User login
DSM-5 criteria 'at odds' with early autism diagnosis
WASHINGTON – The new Diagnostic and Statistical Manual of Mental Disorders criteria for autism spectrum disorder might significantly affect the diagnosis of ASD in very young children, a retrospective analysis has shown.
Only 35% of a sample of children diagnosed with ASD before age 3 based on DSM-IV criteria retained the diagnosis when DSM-5 criteria were applied.
"The strict nature of the criteria in a population whose symptomatology may be emerging is at odds with an early diagnosis model," said Dr. Lisa H. Shulman, director of the Rehabilitation, Evaluation and Learning for Autistic Infants and Toddlers program at the Albert Einstein College of Medicine, New York.
"Clearly, prospective studies on the impact of DSM-5 on early diagnosis are needed," she said at the annual meeting of the Pediatric Academic Societies (PAS).
Studies of the impact of the new criteria on diagnosis of ASD have focused on school-age children. Dr. Shulman and her coinvestigators looked at younger children, examining all the children who had been diagnosed with ASD by 3 years of age based on a multidisciplinary evaluation at their center during 2003-2010. Diagnoses were based on DSM-IV criteria. Childhood Autism Rating Scale (CARS) scores also were examined, however, and cognitive testing was completed in some of the children.
To determine how many of the children would retain the diagnosis using DSM-5 criteria, an algorithm was used to map data from the DSM-IV and the CARS scores onto the DSM-5 criteria. Of 237 children who had been diagnosed with ASD by age 3 at the inner-city early intervention program, only 84 children (35%) met the criteria for ASD using the DSM-5 criteria.
The children whose diagnosis was retained using DSM-5 criteria were significantly more likely to have had higher CARS scores (38.3 vs. 33.5), which are indicative of more severe social impairment. They also had a trend toward lower cognition, with 34% of those with an IQ of less than 70 diagnosed under DSM-5 criteria, compared with 12% with IQ greater than 70, Dr. Shulman reported.
The potential of the DSM-5 criteria to diagnose the more impaired children preferentially might present an obstacle to diagnosis for the children most likely to benefit from early intervention – those with the mildest symptomatology, she said.
To be classified as having ASD using the DSM-5 criteria, a child has to meet each of three categories of social-communication criteria: deficits in social-emotional reciprocity; deficits in nonverbal communicative behaviors used for social interaction; and deficits in developing and maintaining relationships and adjusting behavior to social contexts appropriate to developmental level.
In addition, a child also must have at least two out of four types of restrictive/repetitive patterns of behavior, interests, or activities: stereotyped or repetitive speech, motor movements, or use of objects; excessive adherence to routines or ritualized patterns of verbal or nonverbal behavior; highly restricted fixated interests that are abnormal in intensity or focus; and hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment.
The group of social-communication criteria least commonly met by the children in the study was "deficits in developing relationships." The specific criteria included in this group – difficulty sharing imaginative play, difficulty in making friends, and absence of interest in people – are especially challenging to apply to and evaluate in young children, said Dr. Shulman, associate professor of pediatrics at Albert Einstein.
Only 61% of the children met at least one of the criteria in this category. "For very young children, where we’re not in the situation to have information or parental concerns regarding making friends, we’re left with ‘absence of interest in people’ – a pretty extreme criteria," she said.
Three of the four "restrictive/repetitive" interests were reported in less than half of the children. While repetitive use of objects or motor movements was present in 89%, excessive adherence to routines was reported in 28%, restricted interests in 41%, and hyper-hypo sensitivity in 25%.
The low rate of hyper-hypo sensitivity was "interesting," Dr. Shulman noted, as inclusion of these sensitivities is new to the manual and "thought to be a nod to young children, who often have more of these symptoms." Consideration of CARS scores in the analysis provided some degree of a measure for these sensitivities, she noted.
The DSM-IV described five different disorders under the general category of "pervasive developmental disorders," for which diagnoses could be made based on 12 criteria; this allowed for any of 2,688 combinations of criteria to arrive at a diagnosis. Under the new version, which describes 1 disorder based on 5 out of 7 criteria being met, "only 12 combinations of criteria can arrive at a diagnosis," Dr. Shulman noted.
The children in the analysis had a mean age of 26.7 months and were 76% male, 19% white, 43% Hispanic, and 25% black.
"From our experience in New York City, a diagnosis made early is largely a valid one," Dr. Shulman said. "The kids who do best [with intervention] have the milder social impairment and the higher cognitive functioning."
Thus far, New York has had a "very generous" approach to intervention for ASD, with early intervention programs making their own diagnoses. "I’m more concerned about places that require [an outside] diagnosis in order to get ASD-specific services in early intervention programs," she noted.
The fifth edition of psychiatry’s diagnostic guide was officially released in May at the American Psychiatric Association’s annual meeting, shortly after Dr. Shulman presented the findings at the PAS meeting. The update is the first in nearly 20 years.
Dr. Shulman reported that she and her coinvestigators have no relevant disclosures.
WASHINGTON – The new Diagnostic and Statistical Manual of Mental Disorders criteria for autism spectrum disorder might significantly affect the diagnosis of ASD in very young children, a retrospective analysis has shown.
Only 35% of a sample of children diagnosed with ASD before age 3 based on DSM-IV criteria retained the diagnosis when DSM-5 criteria were applied.
"The strict nature of the criteria in a population whose symptomatology may be emerging is at odds with an early diagnosis model," said Dr. Lisa H. Shulman, director of the Rehabilitation, Evaluation and Learning for Autistic Infants and Toddlers program at the Albert Einstein College of Medicine, New York.
"Clearly, prospective studies on the impact of DSM-5 on early diagnosis are needed," she said at the annual meeting of the Pediatric Academic Societies (PAS).
Studies of the impact of the new criteria on diagnosis of ASD have focused on school-age children. Dr. Shulman and her coinvestigators looked at younger children, examining all the children who had been diagnosed with ASD by 3 years of age based on a multidisciplinary evaluation at their center during 2003-2010. Diagnoses were based on DSM-IV criteria. Childhood Autism Rating Scale (CARS) scores also were examined, however, and cognitive testing was completed in some of the children.
To determine how many of the children would retain the diagnosis using DSM-5 criteria, an algorithm was used to map data from the DSM-IV and the CARS scores onto the DSM-5 criteria. Of 237 children who had been diagnosed with ASD by age 3 at the inner-city early intervention program, only 84 children (35%) met the criteria for ASD using the DSM-5 criteria.
The children whose diagnosis was retained using DSM-5 criteria were significantly more likely to have had higher CARS scores (38.3 vs. 33.5), which are indicative of more severe social impairment. They also had a trend toward lower cognition, with 34% of those with an IQ of less than 70 diagnosed under DSM-5 criteria, compared with 12% with IQ greater than 70, Dr. Shulman reported.
The potential of the DSM-5 criteria to diagnose the more impaired children preferentially might present an obstacle to diagnosis for the children most likely to benefit from early intervention – those with the mildest symptomatology, she said.
To be classified as having ASD using the DSM-5 criteria, a child has to meet each of three categories of social-communication criteria: deficits in social-emotional reciprocity; deficits in nonverbal communicative behaviors used for social interaction; and deficits in developing and maintaining relationships and adjusting behavior to social contexts appropriate to developmental level.
In addition, a child also must have at least two out of four types of restrictive/repetitive patterns of behavior, interests, or activities: stereotyped or repetitive speech, motor movements, or use of objects; excessive adherence to routines or ritualized patterns of verbal or nonverbal behavior; highly restricted fixated interests that are abnormal in intensity or focus; and hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment.
The group of social-communication criteria least commonly met by the children in the study was "deficits in developing relationships." The specific criteria included in this group – difficulty sharing imaginative play, difficulty in making friends, and absence of interest in people – are especially challenging to apply to and evaluate in young children, said Dr. Shulman, associate professor of pediatrics at Albert Einstein.
Only 61% of the children met at least one of the criteria in this category. "For very young children, where we’re not in the situation to have information or parental concerns regarding making friends, we’re left with ‘absence of interest in people’ – a pretty extreme criteria," she said.
Three of the four "restrictive/repetitive" interests were reported in less than half of the children. While repetitive use of objects or motor movements was present in 89%, excessive adherence to routines was reported in 28%, restricted interests in 41%, and hyper-hypo sensitivity in 25%.
The low rate of hyper-hypo sensitivity was "interesting," Dr. Shulman noted, as inclusion of these sensitivities is new to the manual and "thought to be a nod to young children, who often have more of these symptoms." Consideration of CARS scores in the analysis provided some degree of a measure for these sensitivities, she noted.
The DSM-IV described five different disorders under the general category of "pervasive developmental disorders," for which diagnoses could be made based on 12 criteria; this allowed for any of 2,688 combinations of criteria to arrive at a diagnosis. Under the new version, which describes 1 disorder based on 5 out of 7 criteria being met, "only 12 combinations of criteria can arrive at a diagnosis," Dr. Shulman noted.
The children in the analysis had a mean age of 26.7 months and were 76% male, 19% white, 43% Hispanic, and 25% black.
"From our experience in New York City, a diagnosis made early is largely a valid one," Dr. Shulman said. "The kids who do best [with intervention] have the milder social impairment and the higher cognitive functioning."
Thus far, New York has had a "very generous" approach to intervention for ASD, with early intervention programs making their own diagnoses. "I’m more concerned about places that require [an outside] diagnosis in order to get ASD-specific services in early intervention programs," she noted.
The fifth edition of psychiatry’s diagnostic guide was officially released in May at the American Psychiatric Association’s annual meeting, shortly after Dr. Shulman presented the findings at the PAS meeting. The update is the first in nearly 20 years.
Dr. Shulman reported that she and her coinvestigators have no relevant disclosures.
WASHINGTON – The new Diagnostic and Statistical Manual of Mental Disorders criteria for autism spectrum disorder might significantly affect the diagnosis of ASD in very young children, a retrospective analysis has shown.
Only 35% of a sample of children diagnosed with ASD before age 3 based on DSM-IV criteria retained the diagnosis when DSM-5 criteria were applied.
"The strict nature of the criteria in a population whose symptomatology may be emerging is at odds with an early diagnosis model," said Dr. Lisa H. Shulman, director of the Rehabilitation, Evaluation and Learning for Autistic Infants and Toddlers program at the Albert Einstein College of Medicine, New York.
"Clearly, prospective studies on the impact of DSM-5 on early diagnosis are needed," she said at the annual meeting of the Pediatric Academic Societies (PAS).
Studies of the impact of the new criteria on diagnosis of ASD have focused on school-age children. Dr. Shulman and her coinvestigators looked at younger children, examining all the children who had been diagnosed with ASD by 3 years of age based on a multidisciplinary evaluation at their center during 2003-2010. Diagnoses were based on DSM-IV criteria. Childhood Autism Rating Scale (CARS) scores also were examined, however, and cognitive testing was completed in some of the children.
To determine how many of the children would retain the diagnosis using DSM-5 criteria, an algorithm was used to map data from the DSM-IV and the CARS scores onto the DSM-5 criteria. Of 237 children who had been diagnosed with ASD by age 3 at the inner-city early intervention program, only 84 children (35%) met the criteria for ASD using the DSM-5 criteria.
The children whose diagnosis was retained using DSM-5 criteria were significantly more likely to have had higher CARS scores (38.3 vs. 33.5), which are indicative of more severe social impairment. They also had a trend toward lower cognition, with 34% of those with an IQ of less than 70 diagnosed under DSM-5 criteria, compared with 12% with IQ greater than 70, Dr. Shulman reported.
The potential of the DSM-5 criteria to diagnose the more impaired children preferentially might present an obstacle to diagnosis for the children most likely to benefit from early intervention – those with the mildest symptomatology, she said.
To be classified as having ASD using the DSM-5 criteria, a child has to meet each of three categories of social-communication criteria: deficits in social-emotional reciprocity; deficits in nonverbal communicative behaviors used for social interaction; and deficits in developing and maintaining relationships and adjusting behavior to social contexts appropriate to developmental level.
In addition, a child also must have at least two out of four types of restrictive/repetitive patterns of behavior, interests, or activities: stereotyped or repetitive speech, motor movements, or use of objects; excessive adherence to routines or ritualized patterns of verbal or nonverbal behavior; highly restricted fixated interests that are abnormal in intensity or focus; and hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment.
The group of social-communication criteria least commonly met by the children in the study was "deficits in developing relationships." The specific criteria included in this group – difficulty sharing imaginative play, difficulty in making friends, and absence of interest in people – are especially challenging to apply to and evaluate in young children, said Dr. Shulman, associate professor of pediatrics at Albert Einstein.
Only 61% of the children met at least one of the criteria in this category. "For very young children, where we’re not in the situation to have information or parental concerns regarding making friends, we’re left with ‘absence of interest in people’ – a pretty extreme criteria," she said.
Three of the four "restrictive/repetitive" interests were reported in less than half of the children. While repetitive use of objects or motor movements was present in 89%, excessive adherence to routines was reported in 28%, restricted interests in 41%, and hyper-hypo sensitivity in 25%.
The low rate of hyper-hypo sensitivity was "interesting," Dr. Shulman noted, as inclusion of these sensitivities is new to the manual and "thought to be a nod to young children, who often have more of these symptoms." Consideration of CARS scores in the analysis provided some degree of a measure for these sensitivities, she noted.
The DSM-IV described five different disorders under the general category of "pervasive developmental disorders," for which diagnoses could be made based on 12 criteria; this allowed for any of 2,688 combinations of criteria to arrive at a diagnosis. Under the new version, which describes 1 disorder based on 5 out of 7 criteria being met, "only 12 combinations of criteria can arrive at a diagnosis," Dr. Shulman noted.
The children in the analysis had a mean age of 26.7 months and were 76% male, 19% white, 43% Hispanic, and 25% black.
"From our experience in New York City, a diagnosis made early is largely a valid one," Dr. Shulman said. "The kids who do best [with intervention] have the milder social impairment and the higher cognitive functioning."
Thus far, New York has had a "very generous" approach to intervention for ASD, with early intervention programs making their own diagnoses. "I’m more concerned about places that require [an outside] diagnosis in order to get ASD-specific services in early intervention programs," she noted.
