined which clinical demographic, patient-reported outcome, or MRI characteristic predicted neuroperformance test results.
Patients had a mean age of about 48 years, and the population was predominantly female and white with relapsing remitting MS.
“There were significant correlations between all neuroperformance tests and all patient-reported outcomes except for the contrast sensitivity test and PROMIS physical,” Dr. Baldassari said. “The processing speed test was most strongly correlated with the PDDS as well as the Neuro-QoL lower extremity. The contrast sensitivity test was correlated with Neuro-QoL lower extremity as well.” The manual dexterity test correlated with PDDS and Neuro-QoL upper and lower extremity and the walking speed test correlated with PDDS and Neuro-QoL lower extremity.
“With worsening self-reported functions, these neuroperformance test results demonstrated impairment as well,” she said.
The neuroperformance tests and all MRI metrics had significant, moderate correlations. “The strongest correlations here are between the processing speed test and whole brain fraction and T2 lesion volume; contrast sensitivity and T2 lesion volume, whole brain fraction, and thalamic volume; manual dexterity test and T2 lesion volume and whole brain fraction; and walking speed test and whole brain fraction and cord area,” she said.
“The strongest predictors of each neuroperformance test varied, which highlights the unique complementary contribution of each patient-reported outcome measure and MRI metric to the complex domains of disability in MS,” Dr. Baldassari said.
Comprehensive, quantitative MS assessments may lead to detailed patient profiles, which could support more precise clinical care and observational studies. In future studies, the researchers plan to examine how these measures relate over time.
The MSPT was developed by the Cleveland Clinic in partnership with Biogen. Dr. Baldassari reported receiving funding through the National Multiple Sclerosis Society and personal fees for serving on a scientific advisory board for Teva. His coauthors’ disclosures included the contribution of intellectual property to the MSPT, for which they could receive royalties.
SOURCE: Baldassari L et al. ACTRIMS Forum 2019, Abstract 32.
DALLAS – according to research described at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
An analysis of data collected using these methods found that patient-reported outcomes and MRI measures correlate with neuroperformance test results, said Laura Baldassari, MD, a clinical neuroimmunology fellow at the Mellen Center for Multiple Sclerosis at the Cleveland Clinic. Such assessments “could potentially enable us to better tune in to disability worsening and treatment response in our patients.”
The Multiple Sclerosis Performance Test (MSPT) collects patient-reported outcomes and tests patients’ processing speed, contrast sensitivity, manual dexterity, and walking speed. The MSPT is designed for supervised or independent administration with an assistant and has been “incorporated into routine clinical care at the Mellen Center,” Dr. Baldassari said. Before seeing their provider, patients complete the MSPT with a biomedical assistant, which usually takes 30-40 minutes. The data are scored instantly and “integrated into the electronic medical record for use during the clinical encounter.”
Dr. Baldassari and her research colleagues analyzed associations between the neuroperformance metrics, patient-reported outcome measures, and quantitative MRI metrics. The analysis included 976 patients who completed the MSPT between December 2015 and December 2017 and had an MRI within 3 months of a clinical encounter. T2 lesion volume, normalized whole brain volume or whole brain fraction, thalamic volume, and cross-sectional upper cervical spinal cord area at the level of C2 on MRI were calculated using a fully automated method.
Patient-reported outcomes included Quality of Life in Neurological Disorders (Neuro-QoL) upper and lower extremity function, Patient-Reported Outcomes Measurement Information System (PROMIS) physical, and Patient Determined Disease Steps (PDDS).
The researchers used Spearman correlation coefficients to examine the relationships between each neuroperformance test, patient-reported outcome, and MRI measure. Linear regression models determined which clinical demographic, patient-reported outcome, or MRI characteristic predicted neuroperformance test results.
Patients had a mean age of about 48 years, and the population was predominantly female and white with relapsing remitting MS.
“There were significant correlations between all neuroperformance tests and all patient-reported outcomes except for the contrast sensitivity test and PROMIS physical,” Dr. Baldassari said. “The processing speed test was most strongly correlated with the PDDS as well as the Neuro-QoL lower extremity. The contrast sensitivity test was correlated with Neuro-QoL lower extremity as well.” The manual dexterity test correlated with PDDS and Neuro-QoL upper and lower extremity and the walking speed test correlated with PDDS and Neuro-QoL lower extremity.
“With worsening self-reported functions, these neuroperformance test results demonstrated impairment as well,” she said.
The neuroperformance tests and all MRI metrics had significant, moderate correlations. “The strongest correlations here are between the processing speed test and whole brain fraction and T2 lesion volume; contrast sensitivity and T2 lesion volume, whole brain fraction, and thalamic volume; manual dexterity test and T2 lesion volume and whole brain fraction; and walking speed test and whole brain fraction and cord area,” she said.
“The strongest predictors of each neuroperformance test varied, which highlights the unique complementary contribution of each patient-reported outcome measure and MRI metric to the complex domains of disability in MS,” Dr. Baldassari said.
Comprehensive, quantitative MS assessments may lead to detailed patient profiles, which could support more precise clinical care and observational studies. In future studies, the researchers plan to examine how these measures relate over time.
