User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Strength of fibromyalgia as marker for seizures questioned
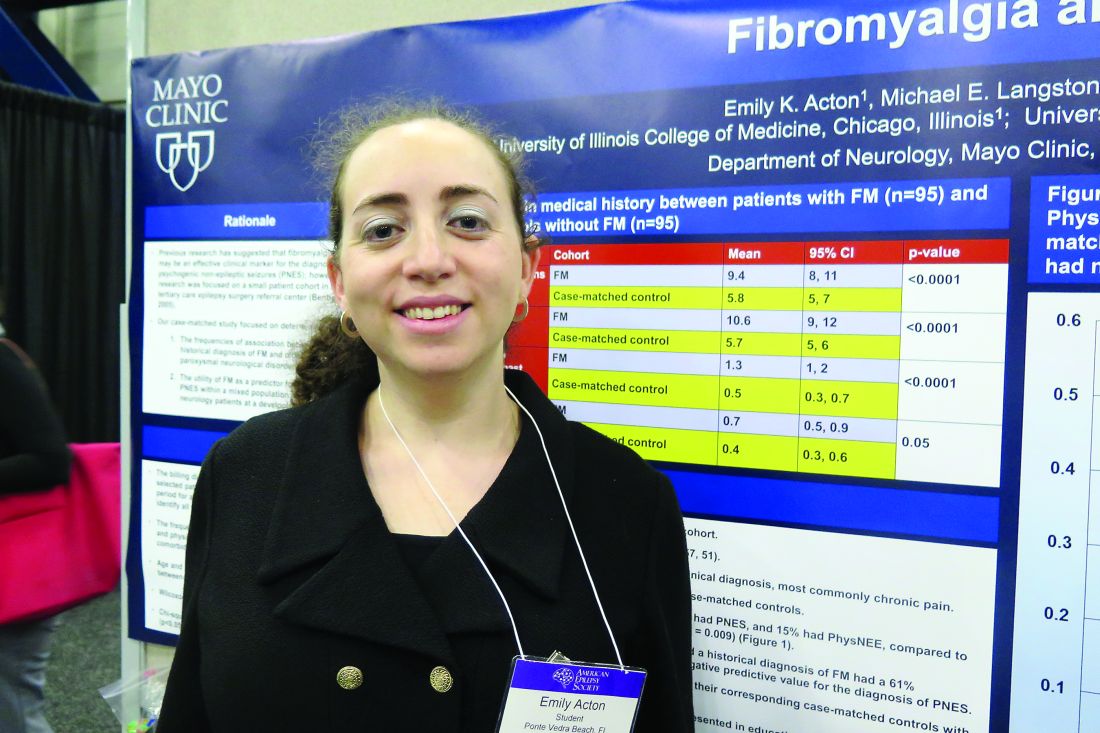
HOUSTON – The specificity of fibromyalgia as a marker for psychogenic nonepileptic seizures is less reliable than previously described, results from a large analysis showed.
“Fibromyalgia has been referred to as a reliable clinical indicator for differentiating psychogenic nonepileptic seizures from epilepsy, but there hasn’t been a lot of research looking into this idea,” Emily K. Acton said in an interview at the annual meeting of the American Epilepsy Society. In fact, the most recent study to investigate the association focused on a small patient cohort in a tertiary care epilepsy referral center and found that a diagnosis of fibromyalgia had a predictive value of 75% and a specificity of 99% for the diagnosis of psychogenic nonepileptic seizures (Epilepsy Behav. 2005; 6[2]:264-5).
Ms. Acton reported that of the 1,730 patients studied, 95 (5.5%) had a medical history of fibromyalgia. A majority of the 95 patients (95%) were female, and the mean age was 53 years. In addition, 43% of fibromyalgia patients had a nonparoxysmal, neurologic primary clinical diagnosis, most commonly chronic pain. She said that no differences were seen between fibromyalgia patients and case-matched controls in terms of age, race, marital status, or reason for referral. However, compared with case-matched controls, fibromyalgia patients were underrepresented in education (P = .02) and employment (P = .009).
Paroxysmal events were present in 57% of fibromyalgia patients and in 54% of case-matched controls. Among fibromyalgia patients with paroxysmal disorders, 11% had epileptic seizures, 74% had PNES, and 15% had physiologic nonepileptic events. Among matched controls, 37% had epileptic seizures, 51% had PNES, and 12% had physiologic nonepileptic events (P = .009).
After comparing the two groups of patients, the researchers determined that a historical diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, 74% positive predictive value, and 49% negative predictive value for the diagnosis of PNES. “Another interesting finding was that quite a few of our fibromyalgia patients felt they didn’t have fibromyalgia,” Ms. Action said. “Unprompted, during the course of their first visit, about 10% of this cohort mentioned to a physician that they were diagnosed with fibromyalgia, but they didn’t believe it.”
In their abstract, the researchers wrote that the study design “and a larger sample size involving mixed general neurology patients may account for the lesser association seen between fibromyalgia and PNES in this study.” They reported having no financial disclosures.
HOUSTON – The specificity of fibromyalgia as a marker for psychogenic nonepileptic seizures is less reliable than previously described, results from a large analysis showed.
“Fibromyalgia has been referred to as a reliable clinical indicator for differentiating psychogenic nonepileptic seizures from epilepsy, but there hasn’t been a lot of research looking into this idea,” Emily K. Acton said in an interview at the annual meeting of the American Epilepsy Society. In fact, the most recent study to investigate the association focused on a small patient cohort in a tertiary care epilepsy referral center and found that a diagnosis of fibromyalgia had a predictive value of 75% and a specificity of 99% for the diagnosis of psychogenic nonepileptic seizures (Epilepsy Behav. 2005; 6[2]:264-5).
Ms. Acton reported that of the 1,730 patients studied, 95 (5.5%) had a medical history of fibromyalgia. A majority of the 95 patients (95%) were female, and the mean age was 53 years. In addition, 43% of fibromyalgia patients had a nonparoxysmal, neurologic primary clinical diagnosis, most commonly chronic pain. She said that no differences were seen between fibromyalgia patients and case-matched controls in terms of age, race, marital status, or reason for referral. However, compared with case-matched controls, fibromyalgia patients were underrepresented in education (P = .02) and employment (P = .009).
Paroxysmal events were present in 57% of fibromyalgia patients and in 54% of case-matched controls. Among fibromyalgia patients with paroxysmal disorders, 11% had epileptic seizures, 74% had PNES, and 15% had physiologic nonepileptic events. Among matched controls, 37% had epileptic seizures, 51% had PNES, and 12% had physiologic nonepileptic events (P = .009).
After comparing the two groups of patients, the researchers determined that a historical diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, 74% positive predictive value, and 49% negative predictive value for the diagnosis of PNES. “Another interesting finding was that quite a few of our fibromyalgia patients felt they didn’t have fibromyalgia,” Ms. Action said. “Unprompted, during the course of their first visit, about 10% of this cohort mentioned to a physician that they were diagnosed with fibromyalgia, but they didn’t believe it.”
In their abstract, the researchers wrote that the study design “and a larger sample size involving mixed general neurology patients may account for the lesser association seen between fibromyalgia and PNES in this study.” They reported having no financial disclosures.
HOUSTON – The specificity of fibromyalgia as a marker for psychogenic nonepileptic seizures is less reliable than previously described, results from a large analysis showed.
“Fibromyalgia has been referred to as a reliable clinical indicator for differentiating psychogenic nonepileptic seizures from epilepsy, but there hasn’t been a lot of research looking into this idea,” Emily K. Acton said in an interview at the annual meeting of the American Epilepsy Society. In fact, the most recent study to investigate the association focused on a small patient cohort in a tertiary care epilepsy referral center and found that a diagnosis of fibromyalgia had a predictive value of 75% and a specificity of 99% for the diagnosis of psychogenic nonepileptic seizures (Epilepsy Behav. 2005; 6[2]:264-5).
Ms. Acton reported that of the 1,730 patients studied, 95 (5.5%) had a medical history of fibromyalgia. A majority of the 95 patients (95%) were female, and the mean age was 53 years. In addition, 43% of fibromyalgia patients had a nonparoxysmal, neurologic primary clinical diagnosis, most commonly chronic pain. She said that no differences were seen between fibromyalgia patients and case-matched controls in terms of age, race, marital status, or reason for referral. However, compared with case-matched controls, fibromyalgia patients were underrepresented in education (P = .02) and employment (P = .009).
Paroxysmal events were present in 57% of fibromyalgia patients and in 54% of case-matched controls. Among fibromyalgia patients with paroxysmal disorders, 11% had epileptic seizures, 74% had PNES, and 15% had physiologic nonepileptic events. Among matched controls, 37% had epileptic seizures, 51% had PNES, and 12% had physiologic nonepileptic events (P = .009).
After comparing the two groups of patients, the researchers determined that a historical diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, 74% positive predictive value, and 49% negative predictive value for the diagnosis of PNES. “Another interesting finding was that quite a few of our fibromyalgia patients felt they didn’t have fibromyalgia,” Ms. Action said. “Unprompted, during the course of their first visit, about 10% of this cohort mentioned to a physician that they were diagnosed with fibromyalgia, but they didn’t believe it.”
In their abstract, the researchers wrote that the study design “and a larger sample size involving mixed general neurology patients may account for the lesser association seen between fibromyalgia and PNES in this study.” They reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: The diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, and a 74% positive predictive value for the diagnosis of PNES.
Data source: A retrospective review of 1,730 consecutive patients seen by a single epileptologist at a neurology clinic over a 3-year period.
Disclosures: The researchers reported having no financial disclosures.
Selected elderly trauma patients do well in non–ICU wards
CORONADO, CALIF. – When elderly patients are appropriately triaged, they can be selectively admitted to non–intensive care wards with acceptable outcomes, results from a single-center study showed.
“Trauma centers across the United States are caring for elderly trauma patients with greater frequency,” researchers led by Marc D. Trust, MD, wrote in an abstract presented during a poster session at the annual meeting of the Western Surgical Association.
“Previous literature showed improved outcomes in this population from aggressive care and invasive monitoring. This may have led to an increased utilization of intensive care resources for these patients,” they noted.
In an effort to assess the safety of admitting this population of patients to non–intensive care units, Dr. Trust, a surgery resident at the University of Texas at Austin, and his associates retrospectively reviewed the medical records of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015. They compared demographic data and outcomes between patients admitted to the ICU and those admitted to the surgical ward. The primary endpoint was mortality, while secondary endpoints were transfer to higher level of care and hospital length of stay. Patients admitted only for comfort care and those with injuries thought to be terminal and irreversible were excluded from the analysis.
The mean age of the 3,682 patients was 76 years and 1,838 (50%) were admitted to the ICU, while the remaining 1,844 (50%) were admitted to the surgical ward. When the researchers compared patients admitted to the ICU with those admitted to the surgical ward, they observed significant differences in mortality (7% vs. 0.82%, respectively; P less than .001), as well as systolic blood pressure on admission (146 vs. 149 mm Hg, respectively; P = .0002), pulse (85 vs. 81 beats per minute; P less than .0001), Glasgow Coma Scale (14 vs. 15; P less than .001), Injury Severity Score (16 vs. 8; P less than .001), and hospital stay (a mean of 8 vs. 4 days; P less than .0001). In addition, fewer than 1% of patients admitted to the surgical ward required transfer to a higher level of care (P less than .0001).
