User login
Quality and Safety During Off Hours
Patients experience acute illness at all hours of the day. In acute care hospitals, over 60% of patient admissions occur outside of normal business hours, or the off hours.[1, 2] Similarly, the acute decompensation of patients already admitted to hospital‐based units is frequent, with 90% of rapid responses occurring between 9 pm and 6 am.[3] Research suggests worse hospital performance during off hours, including increased patient falls, in‐hospital cardiac arrest mortality, and severity of hospital employee injuries.[2, 4, 5, 6, 7]
Although hospital‐based services should match care demand, the disparity between patient acuity and hospital capability at night is significant. Off hours typically have lower staffing of nurses, and attending and housestaff physicians, and ancillary staff as well as limited availability of consultative and supportive services.[8] Additionally, off‐hours providers are subject to the physiological effects of imbalanced circadian rhythms, including fatigue, attenuating their abilities to provide high‐quality care. The significant patient care needs mandate continuous patient care delivery without compromising quality or safety. To achieve this, further defining the barriers to delivering quality care during off hours is essential to improvement efforts in medicine‐based units.
Previous investigations have found increased occurrence and severity of worker accidents, increased potential for higher occurrence of preventable adverse patient events, and decreased performance during off hours.[4, 9, 10] Additionally, detrimental effects of off‐hours care may be further magnified by rotating employees through both day and night shifts, a common practice in academic hospitals.[11, 12] Potentially modifiable outcomes, such as patient fall rate and in‐hospital cardiac arrest survival differ markedly between day and night shifts.[6, 13] These studies primarily report on specific diseases, such as myocardial infarction and stroke, and are investigated from the perspective of hospital‐level outcomes.
To our knowledge, no study has reported provider‐perceived quality and safety issues occurring during off hours in an academic setting. Likewise, although off‐hours collaborative care requires shared, interprofessional conceptualization regarding care delivery, this perspective has not been reported. Understanding the similarities and differences between provider perceptions will allow the construction of an interprofessional team mental model, facilitating the design of future quality improvement initiatives.[14, 15] Our objectives were to: (1) identify off‐hours quality and safety issues, (2) assess which issues are perceived as most significant, and (3) evaluate differences in perceptions of these issues between nurses, and attending and housestaff physicians.
METHODS
Study Design
To investigate quality and safety issues occurring during off hours, we employed a prospective, mixed‐methods sequential exploratory study design, involving an initial qualitative analysis of adverse events followed by quantitative survey assessment.[16] We chose a mixed‐methods approach because provider‐perceived off‐hours issues had not been explicitly identified in the literature, requiring preliminary qualitative assessment. For the purpose of this study, we defined off hours as the 7 pm to 7am time period, which overlapped night shifts for both nurses and physicians. The study was approved by the institutional review board as a quality improvement project.
Study Setting
The study was conducted at a 378‐bed, university‐based acute care hospital in central Pennsylvania. There are a total of 64 internal medicine beds located in 2 units: a general medicine unit (44 beds, staffed by 60 nurses, nurse‐to‐patient ratio 1:4) and an intermediate care unit (20 beds, staffed by 41 nurses, nurse‐to‐patient ratio 1:3). The medicine residency program consists of 69 residents and 14 combined internal medicinepediatrics residents. During the day, 3 teaching teams and 1 nonteaching team care for all medicine patients. Overnight, 3 junior/senior level residents admit patients to the medicine service, whereas 2 interns provide cross‐coverage for all medicine and specialty service patients. Starting in September 2012 (before data collection), an overnight faculty‐level academic hospitalist, or nocturnist, provided on‐site housestaff supervision.
Qualitative Data Collection
For the qualitative analysis, we used 2 methods to develop our database. First, we created an electronic survey (see Supporting Information, Appendix 1, in the online version of this article) to identify near misses/adverse events occurring overnight, distributed to the nocturnist, 3 daytime hospitalists, and unit charge nurses following each shift (October 2012March 2013). The survey items were developed for the purpose of this study, with several items modified from a previously published survey.[17] Second, residency program directors recorded field notes during end‐of‐rotation debriefings (1 hour) with departing overnight housestaff, which were then dictated and transcribed. The subsequent analysis from these sources informed the quantitative survey (see Supporting Information, Appendix 2, in the online version of this article).
Survey Instrument
Three months after the initiation of qualitative data collection, 1 investigator (J.D.G.) developed a preliminary codebook to identify categories and themes. From this codebook, the research team drafted a survey instrument (the complete qualitative analysis occurred after survey development). To maintain focus on systematic quality improvement, items related to perceived mismanagement, relationship tensions, and professionalism were excluded. The survey was pilot‐tested with 5 faculty physicians and 2 nursing staff, prompting several modifications to improve clarity. Primary demographic items included provider role (nurse, attending physician, or housestaff physician) and years in current role. The 24 survey items were grouped into 5 different categories: (1) Quality of Care Delivery, (2) Communication and Coordination, (3) Staffing and Supervision, (4) Patient Transfers, and (5) Consulting Service Issues. Each item was investigated on a 7‐point scale (1=lowest rating, 7=highest rating). Descriptive text was provided at the extremes (choices 1 and 7), whereas intermediary values (26) did not have descriptive cues. The descriptive anchors for Quality of Care Delivery and Patient Transfers were 1=never and 7=always, whereas the descriptive anchors Communication and Coordination and Staffing and Supervision were 1=poor and 7=superior; Consulting Service Issues used a mix of both. Providers with off‐hours experience were asked to rank 4 time periods (710 pm, 10 pm1 am, 14 am, 47 am) regarding quality of care delivery in the medicine units (1=best, 4=worst). We asked both daytime and nighttime providers about perceptions of off‐hours care because, given the boundary spanning the nature of medical care across work shifts, daytime providers frequently identify issues not apparent until hours (or even days) after completion of a night shift. A similar design was used in prior work investigating safety at night.[17]
Quantitative Data Collection
In June of 2013, we emailed a survey link (
Data Analysis
Using the preliminary codebook, 2 investigators (J.D.G., E.M.) jointly analyzed a segment of the dataset using Atlas.ti 6.0 (Scientific Software, Berlin, Germany). Two investigators independently coded the data, compared codes for agreement, and updated the codebook. The remaining data were coded independently, with regular adjudication sessions to modify the codebook. All investigators reviewed and agreed upon themes and representative quotations.
Descriptive statistics, Pearson correlation statistics, Kruskal‐Wallis tests, and signed rank tests (with Bonferroni correction) were used to report group characteristics, correlate rank order, make comparisons between groups (nursing staff, and attending and housestaff physicians; day/night providers), and compare quality rankings by time period, respectively. The data were analyzed using SAS 9.3 (SAS Institute Inc., Cary, NC) and Stata/IC‐8 (StataCorp, College Park, TX).
RESULTS
Qualitative Analysis of Off‐Hours' Adverse Events and Near Misses
A total of 190 events were reported by daytime attending physicians (n=100), nocturnists (n=60), and nighttime charge nurses (n=30). Although questions asked participants to describe near misses/adverse events, respondents also reported a number of global quality issues not related to specific events. Similarly, debriefing sessions with housestaff (n=5) addressed both specific overnight events and residency‐related issues. Seven themes were identified: (1) perceived mismanagement, (2) quality of delivery processes, (3) communication and coordination, (4) staffing and supervision, (5) patient transfers, (6) consulting service issues, and, (7) professionalism/relational tensions. Table 1 lists the code frequencies and exemplary quotations.
| Category and Themes | Code Frequency No. (% of 322) | Representative Quotation |
|---|---|---|
| ||
| Perceived mismanagement | 97 (30) | We had a new admission to the general medicine unit with atrial flutter and rapid ventricular response who did not receive rate controlling agents but rather received diuretics. [The patient's] heart rate remained between 110 and 130 overnight, with a troponin rise in the am likely from demand. The attending note states rate controllers and discussed with housestaff, but this was not performed. |
| Quality of delivery processes | 63 (20) | One patient had a delay in MRI scanning in the off hours due to the scanner being down and scheduling. When the patient went down, there seemed to be little attempt to make sure patient went through scanner; unclear if housestaff called or not to come to assist. Now, the delay in care is even further along. |
| Communication and coordination | 50 (16) | A patient was transferred to the intermediate care unit with hypercarbic respiratory failure. The patient had delay of >1 hour to receive IV Bumex because pharmacy would not release the dose from Pyxis, and the nurse did not let us know there was a delay. When I asked the nurse why, she responded because she's not the only patient I have. I pointed out that the patient was in failure and needed Bumex, stat. If we had not clearly communicated either verbally or via computer, she should let us know how to do that better. |
| Staffing and supervision | 39 (12) | A patient was admitted DNR/DNI with advanced dementia, new on BiPaP at 100%, and hypotensive. The team's intern [identified] the need for interventions, including a central line. This was discussed with overloaded intensive care unit resident. The intern struggled until another resident assisted along with the night attending. Issues included: initial triage, no resident backup for team, and attending backup. I should have been more hands on in the moment to assist the intern navigating the system of care. Many issues here, but no senior resident was involved in care until [late]. |
| Patient transfers | 38 (12) | One patient went from the emergency department [to us] on the 5th floor at 7:45 pm. The ED placed an order for packed red blood cells and it was written at 4:45 pm. When patient arrived on our floor at 7:45 pm, the transfusion had not been started. The floor nurse started it at 8:10 pm . |
| Consulting services | 18 (6) | Regarding a new outside hospital transfer, the medicine team was informed that [the consulting service] would place official consult on the chart when imaging studies from the outside institution were available. Despite this, the consult was still not done after 36 hours, and [we are] still waiting. We contacted service several times. |
| Professionalism and relational tensions | 17 (5) | [One admission from the emergency department] involved a patient who received subcutaneous insulin for hyperkalemia as opposed to intravenous insulin. When brought to [their] attention, they became very confrontational and abrupt and denied having ordered or administered it that way, although it was documented in the EMR. |
Perceived Mismanagement
Participants commonly questioned the decision making, diagnosis, or management of off‐hours providers. Concerns included the response to acute illness (eg, delay in calling a code), treatment decisions (eg, diuresis in a patient with urinary retention), or omission of necessary actions (eg, no cultures ordered for septicemia).
Quality of Delivery Processes
Participants frequently described quality of care delivery issues primarily related to timeliness or delays in delivery processes (34/63 coding references), or patient safety issues (29/63 coding references). Described events revealed concerns about the timeliness of lab reporting, imaging, blood draws, and medication ordering/processing.
Communication and Coordination
Breakdowns in communication and coordination often threatened patient safety. Identified issues included poor communication between primary physicians, nurses, consulting services, and emergency department (ED) providers, as well as documentation within the electronic medical record.
Staffing and Supervision
Several events highlighted staffing or supervision limitations, such as perceived low nursing or physician staffing levels. The degree of nocturnist supervision was polarizing, with both increased and decreased levels of supervision reported as limiting care delivery (or housestaff education).
Patient Transfers
Patient transfers to medicine units from the ED, other inpatient units, or outside hospitals, were identified several times as an influential factor. The care transition and need for information exchange led to a perceived compromise in quality or safety.
Consulting Service Issues
Several examples highlighted perceived issues related to the communication, coordination, or timeliness of consultant services in providing care.
Professionalism/Relational Tensions
Last, providers described situations in which they perceived lack of professionalism or relational tensions between providers, either in regard to interactions or clinical decisions in patient care.
Quantitative Results
Of 214 surveys sent, data were collected from 160 respondents (75% response), including 64/101 nursing staff (63% response), 25/28 attending physicians (80% response), and 71/85 housestaff physicians (84% response). Table 2 describes the participant demographics.
| Variable | No. (%) |
|---|---|
| |
| Nursing staff | 64 (40) |
| Intermediate care unit | 20 |
| General medicine ward | 44 |
| All night shifts | 16 |
| Mix of day and night shifts | 26 |
| Years of experience, mean (SD) | 7.7 (9.7) |
| Attending physicians | 25 (16) |
| No. providing care only at night | 4 |
| No. of weeks as overnight hospitalist in past year, mean (SD) | 11.5 (4.1) |
| No. providing care only during the day | 21 |
| Years since residency graduation, mean (SD) | 9.0 (8.5) |
| Medicine residents | 71 (44) |
| Intern | 27 |
| Junior resident | 23 |
| Senior resident* | 21 |
Off‐Hours Quality and Safety Issues
Ratings and comparisons of the 24 items are shown in Table 3. For all items, the mean rating was below 5 (7‐point scale). Lowest‐rated (least optimal) items were: timeliness, safety, and communication involved with patients admitted from the ED, number of attending physicians, and timeliness of consults and blood draws. Highest‐rated (more optimal) items were: timely reporting of labs, timely identification of deteriorating status, medication ordering and processing, communication between physicians, and safety and communication involved with intraservice transfers.
| Category and Survey Item, Mean (SD)* | Total (160) | Providers With Night Experience | Nighttime Providers (116) | Daytime Providers (44) | P Value | |||
|---|---|---|---|---|---|---|---|---|
| Nurses (41) | Attending Physicians (4) | Housestaff (71) | P Value | |||||
| ||||||||
| Quality of care delivery | ||||||||
| Timely reporting of labs at night | 4.70 (1.39) | 5.12 (1.50) | 4.50 (1.00) | 4.61 (1.47) | 0.11 | 4.78 (1.48) | 4.48 (1.11) | 0.09 |
| Timely identification of deteriorating status | 4.67 (1.34) | 4.88 (1.36) | 5.00 (0.82) | 4.85 (1.20) | 0.93 | 4.86 (1.24) | 4.16 (1.45) | 0.006 |
| Medication ordering and processing | 4.63 (1.13) | 4.88 (1.25) | 5.25 (0.50) | 4.66 (1.08) | 0.19 | 4.76 (1.13) | 4.27 (1.06) | 0.01 |
| Timely completion of imaging at night | 4.29 (1.32) | 4.32 (1.46) | 4.75 (0.96) | 4.39 (1.29) | 0.88 | 4.38 (1.34) | 4.05 (1.26) | 0.12 |
| Timely reporting of results at night | 4.19 (1.43) | 4.27 (1.53) | 4.00 (1.83) | 4.11 (1.44) | 0.84 | 4.16 (1.47) | 4.27 (1.30) | 0.76 |
| Timely med release from pharmacy at night | 4.16 (1.29) | 4.00 (1.32) | 4.50 (0.58) | 4.28 (1.29) | 0.44 | 4.19 (1.28) | 4.09 (1.31) | 0.90 |
| Timely blood draws at night | 3.96 (1.52) | 4.63 (1.44) | 4.50 (0.58) | 3.53 (1.49) | <0.001 | 3.96 (1.54) | 3.98 (1.47) | 0.98 |
| Communication and coordination | ||||||||
| Communication between physicians | 4.63 (1.26) | 4.29 (1.23) | 6.00 (1.15) | 5.14 (1.12) | <0.001 | 4.87 (1.24) | 3.98 (1.09) | <0.001 |
| Communication between nursing and pharmacy | 4.39 (1.27) | 4.83 (1.41) | 5.00 (0.82) | 4.27 (1.29) | 0.04 | 4.49 (1.34) | 4.11 (4.11) | 0.08 |
| Communication between nursing and physicians | 4.39 (1.28) | 4.44 (1.36) | 5.00 (0.82) | 4.58 (1.31) | 0.64 | 4.54 (1.31) | 3.98 (1.13) | 0.01 |
| Documentation in medical record | 4.33 (1.36) | 5.00 (1.36) | 6.00 (0.82) | 4.23 1.19) | <0.001 | 4.56 (1.31) | 3.70 (1.30) | <0.001 |
| Ease of contacting primary providers at night | 4.31 (1.29) | 4.46 (1.27) | 6.00 (0.00) | 4.54 (1.18) | 0.02 | 4.56 (1.22) | 3.66 (1.27) | <0.001 |
| Staffing and supervision | ||||||||
| No. of nursing staff | 4.51 (1.27) | 4.54 (1.50) | 5.50 (0.58) | 4.59 (1.21) | 0.25 | 4.60 (1.31) | 4.25 (1.14) | 0.025 |
| Supervision of housestaff | 4.43 (1.34) | 4.56 (1.40) | 6.25 (0.50) | 4.55 (1.34) | 0.03 | 4.61 (1.37) | 3.95 (1.14) | 0.002 |
| No. of housestaff | 4.09 (1.39) | 4.27 (1.40) | 4.50 (1.29) | 4.11 (1.44) | 0.70 | 4.18 (1.41) | 3.86 (1.32) | 0.12 |
| No. of ancillary staff | 4.00 (1.40) | 4.27 (1.53) | 5.75 (0.96) | 3.85 (1.40) | 0.02 | 4.06 (1.48) | 3.84 (1.18) | 0.27 |
| No. of attending physicians | 3.79 (1.50) | 3.49 (1.76) | 5.25 (0.96) | 3.89 (1.43) | 0.07 | 3.79 (1.57) | 3.80 (1.32) | 0.98 |
| Patient transfers | ||||||||
| For patients accepted to medicine from another medicine unit | ||||||||
| Timely and safe patient transfers | 4.56 (1.28) | 5.15 (1.11) | 4.75 (0.50) | 4.55 (1.23) | 0.025 | 4.77 (1.20) | 4.00 (1.33) | 0.001 |
| High quality communication between providers | 4.55 (1.35) | 5.34 (1.13) | 5.00 (0.82) | 4.49 (1.22) | 0.001 | 4.81 (1.24) | 3.86 (1.41) | <0.001 |
| For patients admitted from emergency department to medicine unit | ||||||||
| Appropriate testing and treatment | 4.16 (1.34) | 4.15 (1.30) | 4.00 (1.83) | 4.21 (1.43) | 0.96 | 4.18 (1.39) | 4.11 (1.20) | 0.66 |
| Timely and safe transfers | 3.89 (1.38) | 3.63 (1.50) | 5.50 (0.58) | 4.08 (1.32) | 0.02 | 3.97 (1.40) | 3.68 1.29) | 0.23 |
| High‐quality communication between providers | 2.93 (1.38) | 2.56 (1.23) | 3.75 (1.26) | 3.00 (1.39) | 0.08 | 2.87 (1.35) | 3.07 (1.47) | 0.41 |
| Consulting service issues | ||||||||
| Timely consults at night | 4.04 (1.35) | 4.27 (1.28) | 4.00 (0.82) | 4.10 (1.47) | 0.69 | 4.16 (1.38) | 3.73 (1.25) | 0.053 |
| Communication between consults and physicians | 3.93 (1.40) | 3.46 (1.45) | 5.75 (1.26) | 4.35 (1.27) | <0.001 | 4.09 (1.42) | 3.50 (1.27) | 0.016 |
Comparisons Between Professional Groups With Night Experience
Of the 24 items, 11 showed statistically significant differences between groups (P<0.05). Items with the largest difference between groups included: timely blood draws at night (housestaff physicians lowest), communication between physicians (nursing lowest), documentation in medical record (housestaff physicians lowest), and communication between consults and physicians (nursing lowest). The rank order between housestaff physicians and nurses, and housestaff and attending physicians showed moderately positive correlations (r=0.61, P=0.002 and r=0.47, P=0.022, respectively). The correlation between nurses and attending physicians showed a weak correlation (r=0.19, P=0.375).
Comparisons Between Front‐Line Providers With and Without Night Experience
Of the 24 items, 12 showed statistically significant differences between groups (P<0.05), with day providers reporting lower ratings in all 12. Items with the largest difference between groups included: communication between consults and physicians, ease of contacting providers, communication between providers, documentation, and safety and communication related to transfers from other units. The rank order between night and day groups showed a statistically significant positive correlation (r=0.65, P=0.001).
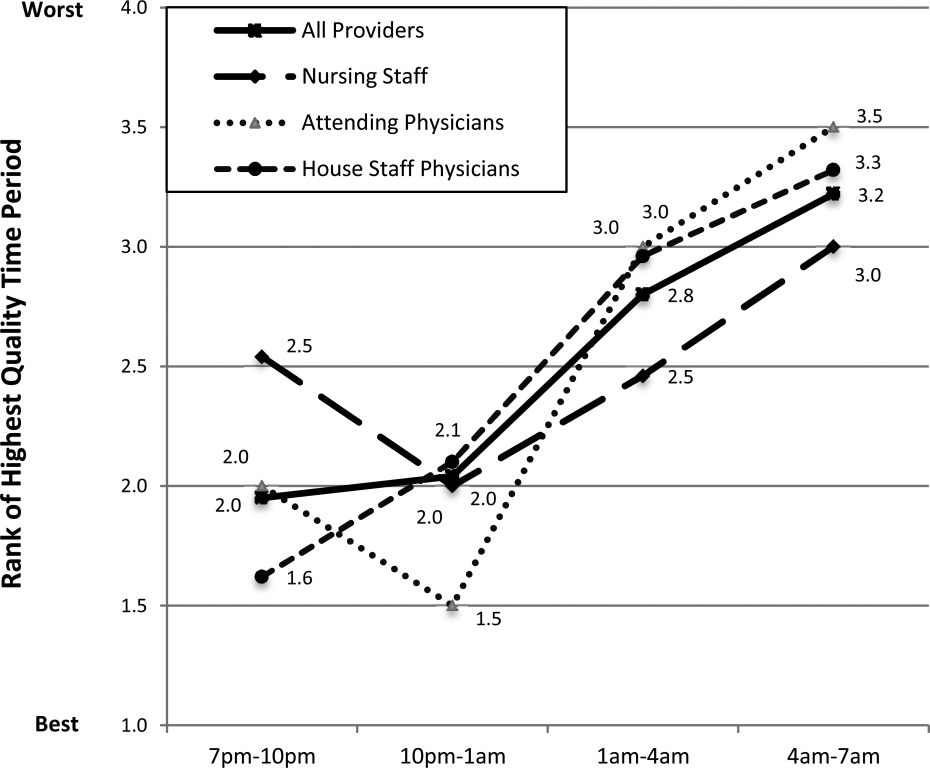
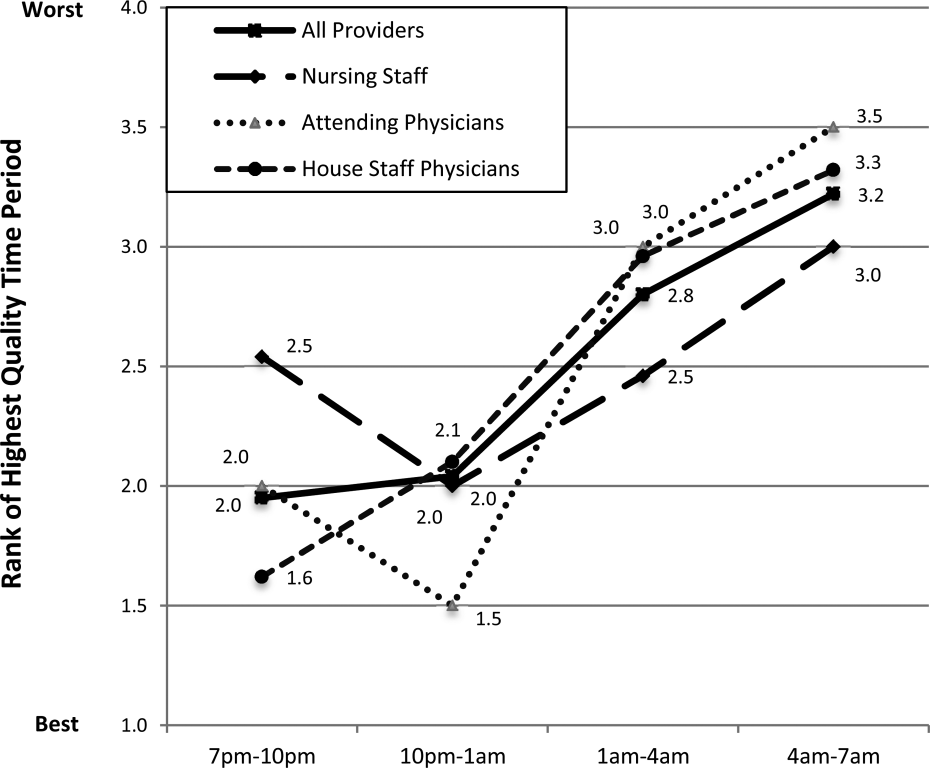
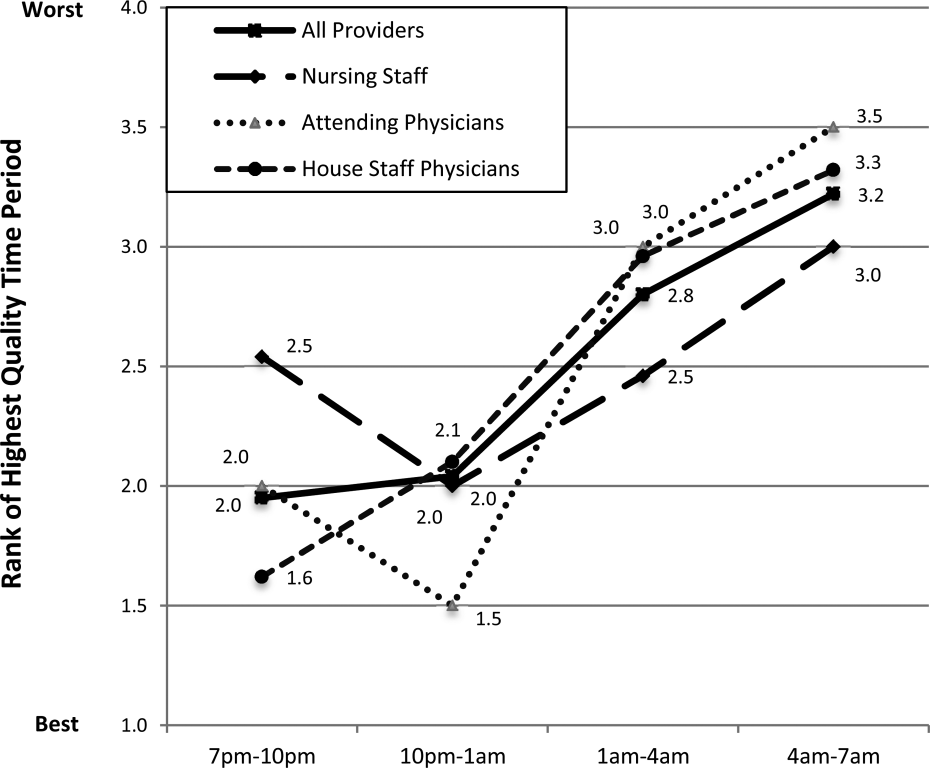
Perceived Highest Quality of Care Time Period During Off Hours
Compared with other time periods, all providers ranked 4 to 7 am as the period with the lowest quality of care delivery (mean rank 3.2, P0.001) (Figure 1). Nursing staff and attending physicians both ranked the 10 pm to 1 am time period as the best period (mean of 2.0 and 1.5, respectively), whereas housestaff physicians ranked the 7 to 10 pm as the best time period (mean 1.62). The only statistical difference between provider groups for any given time period was the 7 to 10 pm time period (P=0.002).
DISCUSSION
In this prospective, mixed‐methods study evaluating perceived off‐hours quality and safety issues, several themes were identified, including perceived mismanagement, insufficient quality of delivery processes, communication/coordination breakdowns, and staffing and supervision issues. In the quantitative analysis, lowest‐rated items (lowest quality) related to timeliness/safety/communication involved with ED transfers, number of attending physicians, and timeliness of consults and blood draws. Highest‐rated items (highest quality) related to timeliness of lab reporting and identification of deteriorating patients, medication ordering/processing, communication between physicians, and safety/communication during intraservice transfers. In general, day providers reported lower ratings than night providers on nearly all quality‐related items. Nursing staff reported the lowest ratings regarding communication between physicians and consults, whereas housestaff physicians reported the lowest ratings regarding documentation in the medical record and timely blood draws. These between‐group differences reveal the lack of shared conceptual understanding regarding off‐hours care delivery.
Our qualitative results reveal several significant issues related to care delivery during off hours, many of which are not obtainable by hospital‐level data or chart review.[18] For hospital‐based medicine units, an understanding of the structure‐ and process‐related factors associated with events is required for quality improvement efforts. Although the primary focus for this work was the off hours, it is plausible that providers may have identified similar issues as important issues during daytime hours. Our study was not designed to investigate if these perceived issues are specific to off hours, or if these issues are an accurate reflection of objective events occurring during this time period. We believe this topic deserves further investigation, as understanding if these off‐hours perceptions are unique to this time period would change the scope of future quality improvement initiatives.
The most significant finding in the quantitative results was the vulnerability in quality and safety during patient admissions from the ED, specifically in relation to communication and timeliness of transfer. Between‐unit handoffs for patients admitted from the ED to medicine units have been identified as particularly vulnerable to breakdowns in the communication process.[19, 20, 21, 22] There are multiple etiologies, including clinical uncertainty, higher acuity in patient illness early in hospitalization, and cultural differences between services.[23] Additionally, patterns of communication and standardized handoff processes are often insufficient. In our hospital system, the transfer process relies primarily upon synchronous communication methods without standardized, asynchronous information exchange. We hypothesize front‐line providers perceive this lack of standardization as a primary threat to quality. Because approximately 60% of new patient admissions from the ED to medicine service (both in our hospital and in prior studies) occur during off hours, these findings highlight a need for subsequent study and quality improvement efforts.[24]
During the time of this study, our medicine units were staffed at night by 5 medicine housestaff physicians and 1 academic hospitalist, or nocturnist. In efforts to improve quality and safety during off hours, our hospital, as well as other health systems, implemented the nocturnist position, a faculty‐level attending physician to provide off‐hours clinical care and housestaff supervision.[25] Although participants reported a moderate rating of housestaff supervision, participants provided lower scores for staffing numbers of nurses, and housestaff and attending physicians, despite nocturnist presence. With both increased off‐hours supervision in our hospital and increasing use of faculty‐level physicians in other academic programs, these results provide context for the anticipated level of overnight housestaff supervision.[26, 27] To our knowledge, this is the first study to investigate perceived overnight quality issues on medicine units following such staffing models. Although this model of direct, on‐site supervision in academic medicine programs may help offset staffing and supervisory issues during off hours, the nocturnist role is insufficient to offset threats to quality/safety already inherent within the system. Furthermore, prospective trials following implementation of nocturnist systems have shown mixed results in improving patient outcomes.[28] These findings have led some to question whether resources dedicated to nocturnist staffing may be better allocated to other overnight initiatives, highlighting the need for a more subtle understanding of quality issues to design targeted interventions.[29]
A notable finding from this work is that providers without night experience reported lower scores for 20 of 24 items, highlighting their perceptions of the quality of care delivery during off hours are lower than those who experience this environment. Although day providers are not directly experiencing off‐hours delivery processes, these providers receive and detect the results from care delivery at night.[17] Most nurse, physician, and hospital leaders are present in the hospital only during day hours, requiring these individuals to account for differences in perceived and actual care delivered overnight.[1] These individuals make critical decisions pertaining to process changes and quality improvement efforts in these units. We believe these results raise awareness for leadership decisions and quality improvement efforts in medicine service units, specifically to focus on overnight issues beyond staffing issues alone.
All respondent groups ranked the latter half of the shift (17 am) as lower in quality compared to the first 6 hours (7 pm1 am). This finding is contrary to our hypothesis that earlier time periods, during the majority of patient admissions (and presumed higher workload for all providers), would be perceived as lower quality. Reasons for this finding are unknown, but may relate to end‐of‐shift tasks, sign‐out preparation, provider fatigue, or disease‐related concerns (eg, increased incidence of stroke and myocardial infarction) during the latter portions of night shifts. One study identified a decrease in nursing clinical judgments from the beginning to end of 12‐hour shifts, with a potential suggested mechanism of decrease in ability to maintain attention during judgments.[30] Additionally, in a study by Folkard et al., risk was highest within the first several hours and fell substantially thereafter during a shift.[9] To our knowledge, no work has investigated perceived or objective quality outcomes by time period during the off‐hours shift in medicine units. Further work could help delineate why provider‐perceived compromises in quality occur late in off‐hours shifts and whether this correlates to safety events.
There are several limitations to our study. First, although all surveys were pilot tested for content validity, the construct validity was not rigorously assessed. Second, although data were collected from all participant groups, the collection methods were unbalanced, favoring attending‐level physician perspectives. Although the relative incidence of vulnerabilities in quality and safety should be interpreted with caution, our methods and general taxonomy provide a framework for developing and monitoring the perceptions of future interventions. Due to limitations in infrastructure, our findings could not be independently validated through review of reported adverse events, but previous investigations have found the vast majority of adverse events are not detected by standard anonymous reporting.[31, 32, 33] Our methodology (used in our prior work) may provide an independent means of detecting causes of poor quality not easily observed through routine surveillance.[22] Although many survey items showed statistical differences between provider groups, the clinical significance is subject to interpretation. Last, the perceptions and events related to our institution may not be fully generalizable to other academic programs or service lines, particularly in community‐based, nonteaching hospitals.
In conclusion, our results suggest a significant discrepancy between the concerns of day and night providers regarding the quality of care delivered to inpatients during the off hours, specifically with issues related to communication, quality‐of‐care delivery processes, and patient transfers from the ED. Although specific concerns may be institution‐ (and service line‐) dependent, appropriately designing initiatives to improve the quality of care delivered overnight will need to take the perspectives of both provider groups into account. Additionally, educational initiatives should focus on achieving a shared mental model among all providers to improve collaboration and performance.
Acknowledgements
The authors thank the nurses, internal medicine housestaff physicians, and general internal medicine attending physicians at the Penn State Hershey Medical Center for their participation in this study.
Disclosure: Nothing to report.
- . Like night and day—shedding light on off‐hours care. N Engl J Med. 2008;358(20):2091–2093.
- , , , . Call nights and patient care. J Gen Intern Med. 1992;7(4):405–410.
- , , , et al. Uncovering system errors using a rapid response team: cross‐coverage caught in the crossfire. Discussion. J Trauma. 2009;67(1):173–179.
- , . The impact of shift work on the risk and severity of injuries for hospital employees: an analysis using Oregon workers' compensation data. Occup Med (Lond). 2004;54(8):556–563.
- , . Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668.
- , , , et al. The association of shift‐level nurse staffing with adverse patient events. J Nurs Adm. 2011;41(2):64–70.
- , , , et al. Heart disease and stroke statistics—2010 update A report from the American Heart Association. Circulation. 2010;121(7):e46–e215.
- , , , , O'Neil E. Minimum Nurse Staffing Ratios In California Acute Care Hospitals. Oakland, CA: California Workforce Initiative; 2000.
- , . Shift work, safety and productivity. Occup Med (Lond). 2003;53(2):95–101.
- , , . Increased injuries on night shift. Lancet. 1994;344(8930):1137–1139.
- , . Shift and night work and long working hours‐a systematic review of safety implications. Scand J Work Environ Health. 2011:37(3):173–185.
- , , , et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82(7):1011–1014.
- , , , et al. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792.
- , , , , . The influence of shared mental models on team process and performance. J Appl Psychol. 2000;85(2):273.
- , . Team mental models and their potential to improve teamwork and safety: a review and implications for future research in healthcare. Saf Sci. 2012;50(5):1344–1354.
- . Editorial: mapping the field of mixed methods research. J Mix Methods Res. 2009;3(2):95–108.
- , . Decreasing adverse events through night talks: an interdisciplinary, hospital‐based quality improvement project. Perm J. Fall 2009;13(4):16–22.
- , , , et al. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff (Millwood). 2011;30(4):581–589.
- , , , , , . Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701–710.e704.
- . Smoothing transitions. Joint Commission targets patient handoffs. Mod Healthc. 2010;40(43):8–9.
- , , , , , . The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med. 2012;87(4):411–418.
- , , , , , . Patient care transitions from the emergency department to the medicine ward: evaluation of a standardized electronic signout tool. Int J Qual Health Care. 2014;26(4):337–347.
- , . The unappreciated challenges of between‐unit handoffs: negotiating and coordinating across boundaries. Ann Emerg Med. 2013;61(2):155–160.
- , , , , , . The association between night or weekend admission and hospitalization‐relevant patient outcomes. J Hosp Med. 2011;6(1):10–14.
- . Middle‐of‐the‐night medicine is rarely patient‐centred. CMAJ. 2011;183(13):1467–1468.
- , , , et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521–523.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- , , , et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209.
- . Intensivists at night: putting resources in the right place. Crit Care. 2013;17(5):1008.
- , , . Changes in nurses' decision making during a 12‐h day shift. Occup Med (Lond). 2013;63(1):60–65.
- , , , , , . The incident reporting system does not detect adverse drug events: a problem for quality improvement. Jt Comm J Qual Improv. 1995;21(10):541–548.
- , , , , . An evaluation of adverse incident reporting. J Eval Clin Pract. 1999;5(1):5–12.
- , . Reporting and preventing medical mishaps: lessons from non‐medical near miss reporting systems. BMJ. 2000;320(7237):759–763.
Patients experience acute illness at all hours of the day. In acute care hospitals, over 60% of patient admissions occur outside of normal business hours, or the off hours.[1, 2] Similarly, the acute decompensation of patients already admitted to hospital‐based units is frequent, with 90% of rapid responses occurring between 9 pm and 6 am.[3] Research suggests worse hospital performance during off hours, including increased patient falls, in‐hospital cardiac arrest mortality, and severity of hospital employee injuries.[2, 4, 5, 6, 7]
Although hospital‐based services should match care demand, the disparity between patient acuity and hospital capability at night is significant. Off hours typically have lower staffing of nurses, and attending and housestaff physicians, and ancillary staff as well as limited availability of consultative and supportive services.[8] Additionally, off‐hours providers are subject to the physiological effects of imbalanced circadian rhythms, including fatigue, attenuating their abilities to provide high‐quality care. The significant patient care needs mandate continuous patient care delivery without compromising quality or safety. To achieve this, further defining the barriers to delivering quality care during off hours is essential to improvement efforts in medicine‐based units.
Previous investigations have found increased occurrence and severity of worker accidents, increased potential for higher occurrence of preventable adverse patient events, and decreased performance during off hours.[4, 9, 10] Additionally, detrimental effects of off‐hours care may be further magnified by rotating employees through both day and night shifts, a common practice in academic hospitals.[11, 12] Potentially modifiable outcomes, such as patient fall rate and in‐hospital cardiac arrest survival differ markedly between day and night shifts.[6, 13] These studies primarily report on specific diseases, such as myocardial infarction and stroke, and are investigated from the perspective of hospital‐level outcomes.
To our knowledge, no study has reported provider‐perceived quality and safety issues occurring during off hours in an academic setting. Likewise, although off‐hours collaborative care requires shared, interprofessional conceptualization regarding care delivery, this perspective has not been reported. Understanding the similarities and differences between provider perceptions will allow the construction of an interprofessional team mental model, facilitating the design of future quality improvement initiatives.[14, 15] Our objectives were to: (1) identify off‐hours quality and safety issues, (2) assess which issues are perceived as most significant, and (3) evaluate differences in perceptions of these issues between nurses, and attending and housestaff physicians.
METHODS
Study Design
To investigate quality and safety issues occurring during off hours, we employed a prospective, mixed‐methods sequential exploratory study design, involving an initial qualitative analysis of adverse events followed by quantitative survey assessment.[16] We chose a mixed‐methods approach because provider‐perceived off‐hours issues had not been explicitly identified in the literature, requiring preliminary qualitative assessment. For the purpose of this study, we defined off hours as the 7 pm to 7am time period, which overlapped night shifts for both nurses and physicians. The study was approved by the institutional review board as a quality improvement project.
Study Setting
The study was conducted at a 378‐bed, university‐based acute care hospital in central Pennsylvania. There are a total of 64 internal medicine beds located in 2 units: a general medicine unit (44 beds, staffed by 60 nurses, nurse‐to‐patient ratio 1:4) and an intermediate care unit (20 beds, staffed by 41 nurses, nurse‐to‐patient ratio 1:3). The medicine residency program consists of 69 residents and 14 combined internal medicinepediatrics residents. During the day, 3 teaching teams and 1 nonteaching team care for all medicine patients. Overnight, 3 junior/senior level residents admit patients to the medicine service, whereas 2 interns provide cross‐coverage for all medicine and specialty service patients. Starting in September 2012 (before data collection), an overnight faculty‐level academic hospitalist, or nocturnist, provided on‐site housestaff supervision.