The fifth edition of psychiatry’s diagnostic guide was officially released in May at the American Psychiatric Association’s annual meeting, shortly after Dr. Shulman presented the findings at the PAS meeting. The update is the first in nearly 20 years.
Dr. Shulman reported that she and her coinvestigators have no relevant disclosures.
AT THE PAS ANNUAL MEETING
Major finding: Of 237 children who had been diagnosed with ASD by age 3 based on DSM-IV criteria over a 7-year period, only 35% met the criteria for ASD using the DSM-5 criteria.
Data source: Retrospective analysis of all children with ASD diagnosed at an early intervention program during 2003-2010.
Disclosures: Dr. Shulman reported that she and her coinvestigators have no relevant disclosures.
Despite laws, almost half of teens text while driving
WASHINGTON – Nearly half of teens reported texting while driving at least once in the past 30 days, according to two analyses of survey data from the Centers for Disease Control and Prevention.
And state laws banning texting while driving are having little impact among teen drivers, researchers cautioned.
Physicians "need to discuss this with license-eligible teens, and they need to [help ensure], too, that parents are not [setting an example] by texting while driving," said Dr. Andrew Adesman, chief of developmental and behavioral pediatrics at Cohen Children’s Medical Center of New York in New Hyde Park, who presented an analysis of the CDC survey data at the annual meeting of the Pediatric Academic Societies.
Motor vehicle accidents are the leading cause of death among teenagers, and many experts believe that texting while driving is more dangerous for all drivers than driving while intoxicated. One previous study of adult drivers found that the act of texting while driving raises the risk of a crash 23-fold.
The CDC conducts its national Youth Risk Behavior Surveillance System survey every 2 years to monitor six types of health risk behaviors that contribute to the leading causes of death, disability, and social problems among U.S. youths.
For the first time, the 2011 survey included a question about texting while driving: "During the past 30 days, on how many days did you text or e-mail while driving a car or other vehicle?" Of the nationally representative sample of high school students, approximately 8,500 students responded to the question.
Researchers performed two separate analyses of the CDC survey data – one conducted by CDC officials and published in June in Pediatrics, and another presented by Dr. Adesman at the meeting.
According to the CDC analysis, approximately 45% of respondents reported texting while driving during the 30 days before the survey, and more than one in four of these teens (12% of the total) said they do so everyday. The prevalence of any texting while driving increased with age, from 33% for 16-year-olds to 58% for students aged 18 and older.
Male students also were more likely to report texting while driving (46%) than female students (42%), reported Emily O’Malley Olsen and her associates at the CDC (Pediatrics 2013 [doi:10.1542/peds.2012-3462]).
The analyses also demonstrated that students who text while driving are more likely to engage in several other high-risk behaviors.
Students who engaged in texting while driving were 5.33 times more likely to drive when they had been drinking alcohol than students who did not engage in texting while driving. They were also more likely to not always wear their seatbelts and to ride with a driver who had been drinking alcohol. The prevalence of each risky motor-vehicle behavior increased as the frequency of texting while driving increased.
Dr. Adesman’s study assessed a broader range of high-risk behaviors – not only driving-related behaviors – in examining the association of other behaviors with texting while driving. He and his coinvestigators found that teens who texted while driving were significantly more likely to drink and drive, frequently consume alcohol, use indoor tanning devices, and have unprotected sex.
They also examined the effectiveness of state laws. Teens living in a state with a law that prohibits texting while driving were only slightly less likely to report the practice than teens living in a state without such a law.
"State laws banning texting while driving are not effective," Dr. Adesman said in an interview after the meeting. "The most likely effective intervention would be for parents, with their teens’ consent, to download applications that turn off the texting function while the car is in motion. We have some of this technology available today, and more should be developed."
Physicians can also suggest that teens pledge – in official agreements or "contracts" with their parents – not to text while driving, he said.
The two studies used different criteria for their samples. While the CDC analysis looked at all students 16 years of age and older, Dr. Adesman and his coinvestigators limited their sample to teens who, in their states, were eligible to drive with a full or unrestricted license. The two analyses’ main findings on the prevalence of texting while driving were similar, however, with 49% of males and 45% of females reportedly engaging in the practice.
The new data build on several previous studies that show high rates of texting while driving among teens. In an Insurance Institute for Highway Safety telephone survey in 2010 of approximately 1,200 drivers across the United States, 13% of drivers of all ages, and 43% of drivers aged 18-24 years, reported texting while driving.
The investigators of both studies reported that they had no relevant financial disclosures.
WASHINGTON – Nearly half of teens reported texting while driving at least once in the past 30 days, according to two analyses of survey data from the Centers for Disease Control and Prevention.
And state laws banning texting while driving are having little impact among teen drivers, researchers cautioned.
Physicians "need to discuss this with license-eligible teens, and they need to [help ensure], too, that parents are not [setting an example] by texting while driving," said Dr. Andrew Adesman, chief of developmental and behavioral pediatrics at Cohen Children’s Medical Center of New York in New Hyde Park, who presented an analysis of the CDC survey data at the annual meeting of the Pediatric Academic Societies.
Motor vehicle accidents are the leading cause of death among teenagers, and many experts believe that texting while driving is more dangerous for all drivers than driving while intoxicated. One previous study of adult drivers found that the act of texting while driving raises the risk of a crash 23-fold.
The CDC conducts its national Youth Risk Behavior Surveillance System survey every 2 years to monitor six types of health risk behaviors that contribute to the leading causes of death, disability, and social problems among U.S. youths.
For the first time, the 2011 survey included a question about texting while driving: "During the past 30 days, on how many days did you text or e-mail while driving a car or other vehicle?" Of the nationally representative sample of high school students, approximately 8,500 students responded to the question.
Researchers performed two separate analyses of the CDC survey data – one conducted by CDC officials and published in June in Pediatrics, and another presented by Dr. Adesman at the meeting.
According to the CDC analysis, approximately 45% of respondents reported texting while driving during the 30 days before the survey, and more than one in four of these teens (12% of the total) said they do so everyday. The prevalence of any texting while driving increased with age, from 33% for 16-year-olds to 58% for students aged 18 and older.
Male students also were more likely to report texting while driving (46%) than female students (42%), reported Emily O’Malley Olsen and her associates at the CDC (Pediatrics 2013 [doi:10.1542/peds.2012-3462]).
The analyses also demonstrated that students who text while driving are more likely to engage in several other high-risk behaviors.
Students who engaged in texting while driving were 5.33 times more likely to drive when they had been drinking alcohol than students who did not engage in texting while driving. They were also more likely to not always wear their seatbelts and to ride with a driver who had been drinking alcohol. The prevalence of each risky motor-vehicle behavior increased as the frequency of texting while driving increased.
Dr. Adesman’s study assessed a broader range of high-risk behaviors – not only driving-related behaviors – in examining the association of other behaviors with texting while driving. He and his coinvestigators found that teens who texted while driving were significantly more likely to drink and drive, frequently consume alcohol, use indoor tanning devices, and have unprotected sex.
They also examined the effectiveness of state laws. Teens living in a state with a law that prohibits texting while driving were only slightly less likely to report the practice than teens living in a state without such a law.
"State laws banning texting while driving are not effective," Dr. Adesman said in an interview after the meeting. "The most likely effective intervention would be for parents, with their teens’ consent, to download applications that turn off the texting function while the car is in motion. We have some of this technology available today, and more should be developed."
Physicians can also suggest that teens pledge – in official agreements or "contracts" with their parents – not to text while driving, he said.
The two studies used different criteria for their samples. While the CDC analysis looked at all students 16 years of age and older, Dr. Adesman and his coinvestigators limited their sample to teens who, in their states, were eligible to drive with a full or unrestricted license. The two analyses’ main findings on the prevalence of texting while driving were similar, however, with 49% of males and 45% of females reportedly engaging in the practice.
The new data build on several previous studies that show high rates of texting while driving among teens. In an Insurance Institute for Highway Safety telephone survey in 2010 of approximately 1,200 drivers across the United States, 13% of drivers of all ages, and 43% of drivers aged 18-24 years, reported texting while driving.
The investigators of both studies reported that they had no relevant financial disclosures.
WASHINGTON – Nearly half of teens reported texting while driving at least once in the past 30 days, according to two analyses of survey data from the Centers for Disease Control and Prevention.
And state laws banning texting while driving are having little impact among teen drivers, researchers cautioned.
Physicians "need to discuss this with license-eligible teens, and they need to [help ensure], too, that parents are not [setting an example] by texting while driving," said Dr. Andrew Adesman, chief of developmental and behavioral pediatrics at Cohen Children’s Medical Center of New York in New Hyde Park, who presented an analysis of the CDC survey data at the annual meeting of the Pediatric Academic Societies.
Motor vehicle accidents are the leading cause of death among teenagers, and many experts believe that texting while driving is more dangerous for all drivers than driving while intoxicated. One previous study of adult drivers found that the act of texting while driving raises the risk of a crash 23-fold.
The CDC conducts its national Youth Risk Behavior Surveillance System survey every 2 years to monitor six types of health risk behaviors that contribute to the leading causes of death, disability, and social problems among U.S. youths.
For the first time, the 2011 survey included a question about texting while driving: "During the past 30 days, on how many days did you text or e-mail while driving a car or other vehicle?" Of the nationally representative sample of high school students, approximately 8,500 students responded to the question.
Researchers performed two separate analyses of the CDC survey data – one conducted by CDC officials and published in June in Pediatrics, and another presented by Dr. Adesman at the meeting.
According to the CDC analysis, approximately 45% of respondents reported texting while driving during the 30 days before the survey, and more than one in four of these teens (12% of the total) said they do so everyday. The prevalence of any texting while driving increased with age, from 33% for 16-year-olds to 58% for students aged 18 and older.
Male students also were more likely to report texting while driving (46%) than female students (42%), reported Emily O’Malley Olsen and her associates at the CDC (Pediatrics 2013 [doi:10.1542/peds.2012-3462]).
The analyses also demonstrated that students who text while driving are more likely to engage in several other high-risk behaviors.
Students who engaged in texting while driving were 5.33 times more likely to drive when they had been drinking alcohol than students who did not engage in texting while driving. They were also more likely to not always wear their seatbelts and to ride with a driver who had been drinking alcohol. The prevalence of each risky motor-vehicle behavior increased as the frequency of texting while driving increased.
Dr. Adesman’s study assessed a broader range of high-risk behaviors – not only driving-related behaviors – in examining the association of other behaviors with texting while driving. He and his coinvestigators found that teens who texted while driving were significantly more likely to drink and drive, frequently consume alcohol, use indoor tanning devices, and have unprotected sex.
They also examined the effectiveness of state laws. Teens living in a state with a law that prohibits texting while driving were only slightly less likely to report the practice than teens living in a state without such a law.
"State laws banning texting while driving are not effective," Dr. Adesman said in an interview after the meeting. "The most likely effective intervention would be for parents, with their teens’ consent, to download applications that turn off the texting function while the car is in motion. We have some of this technology available today, and more should be developed."
Physicians can also suggest that teens pledge – in official agreements or "contracts" with their parents – not to text while driving, he said.
The two studies used different criteria for their samples. While the CDC analysis looked at all students 16 years of age and older, Dr. Adesman and his coinvestigators limited their sample to teens who, in their states, were eligible to drive with a full or unrestricted license. The two analyses’ main findings on the prevalence of texting while driving were similar, however, with 49% of males and 45% of females reportedly engaging in the practice.
The new data build on several previous studies that show high rates of texting while driving among teens. In an Insurance Institute for Highway Safety telephone survey in 2010 of approximately 1,200 drivers across the United States, 13% of drivers of all ages, and 43% of drivers aged 18-24 years, reported texting while driving.
The investigators of both studies reported that they had no relevant financial disclosures.
AT THE PAS ANNUAL MEETING
Major finding: Approximately 45% of teens reported texting while driving at least once in the past 30 days, according to one analysis of national survey data. In another analysis, the prevalence was slightly higher.
Data source: The CDC’s 2011 Youth Risk Behavior Surveillance System involving a nationally representative sample of high school students.
Disclosures: Ms. Olsen and her associates and Dr. Andrew Adesman and his associates reported that they had no relevant financial disclosures.
Study supports laws requiring cyclists to wear helmets
WASHINGTON – Mandatory bicycle helmet laws are associated with a lower incidence of fatalities among youth cyclists involved in motor vehicle collisions, a national analysis has shown.
States with laws that require bicyclists to wear helmets had only 84% of the deaths per population that those without helmet laws had, after adjustment for other potential confounding factors, Dr. William P. Meehan III reported at the annual meeting of the Pediatric Academic Societies.
"Twenty-nine states still do not have [laws requiring cyclists to wear helmets], and we think they should be considered," said Dr. Meehan, director of the Micheli Center for Sports Injury Prevention and the Sports Concussion Clinic in the division of sports medicine at Boston Children’s Hospital.
Approximately 900 people die each year in bicycle crashes, three-quarters of them from traumatic brain injuries. On a local level, previous studies have shown that the laws result in increased helmet usage and decreased risk of injury and death in bicycle–motor vehicle collisions.
To assess the effect nationally, Dr. Meehan and his colleagues analyzed data on U.S. bicyclists younger than 16 years of age who died between January 1999 and December 2009. They used the Fatality Analysis Reporting System (FARS) to compare death rates in states with and without mandatory helmet laws. FARS is run by the National Highway Traffic Safety Administration and collects data on all motor vehicle accidents that result in the death of someone involved in a collision.
Over the study period, 1,612 bicyclists under the age of 16 died in a collision with a motor vehicle. The mean unadjusted rate of fatalities was 2 per million in states with helmet laws, versus 2.5 per million in states without the laws. The overall unadjusted incidence rate ratio was 0.83.
After adjustment for three factors that could potentially influence the rate of fatality in bicycle–motor vehicle collisions – elderly driver licensure laws, legal blood alcohol limits (lower than .08% versus .08% or higher), and household income, states with mandatory helmet laws continued to be associated with lower rates of fatalities, with an adjusted incidence rate ratio of 0.84, reported Dr. Meehan, also of the department of pediatrics at Harvard Medical School, Boston.