The MSPT was developed by the Cleveland Clinic in partnership with Biogen. Dr. Baldassari reported receiving funding through the National Multiple Sclerosis Society and personal fees for serving on a scientific advisory board for Teva. His coauthors’ disclosures included the contribution of intellectual property to the MSPT, for which they could receive royalties.
SOURCE: Baldassari L et al. ACTRIMS Forum 2019, Abstract 32.
DALLAS – according to research described at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
An analysis of data collected using these methods found that patient-reported outcomes and MRI measures correlate with neuroperformance test results, said Laura Baldassari, MD, a clinical neuroimmunology fellow at the Mellen Center for Multiple Sclerosis at the Cleveland Clinic. Such assessments “could potentially enable us to better tune in to disability worsening and treatment response in our patients.”
The Multiple Sclerosis Performance Test (MSPT) collects patient-reported outcomes and tests patients’ processing speed, contrast sensitivity, manual dexterity, and walking speed. The MSPT is designed for supervised or independent administration with an assistant and has been “incorporated into routine clinical care at the Mellen Center,” Dr. Baldassari said. Before seeing their provider, patients complete the MSPT with a biomedical assistant, which usually takes 30-40 minutes. The data are scored instantly and “integrated into the electronic medical record for use during the clinical encounter.”
Dr. Baldassari and her research colleagues analyzed associations between the neuroperformance metrics, patient-reported outcome measures, and quantitative MRI metrics. The analysis included 976 patients who completed the MSPT between December 2015 and December 2017 and had an MRI within 3 months of a clinical encounter. T2 lesion volume, normalized whole brain volume or whole brain fraction, thalamic volume, and cross-sectional upper cervical spinal cord area at the level of C2 on MRI were calculated using a fully automated method.
Patient-reported outcomes included Quality of Life in Neurological Disorders (Neuro-QoL) upper and lower extremity function, Patient-Reported Outcomes Measurement Information System (PROMIS) physical, and Patient Determined Disease Steps (PDDS).
The researchers used Spearman correlation coefficients to examine the relationships between each neuroperformance test, patient-reported outcome, and MRI measure. Linear regression models determined which clinical demographic, patient-reported outcome, or MRI characteristic predicted neuroperformance test results.
Patients had a mean age of about 48 years, and the population was predominantly female and white with relapsing remitting MS.
“There were significant correlations between all neuroperformance tests and all patient-reported outcomes except for the contrast sensitivity test and PROMIS physical,” Dr. Baldassari said. “The processing speed test was most strongly correlated with the PDDS as well as the Neuro-QoL lower extremity. The contrast sensitivity test was correlated with Neuro-QoL lower extremity as well.” The manual dexterity test correlated with PDDS and Neuro-QoL upper and lower extremity and the walking speed test correlated with PDDS and Neuro-QoL lower extremity.
“With worsening self-reported functions, these neuroperformance test results demonstrated impairment as well,” she said.
The neuroperformance tests and all MRI metrics had significant, moderate correlations. “The strongest correlations here are between the processing speed test and whole brain fraction and T2 lesion volume; contrast sensitivity and T2 lesion volume, whole brain fraction, and thalamic volume; manual dexterity test and T2 lesion volume and whole brain fraction; and walking speed test and whole brain fraction and cord area,” she said.
“The strongest predictors of each neuroperformance test varied, which highlights the unique complementary contribution of each patient-reported outcome measure and MRI metric to the complex domains of disability in MS,” Dr. Baldassari said.
Comprehensive, quantitative MS assessments may lead to detailed patient profiles, which could support more precise clinical care and observational studies. In future studies, the researchers plan to examine how these measures relate over time.
The MSPT was developed by the Cleveland Clinic in partnership with Biogen. Dr. Baldassari reported receiving funding through the National Multiple Sclerosis Society and personal fees for serving on a scientific advisory board for Teva. His coauthors’ disclosures included the contribution of intellectual property to the MSPT, for which they could receive royalties.
SOURCE: Baldassari L et al. ACTRIMS Forum 2019, Abstract 32.
REPORTING FROM ACTRIMS FORUM 2019
Ublituximab depletes B cells in phase 2 trial
DALLAS – (MS), according to phase 2 trial results presented at ACTRIMS Forum 2019. Patients treated with the investigational therapy had reduced MRI activity and relapse rates during the 48-week trial, and the treatment was well tolerated, researchers said.
The monoclonal antibody targets a unique epitope on the CD20 antigen and is glycoengineered for enhanced B-cell targeting through antibody-dependent cellular cytotoxicity, said presenting author Edward Fox, MD, PhD, director of the MS Clinic of Central Texas, Round Rock. Ublituximab’s potency “may offer a benefit over currently available anti-CD20s in terms of lower doses and shorter infusion times,” Dr. Fox and his research colleagues said.
