User login
Preauthorization for medications: Who oversees placement of the hoops?
The letter from the insurance company was addressed to my patient. The two pages of information boiled down to one simple sentence: “After a thorough review, our decision to not cover the medication Provigil (modafinil) is unchanged.” The letter went on to explain that there was no further recourse, and that the medication would not be approved because it was not Food and Drug Administration–approved for the condition my patient had: major depression. If she chose to take it, there would be no reimbursement. In many psychiatric conditions, the FDA-approved options are very limited; for some disorders, there simply are no approved medications, despite the fact that research has shown medications to be helpful. For a medication that now has a generic, there is no reason for the pharmaceutical agency to incur the cost of getting a medication approved by the FDA for a specific use.
Psychiatrists are all familiar with the process of medication preauthorization. Insurance companies require the physician to make an extra effort in order to prescribe certain medications. Often, as in the case of modafinil, the medications are expensive, and one might wonder why a generic medication costs $25 a pill. The name-brand medication, Provigil, costs more than $33 for a single dose. Sometimes, however, a preauthorization process is put in place for very inexpensive medications that might cost only a few dollars a month. Preauthorization requirements waste enormous amounts of physician time and don’t necessarily save money for insurers.
What many physicians don’t realize is that there is no national oversight to this process. In some arenas, the insurers can set the hoops as high as they want and in perpetual motion, thereby making the process a long and miserable adventure – all while the patient suffers.
Nothing about my patient’s depression has been easy to treat. We started working together 8 years ago; her suffering at that time was extreme and her presentation was unusual. I arranged for her admission to a specialty unit in a psychiatric hospital, and she remained under their care for several months – an astounding period of time in an era where the average length of stay is 7 to 10 days. She was discharged – very much improved – on an unusual cocktail of medications.
Over time, we tapered some of the medications because of side effects. Five years ago, her insurance changed and after I answered a 13-question prior authorization form, the medication was denied because she did not have narcolepsy or any of the sleep disorders for which the FDA does approve the use of Provigil. An appeal was denied, and I prescribed stimulants instead. It wasn’t until recently, when the patient’s depression returned full-force, and every medication option I could think of had been tried, that I decided to try modafinil again, especially since I have found it helpful in another patient with a treatment-resistant depression.
I wrote a prescription and heard from the pharmacy that Provigil required preauthorization. I prescribed Nuvigil instead, but that too required preauthorization. A 20-minute phone call resulted in directions on how to find a form and fax a request for the medication. It contained many of the same questions from years ago, and the request was denied.
Several more phone calls led me to a reviewer with the pharmacy benefits company in Nevada, who told me I could find a form on the website, send in an appeal to the insurance company in Iowa, and I would hear within 15 business days if my patient could get the medication. When I said that was not acceptable – the patient was suffering and needed the medication now – I was told I would receive a call from a peer reviewer within 48 hours. A week later, a pharmacist called and asked the exact same questions that I had already answered. When I said that no, I had not ordered polysomnography or multiple sleep latency tests because they were not medically indicated, she denied approval of the medication and said she had no leeway to approve its use if the questions were not answered correctly. I found it curious that this step was called a “peer-to-peer” review. By this point, I had spent about an hour in a two-step process where the second step was exactly the same as the first step. It’s okay; the insurance company doesn’t mind the inefficient use of everyone’s time.
I was told that to file an appeal, I would need more forms off the website, and I was given (at my request) directions on where to find those forms. But first, I needed to get the patient to sign a form to authorize to release information on her behalf. The patient lives a 90-minute drive from my office and does not have a fax machine, and this delayed the process. It remained unclear to me why the patient’s permission was needed when it had not been needed for the first two steps of the process. The authorization was to be mailed or faxed to one location, while the appeal letter was to be mailed (fax or electronic submissions were not options) to another address.
In the appeal letter, I discussed her past history of a lengthy hospitalization, a long list of other medications that had been tried, and a study that documented the efficacy of modafinil as an adjunct agent in the treatment of depression.
As the weeks ticked by, I contacted the chief medical officer of the insurance company and complained; I had spent hours on an arbitrary, repetitive, and inefficient process that was yielding no results. I asked how he sleeps at night.
The response was infuriating: “I know that the appeal is being set up in the queue. I am sorry that this process has been drawn out for you and your patient.” In the queue? Had he ever sat with a sobbing, depressed patient who couldn’t get out of bed all day? A family member was taking off work to stay with her, and her life was on hold. The chief medical officer didn’t give any indication as to how long this queue might be. The family was hurting both emotionally and financially.
I tried one of my U.S. senators. His office replied that preauthorization oversight was not a legislative issue. I spoke with the insurance commission in Maryland where I practice, and I filed a formal complaint with the insurance commissioner in Iowa. I was told it could take up to 45 days for a response, but the next day, I heard back: The plan is funded through a family member’s employer and is not under the jurisdiction of the insurance commissioner. Simply put, the insurance company can set up as many hurdles as they like and take as long as they want to respond, regardless of the patient’s need.
Eight weeks after I wrote the prescription, a copy of the denial letter arrived in my mail. A physician in Iowa has determined that the medication is not medically necessary for a patient he or she had never seen in Maryland. I’ve turned to the American Psychiatric Association. With so many psychiatrists complaining about the burdens of preauthorization, this case would be a good example; one of its attorneys has agreed to write a letter to the Department of Labor. Perhaps that will help, but as of this writing, I have not yet seen that letter. All in all, it has been hours of my time, and lots of waiting, all without regard to the person who could possibly find some relief with a medication that is available to some, but not to her.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
The letter from the insurance company was addressed to my patient. The two pages of information boiled down to one simple sentence: “After a thorough review, our decision to not cover the medication Provigil (modafinil) is unchanged.” The letter went on to explain that there was no further recourse, and that the medication would not be approved because it was not Food and Drug Administration–approved for the condition my patient had: major depression. If she chose to take it, there would be no reimbursement. In many psychiatric conditions, the FDA-approved options are very limited; for some disorders, there simply are no approved medications, despite the fact that research has shown medications to be helpful. For a medication that now has a generic, there is no reason for the pharmaceutical agency to incur the cost of getting a medication approved by the FDA for a specific use.
Psychiatrists are all familiar with the process of medication preauthorization. Insurance companies require the physician to make an extra effort in order to prescribe certain medications. Often, as in the case of modafinil, the medications are expensive, and one might wonder why a generic medication costs $25 a pill. The name-brand medication, Provigil, costs more than $33 for a single dose. Sometimes, however, a preauthorization process is put in place for very inexpensive medications that might cost only a few dollars a month. Preauthorization requirements waste enormous amounts of physician time and don’t necessarily save money for insurers.
What many physicians don’t realize is that there is no national oversight to this process. In some arenas, the insurers can set the hoops as high as they want and in perpetual motion, thereby making the process a long and miserable adventure – all while the patient suffers.
Nothing about my patient’s depression has been easy to treat. We started working together 8 years ago; her suffering at that time was extreme and her presentation was unusual. I arranged for her admission to a specialty unit in a psychiatric hospital, and she remained under their care for several months – an astounding period of time in an era where the average length of stay is 7 to 10 days. She was discharged – very much improved – on an unusual cocktail of medications.
Over time, we tapered some of the medications because of side effects. Five years ago, her insurance changed and after I answered a 13-question prior authorization form, the medication was denied because she did not have narcolepsy or any of the sleep disorders for which the FDA does approve the use of Provigil. An appeal was denied, and I prescribed stimulants instead. It wasn’t until recently, when the patient’s depression returned full-force, and every medication option I could think of had been tried, that I decided to try modafinil again, especially since I have found it helpful in another patient with a treatment-resistant depression.
I wrote a prescription and heard from the pharmacy that Provigil required preauthorization. I prescribed Nuvigil instead, but that too required preauthorization. A 20-minute phone call resulted in directions on how to find a form and fax a request for the medication. It contained many of the same questions from years ago, and the request was denied.
Several more phone calls led me to a reviewer with the pharmacy benefits company in Nevada, who told me I could find a form on the website, send in an appeal to the insurance company in Iowa, and I would hear within 15 business days if my patient could get the medication. When I said that was not acceptable – the patient was suffering and needed the medication now – I was told I would receive a call from a peer reviewer within 48 hours. A week later, a pharmacist called and asked the exact same questions that I had already answered. When I said that no, I had not ordered polysomnography or multiple sleep latency tests because they were not medically indicated, she denied approval of the medication and said she had no leeway to approve its use if the questions were not answered correctly. I found it curious that this step was called a “peer-to-peer” review. By this point, I had spent about an hour in a two-step process where the second step was exactly the same as the first step. It’s okay; the insurance company doesn’t mind the inefficient use of everyone’s time.
I was told that to file an appeal, I would need more forms off the website, and I was given (at my request) directions on where to find those forms. But first, I needed to get the patient to sign a form to authorize to release information on her behalf. The patient lives a 90-minute drive from my office and does not have a fax machine, and this delayed the process. It remained unclear to me why the patient’s permission was needed when it had not been needed for the first two steps of the process. The authorization was to be mailed or faxed to one location, while the appeal letter was to be mailed (fax or electronic submissions were not options) to another address.
In the appeal letter, I discussed her past history of a lengthy hospitalization, a long list of other medications that had been tried, and a study that documented the efficacy of modafinil as an adjunct agent in the treatment of depression.
As the weeks ticked by, I contacted the chief medical officer of the insurance company and complained; I had spent hours on an arbitrary, repetitive, and inefficient process that was yielding no results. I asked how he sleeps at night.
The response was infuriating: “I know that the appeal is being set up in the queue. I am sorry that this process has been drawn out for you and your patient.” In the queue? Had he ever sat with a sobbing, depressed patient who couldn’t get out of bed all day? A family member was taking off work to stay with her, and her life was on hold. The chief medical officer didn’t give any indication as to how long this queue might be. The family was hurting both emotionally and financially.
I tried one of my U.S. senators. His office replied that preauthorization oversight was not a legislative issue. I spoke with the insurance commission in Maryland where I practice, and I filed a formal complaint with the insurance commissioner in Iowa. I was told it could take up to 45 days for a response, but the next day, I heard back: The plan is funded through a family member’s employer and is not under the jurisdiction of the insurance commissioner. Simply put, the insurance company can set up as many hurdles as they like and take as long as they want to respond, regardless of the patient’s need.
Eight weeks after I wrote the prescription, a copy of the denial letter arrived in my mail. A physician in Iowa has determined that the medication is not medically necessary for a patient he or she had never seen in Maryland. I’ve turned to the American Psychiatric Association. With so many psychiatrists complaining about the burdens of preauthorization, this case would be a good example; one of its attorneys has agreed to write a letter to the Department of Labor. Perhaps that will help, but as of this writing, I have not yet seen that letter. All in all, it has been hours of my time, and lots of waiting, all without regard to the person who could possibly find some relief with a medication that is available to some, but not to her.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
The letter from the insurance company was addressed to my patient. The two pages of information boiled down to one simple sentence: “After a thorough review, our decision to not cover the medication Provigil (modafinil) is unchanged.” The letter went on to explain that there was no further recourse, and that the medication would not be approved because it was not Food and Drug Administration–approved for the condition my patient had: major depression. If she chose to take it, there would be no reimbursement. In many psychiatric conditions, the FDA-approved options are very limited; for some disorders, there simply are no approved medications, despite the fact that research has shown medications to be helpful. For a medication that now has a generic, there is no reason for the pharmaceutical agency to incur the cost of getting a medication approved by the FDA for a specific use.
Psychiatrists are all familiar with the process of medication preauthorization. Insurance companies require the physician to make an extra effort in order to prescribe certain medications. Often, as in the case of modafinil, the medications are expensive, and one might wonder why a generic medication costs $25 a pill. The name-brand medication, Provigil, costs more than $33 for a single dose. Sometimes, however, a preauthorization process is put in place for very inexpensive medications that might cost only a few dollars a month. Preauthorization requirements waste enormous amounts of physician time and don’t necessarily save money for insurers.
What many physicians don’t realize is that there is no national oversight to this process. In some arenas, the insurers can set the hoops as high as they want and in perpetual motion, thereby making the process a long and miserable adventure – all while the patient suffers.
Nothing about my patient’s depression has been easy to treat. We started working together 8 years ago; her suffering at that time was extreme and her presentation was unusual. I arranged for her admission to a specialty unit in a psychiatric hospital, and she remained under their care for several months – an astounding period of time in an era where the average length of stay is 7 to 10 days. She was discharged – very much improved – on an unusual cocktail of medications.
Over time, we tapered some of the medications because of side effects. Five years ago, her insurance changed and after I answered a 13-question prior authorization form, the medication was denied because she did not have narcolepsy or any of the sleep disorders for which the FDA does approve the use of Provigil. An appeal was denied, and I prescribed stimulants instead. It wasn’t until recently, when the patient’s depression returned full-force, and every medication option I could think of had been tried, that I decided to try modafinil again, especially since I have found it helpful in another patient with a treatment-resistant depression.
I wrote a prescription and heard from the pharmacy that Provigil required preauthorization. I prescribed Nuvigil instead, but that too required preauthorization. A 20-minute phone call resulted in directions on how to find a form and fax a request for the medication. It contained many of the same questions from years ago, and the request was denied.
Several more phone calls led me to a reviewer with the pharmacy benefits company in Nevada, who told me I could find a form on the website, send in an appeal to the insurance company in Iowa, and I would hear within 15 business days if my patient could get the medication. When I said that was not acceptable – the patient was suffering and needed the medication now – I was told I would receive a call from a peer reviewer within 48 hours. A week later, a pharmacist called and asked the exact same questions that I had already answered. When I said that no, I had not ordered polysomnography or multiple sleep latency tests because they were not medically indicated, she denied approval of the medication and said she had no leeway to approve its use if the questions were not answered correctly. I found it curious that this step was called a “peer-to-peer” review. By this point, I had spent about an hour in a two-step process where the second step was exactly the same as the first step. It’s okay; the insurance company doesn’t mind the inefficient use of everyone’s time.
I was told that to file an appeal, I would need more forms off the website, and I was given (at my request) directions on where to find those forms. But first, I needed to get the patient to sign a form to authorize to release information on her behalf. The patient lives a 90-minute drive from my office and does not have a fax machine, and this delayed the process. It remained unclear to me why the patient’s permission was needed when it had not been needed for the first two steps of the process. The authorization was to be mailed or faxed to one location, while the appeal letter was to be mailed (fax or electronic submissions were not options) to another address.
In the appeal letter, I discussed her past history of a lengthy hospitalization, a long list of other medications that had been tried, and a study that documented the efficacy of modafinil as an adjunct agent in the treatment of depression.
As the weeks ticked by, I contacted the chief medical officer of the insurance company and complained; I had spent hours on an arbitrary, repetitive, and inefficient process that was yielding no results. I asked how he sleeps at night.
The response was infuriating: “I know that the appeal is being set up in the queue. I am sorry that this process has been drawn out for you and your patient.” In the queue? Had he ever sat with a sobbing, depressed patient who couldn’t get out of bed all day? A family member was taking off work to stay with her, and her life was on hold. The chief medical officer didn’t give any indication as to how long this queue might be. The family was hurting both emotionally and financially.
I tried one of my U.S. senators. His office replied that preauthorization oversight was not a legislative issue. I spoke with the insurance commission in Maryland where I practice, and I filed a formal complaint with the insurance commissioner in Iowa. I was told it could take up to 45 days for a response, but the next day, I heard back: The plan is funded through a family member’s employer and is not under the jurisdiction of the insurance commissioner. Simply put, the insurance company can set up as many hurdles as they like and take as long as they want to respond, regardless of the patient’s need.
Eight weeks after I wrote the prescription, a copy of the denial letter arrived in my mail. A physician in Iowa has determined that the medication is not medically necessary for a patient he or she had never seen in Maryland. I’ve turned to the American Psychiatric Association. With so many psychiatrists complaining about the burdens of preauthorization, this case would be a good example; one of its attorneys has agreed to write a letter to the Department of Labor. Perhaps that will help, but as of this writing, I have not yet seen that letter. All in all, it has been hours of my time, and lots of waiting, all without regard to the person who could possibly find some relief with a medication that is available to some, but not to her.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Does psychiatric treatment prevent suicide?
Over the past 2 decades, more and more people have been treated with antidepressant medications. In the same period of time, suicide rates have gone up – not down. To those of us who treat patients, this fact is both surprising and perplexing. It seems that suicidal thoughts are a common feature of major depression, and when the depressive symptoms abate with treatment, the suicidal thoughts dissipate. Intuitively, it seems that treating depression on a larger scale should prevent suicides, but we still don’t know that conclusively.
According to the National Health and Nutrition Examination Survey (NHANES), 11% percent of Americans over the age of 12 are taking an antidepressant medication. In women aged 40-59, this number is 23%. Of those taking antidepressants, only one-third have seen a mental health professional in the past 12 months. What also is striking is that for people surveyed with symptoms of severe depression, only one-third were on medication.
In 2013, just over 40,000 Americans died of suicide. From 2000 to 2013, the suicide rate per 100,000 Americans has steadily increased from 10.4 to 12.6 per 100,000 people. While we know that people with psychiatric illnesses have higher rates of suicide compared with the general population, what we don’t know is whether the people dying are the same people who are getting treatment.
Thinking about this gets very difficult. It has been estimated that 90% of those who die of suicide have suffered from a mental illness. This figure includes those who were treated, untreated, and previously treated, but the studies have methodologic inconsistencies and that 90% estimate may not be accurate. Certainly, however, people die of suicide for reasons that have nothing to do with psychiatric illness, and we do know that impulsive responses to distressing circumstances are a factor, especially when a lethal method is easily available.
Several studies have shown that antidepressant use, particularly in older adults, may be associated with a decrease in suicidality. The studies often combine suicide attempts and completions. The issues with younger patients are more complicated, and in recent weeks, the reanalysis of the 2001 Paxil 329 study has again raised issues about the safety of certain antidepressants in children and adolescents. The data for all these studies are both confusing and contradictory, and are not easy to examine or interpret.
We also don’t know what role psychotherapy plays. A study done at Johns Hopkins Bloomberg School of Public Health looked at the follow-up for 65,000 people in Denmark who had attempted suicide and found that the rates for completed suicide dropped if the patient received a short course of psychosocial therapy at a suicide prevention center. But again, this study looked at a select group of people who had already attempted suicide.
I began to think it might help to ask these questions in a closed system where patients could be tallied with regard to requests for treatment, what type of treatment was provided, and even access to autopsy results. The U.S. Department of Veterans Affairs seemed to be a source where such answers might be found. It has been reported that 22 veterans a day die by suicide, and many veterans get their care in VA facilities, with VA pharmacy benefits, and treatment effects can, in theory, be studied.
Hoping to get a better sense of the relationship between treatment and suicide, I met with Robert Bossarte, Ph.D., director of the Epidemiology Program in the VA’s Office of Public Health. His career has been focused on suicide prevention.
The first thing Dr. Bossarte did was dissuade me of the idea that the VA is a closed system. Not all veterans receive lifelong benefits from the VA, and the formulas for determining who is entitled to what benefits, and for how long, is rather complicated. Dr. Bossarte also noted that some patients go outside of the system for their care.
“What we do know is that among those who have used VA services in the previous year, about 2,000 veterans a year die from suicide. It’s been hovering around that for the past decade,” Dr. Bossarte explained, again emphasizing that many veterans do not receive care at VA facilities. “We published a report in 2012 where we estimated 22 veterans a day die by suicide and that caught fire, but it is purely an estimate. The truth is we have no idea what the real count is, because until we began working on the Suicide Data Repository there was no national register of veteran mortality and there has been no way for us to know.”