Because the FARS database includes only collisions that resulted in fatalities – and not other severe injuries – there’s "potentially much greater benefit in helmet legislation" than is reflected by the study findings, he noted.
The American Academy of Pediatrics supports legislation that requires all cyclists to use helmets.
State laws requiring the use of bicycle helmets cover populations up to varying ages, but almost all cover children up to 16 years of age.
At the start of the study period, 16 states had bicycle helmet laws. By the end, in 2009, 19 states and the District of Columbia had helmet laws. (At least two of the additional laws were enacted in the earlier part of the study period). Helmet mandates have also been established by some local municipalities throughout the country, but the analysis covered only states.
The study was funded in part by the Micheli Center for Sports Injury Prevention and the National Institutes of Health. Dr. Meehan reported that he had no relevant financial disclosures.
WASHINGTON – Mandatory bicycle helmet laws are associated with a lower incidence of fatalities among youth cyclists involved in motor vehicle collisions, a national analysis has shown.
States with laws that require bicyclists to wear helmets had only 84% of the deaths per population that those without helmet laws had, after adjustment for other potential confounding factors, Dr. William P. Meehan III reported at the annual meeting of the Pediatric Academic Societies.
"Twenty-nine states still do not have [laws requiring cyclists to wear helmets], and we think they should be considered," said Dr. Meehan, director of the Micheli Center for Sports Injury Prevention and the Sports Concussion Clinic in the division of sports medicine at Boston Children’s Hospital.
Approximately 900 people die each year in bicycle crashes, three-quarters of them from traumatic brain injuries. On a local level, previous studies have shown that the laws result in increased helmet usage and decreased risk of injury and death in bicycle–motor vehicle collisions.
To assess the effect nationally, Dr. Meehan and his colleagues analyzed data on U.S. bicyclists younger than 16 years of age who died between January 1999 and December 2009. They used the Fatality Analysis Reporting System (FARS) to compare death rates in states with and without mandatory helmet laws. FARS is run by the National Highway Traffic Safety Administration and collects data on all motor vehicle accidents that result in the death of someone involved in a collision.
Over the study period, 1,612 bicyclists under the age of 16 died in a collision with a motor vehicle. The mean unadjusted rate of fatalities was 2 per million in states with helmet laws, versus 2.5 per million in states without the laws. The overall unadjusted incidence rate ratio was 0.83.
After adjustment for three factors that could potentially influence the rate of fatality in bicycle–motor vehicle collisions – elderly driver licensure laws, legal blood alcohol limits (lower than .08% versus .08% or higher), and household income, states with mandatory helmet laws continued to be associated with lower rates of fatalities, with an adjusted incidence rate ratio of 0.84, reported Dr. Meehan, also of the department of pediatrics at Harvard Medical School, Boston.
Because the FARS database includes only collisions that resulted in fatalities – and not other severe injuries – there’s "potentially much greater benefit in helmet legislation" than is reflected by the study findings, he noted.
The American Academy of Pediatrics supports legislation that requires all cyclists to use helmets.
State laws requiring the use of bicycle helmets cover populations up to varying ages, but almost all cover children up to 16 years of age.
At the start of the study period, 16 states had bicycle helmet laws. By the end, in 2009, 19 states and the District of Columbia had helmet laws. (At least two of the additional laws were enacted in the earlier part of the study period). Helmet mandates have also been established by some local municipalities throughout the country, but the analysis covered only states.
The study was funded in part by the Micheli Center for Sports Injury Prevention and the National Institutes of Health. Dr. Meehan reported that he had no relevant financial disclosures.
WASHINGTON – Mandatory bicycle helmet laws are associated with a lower incidence of fatalities among youth cyclists involved in motor vehicle collisions, a national analysis has shown.
States with laws that require bicyclists to wear helmets had only 84% of the deaths per population that those without helmet laws had, after adjustment for other potential confounding factors, Dr. William P. Meehan III reported at the annual meeting of the Pediatric Academic Societies.
"Twenty-nine states still do not have [laws requiring cyclists to wear helmets], and we think they should be considered," said Dr. Meehan, director of the Micheli Center for Sports Injury Prevention and the Sports Concussion Clinic in the division of sports medicine at Boston Children’s Hospital.
Approximately 900 people die each year in bicycle crashes, three-quarters of them from traumatic brain injuries. On a local level, previous studies have shown that the laws result in increased helmet usage and decreased risk of injury and death in bicycle–motor vehicle collisions.
To assess the effect nationally, Dr. Meehan and his colleagues analyzed data on U.S. bicyclists younger than 16 years of age who died between January 1999 and December 2009. They used the Fatality Analysis Reporting System (FARS) to compare death rates in states with and without mandatory helmet laws. FARS is run by the National Highway Traffic Safety Administration and collects data on all motor vehicle accidents that result in the death of someone involved in a collision.
Over the study period, 1,612 bicyclists under the age of 16 died in a collision with a motor vehicle. The mean unadjusted rate of fatalities was 2 per million in states with helmet laws, versus 2.5 per million in states without the laws. The overall unadjusted incidence rate ratio was 0.83.
After adjustment for three factors that could potentially influence the rate of fatality in bicycle–motor vehicle collisions – elderly driver licensure laws, legal blood alcohol limits (lower than .08% versus .08% or higher), and household income, states with mandatory helmet laws continued to be associated with lower rates of fatalities, with an adjusted incidence rate ratio of 0.84, reported Dr. Meehan, also of the department of pediatrics at Harvard Medical School, Boston.
Because the FARS database includes only collisions that resulted in fatalities – and not other severe injuries – there’s "potentially much greater benefit in helmet legislation" than is reflected by the study findings, he noted.
The American Academy of Pediatrics supports legislation that requires all cyclists to use helmets.
State laws requiring the use of bicycle helmets cover populations up to varying ages, but almost all cover children up to 16 years of age.
At the start of the study period, 16 states had bicycle helmet laws. By the end, in 2009, 19 states and the District of Columbia had helmet laws. (At least two of the additional laws were enacted in the earlier part of the study period). Helmet mandates have also been established by some local municipalities throughout the country, but the analysis covered only states.
The study was funded in part by the Micheli Center for Sports Injury Prevention and the National Institutes of Health. Dr. Meehan reported that he had no relevant financial disclosures.
AT THE PAS ANNUAL MEETING
Major finding: States with mandatory bicycle helmet laws had only 84% of the deaths per population that states without helmet laws had, after adjustment for potential confounding factors.
Data source: A cross-sectional study of data from the national Fatality Analysis Reporting System.
Disclosures: Dr. Meehan reported that he had no relevant financial disclosures.
Robotic Hysterectomy Takes Off, Causing Concern
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
“Robotics will probably be the future of surgery,” said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). “We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery.”
Robotic assistance “is great for some procedures, like myomectomies, where there is more suturing. But I really don't see a huge benefit overall for less complex, benign cases,” he said in an interview. “We're even seeing supracervical hysterectomies being done [robotically] – that doesn't make any sense.”
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
“Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy,” they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization's Robert Hunt Award for the “best article” published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. “We're not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible,” he said.
Authors of a broader recently published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, “across the full range of 20 types of surgery for which studies exist,” the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the “limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures,” said Dr. Gabriel I. Barbash of the medical school at Tel Aviv University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
“Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we're using for laparoscopy and now robotics? Maybe … there are some studies suggesting [this], but we have no definitive data,” Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be “stable in spite of robotics,” comprising about 20%-25% of all hysterectomies. “The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good,” he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
“At least in our community of 400,000 women, there was a positive shift,” Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. “If there's a big shift from abdominal surgery to robotic surgery, that will be cost effective. … But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society,” said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is “whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities].”
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for nonsurgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical's five main “target markets,” according to a company investor presentation, and hysterectomy is one of four “target” gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical's Mr. Simmonds.
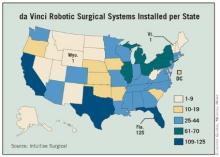
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
“General ob.gyns. don't want to be the only physicians in the community not offering it,” said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an “unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies,” they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. “What if residents go somewhere afterward where there isn't a robot, for instance? Will [they have learned enough] to safely operate?” he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
'Are we killing the art with the new technology we're using for laparoscopy and now robotics?'
Source DR. PASIC
'The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good.'
Source DR. MAGRINA
'General ob.gyns. don't want to be the only physicians in the community not offering [robotic surgery].'
Source DR. DELMORE
Source Elsevier Global Medical News
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
“Robotics will probably be the future of surgery,” said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). “We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery.”
Robotic assistance “is great for some procedures, like myomectomies, where there is more suturing. But I really don't see a huge benefit overall for less complex, benign cases,” he said in an interview. “We're even seeing supracervical hysterectomies being done [robotically] – that doesn't make any sense.”
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
“Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy,” they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization's Robert Hunt Award for the “best article” published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. “We're not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible,” he said.
Authors of a broader recently published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, “across the full range of 20 types of surgery for which studies exist,” the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the “limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures,” said Dr. Gabriel I. Barbash of the medical school at Tel Aviv University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
“Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we're using for laparoscopy and now robotics? Maybe … there are some studies suggesting [this], but we have no definitive data,” Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be “stable in spite of robotics,” comprising about 20%-25% of all hysterectomies. “The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good,” he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
“At least in our community of 400,000 women, there was a positive shift,” Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. “If there's a big shift from abdominal surgery to robotic surgery, that will be cost effective. … But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society,” said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is “whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities].”
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for nonsurgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical's five main “target markets,” according to a company investor presentation, and hysterectomy is one of four “target” gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical's Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
“General ob.gyns. don't want to be the only physicians in the community not offering it,” said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an “unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies,” they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. “What if residents go somewhere afterward where there isn't a robot, for instance? Will [they have learned enough] to safely operate?” he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
'Are we killing the art with the new technology we're using for laparoscopy and now robotics?'
Source DR. PASIC
'The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good.'
Source DR. MAGRINA
'General ob.gyns. don't want to be the only physicians in the community not offering [robotic surgery].'
Source DR. DELMORE
Source Elsevier Global Medical News
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
“Robotics will probably be the future of surgery,” said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). “We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery.”
Robotic assistance “is great for some procedures, like myomectomies, where there is more suturing. But I really don't see a huge benefit overall for less complex, benign cases,” he said in an interview. “We're even seeing supracervical hysterectomies being done [robotically] – that doesn't make any sense.”
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
“Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy,” they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization's Robert Hunt Award for the “best article” published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. “We're not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible,” he said.
Authors of a broader recently published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, “across the full range of 20 types of surgery for which studies exist,” the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the “limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures,” said Dr. Gabriel I. Barbash of the medical school at Tel Aviv University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
“Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we're using for laparoscopy and now robotics? Maybe … there are some studies suggesting [this], but we have no definitive data,” Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be “stable in spite of robotics,” comprising about 20%-25% of all hysterectomies. “The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good,” he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
“At least in our community of 400,000 women, there was a positive shift,” Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. “If there's a big shift from abdominal surgery to robotic surgery, that will be cost effective. … But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society,” said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is “whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities].”
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for nonsurgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical's five main “target markets,” according to a company investor presentation, and hysterectomy is one of four “target” gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical's Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
“General ob.gyns. don't want to be the only physicians in the community not offering it,” said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an “unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies,” they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. “What if residents go somewhere afterward where there isn't a robot, for instance? Will [they have learned enough] to safely operate?” he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
'Are we killing the art with the new technology we're using for laparoscopy and now robotics?'
Source DR. PASIC
'The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good.'
Source DR. MAGRINA
'General ob.gyns. don't want to be the only physicians in the community not offering [robotic surgery].'
Source DR. DELMORE
Source Elsevier Global Medical News
Robotic Hysterectomy Takes Off, Causing Some Concern
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically-assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
"Robotics will probably be the future of surgery," said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). "We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery."
Robotic assistance "is great for some procedures, like myomectomies, where there is more suturing. But I really don’t see a huge benefit overall for less complex, benign cases," he said in an interview. "We’re even seeing supracervical hysterectomies being done [robotically] – that doesn’t make any sense."
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
"Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy," they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization’s Robert Hunt Award for the "best article" published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. "We’re not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible," he said.
Authors of a broader recently-published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, "across the full range of 20 types of surgery for which studies exist," the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the "limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures," said Dr. Gabriel I. Barbash of the medical school at Tel Aviv (Israel) University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
"Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we’re using for laparoscopy and now robotics? Maybe ... there are some studies suggesting [this], but we have no definitive data," Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be "stable in spite of robotics," comprising about 20%-25% of all hysterectomies. "The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good," he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
"At least in our community of 400,000 women, there was a positive shift," Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. "If there’s a big shift from abdominal surgery to robotic surgery, that will be cost-effective. ... But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society," said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is "whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities]."
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for non-surgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical’s five main "target markets," according to a company investor presentation, and hysterectomy is one of four "target" gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical’s Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
"General ob.gyns. don’t want to be the only physicians in the community not offering it," said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an "unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies," they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. "What if residents go somewhere afterward where there isn’t a robot, for instance? Will [they have learned enough] to safely operate?" he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically-assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
"Robotics will probably be the future of surgery," said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). "We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery."
Robotic assistance "is great for some procedures, like myomectomies, where there is more suturing. But I really don’t see a huge benefit overall for less complex, benign cases," he said in an interview. "We’re even seeing supracervical hysterectomies being done [robotically] – that doesn’t make any sense."
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
"Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy," they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization’s Robert Hunt Award for the "best article" published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. "We’re not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible," he said.
Authors of a broader recently-published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, "across the full range of 20 types of surgery for which studies exist," the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the "limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures," said Dr. Gabriel I. Barbash of the medical school at Tel Aviv (Israel) University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
"Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we’re using for laparoscopy and now robotics? Maybe ... there are some studies suggesting [this], but we have no definitive data," Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be "stable in spite of robotics," comprising about 20%-25% of all hysterectomies. "The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good," he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
"At least in our community of 400,000 women, there was a positive shift," Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. "If there’s a big shift from abdominal surgery to robotic surgery, that will be cost-effective. ... But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society," said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is "whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities]."