To assess the optimal dose, infusion time, safety, and tolerability of ublituximab in relapsing MS, investigators conducted a phase 2, multicenter study. The trial included 48 patients with relapsing MS; 65% were female. Patients’ average age was 40 years and average disease duration was 7.7 years. The researchers included patients with one or more confirmed relapse in the past year, two relapses in the past 2 years, or at least one active gadolinium-enhancing T1 lesion. The primary endpoint was the percentage of patients with at least a 95% reduction in peripheral CD19+ B cells within 2 weeks after the second infusion on day 15.
For their first infusions, patients received 150 mg of ublituximab over an infusion time of 1, 2, 3, or 4 hours. On day 15, patients received 450 mg or 600 mg of ublituximab over an infusion time of 1, 1.5, or 3 hours. At week 24, patients received 450 mg or 650 mg of ublituximab infused over 1 hour or 1.5 hours.
All patients met the primary endpoint of greater than 95% B-cell depletion between baseline and week 4. Median B-cell depletion was 99% at week 4, and this effect was maintained at weeks 24 and 48.
The researchers detected no T1 gadolinium-enhancing lesions at week 24 or week 48, and total T2 lesion volume decreased by 10.6% between baseline and week 48.
The most frequent adverse events were infusion-related reactions, which occurred in 48% of patients and were more common with the first infusion, particularly when the infusion time was less than 4 hours. All of the infusion-related reactions were grade 1 or 2. One grade 3 serious adverse event of fatigue was considered possibly related to ublituximab. No patients withdrew from the study because of drug-related adverse events. At week 48, 93% of the patients were relapse free, 7% had 24-week confirmed disability progression, and 17% had confirmed disability improvement.
TG Therapeutics, the company developing ublituximab, is evaluating the therapy in phase 3 trials known as ULTIMATE I and 2. The phase 3 trials are using the 450-mg dose with a first dose of 150 mg delivered over 4 hours.
Dr. Fox has disclosed research support from TG Therapeutics and other pharmaceutical companies and working as a consultant and speaker for TG Therapeutics and other companies.
SOURCE: Fox E et al. ACTRIMS Forum 2019, Abstract 66.
DALLAS – (MS), according to phase 2 trial results presented at ACTRIMS Forum 2019. Patients treated with the investigational therapy had reduced MRI activity and relapse rates during the 48-week trial, and the treatment was well tolerated, researchers said.
The monoclonal antibody targets a unique epitope on the CD20 antigen and is glycoengineered for enhanced B-cell targeting through antibody-dependent cellular cytotoxicity, said presenting author Edward Fox, MD, PhD, director of the MS Clinic of Central Texas, Round Rock. Ublituximab’s potency “may offer a benefit over currently available anti-CD20s in terms of lower doses and shorter infusion times,” Dr. Fox and his research colleagues said.
To assess the optimal dose, infusion time, safety, and tolerability of ublituximab in relapsing MS, investigators conducted a phase 2, multicenter study. The trial included 48 patients with relapsing MS; 65% were female. Patients’ average age was 40 years and average disease duration was 7.7 years. The researchers included patients with one or more confirmed relapse in the past year, two relapses in the past 2 years, or at least one active gadolinium-enhancing T1 lesion. The primary endpoint was the percentage of patients with at least a 95% reduction in peripheral CD19+ B cells within 2 weeks after the second infusion on day 15.
For their first infusions, patients received 150 mg of ublituximab over an infusion time of 1, 2, 3, or 4 hours. On day 15, patients received 450 mg or 600 mg of ublituximab over an infusion time of 1, 1.5, or 3 hours. At week 24, patients received 450 mg or 650 mg of ublituximab infused over 1 hour or 1.5 hours.
All patients met the primary endpoint of greater than 95% B-cell depletion between baseline and week 4. Median B-cell depletion was 99% at week 4, and this effect was maintained at weeks 24 and 48.
The researchers detected no T1 gadolinium-enhancing lesions at week 24 or week 48, and total T2 lesion volume decreased by 10.6% between baseline and week 48.
The most frequent adverse events were infusion-related reactions, which occurred in 48% of patients and were more common with the first infusion, particularly when the infusion time was less than 4 hours. All of the infusion-related reactions were grade 1 or 2. One grade 3 serious adverse event of fatigue was considered possibly related to ublituximab. No patients withdrew from the study because of drug-related adverse events. At week 48, 93% of the patients were relapse free, 7% had 24-week confirmed disability progression, and 17% had confirmed disability improvement.
TG Therapeutics, the company developing ublituximab, is evaluating the therapy in phase 3 trials known as ULTIMATE I and 2. The phase 3 trials are using the 450-mg dose with a first dose of 150 mg delivered over 4 hours.
Dr. Fox has disclosed research support from TG Therapeutics and other pharmaceutical companies and working as a consultant and speaker for TG Therapeutics and other companies.
SOURCE: Fox E et al. ACTRIMS Forum 2019, Abstract 66.
DALLAS – (MS), according to phase 2 trial results presented at ACTRIMS Forum 2019. Patients treated with the investigational therapy had reduced MRI activity and relapse rates during the 48-week trial, and the treatment was well tolerated, researchers said.