Qualitative Data Collection
For the qualitative analysis, we used 2 methods to develop our database. First, we created an electronic survey (see Supporting Information, Appendix 1, in the online version of this article) to identify near misses/adverse events occurring overnight, distributed to the nocturnist, 3 daytime hospitalists, and unit charge nurses following each shift (October 2012March 2013). The survey items were developed for the purpose of this study, with several items modified from a previously published survey.[17] Second, residency program directors recorded field notes during end‐of‐rotation debriefings (1 hour) with departing overnight housestaff, which were then dictated and transcribed. The subsequent analysis from these sources informed the quantitative survey (see Supporting Information, Appendix 2, in the online version of this article).
Survey Instrument
Three months after the initiation of qualitative data collection, 1 investigator (J.D.G.) developed a preliminary codebook to identify categories and themes. From this codebook, the research team drafted a survey instrument (the complete qualitative analysis occurred after survey development). To maintain focus on systematic quality improvement, items related to perceived mismanagement, relationship tensions, and professionalism were excluded. The survey was pilot‐tested with 5 faculty physicians and 2 nursing staff, prompting several modifications to improve clarity. Primary demographic items included provider role (nurse, attending physician, or housestaff physician) and years in current role. The 24 survey items were grouped into 5 different categories: (1) Quality of Care Delivery, (2) Communication and Coordination, (3) Staffing and Supervision, (4) Patient Transfers, and (5) Consulting Service Issues. Each item was investigated on a 7‐point scale (1=lowest rating, 7=highest rating). Descriptive text was provided at the extremes (choices 1 and 7), whereas intermediary values (26) did not have descriptive cues. The descriptive anchors for Quality of Care Delivery and Patient Transfers were 1=never and 7=always, whereas the descriptive anchors Communication and Coordination and Staffing and Supervision were 1=poor and 7=superior; Consulting Service Issues used a mix of both. Providers with off‐hours experience were asked to rank 4 time periods (710 pm, 10 pm1 am, 14 am, 47 am) regarding quality of care delivery in the medicine units (1=best, 4=worst). We asked both daytime and nighttime providers about perceptions of off‐hours care because, given the boundary spanning the nature of medical care across work shifts, daytime providers frequently identify issues not apparent until hours (or even days) after completion of a night shift. A similar design was used in prior work investigating safety at night.[17]
Quantitative Data Collection
In June of 2013, we emailed a survey link (
Data Analysis
Using the preliminary codebook, 2 investigators (J.D.G., E.M.) jointly analyzed a segment of the dataset using Atlas.ti 6.0 (Scientific Software, Berlin, Germany). Two investigators independently coded the data, compared codes for agreement, and updated the codebook. The remaining data were coded independently, with regular adjudication sessions to modify the codebook. All investigators reviewed and agreed upon themes and representative quotations.
Descriptive statistics, Pearson correlation statistics, Kruskal‐Wallis tests, and signed rank tests (with Bonferroni correction) were used to report group characteristics, correlate rank order, make comparisons between groups (nursing staff, and attending and housestaff physicians; day/night providers), and compare quality rankings by time period, respectively. The data were analyzed using SAS 9.3 (SAS Institute Inc., Cary, NC) and Stata/IC‐8 (StataCorp, College Park, TX).
RESULTS
Qualitative Analysis of Off‐Hours' Adverse Events and Near Misses
A total of 190 events were reported by daytime attending physicians (n=100), nocturnists (n=60), and nighttime charge nurses (n=30). Although questions asked participants to describe near misses/adverse events, respondents also reported a number of global quality issues not related to specific events. Similarly, debriefing sessions with housestaff (n=5) addressed both specific overnight events and residency‐related issues. Seven themes were identified: (1) perceived mismanagement, (2) quality of delivery processes, (3) communication and coordination, (4) staffing and supervision, (5) patient transfers, (6) consulting service issues, and, (7) professionalism/relational tensions. Table 1 lists the code frequencies and exemplary quotations.
| Category and Themes | Code Frequency No. (% of 322) | Representative Quotation |
|---|---|---|
| ||
| Perceived mismanagement | 97 (30) | We had a new admission to the general medicine unit with atrial flutter and rapid ventricular response who did not receive rate controlling agents but rather received diuretics. [The patient's] heart rate remained between 110 and 130 overnight, with a troponin rise in the am likely from demand. The attending note states rate controllers and discussed with housestaff, but this was not performed. |
| Quality of delivery processes | 63 (20) | One patient had a delay in MRI scanning in the off hours due to the scanner being down and scheduling. When the patient went down, there seemed to be little attempt to make sure patient went through scanner; unclear if housestaff called or not to come to assist. Now, the delay in care is even further along. |
| Communication and coordination | 50 (16) | A patient was transferred to the intermediate care unit with hypercarbic respiratory failure. The patient had delay of >1 hour to receive IV Bumex because pharmacy would not release the dose from Pyxis, and the nurse did not let us know there was a delay. When I asked the nurse why, she responded because she's not the only patient I have. I pointed out that the patient was in failure and needed Bumex, stat. If we had not clearly communicated either verbally or via computer, she should let us know how to do that better. |
| Staffing and supervision | 39 (12) | A patient was admitted DNR/DNI with advanced dementia, new on BiPaP at 100%, and hypotensive. The team's intern [identified] the need for interventions, including a central line. This was discussed with overloaded intensive care unit resident. The intern struggled until another resident assisted along with the night attending. Issues included: initial triage, no resident backup for team, and attending backup. I should have been more hands on in the moment to assist the intern navigating the system of care. Many issues here, but no senior resident was involved in care until [late]. |
| Patient transfers | 38 (12) | One patient went from the emergency department [to us] on the 5th floor at 7:45 pm. The ED placed an order for packed red blood cells and it was written at 4:45 pm. When patient arrived on our floor at 7:45 pm, the transfusion had not been started. The floor nurse started it at 8:10 pm . |
| Consulting services | 18 (6) | Regarding a new outside hospital transfer, the medicine team was informed that [the consulting service] would place official consult on the chart when imaging studies from the outside institution were available. Despite this, the consult was still not done after 36 hours, and [we are] still waiting. We contacted service several times. |
| Professionalism and relational tensions | 17 (5) | [One admission from the emergency department] involved a patient who received subcutaneous insulin for hyperkalemia as opposed to intravenous insulin. When brought to [their] attention, they became very confrontational and abrupt and denied having ordered or administered it that way, although it was documented in the EMR. |
Perceived Mismanagement
Participants commonly questioned the decision making, diagnosis, or management of off‐hours providers. Concerns included the response to acute illness (eg, delay in calling a code), treatment decisions (eg, diuresis in a patient with urinary retention), or omission of necessary actions (eg, no cultures ordered for septicemia).
Quality of Delivery Processes
Participants frequently described quality of care delivery issues primarily related to timeliness or delays in delivery processes (34/63 coding references), or patient safety issues (29/63 coding references). Described events revealed concerns about the timeliness of lab reporting, imaging, blood draws, and medication ordering/processing.
Communication and Coordination
Breakdowns in communication and coordination often threatened patient safety. Identified issues included poor communication between primary physicians, nurses, consulting services, and emergency department (ED) providers, as well as documentation within the electronic medical record.
Staffing and Supervision
Several events highlighted staffing or supervision limitations, such as perceived low nursing or physician staffing levels. The degree of nocturnist supervision was polarizing, with both increased and decreased levels of supervision reported as limiting care delivery (or housestaff education).
Patient Transfers
Patient transfers to medicine units from the ED, other inpatient units, or outside hospitals, were identified several times as an influential factor. The care transition and need for information exchange led to a perceived compromise in quality or safety.
Consulting Service Issues
Several examples highlighted perceived issues related to the communication, coordination, or timeliness of consultant services in providing care.
Professionalism/Relational Tensions
Last, providers described situations in which they perceived lack of professionalism or relational tensions between providers, either in regard to interactions or clinical decisions in patient care.
Quantitative Results
Of 214 surveys sent, data were collected from 160 respondents (75% response), including 64/101 nursing staff (63% response), 25/28 attending physicians (80% response), and 71/85 housestaff physicians (84% response). Table 2 describes the participant demographics.
| Variable | No. (%) |
|---|---|
| |
| Nursing staff | 64 (40) |
| Intermediate care unit | 20 |
| General medicine ward | 44 |
| All night shifts | 16 |
| Mix of day and night shifts | 26 |
| Years of experience, mean (SD) | 7.7 (9.7) |
| Attending physicians | 25 (16) |
| No. providing care only at night | 4 |
| No. of weeks as overnight hospitalist in past year, mean (SD) | 11.5 (4.1) |
| No. providing care only during the day | 21 |
| Years since residency graduation, mean (SD) | 9.0 (8.5) |
| Medicine residents | 71 (44) |
| Intern | 27 |
| Junior resident | 23 |
| Senior resident* | 21 |
Off‐Hours Quality and Safety Issues
Ratings and comparisons of the 24 items are shown in Table 3. For all items, the mean rating was below 5 (7‐point scale). Lowest‐rated (least optimal) items were: timeliness, safety, and communication involved with patients admitted from the ED, number of attending physicians, and timeliness of consults and blood draws. Highest‐rated (more optimal) items were: timely reporting of labs, timely identification of deteriorating status, medication ordering and processing, communication between physicians, and safety and communication involved with intraservice transfers.
| Category and Survey Item, Mean (SD)* | Total (160) | Providers With Night Experience | Nighttime Providers (116) | Daytime Providers (44) | P Value | |||
|---|---|---|---|---|---|---|---|---|
| Nurses (41) | Attending Physicians (4) | Housestaff (71) | P Value | |||||
| ||||||||
| Quality of care delivery | ||||||||
| Timely reporting of labs at night | 4.70 (1.39) | 5.12 (1.50) | 4.50 (1.00) | 4.61 (1.47) | 0.11 | 4.78 (1.48) | 4.48 (1.11) | 0.09 |
| Timely identification of deteriorating status | 4.67 (1.34) | 4.88 (1.36) | 5.00 (0.82) | 4.85 (1.20) | 0.93 | 4.86 (1.24) | 4.16 (1.45) | 0.006 |
| Medication ordering and processing | 4.63 (1.13) | 4.88 (1.25) | 5.25 (0.50) | 4.66 (1.08) | 0.19 | 4.76 (1.13) | 4.27 (1.06) | 0.01 |
| Timely completion of imaging at night | 4.29 (1.32) | 4.32 (1.46) | 4.75 (0.96) | 4.39 (1.29) | 0.88 | 4.38 (1.34) | 4.05 (1.26) | 0.12 |
| Timely reporting of results at night | 4.19 (1.43) | 4.27 (1.53) | 4.00 (1.83) | 4.11 (1.44) | 0.84 | 4.16 (1.47) | 4.27 (1.30) | 0.76 |
| Timely med release from pharmacy at night | 4.16 (1.29) | 4.00 (1.32) | 4.50 (0.58) | 4.28 (1.29) | 0.44 | 4.19 (1.28) | 4.09 (1.31) | 0.90 |
| Timely blood draws at night | 3.96 (1.52) | 4.63 (1.44) | 4.50 (0.58) | 3.53 (1.49) | <0.001 | 3.96 (1.54) | 3.98 (1.47) | 0.98 |
| Communication and coordination | ||||||||
| Communication between physicians | 4.63 (1.26) | 4.29 (1.23) | 6.00 (1.15) | 5.14 (1.12) | <0.001 | 4.87 (1.24) | 3.98 (1.09) | <0.001 |
| Communication between nursing and pharmacy | 4.39 (1.27) | 4.83 (1.41) | 5.00 (0.82) | 4.27 (1.29) | 0.04 | 4.49 (1.34) | 4.11 (4.11) | 0.08 |
| Communication between nursing and physicians | 4.39 (1.28) | 4.44 (1.36) | 5.00 (0.82) | 4.58 (1.31) | 0.64 | 4.54 (1.31) | 3.98 (1.13) | 0.01 |
| Documentation in medical record | 4.33 (1.36) | 5.00 (1.36) | 6.00 (0.82) | 4.23 1.19) | <0.001 | 4.56 (1.31) | 3.70 (1.30) | <0.001 |
| Ease of contacting primary providers at night | 4.31 (1.29) | 4.46 (1.27) | 6.00 (0.00) | 4.54 (1.18) | 0.02 | 4.56 (1.22) | 3.66 (1.27) | <0.001 |
| Staffing and supervision | ||||||||
| No. of nursing staff | 4.51 (1.27) | 4.54 (1.50) | 5.50 (0.58) | 4.59 (1.21) | 0.25 | 4.60 (1.31) | 4.25 (1.14) | 0.025 |
| Supervision of housestaff | 4.43 (1.34) | 4.56 (1.40) | 6.25 (0.50) | 4.55 (1.34) | 0.03 | 4.61 (1.37) | 3.95 (1.14) | 0.002 |
| No. of housestaff | 4.09 (1.39) | 4.27 (1.40) | 4.50 (1.29) | 4.11 (1.44) | 0.70 | 4.18 (1.41) | 3.86 (1.32) | 0.12 |
| No. of ancillary staff | 4.00 (1.40) | 4.27 (1.53) | 5.75 (0.96) | 3.85 (1.40) | 0.02 | 4.06 (1.48) | 3.84 (1.18) | 0.27 |
| No. of attending physicians | 3.79 (1.50) | 3.49 (1.76) | 5.25 (0.96) | 3.89 (1.43) | 0.07 | 3.79 (1.57) | 3.80 (1.32) | 0.98 |
| Patient transfers | ||||||||
| For patients accepted to medicine from another medicine unit | ||||||||
| Timely and safe patient transfers | 4.56 (1.28) | 5.15 (1.11) | 4.75 (0.50) | 4.55 (1.23) | 0.025 | 4.77 (1.20) | 4.00 (1.33) | 0.001 |
| High quality communication between providers | 4.55 (1.35) | 5.34 (1.13) | 5.00 (0.82) | 4.49 (1.22) | 0.001 | 4.81 (1.24) | 3.86 (1.41) | <0.001 |
| For patients admitted from emergency department to medicine unit | ||||||||
| Appropriate testing and treatment | 4.16 (1.34) | 4.15 (1.30) | 4.00 (1.83) | 4.21 (1.43) | 0.96 | 4.18 (1.39) | 4.11 (1.20) | 0.66 |
| Timely and safe transfers | 3.89 (1.38) | 3.63 (1.50) | 5.50 (0.58) | 4.08 (1.32) | 0.02 | 3.97 (1.40) | 3.68 1.29) | 0.23 |
| High‐quality communication between providers | 2.93 (1.38) | 2.56 (1.23) | 3.75 (1.26) | 3.00 (1.39) | 0.08 | 2.87 (1.35) | 3.07 (1.47) | 0.41 |
| Consulting service issues | ||||||||
| Timely consults at night | 4.04 (1.35) | 4.27 (1.28) | 4.00 (0.82) | 4.10 (1.47) | 0.69 | 4.16 (1.38) | 3.73 (1.25) | 0.053 |
| Communication between consults and physicians | 3.93 (1.40) | 3.46 (1.45) | 5.75 (1.26) | 4.35 (1.27) | <0.001 | 4.09 (1.42) | 3.50 (1.27) | 0.016 |
Comparisons Between Professional Groups With Night Experience
Of the 24 items, 11 showed statistically significant differences between groups (P<0.05). Items with the largest difference between groups included: timely blood draws at night (housestaff physicians lowest), communication between physicians (nursing lowest), documentation in medical record (housestaff physicians lowest), and communication between consults and physicians (nursing lowest). The rank order between housestaff physicians and nurses, and housestaff and attending physicians showed moderately positive correlations (r=0.61, P=0.002 and r=0.47, P=0.022, respectively). The correlation between nurses and attending physicians showed a weak correlation (r=0.19, P=0.375).
Comparisons Between Front‐Line Providers With and Without Night Experience
Of the 24 items, 12 showed statistically significant differences between groups (P<0.05), with day providers reporting lower ratings in all 12. Items with the largest difference between groups included: communication between consults and physicians, ease of contacting providers, communication between providers, documentation, and safety and communication related to transfers from other units. The rank order between night and day groups showed a statistically significant positive correlation (r=0.65, P=0.001).
Perceived Highest Quality of Care Time Period During Off Hours
Compared with other time periods, all providers ranked 4 to 7 am as the period with the lowest quality of care delivery (mean rank 3.2, P0.001) (Figure 1). Nursing staff and attending physicians both ranked the 10 pm to 1 am time period as the best period (mean of 2.0 and 1.5, respectively), whereas housestaff physicians ranked the 7 to 10 pm as the best time period (mean 1.62). The only statistical difference between provider groups for any given time period was the 7 to 10 pm time period (P=0.002).
DISCUSSION
In this prospective, mixed‐methods study evaluating perceived off‐hours quality and safety issues, several themes were identified, including perceived mismanagement, insufficient quality of delivery processes, communication/coordination breakdowns, and staffing and supervision issues. In the quantitative analysis, lowest‐rated items (lowest quality) related to timeliness/safety/communication involved with ED transfers, number of attending physicians, and timeliness of consults and blood draws. Highest‐rated items (highest quality) related to timeliness of lab reporting and identification of deteriorating patients, medication ordering/processing, communication between physicians, and safety/communication during intraservice transfers. In general, day providers reported lower ratings than night providers on nearly all quality‐related items. Nursing staff reported the lowest ratings regarding communication between physicians and consults, whereas housestaff physicians reported the lowest ratings regarding documentation in the medical record and timely blood draws. These between‐group differences reveal the lack of shared conceptual understanding regarding off‐hours care delivery.
Our qualitative results reveal several significant issues related to care delivery during off hours, many of which are not obtainable by hospital‐level data or chart review.[18] For hospital‐based medicine units, an understanding of the structure‐ and process‐related factors associated with events is required for quality improvement efforts. Although the primary focus for this work was the off hours, it is plausible that providers may have identified similar issues as important issues during daytime hours. Our study was not designed to investigate if these perceived issues are specific to off hours, or if these issues are an accurate reflection of objective events occurring during this time period. We believe this topic deserves further investigation, as understanding if these off‐hours perceptions are unique to this time period would change the scope of future quality improvement initiatives.
The most significant finding in the quantitative results was the vulnerability in quality and safety during patient admissions from the ED, specifically in relation to communication and timeliness of transfer. Between‐unit handoffs for patients admitted from the ED to medicine units have been identified as particularly vulnerable to breakdowns in the communication process.[19, 20, 21, 22] There are multiple etiologies, including clinical uncertainty, higher acuity in patient illness early in hospitalization, and cultural differences between services.[23] Additionally, patterns of communication and standardized handoff processes are often insufficient. In our hospital system, the transfer process relies primarily upon synchronous communication methods without standardized, asynchronous information exchange. We hypothesize front‐line providers perceive this lack of standardization as a primary threat to quality. Because approximately 60% of new patient admissions from the ED to medicine service (both in our hospital and in prior studies) occur during off hours, these findings highlight a need for subsequent study and quality improvement efforts.[24]
During the time of this study, our medicine units were staffed at night by 5 medicine housestaff physicians and 1 academic hospitalist, or nocturnist. In efforts to improve quality and safety during off hours, our hospital, as well as other health systems, implemented the nocturnist position, a faculty‐level attending physician to provide off‐hours clinical care and housestaff supervision.[25] Although participants reported a moderate rating of housestaff supervision, participants provided lower scores for staffing numbers of nurses, and housestaff and attending physicians, despite nocturnist presence. With both increased off‐hours supervision in our hospital and increasing use of faculty‐level physicians in other academic programs, these results provide context for the anticipated level of overnight housestaff supervision.[26, 27] To our knowledge, this is the first study to investigate perceived overnight quality issues on medicine units following such staffing models. Although this model of direct, on‐site supervision in academic medicine programs may help offset staffing and supervisory issues during off hours, the nocturnist role is insufficient to offset threats to quality/safety already inherent within the system. Furthermore, prospective trials following implementation of nocturnist systems have shown mixed results in improving patient outcomes.[28] These findings have led some to question whether resources dedicated to nocturnist staffing may be better allocated to other overnight initiatives, highlighting the need for a more subtle understanding of quality issues to design targeted interventions.[29]
A notable finding from this work is that providers without night experience reported lower scores for 20 of 24 items, highlighting their perceptions of the quality of care delivery during off hours are lower than those who experience this environment. Although day providers are not directly experiencing off‐hours delivery processes, these providers receive and detect the results from care delivery at night.[17] Most nurse, physician, and hospital leaders are present in the hospital only during day hours, requiring these individuals to account for differences in perceived and actual care delivered overnight.[1] These individuals make critical decisions pertaining to process changes and quality improvement efforts in these units. We believe these results raise awareness for leadership decisions and quality improvement efforts in medicine service units, specifically to focus on overnight issues beyond staffing issues alone.
All respondent groups ranked the latter half of the shift (17 am) as lower in quality compared to the first 6 hours (7 pm1 am). This finding is contrary to our hypothesis that earlier time periods, during the majority of patient admissions (and presumed higher workload for all providers), would be perceived as lower quality. Reasons for this finding are unknown, but may relate to end‐of‐shift tasks, sign‐out preparation, provider fatigue, or disease‐related concerns (eg, increased incidence of stroke and myocardial infarction) during the latter portions of night shifts. One study identified a decrease in nursing clinical judgments from the beginning to end of 12‐hour shifts, with a potential suggested mechanism of decrease in ability to maintain attention during judgments.[30] Additionally, in a study by Folkard et al., risk was highest within the first several hours and fell substantially thereafter during a shift.[9] To our knowledge, no work has investigated perceived or objective quality outcomes by time period during the off‐hours shift in medicine units. Further work could help delineate why provider‐perceived compromises in quality occur late in off‐hours shifts and whether this correlates to safety events.
There are several limitations to our study. First, although all surveys were pilot tested for content validity, the construct validity was not rigorously assessed. Second, although data were collected from all participant groups, the collection methods were unbalanced, favoring attending‐level physician perspectives. Although the relative incidence of vulnerabilities in quality and safety should be interpreted with caution, our methods and general taxonomy provide a framework for developing and monitoring the perceptions of future interventions. Due to limitations in infrastructure, our findings could not be independently validated through review of reported adverse events, but previous investigations have found the vast majority of adverse events are not detected by standard anonymous reporting.[31, 32, 33] Our methodology (used in our prior work) may provide an independent means of detecting causes of poor quality not easily observed through routine surveillance.[22] Although many survey items showed statistical differences between provider groups, the clinical significance is subject to interpretation. Last, the perceptions and events related to our institution may not be fully generalizable to other academic programs or service lines, particularly in community‐based, nonteaching hospitals.
In conclusion, our results suggest a significant discrepancy between the concerns of day and night providers regarding the quality of care delivered to inpatients during the off hours, specifically with issues related to communication, quality‐of‐care delivery processes, and patient transfers from the ED. Although specific concerns may be institution‐ (and service line‐) dependent, appropriately designing initiatives to improve the quality of care delivered overnight will need to take the perspectives of both provider groups into account. Additionally, educational initiatives should focus on achieving a shared mental model among all providers to improve collaboration and performance.
Acknowledgements
The authors thank the nurses, internal medicine housestaff physicians, and general internal medicine attending physicians at the Penn State Hershey Medical Center for their participation in this study.
Disclosure: Nothing to report.
Patients experience acute illness at all hours of the day. In acute care hospitals, over 60% of patient admissions occur outside of normal business hours, or the off hours.[1, 2] Similarly, the acute decompensation of patients already admitted to hospital‐based units is frequent, with 90% of rapid responses occurring between 9 pm and 6 am.[3] Research suggests worse hospital performance during off hours, including increased patient falls, in‐hospital cardiac arrest mortality, and severity of hospital employee injuries.[2, 4, 5, 6, 7]
Although hospital‐based services should match care demand, the disparity between patient acuity and hospital capability at night is significant. Off hours typically have lower staffing of nurses, and attending and housestaff physicians, and ancillary staff as well as limited availability of consultative and supportive services.[8] Additionally, off‐hours providers are subject to the physiological effects of imbalanced circadian rhythms, including fatigue, attenuating their abilities to provide high‐quality care. The significant patient care needs mandate continuous patient care delivery without compromising quality or safety. To achieve this, further defining the barriers to delivering quality care during off hours is essential to improvement efforts in medicine‐based units.
Previous investigations have found increased occurrence and severity of worker accidents, increased potential for higher occurrence of preventable adverse patient events, and decreased performance during off hours.[4, 9, 10] Additionally, detrimental effects of off‐hours care may be further magnified by rotating employees through both day and night shifts, a common practice in academic hospitals.[11, 12] Potentially modifiable outcomes, such as patient fall rate and in‐hospital cardiac arrest survival differ markedly between day and night shifts.[6, 13] These studies primarily report on specific diseases, such as myocardial infarction and stroke, and are investigated from the perspective of hospital‐level outcomes.
To our knowledge, no study has reported provider‐perceived quality and safety issues occurring during off hours in an academic setting. Likewise, although off‐hours collaborative care requires shared, interprofessional conceptualization regarding care delivery, this perspective has not been reported. Understanding the similarities and differences between provider perceptions will allow the construction of an interprofessional team mental model, facilitating the design of future quality improvement initiatives.[14, 15] Our objectives were to: (1) identify off‐hours quality and safety issues, (2) assess which issues are perceived as most significant, and (3) evaluate differences in perceptions of these issues between nurses, and attending and housestaff physicians.
METHODS
Study Design
To investigate quality and safety issues occurring during off hours, we employed a prospective, mixed‐methods sequential exploratory study design, involving an initial qualitative analysis of adverse events followed by quantitative survey assessment.[16] We chose a mixed‐methods approach because provider‐perceived off‐hours issues had not been explicitly identified in the literature, requiring preliminary qualitative assessment. For the purpose of this study, we defined off hours as the 7 pm to 7am time period, which overlapped night shifts for both nurses and physicians. The study was approved by the institutional review board as a quality improvement project.
Study Setting
The study was conducted at a 378‐bed, university‐based acute care hospital in central Pennsylvania. There are a total of 64 internal medicine beds located in 2 units: a general medicine unit (44 beds, staffed by 60 nurses, nurse‐to‐patient ratio 1:4) and an intermediate care unit (20 beds, staffed by 41 nurses, nurse‐to‐patient ratio 1:3). The medicine residency program consists of 69 residents and 14 combined internal medicinepediatrics residents. During the day, 3 teaching teams and 1 nonteaching team care for all medicine patients. Overnight, 3 junior/senior level residents admit patients to the medicine service, whereas 2 interns provide cross‐coverage for all medicine and specialty service patients. Starting in September 2012 (before data collection), an overnight faculty‐level academic hospitalist, or nocturnist, provided on‐site housestaff supervision.
Qualitative Data Collection
For the qualitative analysis, we used 2 methods to develop our database. First, we created an electronic survey (see Supporting Information, Appendix 1, in the online version of this article) to identify near misses/adverse events occurring overnight, distributed to the nocturnist, 3 daytime hospitalists, and unit charge nurses following each shift (October 2012March 2013). The survey items were developed for the purpose of this study, with several items modified from a previously published survey.[17] Second, residency program directors recorded field notes during end‐of‐rotation debriefings (1 hour) with departing overnight housestaff, which were then dictated and transcribed. The subsequent analysis from these sources informed the quantitative survey (see Supporting Information, Appendix 2, in the online version of this article).
Survey Instrument
Three months after the initiation of qualitative data collection, 1 investigator (J.D.G.) developed a preliminary codebook to identify categories and themes. From this codebook, the research team drafted a survey instrument (the complete qualitative analysis occurred after survey development). To maintain focus on systematic quality improvement, items related to perceived mismanagement, relationship tensions, and professionalism were excluded. The survey was pilot‐tested with 5 faculty physicians and 2 nursing staff, prompting several modifications to improve clarity. Primary demographic items included provider role (nurse, attending physician, or housestaff physician) and years in current role. The 24 survey items were grouped into 5 different categories: (1) Quality of Care Delivery, (2) Communication and Coordination, (3) Staffing and Supervision, (4) Patient Transfers, and (5) Consulting Service Issues. Each item was investigated on a 7‐point scale (1=lowest rating, 7=highest rating). Descriptive text was provided at the extremes (choices 1 and 7), whereas intermediary values (26) did not have descriptive cues. The descriptive anchors for Quality of Care Delivery and Patient Transfers were 1=never and 7=always, whereas the descriptive anchors Communication and Coordination and Staffing and Supervision were 1=poor and 7=superior; Consulting Service Issues used a mix of both. Providers with off‐hours experience were asked to rank 4 time periods (710 pm, 10 pm1 am, 14 am, 47 am) regarding quality of care delivery in the medicine units (1=best, 4=worst). We asked both daytime and nighttime providers about perceptions of off‐hours care because, given the boundary spanning the nature of medical care across work shifts, daytime providers frequently identify issues not apparent until hours (or even days) after completion of a night shift. A similar design was used in prior work investigating safety at night.[17]
Quantitative Data Collection
In June of 2013, we emailed a survey link (
Data Analysis
Using the preliminary codebook, 2 investigators (J.D.G., E.M.) jointly analyzed a segment of the dataset using Atlas.ti 6.0 (Scientific Software, Berlin, Germany). Two investigators independently coded the data, compared codes for agreement, and updated the codebook. The remaining data were coded independently, with regular adjudication sessions to modify the codebook. All investigators reviewed and agreed upon themes and representative quotations.
Descriptive statistics, Pearson correlation statistics, Kruskal‐Wallis tests, and signed rank tests (with Bonferroni correction) were used to report group characteristics, correlate rank order, make comparisons between groups (nursing staff, and attending and housestaff physicians; day/night providers), and compare quality rankings by time period, respectively. The data were analyzed using SAS 9.3 (SAS Institute Inc., Cary, NC) and Stata/IC‐8 (StataCorp, College Park, TX).
RESULTS
Qualitative Analysis of Off‐Hours' Adverse Events and Near Misses
A total of 190 events were reported by daytime attending physicians (n=100), nocturnists (n=60), and nighttime charge nurses (n=30). Although questions asked participants to describe near misses/adverse events, respondents also reported a number of global quality issues not related to specific events. Similarly, debriefing sessions with housestaff (n=5) addressed both specific overnight events and residency‐related issues. Seven themes were identified: (1) perceived mismanagement, (2) quality of delivery processes, (3) communication and coordination, (4) staffing and supervision, (5) patient transfers, (6) consulting service issues, and, (7) professionalism/relational tensions. Table 1 lists the code frequencies and exemplary quotations.
| Category and Themes | Code Frequency No. (% of 322) | Representative Quotation |
|---|---|---|
| ||
| Perceived mismanagement | 97 (30) | We had a new admission to the general medicine unit with atrial flutter and rapid ventricular response who did not receive rate controlling agents but rather received diuretics. [The patient's] heart rate remained between 110 and 130 overnight, with a troponin rise in the am likely from demand. The attending note states rate controllers and discussed with housestaff, but this was not performed. |
| Quality of delivery processes | 63 (20) | One patient had a delay in MRI scanning in the off hours due to the scanner being down and scheduling. When the patient went down, there seemed to be little attempt to make sure patient went through scanner; unclear if housestaff called or not to come to assist. Now, the delay in care is even further along. |
| Communication and coordination | 50 (16) | A patient was transferred to the intermediate care unit with hypercarbic respiratory failure. The patient had delay of >1 hour to receive IV Bumex because pharmacy would not release the dose from Pyxis, and the nurse did not let us know there was a delay. When I asked the nurse why, she responded because she's not the only patient I have. I pointed out that the patient was in failure and needed Bumex, stat. If we had not clearly communicated either verbally or via computer, she should let us know how to do that better. |
| Staffing and supervision | 39 (12) | A patient was admitted DNR/DNI with advanced dementia, new on BiPaP at 100%, and hypotensive. The team's intern [identified] the need for interventions, including a central line. This was discussed with overloaded intensive care unit resident. The intern struggled until another resident assisted along with the night attending. Issues included: initial triage, no resident backup for team, and attending backup. I should have been more hands on in the moment to assist the intern navigating the system of care. Many issues here, but no senior resident was involved in care until [late]. |
| Patient transfers | 38 (12) | One patient went from the emergency department [to us] on the 5th floor at 7:45 pm. The ED placed an order for packed red blood cells and it was written at 4:45 pm. When patient arrived on our floor at 7:45 pm, the transfusion had not been started. The floor nurse started it at 8:10 pm . |
| Consulting services | 18 (6) | Regarding a new outside hospital transfer, the medicine team was informed that [the consulting service] would place official consult on the chart when imaging studies from the outside institution were available. Despite this, the consult was still not done after 36 hours, and [we are] still waiting. We contacted service several times. |
| Professionalism and relational tensions | 17 (5) | [One admission from the emergency department] involved a patient who received subcutaneous insulin for hyperkalemia as opposed to intravenous insulin. When brought to [their] attention, they became very confrontational and abrupt and denied having ordered or administered it that way, although it was documented in the EMR. |
Perceived Mismanagement
Participants commonly questioned the decision making, diagnosis, or management of off‐hours providers. Concerns included the response to acute illness (eg, delay in calling a code), treatment decisions (eg, diuresis in a patient with urinary retention), or omission of necessary actions (eg, no cultures ordered for septicemia).
Quality of Delivery Processes
Participants frequently described quality of care delivery issues primarily related to timeliness or delays in delivery processes (34/63 coding references), or patient safety issues (29/63 coding references). Described events revealed concerns about the timeliness of lab reporting, imaging, blood draws, and medication ordering/processing.
Communication and Coordination
Breakdowns in communication and coordination often threatened patient safety. Identified issues included poor communication between primary physicians, nurses, consulting services, and emergency department (ED) providers, as well as documentation within the electronic medical record.
Staffing and Supervision
Several events highlighted staffing or supervision limitations, such as perceived low nursing or physician staffing levels. The degree of nocturnist supervision was polarizing, with both increased and decreased levels of supervision reported as limiting care delivery (or housestaff education).
Patient Transfers
Patient transfers to medicine units from the ED, other inpatient units, or outside hospitals, were identified several times as an influential factor. The care transition and need for information exchange led to a perceived compromise in quality or safety.
Consulting Service Issues
Several examples highlighted perceived issues related to the communication, coordination, or timeliness of consultant services in providing care.
Professionalism/Relational Tensions
Last, providers described situations in which they perceived lack of professionalism or relational tensions between providers, either in regard to interactions or clinical decisions in patient care.
Quantitative Results
Of 214 surveys sent, data were collected from 160 respondents (75% response), including 64/101 nursing staff (63% response), 25/28 attending physicians (80% response), and 71/85 housestaff physicians (84% response). Table 2 describes the participant demographics.
| Variable | No. (%) |
|---|---|
| |
| Nursing staff | 64 (40) |
| Intermediate care unit | 20 |
| General medicine ward | 44 |
| All night shifts | 16 |
| Mix of day and night shifts | 26 |
| Years of experience, mean (SD) | 7.7 (9.7) |
| Attending physicians | 25 (16) |
| No. providing care only at night | 4 |
| No. of weeks as overnight hospitalist in past year, mean (SD) | 11.5 (4.1) |
| No. providing care only during the day | 21 |
| Years since residency graduation, mean (SD) | 9.0 (8.5) |
| Medicine residents | 71 (44) |
| Intern | 27 |
| Junior resident | 23 |
| Senior resident* | 21 |
Off‐Hours Quality and Safety Issues
Ratings and comparisons of the 24 items are shown in Table 3. For all items, the mean rating was below 5 (7‐point scale). Lowest‐rated (least optimal) items were: timeliness, safety, and communication involved with patients admitted from the ED, number of attending physicians, and timeliness of consults and blood draws. Highest‐rated (more optimal) items were: timely reporting of labs, timely identification of deteriorating status, medication ordering and processing, communication between physicians, and safety and communication involved with intraservice transfers.
| Category and Survey Item, Mean (SD)* | Total (160) | Providers With Night Experience | Nighttime Providers (116) | Daytime Providers (44) | P Value | |||
|---|---|---|---|---|---|---|---|---|
| Nurses (41) | Attending Physicians (4) | Housestaff (71) | P Value | |||||
| ||||||||
| Quality of care delivery | ||||||||
| Timely reporting of labs at night | 4.70 (1.39) | 5.12 (1.50) | 4.50 (1.00) | 4.61 (1.47) | 0.11 | 4.78 (1.48) | 4.48 (1.11) | 0.09 |
| Timely identification of deteriorating status | 4.67 (1.34) | 4.88 (1.36) | 5.00 (0.82) | 4.85 (1.20) | 0.93 | 4.86 (1.24) | 4.16 (1.45) | 0.006 |
| Medication ordering and processing | 4.63 (1.13) | 4.88 (1.25) | 5.25 (0.50) | 4.66 (1.08) | 0.19 | 4.76 (1.13) | 4.27 (1.06) | 0.01 |
| Timely completion of imaging at night | 4.29 (1.32) | 4.32 (1.46) | 4.75 (0.96) | 4.39 (1.29) | 0.88 | 4.38 (1.34) | 4.05 (1.26) | 0.12 |
| Timely reporting of results at night | 4.19 (1.43) | 4.27 (1.53) | 4.00 (1.83) | 4.11 (1.44) | 0.84 | 4.16 (1.47) | 4.27 (1.30) | 0.76 |
| Timely med release from pharmacy at night | 4.16 (1.29) | 4.00 (1.32) | 4.50 (0.58) | 4.28 (1.29) | 0.44 | 4.19 (1.28) | 4.09 (1.31) | 0.90 |
| Timely blood draws at night | 3.96 (1.52) | 4.63 (1.44) | 4.50 (0.58) | 3.53 (1.49) | <0.001 | 3.96 (1.54) | 3.98 (1.47) | 0.98 |
| Communication and coordination | ||||||||
| Communication between physicians | 4.63 (1.26) | 4.29 (1.23) | 6.00 (1.15) | 5.14 (1.12) | <0.001 | 4.87 (1.24) | 3.98 (1.09) | <0.001 |
| Communication between nursing and pharmacy | 4.39 (1.27) | 4.83 (1.41) | 5.00 (0.82) | 4.27 (1.29) | 0.04 | 4.49 (1.34) | 4.11 (4.11) | 0.08 |
| Communication between nursing and physicians | 4.39 (1.28) | 4.44 (1.36) | 5.00 (0.82) | 4.58 (1.31) | 0.64 | 4.54 (1.31) | 3.98 (1.13) | 0.01 |
| Documentation in medical record | 4.33 (1.36) | 5.00 (1.36) | 6.00 (0.82) | 4.23 1.19) | <0.001 | 4.56 (1.31) | 3.70 (1.30) | <0.001 |
| Ease of contacting primary providers at night | 4.31 (1.29) | 4.46 (1.27) | 6.00 (0.00) | 4.54 (1.18) | 0.02 | 4.56 (1.22) | 3.66 (1.27) | <0.001 |
| Staffing and supervision | ||||||||
| No. of nursing staff | 4.51 (1.27) | 4.54 (1.50) | 5.50 (0.58) | 4.59 (1.21) | 0.25 | 4.60 (1.31) | 4.25 (1.14) | 0.025 |
| Supervision of housestaff | 4.43 (1.34) | 4.56 (1.40) | 6.25 (0.50) | 4.55 (1.34) | 0.03 | 4.61 (1.37) | 3.95 (1.14) | 0.002 |
| No. of housestaff | 4.09 (1.39) | 4.27 (1.40) | 4.50 (1.29) | 4.11 (1.44) | 0.70 | 4.18 (1.41) | 3.86 (1.32) | 0.12 |
| No. of ancillary staff | 4.00 (1.40) | 4.27 (1.53) | 5.75 (0.96) | 3.85 (1.40) | 0.02 | 4.06 (1.48) | 3.84 (1.18) | 0.27 |
| No. of attending physicians | 3.79 (1.50) | 3.49 (1.76) | 5.25 (0.96) | 3.89 (1.43) | 0.07 | 3.79 (1.57) | 3.80 (1.32) | 0.98 |
| Patient transfers | ||||||||
| For patients accepted to medicine from another medicine unit | ||||||||
| Timely and safe patient transfers | 4.56 (1.28) | 5.15 (1.11) | 4.75 (0.50) | 4.55 (1.23) | 0.025 | 4.77 (1.20) | 4.00 (1.33) | 0.001 |
| High quality communication between providers | 4.55 (1.35) | 5.34 (1.13) | 5.00 (0.82) | 4.49 (1.22) | 0.001 | 4.81 (1.24) | 3.86 (1.41) | <0.001 |
| For patients admitted from emergency department to medicine unit | ||||||||
| Appropriate testing and treatment | 4.16 (1.34) | 4.15 (1.30) | 4.00 (1.83) | 4.21 (1.43) | 0.96 | 4.18 (1.39) | 4.11 (1.20) | 0.66 |
| Timely and safe transfers | 3.89 (1.38) | 3.63 (1.50) | 5.50 (0.58) | 4.08 (1.32) | 0.02 | 3.97 (1.40) | 3.68 1.29) | 0.23 |
| High‐quality communication between providers | 2.93 (1.38) | 2.56 (1.23) | 3.75 (1.26) | 3.00 (1.39) | 0.08 | 2.87 (1.35) | 3.07 (1.47) | 0.41 |
| Consulting service issues | ||||||||
| Timely consults at night | 4.04 (1.35) | 4.27 (1.28) | 4.00 (0.82) | 4.10 (1.47) | 0.69 | 4.16 (1.38) | 3.73 (1.25) | 0.053 |
| Communication between consults and physicians | 3.93 (1.40) | 3.46 (1.45) | 5.75 (1.26) | 4.35 (1.27) | <0.001 | 4.09 (1.42) | 3.50 (1.27) | 0.016 |
Comparisons Between Professional Groups With Night Experience
Of the 24 items, 11 showed statistically significant differences between groups (P<0.05). Items with the largest difference between groups included: timely blood draws at night (housestaff physicians lowest), communication between physicians (nursing lowest), documentation in medical record (housestaff physicians lowest), and communication between consults and physicians (nursing lowest). The rank order between housestaff physicians and nurses, and housestaff and attending physicians showed moderately positive correlations (r=0.61, P=0.002 and r=0.47, P=0.022, respectively). The correlation between nurses and attending physicians showed a weak correlation (r=0.19, P=0.375).