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for non-surgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical’s five main "target markets," according to a company investor presentation, and hysterectomy is one of four "target" gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical’s Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
"General ob.gyns. don’t want to be the only physicians in the community not offering it," said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an "unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies," they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. "What if residents go somewhere afterward where there isn’t a robot, for instance? Will [they have learned enough] to safely operate?" he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
A recent explosion of interest in robotic surgery for routine hysterectomies and treatment of other nononcologic gynecologic conditions is raising concern about the cost and comparative value of the robot over conventional laparoscopy, as well as the future of vaginal hysterectomy and current and future training needs.
In 2010, for the first time, more hysterectomies were performed with the da Vinci Surgical System than any other procedure, including prostatectomy. The number of robotic-assisted hysterectomies performed worldwide grew to 110,000 in 2010, from approximately 69,000 the year before.
Approximately 32,000 of these hysterectomies were for treatment of cancer, and the remaining 78,000 were related to benign conditions, according to Chris Simmonds, senior director of marketing for Intuitive Surgical, which makes the da Vinci, the only such system currently on the market.
Gynecologic oncologists swiftly embraced the robotic surgical system after it was approved in 2005 for gynecologic surgical procedures because it enabled them to perform minimally invasive endometrial cancer staging – something most surgeons found too technically challenging with pure laparoscopy.
While issues of cost and training have been part of an ongoing debate in gynecologic oncology, such issues have taken on new meaning – and more urgency – with the more recent rise in robotically-assisted routine hysterectomy. It can be argued, some experts explain, that an advantage exists for robotics in gynecologic oncology that, overall, does not exist for benign disease.
"Robotics will probably be the future of surgery," said Dr. Resad P. Pasic, professor of obstetrics and gynecology and director of operative gynecologic endoscopy at the University of Louisville (Ky.). "We need to [better understand] what the real advantages are, however, especially for routine laparoscopic hysterectomies, because the cost is higher than traditional laparoscopy and vaginal surgery."
Robotic assistance "is great for some procedures, like myomectomies, where there is more suturing. But I really don’t see a huge benefit overall for less complex, benign cases," he said in an interview. "We’re even seeing supracervical hysterectomies being done [robotically] – that doesn’t make any sense."
A study published last year, which Dr. Pasic coauthored, found higher per-case hospital costs with robotic-assisted hysterectomies, compared with conventional laparoscopic hysterectomies, without any significant differences in complications, postsurgical infections, or frequency of hemorrhage.
Robot-assisted hysterectomies were associated with longer surgical times and cost an average of $2,600 more, the investigators reported (J. Minim. Invasive Gynecol. 2010;17:730-8).
Using the Premier hospital database, they analyzed patient records and billing and insurance data for more than 36,000 women who received minimally invasive hysterectomy during 2007-2008 in more than 350 hospitals. Their cost analysis reflected the cost of the robotic procedure to the hospital but did not include the acquisition or maintenance costs of the robotic device over time.
The robotic unit costs between $1 million and $2.3 million and is associated with annual maintenance costs of $100,000-$170,000 a year, and instrumentation/accessories costs of $1,300-$2,200 per procedure, according to Intuitive Surgical.
"Further decisions regarding the diffusion of robot technology in routine laparoscopic hysterectomy," they concluded, must be informed by randomized controlled studies of comparative effectiveness.
At the annual meeting of the American Association of Gynecologic Laparoscopists last month, the paper won the organization’s Robert Hunt Award for the "best article" published in the Journal of Minimally Invasive Gynecology in the past year. The study may cause some to pause, however, in that it was funded by Ethicon Endo-Surgery, and because three of the six coauthors have notable ties with Ethicon – one is employed by the company, one is a consultant, and Dr. Pasic is a speaker for the company.
Dr. Pasic, who said he uses the da Vinci for about 10% of his procedures, dismissed any suggestions of bias. "We’re not the only paper concluding there is a high cost to robotics, and we made every effort to be as impartial as possible," he said.
Authors of a broader recently-published analysis of robotic-assisted surgery and health care costs drew similar conclusions about comparative value. The investigators examined all the cost studies of robot-assisted procedures published since 2005 and reported that, on average, "across the full range of 20 types of surgery for which studies exist," the additional cost of using a robot-assisted procedure was about $1,600, or about 6% of the cost of the procedure in 2007 (N. Eng. J. Med. 2010;363:701-4).
There have not been any large-scale randomized trials of robot-assisted surgery, and the "limited observational evidence fails to show that the long-term outcomes of robot-assisted surgery are superior to those of conventional procedures," said Dr. Gabriel I. Barbash of the medical school at Tel Aviv (Israel) University and Sherry A. Glied, Ph.D., of the school of public health at Columbia University, New York.
With hysterectomy, a pure vaginal approach has long been viewed by many experts as the preferable approach whenever possible – the most cost-effective minimally invasive method – and some experts are concerned that the growing popularity of robotics may chip away at its use.
"Vaginal hysterectomy is an art, so the question is, are we killing the art with the new technology we’re using for laparoscopy and now robotics? Maybe ... there are some studies suggesting [this], but we have no definitive data," Dr. Pasic said.
Dr. Javier Magrina, a professor of obstetrics and gynecology and director of gynecologic oncology at the Mayo Clinic in Scottsdale, Ariz., who has written and lectured extensively on robotic surgery from the standpoint of both benign and malignant disease, said that so far, vaginal hysterectomy rates appear to be "stable in spite of robotics," comprising about 20%-25% of all hysterectomies. "The increase of robotic hysterectomy so far has decreased the number of laparotomies, which is very good," he said in an interview.
Dr. Jed Delmore and his colleagues at the University of Kansas in Wichita found just this when they compared the types of hysterectomy performed at their teaching hospital and two outpatient surgery centers during two periods of time: before robotic surgery became locally available (2006-2007) and 2 years after it arrived (2009-2010).
Using electronic medical record and billing data to identify hysterectomies, they found that the number of abdominal hysterectomies decreased significantly, while the number of vaginal hysterectomies remained relatively constant. The unpublished findings were presented at the American Congress of Obstetricians and Gynecologists District VII meeting in Kansas City in September.
"At least in our community of 400,000 women, there was a positive shift," Dr. Delmore said in an interview.
Still, he said, the potential longer-term impact of robotics on vaginal hysterectomy is a concern. "If there’s a big shift from abdominal surgery to robotic surgery, that will be cost-effective. ... But if it turns out that over time fewer women end up having vaginal hysterectomies, and have robotic hysterectomies instead, there will be greater expense to individuals and society," said Dr. Delmore, professor of obstetrics and gynecology and director of gynecologic oncology at the university.
An even larger concern, he noted, is "whether robotic surgery, as it becomes more and more available, will increase the total volume of hysterectomies – in women who would have previously been treated with hormone therapy or [other modalities]."
Such a trend may be occurring with prostatectomy, note the authors of the New England Journal of Medicine cost analysis, with robotic technology possibly contributing to the substitution of surgical for non-surgical treatments for prostate cancer.
This does not appear to be happening with hysterectomy in the Kansas City area thus far, Dr. Delmore said.
The undercurrents may already exist, however. Gynecology is one of Intuitive Surgical’s five main "target markets," according to a company investor presentation, and hysterectomy is one of four "target" gynecologic procedures, along with sacral colpopexy, myomectomy, and endometrial resection.
With an estimated 600,000 hysterectomies being performed each year in the United States, Intuitive sees potential for growth. As of this fall, the 2011 surgical volume with the da Vinci had increased 30% over 2010 volume across all types of procedures, said Intuitive Surgical’s Mr. Simmonds.
Having a surgical robot has become a status symbol of sorts for hospitals in many urban areas – as of September, Intuitive had installed 1,478 da Vinci surgical systems in the United States – and ob.gyns. may feel compelled to keep up with market demands.
"General ob.gyns. don’t want to be the only physicians in the community not offering it," said Dr. Delmore, who teaches robotic surgery as a proctor for Intuitive Surgical.
Many ob.gyns., moreover, find robotic-assisted laparoscopy much easier than conventional laparoscopy to learn and adopt. Suturing is easier, and Dr. Magrina and other proponents of robotics maintain that the advantages of instrument articulation and steady three-dimensional vision have proven even higher than expected – for hysterectomies as well as more complex gynecologic procedures.
While the learning curve for robotics is said to be relatively short, Dr. Pasic and his coauthors caution that robotic assistance should not be used by physicians who are unwilling to invest time and effort into laparoscopic training. Exuberance for the da Vinci could have an "unintended negative effect on resident and fellow training as it relates to overall laparoscopic competencies," they said.
Institutions, in the meantime, are individually attempting to determine how best to train residents in robotic-assisted surgery. The University of Kansas is implementing a training model for ob.gyn. residents that includes an online tutorial, training with inanimate objects, animal lab training, and bedside assistance in real robotic-assisted hysterectomies.
Dr. Delmore and his colleagues have a study underway to look at how graduate ob.gyns. utilize this training. "What if residents go somewhere afterward where there isn’t a robot, for instance? Will [they have learned enough] to safely operate?" he said.
Dr. Magrina said he had no relevant financial disclosures. Dr. Delmore teaches robotic surgery as a proctor for Intuitive Surgical. Dr. Pasic is a speaker for Ethicon Endo-Surgery.
Repeated Anesthesia Before Age 2 Linked to Learning Disabilities
Repeated exposure to anesthesia and surgery before the age of 2 years was a significant independent risk factor for the later development of learning disabilities in a matched cohort study involving children in one school district, adjustment for comorbidity, and multiple outcome measures.
No association was seen after a single episode of anesthesia and surgery, according to Dr. Randall P. Flick and his colleagues at the Mayo Clinic in Rochester, Minn.
In the past decade, animal studies have firmly established a relationship between the use of general anesthetics during periods of rapid brain growth and widespread apoptotic neurodegeneration, with adverse effects of learning and behavior, according to the researchers.
Some clinical studies have provided insight, but with mixed findings and without controlling for comorbidity and without examining multiple types of outcomes, they wrote.
Even with the new study, which identified multiple anesthesia exposures as a significant risk factor for the development of learning disabilities (hazard ratio of 2.16), the clinical relevance remains uncertain. But "at this point, we cannot exclude the possibility that multiple exposures to anesthesia/surgery may adversely affect neurodevelopment," said Dr. Flick of the department of anesthesiology, and his associates (Pediatrics 2011 [doi:10.1542/peds.2011-0351]).
The investigators followed a cohort of children born between 1976 and 1982 to mothers who resided in the same community, attended the same schools, and received virtually all their health care at the Mayo Clinic or at Olmstead Medical Center in Rochester, Minn.
Children who were exposed to anesthesia before age 2 years (350 of the 5,357 children in the cohort) were matched with two unexposed children (700 of the children in the cohort) on the basis on factors known to influence the incidence of learning disabilities, including gender, mother’s education, birth weight, and gestational age.
Two methods were used to quantify health status at age 5 years, and school records were used to track when children developed learning disabilities.
In addition to learning disabilities (overall as well as the subtypes of reading, written language, and mathematics), the study’s outcomes included receipt of an individualized education program (IEP) and results of group-administered tests of cognition and achievement.
By age 19, the cumulative incidence of learning disabilities (with adjustments made for comorbidities and health status) was 21.3% for unexposed controls, 23.6% for those with a single exposure, and 36.6% for those with multiple exposures.
A similar pattern was observed for each subtype of learning disability and in group-administered tests of achievement and cognition. Multiple exposures were associated with lower scores in most of the standardized tests.
Multiple exposures to anesthesia also appeared to affect the rate of children receiving an IEP for difficulties with speech and language, but had no effect on the need for an IEP relating to emotional/behavioral disorders, the investigators reported.
Of the 350 children exposed to general anesthesia early on, 286 were exposed once and 64 were exposed more than once. The most frequent anesthesia was a combination of halothane (87.5%) and nitrous oxide (88.1%).
The findings suggest that any neurodevelopmental effects of multiple exposure may be limited to impairment of speech and language rather than to developmental disorders more generally, the researchers wrote. "However, this can only be a provisional conclusion," they wrote, because the IEP for emotional/behavioral disorders captures only more severely disruptive behaviors.
Overall, they cautioned, the study cannot distinguish between the effects of anesthesia per se, and surgery or the need for surgery. In addition, the measures used to control for health status may not have captured all potential confounders.
Children who were severely mentally retarded were excluded from the study; of these 19 children, all but 1 were known to have profound neurodevelopmental deficits before exposure to anesthesia and surgery.
The study was supported by a grant from the U.S. National Institute of Aging. Dr. Flick and his colleagues reported no relevant financial relationships.
The clinical significance of anesthesia neurotoxicity is controversial and remains uncertain, but with publication of the study by researchers at the Mayo Clinic, pediatricians can expect questions from parents and should "verse themselves on the subject," said Dr. Robert K. Williams.
"From this point forward, pediatricians must be an intimate part of the discussion," he said. "As the primary drivers of most surgical and diagnostic procedures, pediatricians will have to assess whether the benefits [of procedures] justify the purported but completely unquantifiable risk of the anesthetic or sedative."
Anesthesia neurotoxicity is a difficult issue to investigate, he noted, as it is "extraordinarily difficult" to isolate the effects of general anesthesia per se. The Mayo group’s study is important, however, because it took advantage of a unique database, and because the findings suggest an association between 2 or more episodes of anesthesia and surgery, and the subsequent development of learning disabilities.
"Although the authors controlled for burden of illness as best as was practical, it is not possible to completely isolate the need for surgery and any potential effects of the surgical procedure from the effects of the anesthetic per se. The clinical significance of these limitations remains subject to vigorous debate," he said.
Pediatricians and parents should be reassured by the study’s "failure to reveal any discernible clinical effects after a single exposure," and the fact that "regional anesthesia seems to be free of risk from neurotoxicity," Dr. Williams said.
Several other prospective human trials are underway, he noted, but these studies will only examine the effect of a single exposure to surgery and anesthesia. A well-designed comprehensive study on the effects of multiple episodes seems "many years away at best and, perhaps ultimately, impractical."