The monoclonal antibody targets a unique epitope on the CD20 antigen and is glycoengineered for enhanced B-cell targeting through antibody-dependent cellular cytotoxicity, said presenting author Edward Fox, MD, PhD, director of the MS Clinic of Central Texas, Round Rock. Ublituximab’s potency “may offer a benefit over currently available anti-CD20s in terms of lower doses and shorter infusion times,” Dr. Fox and his research colleagues said.
To assess the optimal dose, infusion time, safety, and tolerability of ublituximab in relapsing MS, investigators conducted a phase 2, multicenter study. The trial included 48 patients with relapsing MS; 65% were female. Patients’ average age was 40 years and average disease duration was 7.7 years. The researchers included patients with one or more confirmed relapse in the past year, two relapses in the past 2 years, or at least one active gadolinium-enhancing T1 lesion. The primary endpoint was the percentage of patients with at least a 95% reduction in peripheral CD19+ B cells within 2 weeks after the second infusion on day 15.
For their first infusions, patients received 150 mg of ublituximab over an infusion time of 1, 2, 3, or 4 hours. On day 15, patients received 450 mg or 600 mg of ublituximab over an infusion time of 1, 1.5, or 3 hours. At week 24, patients received 450 mg or 650 mg of ublituximab infused over 1 hour or 1.5 hours.
All patients met the primary endpoint of greater than 95% B-cell depletion between baseline and week 4. Median B-cell depletion was 99% at week 4, and this effect was maintained at weeks 24 and 48.
The researchers detected no T1 gadolinium-enhancing lesions at week 24 or week 48, and total T2 lesion volume decreased by 10.6% between baseline and week 48.
The most frequent adverse events were infusion-related reactions, which occurred in 48% of patients and were more common with the first infusion, particularly when the infusion time was less than 4 hours. All of the infusion-related reactions were grade 1 or 2. One grade 3 serious adverse event of fatigue was considered possibly related to ublituximab. No patients withdrew from the study because of drug-related adverse events. At week 48, 93% of the patients were relapse free, 7% had 24-week confirmed disability progression, and 17% had confirmed disability improvement.
TG Therapeutics, the company developing ublituximab, is evaluating the therapy in phase 3 trials known as ULTIMATE I and 2. The phase 3 trials are using the 450-mg dose with a first dose of 150 mg delivered over 4 hours.
Dr. Fox has disclosed research support from TG Therapeutics and other pharmaceutical companies and working as a consultant and speaker for TG Therapeutics and other companies.
SOURCE: Fox E et al. ACTRIMS Forum 2019, Abstract 66.
REPORTING FROM ACTRIMS FORUM 2019
CSF biomarker clusters correlate with MS severity
DALLAS – Patients with multiple sclerosis (MS) have elevated levels of specific clusters of cerebrospinal fluid (CSF) biomarkers related to astrocytes and microglia that correlated with disease severity in a blinded analysis of more than 1,000 proteins from the CSF of more than 400 patients with neuroimmunologic disease and healthy volunteers.
Previous studies have indicated that aberrant activation of astrocytes and microglia underlies disability progression in older patients with MS, but researchers have lacked biomarkers of these processes in living subjects. In a presentation at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, Ruturaj R. Masvekar, PhD, described developing biomarkers of CNS cell–specific processes and examining how they relate to MS disability progression. Dr. Masvekar, a researcher at the National Institute of Allergy and Infectious Diseases, and his coinvestigators used a modified DNA aptamer assay to measure proteins in the CSF of 431 patients with neuroimmunologic diseases and healthy volunteers, followed by variable cluster analysis and in vitro modeling to define 64 clusters of CSF biomarkers that relate to CNS cell types.
The study included 42 healthy donors, 20 patients with clinically isolated syndrome, 57 patients with noninflammatory neurologic disorders, 127 patients with relapsing-remitting MS, 72 patients with secondary progressive MS, and 113 patients with primary progressive MS. In a training cohort of 217 participants, the researchers assessed how biomarkers differed between the diagnostic categories. The researchers then validated the results in an independent cohort of 214 participants.
One astrocyte-related cluster (MMP7, SERPINA3, GZMA, and CLIC1) and one microglia-related cluster (DSG2 and TNFRSF25) was significantly elevated in all MS subgroups, compared with healthy controls and patients with noninflammatory neurologic disorders.
In addition, these clusters “significantly correlated with clinical measures of disability, CNS tissue destruction, and MS severity,” Dr. Masvekar said.
The microglial cluster was significantly elevated in all MS subgroups, whereas neuronal endothelial, astrocytic, and oligodendroglial biomarker clusters were elevated only in patients with progressive MS.
“Microglial activation is present in all stages of MS, while toxic astrogliosis increases with MS duration, concomitantly with neuronal and oligodendroglial degeneration,” Dr. Masvekar said. “Microglial activation and toxic astrogliosis likely partake in CNS tissue destruction and enhance MS severity.”
This study, which was recently published in Multiple Sclerosis and Related Disorders (2019 Feb;28:34-43), was supported by the intramural research program at NIAID.
SOURCE: Masvekar RR et al. ACTRIMS Forum 2019, Abstract 281.
