User login
Suspect myopathy? Take this approach to the work-up
› Categorize patients with muscle complaints into suspected myositic, intrinsic, or toxic myopathy to help guide subsequent work-up. C
› Look for diffusely painful, swollen, or boggy-feeling muscles—as well as weakness and pain with exertion—in patients you suspect may have viral myopathy. C
› Consider electromyography and muscle biopsy for patients you suspect may have dermatomyositis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Marie C, a 75-year-old Asian woman, reports weakness in her legs and arms with unsteadiness when walking. She has a vague but persistent ache in her large muscles. Her symptoms have developed slowly over the past 3 months. She denies recent signs or symptoms of infection or other illness. Her medical history includes hypertension, hyperlipidemia, osteopenia, and obesity. Ms. C takes lisinopril 10 mg/d and atorvastatin, which was recently increased from 10 to 20 mg/d.
What would your next steps be in caring for this patient?
Patients who experience muscle-related symptoms such as pain, fatigue, or weakness often seek help from their family physician (FP). The list of possible causes of these complaints can be lengthy and vary greatly, from nonmyopathic conditions such as fibromyalgia to worrisome forms of myopathy such as inclusion body myositis or polymyositis. This article will help you to quickly identify which patients with muscle-related complaints should be evaluated for myopathy and what your work-up should include.
Myopathy or not?
Distinguishing between myopathy and nonmyopathic muscle pain or weakness is the first step in evaluating patients with muscle-related complaints. Many conditions share muscle-related symptoms, but actual muscle damage is not always present (eg, fibromyalgia, chronic pain, and chronic fatigue syndromes).1 While there is some overlap in presentation between patients with myopathy and nonmyopathic conditions, there are important differences in symptoms, physical exam findings, and lab test results (TABLE 11-4). Notably, in myopathic disease, patients’ symptoms are usually progressive, vital signs are abnormal, and weakness is common, whereas patients with nonmyopathic disease typically have remitting and relapsing symptoms, normal vital signs, and no weakness.
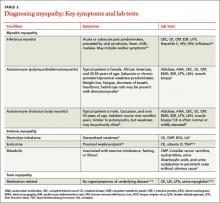
Myopathy itself is divided into 3 categories—myositic, intrinsic, and toxic—which reflect the condition, or medication, that brought on the muscle damage (TABLE 22,4-15). Placing patients into one of these categories based on their risk factors, history, and physical exam findings can help to focus the diagnostic work-up on areas most likely to provide useful information.
Myositic myopathy can be caused by infection or autoimmunity
Myositic myopathies result in inflammatory destruction of muscle tissue. Patients with myositic myopathy often exhibit fever, malaise, weight loss, and general fatigue. Though weakness and pain are common, both can be variable or even absent in myositic myopathy.2,5 Myositic myopathy can be caused by infectious agents or can develop from an autoimmune disease.
Infectious myositic myopathy is one of the more common types of myopathy that FPs will encounter.2 Viruses such as influenza, parainfluenza, coxsackievirus, human immunodeficiency virus, cytomegalovirus, echovirus, adenovirus, Epstein-Barr, and hepatitis C are common causes.2,4,16 Bacterial and fungal myositides are relatively rare. Both most often occur as the result of penetrating trauma or immunocompromise, and are generally not subtle.2 Parasitic myopathy can occur from the invasion of skeletal muscle by trichinella after ingesting undercooked, infected meat.2 Although previously a more common problem, currently only 10 to 20 cases of trichinellosis are reported in the United States each year.17 Due to their rarity, bacterial, fungal, and parasitic myositides are not reviewed here.
Patients with a viral myositis often report prodromal symptoms such as fever, upper respiratory illness, or gastrointestinal distress one to 2 weeks before the onset of muscle complaints. Muscle pain is usually multifocal, involving larger, bilateral muscle groups, and may be associated with swelling.
Patients with viral myositis may exhibit diffusely painful, swollen, or boggy-feeling muscles as well as weakness and pain with exertion. Other signs of viral infection such as rash, fever, upper respiratory symptoms, or meningeal signs may be present. Severe signs include arrhythmia or respiratory failure due to cardiac muscle or diaphragm involvement, or signs of renal failure due to precipitation of myoglobin in the renal system (ie, rhabdomyolysis).2 If the infection affects the heart, patients may develop palpitations, pleuritic chest pain, or shortness of breath.2
Diagnosis of viral myositis relies heavily on clinical suspicion in patients with a fitting history and physical exam findings. Helpful lab tests include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), creatine kinase (CK), and liver function tests (LFTs), all of which can be abnormal in viral myositis. Viral polymerase chain reaction, culture, or antigen testing may be helpful in severe or confusing cases, but in most cases such testing is unnecessary. Muscle biopsy is not recommended except in persistent cases, where definitive identification of the causative agent might alter treatment or when nonviral infection is suspected.2
Autoimmune myositic myopathy. Unlike infectious myopathies, autoimmune myopathies are usually chronic, subtle, and relatively rare. The 3 most common autoimmune myopathies—polymyositis, dermatomyositis, and inclusion body myositis—have a combined prevalence of approximately 10:100,000.6 Although these types of myopathies are uncommon, FPs will likely be the first to evaluate a patient with one of them.
Patients with an autoimmune myopathy typically complain of weakness and mild to moderate muscle pain, although pain may be absent. Compared to infectious myopathies, autoimmune myopathies usually exhibit a more indolent course. Patients with advanced disease may report fever, weight loss, shortness of breath from cardiomyopathy, heartburn from a weakened lower esophageal sphincter, and/or a rash.5
Physical examination may reveal symmetric, proximal muscle weakness. Atrophy is typically not seen until late in the disease. Skin exam usually is normal in patients with inclusion body myositis and polymyositis. The typical rash of dermatomyositis is a heliotrope (blue-purple) discoloration on the upper eyelids and a raised, violaceous, scaly eruption on the knuckles (Gottron’s papules).
