User login
Nonsurgical biomarkers show potential in chronic endometriosis
SALT LAKE CITY – and might soon spare patients from years of misdiagnosis and the costs and burden of diagnostic surgery, according to experts at the annual meeting of the American Society for Reproductive Medicine.
Most notably, expression levels of three microRNAs, 125-b-5p, 451a, and 3613-5p, correctly distinguished patients with chronic endometriosis from healthy controls, said Hugh S. Taylor, MD, of Yale University in New Haven, Conn.
Chronic endometriosis affects about 10% of women and up to half of those with infertility, Dr. Taylor noted. The disease costs the United States at least $22 billion annually and is the second most-common reason for hysterectomy (Reprod Sci. 2009 Apr;16[4]:335-46). Its complexity means that patients face many barriers to diagnosis, particularly young women, who are often told they have “routine” menstrual pain, Dr. Taylor said.
Patients may go up to 12 years and see five or more physicians before they are diagnosed. Clinicians tend to rely on surgical diagnosis, but “there is a reluctance to perform surgery unless there is severe disease,” he added. “The lack of nonsurgical biomarkers contributes significantly to delays in diagnosis and timely intervention.”
These concerns prompted Dr. Taylor and his associates to study microRNAs – the short, noncoding, functional RNAs that promote messenger RNA breakdown or repress its translation. MicroRNA expression varies by tissue type and disease status, and occurs in a variety of body fluids, giving them real potential as nonsurgical biomarkers, Dr. Taylor said. To examine their role in endometriosis, he and his associates performed microarray profiling and confirmatory quantitative real-time polymerase chain reaction testing of serum samples from 24 women with chronic endometriosis and 24 healthy women who served as controls (Fertil Steril. 2016 Aug;106[2]:402-9).
MicroRNA 125b-5p was upregulated the most in endometriosis patients and distinguished patients from controls with a “giant” area under the receiver operating characteristic curve value of 0.974, Dr. Taylor said. Remarkably, this value rose to 1 – meaning that sensitivity and specificity both were 100% – when the researchers added another upregulated microRNA (451a) and a downregulated microRNA (3613-5p) to the model. More work is underway to understand how a test for these microRNAs would perform in larger populations, Dr. Taylor said.
MicroRNAs also are likely to play functional roles in chronic endometriosis and may mediate treatment response, he noted. For example, the microRNA 125b-5p, which is upregulated in endometriosis, increases the expression of inflammatory cytokines and tumor necrosis factor alpha in macrophages, and the aromatase inhibitor letrozole, which reduces pelvic pain in the disease, increases the expression of let-7 microRNAs, with corresponding decreases in the migration of endometrial cells (Fertil Steril. 2016 Sep 1;106[3]:673-80). “Maybe these microRNAs are changing metabolism. Maybe they are changing immune cell activity,” Dr. Taylor said. “I think they are doing a lot more than sitting around waiting for us to discover them.”
None of the 24 patients with endometriosis in his study had taken oral contraceptives in the 3 months prior to serum sampling, Dr. Taylor noted. “We need to look at oral contraception as a potential confounder,” he acknowledged. “If something is independent of the menstrual cycle phase, that is much better than a marker that is dependent on cycle phase.”
Menstrual cycle phase and oral contraceptives are just two of many potential confounders of biomarkers in chronic endometriosis, according to Linda Giudice, MD, PhD, of the University of California, San Francisco. Disease severity, as well as the type, number, and location of lesions and the presence or absence of coexisting inflammatory disorders all can potentially affect the sensitivity and specificity of a marker, she said. Consequently, “there is no single biomarker for chronic endometriosis,” but there are several candidates besides microRNAs, she added. For example, studies show that menstrual blood is readily distinguishable from peripheral blood, and closely resembles the immune environment of the uterus. Another study found that urinary peptides distinguished patients with moderate to severe endometriosis from healthy controls, and mild disease from severe disease, with sensitivities and specificities ranging from 72% to 88% (Fertil Steril. 2011 Mar 15;95[4]:1261-6).
Other potential sources of diagnostic tests include the endometrial proteome, transcriptome, and methylome, as well as endometrial stem cells, Dr. Giudice said. But for now, surgical diagnosis remains the gold standard, and the World Endometriosis Research Foundation is working to homogenize recording of surgical phenotypic information and laparoscopic specimens to improve data quality, she added.
Dr. Taylor did not report funding sources. He disclosed financial ties to Pfizer, OvaScience AbbVie, Bayer, and Euroscreen. Dr. Giudice acknowledged support from the National Institutes of Health and the UCSF NIH Human Endometrial Tissue and DNA Bank. She disclosed ties to Merck, Pfizer, NextGen Jane, AbbVie, and Juniper Pharmaceuticals.
SALT LAKE CITY – and might soon spare patients from years of misdiagnosis and the costs and burden of diagnostic surgery, according to experts at the annual meeting of the American Society for Reproductive Medicine.
Most notably, expression levels of three microRNAs, 125-b-5p, 451a, and 3613-5p, correctly distinguished patients with chronic endometriosis from healthy controls, said Hugh S. Taylor, MD, of Yale University in New Haven, Conn.
Chronic endometriosis affects about 10% of women and up to half of those with infertility, Dr. Taylor noted. The disease costs the United States at least $22 billion annually and is the second most-common reason for hysterectomy (Reprod Sci. 2009 Apr;16[4]:335-46). Its complexity means that patients face many barriers to diagnosis, particularly young women, who are often told they have “routine” menstrual pain, Dr. Taylor said.
Patients may go up to 12 years and see five or more physicians before they are diagnosed. Clinicians tend to rely on surgical diagnosis, but “there is a reluctance to perform surgery unless there is severe disease,” he added. “The lack of nonsurgical biomarkers contributes significantly to delays in diagnosis and timely intervention.”
These concerns prompted Dr. Taylor and his associates to study microRNAs – the short, noncoding, functional RNAs that promote messenger RNA breakdown or repress its translation. MicroRNA expression varies by tissue type and disease status, and occurs in a variety of body fluids, giving them real potential as nonsurgical biomarkers, Dr. Taylor said. To examine their role in endometriosis, he and his associates performed microarray profiling and confirmatory quantitative real-time polymerase chain reaction testing of serum samples from 24 women with chronic endometriosis and 24 healthy women who served as controls (Fertil Steril. 2016 Aug;106[2]:402-9).
MicroRNA 125b-5p was upregulated the most in endometriosis patients and distinguished patients from controls with a “giant” area under the receiver operating characteristic curve value of 0.974, Dr. Taylor said. Remarkably, this value rose to 1 – meaning that sensitivity and specificity both were 100% – when the researchers added another upregulated microRNA (451a) and a downregulated microRNA (3613-5p) to the model. More work is underway to understand how a test for these microRNAs would perform in larger populations, Dr. Taylor said.
MicroRNAs also are likely to play functional roles in chronic endometriosis and may mediate treatment response, he noted. For example, the microRNA 125b-5p, which is upregulated in endometriosis, increases the expression of inflammatory cytokines and tumor necrosis factor alpha in macrophages, and the aromatase inhibitor letrozole, which reduces pelvic pain in the disease, increases the expression of let-7 microRNAs, with corresponding decreases in the migration of endometrial cells (Fertil Steril. 2016 Sep 1;106[3]:673-80). “Maybe these microRNAs are changing metabolism. Maybe they are changing immune cell activity,” Dr. Taylor said. “I think they are doing a lot more than sitting around waiting for us to discover them.”
None of the 24 patients with endometriosis in his study had taken oral contraceptives in the 3 months prior to serum sampling, Dr. Taylor noted. “We need to look at oral contraception as a potential confounder,” he acknowledged. “If something is independent of the menstrual cycle phase, that is much better than a marker that is dependent on cycle phase.”
Menstrual cycle phase and oral contraceptives are just two of many potential confounders of biomarkers in chronic endometriosis, according to Linda Giudice, MD, PhD, of the University of California, San Francisco. Disease severity, as well as the type, number, and location of lesions and the presence or absence of coexisting inflammatory disorders all can potentially affect the sensitivity and specificity of a marker, she said. Consequently, “there is no single biomarker for chronic endometriosis,” but there are several candidates besides microRNAs, she added. For example, studies show that menstrual blood is readily distinguishable from peripheral blood, and closely resembles the immune environment of the uterus. Another study found that urinary peptides distinguished patients with moderate to severe endometriosis from healthy controls, and mild disease from severe disease, with sensitivities and specificities ranging from 72% to 88% (Fertil Steril. 2011 Mar 15;95[4]:1261-6).
Other potential sources of diagnostic tests include the endometrial proteome, transcriptome, and methylome, as well as endometrial stem cells, Dr. Giudice said. But for now, surgical diagnosis remains the gold standard, and the World Endometriosis Research Foundation is working to homogenize recording of surgical phenotypic information and laparoscopic specimens to improve data quality, she added.
Dr. Taylor did not report funding sources. He disclosed financial ties to Pfizer, OvaScience AbbVie, Bayer, and Euroscreen. Dr. Giudice acknowledged support from the National Institutes of Health and the UCSF NIH Human Endometrial Tissue and DNA Bank. She disclosed ties to Merck, Pfizer, NextGen Jane, AbbVie, and Juniper Pharmaceuticals.
SALT LAKE CITY – and might soon spare patients from years of misdiagnosis and the costs and burden of diagnostic surgery, according to experts at the annual meeting of the American Society for Reproductive Medicine.
Most notably, expression levels of three microRNAs, 125-b-5p, 451a, and 3613-5p, correctly distinguished patients with chronic endometriosis from healthy controls, said Hugh S. Taylor, MD, of Yale University in New Haven, Conn.
Chronic endometriosis affects about 10% of women and up to half of those with infertility, Dr. Taylor noted. The disease costs the United States at least $22 billion annually and is the second most-common reason for hysterectomy (Reprod Sci. 2009 Apr;16[4]:335-46). Its complexity means that patients face many barriers to diagnosis, particularly young women, who are often told they have “routine” menstrual pain, Dr. Taylor said.
Patients may go up to 12 years and see five or more physicians before they are diagnosed. Clinicians tend to rely on surgical diagnosis, but “there is a reluctance to perform surgery unless there is severe disease,” he added. “The lack of nonsurgical biomarkers contributes significantly to delays in diagnosis and timely intervention.”
These concerns prompted Dr. Taylor and his associates to study microRNAs – the short, noncoding, functional RNAs that promote messenger RNA breakdown or repress its translation. MicroRNA expression varies by tissue type and disease status, and occurs in a variety of body fluids, giving them real potential as nonsurgical biomarkers, Dr. Taylor said. To examine their role in endometriosis, he and his associates performed microarray profiling and confirmatory quantitative real-time polymerase chain reaction testing of serum samples from 24 women with chronic endometriosis and 24 healthy women who served as controls (Fertil Steril. 2016 Aug;106[2]:402-9).
MicroRNA 125b-5p was upregulated the most in endometriosis patients and distinguished patients from controls with a “giant” area under the receiver operating characteristic curve value of 0.974, Dr. Taylor said. Remarkably, this value rose to 1 – meaning that sensitivity and specificity both were 100% – when the researchers added another upregulated microRNA (451a) and a downregulated microRNA (3613-5p) to the model. More work is underway to understand how a test for these microRNAs would perform in larger populations, Dr. Taylor said.
MicroRNAs also are likely to play functional roles in chronic endometriosis and may mediate treatment response, he noted. For example, the microRNA 125b-5p, which is upregulated in endometriosis, increases the expression of inflammatory cytokines and tumor necrosis factor alpha in macrophages, and the aromatase inhibitor letrozole, which reduces pelvic pain in the disease, increases the expression of let-7 microRNAs, with corresponding decreases in the migration of endometrial cells (Fertil Steril. 2016 Sep 1;106[3]:673-80). “Maybe these microRNAs are changing metabolism. Maybe they are changing immune cell activity,” Dr. Taylor said. “I think they are doing a lot more than sitting around waiting for us to discover them.”
None of the 24 patients with endometriosis in his study had taken oral contraceptives in the 3 months prior to serum sampling, Dr. Taylor noted. “We need to look at oral contraception as a potential confounder,” he acknowledged. “If something is independent of the menstrual cycle phase, that is much better than a marker that is dependent on cycle phase.”