DALLAS – Patients with multiple sclerosis (MS) have elevated levels of specific clusters of cerebrospinal fluid (CSF) biomarkers related to astrocytes and microglia that correlated with disease severity in a blinded analysis of more than 1,000 proteins from the CSF of more than 400 patients with neuroimmunologic disease and healthy volunteers.
Previous studies have indicated that aberrant activation of astrocytes and microglia underlies disability progression in older patients with MS, but researchers have lacked biomarkers of these processes in living subjects. In a presentation at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, Ruturaj R. Masvekar, PhD, described developing biomarkers of CNS cell–specific processes and examining how they relate to MS disability progression. Dr. Masvekar, a researcher at the National Institute of Allergy and Infectious Diseases, and his coinvestigators used a modified DNA aptamer assay to measure proteins in the CSF of 431 patients with neuroimmunologic diseases and healthy volunteers, followed by variable cluster analysis and in vitro modeling to define 64 clusters of CSF biomarkers that relate to CNS cell types.
The study included 42 healthy donors, 20 patients with clinically isolated syndrome, 57 patients with noninflammatory neurologic disorders, 127 patients with relapsing-remitting MS, 72 patients with secondary progressive MS, and 113 patients with primary progressive MS. In a training cohort of 217 participants, the researchers assessed how biomarkers differed between the diagnostic categories. The researchers then validated the results in an independent cohort of 214 participants.
One astrocyte-related cluster (MMP7, SERPINA3, GZMA, and CLIC1) and one microglia-related cluster (DSG2 and TNFRSF25) was significantly elevated in all MS subgroups, compared with healthy controls and patients with noninflammatory neurologic disorders.
In addition, these clusters “significantly correlated with clinical measures of disability, CNS tissue destruction, and MS severity,” Dr. Masvekar said.
The microglial cluster was significantly elevated in all MS subgroups, whereas neuronal endothelial, astrocytic, and oligodendroglial biomarker clusters were elevated only in patients with progressive MS.
“Microglial activation is present in all stages of MS, while toxic astrogliosis increases with MS duration, concomitantly with neuronal and oligodendroglial degeneration,” Dr. Masvekar said. “Microglial activation and toxic astrogliosis likely partake in CNS tissue destruction and enhance MS severity.”
This study, which was recently published in Multiple Sclerosis and Related Disorders (2019 Feb;28:34-43), was supported by the intramural research program at NIAID.
SOURCE: Masvekar RR et al. ACTRIMS Forum 2019, Abstract 281.
DALLAS – Patients with multiple sclerosis (MS) have elevated levels of specific clusters of cerebrospinal fluid (CSF) biomarkers related to astrocytes and microglia that correlated with disease severity in a blinded analysis of more than 1,000 proteins from the CSF of more than 400 patients with neuroimmunologic disease and healthy volunteers.
Previous studies have indicated that aberrant activation of astrocytes and microglia underlies disability progression in older patients with MS, but researchers have lacked biomarkers of these processes in living subjects. In a presentation at a meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis, Ruturaj R. Masvekar, PhD, described developing biomarkers of CNS cell–specific processes and examining how they relate to MS disability progression. Dr. Masvekar, a researcher at the National Institute of Allergy and Infectious Diseases, and his coinvestigators used a modified DNA aptamer assay to measure proteins in the CSF of 431 patients with neuroimmunologic diseases and healthy volunteers, followed by variable cluster analysis and in vitro modeling to define 64 clusters of CSF biomarkers that relate to CNS cell types.
The study included 42 healthy donors, 20 patients with clinically isolated syndrome, 57 patients with noninflammatory neurologic disorders, 127 patients with relapsing-remitting MS, 72 patients with secondary progressive MS, and 113 patients with primary progressive MS. In a training cohort of 217 participants, the researchers assessed how biomarkers differed between the diagnostic categories. The researchers then validated the results in an independent cohort of 214 participants.
One astrocyte-related cluster (MMP7, SERPINA3, GZMA, and CLIC1) and one microglia-related cluster (DSG2 and TNFRSF25) was significantly elevated in all MS subgroups, compared with healthy controls and patients with noninflammatory neurologic disorders.
In addition, these clusters “significantly correlated with clinical measures of disability, CNS tissue destruction, and MS severity,” Dr. Masvekar said.
The microglial cluster was significantly elevated in all MS subgroups, whereas neuronal endothelial, astrocytic, and oligodendroglial biomarker clusters were elevated only in patients with progressive MS.
“Microglial activation is present in all stages of MS, while toxic astrogliosis increases with MS duration, concomitantly with neuronal and oligodendroglial degeneration,” Dr. Masvekar said. “Microglial activation and toxic astrogliosis likely partake in CNS tissue destruction and enhance MS severity.”
This study, which was recently published in Multiple Sclerosis and Related Disorders (2019 Feb;28:34-43), was supported by the intramural research program at NIAID.
SOURCE: Masvekar RR et al. ACTRIMS Forum 2019, Abstract 281.