Dr. Bossarte anticipates that the VA will have the data necessary to calculate more accurate statistics by the end of the year. “More than 70% of veteran suicide are in people over age 50; but the rates are going up most among the youngest.”
A notable drop in veteran suicide rates for those who used services occurred between 2001 and 2003, and that decrease remains unexplained; it preceded later changes in mental health services and enhanced suicide prevention programs. Dr. Bossarte also pointed out that just under half of veterans who die from suicide have no mental health diagnosis, despite yearly screening to identify people who may be suffering from posttraumatic stress disorder, alcohol-related disorders, and depression.
“The attention on veteran suicide started around 2007,” Dr. Bossarte explained. “Mark Kaplan published a study using publicly available mortality data; those who reported they were veterans were twice as likely to die of suicide as those who were not.”
While this sparked interest in veteran suicide, it’s important to note that a replication of that study in 2012 by Matthew Miller did not have the same findings.
“Then, in 2008, for the first time in recent history,” Dr. Bossarte continued, “the suicide rate among active duty military personnel exceeded that of the general population. Traditionally, rates of suicide in this population have been 40%-50% lower than in the general population. The increased rate was seen primarily in the Army and Marines. Serious mental illness may make people ineligible for military service, as can violent and disruptive behavior – things that are associated with suicide – so you tended to get a healthier population in the military.”
Dr. Bossarte noted that there was conjecture that increased suicide rates among active military might be related to more waivers that allowed people to enlist who would not ordinarily be eligible, and/or to higher rates of deployment. He went on to talk about Army STARRS (Army Study to Assess Risk and Resilience in Servicemembers).
“STARRS devoted $50 million over 5 years to the largest suicide study and did not find an effect of waivers. They did report a higher suicide rate among those who were deployed, however. But then Tim Bullman in my office looked at suicide rates 7 years after separation from service, and he reported a higher suicide rate among those who were never deployed.” The VA studies, I quickly realized, were also confusing and contradictory.
The VA has greatly expanded its mental health and suicide prevention services. For veterans overall, suicide rates have stabilized, but they have not decreased. For those veterans with psychiatric disorders, however, the suicide rates have gone down.
“When you ask ‘does treatment matter?’ it’s so hard to disentangle psychotherapy from pharmacotherapy. Over the past decade, we’ve seen a significant decrease in the suicide rate among those veterans with mental health disorders. We’ve looked at suicide rates every way you can think of. One thing we do know is that the better the relationship with the clinician, the lower the suicide risk.”
We talked about the role of hospitalization in preventing suicide, and Dr. Bossarte noted that the highest risk for suicide is immediately following hospital discharge.
“We are looking at people hospitalized after their first-ever suicide attempts and rates of mortality, including suicidal behavior, for 1 year after discharge. In very preliminary findings, we didn’t see any difference in the outcome for either all-cause mortality or repeat suicide attempts in those who were hospitalized, compared to those who were not. We don’t yet know about completed suicide.”
I left my discussion with Dr. Bossarte with more questions than answers. We have reason to believe that treatment helps, but we still don’t know which treatments help which people, and we do know that treatment doesn’t prevent suicide in every patient. In a culture where “treatment” has come to be equated with “prescribing” and is often based on a checklist of symptoms done by a primary care clinician, one might wonder if combining psychotherapy and medication – an increasingly rare offering – might have a better outcome. Simply put, for a problem that prematurely takes more than 40,000 lives a year, we know much too little.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Over the past 2 decades, more and more people have been treated with antidepressant medications. In the same period of time, suicide rates have gone up – not down. To those of us who treat patients, this fact is both surprising and perplexing. It seems that suicidal thoughts are a common feature of major depression, and when the depressive symptoms abate with treatment, the suicidal thoughts dissipate. Intuitively, it seems that treating depression on a larger scale should prevent suicides, but we still don’t know that conclusively.
According to the National Health and Nutrition Examination Survey (NHANES), 11% percent of Americans over the age of 12 are taking an antidepressant medication. In women aged 40-59, this number is 23%. Of those taking antidepressants, only one-third have seen a mental health professional in the past 12 months. What also is striking is that for people surveyed with symptoms of severe depression, only one-third were on medication.
In 2013, just over 40,000 Americans died of suicide. From 2000 to 2013, the suicide rate per 100,000 Americans has steadily increased from 10.4 to 12.6 per 100,000 people. While we know that people with psychiatric illnesses have higher rates of suicide compared with the general population, what we don’t know is whether the people dying are the same people who are getting treatment.
Thinking about this gets very difficult. It has been estimated that 90% of those who die of suicide have suffered from a mental illness. This figure includes those who were treated, untreated, and previously treated, but the studies have methodologic inconsistencies and that 90% estimate may not be accurate. Certainly, however, people die of suicide for reasons that have nothing to do with psychiatric illness, and we do know that impulsive responses to distressing circumstances are a factor, especially when a lethal method is easily available.
Several studies have shown that antidepressant use, particularly in older adults, may be associated with a decrease in suicidality. The studies often combine suicide attempts and completions. The issues with younger patients are more complicated, and in recent weeks, the reanalysis of the 2001 Paxil 329 study has again raised issues about the safety of certain antidepressants in children and adolescents. The data for all these studies are both confusing and contradictory, and are not easy to examine or interpret.
We also don’t know what role psychotherapy plays. A study done at Johns Hopkins Bloomberg School of Public Health looked at the follow-up for 65,000 people in Denmark who had attempted suicide and found that the rates for completed suicide dropped if the patient received a short course of psychosocial therapy at a suicide prevention center. But again, this study looked at a select group of people who had already attempted suicide.
I began to think it might help to ask these questions in a closed system where patients could be tallied with regard to requests for treatment, what type of treatment was provided, and even access to autopsy results. The U.S. Department of Veterans Affairs seemed to be a source where such answers might be found. It has been reported that 22 veterans a day die by suicide, and many veterans get their care in VA facilities, with VA pharmacy benefits, and treatment effects can, in theory, be studied.
Hoping to get a better sense of the relationship between treatment and suicide, I met with Robert Bossarte, Ph.D., director of the Epidemiology Program in the VA’s Office of Public Health. His career has been focused on suicide prevention.
The first thing Dr. Bossarte did was dissuade me of the idea that the VA is a closed system. Not all veterans receive lifelong benefits from the VA, and the formulas for determining who is entitled to what benefits, and for how long, is rather complicated. Dr. Bossarte also noted that some patients go outside of the system for their care.
“What we do know is that among those who have used VA services in the previous year, about 2,000 veterans a year die from suicide. It’s been hovering around that for the past decade,” Dr. Bossarte explained, again emphasizing that many veterans do not receive care at VA facilities. “We published a report in 2012 where we estimated 22 veterans a day die by suicide and that caught fire, but it is purely an estimate. The truth is we have no idea what the real count is, because until we began working on the Suicide Data Repository there was no national register of veteran mortality and there has been no way for us to know.”
Dr. Bossarte anticipates that the VA will have the data necessary to calculate more accurate statistics by the end of the year. “More than 70% of veteran suicide are in people over age 50; but the rates are going up most among the youngest.”
A notable drop in veteran suicide rates for those who used services occurred between 2001 and 2003, and that decrease remains unexplained; it preceded later changes in mental health services and enhanced suicide prevention programs. Dr. Bossarte also pointed out that just under half of veterans who die from suicide have no mental health diagnosis, despite yearly screening to identify people who may be suffering from posttraumatic stress disorder, alcohol-related disorders, and depression.
“The attention on veteran suicide started around 2007,” Dr. Bossarte explained. “Mark Kaplan published a study using publicly available mortality data; those who reported they were veterans were twice as likely to die of suicide as those who were not.”
While this sparked interest in veteran suicide, it’s important to note that a replication of that study in 2012 by Matthew Miller did not have the same findings.
“Then, in 2008, for the first time in recent history,” Dr. Bossarte continued, “the suicide rate among active duty military personnel exceeded that of the general population. Traditionally, rates of suicide in this population have been 40%-50% lower than in the general population. The increased rate was seen primarily in the Army and Marines. Serious mental illness may make people ineligible for military service, as can violent and disruptive behavior – things that are associated with suicide – so you tended to get a healthier population in the military.”
Dr. Bossarte noted that there was conjecture that increased suicide rates among active military might be related to more waivers that allowed people to enlist who would not ordinarily be eligible, and/or to higher rates of deployment. He went on to talk about Army STARRS (Army Study to Assess Risk and Resilience in Servicemembers).
“STARRS devoted $50 million over 5 years to the largest suicide study and did not find an effect of waivers. They did report a higher suicide rate among those who were deployed, however. But then Tim Bullman in my office looked at suicide rates 7 years after separation from service, and he reported a higher suicide rate among those who were never deployed.” The VA studies, I quickly realized, were also confusing and contradictory.
The VA has greatly expanded its mental health and suicide prevention services. For veterans overall, suicide rates have stabilized, but they have not decreased. For those veterans with psychiatric disorders, however, the suicide rates have gone down.
“When you ask ‘does treatment matter?’ it’s so hard to disentangle psychotherapy from pharmacotherapy. Over the past decade, we’ve seen a significant decrease in the suicide rate among those veterans with mental health disorders. We’ve looked at suicide rates every way you can think of. One thing we do know is that the better the relationship with the clinician, the lower the suicide risk.”
We talked about the role of hospitalization in preventing suicide, and Dr. Bossarte noted that the highest risk for suicide is immediately following hospital discharge.
“We are looking at people hospitalized after their first-ever suicide attempts and rates of mortality, including suicidal behavior, for 1 year after discharge. In very preliminary findings, we didn’t see any difference in the outcome for either all-cause mortality or repeat suicide attempts in those who were hospitalized, compared to those who were not. We don’t yet know about completed suicide.”
I left my discussion with Dr. Bossarte with more questions than answers. We have reason to believe that treatment helps, but we still don’t know which treatments help which people, and we do know that treatment doesn’t prevent suicide in every patient. In a culture where “treatment” has come to be equated with “prescribing” and is often based on a checklist of symptoms done by a primary care clinician, one might wonder if combining psychotherapy and medication – an increasingly rare offering – might have a better outcome. Simply put, for a problem that prematurely takes more than 40,000 lives a year, we know much too little.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Over the past 2 decades, more and more people have been treated with antidepressant medications. In the same period of time, suicide rates have gone up – not down. To those of us who treat patients, this fact is both surprising and perplexing. It seems that suicidal thoughts are a common feature of major depression, and when the depressive symptoms abate with treatment, the suicidal thoughts dissipate. Intuitively, it seems that treating depression on a larger scale should prevent suicides, but we still don’t know that conclusively.
According to the National Health and Nutrition Examination Survey (NHANES), 11% percent of Americans over the age of 12 are taking an antidepressant medication. In women aged 40-59, this number is 23%. Of those taking antidepressants, only one-third have seen a mental health professional in the past 12 months. What also is striking is that for people surveyed with symptoms of severe depression, only one-third were on medication.
In 2013, just over 40,000 Americans died of suicide. From 2000 to 2013, the suicide rate per 100,000 Americans has steadily increased from 10.4 to 12.6 per 100,000 people. While we know that people with psychiatric illnesses have higher rates of suicide compared with the general population, what we don’t know is whether the people dying are the same people who are getting treatment.
Thinking about this gets very difficult. It has been estimated that 90% of those who die of suicide have suffered from a mental illness. This figure includes those who were treated, untreated, and previously treated, but the studies have methodologic inconsistencies and that 90% estimate may not be accurate. Certainly, however, people die of suicide for reasons that have nothing to do with psychiatric illness, and we do know that impulsive responses to distressing circumstances are a factor, especially when a lethal method is easily available.
Several studies have shown that antidepressant use, particularly in older adults, may be associated with a decrease in suicidality. The studies often combine suicide attempts and completions. The issues with younger patients are more complicated, and in recent weeks, the reanalysis of the 2001 Paxil 329 study has again raised issues about the safety of certain antidepressants in children and adolescents. The data for all these studies are both confusing and contradictory, and are not easy to examine or interpret.
We also don’t know what role psychotherapy plays. A study done at Johns Hopkins Bloomberg School of Public Health looked at the follow-up for 65,000 people in Denmark who had attempted suicide and found that the rates for completed suicide dropped if the patient received a short course of psychosocial therapy at a suicide prevention center. But again, this study looked at a select group of people who had already attempted suicide.
I began to think it might help to ask these questions in a closed system where patients could be tallied with regard to requests for treatment, what type of treatment was provided, and even access to autopsy results. The U.S. Department of Veterans Affairs seemed to be a source where such answers might be found. It has been reported that 22 veterans a day die by suicide, and many veterans get their care in VA facilities, with VA pharmacy benefits, and treatment effects can, in theory, be studied.
Hoping to get a better sense of the relationship between treatment and suicide, I met with Robert Bossarte, Ph.D., director of the Epidemiology Program in the VA’s Office of Public Health. His career has been focused on suicide prevention.
The first thing Dr. Bossarte did was dissuade me of the idea that the VA is a closed system. Not all veterans receive lifelong benefits from the VA, and the formulas for determining who is entitled to what benefits, and for how long, is rather complicated. Dr. Bossarte also noted that some patients go outside of the system for their care.
“What we do know is that among those who have used VA services in the previous year, about 2,000 veterans a year die from suicide. It’s been hovering around that for the past decade,” Dr. Bossarte explained, again emphasizing that many veterans do not receive care at VA facilities. “We published a report in 2012 where we estimated 22 veterans a day die by suicide and that caught fire, but it is purely an estimate. The truth is we have no idea what the real count is, because until we began working on the Suicide Data Repository there was no national register of veteran mortality and there has been no way for us to know.”
Dr. Bossarte anticipates that the VA will have the data necessary to calculate more accurate statistics by the end of the year. “More than 70% of veteran suicide are in people over age 50; but the rates are going up most among the youngest.”
A notable drop in veteran suicide rates for those who used services occurred between 2001 and 2003, and that decrease remains unexplained; it preceded later changes in mental health services and enhanced suicide prevention programs. Dr. Bossarte also pointed out that just under half of veterans who die from suicide have no mental health diagnosis, despite yearly screening to identify people who may be suffering from posttraumatic stress disorder, alcohol-related disorders, and depression.
“The attention on veteran suicide started around 2007,” Dr. Bossarte explained. “Mark Kaplan published a study using publicly available mortality data; those who reported they were veterans were twice as likely to die of suicide as those who were not.”
While this sparked interest in veteran suicide, it’s important to note that a replication of that study in 2012 by Matthew Miller did not have the same findings.
“Then, in 2008, for the first time in recent history,” Dr. Bossarte continued, “the suicide rate among active duty military personnel exceeded that of the general population. Traditionally, rates of suicide in this population have been 40%-50% lower than in the general population. The increased rate was seen primarily in the Army and Marines. Serious mental illness may make people ineligible for military service, as can violent and disruptive behavior – things that are associated with suicide – so you tended to get a healthier population in the military.”
Dr. Bossarte noted that there was conjecture that increased suicide rates among active military might be related to more waivers that allowed people to enlist who would not ordinarily be eligible, and/or to higher rates of deployment. He went on to talk about Army STARRS (Army Study to Assess Risk and Resilience in Servicemembers).
“STARRS devoted $50 million over 5 years to the largest suicide study and did not find an effect of waivers. They did report a higher suicide rate among those who were deployed, however. But then Tim Bullman in my office looked at suicide rates 7 years after separation from service, and he reported a higher suicide rate among those who were never deployed.” The VA studies, I quickly realized, were also confusing and contradictory.
The VA has greatly expanded its mental health and suicide prevention services. For veterans overall, suicide rates have stabilized, but they have not decreased. For those veterans with psychiatric disorders, however, the suicide rates have gone down.
“When you ask ‘does treatment matter?’ it’s so hard to disentangle psychotherapy from pharmacotherapy. Over the past decade, we’ve seen a significant decrease in the suicide rate among those veterans with mental health disorders. We’ve looked at suicide rates every way you can think of. One thing we do know is that the better the relationship with the clinician, the lower the suicide risk.”
We talked about the role of hospitalization in preventing suicide, and Dr. Bossarte noted that the highest risk for suicide is immediately following hospital discharge.
“We are looking at people hospitalized after their first-ever suicide attempts and rates of mortality, including suicidal behavior, for 1 year after discharge. In very preliminary findings, we didn’t see any difference in the outcome for either all-cause mortality or repeat suicide attempts in those who were hospitalized, compared to those who were not. We don’t yet know about completed suicide.”
I left my discussion with Dr. Bossarte with more questions than answers. We have reason to believe that treatment helps, but we still don’t know which treatments help which people, and we do know that treatment doesn’t prevent suicide in every patient. In a culture where “treatment” has come to be equated with “prescribing” and is often based on a checklist of symptoms done by a primary care clinician, one might wonder if combining psychotherapy and medication – an increasingly rare offering – might have a better outcome. Simply put, for a problem that prematurely takes more than 40,000 lives a year, we know much too little.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Catching up on brain stimulation with Dr. Irving Reti
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Psychiatry is a field where the treatment of our disorders remains perplexing: We’re still trying to figure out if the best way to treat psychiatric conditions is through psychotherapy, with medications, or for more resistant conditions, by stimulating activity in the brain in several different ways.
The field of brain stimulation includes electroconvulsive therapy, as well as transcranial magnetic stimulation (TMS), direct transcranial current stimulation (tDCS), and deep brain stimulation (DBS), all of which are examples of treatments that are still just coming into their own.
In search of an update on brain stimulation, I met with Dr. Irving Reti, director of the Johns Hopkins Hospital Brain Stimulation Program and editor of “Brain Stimulation: Methodologies and Interventions” (Hoboken, N.J.: Wiley-Blackwell, 2015). We met at a Starbucks in Baltimore, and I’ll tell you that a one-on-one conversation with an expert is a wonderful way to learn about state-of-the-art treatments, the only downside being that Starbucks does not offer CME credit.
Dr. Reti, who went to medical school at the University of Sydney and speaks with a charming Australian accent, trained in psychiatry at Johns Hopkins, and then did a neuroscience fellowship.
“I’d just finished residency training, and I was giving ECT to rats. We were looking at the expression of immediate-early genes. At the same time, I started doing consults in the mood disorders clinic.”
In 2006, Dr. Reti took over as director of ECT at Hopkins, and that same year, Dr. Jimmy Potash got funding to study TMS. Dr. Potash has since moved to the University of Iowa, and Dr. Reti took over TMS administration at Hopkins. Dr. Reti was flattered to be approached by Wiley to edit “Brain Stimulation,” and he talked about how he was pleased with the final edition of the book.
“I ended up getting the top people to write the chapters, people like Sarah Lisanby, Michael Nitsche, John Rothwell, and Mark George. These are the leaders in the field of brain stimulation.”
I asked Dr. Reti to walk me through what was happening in each brain stimulation area.
“In ECT,” he said, “we know a lot more now about how both the settings and the anesthesia regimen affect the outcomes. We didn’t know this when I trained in the ’90s.” Dr. Reti estimated that he’s administered ECT to close to 2,000 patients.
TMS is done less often at Hopkins; he estimated that 10-20 patients receive the treatment, and each patient comes 30-40 times, with each session lasting 40 minutes.
“It’s better than medicine but not as effective as ECT. We’re seeing an efficacy rate around 50%-60%,” and he noted that some patients have trouble tolerating the procedure as the magnetic stimulation can be uncomfortable. “The TMS coil stimulates the scalp nerves and muscles immediately under the coil, which causes discomfort.” He noted that some patients need to premedicate with over-the-counter pain medicines.
“We’re also finding that low-frequency stimulation on the right can be helpful for anxiety,” Dr. Reti said.