Menstrual cycle phase and oral contraceptives are just two of many potential confounders of biomarkers in chronic endometriosis, according to Linda Giudice, MD, PhD, of the University of California, San Francisco. Disease severity, as well as the type, number, and location of lesions and the presence or absence of coexisting inflammatory disorders all can potentially affect the sensitivity and specificity of a marker, she said. Consequently, “there is no single biomarker for chronic endometriosis,” but there are several candidates besides microRNAs, she added. For example, studies show that menstrual blood is readily distinguishable from peripheral blood, and closely resembles the immune environment of the uterus. Another study found that urinary peptides distinguished patients with moderate to severe endometriosis from healthy controls, and mild disease from severe disease, with sensitivities and specificities ranging from 72% to 88% (Fertil Steril. 2011 Mar 15;95[4]:1261-6).
Other potential sources of diagnostic tests include the endometrial proteome, transcriptome, and methylome, as well as endometrial stem cells, Dr. Giudice said. But for now, surgical diagnosis remains the gold standard, and the World Endometriosis Research Foundation is working to homogenize recording of surgical phenotypic information and laparoscopic specimens to improve data quality, she added.
Dr. Taylor did not report funding sources. He disclosed financial ties to Pfizer, OvaScience AbbVie, Bayer, and Euroscreen. Dr. Giudice acknowledged support from the National Institutes of Health and the UCSF NIH Human Endometrial Tissue and DNA Bank. She disclosed ties to Merck, Pfizer, NextGen Jane, AbbVie, and Juniper Pharmaceuticals.
EXPERT ANALYSIS FROM 2016 ASRM
Expert tips for working with aspiring LGBT parents
SALT LAKE CITY – An aspiring mother calls the sperm bank she has arranged to work with for insemination. “We can ship sperm across state lines,” she is told – until the clinic learns she has a wife and reverses its policy.
This is just one of many experiences faced by lesbian, gay, bisexual, and transgender (LGBT) individuals on the road to parenthood, Sarah R. Holley, PhD, in the psychology department bat San Francisco (Calif.) State University, said at the annual meeting of the American Society of Reproductive Medicine.
Such experiences harm LGBT persons seeking ART and convince them that clinics only care about their money, according to Dr. Holley. So how to do better? “In order to combat heteronormative bias, we first need to get out of problem-solving mode and offer emotional understanding,” she said. For example, providers should never assume that the uteri and eggs of two female partners are interchangeable, or that a woman who is infertile should not grieve, simply because her wife can conceive.
Providers also should be ready to discuss the downsides of tandem pregnancy with lesbian couples, said Angela K. Lawson, PhD, a psychologist at Northwestern University in Chicago. While few studies have examined specific outcomes, “Each woman has a different chance of a successful pregnancy,” she said. “What if one or both women have complications, or a medically challenged child, or they don’t get pregnant at same time?” By taking turns at IVF, couples can better cope with these potential outcomes, she suggested.
Increasingly, lesbian couples are pursuing “reciprocal in vitro fertilization,” in which one woman contributes her ovum for embryo formation, and her partner undergoes implantation. The correct terms here are “genetic mother” and “gestational mother,” not “egg donor” and “gestational carrier,” which have completely different emotional and legal implications, Dr. Lawson emphasized.
That difference makes it imperative for ART clinics to use properly worded consent forms, said Colleen M. Quinn, JD, of the Adoption and Surrogacy Law Center at Locke & Quinn in Richmond, Va. The U.S. Supreme Court decision recognizing same-sex marriage did not clarify legal parental status; birth certificates do not grant legal parental status or rescind the rights of sperm donors, she said. As a result, lesbian couples who separated have won or lost custody battles based on the wording of ART consent forms, she added. Clinics are ethically obligated to advise their LGBT clients to seek legal counsel and create their own agreements about intended parenthood, she emphasized.
For their own protection, clinics also should insist that couples create a legal property disposition agreement between themselves before creating or storing embryos on their behalf, Ms. Quinn said. “An informed consent document is not sufficient,” she added. “Neither is a disposition agreement with the clinic.”
Prospective transgender parents also merit empathic consideration, said Dr. Lawson. Self-identified women who are biologically male may face “profound sadness” because they cannot carry a pregnancy. Conversely, transgender men who become pregnant in order to fulfill dreams of children may nonetheless experience intense gender dysphoria. In at least one case, a transgender male secluded himself at home throughout his pregnancy to avoid public scrutiny, Dr. Lawson said. In all cases, it helps to identify local sources of support and information and refer patients appropriately, Dr. Holley noted.
The experts also briefly covered prospective gay male fathers, who may pay upward of $100,000 to work with a gestational carrier from an agency, they said. Couples who cannot afford to do so may work with a female friend or seek a gestational carrier in another country, each of which raises questions about parental involvement and legal rights. When same-sex male partners are both donating sperm for embryo formation, “One of the biggest controversies is what to do if only one embryo implants,” Dr. Lawson said. “Will the fathers pursue DNA testing of that child? This gets us into issues of intentional unknowing and secrecy, and we know that secrecy can destroy families, whereas privacy typically doesn’t. It’s in the best interest of children to know the story of their parentage.”
None of the experts acknowledged funding sources. Ms. Quinn had no disclosures.
SALT LAKE CITY – An aspiring mother calls the sperm bank she has arranged to work with for insemination. “We can ship sperm across state lines,” she is told – until the clinic learns she has a wife and reverses its policy.
This is just one of many experiences faced by lesbian, gay, bisexual, and transgender (LGBT) individuals on the road to parenthood, Sarah R. Holley, PhD, in the psychology department bat San Francisco (Calif.) State University, said at the annual meeting of the American Society of Reproductive Medicine.
Such experiences harm LGBT persons seeking ART and convince them that clinics only care about their money, according to Dr. Holley. So how to do better? “In order to combat heteronormative bias, we first need to get out of problem-solving mode and offer emotional understanding,” she said. For example, providers should never assume that the uteri and eggs of two female partners are interchangeable, or that a woman who is infertile should not grieve, simply because her wife can conceive.
Providers also should be ready to discuss the downsides of tandem pregnancy with lesbian couples, said Angela K. Lawson, PhD, a psychologist at Northwestern University in Chicago. While few studies have examined specific outcomes, “Each woman has a different chance of a successful pregnancy,” she said. “What if one or both women have complications, or a medically challenged child, or they don’t get pregnant at same time?” By taking turns at IVF, couples can better cope with these potential outcomes, she suggested.
Increasingly, lesbian couples are pursuing “reciprocal in vitro fertilization,” in which one woman contributes her ovum for embryo formation, and her partner undergoes implantation. The correct terms here are “genetic mother” and “gestational mother,” not “egg donor” and “gestational carrier,” which have completely different emotional and legal implications, Dr. Lawson emphasized.
That difference makes it imperative for ART clinics to use properly worded consent forms, said Colleen M. Quinn, JD, of the Adoption and Surrogacy Law Center at Locke & Quinn in Richmond, Va. The U.S. Supreme Court decision recognizing same-sex marriage did not clarify legal parental status; birth certificates do not grant legal parental status or rescind the rights of sperm donors, she said. As a result, lesbian couples who separated have won or lost custody battles based on the wording of ART consent forms, she added. Clinics are ethically obligated to advise their LGBT clients to seek legal counsel and create their own agreements about intended parenthood, she emphasized.
For their own protection, clinics also should insist that couples create a legal property disposition agreement between themselves before creating or storing embryos on their behalf, Ms. Quinn said. “An informed consent document is not sufficient,” she added. “Neither is a disposition agreement with the clinic.”
Prospective transgender parents also merit empathic consideration, said Dr. Lawson. Self-identified women who are biologically male may face “profound sadness” because they cannot carry a pregnancy. Conversely, transgender men who become pregnant in order to fulfill dreams of children may nonetheless experience intense gender dysphoria. In at least one case, a transgender male secluded himself at home throughout his pregnancy to avoid public scrutiny, Dr. Lawson said. In all cases, it helps to identify local sources of support and information and refer patients appropriately, Dr. Holley noted.
The experts also briefly covered prospective gay male fathers, who may pay upward of $100,000 to work with a gestational carrier from an agency, they said. Couples who cannot afford to do so may work with a female friend or seek a gestational carrier in another country, each of which raises questions about parental involvement and legal rights. When same-sex male partners are both donating sperm for embryo formation, “One of the biggest controversies is what to do if only one embryo implants,” Dr. Lawson said. “Will the fathers pursue DNA testing of that child? This gets us into issues of intentional unknowing and secrecy, and we know that secrecy can destroy families, whereas privacy typically doesn’t. It’s in the best interest of children to know the story of their parentage.”
None of the experts acknowledged funding sources. Ms. Quinn had no disclosures.
SALT LAKE CITY – An aspiring mother calls the sperm bank she has arranged to work with for insemination. “We can ship sperm across state lines,” she is told – until the clinic learns she has a wife and reverses its policy.
This is just one of many experiences faced by lesbian, gay, bisexual, and transgender (LGBT) individuals on the road to parenthood, Sarah R. Holley, PhD, in the psychology department bat San Francisco (Calif.) State University, said at the annual meeting of the American Society of Reproductive Medicine.
Such experiences harm LGBT persons seeking ART and convince them that clinics only care about their money, according to Dr. Holley. So how to do better? “In order to combat heteronormative bias, we first need to get out of problem-solving mode and offer emotional understanding,” she said. For example, providers should never assume that the uteri and eggs of two female partners are interchangeable, or that a woman who is infertile should not grieve, simply because her wife can conceive.
Providers also should be ready to discuss the downsides of tandem pregnancy with lesbian couples, said Angela K. Lawson, PhD, a psychologist at Northwestern University in Chicago. While few studies have examined specific outcomes, “Each woman has a different chance of a successful pregnancy,” she said. “What if one or both women have complications, or a medically challenged child, or they don’t get pregnant at same time?” By taking turns at IVF, couples can better cope with these potential outcomes, she suggested.
Increasingly, lesbian couples are pursuing “reciprocal in vitro fertilization,” in which one woman contributes her ovum for embryo formation, and her partner undergoes implantation. The correct terms here are “genetic mother” and “gestational mother,” not “egg donor” and “gestational carrier,” which have completely different emotional and legal implications, Dr. Lawson emphasized.
That difference makes it imperative for ART clinics to use properly worded consent forms, said Colleen M. Quinn, JD, of the Adoption and Surrogacy Law Center at Locke & Quinn in Richmond, Va. The U.S. Supreme Court decision recognizing same-sex marriage did not clarify legal parental status; birth certificates do not grant legal parental status or rescind the rights of sperm donors, she said. As a result, lesbian couples who separated have won or lost custody battles based on the wording of ART consent forms, she added. Clinics are ethically obligated to advise their LGBT clients to seek legal counsel and create their own agreements about intended parenthood, she emphasized.
For their own protection, clinics also should insist that couples create a legal property disposition agreement between themselves before creating or storing embryos on their behalf, Ms. Quinn said. “An informed consent document is not sufficient,” she added. “Neither is a disposition agreement with the clinic.”
Prospective transgender parents also merit empathic consideration, said Dr. Lawson. Self-identified women who are biologically male may face “profound sadness” because they cannot carry a pregnancy. Conversely, transgender men who become pregnant in order to fulfill dreams of children may nonetheless experience intense gender dysphoria. In at least one case, a transgender male secluded himself at home throughout his pregnancy to avoid public scrutiny, Dr. Lawson said. In all cases, it helps to identify local sources of support and information and refer patients appropriately, Dr. Holley noted.
The experts also briefly covered prospective gay male fathers, who may pay upward of $100,000 to work with a gestational carrier from an agency, they said. Couples who cannot afford to do so may work with a female friend or seek a gestational carrier in another country, each of which raises questions about parental involvement and legal rights. When same-sex male partners are both donating sperm for embryo formation, “One of the biggest controversies is what to do if only one embryo implants,” Dr. Lawson said. “Will the fathers pursue DNA testing of that child? This gets us into issues of intentional unknowing and secrecy, and we know that secrecy can destroy families, whereas privacy typically doesn’t. It’s in the best interest of children to know the story of their parentage.”
None of the experts acknowledged funding sources. Ms. Quinn had no disclosures.
EXPERT ANALYSIS FROM ASRM 2016
Obese IVF patients need higher HCG trigger dose
SALT LAKE CITY – Women who are obese should receive more than 5,000 IU of human chorionic gonadotropin (HCG) to trigger final oocyte maturation during in vitro fertilization, findings of a retrospective cohort study suggest.