Laboratory tests that can be helpful include CK, lactate dehydrogenase (LDH), aldolase, and LFTs (reflecting muscle injury, not liver involvement). For polymyositis and dermatomyositis, CK is the most sensitive lab test and often exhibits the highest elevation above normal.6 Conversely, CK is often normal or only mildly elevated in inclusion body myositis. Up to 80% of patients with autoimmune myopathy will have antinuclear antibodies.3,5 ESR and CRP levels are also often elevated.
Both electromyography (EMG) and muscle biopsy may be required to diagnose autoimmune myopathy, but these are typically done under the direction of a rheumatologist after an FP’s initial work-up is inconclusive.
Intrinsic myopathy: Suspect electrolyte problems, other causes
Intrinsic myopathy occurs in patients with electrolyte disorders, diseases of the endocrine system, or underlying metabolic dysfunction.
Electrolyte disorders. Muscle-related symptoms are unlikely to be the chief complaint of patients with severe electrolyte imbalance. However, a patient with mild to moderate electrolyte problems may develop muscle fatigue, weakness, or pain. TABLE 3 reviews other signs and symptoms of electrolyte abnormalities that may be helpful in establishing a diagnosis in a patient with muscle complaints.
Ordering a complete metabolic panel (CMP), CK, and urinalysis (UA) can help rule out electrolyte disorders. If electrolyte disorders are detected, an electrocardiogram is useful to evaluate for cardiac dysfunction. Once an electrolyte disorder is identified, investigate its underlying cause. Correcting the electrolyte disorder should help improve symptoms of myopathy.
Endocrine myopathy can be associated with hypothyroidism, hyperthyroidism, parathyroid disease, vitamin D deficiency, or Cushing syndrome.8-10,18,19 Although less common than some other causes, identifying endocrine myopathy is crucial because correcting the underlying disease will often improve multiple aspects of the patient’s health.
The presentation of endocrine myopathy may be subtle. Patients with hypothyroidism may experience muscle pain or weakness, fatigue, cold sensitivity, constipation, and dry skin.20 Muscle-related symptoms may be the only sign of endocrine myopathy in a patient who would otherwise be considered to have subclinical hypothyroidism.8,18 Hyperthyroidism can present with weight loss, heat intolerance, frequent bowel movements, tachycardia, and muscle weakness.21
Patients with parathyroid disease— especially patients with chronic renal failure—may report proximal muscle weakness, often in the lower extremities.19 Complaints of muscle weakness or pain can occur with severe vitamin D deficiency.10 Patients with Cushing syndrome often experience proximal weakness and weight gain.9
Patients with a personal or family history of endocrine disorders, previous thyroid surgery, or those taking medications that can impair thyroid function, such as lithium, amiodarone, or interferon, are at risk for endocrine myopathy.18-20 Suspect hyperparathyroidism in patients with chronic kidney disease who complain of weakness.
Vitamin D deficiency is relatively common, with at minimum 20% of elderly adults estimated to be deficient.10 Patients at risk for Cushing disease are most likely receiving pharmacologic doses of glucocorticoids, which can increase their risk of myopathy, or to have ectopic adrenocorticotropic hormone secretion.
Metabolic myopathy results from a lack of sufficient energy production in the muscle. The 3 main groups of metabolic myopathy are impaired muscle glycogenoses, disorders of fatty acid oxidation, and mitochondrial myopathies.7
Because metabolic myopathy can occur at any age, a thorough history and physical is crucial for diagnosis. Proximal weakness in metabolic myopathy is often associated with exercise intolerance, stressful illness, or fasting. Patients often present with dynamic abnormalities such as fatigue, muscle cramping, and even rhabdomyolysis during exertion.7
When evaluating patients you suspect may have metabolic myopathy, a physical exam may reveal muscle contractures, muscle swelling, or proximal muscle weakness. Patients with certain types of fatty acid oxidation disorders or mitochondrial disorders may also exhibit cardiomyopathy, neuropathy, retinopathy, ataxia, hearing loss, or other systemic manifestations.7
Basic labs for investigating suspected metabolic myopathy include serum electrolytes, glucose, LFTs, CK (which may or may not be elevated), lactate, ammonia, and UA for myoglobinuria. More advanced labs, such as serum total carnitine and acylcarnitine as well as urinary levels of dicarboxylic acids and acylglycines, may be needed if a metabolic disorder is strongly suspected.7 Muscle biopsy, EMG, and genetic testing can also prove helpful in diagnosis. Definitive diagnosis and treatment of metabolic myopathy usually requires a multidisciplinary team of providers, including subspecialty referral.
Toxic myopathy
Toxic myopathy refers to muscle damage caused by an exogenous chemical agent, most often a drug. The mechanism of toxicity is not always clear and may result from the activation of inflammatory responses similar to autoimmune myopathy.22 Toxic myopathies may result from several commonly used medications; cholesterol-lowering medications are a common culprit.13-15,23-25 Drug-induced myopathies vary in frequency and severity. For instance, in patients taking statins, the rate of myalgias is 6%, while the incidence of rhabdomyolysis is estimated to be 4 per 100,000, and is found most often in patients taking concomitant fibrates.23
Drug-induced toxic myopathy differs from previously discussed myopathies in that symptoms are usually more insidious, findings on exam are more often mixed muscular and neurologic, and lab abnormalities are usually more subtle.11,12 Symptoms of myopathy typically occur weeks or months after initiating a drug and usually improve or resolve within weeks after discontinuing the offending agent. Knowing the patient’s medication list and which medications cause certain patterns of myopathy symptoms can help guide the differential diagnosis (TABLE 411-15,22-25).
Risk factors for most medication-related myopathies are polypharmacy, renal or liver disease, and age over 50 years13-15,23-25 The physical exam for patients with drug- or toxin-related myopathy will most often reveal relatively minor abnormalities such as muscle tenderness and mild weakness, except for the most severe or advanced cases. Most patients will not have physical signs that suggest an underlying illness. CK levels and LFTs should be obtained. Basic chemistry and UA may also be helpful in patients with risk factors for renal disease.