He talked about treating patients with psychotherapy along with TMS. The brain changes are thought to increase the brain’s plasticity and perhaps make psychotherapy more effective.
“It’s being studied in drug treatment. You can show someone with an addiction stimuli to trigger cravings, and doing this with TMS may block the response,” he said.
He talked for a while about direct transcranial brain stimulation, which I was not very familiar with. Because it is being used to improve focus-playing video games, the equipment is not being marketed as a psychiatric treatment and doesn’t fall under the domain of the Food and Drug Administration.
“Kids are using it to improve their concentration and performance with video games; all you need is a 9-volt battery and some electrodes that are attached to the scalp. The kits cost about $250, but you can burn your scalp,” he said.
Dr. Reti referred me to an article in the New Yorker on tDCS, “Electrified: Adventures in transcranial direct-current stimulation” by Elif Batuman. He noted that there are studies in progress to look at therapeutic uses for tDCS, including one at Johns Hopkins where neuropsychologist David Schretlen is looking at improving cognition in schizophrenia. Dr. Reti is interested in seeing if tDCS might be helpful in decreasing self-injurious behaviors in autistic children, as ECT has been effective in severe cases. He noted that while ECT and TMS stimulate neurons in the brain to fire, tDCS changes the stimulation threshold without directly causing the neurons to discharge.
Finally, we talked a little about deep brain stimulation. Thin electrodes directly target nodes in brain circuits that can modulate the activity of those circuits. He noted that deep brain stimulation was being used at Johns Hopkins to treat Parkinson’s disease, and other centers have looked at its use for severe obsessive-compulsive disorder and treatment-resistant depression.
“We know that the response habituates; now they are trying on-demand DBS,” Dr. Reti noted.
So, although I got no continuing medical education credits, I did get to try a new Starbucks drink while having a very stimulating discussion on the latest convulsive and nonconvulsive psychiatric brain research.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Single-session psychiatry at 11,000 feet
The woman sitting across from me talked, through two translators (Quechua to Spanish to English) about how sad she had been since the death of her husband last year. “I eat alone,” she said, and my Spanish translator, a native Peruvian, explained the cultural significance of such a phrase to me. Eating alone is not a good thing; sometimes it’s how people are shunned. The woman talked about her adult children and how little contact she had with them, a continual disappointment in a poor rural area where the younger generation often flocked to the city and the hope of a better life.
She was in her 60s and dressed in the traditional attire of the indigenous people of the Andes: a high bowler hat, layers of sweaters, a long skirt, and woolen stockings. Her long black braids remained ageless in a land where somehow hair does not turn gray, but her bronze skin was leathery from generations in the sun. Her problems – grief and loneliness – are universal issues, and while she had moments where she longed for death, she felt her animals, and her cow in particular, needed her now.
Months ago, a friend – an internist – asked if my husband and I would join him, his wife, and some other families we knew on a volunteer medical mission to Peru. Hands Across the Americas is an organization founded by Jennifer Diamond and it has sent 27 medical and surgical missions to Latin America to serve those with limited access to medical treatments. I hesitated when I heard the request, and in case I wasn’t entranced by the idea of spending a week addressing the mental health needs of indigenous people in remote Andean villages, he added that another friend of ours, Patricia Poppe, a native of Peru and an expert on health communications at the Johns Hopkins School of Public Health, was eager to show our group of friends around her homeland before we all joined the mission. With this, I was sold on the whole adventure. I will spare you the details of our wonderful vacation, but will share with you, instead, what I learned about psychiatry in the Andes.
The mission orientation began in Cusco, Peru’s second-largest city and a way station for travelers headed to Machu Picchu. The tourist district of Cusco is a beautiful and fascinating city that reflects both Incan and pre-Incan Latin America and the heavy Spanish influence brought by the 16th- century conquistadors. While the city is beautiful, and the worlds have intertwined over the centuries, it remains a land where there is tension between the different cultures.
At just over 11,000 feet, the air is thin and visitors get easily winded just walking the hills. The villages we worked in were all about an hour outside of Cusco. They were impoverished and dilapidated, with some of the homes still constructed of bricks made from mud and straw. Dogs and farm animals roamed the streets. July is midwinter there, and it’s the dry season, so everything – and everyone – was covered in a layer of Andean grit. By the end of each day, we were as well.
I wish I could say that I wasn’t anxious about the work, but I was. What can a psychiatrist do in a single visit, much less a single session that requires one, and occasionally two, translators, in a population where I had no knowledge of their culture or resources? I didn’t know what types of patients I might see, if using medication would be reasonable, or if follow-up of any kind would be feasible. In the 27 missions of Hands Across the Americas, I was to be the first psychiatrist.
Four years earlier, a psychologist, Dr. David Doolittle, had gone with another psychologist, and when we spoke on the phone, he was very enthusiastic. He told me that this had been one of the best experiences of his professional life, and he was pleased to hear that mental health would continue to be a part of the agenda.
Finally, I should add that despite my hesitation about how helpful I might be as part of a medical team offering one-time services, I did have a similar experience in a different setting; In 2005, I volunteered for 2 weeks with the Substance Abuse and Mental Health Services Administration’s Katrina Assistance Project, and while I wondered then if my efforts were helpful to those I was trying to serve, I walked away feeling that I personally had gotten a great deal from the experience. I decided I would go to Peru with limited expectations and one simple agenda: I would try to be helpful.
The mission started with a brief orientation in Cusco, and it didn’t escape me when the medical director announced that patients could be seen by internal medicine, pediatrics, ENT, gynecology, and optometry. Psychiatry was strangely missing from the list, and when I pointed this out, he told me he had a special job for me: to run the pharmacy. While I was happy to help dispense medications, I had the sense that this population might have unmet mental health needs and suggested that it could be worthwhile to offer psychiatry as a specialty as well!
While the group came with an extensive supply of medications, vitamins, reading glasses, toothbrushes, and some wheelchairs, canes, and walkers, there were no psychotropic medications in the stash. I spoke with a local doctor who served as a liaison, and learned that he was familiar only with diazepam and alprazolam. Psychiatric patients were referred to doctors in Cusco, and local doctors did not prescribe antidepressants. For complex issues that required medical or surgical subspecialization, the referrals were even more complex: Patients traveled 18 hours by bus to be treated in Lima.
On the morning of our first clinic, I was given a small supply of fluoxetine (per my request) and alprazolam. Over 5 days we worked in three sites. On the first day, we were at the municipal center in Huarocondo, a little more than an hour outside of Cusco. Tents were set up inside the building, with the waiting room, triage, and pharmacy all stationed outside on the dirt. Inside, there was very little light, and like the other places we’d set up, no heat. My tent had a table and two chairs meant for primary school children, and I absconded with an adult-sized plastic chair for my interpreter. We had no access to medical records, no labs or radiographic equipment, and no clear place to send anyone for follow-up – this was true across all specialties, though the ENT who was working with us had come with suitcases full of his own equipment. Patients didn’t know what a psychiatrist or psychologist was, and some responded to questions about depression by saying that their blood pressure was just fine. Triage resorted to asking people if they felt sad and wanted to talk to a doctor about it.
The next 2 days, we worked in medical clinics in Ancahuasi and Anta, and while the conditions were more conducive to providing medical care, there was still no heat, the lighting was poor, and the buildings had not seen new coats of paint or furniture in many years. The clinics did not have psychiatrists, but they did each have a psychologist, and a couple of the people I saw had been seen. I was also told that fluoxetine could be obtained in Anta.
Hundreds of patients came each day, and all told, more than a thousand patients were seen by nine doctors in those 5 days. My official psychiatry tally was 79, but my personal count was less – I imagine some people became impatient with the long line and left without being seen – I recorded visits with 8-15 people each day.
First, let me say that I was surprised at the lack of pure psychopathology; the issues were more reactions to tremendous deprivation, violence, loneliness, medical and developmental disorders, and chronic struggles. I saw only two adult men, the rest of the patients were women and a few children. No one I saw had ever seen a psychiatrist before, and no one had taken psychotropic medications (not even the diazepam or alprazolam, which I was told could be obtained), and in fact, very few were on any medications of any kind. No one had ever been in a psychiatric hospital. Poverty was rampant, as was domestic violence: Men beat their wives, parents beat their children, and there seemed to be no societal means to interrupt this. One bruised woman said her husband had been released from jail in a day, and several women spoke of living in fear for their lives; still, their families encouraged them to stay with men who were abusive or unfaithful. I was told that the statistic for spousal abuse in Peru was 60%, in Cusco it was 75%; I suspect it was even higher in these outlying villages. Families were fractured; employment was physically very difficult; and stress was extreme. Low mood and poor sleep were pervasive, but given the fact that I was unsure if people could get follow-up or even afford to refill medications, I gave out very little in the way of medications, and used the fluoxetine only for a few people where I felt their mood and circumstances were so dire that perhaps it would help – and it seemed unlikely to hurt. I was able to hospitalize one 18-year-old mother who was suicidal and said she had tried to hang herself, though she was released early the next morning before she was ever seen by a doctor; she did note she felt much better and was grateful for the help.
Despite tremendous stresses and limited access to care, the suicide rate in Peru are quite low at 3.2 per 100,000 (as compared with nearly 14 per 100,000 in the United States), and despite the fact that some of the patients I saw had considered it, most said that their children or animals needed them, and there are religious prohibitions.
At moments, I wondered what I could possibly offer. One woman came in with a 5-year-old child with Down syndrome strapped to her, and another, older, developmentally delayed child in tow. There were other children at home, and while many women noted that their husbands beat them while they were drunk, this woman said her husband was calmer when he was drinking; he beat her when he was sober. I asked her what would help, and she said she needed money. Feeling I had nothing else to offer, I did something I have never done in my years as a psychiatrist: I gave her money. I hoped that she would spend it on something that might provide a moment of relief from her anguished life.
For the most part, it was interesting work, and often, it felt useful to make psychological interventions, to validate the distress the patients felt and to reorient them to seeing their own strengths. The people talked of holding their problems close, and of a relief and ease that came with sharing their difficulties.
In the end, I did feel helpful for at least some of the patients some of the time. At the very least, I felt appreciated – in one clinic, we were greeted by the mayor and a band – and patients expressed their thanks to both me and my cadre of interpreters, sometimes profusely. In the end, it was an adventure, from the vacation with 16 people to Lima, the Sacred Valley, and Machu Picchu, to my foray into high-volume, single-session psychiatry in a culture so vastly different from my own.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
The woman sitting across from me talked, through two translators (Quechua to Spanish to English) about how sad she had been since the death of her husband last year. “I eat alone,” she said, and my Spanish translator, a native Peruvian, explained the cultural significance of such a phrase to me. Eating alone is not a good thing; sometimes it’s how people are shunned. The woman talked about her adult children and how little contact she had with them, a continual disappointment in a poor rural area where the younger generation often flocked to the city and the hope of a better life.
She was in her 60s and dressed in the traditional attire of the indigenous people of the Andes: a high bowler hat, layers of sweaters, a long skirt, and woolen stockings. Her long black braids remained ageless in a land where somehow hair does not turn gray, but her bronze skin was leathery from generations in the sun. Her problems – grief and loneliness – are universal issues, and while she had moments where she longed for death, she felt her animals, and her cow in particular, needed her now.
Months ago, a friend – an internist – asked if my husband and I would join him, his wife, and some other families we knew on a volunteer medical mission to Peru. Hands Across the Americas is an organization founded by Jennifer Diamond and it has sent 27 medical and surgical missions to Latin America to serve those with limited access to medical treatments. I hesitated when I heard the request, and in case I wasn’t entranced by the idea of spending a week addressing the mental health needs of indigenous people in remote Andean villages, he added that another friend of ours, Patricia Poppe, a native of Peru and an expert on health communications at the Johns Hopkins School of Public Health, was eager to show our group of friends around her homeland before we all joined the mission. With this, I was sold on the whole adventure. I will spare you the details of our wonderful vacation, but will share with you, instead, what I learned about psychiatry in the Andes.
The mission orientation began in Cusco, Peru’s second-largest city and a way station for travelers headed to Machu Picchu. The tourist district of Cusco is a beautiful and fascinating city that reflects both Incan and pre-Incan Latin America and the heavy Spanish influence brought by the 16th- century conquistadors. While the city is beautiful, and the worlds have intertwined over the centuries, it remains a land where there is tension between the different cultures.
At just over 11,000 feet, the air is thin and visitors get easily winded just walking the hills. The villages we worked in were all about an hour outside of Cusco. They were impoverished and dilapidated, with some of the homes still constructed of bricks made from mud and straw. Dogs and farm animals roamed the streets. July is midwinter there, and it’s the dry season, so everything – and everyone – was covered in a layer of Andean grit. By the end of each day, we were as well.
I wish I could say that I wasn’t anxious about the work, but I was. What can a psychiatrist do in a single visit, much less a single session that requires one, and occasionally two, translators, in a population where I had no knowledge of their culture or resources? I didn’t know what types of patients I might see, if using medication would be reasonable, or if follow-up of any kind would be feasible. In the 27 missions of Hands Across the Americas, I was to be the first psychiatrist.
Four years earlier, a psychologist, Dr. David Doolittle, had gone with another psychologist, and when we spoke on the phone, he was very enthusiastic. He told me that this had been one of the best experiences of his professional life, and he was pleased to hear that mental health would continue to be a part of the agenda.
Finally, I should add that despite my hesitation about how helpful I might be as part of a medical team offering one-time services, I did have a similar experience in a different setting; In 2005, I volunteered for 2 weeks with the Substance Abuse and Mental Health Services Administration’s Katrina Assistance Project, and while I wondered then if my efforts were helpful to those I was trying to serve, I walked away feeling that I personally had gotten a great deal from the experience. I decided I would go to Peru with limited expectations and one simple agenda: I would try to be helpful.
The mission started with a brief orientation in Cusco, and it didn’t escape me when the medical director announced that patients could be seen by internal medicine, pediatrics, ENT, gynecology, and optometry. Psychiatry was strangely missing from the list, and when I pointed this out, he told me he had a special job for me: to run the pharmacy. While I was happy to help dispense medications, I had the sense that this population might have unmet mental health needs and suggested that it could be worthwhile to offer psychiatry as a specialty as well!
While the group came with an extensive supply of medications, vitamins, reading glasses, toothbrushes, and some wheelchairs, canes, and walkers, there were no psychotropic medications in the stash. I spoke with a local doctor who served as a liaison, and learned that he was familiar only with diazepam and alprazolam. Psychiatric patients were referred to doctors in Cusco, and local doctors did not prescribe antidepressants. For complex issues that required medical or surgical subspecialization, the referrals were even more complex: Patients traveled 18 hours by bus to be treated in Lima.
On the morning of our first clinic, I was given a small supply of fluoxetine (per my request) and alprazolam. Over 5 days we worked in three sites. On the first day, we were at the municipal center in Huarocondo, a little more than an hour outside of Cusco. Tents were set up inside the building, with the waiting room, triage, and pharmacy all stationed outside on the dirt. Inside, there was very little light, and like the other places we’d set up, no heat. My tent had a table and two chairs meant for primary school children, and I absconded with an adult-sized plastic chair for my interpreter. We had no access to medical records, no labs or radiographic equipment, and no clear place to send anyone for follow-up – this was true across all specialties, though the ENT who was working with us had come with suitcases full of his own equipment. Patients didn’t know what a psychiatrist or psychologist was, and some responded to questions about depression by saying that their blood pressure was just fine. Triage resorted to asking people if they felt sad and wanted to talk to a doctor about it.
The next 2 days, we worked in medical clinics in Ancahuasi and Anta, and while the conditions were more conducive to providing medical care, there was still no heat, the lighting was poor, and the buildings had not seen new coats of paint or furniture in many years. The clinics did not have psychiatrists, but they did each have a psychologist, and a couple of the people I saw had been seen. I was also told that fluoxetine could be obtained in Anta.
Hundreds of patients came each day, and all told, more than a thousand patients were seen by nine doctors in those 5 days. My official psychiatry tally was 79, but my personal count was less – I imagine some people became impatient with the long line and left without being seen – I recorded visits with 8-15 people each day.
First, let me say that I was surprised at the lack of pure psychopathology; the issues were more reactions to tremendous deprivation, violence, loneliness, medical and developmental disorders, and chronic struggles. I saw only two adult men, the rest of the patients were women and a few children. No one I saw had ever seen a psychiatrist before, and no one had taken psychotropic medications (not even the diazepam or alprazolam, which I was told could be obtained), and in fact, very few were on any medications of any kind. No one had ever been in a psychiatric hospital. Poverty was rampant, as was domestic violence: Men beat their wives, parents beat their children, and there seemed to be no societal means to interrupt this. One bruised woman said her husband had been released from jail in a day, and several women spoke of living in fear for their lives; still, their families encouraged them to stay with men who were abusive or unfaithful. I was told that the statistic for spousal abuse in Peru was 60%, in Cusco it was 75%; I suspect it was even higher in these outlying villages. Families were fractured; employment was physically very difficult; and stress was extreme. Low mood and poor sleep were pervasive, but given the fact that I was unsure if people could get follow-up or even afford to refill medications, I gave out very little in the way of medications, and used the fluoxetine only for a few people where I felt their mood and circumstances were so dire that perhaps it would help – and it seemed unlikely to hurt. I was able to hospitalize one 18-year-old mother who was suicidal and said she had tried to hang herself, though she was released early the next morning before she was ever seen by a doctor; she did note she felt much better and was grateful for the help.
Despite tremendous stresses and limited access to care, the suicide rate in Peru are quite low at 3.2 per 100,000 (as compared with nearly 14 per 100,000 in the United States), and despite the fact that some of the patients I saw had considered it, most said that their children or animals needed them, and there are religious prohibitions.
At moments, I wondered what I could possibly offer. One woman came in with a 5-year-old child with Down syndrome strapped to her, and another, older, developmentally delayed child in tow. There were other children at home, and while many women noted that their husbands beat them while they were drunk, this woman said her husband was calmer when he was drinking; he beat her when he was sober. I asked her what would help, and she said she needed money. Feeling I had nothing else to offer, I did something I have never done in my years as a psychiatrist: I gave her money. I hoped that she would spend it on something that might provide a moment of relief from her anguished life.
For the most part, it was interesting work, and often, it felt useful to make psychological interventions, to validate the distress the patients felt and to reorient them to seeing their own strengths. The people talked of holding their problems close, and of a relief and ease that came with sharing their difficulties.
In the end, I did feel helpful for at least some of the patients some of the time. At the very least, I felt appreciated – in one clinic, we were greeted by the mayor and a band – and patients expressed their thanks to both me and my cadre of interpreters, sometimes profusely. In the end, it was an adventure, from the vacation with 16 people to Lima, the Sacred Valley, and Machu Picchu, to my foray into high-volume, single-session psychiatry in a culture so vastly different from my own.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
The woman sitting across from me talked, through two translators (Quechua to Spanish to English) about how sad she had been since the death of her husband last year. “I eat alone,” she said, and my Spanish translator, a native Peruvian, explained the cultural significance of such a phrase to me. Eating alone is not a good thing; sometimes it’s how people are shunned. The woman talked about her adult children and how little contact she had with them, a continual disappointment in a poor rural area where the younger generation often flocked to the city and the hope of a better life.
She was in her 60s and dressed in the traditional attire of the indigenous people of the Andes: a high bowler hat, layers of sweaters, a long skirt, and woolen stockings. Her long black braids remained ageless in a land where somehow hair does not turn gray, but her bronze skin was leathery from generations in the sun. Her problems – grief and loneliness – are universal issues, and while she had moments where she longed for death, she felt her animals, and her cow in particular, needed her now.