Fully 23% of obese women had low beta-HCG levels the day after receiving a 5,000 IU HCG trigger dose, compared with 1% of non-obese women (odds ratio, 21.4; 95% confidence interval, 15.0-30.4), reported Mohamad Irani, MD, and his associates from Cornell University, New York. In contrast, 10,000 IU HCG triggered adequate beta-HCG levels in 81% of obese patients with a BMI of 30-40 kg/m2, and in 90% of those whose BMI exceeded 40 kg/m2.
Low beta-HCG levels decreased the chances of oocyte maturation, fertilization, and live birth in the study. “Patients’ BMI should be taken into consideration when determining the dose of HCG trigger,” the investigators concluded in a poster presented at the annual meeting of the American Society for Reproductive Medicine.
Patients with hypothalamic amenorrhea or who are undergoing stimulation with a gonadotropin-releasing hormone (GnRH) agonist are not candidates for a GnRH-agonist trigger and therefore need to receive HCG instead, the researchers noted. To understand how the dose of HCG affects the chances of final oocyte maturation, they studied 19,084 HCG trigger recipients at their center between 2004 and 2013.
By protocol, patients received 10,000 IU HCG if their serum estradiol (E2) level was less than 1,500 pg/mL on the day of trigger; 5,000 IU if it measured 1,501-2,500 pg/mL; 4,000 IU if it was 2,501-3,000 pg/mL; and 3,300 IU if it exceeded 3,000 pg/mL.
The day after HCG trigger, 18,666 patients had beta-HCG levels of at least 50 mIU/mL, while 418 patients had low beta-HCG levels of less than 50 mIU/mL. A comparison of the two groups showed that low beta-HCG was associated with significantly lower rates of oocyte maturation (77% vs. 81%; P less than .001) and fertilization (63% vs. 72%; P less than .001). It was also associated with more than a 30% lower chance of a live birth (adjusted OR, 0.67; 95% CI, 0.5-0.8), even after accounting for age, and the stage and number of embryos transferred.
The researchers also examined response to HCG trigger among non-obese patients. Among patients who were overweight (BMI 25 to 30 kg/m2), the chances of a low beta-HCG level the day after trigger were 14% when the HCG dose was 3,300 IU, 12.5% when it was 4,000 IU, 4.3% when it was 5,000 IU, and 0.4% when it was 10,000 IU.
Among healthy-weight patients (BMI 18.5-25 kg/m2), low beta-HCG levels occurred 3.6% of the time when the HCG dose was 3,300 IU, 2.3% of the time when it was 4,000 IU, 0.6% of the time when it was 5,000 IU, and 0.08% of the time when it was 10,000 IU. Notably, these same doses triggered adequate beta-HCG levels in all 660 patients who were underweight (BMI less than 18.5 kg/m2), the researchers reported.
Dr. Irani reported having no relevant financial disclosures.
SALT LAKE CITY – Women who are obese should receive more than 5,000 IU of human chorionic gonadotropin (HCG) to trigger final oocyte maturation during in vitro fertilization, findings of a retrospective cohort study suggest.
Fully 23% of obese women had low beta-HCG levels the day after receiving a 5,000 IU HCG trigger dose, compared with 1% of non-obese women (odds ratio, 21.4; 95% confidence interval, 15.0-30.4), reported Mohamad Irani, MD, and his associates from Cornell University, New York. In contrast, 10,000 IU HCG triggered adequate beta-HCG levels in 81% of obese patients with a BMI of 30-40 kg/m2, and in 90% of those whose BMI exceeded 40 kg/m2.
Low beta-HCG levels decreased the chances of oocyte maturation, fertilization, and live birth in the study. “Patients’ BMI should be taken into consideration when determining the dose of HCG trigger,” the investigators concluded in a poster presented at the annual meeting of the American Society for Reproductive Medicine.
Patients with hypothalamic amenorrhea or who are undergoing stimulation with a gonadotropin-releasing hormone (GnRH) agonist are not candidates for a GnRH-agonist trigger and therefore need to receive HCG instead, the researchers noted. To understand how the dose of HCG affects the chances of final oocyte maturation, they studied 19,084 HCG trigger recipients at their center between 2004 and 2013.
By protocol, patients received 10,000 IU HCG if their serum estradiol (E2) level was less than 1,500 pg/mL on the day of trigger; 5,000 IU if it measured 1,501-2,500 pg/mL; 4,000 IU if it was 2,501-3,000 pg/mL; and 3,300 IU if it exceeded 3,000 pg/mL.
The day after HCG trigger, 18,666 patients had beta-HCG levels of at least 50 mIU/mL, while 418 patients had low beta-HCG levels of less than 50 mIU/mL. A comparison of the two groups showed that low beta-HCG was associated with significantly lower rates of oocyte maturation (77% vs. 81%; P less than .001) and fertilization (63% vs. 72%; P less than .001). It was also associated with more than a 30% lower chance of a live birth (adjusted OR, 0.67; 95% CI, 0.5-0.8), even after accounting for age, and the stage and number of embryos transferred.
The researchers also examined response to HCG trigger among non-obese patients. Among patients who were overweight (BMI 25 to 30 kg/m2), the chances of a low beta-HCG level the day after trigger were 14% when the HCG dose was 3,300 IU, 12.5% when it was 4,000 IU, 4.3% when it was 5,000 IU, and 0.4% when it was 10,000 IU.
Among healthy-weight patients (BMI 18.5-25 kg/m2), low beta-HCG levels occurred 3.6% of the time when the HCG dose was 3,300 IU, 2.3% of the time when it was 4,000 IU, 0.6% of the time when it was 5,000 IU, and 0.08% of the time when it was 10,000 IU. Notably, these same doses triggered adequate beta-HCG levels in all 660 patients who were underweight (BMI less than 18.5 kg/m2), the researchers reported.
Dr. Irani reported having no relevant financial disclosures.
SALT LAKE CITY – Women who are obese should receive more than 5,000 IU of human chorionic gonadotropin (HCG) to trigger final oocyte maturation during in vitro fertilization, findings of a retrospective cohort study suggest.
Fully 23% of obese women had low beta-HCG levels the day after receiving a 5,000 IU HCG trigger dose, compared with 1% of non-obese women (odds ratio, 21.4; 95% confidence interval, 15.0-30.4), reported Mohamad Irani, MD, and his associates from Cornell University, New York. In contrast, 10,000 IU HCG triggered adequate beta-HCG levels in 81% of obese patients with a BMI of 30-40 kg/m2, and in 90% of those whose BMI exceeded 40 kg/m2.
Low beta-HCG levels decreased the chances of oocyte maturation, fertilization, and live birth in the study. “Patients’ BMI should be taken into consideration when determining the dose of HCG trigger,” the investigators concluded in a poster presented at the annual meeting of the American Society for Reproductive Medicine.
Patients with hypothalamic amenorrhea or who are undergoing stimulation with a gonadotropin-releasing hormone (GnRH) agonist are not candidates for a GnRH-agonist trigger and therefore need to receive HCG instead, the researchers noted. To understand how the dose of HCG affects the chances of final oocyte maturation, they studied 19,084 HCG trigger recipients at their center between 2004 and 2013.
By protocol, patients received 10,000 IU HCG if their serum estradiol (E2) level was less than 1,500 pg/mL on the day of trigger; 5,000 IU if it measured 1,501-2,500 pg/mL; 4,000 IU if it was 2,501-3,000 pg/mL; and 3,300 IU if it exceeded 3,000 pg/mL.
The day after HCG trigger, 18,666 patients had beta-HCG levels of at least 50 mIU/mL, while 418 patients had low beta-HCG levels of less than 50 mIU/mL. A comparison of the two groups showed that low beta-HCG was associated with significantly lower rates of oocyte maturation (77% vs. 81%; P less than .001) and fertilization (63% vs. 72%; P less than .001). It was also associated with more than a 30% lower chance of a live birth (adjusted OR, 0.67; 95% CI, 0.5-0.8), even after accounting for age, and the stage and number of embryos transferred.
The researchers also examined response to HCG trigger among non-obese patients. Among patients who were overweight (BMI 25 to 30 kg/m2), the chances of a low beta-HCG level the day after trigger were 14% when the HCG dose was 3,300 IU, 12.5% when it was 4,000 IU, 4.3% when it was 5,000 IU, and 0.4% when it was 10,000 IU.
Among healthy-weight patients (BMI 18.5-25 kg/m2), low beta-HCG levels occurred 3.6% of the time when the HCG dose was 3,300 IU, 2.3% of the time when it was 4,000 IU, 0.6% of the time when it was 5,000 IU, and 0.08% of the time when it was 10,000 IU. Notably, these same doses triggered adequate beta-HCG levels in all 660 patients who were underweight (BMI less than 18.5 kg/m2), the researchers reported.
Dr. Irani reported having no relevant financial disclosures.
AT 2016 ASRM
Key clinical point:
Major finding: Fully 23% of obese individuals had low beta-HCG levels the day after receiving a 5,000 IU HCG trigger, compared with 1% of non-obese patients (OR, 21.4).
Data source: A retrospective cohort study of 18,666 patients with beta-HCG levels of at least 50 mIU/mL and 418 patients with “low” levels of less than 50 mIU/mL the day after HCG trigger.
Disclosures: Dr. Irani reported having no relevant financial disclosures.
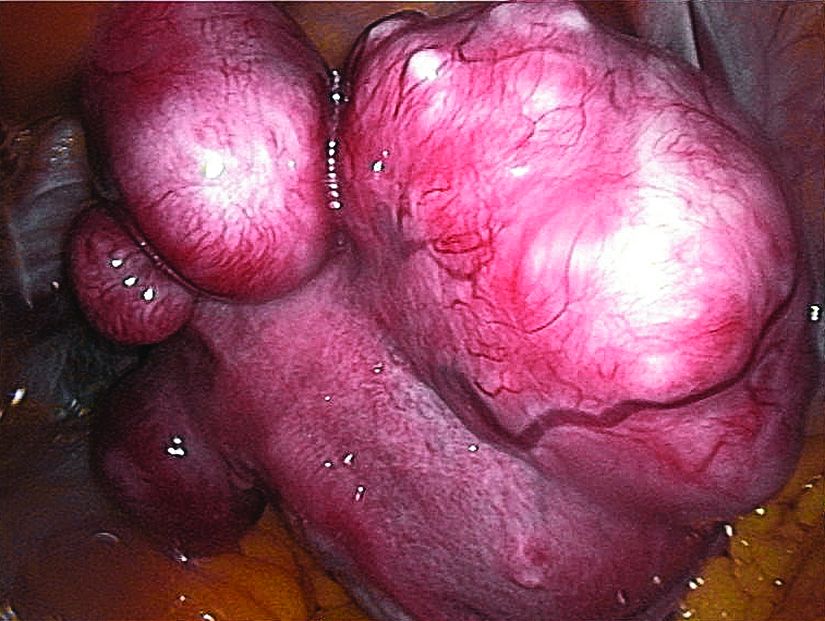
Ulipristal acetate meets primary endpoint in pivotal uterine fibroids trial
SALT LAKE CITY – The selective progesterone receptor modulator ulipristal acetate significantly reduced bleeding associated with fibroids in VENUS-I, a pivotal phase III trial of 147 premenopausal women.
A total of 58% of patients who took 10 mg ulipristal acetate per day had no bleeding except spotting during the last 35 days of treatment, compared with 2% of the placebo group (P less than .0001), James Simon, MD, said at the annual meeting of the American Society for Reproductive Medicine. Forty-seven percent of patients who took 5 mg ulipristal acetate per day also met the primary endpoint (P less than .0001, compared with placebo), he said.
The most common treatment-related adverse effect was hypertension, which affected 8% of women in the 10-mg group and 4% of women in the 5-mg group, he added during the late-breaking oral presentation.
Ulipristal acetate is currently approved in the United States as an emergency contraceptive, but is marketed for treating symptomatic fibroids in Canada and Europe. The drug reduced bleeding in about 90% of patients in the European trials (N Engl J Med. 2012;366:409-20; Fertil Steril. 2014 Jun;101[6]:1565-73).
The VENUS-I trial included premenopausal women aged 18-50 years who had experienced 22-35 days of bleeding during at least four of their last six menstrual cycles, with at least 80 mL menstrual blood loss, and at least one fibroid confirmed by transvaginal ultrasound.
“The women in our study were more severely affected, in terms of the amount of bleeding and in terms of fibroid size and uterine size, than what was reported in the European trials,” Dr. Simon said.
The average age of the patients was 41 years, and 69% were African-American, reflecting the disproportionate burden of severely symptomatic fibroids in this group, he said.