REPORTING FROM ACTRIMS FORUM 2019
Biologic aging is associated with MS disability progression
DALLAS – according to a study presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Shorter telomere length is associated with increased MS disability in cross-sectional and longitudinal analyses, said Kristen M. Krysko, MD, clinical fellow in neurology at University of California, San Francisco. The results suggest that biologic aging may contribute to neurologic injury in MS and that “targeting aging-related mechanisms may be a potential therapeutic strategy,” said Dr. Krysko.
If validated, telomere length may be a biomarker that neurologists could use to guide decisions about MS treatment, said principal investigator Jennifer Graves, MD, PhD, also of UCSF.
“Factors leading to MS progression are not fully understood,” Dr. Krysko said. “But consistently, older chronological age has been associated with a faster time to disability milestones.” Aging may reduce remyelination capacity and alter immunologic responses. Telomere shortening, a marker of cellular aging, is “the ultimate biological clock.” It has been associated with cardiovascular disease, dementia, and autoimmune diseases, and one study found that patients with primary progressive MS have shorter telomere length, compared with controls.
To assess whether LTL is associated with clinical disability and brain volume in patients with MS, the researchers analyzed data from 516 adults with MS or clinically isolated syndrome in the EPIC cohort study at UCSF. Telomere length was measured on stored baseline DNA samples and expressed as the ratio of telomere to a single-copy gene.
The patients had an average age of 43 years, median disease duration of 6 years, and median Expanded Disability Status Scale (EDSS) score of 1.5; about 70% were women. The average telomere length was 0.97.
Older age and longer disease duration were associated with shorter LTL. For every 0.2-unit decrease in telomere length, EDSS score increased by 0.41. After adjusting for age, disease duration, and sex, every 0.2-unit decrease in telomere length was associated with a score increase of 0.27 on the EDSS. LTL also was associated with total brain volume and total white matter volume.
In addition, the investigators conducted a case control study that included a subset of 23 patients who developed secondary progressive MS during follow-up and had DNA available at multiple time points. The researchers matched these patients with 23 patients who continued to have relapsing MS. Patients were matched by age, sex, and disease duration. An adjusted analysis found that change in LTL was predictive of change in EDSS over 10 years such that every 0.2-unit decrease in LTL was associated with a 0.34-unit increase in EDSS.
Longitudinal analyses found that baseline LTL predicted higher levels of disability over time.
The study was funded by the National Multiple Sclerosis Society.
SOURCE: Krysko KM et al. ACTRIMS Forum 2019, Abstract 289.
DALLAS – according to a study presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Shorter telomere length is associated with increased MS disability in cross-sectional and longitudinal analyses, said Kristen M. Krysko, MD, clinical fellow in neurology at University of California, San Francisco. The results suggest that biologic aging may contribute to neurologic injury in MS and that “targeting aging-related mechanisms may be a potential therapeutic strategy,” said Dr. Krysko.
If validated, telomere length may be a biomarker that neurologists could use to guide decisions about MS treatment, said principal investigator Jennifer Graves, MD, PhD, also of UCSF.
“Factors leading to MS progression are not fully understood,” Dr. Krysko said. “But consistently, older chronological age has been associated with a faster time to disability milestones.” Aging may reduce remyelination capacity and alter immunologic responses. Telomere shortening, a marker of cellular aging, is “the ultimate biological clock.” It has been associated with cardiovascular disease, dementia, and autoimmune diseases, and one study found that patients with primary progressive MS have shorter telomere length, compared with controls.
To assess whether LTL is associated with clinical disability and brain volume in patients with MS, the researchers analyzed data from 516 adults with MS or clinically isolated syndrome in the EPIC cohort study at UCSF. Telomere length was measured on stored baseline DNA samples and expressed as the ratio of telomere to a single-copy gene.
The patients had an average age of 43 years, median disease duration of 6 years, and median Expanded Disability Status Scale (EDSS) score of 1.5; about 70% were women. The average telomere length was 0.97.
Older age and longer disease duration were associated with shorter LTL. For every 0.2-unit decrease in telomere length, EDSS score increased by 0.41. After adjusting for age, disease duration, and sex, every 0.2-unit decrease in telomere length was associated with a score increase of 0.27 on the EDSS. LTL also was associated with total brain volume and total white matter volume.
In addition, the investigators conducted a case control study that included a subset of 23 patients who developed secondary progressive MS during follow-up and had DNA available at multiple time points. The researchers matched these patients with 23 patients who continued to have relapsing MS. Patients were matched by age, sex, and disease duration. An adjusted analysis found that change in LTL was predictive of change in EDSS over 10 years such that every 0.2-unit decrease in LTL was associated with a 0.34-unit increase in EDSS.
Longitudinal analyses found that baseline LTL predicted higher levels of disability over time.
The study was funded by the National Multiple Sclerosis Society.
SOURCE: Krysko KM et al. ACTRIMS Forum 2019, Abstract 289.
DALLAS – according to a study presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
Shorter telomere length is associated with increased MS disability in cross-sectional and longitudinal analyses, said Kristen M. Krysko, MD, clinical fellow in neurology at University of California, San Francisco. The results suggest that biologic aging may contribute to neurologic injury in MS and that “targeting aging-related mechanisms may be a potential therapeutic strategy,” said Dr. Krysko.