Comparisons Between Front‐Line Providers With and Without Night Experience
Of the 24 items, 12 showed statistically significant differences between groups (P<0.05), with day providers reporting lower ratings in all 12. Items with the largest difference between groups included: communication between consults and physicians, ease of contacting providers, communication between providers, documentation, and safety and communication related to transfers from other units. The rank order between night and day groups showed a statistically significant positive correlation (r=0.65, P=0.001).
Perceived Highest Quality of Care Time Period During Off Hours
Compared with other time periods, all providers ranked 4 to 7 am as the period with the lowest quality of care delivery (mean rank 3.2, P0.001) (Figure 1). Nursing staff and attending physicians both ranked the 10 pm to 1 am time period as the best period (mean of 2.0 and 1.5, respectively), whereas housestaff physicians ranked the 7 to 10 pm as the best time period (mean 1.62). The only statistical difference between provider groups for any given time period was the 7 to 10 pm time period (P=0.002).
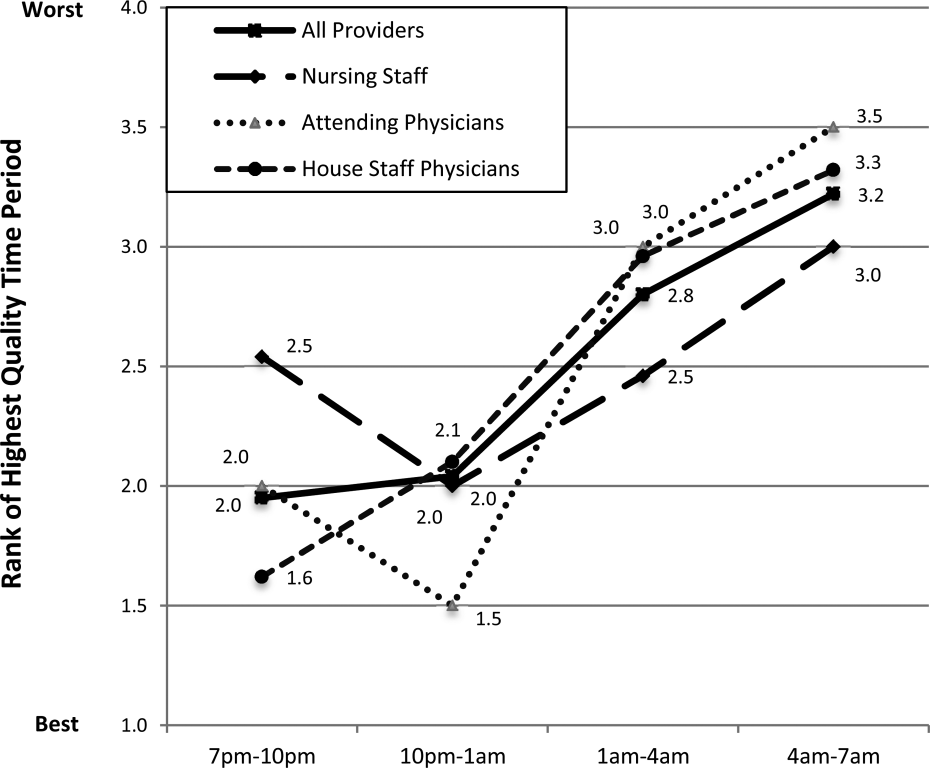
DISCUSSION
In this prospective, mixed‐methods study evaluating perceived off‐hours quality and safety issues, several themes were identified, including perceived mismanagement, insufficient quality of delivery processes, communication/coordination breakdowns, and staffing and supervision issues. In the quantitative analysis, lowest‐rated items (lowest quality) related to timeliness/safety/communication involved with ED transfers, number of attending physicians, and timeliness of consults and blood draws. Highest‐rated items (highest quality) related to timeliness of lab reporting and identification of deteriorating patients, medication ordering/processing, communication between physicians, and safety/communication during intraservice transfers. In general, day providers reported lower ratings than night providers on nearly all quality‐related items. Nursing staff reported the lowest ratings regarding communication between physicians and consults, whereas housestaff physicians reported the lowest ratings regarding documentation in the medical record and timely blood draws. These between‐group differences reveal the lack of shared conceptual understanding regarding off‐hours care delivery.
Our qualitative results reveal several significant issues related to care delivery during off hours, many of which are not obtainable by hospital‐level data or chart review.[18] For hospital‐based medicine units, an understanding of the structure‐ and process‐related factors associated with events is required for quality improvement efforts. Although the primary focus for this work was the off hours, it is plausible that providers may have identified similar issues as important issues during daytime hours. Our study was not designed to investigate if these perceived issues are specific to off hours, or if these issues are an accurate reflection of objective events occurring during this time period. We believe this topic deserves further investigation, as understanding if these off‐hours perceptions are unique to this time period would change the scope of future quality improvement initiatives.
The most significant finding in the quantitative results was the vulnerability in quality and safety during patient admissions from the ED, specifically in relation to communication and timeliness of transfer. Between‐unit handoffs for patients admitted from the ED to medicine units have been identified as particularly vulnerable to breakdowns in the communication process.[19, 20, 21, 22] There are multiple etiologies, including clinical uncertainty, higher acuity in patient illness early in hospitalization, and cultural differences between services.[23] Additionally, patterns of communication and standardized handoff processes are often insufficient. In our hospital system, the transfer process relies primarily upon synchronous communication methods without standardized, asynchronous information exchange. We hypothesize front‐line providers perceive this lack of standardization as a primary threat to quality. Because approximately 60% of new patient admissions from the ED to medicine service (both in our hospital and in prior studies) occur during off hours, these findings highlight a need for subsequent study and quality improvement efforts.[24]
During the time of this study, our medicine units were staffed at night by 5 medicine housestaff physicians and 1 academic hospitalist, or nocturnist. In efforts to improve quality and safety during off hours, our hospital, as well as other health systems, implemented the nocturnist position, a faculty‐level attending physician to provide off‐hours clinical care and housestaff supervision.[25] Although participants reported a moderate rating of housestaff supervision, participants provided lower scores for staffing numbers of nurses, and housestaff and attending physicians, despite nocturnist presence. With both increased off‐hours supervision in our hospital and increasing use of faculty‐level physicians in other academic programs, these results provide context for the anticipated level of overnight housestaff supervision.[26, 27] To our knowledge, this is the first study to investigate perceived overnight quality issues on medicine units following such staffing models. Although this model of direct, on‐site supervision in academic medicine programs may help offset staffing and supervisory issues during off hours, the nocturnist role is insufficient to offset threats to quality/safety already inherent within the system. Furthermore, prospective trials following implementation of nocturnist systems have shown mixed results in improving patient outcomes.[28] These findings have led some to question whether resources dedicated to nocturnist staffing may be better allocated to other overnight initiatives, highlighting the need for a more subtle understanding of quality issues to design targeted interventions.[29]
A notable finding from this work is that providers without night experience reported lower scores for 20 of 24 items, highlighting their perceptions of the quality of care delivery during off hours are lower than those who experience this environment. Although day providers are not directly experiencing off‐hours delivery processes, these providers receive and detect the results from care delivery at night.[17] Most nurse, physician, and hospital leaders are present in the hospital only during day hours, requiring these individuals to account for differences in perceived and actual care delivered overnight.[1] These individuals make critical decisions pertaining to process changes and quality improvement efforts in these units. We believe these results raise awareness for leadership decisions and quality improvement efforts in medicine service units, specifically to focus on overnight issues beyond staffing issues alone.
All respondent groups ranked the latter half of the shift (17 am) as lower in quality compared to the first 6 hours (7 pm1 am). This finding is contrary to our hypothesis that earlier time periods, during the majority of patient admissions (and presumed higher workload for all providers), would be perceived as lower quality. Reasons for this finding are unknown, but may relate to end‐of‐shift tasks, sign‐out preparation, provider fatigue, or disease‐related concerns (eg, increased incidence of stroke and myocardial infarction) during the latter portions of night shifts. One study identified a decrease in nursing clinical judgments from the beginning to end of 12‐hour shifts, with a potential suggested mechanism of decrease in ability to maintain attention during judgments.[30] Additionally, in a study by Folkard et al., risk was highest within the first several hours and fell substantially thereafter during a shift.[9] To our knowledge, no work has investigated perceived or objective quality outcomes by time period during the off‐hours shift in medicine units. Further work could help delineate why provider‐perceived compromises in quality occur late in off‐hours shifts and whether this correlates to safety events.
There are several limitations to our study. First, although all surveys were pilot tested for content validity, the construct validity was not rigorously assessed. Second, although data were collected from all participant groups, the collection methods were unbalanced, favoring attending‐level physician perspectives. Although the relative incidence of vulnerabilities in quality and safety should be interpreted with caution, our methods and general taxonomy provide a framework for developing and monitoring the perceptions of future interventions. Due to limitations in infrastructure, our findings could not be independently validated through review of reported adverse events, but previous investigations have found the vast majority of adverse events are not detected by standard anonymous reporting.[31, 32, 33] Our methodology (used in our prior work) may provide an independent means of detecting causes of poor quality not easily observed through routine surveillance.[22] Although many survey items showed statistical differences between provider groups, the clinical significance is subject to interpretation. Last, the perceptions and events related to our institution may not be fully generalizable to other academic programs or service lines, particularly in community‐based, nonteaching hospitals.
In conclusion, our results suggest a significant discrepancy between the concerns of day and night providers regarding the quality of care delivered to inpatients during the off hours, specifically with issues related to communication, quality‐of‐care delivery processes, and patient transfers from the ED. Although specific concerns may be institution‐ (and service line‐) dependent, appropriately designing initiatives to improve the quality of care delivered overnight will need to take the perspectives of both provider groups into account. Additionally, educational initiatives should focus on achieving a shared mental model among all providers to improve collaboration and performance.
Acknowledgements
The authors thank the nurses, internal medicine housestaff physicians, and general internal medicine attending physicians at the Penn State Hershey Medical Center for their participation in this study.
Disclosure: Nothing to report.
- . Like night and day—shedding light on off‐hours care. N Engl J Med. 2008;358(20):2091–2093.
- , , , . Call nights and patient care. J Gen Intern Med. 1992;7(4):405–410.
- , , , et al. Uncovering system errors using a rapid response team: cross‐coverage caught in the crossfire. Discussion. J Trauma. 2009;67(1):173–179.
- , . The impact of shift work on the risk and severity of injuries for hospital employees: an analysis using Oregon workers' compensation data. Occup Med (Lond). 2004;54(8):556–563.
- , . Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668.
- , , , et al. The association of shift‐level nurse staffing with adverse patient events. J Nurs Adm. 2011;41(2):64–70.
- , , , et al. Heart disease and stroke statistics—2010 update A report from the American Heart Association. Circulation. 2010;121(7):e46–e215.
- , , , , O'Neil E. Minimum Nurse Staffing Ratios In California Acute Care Hospitals. Oakland, CA: California Workforce Initiative; 2000.
- , . Shift work, safety and productivity. Occup Med (Lond). 2003;53(2):95–101.
- , , . Increased injuries on night shift. Lancet. 1994;344(8930):1137–1139.
- , . Shift and night work and long working hours‐a systematic review of safety implications. Scand J Work Environ Health. 2011:37(3):173–185.
- , , , et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82(7):1011–1014.
- , , , et al. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792.
- , , , , . The influence of shared mental models on team process and performance. J Appl Psychol. 2000;85(2):273.
- , . Team mental models and their potential to improve teamwork and safety: a review and implications for future research in healthcare. Saf Sci. 2012;50(5):1344–1354.
- . Editorial: mapping the field of mixed methods research. J Mix Methods Res. 2009;3(2):95–108.
- , . Decreasing adverse events through night talks: an interdisciplinary, hospital‐based quality improvement project. Perm J. Fall 2009;13(4):16–22.
- , , , et al. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff (Millwood). 2011;30(4):581–589.
- , , , , , . Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701–710.e704.
- . Smoothing transitions. Joint Commission targets patient handoffs. Mod Healthc. 2010;40(43):8–9.
- , , , , , . The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med. 2012;87(4):411–418.
- , , , , , . Patient care transitions from the emergency department to the medicine ward: evaluation of a standardized electronic signout tool. Int J Qual Health Care. 2014;26(4):337–347.
- , . The unappreciated challenges of between‐unit handoffs: negotiating and coordinating across boundaries. Ann Emerg Med. 2013;61(2):155–160.
- , , , , , . The association between night or weekend admission and hospitalization‐relevant patient outcomes. J Hosp Med. 2011;6(1):10–14.
- . Middle‐of‐the‐night medicine is rarely patient‐centred. CMAJ. 2011;183(13):1467–1468.
- , , , et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521–523.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- , , , et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209.
- . Intensivists at night: putting resources in the right place. Crit Care. 2013;17(5):1008.
- , , . Changes in nurses' decision making during a 12‐h day shift. Occup Med (Lond). 2013;63(1):60–65.
- , , , , , . The incident reporting system does not detect adverse drug events: a problem for quality improvement. Jt Comm J Qual Improv. 1995;21(10):541–548.
- , , , , . An evaluation of adverse incident reporting. J Eval Clin Pract. 1999;5(1):5–12.
- , . Reporting and preventing medical mishaps: lessons from non‐medical near miss reporting systems. BMJ. 2000;320(7237):759–763.
- . Like night and day—shedding light on off‐hours care. N Engl J Med. 2008;358(20):2091–2093.
- , , , . Call nights and patient care. J Gen Intern Med. 1992;7(4):405–410.
- , , , et al. Uncovering system errors using a rapid response team: cross‐coverage caught in the crossfire. Discussion. J Trauma. 2009;67(1):173–179.
- , . The impact of shift work on the risk and severity of injuries for hospital employees: an analysis using Oregon workers' compensation data. Occup Med (Lond). 2004;54(8):556–563.
- , . Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668.
- , , , et al. The association of shift‐level nurse staffing with adverse patient events. J Nurs Adm. 2011;41(2):64–70.
- , , , et al. Heart disease and stroke statistics—2010 update A report from the American Heart Association. Circulation. 2010;121(7):e46–e215.
- , , , , O'Neil E. Minimum Nurse Staffing Ratios In California Acute Care Hospitals. Oakland, CA: California Workforce Initiative; 2000.
- , . Shift work, safety and productivity. Occup Med (Lond). 2003;53(2):95–101.
- , , . Increased injuries on night shift. Lancet. 1994;344(8930):1137–1139.
- , . Shift and night work and long working hours‐a systematic review of safety implications. Scand J Work Environ Health. 2011:37(3):173–185.
- , , , et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82(7):1011–1014.
- , , , et al. Survival from in‐hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792.
- , , , , . The influence of shared mental models on team process and performance. J Appl Psychol. 2000;85(2):273.
- , . Team mental models and their potential to improve teamwork and safety: a review and implications for future research in healthcare. Saf Sci. 2012;50(5):1344–1354.
- . Editorial: mapping the field of mixed methods research. J Mix Methods Res. 2009;3(2):95–108.
- , . Decreasing adverse events through night talks: an interdisciplinary, hospital‐based quality improvement project. Perm J. Fall 2009;13(4):16–22.
- , , , et al. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff (Millwood). 2011;30(4):581–589.
- , , , , , . Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009;53(6):701–710.e704.
- . Smoothing transitions. Joint Commission targets patient handoffs. Mod Healthc. 2010;40(43):8–9.
- , , , , , . The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med. 2012;87(4):411–418.
- , , , , , . Patient care transitions from the emergency department to the medicine ward: evaluation of a standardized electronic signout tool. Int J Qual Health Care. 2014;26(4):337–347.
- , . The unappreciated challenges of between‐unit handoffs: negotiating and coordinating across boundaries. Ann Emerg Med. 2013;61(2):155–160.
- , , , , , . The association between night or weekend admission and hospitalization‐relevant patient outcomes. J Hosp Med. 2011;6(1):10–14.
- . Middle‐of‐the‐night medicine is rarely patient‐centred. CMAJ. 2011;183(13):1467–1468.
- , , , et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521–523.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- , , , et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209.
- . Intensivists at night: putting resources in the right place. Crit Care. 2013;17(5):1008.
- , , . Changes in nurses' decision making during a 12‐h day shift. Occup Med (Lond). 2013;63(1):60–65.
- , , , , , . The incident reporting system does not detect adverse drug events: a problem for quality improvement. Jt Comm J Qual Improv. 1995;21(10):541–548.
- , , , , . An evaluation of adverse incident reporting. J Eval Clin Pract. 1999;5(1):5–12.
- , . Reporting and preventing medical mishaps: lessons from non‐medical near miss reporting systems. BMJ. 2000;320(7237):759–763.
© 2014 Society of Hospital Medicine
Bedside Interprofessional Rounds
Interprofessional collaborative care (IPCC) involves members from different professions working together to enhance communication, coordination, and healthcare quality.[1, 2, 3] Because several current healthcare policy initiatives include financial incentives for increased quality of care, there has been resultant interest in the implementation of IPCC in healthcare systems.[4, 5] Unfortunately, many hospitals have found IPCC difficult to achieve. Hospital‐based medicine units are complex, time‐constrained environments requiring a high degree of collaboration and mutual decision‐making between nurses, physicians, therapists, pharmacists, care coordinators, and patients. In addition, despite recommendations for interprofessional collaborative care, the implementation and assessment of IPCC within this environment has not been well studied.[6, 7]
On academic internal medicine services, the majority of care decisions occur during rounds. Although rounds provide a common structure, the participants, length, location, and agenda of rounds tend to vary by institution and individual physician preference.[8, 9, 10, 11] Traditionally, ward rounds occur mostly in hallways and conference rooms rather than the patient's bedside.[12] Additionally, during rounds, nurse‐physician collaboration occurs infrequently, estimated at <10% of rounding time.[13] Recently, an increased focus on quality, safety, and collaboration has inspired the investigation and implementation of new methods to increase interprofessional collaboration during rounds, but many of these interventions occurred away from the patient's bedside.[14, 15] One trial of bedside interprofessional rounds (BIRs) by Curley et al. suggested improvements in patient‐level outcomes (cost and length of stay) versus traditional physician‐based rounds.[16] Although interprofessional nurse‐physician rounds at patients' bedsides may represent an ideal process, limited work has investigated this activity.[17]
A prerequisite for successful and sustained integration of BIRs is a shared conceptualization among physicians and nurses regarding the process. Such a shared conceptualization would include perceptions of benefits and barriers to implementation.[18] Currently, such perceptions have not been measured. In this study, we sought to evaluate perceptions of front‐line care providers on inpatient units, specifically nursing staff, attending physicians, and housestaff physicians, regarding the benefits and barriers to BIRs.
METHODS
Study Design and Participants
In June 2013, we performed a cross‐sectional assessment of front‐line providers caring for patients on the internal medicine services in our academic hospital. Participants included medicine nursing staff in acute care and intermediate care units, medicine and combined medicine‐pediatrics housestaff physicians, and general internal medicine faculty physicians who supervised the housestaff physicians.
Study Setting
The study was conducted at a 378‐bed, university‐based, acute care teaching hospital in central Pennsylvania. There are a total of 64 internal medicine beds located in2 units, a general medicine unit (44 beds, staffed by 60 nurses, nurse‐to‐patient ratio 1:4) and an intermediate care unit (20 beds, staffed by 41 nurses, nurse‐to‐patient ratio 1:3). Both units are staffed by the general internal medicine physician teams. The academic medicine residency program consists of 69 internal medicine housestaff and 14 combined internal medicine‐pediatrics housestaff. Five teams, organized into 3 academic teaching teams and 2 nonteaching teams, provide care for all patients admitted to the medicine units. Teaching teams consist of 1 junior (postgraduate year [PGY]2) or senior (PGY34) housestaff member, 2 interns (PGY1), 2 medical students, and 1 attending physician.
There are several main features of BIRs in our medicine units. The rounding team of physicians alerts the assigned nurse about the start of rounds. In our main medicine unit, each doorway is equipped with a light that allows the physician team to indicate the start of the BIRs encounter. Case presentations by trainees occur either in the hallway or bedside, at the discretion of the attending physician. During bedside encounters, nurses typically contribute to the discussion about clinical status, decision making, patient concerns, and disposition. Patients are encouraged to contribute to the discussion and are provided the opportunity to ask questions.
For the purposes of this study, we specifically defined BIRs as: encounters that include the team of providers, at least 2 physicians plus a nurse or other care provider, discussing the case at the patient's bedside. In our prior work performed during the same time period as this study, we used the same definition to examine the incidence of and time spent in BIRs in both of our medicine units.[19] We found that 63% to 81% of patients in both units received BIRs. As a result, we assumed all nursing staff, attending physicians, and housestaff physicians had experienced this process, and their responses to this survey were contextualized in these experiences.
Survey Instrument
We developed a survey instrument specifically for this study. We derived items primarily from our prior qualitative work on physician‐based team bedside rounds and a literature review.[20, 21, 22, 23, 24, 25] For the benefits to BIRs, we developed items related to 5 domains, including factors related to the patient, education, communication/coordination/teamwork, efficiency and process, and outcomes.[20, 26] For the barriers to BIRs, we developed items related to 4 domains, including factors related to the patient, time, systems issues, and providers (nurses, attending physicians, and housestaff physicians).[22, 24, 25] We included our definition of BIRs into the survey instructions. We pilot tested the survey with 3 medicine faculty and 3 nursing staff and, based on our pilot, modified several questions to improve clarity. Primary demographic items in the survey included identification of provider role (nurses, attending physicians, or housestaff physicians) and years in the current role. Respondent preference for the benefits and barriers were investigated on a 7‐point scale (1=lowest response and 7=high response possible). Descriptive text was provided at the extremes (choice 1 and 7), but intermediary values (26) did not have descriptive cues.[27] As an incentive, the end of the survey provided respondents with an option for submitting their name to be entered into a raffle to win 1 of 50, $5 gift certificates to a coffee shop.
Prior to the end of the academic year in June 2013, we sent a survey link via e‐mail to all medicine nursing staff, housestaff physicians, and attending physicians. The email described the study and explained the voluntary nature of the work, and that informed consent would be implied by survey completion. Following the initial e‐mail, 3 additional weekly e‐mail reminders were sent by the lead investigator. The study was approved by the institutional review board at the Pennsylvania State College of Medicine.
Data Analysis
Descriptive statistics were used to examine the characteristics of the 3 respondent groups and combined totals for each survey item. The nonparametric Wilcoxon rank sum test was used to compare the average values between groups (nursing staff vs all physicians, attending physicians vs housestaff physicians) for both sets of survey variables (benefits and barriers). The nonparametric correlation statistical test Spearman rank was used to assess the degree of correlation between respondent groups for both survey variables. The data were analyzed using SAS 9.3 (SAS Institute, Cary, NC) and Stata/IC‐8 (StataCorp, College Station, Texas).
RESULTS
Of the 171 surveys sent, 149 participants completed surveys (response rate 87%). Responses were received from 53/58 nursing staff (91% response), 21/28 attending physicians (75% response), and 75/85 housestaff physicians (88% response). Table 1 describes the participant response demographics.
| Variable | Value |
|---|---|
| |
| Nursing staff, n=58, n (%) | 53 (36) |
| Intermediate care unit, n (%) | 14 (26) |
| General medicine ward, n (%) | 39 (74) |
| All day shifts, n (%) | 25 (47) |
| Mix of day and night shifts, n (%) | 32 (60) |
| Years of experience, mean (SD) | 7.4 (9) |
| Attending physicians, n=28, n (%) | 21 (14) |
| Years since residency graduation, mean (SD) | 10.5 (8) |
| No. of weeks in past year serving as teaching attending, mean (SD) | 9.1(8) |
| Housestaff physicians (n=85), n (%) | 75 (50) |
| Intern, n (%) | 28 (37) |
| Junior resident, n (%) | 25 (33) |
| Senior resident, n (%)a | 22 (29) |
Benefits of BIRs
Respondents' perceptions of the benefits of BIRs are shown by mean value (between 1 and 7) for the total respondent pool and by each participant group (Table 2). Six of the 7 highest‐ranked benefits were related to communication, coordination, and teamwork, including improves communication between nurses and physicians, improves awareness of clinical issues that need to be addressed, and improves team‐building between nurses and physicians. Lowest‐ranked benefits were related to efficiency, process, and outcomes, including decreases patients' hospital length‐of‐stay, improves timeliness of consultations, and reduces ordering of unnecessary tests and treatments. Comparing mean values among the 3 groups, all 18 items showed statistical differences in response rates (all P values <0.05). Nursing staff reported more favorable ratings than both attending physicians and housestaff physicians for each of the 18 items, whereas attending physicians reported more favorable ratings than housestaff physicians in 16/18 items. The rank order among provider groups showed a high degree of correlation (r=0.92, P<0.001).
| Survey Itema | Item Domain | Total, N=149, Mean (SD) | Nurses, N=53, Mean (SD) | Attending Physicians, N=21, Mean (SD) | House staff Physicians, N=75, Mean (SD)b |
|---|---|---|---|---|---|
| |||||
| Improves communication between nurses and physicians. | CCT | 6.26 (1.11) | 6.74 (0.59)c | 6.52 (1.03)d | 5.85 (1.26) |
| Improves awareness of clinical issues needing to be addressed. | CCT | 6.05 (1.12) | 6.57 (0.64)c | 5.95 (1.07) | 5.71 (1.26) |
| Improves team‐building between nurses and physicians. | CCT | 6.03 (1.32) | 6.72 (0.60)c | 6.14 (1.11) | 5.52 (1.51) |
| Improves coordination of the patient's care. | CCT | 5.98 (1.34) | 6.60 (0.72)c | 6.00 (1.18) | 5.53 (1.55) |
| Improves nursing contributions to a patient's care plan. | CCT | 5.91 (1.25) | 6.47 (0.77)c | 6.14 (0.85) | 5.44 (1.43) |
| Improves quality of care delivered in our unit. | O | 5.72 (1.42) | 6.34 (0.83)c | 5.81 (1.33) | 5.25 (1.61) |
| Improves appreciation of the roles/contributions of other providers. | CCT | 5.69 (1.49) | 6.36 (0.86)c | 5.90 (1.04) | 5.16 (1.73) |
| Promotes shared decision making between patients and providers. | P | 5.62 (1.51) | 6.43 (0.77)c | 5.57 (1.40) | 5.05 (1.68) |
| Improves patients' satisfaction with their hospitalization. | P, O | 5.53 (1.40) | 6.15 (0.95)c | 5.38 (1.12) | 5.13 (1.58) |
| Provides more respect/dignity to patients. | P | 5.31 (1.55) | 6.23 (0.89)c | 5.10 (1.18) | 4.72 (1.71) |
| Decreases number of pages/phone calls between nurses and physicians. | EP | 5.28 (1.82) | 6.28 (0.93)c | 5.24 (1.30) | 4.57 (2.09) |
| Improves educational opportunities for housestaff/students. | E | 5.07 (1.77) | 6.08 (0.98)c | 4.81 (1.60) | 4.43 (1.93) |
| Improves the efficiency of your work. | EP | 5.01 (1.77) | 6.04 (1.13)c | 4.90 (1.30) | 4.31 (1.92) |
| Improves adherence to evidence‐based guidelines or interventions. | EP | 4.89 (1.79) | 6.06 (0.91)c | 4.00 (1.18) | 4.31 (1.97) |
| Improves the accuracy of your sign‐outs (or reports) to the next shift. | EP | 4.80 (1.99) | 6.30 (0.93)c | 4.05 (1.66) | 3.95 (2.01) |
| Reduces ordering of unnecessary tests and treatments. | O | 4.51 (1.86) | 5.77 (1.15)c | 3.86 (1.11) | 3.8 (1.97) |
| Improves the timeliness of consultations. | EP | 4.28 (1.99) | 5.66 (1.22)c | 3.24 (1.48) | 3.59 (2.02) |
| Decreases patients' hospital length of stay. | O | 4.15 (1.68) | 5.04 (1.24)c | 3.95 (1.16) | 3.57 (1.81) |
Barriers to BIRs
Respondents' perceptions of barriers to BIRs are shown by mean value (between 1 and 7) for the total respondent pool and by each participant group (Table 3). The 6 highest‐ranked barriers were related to time, including nursing staff have limited time, the time required for bedside nurse‐physician encounters, and coordinating the start time of encounters with arrival of both physicians and nursing. The lowest‐ranked barriers were related to provider‐ and patient‐related factors, including patient lack of comfort with bedside nurse‐physician encounters, attending physicians/housestaff lack bedside skills, and attending physicians lack comfort with bedside nurse‐physician encounters. Comparing mean values between groups, 10 of 21 items showed statistical differences (P<0.05). The rank order among groups showed moderate correlation (nurses‐attending physicians r=0.62, nurses‐housestaff physicians r=0.76, attending physicians‐housestaff physicians r=0.82). A qualitative inspection of disparities among respondent groups highlighted that nursing staff were more likely to rank bedside rounds are not part of the unit's culture lower than physician groups.
| Survey Itema | Item Domain | Total, N=149, Mean (SD) | Nurses, n=53, Mean (SD) | Attending Physicians, n=21, Mean (SD) | Housestaff Physicians, n=75,b Mean (SD) |
|---|---|---|---|---|---|
| |||||
| Nursing staff have limited time. | T | 4.89 (1.34) | 4.96 (1.27) | 4.86 (1.65) | 4.85 (1.30) |
| Coordinating start time of encounters with arrival of physicians and nursing. | T | 4.80 (1.50) | 4.58 (1.43) | 5.24 (1.45) | 4.84 (1.55) |
| Housestaff have limited time. | T | 4.68 (1.47) | 4.56 (1.26) | 4.24 (1.81) | 4.89 (1.48) |
| Attending physicians have limited time. | T | 4.50 (1.49) | 4.81 (1.34) | 4.33 (1.65) | 4.34 (1.53) |
| Other acutely sick patients in unit. | T | 4.39 (1.42) | 4.79 (1.30)c | 4.52 (1.21) | 4.08 (1.49) |
| Time required for bedside nurse‐physician encounters. | T | 4.32 (1.55) | 4.85 (1.38)c | 3.62 (1.80) | 4.15 (1.49) |
| Lack of use of the pink‐rounding light to alert nursing staff. | S | 3.77 (1.75) | 4.71 (1.70)c | 3.48 (1.86) | 3.19 (1.46) |
| Patient not available (eg, off to test, getting bathed) | S | 3.74 (1.40) | 3.98 (1.28) | 4.52 (1.36)d | 3.35 (1.37) |
| Large team size. | S | 3.64 (1.74) | 3.12 (1.58)c | 3.95 (1.83) | 3.92 (1.77) |
| Patients in dispersed locations (eg, other units or in different hallways). | S | 3.64 (1.77) | 2.77 (1.55)c | 4.52 (1.83) | 4.00 (1.66) |
| Bedside nurse‐physician rounds are not part of the unit's culture. | S | 3.35 (1.94) | 2.25 (1.47)c | 4.76 (1.92) | 3.72 (1.85) |
| Limitations in physical facilities (eg, rooms too small, limited chairs). | S | 3.25 (1.71) | 2.71 (1.72) | 3.33 (1.71) | 3.59 (1.62) |
| Insufficient nurse engagement during bedside nurse‐physician encounters. | PR | 3.24 (1.63) | 2.71 (1.47)c | 3.67 (1.68) | 3.49 (1.65) |
| Patient on contact or respiratory isolation. | S | 3.20 (1.82) | 2.42 (1.67)c | 3.43 (1.63) | 3.69 (1.80) |
| Language barrier between providers and patients. | P | 2.69 (1.37) | 2.77 (1.39) | 2.57 (1.08) | 2.68 (1.43) |
| Privacy/sensitive patient issues. | P | 2.65 (1.45) | 2.27 (1.24) | 2.57 (1.33) | 2.93 (1.56) |
| Housestaff lack comfort with bedside nurse‐physician encounters. | PR | 2.55 (1.49) | 2.48 (1.15) | 2.67 (1.68) | 2.57 (1.65) |
| Nurses lack comfort with bedside nurse‐physician encounters. | PR | 2.45 (1.45) | 2.35 (1.27) | 2.48 (1.66) | 2.51 (1.53) |
| Attending physicians lack comfort with bedside nurse‐physician encounters. | PR | 2.35 (1.38) | 2.33 (1.25) | 2.33 (1.62) | 2.36 (1.41) |
| Attending physician/housestaff lack bedside skills (eg, history, exam). | PR | 2.34 (1.34) | 2.19 (1.19) | 2.85 (1.69) | 2.30 (1.32) |
| Patient lack of comfort with bedside nurse‐physician encounters. | P | 2.33 (1.48) | 2.23 (1.37) | 1.95 (1.32) | 2.5 (1.59) |
DISCUSSION
In this study, we sought to compare perceptions of nurses and physicians on the benefits and barriers to BIRs. Nursing staff ranked each benefit higher than physicians, though rank orders of specific benefits were highly correlated. Highest‐ranked benefits related to coordination and communication more than quality or process benefits. Across groups, the highest‐ranked barriers to BIRs were related to time, whereas the lowest‐ranked factors were related to provider and patient discomfort. These results highlight important similarities and differences in perceptions between front‐line providers.
The highest‐ranked benefits were related to improved interprofessional communication and coordination. Combining interprofessional team members during care delivery allows for integrated understanding of daily care plans and clinical issues, and fosters collaboration and a team‐based atmosphere.[1, 20, 26] The lowest‐ranked benefits were related to more tangible measures, including length of stay, timely consultations, and judicious laboratory ordering. This finding contrasts with the limited literature demonstrating increased efficiency in general medicine units practicing IPCC.[16] These rankings may reflect a poor understanding or self‐assessment of outcome measures by healthcare providers, representing a potential focus for educational initiatives. Future investigations using objective assessment methods of outcomes and collaboration will provide a more accurate understanding of these findings.
The highest‐ranked barriers were related to time and systems issues. Several studies of physician‐based bedside rounds have identified systems‐ and time‐related issues as primary limiting barriers.[22, 24] In units without colocalization of patients and providers, finding receptive times for BIRs can be difficult. Although time‐related issues could be addressed by decreasing patient‐provider ratios, these changes require substantial investment in resources. A reasonable degree of improvement in efficiency and coordination is expected following acclimation to BIRs or by addressing modifiable systems factors to increase this activity. Less costly interventions, such as tailoring provider schedules, prescheduling patient rounding times, and geographic colocalization of patients and providers may be more feasible. However, the clinical microsystems within which medicine patients are cared for are often chaotic and disorganized at the infrastructural and cultural levels, which may be less influenced by surface‐level interventions. Such interventions may be ward specific and require customization to individual team needs.
The lowest‐ranked barriers to BIRs were related to provider‐ and patient‐related factors, including comfort level of patients and providers. Prior work on bedside rounds has identified physicians who are apprehensive about performing bedside rounds, but those who experience this activity are more likely to be comfortable with it.[12, 28] Our results from a culture where BIRs occur on nearly two‐thirds of patients suggest provider discomfort is not a predominant barrier.[22, 29] Additionally, educators have raised concerns about patient discomfort with bedside rounds, but nearly all studies evaluating patients' perspectives reveal patient preference for bedside case presentations over activities occurring in alternative locations.[30, 31, 32] Little work has investigated patient preference for BIRs as per our definition; our participants do not believe patients are discomforted by BIRs, building upon evidence in the literature for patient preferences regarding bedside activities.
Nursing staff perceptions of the benefits and culture related to BIRs were more positive than physicians. We hypothesize several reasons for this disparity. First, nursing staff may have more experience with observing and understanding the positive impact of BIRs and therefore are more likely to understand the positive ramifications. Alternatively, nursing staff may be satisfied with active integration into traditional physician‐centric decisions. Additionally, the professional culture and educational foundation of the nursing culture is based upon a patient‐centered approach and therefore may be more aligned with the goals of BIRs. Last, physicians may have competing priorities, favoring productivity and didactic learning rather than interprofessional collaboration. Further investigation is required to understand differences between nurses and physicians, in addition to other providers integral to BIRs (eg, care coordinators, pharmacists). Regardless, during the implementation of interprofessional collaborative care models, our findings suggest initial challenges, and the focus of educational initiatives may necessitate acclimating physician groups to benefits identified by front‐line nursing staff.
There are several limitations to our study. We investigated the perceptions of medicine nurses and physicians in 1 teaching hospital, limiting generalizability to other specialties, other vital professional groups, and nonteaching hospitals. Additionally, BIRs has been a focus of our hospital for several years. Therefore, perceived barriers may differ in BIRs‐nave hospitals. Second, although pilot‐tested for content, the construct validity of the instrument was not rigorously assessed, and the instrument was not designed to measure benefits and barriers not explicitly identified during pilot testing. Last, although surveys were anonymous, the possibility of social desirability bias exists, thereby limiting accuracy.
For over a century, physician‐led rounds have been the preferred modality for point‐of‐care decision making.[10, 15, 32, 33] BIRs address our growing understanding of patient‐centered care. Future efforts should address the quality of collaboration and current hospital and unit structures hindering patient‐centered IPCC and patient outcomes.
Acknowledgements
The authors thank the medicine nursing staff and physicians for their dedication to patient‐centered care and willingness to participate in this study.
Disclosures: The Department of Medicine at the Penn State Hershey Medical Center provided funding for this project. There are no conflicts of interest to report.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- . Teamswork! Hosp Health Netw. 2012;86(3):24–27, 21.
- , , , . The coming of age for interprofessional education and practice. Am J Med. 2013;126(4):284–288.
- , . Payment incentives and integrated care delivery: levers for health system reform and cost containment. Inquiry. 2011;48(4):277–287.
- . Payment reform and the mission of academic medical centers. N Engl J Med. 2010;363(19):1784–1786.
- Josiah Macy Jr. Foundation. Transforming patient care: aligning interprofessional education and clinical practice redesign. In: Proceedings of the Josiah Macy Jr. Foundation Conference; January 17–20, 2013; Atlanta, GA.
- , , , . Bridging the quality chasm: interprofessional teams to the rescue? Am J Med. 2013;126(4):276–277.
- . Attending rounds: guidelines for teaching on the wards. J Gen Intern Med. 1992;7(1):68–75.
- , . Teaching at the bedside: a new model. Med Teach. 2003;25(2):127–130.
- . On bedside teaching. Ann Intern Med. 1997;126(3):217–220.