Patients were randomly assigned to oral treatment with either placebo or 10 mg or 5 mg ulipristal acetate for 12 weeks, followed by a 12-week drug-free observation period. The primary endpoint was amenorrhea, not including spotting, during the last 35 consecutive days of treatment.
The 10-mg group was 49 times more likely to reach this endpoint than was the placebo arm (P less than .0001), even after the researchers controlled for multiple potential confounders, Dr. Simon reported. The hazard ratio for the 5-mg group was also highly statistically significant at 35.5 (P less than .0001).
“Almost all patients who achieved amenorrhea in the ulipristal acetate groups did so by day 11,” Dr. Simon said.
Rates of amenorrhea from day 11 through the end of treatment were 58% in the 10-mg group, 43% in the 5-mg group, and 0% in the placebo group (P less than .0001 for differences among groups). Patients who received ulipristal acetate also reported significantly greater improvements on the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire than did the placebo group.
No patients stopped treatment because of adverse effects. Of the six patients who developed hypertension while on ulipristal acetate, five had a history of high blood pressure, and the increases were generally “slight,” Dr. Simon said. The other common treatment-emergent adverse effects included increased creatinine phosphokinase, hot flashes, acne, and nausea.
Blinded pathologists interpreted endometrial biopsies at baseline, the end of treatment, and at the end of the drug-free observation period. These revealed no cases of atypical endometrial hyperplasia or malignancy, and no baseline increases in rates of progesterone receptor modulator–associated endometrial changes, Dr. Simon said. One patient developed endometrial hyperplasia without atypia at the end of treatment, which resolved by the end of the 12-week drug-free observation period.
VENUS-I is one of two pivotal trials of ulipristal acetate for the treatment of uterine fibroids in the United States. Results from the second trial, VENUS-II, are expected in 2017.
The VENUS-I trial was supported by Allergan and Gedeon Richter. Dr. Simon reported ties to numerous other pharmaceutical companies, but not to Allergan or Gedeon Richter.
SALT LAKE CITY – The selective progesterone receptor modulator ulipristal acetate significantly reduced bleeding associated with fibroids in VENUS-I, a pivotal phase III trial of 147 premenopausal women.
A total of 58% of patients who took 10 mg ulipristal acetate per day had no bleeding except spotting during the last 35 days of treatment, compared with 2% of the placebo group (P less than .0001), James Simon, MD, said at the annual meeting of the American Society for Reproductive Medicine. Forty-seven percent of patients who took 5 mg ulipristal acetate per day also met the primary endpoint (P less than .0001, compared with placebo), he said.
The most common treatment-related adverse effect was hypertension, which affected 8% of women in the 10-mg group and 4% of women in the 5-mg group, he added during the late-breaking oral presentation.
Ulipristal acetate is currently approved in the United States as an emergency contraceptive, but is marketed for treating symptomatic fibroids in Canada and Europe. The drug reduced bleeding in about 90% of patients in the European trials (N Engl J Med. 2012;366:409-20; Fertil Steril. 2014 Jun;101[6]:1565-73).
The VENUS-I trial included premenopausal women aged 18-50 years who had experienced 22-35 days of bleeding during at least four of their last six menstrual cycles, with at least 80 mL menstrual blood loss, and at least one fibroid confirmed by transvaginal ultrasound.
“The women in our study were more severely affected, in terms of the amount of bleeding and in terms of fibroid size and uterine size, than what was reported in the European trials,” Dr. Simon said.
The average age of the patients was 41 years, and 69% were African-American, reflecting the disproportionate burden of severely symptomatic fibroids in this group, he said.
Patients were randomly assigned to oral treatment with either placebo or 10 mg or 5 mg ulipristal acetate for 12 weeks, followed by a 12-week drug-free observation period. The primary endpoint was amenorrhea, not including spotting, during the last 35 consecutive days of treatment.
The 10-mg group was 49 times more likely to reach this endpoint than was the placebo arm (P less than .0001), even after the researchers controlled for multiple potential confounders, Dr. Simon reported. The hazard ratio for the 5-mg group was also highly statistically significant at 35.5 (P less than .0001).
“Almost all patients who achieved amenorrhea in the ulipristal acetate groups did so by day 11,” Dr. Simon said.
Rates of amenorrhea from day 11 through the end of treatment were 58% in the 10-mg group, 43% in the 5-mg group, and 0% in the placebo group (P less than .0001 for differences among groups). Patients who received ulipristal acetate also reported significantly greater improvements on the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire than did the placebo group.
No patients stopped treatment because of adverse effects. Of the six patients who developed hypertension while on ulipristal acetate, five had a history of high blood pressure, and the increases were generally “slight,” Dr. Simon said. The other common treatment-emergent adverse effects included increased creatinine phosphokinase, hot flashes, acne, and nausea.
Blinded pathologists interpreted endometrial biopsies at baseline, the end of treatment, and at the end of the drug-free observation period. These revealed no cases of atypical endometrial hyperplasia or malignancy, and no baseline increases in rates of progesterone receptor modulator–associated endometrial changes, Dr. Simon said. One patient developed endometrial hyperplasia without atypia at the end of treatment, which resolved by the end of the 12-week drug-free observation period.
VENUS-I is one of two pivotal trials of ulipristal acetate for the treatment of uterine fibroids in the United States. Results from the second trial, VENUS-II, are expected in 2017.
The VENUS-I trial was supported by Allergan and Gedeon Richter. Dr. Simon reported ties to numerous other pharmaceutical companies, but not to Allergan or Gedeon Richter.
SALT LAKE CITY – The selective progesterone receptor modulator ulipristal acetate significantly reduced bleeding associated with fibroids in VENUS-I, a pivotal phase III trial of 147 premenopausal women.
A total of 58% of patients who took 10 mg ulipristal acetate per day had no bleeding except spotting during the last 35 days of treatment, compared with 2% of the placebo group (P less than .0001), James Simon, MD, said at the annual meeting of the American Society for Reproductive Medicine. Forty-seven percent of patients who took 5 mg ulipristal acetate per day also met the primary endpoint (P less than .0001, compared with placebo), he said.
The most common treatment-related adverse effect was hypertension, which affected 8% of women in the 10-mg group and 4% of women in the 5-mg group, he added during the late-breaking oral presentation.
Ulipristal acetate is currently approved in the United States as an emergency contraceptive, but is marketed for treating symptomatic fibroids in Canada and Europe. The drug reduced bleeding in about 90% of patients in the European trials (N Engl J Med. 2012;366:409-20; Fertil Steril. 2014 Jun;101[6]:1565-73).
The VENUS-I trial included premenopausal women aged 18-50 years who had experienced 22-35 days of bleeding during at least four of their last six menstrual cycles, with at least 80 mL menstrual blood loss, and at least one fibroid confirmed by transvaginal ultrasound.
“The women in our study were more severely affected, in terms of the amount of bleeding and in terms of fibroid size and uterine size, than what was reported in the European trials,” Dr. Simon said.
The average age of the patients was 41 years, and 69% were African-American, reflecting the disproportionate burden of severely symptomatic fibroids in this group, he said.
Patients were randomly assigned to oral treatment with either placebo or 10 mg or 5 mg ulipristal acetate for 12 weeks, followed by a 12-week drug-free observation period. The primary endpoint was amenorrhea, not including spotting, during the last 35 consecutive days of treatment.
The 10-mg group was 49 times more likely to reach this endpoint than was the placebo arm (P less than .0001), even after the researchers controlled for multiple potential confounders, Dr. Simon reported. The hazard ratio for the 5-mg group was also highly statistically significant at 35.5 (P less than .0001).
“Almost all patients who achieved amenorrhea in the ulipristal acetate groups did so by day 11,” Dr. Simon said.
Rates of amenorrhea from day 11 through the end of treatment were 58% in the 10-mg group, 43% in the 5-mg group, and 0% in the placebo group (P less than .0001 for differences among groups). Patients who received ulipristal acetate also reported significantly greater improvements on the Uterine Fibroid Symptom and Quality of Life (UFS-QOL) questionnaire than did the placebo group.
No patients stopped treatment because of adverse effects. Of the six patients who developed hypertension while on ulipristal acetate, five had a history of high blood pressure, and the increases were generally “slight,” Dr. Simon said. The other common treatment-emergent adverse effects included increased creatinine phosphokinase, hot flashes, acne, and nausea.
Blinded pathologists interpreted endometrial biopsies at baseline, the end of treatment, and at the end of the drug-free observation period. These revealed no cases of atypical endometrial hyperplasia or malignancy, and no baseline increases in rates of progesterone receptor modulator–associated endometrial changes, Dr. Simon said. One patient developed endometrial hyperplasia without atypia at the end of treatment, which resolved by the end of the 12-week drug-free observation period.
VENUS-I is one of two pivotal trials of ulipristal acetate for the treatment of uterine fibroids in the United States. Results from the second trial, VENUS-II, are expected in 2017.
The VENUS-I trial was supported by Allergan and Gedeon Richter. Dr. Simon reported ties to numerous other pharmaceutical companies, but not to Allergan or Gedeon Richter.
AT 2016 ASRM
Key clinical point:
Major finding: Rates of amenorrhea during the last 35 consecutive days of treatment were 58% in the 10-mg group, compared with 2% in the placebo group (P less than .0001).
Data source: A randomized, double-blind trial of 147 premenopausal women with uterine fibroids and an average of 80 mL menstrual blood loss.
Disclosures: VENUS-I was supported by Allergan and Gedeon Richter. Dr. Simon reported ties to numerous other pharmaceutical companies, but not to Allergan or Gedeon Richter.
Metabolic syndrome predicts cardiovascular events in HBV infection
Metabolic syndrome was associated with a fourfold rise in cardiovascular events among patients with chronic hepatitis B virus infection, according to a prospective cohort study published in Hepatology.
Over a median of 7.3 years of follow-up, 8% of patients with metabolic syndrome developed ischemic or hemorrhagic stroke, acute coronary syndrome, or congestive heart failure, or underwent revascularization, compared with 2% of patients without metabolic syndrome (P less than .0001), reported Jenny Yeuk-Ki Cheng, MD, and her associates at The Chinese University of Hong Kong.
But it was liver stiffness measure (LSM), not metabolic syndrome, that predicted hepatic events (hazard ratio, 1.6; 95% confidence interval, 1.0 to 2.5) and death (HR, 1.9; 95% CI, 1.1 to 3.2), the investigators reported (Hepatology. 2016 Sep 29. doi: 10.1002/hep.28778).
Their study included 1,466 patients with chronic HBV infection who averaged 46 years of age, with an average baseline LSM of 8.4 kPa (standard deviation, 6.3 kPa). A total of 188 patients (12.8%) had metabolic syndrome at baseline, defined as at least three of the following five factors: central obesity, hypertriglyceridemia, low high-density lipoprotein cholesterol, hypertension, and type 2 diabetes mellitus or fasting hyperglycemia.
In all, 44 patients (3.0%) developed cardiovascular events during follow-up, while 93 (6.3%) developed cirrhotic events and hepatocellular carcinoma, and 70 (4.8%) died. Patients whose LSM exceeded 8.0 kPa at baseline had a significantly higher cumulative risk of hepatic events over the next 8 years than did patients with lower baseline LSM (12.3% versus 3%; P less than .001).
But high LSM “had no impact on cardiovascular events,” just as metabolic syndrome did not increase the risk of hepatic events or death, the investigators said. The study, the first to evaluate this group of clinical correlates in HBV-infected patients, highlights the need to monitor their metabolic risk factors over time, they concluded.
The researchers reported having no funding sources. Dr. Cheng had no relevant financial disclosures, although other coauthors reported multiple relationships with pharmaceutical and device firms.
Metabolic syndrome was associated with a fourfold rise in cardiovascular events among patients with chronic hepatitis B virus infection, according to a prospective cohort study published in Hepatology.
Over a median of 7.3 years of follow-up, 8% of patients with metabolic syndrome developed ischemic or hemorrhagic stroke, acute coronary syndrome, or congestive heart failure, or underwent revascularization, compared with 2% of patients without metabolic syndrome (P less than .0001), reported Jenny Yeuk-Ki Cheng, MD, and her associates at The Chinese University of Hong Kong.
But it was liver stiffness measure (LSM), not metabolic syndrome, that predicted hepatic events (hazard ratio, 1.6; 95% confidence interval, 1.0 to 2.5) and death (HR, 1.9; 95% CI, 1.1 to 3.2), the investigators reported (Hepatology. 2016 Sep 29. doi: 10.1002/hep.28778).