Next, Dr. Trust and his associates conducted a subgroup analysis of 300 patients admitted to the ICU (28%) and 766 (72%) admitted to the surgical ward who had all-system Abbreviated Injury Scale scores of less than 3, no hypotension on admission, and a Glasgow Coma Scale of 14 or greater. Compared with those admitted to the surgical ward, those admitted to the ICU were older (77 vs. 76 years old, respectively; P = .003), more likely to be male (54% vs. 45%; P = .007), more tachycardic (HR 84 vs. 81; P = .004), more severely injured (ISS score of 5 vs. 4; P less than .0001), and more likely to have a longer hospital stay (a mean of 6 vs. 4 days; P less than .0001). Two patients admitted to the surgical ward died (0.26%; P = .0009) and none required transfer to a higher level of care.
The researchers reported having no financial disclosures.
CORONADO, CALIF. – When elderly patients are appropriately triaged, they can be selectively admitted to non–intensive care wards with acceptable outcomes, results from a single-center study showed.
“Trauma centers across the United States are caring for elderly trauma patients with greater frequency,” researchers led by Marc D. Trust, MD, wrote in an abstract presented during a poster session at the annual meeting of the Western Surgical Association.
“Previous literature showed improved outcomes in this population from aggressive care and invasive monitoring. This may have led to an increased utilization of intensive care resources for these patients,” they noted.
In an effort to assess the safety of admitting this population of patients to non–intensive care units, Dr. Trust, a surgery resident at the University of Texas at Austin, and his associates retrospectively reviewed the medical records of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015. They compared demographic data and outcomes between patients admitted to the ICU and those admitted to the surgical ward. The primary endpoint was mortality, while secondary endpoints were transfer to higher level of care and hospital length of stay. Patients admitted only for comfort care and those with injuries thought to be terminal and irreversible were excluded from the analysis.
The mean age of the 3,682 patients was 76 years and 1,838 (50%) were admitted to the ICU, while the remaining 1,844 (50%) were admitted to the surgical ward. When the researchers compared patients admitted to the ICU with those admitted to the surgical ward, they observed significant differences in mortality (7% vs. 0.82%, respectively; P less than .001), as well as systolic blood pressure on admission (146 vs. 149 mm Hg, respectively; P = .0002), pulse (85 vs. 81 beats per minute; P less than .0001), Glasgow Coma Scale (14 vs. 15; P less than .001), Injury Severity Score (16 vs. 8; P less than .001), and hospital stay (a mean of 8 vs. 4 days; P less than .0001). In addition, fewer than 1% of patients admitted to the surgical ward required transfer to a higher level of care (P less than .0001).
Next, Dr. Trust and his associates conducted a subgroup analysis of 300 patients admitted to the ICU (28%) and 766 (72%) admitted to the surgical ward who had all-system Abbreviated Injury Scale scores of less than 3, no hypotension on admission, and a Glasgow Coma Scale of 14 or greater. Compared with those admitted to the surgical ward, those admitted to the ICU were older (77 vs. 76 years old, respectively; P = .003), more likely to be male (54% vs. 45%; P = .007), more tachycardic (HR 84 vs. 81; P = .004), more severely injured (ISS score of 5 vs. 4; P less than .0001), and more likely to have a longer hospital stay (a mean of 6 vs. 4 days; P less than .0001). Two patients admitted to the surgical ward died (0.26%; P = .0009) and none required transfer to a higher level of care.
The researchers reported having no financial disclosures.
CORONADO, CALIF. – When elderly patients are appropriately triaged, they can be selectively admitted to non–intensive care wards with acceptable outcomes, results from a single-center study showed.
“Trauma centers across the United States are caring for elderly trauma patients with greater frequency,” researchers led by Marc D. Trust, MD, wrote in an abstract presented during a poster session at the annual meeting of the Western Surgical Association.
“Previous literature showed improved outcomes in this population from aggressive care and invasive monitoring. This may have led to an increased utilization of intensive care resources for these patients,” they noted.
In an effort to assess the safety of admitting this population of patients to non–intensive care units, Dr. Trust, a surgery resident at the University of Texas at Austin, and his associates retrospectively reviewed the medical records of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015. They compared demographic data and outcomes between patients admitted to the ICU and those admitted to the surgical ward. The primary endpoint was mortality, while secondary endpoints were transfer to higher level of care and hospital length of stay. Patients admitted only for comfort care and those with injuries thought to be terminal and irreversible were excluded from the analysis.
The mean age of the 3,682 patients was 76 years and 1,838 (50%) were admitted to the ICU, while the remaining 1,844 (50%) were admitted to the surgical ward. When the researchers compared patients admitted to the ICU with those admitted to the surgical ward, they observed significant differences in mortality (7% vs. 0.82%, respectively; P less than .001), as well as systolic blood pressure on admission (146 vs. 149 mm Hg, respectively; P = .0002), pulse (85 vs. 81 beats per minute; P less than .0001), Glasgow Coma Scale (14 vs. 15; P less than .001), Injury Severity Score (16 vs. 8; P less than .001), and hospital stay (a mean of 8 vs. 4 days; P less than .0001). In addition, fewer than 1% of patients admitted to the surgical ward required transfer to a higher level of care (P less than .0001).
Next, Dr. Trust and his associates conducted a subgroup analysis of 300 patients admitted to the ICU (28%) and 766 (72%) admitted to the surgical ward who had all-system Abbreviated Injury Scale scores of less than 3, no hypotension on admission, and a Glasgow Coma Scale of 14 or greater. Compared with those admitted to the surgical ward, those admitted to the ICU were older (77 vs. 76 years old, respectively; P = .003), more likely to be male (54% vs. 45%; P = .007), more tachycardic (HR 84 vs. 81; P = .004), more severely injured (ISS score of 5 vs. 4; P less than .0001), and more likely to have a longer hospital stay (a mean of 6 vs. 4 days; P less than .0001). Two patients admitted to the surgical ward died (0.26%; P = .0009) and none required transfer to a higher level of care.
The researchers reported having no financial disclosures.
AT WSA 2016
Key clinical point:
Major finding: Mortality rates were significantly higher among elderly trauma patients admitted to the ICU, compared with those admitted to the surgical ward (7% vs. 0.82%, respectively; P less than .001).
Data source: A retrospective review of 3,682 trauma patients aged 65 and older who were admitted from 2006 to 2015.
Disclosures: The researchers reported having no financial disclosures.
Aspirin use linked to increased ICH in trauma patients
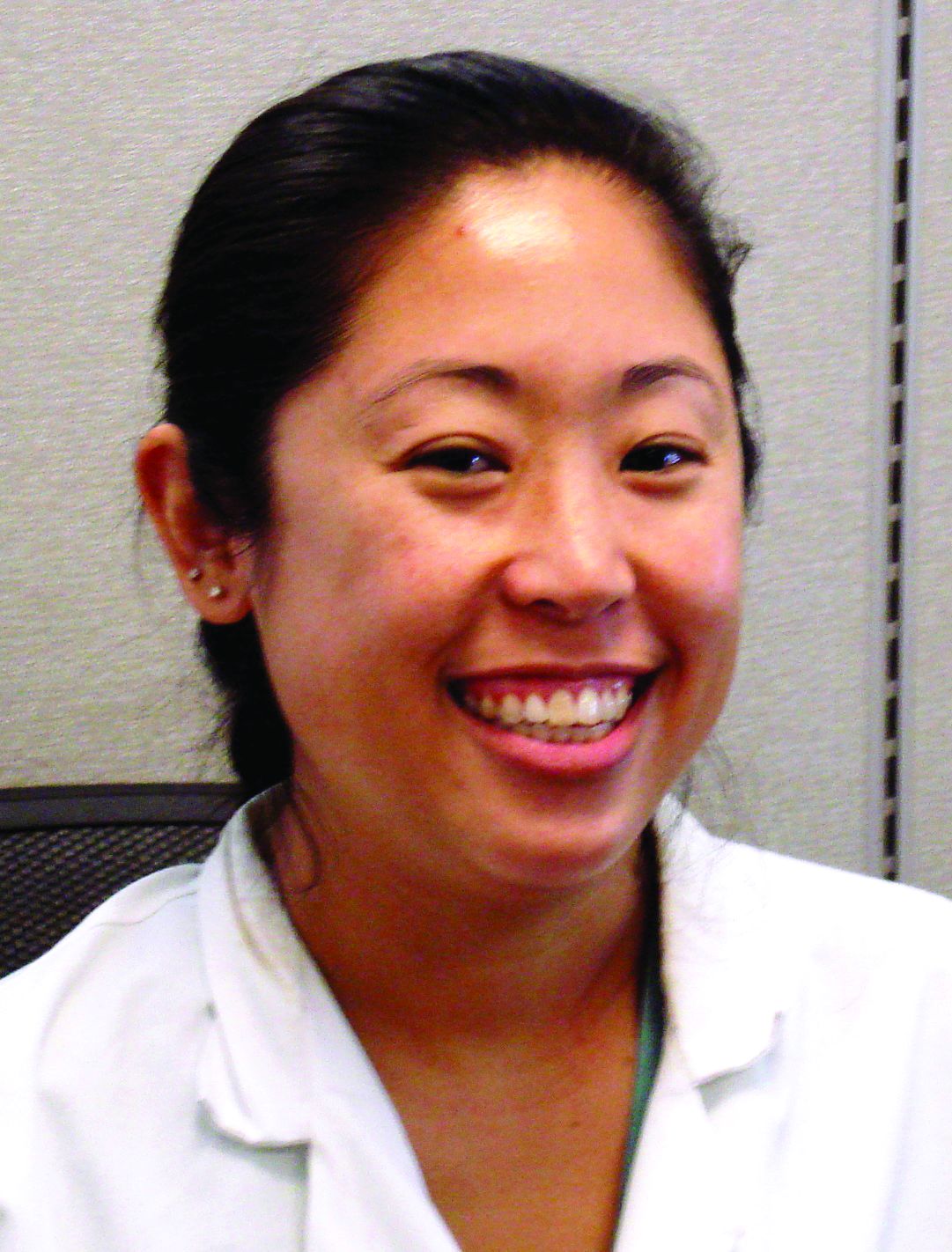
WAIKOLOA, HAWAII – Among a group of anticoagulated trauma patients, those on aspirin had the highest rate and risk of intracranial hemorrhage (ICH), while those on novel oral anticoagulants were not at higher risk for ICH, ICH progression, or death, a multicenter study found.
“The number of patients on warfarin and antiplatelet agents has significantly increased over time,” Leslie Kobayashi, MD, said at the annual meeting of the American Association for the Surgery of Trauma. “These oral antithrombotic agents have been associated with poor outcomes following traumatic injury, including increased rates of intracranial hemorrhage, increased progression of intracranial hemorrhage, and increased mortality.”
In a prospective, multicenter observational study conducted by the AAST’s Multi-institutional Trials Committee, Dr. Kobayashi and her associates set out identify injury patterns and outcomes in trauma patients taking the NOAs, and to test their hypothesis that patients taking NOAs would have higher rates of ICH, ICH progression, and death, compared with patients taking traditional oral anticoagulant therapies (OATs). Patients were included if they were admitted to the trauma service on warfarin, aspirin, clopidogrel, dabigatran, apixaban, or rivaroxaban. Pregnant patients, prisoners, and minors were excluded from the study. Data collected included demographics, mechanism of injury, vitals on admission, injuries/injury severity scores, labs, interventions, and reversal agents used such as vitamin K, prothrombin complexes, dialysis, and transfusion of fresh frozen plasma (FFP). Outcomes studied included ICH, ICH progression, and death.