CASE › Ms. C has been taking a statin for more than 10 years, and the dose was recently increased. You are aware that statin-related muscle injury can develop even after years of use, and suspect the statin may be causing her myopathy. You order a CK test, which is mildly elevated. You recommend discontinuing the statin. After 8 weeks off her statin, Ms. C’s Symptoms do not improve. Given her lack of systemic complaints, myositic myopathy from an infectious or rheumatologic cause seems unlikely. You begin to consider an intrinsic cause of myopathy, and order the following tests: a CMP, UA, thyroid-stimulating hormone, repeat CK, and vitamin D level. This testing reveals a vitamin D deficiency at 17 ng/ml (normal range: 30-74 ng/ml). You recommend vitamin D, 50,000 IU per week for 8 weeks. At follow-up, Ms. C's vitamin D level is 40. She says she feels better and her muscle complaints have resolved.
CORRESPONDENCE
Brent W. Smith, MD, Travis Air Force Base Family Medicine Residency, 101 Bodin Circle, Travis Air Force Base, CA 94535; [email protected]
1. Huynh CN, Yanni LM, Morgan LA. Fibromyalgia: diagnosis and management for the primary healthcare provider. J Womens Health. 2008;8:1379-1387.
2. Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev. 2008;21:473-494.
3. Reichlin M, Arnett FC Jr. Multiplicity of antibodies in myositis sera. Arthritis Rheum. 1984;27:1150-1156.
4. Yoshino M, Suzuki S, Adachi K, et al. High incidence of acute myositis with type A influenza virus infection in the elderly. Intern Med. 2000;39:431-432.
5. Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003;362:971-982.
6. Wilson FC, Ytterberg SR, St Sauver JL, et al. Epidemiology of sporadic inclusion body myositis and polymyositis in Olmsted County, Minnesota. J Rheumatol. 2008;35:445-447.
7. Smith EC, El-Gharbawy A, Koeberl DD. Metabolic myopathies: clinical features and diagnostic approach. Rheum Dis Clin N Am. 2011:37:201-217.
8. Reuters V, Teixeira Pde F, Vigário PS, et al. Functional capacity and muscular abnormalities in subclinical hypothyroidism. Am J Med Sci. 2009;338:259-263.
9. Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:1526-1540.
10. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930.
11. Antons KA, Williams CD, Baker SK, et al. Clinical perspectives of statin-induced rhabdomyolysis. Am J Med. 2006;119:400-409.
12. Phillips PS, Haas RH, Bannykh S, et al; Scripps Mercy Clinical Research Center. Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2002;137:581-585.
13. Pereira RM, Freire de Carvalho J. Glucocorticoid-induced myopathy. Joint Bone Spine. 2011;78:41-44.
14. Posada C, García-Cruz A, García-Doval I, et al. Chloroquine-induced myopathy. Lupus. 2011;20:773-774.
15. Uri DS, Biavis M. Colchicine neuromyopathy. J Clin Rheumatol. 1996;2:163-166.
16. Mannix R, Tan ML, Wright R, et al. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006;118:2119-2125.
17. Pozio E. World distribution of Trichinella spp. infections in animals and humans. Vet Parasitol. 2007;149:3-21.
18. Rodolico C, Toscano A, Benvenga S, et al. Myopathy as the persistently isolated symptomatology of primary autoimmune hypothyroidism. Thyroid.1998;8:1033-1038.
19. AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of Clinical Endocrinologists and The American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49-54.
20. Garber JR, Cobin RH, Gharib H, et al; American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocrine Pract. 2012;18:988-1028.
21. Bahn Chair RS, Burch HB, Cooper DS, et al; American Thyroid Association; American Association of Clinical Endocrinologists. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21:593-646.
22. Mammen AL, Amato AA. Statin myopathy: a review of recent progress. Curr Opin Rheumatol. 2010;22:644-650.
23. Buettner C, Davis RB, Leveille SG, et al. Prevalence of musculoskeletal pain and statin use. J Gen Intern Med. 2008;23: 1182-1186.
24. Marot A, Morelle J, Chouinard VA, et al. Concomitant use of simvastatin and amiodarone resulting in severe rhabdomyolysis: a case report and review of the literature. Acta Clin Belg. 2011;66:134-136.
25. Peters BS, Winer J, Landon DN, et al. Mitochondrial myopathy associated with chronic zidovudine therapy in AIDS. Q J Med. 1993;86:5-15.
› Categorize patients with muscle complaints into suspected myositic, intrinsic, or toxic myopathy to help guide subsequent work-up. C
› Look for diffusely painful, swollen, or boggy-feeling muscles—as well as weakness and pain with exertion—in patients you suspect may have viral myopathy. C
› Consider electromyography and muscle biopsy for patients you suspect may have dermatomyositis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Marie C, a 75-year-old Asian woman, reports weakness in her legs and arms with unsteadiness when walking. She has a vague but persistent ache in her large muscles. Her symptoms have developed slowly over the past 3 months. She denies recent signs or symptoms of infection or other illness. Her medical history includes hypertension, hyperlipidemia, osteopenia, and obesity. Ms. C takes lisinopril 10 mg/d and atorvastatin, which was recently increased from 10 to 20 mg/d.
What would your next steps be in caring for this patient?
Patients who experience muscle-related symptoms such as pain, fatigue, or weakness often seek help from their family physician (FP). The list of possible causes of these complaints can be lengthy and vary greatly, from nonmyopathic conditions such as fibromyalgia to worrisome forms of myopathy such as inclusion body myositis or polymyositis. This article will help you to quickly identify which patients with muscle-related complaints should be evaluated for myopathy and what your work-up should include.
Myopathy or not?
Distinguishing between myopathy and nonmyopathic muscle pain or weakness is the first step in evaluating patients with muscle-related complaints. Many conditions share muscle-related symptoms, but actual muscle damage is not always present (eg, fibromyalgia, chronic pain, and chronic fatigue syndromes).1 While there is some overlap in presentation between patients with myopathy and nonmyopathic conditions, there are important differences in symptoms, physical exam findings, and lab test results (TABLE 11-4). Notably, in myopathic disease, patients’ symptoms are usually progressive, vital signs are abnormal, and weakness is common, whereas patients with nonmyopathic disease typically have remitting and relapsing symptoms, normal vital signs, and no weakness.