- , , , . Relationships of the location and content of rounds to specialty, institution, patient‐census, and team size. PloS One. 2010;5(6):e11246.
- , , , . Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110.
- , , , et al. Attending rounds in the current era: what is and is not happening. JAMA Intern Med. 2013;173(12):1084–1089.
- , , , et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684.
- , , , , . Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med. 2007;22(8):1073–1079.
- , , . A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement. Med Care. 1998;36(8 suppl):AS4–AS12.
- , , , . A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275–280.
- , . The challenge of innovation implementation. Acad Manage Rev. 1996;21(4):1055–1080.
- , , , . Ocular dipping in creutzfeldt‐jakob disease. J Clin Neurol. 2014;10(2):162–165.
- , , , et al. The value of bedside rounds: a multicenter qualitative study. Teach Learn Med. 2013;25(4):326–333.
- , , , et al. The art of bedside rounds: a multi‐center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412–420.
- , , , et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326–334.
- , . Bedside teaching in medical education: a literature review. Perspec Med Educ. 2014;3(2):76–88.
- , , . Impediments to bed‐side teaching. Med Educ. 1998;32(2):159–162.
- , , , . Whither bedside teaching? A focus‐group study of clinical teachers. Acad Med. 2003;78(4):384–390.
- , . Staff preference for multidisciplinary rounding practices in the critical care setting. 2011. Paper presented at: Design July 6–10, 2011. Boston, MA. Available at: http://www.designandhealth.com/uploaded/documents/Awards‐and‐events/WCDH2011/Presentations/Friday/Session‐8/DianaAnderson.pdf. Accessed July 6, 2014.
- , . Health Measurement Scales: A Practical Guide to Their Development and Use. 2nd ed. New York, NY: Oxford University Press; 1995.
- , , . Student and patient perspectives on bedside teaching. Med Educ. 1997;31(5):341–346.
- , , , , , . The positive impact of portfolios on health care assistants' clinical practice. J Eval Clin Pract. 2008;14(1):172–174.
- , , , . The physiologic and psychological effects of the bedside presentation. N Engl J Med. 1989;321(18):1273–1275.
- , , , , . The effect of bedside case presentations on patients' perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155.
- , , , . The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792–798.
- . Bedside rounds revisited. N Engl J Med. 1997;336(16):1174–1175.
Interprofessional collaborative care (IPCC) involves members from different professions working together to enhance communication, coordination, and healthcare quality.[1, 2, 3] Because several current healthcare policy initiatives include financial incentives for increased quality of care, there has been resultant interest in the implementation of IPCC in healthcare systems.[4, 5] Unfortunately, many hospitals have found IPCC difficult to achieve. Hospital‐based medicine units are complex, time‐constrained environments requiring a high degree of collaboration and mutual decision‐making between nurses, physicians, therapists, pharmacists, care coordinators, and patients. In addition, despite recommendations for interprofessional collaborative care, the implementation and assessment of IPCC within this environment has not been well studied.[6, 7]
On academic internal medicine services, the majority of care decisions occur during rounds. Although rounds provide a common structure, the participants, length, location, and agenda of rounds tend to vary by institution and individual physician preference.[8, 9, 10, 11] Traditionally, ward rounds occur mostly in hallways and conference rooms rather than the patient's bedside.[12] Additionally, during rounds, nurse‐physician collaboration occurs infrequently, estimated at <10% of rounding time.[13] Recently, an increased focus on quality, safety, and collaboration has inspired the investigation and implementation of new methods to increase interprofessional collaboration during rounds, but many of these interventions occurred away from the patient's bedside.[14, 15] One trial of bedside interprofessional rounds (BIRs) by Curley et al. suggested improvements in patient‐level outcomes (cost and length of stay) versus traditional physician‐based rounds.[16] Although interprofessional nurse‐physician rounds at patients' bedsides may represent an ideal process, limited work has investigated this activity.[17]
A prerequisite for successful and sustained integration of BIRs is a shared conceptualization among physicians and nurses regarding the process. Such a shared conceptualization would include perceptions of benefits and barriers to implementation.[18] Currently, such perceptions have not been measured. In this study, we sought to evaluate perceptions of front‐line care providers on inpatient units, specifically nursing staff, attending physicians, and housestaff physicians, regarding the benefits and barriers to BIRs.
METHODS
Study Design and Participants
In June 2013, we performed a cross‐sectional assessment of front‐line providers caring for patients on the internal medicine services in our academic hospital. Participants included medicine nursing staff in acute care and intermediate care units, medicine and combined medicine‐pediatrics housestaff physicians, and general internal medicine faculty physicians who supervised the housestaff physicians.
Study Setting
The study was conducted at a 378‐bed, university‐based, acute care teaching hospital in central Pennsylvania. There are a total of 64 internal medicine beds located in2 units, a general medicine unit (44 beds, staffed by 60 nurses, nurse‐to‐patient ratio 1:4) and an intermediate care unit (20 beds, staffed by 41 nurses, nurse‐to‐patient ratio 1:3). Both units are staffed by the general internal medicine physician teams. The academic medicine residency program consists of 69 internal medicine housestaff and 14 combined internal medicine‐pediatrics housestaff. Five teams, organized into 3 academic teaching teams and 2 nonteaching teams, provide care for all patients admitted to the medicine units. Teaching teams consist of 1 junior (postgraduate year [PGY]2) or senior (PGY34) housestaff member, 2 interns (PGY1), 2 medical students, and 1 attending physician.
There are several main features of BIRs in our medicine units. The rounding team of physicians alerts the assigned nurse about the start of rounds. In our main medicine unit, each doorway is equipped with a light that allows the physician team to indicate the start of the BIRs encounter. Case presentations by trainees occur either in the hallway or bedside, at the discretion of the attending physician. During bedside encounters, nurses typically contribute to the discussion about clinical status, decision making, patient concerns, and disposition. Patients are encouraged to contribute to the discussion and are provided the opportunity to ask questions.
For the purposes of this study, we specifically defined BIRs as: encounters that include the team of providers, at least 2 physicians plus a nurse or other care provider, discussing the case at the patient's bedside. In our prior work performed during the same time period as this study, we used the same definition to examine the incidence of and time spent in BIRs in both of our medicine units.[19] We found that 63% to 81% of patients in both units received BIRs. As a result, we assumed all nursing staff, attending physicians, and housestaff physicians had experienced this process, and their responses to this survey were contextualized in these experiences.
Survey Instrument
We developed a survey instrument specifically for this study. We derived items primarily from our prior qualitative work on physician‐based team bedside rounds and a literature review.[20, 21, 22, 23, 24, 25] For the benefits to BIRs, we developed items related to 5 domains, including factors related to the patient, education, communication/coordination/teamwork, efficiency and process, and outcomes.[20, 26] For the barriers to BIRs, we developed items related to 4 domains, including factors related to the patient, time, systems issues, and providers (nurses, attending physicians, and housestaff physicians).[22, 24, 25] We included our definition of BIRs into the survey instructions. We pilot tested the survey with 3 medicine faculty and 3 nursing staff and, based on our pilot, modified several questions to improve clarity. Primary demographic items in the survey included identification of provider role (nurses, attending physicians, or housestaff physicians) and years in the current role. Respondent preference for the benefits and barriers were investigated on a 7‐point scale (1=lowest response and 7=high response possible). Descriptive text was provided at the extremes (choice 1 and 7), but intermediary values (26) did not have descriptive cues.[27] As an incentive, the end of the survey provided respondents with an option for submitting their name to be entered into a raffle to win 1 of 50, $5 gift certificates to a coffee shop.
Prior to the end of the academic year in June 2013, we sent a survey link via e‐mail to all medicine nursing staff, housestaff physicians, and attending physicians. The email described the study and explained the voluntary nature of the work, and that informed consent would be implied by survey completion. Following the initial e‐mail, 3 additional weekly e‐mail reminders were sent by the lead investigator. The study was approved by the institutional review board at the Pennsylvania State College of Medicine.
Data Analysis
Descriptive statistics were used to examine the characteristics of the 3 respondent groups and combined totals for each survey item. The nonparametric Wilcoxon rank sum test was used to compare the average values between groups (nursing staff vs all physicians, attending physicians vs housestaff physicians) for both sets of survey variables (benefits and barriers). The nonparametric correlation statistical test Spearman rank was used to assess the degree of correlation between respondent groups for both survey variables. The data were analyzed using SAS 9.3 (SAS Institute, Cary, NC) and Stata/IC‐8 (StataCorp, College Station, Texas).
RESULTS
Of the 171 surveys sent, 149 participants completed surveys (response rate 87%). Responses were received from 53/58 nursing staff (91% response), 21/28 attending physicians (75% response), and 75/85 housestaff physicians (88% response). Table 1 describes the participant response demographics.
| Variable | Value |
|---|---|
| |
| Nursing staff, n=58, n (%) | 53 (36) |
| Intermediate care unit, n (%) | 14 (26) |
| General medicine ward, n (%) | 39 (74) |
| All day shifts, n (%) | 25 (47) |
| Mix of day and night shifts, n (%) | 32 (60) |
| Years of experience, mean (SD) | 7.4 (9) |
| Attending physicians, n=28, n (%) | 21 (14) |
| Years since residency graduation, mean (SD) | 10.5 (8) |
| No. of weeks in past year serving as teaching attending, mean (SD) | 9.1(8) |
| Housestaff physicians (n=85), n (%) | 75 (50) |
| Intern, n (%) | 28 (37) |
| Junior resident, n (%) | 25 (33) |
| Senior resident, n (%)a | 22 (29) |
Benefits of BIRs
Respondents' perceptions of the benefits of BIRs are shown by mean value (between 1 and 7) for the total respondent pool and by each participant group (Table 2). Six of the 7 highest‐ranked benefits were related to communication, coordination, and teamwork, including improves communication between nurses and physicians, improves awareness of clinical issues that need to be addressed, and improves team‐building between nurses and physicians. Lowest‐ranked benefits were related to efficiency, process, and outcomes, including decreases patients' hospital length‐of‐stay, improves timeliness of consultations, and reduces ordering of unnecessary tests and treatments. Comparing mean values among the 3 groups, all 18 items showed statistical differences in response rates (all P values <0.05). Nursing staff reported more favorable ratings than both attending physicians and housestaff physicians for each of the 18 items, whereas attending physicians reported more favorable ratings than housestaff physicians in 16/18 items. The rank order among provider groups showed a high degree of correlation (r=0.92, P<0.001).
| Survey Itema | Item Domain | Total, N=149, Mean (SD) | Nurses, N=53, Mean (SD) | Attending Physicians, N=21, Mean (SD) | House staff Physicians, N=75, Mean (SD)b |
|---|---|---|---|---|---|
| |||||
| Improves communication between nurses and physicians. | CCT | 6.26 (1.11) | 6.74 (0.59)c | 6.52 (1.03)d | 5.85 (1.26) |
| Improves awareness of clinical issues needing to be addressed. | CCT | 6.05 (1.12) | 6.57 (0.64)c | 5.95 (1.07) | 5.71 (1.26) |
| Improves team‐building between nurses and physicians. | CCT | 6.03 (1.32) | 6.72 (0.60)c | 6.14 (1.11) | 5.52 (1.51) |
| Improves coordination of the patient's care. | CCT | 5.98 (1.34) | 6.60 (0.72)c | 6.00 (1.18) | 5.53 (1.55) |
| Improves nursing contributions to a patient's care plan. | CCT | 5.91 (1.25) | 6.47 (0.77)c | 6.14 (0.85) | 5.44 (1.43) |
| Improves quality of care delivered in our unit. | O | 5.72 (1.42) | 6.34 (0.83)c | 5.81 (1.33) | 5.25 (1.61) |
| Improves appreciation of the roles/contributions of other providers. | CCT | 5.69 (1.49) | 6.36 (0.86)c | 5.90 (1.04) | 5.16 (1.73) |
| Promotes shared decision making between patients and providers. | P | 5.62 (1.51) | 6.43 (0.77)c | 5.57 (1.40) | 5.05 (1.68) |
| Improves patients' satisfaction with their hospitalization. | P, O | 5.53 (1.40) | 6.15 (0.95)c | 5.38 (1.12) | 5.13 (1.58) |
| Provides more respect/dignity to patients. | P | 5.31 (1.55) | 6.23 (0.89)c | 5.10 (1.18) | 4.72 (1.71) |
| Decreases number of pages/phone calls between nurses and physicians. | EP | 5.28 (1.82) | 6.28 (0.93)c | 5.24 (1.30) | 4.57 (2.09) |
| Improves educational opportunities for housestaff/students. | E | 5.07 (1.77) | 6.08 (0.98)c | 4.81 (1.60) | 4.43 (1.93) |
| Improves the efficiency of your work. | EP | 5.01 (1.77) | 6.04 (1.13)c | 4.90 (1.30) | 4.31 (1.92) |
| Improves adherence to evidence‐based guidelines or interventions. | EP | 4.89 (1.79) | 6.06 (0.91)c | 4.00 (1.18) | 4.31 (1.97) |
| Improves the accuracy of your sign‐outs (or reports) to the next shift. | EP | 4.80 (1.99) | 6.30 (0.93)c | 4.05 (1.66) | 3.95 (2.01) |
| Reduces ordering of unnecessary tests and treatments. | O | 4.51 (1.86) | 5.77 (1.15)c | 3.86 (1.11) | 3.8 (1.97) |
| Improves the timeliness of consultations. | EP | 4.28 (1.99) | 5.66 (1.22)c | 3.24 (1.48) | 3.59 (2.02) |
| Decreases patients' hospital length of stay. | O | 4.15 (1.68) | 5.04 (1.24)c | 3.95 (1.16) | 3.57 (1.81) |
Barriers to BIRs
Respondents' perceptions of barriers to BIRs are shown by mean value (between 1 and 7) for the total respondent pool and by each participant group (Table 3). The 6 highest‐ranked barriers were related to time, including nursing staff have limited time, the time required for bedside nurse‐physician encounters, and coordinating the start time of encounters with arrival of both physicians and nursing. The lowest‐ranked barriers were related to provider‐ and patient‐related factors, including patient lack of comfort with bedside nurse‐physician encounters, attending physicians/housestaff lack bedside skills, and attending physicians lack comfort with bedside nurse‐physician encounters. Comparing mean values between groups, 10 of 21 items showed statistical differences (P<0.05). The rank order among groups showed moderate correlation (nurses‐attending physicians r=0.62, nurses‐housestaff physicians r=0.76, attending physicians‐housestaff physicians r=0.82). A qualitative inspection of disparities among respondent groups highlighted that nursing staff were more likely to rank bedside rounds are not part of the unit's culture lower than physician groups.
| Survey Itema | Item Domain | Total, N=149, Mean (SD) | Nurses, n=53, Mean (SD) | Attending Physicians, n=21, Mean (SD) | Housestaff Physicians, n=75,b Mean (SD) |
|---|---|---|---|---|---|
| |||||
| Nursing staff have limited time. | T | 4.89 (1.34) | 4.96 (1.27) | 4.86 (1.65) | 4.85 (1.30) |
| Coordinating start time of encounters with arrival of physicians and nursing. | T | 4.80 (1.50) | 4.58 (1.43) | 5.24 (1.45) | 4.84 (1.55) |
| Housestaff have limited time. | T | 4.68 (1.47) | 4.56 (1.26) | 4.24 (1.81) | 4.89 (1.48) |
| Attending physicians have limited time. | T | 4.50 (1.49) | 4.81 (1.34) | 4.33 (1.65) | 4.34 (1.53) |
| Other acutely sick patients in unit. | T | 4.39 (1.42) | 4.79 (1.30)c | 4.52 (1.21) | 4.08 (1.49) |
| Time required for bedside nurse‐physician encounters. | T | 4.32 (1.55) | 4.85 (1.38)c | 3.62 (1.80) | 4.15 (1.49) |
| Lack of use of the pink‐rounding light to alert nursing staff. | S | 3.77 (1.75) | 4.71 (1.70)c | 3.48 (1.86) | 3.19 (1.46) |
| Patient not available (eg, off to test, getting bathed) | S | 3.74 (1.40) | 3.98 (1.28) | 4.52 (1.36)d | 3.35 (1.37) |
| Large team size. | S | 3.64 (1.74) | 3.12 (1.58)c | 3.95 (1.83) | 3.92 (1.77) |
| Patients in dispersed locations (eg, other units or in different hallways). | S | 3.64 (1.77) | 2.77 (1.55)c | 4.52 (1.83) | 4.00 (1.66) |
| Bedside nurse‐physician rounds are not part of the unit's culture. | S | 3.35 (1.94) | 2.25 (1.47)c | 4.76 (1.92) | 3.72 (1.85) |
| Limitations in physical facilities (eg, rooms too small, limited chairs). | S | 3.25 (1.71) | 2.71 (1.72) | 3.33 (1.71) | 3.59 (1.62) |
| Insufficient nurse engagement during bedside nurse‐physician encounters. | PR | 3.24 (1.63) | 2.71 (1.47)c | 3.67 (1.68) | 3.49 (1.65) |
| Patient on contact or respiratory isolation. | S | 3.20 (1.82) | 2.42 (1.67)c | 3.43 (1.63) | 3.69 (1.80) |
| Language barrier between providers and patients. | P | 2.69 (1.37) | 2.77 (1.39) | 2.57 (1.08) | 2.68 (1.43) |
| Privacy/sensitive patient issues. | P | 2.65 (1.45) | 2.27 (1.24) | 2.57 (1.33) | 2.93 (1.56) |
| Housestaff lack comfort with bedside nurse‐physician encounters. | PR | 2.55 (1.49) | 2.48 (1.15) | 2.67 (1.68) | 2.57 (1.65) |
| Nurses lack comfort with bedside nurse‐physician encounters. | PR | 2.45 (1.45) | 2.35 (1.27) | 2.48 (1.66) | 2.51 (1.53) |
| Attending physicians lack comfort with bedside nurse‐physician encounters. | PR | 2.35 (1.38) | 2.33 (1.25) | 2.33 (1.62) | 2.36 (1.41) |
| Attending physician/housestaff lack bedside skills (eg, history, exam). | PR | 2.34 (1.34) | 2.19 (1.19) | 2.85 (1.69) | 2.30 (1.32) |
| Patient lack of comfort with bedside nurse‐physician encounters. | P | 2.33 (1.48) | 2.23 (1.37) | 1.95 (1.32) | 2.5 (1.59) |
DISCUSSION
In this study, we sought to compare perceptions of nurses and physicians on the benefits and barriers to BIRs. Nursing staff ranked each benefit higher than physicians, though rank orders of specific benefits were highly correlated. Highest‐ranked benefits related to coordination and communication more than quality or process benefits. Across groups, the highest‐ranked barriers to BIRs were related to time, whereas the lowest‐ranked factors were related to provider and patient discomfort. These results highlight important similarities and differences in perceptions between front‐line providers.
The highest‐ranked benefits were related to improved interprofessional communication and coordination. Combining interprofessional team members during care delivery allows for integrated understanding of daily care plans and clinical issues, and fosters collaboration and a team‐based atmosphere.[1, 20, 26] The lowest‐ranked benefits were related to more tangible measures, including length of stay, timely consultations, and judicious laboratory ordering. This finding contrasts with the limited literature demonstrating increased efficiency in general medicine units practicing IPCC.[16] These rankings may reflect a poor understanding or self‐assessment of outcome measures by healthcare providers, representing a potential focus for educational initiatives. Future investigations using objective assessment methods of outcomes and collaboration will provide a more accurate understanding of these findings.
The highest‐ranked barriers were related to time and systems issues. Several studies of physician‐based bedside rounds have identified systems‐ and time‐related issues as primary limiting barriers.[22, 24] In units without colocalization of patients and providers, finding receptive times for BIRs can be difficult. Although time‐related issues could be addressed by decreasing patient‐provider ratios, these changes require substantial investment in resources. A reasonable degree of improvement in efficiency and coordination is expected following acclimation to BIRs or by addressing modifiable systems factors to increase this activity. Less costly interventions, such as tailoring provider schedules, prescheduling patient rounding times, and geographic colocalization of patients and providers may be more feasible. However, the clinical microsystems within which medicine patients are cared for are often chaotic and disorganized at the infrastructural and cultural levels, which may be less influenced by surface‐level interventions. Such interventions may be ward specific and require customization to individual team needs.
The lowest‐ranked barriers to BIRs were related to provider‐ and patient‐related factors, including comfort level of patients and providers. Prior work on bedside rounds has identified physicians who are apprehensive about performing bedside rounds, but those who experience this activity are more likely to be comfortable with it.[12, 28] Our results from a culture where BIRs occur on nearly two‐thirds of patients suggest provider discomfort is not a predominant barrier.[22, 29] Additionally, educators have raised concerns about patient discomfort with bedside rounds, but nearly all studies evaluating patients' perspectives reveal patient preference for bedside case presentations over activities occurring in alternative locations.[30, 31, 32] Little work has investigated patient preference for BIRs as per our definition; our participants do not believe patients are discomforted by BIRs, building upon evidence in the literature for patient preferences regarding bedside activities.
Nursing staff perceptions of the benefits and culture related to BIRs were more positive than physicians. We hypothesize several reasons for this disparity. First, nursing staff may have more experience with observing and understanding the positive impact of BIRs and therefore are more likely to understand the positive ramifications. Alternatively, nursing staff may be satisfied with active integration into traditional physician‐centric decisions. Additionally, the professional culture and educational foundation of the nursing culture is based upon a patient‐centered approach and therefore may be more aligned with the goals of BIRs. Last, physicians may have competing priorities, favoring productivity and didactic learning rather than interprofessional collaboration. Further investigation is required to understand differences between nurses and physicians, in addition to other providers integral to BIRs (eg, care coordinators, pharmacists). Regardless, during the implementation of interprofessional collaborative care models, our findings suggest initial challenges, and the focus of educational initiatives may necessitate acclimating physician groups to benefits identified by front‐line nursing staff.
There are several limitations to our study. We investigated the perceptions of medicine nurses and physicians in 1 teaching hospital, limiting generalizability to other specialties, other vital professional groups, and nonteaching hospitals. Additionally, BIRs has been a focus of our hospital for several years. Therefore, perceived barriers may differ in BIRs‐nave hospitals. Second, although pilot‐tested for content, the construct validity of the instrument was not rigorously assessed, and the instrument was not designed to measure benefits and barriers not explicitly identified during pilot testing. Last, although surveys were anonymous, the possibility of social desirability bias exists, thereby limiting accuracy.
For over a century, physician‐led rounds have been the preferred modality for point‐of‐care decision making.[10, 15, 32, 33] BIRs address our growing understanding of patient‐centered care. Future efforts should address the quality of collaboration and current hospital and unit structures hindering patient‐centered IPCC and patient outcomes.
Acknowledgements
The authors thank the medicine nursing staff and physicians for their dedication to patient‐centered care and willingness to participate in this study.
Disclosures: The Department of Medicine at the Penn State Hershey Medical Center provided funding for this project. There are no conflicts of interest to report.
Interprofessional collaborative care (IPCC) involves members from different professions working together to enhance communication, coordination, and healthcare quality.[1, 2, 3] Because several current healthcare policy initiatives include financial incentives for increased quality of care, there has been resultant interest in the implementation of IPCC in healthcare systems.[4, 5] Unfortunately, many hospitals have found IPCC difficult to achieve. Hospital‐based medicine units are complex, time‐constrained environments requiring a high degree of collaboration and mutual decision‐making between nurses, physicians, therapists, pharmacists, care coordinators, and patients. In addition, despite recommendations for interprofessional collaborative care, the implementation and assessment of IPCC within this environment has not been well studied.[6, 7]
On academic internal medicine services, the majority of care decisions occur during rounds. Although rounds provide a common structure, the participants, length, location, and agenda of rounds tend to vary by institution and individual physician preference.[8, 9, 10, 11] Traditionally, ward rounds occur mostly in hallways and conference rooms rather than the patient's bedside.[12] Additionally, during rounds, nurse‐physician collaboration occurs infrequently, estimated at <10% of rounding time.[13] Recently, an increased focus on quality, safety, and collaboration has inspired the investigation and implementation of new methods to increase interprofessional collaboration during rounds, but many of these interventions occurred away from the patient's bedside.[14, 15] One trial of bedside interprofessional rounds (BIRs) by Curley et al. suggested improvements in patient‐level outcomes (cost and length of stay) versus traditional physician‐based rounds.[16] Although interprofessional nurse‐physician rounds at patients' bedsides may represent an ideal process, limited work has investigated this activity.[17]
A prerequisite for successful and sustained integration of BIRs is a shared conceptualization among physicians and nurses regarding the process. Such a shared conceptualization would include perceptions of benefits and barriers to implementation.[18] Currently, such perceptions have not been measured. In this study, we sought to evaluate perceptions of front‐line care providers on inpatient units, specifically nursing staff, attending physicians, and housestaff physicians, regarding the benefits and barriers to BIRs.
METHODS
Study Design and Participants
In June 2013, we performed a cross‐sectional assessment of front‐line providers caring for patients on the internal medicine services in our academic hospital. Participants included medicine nursing staff in acute care and intermediate care units, medicine and combined medicine‐pediatrics housestaff physicians, and general internal medicine faculty physicians who supervised the housestaff physicians.
Study Setting
The study was conducted at a 378‐bed, university‐based, acute care teaching hospital in central Pennsylvania. There are a total of 64 internal medicine beds located in2 units, a general medicine unit (44 beds, staffed by 60 nurses, nurse‐to‐patient ratio 1:4) and an intermediate care unit (20 beds, staffed by 41 nurses, nurse‐to‐patient ratio 1:3). Both units are staffed by the general internal medicine physician teams. The academic medicine residency program consists of 69 internal medicine housestaff and 14 combined internal medicine‐pediatrics housestaff. Five teams, organized into 3 academic teaching teams and 2 nonteaching teams, provide care for all patients admitted to the medicine units. Teaching teams consist of 1 junior (postgraduate year [PGY]2) or senior (PGY34) housestaff member, 2 interns (PGY1), 2 medical students, and 1 attending physician.
There are several main features of BIRs in our medicine units. The rounding team of physicians alerts the assigned nurse about the start of rounds. In our main medicine unit, each doorway is equipped with a light that allows the physician team to indicate the start of the BIRs encounter. Case presentations by trainees occur either in the hallway or bedside, at the discretion of the attending physician. During bedside encounters, nurses typically contribute to the discussion about clinical status, decision making, patient concerns, and disposition. Patients are encouraged to contribute to the discussion and are provided the opportunity to ask questions.
For the purposes of this study, we specifically defined BIRs as: encounters that include the team of providers, at least 2 physicians plus a nurse or other care provider, discussing the case at the patient's bedside. In our prior work performed during the same time period as this study, we used the same definition to examine the incidence of and time spent in BIRs in both of our medicine units.[19] We found that 63% to 81% of patients in both units received BIRs. As a result, we assumed all nursing staff, attending physicians, and housestaff physicians had experienced this process, and their responses to this survey were contextualized in these experiences.
Survey Instrument
We developed a survey instrument specifically for this study. We derived items primarily from our prior qualitative work on physician‐based team bedside rounds and a literature review.[20, 21, 22, 23, 24, 25] For the benefits to BIRs, we developed items related to 5 domains, including factors related to the patient, education, communication/coordination/teamwork, efficiency and process, and outcomes.[20, 26] For the barriers to BIRs, we developed items related to 4 domains, including factors related to the patient, time, systems issues, and providers (nurses, attending physicians, and housestaff physicians).[22, 24, 25] We included our definition of BIRs into the survey instructions. We pilot tested the survey with 3 medicine faculty and 3 nursing staff and, based on our pilot, modified several questions to improve clarity. Primary demographic items in the survey included identification of provider role (nurses, attending physicians, or housestaff physicians) and years in the current role. Respondent preference for the benefits and barriers were investigated on a 7‐point scale (1=lowest response and 7=high response possible). Descriptive text was provided at the extremes (choice 1 and 7), but intermediary values (26) did not have descriptive cues.[27] As an incentive, the end of the survey provided respondents with an option for submitting their name to be entered into a raffle to win 1 of 50, $5 gift certificates to a coffee shop.
Prior to the end of the academic year in June 2013, we sent a survey link via e‐mail to all medicine nursing staff, housestaff physicians, and attending physicians. The email described the study and explained the voluntary nature of the work, and that informed consent would be implied by survey completion. Following the initial e‐mail, 3 additional weekly e‐mail reminders were sent by the lead investigator. The study was approved by the institutional review board at the Pennsylvania State College of Medicine.
Data Analysis
Descriptive statistics were used to examine the characteristics of the 3 respondent groups and combined totals for each survey item. The nonparametric Wilcoxon rank sum test was used to compare the average values between groups (nursing staff vs all physicians, attending physicians vs housestaff physicians) for both sets of survey variables (benefits and barriers). The nonparametric correlation statistical test Spearman rank was used to assess the degree of correlation between respondent groups for both survey variables. The data were analyzed using SAS 9.3 (SAS Institute, Cary, NC) and Stata/IC‐8 (StataCorp, College Station, Texas).
RESULTS
Of the 171 surveys sent, 149 participants completed surveys (response rate 87%). Responses were received from 53/58 nursing staff (91% response), 21/28 attending physicians (75% response), and 75/85 housestaff physicians (88% response). Table 1 describes the participant response demographics.
| Variable | Value |
|---|---|
| |
| Nursing staff, n=58, n (%) | 53 (36) |
| Intermediate care unit, n (%) | 14 (26) |
| General medicine ward, n (%) | 39 (74) |
| All day shifts, n (%) | 25 (47) |
| Mix of day and night shifts, n (%) | 32 (60) |
| Years of experience, mean (SD) | 7.4 (9) |
| Attending physicians, n=28, n (%) | 21 (14) |
| Years since residency graduation, mean (SD) | 10.5 (8) |
| No. of weeks in past year serving as teaching attending, mean (SD) | 9.1(8) |
| Housestaff physicians (n=85), n (%) | 75 (50) |
| Intern, n (%) | 28 (37) |
| Junior resident, n (%) | 25 (33) |
| Senior resident, n (%)a | 22 (29) |
Benefits of BIRs
Respondents' perceptions of the benefits of BIRs are shown by mean value (between 1 and 7) for the total respondent pool and by each participant group (Table 2). Six of the 7 highest‐ranked benefits were related to communication, coordination, and teamwork, including improves communication between nurses and physicians, improves awareness of clinical issues that need to be addressed, and improves team‐building between nurses and physicians. Lowest‐ranked benefits were related to efficiency, process, and outcomes, including decreases patients' hospital length‐of‐stay, improves timeliness of consultations, and reduces ordering of unnecessary tests and treatments. Comparing mean values among the 3 groups, all 18 items showed statistical differences in response rates (all P values <0.05). Nursing staff reported more favorable ratings than both attending physicians and housestaff physicians for each of the 18 items, whereas attending physicians reported more favorable ratings than housestaff physicians in 16/18 items. The rank order among provider groups showed a high degree of correlation (r=0.92, P<0.001).
| Survey Itema | Item Domain | Total, N=149, Mean (SD) | Nurses, N=53, Mean (SD) | Attending Physicians, N=21, Mean (SD) | House staff Physicians, N=75, Mean (SD)b |
|---|---|---|---|---|---|
| |||||
| Improves communication between nurses and physicians. | CCT | 6.26 (1.11) | 6.74 (0.59)c | 6.52 (1.03)d | 5.85 (1.26) |
| Improves awareness of clinical issues needing to be addressed. | CCT | 6.05 (1.12) | 6.57 (0.64)c | 5.95 (1.07) | 5.71 (1.26) |
| Improves team‐building between nurses and physicians. | CCT | 6.03 (1.32) | 6.72 (0.60)c | 6.14 (1.11) | 5.52 (1.51) |
| Improves coordination of the patient's care. | CCT | 5.98 (1.34) | 6.60 (0.72)c | 6.00 (1.18) | 5.53 (1.55) |
| Improves nursing contributions to a patient's care plan. | CCT | 5.91 (1.25) | 6.47 (0.77)c | 6.14 (0.85) | 5.44 (1.43) |
| Improves quality of care delivered in our unit. | O | 5.72 (1.42) | 6.34 (0.83)c | 5.81 (1.33) | 5.25 (1.61) |
| Improves appreciation of the roles/contributions of other providers. | CCT | 5.69 (1.49) | 6.36 (0.86)c | 5.90 (1.04) | 5.16 (1.73) |
| Promotes shared decision making between patients and providers. | P | 5.62 (1.51) | 6.43 (0.77)c | 5.57 (1.40) | 5.05 (1.68) |
| Improves patients' satisfaction with their hospitalization. | P, O | 5.53 (1.40) | 6.15 (0.95)c | 5.38 (1.12) | 5.13 (1.58) |
| Provides more respect/dignity to patients. | P | 5.31 (1.55) | 6.23 (0.89)c | 5.10 (1.18) | 4.72 (1.71) |
| Decreases number of pages/phone calls between nurses and physicians. | EP | 5.28 (1.82) | 6.28 (0.93)c | 5.24 (1.30) | 4.57 (2.09) |
| Improves educational opportunities for housestaff/students. | E | 5.07 (1.77) | 6.08 (0.98)c | 4.81 (1.60) | 4.43 (1.93) |
| Improves the efficiency of your work. | EP | 5.01 (1.77) | 6.04 (1.13)c | 4.90 (1.30) | 4.31 (1.92) |
| Improves adherence to evidence‐based guidelines or interventions. | EP | 4.89 (1.79) | 6.06 (0.91)c | 4.00 (1.18) | 4.31 (1.97) |
| Improves the accuracy of your sign‐outs (or reports) to the next shift. | EP | 4.80 (1.99) | 6.30 (0.93)c | 4.05 (1.66) | 3.95 (2.01) |
| Reduces ordering of unnecessary tests and treatments. | O | 4.51 (1.86) | 5.77 (1.15)c | 3.86 (1.11) | 3.8 (1.97) |
| Improves the timeliness of consultations. | EP | 4.28 (1.99) | 5.66 (1.22)c | 3.24 (1.48) | 3.59 (2.02) |
| Decreases patients' hospital length of stay. | O | 4.15 (1.68) | 5.04 (1.24)c | 3.95 (1.16) | 3.57 (1.81) |
Barriers to BIRs
Respondents' perceptions of barriers to BIRs are shown by mean value (between 1 and 7) for the total respondent pool and by each participant group (Table 3). The 6 highest‐ranked barriers were related to time, including nursing staff have limited time, the time required for bedside nurse‐physician encounters, and coordinating the start time of encounters with arrival of both physicians and nursing. The lowest‐ranked barriers were related to provider‐ and patient‐related factors, including patient lack of comfort with bedside nurse‐physician encounters, attending physicians/housestaff lack bedside skills, and attending physicians lack comfort with bedside nurse‐physician encounters. Comparing mean values between groups, 10 of 21 items showed statistical differences (P<0.05). The rank order among groups showed moderate correlation (nurses‐attending physicians r=0.62, nurses‐housestaff physicians r=0.76, attending physicians‐housestaff physicians r=0.82). A qualitative inspection of disparities among respondent groups highlighted that nursing staff were more likely to rank bedside rounds are not part of the unit's culture lower than physician groups.
| Survey Itema | Item Domain | Total, N=149, Mean (SD) | Nurses, n=53, Mean (SD) | Attending Physicians, n=21, Mean (SD) | Housestaff Physicians, n=75,b Mean (SD) |
|---|---|---|---|---|---|
| |||||
| Nursing staff have limited time. | T | 4.89 (1.34) | 4.96 (1.27) | 4.86 (1.65) | 4.85 (1.30) |
| Coordinating start time of encounters with arrival of physicians and nursing. | T | 4.80 (1.50) | 4.58 (1.43) | 5.24 (1.45) | 4.84 (1.55) |
| Housestaff have limited time. | T | 4.68 (1.47) | 4.56 (1.26) | 4.24 (1.81) | 4.89 (1.48) |
| Attending physicians have limited time. | T | 4.50 (1.49) | 4.81 (1.34) | 4.33 (1.65) | 4.34 (1.53) |
| Other acutely sick patients in unit. | T | 4.39 (1.42) | 4.79 (1.30)c | 4.52 (1.21) | 4.08 (1.49) |
| Time required for bedside nurse‐physician encounters. | T | 4.32 (1.55) | 4.85 (1.38)c | 3.62 (1.80) | 4.15 (1.49) |
| Lack of use of the pink‐rounding light to alert nursing staff. | S | 3.77 (1.75) | 4.71 (1.70)c | 3.48 (1.86) | 3.19 (1.46) |
| Patient not available (eg, off to test, getting bathed) | S | 3.74 (1.40) | 3.98 (1.28) | 4.52 (1.36)d | 3.35 (1.37) |
| Large team size. | S | 3.64 (1.74) | 3.12 (1.58)c | 3.95 (1.83) | 3.92 (1.77) |
| Patients in dispersed locations (eg, other units or in different hallways). | S | 3.64 (1.77) | 2.77 (1.55)c | 4.52 (1.83) | 4.00 (1.66) |
| Bedside nurse‐physician rounds are not part of the unit's culture. | S | 3.35 (1.94) | 2.25 (1.47)c | 4.76 (1.92) | 3.72 (1.85) |
| Limitations in physical facilities (eg, rooms too small, limited chairs). | S | 3.25 (1.71) | 2.71 (1.72) | 3.33 (1.71) | 3.59 (1.62) |
| Insufficient nurse engagement during bedside nurse‐physician encounters. | PR | 3.24 (1.63) | 2.71 (1.47)c | 3.67 (1.68) | 3.49 (1.65) |
| Patient on contact or respiratory isolation. | S | 3.20 (1.82) | 2.42 (1.67)c | 3.43 (1.63) | 3.69 (1.80) |
| Language barrier between providers and patients. | P | 2.69 (1.37) | 2.77 (1.39) | 2.57 (1.08) | 2.68 (1.43) |
| Privacy/sensitive patient issues. | P | 2.65 (1.45) | 2.27 (1.24) | 2.57 (1.33) | 2.93 (1.56) |
| Housestaff lack comfort with bedside nurse‐physician encounters. | PR | 2.55 (1.49) | 2.48 (1.15) | 2.67 (1.68) | 2.57 (1.65) |
| Nurses lack comfort with bedside nurse‐physician encounters. | PR | 2.45 (1.45) | 2.35 (1.27) | 2.48 (1.66) | 2.51 (1.53) |
| Attending physicians lack comfort with bedside nurse‐physician encounters. | PR | 2.35 (1.38) | 2.33 (1.25) | 2.33 (1.62) | 2.36 (1.41) |
| Attending physician/housestaff lack bedside skills (eg, history, exam). | PR | 2.34 (1.34) | 2.19 (1.19) | 2.85 (1.69) | 2.30 (1.32) |
| Patient lack of comfort with bedside nurse‐physician encounters. | P | 2.33 (1.48) | 2.23 (1.37) | 1.95 (1.32) | 2.5 (1.59) |
DISCUSSION
In this study, we sought to compare perceptions of nurses and physicians on the benefits and barriers to BIRs. Nursing staff ranked each benefit higher than physicians, though rank orders of specific benefits were highly correlated. Highest‐ranked benefits related to coordination and communication more than quality or process benefits. Across groups, the highest‐ranked barriers to BIRs were related to time, whereas the lowest‐ranked factors were related to provider and patient discomfort. These results highlight important similarities and differences in perceptions between front‐line providers.
The highest‐ranked benefits were related to improved interprofessional communication and coordination. Combining interprofessional team members during care delivery allows for integrated understanding of daily care plans and clinical issues, and fosters collaboration and a team‐based atmosphere.[1, 20, 26] The lowest‐ranked benefits were related to more tangible measures, including length of stay, timely consultations, and judicious laboratory ordering. This finding contrasts with the limited literature demonstrating increased efficiency in general medicine units practicing IPCC.[16] These rankings may reflect a poor understanding or self‐assessment of outcome measures by healthcare providers, representing a potential focus for educational initiatives. Future investigations using objective assessment methods of outcomes and collaboration will provide a more accurate understanding of these findings.