In all, 16 Level 1 trauma centers enrolled 1,847 patients over a 2-year period. Their average age was 75 years, 46% were female, 77% were white, their median Injury Severity Score (ISS) was 9, and 99% sustained a blunt mechanism of trauma. The top two causes of injury were falls (71%) and motor vehicle crashes (15%). One-third of patients (33%) were on warfarin, while the remainder were on aspirin (26%), clopidogrel (24%), NOAs (10%), and 7% took multiple or other agents.
The mechanism of injury pattern was similar between patients taking NOAs and those taking OATs, with the exception of patients on aspirin being significantly less likely to have sustained a fall. Patients on aspirin also had a significantly higher median ISS. “Patients on NOAs presented more frequently in shock as defined by a systolic blood pressure of less than 90 mmHg, but this was not associated with increased need for packed red blood cell transfusion, bleeding requiring an intervention, need for surgical procedure, hospital LOS, complications, or death,” Dr. Kobayashi said.
About 30% of all patients studied underwent an attempt at reversal. The types of agents used to reverse the patients differed depending on drug agent, with antiplatelet patients more frequently getting platelets, and patients on warfarin more frequently receiving FFP, vitamin K, and prothrombin complex. “Interestingly, patients on the anti-Xa inhibitors more frequently received prothrombin complex as well,” she said. “This likely reflects some of the recent literature which suggests that there may be a therapeutic benefit to using prothrombin complex in patients taking the oral anti-Xa inhibitors but not in patients on dabigatran.”
Overall, bleeding, need for surgical procedure, need for neurosurgical procedure, complications, length of stay, and death were similar between those on NOAs and those on OATs. However, the rate of ICH was significantly higher in patients on aspirin. “What is even more surprising is that 89% of the patients in the aspirin-only group were on an 81-mg baby aspirin rather than the larger 325-mg dose,” Dr. Kobayashi said. This difference was significant on univariate analysis and was retained after multivariate logistic regression adjusted for differences between populations, with an OR for aspirin of 1.7 and a P value of .024. “This is not to suggest that patients on aspirin are doing markedly worse, compared to their counterparts, but I think most of us would have assumed that aspirin patients would have done better,” she commented. “I think we’ve definitively shown that is not the case.” Other independent predictors of ICH were advanced age (OR, 1.02), Asian race (OR, 3.1), ISS of 10 or greater (OR, 2.2), and a Glasgow coma score (GCS) of 8 or less (OR, 5.6).
Despite their increased risk for ICH, patients on aspirin were significantly less likely to undergo an attempt at reversal with any type of agent, at 16% with a P value of less than .001, on univariate analysis. “This was significantly lower than all other medications and was retained after multivariate logistic regression, with an OR of 0.3 and a P value of less than .001,” she said.
Progression of ICH did not differ by medication group. Other independent predictors included intraparenchymal location of hemorrhage (OR, 2.2), need for a neurosurgical procedure (OR, 5.1), an attempt at reversal (OR, 2.3) and a GCS of 8 or lower at admission (OR, 4.3). Similarly, multivariate analysis of death showed no significant differences between the different medication groups. Independent predictors included advanced age (OR, 1.06), GCS of 8 or less (OR, 13), progression of head injury (OR, 10), bleeding (OR, 2.3), and complications (OR, 2.1).
Dr. Kobayashi acknowledged that the study’s observational design is a limitation, as well as the fact that it lacked a control group of age-matched patients who were not taking anticoagulants. “Additionally, we had a relatively low number of patients on NOAs, at only 10% of the study population,” she said. “Lastly, there is potential for enrollment bias as all sites involved in this study were level one trauma centers.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Among a group of anticoagulated trauma patients, those on aspirin had the highest rate and risk of intracranial hemorrhage (ICH), while those on novel oral anticoagulants were not at higher risk for ICH, ICH progression, or death, a multicenter study found.
“The number of patients on warfarin and antiplatelet agents has significantly increased over time,” Leslie Kobayashi, MD, said at the annual meeting of the American Association for the Surgery of Trauma. “These oral antithrombotic agents have been associated with poor outcomes following traumatic injury, including increased rates of intracranial hemorrhage, increased progression of intracranial hemorrhage, and increased mortality.”
In a prospective, multicenter observational study conducted by the AAST’s Multi-institutional Trials Committee, Dr. Kobayashi and her associates set out identify injury patterns and outcomes in trauma patients taking the NOAs, and to test their hypothesis that patients taking NOAs would have higher rates of ICH, ICH progression, and death, compared with patients taking traditional oral anticoagulant therapies (OATs). Patients were included if they were admitted to the trauma service on warfarin, aspirin, clopidogrel, dabigatran, apixaban, or rivaroxaban. Pregnant patients, prisoners, and minors were excluded from the study. Data collected included demographics, mechanism of injury, vitals on admission, injuries/injury severity scores, labs, interventions, and reversal agents used such as vitamin K, prothrombin complexes, dialysis, and transfusion of fresh frozen plasma (FFP). Outcomes studied included ICH, ICH progression, and death.
In all, 16 Level 1 trauma centers enrolled 1,847 patients over a 2-year period. Their average age was 75 years, 46% were female, 77% were white, their median Injury Severity Score (ISS) was 9, and 99% sustained a blunt mechanism of trauma. The top two causes of injury were falls (71%) and motor vehicle crashes (15%). One-third of patients (33%) were on warfarin, while the remainder were on aspirin (26%), clopidogrel (24%), NOAs (10%), and 7% took multiple or other agents.
The mechanism of injury pattern was similar between patients taking NOAs and those taking OATs, with the exception of patients on aspirin being significantly less likely to have sustained a fall. Patients on aspirin also had a significantly higher median ISS. “Patients on NOAs presented more frequently in shock as defined by a systolic blood pressure of less than 90 mmHg, but this was not associated with increased need for packed red blood cell transfusion, bleeding requiring an intervention, need for surgical procedure, hospital LOS, complications, or death,” Dr. Kobayashi said.
About 30% of all patients studied underwent an attempt at reversal. The types of agents used to reverse the patients differed depending on drug agent, with antiplatelet patients more frequently getting platelets, and patients on warfarin more frequently receiving FFP, vitamin K, and prothrombin complex. “Interestingly, patients on the anti-Xa inhibitors more frequently received prothrombin complex as well,” she said. “This likely reflects some of the recent literature which suggests that there may be a therapeutic benefit to using prothrombin complex in patients taking the oral anti-Xa inhibitors but not in patients on dabigatran.”
Overall, bleeding, need for surgical procedure, need for neurosurgical procedure, complications, length of stay, and death were similar between those on NOAs and those on OATs. However, the rate of ICH was significantly higher in patients on aspirin. “What is even more surprising is that 89% of the patients in the aspirin-only group were on an 81-mg baby aspirin rather than the larger 325-mg dose,” Dr. Kobayashi said. This difference was significant on univariate analysis and was retained after multivariate logistic regression adjusted for differences between populations, with an OR for aspirin of 1.7 and a P value of .024. “This is not to suggest that patients on aspirin are doing markedly worse, compared to their counterparts, but I think most of us would have assumed that aspirin patients would have done better,” she commented. “I think we’ve definitively shown that is not the case.” Other independent predictors of ICH were advanced age (OR, 1.02), Asian race (OR, 3.1), ISS of 10 or greater (OR, 2.2), and a Glasgow coma score (GCS) of 8 or less (OR, 5.6).
Despite their increased risk for ICH, patients on aspirin were significantly less likely to undergo an attempt at reversal with any type of agent, at 16% with a P value of less than .001, on univariate analysis. “This was significantly lower than all other medications and was retained after multivariate logistic regression, with an OR of 0.3 and a P value of less than .001,” she said.
Progression of ICH did not differ by medication group. Other independent predictors included intraparenchymal location of hemorrhage (OR, 2.2), need for a neurosurgical procedure (OR, 5.1), an attempt at reversal (OR, 2.3) and a GCS of 8 or lower at admission (OR, 4.3). Similarly, multivariate analysis of death showed no significant differences between the different medication groups. Independent predictors included advanced age (OR, 1.06), GCS of 8 or less (OR, 13), progression of head injury (OR, 10), bleeding (OR, 2.3), and complications (OR, 2.1).
Dr. Kobayashi acknowledged that the study’s observational design is a limitation, as well as the fact that it lacked a control group of age-matched patients who were not taking anticoagulants. “Additionally, we had a relatively low number of patients on NOAs, at only 10% of the study population,” she said. “Lastly, there is potential for enrollment bias as all sites involved in this study were level one trauma centers.” She reported having no financial disclosures.
WAIKOLOA, HAWAII – Among a group of anticoagulated trauma patients, those on aspirin had the highest rate and risk of intracranial hemorrhage (ICH), while those on novel oral anticoagulants were not at higher risk for ICH, ICH progression, or death, a multicenter study found.
“The number of patients on warfarin and antiplatelet agents has significantly increased over time,” Leslie Kobayashi, MD, said at the annual meeting of the American Association for the Surgery of Trauma. “These oral antithrombotic agents have been associated with poor outcomes following traumatic injury, including increased rates of intracranial hemorrhage, increased progression of intracranial hemorrhage, and increased mortality.”
In a prospective, multicenter observational study conducted by the AAST’s Multi-institutional Trials Committee, Dr. Kobayashi and her associates set out identify injury patterns and outcomes in trauma patients taking the NOAs, and to test their hypothesis that patients taking NOAs would have higher rates of ICH, ICH progression, and death, compared with patients taking traditional oral anticoagulant therapies (OATs). Patients were included if they were admitted to the trauma service on warfarin, aspirin, clopidogrel, dabigatran, apixaban, or rivaroxaban. Pregnant patients, prisoners, and minors were excluded from the study. Data collected included demographics, mechanism of injury, vitals on admission, injuries/injury severity scores, labs, interventions, and reversal agents used such as vitamin K, prothrombin complexes, dialysis, and transfusion of fresh frozen plasma (FFP). Outcomes studied included ICH, ICH progression, and death.
In all, 16 Level 1 trauma centers enrolled 1,847 patients over a 2-year period. Their average age was 75 years, 46% were female, 77% were white, their median Injury Severity Score (ISS) was 9, and 99% sustained a blunt mechanism of trauma. The top two causes of injury were falls (71%) and motor vehicle crashes (15%). One-third of patients (33%) were on warfarin, while the remainder were on aspirin (26%), clopidogrel (24%), NOAs (10%), and 7% took multiple or other agents.
The mechanism of injury pattern was similar between patients taking NOAs and those taking OATs, with the exception of patients on aspirin being significantly less likely to have sustained a fall. Patients on aspirin also had a significantly higher median ISS. “Patients on NOAs presented more frequently in shock as defined by a systolic blood pressure of less than 90 mmHg, but this was not associated with increased need for packed red blood cell transfusion, bleeding requiring an intervention, need for surgical procedure, hospital LOS, complications, or death,” Dr. Kobayashi said.