Their study included 1,466 patients with chronic HBV infection who averaged 46 years of age, with an average baseline LSM of 8.4 kPa (standard deviation, 6.3 kPa). A total of 188 patients (12.8%) had metabolic syndrome at baseline, defined as at least three of the following five factors: central obesity, hypertriglyceridemia, low high-density lipoprotein cholesterol, hypertension, and type 2 diabetes mellitus or fasting hyperglycemia.
In all, 44 patients (3.0%) developed cardiovascular events during follow-up, while 93 (6.3%) developed cirrhotic events and hepatocellular carcinoma, and 70 (4.8%) died. Patients whose LSM exceeded 8.0 kPa at baseline had a significantly higher cumulative risk of hepatic events over the next 8 years than did patients with lower baseline LSM (12.3% versus 3%; P less than .001).
But high LSM “had no impact on cardiovascular events,” just as metabolic syndrome did not increase the risk of hepatic events or death, the investigators said. The study, the first to evaluate this group of clinical correlates in HBV-infected patients, highlights the need to monitor their metabolic risk factors over time, they concluded.
The researchers reported having no funding sources. Dr. Cheng had no relevant financial disclosures, although other coauthors reported multiple relationships with pharmaceutical and device firms.
Metabolic syndrome was associated with a fourfold rise in cardiovascular events among patients with chronic hepatitis B virus infection, according to a prospective cohort study published in Hepatology.
Over a median of 7.3 years of follow-up, 8% of patients with metabolic syndrome developed ischemic or hemorrhagic stroke, acute coronary syndrome, or congestive heart failure, or underwent revascularization, compared with 2% of patients without metabolic syndrome (P less than .0001), reported Jenny Yeuk-Ki Cheng, MD, and her associates at The Chinese University of Hong Kong.
But it was liver stiffness measure (LSM), not metabolic syndrome, that predicted hepatic events (hazard ratio, 1.6; 95% confidence interval, 1.0 to 2.5) and death (HR, 1.9; 95% CI, 1.1 to 3.2), the investigators reported (Hepatology. 2016 Sep 29. doi: 10.1002/hep.28778).
Their study included 1,466 patients with chronic HBV infection who averaged 46 years of age, with an average baseline LSM of 8.4 kPa (standard deviation, 6.3 kPa). A total of 188 patients (12.8%) had metabolic syndrome at baseline, defined as at least three of the following five factors: central obesity, hypertriglyceridemia, low high-density lipoprotein cholesterol, hypertension, and type 2 diabetes mellitus or fasting hyperglycemia.
In all, 44 patients (3.0%) developed cardiovascular events during follow-up, while 93 (6.3%) developed cirrhotic events and hepatocellular carcinoma, and 70 (4.8%) died. Patients whose LSM exceeded 8.0 kPa at baseline had a significantly higher cumulative risk of hepatic events over the next 8 years than did patients with lower baseline LSM (12.3% versus 3%; P less than .001).
But high LSM “had no impact on cardiovascular events,” just as metabolic syndrome did not increase the risk of hepatic events or death, the investigators said. The study, the first to evaluate this group of clinical correlates in HBV-infected patients, highlights the need to monitor their metabolic risk factors over time, they concluded.
The researchers reported having no funding sources. Dr. Cheng had no relevant financial disclosures, although other coauthors reported multiple relationships with pharmaceutical and device firms.
Key clinical point: Metabolic syndrome significantly increases the risk of cardiovascular events in patients with chronic hepatitis B virus infection.
Major finding: In all, 8% of patients with metabolic syndrome had a cardiovascular event, compared with 2% of patients without metabolic syndrome (P less than .0001).
Data source: A single-center prospective cohort study of 1,466 patients with chronic hepatitis B virus infection.
Disclosures: The researchers reported having no funding sources. Dr. Cheng had no relevant financial disclosures, although other coauthors reported multiple relationships with pharmaceutical and device firms.
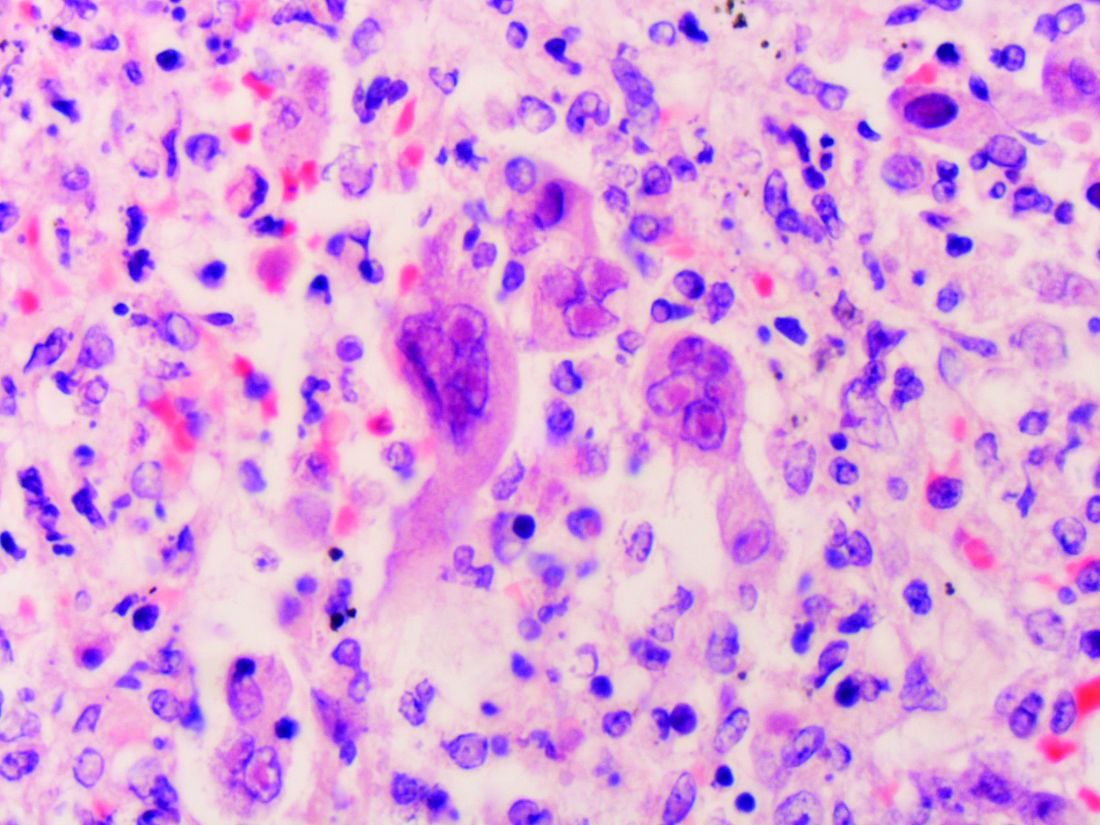
Healthy relatives of IBD patients have intestinal dysbiosis
Healthy first-degree relatives of children and adolescents with inflammatory bowel disease had intestinal dysbiosis and an altered intestinal metabolome that correlated with one another and with the disease state, researchers reported in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
These findings suggest the existence of a “high-risk microbiome/metabolome” that may increase susceptibility to inflammatory bowel disease (IBD), Jonathan Jacobs, MD, of the University of California, Los Angeles, reported with his associates. Among the healthy relatives with dysbiosis, nearly one-third also had elevated levels of fecal calprotectin, a marker of intestinal inflammation that has been previously reported in family members of patients with ulcerative colitis, the researchers noted. “If validated, prospective identification of [high-risk individuals] creates the opportunity to prevent disease development by targeting the dysbiosis and/or its metabolic consequences in the intestine,” they wrote.
Participants in the study fell into one of two “operational taxonomic units” based on their microbial communities, the researchers said. The second taxonomic unit not only was associated with IBD, “but irrespective of disease status, had lower microbial diversity and characteristic shifts in microbial composition, including increased Enterobacteriaceae, consistent with dysbiosis.” Among 21 families in the study, 19 had at least one member in this group. Furthermore, tests of an independent pediatric cohort revealed this same taxonomic group characterized by low microbial diversity and associated with IBD.
Participants also fell into two distinct metabotypes, one of which was associated with IBD and had increased levels of bile acids and amino acid derivatives previously linked to Crohn’s disease, as well as elevated levels of taurine, tryptophan, serinyl tryptophan, and adrenic acid, an omega-6 fatty acid, the researchers said. Taxonomic units and metabolic groups correlated highly with one another among both IBD patients and healthy relatives (P = 3 × 10-8), suggesting a “functional relationship between the microbiome and the metabolome,” the investigators said. Additionally, although most healthy relatives had normal fecal calprotectin levels, those in the second operational taxonomic unit had about sixfold greater odds of elevated calprotectin, compared with those in the first group (P = .05).
“The existence of an IBD-associated operational taxonomic unit type and metabotype in healthy relatives suggests that dysbiosis with its associated metabolic products may be a preexisting trait that precedes the acquisition of [inflammatory bowel] disease,” the investigators concluded. “Validating this interpretation will require prospective longitudinal studies to assess the incidence of IBD in individuals stratified by operational taxonomic type, metabotype, and calprotectin, and to assess the stability of operational taxonomic unit types and metabotypes across time and diet.”
The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Numerous studies have established an association between intestinal dysbiosis and inflammatory bowel disease, and data from mouse models of colitis show that IBD-associated microbiota can exacerbate ongoing inflammation. Still, it is not clear that dysbiosis is either necessary or sufficient to trigger IBD – it could be that the microbiome must first be shaped by an inflammatory state on the host’s side before it can achieve a pathogenic signature and contribute to disease. New findings reported here speak to this question by demonstrating the presence of an IBD-like intestinal microbiome signature in a high-risk population, healthy first-degree relatives of IBD patients. The observation of dysbiosis in at-risk but asymptomatic individuals is an important step toward understanding the sequence of disease onset, raising the provocative possibility that, at least in some cases, dysbiosis is a predisease state, and could potentially be an instigator. The key next step will be longitudinal studies testing the predictive power of these findings. If healthy relatives with the IBD-associated microbiome signatures proceed to develop disease at an increased rate versus relatives with normal gut flora, these signatures would have potential clinical utility either as a screening and risk-assessment tool, or possibly as a target for preventative treatment.
Mark R. Frey, PhD, is assistant professor of pediatrics and biochemistry & molecular medicine at the Saban Research Institute at Children’s Hospital Los Angeles, University of Southern California, Los Angeles. He has no conflicts of interest to disclose.
Numerous studies have established an association between intestinal dysbiosis and inflammatory bowel disease, and data from mouse models of colitis show that IBD-associated microbiota can exacerbate ongoing inflammation. Still, it is not clear that dysbiosis is either necessary or sufficient to trigger IBD – it could be that the microbiome must first be shaped by an inflammatory state on the host’s side before it can achieve a pathogenic signature and contribute to disease. New findings reported here speak to this question by demonstrating the presence of an IBD-like intestinal microbiome signature in a high-risk population, healthy first-degree relatives of IBD patients. The observation of dysbiosis in at-risk but asymptomatic individuals is an important step toward understanding the sequence of disease onset, raising the provocative possibility that, at least in some cases, dysbiosis is a predisease state, and could potentially be an instigator. The key next step will be longitudinal studies testing the predictive power of these findings. If healthy relatives with the IBD-associated microbiome signatures proceed to develop disease at an increased rate versus relatives with normal gut flora, these signatures would have potential clinical utility either as a screening and risk-assessment tool, or possibly as a target for preventative treatment.
Mark R. Frey, PhD, is assistant professor of pediatrics and biochemistry & molecular medicine at the Saban Research Institute at Children’s Hospital Los Angeles, University of Southern California, Los Angeles. He has no conflicts of interest to disclose.
Numerous studies have established an association between intestinal dysbiosis and inflammatory bowel disease, and data from mouse models of colitis show that IBD-associated microbiota can exacerbate ongoing inflammation. Still, it is not clear that dysbiosis is either necessary or sufficient to trigger IBD – it could be that the microbiome must first be shaped by an inflammatory state on the host’s side before it can achieve a pathogenic signature and contribute to disease. New findings reported here speak to this question by demonstrating the presence of an IBD-like intestinal microbiome signature in a high-risk population, healthy first-degree relatives of IBD patients. The observation of dysbiosis in at-risk but asymptomatic individuals is an important step toward understanding the sequence of disease onset, raising the provocative possibility that, at least in some cases, dysbiosis is a predisease state, and could potentially be an instigator. The key next step will be longitudinal studies testing the predictive power of these findings. If healthy relatives with the IBD-associated microbiome signatures proceed to develop disease at an increased rate versus relatives with normal gut flora, these signatures would have potential clinical utility either as a screening and risk-assessment tool, or possibly as a target for preventative treatment.