The highest‐ranked barriers were related to time and systems issues. Several studies of physician‐based bedside rounds have identified systems‐ and time‐related issues as primary limiting barriers.[22, 24] In units without colocalization of patients and providers, finding receptive times for BIRs can be difficult. Although time‐related issues could be addressed by decreasing patient‐provider ratios, these changes require substantial investment in resources. A reasonable degree of improvement in efficiency and coordination is expected following acclimation to BIRs or by addressing modifiable systems factors to increase this activity. Less costly interventions, such as tailoring provider schedules, prescheduling patient rounding times, and geographic colocalization of patients and providers may be more feasible. However, the clinical microsystems within which medicine patients are cared for are often chaotic and disorganized at the infrastructural and cultural levels, which may be less influenced by surface‐level interventions. Such interventions may be ward specific and require customization to individual team needs.
The lowest‐ranked barriers to BIRs were related to provider‐ and patient‐related factors, including comfort level of patients and providers. Prior work on bedside rounds has identified physicians who are apprehensive about performing bedside rounds, but those who experience this activity are more likely to be comfortable with it.[12, 28] Our results from a culture where BIRs occur on nearly two‐thirds of patients suggest provider discomfort is not a predominant barrier.[22, 29] Additionally, educators have raised concerns about patient discomfort with bedside rounds, but nearly all studies evaluating patients' perspectives reveal patient preference for bedside case presentations over activities occurring in alternative locations.[30, 31, 32] Little work has investigated patient preference for BIRs as per our definition; our participants do not believe patients are discomforted by BIRs, building upon evidence in the literature for patient preferences regarding bedside activities.
Nursing staff perceptions of the benefits and culture related to BIRs were more positive than physicians. We hypothesize several reasons for this disparity. First, nursing staff may have more experience with observing and understanding the positive impact of BIRs and therefore are more likely to understand the positive ramifications. Alternatively, nursing staff may be satisfied with active integration into traditional physician‐centric decisions. Additionally, the professional culture and educational foundation of the nursing culture is based upon a patient‐centered approach and therefore may be more aligned with the goals of BIRs. Last, physicians may have competing priorities, favoring productivity and didactic learning rather than interprofessional collaboration. Further investigation is required to understand differences between nurses and physicians, in addition to other providers integral to BIRs (eg, care coordinators, pharmacists). Regardless, during the implementation of interprofessional collaborative care models, our findings suggest initial challenges, and the focus of educational initiatives may necessitate acclimating physician groups to benefits identified by front‐line nursing staff.
There are several limitations to our study. We investigated the perceptions of medicine nurses and physicians in 1 teaching hospital, limiting generalizability to other specialties, other vital professional groups, and nonteaching hospitals. Additionally, BIRs has been a focus of our hospital for several years. Therefore, perceived barriers may differ in BIRs‐nave hospitals. Second, although pilot‐tested for content, the construct validity of the instrument was not rigorously assessed, and the instrument was not designed to measure benefits and barriers not explicitly identified during pilot testing. Last, although surveys were anonymous, the possibility of social desirability bias exists, thereby limiting accuracy.
For over a century, physician‐led rounds have been the preferred modality for point‐of‐care decision making.[10, 15, 32, 33] BIRs address our growing understanding of patient‐centered care. Future efforts should address the quality of collaboration and current hospital and unit structures hindering patient‐centered IPCC and patient outcomes.
Acknowledgements
The authors thank the medicine nursing staff and physicians for their dedication to patient‐centered care and willingness to participate in this study.
Disclosures: The Department of Medicine at the Penn State Hershey Medical Center provided funding for this project. There are no conflicts of interest to report.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- . Teamswork! Hosp Health Netw. 2012;86(3):24–27, 21.
- , , , . The coming of age for interprofessional education and practice. Am J Med. 2013;126(4):284–288.
- , . Payment incentives and integrated care delivery: levers for health system reform and cost containment. Inquiry. 2011;48(4):277–287.
- . Payment reform and the mission of academic medical centers. N Engl J Med. 2010;363(19):1784–1786.
- Josiah Macy Jr. Foundation. Transforming patient care: aligning interprofessional education and clinical practice redesign. In: Proceedings of the Josiah Macy Jr. Foundation Conference; January 17–20, 2013; Atlanta, GA.
- , , , . Bridging the quality chasm: interprofessional teams to the rescue? Am J Med. 2013;126(4):276–277.
- . Attending rounds: guidelines for teaching on the wards. J Gen Intern Med. 1992;7(1):68–75.
- , . Teaching at the bedside: a new model. Med Teach. 2003;25(2):127–130.
- . On bedside teaching. Ann Intern Med. 1997;126(3):217–220.
- , , , . Relationships of the location and content of rounds to specialty, institution, patient‐census, and team size. PloS One. 2010;5(6):e11246.
- , , , . Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110.
- , , , et al. Attending rounds in the current era: what is and is not happening. JAMA Intern Med. 2013;173(12):1084–1089.
- , , , et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684.
- , , , , . Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med. 2007;22(8):1073–1079.
- , , . A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement. Med Care. 1998;36(8 suppl):AS4–AS12.
- , , , . A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275–280.
- , . The challenge of innovation implementation. Acad Manage Rev. 1996;21(4):1055–1080.
- , , , . Ocular dipping in creutzfeldt‐jakob disease. J Clin Neurol. 2014;10(2):162–165.
- , , , et al. The value of bedside rounds: a multicenter qualitative study. Teach Learn Med. 2013;25(4):326–333.
- , , , et al. The art of bedside rounds: a multi‐center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412–420.
- , , , et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326–334.
- , . Bedside teaching in medical education: a literature review. Perspec Med Educ. 2014;3(2):76–88.
- , , . Impediments to bed‐side teaching. Med Educ. 1998;32(2):159–162.
- , , , . Whither bedside teaching? A focus‐group study of clinical teachers. Acad Med. 2003;78(4):384–390.
- , . Staff preference for multidisciplinary rounding practices in the critical care setting. 2011. Paper presented at: Design July 6–10, 2011. Boston, MA. Available at: http://www.designandhealth.com/uploaded/documents/Awards‐and‐events/WCDH2011/Presentations/Friday/Session‐8/DianaAnderson.pdf. Accessed July 6, 2014.
- , . Health Measurement Scales: A Practical Guide to Their Development and Use. 2nd ed. New York, NY: Oxford University Press; 1995.
- , , . Student and patient perspectives on bedside teaching. Med Educ. 1997;31(5):341–346.
- , , , , , . The positive impact of portfolios on health care assistants' clinical practice. J Eval Clin Pract. 2008;14(1):172–174.
- , , , . The physiologic and psychological effects of the bedside presentation. N Engl J Med. 1989;321(18):1273–1275.
- , , , , . The effect of bedside case presentations on patients' perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155.
- , , , . The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792–798.
- . Bedside rounds revisited. N Engl J Med. 1997;336(16):1174–1175.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- . Teamswork! Hosp Health Netw. 2012;86(3):24–27, 21.
- , , , . The coming of age for interprofessional education and practice. Am J Med. 2013;126(4):284–288.
- , . Payment incentives and integrated care delivery: levers for health system reform and cost containment. Inquiry. 2011;48(4):277–287.
- . Payment reform and the mission of academic medical centers. N Engl J Med. 2010;363(19):1784–1786.
- Josiah Macy Jr. Foundation. Transforming patient care: aligning interprofessional education and clinical practice redesign. In: Proceedings of the Josiah Macy Jr. Foundation Conference; January 17–20, 2013; Atlanta, GA.
- , , , . Bridging the quality chasm: interprofessional teams to the rescue? Am J Med. 2013;126(4):276–277.
- . Attending rounds: guidelines for teaching on the wards. J Gen Intern Med. 1992;7(1):68–75.
- , . Teaching at the bedside: a new model. Med Teach. 2003;25(2):127–130.
- . On bedside teaching. Ann Intern Med. 1997;126(3):217–220.
- , , , . Relationships of the location and content of rounds to specialty, institution, patient‐census, and team size. PloS One. 2010;5(6):e11246.
- , , , . Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110.
- , , , et al. Attending rounds in the current era: what is and is not happening. JAMA Intern Med. 2013;173(12):1084–1089.
- , , , et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684.
- , , , , . Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med. 2007;22(8):1073–1079.
- , , . A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement. Med Care. 1998;36(8 suppl):AS4–AS12.
- , , , . A randomized, controlled trial of bedside versus conference‐room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120(2):275–280.
- , . The challenge of innovation implementation. Acad Manage Rev. 1996;21(4):1055–1080.
- , , , . Ocular dipping in creutzfeldt‐jakob disease. J Clin Neurol. 2014;10(2):162–165.
- , , , et al. The value of bedside rounds: a multicenter qualitative study. Teach Learn Med. 2013;25(4):326–333.
- , , , et al. The art of bedside rounds: a multi‐center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412–420.
- , , , et al. Identifying and overcoming the barriers to bedside rounds: a multicenter qualitative study. Acad Med. 2014;89(2):326–334.
- , . Bedside teaching in medical education: a literature review. Perspec Med Educ. 2014;3(2):76–88.
- , , . Impediments to bed‐side teaching. Med Educ. 1998;32(2):159–162.
- , , , . Whither bedside teaching? A focus‐group study of clinical teachers. Acad Med. 2003;78(4):384–390.
- , . Staff preference for multidisciplinary rounding practices in the critical care setting. 2011. Paper presented at: Design July 6–10, 2011. Boston, MA. Available at: http://www.designandhealth.com/uploaded/documents/Awards‐and‐events/WCDH2011/Presentations/Friday/Session‐8/DianaAnderson.pdf. Accessed July 6, 2014.
- , . Health Measurement Scales: A Practical Guide to Their Development and Use. 2nd ed. New York, NY: Oxford University Press; 1995.
- , , . Student and patient perspectives on bedside teaching. Med Educ. 1997;31(5):341–346.
- , , , , , . The positive impact of portfolios on health care assistants' clinical practice. J Eval Clin Pract. 2008;14(1):172–174.
- , , , . The physiologic and psychological effects of the bedside presentation. N Engl J Med. 1989;321(18):1273–1275.
- , , , , . The effect of bedside case presentations on patients' perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155.
- , , , . The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792–798.
- . Bedside rounds revisited. N Engl J Med. 1997;336(16):1174–1175.
© 2014 Society of Hospital Medicine
AAB Therapy Risks in Orthopedic Surgery
Patients presenting for surgery with angiotensin axis blockade (AAB) from therapy with either angiotensin‐converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) experience an increased incidence of perioperative hypotension.[1, 2, 3, 4] Debate continues as to whether this hypotension results in any significant clinical sequelae. Some authors found that the use of an ACEI decreased the incidence of acute kidney injury (AKI),[5] mortality, and septicemia in cardiac and vascular surgical patients.[6] However, others found that in vascular and cardiac surgery there is increased mortality[7] as well as increased incidence of postoperative AKI.[8, 9, 10] A retrospective study of 10,000 coronary artery bypass graft patients found that ACEI was associated with increased inotropic support, AKI, mortality, and new onset atrial fibrillation.[11] In a meta‐analysis of 69,000 cardiothoracic surgery patients, the use of ACEIs/ARBs was associated with an increase in AKI and mortality.[12] AKI has also been demonstrated after lung resection surgery in patients receiving preoperative therapy with an ARB.[13]
Studies on noncardiac general surgery patients demonstrate that the use of AAB results in postinduction hypotension, but they fail to show an increased incidence in postoperative AKI.[14, 15] We propose, however, that major orthopedic surgery patients are a specific surgical cohort, like cardiac, vascular, and lung, who can develop operative hypotension and postoperative AKI when AAB is taken on the morning of surgery. To address this question we performed a retrospective study of 1154 patients undergoing either spinal fusion, total knee arthroplasty (TKA), or total hip arthroplasty (THA) during the 2010 calendar year in our academic medical center. We measured the incidence of postanesthesia induction hypotension, intraoperative hypotension, and postoperative AKI as it relates to the administration of AAB preoperatively.
MATERIALS AND METHODS
This study was a retrospective, observational investigation at a single, large academic hospital. The study design for chart review was approved by the institutional review board prior to data collection. Informed patient consent was not required for this retrospective study.
Patient Selection
We retrospectively reviewed the computerized chart and operating room electronic medical records of all patients who underwent elective major orthopedic surgery in the 2010 calendar year. We chose vertebral spine fusion, TKA, and THA as the 3 surgeries to represent major elective orthopedic surgery. Electronic query of the hospital database identified 1154 patients having undergone these surgeries in the year 2010. Nine hundred twenty‐two patients met inclusion criteria: 21 years old and evaluated in the preanesthesia clinic with documented vital signs and clearly defined preoperative medication recommendations. The policy in the preanesthesia clinic was to recommend taking the ACEI and ARB on the morning of surgery. All 922 patients were included in the analysis of the outcomes for induction hypotension and intraoperative hypotension. Of the 922 patients, 798 had the documented preoperative and postoperative creatinine values needed to define AKI. Therefore, only these 798 patients were included in the AKI outcome analysis. During the time of the study it was the practice at our medical center that all such surgeries were performed under general anesthesia.
Data Collection
Preanesthesia records were reviewed for patient demographics including age, body mass index (BMI), baseline blood pressure, diabetes mellitus (DM), coronary artery disease (CAD), hypertension (HTN), and congestive heart failure (CHF), as well as for therapy with ACEI or ARB, diuretics, ‐blockers, nonsteroidal anti‐inflammatory drugs (NSAIDs), and calcium channel blockers (CCB). The 4 statistically and clinically significant comorbidities were looked at individually as well as added together for a total sum of weighted comorbidity risk factors. The Anesthesia Electronic Record (Surginet Anesthesia, Kansas City, MO) was reviewed for each corresponding patient to determine the general anesthesia induction agent used and to assess the postinduction and intraoperative systolic blood pressures. Blood pressure was determined using an automated blood pressure cuff and automatically recorded at intervals of 5 minutes or less. Further, ephedrine, phenylephrine and vasopressin doses, estimated blood loss, blood transfusion requirements, and intravenous fluid administration (colloid and crystalloid) were noted. Preoperative (<30 days) and postoperative (within 24 hours after surgery) serum creatinine and hematocrit values were also recorded.
Outcome Measures
The primary outcome measures studied were:
- Postinduction hypotension (systolic blood pressure [SBP] 80 mm Hg for5 minutes) occurring within 30 minutes after anesthesia induction but before surgical incision.[16]
- Intraoperative hypotension (SBP 80 mm Hg for 10 minutes) occurring after surgical incision.[16]
- Postoperative AKI defined as an increase in serum creatinine 0.3 mg/dL or an increase of 50% from preoperative creatinine (Kidney Disease: Improving Global Outcomes Clinical Practice Guideline for Acute Kidney Injury)[17] within 24 hours postoperatively.
The secondary outcome measures were:
- Hospital length of stay (LOS).
- Two‐year mortality associated with the development of AKI.
Statistical Analysis
Categorical variables were summarized with frequencies and percentages, whereas continuous variables were summarized with means, standard deviations, medians, and quartiles. A [2] test or a Wilcoxon rank sum test was used to determine differences in preoperative and intraoperative characteristics between those patients with AAB and those patients without AAB. Logistic regression was used to determine the association between the main outcome variables (hypotension at anesthetic induction, hypotension during the operative procedure, and postoperative AKI) and the primary independent variable, AAB, as well as other preoperative and intraoperative characteristics. The significance and magnitude of the associations were quantified with percentages and odds ratios. Exact logistic regression was used as necessary when expected cell counts were too small for the usual asymptotic logistic regression to be valid. The statistically significant (P<0.05) variables resulting from this bivariate analysis as well as important clinically significant variables with known associations with the outcome variables were included as covariates in a multivariable logistic regression model for each outcome variable with AAB. By adjusting for these covariates, any potential and unwanted variation resulting from differences between the AAB groups in other preoperative or postoperative characteristics is removed from the association between each outcome variable and AAB. Variance inflation factor and tolerance statistics were used to test for multicollinearity between all independent variables before including them in the final models. The Hosmer and Lemeshow goodness‐of‐fit test was used to assess the fit of the final models. Logistic regression was used to test the association of AKI with mortality, whereas a Wilcoxon rank sum test was used to test the difference in mean/median LOS between AKI and non‐AKI groups.
RESULTS
Preoperative, Surgical, and Anesthesia Data
A total of 922 patients met inclusion criteria, of which 343 (37%) were receiving AAB with either an ACEI or ARB preoperatively. Preoperative characteristics are documented in Table 1. Patients receiving AAB were older (63.010.8 vs 57.313.9 years) and had a higher BMI (34.67.3 vs 31.97.7) than patients not receiving this therapy. They were also more likely to be receiving diuretics, ‐blockers, and CCBs as well as have DM, CHF, CAD, and HTN. These characteristics were included as covariates in a multivariable logistic regression model so that any confounding resulting differences caused by these variables were removed from the association between each outcome variable and AAB use. There was no difference in baseline SBP or diastolic blood pressures. There was no difference in the use of NSAIDs. Patients receiving AAB underwent a higher percentage of TKAs (56.0% vs 44.2%) and lower percentage of spine fusions (16.6% vs 24.4%) and THAs (27.4% vs 31.4%). Propofol was the most commonly used general anesthetic induction agent (78%). Anesthetic induction agent usage was not different across the groups.
| AAB (N=343) | Non‐AAB (N=579) | P Value* | |
|---|---|---|---|
| |||
| Patient demographics | |||
| Age (y), meanSD | 63.010.8 | 57.313.9 | <0.001 |
| BMI (kg/m2), meanSD | 34.67.3 | 31.87.7 | <0.001 |
| Baseline systolic BP (mm Hg), meanSD | 135.016.8 | 130.819.8 | 0.339 |
| Baseline diastolic BP (mm Hg), meanSD | 74.514.5 | 75.311.8 | 0.798 |
| Medications | |||
| Diuretic, % | 53.6 | 18.5 | <0.001 |
| ‐Blocker, % | 39.4 | 22.4 | <0.001 |
| Calcium channel blocker, % | 23.3 | 9.9 | <0.001 |
| Nonsteroidal anti‐inflammatory drug, % | 36.1 | 35.7 | 0.901 |
| Comorbidities | |||
| Diabetes mellitus, % | 32.9 | 9.5 | <0.001 |
| Congestive heart failure, % | 2.9 | 0.4 | 0.001 |
| Coronary artery disease, % | 20.1 | 9.5 | <0.001 |
| Hypertension, % | 95.3 | 36.8 | <0.001 |
| Total comorbidities, meanSD | 1.50.7 | 0.50.7 | <0.001 |
| Procedure type | |||
| Spinal fusions, % | 16.6 | 24.4 | 0.001 |
| Total knee arthroplasty, % | 56.0 | 44.2 | 0.001 |
| Total hip arthroplasty, % | 27.4 | 31.4 | 0.001 |
| Induction agents | |||
| Etomidate, % | 14.9 | 11.9 | 0.199 |
| Propofol, % | 77.6 | 78.3 | 0.801 |
| Methohexital, % | 7.3 | 9.2 | 0.329 |
| Other (gas, ketamine), % | 0.3 | 1.2 | 0.270 |
| Hematocrit | |||
| Preoperative (%), meanSD | 40.53.7 | 40.23.8 | 0.150 |
| Postoperative (%), meanSD | 34.04.6 | 33.74.3 | 0.511 |
| % Change, meanSD | 15.38.5 | 16.88.9 | 0.036 |
| Creatinine | |||
| Preoperative (mg/dL), meanSD | 0.960.41 | 0.850.23 | <0.001 |
| Postoperative (mg/dL), meanSD | 0.960.42 | 0.810.23 | <0.001 |
| % change, meanSD | 1.4829.22 | 4.1414.18 | 0.235 |
| Fluids | |||
| Estimated blood loss (mL), meanSD | 301.2340.0 | 356.9482.7 | 0.125 |
| Crystalloid (mL), meanSD | 2584.41401.6 | 2765.21487.2 | 0.036 |
| Colloid (mL), meanSD | 124.3322.4 | 151.0553.5 | 0.810 |
| Packed red blood cells (mL), meanSD | 78.5323.1 | 99.5452.0 | 0.613 |
| Vasopressors | |||
| Ephedrine (mg), meanSD | 11.715.0 | 8.013.0 | <0.001 |
| Phenylephrine (g), meanSD | 615.72210.9 | 687.13905.3 | 0.002 |
| Vasopressin (U), meanSD | 0.351.90 | 0.080.90 | <0.001 |
| Outcomes | |||
| Induction hypotension, % | 12.2 | 1.93 | 0.005 |
| Intraoperative hypotension, % | 26.0 | 20.9 | 0.078 |
| Acute kidney injury, % | 8.3 | 1.7 | <0.001 |
Estimated blood loss for the procedures was similar between the 2 groups (301.2340 vs 356.9482.7 mL) and similar colloid and packed red cell administration occurred. However, patients receiving AAB were administered less crystalloid infusion (2584.41401.6 vs 2765.21487.2 mL, P=0.036) and received less phenylephrine but higher ephedrine and vasopressin dosages as a group. Patients in both groups had similar preoperative and postoperative hematocrit concentrations. Average preoperative serum creatinine was higher in the AAB group than in the non‐AAB group (0.960.41 vs 0.850.23, P<0.001) and remained so postoperatively (0.960.42 vs 0.810.23, P<0.001).
Primary and Secondary Outcome Measures
Postinduction Hypotension
Therapy with AAB was associated with a greater incidence of postinduction hypotension (12.2% vs 6.7%, P=0.005). Using a multivariate logistic regression model adjusting for the effects of age, BMI, antihypertensive medications, comorbidities, and anesthetic induction agents, the use of AAB had a greater odds ratio (OR) of 1.93 (95% confidence interval [CI]: 1.10‐3.41, P=0.023) for developing postinduction hypotension (Table 2). A higher BMI had a lower OR for postinduction hypotension.
| Comparison | Hypotension at Induction, OR (95% CI), P Value | Intraoperative Hypotension, OR (95% CI), P Value | Acute Kidney Injury, OR (95% CI), P Value |
|---|---|---|---|
| |||
| AAB vs none, unadjusted | 1.93 (1.223.06), 0.005 | 1.33 (0.971.82), 0.078 | 5.40 (2.4112.06), <0.001 |
| AAB vs none, adjusted for covariates | 1.93 (1.103.41), 0.023 | 1.30 (0.851.97), 0.226 | 2.68 (1.086.69), 0.034 |
| AAB vs none, adjusted for covariates+hypotension at induction | N/A | N/A | 2.51 (1.06.32), 0.051 |
| AAB vs none, adjusted for covariates+intraoperative hypotension | N/A | N/A | 2.66 (1.066.64), 0.037 |
| AAB vs none, adjusted for covariates+any hypotension | N/A | N/A | 2.60 (1.046.51), 0.042 |
Postincision (Intraoperative) Hypotension
The incidence of postincision, intraoperative hypotension in patients receiving AAB (26.0%) was not statistically different (P=0.078) from those not receiving these agents (20.9%). Multivariate logistic regression demonstrated that preoperative hypertension (OR: 1.73, 95% CI: 1.05‐2.85, P=0.031) and THA were each independent risk factors for intraoperative hypotension. The other comorbidities of DM, CHF, CAD, and the individual antihypertensive agents were not found to have a strong influence on the outcome of intraoperative hypotension. The odds ratio of developing intraoperative hypotension during the procedure in patients receiving AAB was not statistically significant (OR: 1.30, 95% CI: 0.85‐1.97, P=0.226) from those not receiving this therapy preoperatively (Table 2).
AKI
There was a significantly higher incidence of AKI (26/313 [8.3%] vs 8/485 [1.7%], P<0.001) in patients receiving preoperative AAB. No patients required renal replacement therapy. Of those patients who developed postoperative AKI, 73% of the AAB group and 75% of the non‐AAB group had a normal glomerular filtration rate (GFR) (mL/min/1.73 m2, GFR >90 prior to surgery. Of both the AAB and non‐AAB groups, 20% to 25% were in stage 2 (GFR 6089) chronic kidney disease (CKD)[18] preoperatively. Only 2 patients in the AAB group began in stage 3 (GFR 3059) CKD. Fifty percent of both groups went from stage 1 kidney function to stage 3. For all others who developed AKI, the GFR rose by a single stage.
Multivariate logistic regression, controlling for statistically significant and clinically significant variables, demonstrated that AAB administered preoperatively was independently associated with a greater OR of 2.68 (95% CI: 1.08‐6.69, P=0.034) for developing AKI postoperatively than if AAB was not taken (Table 2). Higher BMI was a further independent risk factor for postoperative AKI; a 5‐unit increase in BMI revealed an OR of 1.58 (95% CI: 1.25‐1.99, P<0.001) for experiencing postoperative AKI. Although the AAB group had statistically significantly more comorbidities, in the final analysis only the presence of CAD trended to an association with the development of AKI (OR: 2.37, 95% CI: 1.005.60, P=0.050).
We wished to determine whether the increased risk of AKI associated with AAB therapy was explained by the associated postinduction or postincision, intraoperative hypotension experienced by the patients or independent of these effects. To do so we accounted for the development of either postinduction or intraoperative hypotension as a possible confounder in the multivariate analysis for the development of AKI (Table 2). Postinduction hypotension alone was not statistically associated with AKI (OR 2.04, 95% CI: 0.70‐6.0, P=0.193). However, intraoperative hypotension was found to be an independent risk factor for the development of AKI (OR: 2.62, 95% CI: 1.17‐5.84, P=0.019). When eliminating the effect of this intraoperative hypotension as a confounder, patients on AAB therapy continued to have a 2.66 OR for the development of AKI postoperatively (95% CI: 1.06‐6.64, P=0.037), independent of the development of intraoperative hypotension. When eliminating the effect of both postinduction and intraoperative hypotension (all hypotension Table 2), AAB therapy continued to have a statistically significant independent effect (OR: 2.60, 95% CI: 1.046.51, P=0.042) on developing postoperative AKI.
As secondary outcome measures, we looked at the development of AKI and its relationship to hospital LOS and mortality. The development of AKI was associated with a significantly greater mean length of hospital stay (5.76 days vs 3.28 days, P<0.001). Although 2‐year mortality was higher, 5.9% in the AKI group compared to 2.4% in the non‐AAB group, it was not statistically significant (P=0.211).
DISCUSSION
In this retrospective review of 922 patients presenting for major orthopedic surgery, we found that 343(37%) were receiving therapy with either ACEIs or ARBs. In such patients, we demonstrated a higher incidence of postinduction hypotension and an increased incidence of AKI. We further demonstrated that the development of AKI associated with AAB therapy was independent of hypotension occurring either postinduction or intraoperatively after incision.
Postinduction hypotension in patients receiving AAB was demonstrated to be 12.2% compared to 7.7% in patients not receiving this therapy. Hypotension after general anesthesia induction in patients receiving AAB is widely reported,[1, 14, 15] and ranges from 22% to 100%[19, 20] based on varying definitions of what constitutes hypotension. We chose an absolute value of a systolic blood pressure of 80 mm Hg occurring for 5 minutes as constituting significant hypotension.[16] Monk et al. reported an increased one year postnon‐cardiac surgery mortality risk of 1.036 times per minute of intraoperative hypotension, defining hypotension as a systolic blood pressure of <80 mm Hg.[21]
We further demonstrated that AAB therapy resulted in an 8.3% incidence of AKI versus 1.7% in non‐AAB patients (P<0.001). AKI was defined as an increase in serum creatinine of 0.3 mg/dL or a 50% increase in creatinine when pre‐ and postoperative values were compared.[17] A number of other investigators have identified AKI associated with AAB use in patients undergoing cardiac,[6, 11] vascular,[7, 10] and lung[13] surgery. Similarly, in the present study, in orthopedic patients, AAB remained a significant risk factor for developing AKI (OR: 2.68, P=0.034) independent of patient comorbidities and adjunct therapy (Table 2).
ACEIs and ARBs are prescribed to treat HTN, CHF, and improve renal function in diabetic and proteinuric nephropathy.[22] AAB therapy is prescribed for nephropathy because these medications decrease glomerular pressure by selective inhibition of angiotensin II mediated vasoconstriction of the efferent glomerular arteriole.[23] Normally, this is beneficial to patients and is associated with a decrease in serum creatinine concentration. However, during hypotension, when there is decreased renal perfusion, further decreases in intraglomerular pressure may occur, precipitating renal failure.[23] In addition, other factors may contribute to the development of AKI, as AAB has both tissue and systemic effects that extend beyond simply dilating the efferent glomerular arteriole. These include effects on the sympathetic nervous system, oxidative stress, and altering the release and synthesis of vasodilators such as bradykinin, nitric oxide, and prostacyclins[24] as well as effects through the release of aldosterone and arginine‐vasopressin.[25] These other factors might help explain the present study's findings that, when eliminating the effect of both postinduction and intraoperative hypotension, AAB therapy continued to have a statistically significant independent effect (OR: 2.60, 95% CI: 1.046.51, P=0.042) on developing postoperative AKI.
Although we demonstrated an association of AAB therapy with the development of hypotension after induction, we demonstrated only a trend in the development of postincisional, intraoperative hypotension (P=0.078). We defined intraoperative hypotension as a systolic BP <80 mm Hg for 10 minutes occurring after skin incision.[16] One must take into consideration, however, that a significant number of AAB patients were hypotensive during induction and received higher doses of ephedrine and vasopressin during the operative period. These patients may have been rescued from intraoperative hypotension by receiving vasopressor treatment at the outset. We did find that intraoperative hypotension was a significant, independent risk factor for AKI (OR: 2.62, P=0.019).
We looked further at the consequences of developing AKI. Patients who developed AKI had a significant greater mean length of hospital stay (5.76 days vs 3.28 days, P<0.001), which is consistent with other investigators' findings.[25, 26, 27] Although 2‐year mortality was higher at 5.88% in the AKI group compared to 2.38% in the non‐AAB group, this was not statistically significant (P=0.211). Other studies have shown that the development of AKI results in greater mortality.[26, 28]
The American College of Physicians (ACP) recommendations as of 2013 regarding the use of ACEIs and ARBs preoperatively is: uncertain, continue with caution, avoid hypovolemia. Potential for hypotension with induction of anesthesia and increased vasoconstrictor requirements and decreased responsiveness to pressors.[29] The ACP acknowledges that preoperative ACEIs and ARBs have the potential for postinduction hypotension and increased requirements for vasopressors. We have implemented recommendations at our preoperative anesthesia clinic to hold ACEIs and ARBs on the morning of surgery in patients with controlled blood pressure scheduled for spine fusion, and hip and knee arthroplasties. In accordance with ACP guidelines, other antihypertensives such as ‐blockers, calcium channel blockers, nitrates, and sympatholytics should be continued preoperatively and can be used perioperatively.
Limitations of the Study
There are several limitations to our study. This was a retrospective analysis over a fixed time period in one academic institution. Further, because of the retrospective nature, anesthesia and intraoperative (fluid and vasoconstrictor) management was not standardized. The definition of hypotension (SBP 80 mm Hg for 5 minutes after induction and 10 minutes after incision) may have been too stringent, so that more subtle decreases in blood pressure that could have impacted AKI might not have been captured to show statistical significance. Thus, our finding, that the development of AKI associated with preoperative AAB therapy may be independent of the occurrence of hypotension, must be interpreted with this in mind.
CONCLUSIONS
Patients who receive preoperative ACEI or ARB therapy and undergo major orthopedic surgery such as spinal fusion, and hip or knee arthroplasties experience a higher incidence of postinduction hypotension and AKI than those not receiving such therapy. The development of AKI in such patients is associated with a significantly prolonged length of hospital stay. Our findings suggest an association between preoperative ACEI/ARB use and moderate kidney injury following major orthopedic surgeries. However, a prospective, multicentered, randomized trial needs to be performed to confirm that withdrawal of AAB therapy preoperatively will decrease the incidence of AKI in patients undergoing major orthopedic procedures under general anesthesia. Future studies also need to determine the optimal time duration of withholding AAB therapy and the consequences on cardiac outcomes.
ACKNOWLEDGMENTS
Disclosures: Presented at the Society of Hospital Medicine National Meeting, May 18, 2013, National Harbor, Maryland; and the Society of General Internal Medicine Mid‐Atlantic Regional Meeting, March 1, 2013, Philadelphia, Pennsylvania. The authors report no conflicts of interest.
- . Management of hypotension associated with angiotensin‐axis blockade and general anesthesia administration. J Cardiothorac Vasc Anesth. 2013;27:156–167.
- , , , , , . Clinical consequences of withholding versus administering renin‐angiotensin‐aldosterone system antagonists in the preoperative period. J Hosp Med. 2008;3:319–325.
- , , , et al. Influence of chronic angiotensin‐converting enzyme inhibition on anesthetic induction. Anesthesiology. 1994;81(2):299–307.
- , , , , . Pressor responses to tracheal intubation after sublingual captopril. A pilot study. Anaesthesia. 1990;45(3):243–245.
- , , , , , , . Preoperative angiotensin‐converting enzyme inhibitors and acute kidney injury after coronary artery bypass grafting. Ann Thorac Surg. 2008;86(4):1160–1165.
- , , , et al. The effects of preoperative renin‐angiotensin system inhibitors on outcomes in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27(4):703–709.
- , , , . Renin‐angiotensin blockade is associated with increased mortality after vascular surgery. Can J Anaesth. 2010;57:736–744.
- , . , et al. Preoperative use of angiotensin‐converting enzyme inhibitors/angiotensin receptor blockers is associated with increased risk for acute kidney injury after cardiovascular surgery. Clin J Am Soc Nephrol. 2008;3(5):1266–1273.
- , , , et al.; TRIBE‐AKI Consortium. Preoperative angiotensin‐converting enzyme inhibitors and angiotensin receptor blocker use and acute kidney injury in patients undergoing cardiac surgery. Nephrol Dial Transplant. 2013;28(11):2787–2799.
- , , , et al. The chronic inhibition of angiotensin‐converting enzyme impairs postoperative renal function. Anesth Analg. 2001;93(5):1111–1115.
- , , , et al. Effects of angiotensin‐converting enzyme inhibitor therapy on clinical outcome in patients undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2009;54:1778–1784.
- , , , , , . Acute kidney injury and death associated with renin angiotensin system blockade in cardiothoracic surgery: a meta‐analysis of observational studies. Am J Kidney Dis. 2013;63(6):1077–1086.
- , , . Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg. 2012;114:1256–1262.
- , , , et al. Angiotensin system inhibitors in a general surgical population. Anesth Analg. 2005;100:636–644, table of contents.
- , , , , . Chronic angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker therapy combined with diuretic therapy is associated with increased episodes of hypotension in noncardiac surgery. J Cardiothorac Vasc Anesth. 2008;22:180–186.
- , , , , . Hemodynamic impact of dexmedetomidine administration in 15,656 noncardiac surgical cases. J Clin Anesth. 2012;24:212–220.
- Kidney Disease: Improving Global Outcomes (KDIGO). Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:8.
- Kidney Disease: Improving Global Outcomes (KDIGO). Clincal practice guidelines for evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):8.
- , . Hemodynamic effects of anesthesia in patients with ischemic heart failure chronically treated with angiotensin‐converting enzyme inhibitors. Anesth Analg. 1997;84:945–949.
- , , , , . The hemodynamic effects of anesthetic induction in vascular surgical patients chronically treated with angiotensin II receptor antagonists. Anesth Analg. 1999;89:1388–1392.
- , , , . Anesthetic management and one‐year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10.
- , , , , . Use of angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers in clinical practice. Expert Rev Cardiovasc Ther. 2012;10:159–166.
- , . An overview of drug‐induced acute kidney injury. Crit Care Med. 2008;36:S216–S223.
- , , , et al. Improvement of endothelial function by chronic angiotensin‐converting enzyme inhibition in heart failure: role of nitric oxide, prostanoids, oxidant stress, and bradykinin. Circulation. 2000;102:351–356.
- , , , . Renin‐angiotensin system antagonists in the perioperative setting: clinical consequences and recommendations for practice. Postgrad Med J. 2011;87:472–481.
- , , , , . Early postoperative statin therapy is associated with a lower incidence of acute kidney injury after cardiac surgery. J Cardiothorac Vasc Anesth. 2010;24:913–920.
- , , , , . Improved survival in acute kidney injury after cardiac surgery. Am J Kidney Dis. 2007;50:703–711.
- , , , . Determinants of postoperative acute kidney injury. Crit Care. 2009;13:R79.
- American College of Physicians. ACP Smart Medicine: Perioperative Medication Management. Tables: Perioperative Cardiovascular Medication Management. http://smartmedicine.acponline.org/content.aspx?gbosID=336. Accessed January 19, 2014.
Patients presenting for surgery with angiotensin axis blockade (AAB) from therapy with either angiotensin‐converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) experience an increased incidence of perioperative hypotension.[1, 2, 3, 4] Debate continues as to whether this hypotension results in any significant clinical sequelae. Some authors found that the use of an ACEI decreased the incidence of acute kidney injury (AKI),[5] mortality, and septicemia in cardiac and vascular surgical patients.[6] However, others found that in vascular and cardiac surgery there is increased mortality[7] as well as increased incidence of postoperative AKI.[8, 9, 10] A retrospective study of 10,000 coronary artery bypass graft patients found that ACEI was associated with increased inotropic support, AKI, mortality, and new onset atrial fibrillation.[11] In a meta‐analysis of 69,000 cardiothoracic surgery patients, the use of ACEIs/ARBs was associated with an increase in AKI and mortality.[12] AKI has also been demonstrated after lung resection surgery in patients receiving preoperative therapy with an ARB.[13]
Studies on noncardiac general surgery patients demonstrate that the use of AAB results in postinduction hypotension, but they fail to show an increased incidence in postoperative AKI.[14, 15] We propose, however, that major orthopedic surgery patients are a specific surgical cohort, like cardiac, vascular, and lung, who can develop operative hypotension and postoperative AKI when AAB is taken on the morning of surgery. To address this question we performed a retrospective study of 1154 patients undergoing either spinal fusion, total knee arthroplasty (TKA), or total hip arthroplasty (THA) during the 2010 calendar year in our academic medical center. We measured the incidence of postanesthesia induction hypotension, intraoperative hypotension, and postoperative AKI as it relates to the administration of AAB preoperatively.
MATERIALS AND METHODS
This study was a retrospective, observational investigation at a single, large academic hospital. The study design for chart review was approved by the institutional review board prior to data collection. Informed patient consent was not required for this retrospective study.
Patient Selection
We retrospectively reviewed the computerized chart and operating room electronic medical records of all patients who underwent elective major orthopedic surgery in the 2010 calendar year. We chose vertebral spine fusion, TKA, and THA as the 3 surgeries to represent major elective orthopedic surgery. Electronic query of the hospital database identified 1154 patients having undergone these surgeries in the year 2010. Nine hundred twenty‐two patients met inclusion criteria: 21 years old and evaluated in the preanesthesia clinic with documented vital signs and clearly defined preoperative medication recommendations. The policy in the preanesthesia clinic was to recommend taking the ACEI and ARB on the morning of surgery. All 922 patients were included in the analysis of the outcomes for induction hypotension and intraoperative hypotension. Of the 922 patients, 798 had the documented preoperative and postoperative creatinine values needed to define AKI. Therefore, only these 798 patients were included in the AKI outcome analysis. During the time of the study it was the practice at our medical center that all such surgeries were performed under general anesthesia.
Data Collection
Preanesthesia records were reviewed for patient demographics including age, body mass index (BMI), baseline blood pressure, diabetes mellitus (DM), coronary artery disease (CAD), hypertension (HTN), and congestive heart failure (CHF), as well as for therapy with ACEI or ARB, diuretics, ‐blockers, nonsteroidal anti‐inflammatory drugs (NSAIDs), and calcium channel blockers (CCB). The 4 statistically and clinically significant comorbidities were looked at individually as well as added together for a total sum of weighted comorbidity risk factors. The Anesthesia Electronic Record (Surginet Anesthesia, Kansas City, MO) was reviewed for each corresponding patient to determine the general anesthesia induction agent used and to assess the postinduction and intraoperative systolic blood pressures. Blood pressure was determined using an automated blood pressure cuff and automatically recorded at intervals of 5 minutes or less. Further, ephedrine, phenylephrine and vasopressin doses, estimated blood loss, blood transfusion requirements, and intravenous fluid administration (colloid and crystalloid) were noted. Preoperative (<30 days) and postoperative (within 24 hours after surgery) serum creatinine and hematocrit values were also recorded.