About 30% of all patients studied underwent an attempt at reversal. The types of agents used to reverse the patients differed depending on drug agent, with antiplatelet patients more frequently getting platelets, and patients on warfarin more frequently receiving FFP, vitamin K, and prothrombin complex. “Interestingly, patients on the anti-Xa inhibitors more frequently received prothrombin complex as well,” she said. “This likely reflects some of the recent literature which suggests that there may be a therapeutic benefit to using prothrombin complex in patients taking the oral anti-Xa inhibitors but not in patients on dabigatran.”
Overall, bleeding, need for surgical procedure, need for neurosurgical procedure, complications, length of stay, and death were similar between those on NOAs and those on OATs. However, the rate of ICH was significantly higher in patients on aspirin. “What is even more surprising is that 89% of the patients in the aspirin-only group were on an 81-mg baby aspirin rather than the larger 325-mg dose,” Dr. Kobayashi said. This difference was significant on univariate analysis and was retained after multivariate logistic regression adjusted for differences between populations, with an OR for aspirin of 1.7 and a P value of .024. “This is not to suggest that patients on aspirin are doing markedly worse, compared to their counterparts, but I think most of us would have assumed that aspirin patients would have done better,” she commented. “I think we’ve definitively shown that is not the case.” Other independent predictors of ICH were advanced age (OR, 1.02), Asian race (OR, 3.1), ISS of 10 or greater (OR, 2.2), and a Glasgow coma score (GCS) of 8 or less (OR, 5.6).
Despite their increased risk for ICH, patients on aspirin were significantly less likely to undergo an attempt at reversal with any type of agent, at 16% with a P value of less than .001, on univariate analysis. “This was significantly lower than all other medications and was retained after multivariate logistic regression, with an OR of 0.3 and a P value of less than .001,” she said.
Progression of ICH did not differ by medication group. Other independent predictors included intraparenchymal location of hemorrhage (OR, 2.2), need for a neurosurgical procedure (OR, 5.1), an attempt at reversal (OR, 2.3) and a GCS of 8 or lower at admission (OR, 4.3). Similarly, multivariate analysis of death showed no significant differences between the different medication groups. Independent predictors included advanced age (OR, 1.06), GCS of 8 or less (OR, 13), progression of head injury (OR, 10), bleeding (OR, 2.3), and complications (OR, 2.1).
Dr. Kobayashi acknowledged that the study’s observational design is a limitation, as well as the fact that it lacked a control group of age-matched patients who were not taking anticoagulants. “Additionally, we had a relatively low number of patients on NOAs, at only 10% of the study population,” she said. “Lastly, there is potential for enrollment bias as all sites involved in this study were level one trauma centers.” She reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point:
Major finding: The rate of ICH was significantly higher in patients on aspirin, compared with those on novel oral anticoagulant therapies (OR, 1.7; P = .024).
Data source: A prospective evaluation of 1,847 patients treated at 16 level one trauma centers over a 2-year period.
Disclosures: Dr. Kobayashi reported having no financial disclosures.
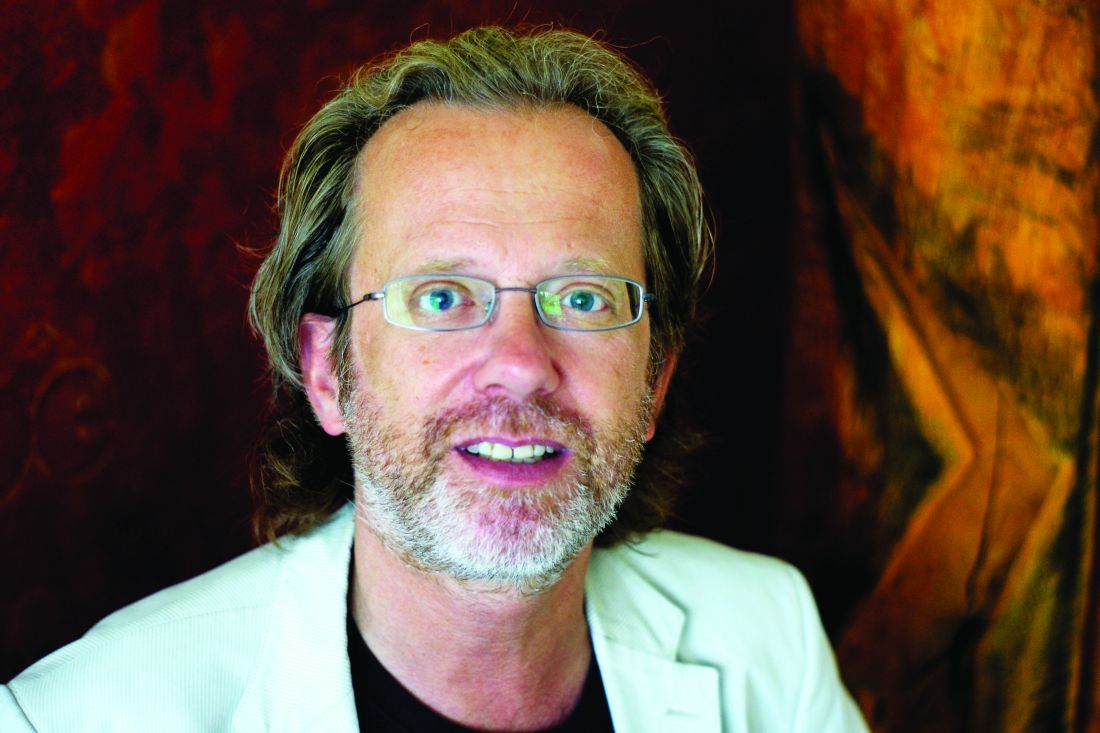
Few drug-resistant epilepsy patients recruitable for trials of new AEDs
HOUSTON – Fewer than 8% of adult patients with drug-resistant epilepsy would have been recruitable for recent phase II and III trials of new antiepileptic drugs (AEDs), results from a single-center study showed.
The findings underscore a need to rethink how phase II and III trials of AEDs are conducted, Bernhard J. Steinhoff, MD, said in an interview prior to the annual meeting of the American Epilepsy Society. “In spite of the marketing of numerous new antiepileptic drugs, the percentage of drug-resistant epilepsies has remained almost unchanged,” said Dr. Steinhoff of the Kork (Germany) Epilepsy Center. “I am not aware that anybody involved in the issue of clinical trials with AEDs addressed the problem [of] whether the pivotal trials really cover the patients the new AEDs are developed for: namely, patients with drug-resistant epilepsies. Every time we start with a new drug after licensing, we realize that we have no clue whether this drug will be appropriate for our difficult-to-treat patients. We wondered whether the design of the usual phase II and III randomized controlled trials covers an acceptable percentage of AED-resistant epilepsy patients.”
“The result was frightening because less than 10% [of patients] would have been covered by the trials,” Dr. Steinhoff said. “Therefore, we suggest that a bad trials strategy may be responsible for the fact that the percentage of drug-resistant patients has not been markedly reduced by more than 15 new AEDs that were introduced during the recent years.” He added that pivotal trials with new AEDs “show superiority over placebo as add-on in an extremely limited group of difficult-to-treat patients. After licensing and marketing, we start to learn whether a new AED is appropriate for our drug-resistant patients.”
Medical writing was funded by an unrestricted grant from UCB. Dr. Steinhoff reported having no financial conflicts.
HOUSTON – Fewer than 8% of adult patients with drug-resistant epilepsy would have been recruitable for recent phase II and III trials of new antiepileptic drugs (AEDs), results from a single-center study showed.
The findings underscore a need to rethink how phase II and III trials of AEDs are conducted, Bernhard J. Steinhoff, MD, said in an interview prior to the annual meeting of the American Epilepsy Society. “In spite of the marketing of numerous new antiepileptic drugs, the percentage of drug-resistant epilepsies has remained almost unchanged,” said Dr. Steinhoff of the Kork (Germany) Epilepsy Center. “I am not aware that anybody involved in the issue of clinical trials with AEDs addressed the problem [of] whether the pivotal trials really cover the patients the new AEDs are developed for: namely, patients with drug-resistant epilepsies. Every time we start with a new drug after licensing, we realize that we have no clue whether this drug will be appropriate for our difficult-to-treat patients. We wondered whether the design of the usual phase II and III randomized controlled trials covers an acceptable percentage of AED-resistant epilepsy patients.”
“The result was frightening because less than 10% [of patients] would have been covered by the trials,” Dr. Steinhoff said. “Therefore, we suggest that a bad trials strategy may be responsible for the fact that the percentage of drug-resistant patients has not been markedly reduced by more than 15 new AEDs that were introduced during the recent years.” He added that pivotal trials with new AEDs “show superiority over placebo as add-on in an extremely limited group of difficult-to-treat patients. After licensing and marketing, we start to learn whether a new AED is appropriate for our drug-resistant patients.”
Medical writing was funded by an unrestricted grant from UCB. Dr. Steinhoff reported having no financial conflicts.
HOUSTON – Fewer than 8% of adult patients with drug-resistant epilepsy would have been recruitable for recent phase II and III trials of new antiepileptic drugs (AEDs), results from a single-center study showed.
The findings underscore a need to rethink how phase II and III trials of AEDs are conducted, Bernhard J. Steinhoff, MD, said in an interview prior to the annual meeting of the American Epilepsy Society. “In spite of the marketing of numerous new antiepileptic drugs, the percentage of drug-resistant epilepsies has remained almost unchanged,” said Dr. Steinhoff of the Kork (Germany) Epilepsy Center. “I am not aware that anybody involved in the issue of clinical trials with AEDs addressed the problem [of] whether the pivotal trials really cover the patients the new AEDs are developed for: namely, patients with drug-resistant epilepsies. Every time we start with a new drug after licensing, we realize that we have no clue whether this drug will be appropriate for our difficult-to-treat patients. We wondered whether the design of the usual phase II and III randomized controlled trials covers an acceptable percentage of AED-resistant epilepsy patients.”
“The result was frightening because less than 10% [of patients] would have been covered by the trials,” Dr. Steinhoff said. “Therefore, we suggest that a bad trials strategy may be responsible for the fact that the percentage of drug-resistant patients has not been markedly reduced by more than 15 new AEDs that were introduced during the recent years.” He added that pivotal trials with new AEDs “show superiority over placebo as add-on in an extremely limited group of difficult-to-treat patients. After licensing and marketing, we start to learn whether a new AED is appropriate for our drug-resistant patients.”
Medical writing was funded by an unrestricted grant from UCB. Dr. Steinhoff reported having no financial conflicts.
AT AES 2016
Key clinical point:
Major finding: Only 7.4% of patients would have fulfilled the inclusion criteria of five phase II and III trials of new AEDs.
Data source: A review of 216 outpatients with drug-resistant epilepsies.
Disclosures: Medical writing was funded by an unrestricted grant from UCB. Dr. Steinhoff reported having no financial disclosures.
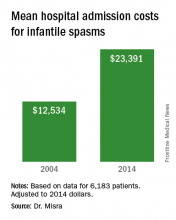
Wide variation seen in treatment of infantile spasms
HOUSTON – The types of diagnostic tests ordered and medication used for treatment of infantile spasms vary considerably, a large study of children’s hospitals showed.
“Children with infantile spasms often require extensive diagnostic work-up to determine etiology, expensive medications for treatment, and hospitalization during the initiation of certain therapies,” researchers led by Sunita N. Misra, MD, PhD, wrote in an abstract presented at the annual meeting of the American Epilepsy Society. “The common diagnostic studies and therapies have evolved over the last several decades.”