Mark R. Frey, PhD, is assistant professor of pediatrics and biochemistry & molecular medicine at the Saban Research Institute at Children’s Hospital Los Angeles, University of Southern California, Los Angeles. He has no conflicts of interest to disclose.
Healthy first-degree relatives of children and adolescents with inflammatory bowel disease had intestinal dysbiosis and an altered intestinal metabolome that correlated with one another and with the disease state, researchers reported in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
These findings suggest the existence of a “high-risk microbiome/metabolome” that may increase susceptibility to inflammatory bowel disease (IBD), Jonathan Jacobs, MD, of the University of California, Los Angeles, reported with his associates. Among the healthy relatives with dysbiosis, nearly one-third also had elevated levels of fecal calprotectin, a marker of intestinal inflammation that has been previously reported in family members of patients with ulcerative colitis, the researchers noted. “If validated, prospective identification of [high-risk individuals] creates the opportunity to prevent disease development by targeting the dysbiosis and/or its metabolic consequences in the intestine,” they wrote.
Participants in the study fell into one of two “operational taxonomic units” based on their microbial communities, the researchers said. The second taxonomic unit not only was associated with IBD, “but irrespective of disease status, had lower microbial diversity and characteristic shifts in microbial composition, including increased Enterobacteriaceae, consistent with dysbiosis.” Among 21 families in the study, 19 had at least one member in this group. Furthermore, tests of an independent pediatric cohort revealed this same taxonomic group characterized by low microbial diversity and associated with IBD.
Participants also fell into two distinct metabotypes, one of which was associated with IBD and had increased levels of bile acids and amino acid derivatives previously linked to Crohn’s disease, as well as elevated levels of taurine, tryptophan, serinyl tryptophan, and adrenic acid, an omega-6 fatty acid, the researchers said. Taxonomic units and metabolic groups correlated highly with one another among both IBD patients and healthy relatives (P = 3 × 10-8), suggesting a “functional relationship between the microbiome and the metabolome,” the investigators said. Additionally, although most healthy relatives had normal fecal calprotectin levels, those in the second operational taxonomic unit had about sixfold greater odds of elevated calprotectin, compared with those in the first group (P = .05).
“The existence of an IBD-associated operational taxonomic unit type and metabotype in healthy relatives suggests that dysbiosis with its associated metabolic products may be a preexisting trait that precedes the acquisition of [inflammatory bowel] disease,” the investigators concluded. “Validating this interpretation will require prospective longitudinal studies to assess the incidence of IBD in individuals stratified by operational taxonomic type, metabotype, and calprotectin, and to assess the stability of operational taxonomic unit types and metabotypes across time and diet.”
The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Healthy first-degree relatives of children and adolescents with inflammatory bowel disease had intestinal dysbiosis and an altered intestinal metabolome that correlated with one another and with the disease state, researchers reported in the November issue of Cellular and Molecular Gastroenterology and Hepatology.
These findings suggest the existence of a “high-risk microbiome/metabolome” that may increase susceptibility to inflammatory bowel disease (IBD), Jonathan Jacobs, MD, of the University of California, Los Angeles, reported with his associates. Among the healthy relatives with dysbiosis, nearly one-third also had elevated levels of fecal calprotectin, a marker of intestinal inflammation that has been previously reported in family members of patients with ulcerative colitis, the researchers noted. “If validated, prospective identification of [high-risk individuals] creates the opportunity to prevent disease development by targeting the dysbiosis and/or its metabolic consequences in the intestine,” they wrote.
Participants in the study fell into one of two “operational taxonomic units” based on their microbial communities, the researchers said. The second taxonomic unit not only was associated with IBD, “but irrespective of disease status, had lower microbial diversity and characteristic shifts in microbial composition, including increased Enterobacteriaceae, consistent with dysbiosis.” Among 21 families in the study, 19 had at least one member in this group. Furthermore, tests of an independent pediatric cohort revealed this same taxonomic group characterized by low microbial diversity and associated with IBD.
Participants also fell into two distinct metabotypes, one of which was associated with IBD and had increased levels of bile acids and amino acid derivatives previously linked to Crohn’s disease, as well as elevated levels of taurine, tryptophan, serinyl tryptophan, and adrenic acid, an omega-6 fatty acid, the researchers said. Taxonomic units and metabolic groups correlated highly with one another among both IBD patients and healthy relatives (P = 3 × 10-8), suggesting a “functional relationship between the microbiome and the metabolome,” the investigators said. Additionally, although most healthy relatives had normal fecal calprotectin levels, those in the second operational taxonomic unit had about sixfold greater odds of elevated calprotectin, compared with those in the first group (P = .05).
“The existence of an IBD-associated operational taxonomic unit type and metabotype in healthy relatives suggests that dysbiosis with its associated metabolic products may be a preexisting trait that precedes the acquisition of [inflammatory bowel] disease,” the investigators concluded. “Validating this interpretation will require prospective longitudinal studies to assess the incidence of IBD in individuals stratified by operational taxonomic type, metabotype, and calprotectin, and to assess the stability of operational taxonomic unit types and metabotypes across time and diet.”
The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Key clinical point: Healthy first-degree relatives of patients with remitted inflammatory bowel disease can have intestinal dysbiosis and an altered intestinal metabolome that may signify subclinical inflammation or a “pre-IBD” state.
Major finding: Nineteen of 21 families had at least one member whose microbial taxonomy and metabolome correlated with IBD.
Data source: A cross-sectional study of 21 pediatric and adolescent probands with inflammatory bowel disease, nine parents and six siblings with IBD, and 54 healthy first-degree relatives.
Disclosures: The research was supported by the Helmsley Charitable Trust, the Crohn’s and Colitis Foundation of America, the Fineberg Foundation, the United States Public Health Service, the National Institutes of Health, the Cedars-Sinai F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute, the European Union, and the Joshua L. and Lisa Z. Greer Chair in Inflammatory Bowel Disease Genetics. The investigators had no conflicts of interest.
Interferon-free HCV treatment can lead to herpesvirus reactivation, experts say
Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Key clinical point: Latent herpesvirus infection may reactivate with interferon-free direct-acting antiviral treatment for chronic hepatitis C virus infection.
Major finding: In all, 2% of recipients of these regimens had herpesvirus reactivation a median of 8 weeks after starting treatment. Historical controls had no documented reactivations.
Data source: A multicenter retrospective study of 576 HCV-infected patients treated with interferon-free DAA regimens and 230 historical matched controls.
Disclosures: The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.
Study reinforces need to properly examine proximal large bowel during colonoscopy
Interval colorectal cancers were proximally located and had DNA mismatch repair deficiency significantly more often than did colorectal cancers in colonoscopy-naive patients, researchers reported in the November issue of Gastroenterology.
The findings underscore the need to effectively visualize the large colon to avoid missing lesions during colonoscopy, said Elena M. Stoffel, MD, MPH, of the University of Michigan Health System, Ann Arbor, and her associates. “Studies consistently show that colonoscopy affords less protection against proximal cancers, and DNA mismatch repair deficiency tumors are more frequent among proximal cancers,” they noted. But the proximal and distal colon also have different embryologic origins and gene expression profiles, “prompting some to suggest that these might be considered as two distinct organs. Whether the precursors of postcolonoscopy colorectal cancers are simply harder to detect or resect endoscopically, or whether their behavior differs on the basis of anatomic location or molecular subtype remains unclear,” they added.
A variety of quality-related factors contribute to the risk of postcolonoscopy or interval colorectal cancer, as do clinical characteristics such as older age at diagnosis, proximal tumor location, family history of colorectal cancer, and previous polypectomy, the investigators noted. To further explore the clinical and molecular correlates of postcolonoscopy tumors, they conducted a cross-sectional study of 10,365 colorectal cancers diagnosed in Denmark between 2007 and 2011 (Gastroenterology. 2016 Jul 18. doi: 10.1053/j.gastro.2016.07.010). A total of 725 (7%) of the colorectal cancers occurred after colonoscopy, the researchers determined. These lesions were significantly more often located in the proximal colon (odds ratio, 2.34; 95% confidence interval, 1.90-2.89) and were more likely to have DNA mismatch repair deficiency (OR, 1.26; 95% CI, 1.00-59) when compared with colorectal cancers diagnosed in patients with no prior colonoscopy. However, they also were significantly less likely to be metastatic at presentation (OR, 0.65; 95% CI, 0.48-0.89). Interval colorectal cancers were particularly likely to be located in the proximal colon and/or to have DNA mismatch repair deficiency when diagnosed 3-6 years after colonoscopy, but the excess burden of these characteristics persisted up to 10 years after colonoscopy, the researchers said.
Molecular analyses of 85 postcolonoscopy colorectal cancers from one hospital indicated that 24% had DNA mismatch repair deficiency. When considering only those tumors diagnosed within 10 years after colonoscopy, 27% had KRAS/NRAS mutations, 19% had BRAF mutations, and 19% had PIK3CA mutations. The 7% of tumors with molecular features of Lynch syndrome all occurred within 10 years after index colonoscopy and accounted for a third of cases of DNA mismatch repair deficiency, reflecting the role of this mutation pathway in Lynch syndrome and its tendency to rapidly progress, the investigators said.
Notably, 38% of colorectal cancers diagnosed within a year after colonoscopy involved an incomplete examination, compared with only 16% of cases diagnosed within 1-10 years after colonoscopy, they also reported. This finding and the clinical and molecular correlates of the interval cancers “supports the popular assumption that many cancers diagnosed soon after colonoscopy result from missed lesions,” they concluded. “However, the heterogeneity in clinical and molecular features of cancers diagnosed at different time intervals suggests postcolonoscopy colorectal cancers are likely multifactorial in their etiology and clinical behavior.”
The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
Interval colorectal cancers were proximally located and had DNA mismatch repair deficiency significantly more often than did colorectal cancers in colonoscopy-naive patients, researchers reported in the November issue of Gastroenterology.
The findings underscore the need to effectively visualize the large colon to avoid missing lesions during colonoscopy, said Elena M. Stoffel, MD, MPH, of the University of Michigan Health System, Ann Arbor, and her associates. “Studies consistently show that colonoscopy affords less protection against proximal cancers, and DNA mismatch repair deficiency tumors are more frequent among proximal cancers,” they noted. But the proximal and distal colon also have different embryologic origins and gene expression profiles, “prompting some to suggest that these might be considered as two distinct organs. Whether the precursors of postcolonoscopy colorectal cancers are simply harder to detect or resect endoscopically, or whether their behavior differs on the basis of anatomic location or molecular subtype remains unclear,” they added.
A variety of quality-related factors contribute to the risk of postcolonoscopy or interval colorectal cancer, as do clinical characteristics such as older age at diagnosis, proximal tumor location, family history of colorectal cancer, and previous polypectomy, the investigators noted. To further explore the clinical and molecular correlates of postcolonoscopy tumors, they conducted a cross-sectional study of 10,365 colorectal cancers diagnosed in Denmark between 2007 and 2011 (Gastroenterology. 2016 Jul 18. doi: 10.1053/j.gastro.2016.07.010). A total of 725 (7%) of the colorectal cancers occurred after colonoscopy, the researchers determined. These lesions were significantly more often located in the proximal colon (odds ratio, 2.34; 95% confidence interval, 1.90-2.89) and were more likely to have DNA mismatch repair deficiency (OR, 1.26; 95% CI, 1.00-59) when compared with colorectal cancers diagnosed in patients with no prior colonoscopy. However, they also were significantly less likely to be metastatic at presentation (OR, 0.65; 95% CI, 0.48-0.89). Interval colorectal cancers were particularly likely to be located in the proximal colon and/or to have DNA mismatch repair deficiency when diagnosed 3-6 years after colonoscopy, but the excess burden of these characteristics persisted up to 10 years after colonoscopy, the researchers said.
Molecular analyses of 85 postcolonoscopy colorectal cancers from one hospital indicated that 24% had DNA mismatch repair deficiency. When considering only those tumors diagnosed within 10 years after colonoscopy, 27% had KRAS/NRAS mutations, 19% had BRAF mutations, and 19% had PIK3CA mutations. The 7% of tumors with molecular features of Lynch syndrome all occurred within 10 years after index colonoscopy and accounted for a third of cases of DNA mismatch repair deficiency, reflecting the role of this mutation pathway in Lynch syndrome and its tendency to rapidly progress, the investigators said.