Outcome Measures
The primary outcome measures studied were:
- Postinduction hypotension (systolic blood pressure [SBP] 80 mm Hg for5 minutes) occurring within 30 minutes after anesthesia induction but before surgical incision.[16]
- Intraoperative hypotension (SBP 80 mm Hg for 10 minutes) occurring after surgical incision.[16]
- Postoperative AKI defined as an increase in serum creatinine 0.3 mg/dL or an increase of 50% from preoperative creatinine (Kidney Disease: Improving Global Outcomes Clinical Practice Guideline for Acute Kidney Injury)[17] within 24 hours postoperatively.
The secondary outcome measures were:
- Hospital length of stay (LOS).
- Two‐year mortality associated with the development of AKI.
Statistical Analysis
Categorical variables were summarized with frequencies and percentages, whereas continuous variables were summarized with means, standard deviations, medians, and quartiles. A [2] test or a Wilcoxon rank sum test was used to determine differences in preoperative and intraoperative characteristics between those patients with AAB and those patients without AAB. Logistic regression was used to determine the association between the main outcome variables (hypotension at anesthetic induction, hypotension during the operative procedure, and postoperative AKI) and the primary independent variable, AAB, as well as other preoperative and intraoperative characteristics. The significance and magnitude of the associations were quantified with percentages and odds ratios. Exact logistic regression was used as necessary when expected cell counts were too small for the usual asymptotic logistic regression to be valid. The statistically significant (P<0.05) variables resulting from this bivariate analysis as well as important clinically significant variables with known associations with the outcome variables were included as covariates in a multivariable logistic regression model for each outcome variable with AAB. By adjusting for these covariates, any potential and unwanted variation resulting from differences between the AAB groups in other preoperative or postoperative characteristics is removed from the association between each outcome variable and AAB. Variance inflation factor and tolerance statistics were used to test for multicollinearity between all independent variables before including them in the final models. The Hosmer and Lemeshow goodness‐of‐fit test was used to assess the fit of the final models. Logistic regression was used to test the association of AKI with mortality, whereas a Wilcoxon rank sum test was used to test the difference in mean/median LOS between AKI and non‐AKI groups.
RESULTS
Preoperative, Surgical, and Anesthesia Data
A total of 922 patients met inclusion criteria, of which 343 (37%) were receiving AAB with either an ACEI or ARB preoperatively. Preoperative characteristics are documented in Table 1. Patients receiving AAB were older (63.010.8 vs 57.313.9 years) and had a higher BMI (34.67.3 vs 31.97.7) than patients not receiving this therapy. They were also more likely to be receiving diuretics, ‐blockers, and CCBs as well as have DM, CHF, CAD, and HTN. These characteristics were included as covariates in a multivariable logistic regression model so that any confounding resulting differences caused by these variables were removed from the association between each outcome variable and AAB use. There was no difference in baseline SBP or diastolic blood pressures. There was no difference in the use of NSAIDs. Patients receiving AAB underwent a higher percentage of TKAs (56.0% vs 44.2%) and lower percentage of spine fusions (16.6% vs 24.4%) and THAs (27.4% vs 31.4%). Propofol was the most commonly used general anesthetic induction agent (78%). Anesthetic induction agent usage was not different across the groups.
| AAB (N=343) | Non‐AAB (N=579) | P Value* | |
|---|---|---|---|
| |||
| Patient demographics | |||
| Age (y), meanSD | 63.010.8 | 57.313.9 | <0.001 |
| BMI (kg/m2), meanSD | 34.67.3 | 31.87.7 | <0.001 |
| Baseline systolic BP (mm Hg), meanSD | 135.016.8 | 130.819.8 | 0.339 |
| Baseline diastolic BP (mm Hg), meanSD | 74.514.5 | 75.311.8 | 0.798 |
| Medications | |||
| Diuretic, % | 53.6 | 18.5 | <0.001 |
| ‐Blocker, % | 39.4 | 22.4 | <0.001 |
| Calcium channel blocker, % | 23.3 | 9.9 | <0.001 |
| Nonsteroidal anti‐inflammatory drug, % | 36.1 | 35.7 | 0.901 |
| Comorbidities | |||
| Diabetes mellitus, % | 32.9 | 9.5 | <0.001 |
| Congestive heart failure, % | 2.9 | 0.4 | 0.001 |
| Coronary artery disease, % | 20.1 | 9.5 | <0.001 |
| Hypertension, % | 95.3 | 36.8 | <0.001 |
| Total comorbidities, meanSD | 1.50.7 | 0.50.7 | <0.001 |
| Procedure type | |||
| Spinal fusions, % | 16.6 | 24.4 | 0.001 |
| Total knee arthroplasty, % | 56.0 | 44.2 | 0.001 |
| Total hip arthroplasty, % | 27.4 | 31.4 | 0.001 |
| Induction agents | |||
| Etomidate, % | 14.9 | 11.9 | 0.199 |
| Propofol, % | 77.6 | 78.3 | 0.801 |
| Methohexital, % | 7.3 | 9.2 | 0.329 |
| Other (gas, ketamine), % | 0.3 | 1.2 | 0.270 |
| Hematocrit | |||
| Preoperative (%), meanSD | 40.53.7 | 40.23.8 | 0.150 |
| Postoperative (%), meanSD | 34.04.6 | 33.74.3 | 0.511 |
| % Change, meanSD | 15.38.5 | 16.88.9 | 0.036 |
| Creatinine | |||
| Preoperative (mg/dL), meanSD | 0.960.41 | 0.850.23 | <0.001 |
| Postoperative (mg/dL), meanSD | 0.960.42 | 0.810.23 | <0.001 |
| % change, meanSD | 1.4829.22 | 4.1414.18 | 0.235 |
| Fluids | |||
| Estimated blood loss (mL), meanSD | 301.2340.0 | 356.9482.7 | 0.125 |
| Crystalloid (mL), meanSD | 2584.41401.6 | 2765.21487.2 | 0.036 |
| Colloid (mL), meanSD | 124.3322.4 | 151.0553.5 | 0.810 |
| Packed red blood cells (mL), meanSD | 78.5323.1 | 99.5452.0 | 0.613 |
| Vasopressors | |||
| Ephedrine (mg), meanSD | 11.715.0 | 8.013.0 | <0.001 |
| Phenylephrine (g), meanSD | 615.72210.9 | 687.13905.3 | 0.002 |
| Vasopressin (U), meanSD | 0.351.90 | 0.080.90 | <0.001 |
| Outcomes | |||
| Induction hypotension, % | 12.2 | 1.93 | 0.005 |
| Intraoperative hypotension, % | 26.0 | 20.9 | 0.078 |
| Acute kidney injury, % | 8.3 | 1.7 | <0.001 |
Estimated blood loss for the procedures was similar between the 2 groups (301.2340 vs 356.9482.7 mL) and similar colloid and packed red cell administration occurred. However, patients receiving AAB were administered less crystalloid infusion (2584.41401.6 vs 2765.21487.2 mL, P=0.036) and received less phenylephrine but higher ephedrine and vasopressin dosages as a group. Patients in both groups had similar preoperative and postoperative hematocrit concentrations. Average preoperative serum creatinine was higher in the AAB group than in the non‐AAB group (0.960.41 vs 0.850.23, P<0.001) and remained so postoperatively (0.960.42 vs 0.810.23, P<0.001).
Primary and Secondary Outcome Measures
Postinduction Hypotension
Therapy with AAB was associated with a greater incidence of postinduction hypotension (12.2% vs 6.7%, P=0.005). Using a multivariate logistic regression model adjusting for the effects of age, BMI, antihypertensive medications, comorbidities, and anesthetic induction agents, the use of AAB had a greater odds ratio (OR) of 1.93 (95% confidence interval [CI]: 1.10‐3.41, P=0.023) for developing postinduction hypotension (Table 2). A higher BMI had a lower OR for postinduction hypotension.
| Comparison | Hypotension at Induction, OR (95% CI), P Value | Intraoperative Hypotension, OR (95% CI), P Value | Acute Kidney Injury, OR (95% CI), P Value |
|---|---|---|---|
| |||
| AAB vs none, unadjusted | 1.93 (1.223.06), 0.005 | 1.33 (0.971.82), 0.078 | 5.40 (2.4112.06), <0.001 |
| AAB vs none, adjusted for covariates | 1.93 (1.103.41), 0.023 | 1.30 (0.851.97), 0.226 | 2.68 (1.086.69), 0.034 |
| AAB vs none, adjusted for covariates+hypotension at induction | N/A | N/A | 2.51 (1.06.32), 0.051 |
| AAB vs none, adjusted for covariates+intraoperative hypotension | N/A | N/A | 2.66 (1.066.64), 0.037 |
| AAB vs none, adjusted for covariates+any hypotension | N/A | N/A | 2.60 (1.046.51), 0.042 |
Postincision (Intraoperative) Hypotension
The incidence of postincision, intraoperative hypotension in patients receiving AAB (26.0%) was not statistically different (P=0.078) from those not receiving these agents (20.9%). Multivariate logistic regression demonstrated that preoperative hypertension (OR: 1.73, 95% CI: 1.05‐2.85, P=0.031) and THA were each independent risk factors for intraoperative hypotension. The other comorbidities of DM, CHF, CAD, and the individual antihypertensive agents were not found to have a strong influence on the outcome of intraoperative hypotension. The odds ratio of developing intraoperative hypotension during the procedure in patients receiving AAB was not statistically significant (OR: 1.30, 95% CI: 0.85‐1.97, P=0.226) from those not receiving this therapy preoperatively (Table 2).
AKI
There was a significantly higher incidence of AKI (26/313 [8.3%] vs 8/485 [1.7%], P<0.001) in patients receiving preoperative AAB. No patients required renal replacement therapy. Of those patients who developed postoperative AKI, 73% of the AAB group and 75% of the non‐AAB group had a normal glomerular filtration rate (GFR) (mL/min/1.73 m2, GFR >90 prior to surgery. Of both the AAB and non‐AAB groups, 20% to 25% were in stage 2 (GFR 6089) chronic kidney disease (CKD)[18] preoperatively. Only 2 patients in the AAB group began in stage 3 (GFR 3059) CKD. Fifty percent of both groups went from stage 1 kidney function to stage 3. For all others who developed AKI, the GFR rose by a single stage.
Multivariate logistic regression, controlling for statistically significant and clinically significant variables, demonstrated that AAB administered preoperatively was independently associated with a greater OR of 2.68 (95% CI: 1.08‐6.69, P=0.034) for developing AKI postoperatively than if AAB was not taken (Table 2). Higher BMI was a further independent risk factor for postoperative AKI; a 5‐unit increase in BMI revealed an OR of 1.58 (95% CI: 1.25‐1.99, P<0.001) for experiencing postoperative AKI. Although the AAB group had statistically significantly more comorbidities, in the final analysis only the presence of CAD trended to an association with the development of AKI (OR: 2.37, 95% CI: 1.005.60, P=0.050).
We wished to determine whether the increased risk of AKI associated with AAB therapy was explained by the associated postinduction or postincision, intraoperative hypotension experienced by the patients or independent of these effects. To do so we accounted for the development of either postinduction or intraoperative hypotension as a possible confounder in the multivariate analysis for the development of AKI (Table 2). Postinduction hypotension alone was not statistically associated with AKI (OR 2.04, 95% CI: 0.70‐6.0, P=0.193). However, intraoperative hypotension was found to be an independent risk factor for the development of AKI (OR: 2.62, 95% CI: 1.17‐5.84, P=0.019). When eliminating the effect of this intraoperative hypotension as a confounder, patients on AAB therapy continued to have a 2.66 OR for the development of AKI postoperatively (95% CI: 1.06‐6.64, P=0.037), independent of the development of intraoperative hypotension. When eliminating the effect of both postinduction and intraoperative hypotension (all hypotension Table 2), AAB therapy continued to have a statistically significant independent effect (OR: 2.60, 95% CI: 1.046.51, P=0.042) on developing postoperative AKI.
As secondary outcome measures, we looked at the development of AKI and its relationship to hospital LOS and mortality. The development of AKI was associated with a significantly greater mean length of hospital stay (5.76 days vs 3.28 days, P<0.001). Although 2‐year mortality was higher, 5.9% in the AKI group compared to 2.4% in the non‐AAB group, it was not statistically significant (P=0.211).
DISCUSSION
In this retrospective review of 922 patients presenting for major orthopedic surgery, we found that 343(37%) were receiving therapy with either ACEIs or ARBs. In such patients, we demonstrated a higher incidence of postinduction hypotension and an increased incidence of AKI. We further demonstrated that the development of AKI associated with AAB therapy was independent of hypotension occurring either postinduction or intraoperatively after incision.
Postinduction hypotension in patients receiving AAB was demonstrated to be 12.2% compared to 7.7% in patients not receiving this therapy. Hypotension after general anesthesia induction in patients receiving AAB is widely reported,[1, 14, 15] and ranges from 22% to 100%[19, 20] based on varying definitions of what constitutes hypotension. We chose an absolute value of a systolic blood pressure of 80 mm Hg occurring for 5 minutes as constituting significant hypotension.[16] Monk et al. reported an increased one year postnon‐cardiac surgery mortality risk of 1.036 times per minute of intraoperative hypotension, defining hypotension as a systolic blood pressure of <80 mm Hg.[21]
We further demonstrated that AAB therapy resulted in an 8.3% incidence of AKI versus 1.7% in non‐AAB patients (P<0.001). AKI was defined as an increase in serum creatinine of 0.3 mg/dL or a 50% increase in creatinine when pre‐ and postoperative values were compared.[17] A number of other investigators have identified AKI associated with AAB use in patients undergoing cardiac,[6, 11] vascular,[7, 10] and lung[13] surgery. Similarly, in the present study, in orthopedic patients, AAB remained a significant risk factor for developing AKI (OR: 2.68, P=0.034) independent of patient comorbidities and adjunct therapy (Table 2).
ACEIs and ARBs are prescribed to treat HTN, CHF, and improve renal function in diabetic and proteinuric nephropathy.[22] AAB therapy is prescribed for nephropathy because these medications decrease glomerular pressure by selective inhibition of angiotensin II mediated vasoconstriction of the efferent glomerular arteriole.[23] Normally, this is beneficial to patients and is associated with a decrease in serum creatinine concentration. However, during hypotension, when there is decreased renal perfusion, further decreases in intraglomerular pressure may occur, precipitating renal failure.[23] In addition, other factors may contribute to the development of AKI, as AAB has both tissue and systemic effects that extend beyond simply dilating the efferent glomerular arteriole. These include effects on the sympathetic nervous system, oxidative stress, and altering the release and synthesis of vasodilators such as bradykinin, nitric oxide, and prostacyclins[24] as well as effects through the release of aldosterone and arginine‐vasopressin.[25] These other factors might help explain the present study's findings that, when eliminating the effect of both postinduction and intraoperative hypotension, AAB therapy continued to have a statistically significant independent effect (OR: 2.60, 95% CI: 1.046.51, P=0.042) on developing postoperative AKI.
Although we demonstrated an association of AAB therapy with the development of hypotension after induction, we demonstrated only a trend in the development of postincisional, intraoperative hypotension (P=0.078). We defined intraoperative hypotension as a systolic BP <80 mm Hg for 10 minutes occurring after skin incision.[16] One must take into consideration, however, that a significant number of AAB patients were hypotensive during induction and received higher doses of ephedrine and vasopressin during the operative period. These patients may have been rescued from intraoperative hypotension by receiving vasopressor treatment at the outset. We did find that intraoperative hypotension was a significant, independent risk factor for AKI (OR: 2.62, P=0.019).
We looked further at the consequences of developing AKI. Patients who developed AKI had a significant greater mean length of hospital stay (5.76 days vs 3.28 days, P<0.001), which is consistent with other investigators' findings.[25, 26, 27] Although 2‐year mortality was higher at 5.88% in the AKI group compared to 2.38% in the non‐AAB group, this was not statistically significant (P=0.211). Other studies have shown that the development of AKI results in greater mortality.[26, 28]
The American College of Physicians (ACP) recommendations as of 2013 regarding the use of ACEIs and ARBs preoperatively is: uncertain, continue with caution, avoid hypovolemia. Potential for hypotension with induction of anesthesia and increased vasoconstrictor requirements and decreased responsiveness to pressors.[29] The ACP acknowledges that preoperative ACEIs and ARBs have the potential for postinduction hypotension and increased requirements for vasopressors. We have implemented recommendations at our preoperative anesthesia clinic to hold ACEIs and ARBs on the morning of surgery in patients with controlled blood pressure scheduled for spine fusion, and hip and knee arthroplasties. In accordance with ACP guidelines, other antihypertensives such as ‐blockers, calcium channel blockers, nitrates, and sympatholytics should be continued preoperatively and can be used perioperatively.
Limitations of the Study
There are several limitations to our study. This was a retrospective analysis over a fixed time period in one academic institution. Further, because of the retrospective nature, anesthesia and intraoperative (fluid and vasoconstrictor) management was not standardized. The definition of hypotension (SBP 80 mm Hg for 5 minutes after induction and 10 minutes after incision) may have been too stringent, so that more subtle decreases in blood pressure that could have impacted AKI might not have been captured to show statistical significance. Thus, our finding, that the development of AKI associated with preoperative AAB therapy may be independent of the occurrence of hypotension, must be interpreted with this in mind.
CONCLUSIONS
Patients who receive preoperative ACEI or ARB therapy and undergo major orthopedic surgery such as spinal fusion, and hip or knee arthroplasties experience a higher incidence of postinduction hypotension and AKI than those not receiving such therapy. The development of AKI in such patients is associated with a significantly prolonged length of hospital stay. Our findings suggest an association between preoperative ACEI/ARB use and moderate kidney injury following major orthopedic surgeries. However, a prospective, multicentered, randomized trial needs to be performed to confirm that withdrawal of AAB therapy preoperatively will decrease the incidence of AKI in patients undergoing major orthopedic procedures under general anesthesia. Future studies also need to determine the optimal time duration of withholding AAB therapy and the consequences on cardiac outcomes.
ACKNOWLEDGMENTS
Disclosures: Presented at the Society of Hospital Medicine National Meeting, May 18, 2013, National Harbor, Maryland; and the Society of General Internal Medicine Mid‐Atlantic Regional Meeting, March 1, 2013, Philadelphia, Pennsylvania. The authors report no conflicts of interest.
Patients presenting for surgery with angiotensin axis blockade (AAB) from therapy with either angiotensin‐converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) experience an increased incidence of perioperative hypotension.[1, 2, 3, 4] Debate continues as to whether this hypotension results in any significant clinical sequelae. Some authors found that the use of an ACEI decreased the incidence of acute kidney injury (AKI),[5] mortality, and septicemia in cardiac and vascular surgical patients.[6] However, others found that in vascular and cardiac surgery there is increased mortality[7] as well as increased incidence of postoperative AKI.[8, 9, 10] A retrospective study of 10,000 coronary artery bypass graft patients found that ACEI was associated with increased inotropic support, AKI, mortality, and new onset atrial fibrillation.[11] In a meta‐analysis of 69,000 cardiothoracic surgery patients, the use of ACEIs/ARBs was associated with an increase in AKI and mortality.[12] AKI has also been demonstrated after lung resection surgery in patients receiving preoperative therapy with an ARB.[13]
Studies on noncardiac general surgery patients demonstrate that the use of AAB results in postinduction hypotension, but they fail to show an increased incidence in postoperative AKI.[14, 15] We propose, however, that major orthopedic surgery patients are a specific surgical cohort, like cardiac, vascular, and lung, who can develop operative hypotension and postoperative AKI when AAB is taken on the morning of surgery. To address this question we performed a retrospective study of 1154 patients undergoing either spinal fusion, total knee arthroplasty (TKA), or total hip arthroplasty (THA) during the 2010 calendar year in our academic medical center. We measured the incidence of postanesthesia induction hypotension, intraoperative hypotension, and postoperative AKI as it relates to the administration of AAB preoperatively.
MATERIALS AND METHODS
This study was a retrospective, observational investigation at a single, large academic hospital. The study design for chart review was approved by the institutional review board prior to data collection. Informed patient consent was not required for this retrospective study.
Patient Selection
We retrospectively reviewed the computerized chart and operating room electronic medical records of all patients who underwent elective major orthopedic surgery in the 2010 calendar year. We chose vertebral spine fusion, TKA, and THA as the 3 surgeries to represent major elective orthopedic surgery. Electronic query of the hospital database identified 1154 patients having undergone these surgeries in the year 2010. Nine hundred twenty‐two patients met inclusion criteria: 21 years old and evaluated in the preanesthesia clinic with documented vital signs and clearly defined preoperative medication recommendations. The policy in the preanesthesia clinic was to recommend taking the ACEI and ARB on the morning of surgery. All 922 patients were included in the analysis of the outcomes for induction hypotension and intraoperative hypotension. Of the 922 patients, 798 had the documented preoperative and postoperative creatinine values needed to define AKI. Therefore, only these 798 patients were included in the AKI outcome analysis. During the time of the study it was the practice at our medical center that all such surgeries were performed under general anesthesia.
Data Collection
Preanesthesia records were reviewed for patient demographics including age, body mass index (BMI), baseline blood pressure, diabetes mellitus (DM), coronary artery disease (CAD), hypertension (HTN), and congestive heart failure (CHF), as well as for therapy with ACEI or ARB, diuretics, ‐blockers, nonsteroidal anti‐inflammatory drugs (NSAIDs), and calcium channel blockers (CCB). The 4 statistically and clinically significant comorbidities were looked at individually as well as added together for a total sum of weighted comorbidity risk factors. The Anesthesia Electronic Record (Surginet Anesthesia, Kansas City, MO) was reviewed for each corresponding patient to determine the general anesthesia induction agent used and to assess the postinduction and intraoperative systolic blood pressures. Blood pressure was determined using an automated blood pressure cuff and automatically recorded at intervals of 5 minutes or less. Further, ephedrine, phenylephrine and vasopressin doses, estimated blood loss, blood transfusion requirements, and intravenous fluid administration (colloid and crystalloid) were noted. Preoperative (<30 days) and postoperative (within 24 hours after surgery) serum creatinine and hematocrit values were also recorded.
Outcome Measures
The primary outcome measures studied were:
- Postinduction hypotension (systolic blood pressure [SBP] 80 mm Hg for5 minutes) occurring within 30 minutes after anesthesia induction but before surgical incision.[16]
- Intraoperative hypotension (SBP 80 mm Hg for 10 minutes) occurring after surgical incision.[16]
- Postoperative AKI defined as an increase in serum creatinine 0.3 mg/dL or an increase of 50% from preoperative creatinine (Kidney Disease: Improving Global Outcomes Clinical Practice Guideline for Acute Kidney Injury)[17] within 24 hours postoperatively.
The secondary outcome measures were:
- Hospital length of stay (LOS).
- Two‐year mortality associated with the development of AKI.
Statistical Analysis
Categorical variables were summarized with frequencies and percentages, whereas continuous variables were summarized with means, standard deviations, medians, and quartiles. A [2] test or a Wilcoxon rank sum test was used to determine differences in preoperative and intraoperative characteristics between those patients with AAB and those patients without AAB. Logistic regression was used to determine the association between the main outcome variables (hypotension at anesthetic induction, hypotension during the operative procedure, and postoperative AKI) and the primary independent variable, AAB, as well as other preoperative and intraoperative characteristics. The significance and magnitude of the associations were quantified with percentages and odds ratios. Exact logistic regression was used as necessary when expected cell counts were too small for the usual asymptotic logistic regression to be valid. The statistically significant (P<0.05) variables resulting from this bivariate analysis as well as important clinically significant variables with known associations with the outcome variables were included as covariates in a multivariable logistic regression model for each outcome variable with AAB. By adjusting for these covariates, any potential and unwanted variation resulting from differences between the AAB groups in other preoperative or postoperative characteristics is removed from the association between each outcome variable and AAB. Variance inflation factor and tolerance statistics were used to test for multicollinearity between all independent variables before including them in the final models. The Hosmer and Lemeshow goodness‐of‐fit test was used to assess the fit of the final models. Logistic regression was used to test the association of AKI with mortality, whereas a Wilcoxon rank sum test was used to test the difference in mean/median LOS between AKI and non‐AKI groups.
RESULTS
Preoperative, Surgical, and Anesthesia Data
A total of 922 patients met inclusion criteria, of which 343 (37%) were receiving AAB with either an ACEI or ARB preoperatively. Preoperative characteristics are documented in Table 1. Patients receiving AAB were older (63.010.8 vs 57.313.9 years) and had a higher BMI (34.67.3 vs 31.97.7) than patients not receiving this therapy. They were also more likely to be receiving diuretics, ‐blockers, and CCBs as well as have DM, CHF, CAD, and HTN. These characteristics were included as covariates in a multivariable logistic regression model so that any confounding resulting differences caused by these variables were removed from the association between each outcome variable and AAB use. There was no difference in baseline SBP or diastolic blood pressures. There was no difference in the use of NSAIDs. Patients receiving AAB underwent a higher percentage of TKAs (56.0% vs 44.2%) and lower percentage of spine fusions (16.6% vs 24.4%) and THAs (27.4% vs 31.4%). Propofol was the most commonly used general anesthetic induction agent (78%). Anesthetic induction agent usage was not different across the groups.
| AAB (N=343) | Non‐AAB (N=579) | P Value* | |
|---|---|---|---|
| |||
| Patient demographics | |||
| Age (y), meanSD | 63.010.8 | 57.313.9 | <0.001 |
| BMI (kg/m2), meanSD | 34.67.3 | 31.87.7 | <0.001 |
| Baseline systolic BP (mm Hg), meanSD | 135.016.8 | 130.819.8 | 0.339 |
| Baseline diastolic BP (mm Hg), meanSD | 74.514.5 | 75.311.8 | 0.798 |
| Medications | |||
| Diuretic, % | 53.6 | 18.5 | <0.001 |
| ‐Blocker, % | 39.4 | 22.4 | <0.001 |
| Calcium channel blocker, % | 23.3 | 9.9 | <0.001 |
| Nonsteroidal anti‐inflammatory drug, % | 36.1 | 35.7 | 0.901 |
| Comorbidities | |||
| Diabetes mellitus, % | 32.9 | 9.5 | <0.001 |
| Congestive heart failure, % | 2.9 | 0.4 | 0.001 |
| Coronary artery disease, % | 20.1 | 9.5 | <0.001 |
| Hypertension, % | 95.3 | 36.8 | <0.001 |
| Total comorbidities, meanSD | 1.50.7 | 0.50.7 | <0.001 |
| Procedure type | |||
| Spinal fusions, % | 16.6 | 24.4 | 0.001 |
| Total knee arthroplasty, % | 56.0 | 44.2 | 0.001 |
| Total hip arthroplasty, % | 27.4 | 31.4 | 0.001 |
| Induction agents | |||
| Etomidate, % | 14.9 | 11.9 | 0.199 |
| Propofol, % | 77.6 | 78.3 | 0.801 |
| Methohexital, % | 7.3 | 9.2 | 0.329 |
| Other (gas, ketamine), % | 0.3 | 1.2 | 0.270 |
| Hematocrit | |||
| Preoperative (%), meanSD | 40.53.7 | 40.23.8 | 0.150 |
| Postoperative (%), meanSD | 34.04.6 | 33.74.3 | 0.511 |
| % Change, meanSD | 15.38.5 | 16.88.9 | 0.036 |
| Creatinine | |||
| Preoperative (mg/dL), meanSD | 0.960.41 | 0.850.23 | <0.001 |
| Postoperative (mg/dL), meanSD | 0.960.42 | 0.810.23 | <0.001 |
| % change, meanSD | 1.4829.22 | 4.1414.18 | 0.235 |
| Fluids | |||
| Estimated blood loss (mL), meanSD | 301.2340.0 | 356.9482.7 | 0.125 |
| Crystalloid (mL), meanSD | 2584.41401.6 | 2765.21487.2 | 0.036 |
| Colloid (mL), meanSD | 124.3322.4 | 151.0553.5 | 0.810 |
| Packed red blood cells (mL), meanSD | 78.5323.1 | 99.5452.0 | 0.613 |
| Vasopressors | |||
| Ephedrine (mg), meanSD | 11.715.0 | 8.013.0 | <0.001 |
| Phenylephrine (g), meanSD | 615.72210.9 | 687.13905.3 | 0.002 |
| Vasopressin (U), meanSD | 0.351.90 | 0.080.90 | <0.001 |
| Outcomes | |||
| Induction hypotension, % | 12.2 | 1.93 | 0.005 |
| Intraoperative hypotension, % | 26.0 | 20.9 | 0.078 |
| Acute kidney injury, % | 8.3 | 1.7 | <0.001 |
Estimated blood loss for the procedures was similar between the 2 groups (301.2340 vs 356.9482.7 mL) and similar colloid and packed red cell administration occurred. However, patients receiving AAB were administered less crystalloid infusion (2584.41401.6 vs 2765.21487.2 mL, P=0.036) and received less phenylephrine but higher ephedrine and vasopressin dosages as a group. Patients in both groups had similar preoperative and postoperative hematocrit concentrations. Average preoperative serum creatinine was higher in the AAB group than in the non‐AAB group (0.960.41 vs 0.850.23, P<0.001) and remained so postoperatively (0.960.42 vs 0.810.23, P<0.001).
Primary and Secondary Outcome Measures
Postinduction Hypotension
Therapy with AAB was associated with a greater incidence of postinduction hypotension (12.2% vs 6.7%, P=0.005). Using a multivariate logistic regression model adjusting for the effects of age, BMI, antihypertensive medications, comorbidities, and anesthetic induction agents, the use of AAB had a greater odds ratio (OR) of 1.93 (95% confidence interval [CI]: 1.10‐3.41, P=0.023) for developing postinduction hypotension (Table 2). A higher BMI had a lower OR for postinduction hypotension.
| Comparison | Hypotension at Induction, OR (95% CI), P Value | Intraoperative Hypotension, OR (95% CI), P Value | Acute Kidney Injury, OR (95% CI), P Value |
|---|---|---|---|
| |||
| AAB vs none, unadjusted | 1.93 (1.223.06), 0.005 | 1.33 (0.971.82), 0.078 | 5.40 (2.4112.06), <0.001 |
| AAB vs none, adjusted for covariates | 1.93 (1.103.41), 0.023 | 1.30 (0.851.97), 0.226 | 2.68 (1.086.69), 0.034 |
| AAB vs none, adjusted for covariates+hypotension at induction | N/A | N/A | 2.51 (1.06.32), 0.051 |
| AAB vs none, adjusted for covariates+intraoperative hypotension | N/A | N/A | 2.66 (1.066.64), 0.037 |
| AAB vs none, adjusted for covariates+any hypotension | N/A | N/A | 2.60 (1.046.51), 0.042 |
Postincision (Intraoperative) Hypotension
The incidence of postincision, intraoperative hypotension in patients receiving AAB (26.0%) was not statistically different (P=0.078) from those not receiving these agents (20.9%). Multivariate logistic regression demonstrated that preoperative hypertension (OR: 1.73, 95% CI: 1.05‐2.85, P=0.031) and THA were each independent risk factors for intraoperative hypotension. The other comorbidities of DM, CHF, CAD, and the individual antihypertensive agents were not found to have a strong influence on the outcome of intraoperative hypotension. The odds ratio of developing intraoperative hypotension during the procedure in patients receiving AAB was not statistically significant (OR: 1.30, 95% CI: 0.85‐1.97, P=0.226) from those not receiving this therapy preoperatively (Table 2).
AKI
There was a significantly higher incidence of AKI (26/313 [8.3%] vs 8/485 [1.7%], P<0.001) in patients receiving preoperative AAB. No patients required renal replacement therapy. Of those patients who developed postoperative AKI, 73% of the AAB group and 75% of the non‐AAB group had a normal glomerular filtration rate (GFR) (mL/min/1.73 m2, GFR >90 prior to surgery. Of both the AAB and non‐AAB groups, 20% to 25% were in stage 2 (GFR 6089) chronic kidney disease (CKD)[18] preoperatively. Only 2 patients in the AAB group began in stage 3 (GFR 3059) CKD. Fifty percent of both groups went from stage 1 kidney function to stage 3. For all others who developed AKI, the GFR rose by a single stage.
Multivariate logistic regression, controlling for statistically significant and clinically significant variables, demonstrated that AAB administered preoperatively was independently associated with a greater OR of 2.68 (95% CI: 1.08‐6.69, P=0.034) for developing AKI postoperatively than if AAB was not taken (Table 2). Higher BMI was a further independent risk factor for postoperative AKI; a 5‐unit increase in BMI revealed an OR of 1.58 (95% CI: 1.25‐1.99, P<0.001) for experiencing postoperative AKI. Although the AAB group had statistically significantly more comorbidities, in the final analysis only the presence of CAD trended to an association with the development of AKI (OR: 2.37, 95% CI: 1.005.60, P=0.050).
We wished to determine whether the increased risk of AKI associated with AAB therapy was explained by the associated postinduction or postincision, intraoperative hypotension experienced by the patients or independent of these effects. To do so we accounted for the development of either postinduction or intraoperative hypotension as a possible confounder in the multivariate analysis for the development of AKI (Table 2). Postinduction hypotension alone was not statistically associated with AKI (OR 2.04, 95% CI: 0.70‐6.0, P=0.193). However, intraoperative hypotension was found to be an independent risk factor for the development of AKI (OR: 2.62, 95% CI: 1.17‐5.84, P=0.019). When eliminating the effect of this intraoperative hypotension as a confounder, patients on AAB therapy continued to have a 2.66 OR for the development of AKI postoperatively (95% CI: 1.06‐6.64, P=0.037), independent of the development of intraoperative hypotension. When eliminating the effect of both postinduction and intraoperative hypotension (all hypotension Table 2), AAB therapy continued to have a statistically significant independent effect (OR: 2.60, 95% CI: 1.046.51, P=0.042) on developing postoperative AKI.
As secondary outcome measures, we looked at the development of AKI and its relationship to hospital LOS and mortality. The development of AKI was associated with a significantly greater mean length of hospital stay (5.76 days vs 3.28 days, P<0.001). Although 2‐year mortality was higher, 5.9% in the AKI group compared to 2.4% in the non‐AAB group, it was not statistically significant (P=0.211).
DISCUSSION
In this retrospective review of 922 patients presenting for major orthopedic surgery, we found that 343(37%) were receiving therapy with either ACEIs or ARBs. In such patients, we demonstrated a higher incidence of postinduction hypotension and an increased incidence of AKI. We further demonstrated that the development of AKI associated with AAB therapy was independent of hypotension occurring either postinduction or intraoperatively after incision.
Postinduction hypotension in patients receiving AAB was demonstrated to be 12.2% compared to 7.7% in patients not receiving this therapy. Hypotension after general anesthesia induction in patients receiving AAB is widely reported,[1, 14, 15] and ranges from 22% to 100%[19, 20] based on varying definitions of what constitutes hypotension. We chose an absolute value of a systolic blood pressure of 80 mm Hg occurring for 5 minutes as constituting significant hypotension.[16] Monk et al. reported an increased one year postnon‐cardiac surgery mortality risk of 1.036 times per minute of intraoperative hypotension, defining hypotension as a systolic blood pressure of <80 mm Hg.[21]
We further demonstrated that AAB therapy resulted in an 8.3% incidence of AKI versus 1.7% in non‐AAB patients (P<0.001). AKI was defined as an increase in serum creatinine of 0.3 mg/dL or a 50% increase in creatinine when pre‐ and postoperative values were compared.[17] A number of other investigators have identified AKI associated with AAB use in patients undergoing cardiac,[6, 11] vascular,[7, 10] and lung[13] surgery. Similarly, in the present study, in orthopedic patients, AAB remained a significant risk factor for developing AKI (OR: 2.68, P=0.034) independent of patient comorbidities and adjunct therapy (Table 2).
ACEIs and ARBs are prescribed to treat HTN, CHF, and improve renal function in diabetic and proteinuric nephropathy.[22] AAB therapy is prescribed for nephropathy because these medications decrease glomerular pressure by selective inhibition of angiotensin II mediated vasoconstriction of the efferent glomerular arteriole.[23] Normally, this is beneficial to patients and is associated with a decrease in serum creatinine concentration. However, during hypotension, when there is decreased renal perfusion, further decreases in intraglomerular pressure may occur, precipitating renal failure.[23] In addition, other factors may contribute to the development of AKI, as AAB has both tissue and systemic effects that extend beyond simply dilating the efferent glomerular arteriole. These include effects on the sympathetic nervous system, oxidative stress, and altering the release and synthesis of vasodilators such as bradykinin, nitric oxide, and prostacyclins[24] as well as effects through the release of aldosterone and arginine‐vasopressin.[25] These other factors might help explain the present study's findings that, when eliminating the effect of both postinduction and intraoperative hypotension, AAB therapy continued to have a statistically significant independent effect (OR: 2.60, 95% CI: 1.046.51, P=0.042) on developing postoperative AKI.
Although we demonstrated an association of AAB therapy with the development of hypotension after induction, we demonstrated only a trend in the development of postincisional, intraoperative hypotension (P=0.078). We defined intraoperative hypotension as a systolic BP <80 mm Hg for 10 minutes occurring after skin incision.[16] One must take into consideration, however, that a significant number of AAB patients were hypotensive during induction and received higher doses of ephedrine and vasopressin during the operative period. These patients may have been rescued from intraoperative hypotension by receiving vasopressor treatment at the outset. We did find that intraoperative hypotension was a significant, independent risk factor for AKI (OR: 2.62, P=0.019).
We looked further at the consequences of developing AKI. Patients who developed AKI had a significant greater mean length of hospital stay (5.76 days vs 3.28 days, P<0.001), which is consistent with other investigators' findings.[25, 26, 27] Although 2‐year mortality was higher at 5.88% in the AKI group compared to 2.38% in the non‐AAB group, this was not statistically significant (P=0.211). Other studies have shown that the development of AKI results in greater mortality.[26, 28]
The American College of Physicians (ACP) recommendations as of 2013 regarding the use of ACEIs and ARBs preoperatively is: uncertain, continue with caution, avoid hypovolemia. Potential for hypotension with induction of anesthesia and increased vasoconstrictor requirements and decreased responsiveness to pressors.[29] The ACP acknowledges that preoperative ACEIs and ARBs have the potential for postinduction hypotension and increased requirements for vasopressors. We have implemented recommendations at our preoperative anesthesia clinic to hold ACEIs and ARBs on the morning of surgery in patients with controlled blood pressure scheduled for spine fusion, and hip and knee arthroplasties. In accordance with ACP guidelines, other antihypertensives such as ‐blockers, calcium channel blockers, nitrates, and sympatholytics should be continued preoperatively and can be used perioperatively.
Limitations of the Study
There are several limitations to our study. This was a retrospective analysis over a fixed time period in one academic institution. Further, because of the retrospective nature, anesthesia and intraoperative (fluid and vasoconstrictor) management was not standardized. The definition of hypotension (SBP 80 mm Hg for 5 minutes after induction and 10 minutes after incision) may have been too stringent, so that more subtle decreases in blood pressure that could have impacted AKI might not have been captured to show statistical significance. Thus, our finding, that the development of AKI associated with preoperative AAB therapy may be independent of the occurrence of hypotension, must be interpreted with this in mind.
CONCLUSIONS
Patients who receive preoperative ACEI or ARB therapy and undergo major orthopedic surgery such as spinal fusion, and hip or knee arthroplasties experience a higher incidence of postinduction hypotension and AKI than those not receiving such therapy. The development of AKI in such patients is associated with a significantly prolonged length of hospital stay. Our findings suggest an association between preoperative ACEI/ARB use and moderate kidney injury following major orthopedic surgeries. However, a prospective, multicentered, randomized trial needs to be performed to confirm that withdrawal of AAB therapy preoperatively will decrease the incidence of AKI in patients undergoing major orthopedic procedures under general anesthesia. Future studies also need to determine the optimal time duration of withholding AAB therapy and the consequences on cardiac outcomes.
ACKNOWLEDGMENTS
Disclosures: Presented at the Society of Hospital Medicine National Meeting, May 18, 2013, National Harbor, Maryland; and the Society of General Internal Medicine Mid‐Atlantic Regional Meeting, March 1, 2013, Philadelphia, Pennsylvania. The authors report no conflicts of interest.
- . Management of hypotension associated with angiotensin‐axis blockade and general anesthesia administration. J Cardiothorac Vasc Anesth. 2013;27:156–167.