The researchers collected patient demographics, hospital length of stay, hospital admission cost, use of various diagnostic studies (such as lumbar puncture, brain MRI, and EEG), and medications used for infantile spasms (including antiepileptic drugs, corticotropin, and steroids). Cost data, calculated as a ratio of cost to charges, were collected and adjusted to 2014 dollars.
A total of 6,183 patients were included in the analysis and their average age of infantile-spasm diagnosis was 9 months. The most common diagnostic test ordered was EEG (76%), followed by brain imaging (57%), organic acids (38%), and lumbar puncture (17%). Medications were started during inpatient hospitalization in two-thirds of patients, with 33% starting on corticotropin; 29% on topiramate; and fewer than 10% of patients on an oral or intravenous steroid, zonisamide, or vigabatrin (Sabril). Use of corticotropin decreased over time, while use of oral steroids trended upwards. “We were surprised that one-third of patients did not have a medication initiated as an inpatient, given the studies showing earlier use of effective therapy has better outcomes,” Dr. Misra said in an interview in advance of the meeting.
“The cost of taking care of children with infantile spasms has increased over the study period 2004-2014,” Dr. Misra said. “Although we identified a few contributors to rising cost, there are probably other factors that need to be considered in future studies.” She acknowledged certain limitations of the analysis, including its retrospective design and the fact that it only identified cost associated with the initial admission. “Several of the diagnostic studies and medications may be initiated as an outpatient, for which we do not have the data,” she said.
Dr. Misra reported having no financial disclosures.
HOUSTON – The types of diagnostic tests ordered and medication used for treatment of infantile spasms vary considerably, a large study of children’s hospitals showed.
“Children with infantile spasms often require extensive diagnostic work-up to determine etiology, expensive medications for treatment, and hospitalization during the initiation of certain therapies,” researchers led by Sunita N. Misra, MD, PhD, wrote in an abstract presented at the annual meeting of the American Epilepsy Society. “The common diagnostic studies and therapies have evolved over the last several decades.”
The researchers collected patient demographics, hospital length of stay, hospital admission cost, use of various diagnostic studies (such as lumbar puncture, brain MRI, and EEG), and medications used for infantile spasms (including antiepileptic drugs, corticotropin, and steroids). Cost data, calculated as a ratio of cost to charges, were collected and adjusted to 2014 dollars.
A total of 6,183 patients were included in the analysis and their average age of infantile-spasm diagnosis was 9 months. The most common diagnostic test ordered was EEG (76%), followed by brain imaging (57%), organic acids (38%), and lumbar puncture (17%). Medications were started during inpatient hospitalization in two-thirds of patients, with 33% starting on corticotropin; 29% on topiramate; and fewer than 10% of patients on an oral or intravenous steroid, zonisamide, or vigabatrin (Sabril). Use of corticotropin decreased over time, while use of oral steroids trended upwards. “We were surprised that one-third of patients did not have a medication initiated as an inpatient, given the studies showing earlier use of effective therapy has better outcomes,” Dr. Misra said in an interview in advance of the meeting.
“The cost of taking care of children with infantile spasms has increased over the study period 2004-2014,” Dr. Misra said. “Although we identified a few contributors to rising cost, there are probably other factors that need to be considered in future studies.” She acknowledged certain limitations of the analysis, including its retrospective design and the fact that it only identified cost associated with the initial admission. “Several of the diagnostic studies and medications may be initiated as an outpatient, for which we do not have the data,” she said.
Dr. Misra reported having no financial disclosures.
HOUSTON – The types of diagnostic tests ordered and medication used for treatment of infantile spasms vary considerably, a large study of children’s hospitals showed.
“Children with infantile spasms often require extensive diagnostic work-up to determine etiology, expensive medications for treatment, and hospitalization during the initiation of certain therapies,” researchers led by Sunita N. Misra, MD, PhD, wrote in an abstract presented at the annual meeting of the American Epilepsy Society. “The common diagnostic studies and therapies have evolved over the last several decades.”
The researchers collected patient demographics, hospital length of stay, hospital admission cost, use of various diagnostic studies (such as lumbar puncture, brain MRI, and EEG), and medications used for infantile spasms (including antiepileptic drugs, corticotropin, and steroids). Cost data, calculated as a ratio of cost to charges, were collected and adjusted to 2014 dollars.
A total of 6,183 patients were included in the analysis and their average age of infantile-spasm diagnosis was 9 months. The most common diagnostic test ordered was EEG (76%), followed by brain imaging (57%), organic acids (38%), and lumbar puncture (17%). Medications were started during inpatient hospitalization in two-thirds of patients, with 33% starting on corticotropin; 29% on topiramate; and fewer than 10% of patients on an oral or intravenous steroid, zonisamide, or vigabatrin (Sabril). Use of corticotropin decreased over time, while use of oral steroids trended upwards. “We were surprised that one-third of patients did not have a medication initiated as an inpatient, given the studies showing earlier use of effective therapy has better outcomes,” Dr. Misra said in an interview in advance of the meeting.
“The cost of taking care of children with infantile spasms has increased over the study period 2004-2014,” Dr. Misra said. “Although we identified a few contributors to rising cost, there are probably other factors that need to be considered in future studies.” She acknowledged certain limitations of the analysis, including its retrospective design and the fact that it only identified cost associated with the initial admission. “Several of the diagnostic studies and medications may be initiated as an outpatient, for which we do not have the data,” she said.
Dr. Misra reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: The most common diagnostic test ordered was EEG (76%), followed by brain imaging (57%), organic acids (38%), and lumbar puncture (17%).
Data source: Retrospective analysis of data on 6,183 patients with infantile spasms between 2004 and 2014.
Disclosures: Dr. Misra reported having no financial disclosures.
Wrist-worn system detected convulsive seizures in home setting
HOUSTON – A wrist-worn device and smartphone-based alert system worn by a patient outside of the epilepsy monitoring unit for 3 months effectively detected convulsive seizure events and minimized false alarms, results from a long-term study found.
The automated device, known as Embrace, relies on an accelerometer and electrodermal activity to detect convulsive seizures. It pairs a wrist-worn device with a smartphone-based application that provides an alert to designated caregivers when an unusual event is detected. Embrace, which is being developed by Empatica Inc., received clearance by the European Union as a medical device for convulsive seizure detection but is still under consideration by the Food and Drug Administration. Previous reports evaluating the automated detector used by Embrace have always relied on data from epilepsy monitoring units (EMUs), where it achieved sensitivity scores ranging from 92% to 100% and 0.15-2.02 false alarms per day in detecting convulsive seizures.
To find out, Dr. Picard, chief scientist at Empatica, and her associates conducted a case study of a 14-year-old patient with Dravet syndrome who was enrolled in a trial of Embrace in the outpatient setting. No data from this patient were used in training the system. The patient’s caregiver was asked to annotate the occurrence of each convulsive seizure and any activity that generated an alert. The number of false alerts was obtained by subtracting the number of correctly recognized convulsive seizures from the total alerts fired by the device. Sensitivity was the percentage of convulsive seizures that automatically triggered an alert.
“Embrace can work for patients outside the EMU, detecting events and issuing alerts through a paired smartphone to a designated caregiver. Also, for clinicians who understand machine learning, we should be clear that we used the strongest test possible: none of the patient’s data were used to train the algorithm that was used, nor was it tuned in any way special for this patient. Had we done so, the results could have possibly appeared even better. However, we chose to use this test of generalization to better get a sense of how it might work on new patients, whose data had never been seen before.”
Dr. Picard acknowledged certain limitations of the study, including the fact that it was a single case and that the patient had Dravet syndrome. She disclosed that she is a cofounder of Empatica and owns shares in the company.
HOUSTON – A wrist-worn device and smartphone-based alert system worn by a patient outside of the epilepsy monitoring unit for 3 months effectively detected convulsive seizure events and minimized false alarms, results from a long-term study found.
The automated device, known as Embrace, relies on an accelerometer and electrodermal activity to detect convulsive seizures. It pairs a wrist-worn device with a smartphone-based application that provides an alert to designated caregivers when an unusual event is detected. Embrace, which is being developed by Empatica Inc., received clearance by the European Union as a medical device for convulsive seizure detection but is still under consideration by the Food and Drug Administration. Previous reports evaluating the automated detector used by Embrace have always relied on data from epilepsy monitoring units (EMUs), where it achieved sensitivity scores ranging from 92% to 100% and 0.15-2.02 false alarms per day in detecting convulsive seizures.
To find out, Dr. Picard, chief scientist at Empatica, and her associates conducted a case study of a 14-year-old patient with Dravet syndrome who was enrolled in a trial of Embrace in the outpatient setting. No data from this patient were used in training the system. The patient’s caregiver was asked to annotate the occurrence of each convulsive seizure and any activity that generated an alert. The number of false alerts was obtained by subtracting the number of correctly recognized convulsive seizures from the total alerts fired by the device. Sensitivity was the percentage of convulsive seizures that automatically triggered an alert.
“Embrace can work for patients outside the EMU, detecting events and issuing alerts through a paired smartphone to a designated caregiver. Also, for clinicians who understand machine learning, we should be clear that we used the strongest test possible: none of the patient’s data were used to train the algorithm that was used, nor was it tuned in any way special for this patient. Had we done so, the results could have possibly appeared even better. However, we chose to use this test of generalization to better get a sense of how it might work on new patients, whose data had never been seen before.”
Dr. Picard acknowledged certain limitations of the study, including the fact that it was a single case and that the patient had Dravet syndrome. She disclosed that she is a cofounder of Empatica and owns shares in the company.
HOUSTON – A wrist-worn device and smartphone-based alert system worn by a patient outside of the epilepsy monitoring unit for 3 months effectively detected convulsive seizure events and minimized false alarms, results from a long-term study found.
The automated device, known as Embrace, relies on an accelerometer and electrodermal activity to detect convulsive seizures. It pairs a wrist-worn device with a smartphone-based application that provides an alert to designated caregivers when an unusual event is detected. Embrace, which is being developed by Empatica Inc., received clearance by the European Union as a medical device for convulsive seizure detection but is still under consideration by the Food and Drug Administration. Previous reports evaluating the automated detector used by Embrace have always relied on data from epilepsy monitoring units (EMUs), where it achieved sensitivity scores ranging from 92% to 100% and 0.15-2.02 false alarms per day in detecting convulsive seizures.
To find out, Dr. Picard, chief scientist at Empatica, and her associates conducted a case study of a 14-year-old patient with Dravet syndrome who was enrolled in a trial of Embrace in the outpatient setting. No data from this patient were used in training the system. The patient’s caregiver was asked to annotate the occurrence of each convulsive seizure and any activity that generated an alert. The number of false alerts was obtained by subtracting the number of correctly recognized convulsive seizures from the total alerts fired by the device. Sensitivity was the percentage of convulsive seizures that automatically triggered an alert.
“Embrace can work for patients outside the EMU, detecting events and issuing alerts through a paired smartphone to a designated caregiver. Also, for clinicians who understand machine learning, we should be clear that we used the strongest test possible: none of the patient’s data were used to train the algorithm that was used, nor was it tuned in any way special for this patient. Had we done so, the results could have possibly appeared even better. However, we chose to use this test of generalization to better get a sense of how it might work on new patients, whose data had never been seen before.”