Notably, 38% of colorectal cancers diagnosed within a year after colonoscopy involved an incomplete examination, compared with only 16% of cases diagnosed within 1-10 years after colonoscopy, they also reported. This finding and the clinical and molecular correlates of the interval cancers “supports the popular assumption that many cancers diagnosed soon after colonoscopy result from missed lesions,” they concluded. “However, the heterogeneity in clinical and molecular features of cancers diagnosed at different time intervals suggests postcolonoscopy colorectal cancers are likely multifactorial in their etiology and clinical behavior.”
The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
Interval colorectal cancers were proximally located and had DNA mismatch repair deficiency significantly more often than did colorectal cancers in colonoscopy-naive patients, researchers reported in the November issue of Gastroenterology.
The findings underscore the need to effectively visualize the large colon to avoid missing lesions during colonoscopy, said Elena M. Stoffel, MD, MPH, of the University of Michigan Health System, Ann Arbor, and her associates. “Studies consistently show that colonoscopy affords less protection against proximal cancers, and DNA mismatch repair deficiency tumors are more frequent among proximal cancers,” they noted. But the proximal and distal colon also have different embryologic origins and gene expression profiles, “prompting some to suggest that these might be considered as two distinct organs. Whether the precursors of postcolonoscopy colorectal cancers are simply harder to detect or resect endoscopically, or whether their behavior differs on the basis of anatomic location or molecular subtype remains unclear,” they added.
A variety of quality-related factors contribute to the risk of postcolonoscopy or interval colorectal cancer, as do clinical characteristics such as older age at diagnosis, proximal tumor location, family history of colorectal cancer, and previous polypectomy, the investigators noted. To further explore the clinical and molecular correlates of postcolonoscopy tumors, they conducted a cross-sectional study of 10,365 colorectal cancers diagnosed in Denmark between 2007 and 2011 (Gastroenterology. 2016 Jul 18. doi: 10.1053/j.gastro.2016.07.010). A total of 725 (7%) of the colorectal cancers occurred after colonoscopy, the researchers determined. These lesions were significantly more often located in the proximal colon (odds ratio, 2.34; 95% confidence interval, 1.90-2.89) and were more likely to have DNA mismatch repair deficiency (OR, 1.26; 95% CI, 1.00-59) when compared with colorectal cancers diagnosed in patients with no prior colonoscopy. However, they also were significantly less likely to be metastatic at presentation (OR, 0.65; 95% CI, 0.48-0.89). Interval colorectal cancers were particularly likely to be located in the proximal colon and/or to have DNA mismatch repair deficiency when diagnosed 3-6 years after colonoscopy, but the excess burden of these characteristics persisted up to 10 years after colonoscopy, the researchers said.
Molecular analyses of 85 postcolonoscopy colorectal cancers from one hospital indicated that 24% had DNA mismatch repair deficiency. When considering only those tumors diagnosed within 10 years after colonoscopy, 27% had KRAS/NRAS mutations, 19% had BRAF mutations, and 19% had PIK3CA mutations. The 7% of tumors with molecular features of Lynch syndrome all occurred within 10 years after index colonoscopy and accounted for a third of cases of DNA mismatch repair deficiency, reflecting the role of this mutation pathway in Lynch syndrome and its tendency to rapidly progress, the investigators said.
Notably, 38% of colorectal cancers diagnosed within a year after colonoscopy involved an incomplete examination, compared with only 16% of cases diagnosed within 1-10 years after colonoscopy, they also reported. This finding and the clinical and molecular correlates of the interval cancers “supports the popular assumption that many cancers diagnosed soon after colonoscopy result from missed lesions,” they concluded. “However, the heterogeneity in clinical and molecular features of cancers diagnosed at different time intervals suggests postcolonoscopy colorectal cancers are likely multifactorial in their etiology and clinical behavior.”
The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
FROM GASTROENTEROLOGY
Key clinical point: A large population-based study reinforced the need to properly examine the proximal large bowel during colonoscopy.
Major finding: Postcolonoscopy colorectal cancers were significantly more likely to be proximal (OR, 2.34) and to have DNA mismatch repair deficiency (OR, 1.26) compared with colorectal cancers diagnosed in patients with no prior colonoscopy.
Data source: A population-based, cross-sectional study of 10,365 newly diagnosed colorectal cancer cases.
Disclosures: The study was supported by the Danish Cancer Society, the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, M.D. Anderson Cancer Center, and a University of Texas Frederick Becker Distinguished University Chair in Cancer Research. The investigators had no disclosures.
VIDEO: Duodenal bulb sampling barely increased celiac yield in low-probability cohort
Separate sampling of the duodenal bulb increased detection of celiac disease by only 0.1% when endoscopy patients had a low pretest probability of celiac disease, according to research published in the November issue of Clinical Gastroenterology and Hepatology.
Duodenal bulb histology did reveal other abnormal findings, such as chronic peptic duodenitis, gastric heterotopia, and Brunner gland hyperplasia, wrote Samantha Stoven, MD, of Mayo Clinic, Rochester, Minn., and her associates. These findings did not seem to impede the identification of celiac disease, but their clinical implications were unclear, the researchers noted.
Most studies of the diagnostic yield of duodenal bulb specimens have been performed in patients with known celiac disease or positive serology. In past studies of these high-probability cohorts, duodenal bulb sampling increased the diagnostic yield of celiac disease anywhere from 1.8% to 18%, but whether and how that finding translates to low-probability cohorts is unclear, the researchers said. Therefore, they retrospectively analyzed data from 679 endoscopy patients who had both duodenal bulb and small bowel biopsies collected at three Mayo Clinic sites in 2011. These sites are “open access,” meaning that patients can be referred for endoscopy without the approval of a gastroenterologist.
The average age of the patients was 50 years, and 63% were female. They were most commonly referred for duodenal biopsy because of chronic dyspepsia (46% of patients), diarrhea (35%), or nausea (17%). Patients with either known celiac disease or positive serology were excluded from the study (Clin Gastroenterol Hepatol. 2016 Mar 7. doi: 10.1016/j.cgh.2016.02.026). A total of 265 patients (39%) had abnormal duodenal histology, which was most often diagnosed as chronic peptic duodenitis, the researchers said. Histologic abnormalities usually involved the duodenal bulb (36% of cases), not the distal duodenum (15%; P less than .0001). However, among the 16 patients (2%) found to have celiac disease, just one patient had disease only in the duodenal bulb. Thus, duodenal bulb sampling increased the diagnostic yield of celiac disease by only 0.1% when considering the overall cohort. The patient with celiac disease limited to the bulb was a 46-year-old female presenting with diarrhea and anemia who had normal serologies but a permissive human leukocyte antigen test. Her duodenal bulb had villous atrophy and more than 25 intraepithelial lymphocytes per 100 epithelial cells, while her distal duodenum was normal.
Among the 85% of patients who had normal distal duodenums, 28% had abnormal bulb histology, most often chronic peptic duodenitis, active chronic peptic duodenitis, or gastric heterotopia, the researchers said. Among the 59% of patients whose celiac serology before endoscopy was truly unknown, only two (0.5%) had histologic changes consistent with celiac disease, which in both cases were located in the distal duodenum.
SOURCE: American Gastroenterological Association
“Individual sampling of the duodenal bulb in patients with either negative or unknown celiac serologic status can be considered in practices where expert gastrointestinal pathologists are present and there is agreement that both samples can be submitted in the same bottle, or there is not a separate charge for the additional container. Further studies may be needed to assess the diagnostic yield of separate bulb biopsies for celiac detection in all comers.”
An American College of Gastroenterology Junior Faculty Development Award helped support the work. Senior author Joseph A. Murray, MD, disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, AMAG Pharmaceuticals, and several other corporate entities. The remaining authors had no disclosures.
Histologic diagnosis of celiac disease has traditionally relied upon endoscopic biopsies from the second and third portions of the duodenum. However, several recent studies indicate that duodenal bulb biopsies may show changes of celiac disease, despite normal histology in the more distal duodenum.
In their study, Dr. Stoven and her colleagues evaluated the diagnostic utility of endoscopic duodenal bulb biopsy in patients with a low probability for celiac disease. A new diagnosis of celiac disease was made in 16 of their 679 patients (2.4%). Only one patient showed villous atrophy of the duodenal bulb with normal histology of the more distal duodenum. Although a diagnosis of celiac disease was made, the case was atypical not only because distal duodenal biopsies were normal but also because multiple celiac serology tests were negative, raising the possibility of nonceliac villous atrophy. Thus, the added diagnostic yield of duodenal bulb biopsies in this low-risk population was extremely low (0.15% at most).
Ciaran P. Kelly, MD, AGAF, professor of medicine, Harvard Medical School, director Celiac Center, Beth Israel Deaconess Medical Center, Boston, has acted as a scientific adviser to companies including Celimmune, Cour Pharmaceuticals, ImmunogenX, and Takeda; he also acts as principal investigator on a research grant on celiac disease supported by Aptalis.
Histologic diagnosis of celiac disease has traditionally relied upon endoscopic biopsies from the second and third portions of the duodenum. However, several recent studies indicate that duodenal bulb biopsies may show changes of celiac disease, despite normal histology in the more distal duodenum.
In their study, Dr. Stoven and her colleagues evaluated the diagnostic utility of endoscopic duodenal bulb biopsy in patients with a low probability for celiac disease. A new diagnosis of celiac disease was made in 16 of their 679 patients (2.4%). Only one patient showed villous atrophy of the duodenal bulb with normal histology of the more distal duodenum. Although a diagnosis of celiac disease was made, the case was atypical not only because distal duodenal biopsies were normal but also because multiple celiac serology tests were negative, raising the possibility of nonceliac villous atrophy. Thus, the added diagnostic yield of duodenal bulb biopsies in this low-risk population was extremely low (0.15% at most).
Ciaran P. Kelly, MD, AGAF, professor of medicine, Harvard Medical School, director Celiac Center, Beth Israel Deaconess Medical Center, Boston, has acted as a scientific adviser to companies including Celimmune, Cour Pharmaceuticals, ImmunogenX, and Takeda; he also acts as principal investigator on a research grant on celiac disease supported by Aptalis.
Histologic diagnosis of celiac disease has traditionally relied upon endoscopic biopsies from the second and third portions of the duodenum. However, several recent studies indicate that duodenal bulb biopsies may show changes of celiac disease, despite normal histology in the more distal duodenum.
In their study, Dr. Stoven and her colleagues evaluated the diagnostic utility of endoscopic duodenal bulb biopsy in patients with a low probability for celiac disease. A new diagnosis of celiac disease was made in 16 of their 679 patients (2.4%). Only one patient showed villous atrophy of the duodenal bulb with normal histology of the more distal duodenum. Although a diagnosis of celiac disease was made, the case was atypical not only because distal duodenal biopsies were normal but also because multiple celiac serology tests were negative, raising the possibility of nonceliac villous atrophy. Thus, the added diagnostic yield of duodenal bulb biopsies in this low-risk population was extremely low (0.15% at most).
Ciaran P. Kelly, MD, AGAF, professor of medicine, Harvard Medical School, director Celiac Center, Beth Israel Deaconess Medical Center, Boston, has acted as a scientific adviser to companies including Celimmune, Cour Pharmaceuticals, ImmunogenX, and Takeda; he also acts as principal investigator on a research grant on celiac disease supported by Aptalis.
Separate sampling of the duodenal bulb increased detection of celiac disease by only 0.1% when endoscopy patients had a low pretest probability of celiac disease, according to research published in the November issue of Clinical Gastroenterology and Hepatology.
Duodenal bulb histology did reveal other abnormal findings, such as chronic peptic duodenitis, gastric heterotopia, and Brunner gland hyperplasia, wrote Samantha Stoven, MD, of Mayo Clinic, Rochester, Minn., and her associates. These findings did not seem to impede the identification of celiac disease, but their clinical implications were unclear, the researchers noted.
Most studies of the diagnostic yield of duodenal bulb specimens have been performed in patients with known celiac disease or positive serology. In past studies of these high-probability cohorts, duodenal bulb sampling increased the diagnostic yield of celiac disease anywhere from 1.8% to 18%, but whether and how that finding translates to low-probability cohorts is unclear, the researchers said. Therefore, they retrospectively analyzed data from 679 endoscopy patients who had both duodenal bulb and small bowel biopsies collected at three Mayo Clinic sites in 2011. These sites are “open access,” meaning that patients can be referred for endoscopy without the approval of a gastroenterologist.