- , , , , , . Clinical consequences of withholding versus administering renin‐angiotensin‐aldosterone system antagonists in the preoperative period. J Hosp Med. 2008;3:319–325.
- , , , et al. Influence of chronic angiotensin‐converting enzyme inhibition on anesthetic induction. Anesthesiology. 1994;81(2):299–307.
- , , , , . Pressor responses to tracheal intubation after sublingual captopril. A pilot study. Anaesthesia. 1990;45(3):243–245.
- , , , , , , . Preoperative angiotensin‐converting enzyme inhibitors and acute kidney injury after coronary artery bypass grafting. Ann Thorac Surg. 2008;86(4):1160–1165.
- , , , et al. The effects of preoperative renin‐angiotensin system inhibitors on outcomes in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27(4):703–709.
- , , , . Renin‐angiotensin blockade is associated with increased mortality after vascular surgery. Can J Anaesth. 2010;57:736–744.
- , . , et al. Preoperative use of angiotensin‐converting enzyme inhibitors/angiotensin receptor blockers is associated with increased risk for acute kidney injury after cardiovascular surgery. Clin J Am Soc Nephrol. 2008;3(5):1266–1273.
- , , , et al.; TRIBE‐AKI Consortium. Preoperative angiotensin‐converting enzyme inhibitors and angiotensin receptor blocker use and acute kidney injury in patients undergoing cardiac surgery. Nephrol Dial Transplant. 2013;28(11):2787–2799.
- , , , et al. The chronic inhibition of angiotensin‐converting enzyme impairs postoperative renal function. Anesth Analg. 2001;93(5):1111–1115.
- , , , et al. Effects of angiotensin‐converting enzyme inhibitor therapy on clinical outcome in patients undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2009;54:1778–1784.
- , , , , , . Acute kidney injury and death associated with renin angiotensin system blockade in cardiothoracic surgery: a meta‐analysis of observational studies. Am J Kidney Dis. 2013;63(6):1077–1086.
- , , . Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg. 2012;114:1256–1262.
- , , , et al. Angiotensin system inhibitors in a general surgical population. Anesth Analg. 2005;100:636–644, table of contents.
- , , , , . Chronic angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker therapy combined with diuretic therapy is associated with increased episodes of hypotension in noncardiac surgery. J Cardiothorac Vasc Anesth. 2008;22:180–186.
- , , , , . Hemodynamic impact of dexmedetomidine administration in 15,656 noncardiac surgical cases. J Clin Anesth. 2012;24:212–220.
- Kidney Disease: Improving Global Outcomes (KDIGO). Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:8.
- Kidney Disease: Improving Global Outcomes (KDIGO). Clincal practice guidelines for evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):8.
- , . Hemodynamic effects of anesthesia in patients with ischemic heart failure chronically treated with angiotensin‐converting enzyme inhibitors. Anesth Analg. 1997;84:945–949.
- , , , , . The hemodynamic effects of anesthetic induction in vascular surgical patients chronically treated with angiotensin II receptor antagonists. Anesth Analg. 1999;89:1388–1392.
- , , , . Anesthetic management and one‐year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10.
- , , , , . Use of angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers in clinical practice. Expert Rev Cardiovasc Ther. 2012;10:159–166.
- , . An overview of drug‐induced acute kidney injury. Crit Care Med. 2008;36:S216–S223.
- , , , et al. Improvement of endothelial function by chronic angiotensin‐converting enzyme inhibition in heart failure: role of nitric oxide, prostanoids, oxidant stress, and bradykinin. Circulation. 2000;102:351–356.
- , , , . Renin‐angiotensin system antagonists in the perioperative setting: clinical consequences and recommendations for practice. Postgrad Med J. 2011;87:472–481.
- , , , , . Early postoperative statin therapy is associated with a lower incidence of acute kidney injury after cardiac surgery. J Cardiothorac Vasc Anesth. 2010;24:913–920.
- , , , , . Improved survival in acute kidney injury after cardiac surgery. Am J Kidney Dis. 2007;50:703–711.
- , , , . Determinants of postoperative acute kidney injury. Crit Care. 2009;13:R79.
- American College of Physicians. ACP Smart Medicine: Perioperative Medication Management. Tables: Perioperative Cardiovascular Medication Management. http://smartmedicine.acponline.org/content.aspx?gbosID=336. Accessed January 19, 2014.
- . Management of hypotension associated with angiotensin‐axis blockade and general anesthesia administration. J Cardiothorac Vasc Anesth. 2013;27:156–167.
- , , , , , . Clinical consequences of withholding versus administering renin‐angiotensin‐aldosterone system antagonists in the preoperative period. J Hosp Med. 2008;3:319–325.
- , , , et al. Influence of chronic angiotensin‐converting enzyme inhibition on anesthetic induction. Anesthesiology. 1994;81(2):299–307.
- , , , , . Pressor responses to tracheal intubation after sublingual captopril. A pilot study. Anaesthesia. 1990;45(3):243–245.
- , , , , , , . Preoperative angiotensin‐converting enzyme inhibitors and acute kidney injury after coronary artery bypass grafting. Ann Thorac Surg. 2008;86(4):1160–1165.
- , , , et al. The effects of preoperative renin‐angiotensin system inhibitors on outcomes in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27(4):703–709.
- , , , . Renin‐angiotensin blockade is associated with increased mortality after vascular surgery. Can J Anaesth. 2010;57:736–744.
- , . , et al. Preoperative use of angiotensin‐converting enzyme inhibitors/angiotensin receptor blockers is associated with increased risk for acute kidney injury after cardiovascular surgery. Clin J Am Soc Nephrol. 2008;3(5):1266–1273.
- , , , et al.; TRIBE‐AKI Consortium. Preoperative angiotensin‐converting enzyme inhibitors and angiotensin receptor blocker use and acute kidney injury in patients undergoing cardiac surgery. Nephrol Dial Transplant. 2013;28(11):2787–2799.
- , , , et al. The chronic inhibition of angiotensin‐converting enzyme impairs postoperative renal function. Anesth Analg. 2001;93(5):1111–1115.
- , , , et al. Effects of angiotensin‐converting enzyme inhibitor therapy on clinical outcome in patients undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2009;54:1778–1784.
- , , , , , . Acute kidney injury and death associated with renin angiotensin system blockade in cardiothoracic surgery: a meta‐analysis of observational studies. Am J Kidney Dis. 2013;63(6):1077–1086.
- , , . Acute kidney injury after lung resection surgery: incidence and perioperative risk factors. Anesth Analg. 2012;114:1256–1262.
- , , , et al. Angiotensin system inhibitors in a general surgical population. Anesth Analg. 2005;100:636–644, table of contents.
- , , , , . Chronic angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker therapy combined with diuretic therapy is associated with increased episodes of hypotension in noncardiac surgery. J Cardiothorac Vasc Anesth. 2008;22:180–186.
- , , , , . Hemodynamic impact of dexmedetomidine administration in 15,656 noncardiac surgical cases. J Clin Anesth. 2012;24:212–220.
- Kidney Disease: Improving Global Outcomes (KDIGO). Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:8.
- Kidney Disease: Improving Global Outcomes (KDIGO). Clincal practice guidelines for evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):8.
- , . Hemodynamic effects of anesthesia in patients with ischemic heart failure chronically treated with angiotensin‐converting enzyme inhibitors. Anesth Analg. 1997;84:945–949.
- , , , , . The hemodynamic effects of anesthetic induction in vascular surgical patients chronically treated with angiotensin II receptor antagonists. Anesth Analg. 1999;89:1388–1392.
- , , , . Anesthetic management and one‐year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10.
- , , , , . Use of angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers in clinical practice. Expert Rev Cardiovasc Ther. 2012;10:159–166.
- , . An overview of drug‐induced acute kidney injury. Crit Care Med. 2008;36:S216–S223.
- , , , et al. Improvement of endothelial function by chronic angiotensin‐converting enzyme inhibition in heart failure: role of nitric oxide, prostanoids, oxidant stress, and bradykinin. Circulation. 2000;102:351–356.
- , , , . Renin‐angiotensin system antagonists in the perioperative setting: clinical consequences and recommendations for practice. Postgrad Med J. 2011;87:472–481.
- , , , , . Early postoperative statin therapy is associated with a lower incidence of acute kidney injury after cardiac surgery. J Cardiothorac Vasc Anesth. 2010;24:913–920.
- , , , , . Improved survival in acute kidney injury after cardiac surgery. Am J Kidney Dis. 2007;50:703–711.
- , , , . Determinants of postoperative acute kidney injury. Crit Care. 2009;13:R79.
- American College of Physicians. ACP Smart Medicine: Perioperative Medication Management. Tables: Perioperative Cardiovascular Medication Management. http://smartmedicine.acponline.org/content.aspx?gbosID=336. Accessed January 19, 2014.
© 2014 Society of Hospital Medicine
Assessment Tool in the Hands of Medical Residents
Venous thromboembolic events (VTE) are a significant cause of mortality in hospitalized medical and surgical patients.1, 2 The incidence of hospital‐acquired deep vein thrombosis (DVT) is 1040% among medical or general surgical patients in the absence of VTE prophylaxis.3 Approximately 5075% of these cases are preventable with appropriate prophylaxis.3, 4 To reduce hospital‐acquired VTE, the American College of Chest Physicians (ACCP) has published VTE prevention guidelines regularly since 1986. The latest version of the ACCP guidelines recommends that every hospital have an institution‐wide policy that encourages use of VTE prevention strategies. Nevertheless, current evidence demonstrates that VTE prophylaxis remains underutilized in at‐risk patients.5, 6 For example, the ENDORSE study showed that only 39% of at‐risk medical patients received appropriate VTE prophylaxis.6 A more recent study estimated that 58% of hospital‐acquired VTEs were preventable with appropriate prophylaxis utilization.7
Such data demonstrate that a quality gap exists between VTE prophylaxis guideline recommendations and actual practice. Such a gap highlights the need to identify barriers to appropriate implementation of systems‐based strategies aimed at preventing VTE. A presumed barrier for adherence to any VTE protocol is the complexity involved in performing individualized risk assessments.810 All VTE prophylaxis strategies require the clinician to risk‐stratify each patient, identify contraindications to a prophylaxis strategy, and select an accepted strategy. While many VTE risk assessment protocols exist, they tend to fall into two categories: 1) a point‐based system, and 2) a simplified tiered system. Point‐based clinical prediction rules have been advocated by Caprini and others.1115 Such approaches require the clinician to assign points during the identification of VTE risk factors. The clinician must add the points to determine a patient's cumulative VTE risk and use the points to classify that risk as low, moderate, or high. Such point‐based systems are generally considered complex and may underestimate VTE risk, potentially leading to underutilization of prophylaxis strategies.16
Studies have demonstrated that complexity introduces variation into the decision‐making process.17 As a result, both the ACCP and SHM advocate for simplifying the VTE risk assessment process.4, 18 To date, several studies have demonstrated that attending physicians and nurses can reliably apply a VTE risk assessment tool, but none that measure how reliably residents can perform this task when using a point‐based tool.18, 19 For academic medical centers, information about the reliability of such tools is especially important, since they will often be applied by physicians‐in‐training, who have limited knowledge and experience with VTE guidelines and risk assessment. The goal of our study, therefore, was to use clinical vignettes to determine the reliability and protocol adherence of medical residents' application of an adapted point‐based VTE risk assessment tool, independent of other interventions.
Methods
Development of the Risk Assessment Tool
A multispecialty team adapted existing individualized VTE risk assessment tools based on one developed by Caprini.11 The VTE tool (Fig. 1) was designed to assist residents in making two essential determinations prior to ordering a prophylaxis plan. The first determination was the calculation of a total risk score (070 points). This score was determined by identifying and assigning a point value to all medical and surgical risk factors, and summing the points into 3 categories: low (01 point), moderate (24 points), and high (>4 points) VTE risk. The second determination was to identify any contraindications to pharmacological prophylaxis. Like other nonvalidated tools, our tool divided contraindications into absolute or relative. After making these two determinations, residents were encouraged to order 1 of 6 VTE prophylaxis plans. These plans were intended to balance VTE risk against risk factors for bleeding due to prophylaxis.
Construction of Clinical Vignettes
Approval was obtained by the Pennsylvania State University Institutional Review Board. Since previous research demonstrates the utility of clinical vignettes to study the effectiveness of guideline application and decision making, we used a series of 21 randomly selected and de‐identified clinical vignettes to portray a range of real‐world patient admission scenarios.2022 We identified individuals who had been admitted to the Hershey Medical Center using data from the inpatient electronic health record and applying the following inclusion criteria: age >17 years, and admission to a general medical service from the Emergency Department during a 14‐day period in 2008. Since more than 80% of patients admitted to our medical service are admitted through the Emergency Department and residents place all of the admission orders, our goal was to use vignettes that were typical of patients they commonly admit. We attached a paper form of our institution's VTE prophylaxis strategy (Figure 1) to each vignette.
Data Collection
A 1‐hour noon conference titled VTE Workshop was conducted by one of the authors (M.J.B.) during the first quarter of the 2008 academic year. We asked the medical residents to apply the VTE prophylaxis protocol to 21 vignettes during this session. In order to determine the appropriate time allotted to complete the vignettes, each case was completed by M.J.B. and three medical residents (one intern, one second year, and one third year) prior to conducting the VTE workshop. Based on these data, we determined that the median time to complete each vignette was 2 minutes and 15 seconds (range 30 seconds to 7 minutes). Therefore, we assumed that the 21 vignettes could be completed within 1 hour. At the beginning of the conference, the residents were provided with 10 minutes of verbal instruction about how to apply the VTE risk assessment tool. They were instructed to provide a total risk score (070 points) and, based on the total score, to classify each patient as low, moderate, or high risk for VTE. Following the risk assignment, they were instructed to document any absolute and relative contraindications. Finally, they were asked to select the most appropriate VTE prophylaxis plan according to the recommendations of the protocol. Vignettes were considered complete if they had an assessment and plan for >75% of the cases.
Prior to conducting this study, there had been no formal orientation regarding use of the VTE risk assessment tool or incorporation of it into our institution's computerized order entry system. Average attendance for the noon conference is between 20 and 30 house staff, approximately one‐third of the entire residency. Medical students were excluded from the study. All respondents voluntarily and anonymously performed the assessments, and indicated on the front of their vignette packet their level of training as PGY‐1, ‐2, or ‐3. The sessions were overseen by one of the authors to ensure that no communication occurred among the residents.
Data Analysis
We constructed a database with five variables collected from each resident's VTE risk assessment form: 1) a total risk score, 2) a risk classification (low, medium, or high), 3) the number and type of absolute contraindications to pharmacological prophylaxis, 4) the number and type of relative contraindications to pharmacological prophylaxis, and 5) a VTE prophylaxis plan. The lead author also performed these assessments of the 21 vignettes 1 month prior to the resident session. In power calculations performed prior to the session, we determined that the study would need at least 300 observations in order to calculate inter‐rater reliability.23 With the estimation that between 20 and 30 residents would attend, we determined that 21 vignettes would exceed the minimum required observations to allow for an accurate calculation of inter‐rater reliability.
The total risk score was treated as a continuous variable for which the intra‐class correlation (ICC) was calculated. The ICC is used to assess the consistency, or conformity, of measurements made by multiple observers measuring the same quantity.24 Risk stratification, presence of absolute and relative contraindications, and VTE plan were treated as categorical variables. For these, we used Cohen's kappa to assess variability in resident ratings. The kappa score has been used in other studies to determine inter‐rater reliability using similar VTE risk assessment tools.18, 19 Finally, adherence to our hospital's protocol was determined by comparing the residents' VTE plans with the lead author's VTE plans for each of the 21 vignettes. We used SAS 9.1.3 for all statistical analyses (SAS Institute, Cary, NC).
Results
Twenty‐six medical residents attended the conference. Three residents left without submitting their assessments and were excluded from the analysis. Of the 23 residents included in the analysis, 15 (65%) were interns, 5 (22%) second‐year residents, and 3 (13%) third‐year residents. A maximum of 483 observations (21 clinical vignettes and 23 residents) was possible. Six (1%) risk stratifications were missing, and 14 (3%) VTE prophylaxis plans were missing. Therefore, out of a possible 483 paired assessments and plans, complete data existed for 95% (469) of the observations. Residents risk‐stratified the vignettes as low risk for 27% of cases, moderate risk for 38%, and high risk 34%. These differed from those of the lead author, who stratified proportionately more vignettes as high risk (Table 1).
| Risk Stratification | Resident no./total (%) | Attending no./total (%) |
|---|---|---|
| Low | 130/479 (27) | 3/21 (14) |
| Moderate | 183/479 (38) | 7/21 (33) |
| High | 166/479 (34) | 11/21 (52) |
Of those vignette patients stratified as high risk, 77% (128/166) received some form of prophylaxis. Of those stratified as moderate risk, 66% (121/183) received some form of prophylaxis. Finally, of those stratified as low risk, 15% (20/130) received some form of prophylaxis. To explore the impact of the disparity in risk assessments between residents and attending physicians, we used the lead author's assessments as the standard for comparison, and determined that only 64% (309/479) of the observations were risk‐stratified correctly. To emphasize further the potential negative impact of these misclassifications, we determined that appropriate plans would have occurred only 47% of the time. Analysis of these data via risk category showed that low‐risk patients received appropriate prophylaxis 84% of the time. However, protocol adherence for moderate and high‐risk patients occurred only 33 and 40% of the time, respectively (Table 2). Making the assumption that those vignette patients at moderate and high risk who only received mechanical prophylaxis had appropriate contraindications to heparin prophylaxis, protocol adherence remained low at 54 and 58%, respectively.
| Attending Classification | Total | Appropriate Risk Assessment No. (%) | SCDs Only No. (%) | Heparin Only | Both Heparin and SCDs | Ambulation |
|---|---|---|---|---|---|---|
| ||||||
| Low risk | 115 | 86 (75) | 11 (10) | 7 (6) | 0 | 93 (84)a |
| Moderate risk | 138 | 85 (62) | 28 (21)b | 44 (33)a | 16 (12) | 47 (35) |
| High risk | 230 | 138 (60) | 39 (18)b | 69 (31) | 88 (40)a | 27 (12) |
| Total | 483 | 309 (64) | 78 (16) | 120 (26) | 104 (22) | 167 (36) |
The ICC for the total risk score was 0.66, and the kappa coefficient for risk stratification was 0.51 (95% CI 0.50, 0.53), both of which represent moderate agreement. Absolute and relative contraindications were identified 12% (57/483) and 13% (61/483) of the time, respectively. The kappa scores for absolute and relative contraindications were 0.29 and 0.23, respectively. The kappa score for the VTE plan was 0.28 and represents only fair agreement (Table 2).
Subgroup analysis of the 15 intern participants for ICC for the risk score was 0.63. The kappa scores for risk stratification and VTE plan were 0.47 and 0.23, respectively. The kappa scores for senior residents represent aggregate data of 168 observations of second‐ and third‐year residents. For senior residents, the kappa scores for risk stratification and VTE plan were 0.61 and 0.35, respectively (Table 3).
| Risk Score | Stratification | Absolute Contraindication | Relative Contraindication | VTE Plan | ||
|---|---|---|---|---|---|---|
| ||||||
| Aggregate | ICC | 0.66 | ||||
| Kappa | 0.51 | 0.29 | 0.23 | 0.28 | ||
| Intern | ICC | 0.63 | ||||
| Kappa | 0.47 | NA | NA | 0.23 | ||
| Seniora | ICC | 0.73 | ||||
| Kappa | 0.61 | NA | NA | 0.35 | ||
Discussion
We performed this study to determine how reliably our medical residents could apply a point‐based VTE risk assessment tool, similar to those published previously.11 We observed that early in the academic year, our residents were not able to use this tool reliably. While our study does not evaluate the effects of audit and feedback, reminder alerts, or educational interventions, an important first step toward quality improvement in VTE prophylaxis is to reduce variability in risk assessment and decision making. In this endeavor, our results differ markedly from those in the literature. For instance, one study used 3 trained nurses to employ a similar risk assessment tool, and found an ICC of 0.98 for overall assessments of VTE risk, but did not report protocol adherence.19 Another study found inter‐rater reliability to be high among 5 physician observers (kappa scores of 0.81 and 0.90 for risk stratification and VTE plan, respectively).18 These two studies evaluated the performance of experienced evaluators who employed different and simpler VTE risk assessment tools. Our study determined that the inter‐rater reliability of risk assessment and VTE plan between residents using a point‐based VTE risk assessment tool was significantly lower, at 0.51 and 0.28, respectively. There was marked disparity between the lead author's and residents' risk assessments of those deemed to be at low and high risk (Table 1). While both determined approximately one‐third of the patient vignettes to be at moderate risk, the residents misclassified those at high risk in comparison with the author's assessments. This underestimation of VTE risk could lead to profound underprophylaxis in at‐risk patients. To the extent that our findings represent those in other teaching hospitals, such errors could hinder VTE quality improvement efforts in such institutions.
Previous studies that successfully improved VTE prophylaxis rates coupled a risk assessment tool with provider education as well as audit‐and‐feedback interventions.25, 26 In one study, provider education occurred on the first day of every month with an orientation to the hospital's recommended VTE prevention strategies.26 Another study sought to improve the rates of VTE prophylaxis in medical intensive care (MICU) patients without performing individualized risk assessment.27 Using only weekly graphic feedback and verbal reminders to the medical team, it showed an improvement in VTE prophylaxis for 1 year. A third study improved VTE prophylaxis adherence and reduced VTE at 90 days using only reminder alerts.28 Interestingly, several studies reduced the incidence of VTE without employing any patient risk stratification.29 These studies suggest that improvement in VTE prophylaxis rates could have occurred as result of audit‐and‐feedback or reminder systems and perhaps independent of the reliable application of a risk assessment tool.29 The studies that used risk assessment tools with layered interventions make it difficult to interpret whether the tool or the layered interventions were responsible for the improvement in VTE outcomes. Ours is the first study to evaluate how reliably residents can apply a tool independent of other interventions. With only fair to moderate resident agreement in patient risk assessment and VTE plan, our study suggests that the complexity of a point‐based risk assessment protocol (as opposed to a simplified three‐tiered approach) may affect resident prescriptive behavior.
As a result, our study corroborates two things: first, in medical centers that rely on residents to perform VTE prevention using individualized risk assessment, a multilayered approach for VTE prevention must occur. Second, a passively disseminated VTE protocol in the form of a pocket card will most likely not create a sustained improvement in VTE prophylaxis rates or reduce VTE.3035
When addressing certain aspects of quality improvement and safety, teaching hospitals must recognize that their efforts largely rely on resident performance. The 2009 National Resident Matching Program data indicate that there are 22,427 intern positions available in the United States. Often it is the resident's responsibility to perform risk assessments and provide prophylaxis, possibly using a tool that is too complex to apply reliably. Several studies have determined that 65% of medical errors were committed by interns and that 35‐44% of those errors resulted from knowledge deficits.3638 In order to best improve adherence to clinical guidelines, strategies that result in changing physician behavior need to be implemented, and can include but are not limited to the ones found in Figure 2.39 Ideally, teaching centers with computerized order entry should embed the risk assessment process as part of an admission/transfer order set, with a reminder alert. The alert would be activated when at‐risk patients do not receive appropriate prophylaxis. Most alert systems require hospitals to have computerized order entry, which has achieved only 20% market penetration in US hospitals.40, 41 Therefore, some hospitals employ, or intend to employ, passively disseminated risk assessment tools in the form of pocket cards or preprinted forms. These methods are estimated to improve prophylaxis by only 50% and are therefore not considered to be highly reliable strategies.3135
Our study demonstrates only fair to moderate reliability of a point‐based VTE risk assessment tool when used by residents independent of other strategies. It also suggests that residents underestimate those at high risk. In addition, our residents' protocol adherence was suboptimal and would have resulted in appropriate prophylaxis approximately 50% of the time in patients at moderate or high VTE risk. Therefore, when risk assessment tools such as ours are used, it is imperative that frequent education be combined with real‐time patient identification strategies as well as audit and feedback, a process called measure‐vention.13, 14 This is especially true when the risk assessment process is not linked to a reminder system as part of computer‐assisted order entry protocols.
A limitation of our study was the lack of a control group. Since all the residents in attendance received the same clinical vignettes, it would have been of interest to see how the risk assessment tool performed compared with residents who did not have access to the tool. However, based on average noon conference attendance, it would have been difficult to achieve an adequate number of observations to calculate credible ICC and kappa scores. Other limitations include the high number of interns who completed the vignettes compared with senior residents, and the lack of additional attending reviewers to score the vignettes prior to the session. Ideally, in determining the accuracy of protocol adherence, we would have compared residents' determinations with those of several experts who had used an adjudication process in the event of disagreement. In our ongoing work, we are collecting data from a representative sample of attending physicians at our hospital to compare their assessments both with each other and with those of the residents.
Another issue in our design was that the study presented only a limited amount of medical information in the vignettes. In actual clinical circumstances, the amount of historical information is greater and more complicated. One could argue that the artificiality of clinical vignettes is not an accurate representation of resident performance when ordering VTE prophylaxis. However, this approach limits case‐mix variation, so residents should have been able to reach similar conclusions with the information given. Thus the limited information should have maximized residents' intentions to prescribe VTE prophylaxis, and kappa scores would likely be lower in real clinical settings. Finally, our kappa scores were calculated based on aggregate data of interns and residents; however, interns comprised almost two‐thirds of the resident participants. As reported in the results section, intern inter‐rater reliability was slightly lower compared with the senior resident subgroup, suggesting that the variability may be a result of less clinical experience of the interns. However, the study was not powered to assess differences in kappa scores for level of training.
In conclusion, we determined the inter‐rater reliability of an individualized, point‐based VTE risk assessment tool when used by medical residents unfamiliar with its use. Our study showed that under conditions of minimal education, a point‐based VTE assessment tool achieves only fair to moderate reliability. It also suggests that as a stand‐alone tool without a reminder alert, adherence to VTE prevention guidelines is suboptimal and might result in underprophylaxis of hospitalized medical patients at moderate or high VTE risk. In fact, with appropriate prophylaxis, rates were maximally estimated to be 55% (Table 2). Because of the high percentage of interns in the study, these results approximate intern application of a VTE prevention protocol independent of other interventions. Comparing reliability data from our study with those of others raises the question of whether the observed differences in kappa score are because other studies used highly trained observers or because their protocols were less complex. However, a recent study validated a simpler method of VTE risk grouping that performs well regardless of clinical experience.20 Future studies are needed to determine whether there is improved resident inter‐rater reliability using a point‐based risk assessment tool that is embedded into a computerized order entry system with electronic reminder alerts. Finally, in actual clinical settings, the question remains of whether kappa scores correlate with protocol adherence, prophylaxis rates, and VTE reduction when using point‐based tools. If not, then the use of simplified risk‐stratification tools and VTE measure‐vention strategies should be implemented.
Acknowledgements
The authors thank Lisabeth V. Scalzi, MD, MS, Lora Moyer, Kevin McKenna MD, Hammid Al‐Mondhiry, Lucille Anderson, MD, Kathleen Williams, Kevin Larraway, Cynthia Chuang, MD, MS, the residents of the Internal Medicine and Combined Medicine/Pediatrics residencies, and the division of General Internal Medicine at Hershey Medical Center.
- ,,.Autopsy‐verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988.Br J Surg.1991;78(7):849–852.
- , , , , et al.Fatal pulmonary embolism in hospitalised patients: a necropsy review.J Clin Pathol.2004;57(12):1254–1257.
- , , , et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):381S–453S.
- ,.Coronary artery vasculitis and myocardial infarction with systemic lupus erythematosus.NY State J Med.1974;74(5):873–874.
- , , , et al.Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism.Chest.2007;132(3):936–945.
- , , , et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross‐sectional study.Lancet.2008;371(9610):387–394.
- , , , .Venous thromboembolic events in hospitalised medical patients.Thromb Haemost.2009;102(3):505–510.
- ,,.Compliance with recommended prophylaxis for venous thromboembolism: improving the use and rate of uptake of clinical practice guidelines.J Thromb Haemost.2004;2(2):221–227.
- , , , et al.A systematic review of strategies to improve prophylaxis for venous thromboembolism in hospitals.Ann Surg.2005;241(3):397–415.
- ,.Prevention of venous thromboembolism: consensus, controversies, and challenges.Hematol Am Soc Hematol Educ Program.2009:286–292.
- ,,.International perspective on venous thromboembolism prophylaxis in surgery.Semin Thromb Hemost.1991;17(4):322–325.
- , , , et al.Clinical assessment of venous thromboembolic risk in surgical patients.Semin Thromb Hemost.1991;17(suppl 3):304–312.
- , et al.Risk factor assessment in the management of patients with suspected deep venous thrombosis.Int Angiol.2000;19(1):47–51.
- ,,.Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease.Semin Hematol.2001;38(2 suppl 5):12–19.
- .Thrombosis risk assessment as a guide to quality patient care.Dis Mon.2005;51(2–3):70–78.
- ,.Designing and implementing effective venous thromboembolism prevention protocols: lessons from collaborative efforts.J Thromb Thrombolysis.2010;29(2):159–166.
- ,,.Emergency medicine practitioner knowledge and use of decision rules for the evaluation of patients with suspected pulmonary embolism: variations by practice setting and training level.Acad Emerg Med.2007;14(1):53–57.
- , , , , , , , .Optimizing prevention of hospital‐acquired (HA) venous thromboembolism (VTE): prospective validation of a VTE risk assessment model (RAM).J Hosp Med.2010;5(1):10–18..
- , , , et al.Development and testing of a DVT risk assessment tool: providing evidence of validity and reliability.Worldviews Evid Based Nurs.2007;4(1):14–20.
- , , , et al.A novel educational strategy to enhance internal medicine residents' familial colorectal cancer knowledge and risk assessment skills.Am J Gastroenterol.2005;100(3):677–684.
- ,, , , , .Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- , , , et al.Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality.JAMA.2000;283(13):1715–1722.
- .Psychometric Theory.New Delhi:Tate McGraw‐Hill;1981.
- ,.Intraclass correlations: uses in assessing rater reliability.Psychol Bull.1979;86(2):420–428.
- ,,.Innovative approaches to increase deep vein thrombosis prophylaxis rate resulting in a decrease in hospital‐acquired deep vein thrombosis at a tertiary‐care teaching hospital.J Hosp Med.2008;3(2):148–155.
- ,,.Improved use of thromboprophylaxis for deep vein thrombosis following an educational intervention.J Hosp Med.2006;1(6):331–338.
- , , , et al.Minimizing errors of omission: behavioural reenforcement of heparin to avert venous emboli: the BEHAVE study.Crit Care Med.2006;34(3):694–699.
- , , , et al.Electronic alerts to prevent venous thromboembolism among hospitalized patients.N Engl J Med.2005;352(10):969–977.
- , , , .Getting a validated guideline into local practice: implementation and audit of the SIGN guideline on the prevention of deep vein thrombosis in a district general hospital.Scott Med J.1998;43(1):23–25.
- ,,. Improving the Reliability of Health Care. IHI Innovation Series white paper 2004. Available at: www.IHI.org/IHI/Results/WhitePapers/Improving theReliabilityof HealthCare.htm. Accessed October 4,2010.
- , , , et al.Thrombosis prophylaxis in medical patients: a retrospective review of clinical practice patterns.Haematologica.2002;87(7):746–750; discussion 250.
- ,.Genetic epidemiology: systemic lupus erythematosus.Arthritis Res.2001;3(6):331–336.
- ,,.Missed opportunities for prevention of venous thromboembolism: an evaluation of the use of thromboprophylaxis guidelines.Chest.2001;120(6):1964–1971.
- , , , , .Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting.Arch Intern Med.1998;158(17):1909–1912.
- ,,.Venous thromboembolism prophylaxis used by consultant general surgeons in Scotland.J R Coll Surg Edinb.2001;46(6):329–333.
- ,.Ordering errors by first‐year residents: evidence of learning from mistakes.Mo Med.2004;101(2):128–131.
- ,.Prevention of medication errors: teaching and training.Br J Clin Pharmacol.2009;67(6):656–661.
- ,,.Reducing medication errors in a surgical residency training program.Am Surg.2004;70(5):467–471.
- , , , et al.Why don't physicians follow clinical practice guidelines? A framework for improvement.JAMA.1999;282(15):1458–1465.
- , , , , .Predicting computerized physician order entry system adoption in US hospitals: can the federal mandate be met?Int J Med Inform.2008;77(8):539–545.
- ,.Implementation of computerized physician order entry in seven countries.Health Aff (Millwood).2009;28(2):404–414.
Venous thromboembolic events (VTE) are a significant cause of mortality in hospitalized medical and surgical patients.1, 2 The incidence of hospital‐acquired deep vein thrombosis (DVT) is 1040% among medical or general surgical patients in the absence of VTE prophylaxis.3 Approximately 5075% of these cases are preventable with appropriate prophylaxis.3, 4 To reduce hospital‐acquired VTE, the American College of Chest Physicians (ACCP) has published VTE prevention guidelines regularly since 1986. The latest version of the ACCP guidelines recommends that every hospital have an institution‐wide policy that encourages use of VTE prevention strategies. Nevertheless, current evidence demonstrates that VTE prophylaxis remains underutilized in at‐risk patients.5, 6 For example, the ENDORSE study showed that only 39% of at‐risk medical patients received appropriate VTE prophylaxis.6 A more recent study estimated that 58% of hospital‐acquired VTEs were preventable with appropriate prophylaxis utilization.7
Such data demonstrate that a quality gap exists between VTE prophylaxis guideline recommendations and actual practice. Such a gap highlights the need to identify barriers to appropriate implementation of systems‐based strategies aimed at preventing VTE. A presumed barrier for adherence to any VTE protocol is the complexity involved in performing individualized risk assessments.810 All VTE prophylaxis strategies require the clinician to risk‐stratify each patient, identify contraindications to a prophylaxis strategy, and select an accepted strategy. While many VTE risk assessment protocols exist, they tend to fall into two categories: 1) a point‐based system, and 2) a simplified tiered system. Point‐based clinical prediction rules have been advocated by Caprini and others.1115 Such approaches require the clinician to assign points during the identification of VTE risk factors. The clinician must add the points to determine a patient's cumulative VTE risk and use the points to classify that risk as low, moderate, or high. Such point‐based systems are generally considered complex and may underestimate VTE risk, potentially leading to underutilization of prophylaxis strategies.16
Studies have demonstrated that complexity introduces variation into the decision‐making process.17 As a result, both the ACCP and SHM advocate for simplifying the VTE risk assessment process.4, 18 To date, several studies have demonstrated that attending physicians and nurses can reliably apply a VTE risk assessment tool, but none that measure how reliably residents can perform this task when using a point‐based tool.18, 19 For academic medical centers, information about the reliability of such tools is especially important, since they will often be applied by physicians‐in‐training, who have limited knowledge and experience with VTE guidelines and risk assessment. The goal of our study, therefore, was to use clinical vignettes to determine the reliability and protocol adherence of medical residents' application of an adapted point‐based VTE risk assessment tool, independent of other interventions.
Methods
Development of the Risk Assessment Tool
A multispecialty team adapted existing individualized VTE risk assessment tools based on one developed by Caprini.11 The VTE tool (Fig. 1) was designed to assist residents in making two essential determinations prior to ordering a prophylaxis plan. The first determination was the calculation of a total risk score (070 points). This score was determined by identifying and assigning a point value to all medical and surgical risk factors, and summing the points into 3 categories: low (01 point), moderate (24 points), and high (>4 points) VTE risk. The second determination was to identify any contraindications to pharmacological prophylaxis. Like other nonvalidated tools, our tool divided contraindications into absolute or relative. After making these two determinations, residents were encouraged to order 1 of 6 VTE prophylaxis plans. These plans were intended to balance VTE risk against risk factors for bleeding due to prophylaxis.
Construction of Clinical Vignettes
Approval was obtained by the Pennsylvania State University Institutional Review Board. Since previous research demonstrates the utility of clinical vignettes to study the effectiveness of guideline application and decision making, we used a series of 21 randomly selected and de‐identified clinical vignettes to portray a range of real‐world patient admission scenarios.2022 We identified individuals who had been admitted to the Hershey Medical Center using data from the inpatient electronic health record and applying the following inclusion criteria: age >17 years, and admission to a general medical service from the Emergency Department during a 14‐day period in 2008. Since more than 80% of patients admitted to our medical service are admitted through the Emergency Department and residents place all of the admission orders, our goal was to use vignettes that were typical of patients they commonly admit. We attached a paper form of our institution's VTE prophylaxis strategy (Figure 1) to each vignette.
Data Collection
A 1‐hour noon conference titled VTE Workshop was conducted by one of the authors (M.J.B.) during the first quarter of the 2008 academic year. We asked the medical residents to apply the VTE prophylaxis protocol to 21 vignettes during this session. In order to determine the appropriate time allotted to complete the vignettes, each case was completed by M.J.B. and three medical residents (one intern, one second year, and one third year) prior to conducting the VTE workshop. Based on these data, we determined that the median time to complete each vignette was 2 minutes and 15 seconds (range 30 seconds to 7 minutes). Therefore, we assumed that the 21 vignettes could be completed within 1 hour. At the beginning of the conference, the residents were provided with 10 minutes of verbal instruction about how to apply the VTE risk assessment tool. They were instructed to provide a total risk score (070 points) and, based on the total score, to classify each patient as low, moderate, or high risk for VTE. Following the risk assignment, they were instructed to document any absolute and relative contraindications. Finally, they were asked to select the most appropriate VTE prophylaxis plan according to the recommendations of the protocol. Vignettes were considered complete if they had an assessment and plan for >75% of the cases.
Prior to conducting this study, there had been no formal orientation regarding use of the VTE risk assessment tool or incorporation of it into our institution's computerized order entry system. Average attendance for the noon conference is between 20 and 30 house staff, approximately one‐third of the entire residency. Medical students were excluded from the study. All respondents voluntarily and anonymously performed the assessments, and indicated on the front of their vignette packet their level of training as PGY‐1, ‐2, or ‐3. The sessions were overseen by one of the authors to ensure that no communication occurred among the residents.
Data Analysis
We constructed a database with five variables collected from each resident's VTE risk assessment form: 1) a total risk score, 2) a risk classification (low, medium, or high), 3) the number and type of absolute contraindications to pharmacological prophylaxis, 4) the number and type of relative contraindications to pharmacological prophylaxis, and 5) a VTE prophylaxis plan. The lead author also performed these assessments of the 21 vignettes 1 month prior to the resident session. In power calculations performed prior to the session, we determined that the study would need at least 300 observations in order to calculate inter‐rater reliability.23 With the estimation that between 20 and 30 residents would attend, we determined that 21 vignettes would exceed the minimum required observations to allow for an accurate calculation of inter‐rater reliability.
The total risk score was treated as a continuous variable for which the intra‐class correlation (ICC) was calculated. The ICC is used to assess the consistency, or conformity, of measurements made by multiple observers measuring the same quantity.24 Risk stratification, presence of absolute and relative contraindications, and VTE plan were treated as categorical variables. For these, we used Cohen's kappa to assess variability in resident ratings. The kappa score has been used in other studies to determine inter‐rater reliability using similar VTE risk assessment tools.18, 19 Finally, adherence to our hospital's protocol was determined by comparing the residents' VTE plans with the lead author's VTE plans for each of the 21 vignettes. We used SAS 9.1.3 for all statistical analyses (SAS Institute, Cary, NC).