Myopathy itself is divided into 3 categories—myositic, intrinsic, and toxic—which reflect the condition, or medication, that brought on the muscle damage (TABLE 22,4-15). Placing patients into one of these categories based on their risk factors, history, and physical exam findings can help to focus the diagnostic work-up on areas most likely to provide useful information.
Myositic myopathy can be caused by infection or autoimmunity
Myositic myopathies result in inflammatory destruction of muscle tissue. Patients with myositic myopathy often exhibit fever, malaise, weight loss, and general fatigue. Though weakness and pain are common, both can be variable or even absent in myositic myopathy.2,5 Myositic myopathy can be caused by infectious agents or can develop from an autoimmune disease.
Infectious myositic myopathy is one of the more common types of myopathy that FPs will encounter.2 Viruses such as influenza, parainfluenza, coxsackievirus, human immunodeficiency virus, cytomegalovirus, echovirus, adenovirus, Epstein-Barr, and hepatitis C are common causes.2,4,16 Bacterial and fungal myositides are relatively rare. Both most often occur as the result of penetrating trauma or immunocompromise, and are generally not subtle.2 Parasitic myopathy can occur from the invasion of skeletal muscle by trichinella after ingesting undercooked, infected meat.2 Although previously a more common problem, currently only 10 to 20 cases of trichinellosis are reported in the United States each year.17 Due to their rarity, bacterial, fungal, and parasitic myositides are not reviewed here.
Patients with a viral myositis often report prodromal symptoms such as fever, upper respiratory illness, or gastrointestinal distress one to 2 weeks before the onset of muscle complaints. Muscle pain is usually multifocal, involving larger, bilateral muscle groups, and may be associated with swelling.
Patients with viral myositis may exhibit diffusely painful, swollen, or boggy-feeling muscles as well as weakness and pain with exertion. Other signs of viral infection such as rash, fever, upper respiratory symptoms, or meningeal signs may be present. Severe signs include arrhythmia or respiratory failure due to cardiac muscle or diaphragm involvement, or signs of renal failure due to precipitation of myoglobin in the renal system (ie, rhabdomyolysis).2 If the infection affects the heart, patients may develop palpitations, pleuritic chest pain, or shortness of breath.2
Diagnosis of viral myositis relies heavily on clinical suspicion in patients with a fitting history and physical exam findings. Helpful lab tests include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), creatine kinase (CK), and liver function tests (LFTs), all of which can be abnormal in viral myositis. Viral polymerase chain reaction, culture, or antigen testing may be helpful in severe or confusing cases, but in most cases such testing is unnecessary. Muscle biopsy is not recommended except in persistent cases, where definitive identification of the causative agent might alter treatment or when nonviral infection is suspected.2
Autoimmune myositic myopathy. Unlike infectious myopathies, autoimmune myopathies are usually chronic, subtle, and relatively rare. The 3 most common autoimmune myopathies—polymyositis, dermatomyositis, and inclusion body myositis—have a combined prevalence of approximately 10:100,000.6 Although these types of myopathies are uncommon, FPs will likely be the first to evaluate a patient with one of them.
Patients with an autoimmune myopathy typically complain of weakness and mild to moderate muscle pain, although pain may be absent. Compared to infectious myopathies, autoimmune myopathies usually exhibit a more indolent course. Patients with advanced disease may report fever, weight loss, shortness of breath from cardiomyopathy, heartburn from a weakened lower esophageal sphincter, and/or a rash.5
Physical examination may reveal symmetric, proximal muscle weakness. Atrophy is typically not seen until late in the disease. Skin exam usually is normal in patients with inclusion body myositis and polymyositis. The typical rash of dermatomyositis is a heliotrope (blue-purple) discoloration on the upper eyelids and a raised, violaceous, scaly eruption on the knuckles (Gottron’s papules).
Laboratory tests that can be helpful include CK, lactate dehydrogenase (LDH), aldolase, and LFTs (reflecting muscle injury, not liver involvement). For polymyositis and dermatomyositis, CK is the most sensitive lab test and often exhibits the highest elevation above normal.6 Conversely, CK is often normal or only mildly elevated in inclusion body myositis. Up to 80% of patients with autoimmune myopathy will have antinuclear antibodies.3,5 ESR and CRP levels are also often elevated.
Both electromyography (EMG) and muscle biopsy may be required to diagnose autoimmune myopathy, but these are typically done under the direction of a rheumatologist after an FP’s initial work-up is inconclusive.
Intrinsic myopathy: Suspect electrolyte problems, other causes
Intrinsic myopathy occurs in patients with electrolyte disorders, diseases of the endocrine system, or underlying metabolic dysfunction.
Electrolyte disorders. Muscle-related symptoms are unlikely to be the chief complaint of patients with severe electrolyte imbalance. However, a patient with mild to moderate electrolyte problems may develop muscle fatigue, weakness, or pain. TABLE 3 reviews other signs and symptoms of electrolyte abnormalities that may be helpful in establishing a diagnosis in a patient with muscle complaints.
Ordering a complete metabolic panel (CMP), CK, and urinalysis (UA) can help rule out electrolyte disorders. If electrolyte disorders are detected, an electrocardiogram is useful to evaluate for cardiac dysfunction. Once an electrolyte disorder is identified, investigate its underlying cause. Correcting the electrolyte disorder should help improve symptoms of myopathy.
Endocrine myopathy can be associated with hypothyroidism, hyperthyroidism, parathyroid disease, vitamin D deficiency, or Cushing syndrome.8-10,18,19 Although less common than some other causes, identifying endocrine myopathy is crucial because correcting the underlying disease will often improve multiple aspects of the patient’s health.