In the meantime, pediatricians should be aware of the concerns about potential neurotoxicity of general anesthetics, but should "also understand the current limitations of the evidence," he said.
Dr. Williams is a pediatric anesthesiologist at the University of Vermont in Burlington. His comments were adapted from an accompanying editorial (Pediatrics 2011[doi:10.1542/peds.2011-2489]). Dr. Williams reported that he has no relevant financial relationships.
The clinical significance of anesthesia neurotoxicity is controversial and remains uncertain, but with publication of the study by researchers at the Mayo Clinic, pediatricians can expect questions from parents and should "verse themselves on the subject," said Dr. Robert K. Williams.
"From this point forward, pediatricians must be an intimate part of the discussion," he said. "As the primary drivers of most surgical and diagnostic procedures, pediatricians will have to assess whether the benefits [of procedures] justify the purported but completely unquantifiable risk of the anesthetic or sedative."
Anesthesia neurotoxicity is a difficult issue to investigate, he noted, as it is "extraordinarily difficult" to isolate the effects of general anesthesia per se. The Mayo group’s study is important, however, because it took advantage of a unique database, and because the findings suggest an association between 2 or more episodes of anesthesia and surgery, and the subsequent development of learning disabilities.
"Although the authors controlled for burden of illness as best as was practical, it is not possible to completely isolate the need for surgery and any potential effects of the surgical procedure from the effects of the anesthetic per se. The clinical significance of these limitations remains subject to vigorous debate," he said.
Pediatricians and parents should be reassured by the study’s "failure to reveal any discernible clinical effects after a single exposure," and the fact that "regional anesthesia seems to be free of risk from neurotoxicity," Dr. Williams said.
Several other prospective human trials are underway, he noted, but these studies will only examine the effect of a single exposure to surgery and anesthesia. A well-designed comprehensive study on the effects of multiple episodes seems "many years away at best and, perhaps ultimately, impractical."
In the meantime, pediatricians should be aware of the concerns about potential neurotoxicity of general anesthetics, but should "also understand the current limitations of the evidence," he said.
Dr. Williams is a pediatric anesthesiologist at the University of Vermont in Burlington. His comments were adapted from an accompanying editorial (Pediatrics 2011[doi:10.1542/peds.2011-2489]). Dr. Williams reported that he has no relevant financial relationships.
The clinical significance of anesthesia neurotoxicity is controversial and remains uncertain, but with publication of the study by researchers at the Mayo Clinic, pediatricians can expect questions from parents and should "verse themselves on the subject," said Dr. Robert K. Williams.
"From this point forward, pediatricians must be an intimate part of the discussion," he said. "As the primary drivers of most surgical and diagnostic procedures, pediatricians will have to assess whether the benefits [of procedures] justify the purported but completely unquantifiable risk of the anesthetic or sedative."
Anesthesia neurotoxicity is a difficult issue to investigate, he noted, as it is "extraordinarily difficult" to isolate the effects of general anesthesia per se. The Mayo group’s study is important, however, because it took advantage of a unique database, and because the findings suggest an association between 2 or more episodes of anesthesia and surgery, and the subsequent development of learning disabilities.
"Although the authors controlled for burden of illness as best as was practical, it is not possible to completely isolate the need for surgery and any potential effects of the surgical procedure from the effects of the anesthetic per se. The clinical significance of these limitations remains subject to vigorous debate," he said.
Pediatricians and parents should be reassured by the study’s "failure to reveal any discernible clinical effects after a single exposure," and the fact that "regional anesthesia seems to be free of risk from neurotoxicity," Dr. Williams said.
Several other prospective human trials are underway, he noted, but these studies will only examine the effect of a single exposure to surgery and anesthesia. A well-designed comprehensive study on the effects of multiple episodes seems "many years away at best and, perhaps ultimately, impractical."
In the meantime, pediatricians should be aware of the concerns about potential neurotoxicity of general anesthetics, but should "also understand the current limitations of the evidence," he said.
Dr. Williams is a pediatric anesthesiologist at the University of Vermont in Burlington. His comments were adapted from an accompanying editorial (Pediatrics 2011[doi:10.1542/peds.2011-2489]). Dr. Williams reported that he has no relevant financial relationships.
Repeated exposure to anesthesia and surgery before the age of 2 years was a significant independent risk factor for the later development of learning disabilities in a matched cohort study involving children in one school district, adjustment for comorbidity, and multiple outcome measures.
No association was seen after a single episode of anesthesia and surgery, according to Dr. Randall P. Flick and his colleagues at the Mayo Clinic in Rochester, Minn.
In the past decade, animal studies have firmly established a relationship between the use of general anesthetics during periods of rapid brain growth and widespread apoptotic neurodegeneration, with adverse effects of learning and behavior, according to the researchers.
Some clinical studies have provided insight, but with mixed findings and without controlling for comorbidity and without examining multiple types of outcomes, they wrote.
Even with the new study, which identified multiple anesthesia exposures as a significant risk factor for the development of learning disabilities (hazard ratio of 2.16), the clinical relevance remains uncertain. But "at this point, we cannot exclude the possibility that multiple exposures to anesthesia/surgery may adversely affect neurodevelopment," said Dr. Flick of the department of anesthesiology, and his associates (Pediatrics 2011 [doi:10.1542/peds.2011-0351]).
The investigators followed a cohort of children born between 1976 and 1982 to mothers who resided in the same community, attended the same schools, and received virtually all their health care at the Mayo Clinic or at Olmstead Medical Center in Rochester, Minn.
Children who were exposed to anesthesia before age 2 years (350 of the 5,357 children in the cohort) were matched with two unexposed children (700 of the children in the cohort) on the basis on factors known to influence the incidence of learning disabilities, including gender, mother’s education, birth weight, and gestational age.
Two methods were used to quantify health status at age 5 years, and school records were used to track when children developed learning disabilities.
In addition to learning disabilities (overall as well as the subtypes of reading, written language, and mathematics), the study’s outcomes included receipt of an individualized education program (IEP) and results of group-administered tests of cognition and achievement.
By age 19, the cumulative incidence of learning disabilities (with adjustments made for comorbidities and health status) was 21.3% for unexposed controls, 23.6% for those with a single exposure, and 36.6% for those with multiple exposures.
A similar pattern was observed for each subtype of learning disability and in group-administered tests of achievement and cognition. Multiple exposures were associated with lower scores in most of the standardized tests.
Multiple exposures to anesthesia also appeared to affect the rate of children receiving an IEP for difficulties with speech and language, but had no effect on the need for an IEP relating to emotional/behavioral disorders, the investigators reported.
Of the 350 children exposed to general anesthesia early on, 286 were exposed once and 64 were exposed more than once. The most frequent anesthesia was a combination of halothane (87.5%) and nitrous oxide (88.1%).
The findings suggest that any neurodevelopmental effects of multiple exposure may be limited to impairment of speech and language rather than to developmental disorders more generally, the researchers wrote. "However, this can only be a provisional conclusion," they wrote, because the IEP for emotional/behavioral disorders captures only more severely disruptive behaviors.
Overall, they cautioned, the study cannot distinguish between the effects of anesthesia per se, and surgery or the need for surgery. In addition, the measures used to control for health status may not have captured all potential confounders.
Children who were severely mentally retarded were excluded from the study; of these 19 children, all but 1 were known to have profound neurodevelopmental deficits before exposure to anesthesia and surgery.
The study was supported by a grant from the U.S. National Institute of Aging. Dr. Flick and his colleagues reported no relevant financial relationships.
Repeated exposure to anesthesia and surgery before the age of 2 years was a significant independent risk factor for the later development of learning disabilities in a matched cohort study involving children in one school district, adjustment for comorbidity, and multiple outcome measures.
No association was seen after a single episode of anesthesia and surgery, according to Dr. Randall P. Flick and his colleagues at the Mayo Clinic in Rochester, Minn.
In the past decade, animal studies have firmly established a relationship between the use of general anesthetics during periods of rapid brain growth and widespread apoptotic neurodegeneration, with adverse effects of learning and behavior, according to the researchers.
Some clinical studies have provided insight, but with mixed findings and without controlling for comorbidity and without examining multiple types of outcomes, they wrote.
Even with the new study, which identified multiple anesthesia exposures as a significant risk factor for the development of learning disabilities (hazard ratio of 2.16), the clinical relevance remains uncertain. But "at this point, we cannot exclude the possibility that multiple exposures to anesthesia/surgery may adversely affect neurodevelopment," said Dr. Flick of the department of anesthesiology, and his associates (Pediatrics 2011 [doi:10.1542/peds.2011-0351]).
The investigators followed a cohort of children born between 1976 and 1982 to mothers who resided in the same community, attended the same schools, and received virtually all their health care at the Mayo Clinic or at Olmstead Medical Center in Rochester, Minn.
Children who were exposed to anesthesia before age 2 years (350 of the 5,357 children in the cohort) were matched with two unexposed children (700 of the children in the cohort) on the basis on factors known to influence the incidence of learning disabilities, including gender, mother’s education, birth weight, and gestational age.
Two methods were used to quantify health status at age 5 years, and school records were used to track when children developed learning disabilities.
In addition to learning disabilities (overall as well as the subtypes of reading, written language, and mathematics), the study’s outcomes included receipt of an individualized education program (IEP) and results of group-administered tests of cognition and achievement.
By age 19, the cumulative incidence of learning disabilities (with adjustments made for comorbidities and health status) was 21.3% for unexposed controls, 23.6% for those with a single exposure, and 36.6% for those with multiple exposures.
A similar pattern was observed for each subtype of learning disability and in group-administered tests of achievement and cognition. Multiple exposures were associated with lower scores in most of the standardized tests.
Multiple exposures to anesthesia also appeared to affect the rate of children receiving an IEP for difficulties with speech and language, but had no effect on the need for an IEP relating to emotional/behavioral disorders, the investigators reported.
Of the 350 children exposed to general anesthesia early on, 286 were exposed once and 64 were exposed more than once. The most frequent anesthesia was a combination of halothane (87.5%) and nitrous oxide (88.1%).
The findings suggest that any neurodevelopmental effects of multiple exposure may be limited to impairment of speech and language rather than to developmental disorders more generally, the researchers wrote. "However, this can only be a provisional conclusion," they wrote, because the IEP for emotional/behavioral disorders captures only more severely disruptive behaviors.
Overall, they cautioned, the study cannot distinguish between the effects of anesthesia per se, and surgery or the need for surgery. In addition, the measures used to control for health status may not have captured all potential confounders.
Children who were severely mentally retarded were excluded from the study; of these 19 children, all but 1 were known to have profound neurodevelopmental deficits before exposure to anesthesia and surgery.
The study was supported by a grant from the U.S. National Institute of Aging. Dr. Flick and his colleagues reported no relevant financial relationships.
FROM PEDIATRICS
Major Finding: Repeated exposure to anesthesia before age 2 was a significant, independent risk factor for later development of learning disabilities and receipt of individual education plans related to speech and language. The cumulative incidence of learning disabilities (with adjustments made for comorbidities and health status) was 21.3% for unexposed controls, 23.6% for those with a single exposure, and 36.6% for those with multiple exposures.
Data Source: Matched single-community cohort study in which 350 children who underwent procedures with general anesthesia before age 2 were each matched with two unexposed children and followed for numerous measures of learning and behavior.
Disclosures: Dr. Flick and his colleagues reported no relevant financial relationships.
Treating GDM: Evidence of Fetal Harm Lacking
WASHINGTON – Insulins and oral hypoglycemics used during pregnancy can theoretically cause harm to the fetus, but evidence of harm is lacking, said Dr. Barak M. Rosenn.
“Is there any evidence that pharmacologic agents used in the treatment of gestational diabetes can indeed and do indeed cause harm? Not really,” said Dr. Rosenn, director of the division of obstetrics and maternal-fetal medicine at St. Luke's-Roosevelt Hospital in New York.
On the other hand, there have been “no long-term follow-up studies of infants whose mothers were treated with metformin, glyburide, or any of the insulin analogues,” he noted, and past experience with thalidomide has shown that “what may seem safe in the present may prove to be unsafe in the future.”
“Like anything in medicine, we have to be aware of potential risks and weigh the potential risks and benefits,” he said at the meeting. “We can't ignore the fact that diabetes in pregnancy has to be treated.”
Transplacental passage of insulin, insulin analogues, and metformin has indeed been demonstrated, he said.
In 1990, for instance, investigators reported that antibody-bound animal insulin was transferred from mother to fetus, and that the extent of transfer correlated with the maternal concentration of anti-insulin antibody (N. Engl. J. Med. 1990;323:309-15). Another study published in 2007 reported a similar insulin antibody response – and placental passage – in women with gestational diabetes mellitus (GDM) who were receiving human insulin (Diabetes Care 1997;20:1172-5).
In vitro studies on term placentas have demonstrated the transfer of lispro, and aspart has been detected in the cord blood at delivery (Diabet. Med. 2007; 24:1129-35). A transplacental passage study of glargine “again showed small amounts crossing into the fetal circulation” but with higher doses, Dr. Rosenn said (Diabetes Care 2010;33:29-33). hWe don't know what this small amount [of transfer] means for the fetus,” he noted.
In vitro studies have shown metformin to cross the placenta “almost freely,” and clinical studies measuring metformin concentrations in the maternal and cord blood have shown at least comparable maternal-fetal levels of the antihyperglycemic agent. “There's some suggestion that [metformin concentrations] may even be higher in [the fetus],” he said. “But again, the question is, 'What does it do to the fetus apart from the fact that it controls glucose in the mother?'”
With glyburide, the degree of transplacental passage is less clear. Investigators in a recent Obstetric-Fetal Pharmacology Research Unit Network study on glyburide in 40 women with GDM reported that the average ratio of umbilical cord to maternal plasma glyburide concentration was 0.7 at the time of delivery (Clin. Pharmacol. Ther. 2009;85:607-14).
“I do have an argument with the validity of this declaration … because it's pretty obvious that, based on concentrations in the mothers … it [had been] a long time after the last dose [in most mothers],” he said.