Dr. Picard acknowledged certain limitations of the study, including the fact that it was a single case and that the patient had Dravet syndrome. She disclosed that she is a cofounder of Empatica and owns shares in the company.
AT AES 2016
Key clinical point:
Major finding: A device known as Embrace detected 22 of the patient’s 24 convulsive seizure events, for a sensitivity of 92% and a false-alarm rate of 0.35 false alarms per day worn.
Data source: Case study of a 14-year-old patient with Dravet syndrome who was enrolled in a trial of Embrace in the outpatient setting and used the device for 113 days.
Disclosures: Dr. Picard is a cofounder of Empatica. She also owns shares in the company.
Rate of mosaicism in parents of children with epileptic encephalopathy likely underestimated
HOUSTON – The rate of parental mosaicism in children with sporadic cases of epileptic encephalopathy and an apparent de novo mutation is believed to be at least 10%, which is much higher than previously thought.
The discovery, which was revealed with advanced genetic testing methods, underscores the need to rethink how parents of children with epileptic encephalopathy are counseled with regard to family planning, lead study author Candace T. Myers, PhD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “Generally, families are counseled with a recurrence risk of 1%-3%, but we found that in 10% of our families their recurrence risk is much higher because we’re able to see the genetic mutation in either blood or saliva of an unaffected parent,” said Dr. Myers of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle. “If we’re able to detect it in either of those tissues that means that the level in their gametes is much higher than just a single cell or a handful of cells, which is usually how people think about de novo mutations. What we’re finding is that in 10% of cases these mutations happen during embryonic development of the parent.”
Dr. Myers reported that of the 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers. The fraction of mutant alleles identified ranged from 3%-25%, which are levels that would pass undetected by traditional Sanger sequencing methods. In three families where a mosaic parent was identified, there were multiple affected children. The finding “opens up more questions for families that are thinking about future pregnancies,” she said. “I think we should have more genetic counselors working with pediatric neurologists to facilitate those discussions.”
She acknowledged certain limitations of the study, including the fact that DNA samples were extracted only from blood and saliva. “If the mutation is not present or detected in those particular tissues, it is still possible for the parent to be a germline carrier,” Dr. Myers said. “The most relevant tissue type for us to be testing would be the sex cells. We’ll have to look for families to see if they’re willing to donate [those cells] for future studies.”
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
HOUSTON – The rate of parental mosaicism in children with sporadic cases of epileptic encephalopathy and an apparent de novo mutation is believed to be at least 10%, which is much higher than previously thought.
The discovery, which was revealed with advanced genetic testing methods, underscores the need to rethink how parents of children with epileptic encephalopathy are counseled with regard to family planning, lead study author Candace T. Myers, PhD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “Generally, families are counseled with a recurrence risk of 1%-3%, but we found that in 10% of our families their recurrence risk is much higher because we’re able to see the genetic mutation in either blood or saliva of an unaffected parent,” said Dr. Myers of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle. “If we’re able to detect it in either of those tissues that means that the level in their gametes is much higher than just a single cell or a handful of cells, which is usually how people think about de novo mutations. What we’re finding is that in 10% of cases these mutations happen during embryonic development of the parent.”
Dr. Myers reported that of the 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers. The fraction of mutant alleles identified ranged from 3%-25%, which are levels that would pass undetected by traditional Sanger sequencing methods. In three families where a mosaic parent was identified, there were multiple affected children. The finding “opens up more questions for families that are thinking about future pregnancies,” she said. “I think we should have more genetic counselors working with pediatric neurologists to facilitate those discussions.”
She acknowledged certain limitations of the study, including the fact that DNA samples were extracted only from blood and saliva. “If the mutation is not present or detected in those particular tissues, it is still possible for the parent to be a germline carrier,” Dr. Myers said. “The most relevant tissue type for us to be testing would be the sex cells. We’ll have to look for families to see if they’re willing to donate [those cells] for future studies.”
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
HOUSTON – The rate of parental mosaicism in children with sporadic cases of epileptic encephalopathy and an apparent de novo mutation is believed to be at least 10%, which is much higher than previously thought.
The discovery, which was revealed with advanced genetic testing methods, underscores the need to rethink how parents of children with epileptic encephalopathy are counseled with regard to family planning, lead study author Candace T. Myers, PhD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “Generally, families are counseled with a recurrence risk of 1%-3%, but we found that in 10% of our families their recurrence risk is much higher because we’re able to see the genetic mutation in either blood or saliva of an unaffected parent,” said Dr. Myers of the division of genetic medicine in the department of pediatrics at the University of Washington, Seattle. “If we’re able to detect it in either of those tissues that means that the level in their gametes is much higher than just a single cell or a handful of cells, which is usually how people think about de novo mutations. What we’re finding is that in 10% of cases these mutations happen during embryonic development of the parent.”
Dr. Myers reported that of the 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers. The fraction of mutant alleles identified ranged from 3%-25%, which are levels that would pass undetected by traditional Sanger sequencing methods. In three families where a mosaic parent was identified, there were multiple affected children. The finding “opens up more questions for families that are thinking about future pregnancies,” she said. “I think we should have more genetic counselors working with pediatric neurologists to facilitate those discussions.”
She acknowledged certain limitations of the study, including the fact that DNA samples were extracted only from blood and saliva. “If the mutation is not present or detected in those particular tissues, it is still possible for the parent to be a germline carrier,” Dr. Myers said. “The most relevant tissue type for us to be testing would be the sex cells. We’ll have to look for families to see if they’re willing to donate [those cells] for future studies.”
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: Of 109 families screened, 10 cases of low-level somatic mosaicism were identified: 6 in fathers and 4 in mothers.
Data source: Screening of 109 families where the affected child’s epileptic encephalopathy was attributed to a substitution or small indel in 1 of 31 established epilepsy genes and reported as “de novo” by either clinical or research analysis of parental DNA.
Disclosures: The study was funded by National Institute of Neurological Disorders and Stroke. Dr. Myers is supported by a postdoctoral fellowship provided by the Lennox-Gastaut Syndrome Foundation and by the American Epilepsy Society. She reported having no financial disclosures.
Survey sheds light on clinical neurophysiology fellowship training
HOUSTON – Fellowship training in clinical neurophysiology delivered high rates of satisfaction, but recommended areas for improvements include more focus on training in sleep, brain mapping, and evoked potentials, results from a survey of current trainees found.
“There has been no systematic evaluation of neurophysiology fellowships,” Zulfi Haneef, MD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “In fact, there are some studies on neurology residency, but not on any of the neurology fellowships. This study opens a window into what the situation is after residency: what makes the residents decide on a fellowship, and how they feel they have done with the choice of fellowship.”
Overall, 87% of respondents expressed satisfaction with their current program and rated it as 4 or a 5 on a 1-5 Likert scale. “It seems that choosing a program based on the location may not have been the best thing to do,” he said. “Satisfaction scores (on a 1-5 scale for the training) were lower among those who chose a program based on location.” Less time spent in the epilepsy monitoring unit and EEG monitoring was also associated with higher satisfaction scores. “Rather than a lack of interest in epilepsy monitoring and EEG, this may reflect overemphasis on these at the expense of other areas, as these were also the areas that appeared to be most stressed during training,” Dr. Haneef said. The researchers observed no differences between male and female respondents in their answers to the various survey questions.
Based on the survey results, better clinical neurophysiology training in some areas were deemed necessary by the responding fellows, including sleep, brain mapping, and evoked potentials. Dr. Haneef acknowledged certain limitations of the study, including the fact that it was voluntary. “As such there could be some self-selection of fellows who have stronger viewpoints that pushed them to respond to a survey,” he said. He reported having no financial disclosures related to the study.
HOUSTON – Fellowship training in clinical neurophysiology delivered high rates of satisfaction, but recommended areas for improvements include more focus on training in sleep, brain mapping, and evoked potentials, results from a survey of current trainees found.
“There has been no systematic evaluation of neurophysiology fellowships,” Zulfi Haneef, MD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “In fact, there are some studies on neurology residency, but not on any of the neurology fellowships. This study opens a window into what the situation is after residency: what makes the residents decide on a fellowship, and how they feel they have done with the choice of fellowship.”
Overall, 87% of respondents expressed satisfaction with their current program and rated it as 4 or a 5 on a 1-5 Likert scale. “It seems that choosing a program based on the location may not have been the best thing to do,” he said. “Satisfaction scores (on a 1-5 scale for the training) were lower among those who chose a program based on location.” Less time spent in the epilepsy monitoring unit and EEG monitoring was also associated with higher satisfaction scores. “Rather than a lack of interest in epilepsy monitoring and EEG, this may reflect overemphasis on these at the expense of other areas, as these were also the areas that appeared to be most stressed during training,” Dr. Haneef said. The researchers observed no differences between male and female respondents in their answers to the various survey questions.
Based on the survey results, better clinical neurophysiology training in some areas were deemed necessary by the responding fellows, including sleep, brain mapping, and evoked potentials. Dr. Haneef acknowledged certain limitations of the study, including the fact that it was voluntary. “As such there could be some self-selection of fellows who have stronger viewpoints that pushed them to respond to a survey,” he said. He reported having no financial disclosures related to the study.
HOUSTON – Fellowship training in clinical neurophysiology delivered high rates of satisfaction, but recommended areas for improvements include more focus on training in sleep, brain mapping, and evoked potentials, results from a survey of current trainees found.
“There has been no systematic evaluation of neurophysiology fellowships,” Zulfi Haneef, MD, said in an interview in advance of the annual meeting of the American Epilepsy Society. “In fact, there are some studies on neurology residency, but not on any of the neurology fellowships. This study opens a window into what the situation is after residency: what makes the residents decide on a fellowship, and how they feel they have done with the choice of fellowship.”
Overall, 87% of respondents expressed satisfaction with their current program and rated it as 4 or a 5 on a 1-5 Likert scale. “It seems that choosing a program based on the location may not have been the best thing to do,” he said. “Satisfaction scores (on a 1-5 scale for the training) were lower among those who chose a program based on location.” Less time spent in the epilepsy monitoring unit and EEG monitoring was also associated with higher satisfaction scores. “Rather than a lack of interest in epilepsy monitoring and EEG, this may reflect overemphasis on these at the expense of other areas, as these were also the areas that appeared to be most stressed during training,” Dr. Haneef said. The researchers observed no differences between male and female respondents in their answers to the various survey questions.
Based on the survey results, better clinical neurophysiology training in some areas were deemed necessary by the responding fellows, including sleep, brain mapping, and evoked potentials. Dr. Haneef acknowledged certain limitations of the study, including the fact that it was voluntary. “As such there could be some self-selection of fellows who have stronger viewpoints that pushed them to respond to a survey,” he said. He reported having no financial disclosures related to the study.
AT AES 2016
Key clinical point:
Major finding: Overall, 87% of clinical neurophysiology fellows expressed satisfaction with their current program and rated it as 4 or a 5 on a 1-5 Likert scale.
Data source: An Internet-based survey of 49 clinical neurophysiology fellows in the United States.
Disclosures: Dr. Haneef reported having no financial disclosures related to the study.
Study shows NJ tube and PEG-J on par for enteral nutrition, but each has complications
CORONADO, CALIF. – Percutaneous gastrostomy with jejunal extension (PEG-J) is an appealing and effective method for delivery of enteral nutrition in necrotizing pancreatitis patients, without the mechanical issues and discomfort associated with nasojejunal (NJ) tube, results from a single-center retrospective study showed.