The presentation of endocrine myopathy may be subtle. Patients with hypothyroidism may experience muscle pain or weakness, fatigue, cold sensitivity, constipation, and dry skin.20 Muscle-related symptoms may be the only sign of endocrine myopathy in a patient who would otherwise be considered to have subclinical hypothyroidism.8,18 Hyperthyroidism can present with weight loss, heat intolerance, frequent bowel movements, tachycardia, and muscle weakness.21
Patients with parathyroid disease— especially patients with chronic renal failure—may report proximal muscle weakness, often in the lower extremities.19 Complaints of muscle weakness or pain can occur with severe vitamin D deficiency.10 Patients with Cushing syndrome often experience proximal weakness and weight gain.9
Patients with a personal or family history of endocrine disorders, previous thyroid surgery, or those taking medications that can impair thyroid function, such as lithium, amiodarone, or interferon, are at risk for endocrine myopathy.18-20 Suspect hyperparathyroidism in patients with chronic kidney disease who complain of weakness.
Vitamin D deficiency is relatively common, with at minimum 20% of elderly adults estimated to be deficient.10 Patients at risk for Cushing disease are most likely receiving pharmacologic doses of glucocorticoids, which can increase their risk of myopathy, or to have ectopic adrenocorticotropic hormone secretion.
Metabolic myopathy results from a lack of sufficient energy production in the muscle. The 3 main groups of metabolic myopathy are impaired muscle glycogenoses, disorders of fatty acid oxidation, and mitochondrial myopathies.7
Because metabolic myopathy can occur at any age, a thorough history and physical is crucial for diagnosis. Proximal weakness in metabolic myopathy is often associated with exercise intolerance, stressful illness, or fasting. Patients often present with dynamic abnormalities such as fatigue, muscle cramping, and even rhabdomyolysis during exertion.7
When evaluating patients you suspect may have metabolic myopathy, a physical exam may reveal muscle contractures, muscle swelling, or proximal muscle weakness. Patients with certain types of fatty acid oxidation disorders or mitochondrial disorders may also exhibit cardiomyopathy, neuropathy, retinopathy, ataxia, hearing loss, or other systemic manifestations.7
Basic labs for investigating suspected metabolic myopathy include serum electrolytes, glucose, LFTs, CK (which may or may not be elevated), lactate, ammonia, and UA for myoglobinuria. More advanced labs, such as serum total carnitine and acylcarnitine as well as urinary levels of dicarboxylic acids and acylglycines, may be needed if a metabolic disorder is strongly suspected.7 Muscle biopsy, EMG, and genetic testing can also prove helpful in diagnosis. Definitive diagnosis and treatment of metabolic myopathy usually requires a multidisciplinary team of providers, including subspecialty referral.
Toxic myopathy
Toxic myopathy refers to muscle damage caused by an exogenous chemical agent, most often a drug. The mechanism of toxicity is not always clear and may result from the activation of inflammatory responses similar to autoimmune myopathy.22 Toxic myopathies may result from several commonly used medications; cholesterol-lowering medications are a common culprit.13-15,23-25 Drug-induced myopathies vary in frequency and severity. For instance, in patients taking statins, the rate of myalgias is 6%, while the incidence of rhabdomyolysis is estimated to be 4 per 100,000, and is found most often in patients taking concomitant fibrates.23
Drug-induced toxic myopathy differs from previously discussed myopathies in that symptoms are usually more insidious, findings on exam are more often mixed muscular and neurologic, and lab abnormalities are usually more subtle.11,12 Symptoms of myopathy typically occur weeks or months after initiating a drug and usually improve or resolve within weeks after discontinuing the offending agent. Knowing the patient’s medication list and which medications cause certain patterns of myopathy symptoms can help guide the differential diagnosis (TABLE 411-15,22-25).
Risk factors for most medication-related myopathies are polypharmacy, renal or liver disease, and age over 50 years13-15,23-25 The physical exam for patients with drug- or toxin-related myopathy will most often reveal relatively minor abnormalities such as muscle tenderness and mild weakness, except for the most severe or advanced cases. Most patients will not have physical signs that suggest an underlying illness. CK levels and LFTs should be obtained. Basic chemistry and UA may also be helpful in patients with risk factors for renal disease.
CASE › Ms. C has been taking a statin for more than 10 years, and the dose was recently increased. You are aware that statin-related muscle injury can develop even after years of use, and suspect the statin may be causing her myopathy. You order a CK test, which is mildly elevated. You recommend discontinuing the statin. After 8 weeks off her statin, Ms. C’s Symptoms do not improve. Given her lack of systemic complaints, myositic myopathy from an infectious or rheumatologic cause seems unlikely. You begin to consider an intrinsic cause of myopathy, and order the following tests: a CMP, UA, thyroid-stimulating hormone, repeat CK, and vitamin D level. This testing reveals a vitamin D deficiency at 17 ng/ml (normal range: 30-74 ng/ml). You recommend vitamin D, 50,000 IU per week for 8 weeks. At follow-up, Ms. C's vitamin D level is 40. She says she feels better and her muscle complaints have resolved.
CORRESPONDENCE
Brent W. Smith, MD, Travis Air Force Base Family Medicine Residency, 101 Bodin Circle, Travis Air Force Base, CA 94535; [email protected]
› Categorize patients with muscle complaints into suspected myositic, intrinsic, or toxic myopathy to help guide subsequent work-up. C
› Look for diffusely painful, swollen, or boggy-feeling muscles—as well as weakness and pain with exertion—in patients you suspect may have viral myopathy. C
› Consider electromyography and muscle biopsy for patients you suspect may have dermatomyositis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Marie C, a 75-year-old Asian woman, reports weakness in her legs and arms with unsteadiness when walking. She has a vague but persistent ache in her large muscles. Her symptoms have developed slowly over the past 3 months. She denies recent signs or symptoms of infection or other illness. Her medical history includes hypertension, hyperlipidemia, osteopenia, and obesity. Ms. C takes lisinopril 10 mg/d and atorvastatin, which was recently increased from 10 to 20 mg/d.
What would your next steps be in caring for this patient?
Patients who experience muscle-related symptoms such as pain, fatigue, or weakness often seek help from their family physician (FP). The list of possible causes of these complaints can be lengthy and vary greatly, from nonmyopathic conditions such as fibromyalgia to worrisome forms of myopathy such as inclusion body myositis or polymyositis. This article will help you to quickly identify which patients with muscle-related complaints should be evaluated for myopathy and what your work-up should include.
Myopathy or not?