The fetal concentration “may be low, but it's not normal,” noted Dr. Rosenn, also professor of obstetrics and gynecology at Columbia University, New York.
Theoretically, it's possible that small quantities of insulin, insulin analogues, or oral hypoglycemics could affect “in utero fetal programming with respect to sensitivity to insulin or insulin resistance” or could cause undetected fetal hypoglycemia in utero,” he said.
Concern has been expressed, moreover, about insulinlike growth factor–I receptor affinity and increased mitogenic potency of some of the insulin analogues. “Concern has been raised with respect to the mom, but if indeed these cross the placenta, we have [to consider] the fetus as well,” Dr. Rosenn said.
He reported that he had no relevant financial disclosures.
WASHINGTON – Insulins and oral hypoglycemics used during pregnancy can theoretically cause harm to the fetus, but evidence of harm is lacking, said Dr. Barak M. Rosenn.
“Is there any evidence that pharmacologic agents used in the treatment of gestational diabetes can indeed and do indeed cause harm? Not really,” said Dr. Rosenn, director of the division of obstetrics and maternal-fetal medicine at St. Luke's-Roosevelt Hospital in New York.
On the other hand, there have been “no long-term follow-up studies of infants whose mothers were treated with metformin, glyburide, or any of the insulin analogues,” he noted, and past experience with thalidomide has shown that “what may seem safe in the present may prove to be unsafe in the future.”
“Like anything in medicine, we have to be aware of potential risks and weigh the potential risks and benefits,” he said at the meeting. “We can't ignore the fact that diabetes in pregnancy has to be treated.”
Transplacental passage of insulin, insulin analogues, and metformin has indeed been demonstrated, he said.
In 1990, for instance, investigators reported that antibody-bound animal insulin was transferred from mother to fetus, and that the extent of transfer correlated with the maternal concentration of anti-insulin antibody (N. Engl. J. Med. 1990;323:309-15). Another study published in 2007 reported a similar insulin antibody response – and placental passage – in women with gestational diabetes mellitus (GDM) who were receiving human insulin (Diabetes Care 1997;20:1172-5).
In vitro studies on term placentas have demonstrated the transfer of lispro, and aspart has been detected in the cord blood at delivery (Diabet. Med. 2007; 24:1129-35). A transplacental passage study of glargine “again showed small amounts crossing into the fetal circulation” but with higher doses, Dr. Rosenn said (Diabetes Care 2010;33:29-33). hWe don't know what this small amount [of transfer] means for the fetus,” he noted.
In vitro studies have shown metformin to cross the placenta “almost freely,” and clinical studies measuring metformin concentrations in the maternal and cord blood have shown at least comparable maternal-fetal levels of the antihyperglycemic agent. “There's some suggestion that [metformin concentrations] may even be higher in [the fetus],” he said. “But again, the question is, 'What does it do to the fetus apart from the fact that it controls glucose in the mother?'”
With glyburide, the degree of transplacental passage is less clear. Investigators in a recent Obstetric-Fetal Pharmacology Research Unit Network study on glyburide in 40 women with GDM reported that the average ratio of umbilical cord to maternal plasma glyburide concentration was 0.7 at the time of delivery (Clin. Pharmacol. Ther. 2009;85:607-14).
“I do have an argument with the validity of this declaration … because it's pretty obvious that, based on concentrations in the mothers … it [had been] a long time after the last dose [in most mothers],” he said.
The fetal concentration “may be low, but it's not normal,” noted Dr. Rosenn, also professor of obstetrics and gynecology at Columbia University, New York.
Theoretically, it's possible that small quantities of insulin, insulin analogues, or oral hypoglycemics could affect “in utero fetal programming with respect to sensitivity to insulin or insulin resistance” or could cause undetected fetal hypoglycemia in utero,” he said.
Concern has been expressed, moreover, about insulinlike growth factor–I receptor affinity and increased mitogenic potency of some of the insulin analogues. “Concern has been raised with respect to the mom, but if indeed these cross the placenta, we have [to consider] the fetus as well,” Dr. Rosenn said.
He reported that he had no relevant financial disclosures.
WASHINGTON – Insulins and oral hypoglycemics used during pregnancy can theoretically cause harm to the fetus, but evidence of harm is lacking, said Dr. Barak M. Rosenn.
“Is there any evidence that pharmacologic agents used in the treatment of gestational diabetes can indeed and do indeed cause harm? Not really,” said Dr. Rosenn, director of the division of obstetrics and maternal-fetal medicine at St. Luke's-Roosevelt Hospital in New York.
On the other hand, there have been “no long-term follow-up studies of infants whose mothers were treated with metformin, glyburide, or any of the insulin analogues,” he noted, and past experience with thalidomide has shown that “what may seem safe in the present may prove to be unsafe in the future.”
“Like anything in medicine, we have to be aware of potential risks and weigh the potential risks and benefits,” he said at the meeting. “We can't ignore the fact that diabetes in pregnancy has to be treated.”
Transplacental passage of insulin, insulin analogues, and metformin has indeed been demonstrated, he said.
In 1990, for instance, investigators reported that antibody-bound animal insulin was transferred from mother to fetus, and that the extent of transfer correlated with the maternal concentration of anti-insulin antibody (N. Engl. J. Med. 1990;323:309-15). Another study published in 2007 reported a similar insulin antibody response – and placental passage – in women with gestational diabetes mellitus (GDM) who were receiving human insulin (Diabetes Care 1997;20:1172-5).
In vitro studies on term placentas have demonstrated the transfer of lispro, and aspart has been detected in the cord blood at delivery (Diabet. Med. 2007; 24:1129-35). A transplacental passage study of glargine “again showed small amounts crossing into the fetal circulation” but with higher doses, Dr. Rosenn said (Diabetes Care 2010;33:29-33). hWe don't know what this small amount [of transfer] means for the fetus,” he noted.
In vitro studies have shown metformin to cross the placenta “almost freely,” and clinical studies measuring metformin concentrations in the maternal and cord blood have shown at least comparable maternal-fetal levels of the antihyperglycemic agent. “There's some suggestion that [metformin concentrations] may even be higher in [the fetus],” he said. “But again, the question is, 'What does it do to the fetus apart from the fact that it controls glucose in the mother?'”
With glyburide, the degree of transplacental passage is less clear. Investigators in a recent Obstetric-Fetal Pharmacology Research Unit Network study on glyburide in 40 women with GDM reported that the average ratio of umbilical cord to maternal plasma glyburide concentration was 0.7 at the time of delivery (Clin. Pharmacol. Ther. 2009;85:607-14).
“I do have an argument with the validity of this declaration … because it's pretty obvious that, based on concentrations in the mothers … it [had been] a long time after the last dose [in most mothers],” he said.
The fetal concentration “may be low, but it's not normal,” noted Dr. Rosenn, also professor of obstetrics and gynecology at Columbia University, New York.
Theoretically, it's possible that small quantities of insulin, insulin analogues, or oral hypoglycemics could affect “in utero fetal programming with respect to sensitivity to insulin or insulin resistance” or could cause undetected fetal hypoglycemia in utero,” he said.
Concern has been expressed, moreover, about insulinlike growth factor–I receptor affinity and increased mitogenic potency of some of the insulin analogues. “Concern has been raised with respect to the mom, but if indeed these cross the placenta, we have [to consider] the fetus as well,” Dr. Rosenn said.
He reported that he had no relevant financial disclosures.
Expert Analysis from the Annual Meeting of the Diabetes in Pregnancy Study Group of North America
Gestational Diabetes Therapies and Fetal Risk
WASHINGTON – Insulins and oral hypoglycemics used during pregnancy can theoretically cause harm to the fetus, but evidence of harm is lacking, said Dr. Barak M. Rosenn.
“Is there any evidence that pharmacologic agents used in the treatment of gestational diabetes can indeed and do indeed cause harm? Not really,” said Dr. Rosenn, director of the division of obstetrics and maternal-fetal medicine at St. Luke's-Roosevelt Hospital in New York.
On the other hand, there have been “no long-term follow-up studies of infants whose mothers were treated with metformin, glyburide, or any of the insulin analogs,” he noted, and past experience with thalidomide has shown that “what may seem safe in the present may prove to be unsafe in the future.”
“Like anything in medicine, we have to be aware of potential risks and weigh the potential risks and benefits,” he said at the meeting. “We can't ignore the fact that diabetes in pregnancy has to be treated.”
Transplacental passage of insulin, insulin analogs, and metformin has indeed been demonstrated, he said.
In 1990, for instance, investigators reported that antibody-bound animal insulin was transferred from mother to fetus, and that the extent of transfer correlated with the maternal concentration of anti-insulin antibody (N. Engl. J. Med. 1990;323:309-15).
Another study published in 2007 reported a similar insulin antibody response – and placental passage – in women with gestational diabetes mellitus (GDM) who were receiving human insulin (Diabetes Care 1997;20:1172-5).
In vitro studies on term placentas have demonstrated the transfer of lispro, and aspart has been detected in the cord blood at delivery (Diabet. Med. 2007;24:1129-35). A transplacental passage study of glargine “again showed small amounts crossing into the fetal circulation,” but with higher doses, Dr. Rosenn said (Diabetes Care 2010;33:29-33). hWe don't know what this small amount [of transfer] means for the fetus,” he noted.
In vitro studies have shown metformin to cross the placenta “almost freely,” and clinical studies measuring metformin concentrations in the maternal and cord blood have shown at least comparable maternal-fetal levels of the antihyperglycemic agent. “There's some suggestion that [metformin concentrations] may even be higher in [the fetus],” he said. “But again, the question is, 'What does it do to the fetus apart from the fact that it controls glucose in the mother?'”
With glyburide, the degree of transplacental passage is less clear. Investigators of a recent Obstetric-Fetal Pharmacology Research Unit Network study on glyburide in 40 women with GDM reported that the average ratio of umbilical cord/maternal plasma glyburide concentration was 0.7 at the time of delivery (Clin. Pharmacol. Ther. 2009;85:607-14).
“I do have an argument with the validity of this declaration … because it's pretty obvious that, based on concentrations in the mothers … it [had been] a long time after the last dose [in most mothers],” he said.
The fetal concentration “may be low, but it's not normal,” noted Dr. Rosenn, also professor of obstetrics and gynecology at Columbia University, New York.
Theoretically, it's possible that small quantities of insulin, insulin analogs, or oral hypoglycemics could affect “in-utero fetal programming with respect to sensitivity to insulin or insulin resistance” or could cause undetected fetal hypoglycemia in utero,” he said.
Concern has been expressed, moreover, about IGF-I receptor affinity and increased mitogenic potency of some of the insulin analogues.
“Concern has been raised with respect to the mom, but if indeed these cross the placenta, we have [to consider] the fetus as well,” Dr. Rosenn said.
Dr. Rosenn reported that he had no relevant financial disclosures.
WASHINGTON – Insulins and oral hypoglycemics used during pregnancy can theoretically cause harm to the fetus, but evidence of harm is lacking, said Dr. Barak M. Rosenn.
“Is there any evidence that pharmacologic agents used in the treatment of gestational diabetes can indeed and do indeed cause harm? Not really,” said Dr. Rosenn, director of the division of obstetrics and maternal-fetal medicine at St. Luke's-Roosevelt Hospital in New York.
On the other hand, there have been “no long-term follow-up studies of infants whose mothers were treated with metformin, glyburide, or any of the insulin analogs,” he noted, and past experience with thalidomide has shown that “what may seem safe in the present may prove to be unsafe in the future.”
“Like anything in medicine, we have to be aware of potential risks and weigh the potential risks and benefits,” he said at the meeting. “We can't ignore the fact that diabetes in pregnancy has to be treated.”
Transplacental passage of insulin, insulin analogs, and metformin has indeed been demonstrated, he said.
In 1990, for instance, investigators reported that antibody-bound animal insulin was transferred from mother to fetus, and that the extent of transfer correlated with the maternal concentration of anti-insulin antibody (N. Engl. J. Med. 1990;323:309-15).
Another study published in 2007 reported a similar insulin antibody response – and placental passage – in women with gestational diabetes mellitus (GDM) who were receiving human insulin (Diabetes Care 1997;20:1172-5).
In vitro studies on term placentas have demonstrated the transfer of lispro, and aspart has been detected in the cord blood at delivery (Diabet. Med. 2007;24:1129-35). A transplacental passage study of glargine “again showed small amounts crossing into the fetal circulation,” but with higher doses, Dr. Rosenn said (Diabetes Care 2010;33:29-33). hWe don't know what this small amount [of transfer] means for the fetus,” he noted.
In vitro studies have shown metformin to cross the placenta “almost freely,” and clinical studies measuring metformin concentrations in the maternal and cord blood have shown at least comparable maternal-fetal levels of the antihyperglycemic agent. “There's some suggestion that [metformin concentrations] may even be higher in [the fetus],” he said. “But again, the question is, 'What does it do to the fetus apart from the fact that it controls glucose in the mother?'”
With glyburide, the degree of transplacental passage is less clear. Investigators of a recent Obstetric-Fetal Pharmacology Research Unit Network study on glyburide in 40 women with GDM reported that the average ratio of umbilical cord/maternal plasma glyburide concentration was 0.7 at the time of delivery (Clin. Pharmacol. Ther. 2009;85:607-14).
“I do have an argument with the validity of this declaration … because it's pretty obvious that, based on concentrations in the mothers … it [had been] a long time after the last dose [in most mothers],” he said.
The fetal concentration “may be low, but it's not normal,” noted Dr. Rosenn, also professor of obstetrics and gynecology at Columbia University, New York.
Theoretically, it's possible that small quantities of insulin, insulin analogs, or oral hypoglycemics could affect “in-utero fetal programming with respect to sensitivity to insulin or insulin resistance” or could cause undetected fetal hypoglycemia in utero,” he said.
Concern has been expressed, moreover, about IGF-I receptor affinity and increased mitogenic potency of some of the insulin analogues.
“Concern has been raised with respect to the mom, but if indeed these cross the placenta, we have [to consider] the fetus as well,” Dr. Rosenn said.
Dr. Rosenn reported that he had no relevant financial disclosures.