Results
Twenty‐six medical residents attended the conference. Three residents left without submitting their assessments and were excluded from the analysis. Of the 23 residents included in the analysis, 15 (65%) were interns, 5 (22%) second‐year residents, and 3 (13%) third‐year residents. A maximum of 483 observations (21 clinical vignettes and 23 residents) was possible. Six (1%) risk stratifications were missing, and 14 (3%) VTE prophylaxis plans were missing. Therefore, out of a possible 483 paired assessments and plans, complete data existed for 95% (469) of the observations. Residents risk‐stratified the vignettes as low risk for 27% of cases, moderate risk for 38%, and high risk 34%. These differed from those of the lead author, who stratified proportionately more vignettes as high risk (Table 1).
| Risk Stratification | Resident no./total (%) | Attending no./total (%) |
|---|---|---|
| Low | 130/479 (27) | 3/21 (14) |
| Moderate | 183/479 (38) | 7/21 (33) |
| High | 166/479 (34) | 11/21 (52) |
Of those vignette patients stratified as high risk, 77% (128/166) received some form of prophylaxis. Of those stratified as moderate risk, 66% (121/183) received some form of prophylaxis. Finally, of those stratified as low risk, 15% (20/130) received some form of prophylaxis. To explore the impact of the disparity in risk assessments between residents and attending physicians, we used the lead author's assessments as the standard for comparison, and determined that only 64% (309/479) of the observations were risk‐stratified correctly. To emphasize further the potential negative impact of these misclassifications, we determined that appropriate plans would have occurred only 47% of the time. Analysis of these data via risk category showed that low‐risk patients received appropriate prophylaxis 84% of the time. However, protocol adherence for moderate and high‐risk patients occurred only 33 and 40% of the time, respectively (Table 2). Making the assumption that those vignette patients at moderate and high risk who only received mechanical prophylaxis had appropriate contraindications to heparin prophylaxis, protocol adherence remained low at 54 and 58%, respectively.
| Attending Classification | Total | Appropriate Risk Assessment No. (%) | SCDs Only No. (%) | Heparin Only | Both Heparin and SCDs | Ambulation |
|---|---|---|---|---|---|---|
| ||||||
| Low risk | 115 | 86 (75) | 11 (10) | 7 (6) | 0 | 93 (84)a |
| Moderate risk | 138 | 85 (62) | 28 (21)b | 44 (33)a | 16 (12) | 47 (35) |
| High risk | 230 | 138 (60) | 39 (18)b | 69 (31) | 88 (40)a | 27 (12) |
| Total | 483 | 309 (64) | 78 (16) | 120 (26) | 104 (22) | 167 (36) |
The ICC for the total risk score was 0.66, and the kappa coefficient for risk stratification was 0.51 (95% CI 0.50, 0.53), both of which represent moderate agreement. Absolute and relative contraindications were identified 12% (57/483) and 13% (61/483) of the time, respectively. The kappa scores for absolute and relative contraindications were 0.29 and 0.23, respectively. The kappa score for the VTE plan was 0.28 and represents only fair agreement (Table 2).
Subgroup analysis of the 15 intern participants for ICC for the risk score was 0.63. The kappa scores for risk stratification and VTE plan were 0.47 and 0.23, respectively. The kappa scores for senior residents represent aggregate data of 168 observations of second‐ and third‐year residents. For senior residents, the kappa scores for risk stratification and VTE plan were 0.61 and 0.35, respectively (Table 3).
| Risk Score | Stratification | Absolute Contraindication | Relative Contraindication | VTE Plan | ||
|---|---|---|---|---|---|---|
| ||||||
| Aggregate | ICC | 0.66 | ||||
| Kappa | 0.51 | 0.29 | 0.23 | 0.28 | ||
| Intern | ICC | 0.63 | ||||
| Kappa | 0.47 | NA | NA | 0.23 | ||
| Seniora | ICC | 0.73 | ||||
| Kappa | 0.61 | NA | NA | 0.35 | ||
Discussion
We performed this study to determine how reliably our medical residents could apply a point‐based VTE risk assessment tool, similar to those published previously.11 We observed that early in the academic year, our residents were not able to use this tool reliably. While our study does not evaluate the effects of audit and feedback, reminder alerts, or educational interventions, an important first step toward quality improvement in VTE prophylaxis is to reduce variability in risk assessment and decision making. In this endeavor, our results differ markedly from those in the literature. For instance, one study used 3 trained nurses to employ a similar risk assessment tool, and found an ICC of 0.98 for overall assessments of VTE risk, but did not report protocol adherence.19 Another study found inter‐rater reliability to be high among 5 physician observers (kappa scores of 0.81 and 0.90 for risk stratification and VTE plan, respectively).18 These two studies evaluated the performance of experienced evaluators who employed different and simpler VTE risk assessment tools. Our study determined that the inter‐rater reliability of risk assessment and VTE plan between residents using a point‐based VTE risk assessment tool was significantly lower, at 0.51 and 0.28, respectively. There was marked disparity between the lead author's and residents' risk assessments of those deemed to be at low and high risk (Table 1). While both determined approximately one‐third of the patient vignettes to be at moderate risk, the residents misclassified those at high risk in comparison with the author's assessments. This underestimation of VTE risk could lead to profound underprophylaxis in at‐risk patients. To the extent that our findings represent those in other teaching hospitals, such errors could hinder VTE quality improvement efforts in such institutions.
Previous studies that successfully improved VTE prophylaxis rates coupled a risk assessment tool with provider education as well as audit‐and‐feedback interventions.25, 26 In one study, provider education occurred on the first day of every month with an orientation to the hospital's recommended VTE prevention strategies.26 Another study sought to improve the rates of VTE prophylaxis in medical intensive care (MICU) patients without performing individualized risk assessment.27 Using only weekly graphic feedback and verbal reminders to the medical team, it showed an improvement in VTE prophylaxis for 1 year. A third study improved VTE prophylaxis adherence and reduced VTE at 90 days using only reminder alerts.28 Interestingly, several studies reduced the incidence of VTE without employing any patient risk stratification.29 These studies suggest that improvement in VTE prophylaxis rates could have occurred as result of audit‐and‐feedback or reminder systems and perhaps independent of the reliable application of a risk assessment tool.29 The studies that used risk assessment tools with layered interventions make it difficult to interpret whether the tool or the layered interventions were responsible for the improvement in VTE outcomes. Ours is the first study to evaluate how reliably residents can apply a tool independent of other interventions. With only fair to moderate resident agreement in patient risk assessment and VTE plan, our study suggests that the complexity of a point‐based risk assessment protocol (as opposed to a simplified three‐tiered approach) may affect resident prescriptive behavior.
As a result, our study corroborates two things: first, in medical centers that rely on residents to perform VTE prevention using individualized risk assessment, a multilayered approach for VTE prevention must occur. Second, a passively disseminated VTE protocol in the form of a pocket card will most likely not create a sustained improvement in VTE prophylaxis rates or reduce VTE.3035
When addressing certain aspects of quality improvement and safety, teaching hospitals must recognize that their efforts largely rely on resident performance. The 2009 National Resident Matching Program data indicate that there are 22,427 intern positions available in the United States. Often it is the resident's responsibility to perform risk assessments and provide prophylaxis, possibly using a tool that is too complex to apply reliably. Several studies have determined that 65% of medical errors were committed by interns and that 35‐44% of those errors resulted from knowledge deficits.3638 In order to best improve adherence to clinical guidelines, strategies that result in changing physician behavior need to be implemented, and can include but are not limited to the ones found in Figure 2.39 Ideally, teaching centers with computerized order entry should embed the risk assessment process as part of an admission/transfer order set, with a reminder alert. The alert would be activated when at‐risk patients do not receive appropriate prophylaxis. Most alert systems require hospitals to have computerized order entry, which has achieved only 20% market penetration in US hospitals.40, 41 Therefore, some hospitals employ, or intend to employ, passively disseminated risk assessment tools in the form of pocket cards or preprinted forms. These methods are estimated to improve prophylaxis by only 50% and are therefore not considered to be highly reliable strategies.3135
Our study demonstrates only fair to moderate reliability of a point‐based VTE risk assessment tool when used by residents independent of other strategies. It also suggests that residents underestimate those at high risk. In addition, our residents' protocol adherence was suboptimal and would have resulted in appropriate prophylaxis approximately 50% of the time in patients at moderate or high VTE risk. Therefore, when risk assessment tools such as ours are used, it is imperative that frequent education be combined with real‐time patient identification strategies as well as audit and feedback, a process called measure‐vention.13, 14 This is especially true when the risk assessment process is not linked to a reminder system as part of computer‐assisted order entry protocols.
A limitation of our study was the lack of a control group. Since all the residents in attendance received the same clinical vignettes, it would have been of interest to see how the risk assessment tool performed compared with residents who did not have access to the tool. However, based on average noon conference attendance, it would have been difficult to achieve an adequate number of observations to calculate credible ICC and kappa scores. Other limitations include the high number of interns who completed the vignettes compared with senior residents, and the lack of additional attending reviewers to score the vignettes prior to the session. Ideally, in determining the accuracy of protocol adherence, we would have compared residents' determinations with those of several experts who had used an adjudication process in the event of disagreement. In our ongoing work, we are collecting data from a representative sample of attending physicians at our hospital to compare their assessments both with each other and with those of the residents.
Another issue in our design was that the study presented only a limited amount of medical information in the vignettes. In actual clinical circumstances, the amount of historical information is greater and more complicated. One could argue that the artificiality of clinical vignettes is not an accurate representation of resident performance when ordering VTE prophylaxis. However, this approach limits case‐mix variation, so residents should have been able to reach similar conclusions with the information given. Thus the limited information should have maximized residents' intentions to prescribe VTE prophylaxis, and kappa scores would likely be lower in real clinical settings. Finally, our kappa scores were calculated based on aggregate data of interns and residents; however, interns comprised almost two‐thirds of the resident participants. As reported in the results section, intern inter‐rater reliability was slightly lower compared with the senior resident subgroup, suggesting that the variability may be a result of less clinical experience of the interns. However, the study was not powered to assess differences in kappa scores for level of training.
In conclusion, we determined the inter‐rater reliability of an individualized, point‐based VTE risk assessment tool when used by medical residents unfamiliar with its use. Our study showed that under conditions of minimal education, a point‐based VTE assessment tool achieves only fair to moderate reliability. It also suggests that as a stand‐alone tool without a reminder alert, adherence to VTE prevention guidelines is suboptimal and might result in underprophylaxis of hospitalized medical patients at moderate or high VTE risk. In fact, with appropriate prophylaxis, rates were maximally estimated to be 55% (Table 2). Because of the high percentage of interns in the study, these results approximate intern application of a VTE prevention protocol independent of other interventions. Comparing reliability data from our study with those of others raises the question of whether the observed differences in kappa score are because other studies used highly trained observers or because their protocols were less complex. However, a recent study validated a simpler method of VTE risk grouping that performs well regardless of clinical experience.20 Future studies are needed to determine whether there is improved resident inter‐rater reliability using a point‐based risk assessment tool that is embedded into a computerized order entry system with electronic reminder alerts. Finally, in actual clinical settings, the question remains of whether kappa scores correlate with protocol adherence, prophylaxis rates, and VTE reduction when using point‐based tools. If not, then the use of simplified risk‐stratification tools and VTE measure‐vention strategies should be implemented.
Acknowledgements
The authors thank Lisabeth V. Scalzi, MD, MS, Lora Moyer, Kevin McKenna MD, Hammid Al‐Mondhiry, Lucille Anderson, MD, Kathleen Williams, Kevin Larraway, Cynthia Chuang, MD, MS, the residents of the Internal Medicine and Combined Medicine/Pediatrics residencies, and the division of General Internal Medicine at Hershey Medical Center.
Venous thromboembolic events (VTE) are a significant cause of mortality in hospitalized medical and surgical patients.1, 2 The incidence of hospital‐acquired deep vein thrombosis (DVT) is 1040% among medical or general surgical patients in the absence of VTE prophylaxis.3 Approximately 5075% of these cases are preventable with appropriate prophylaxis.3, 4 To reduce hospital‐acquired VTE, the American College of Chest Physicians (ACCP) has published VTE prevention guidelines regularly since 1986. The latest version of the ACCP guidelines recommends that every hospital have an institution‐wide policy that encourages use of VTE prevention strategies. Nevertheless, current evidence demonstrates that VTE prophylaxis remains underutilized in at‐risk patients.5, 6 For example, the ENDORSE study showed that only 39% of at‐risk medical patients received appropriate VTE prophylaxis.6 A more recent study estimated that 58% of hospital‐acquired VTEs were preventable with appropriate prophylaxis utilization.7
Such data demonstrate that a quality gap exists between VTE prophylaxis guideline recommendations and actual practice. Such a gap highlights the need to identify barriers to appropriate implementation of systems‐based strategies aimed at preventing VTE. A presumed barrier for adherence to any VTE protocol is the complexity involved in performing individualized risk assessments.810 All VTE prophylaxis strategies require the clinician to risk‐stratify each patient, identify contraindications to a prophylaxis strategy, and select an accepted strategy. While many VTE risk assessment protocols exist, they tend to fall into two categories: 1) a point‐based system, and 2) a simplified tiered system. Point‐based clinical prediction rules have been advocated by Caprini and others.1115 Such approaches require the clinician to assign points during the identification of VTE risk factors. The clinician must add the points to determine a patient's cumulative VTE risk and use the points to classify that risk as low, moderate, or high. Such point‐based systems are generally considered complex and may underestimate VTE risk, potentially leading to underutilization of prophylaxis strategies.16
Studies have demonstrated that complexity introduces variation into the decision‐making process.17 As a result, both the ACCP and SHM advocate for simplifying the VTE risk assessment process.4, 18 To date, several studies have demonstrated that attending physicians and nurses can reliably apply a VTE risk assessment tool, but none that measure how reliably residents can perform this task when using a point‐based tool.18, 19 For academic medical centers, information about the reliability of such tools is especially important, since they will often be applied by physicians‐in‐training, who have limited knowledge and experience with VTE guidelines and risk assessment. The goal of our study, therefore, was to use clinical vignettes to determine the reliability and protocol adherence of medical residents' application of an adapted point‐based VTE risk assessment tool, independent of other interventions.
Methods
Development of the Risk Assessment Tool
A multispecialty team adapted existing individualized VTE risk assessment tools based on one developed by Caprini.11 The VTE tool (Fig. 1) was designed to assist residents in making two essential determinations prior to ordering a prophylaxis plan. The first determination was the calculation of a total risk score (070 points). This score was determined by identifying and assigning a point value to all medical and surgical risk factors, and summing the points into 3 categories: low (01 point), moderate (24 points), and high (>4 points) VTE risk. The second determination was to identify any contraindications to pharmacological prophylaxis. Like other nonvalidated tools, our tool divided contraindications into absolute or relative. After making these two determinations, residents were encouraged to order 1 of 6 VTE prophylaxis plans. These plans were intended to balance VTE risk against risk factors for bleeding due to prophylaxis.
Construction of Clinical Vignettes
Approval was obtained by the Pennsylvania State University Institutional Review Board. Since previous research demonstrates the utility of clinical vignettes to study the effectiveness of guideline application and decision making, we used a series of 21 randomly selected and de‐identified clinical vignettes to portray a range of real‐world patient admission scenarios.2022 We identified individuals who had been admitted to the Hershey Medical Center using data from the inpatient electronic health record and applying the following inclusion criteria: age >17 years, and admission to a general medical service from the Emergency Department during a 14‐day period in 2008. Since more than 80% of patients admitted to our medical service are admitted through the Emergency Department and residents place all of the admission orders, our goal was to use vignettes that were typical of patients they commonly admit. We attached a paper form of our institution's VTE prophylaxis strategy (Figure 1) to each vignette.
Data Collection
A 1‐hour noon conference titled VTE Workshop was conducted by one of the authors (M.J.B.) during the first quarter of the 2008 academic year. We asked the medical residents to apply the VTE prophylaxis protocol to 21 vignettes during this session. In order to determine the appropriate time allotted to complete the vignettes, each case was completed by M.J.B. and three medical residents (one intern, one second year, and one third year) prior to conducting the VTE workshop. Based on these data, we determined that the median time to complete each vignette was 2 minutes and 15 seconds (range 30 seconds to 7 minutes). Therefore, we assumed that the 21 vignettes could be completed within 1 hour. At the beginning of the conference, the residents were provided with 10 minutes of verbal instruction about how to apply the VTE risk assessment tool. They were instructed to provide a total risk score (070 points) and, based on the total score, to classify each patient as low, moderate, or high risk for VTE. Following the risk assignment, they were instructed to document any absolute and relative contraindications. Finally, they were asked to select the most appropriate VTE prophylaxis plan according to the recommendations of the protocol. Vignettes were considered complete if they had an assessment and plan for >75% of the cases.
Prior to conducting this study, there had been no formal orientation regarding use of the VTE risk assessment tool or incorporation of it into our institution's computerized order entry system. Average attendance for the noon conference is between 20 and 30 house staff, approximately one‐third of the entire residency. Medical students were excluded from the study. All respondents voluntarily and anonymously performed the assessments, and indicated on the front of their vignette packet their level of training as PGY‐1, ‐2, or ‐3. The sessions were overseen by one of the authors to ensure that no communication occurred among the residents.
Data Analysis
We constructed a database with five variables collected from each resident's VTE risk assessment form: 1) a total risk score, 2) a risk classification (low, medium, or high), 3) the number and type of absolute contraindications to pharmacological prophylaxis, 4) the number and type of relative contraindications to pharmacological prophylaxis, and 5) a VTE prophylaxis plan. The lead author also performed these assessments of the 21 vignettes 1 month prior to the resident session. In power calculations performed prior to the session, we determined that the study would need at least 300 observations in order to calculate inter‐rater reliability.23 With the estimation that between 20 and 30 residents would attend, we determined that 21 vignettes would exceed the minimum required observations to allow for an accurate calculation of inter‐rater reliability.
The total risk score was treated as a continuous variable for which the intra‐class correlation (ICC) was calculated. The ICC is used to assess the consistency, or conformity, of measurements made by multiple observers measuring the same quantity.24 Risk stratification, presence of absolute and relative contraindications, and VTE plan were treated as categorical variables. For these, we used Cohen's kappa to assess variability in resident ratings. The kappa score has been used in other studies to determine inter‐rater reliability using similar VTE risk assessment tools.18, 19 Finally, adherence to our hospital's protocol was determined by comparing the residents' VTE plans with the lead author's VTE plans for each of the 21 vignettes. We used SAS 9.1.3 for all statistical analyses (SAS Institute, Cary, NC).
Results
Twenty‐six medical residents attended the conference. Three residents left without submitting their assessments and were excluded from the analysis. Of the 23 residents included in the analysis, 15 (65%) were interns, 5 (22%) second‐year residents, and 3 (13%) third‐year residents. A maximum of 483 observations (21 clinical vignettes and 23 residents) was possible. Six (1%) risk stratifications were missing, and 14 (3%) VTE prophylaxis plans were missing. Therefore, out of a possible 483 paired assessments and plans, complete data existed for 95% (469) of the observations. Residents risk‐stratified the vignettes as low risk for 27% of cases, moderate risk for 38%, and high risk 34%. These differed from those of the lead author, who stratified proportionately more vignettes as high risk (Table 1).
| Risk Stratification | Resident no./total (%) | Attending no./total (%) |
|---|---|---|
| Low | 130/479 (27) | 3/21 (14) |
| Moderate | 183/479 (38) | 7/21 (33) |
| High | 166/479 (34) | 11/21 (52) |
Of those vignette patients stratified as high risk, 77% (128/166) received some form of prophylaxis. Of those stratified as moderate risk, 66% (121/183) received some form of prophylaxis. Finally, of those stratified as low risk, 15% (20/130) received some form of prophylaxis. To explore the impact of the disparity in risk assessments between residents and attending physicians, we used the lead author's assessments as the standard for comparison, and determined that only 64% (309/479) of the observations were risk‐stratified correctly. To emphasize further the potential negative impact of these misclassifications, we determined that appropriate plans would have occurred only 47% of the time. Analysis of these data via risk category showed that low‐risk patients received appropriate prophylaxis 84% of the time. However, protocol adherence for moderate and high‐risk patients occurred only 33 and 40% of the time, respectively (Table 2). Making the assumption that those vignette patients at moderate and high risk who only received mechanical prophylaxis had appropriate contraindications to heparin prophylaxis, protocol adherence remained low at 54 and 58%, respectively.
| Attending Classification | Total | Appropriate Risk Assessment No. (%) | SCDs Only No. (%) | Heparin Only | Both Heparin and SCDs | Ambulation |
|---|---|---|---|---|---|---|
| ||||||
| Low risk | 115 | 86 (75) | 11 (10) | 7 (6) | 0 | 93 (84)a |
| Moderate risk | 138 | 85 (62) | 28 (21)b | 44 (33)a | 16 (12) | 47 (35) |
| High risk | 230 | 138 (60) | 39 (18)b | 69 (31) | 88 (40)a | 27 (12) |
| Total | 483 | 309 (64) | 78 (16) | 120 (26) | 104 (22) | 167 (36) |
The ICC for the total risk score was 0.66, and the kappa coefficient for risk stratification was 0.51 (95% CI 0.50, 0.53), both of which represent moderate agreement. Absolute and relative contraindications were identified 12% (57/483) and 13% (61/483) of the time, respectively. The kappa scores for absolute and relative contraindications were 0.29 and 0.23, respectively. The kappa score for the VTE plan was 0.28 and represents only fair agreement (Table 2).
Subgroup analysis of the 15 intern participants for ICC for the risk score was 0.63. The kappa scores for risk stratification and VTE plan were 0.47 and 0.23, respectively. The kappa scores for senior residents represent aggregate data of 168 observations of second‐ and third‐year residents. For senior residents, the kappa scores for risk stratification and VTE plan were 0.61 and 0.35, respectively (Table 3).
| Risk Score | Stratification | Absolute Contraindication | Relative Contraindication | VTE Plan | ||
|---|---|---|---|---|---|---|
| ||||||
| Aggregate | ICC | 0.66 | ||||
| Kappa | 0.51 | 0.29 | 0.23 | 0.28 | ||
| Intern | ICC | 0.63 | ||||
| Kappa | 0.47 | NA | NA | 0.23 | ||
| Seniora | ICC | 0.73 | ||||
| Kappa | 0.61 | NA | NA | 0.35 | ||
Discussion
We performed this study to determine how reliably our medical residents could apply a point‐based VTE risk assessment tool, similar to those published previously.11 We observed that early in the academic year, our residents were not able to use this tool reliably. While our study does not evaluate the effects of audit and feedback, reminder alerts, or educational interventions, an important first step toward quality improvement in VTE prophylaxis is to reduce variability in risk assessment and decision making. In this endeavor, our results differ markedly from those in the literature. For instance, one study used 3 trained nurses to employ a similar risk assessment tool, and found an ICC of 0.98 for overall assessments of VTE risk, but did not report protocol adherence.19 Another study found inter‐rater reliability to be high among 5 physician observers (kappa scores of 0.81 and 0.90 for risk stratification and VTE plan, respectively).18 These two studies evaluated the performance of experienced evaluators who employed different and simpler VTE risk assessment tools. Our study determined that the inter‐rater reliability of risk assessment and VTE plan between residents using a point‐based VTE risk assessment tool was significantly lower, at 0.51 and 0.28, respectively. There was marked disparity between the lead author's and residents' risk assessments of those deemed to be at low and high risk (Table 1). While both determined approximately one‐third of the patient vignettes to be at moderate risk, the residents misclassified those at high risk in comparison with the author's assessments. This underestimation of VTE risk could lead to profound underprophylaxis in at‐risk patients. To the extent that our findings represent those in other teaching hospitals, such errors could hinder VTE quality improvement efforts in such institutions.
Previous studies that successfully improved VTE prophylaxis rates coupled a risk assessment tool with provider education as well as audit‐and‐feedback interventions.25, 26 In one study, provider education occurred on the first day of every month with an orientation to the hospital's recommended VTE prevention strategies.26 Another study sought to improve the rates of VTE prophylaxis in medical intensive care (MICU) patients without performing individualized risk assessment.27 Using only weekly graphic feedback and verbal reminders to the medical team, it showed an improvement in VTE prophylaxis for 1 year. A third study improved VTE prophylaxis adherence and reduced VTE at 90 days using only reminder alerts.28 Interestingly, several studies reduced the incidence of VTE without employing any patient risk stratification.29 These studies suggest that improvement in VTE prophylaxis rates could have occurred as result of audit‐and‐feedback or reminder systems and perhaps independent of the reliable application of a risk assessment tool.29 The studies that used risk assessment tools with layered interventions make it difficult to interpret whether the tool or the layered interventions were responsible for the improvement in VTE outcomes. Ours is the first study to evaluate how reliably residents can apply a tool independent of other interventions. With only fair to moderate resident agreement in patient risk assessment and VTE plan, our study suggests that the complexity of a point‐based risk assessment protocol (as opposed to a simplified three‐tiered approach) may affect resident prescriptive behavior.
As a result, our study corroborates two things: first, in medical centers that rely on residents to perform VTE prevention using individualized risk assessment, a multilayered approach for VTE prevention must occur. Second, a passively disseminated VTE protocol in the form of a pocket card will most likely not create a sustained improvement in VTE prophylaxis rates or reduce VTE.3035
When addressing certain aspects of quality improvement and safety, teaching hospitals must recognize that their efforts largely rely on resident performance. The 2009 National Resident Matching Program data indicate that there are 22,427 intern positions available in the United States. Often it is the resident's responsibility to perform risk assessments and provide prophylaxis, possibly using a tool that is too complex to apply reliably. Several studies have determined that 65% of medical errors were committed by interns and that 35‐44% of those errors resulted from knowledge deficits.3638 In order to best improve adherence to clinical guidelines, strategies that result in changing physician behavior need to be implemented, and can include but are not limited to the ones found in Figure 2.39 Ideally, teaching centers with computerized order entry should embed the risk assessment process as part of an admission/transfer order set, with a reminder alert. The alert would be activated when at‐risk patients do not receive appropriate prophylaxis. Most alert systems require hospitals to have computerized order entry, which has achieved only 20% market penetration in US hospitals.40, 41 Therefore, some hospitals employ, or intend to employ, passively disseminated risk assessment tools in the form of pocket cards or preprinted forms. These methods are estimated to improve prophylaxis by only 50% and are therefore not considered to be highly reliable strategies.3135
Our study demonstrates only fair to moderate reliability of a point‐based VTE risk assessment tool when used by residents independent of other strategies. It also suggests that residents underestimate those at high risk. In addition, our residents' protocol adherence was suboptimal and would have resulted in appropriate prophylaxis approximately 50% of the time in patients at moderate or high VTE risk. Therefore, when risk assessment tools such as ours are used, it is imperative that frequent education be combined with real‐time patient identification strategies as well as audit and feedback, a process called measure‐vention.13, 14 This is especially true when the risk assessment process is not linked to a reminder system as part of computer‐assisted order entry protocols.
A limitation of our study was the lack of a control group. Since all the residents in attendance received the same clinical vignettes, it would have been of interest to see how the risk assessment tool performed compared with residents who did not have access to the tool. However, based on average noon conference attendance, it would have been difficult to achieve an adequate number of observations to calculate credible ICC and kappa scores. Other limitations include the high number of interns who completed the vignettes compared with senior residents, and the lack of additional attending reviewers to score the vignettes prior to the session. Ideally, in determining the accuracy of protocol adherence, we would have compared residents' determinations with those of several experts who had used an adjudication process in the event of disagreement. In our ongoing work, we are collecting data from a representative sample of attending physicians at our hospital to compare their assessments both with each other and with those of the residents.
Another issue in our design was that the study presented only a limited amount of medical information in the vignettes. In actual clinical circumstances, the amount of historical information is greater and more complicated. One could argue that the artificiality of clinical vignettes is not an accurate representation of resident performance when ordering VTE prophylaxis. However, this approach limits case‐mix variation, so residents should have been able to reach similar conclusions with the information given. Thus the limited information should have maximized residents' intentions to prescribe VTE prophylaxis, and kappa scores would likely be lower in real clinical settings. Finally, our kappa scores were calculated based on aggregate data of interns and residents; however, interns comprised almost two‐thirds of the resident participants. As reported in the results section, intern inter‐rater reliability was slightly lower compared with the senior resident subgroup, suggesting that the variability may be a result of less clinical experience of the interns. However, the study was not powered to assess differences in kappa scores for level of training.
In conclusion, we determined the inter‐rater reliability of an individualized, point‐based VTE risk assessment tool when used by medical residents unfamiliar with its use. Our study showed that under conditions of minimal education, a point‐based VTE assessment tool achieves only fair to moderate reliability. It also suggests that as a stand‐alone tool without a reminder alert, adherence to VTE prevention guidelines is suboptimal and might result in underprophylaxis of hospitalized medical patients at moderate or high VTE risk. In fact, with appropriate prophylaxis, rates were maximally estimated to be 55% (Table 2). Because of the high percentage of interns in the study, these results approximate intern application of a VTE prevention protocol independent of other interventions. Comparing reliability data from our study with those of others raises the question of whether the observed differences in kappa score are because other studies used highly trained observers or because their protocols were less complex. However, a recent study validated a simpler method of VTE risk grouping that performs well regardless of clinical experience.20 Future studies are needed to determine whether there is improved resident inter‐rater reliability using a point‐based risk assessment tool that is embedded into a computerized order entry system with electronic reminder alerts. Finally, in actual clinical settings, the question remains of whether kappa scores correlate with protocol adherence, prophylaxis rates, and VTE reduction when using point‐based tools. If not, then the use of simplified risk‐stratification tools and VTE measure‐vention strategies should be implemented.
Acknowledgements
The authors thank Lisabeth V. Scalzi, MD, MS, Lora Moyer, Kevin McKenna MD, Hammid Al‐Mondhiry, Lucille Anderson, MD, Kathleen Williams, Kevin Larraway, Cynthia Chuang, MD, MS, the residents of the Internal Medicine and Combined Medicine/Pediatrics residencies, and the division of General Internal Medicine at Hershey Medical Center.
- ,,.Autopsy‐verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988.Br J Surg.1991;78(7):849–852.
- , , , , et al.Fatal pulmonary embolism in hospitalised patients: a necropsy review.J Clin Pathol.2004;57(12):1254–1257.
- , , , et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):381S–453S.
- ,.Coronary artery vasculitis and myocardial infarction with systemic lupus erythematosus.NY State J Med.1974;74(5):873–874.
- , , , et al.Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism.Chest.2007;132(3):936–945.
- , , , et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross‐sectional study.Lancet.2008;371(9610):387–394.
- , , , .Venous thromboembolic events in hospitalised medical patients.Thromb Haemost.2009;102(3):505–510.
- ,,.Compliance with recommended prophylaxis for venous thromboembolism: improving the use and rate of uptake of clinical practice guidelines.J Thromb Haemost.2004;2(2):221–227.
- , , , et al.A systematic review of strategies to improve prophylaxis for venous thromboembolism in hospitals.Ann Surg.2005;241(3):397–415.
- ,.Prevention of venous thromboembolism: consensus, controversies, and challenges.Hematol Am Soc Hematol Educ Program.2009:286–292.
- ,,.International perspective on venous thromboembolism prophylaxis in surgery.Semin Thromb Hemost.1991;17(4):322–325.
- , , , et al.Clinical assessment of venous thromboembolic risk in surgical patients.Semin Thromb Hemost.1991;17(suppl 3):304–312.
- , et al.Risk factor assessment in the management of patients with suspected deep venous thrombosis.Int Angiol.2000;19(1):47–51.
- ,,.Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease.Semin Hematol.2001;38(2 suppl 5):12–19.
- .Thrombosis risk assessment as a guide to quality patient care.Dis Mon.2005;51(2–3):70–78.
- ,.Designing and implementing effective venous thromboembolism prevention protocols: lessons from collaborative efforts.J Thromb Thrombolysis.2010;29(2):159–166.
- ,,.Emergency medicine practitioner knowledge and use of decision rules for the evaluation of patients with suspected pulmonary embolism: variations by practice setting and training level.Acad Emerg Med.2007;14(1):53–57.
- , , , , , , , .Optimizing prevention of hospital‐acquired (HA) venous thromboembolism (VTE): prospective validation of a VTE risk assessment model (RAM).J Hosp Med.2010;5(1):10–18..
- , , , et al.Development and testing of a DVT risk assessment tool: providing evidence of validity and reliability.Worldviews Evid Based Nurs.2007;4(1):14–20.
- , , , et al.A novel educational strategy to enhance internal medicine residents' familial colorectal cancer knowledge and risk assessment skills.Am J Gastroenterol.2005;100(3):677–684.
- ,, , , , .Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- , , , et al.Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality.JAMA.2000;283(13):1715–1722.
- .Psychometric Theory.New Delhi:Tate McGraw‐Hill;1981.
- ,.Intraclass correlations: uses in assessing rater reliability.Psychol Bull.1979;86(2):420–428.
- ,,.Innovative approaches to increase deep vein thrombosis prophylaxis rate resulting in a decrease in hospital‐acquired deep vein thrombosis at a tertiary‐care teaching hospital.J Hosp Med.2008;3(2):148–155.
- ,,.Improved use of thromboprophylaxis for deep vein thrombosis following an educational intervention.J Hosp Med.2006;1(6):331–338.
- , , , et al.Minimizing errors of omission: behavioural reenforcement of heparin to avert venous emboli: the BEHAVE study.Crit Care Med.2006;34(3):694–699.
- , , , et al.Electronic alerts to prevent venous thromboembolism among hospitalized patients.N Engl J Med.2005;352(10):969–977.
- , , , .Getting a validated guideline into local practice: implementation and audit of the SIGN guideline on the prevention of deep vein thrombosis in a district general hospital.Scott Med J.1998;43(1):23–25.
- ,,. Improving the Reliability of Health Care. IHI Innovation Series white paper 2004. Available at: www.IHI.org/IHI/Results/WhitePapers/Improving theReliabilityof HealthCare.htm. Accessed October 4,2010.
- , , , et al.Thrombosis prophylaxis in medical patients: a retrospective review of clinical practice patterns.Haematologica.2002;87(7):746–750; discussion 250.
- ,.Genetic epidemiology: systemic lupus erythematosus.Arthritis Res.2001;3(6):331–336.
- ,,.Missed opportunities for prevention of venous thromboembolism: an evaluation of the use of thromboprophylaxis guidelines.Chest.2001;120(6):1964–1971.
- , , , , .Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting.Arch Intern Med.1998;158(17):1909–1912.
- ,,.Venous thromboembolism prophylaxis used by consultant general surgeons in Scotland.J R Coll Surg Edinb.2001;46(6):329–333.
- ,.Ordering errors by first‐year residents: evidence of learning from mistakes.Mo Med.2004;101(2):128–131.
- ,.Prevention of medication errors: teaching and training.Br J Clin Pharmacol.2009;67(6):656–661.
- ,,.Reducing medication errors in a surgical residency training program.Am Surg.2004;70(5):467–471.
- , , , et al.Why don't physicians follow clinical practice guidelines? A framework for improvement.JAMA.1999;282(15):1458–1465.
- , , , , .Predicting computerized physician order entry system adoption in US hospitals: can the federal mandate be met?Int J Med Inform.2008;77(8):539–545.
- ,.Implementation of computerized physician order entry in seven countries.Health Aff (Millwood).2009;28(2):404–414.
- ,,.Autopsy‐verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988.Br J Surg.1991;78(7):849–852.
- , , , , et al.Fatal pulmonary embolism in hospitalised patients: a necropsy review.J Clin Pathol.2004;57(12):1254–1257.
- , , , et al.Prevention of venous thromboembolism: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines (8th edition).Chest.2008;133(6 suppl):381S–453S.
- ,.Coronary artery vasculitis and myocardial infarction with systemic lupus erythematosus.NY State J Med.1974;74(5):873–874.
- , , , et al.Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the International Medical Prevention Registry on Venous Thromboembolism.Chest.2007;132(3):936–945.
- , , , et al.Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross‐sectional study.Lancet.2008;371(9610):387–394.
- , , , .Venous thromboembolic events in hospitalised medical patients.Thromb Haemost.2009;102(3):505–510.
- ,,.Compliance with recommended prophylaxis for venous thromboembolism: improving the use and rate of uptake of clinical practice guidelines.J Thromb Haemost.2004;2(2):221–227.
- , , , et al.A systematic review of strategies to improve prophylaxis for venous thromboembolism in hospitals.Ann Surg.2005;241(3):397–415.
- ,.Prevention of venous thromboembolism: consensus, controversies, and challenges.Hematol Am Soc Hematol Educ Program.2009:286–292.
- ,,.International perspective on venous thromboembolism prophylaxis in surgery.Semin Thromb Hemost.1991;17(4):322–325.
- , , , et al.Clinical assessment of venous thromboembolic risk in surgical patients.Semin Thromb Hemost.1991;17(suppl 3):304–312.
- , et al.Risk factor assessment in the management of patients with suspected deep venous thrombosis.Int Angiol.2000;19(1):47–51.
- ,,.Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease.Semin Hematol.2001;38(2 suppl 5):12–19.
- .Thrombosis risk assessment as a guide to quality patient care.Dis Mon.2005;51(2–3):70–78.
- ,.Designing and implementing effective venous thromboembolism prevention protocols: lessons from collaborative efforts.J Thromb Thrombolysis.2010;29(2):159–166.
- ,,.Emergency medicine practitioner knowledge and use of decision rules for the evaluation of patients with suspected pulmonary embolism: variations by practice setting and training level.Acad Emerg Med.2007;14(1):53–57.
- , , , , , , , .Optimizing prevention of hospital‐acquired (HA) venous thromboembolism (VTE): prospective validation of a VTE risk assessment model (RAM).J Hosp Med.2010;5(1):10–18..
- , , , et al.Development and testing of a DVT risk assessment tool: providing evidence of validity and reliability.Worldviews Evid Based Nurs.2007;4(1):14–20.
- , , , et al.A novel educational strategy to enhance internal medicine residents' familial colorectal cancer knowledge and risk assessment skills.Am J Gastroenterol.2005;100(3):677–684.
- ,, , , , .Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- , , , et al.Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality.JAMA.2000;283(13):1715–1722.
- .Psychometric Theory.New Delhi:Tate McGraw‐Hill;1981.
- ,.Intraclass correlations: uses in assessing rater reliability.Psychol Bull.1979;86(2):420–428.
- ,,.Innovative approaches to increase deep vein thrombosis prophylaxis rate resulting in a decrease in hospital‐acquired deep vein thrombosis at a tertiary‐care teaching hospital.J Hosp Med.2008;3(2):148–155.
- ,,.Improved use of thromboprophylaxis for deep vein thrombosis following an educational intervention.J Hosp Med.2006;1(6):331–338.
- , , , et al.Minimizing errors of omission: behavioural reenforcement of heparin to avert venous emboli: the BEHAVE study.Crit Care Med.2006;34(3):694–699.
- , , , et al.Electronic alerts to prevent venous thromboembolism among hospitalized patients.N Engl J Med.2005;352(10):969–977.
- , , , .Getting a validated guideline into local practice: implementation and audit of the SIGN guideline on the prevention of deep vein thrombosis in a district general hospital.Scott Med J.1998;43(1):23–25.
- ,,. Improving the Reliability of Health Care. IHI Innovation Series white paper 2004. Available at: www.IHI.org/IHI/Results/WhitePapers/Improving theReliabilityof HealthCare.htm. Accessed October 4,2010.
- , , , et al.Thrombosis prophylaxis in medical patients: a retrospective review of clinical practice patterns.Haematologica.2002;87(7):746–750; discussion 250.
- ,.Genetic epidemiology: systemic lupus erythematosus.Arthritis Res.2001;3(6):331–336.
- ,,.Missed opportunities for prevention of venous thromboembolism: an evaluation of the use of thromboprophylaxis guidelines.Chest.2001;120(6):1964–1971.
- , , , , .Underuse of venous thromboembolism prophylaxis for general surgery patients: physician practices in the community hospital setting.Arch Intern Med.1998;158(17):1909–1912.
- ,,.Venous thromboembolism prophylaxis used by consultant general surgeons in Scotland.J R Coll Surg Edinb.2001;46(6):329–333.
- ,.Ordering errors by first‐year residents: evidence of learning from mistakes.Mo Med.2004;101(2):128–131.
- ,.Prevention of medication errors: teaching and training.Br J Clin Pharmacol.2009;67(6):656–661.
- ,,.Reducing medication errors in a surgical residency training program.Am Surg.2004;70(5):467–471.
- , , , et al.Why don't physicians follow clinical practice guidelines? A framework for improvement.JAMA.1999;282(15):1458–1465.
- , , , , .Predicting computerized physician order entry system adoption in US hospitals: can the federal mandate be met?Int J Med Inform.2008;77(8):539–545.
- ,.Implementation of computerized physician order entry in seven countries.Health Aff (Millwood).2009;28(2):404–414.
Copyright © 2011 Society of Hospital Medicine