Distinguishing between myopathy and nonmyopathic muscle pain or weakness is the first step in evaluating patients with muscle-related complaints. Many conditions share muscle-related symptoms, but actual muscle damage is not always present (eg, fibromyalgia, chronic pain, and chronic fatigue syndromes).1 While there is some overlap in presentation between patients with myopathy and nonmyopathic conditions, there are important differences in symptoms, physical exam findings, and lab test results (TABLE 11-4). Notably, in myopathic disease, patients’ symptoms are usually progressive, vital signs are abnormal, and weakness is common, whereas patients with nonmyopathic disease typically have remitting and relapsing symptoms, normal vital signs, and no weakness.
Myopathy itself is divided into 3 categories—myositic, intrinsic, and toxic—which reflect the condition, or medication, that brought on the muscle damage (TABLE 22,4-15). Placing patients into one of these categories based on their risk factors, history, and physical exam findings can help to focus the diagnostic work-up on areas most likely to provide useful information.
Myositic myopathy can be caused by infection or autoimmunity
Myositic myopathies result in inflammatory destruction of muscle tissue. Patients with myositic myopathy often exhibit fever, malaise, weight loss, and general fatigue. Though weakness and pain are common, both can be variable or even absent in myositic myopathy.2,5 Myositic myopathy can be caused by infectious agents or can develop from an autoimmune disease.
Infectious myositic myopathy is one of the more common types of myopathy that FPs will encounter.2 Viruses such as influenza, parainfluenza, coxsackievirus, human immunodeficiency virus, cytomegalovirus, echovirus, adenovirus, Epstein-Barr, and hepatitis C are common causes.2,4,16 Bacterial and fungal myositides are relatively rare. Both most often occur as the result of penetrating trauma or immunocompromise, and are generally not subtle.2 Parasitic myopathy can occur from the invasion of skeletal muscle by trichinella after ingesting undercooked, infected meat.2 Although previously a more common problem, currently only 10 to 20 cases of trichinellosis are reported in the United States each year.17 Due to their rarity, bacterial, fungal, and parasitic myositides are not reviewed here.
Patients with a viral myositis often report prodromal symptoms such as fever, upper respiratory illness, or gastrointestinal distress one to 2 weeks before the onset of muscle complaints. Muscle pain is usually multifocal, involving larger, bilateral muscle groups, and may be associated with swelling.
Patients with viral myositis may exhibit diffusely painful, swollen, or boggy-feeling muscles as well as weakness and pain with exertion. Other signs of viral infection such as rash, fever, upper respiratory symptoms, or meningeal signs may be present. Severe signs include arrhythmia or respiratory failure due to cardiac muscle or diaphragm involvement, or signs of renal failure due to precipitation of myoglobin in the renal system (ie, rhabdomyolysis).2 If the infection affects the heart, patients may develop palpitations, pleuritic chest pain, or shortness of breath.2
Diagnosis of viral myositis relies heavily on clinical suspicion in patients with a fitting history and physical exam findings. Helpful lab tests include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), creatine kinase (CK), and liver function tests (LFTs), all of which can be abnormal in viral myositis. Viral polymerase chain reaction, culture, or antigen testing may be helpful in severe or confusing cases, but in most cases such testing is unnecessary. Muscle biopsy is not recommended except in persistent cases, where definitive identification of the causative agent might alter treatment or when nonviral infection is suspected.2
Autoimmune myositic myopathy. Unlike infectious myopathies, autoimmune myopathies are usually chronic, subtle, and relatively rare. The 3 most common autoimmune myopathies—polymyositis, dermatomyositis, and inclusion body myositis—have a combined prevalence of approximately 10:100,000.6 Although these types of myopathies are uncommon, FPs will likely be the first to evaluate a patient with one of them.
Patients with an autoimmune myopathy typically complain of weakness and mild to moderate muscle pain, although pain may be absent. Compared to infectious myopathies, autoimmune myopathies usually exhibit a more indolent course. Patients with advanced disease may report fever, weight loss, shortness of breath from cardiomyopathy, heartburn from a weakened lower esophageal sphincter, and/or a rash.5
Physical examination may reveal symmetric, proximal muscle weakness. Atrophy is typically not seen until late in the disease. Skin exam usually is normal in patients with inclusion body myositis and polymyositis. The typical rash of dermatomyositis is a heliotrope (blue-purple) discoloration on the upper eyelids and a raised, violaceous, scaly eruption on the knuckles (Gottron’s papules).
Laboratory tests that can be helpful include CK, lactate dehydrogenase (LDH), aldolase, and LFTs (reflecting muscle injury, not liver involvement). For polymyositis and dermatomyositis, CK is the most sensitive lab test and often exhibits the highest elevation above normal.6 Conversely, CK is often normal or only mildly elevated in inclusion body myositis. Up to 80% of patients with autoimmune myopathy will have antinuclear antibodies.3,5 ESR and CRP levels are also often elevated.
Both electromyography (EMG) and muscle biopsy may be required to diagnose autoimmune myopathy, but these are typically done under the direction of a rheumatologist after an FP’s initial work-up is inconclusive.
Intrinsic myopathy: Suspect electrolyte problems, other causes
Intrinsic myopathy occurs in patients with electrolyte disorders, diseases of the endocrine system, or underlying metabolic dysfunction.
Electrolyte disorders. Muscle-related symptoms are unlikely to be the chief complaint of patients with severe electrolyte imbalance. However, a patient with mild to moderate electrolyte problems may develop muscle fatigue, weakness, or pain. TABLE 3 reviews other signs and symptoms of electrolyte abnormalities that may be helpful in establishing a diagnosis in a patient with muscle complaints.
Ordering a complete metabolic panel (CMP), CK, and urinalysis (UA) can help rule out electrolyte disorders. If electrolyte disorders are detected, an electrocardiogram is useful to evaluate for cardiac dysfunction. Once an electrolyte disorder is identified, investigate its underlying cause. Correcting the electrolyte disorder should help improve symptoms of myopathy.