WASHINGTON – Insulins and oral hypoglycemics used during pregnancy can theoretically cause harm to the fetus, but evidence of harm is lacking, said Dr. Barak M. Rosenn.
“Is there any evidence that pharmacologic agents used in the treatment of gestational diabetes can indeed and do indeed cause harm? Not really,” said Dr. Rosenn, director of the division of obstetrics and maternal-fetal medicine at St. Luke's-Roosevelt Hospital in New York.
On the other hand, there have been “no long-term follow-up studies of infants whose mothers were treated with metformin, glyburide, or any of the insulin analogs,” he noted, and past experience with thalidomide has shown that “what may seem safe in the present may prove to be unsafe in the future.”
“Like anything in medicine, we have to be aware of potential risks and weigh the potential risks and benefits,” he said at the meeting. “We can't ignore the fact that diabetes in pregnancy has to be treated.”
Transplacental passage of insulin, insulin analogs, and metformin has indeed been demonstrated, he said.
In 1990, for instance, investigators reported that antibody-bound animal insulin was transferred from mother to fetus, and that the extent of transfer correlated with the maternal concentration of anti-insulin antibody (N. Engl. J. Med. 1990;323:309-15).
Another study published in 2007 reported a similar insulin antibody response – and placental passage – in women with gestational diabetes mellitus (GDM) who were receiving human insulin (Diabetes Care 1997;20:1172-5).
In vitro studies on term placentas have demonstrated the transfer of lispro, and aspart has been detected in the cord blood at delivery (Diabet. Med. 2007;24:1129-35). A transplacental passage study of glargine “again showed small amounts crossing into the fetal circulation,” but with higher doses, Dr. Rosenn said (Diabetes Care 2010;33:29-33). hWe don't know what this small amount [of transfer] means for the fetus,” he noted.
In vitro studies have shown metformin to cross the placenta “almost freely,” and clinical studies measuring metformin concentrations in the maternal and cord blood have shown at least comparable maternal-fetal levels of the antihyperglycemic agent. “There's some suggestion that [metformin concentrations] may even be higher in [the fetus],” he said. “But again, the question is, 'What does it do to the fetus apart from the fact that it controls glucose in the mother?'”
With glyburide, the degree of transplacental passage is less clear. Investigators of a recent Obstetric-Fetal Pharmacology Research Unit Network study on glyburide in 40 women with GDM reported that the average ratio of umbilical cord/maternal plasma glyburide concentration was 0.7 at the time of delivery (Clin. Pharmacol. Ther. 2009;85:607-14).
“I do have an argument with the validity of this declaration … because it's pretty obvious that, based on concentrations in the mothers … it [had been] a long time after the last dose [in most mothers],” he said.
The fetal concentration “may be low, but it's not normal,” noted Dr. Rosenn, also professor of obstetrics and gynecology at Columbia University, New York.
Theoretically, it's possible that small quantities of insulin, insulin analogs, or oral hypoglycemics could affect “in-utero fetal programming with respect to sensitivity to insulin or insulin resistance” or could cause undetected fetal hypoglycemia in utero,” he said.
Concern has been expressed, moreover, about IGF-I receptor affinity and increased mitogenic potency of some of the insulin analogues.
“Concern has been raised with respect to the mom, but if indeed these cross the placenta, we have [to consider] the fetus as well,” Dr. Rosenn said.
Dr. Rosenn reported that he had no relevant financial disclosures.
Expert Analysis from the Annual Meeting of the Diabetes In Pregnancy Study Group of North America
Self-Therapy Among Options for Recurring UTIs
WASHINGTON – Recurring, uncomplicated urinary tract infections in female patients may be treated in the future through bacterial interference and other novel approaches, but for now, treatment involves an individualized approach with possible postcoital prophylaxis, chronic low-dose prophylaxis, or self-therapy, said urologist Robert M. Moldwin.
Addressing the case of a 35-year-old, otherwise-healthy woman who has had three culture-documented, symptomatic bacterial cystitis episodes over the last 3 months, Dr. Moldwin said that chronic low-dose prophylaxis may be considered when recurring infections are not related to intercourse.
Chronic prophylaxis should be reserved for frequently recurring infections, he emphasized, and the “goal is to grade down on the dose arbitrarily over a 6- to 12-month span, perhaps going to every other night or every third night, and then hopefully discontinuing this regime altogether,” he said during a panel discussion on UTIs at the meeting.
The two agents that are best supported in the literature for chronic low-dose prophylaxis are nitrofurantoin and methenamine hippurate. Trimethoprim-sulfamethoxazole and early generation cephalosporins “have also been espoused,” said Dr. Moldwin of Hofstra University, Hempstead, N.Y.
“Unfortunately, though,” he said, “recurrent infections are bound to show up at some point when prophylaxis is discontinued.”
Self-therapy can “really pay off” in cases in which infections are recurring less frequently, and it can also be “a great protocol to institute when one takes a patient off of antibiotic prophylaxis,” said Dr. Moldwin, also of the Arthur Smith Institute for Urology in New Hyde Park, N.Y.
In this scenario, the patient is armed with a sterile collection cup, a urinalysis and urine culture prescription, and a prescription for an antibiotic. “At the first sign of infection, the patient is instructed to obtain a midstream urine sample … and start [herself] on an appropriate course of an antibiotic,” he said. “Within 24-48 hours, the patient can bring the specimen to the local laboratory” and can have the results sent to her physician for analysis if symptoms don't resolve, he added.
Cranberry juice has been touted for UTI prevention because it contains various chemicals that may prevent bacterial adherence to the bladder wall. Evidence that was published several years ago concluded that “after many disclaimers, [there] is some evidence to recommend cranberry juice for the prevention of uncomplicated UTIs in women with symptomatic infections,” a randomized clinical trial published this year showed no difference in UTI recurrence between patients who used cranberry juice and those who used placebo (Clin. Infect. Dis. 2011;52:23-30), Dr. Moldwin said.
The trial of 319 college students is “the most recent and probably the best” that has been published to date, he said.
Oral
A Google search shows 45,000-61,000 hits, he said, but a Pub Med search on
Other forms of bacterial interference may prove efficacious, however. The use of vaginal or oral probiotics, for instance, or the introduction of nonpathogenic Escherichia coli “to the vaginal vault, the gut, or even the bladder itself” are among the “novel and viable options that we hope to see more work on in the future,” he said.
Dr. Moldwin disclosed that he is a consultant, adviser, or investigator for Ortho-McNeil Pharmaceuticals, Pfizer, and Pinnacle Pharmaceuticals.
There is some evidence to recommend cranberry juice for prevention of recurring uncomplicated UTIs.
Source ©Tarek El Sombati/iStockphoto.com
WASHINGTON – Recurring, uncomplicated urinary tract infections in female patients may be treated in the future through bacterial interference and other novel approaches, but for now, treatment involves an individualized approach with possible postcoital prophylaxis, chronic low-dose prophylaxis, or self-therapy, said urologist Robert M. Moldwin.
Addressing the case of a 35-year-old, otherwise-healthy woman who has had three culture-documented, symptomatic bacterial cystitis episodes over the last 3 months, Dr. Moldwin said that chronic low-dose prophylaxis may be considered when recurring infections are not related to intercourse.
Chronic prophylaxis should be reserved for frequently recurring infections, he emphasized, and the “goal is to grade down on the dose arbitrarily over a 6- to 12-month span, perhaps going to every other night or every third night, and then hopefully discontinuing this regime altogether,” he said during a panel discussion on UTIs at the meeting.
The two agents that are best supported in the literature for chronic low-dose prophylaxis are nitrofurantoin and methenamine hippurate. Trimethoprim-sulfamethoxazole and early generation cephalosporins “have also been espoused,” said Dr. Moldwin of Hofstra University, Hempstead, N.Y.
“Unfortunately, though,” he said, “recurrent infections are bound to show up at some point when prophylaxis is discontinued.”
Self-therapy can “really pay off” in cases in which infections are recurring less frequently, and it can also be “a great protocol to institute when one takes a patient off of antibiotic prophylaxis,” said Dr. Moldwin, also of the Arthur Smith Institute for Urology in New Hyde Park, N.Y.
In this scenario, the patient is armed with a sterile collection cup, a urinalysis and urine culture prescription, and a prescription for an antibiotic. “At the first sign of infection, the patient is instructed to obtain a midstream urine sample … and start [herself] on an appropriate course of an antibiotic,” he said. “Within 24-48 hours, the patient can bring the specimen to the local laboratory” and can have the results sent to her physician for analysis if symptoms don't resolve, he added.
Cranberry juice has been touted for UTI prevention because it contains various chemicals that may prevent bacterial adherence to the bladder wall. Evidence that was published several years ago concluded that “after many disclaimers, [there] is some evidence to recommend cranberry juice for the prevention of uncomplicated UTIs in women with symptomatic infections,” a randomized clinical trial published this year showed no difference in UTI recurrence between patients who used cranberry juice and those who used placebo (Clin. Infect. Dis. 2011;52:23-30), Dr. Moldwin said.
The trial of 319 college students is “the most recent and probably the best” that has been published to date, he said.
Oral
A Google search shows 45,000-61,000 hits, he said, but a Pub Med search on
Other forms of bacterial interference may prove efficacious, however. The use of vaginal or oral probiotics, for instance, or the introduction of nonpathogenic Escherichia coli “to the vaginal vault, the gut, or even the bladder itself” are among the “novel and viable options that we hope to see more work on in the future,” he said.
Dr. Moldwin disclosed that he is a consultant, adviser, or investigator for Ortho-McNeil Pharmaceuticals, Pfizer, and Pinnacle Pharmaceuticals.
There is some evidence to recommend cranberry juice for prevention of recurring uncomplicated UTIs.
Source ©Tarek El Sombati/iStockphoto.com
WASHINGTON – Recurring, uncomplicated urinary tract infections in female patients may be treated in the future through bacterial interference and other novel approaches, but for now, treatment involves an individualized approach with possible postcoital prophylaxis, chronic low-dose prophylaxis, or self-therapy, said urologist Robert M. Moldwin.
Addressing the case of a 35-year-old, otherwise-healthy woman who has had three culture-documented, symptomatic bacterial cystitis episodes over the last 3 months, Dr. Moldwin said that chronic low-dose prophylaxis may be considered when recurring infections are not related to intercourse.
Chronic prophylaxis should be reserved for frequently recurring infections, he emphasized, and the “goal is to grade down on the dose arbitrarily over a 6- to 12-month span, perhaps going to every other night or every third night, and then hopefully discontinuing this regime altogether,” he said during a panel discussion on UTIs at the meeting.
The two agents that are best supported in the literature for chronic low-dose prophylaxis are nitrofurantoin and methenamine hippurate. Trimethoprim-sulfamethoxazole and early generation cephalosporins “have also been espoused,” said Dr. Moldwin of Hofstra University, Hempstead, N.Y.
“Unfortunately, though,” he said, “recurrent infections are bound to show up at some point when prophylaxis is discontinued.”
Self-therapy can “really pay off” in cases in which infections are recurring less frequently, and it can also be “a great protocol to institute when one takes a patient off of antibiotic prophylaxis,” said Dr. Moldwin, also of the Arthur Smith Institute for Urology in New Hyde Park, N.Y.
In this scenario, the patient is armed with a sterile collection cup, a urinalysis and urine culture prescription, and a prescription for an antibiotic. “At the first sign of infection, the patient is instructed to obtain a midstream urine sample … and start [herself] on an appropriate course of an antibiotic,” he said. “Within 24-48 hours, the patient can bring the specimen to the local laboratory” and can have the results sent to her physician for analysis if symptoms don't resolve, he added.
Cranberry juice has been touted for UTI prevention because it contains various chemicals that may prevent bacterial adherence to the bladder wall. Evidence that was published several years ago concluded that “after many disclaimers, [there] is some evidence to recommend cranberry juice for the prevention of uncomplicated UTIs in women with symptomatic infections,” a randomized clinical trial published this year showed no difference in UTI recurrence between patients who used cranberry juice and those who used placebo (Clin. Infect. Dis. 2011;52:23-30), Dr. Moldwin said.
The trial of 319 college students is “the most recent and probably the best” that has been published to date, he said.
Oral
A Google search shows 45,000-61,000 hits, he said, but a Pub Med search on
Other forms of bacterial interference may prove efficacious, however. The use of vaginal or oral probiotics, for instance, or the introduction of nonpathogenic Escherichia coli “to the vaginal vault, the gut, or even the bladder itself” are among the “novel and viable options that we hope to see more work on in the future,” he said.
Dr. Moldwin disclosed that he is a consultant, adviser, or investigator for Ortho-McNeil Pharmaceuticals, Pfizer, and Pinnacle Pharmaceuticals.
There is some evidence to recommend cranberry juice for prevention of recurring uncomplicated UTIs.
Source ©Tarek El Sombati/iStockphoto.com
Expert Analysis from the Annual Meeting of the American Urological Association
Kidney Stones Linked to CVD, Metabolic Syndrome
WASHINGTON – Research has documented a strong association between the formation of kidney stones and the presence or development of cardiovascular disease, metabolic syndrome, and a number of components of the metabolic syndrome, said Dr. Dean G. Assimos.
"There is increasing evidence" of this link, he noted at the annual meeting of the American Urological Association. "We need to be cognizant of these associations."
Most recently, an analysis of data from the Coronary Artery Risk Development in Young Adults (CARDIA) study showed that individuals who developed kidney stones had a 1.6-fold increased risk of developing subclinical carotid artery atherosclerosis, even after adjustments for major cardiovascular risk factors were made, said Dr. Assimos, professor of urology at Wake Forest University, Winston-Salem, N.C.
The longitudinal cohort study followed 5,115 white and black men and women who were 18-30 years old at the time of recruitment in 1985-1986. Carotid artery intima-media thickness was measured with serial ultrasound periodically throughout the observation period. By 20 years, almost 4% had reported having kidney stones, and kidney stones were associated with a 60% increased risk of carotid atherosclerosis (J. Urol. 2011;185:920-5). Kidney stones were associated with myocardial infarction (MI) in another recent study aimed specifically at assessing "the risk of a kidney stone former developing an MI," Dr. Assimos said. Investigators of this case-controlled study matched almost 4,600 stone formers on age and sex with almost 11,000 control subjects among residents of Olmstead County, Minn.