Months ago, a friend – an internist – asked if my husband and I would join him, his wife, and some other families we knew on a volunteer medical mission to Peru. Hands Across the Americas is an organization founded by Jennifer Diamond and it has sent 27 medical and surgical missions to Latin America to serve those with limited access to medical treatments. I hesitated when I heard the request, and in case I wasn’t entranced by the idea of spending a week addressing the mental health needs of indigenous people in remote Andean villages, he added that another friend of ours, Patricia Poppe, a native of Peru and an expert on health communications at the Johns Hopkins School of Public Health, was eager to show our group of friends around her homeland before we all joined the mission. With this, I was sold on the whole adventure. I will spare you the details of our wonderful vacation, but will share with you, instead, what I learned about psychiatry in the Andes.
The mission orientation began in Cusco, Peru’s second-largest city and a way station for travelers headed to Machu Picchu. The tourist district of Cusco is a beautiful and fascinating city that reflects both Incan and pre-Incan Latin America and the heavy Spanish influence brought by the 16th- century conquistadors. While the city is beautiful, and the worlds have intertwined over the centuries, it remains a land where there is tension between the different cultures.
At just over 11,000 feet, the air is thin and visitors get easily winded just walking the hills. The villages we worked in were all about an hour outside of Cusco. They were impoverished and dilapidated, with some of the homes still constructed of bricks made from mud and straw. Dogs and farm animals roamed the streets. July is midwinter there, and it’s the dry season, so everything – and everyone – was covered in a layer of Andean grit. By the end of each day, we were as well.
I wish I could say that I wasn’t anxious about the work, but I was. What can a psychiatrist do in a single visit, much less a single session that requires one, and occasionally two, translators, in a population where I had no knowledge of their culture or resources? I didn’t know what types of patients I might see, if using medication would be reasonable, or if follow-up of any kind would be feasible. In the 27 missions of Hands Across the Americas, I was to be the first psychiatrist.
Four years earlier, a psychologist, Dr. David Doolittle, had gone with another psychologist, and when we spoke on the phone, he was very enthusiastic. He told me that this had been one of the best experiences of his professional life, and he was pleased to hear that mental health would continue to be a part of the agenda.
Finally, I should add that despite my hesitation about how helpful I might be as part of a medical team offering one-time services, I did have a similar experience in a different setting; In 2005, I volunteered for 2 weeks with the Substance Abuse and Mental Health Services Administration’s Katrina Assistance Project, and while I wondered then if my efforts were helpful to those I was trying to serve, I walked away feeling that I personally had gotten a great deal from the experience. I decided I would go to Peru with limited expectations and one simple agenda: I would try to be helpful.
The mission started with a brief orientation in Cusco, and it didn’t escape me when the medical director announced that patients could be seen by internal medicine, pediatrics, ENT, gynecology, and optometry. Psychiatry was strangely missing from the list, and when I pointed this out, he told me he had a special job for me: to run the pharmacy. While I was happy to help dispense medications, I had the sense that this population might have unmet mental health needs and suggested that it could be worthwhile to offer psychiatry as a specialty as well!
While the group came with an extensive supply of medications, vitamins, reading glasses, toothbrushes, and some wheelchairs, canes, and walkers, there were no psychotropic medications in the stash. I spoke with a local doctor who served as a liaison, and learned that he was familiar only with diazepam and alprazolam. Psychiatric patients were referred to doctors in Cusco, and local doctors did not prescribe antidepressants. For complex issues that required medical or surgical subspecialization, the referrals were even more complex: Patients traveled 18 hours by bus to be treated in Lima.
On the morning of our first clinic, I was given a small supply of fluoxetine (per my request) and alprazolam. Over 5 days we worked in three sites. On the first day, we were at the municipal center in Huarocondo, a little more than an hour outside of Cusco. Tents were set up inside the building, with the waiting room, triage, and pharmacy all stationed outside on the dirt. Inside, there was very little light, and like the other places we’d set up, no heat. My tent had a table and two chairs meant for primary school children, and I absconded with an adult-sized plastic chair for my interpreter. We had no access to medical records, no labs or radiographic equipment, and no clear place to send anyone for follow-up – this was true across all specialties, though the ENT who was working with us had come with suitcases full of his own equipment. Patients didn’t know what a psychiatrist or psychologist was, and some responded to questions about depression by saying that their blood pressure was just fine. Triage resorted to asking people if they felt sad and wanted to talk to a doctor about it.
The next 2 days, we worked in medical clinics in Ancahuasi and Anta, and while the conditions were more conducive to providing medical care, there was still no heat, the lighting was poor, and the buildings had not seen new coats of paint or furniture in many years. The clinics did not have psychiatrists, but they did each have a psychologist, and a couple of the people I saw had been seen. I was also told that fluoxetine could be obtained in Anta.
Hundreds of patients came each day, and all told, more than a thousand patients were seen by nine doctors in those 5 days. My official psychiatry tally was 79, but my personal count was less – I imagine some people became impatient with the long line and left without being seen – I recorded visits with 8-15 people each day.
First, let me say that I was surprised at the lack of pure psychopathology; the issues were more reactions to tremendous deprivation, violence, loneliness, medical and developmental disorders, and chronic struggles. I saw only two adult men, the rest of the patients were women and a few children. No one I saw had ever seen a psychiatrist before, and no one had taken psychotropic medications (not even the diazepam or alprazolam, which I was told could be obtained), and in fact, very few were on any medications of any kind. No one had ever been in a psychiatric hospital. Poverty was rampant, as was domestic violence: Men beat their wives, parents beat their children, and there seemed to be no societal means to interrupt this. One bruised woman said her husband had been released from jail in a day, and several women spoke of living in fear for their lives; still, their families encouraged them to stay with men who were abusive or unfaithful. I was told that the statistic for spousal abuse in Peru was 60%, in Cusco it was 75%; I suspect it was even higher in these outlying villages. Families were fractured; employment was physically very difficult; and stress was extreme. Low mood and poor sleep were pervasive, but given the fact that I was unsure if people could get follow-up or even afford to refill medications, I gave out very little in the way of medications, and used the fluoxetine only for a few people where I felt their mood and circumstances were so dire that perhaps it would help – and it seemed unlikely to hurt. I was able to hospitalize one 18-year-old mother who was suicidal and said she had tried to hang herself, though she was released early the next morning before she was ever seen by a doctor; she did note she felt much better and was grateful for the help.
Despite tremendous stresses and limited access to care, the suicide rate in Peru are quite low at 3.2 per 100,000 (as compared with nearly 14 per 100,000 in the United States), and despite the fact that some of the patients I saw had considered it, most said that their children or animals needed them, and there are religious prohibitions.
At moments, I wondered what I could possibly offer. One woman came in with a 5-year-old child with Down syndrome strapped to her, and another, older, developmentally delayed child in tow. There were other children at home, and while many women noted that their husbands beat them while they were drunk, this woman said her husband was calmer when he was drinking; he beat her when he was sober. I asked her what would help, and she said she needed money. Feeling I had nothing else to offer, I did something I have never done in my years as a psychiatrist: I gave her money. I hoped that she would spend it on something that might provide a moment of relief from her anguished life.
For the most part, it was interesting work, and often, it felt useful to make psychological interventions, to validate the distress the patients felt and to reorient them to seeing their own strengths. The people talked of holding their problems close, and of a relief and ease that came with sharing their difficulties.
In the end, I did feel helpful for at least some of the patients some of the time. At the very least, I felt appreciated – in one clinic, we were greeted by the mayor and a band – and patients expressed their thanks to both me and my cadre of interpreters, sometimes profusely. In the end, it was an adventure, from the vacation with 16 people to Lima, the Sacred Valley, and Machu Picchu, to my foray into high-volume, single-session psychiatry in a culture so vastly different from my own.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
H.R. 2646 vs. H.R. 3717: The difference 2 years makes
In 2013, Rep. Tim Murphy (R-Pa.) proposed the Helping Families in Mental Health Crisis Act, H.R. 3717, as a response to the tragedy in Newtown, Conn. The legislation did not make it out of committee before the congressional session ended, and on June 4, a revised version of the bill – now H.R. 2646 – was introduced in Congress, cosponsored by Texas Democrat Rep. Eddie Bernice Johnson. The legislation is being framed as sweeping legislation “to fix America’s broken health system.” Those familiar with the original version may recall that controversial portions included a requirement for states to have legislation for outpatient civil commitment or lose funding, and allow caretakers to access information for mental health patients without patient consent. That version also proposed the shifting of funds from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health (NIMH) to promote research.
The text of H.R. 2646 is 173 pages long, nearly 40 pages longer than the original version of the bill Even those who are well versed in these issues are having trouble deciphering the new proposals.
Let me start with a rather unusual disclaimer for someone writing about a piece of legislation: I haven’t read the bill. Instead, I read the blog of journalist/advocate Pete Earley, after he went to the effort of reading the text, soliciting the opinions of leadership at several organizations, and putting together a list of comparisons between the 2013 and 2015 versions of the proposed legislation. In a piece headlined, “Murphy Introduces Revamped Mental Health Bill: Will It Fly This Time Around?” Earley compares the new 2015 bill to the original legislation proposed in 2013.
I’m going to summarize the differences Earley noted, and I’ll add his caveat that he is not certain that his interpretations are correct; the wording of the bill is confusing, and there is not yet agreement on what the different components of the legislation mean. Because the issues around requirements for outpatient commitment have been so volatile, let me add that Earley did communicate with a staffer in Murphy’s office and confirmed that his understanding of that portion of the legislation is correct.
Earley noted eight main points:
1. Rather than removing funding from SAMHSA and shifting it to the NIMH, the new bill gives oversight for mental health care and funding to an assistant secretary for mental health and substance abuse treatment within the Department of Health and Human Services. The bill stipulates that the position must be held by a psychiatrist or psychologist.
2. In H.R. 2646, this funding would be provided only for programs recognized as evidence-based practices; it does not target specific SAMHSA programs for elimination.
3. States that implement outpatient civil commitment would receive a 2% increase in block funding grants. In the original version, states without this legislation would lose federal funding.
4. The new bill allows psychiatrists to share only specific information with caretakers without patient consent: diagnoses, treatment plans, and information about medications but not psychotherapy notes.
5. Murphy’s bill would repeal the so-called IMD (institutions for mental disease) exclusion for facilities with more than 16 beds as long as a facility kept patients less than an average of 30 days.
6. In the original version of the bill, Murphy wanted to eliminate funding to protection and advocacy agencies charged with protecting patients’ rights. The 2015 version bill would limit the powers of advocates by restricting their authority to the investigation of abuse and neglect, and would forbid these agencies from lobbying and from “counseling an individual with a serious mental illness who lacks insight into their condition on refusing medical treatment or acting against the wishes of such individual’s caregiver.”
7. The newer version eliminates the 190-day lifetime cap on inpatient psychiatric hospitalizations in Medicare.
8. H.R. 2646 encourages funding and support for peer-to-peer programs, but sets standards for peers and requires their work to be monitored by a mental health professional.
Obviously, legislation of this length includes much more, but these were the differences Earley identified in his comparison to text of the first version. His Website includes more detail and explanation of these points, and I encourage you to visit PeteEarley.com.
Days after the introduction of the bill, now known as the Murphy-Johnson Act, American Psychiatric Association President Renée Binder and CEO Saul Levin wrote a letter of support for the bill. The letter outlines some of the major issues that the legislation addresses, including increases to the psychiatric workforce. In it, they note: “This is historic legislation that would, for the first time in decades, bring systemwide reforms and improvements to care for our patients and for those who currently lack access to needed treatment.”
A hearing will be held on the bill today.
With thanks to Pete Earley who allowed me to hijack his article.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011). Follow Dr. Miller on Twitter @shrinkrapdinah.
In 2013, Rep. Tim Murphy (R-Pa.) proposed the Helping Families in Mental Health Crisis Act, H.R. 3717, as a response to the tragedy in Newtown, Conn. The legislation did not make it out of committee before the congressional session ended, and on June 4, a revised version of the bill – now H.R. 2646 – was introduced in Congress, cosponsored by Texas Democrat Rep. Eddie Bernice Johnson. The legislation is being framed as sweeping legislation “to fix America’s broken health system.” Those familiar with the original version may recall that controversial portions included a requirement for states to have legislation for outpatient civil commitment or lose funding, and allow caretakers to access information for mental health patients without patient consent. That version also proposed the shifting of funds from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health (NIMH) to promote research.
The text of H.R. 2646 is 173 pages long, nearly 40 pages longer than the original version of the bill Even those who are well versed in these issues are having trouble deciphering the new proposals.
Let me start with a rather unusual disclaimer for someone writing about a piece of legislation: I haven’t read the bill. Instead, I read the blog of journalist/advocate Pete Earley, after he went to the effort of reading the text, soliciting the opinions of leadership at several organizations, and putting together a list of comparisons between the 2013 and 2015 versions of the proposed legislation. In a piece headlined, “Murphy Introduces Revamped Mental Health Bill: Will It Fly This Time Around?” Earley compares the new 2015 bill to the original legislation proposed in 2013.
I’m going to summarize the differences Earley noted, and I’ll add his caveat that he is not certain that his interpretations are correct; the wording of the bill is confusing, and there is not yet agreement on what the different components of the legislation mean. Because the issues around requirements for outpatient commitment have been so volatile, let me add that Earley did communicate with a staffer in Murphy’s office and confirmed that his understanding of that portion of the legislation is correct.
Earley noted eight main points:
1. Rather than removing funding from SAMHSA and shifting it to the NIMH, the new bill gives oversight for mental health care and funding to an assistant secretary for mental health and substance abuse treatment within the Department of Health and Human Services. The bill stipulates that the position must be held by a psychiatrist or psychologist.
2. In H.R. 2646, this funding would be provided only for programs recognized as evidence-based practices; it does not target specific SAMHSA programs for elimination.
3. States that implement outpatient civil commitment would receive a 2% increase in block funding grants. In the original version, states without this legislation would lose federal funding.
4. The new bill allows psychiatrists to share only specific information with caretakers without patient consent: diagnoses, treatment plans, and information about medications but not psychotherapy notes.
5. Murphy’s bill would repeal the so-called IMD (institutions for mental disease) exclusion for facilities with more than 16 beds as long as a facility kept patients less than an average of 30 days.
6. In the original version of the bill, Murphy wanted to eliminate funding to protection and advocacy agencies charged with protecting patients’ rights. The 2015 version bill would limit the powers of advocates by restricting their authority to the investigation of abuse and neglect, and would forbid these agencies from lobbying and from “counseling an individual with a serious mental illness who lacks insight into their condition on refusing medical treatment or acting against the wishes of such individual’s caregiver.”
7. The newer version eliminates the 190-day lifetime cap on inpatient psychiatric hospitalizations in Medicare.
8. H.R. 2646 encourages funding and support for peer-to-peer programs, but sets standards for peers and requires their work to be monitored by a mental health professional.
Obviously, legislation of this length includes much more, but these were the differences Earley identified in his comparison to text of the first version. His Website includes more detail and explanation of these points, and I encourage you to visit PeteEarley.com.
Days after the introduction of the bill, now known as the Murphy-Johnson Act, American Psychiatric Association President Renée Binder and CEO Saul Levin wrote a letter of support for the bill. The letter outlines some of the major issues that the legislation addresses, including increases to the psychiatric workforce. In it, they note: “This is historic legislation that would, for the first time in decades, bring systemwide reforms and improvements to care for our patients and for those who currently lack access to needed treatment.”
A hearing will be held on the bill today.
With thanks to Pete Earley who allowed me to hijack his article.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011). Follow Dr. Miller on Twitter @shrinkrapdinah.
In 2013, Rep. Tim Murphy (R-Pa.) proposed the Helping Families in Mental Health Crisis Act, H.R. 3717, as a response to the tragedy in Newtown, Conn. The legislation did not make it out of committee before the congressional session ended, and on June 4, a revised version of the bill – now H.R. 2646 – was introduced in Congress, cosponsored by Texas Democrat Rep. Eddie Bernice Johnson. The legislation is being framed as sweeping legislation “to fix America’s broken health system.” Those familiar with the original version may recall that controversial portions included a requirement for states to have legislation for outpatient civil commitment or lose funding, and allow caretakers to access information for mental health patients without patient consent. That version also proposed the shifting of funds from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health (NIMH) to promote research.
The text of H.R. 2646 is 173 pages long, nearly 40 pages longer than the original version of the bill Even those who are well versed in these issues are having trouble deciphering the new proposals.
Let me start with a rather unusual disclaimer for someone writing about a piece of legislation: I haven’t read the bill. Instead, I read the blog of journalist/advocate Pete Earley, after he went to the effort of reading the text, soliciting the opinions of leadership at several organizations, and putting together a list of comparisons between the 2013 and 2015 versions of the proposed legislation. In a piece headlined, “Murphy Introduces Revamped Mental Health Bill: Will It Fly This Time Around?” Earley compares the new 2015 bill to the original legislation proposed in 2013.
I’m going to summarize the differences Earley noted, and I’ll add his caveat that he is not certain that his interpretations are correct; the wording of the bill is confusing, and there is not yet agreement on what the different components of the legislation mean. Because the issues around requirements for outpatient commitment have been so volatile, let me add that Earley did communicate with a staffer in Murphy’s office and confirmed that his understanding of that portion of the legislation is correct.
Earley noted eight main points:
1. Rather than removing funding from SAMHSA and shifting it to the NIMH, the new bill gives oversight for mental health care and funding to an assistant secretary for mental health and substance abuse treatment within the Department of Health and Human Services. The bill stipulates that the position must be held by a psychiatrist or psychologist.
2. In H.R. 2646, this funding would be provided only for programs recognized as evidence-based practices; it does not target specific SAMHSA programs for elimination.
3. States that implement outpatient civil commitment would receive a 2% increase in block funding grants. In the original version, states without this legislation would lose federal funding.
4. The new bill allows psychiatrists to share only specific information with caretakers without patient consent: diagnoses, treatment plans, and information about medications but not psychotherapy notes.
5. Murphy’s bill would repeal the so-called IMD (institutions for mental disease) exclusion for facilities with more than 16 beds as long as a facility kept patients less than an average of 30 days.
6. In the original version of the bill, Murphy wanted to eliminate funding to protection and advocacy agencies charged with protecting patients’ rights. The 2015 version bill would limit the powers of advocates by restricting their authority to the investigation of abuse and neglect, and would forbid these agencies from lobbying and from “counseling an individual with a serious mental illness who lacks insight into their condition on refusing medical treatment or acting against the wishes of such individual’s caregiver.”
7. The newer version eliminates the 190-day lifetime cap on inpatient psychiatric hospitalizations in Medicare.
8. H.R. 2646 encourages funding and support for peer-to-peer programs, but sets standards for peers and requires their work to be monitored by a mental health professional.
Obviously, legislation of this length includes much more, but these were the differences Earley identified in his comparison to text of the first version. His Website includes more detail and explanation of these points, and I encourage you to visit PeteEarley.com.
Days after the introduction of the bill, now known as the Murphy-Johnson Act, American Psychiatric Association President Renée Binder and CEO Saul Levin wrote a letter of support for the bill. The letter outlines some of the major issues that the legislation addresses, including increases to the psychiatric workforce. In it, they note: “This is historic legislation that would, for the first time in decades, bring systemwide reforms and improvements to care for our patients and for those who currently lack access to needed treatment.”
A hearing will be held on the bill today.
With thanks to Pete Earley who allowed me to hijack his article.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011). Follow Dr. Miller on Twitter @shrinkrapdinah.
Was mental illness a factor in the Germanwings crash?