“The advantages of PEG-J route for enteral nutrition in necrotizing pancreatitis patients must be weighed carefully against the potentially severe complication profile,” study author Alexandra M. Roch, MD, said at the annual meeting of the Western Surgical Association.
Historically, the preferred way to manage patients with necrotizing pancreatitis was via parenteral nutrition with a lack of pancreatic stimulation, said Dr. Roch, of the department of surgery at Indiana University, Indianapolis. However, parenteral nutrition is associated with increased permeability, a lack of peristaltic stimulation, changes in intestinal flora, and an increased risk of infection.
“More recently, enteral nutrition has been used, despite a potential for pancreatic stimulation,” she said. “From 16 randomized, controlled trials with 847 patients, it was associated with decreased mortality, decreased infectious complications, decreased length of hospital stay, and a trend toward decreased rate of organ failure. Based on those findings, enteral nutrition has become the standard of care in acute pancreatitis. The optimal enteral nutrition route, however, is still debated. The traditional route is the nasojejunal [NJ] tube. Its placement is noninvasive, but it is associated with discomfort for the patient, dislodgement in 16%-63% of cases, and potentially sinusitis. Conversely, percutaneous gastrostomy with jejunal extension [PEG-J] is beneficial for patient comfort but has the drawbacks of being an invasive procedure with the risk of cellulitis and more severe complications.”
The aim of the current study was to compare the safety and efficacy of NJ tube and PEG-J enteral nutrition delivery before surgical debridement in patients with necrotizing pancreatitis. Dr. Roch and her associates hypothesized that NJ tube and PEG-J would have a similar complication profile. They retrospectively reviewed the medical records of all patients who underwent surgical debridement for necrotizing pancreatitis at Indiana University Medical Center between 2005 and 2015. Patients with exclusive total parenteral nutrition were excluded from the study, as were those who had incomplete data.
Dr. Roch reported results from 242 patients with a mean age of 54 years. More than half (64%) were men and the main etiology was biliary (47%), followed by alcohol (16%). The median duration of preoperative enteral nutrition was 29 days. Of the 242 patients, 187 had an NJ tube only, 25 had PEG-J only, and 30 patients had an NJ tube followed by PEG-J. More than half of PEG-Js were placed under fluoroscopic guidance, while the remaining 41% were placed endoscopically.
In terms of safety, patients in the NJ tube group had a significantly higher rate of all complications, compared with those in the PEG-J group (52% vs. 27%, respectively; P = .0015). Conversely, there was a significantly higher rate of serious complications among patients in the PEG-J group, compared with the NJ group (11% vs. 0%; P less than .0001). The researchers also found that compared with patients in the PEG-J group, those in the NJ group were more prone to mechanical complications such as difficulty to place (5% vs. 0%, respectively), replacement (30% vs. 5.5%), and repositioning (30% vs. 2%), while PEG-J patients were more prone to infectious complications such as skin infections/cellulitis (4% vs. 0%) and perforation/leakage/peritonitis (11% vs. 0%). When they limited the analysis to grade III or IV complications, the mechanism was always the same: early dislodgement from the GI tract. “The presentation ranged from asymptomatic patients to severe peritonitis,” Dr. Roch said. “Two patients out of the six with severe complications required emergent laparotomy.”
In terms of efficacy, the NJ and PEG-J groups were equivalent in achieving enteral nutrition (67% vs. 68%, respectively). There were also no differences between the two groups in nutritional status when assessed by an increase of serum albumin (38% vs. 36%; P = .87), normalization of serum albumin (9% vs. 16%; P = .14), or in the prevalence of infected necrosis (53% vs. 49%; P = .64).
Dr. Roch acknowledged certain limitations of the study, including its single-center, retrospective design. “Furthermore, we are a tertiary care center, and most patients are referred to us late in the course of their disease,” she said. “Finally, no PEG-Js were placed outside of our institution, raising the question of a selection bias. She reported having no financial disclosures.
CORONADO, CALIF. – Percutaneous gastrostomy with jejunal extension (PEG-J) is an appealing and effective method for delivery of enteral nutrition in necrotizing pancreatitis patients, without the mechanical issues and discomfort associated with nasojejunal (NJ) tube, results from a single-center retrospective study showed.
“The advantages of PEG-J route for enteral nutrition in necrotizing pancreatitis patients must be weighed carefully against the potentially severe complication profile,” study author Alexandra M. Roch, MD, said at the annual meeting of the Western Surgical Association.
Historically, the preferred way to manage patients with necrotizing pancreatitis was via parenteral nutrition with a lack of pancreatic stimulation, said Dr. Roch, of the department of surgery at Indiana University, Indianapolis. However, parenteral nutrition is associated with increased permeability, a lack of peristaltic stimulation, changes in intestinal flora, and an increased risk of infection.
“More recently, enteral nutrition has been used, despite a potential for pancreatic stimulation,” she said. “From 16 randomized, controlled trials with 847 patients, it was associated with decreased mortality, decreased infectious complications, decreased length of hospital stay, and a trend toward decreased rate of organ failure. Based on those findings, enteral nutrition has become the standard of care in acute pancreatitis. The optimal enteral nutrition route, however, is still debated. The traditional route is the nasojejunal [NJ] tube. Its placement is noninvasive, but it is associated with discomfort for the patient, dislodgement in 16%-63% of cases, and potentially sinusitis. Conversely, percutaneous gastrostomy with jejunal extension [PEG-J] is beneficial for patient comfort but has the drawbacks of being an invasive procedure with the risk of cellulitis and more severe complications.”
The aim of the current study was to compare the safety and efficacy of NJ tube and PEG-J enteral nutrition delivery before surgical debridement in patients with necrotizing pancreatitis. Dr. Roch and her associates hypothesized that NJ tube and PEG-J would have a similar complication profile. They retrospectively reviewed the medical records of all patients who underwent surgical debridement for necrotizing pancreatitis at Indiana University Medical Center between 2005 and 2015. Patients with exclusive total parenteral nutrition were excluded from the study, as were those who had incomplete data.
Dr. Roch reported results from 242 patients with a mean age of 54 years. More than half (64%) were men and the main etiology was biliary (47%), followed by alcohol (16%). The median duration of preoperative enteral nutrition was 29 days. Of the 242 patients, 187 had an NJ tube only, 25 had PEG-J only, and 30 patients had an NJ tube followed by PEG-J. More than half of PEG-Js were placed under fluoroscopic guidance, while the remaining 41% were placed endoscopically.
In terms of safety, patients in the NJ tube group had a significantly higher rate of all complications, compared with those in the PEG-J group (52% vs. 27%, respectively; P = .0015). Conversely, there was a significantly higher rate of serious complications among patients in the PEG-J group, compared with the NJ group (11% vs. 0%; P less than .0001). The researchers also found that compared with patients in the PEG-J group, those in the NJ group were more prone to mechanical complications such as difficulty to place (5% vs. 0%, respectively), replacement (30% vs. 5.5%), and repositioning (30% vs. 2%), while PEG-J patients were more prone to infectious complications such as skin infections/cellulitis (4% vs. 0%) and perforation/leakage/peritonitis (11% vs. 0%). When they limited the analysis to grade III or IV complications, the mechanism was always the same: early dislodgement from the GI tract. “The presentation ranged from asymptomatic patients to severe peritonitis,” Dr. Roch said. “Two patients out of the six with severe complications required emergent laparotomy.”
In terms of efficacy, the NJ and PEG-J groups were equivalent in achieving enteral nutrition (67% vs. 68%, respectively). There were also no differences between the two groups in nutritional status when assessed by an increase of serum albumin (38% vs. 36%; P = .87), normalization of serum albumin (9% vs. 16%; P = .14), or in the prevalence of infected necrosis (53% vs. 49%; P = .64).
Dr. Roch acknowledged certain limitations of the study, including its single-center, retrospective design. “Furthermore, we are a tertiary care center, and most patients are referred to us late in the course of their disease,” she said. “Finally, no PEG-Js were placed outside of our institution, raising the question of a selection bias. She reported having no financial disclosures.
CORONADO, CALIF. – Percutaneous gastrostomy with jejunal extension (PEG-J) is an appealing and effective method for delivery of enteral nutrition in necrotizing pancreatitis patients, without the mechanical issues and discomfort associated with nasojejunal (NJ) tube, results from a single-center retrospective study showed.
“The advantages of PEG-J route for enteral nutrition in necrotizing pancreatitis patients must be weighed carefully against the potentially severe complication profile,” study author Alexandra M. Roch, MD, said at the annual meeting of the Western Surgical Association.
Historically, the preferred way to manage patients with necrotizing pancreatitis was via parenteral nutrition with a lack of pancreatic stimulation, said Dr. Roch, of the department of surgery at Indiana University, Indianapolis. However, parenteral nutrition is associated with increased permeability, a lack of peristaltic stimulation, changes in intestinal flora, and an increased risk of infection.
“More recently, enteral nutrition has been used, despite a potential for pancreatic stimulation,” she said. “From 16 randomized, controlled trials with 847 patients, it was associated with decreased mortality, decreased infectious complications, decreased length of hospital stay, and a trend toward decreased rate of organ failure. Based on those findings, enteral nutrition has become the standard of care in acute pancreatitis. The optimal enteral nutrition route, however, is still debated. The traditional route is the nasojejunal [NJ] tube. Its placement is noninvasive, but it is associated with discomfort for the patient, dislodgement in 16%-63% of cases, and potentially sinusitis. Conversely, percutaneous gastrostomy with jejunal extension [PEG-J] is beneficial for patient comfort but has the drawbacks of being an invasive procedure with the risk of cellulitis and more severe complications.”
The aim of the current study was to compare the safety and efficacy of NJ tube and PEG-J enteral nutrition delivery before surgical debridement in patients with necrotizing pancreatitis. Dr. Roch and her associates hypothesized that NJ tube and PEG-J would have a similar complication profile. They retrospectively reviewed the medical records of all patients who underwent surgical debridement for necrotizing pancreatitis at Indiana University Medical Center between 2005 and 2015. Patients with exclusive total parenteral nutrition were excluded from the study, as were those who had incomplete data.
Dr. Roch reported results from 242 patients with a mean age of 54 years. More than half (64%) were men and the main etiology was biliary (47%), followed by alcohol (16%). The median duration of preoperative enteral nutrition was 29 days. Of the 242 patients, 187 had an NJ tube only, 25 had PEG-J only, and 30 patients had an NJ tube followed by PEG-J. More than half of PEG-Js were placed under fluoroscopic guidance, while the remaining 41% were placed endoscopically.
In terms of safety, patients in the NJ tube group had a significantly higher rate of all complications, compared with those in the PEG-J group (52% vs. 27%, respectively; P = .0015). Conversely, there was a significantly higher rate of serious complications among patients in the PEG-J group, compared with the NJ group (11% vs. 0%; P less than .0001). The researchers also found that compared with patients in the PEG-J group, those in the NJ group were more prone to mechanical complications such as difficulty to place (5% vs. 0%, respectively), replacement (30% vs. 5.5%), and repositioning (30% vs. 2%), while PEG-J patients were more prone to infectious complications such as skin infections/cellulitis (4% vs. 0%) and perforation/leakage/peritonitis (11% vs. 0%). When they limited the analysis to grade III or IV complications, the mechanism was always the same: early dislodgement from the GI tract. “The presentation ranged from asymptomatic patients to severe peritonitis,” Dr. Roch said. “Two patients out of the six with severe complications required emergent laparotomy.”