The average age of the patients was 50 years, and 63% were female. They were most commonly referred for duodenal biopsy because of chronic dyspepsia (46% of patients), diarrhea (35%), or nausea (17%). Patients with either known celiac disease or positive serology were excluded from the study (Clin Gastroenterol Hepatol. 2016 Mar 7. doi: 10.1016/j.cgh.2016.02.026). A total of 265 patients (39%) had abnormal duodenal histology, which was most often diagnosed as chronic peptic duodenitis, the researchers said. Histologic abnormalities usually involved the duodenal bulb (36% of cases), not the distal duodenum (15%; P less than .0001). However, among the 16 patients (2%) found to have celiac disease, just one patient had disease only in the duodenal bulb. Thus, duodenal bulb sampling increased the diagnostic yield of celiac disease by only 0.1% when considering the overall cohort. The patient with celiac disease limited to the bulb was a 46-year-old female presenting with diarrhea and anemia who had normal serologies but a permissive human leukocyte antigen test. Her duodenal bulb had villous atrophy and more than 25 intraepithelial lymphocytes per 100 epithelial cells, while her distal duodenum was normal.
Among the 85% of patients who had normal distal duodenums, 28% had abnormal bulb histology, most often chronic peptic duodenitis, active chronic peptic duodenitis, or gastric heterotopia, the researchers said. Among the 59% of patients whose celiac serology before endoscopy was truly unknown, only two (0.5%) had histologic changes consistent with celiac disease, which in both cases were located in the distal duodenum.
SOURCE: American Gastroenterological Association
“Individual sampling of the duodenal bulb in patients with either negative or unknown celiac serologic status can be considered in practices where expert gastrointestinal pathologists are present and there is agreement that both samples can be submitted in the same bottle, or there is not a separate charge for the additional container. Further studies may be needed to assess the diagnostic yield of separate bulb biopsies for celiac detection in all comers.”
An American College of Gastroenterology Junior Faculty Development Award helped support the work. Senior author Joseph A. Murray, MD, disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, AMAG Pharmaceuticals, and several other corporate entities. The remaining authors had no disclosures.
Separate sampling of the duodenal bulb increased detection of celiac disease by only 0.1% when endoscopy patients had a low pretest probability of celiac disease, according to research published in the November issue of Clinical Gastroenterology and Hepatology.
Duodenal bulb histology did reveal other abnormal findings, such as chronic peptic duodenitis, gastric heterotopia, and Brunner gland hyperplasia, wrote Samantha Stoven, MD, of Mayo Clinic, Rochester, Minn., and her associates. These findings did not seem to impede the identification of celiac disease, but their clinical implications were unclear, the researchers noted.
Most studies of the diagnostic yield of duodenal bulb specimens have been performed in patients with known celiac disease or positive serology. In past studies of these high-probability cohorts, duodenal bulb sampling increased the diagnostic yield of celiac disease anywhere from 1.8% to 18%, but whether and how that finding translates to low-probability cohorts is unclear, the researchers said. Therefore, they retrospectively analyzed data from 679 endoscopy patients who had both duodenal bulb and small bowel biopsies collected at three Mayo Clinic sites in 2011. These sites are “open access,” meaning that patients can be referred for endoscopy without the approval of a gastroenterologist.
The average age of the patients was 50 years, and 63% were female. They were most commonly referred for duodenal biopsy because of chronic dyspepsia (46% of patients), diarrhea (35%), or nausea (17%). Patients with either known celiac disease or positive serology were excluded from the study (Clin Gastroenterol Hepatol. 2016 Mar 7. doi: 10.1016/j.cgh.2016.02.026). A total of 265 patients (39%) had abnormal duodenal histology, which was most often diagnosed as chronic peptic duodenitis, the researchers said. Histologic abnormalities usually involved the duodenal bulb (36% of cases), not the distal duodenum (15%; P less than .0001). However, among the 16 patients (2%) found to have celiac disease, just one patient had disease only in the duodenal bulb. Thus, duodenal bulb sampling increased the diagnostic yield of celiac disease by only 0.1% when considering the overall cohort. The patient with celiac disease limited to the bulb was a 46-year-old female presenting with diarrhea and anemia who had normal serologies but a permissive human leukocyte antigen test. Her duodenal bulb had villous atrophy and more than 25 intraepithelial lymphocytes per 100 epithelial cells, while her distal duodenum was normal.
Among the 85% of patients who had normal distal duodenums, 28% had abnormal bulb histology, most often chronic peptic duodenitis, active chronic peptic duodenitis, or gastric heterotopia, the researchers said. Among the 59% of patients whose celiac serology before endoscopy was truly unknown, only two (0.5%) had histologic changes consistent with celiac disease, which in both cases were located in the distal duodenum.
SOURCE: American Gastroenterological Association
“Individual sampling of the duodenal bulb in patients with either negative or unknown celiac serologic status can be considered in practices where expert gastrointestinal pathologists are present and there is agreement that both samples can be submitted in the same bottle, or there is not a separate charge for the additional container. Further studies may be needed to assess the diagnostic yield of separate bulb biopsies for celiac detection in all comers.”
An American College of Gastroenterology Junior Faculty Development Award helped support the work. Senior author Joseph A. Murray, MD, disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, AMAG Pharmaceuticals, and several other corporate entities. The remaining authors had no disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Separate sampling of the duodenal bulb increased detection of celiac disease by only 0.1% when endoscopy patients had a low pretest probability of celiac disease.
Major finding: One (0.1%) patient had celiac disease limited to the duodenal bulb.
Data source: A multicenter retrospective study of 679 patients without celiac disease or positive serology from whom duodenal bulb and small bowel biopsies were collected during endoscopy.
Disclosures: An American College of Gastroenterology Junior Faculty Development Award helped support the work. Senior author Joseph A. Murray, MD, disclosed ties to Alba Therapeutics, Alvine Pharmaceuticals, AMAG Pharmaceuticals, and several other corporate entities. The remaining authors had no disclosures.
Delaying cancer treatment for fertility preservation did not affect outcomes
SALT LAKE CITY – Delaying cancer treatment to allow women to undergo fertility preservation did not affect long-term cancer outcomes, suggest the findings from a retrospective study of more than 500 patients.
Over a median of 3.7 years of follow-up, 2.3% of patients who elected fertility preservation developed recurrent cancer, compared with 5.3% of patients who did not undergo fertility preservation (P = .09), according to Molly Moravek, MD, of the University of Michigan, Ann Arbor, and her associates.
Survival rates were 97.7% for patients who underwent fertility preservation and 94.1% for those who did not (P = .05), the investigators reported in a poster at the annual meeting of the American Society for Reproductive Medicine.
“Pursuing fertility preservation results in minimal delays to initiation of cancer treatment and is unlikely to be clinically significant,” the investigators wrote. “There is no evidence of increased recurrence or mortality in fertility preservation patients versus controls, suggesting fertility preservation is safe for eligible cancer patients.”
Progress in cancer detection and survival has sharpened the focus on quality of life issues, including fertility preservation, the researchers said. But oncologists and patients themselves have raised concerns about postponing cancer treatment for this reason, and some have recommended shortening the delay by triggering ovarian stimulation regardless of the phase of the menstrual cycle – known as the “random start” protocol.
To explore these issues, the researchers reviewed the charts of all 553 cancer patients who had used the online patient navigator for fertility preservation at Northwestern University from 2006 to 2015.
A total of 213 patients pursued fertility preservation, while 340 did not. Undergoing fertility preservation postponed treatment of breast, hematologic, gynecologic, and other cancers by an average of 10 days, but this delay did not translate to worse recurrence rates or mortality, either overall or for any cancer subtype.
Cycle outcomes were similar between the 117 patients who underwent random-start protocols and the 23 patients underwent cycle-specific protocols, the investigators reported. Both protocols were associated with similar numbers of oocytes retrieved, numbers of mature oocytes, peak serum estradiol levels, days of stimulation, and times to cancer treatment.
The Northwestern Memorial Foundation supported the work. Dr. Moravek reported having no relevant financial disclosures.
SALT LAKE CITY – Delaying cancer treatment to allow women to undergo fertility preservation did not affect long-term cancer outcomes, suggest the findings from a retrospective study of more than 500 patients.
Over a median of 3.7 years of follow-up, 2.3% of patients who elected fertility preservation developed recurrent cancer, compared with 5.3% of patients who did not undergo fertility preservation (P = .09), according to Molly Moravek, MD, of the University of Michigan, Ann Arbor, and her associates.
Survival rates were 97.7% for patients who underwent fertility preservation and 94.1% for those who did not (P = .05), the investigators reported in a poster at the annual meeting of the American Society for Reproductive Medicine.
“Pursuing fertility preservation results in minimal delays to initiation of cancer treatment and is unlikely to be clinically significant,” the investigators wrote. “There is no evidence of increased recurrence or mortality in fertility preservation patients versus controls, suggesting fertility preservation is safe for eligible cancer patients.”
Progress in cancer detection and survival has sharpened the focus on quality of life issues, including fertility preservation, the researchers said. But oncologists and patients themselves have raised concerns about postponing cancer treatment for this reason, and some have recommended shortening the delay by triggering ovarian stimulation regardless of the phase of the menstrual cycle – known as the “random start” protocol.
To explore these issues, the researchers reviewed the charts of all 553 cancer patients who had used the online patient navigator for fertility preservation at Northwestern University from 2006 to 2015.
A total of 213 patients pursued fertility preservation, while 340 did not. Undergoing fertility preservation postponed treatment of breast, hematologic, gynecologic, and other cancers by an average of 10 days, but this delay did not translate to worse recurrence rates or mortality, either overall or for any cancer subtype.
Cycle outcomes were similar between the 117 patients who underwent random-start protocols and the 23 patients underwent cycle-specific protocols, the investigators reported. Both protocols were associated with similar numbers of oocytes retrieved, numbers of mature oocytes, peak serum estradiol levels, days of stimulation, and times to cancer treatment.
The Northwestern Memorial Foundation supported the work. Dr. Moravek reported having no relevant financial disclosures.
SALT LAKE CITY – Delaying cancer treatment to allow women to undergo fertility preservation did not affect long-term cancer outcomes, suggest the findings from a retrospective study of more than 500 patients.
Over a median of 3.7 years of follow-up, 2.3% of patients who elected fertility preservation developed recurrent cancer, compared with 5.3% of patients who did not undergo fertility preservation (P = .09), according to Molly Moravek, MD, of the University of Michigan, Ann Arbor, and her associates.
Survival rates were 97.7% for patients who underwent fertility preservation and 94.1% for those who did not (P = .05), the investigators reported in a poster at the annual meeting of the American Society for Reproductive Medicine.
“Pursuing fertility preservation results in minimal delays to initiation of cancer treatment and is unlikely to be clinically significant,” the investigators wrote. “There is no evidence of increased recurrence or mortality in fertility preservation patients versus controls, suggesting fertility preservation is safe for eligible cancer patients.”
Progress in cancer detection and survival has sharpened the focus on quality of life issues, including fertility preservation, the researchers said. But oncologists and patients themselves have raised concerns about postponing cancer treatment for this reason, and some have recommended shortening the delay by triggering ovarian stimulation regardless of the phase of the menstrual cycle – known as the “random start” protocol.
To explore these issues, the researchers reviewed the charts of all 553 cancer patients who had used the online patient navigator for fertility preservation at Northwestern University from 2006 to 2015.
A total of 213 patients pursued fertility preservation, while 340 did not. Undergoing fertility preservation postponed treatment of breast, hematologic, gynecologic, and other cancers by an average of 10 days, but this delay did not translate to worse recurrence rates or mortality, either overall or for any cancer subtype.
Cycle outcomes were similar between the 117 patients who underwent random-start protocols and the 23 patients underwent cycle-specific protocols, the investigators reported. Both protocols were associated with similar numbers of oocytes retrieved, numbers of mature oocytes, peak serum estradiol levels, days of stimulation, and times to cancer treatment.
The Northwestern Memorial Foundation supported the work. Dr. Moravek reported having no relevant financial disclosures.
AT 2016 ASRM
Key clinical point:
Major finding: Fertility preservation was associated with an average 10-day delay in cancer treatment, which did not affect rates of cancer recurrence or mortality.
Data source: Retrospective chart reviews of 553 patients with breast, hematologic, ovarian, and other cancers, with a median of 3.7 years of follow-up.
Disclosures: The Northwestern Memorial Foundation supported the work. Dr. Moravek reported having no relevant financial disclosures.