Earlier this week, an airplane headed from Barcelona to Dusseldorf crashed into the French Alps, leaving 150 people dead. The black box recorder indicated that the copilot was left alone in the cockpit, the pilot was locked out and attempted to gain re-entry, and the flight was reprogrammed to cruise at an altitude of 100 feet, causing the plane to crash after an 8-minute descent. The evidence indicates a deliberate action on the part of the 27-year-old co-pilot, Andreas Lubitz.
With nothing to point to terrorism at this point, the investigation will include the question of whether or not the copilot suffered from a mental illness as a way of explaining his unexplainable actions. In short, was this a combination mass murder/suicide? Was there any way to predict that such an atrocity might happen? Are there measures that can be taken to ensure that it doesn’t happen again?
In the United States, treatment with any psychotropic medication has been a reason to ground a pilot permanently. In April 2010, the Federal Aviation Administration’s rules changed such that a pilot could fly if he’d been treated for mild to moderate depression with a selective serotonin reuptake inhibitor after 12 months. At that time, the FAA announced a 6-month amnesty period where a pilot could come forward about a diagnosis of depression that he had not previously felt comfortable disclosing. Presumably, other countries also have rules that ground pilots for mental illness.
So far, some reports in the media indicate that the copilot was not obviously suffering from a psychiatric disorder; all those who have been interviewed for these reports have expressed shock that Lubitz might have deliberately crashed the plane.
There also has been speculation in the media that a break in the copilot’s training 6 years ago was due to depression, and the mother of a school mate reportedly said that Lubitz had been treated for depression. Finally, investigators found a doctor’s note excusing Lubitz from work. At this point, the Wall Street Journal is reporting that he was being treated for depression. Apparently, he had shredded the note and flew on Tuesday, despite the written work excuse.
Still, all discussion of the copilot’s mental state is purely speculation. The media is noted for sensationalist reporting – and in efforts to get information out quickly, the details are often confused or simply wrong, sometimes to a remarkable extent. We don’t know if the work excuse was written by a psychiatrist or another type of physician; we don’t know if it was for a psychiatric condition, cancer, or simply strep throat.
What we’ve been told is that a copilot who was cleared to fly did so despite a work excuse from a physician, he did not disclose this condition to his employer, and he crashed a plane killing 150 people.
We might assume that the pilot suffered from some type of psychic distress – whether he met criteria for a mental disorder or not, it’s not normal to kill 150 people. If the pilot did have a history of depression and was being treated at the time of this week’s flight, then we may be left with a very unsatisfactory answer.
The anti-psychiatry activists will say that psychotropic medications caused Lubitz to crash the plane. Psychiatrists will be left with no great answer with such a scenario and will be left to say that whatever treatment he was receiving, it wasn’t enough. Certainly, the physician who told Lubitz to take off from work was right: He didn’t belong in a cockpit that day. Presumably, that physician would have done more had he been aware that the patient was about to commit a mass murder.
If the copilot does have a history of depression, but his current work excuse was for an unrelated condition, we might wonder if an untreated recurrence of depression played some role in his actions. One might speculate that the copilot could have been afraid to seek care at this time, perhaps because of a fear that he would lose his vocation.
Still, major depression can hardly explain such an act, and it is unfortunate that the press has already begun to run headlines linking this man’s alleged psychiatric diagnosis to a catastrophic mass murder. Somehow, “mental illness” gets used as an endpoint explanation for why such things happen; and short of a severe psychotic delusional system, it’s a very unsatisfying answer for an unprecedented act of violence.
The facts will unfold and perhaps we’ll learn a little more. We’ll find out what condition the copilot was being treated for and whether there were other stresses going on in his personal life. But people get depressed, take antidepressants, and deal with stress all the time.
It’s possible, if not likely, that we’ll never understand why this copilot decided to end the lives of so many people along with his own.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: The Johns Hopkins University, 2011).
Earlier this week, an airplane headed from Barcelona to Dusseldorf crashed into the French Alps, leaving 150 people dead. The black box recorder indicated that the copilot was left alone in the cockpit, the pilot was locked out and attempted to gain re-entry, and the flight was reprogrammed to cruise at an altitude of 100 feet, causing the plane to crash after an 8-minute descent. The evidence indicates a deliberate action on the part of the 27-year-old co-pilot, Andreas Lubitz.
With nothing to point to terrorism at this point, the investigation will include the question of whether or not the copilot suffered from a mental illness as a way of explaining his unexplainable actions. In short, was this a combination mass murder/suicide? Was there any way to predict that such an atrocity might happen? Are there measures that can be taken to ensure that it doesn’t happen again?
In the United States, treatment with any psychotropic medication has been a reason to ground a pilot permanently. In April 2010, the Federal Aviation Administration’s rules changed such that a pilot could fly if he’d been treated for mild to moderate depression with a selective serotonin reuptake inhibitor after 12 months. At that time, the FAA announced a 6-month amnesty period where a pilot could come forward about a diagnosis of depression that he had not previously felt comfortable disclosing. Presumably, other countries also have rules that ground pilots for mental illness.
So far, some reports in the media indicate that the copilot was not obviously suffering from a psychiatric disorder; all those who have been interviewed for these reports have expressed shock that Lubitz might have deliberately crashed the plane.
There also has been speculation in the media that a break in the copilot’s training 6 years ago was due to depression, and the mother of a school mate reportedly said that Lubitz had been treated for depression. Finally, investigators found a doctor’s note excusing Lubitz from work. At this point, the Wall Street Journal is reporting that he was being treated for depression. Apparently, he had shredded the note and flew on Tuesday, despite the written work excuse.
Still, all discussion of the copilot’s mental state is purely speculation. The media is noted for sensationalist reporting – and in efforts to get information out quickly, the details are often confused or simply wrong, sometimes to a remarkable extent. We don’t know if the work excuse was written by a psychiatrist or another type of physician; we don’t know if it was for a psychiatric condition, cancer, or simply strep throat.
What we’ve been told is that a copilot who was cleared to fly did so despite a work excuse from a physician, he did not disclose this condition to his employer, and he crashed a plane killing 150 people.
We might assume that the pilot suffered from some type of psychic distress – whether he met criteria for a mental disorder or not, it’s not normal to kill 150 people. If the pilot did have a history of depression and was being treated at the time of this week’s flight, then we may be left with a very unsatisfactory answer.
The anti-psychiatry activists will say that psychotropic medications caused Lubitz to crash the plane. Psychiatrists will be left with no great answer with such a scenario and will be left to say that whatever treatment he was receiving, it wasn’t enough. Certainly, the physician who told Lubitz to take off from work was right: He didn’t belong in a cockpit that day. Presumably, that physician would have done more had he been aware that the patient was about to commit a mass murder.
If the copilot does have a history of depression, but his current work excuse was for an unrelated condition, we might wonder if an untreated recurrence of depression played some role in his actions. One might speculate that the copilot could have been afraid to seek care at this time, perhaps because of a fear that he would lose his vocation.
Still, major depression can hardly explain such an act, and it is unfortunate that the press has already begun to run headlines linking this man’s alleged psychiatric diagnosis to a catastrophic mass murder. Somehow, “mental illness” gets used as an endpoint explanation for why such things happen; and short of a severe psychotic delusional system, it’s a very unsatisfying answer for an unprecedented act of violence.
The facts will unfold and perhaps we’ll learn a little more. We’ll find out what condition the copilot was being treated for and whether there were other stresses going on in his personal life. But people get depressed, take antidepressants, and deal with stress all the time.
It’s possible, if not likely, that we’ll never understand why this copilot decided to end the lives of so many people along with his own.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: The Johns Hopkins University, 2011).
Earlier this week, an airplane headed from Barcelona to Dusseldorf crashed into the French Alps, leaving 150 people dead. The black box recorder indicated that the copilot was left alone in the cockpit, the pilot was locked out and attempted to gain re-entry, and the flight was reprogrammed to cruise at an altitude of 100 feet, causing the plane to crash after an 8-minute descent. The evidence indicates a deliberate action on the part of the 27-year-old co-pilot, Andreas Lubitz.
With nothing to point to terrorism at this point, the investigation will include the question of whether or not the copilot suffered from a mental illness as a way of explaining his unexplainable actions. In short, was this a combination mass murder/suicide? Was there any way to predict that such an atrocity might happen? Are there measures that can be taken to ensure that it doesn’t happen again?
In the United States, treatment with any psychotropic medication has been a reason to ground a pilot permanently. In April 2010, the Federal Aviation Administration’s rules changed such that a pilot could fly if he’d been treated for mild to moderate depression with a selective serotonin reuptake inhibitor after 12 months. At that time, the FAA announced a 6-month amnesty period where a pilot could come forward about a diagnosis of depression that he had not previously felt comfortable disclosing. Presumably, other countries also have rules that ground pilots for mental illness.
So far, some reports in the media indicate that the copilot was not obviously suffering from a psychiatric disorder; all those who have been interviewed for these reports have expressed shock that Lubitz might have deliberately crashed the plane.
There also has been speculation in the media that a break in the copilot’s training 6 years ago was due to depression, and the mother of a school mate reportedly said that Lubitz had been treated for depression. Finally, investigators found a doctor’s note excusing Lubitz from work. At this point, the Wall Street Journal is reporting that he was being treated for depression. Apparently, he had shredded the note and flew on Tuesday, despite the written work excuse.
Still, all discussion of the copilot’s mental state is purely speculation. The media is noted for sensationalist reporting – and in efforts to get information out quickly, the details are often confused or simply wrong, sometimes to a remarkable extent. We don’t know if the work excuse was written by a psychiatrist or another type of physician; we don’t know if it was for a psychiatric condition, cancer, or simply strep throat.
What we’ve been told is that a copilot who was cleared to fly did so despite a work excuse from a physician, he did not disclose this condition to his employer, and he crashed a plane killing 150 people.
We might assume that the pilot suffered from some type of psychic distress – whether he met criteria for a mental disorder or not, it’s not normal to kill 150 people. If the pilot did have a history of depression and was being treated at the time of this week’s flight, then we may be left with a very unsatisfactory answer.
The anti-psychiatry activists will say that psychotropic medications caused Lubitz to crash the plane. Psychiatrists will be left with no great answer with such a scenario and will be left to say that whatever treatment he was receiving, it wasn’t enough. Certainly, the physician who told Lubitz to take off from work was right: He didn’t belong in a cockpit that day. Presumably, that physician would have done more had he been aware that the patient was about to commit a mass murder.
If the copilot does have a history of depression, but his current work excuse was for an unrelated condition, we might wonder if an untreated recurrence of depression played some role in his actions. One might speculate that the copilot could have been afraid to seek care at this time, perhaps because of a fear that he would lose his vocation.
Still, major depression can hardly explain such an act, and it is unfortunate that the press has already begun to run headlines linking this man’s alleged psychiatric diagnosis to a catastrophic mass murder. Somehow, “mental illness” gets used as an endpoint explanation for why such things happen; and short of a severe psychotic delusional system, it’s a very unsatisfying answer for an unprecedented act of violence.
The facts will unfold and perhaps we’ll learn a little more. We’ll find out what condition the copilot was being treated for and whether there were other stresses going on in his personal life. But people get depressed, take antidepressants, and deal with stress all the time.
It’s possible, if not likely, that we’ll never understand why this copilot decided to end the lives of so many people along with his own.
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: The Johns Hopkins University, 2011).
Addressing the shortage of psychiatrists: What keeps us from seeing more patients?
Recently I was contacted by a reporter who wanted to speak to me about why it’s so difficult for patients to find a psychiatrist. She’d found me by Googling “Why psychiatrists don’t take insurance” and already had read an article I’d written with that title. That day, it had snowed hard enough that most of my patients had canceled; the grocery store had closed; and I had plenty of time to chat with a reporter. The other thing I noted – perhaps because other psychiatrists had unexpected free time because of the snow – was that Maryland Psychiatric Society’s listserv was getting a lot of posts. The posts focused on issues to do with maintenance of certification (MOC) or with the fact that every physician in the state was now going to be required to have a CME credit on opioid prescribing for licensure renewal, and there would be a requirement for physicians to take a course on substance abuse to renew their CDS registration. The hope is that these courses will reduce deaths caused by narcotic overdose, and the courses would be required for all physicians without regard to whether they are relevant to their practice.
The reporter and I started with a discussion of why so many psychiatrists have chosen not to accept health insurance (myself included). She then told me about an insured man who had been diagnosed with schizophrenia and substance abuse who was unable to get an appointment with a psychiatrist. She asked me an interesting question: “Don’t psychiatrists want the challenge of treating the difficult cases?” The patient in question never did find a psychiatrist in time and he ended up committing a murder then dying by suicide – an awful tragedy that highlights access to care problems.
In addition to a private practice, I have worked in community mental health centers, and I discussed how that setting is often better suited for patients with serious psychiatric illnesses. More services are offered, and having a variety of mental health professionals in the same facility promotes better coordination of care between psychiatrists, therapists, and case managers, as well as with family, residential care providers, and day programs. The problem is that demand for treatment at outpatient clinics is high, and sometimes the waits for an initial appointment are long, or clinics even may stop accepting new patients at times when they get overloaded.
We talked about the logistics and trade-offs of working in a clinic vs. a private practice, and the reasons why working full time in a high-volume clinic might lead physicians to want a change after a few years. And then the reporter asked me another interesting question – with such long waits, why don’t the clinics hire more doctors? I explained that there was a shortage of psychiatrists and began to talk with her about demands on physician time that take time away from patient care. With the e-mails flying about MOC and new course requirements, it was a place to start, but the snow was still falling, and she heard a lot about the factors that drain physician time and money, both limiting how many patients a psychiatrist can see and driving up the cost of care.
By the time I got off the phone, I decided to tally all of the things that we are required to do to see patients. I was able to get some quick help on the listserv, from friends, and on Twitter.
Every time an agency or insurance company sets up a requirement for a physician, there is a small diversion of time. There is no limit on how many different requirements can be set or whether they need to be relevant to the physician’s work. While I realize there is little sympathy for physicians who, for the most part, are still blessed to earn a good living while doing meaningful work, these diversions add hours to a doctor’s day and cause them to burn out more quickly. So the insurance company that demands that a physician devote 20 minutes to get authorization to prescribe a medication that costs pennies a pill is actually harming society. And no one oversees the big picture.
That said, here was the list we came up with of factors that drain time and money in a clinical practice. Please note that some of these items – for example, uncompensated time returning calls to patients or keeping clinical records – are just part of being a doctor; they’re not something that should be eliminated. Similarly, issues related to having a space to work are part of having a business. I wanted the list to be complete to illustrate the demands on a psychiatrist, not to suggest that none of these things are important. Obviously, some doctors are faster or slower at certain tasks, and people vary greatly in how much time they devote to clinical practice vs. teaching, research, or writing articles for Clinical Psychiatry News. I obtained information in a very quick and casual manner; none of this should be construed as scientific.
Here is the list:
• Maintenance of certification requirements and testing. This is required every 10 years and one estimate was that the cost to register, take the test, and purchase review materials came to $2,800, with a time investment of about 50 hours. Some specialties are pushing back against MOC, and some physicians are forgoing board certification. Psychiatrists who subspecialize usually do MOC for general psychiatry and all their subspecialties.
• CME. Twenty to 50 hours per year depending on your state, and presumably physicians choose courses that enrich their ability to practice medicine. This can be expensive, depending on how the physician decides to get these credits, and many valuable learning events do not qualify for CME.
• Writing clinical notes. Again, this is part of routine medical care. Notes must justify the CPT codes on insurance claims, and very specific areas of inquiry and examination are needed to justify billing specific codes. Agency requirements may be different from what is clinically indicated for the care of the patient, and this uses some of the appointment time in a way that may not be helpful to medical care. Copying, faxing, or sending notes to other clinicians and time spent requesting records all add to the mix. One psychiatrist noted that the overall administrative responsibilities for seeing patients takes half an hour for every hour spent with a patient. Others estimated that anywhere from 30 minutes to 2 hours per day are devoted to writing notes, and some mentioned doing this in the evening at home. One child psychiatrist with a large high-volume practice noted that he is required to keep charts until a patient reaches adulthood, and that storing, locating, and shredding charts was a time drain.
• Billing the patient. One private practice psychiatrist estimated this takes approximately 8 hours a month, include record-keeping and rebilling patients who failed to pay. Some psychiatrists have a secretary or billing staff.
• Patient insurance. Time spent preauthorizing care, including time spent to preauthorize hospitalizations or to justify each day of inpatient treatment. (No time estimates were offered.)
• Filing claims. The psychiatrists I spoke with who participate with insurers all had support staff to do this.
• Preauthorizing medications. This was by far the biggest complaint by psychiatrists. One noted that it had taken her 2 hours the night before to get a medication authorized; another had spent an hour that day on it. Another rough figure I got was 20-60 minutes a week, and it was noted that preauthorization often is required for very inexpensive medications. Another psychiatrist said her office manager spends a couple of hours a week on preauthorizations and that she had to give her a raise to get her to agree to do it. Personally, I feel insurance companies should not be permitted to divert physician time away from care for inexpensive medications. Does it really make sense to have a physician spend 20 minutes of uncompensated time getting authorization for a medication that costs $10 a month?
• Paperwork related to being credentialed with insurance companies. This was estimated at 40 minutes every 3 months.
• Credentialing. Cost and paperwork for malpractice insurance varies by state and, some malpractice agencies require doctors to do specific forms of training. In addition, practicing requires renewal of a DEA number, CDS renewal (in Maryland), and state licensure.
• Electronic medical records (EMR). Medicare has provided financial incentives to doctors for the meaningful use of certified electronic health record (EHR) technology to improve patient care and now penalizes doctors who do not have this technology. One psychiatrist told me that she spent hundreds of hours working on this, but something went wrong so she is still penalized. Another said she spent 3 hours in a 3-month period attesting to her compliance with meaningful use. Everyone I spoke to said using an electronic record – related to Medicare’s meaningful use or not – increased the time it takes them to write notes. One psychiatrist reduced her clinical care to 1 day a week, and I left a community clinic when the effort of learning to use EPIC overwhelmed me.
• E-prescribing. One colleague in New York wrote, “E-prescribing takes up a lot of time, especially since I don’t do it during sessions. For a noncontrolled medication, it’s maybe 4-5 minutes per prescription. For controlled, it’s 3-4 minutes more, because I have to check I-STOP and use the token, and then record the I-STOP number. And for all prescriptions, I hand write an entry in the medication record, just for backup.” She noted it took several hours to set up the system. Most psychiatrists still spend significant time calling in prescriptions that patients have forgotten to request during appointments, and pharmacists often call to have refills authorized. This can be quite time consuming, and sometimes refills are requested automatically for medications the patients no longer take, and time spent on hold can be significant. My own experience was that e-prescribing took significantly longer than paper prescribing, and that handing a patient a prescription during a session is simply part of medical care and not a “drain,” per se.
• Secretarial. No one was able to give me an estimate of how many hours per week were spent directing, managing, and training support staff, or of how many hours this freed up to see patients. One psychiatrist in a large practice noted that they have 32 full- and part-time professions, including 3 psychiatrists; they participate with insurance, and this requires 18 full-time support staff.
• Office-related issues. Rent – this is both taste and geographically driven, and there are several ways to come by office space. Other factors are time related to restocking supplies, furnishings, technological hardware, phones, faxes, pagers, mobile lines, postage, technology support, cleaning, and assorted office-related issues. I have no time estimates on this; some people have support staff who do most of it, and again, this is part of the routine practice of having a business. It takes time, but it’s not irrelevant. Also, time is spent keeping an office both OSHA and HIPAA compliant.
• Hospital/agency-related requirements:
– Risk management seminars.
– CPR training.
– Health maintenance (required TB testing and flu shot).