During a mean follow-up of 9 years, "despite controlling for other medical comorbidities," investigators found that "stone formers had a 31% increased risk of sustaining an MI," he said.
Chronic kidney disease, which itself is a risk factor for MI, was one of the comorbidities adjusted for (J. Am. Soc. Nephrol. 2010;21:1641-4).
Numerous studies published since 2005 have demonstrated positive associations between kidney stone formation and specific components of the metabolic syndrome, as well as with the full constellation of disorders, Dr. Assimos said.
An analysis of National Health and Nutrition Examination Survey III data published in 2008, for instance, showed that individuals with four traits of the metabolic syndrome had two times the risk of having a history of kidney stones (Am. J. Kidney Dis. 2008;51:741-7). The prevalence of self-reported history of kidney stones, moreover, increased as the number of traits or component disorders of the metabolic syndrome increased, from 3% with no disorders to 7.5% with three disorders, and to almost 10% with five disorders. (An individual must have at least three of the five component disorders to qualify as having the metabolic syndrome.)
Similarly, in an Italian study of hospitalized adults, more than 10% of 725 patients with metabolic syndrome had evidence of nephrolithiasis on renal ultrasound (Nephrol. Dial. Transplant 2009;24:900-6). "This is 10 times higher than [rates reported from] renal ultrasound screening studies done in the general population," Dr. Assimos said.
Data from three large cohorts – the Nurses’ Health Study (NHS) I of older women, the NHS II of younger women, and the Health Professionals Follow-Up Study (HPFS) of men aged 40-75 years – have been crucial in elucidating the associations between kidney stones and specific components of the metabolic syndrome.
In one prospective study of the cohorts that looked at the incidence of symptomatic kidney stones, for instance, investigators documented that the relative risk of an obese individual (body mass index, 30 kg/m2 or greater) for kidney stone formation, compared with individuals with a BMI of 21-23, was 1.9 in the NHS I cohort, 2.09 in the NHS II cohort, and 1.33 in the HPFS cohort (JAMA 2005;293:455-62).
"There was also a positive correlation in all these cohorts with waist circumference," Dr. Assimos said.
Other analyses of these cohorts have documented positive associations between type 2 diabetes or hypertension, and incident kidney stone formation, as well as associations between a history of kidney stone formation and the diagnosis of diabetes or development of hypertension.
The causative factors underlying the associations between stone formation and cardiovascular disease and the metabolic syndrome include low urinary pH levels. At lower urinary pH levels, "more [of the body’s] uric acid is in its undissociated form and is insoluble in urine," for instance, which increases the risk of uric acid stone formation, Dr. Assimos said.
Studies have demonstrated a negative correlation between BMI and urinary pH, he noted. The reasons are not fully known, but "it is hypothesized that individuals [with higher BMI] do not produce ammonium effectively in the proximal tubule," he said.
Individuals with obesity and low urinary pH also excrete greater amounts of calcium and oxalate, and this increases the risk of calcium oxalate stone formation, he said.
Dr. Assimos’s own research team has identified a possible new pathway for the endogenous synthesis of oxalate. It involves the metabolism of glyoxal, which is stimulated by oxidative stress. The glyoxal metabolism "may explain the increased oxalate excretion in those with obesity as well as diabetes," he said.
The associations between kidney stone formation and cardiovascular risk have hit home for Dr. Assimos, he said at the end of his presentation. At age 39, he developed his first kidney stone. By 3 years later, he developed hypertension. "And 3 years ago. I started having symptoms of gastroesophageal reflux when exercising ... I had a stress test ... and here is my coronary arteriogram," he told the audience. The end result, he said, was successful coronary artery bypass grafting.
Dr. Assimos reported that he is an investigator for the National Institutes of Health and a partner at Piedmont Stone, a facility in Winston-Salem that provides lithotripsy procedures.
WASHINGTON – Research has documented a strong association between the formation of kidney stones and the presence or development of cardiovascular disease, metabolic syndrome, and a number of components of the metabolic syndrome, said Dr. Dean G. Assimos.
"There is increasing evidence" of this link, he noted at the annual meeting of the American Urological Association. "We need to be cognizant of these associations."
Most recently, an analysis of data from the Coronary Artery Risk Development in Young Adults (CARDIA) study showed that individuals who developed kidney stones had a 1.6-fold increased risk of developing subclinical carotid artery atherosclerosis, even after adjustments for major cardiovascular risk factors were made, said Dr. Assimos, professor of urology at Wake Forest University, Winston-Salem, N.C.
The longitudinal cohort study followed 5,115 white and black men and women who were 18-30 years old at the time of recruitment in 1985-1986. Carotid artery intima-media thickness was measured with serial ultrasound periodically throughout the observation period. By 20 years, almost 4% had reported having kidney stones, and kidney stones were associated with a 60% increased risk of carotid atherosclerosis (J. Urol. 2011;185:920-5). Kidney stones were associated with myocardial infarction (MI) in another recent study aimed specifically at assessing "the risk of a kidney stone former developing an MI," Dr. Assimos said. Investigators of this case-controlled study matched almost 4,600 stone formers on age and sex with almost 11,000 control subjects among residents of Olmstead County, Minn.
During a mean follow-up of 9 years, "despite controlling for other medical comorbidities," investigators found that "stone formers had a 31% increased risk of sustaining an MI," he said.
Chronic kidney disease, which itself is a risk factor for MI, was one of the comorbidities adjusted for (J. Am. Soc. Nephrol. 2010;21:1641-4).
Numerous studies published since 2005 have demonstrated positive associations between kidney stone formation and specific components of the metabolic syndrome, as well as with the full constellation of disorders, Dr. Assimos said.
An analysis of National Health and Nutrition Examination Survey III data published in 2008, for instance, showed that individuals with four traits of the metabolic syndrome had two times the risk of having a history of kidney stones (Am. J. Kidney Dis. 2008;51:741-7). The prevalence of self-reported history of kidney stones, moreover, increased as the number of traits or component disorders of the metabolic syndrome increased, from 3% with no disorders to 7.5% with three disorders, and to almost 10% with five disorders. (An individual must have at least three of the five component disorders to qualify as having the metabolic syndrome.)
Similarly, in an Italian study of hospitalized adults, more than 10% of 725 patients with metabolic syndrome had evidence of nephrolithiasis on renal ultrasound (Nephrol. Dial. Transplant 2009;24:900-6). "This is 10 times higher than [rates reported from] renal ultrasound screening studies done in the general population," Dr. Assimos said.
Data from three large cohorts – the Nurses’ Health Study (NHS) I of older women, the NHS II of younger women, and the Health Professionals Follow-Up Study (HPFS) of men aged 40-75 years – have been crucial in elucidating the associations between kidney stones and specific components of the metabolic syndrome.
In one prospective study of the cohorts that looked at the incidence of symptomatic kidney stones, for instance, investigators documented that the relative risk of an obese individual (body mass index, 30 kg/m2 or greater) for kidney stone formation, compared with individuals with a BMI of 21-23, was 1.9 in the NHS I cohort, 2.09 in the NHS II cohort, and 1.33 in the HPFS cohort (JAMA 2005;293:455-62).
"There was also a positive correlation in all these cohorts with waist circumference," Dr. Assimos said.
Other analyses of these cohorts have documented positive associations between type 2 diabetes or hypertension, and incident kidney stone formation, as well as associations between a history of kidney stone formation and the diagnosis of diabetes or development of hypertension.
The causative factors underlying the associations between stone formation and cardiovascular disease and the metabolic syndrome include low urinary pH levels. At lower urinary pH levels, "more [of the body’s] uric acid is in its undissociated form and is insoluble in urine," for instance, which increases the risk of uric acid stone formation, Dr. Assimos said.
Studies have demonstrated a negative correlation between BMI and urinary pH, he noted. The reasons are not fully known, but "it is hypothesized that individuals [with higher BMI] do not produce ammonium effectively in the proximal tubule," he said.
Individuals with obesity and low urinary pH also excrete greater amounts of calcium and oxalate, and this increases the risk of calcium oxalate stone formation, he said.
Dr. Assimos’s own research team has identified a possible new pathway for the endogenous synthesis of oxalate. It involves the metabolism of glyoxal, which is stimulated by oxidative stress. The glyoxal metabolism "may explain the increased oxalate excretion in those with obesity as well as diabetes," he said.
The associations between kidney stone formation and cardiovascular risk have hit home for Dr. Assimos, he said at the end of his presentation. At age 39, he developed his first kidney stone. By 3 years later, he developed hypertension. "And 3 years ago. I started having symptoms of gastroesophageal reflux when exercising ... I had a stress test ... and here is my coronary arteriogram," he told the audience. The end result, he said, was successful coronary artery bypass grafting.
Dr. Assimos reported that he is an investigator for the National Institutes of Health and a partner at Piedmont Stone, a facility in Winston-Salem that provides lithotripsy procedures.
WASHINGTON – Research has documented a strong association between the formation of kidney stones and the presence or development of cardiovascular disease, metabolic syndrome, and a number of components of the metabolic syndrome, said Dr. Dean G. Assimos.
"There is increasing evidence" of this link, he noted at the annual meeting of the American Urological Association. "We need to be cognizant of these associations."
Most recently, an analysis of data from the Coronary Artery Risk Development in Young Adults (CARDIA) study showed that individuals who developed kidney stones had a 1.6-fold increased risk of developing subclinical carotid artery atherosclerosis, even after adjustments for major cardiovascular risk factors were made, said Dr. Assimos, professor of urology at Wake Forest University, Winston-Salem, N.C.
The longitudinal cohort study followed 5,115 white and black men and women who were 18-30 years old at the time of recruitment in 1985-1986. Carotid artery intima-media thickness was measured with serial ultrasound periodically throughout the observation period. By 20 years, almost 4% had reported having kidney stones, and kidney stones were associated with a 60% increased risk of carotid atherosclerosis (J. Urol. 2011;185:920-5). Kidney stones were associated with myocardial infarction (MI) in another recent study aimed specifically at assessing "the risk of a kidney stone former developing an MI," Dr. Assimos said. Investigators of this case-controlled study matched almost 4,600 stone formers on age and sex with almost 11,000 control subjects among residents of Olmstead County, Minn.
During a mean follow-up of 9 years, "despite controlling for other medical comorbidities," investigators found that "stone formers had a 31% increased risk of sustaining an MI," he said.
Chronic kidney disease, which itself is a risk factor for MI, was one of the comorbidities adjusted for (J. Am. Soc. Nephrol. 2010;21:1641-4).
Numerous studies published since 2005 have demonstrated positive associations between kidney stone formation and specific components of the metabolic syndrome, as well as with the full constellation of disorders, Dr. Assimos said.
An analysis of National Health and Nutrition Examination Survey III data published in 2008, for instance, showed that individuals with four traits of the metabolic syndrome had two times the risk of having a history of kidney stones (Am. J. Kidney Dis. 2008;51:741-7). The prevalence of self-reported history of kidney stones, moreover, increased as the number of traits or component disorders of the metabolic syndrome increased, from 3% with no disorders to 7.5% with three disorders, and to almost 10% with five disorders. (An individual must have at least three of the five component disorders to qualify as having the metabolic syndrome.)
Similarly, in an Italian study of hospitalized adults, more than 10% of 725 patients with metabolic syndrome had evidence of nephrolithiasis on renal ultrasound (Nephrol. Dial. Transplant 2009;24:900-6). "This is 10 times higher than [rates reported from] renal ultrasound screening studies done in the general population," Dr. Assimos said.
Data from three large cohorts – the Nurses’ Health Study (NHS) I of older women, the NHS II of younger women, and the Health Professionals Follow-Up Study (HPFS) of men aged 40-75 years – have been crucial in elucidating the associations between kidney stones and specific components of the metabolic syndrome.
In one prospective study of the cohorts that looked at the incidence of symptomatic kidney stones, for instance, investigators documented that the relative risk of an obese individual (body mass index, 30 kg/m2 or greater) for kidney stone formation, compared with individuals with a BMI of 21-23, was 1.9 in the NHS I cohort, 2.09 in the NHS II cohort, and 1.33 in the HPFS cohort (JAMA 2005;293:455-62).
"There was also a positive correlation in all these cohorts with waist circumference," Dr. Assimos said.
Other analyses of these cohorts have documented positive associations between type 2 diabetes or hypertension, and incident kidney stone formation, as well as associations between a history of kidney stone formation and the diagnosis of diabetes or development of hypertension.
The causative factors underlying the associations between stone formation and cardiovascular disease and the metabolic syndrome include low urinary pH levels. At lower urinary pH levels, "more [of the body’s] uric acid is in its undissociated form and is insoluble in urine," for instance, which increases the risk of uric acid stone formation, Dr. Assimos said.
Studies have demonstrated a negative correlation between BMI and urinary pH, he noted. The reasons are not fully known, but "it is hypothesized that individuals [with higher BMI] do not produce ammonium effectively in the proximal tubule," he said.
Individuals with obesity and low urinary pH also excrete greater amounts of calcium and oxalate, and this increases the risk of calcium oxalate stone formation, he said.
Dr. Assimos’s own research team has identified a possible new pathway for the endogenous synthesis of oxalate. It involves the metabolism of glyoxal, which is stimulated by oxidative stress. The glyoxal metabolism "may explain the increased oxalate excretion in those with obesity as well as diabetes," he said.
The associations between kidney stone formation and cardiovascular risk have hit home for Dr. Assimos, he said at the end of his presentation. At age 39, he developed his first kidney stone. By 3 years later, he developed hypertension. "And 3 years ago. I started having symptoms of gastroesophageal reflux when exercising ... I had a stress test ... and here is my coronary arteriogram," he told the audience. The end result, he said, was successful coronary artery bypass grafting.
Dr. Assimos reported that he is an investigator for the National Institutes of Health and a partner at Piedmont Stone, a facility in Winston-Salem that provides lithotripsy procedures.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN UROLOGICAL ASSOCIATION