Endocrine myopathy can be associated with hypothyroidism, hyperthyroidism, parathyroid disease, vitamin D deficiency, or Cushing syndrome.8-10,18,19 Although less common than some other causes, identifying endocrine myopathy is crucial because correcting the underlying disease will often improve multiple aspects of the patient’s health.
The presentation of endocrine myopathy may be subtle. Patients with hypothyroidism may experience muscle pain or weakness, fatigue, cold sensitivity, constipation, and dry skin.20 Muscle-related symptoms may be the only sign of endocrine myopathy in a patient who would otherwise be considered to have subclinical hypothyroidism.8,18 Hyperthyroidism can present with weight loss, heat intolerance, frequent bowel movements, tachycardia, and muscle weakness.21
Patients with parathyroid disease— especially patients with chronic renal failure—may report proximal muscle weakness, often in the lower extremities.19 Complaints of muscle weakness or pain can occur with severe vitamin D deficiency.10 Patients with Cushing syndrome often experience proximal weakness and weight gain.9
Patients with a personal or family history of endocrine disorders, previous thyroid surgery, or those taking medications that can impair thyroid function, such as lithium, amiodarone, or interferon, are at risk for endocrine myopathy.18-20 Suspect hyperparathyroidism in patients with chronic kidney disease who complain of weakness.
Vitamin D deficiency is relatively common, with at minimum 20% of elderly adults estimated to be deficient.10 Patients at risk for Cushing disease are most likely receiving pharmacologic doses of glucocorticoids, which can increase their risk of myopathy, or to have ectopic adrenocorticotropic hormone secretion.
Metabolic myopathy results from a lack of sufficient energy production in the muscle. The 3 main groups of metabolic myopathy are impaired muscle glycogenoses, disorders of fatty acid oxidation, and mitochondrial myopathies.7
Because metabolic myopathy can occur at any age, a thorough history and physical is crucial for diagnosis. Proximal weakness in metabolic myopathy is often associated with exercise intolerance, stressful illness, or fasting. Patients often present with dynamic abnormalities such as fatigue, muscle cramping, and even rhabdomyolysis during exertion.7
When evaluating patients you suspect may have metabolic myopathy, a physical exam may reveal muscle contractures, muscle swelling, or proximal muscle weakness. Patients with certain types of fatty acid oxidation disorders or mitochondrial disorders may also exhibit cardiomyopathy, neuropathy, retinopathy, ataxia, hearing loss, or other systemic manifestations.7
Basic labs for investigating suspected metabolic myopathy include serum electrolytes, glucose, LFTs, CK (which may or may not be elevated), lactate, ammonia, and UA for myoglobinuria. More advanced labs, such as serum total carnitine and acylcarnitine as well as urinary levels of dicarboxylic acids and acylglycines, may be needed if a metabolic disorder is strongly suspected.7 Muscle biopsy, EMG, and genetic testing can also prove helpful in diagnosis. Definitive diagnosis and treatment of metabolic myopathy usually requires a multidisciplinary team of providers, including subspecialty referral.
Toxic myopathy
Toxic myopathy refers to muscle damage caused by an exogenous chemical agent, most often a drug. The mechanism of toxicity is not always clear and may result from the activation of inflammatory responses similar to autoimmune myopathy.22 Toxic myopathies may result from several commonly used medications; cholesterol-lowering medications are a common culprit.13-15,23-25 Drug-induced myopathies vary in frequency and severity. For instance, in patients taking statins, the rate of myalgias is 6%, while the incidence of rhabdomyolysis is estimated to be 4 per 100,000, and is found most often in patients taking concomitant fibrates.23
Drug-induced toxic myopathy differs from previously discussed myopathies in that symptoms are usually more insidious, findings on exam are more often mixed muscular and neurologic, and lab abnormalities are usually more subtle.11,12 Symptoms of myopathy typically occur weeks or months after initiating a drug and usually improve or resolve within weeks after discontinuing the offending agent. Knowing the patient’s medication list and which medications cause certain patterns of myopathy symptoms can help guide the differential diagnosis (TABLE 411-15,22-25).
Risk factors for most medication-related myopathies are polypharmacy, renal or liver disease, and age over 50 years13-15,23-25 The physical exam for patients with drug- or toxin-related myopathy will most often reveal relatively minor abnormalities such as muscle tenderness and mild weakness, except for the most severe or advanced cases. Most patients will not have physical signs that suggest an underlying illness. CK levels and LFTs should be obtained. Basic chemistry and UA may also be helpful in patients with risk factors for renal disease.
CASE › Ms. C has been taking a statin for more than 10 years, and the dose was recently increased. You are aware that statin-related muscle injury can develop even after years of use, and suspect the statin may be causing her myopathy. You order a CK test, which is mildly elevated. You recommend discontinuing the statin. After 8 weeks off her statin, Ms. C’s Symptoms do not improve. Given her lack of systemic complaints, myositic myopathy from an infectious or rheumatologic cause seems unlikely. You begin to consider an intrinsic cause of myopathy, and order the following tests: a CMP, UA, thyroid-stimulating hormone, repeat CK, and vitamin D level. This testing reveals a vitamin D deficiency at 17 ng/ml (normal range: 30-74 ng/ml). You recommend vitamin D, 50,000 IU per week for 8 weeks. At follow-up, Ms. C's vitamin D level is 40. She says she feels better and her muscle complaints have resolved.
CORRESPONDENCE
Brent W. Smith, MD, Travis Air Force Base Family Medicine Residency, 101 Bodin Circle, Travis Air Force Base, CA 94535; [email protected]
1. Huynh CN, Yanni LM, Morgan LA. Fibromyalgia: diagnosis and management for the primary healthcare provider. J Womens Health. 2008;8:1379-1387.
2. Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev. 2008;21:473-494.
3. Reichlin M, Arnett FC Jr. Multiplicity of antibodies in myositis sera. Arthritis Rheum. 1984;27:1150-1156.
4. Yoshino M, Suzuki S, Adachi K, et al. High incidence of acute myositis with type A influenza virus infection in the elderly. Intern Med. 2000;39:431-432.
5. Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003;362:971-982.