• Required learning modules. When I worked 4 hours a week at a hospital clinic, there were many requirements. I watched modules on how to use elevators in buildings I never entered, how to place a central line, hand-washing and infection control, and how to store chemicals I never used. I believe that Maryland state employees may be required to have training in trauma-informed-care.
• Uncompensated time returning calls/communications to patients, families, other clinicians, and prospective patients who then decide not to come in, as well as filling out paperwork for disability claims, other agencies, and writing letters for patients. While this also is part of routine medical care, several people mentioned that other professionals can bill for this work and that insurers can force unnecessary care because only face-to-face treatment gets reimbursed, so issues that might be resolved on the phone or by telepsychiatry then require an office visit.
One colleague was kind enough to examine her own full-time practice and sum up her activities. She came up with an estimate that she devoted 40 hours per month to administrative issues that divert time from seeing patients. This did not include the time she recently devoted to MOC.
Obviously, I want to make the point that part of the psychiatrist shortage is related to the fact that there are administrative demands – many that don’t improve clinical care – that decrease the number of patients we can see and increase the cost of care. In addition to the weekly toll, many of these time drains are frustrating, and serve as disincentives to seeing patients with what time is available. The statistics prove that psychiatrists are less willing than other specialists to participate with insurance networks, and I suspect the litany of clinically irrelevant requirements may lead to earlier retirement by people who might otherwise be willing to practice for more years.
One might ask, at what point do we fight back against spending our time meeting the agendas of agencies and insurers when they aren’t relevant to the care that is needed to help patients?
With thanks to Dr. Mahmood Jarhomi, Dr. Patricia Sullivan, Dr. Sue Kim, Dr. Laura Gaffney, Dr. Maria Yang, Dr. Marsden McGuire, Dr. Annette Hanson, Dr. Robert Herman, Dr. Kimberly Hogan Pesaniello, Dr. Peter Kahn, Dr. Mark Komrad, Dr. Susan Molchan, Dr. Suzy Nashed, and Dr. Rebecca Twersky-Kengmana.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently I was contacted by a reporter who wanted to speak to me about why it’s so difficult for patients to find a psychiatrist. She’d found me by Googling “Why psychiatrists don’t take insurance” and already had read an article I’d written with that title. That day, it had snowed hard enough that most of my patients had canceled; the grocery store had closed; and I had plenty of time to chat with a reporter. The other thing I noted – perhaps because other psychiatrists had unexpected free time because of the snow – was that Maryland Psychiatric Society’s listserv was getting a lot of posts. The posts focused on issues to do with maintenance of certification (MOC) or with the fact that every physician in the state was now going to be required to have a CME credit on opioid prescribing for licensure renewal, and there would be a requirement for physicians to take a course on substance abuse to renew their CDS registration. The hope is that these courses will reduce deaths caused by narcotic overdose, and the courses would be required for all physicians without regard to whether they are relevant to their practice.
The reporter and I started with a discussion of why so many psychiatrists have chosen not to accept health insurance (myself included). She then told me about an insured man who had been diagnosed with schizophrenia and substance abuse who was unable to get an appointment with a psychiatrist. She asked me an interesting question: “Don’t psychiatrists want the challenge of treating the difficult cases?” The patient in question never did find a psychiatrist in time and he ended up committing a murder then dying by suicide – an awful tragedy that highlights access to care problems.
In addition to a private practice, I have worked in community mental health centers, and I discussed how that setting is often better suited for patients with serious psychiatric illnesses. More services are offered, and having a variety of mental health professionals in the same facility promotes better coordination of care between psychiatrists, therapists, and case managers, as well as with family, residential care providers, and day programs. The problem is that demand for treatment at outpatient clinics is high, and sometimes the waits for an initial appointment are long, or clinics even may stop accepting new patients at times when they get overloaded.
We talked about the logistics and trade-offs of working in a clinic vs. a private practice, and the reasons why working full time in a high-volume clinic might lead physicians to want a change after a few years. And then the reporter asked me another interesting question – with such long waits, why don’t the clinics hire more doctors? I explained that there was a shortage of psychiatrists and began to talk with her about demands on physician time that take time away from patient care. With the e-mails flying about MOC and new course requirements, it was a place to start, but the snow was still falling, and she heard a lot about the factors that drain physician time and money, both limiting how many patients a psychiatrist can see and driving up the cost of care.
By the time I got off the phone, I decided to tally all of the things that we are required to do to see patients. I was able to get some quick help on the listserv, from friends, and on Twitter.
Every time an agency or insurance company sets up a requirement for a physician, there is a small diversion of time. There is no limit on how many different requirements can be set or whether they need to be relevant to the physician’s work. While I realize there is little sympathy for physicians who, for the most part, are still blessed to earn a good living while doing meaningful work, these diversions add hours to a doctor’s day and cause them to burn out more quickly. So the insurance company that demands that a physician devote 20 minutes to get authorization to prescribe a medication that costs pennies a pill is actually harming society. And no one oversees the big picture.
That said, here was the list we came up with of factors that drain time and money in a clinical practice. Please note that some of these items – for example, uncompensated time returning calls to patients or keeping clinical records – are just part of being a doctor; they’re not something that should be eliminated. Similarly, issues related to having a space to work are part of having a business. I wanted the list to be complete to illustrate the demands on a psychiatrist, not to suggest that none of these things are important. Obviously, some doctors are faster or slower at certain tasks, and people vary greatly in how much time they devote to clinical practice vs. teaching, research, or writing articles for Clinical Psychiatry News. I obtained information in a very quick and casual manner; none of this should be construed as scientific.
Here is the list:
• Maintenance of certification requirements and testing. This is required every 10 years and one estimate was that the cost to register, take the test, and purchase review materials came to $2,800, with a time investment of about 50 hours. Some specialties are pushing back against MOC, and some physicians are forgoing board certification. Psychiatrists who subspecialize usually do MOC for general psychiatry and all their subspecialties.
• CME. Twenty to 50 hours per year depending on your state, and presumably physicians choose courses that enrich their ability to practice medicine. This can be expensive, depending on how the physician decides to get these credits, and many valuable learning events do not qualify for CME.
• Writing clinical notes. Again, this is part of routine medical care. Notes must justify the CPT codes on insurance claims, and very specific areas of inquiry and examination are needed to justify billing specific codes. Agency requirements may be different from what is clinically indicated for the care of the patient, and this uses some of the appointment time in a way that may not be helpful to medical care. Copying, faxing, or sending notes to other clinicians and time spent requesting records all add to the mix. One psychiatrist noted that the overall administrative responsibilities for seeing patients takes half an hour for every hour spent with a patient. Others estimated that anywhere from 30 minutes to 2 hours per day are devoted to writing notes, and some mentioned doing this in the evening at home. One child psychiatrist with a large high-volume practice noted that he is required to keep charts until a patient reaches adulthood, and that storing, locating, and shredding charts was a time drain.
• Billing the patient. One private practice psychiatrist estimated this takes approximately 8 hours a month, include record-keeping and rebilling patients who failed to pay. Some psychiatrists have a secretary or billing staff.
• Patient insurance. Time spent preauthorizing care, including time spent to preauthorize hospitalizations or to justify each day of inpatient treatment. (No time estimates were offered.)
• Filing claims. The psychiatrists I spoke with who participate with insurers all had support staff to do this.
• Preauthorizing medications. This was by far the biggest complaint by psychiatrists. One noted that it had taken her 2 hours the night before to get a medication authorized; another had spent an hour that day on it. Another rough figure I got was 20-60 minutes a week, and it was noted that preauthorization often is required for very inexpensive medications. Another psychiatrist said her office manager spends a couple of hours a week on preauthorizations and that she had to give her a raise to get her to agree to do it. Personally, I feel insurance companies should not be permitted to divert physician time away from care for inexpensive medications. Does it really make sense to have a physician spend 20 minutes of uncompensated time getting authorization for a medication that costs $10 a month?
• Paperwork related to being credentialed with insurance companies. This was estimated at 40 minutes every 3 months.
• Credentialing. Cost and paperwork for malpractice insurance varies by state and, some malpractice agencies require doctors to do specific forms of training. In addition, practicing requires renewal of a DEA number, CDS renewal (in Maryland), and state licensure.
• Electronic medical records (EMR). Medicare has provided financial incentives to doctors for the meaningful use of certified electronic health record (EHR) technology to improve patient care and now penalizes doctors who do not have this technology. One psychiatrist told me that she spent hundreds of hours working on this, but something went wrong so she is still penalized. Another said she spent 3 hours in a 3-month period attesting to her compliance with meaningful use. Everyone I spoke to said using an electronic record – related to Medicare’s meaningful use or not – increased the time it takes them to write notes. One psychiatrist reduced her clinical care to 1 day a week, and I left a community clinic when the effort of learning to use EPIC overwhelmed me.
• E-prescribing. One colleague in New York wrote, “E-prescribing takes up a lot of time, especially since I don’t do it during sessions. For a noncontrolled medication, it’s maybe 4-5 minutes per prescription. For controlled, it’s 3-4 minutes more, because I have to check I-STOP and use the token, and then record the I-STOP number. And for all prescriptions, I hand write an entry in the medication record, just for backup.” She noted it took several hours to set up the system. Most psychiatrists still spend significant time calling in prescriptions that patients have forgotten to request during appointments, and pharmacists often call to have refills authorized. This can be quite time consuming, and sometimes refills are requested automatically for medications the patients no longer take, and time spent on hold can be significant. My own experience was that e-prescribing took significantly longer than paper prescribing, and that handing a patient a prescription during a session is simply part of medical care and not a “drain,” per se.
• Secretarial. No one was able to give me an estimate of how many hours per week were spent directing, managing, and training support staff, or of how many hours this freed up to see patients. One psychiatrist in a large practice noted that they have 32 full- and part-time professions, including 3 psychiatrists; they participate with insurance, and this requires 18 full-time support staff.
• Office-related issues. Rent – this is both taste and geographically driven, and there are several ways to come by office space. Other factors are time related to restocking supplies, furnishings, technological hardware, phones, faxes, pagers, mobile lines, postage, technology support, cleaning, and assorted office-related issues. I have no time estimates on this; some people have support staff who do most of it, and again, this is part of the routine practice of having a business. It takes time, but it’s not irrelevant. Also, time is spent keeping an office both OSHA and HIPAA compliant.
• Hospital/agency-related requirements:
– Risk management seminars.
– CPR training.
– Health maintenance (required TB testing and flu shot).
• Required learning modules. When I worked 4 hours a week at a hospital clinic, there were many requirements. I watched modules on how to use elevators in buildings I never entered, how to place a central line, hand-washing and infection control, and how to store chemicals I never used. I believe that Maryland state employees may be required to have training in trauma-informed-care.
• Uncompensated time returning calls/communications to patients, families, other clinicians, and prospective patients who then decide not to come in, as well as filling out paperwork for disability claims, other agencies, and writing letters for patients. While this also is part of routine medical care, several people mentioned that other professionals can bill for this work and that insurers can force unnecessary care because only face-to-face treatment gets reimbursed, so issues that might be resolved on the phone or by telepsychiatry then require an office visit.
One colleague was kind enough to examine her own full-time practice and sum up her activities. She came up with an estimate that she devoted 40 hours per month to administrative issues that divert time from seeing patients. This did not include the time she recently devoted to MOC.
Obviously, I want to make the point that part of the psychiatrist shortage is related to the fact that there are administrative demands – many that don’t improve clinical care – that decrease the number of patients we can see and increase the cost of care. In addition to the weekly toll, many of these time drains are frustrating, and serve as disincentives to seeing patients with what time is available. The statistics prove that psychiatrists are less willing than other specialists to participate with insurance networks, and I suspect the litany of clinically irrelevant requirements may lead to earlier retirement by people who might otherwise be willing to practice for more years.
One might ask, at what point do we fight back against spending our time meeting the agendas of agencies and insurers when they aren’t relevant to the care that is needed to help patients?
With thanks to Dr. Mahmood Jarhomi, Dr. Patricia Sullivan, Dr. Sue Kim, Dr. Laura Gaffney, Dr. Maria Yang, Dr. Marsden McGuire, Dr. Annette Hanson, Dr. Robert Herman, Dr. Kimberly Hogan Pesaniello, Dr. Peter Kahn, Dr. Mark Komrad, Dr. Susan Molchan, Dr. Suzy Nashed, and Dr. Rebecca Twersky-Kengmana.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently I was contacted by a reporter who wanted to speak to me about why it’s so difficult for patients to find a psychiatrist. She’d found me by Googling “Why psychiatrists don’t take insurance” and already had read an article I’d written with that title. That day, it had snowed hard enough that most of my patients had canceled; the grocery store had closed; and I had plenty of time to chat with a reporter. The other thing I noted – perhaps because other psychiatrists had unexpected free time because of the snow – was that Maryland Psychiatric Society’s listserv was getting a lot of posts. The posts focused on issues to do with maintenance of certification (MOC) or with the fact that every physician in the state was now going to be required to have a CME credit on opioid prescribing for licensure renewal, and there would be a requirement for physicians to take a course on substance abuse to renew their CDS registration. The hope is that these courses will reduce deaths caused by narcotic overdose, and the courses would be required for all physicians without regard to whether they are relevant to their practice.
The reporter and I started with a discussion of why so many psychiatrists have chosen not to accept health insurance (myself included). She then told me about an insured man who had been diagnosed with schizophrenia and substance abuse who was unable to get an appointment with a psychiatrist. She asked me an interesting question: “Don’t psychiatrists want the challenge of treating the difficult cases?” The patient in question never did find a psychiatrist in time and he ended up committing a murder then dying by suicide – an awful tragedy that highlights access to care problems.
In addition to a private practice, I have worked in community mental health centers, and I discussed how that setting is often better suited for patients with serious psychiatric illnesses. More services are offered, and having a variety of mental health professionals in the same facility promotes better coordination of care between psychiatrists, therapists, and case managers, as well as with family, residential care providers, and day programs. The problem is that demand for treatment at outpatient clinics is high, and sometimes the waits for an initial appointment are long, or clinics even may stop accepting new patients at times when they get overloaded.
We talked about the logistics and trade-offs of working in a clinic vs. a private practice, and the reasons why working full time in a high-volume clinic might lead physicians to want a change after a few years. And then the reporter asked me another interesting question – with such long waits, why don’t the clinics hire more doctors? I explained that there was a shortage of psychiatrists and began to talk with her about demands on physician time that take time away from patient care. With the e-mails flying about MOC and new course requirements, it was a place to start, but the snow was still falling, and she heard a lot about the factors that drain physician time and money, both limiting how many patients a psychiatrist can see and driving up the cost of care.
By the time I got off the phone, I decided to tally all of the things that we are required to do to see patients. I was able to get some quick help on the listserv, from friends, and on Twitter.
Every time an agency or insurance company sets up a requirement for a physician, there is a small diversion of time. There is no limit on how many different requirements can be set or whether they need to be relevant to the physician’s work. While I realize there is little sympathy for physicians who, for the most part, are still blessed to earn a good living while doing meaningful work, these diversions add hours to a doctor’s day and cause them to burn out more quickly. So the insurance company that demands that a physician devote 20 minutes to get authorization to prescribe a medication that costs pennies a pill is actually harming society. And no one oversees the big picture.
That said, here was the list we came up with of factors that drain time and money in a clinical practice. Please note that some of these items – for example, uncompensated time returning calls to patients or keeping clinical records – are just part of being a doctor; they’re not something that should be eliminated. Similarly, issues related to having a space to work are part of having a business. I wanted the list to be complete to illustrate the demands on a psychiatrist, not to suggest that none of these things are important. Obviously, some doctors are faster or slower at certain tasks, and people vary greatly in how much time they devote to clinical practice vs. teaching, research, or writing articles for Clinical Psychiatry News. I obtained information in a very quick and casual manner; none of this should be construed as scientific.
Here is the list:
• Maintenance of certification requirements and testing. This is required every 10 years and one estimate was that the cost to register, take the test, and purchase review materials came to $2,800, with a time investment of about 50 hours. Some specialties are pushing back against MOC, and some physicians are forgoing board certification. Psychiatrists who subspecialize usually do MOC for general psychiatry and all their subspecialties.
• CME. Twenty to 50 hours per year depending on your state, and presumably physicians choose courses that enrich their ability to practice medicine. This can be expensive, depending on how the physician decides to get these credits, and many valuable learning events do not qualify for CME.
• Writing clinical notes. Again, this is part of routine medical care. Notes must justify the CPT codes on insurance claims, and very specific areas of inquiry and examination are needed to justify billing specific codes. Agency requirements may be different from what is clinically indicated for the care of the patient, and this uses some of the appointment time in a way that may not be helpful to medical care. Copying, faxing, or sending notes to other clinicians and time spent requesting records all add to the mix. One psychiatrist noted that the overall administrative responsibilities for seeing patients takes half an hour for every hour spent with a patient. Others estimated that anywhere from 30 minutes to 2 hours per day are devoted to writing notes, and some mentioned doing this in the evening at home. One child psychiatrist with a large high-volume practice noted that he is required to keep charts until a patient reaches adulthood, and that storing, locating, and shredding charts was a time drain.
• Billing the patient. One private practice psychiatrist estimated this takes approximately 8 hours a month, include record-keeping and rebilling patients who failed to pay. Some psychiatrists have a secretary or billing staff.
• Patient insurance. Time spent preauthorizing care, including time spent to preauthorize hospitalizations or to justify each day of inpatient treatment. (No time estimates were offered.)
• Filing claims. The psychiatrists I spoke with who participate with insurers all had support staff to do this.
• Preauthorizing medications. This was by far the biggest complaint by psychiatrists. One noted that it had taken her 2 hours the night before to get a medication authorized; another had spent an hour that day on it. Another rough figure I got was 20-60 minutes a week, and it was noted that preauthorization often is required for very inexpensive medications. Another psychiatrist said her office manager spends a couple of hours a week on preauthorizations and that she had to give her a raise to get her to agree to do it. Personally, I feel insurance companies should not be permitted to divert physician time away from care for inexpensive medications. Does it really make sense to have a physician spend 20 minutes of uncompensated time getting authorization for a medication that costs $10 a month?
• Paperwork related to being credentialed with insurance companies. This was estimated at 40 minutes every 3 months.
• Credentialing. Cost and paperwork for malpractice insurance varies by state and, some malpractice agencies require doctors to do specific forms of training. In addition, practicing requires renewal of a DEA number, CDS renewal (in Maryland), and state licensure.
• Electronic medical records (EMR). Medicare has provided financial incentives to doctors for the meaningful use of certified electronic health record (EHR) technology to improve patient care and now penalizes doctors who do not have this technology. One psychiatrist told me that she spent hundreds of hours working on this, but something went wrong so she is still penalized. Another said she spent 3 hours in a 3-month period attesting to her compliance with meaningful use. Everyone I spoke to said using an electronic record – related to Medicare’s meaningful use or not – increased the time it takes them to write notes. One psychiatrist reduced her clinical care to 1 day a week, and I left a community clinic when the effort of learning to use EPIC overwhelmed me.
• E-prescribing. One colleague in New York wrote, “E-prescribing takes up a lot of time, especially since I don’t do it during sessions. For a noncontrolled medication, it’s maybe 4-5 minutes per prescription. For controlled, it’s 3-4 minutes more, because I have to check I-STOP and use the token, and then record the I-STOP number. And for all prescriptions, I hand write an entry in the medication record, just for backup.” She noted it took several hours to set up the system. Most psychiatrists still spend significant time calling in prescriptions that patients have forgotten to request during appointments, and pharmacists often call to have refills authorized. This can be quite time consuming, and sometimes refills are requested automatically for medications the patients no longer take, and time spent on hold can be significant. My own experience was that e-prescribing took significantly longer than paper prescribing, and that handing a patient a prescription during a session is simply part of medical care and not a “drain,” per se.