If validated, telomere length may be a biomarker that neurologists could use to guide decisions about MS treatment, said principal investigator Jennifer Graves, MD, PhD, also of UCSF.
“Factors leading to MS progression are not fully understood,” Dr. Krysko said. “But consistently, older chronological age has been associated with a faster time to disability milestones.” Aging may reduce remyelination capacity and alter immunologic responses. Telomere shortening, a marker of cellular aging, is “the ultimate biological clock.” It has been associated with cardiovascular disease, dementia, and autoimmune diseases, and one study found that patients with primary progressive MS have shorter telomere length, compared with controls.
To assess whether LTL is associated with clinical disability and brain volume in patients with MS, the researchers analyzed data from 516 adults with MS or clinically isolated syndrome in the EPIC cohort study at UCSF. Telomere length was measured on stored baseline DNA samples and expressed as the ratio of telomere to a single-copy gene.
The patients had an average age of 43 years, median disease duration of 6 years, and median Expanded Disability Status Scale (EDSS) score of 1.5; about 70% were women. The average telomere length was 0.97.
Older age and longer disease duration were associated with shorter LTL. For every 0.2-unit decrease in telomere length, EDSS score increased by 0.41. After adjusting for age, disease duration, and sex, every 0.2-unit decrease in telomere length was associated with a score increase of 0.27 on the EDSS. LTL also was associated with total brain volume and total white matter volume.
In addition, the investigators conducted a case control study that included a subset of 23 patients who developed secondary progressive MS during follow-up and had DNA available at multiple time points. The researchers matched these patients with 23 patients who continued to have relapsing MS. Patients were matched by age, sex, and disease duration. An adjusted analysis found that change in LTL was predictive of change in EDSS over 10 years such that every 0.2-unit decrease in LTL was associated with a 0.34-unit increase in EDSS.
Longitudinal analyses found that baseline LTL predicted higher levels of disability over time.
The study was funded by the National Multiple Sclerosis Society.
SOURCE: Krysko KM et al. ACTRIMS Forum 2019, Abstract 289.
REPORTING FROM ACTRIMS FORUM 2019
Early intensive treatment of MS may benefit patients
First-line treatment of multiple sclerosis with a high-efficacy therapy may produce better long-term outcomes than does an escalation treatment approach, data from a real-world cohort study suggest.
In a population-based cohort of patients with multiple sclerosis (MS) in southeast Wales, those who initiated treatment with a high-efficacy therapy had a smaller average increase in Expanded Disability Status Scale (EDSS) score after 5 years, compared with patients who started on moderate-efficacy therapy, researchers reported Feb. 18 in JAMA Neurology. These outcomes occurred “despite clinical surveillance and targeted escalation” in the group of patients who started on moderate-efficacy drugs, said first author Katharine Harding, PhD, of Cardiff University and the University Hospital of Wales in Cardiff and the Royal Gwent Hospital, Newport, Wales, and her colleagues. “These findings suggest that real-world escalation approaches may be inadequate to prevent unfavorable long-term outcomes and support the need for a prospective clinical trial to compare disease-modifying therapy algorithms.”
The investigators analyzed data collected between January 1998 and December 2016 from 592 patients with MS. Of the 592 patients, 104 initiated treatment with alemtuzumab (Lemtrada) or natalizumab (Tysabri), which the researchers classified as high-efficacy therapies (i.e., early intensive treatment), and 488 initiated treatment with interferons, glatiramer acetate (Copaxone), dimethyl fumarate (Tecfidera), fingolimod (Gilenya), or teriflunomide (Aubagio), which were considered moderate-efficacy therapies (i.e., escalation approach).
At baseline, patients who received early intensive treatment had higher average EDSS scores, compared with patients treated with an escalation approach (4.2 vs. 3.5). After 5 years, the average increase in EDSS score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2). The researchers adjusted for patients’ sex, age at treatment, year of starting treatment, and escalation to high-efficacy treatment in the escalation treatment approach group.
Median time to sustained accumulation of disability was 6.0 years for the early intensive therapy group and 3.1 years for the escalation therapy group, but the risk of sustained accumulation of disability did not differ between the groups after adjustment for covariates.
“Although patients were selected to receive early intensive treatment on the basis of poor prognostic factors, including more active disease, it was this patient group that had better long-term outcomes,” Dr. Harding and her colleagues wrote.
There were no treatment-related deaths in the study. Among patients who received alemtuzumab, 87% developed infusion-related adverse events, and 47% developed autoimmunity. Among patients receiving natalizumab, there were no serious adverse events and no cases of progressive multifocal leukoencephalopathy. In patients receiving moderate-efficacy disease-modifying therapies, there were seven serious adverse events (1.4%).
Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
SOURCE: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905
First-line treatment of multiple sclerosis with a high-efficacy therapy may produce better long-term outcomes than does an escalation treatment approach, data from a real-world cohort study suggest.