6. Wilson FC, Ytterberg SR, St Sauver JL, et al. Epidemiology of sporadic inclusion body myositis and polymyositis in Olmsted County, Minnesota. J Rheumatol. 2008;35:445-447.
7. Smith EC, El-Gharbawy A, Koeberl DD. Metabolic myopathies: clinical features and diagnostic approach. Rheum Dis Clin N Am. 2011:37:201-217.
8. Reuters V, Teixeira Pde F, Vigário PS, et al. Functional capacity and muscular abnormalities in subclinical hypothyroidism. Am J Med Sci. 2009;338:259-263.
9. Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:1526-1540.
10. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930.
11. Antons KA, Williams CD, Baker SK, et al. Clinical perspectives of statin-induced rhabdomyolysis. Am J Med. 2006;119:400-409.
12. Phillips PS, Haas RH, Bannykh S, et al; Scripps Mercy Clinical Research Center. Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2002;137:581-585.
13. Pereira RM, Freire de Carvalho J. Glucocorticoid-induced myopathy. Joint Bone Spine. 2011;78:41-44.
14. Posada C, García-Cruz A, García-Doval I, et al. Chloroquine-induced myopathy. Lupus. 2011;20:773-774.
15. Uri DS, Biavis M. Colchicine neuromyopathy. J Clin Rheumatol. 1996;2:163-166.
16. Mannix R, Tan ML, Wright R, et al. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006;118:2119-2125.
17. Pozio E. World distribution of Trichinella spp. infections in animals and humans. Vet Parasitol. 2007;149:3-21.
18. Rodolico C, Toscano A, Benvenga S, et al. Myopathy as the persistently isolated symptomatology of primary autoimmune hypothyroidism. Thyroid.1998;8:1033-1038.
19. AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of Clinical Endocrinologists and The American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49-54.
20. Garber JR, Cobin RH, Gharib H, et al; American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocrine Pract. 2012;18:988-1028.
21. Bahn Chair RS, Burch HB, Cooper DS, et al; American Thyroid Association; American Association of Clinical Endocrinologists. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21:593-646.
22. Mammen AL, Amato AA. Statin myopathy: a review of recent progress. Curr Opin Rheumatol. 2010;22:644-650.
23. Buettner C, Davis RB, Leveille SG, et al. Prevalence of musculoskeletal pain and statin use. J Gen Intern Med. 2008;23: 1182-1186.
24. Marot A, Morelle J, Chouinard VA, et al. Concomitant use of simvastatin and amiodarone resulting in severe rhabdomyolysis: a case report and review of the literature. Acta Clin Belg. 2011;66:134-136.
25. Peters BS, Winer J, Landon DN, et al. Mitochondrial myopathy associated with chronic zidovudine therapy in AIDS. Q J Med. 1993;86:5-15.
1. Huynh CN, Yanni LM, Morgan LA. Fibromyalgia: diagnosis and management for the primary healthcare provider. J Womens Health. 2008;8:1379-1387.
2. Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev. 2008;21:473-494.
3. Reichlin M, Arnett FC Jr. Multiplicity of antibodies in myositis sera. Arthritis Rheum. 1984;27:1150-1156.
4. Yoshino M, Suzuki S, Adachi K, et al. High incidence of acute myositis with type A influenza virus infection in the elderly. Intern Med. 2000;39:431-432.
5. Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003;362:971-982.
6. Wilson FC, Ytterberg SR, St Sauver JL, et al. Epidemiology of sporadic inclusion body myositis and polymyositis in Olmsted County, Minnesota. J Rheumatol. 2008;35:445-447.
7. Smith EC, El-Gharbawy A, Koeberl DD. Metabolic myopathies: clinical features and diagnostic approach. Rheum Dis Clin N Am. 2011:37:201-217.
8. Reuters V, Teixeira Pde F, Vigário PS, et al. Functional capacity and muscular abnormalities in subclinical hypothyroidism. Am J Med Sci. 2009;338:259-263.
9. Nieman LK, Biller BM, Findling JW, et al. The diagnosis of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:1526-1540.
10. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930.
11. Antons KA, Williams CD, Baker SK, et al. Clinical perspectives of statin-induced rhabdomyolysis. Am J Med. 2006;119:400-409.
12. Phillips PS, Haas RH, Bannykh S, et al; Scripps Mercy Clinical Research Center. Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2002;137:581-585.
13. Pereira RM, Freire de Carvalho J. Glucocorticoid-induced myopathy. Joint Bone Spine. 2011;78:41-44.
14. Posada C, García-Cruz A, García-Doval I, et al. Chloroquine-induced myopathy. Lupus. 2011;20:773-774.
15. Uri DS, Biavis M. Colchicine neuromyopathy. J Clin Rheumatol. 1996;2:163-166.
16. Mannix R, Tan ML, Wright R, et al. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006;118:2119-2125.
17. Pozio E. World distribution of Trichinella spp. infections in animals and humans. Vet Parasitol. 2007;149:3-21.
18. Rodolico C, Toscano A, Benvenga S, et al. Myopathy as the persistently isolated symptomatology of primary autoimmune hypothyroidism. Thyroid.1998;8:1033-1038.
19. AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of Clinical Endocrinologists and The American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49-54.
20. Garber JR, Cobin RH, Gharib H, et al; American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocrine Pract. 2012;18:988-1028.
21. Bahn Chair RS, Burch HB, Cooper DS, et al; American Thyroid Association; American Association of Clinical Endocrinologists. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011;21:593-646.
22. Mammen AL, Amato AA. Statin myopathy: a review of recent progress. Curr Opin Rheumatol. 2010;22:644-650.
23. Buettner C, Davis RB, Leveille SG, et al. Prevalence of musculoskeletal pain and statin use. J Gen Intern Med. 2008;23: 1182-1186.
24. Marot A, Morelle J, Chouinard VA, et al. Concomitant use of simvastatin and amiodarone resulting in severe rhabdomyolysis: a case report and review of the literature. Acta Clin Belg. 2011;66:134-136.
25. Peters BS, Winer J, Landon DN, et al. Mitochondrial myopathy associated with chronic zidovudine therapy in AIDS. Q J Med. 1993;86:5-15.