• Secretarial. No one was able to give me an estimate of how many hours per week were spent directing, managing, and training support staff, or of how many hours this freed up to see patients. One psychiatrist in a large practice noted that they have 32 full- and part-time professions, including 3 psychiatrists; they participate with insurance, and this requires 18 full-time support staff.
• Office-related issues. Rent – this is both taste and geographically driven, and there are several ways to come by office space. Other factors are time related to restocking supplies, furnishings, technological hardware, phones, faxes, pagers, mobile lines, postage, technology support, cleaning, and assorted office-related issues. I have no time estimates on this; some people have support staff who do most of it, and again, this is part of the routine practice of having a business. It takes time, but it’s not irrelevant. Also, time is spent keeping an office both OSHA and HIPAA compliant.
• Hospital/agency-related requirements:
– Risk management seminars.
– CPR training.
– Health maintenance (required TB testing and flu shot).
• Required learning modules. When I worked 4 hours a week at a hospital clinic, there were many requirements. I watched modules on how to use elevators in buildings I never entered, how to place a central line, hand-washing and infection control, and how to store chemicals I never used. I believe that Maryland state employees may be required to have training in trauma-informed-care.
• Uncompensated time returning calls/communications to patients, families, other clinicians, and prospective patients who then decide not to come in, as well as filling out paperwork for disability claims, other agencies, and writing letters for patients. While this also is part of routine medical care, several people mentioned that other professionals can bill for this work and that insurers can force unnecessary care because only face-to-face treatment gets reimbursed, so issues that might be resolved on the phone or by telepsychiatry then require an office visit.
One colleague was kind enough to examine her own full-time practice and sum up her activities. She came up with an estimate that she devoted 40 hours per month to administrative issues that divert time from seeing patients. This did not include the time she recently devoted to MOC.
Obviously, I want to make the point that part of the psychiatrist shortage is related to the fact that there are administrative demands – many that don’t improve clinical care – that decrease the number of patients we can see and increase the cost of care. In addition to the weekly toll, many of these time drains are frustrating, and serve as disincentives to seeing patients with what time is available. The statistics prove that psychiatrists are less willing than other specialists to participate with insurance networks, and I suspect the litany of clinically irrelevant requirements may lead to earlier retirement by people who might otherwise be willing to practice for more years.
One might ask, at what point do we fight back against spending our time meeting the agendas of agencies and insurers when they aren’t relevant to the care that is needed to help patients?
With thanks to Dr. Mahmood Jarhomi, Dr. Patricia Sullivan, Dr. Sue Kim, Dr. Laura Gaffney, Dr. Maria Yang, Dr. Marsden McGuire, Dr. Annette Hanson, Dr. Robert Herman, Dr. Kimberly Hogan Pesaniello, Dr. Peter Kahn, Dr. Mark Komrad, Dr. Susan Molchan, Dr. Suzy Nashed, and Dr. Rebecca Twersky-Kengmana.
Dr. Miller is coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Should APA have endorsed the Helping Families in Mental Health Crisis Act?
After the school shooting in Newtown, Conn., in December 2012, we saw an unprecedented amount of proposed legislation at both the state and national levels. The legislation was aimed at fixing whatever it is that is broken in our country that either causes or allows a young man to kill more than two dozen innocent people. Some legislators focused on gun control, while others focused on changing the mental health system, with the idea that the shooter’s actions were caused by his untreated mental illness.
Rep. Tim Murphy, Ph.D., has the distinction of being the only clinical psychologist in Congress, so it’s certainly understandable that he would focus on making long-overdue changes to our troubled mental health system. In addition, Rep. Murphy, a Republican from Pennsylvania, has a strong history of voting against legislation that would curb gun rights, and he carries an “A” grade from the National Rifle Association. When Rep. Murphy publicly promised the families of the Newtown victims that he would enact change, it was clear that his passion was for changing the mental health system. In 2013, Rep. Murphy, with bipartisan support, proposed The Helping Families in Mental Health Crisis Act.
The Murphy bill proposed sweeping and complex changes, and the text was 135 pages long. A major component of the bill was to create a position for an assistant secretary for mental health and substance use disorders within the Department of Health & Human Services to coordinate federal programs and ensure that evidence-based treatments were being used.
The bill also called for shifting money from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health in the wake of recent thought that SAMHSA has become insensitive to severe mental illness and too oriented toward a recovery model that carries a vague antipsychiatry sentiment.
From there, the issues of patients’ rights versus a doctor-knows-best sentiment have influenced the act, as though one can’t be in favor of both. Perhaps the most controversial requirements include a provision that mandates all states to have outpatient civil commitment programs and a provision that says that health care providers may release information to caretakers of patients with psychiatric disorders without the patient’s consent if the information is felt to be necessary for the patient’s safety or welfare.
This last point is likely to be interpreted as suggesting that psychiatric patients don’t have the same right to confidentiality that other patients have, which would be true. It has the potential to be stigmatizing and infantilizing, and there are people who will not seek care because of the perception this creates. In addition, it may create tension between family members who feel the law now entitles them to information and psychiatrists who don’t see this is as necessary or who fear that releasing information will damage the therapeutic relationship.
Many components of the Helping Families in Mental Health Crisis Act have been applauded universally, but the American Psychiatric Association did not formally support the bill, and an opposing bill was proposed in Congress by Rep. Ron Barber, a Democrat from Arizona who took Gabrielle Giffords’ seat after an assassination attempt by a mentally ill man left her unable to serve. Both bills died when the congressional session ended in December, and Mr. Barber lost a re-election bid and has not returned to Congress.
A new Congress has convened, and Rep. Murphy will be re-introducing the Helping Families in Mental Health Crisis Act with numerous changes. Although the APA did not endorse the previous legislation, the association last week announced, with unanimous backing by the Board of Trustees, its support for the Murphy bill.
“We are pleased that Chairman Murphy is refining and reintroducing his comprehensive mental health reform bill, the Helping Families in Mental Health Crisis Act,” APA President Paul Summergrad said in the last week of January. At an event in early February, he said that he intends to add reforms that align well with APA priorities, including boosting the psychiatric workforce and monitoring and enforcement of mental health parity.
“In December the APA Board of Trustees carefully reviewed its strategy, principles and options for reform and unanimously voted to fully support the efforts of Chairman Murphy and his lead Democratic cosponsor, Rep. Eddie Bernice Johnson. Their efforts are historic in scope, and we are hopeful that Congress will through the legislative process act to pass comprehensive mental health reform with the bipartisan support it deserves.”
Still, I heard the news and was terribly disappointed in the APA. The decision to support this sweeping legislation was made without a vote by the Assembly, with the knowledge that some of these issues are quite polarizing. In addition to the HIPAA disqualification, the issue of outpatient civil commitment, in particular, is controversial. Although proponents are quick to point to research that show its benefits – the research has been done specifically on Kendra’s Law in New York, where $125 million was placed into that state’s mental health system to shore up services – we don’t have the research to know if what helps is providing more services or strong-armed coercion. The text of the bill will be released in the coming weeks. At the very least, couldn’t the APA have waited to see exactly what it is we endorsed?
Dr. Miller is writing a book on involuntary psychiatric care.
After the school shooting in Newtown, Conn., in December 2012, we saw an unprecedented amount of proposed legislation at both the state and national levels. The legislation was aimed at fixing whatever it is that is broken in our country that either causes or allows a young man to kill more than two dozen innocent people. Some legislators focused on gun control, while others focused on changing the mental health system, with the idea that the shooter’s actions were caused by his untreated mental illness.
Rep. Tim Murphy, Ph.D., has the distinction of being the only clinical psychologist in Congress, so it’s certainly understandable that he would focus on making long-overdue changes to our troubled mental health system. In addition, Rep. Murphy, a Republican from Pennsylvania, has a strong history of voting against legislation that would curb gun rights, and he carries an “A” grade from the National Rifle Association. When Rep. Murphy publicly promised the families of the Newtown victims that he would enact change, it was clear that his passion was for changing the mental health system. In 2013, Rep. Murphy, with bipartisan support, proposed The Helping Families in Mental Health Crisis Act.
The Murphy bill proposed sweeping and complex changes, and the text was 135 pages long. A major component of the bill was to create a position for an assistant secretary for mental health and substance use disorders within the Department of Health & Human Services to coordinate federal programs and ensure that evidence-based treatments were being used.
The bill also called for shifting money from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health in the wake of recent thought that SAMHSA has become insensitive to severe mental illness and too oriented toward a recovery model that carries a vague antipsychiatry sentiment.
From there, the issues of patients’ rights versus a doctor-knows-best sentiment have influenced the act, as though one can’t be in favor of both. Perhaps the most controversial requirements include a provision that mandates all states to have outpatient civil commitment programs and a provision that says that health care providers may release information to caretakers of patients with psychiatric disorders without the patient’s consent if the information is felt to be necessary for the patient’s safety or welfare.
This last point is likely to be interpreted as suggesting that psychiatric patients don’t have the same right to confidentiality that other patients have, which would be true. It has the potential to be stigmatizing and infantilizing, and there are people who will not seek care because of the perception this creates. In addition, it may create tension between family members who feel the law now entitles them to information and psychiatrists who don’t see this is as necessary or who fear that releasing information will damage the therapeutic relationship.
Many components of the Helping Families in Mental Health Crisis Act have been applauded universally, but the American Psychiatric Association did not formally support the bill, and an opposing bill was proposed in Congress by Rep. Ron Barber, a Democrat from Arizona who took Gabrielle Giffords’ seat after an assassination attempt by a mentally ill man left her unable to serve. Both bills died when the congressional session ended in December, and Mr. Barber lost a re-election bid and has not returned to Congress.
A new Congress has convened, and Rep. Murphy will be re-introducing the Helping Families in Mental Health Crisis Act with numerous changes. Although the APA did not endorse the previous legislation, the association last week announced, with unanimous backing by the Board of Trustees, its support for the Murphy bill.
“We are pleased that Chairman Murphy is refining and reintroducing his comprehensive mental health reform bill, the Helping Families in Mental Health Crisis Act,” APA President Paul Summergrad said in the last week of January. At an event in early February, he said that he intends to add reforms that align well with APA priorities, including boosting the psychiatric workforce and monitoring and enforcement of mental health parity.
“In December the APA Board of Trustees carefully reviewed its strategy, principles and options for reform and unanimously voted to fully support the efforts of Chairman Murphy and his lead Democratic cosponsor, Rep. Eddie Bernice Johnson. Their efforts are historic in scope, and we are hopeful that Congress will through the legislative process act to pass comprehensive mental health reform with the bipartisan support it deserves.”
Still, I heard the news and was terribly disappointed in the APA. The decision to support this sweeping legislation was made without a vote by the Assembly, with the knowledge that some of these issues are quite polarizing. In addition to the HIPAA disqualification, the issue of outpatient civil commitment, in particular, is controversial. Although proponents are quick to point to research that show its benefits – the research has been done specifically on Kendra’s Law in New York, where $125 million was placed into that state’s mental health system to shore up services – we don’t have the research to know if what helps is providing more services or strong-armed coercion. The text of the bill will be released in the coming weeks. At the very least, couldn’t the APA have waited to see exactly what it is we endorsed?
Dr. Miller is writing a book on involuntary psychiatric care.
After the school shooting in Newtown, Conn., in December 2012, we saw an unprecedented amount of proposed legislation at both the state and national levels. The legislation was aimed at fixing whatever it is that is broken in our country that either causes or allows a young man to kill more than two dozen innocent people. Some legislators focused on gun control, while others focused on changing the mental health system, with the idea that the shooter’s actions were caused by his untreated mental illness.
Rep. Tim Murphy, Ph.D., has the distinction of being the only clinical psychologist in Congress, so it’s certainly understandable that he would focus on making long-overdue changes to our troubled mental health system. In addition, Rep. Murphy, a Republican from Pennsylvania, has a strong history of voting against legislation that would curb gun rights, and he carries an “A” grade from the National Rifle Association. When Rep. Murphy publicly promised the families of the Newtown victims that he would enact change, it was clear that his passion was for changing the mental health system. In 2013, Rep. Murphy, with bipartisan support, proposed The Helping Families in Mental Health Crisis Act.
The Murphy bill proposed sweeping and complex changes, and the text was 135 pages long. A major component of the bill was to create a position for an assistant secretary for mental health and substance use disorders within the Department of Health & Human Services to coordinate federal programs and ensure that evidence-based treatments were being used.
The bill also called for shifting money from the Substance Abuse and Mental Health Services Administration (SAMHSA) to the National Institute of Mental Health in the wake of recent thought that SAMHSA has become insensitive to severe mental illness and too oriented toward a recovery model that carries a vague antipsychiatry sentiment.
From there, the issues of patients’ rights versus a doctor-knows-best sentiment have influenced the act, as though one can’t be in favor of both. Perhaps the most controversial requirements include a provision that mandates all states to have outpatient civil commitment programs and a provision that says that health care providers may release information to caretakers of patients with psychiatric disorders without the patient’s consent if the information is felt to be necessary for the patient’s safety or welfare.
This last point is likely to be interpreted as suggesting that psychiatric patients don’t have the same right to confidentiality that other patients have, which would be true. It has the potential to be stigmatizing and infantilizing, and there are people who will not seek care because of the perception this creates. In addition, it may create tension between family members who feel the law now entitles them to information and psychiatrists who don’t see this is as necessary or who fear that releasing information will damage the therapeutic relationship.
Many components of the Helping Families in Mental Health Crisis Act have been applauded universally, but the American Psychiatric Association did not formally support the bill, and an opposing bill was proposed in Congress by Rep. Ron Barber, a Democrat from Arizona who took Gabrielle Giffords’ seat after an assassination attempt by a mentally ill man left her unable to serve. Both bills died when the congressional session ended in December, and Mr. Barber lost a re-election bid and has not returned to Congress.
A new Congress has convened, and Rep. Murphy will be re-introducing the Helping Families in Mental Health Crisis Act with numerous changes. Although the APA did not endorse the previous legislation, the association last week announced, with unanimous backing by the Board of Trustees, its support for the Murphy bill.
“We are pleased that Chairman Murphy is refining and reintroducing his comprehensive mental health reform bill, the Helping Families in Mental Health Crisis Act,” APA President Paul Summergrad said in the last week of January. At an event in early February, he said that he intends to add reforms that align well with APA priorities, including boosting the psychiatric workforce and monitoring and enforcement of mental health parity.
“In December the APA Board of Trustees carefully reviewed its strategy, principles and options for reform and unanimously voted to fully support the efforts of Chairman Murphy and his lead Democratic cosponsor, Rep. Eddie Bernice Johnson. Their efforts are historic in scope, and we are hopeful that Congress will through the legislative process act to pass comprehensive mental health reform with the bipartisan support it deserves.”
Still, I heard the news and was terribly disappointed in the APA. The decision to support this sweeping legislation was made without a vote by the Assembly, with the knowledge that some of these issues are quite polarizing. In addition to the HIPAA disqualification, the issue of outpatient civil commitment, in particular, is controversial. Although proponents are quick to point to research that show its benefits – the research has been done specifically on Kendra’s Law in New York, where $125 million was placed into that state’s mental health system to shore up services – we don’t have the research to know if what helps is providing more services or strong-armed coercion. The text of the bill will be released in the coming weeks. At the very least, couldn’t the APA have waited to see exactly what it is we endorsed?
Dr. Miller is writing a book on involuntary psychiatric care.
Shrink Rap News: Writing about involuntary treatment is harder than you might think
There are many controversies in psychiatry, but the most controversial issue continues to be that of involuntary treatment. Over the past year, I have been working on a book on forced care, along with Dr. Annette Hanson, the forensic psychiatrist who also writes this Shrink Rap News column. The work I’ve been doing for the manuscript – identifying and interviewing the people with a stake in the issue – has placed me in a funny role of being more journalist than physician. It’s a role I mostly love, and if you’ve hit the midpoint of your career and have an opportunity to dedicate some of your time to doing something completely different, I highly recommend shifting gears for a little while.
One of the things I have found most surprising is the reactions of people when I ask to include them. While most people are willing, almost all hesitate a little. Some are quite eager to participate, and one group in Richmond who uses involuntary electroconvulsive therapy heard of my project and extended an invitation for me to come visit, interview them, watch the procedure, and speak with one of their patients. Many people are proud of the work they do and eager to showcase it; they want to have their viewpoint included. With others, I have needed to ask repeatedly, listen to their concerns, and offer reassurances. I’ve taken to telling people they can read a draft of what I write about them – I learned early in the process that without this offer, few people would be willing to speak to me.
I wish I could say that I’ve noticed a pattern to who is comfortable speaking and who is not. Many of the psychiatrists and researchers I’ve approached have given their time willingly without hesitation ( or at least without that much hesitation), including Dr. E. Fuller Torrey; Dr. Paul Appelbaum; Jeffrey Swanson, Ph.D.; Dr. Steven Sharfstein; Dr. Daniel Fisher; Vermont Psychiatric Society President Margaret Bolton; Dr. Bruce Hershfield; and American Psychiatric Association President Paul Summergrad, to name just a few of the many people who have shared their time, experiences, and wisdom with me. It was not as easy for me to find a psychiatrist I could observe working on an inpatient unit, and the project might have been halted in its tracks if not for the enthusiasm of Johns Hopkins psychiatry chair Raymond DePaulo, who allowed me to shadow his team while they tended to inpatients. It was surprisingly easy to find a Crisis Intervention Team police officer to ride with, a little more effort to engage a mental health court judge.
Those who oppose forced treatment initially were more difficult to engage, but with perseverance, I was able to persuade the leadership of MindFreedom International to speak with me, and well, I ambushed a barely willing Scientologist while I was in New York for APA last May. In terms of patient participation, this hesitation did not hold true – many people volunteered to speak with me about how involuntary treatment harmed them, and it was much more difficult to find patients who felt helped by the treatment that was thrust upon them. Two absolutely wonderful women gave generously of themselves so that this project would have real voices to it: both “Lily” and “Eleanor” relived difficult experiences for me and allowed me to obtain their medical records and to speak with their families and their doctors. None of this was easy for them, but it did provide me with an education I would have gotten no other way as they reflected back on the meaning it had to them to have been committed to psychiatric units.
The subject of involuntary outpatient commitment has been particularly difficult to research, in part because I live in Maryland, a state which has no provision for this. I spoke with one family member in Arizona who initially was eager to be interviewed, along with her adult child who has come to feel that involuntary care has been very helpful. When I called back, the mom had changed her mind about participating: “You’re writing a book with a balanced view. There no balance or controversy here for me; it’s a medical problem that needs treatment. ” Unless I could promise to support, unequivocally, the views she held without qualification, she was not interested in participating in our book, even if it would provide an avenue to express her beliefs about the value of outpatient commitment. For similar reasons, I had to approach Ron Honberg, J.D., at the national office of the National Alliance on Mental Illness (NAMI); the Maryland NAMI members did not want me to speak with me after two articles I wrote for this Clinical Psychiatry News column suggested that I was not wholeheartedly in favor of outpatient commitment. I was told the topic was “too sensitive” for their members to discuss with me. So while I’ve learned that the topic inspires a great deal of emotion, there are still surprises with every step.
With all that as a prelude, I am continuing to look for people to interview who are the subjects of mandated civil outpatient treatment orders, as well as their family members. I thought perhaps readers might be able to help me, and I am interested in hearing both the good and the bad. If you, your patients, or their families would like to participate, by all means contact me at [email protected].
Dr. Miller is a coauthor of Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: Johns Hopkins University Press, 2011).