In a population-based cohort of patients with multiple sclerosis (MS) in southeast Wales, those who initiated treatment with a high-efficacy therapy had a smaller average increase in Expanded Disability Status Scale (EDSS) score after 5 years, compared with patients who started on moderate-efficacy therapy, researchers reported Feb. 18 in JAMA Neurology. These outcomes occurred “despite clinical surveillance and targeted escalation” in the group of patients who started on moderate-efficacy drugs, said first author Katharine Harding, PhD, of Cardiff University and the University Hospital of Wales in Cardiff and the Royal Gwent Hospital, Newport, Wales, and her colleagues. “These findings suggest that real-world escalation approaches may be inadequate to prevent unfavorable long-term outcomes and support the need for a prospective clinical trial to compare disease-modifying therapy algorithms.”
The investigators analyzed data collected between January 1998 and December 2016 from 592 patients with MS. Of the 592 patients, 104 initiated treatment with alemtuzumab (Lemtrada) or natalizumab (Tysabri), which the researchers classified as high-efficacy therapies (i.e., early intensive treatment), and 488 initiated treatment with interferons, glatiramer acetate (Copaxone), dimethyl fumarate (Tecfidera), fingolimod (Gilenya), or teriflunomide (Aubagio), which were considered moderate-efficacy therapies (i.e., escalation approach).
At baseline, patients who received early intensive treatment had higher average EDSS scores, compared with patients treated with an escalation approach (4.2 vs. 3.5). After 5 years, the average increase in EDSS score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2). The researchers adjusted for patients’ sex, age at treatment, year of starting treatment, and escalation to high-efficacy treatment in the escalation treatment approach group.
Median time to sustained accumulation of disability was 6.0 years for the early intensive therapy group and 3.1 years for the escalation therapy group, but the risk of sustained accumulation of disability did not differ between the groups after adjustment for covariates.
“Although patients were selected to receive early intensive treatment on the basis of poor prognostic factors, including more active disease, it was this patient group that had better long-term outcomes,” Dr. Harding and her colleagues wrote.
There were no treatment-related deaths in the study. Among patients who received alemtuzumab, 87% developed infusion-related adverse events, and 47% developed autoimmunity. Among patients receiving natalizumab, there were no serious adverse events and no cases of progressive multifocal leukoencephalopathy. In patients receiving moderate-efficacy disease-modifying therapies, there were seven serious adverse events (1.4%).
Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
SOURCE: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905
First-line treatment of multiple sclerosis with a high-efficacy therapy may produce better long-term outcomes than does an escalation treatment approach, data from a real-world cohort study suggest.
In a population-based cohort of patients with multiple sclerosis (MS) in southeast Wales, those who initiated treatment with a high-efficacy therapy had a smaller average increase in Expanded Disability Status Scale (EDSS) score after 5 years, compared with patients who started on moderate-efficacy therapy, researchers reported Feb. 18 in JAMA Neurology. These outcomes occurred “despite clinical surveillance and targeted escalation” in the group of patients who started on moderate-efficacy drugs, said first author Katharine Harding, PhD, of Cardiff University and the University Hospital of Wales in Cardiff and the Royal Gwent Hospital, Newport, Wales, and her colleagues. “These findings suggest that real-world escalation approaches may be inadequate to prevent unfavorable long-term outcomes and support the need for a prospective clinical trial to compare disease-modifying therapy algorithms.”
The investigators analyzed data collected between January 1998 and December 2016 from 592 patients with MS. Of the 592 patients, 104 initiated treatment with alemtuzumab (Lemtrada) or natalizumab (Tysabri), which the researchers classified as high-efficacy therapies (i.e., early intensive treatment), and 488 initiated treatment with interferons, glatiramer acetate (Copaxone), dimethyl fumarate (Tecfidera), fingolimod (Gilenya), or teriflunomide (Aubagio), which were considered moderate-efficacy therapies (i.e., escalation approach).
At baseline, patients who received early intensive treatment had higher average EDSS scores, compared with patients treated with an escalation approach (4.2 vs. 3.5). After 5 years, the average increase in EDSS score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2). The researchers adjusted for patients’ sex, age at treatment, year of starting treatment, and escalation to high-efficacy treatment in the escalation treatment approach group.
Median time to sustained accumulation of disability was 6.0 years for the early intensive therapy group and 3.1 years for the escalation therapy group, but the risk of sustained accumulation of disability did not differ between the groups after adjustment for covariates.
“Although patients were selected to receive early intensive treatment on the basis of poor prognostic factors, including more active disease, it was this patient group that had better long-term outcomes,” Dr. Harding and her colleagues wrote.
There were no treatment-related deaths in the study. Among patients who received alemtuzumab, 87% developed infusion-related adverse events, and 47% developed autoimmunity. Among patients receiving natalizumab, there were no serious adverse events and no cases of progressive multifocal leukoencephalopathy. In patients receiving moderate-efficacy disease-modifying therapies, there were seven serious adverse events (1.4%).
Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
SOURCE: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: After 5 years, the average increase in Expanded Disability Status Scale score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2).
Study details: A population-based cohort study of 592 patients with MS in southeast Wales.
Disclosures: Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
Source: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905.
When to suspect a severe skin reaction to an AED
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
EXPERT ANALYSIS FROM AES 2018