In terms of efficacy, the NJ and PEG-J groups were equivalent in achieving enteral nutrition (67% vs. 68%, respectively). There were also no differences between the two groups in nutritional status when assessed by an increase of serum albumin (38% vs. 36%; P = .87), normalization of serum albumin (9% vs. 16%; P = .14), or in the prevalence of infected necrosis (53% vs. 49%; P = .64).
Dr. Roch acknowledged certain limitations of the study, including its single-center, retrospective design. “Furthermore, we are a tertiary care center, and most patients are referred to us late in the course of their disease,” she said. “Finally, no PEG-Js were placed outside of our institution, raising the question of a selection bias. She reported having no financial disclosures.
AT WSA 2016
Key clinical point:
Major finding: In terms of efficacy, the NJ and PEG-J groups were equivalent in achieving enteral nutrition (67% vs. 68%, respectively).
Data source: A retrospective review of 242 patients who underwent surgical debridement for necrotizing pancreatitis at Indiana University Medical Center between 2005 and 2015.
Disclosures: Dr. Roch reported having no financial disclosures.
Surgery for bowel obstruction in cancer patients didn’t increase 90-day mortality
CORONADO, CALIF. – Among advanced cancer patients with bowel obstruction, surgery was not an independent predictor of the ability to eat at discharge or survival within 90 days of consultation, results from a long-term retrospective study showed.
“I think this represents the complexity in treating these patients,” lead study author Brian D. Badgwell, MD, said at the annual meeting of the Western Surgical Association. “We need future studies to identify the optimal outcome measures.”
For the current study, the researchers retrospectively reviewed the medical records of 490 patients who required surgical consultation for bowel obstruction at MD Anderson Cancer Center between January 2000 and May 2014. They set out to determine the incidence of obstruction due to intra-abdominal tumor and to identify variables associated with the ability to eat at hospital discharge and 90-day survival. They excluded patients without clinical or radiologic features of mechanical bowel obstruction. Clinical variables of interest included obstruction site, tumor vs. non-tumor cause, laboratory parameters, radiologic extent of malignancy, and the type of treatment performed (surgical, medical, or interventional, defined as interventional radiology or endoscopy). Overall survival was calculated from the date of first surgical evaluation for bowel obstruction to any cause mortality or last follow-up. Univariate and multivariate analyses were performed for ability to eat and a Cox proportional hazards model for 90-day survival.
Dr. Badgwell reported that the most common obstruction site in the 490 patients was the small bowel (64%), followed by large bowel (20%) and gastric outlet (16%). Obstruction etiology was identified as tumor-related in 68% of cases, followed by adhesion-related (20%) and unclear (12%). Nearly half of patients (46%) received chemotherapy within 6 weeks of their surgical consultation, but only 4% were neutropenic. More than half of patients (52%) had an albumin level of less than 3.5 g/dL, 52% had a hemoglobin of 10 g/dL or greater, 36% had lymphadenopathy, 35% had ascites, 34% had peritoneal disease, and 31% had a primary or recurrent tumor in place. In addition, 53% had an abdominal visceral malignancy, 9% had bone metastases, and 14% had lung metastases.
About half of patients (49%) received medical management as their treatment, followed by surgical and procedural treatment (32% and 17%, respectively). Fifteen percent were discharged to in-home hospice or to an inpatient hospice facility. More than two-thirds (68%) were able to eat at the time of discharge, and 43% died within 90 days of surgical consultation.
Multivariate analysis revealed that the following factors were negatively associated with eating at discharge: an intact/primary local recurrence (odds ratio, 0.46), carcinomatosis (OR, 0.34), and albumin level of less than 3.5 g/dL (OR, 0.55). At the same time, variables associated with death within 90 days of consultation included having an intact primary/local recurrence (hazard ratio, 1.75), carcinomatosis (HR, 1.98), and abdominal visceral metastasis (HR, 1.75). Finally, compared with procedural treatment, both medical management and surgical management were negatively associated with death within 90 days (HR of 0.51 and 0.44, respectively).
“There is a high rate of non-mechanical bowel dysfunction in patients undergoing surgical consultation for bowel obstruction,” Dr. Badgwell concluded. “It’s very difficult to categorize these cases preoperatively. They do require a selective approach. Variables associated with outcome measures support caution in patients with carcinomatosis, hypoalbuminemia, and multiple sites of disease on imaging.”
Dr. Badgwell reported having no financial disclosures.
CORONADO, CALIF. – Among advanced cancer patients with bowel obstruction, surgery was not an independent predictor of the ability to eat at discharge or survival within 90 days of consultation, results from a long-term retrospective study showed.
“I think this represents the complexity in treating these patients,” lead study author Brian D. Badgwell, MD, said at the annual meeting of the Western Surgical Association. “We need future studies to identify the optimal outcome measures.”
For the current study, the researchers retrospectively reviewed the medical records of 490 patients who required surgical consultation for bowel obstruction at MD Anderson Cancer Center between January 2000 and May 2014. They set out to determine the incidence of obstruction due to intra-abdominal tumor and to identify variables associated with the ability to eat at hospital discharge and 90-day survival. They excluded patients without clinical or radiologic features of mechanical bowel obstruction. Clinical variables of interest included obstruction site, tumor vs. non-tumor cause, laboratory parameters, radiologic extent of malignancy, and the type of treatment performed (surgical, medical, or interventional, defined as interventional radiology or endoscopy). Overall survival was calculated from the date of first surgical evaluation for bowel obstruction to any cause mortality or last follow-up. Univariate and multivariate analyses were performed for ability to eat and a Cox proportional hazards model for 90-day survival.
Dr. Badgwell reported that the most common obstruction site in the 490 patients was the small bowel (64%), followed by large bowel (20%) and gastric outlet (16%). Obstruction etiology was identified as tumor-related in 68% of cases, followed by adhesion-related (20%) and unclear (12%). Nearly half of patients (46%) received chemotherapy within 6 weeks of their surgical consultation, but only 4% were neutropenic. More than half of patients (52%) had an albumin level of less than 3.5 g/dL, 52% had a hemoglobin of 10 g/dL or greater, 36% had lymphadenopathy, 35% had ascites, 34% had peritoneal disease, and 31% had a primary or recurrent tumor in place. In addition, 53% had an abdominal visceral malignancy, 9% had bone metastases, and 14% had lung metastases.
About half of patients (49%) received medical management as their treatment, followed by surgical and procedural treatment (32% and 17%, respectively). Fifteen percent were discharged to in-home hospice or to an inpatient hospice facility. More than two-thirds (68%) were able to eat at the time of discharge, and 43% died within 90 days of surgical consultation.
Multivariate analysis revealed that the following factors were negatively associated with eating at discharge: an intact/primary local recurrence (odds ratio, 0.46), carcinomatosis (OR, 0.34), and albumin level of less than 3.5 g/dL (OR, 0.55). At the same time, variables associated with death within 90 days of consultation included having an intact primary/local recurrence (hazard ratio, 1.75), carcinomatosis (HR, 1.98), and abdominal visceral metastasis (HR, 1.75). Finally, compared with procedural treatment, both medical management and surgical management were negatively associated with death within 90 days (HR of 0.51 and 0.44, respectively).
“There is a high rate of non-mechanical bowel dysfunction in patients undergoing surgical consultation for bowel obstruction,” Dr. Badgwell concluded. “It’s very difficult to categorize these cases preoperatively. They do require a selective approach. Variables associated with outcome measures support caution in patients with carcinomatosis, hypoalbuminemia, and multiple sites of disease on imaging.”
Dr. Badgwell reported having no financial disclosures.
CORONADO, CALIF. – Among advanced cancer patients with bowel obstruction, surgery was not an independent predictor of the ability to eat at discharge or survival within 90 days of consultation, results from a long-term retrospective study showed.
“I think this represents the complexity in treating these patients,” lead study author Brian D. Badgwell, MD, said at the annual meeting of the Western Surgical Association. “We need future studies to identify the optimal outcome measures.”
For the current study, the researchers retrospectively reviewed the medical records of 490 patients who required surgical consultation for bowel obstruction at MD Anderson Cancer Center between January 2000 and May 2014. They set out to determine the incidence of obstruction due to intra-abdominal tumor and to identify variables associated with the ability to eat at hospital discharge and 90-day survival. They excluded patients without clinical or radiologic features of mechanical bowel obstruction. Clinical variables of interest included obstruction site, tumor vs. non-tumor cause, laboratory parameters, radiologic extent of malignancy, and the type of treatment performed (surgical, medical, or interventional, defined as interventional radiology or endoscopy). Overall survival was calculated from the date of first surgical evaluation for bowel obstruction to any cause mortality or last follow-up. Univariate and multivariate analyses were performed for ability to eat and a Cox proportional hazards model for 90-day survival.
Dr. Badgwell reported that the most common obstruction site in the 490 patients was the small bowel (64%), followed by large bowel (20%) and gastric outlet (16%). Obstruction etiology was identified as tumor-related in 68% of cases, followed by adhesion-related (20%) and unclear (12%). Nearly half of patients (46%) received chemotherapy within 6 weeks of their surgical consultation, but only 4% were neutropenic. More than half of patients (52%) had an albumin level of less than 3.5 g/dL, 52% had a hemoglobin of 10 g/dL or greater, 36% had lymphadenopathy, 35% had ascites, 34% had peritoneal disease, and 31% had a primary or recurrent tumor in place. In addition, 53% had an abdominal visceral malignancy, 9% had bone metastases, and 14% had lung metastases.
About half of patients (49%) received medical management as their treatment, followed by surgical and procedural treatment (32% and 17%, respectively). Fifteen percent were discharged to in-home hospice or to an inpatient hospice facility. More than two-thirds (68%) were able to eat at the time of discharge, and 43% died within 90 days of surgical consultation.
Multivariate analysis revealed that the following factors were negatively associated with eating at discharge: an intact/primary local recurrence (odds ratio, 0.46), carcinomatosis (OR, 0.34), and albumin level of less than 3.5 g/dL (OR, 0.55). At the same time, variables associated with death within 90 days of consultation included having an intact primary/local recurrence (hazard ratio, 1.75), carcinomatosis (HR, 1.98), and abdominal visceral metastasis (HR, 1.75). Finally, compared with procedural treatment, both medical management and surgical management were negatively associated with death within 90 days (HR of 0.51 and 0.44, respectively).
“There is a high rate of non-mechanical bowel dysfunction in patients undergoing surgical consultation for bowel obstruction,” Dr. Badgwell concluded. “It’s very difficult to categorize these cases preoperatively. They do require a selective approach. Variables associated with outcome measures support caution in patients with carcinomatosis, hypoalbuminemia, and multiple sites of disease on imaging.”
Dr. Badgwell reported having no financial disclosures.
AT WSA 2016
Key clinical point:
Major finding: Compared with procedural treatment of bowel obstruction, both medical management and surgical management were negatively associated with death within 90 days (HR of 0.51 and 0.44, respectively).
Data source: A retrospective review of 490 patients with advanced cancer who required surgical consultation for bowel obstruction at MD Anderson Cancer Center, Houston, between January 2000 and May 2014.
Disclosures: Dr. Badgwell reported having no financial disclosures.