There are many controversies in psychiatry, but the most controversial issue continues to be that of involuntary treatment. Over the past year, I have been working on a book on forced care, along with Dr. Annette Hanson, the forensic psychiatrist who also writes this Shrink Rap News column. The work I’ve been doing for the manuscript – identifying and interviewing the people with a stake in the issue – has placed me in a funny role of being more journalist than physician. It’s a role I mostly love, and if you’ve hit the midpoint of your career and have an opportunity to dedicate some of your time to doing something completely different, I highly recommend shifting gears for a little while.
One of the things I have found most surprising is the reactions of people when I ask to include them. While most people are willing, almost all hesitate a little. Some are quite eager to participate, and one group in Richmond who uses involuntary electroconvulsive therapy heard of my project and extended an invitation for me to come visit, interview them, watch the procedure, and speak with one of their patients. Many people are proud of the work they do and eager to showcase it; they want to have their viewpoint included. With others, I have needed to ask repeatedly, listen to their concerns, and offer reassurances. I’ve taken to telling people they can read a draft of what I write about them – I learned early in the process that without this offer, few people would be willing to speak to me.
I wish I could say that I’ve noticed a pattern to who is comfortable speaking and who is not. Many of the psychiatrists and researchers I’ve approached have given their time willingly without hesitation ( or at least without that much hesitation), including Dr. E. Fuller Torrey; Dr. Paul Appelbaum; Jeffrey Swanson, Ph.D.; Dr. Steven Sharfstein; Dr. Daniel Fisher; Vermont Psychiatric Society President Margaret Bolton; Dr. Bruce Hershfield; and American Psychiatric Association President Paul Summergrad, to name just a few of the many people who have shared their time, experiences, and wisdom with me. It was not as easy for me to find a psychiatrist I could observe working on an inpatient unit, and the project might have been halted in its tracks if not for the enthusiasm of Johns Hopkins psychiatry chair Raymond DePaulo, who allowed me to shadow his team while they tended to inpatients. It was surprisingly easy to find a Crisis Intervention Team police officer to ride with, a little more effort to engage a mental health court judge.
Those who oppose forced treatment initially were more difficult to engage, but with perseverance, I was able to persuade the leadership of MindFreedom International to speak with me, and well, I ambushed a barely willing Scientologist while I was in New York for APA last May. In terms of patient participation, this hesitation did not hold true – many people volunteered to speak with me about how involuntary treatment harmed them, and it was much more difficult to find patients who felt helped by the treatment that was thrust upon them. Two absolutely wonderful women gave generously of themselves so that this project would have real voices to it: both “Lily” and “Eleanor” relived difficult experiences for me and allowed me to obtain their medical records and to speak with their families and their doctors. None of this was easy for them, but it did provide me with an education I would have gotten no other way as they reflected back on the meaning it had to them to have been committed to psychiatric units.
The subject of involuntary outpatient commitment has been particularly difficult to research, in part because I live in Maryland, a state which has no provision for this. I spoke with one family member in Arizona who initially was eager to be interviewed, along with her adult child who has come to feel that involuntary care has been very helpful. When I called back, the mom had changed her mind about participating: “You’re writing a book with a balanced view. There no balance or controversy here for me; it’s a medical problem that needs treatment. ” Unless I could promise to support, unequivocally, the views she held without qualification, she was not interested in participating in our book, even if it would provide an avenue to express her beliefs about the value of outpatient commitment. For similar reasons, I had to approach Ron Honberg, J.D., at the national office of the National Alliance on Mental Illness (NAMI); the Maryland NAMI members did not want me to speak with me after two articles I wrote for this Clinical Psychiatry News column suggested that I was not wholeheartedly in favor of outpatient commitment. I was told the topic was “too sensitive” for their members to discuss with me. So while I’ve learned that the topic inspires a great deal of emotion, there are still surprises with every step.
With all that as a prelude, I am continuing to look for people to interview who are the subjects of mandated civil outpatient treatment orders, as well as their family members. I thought perhaps readers might be able to help me, and I am interested in hearing both the good and the bad. If you, your patients, or their families would like to participate, by all means contact me at [email protected].
Dr. Miller is a coauthor of Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: Johns Hopkins University Press, 2011).
There are many controversies in psychiatry, but the most controversial issue continues to be that of involuntary treatment. Over the past year, I have been working on a book on forced care, along with Dr. Annette Hanson, the forensic psychiatrist who also writes this Shrink Rap News column. The work I’ve been doing for the manuscript – identifying and interviewing the people with a stake in the issue – has placed me in a funny role of being more journalist than physician. It’s a role I mostly love, and if you’ve hit the midpoint of your career and have an opportunity to dedicate some of your time to doing something completely different, I highly recommend shifting gears for a little while.
One of the things I have found most surprising is the reactions of people when I ask to include them. While most people are willing, almost all hesitate a little. Some are quite eager to participate, and one group in Richmond who uses involuntary electroconvulsive therapy heard of my project and extended an invitation for me to come visit, interview them, watch the procedure, and speak with one of their patients. Many people are proud of the work they do and eager to showcase it; they want to have their viewpoint included. With others, I have needed to ask repeatedly, listen to their concerns, and offer reassurances. I’ve taken to telling people they can read a draft of what I write about them – I learned early in the process that without this offer, few people would be willing to speak to me.
I wish I could say that I’ve noticed a pattern to who is comfortable speaking and who is not. Many of the psychiatrists and researchers I’ve approached have given their time willingly without hesitation ( or at least without that much hesitation), including Dr. E. Fuller Torrey; Dr. Paul Appelbaum; Jeffrey Swanson, Ph.D.; Dr. Steven Sharfstein; Dr. Daniel Fisher; Vermont Psychiatric Society President Margaret Bolton; Dr. Bruce Hershfield; and American Psychiatric Association President Paul Summergrad, to name just a few of the many people who have shared their time, experiences, and wisdom with me. It was not as easy for me to find a psychiatrist I could observe working on an inpatient unit, and the project might have been halted in its tracks if not for the enthusiasm of Johns Hopkins psychiatry chair Raymond DePaulo, who allowed me to shadow his team while they tended to inpatients. It was surprisingly easy to find a Crisis Intervention Team police officer to ride with, a little more effort to engage a mental health court judge.
Those who oppose forced treatment initially were more difficult to engage, but with perseverance, I was able to persuade the leadership of MindFreedom International to speak with me, and well, I ambushed a barely willing Scientologist while I was in New York for APA last May. In terms of patient participation, this hesitation did not hold true – many people volunteered to speak with me about how involuntary treatment harmed them, and it was much more difficult to find patients who felt helped by the treatment that was thrust upon them. Two absolutely wonderful women gave generously of themselves so that this project would have real voices to it: both “Lily” and “Eleanor” relived difficult experiences for me and allowed me to obtain their medical records and to speak with their families and their doctors. None of this was easy for them, but it did provide me with an education I would have gotten no other way as they reflected back on the meaning it had to them to have been committed to psychiatric units.
The subject of involuntary outpatient commitment has been particularly difficult to research, in part because I live in Maryland, a state which has no provision for this. I spoke with one family member in Arizona who initially was eager to be interviewed, along with her adult child who has come to feel that involuntary care has been very helpful. When I called back, the mom had changed her mind about participating: “You’re writing a book with a balanced view. There no balance or controversy here for me; it’s a medical problem that needs treatment. ” Unless I could promise to support, unequivocally, the views she held without qualification, she was not interested in participating in our book, even if it would provide an avenue to express her beliefs about the value of outpatient commitment. For similar reasons, I had to approach Ron Honberg, J.D., at the national office of the National Alliance on Mental Illness (NAMI); the Maryland NAMI members did not want me to speak with me after two articles I wrote for this Clinical Psychiatry News column suggested that I was not wholeheartedly in favor of outpatient commitment. I was told the topic was “too sensitive” for their members to discuss with me. So while I’ve learned that the topic inspires a great deal of emotion, there are still surprises with every step.
With all that as a prelude, I am continuing to look for people to interview who are the subjects of mandated civil outpatient treatment orders, as well as their family members. I thought perhaps readers might be able to help me, and I am interested in hearing both the good and the bad. If you, your patients, or their families would like to participate, by all means contact me at [email protected].
Dr. Miller is a coauthor of Shrink Rap: Three Psychiatrists Explain Their Work (Baltimore: Johns Hopkins University Press, 2011).
Shrink Rap News: The surprisingly high cost of Abilify
Recently, I gave a patient a prescription for Abilify. I wrote for 30 tablets of the lowest dose, 2 mg. While I knew it was expensive, I was shocked when the patient returned a few days later and told me it had cost $1,100 to fill the prescription; he not yet met the deductible for his health insurance and he had paid cash for the medication.
According to Medscape (and Twitter, too), Abilify is the medication that grosses more money than any other pharmaceutical in the United States. In the 12-month period from July 2013 to June 2014, sales of Abilify totaled $7.2 billion. An atypical antipsychotic medication that is widely marketed to TV viewers as an augmenting agent to treat major depression, Abilify is the 14th most-prescribed medication in the United States. If you’re wondering, the most prescribed medications are Synthroid, Crestor, and Nexium. Abilify has been available in this country since 2002, initially with an indication for schizophrenia. Since then, indications have expanded to include bipolar disorder, irritability in autism, as well as augmentation for major depression.
Still, $1,100 for 30 tablets? I wondered if the high cost was attributed to where the patient went – a boutique independent pharmacy. I decided to make some calls to local pharmacists (see the table), and queried druggists at CVS, Walmart, and Lykos, an independent pharmacy in Towson, Md. I also checked with a Walmart in Vermont to see if the prices were the same in another part of the country, and they were. Let me share with you what I learned.
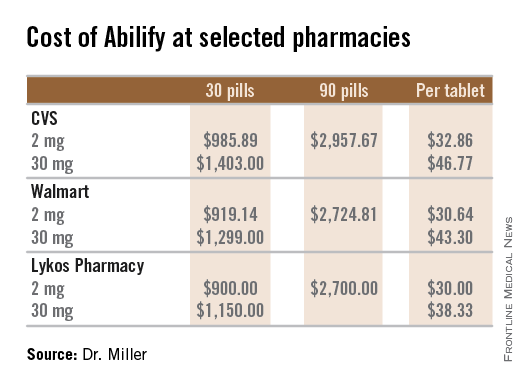
For the three pharmacies I called, a single 2-mg tablet of Abilify cost between $30 and $33, so the cost was less than the $1,100 my patient paid. There is no discount for buying in bulk, and the price per pill stays virtually the same whether a patient buys 1 pill, 30 pills, or 90 pills. I checked with two pharmacies, and the price for a tablet is the same for the dosages of 2 mg, 5 mg, 10 mg, and 15 mg. The price rises to $38-$47 per pill for the 20-mg and 30-mg dose.
As physicians in a health care system where resources are limited, it is incumbent upon us to at least consider the cost of the tests and treatments we order, but we often have no way of knowing what these costs actually are. Was I missing something? Is everyone else aware that Abilify is this costly? I did a quick survey of a handful of psychiatrists by text message (please don’t count this as science), requesting a guess for the cost of a single 2-mg tablet of Abilify. The responses I received ranged from $7 to $20, and a lone respondent answered $40. For the most part, the cost of medications remains opaque to the prescriber.
If I had to do it again, I still would have prescribed Abilify to this particular patient. I would have suggested he buy only a few tablets to start, and I would have prescribed the 5-mg dose and recommended splitting the pills to halve the cost. In a December 2006 article in Current Psychiatry, “Pros and cons of pill splitting,” Dr. Rakesh Jain and Dr. Shailesh Jain note that it is safe to divide Abilify tablets. Filling only a few tablets seems like the prudent thing to do with such an expensive medication, at least until it is clear that it is tolerable to the patient, but as we know, filling less than a month’s supply often creates hurdles and increased copays when health insurance is paying for the prescription. And with requirements for preauthorization, I’m not certain if it’s even possible for a patient to take home just a few to try.
When I informed the psychiatrists I queried that Abilify costs $30-$33 per 2-mg dose, they expressed their surprise. One friend, however, put it most aptly with her reply of simply, “Good grief.”
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently, I gave a patient a prescription for Abilify. I wrote for 30 tablets of the lowest dose, 2 mg. While I knew it was expensive, I was shocked when the patient returned a few days later and told me it had cost $1,100 to fill the prescription; he not yet met the deductible for his health insurance and he had paid cash for the medication.
According to Medscape (and Twitter, too), Abilify is the medication that grosses more money than any other pharmaceutical in the United States. In the 12-month period from July 2013 to June 2014, sales of Abilify totaled $7.2 billion. An atypical antipsychotic medication that is widely marketed to TV viewers as an augmenting agent to treat major depression, Abilify is the 14th most-prescribed medication in the United States. If you’re wondering, the most prescribed medications are Synthroid, Crestor, and Nexium. Abilify has been available in this country since 2002, initially with an indication for schizophrenia. Since then, indications have expanded to include bipolar disorder, irritability in autism, as well as augmentation for major depression.
Still, $1,100 for 30 tablets? I wondered if the high cost was attributed to where the patient went – a boutique independent pharmacy. I decided to make some calls to local pharmacists (see the table), and queried druggists at CVS, Walmart, and Lykos, an independent pharmacy in Towson, Md. I also checked with a Walmart in Vermont to see if the prices were the same in another part of the country, and they were. Let me share with you what I learned.
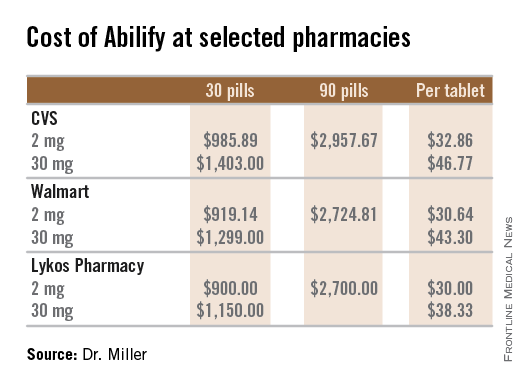
For the three pharmacies I called, a single 2-mg tablet of Abilify cost between $30 and $33, so the cost was less than the $1,100 my patient paid. There is no discount for buying in bulk, and the price per pill stays virtually the same whether a patient buys 1 pill, 30 pills, or 90 pills. I checked with two pharmacies, and the price for a tablet is the same for the dosages of 2 mg, 5 mg, 10 mg, and 15 mg. The price rises to $38-$47 per pill for the 20-mg and 30-mg dose.
As physicians in a health care system where resources are limited, it is incumbent upon us to at least consider the cost of the tests and treatments we order, but we often have no way of knowing what these costs actually are. Was I missing something? Is everyone else aware that Abilify is this costly? I did a quick survey of a handful of psychiatrists by text message (please don’t count this as science), requesting a guess for the cost of a single 2-mg tablet of Abilify. The responses I received ranged from $7 to $20, and a lone respondent answered $40. For the most part, the cost of medications remains opaque to the prescriber.
If I had to do it again, I still would have prescribed Abilify to this particular patient. I would have suggested he buy only a few tablets to start, and I would have prescribed the 5-mg dose and recommended splitting the pills to halve the cost. In a December 2006 article in Current Psychiatry, “Pros and cons of pill splitting,” Dr. Rakesh Jain and Dr. Shailesh Jain note that it is safe to divide Abilify tablets. Filling only a few tablets seems like the prudent thing to do with such an expensive medication, at least until it is clear that it is tolerable to the patient, but as we know, filling less than a month’s supply often creates hurdles and increased copays when health insurance is paying for the prescription. And with requirements for preauthorization, I’m not certain if it’s even possible for a patient to take home just a few to try.
When I informed the psychiatrists I queried that Abilify costs $30-$33 per 2-mg dose, they expressed their surprise. One friend, however, put it most aptly with her reply of simply, “Good grief.”
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).
Recently, I gave a patient a prescription for Abilify. I wrote for 30 tablets of the lowest dose, 2 mg. While I knew it was expensive, I was shocked when the patient returned a few days later and told me it had cost $1,100 to fill the prescription; he not yet met the deductible for his health insurance and he had paid cash for the medication.
According to Medscape (and Twitter, too), Abilify is the medication that grosses more money than any other pharmaceutical in the United States. In the 12-month period from July 2013 to June 2014, sales of Abilify totaled $7.2 billion. An atypical antipsychotic medication that is widely marketed to TV viewers as an augmenting agent to treat major depression, Abilify is the 14th most-prescribed medication in the United States. If you’re wondering, the most prescribed medications are Synthroid, Crestor, and Nexium. Abilify has been available in this country since 2002, initially with an indication for schizophrenia. Since then, indications have expanded to include bipolar disorder, irritability in autism, as well as augmentation for major depression.
Still, $1,100 for 30 tablets? I wondered if the high cost was attributed to where the patient went – a boutique independent pharmacy. I decided to make some calls to local pharmacists (see the table), and queried druggists at CVS, Walmart, and Lykos, an independent pharmacy in Towson, Md. I also checked with a Walmart in Vermont to see if the prices were the same in another part of the country, and they were. Let me share with you what I learned.
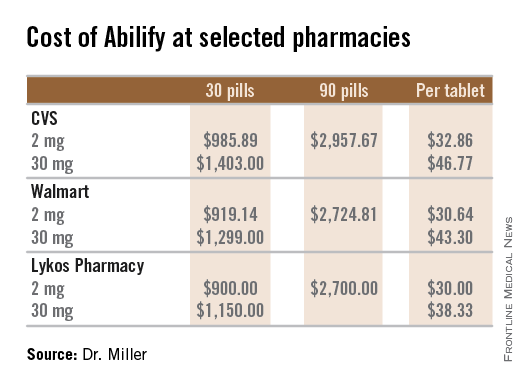
For the three pharmacies I called, a single 2-mg tablet of Abilify cost between $30 and $33, so the cost was less than the $1,100 my patient paid. There is no discount for buying in bulk, and the price per pill stays virtually the same whether a patient buys 1 pill, 30 pills, or 90 pills. I checked with two pharmacies, and the price for a tablet is the same for the dosages of 2 mg, 5 mg, 10 mg, and 15 mg. The price rises to $38-$47 per pill for the 20-mg and 30-mg dose.
As physicians in a health care system where resources are limited, it is incumbent upon us to at least consider the cost of the tests and treatments we order, but we often have no way of knowing what these costs actually are. Was I missing something? Is everyone else aware that Abilify is this costly? I did a quick survey of a handful of psychiatrists by text message (please don’t count this as science), requesting a guess for the cost of a single 2-mg tablet of Abilify. The responses I received ranged from $7 to $20, and a lone respondent answered $40. For the most part, the cost of medications remains opaque to the prescriber.
If I had to do it again, I still would have prescribed Abilify to this particular patient. I would have suggested he buy only a few tablets to start, and I would have prescribed the 5-mg dose and recommended splitting the pills to halve the cost. In a December 2006 article in Current Psychiatry, “Pros and cons of pill splitting,” Dr. Rakesh Jain and Dr. Shailesh Jain note that it is safe to divide Abilify tablets. Filling only a few tablets seems like the prudent thing to do with such an expensive medication, at least until it is clear that it is tolerable to the patient, but as we know, filling less than a month’s supply often creates hurdles and increased copays when health insurance is paying for the prescription. And with requirements for preauthorization, I’m not certain if it’s even possible for a patient to take home just a few to try.
When I informed the psychiatrists I queried that Abilify costs $30-$33 per 2-mg dose, they expressed their surprise. One friend, however, put it most aptly with her reply of simply, “Good grief.”
Dr. Miller is a coauthor of “Shrink Rap: Three Psychiatrists Explain Their Work” (Baltimore: Johns Hopkins University Press, 2011).















