User login
Test your skills: Which imaging studies would you order for these neurologic complaints?
› Use clinical decision tools and American College of Radiology Appropriateness Criteria to determine levels of evidence for ordering specific imaging studies. A
› Consider ordering an imaging study when headache is accompanied by a new neurologic symptom. Computed tomography (CT) without contrast is best for patients who are acutely ill. In the non-emergent setting, magnetic resonance imaging (MRI) with contrast is the optimal study. A
› Order structural neuroimaging as part of the initial work-up of suspected dementia. MRI is the test of choice. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When patients present with neurologic complaints in outpatient primary care practice, 2 key questions often arise: Should brain imaging be ordered, and if so, which study? Careful history-taking and physical exam findings can suggest differential diagnoses and help determine whether imaging studies could identify potential underlying causes. Further considerations in making a decision are the type of information each modality offers, the possible need for contrast media, benefits vs radiation exposure risks, potential contraindications, and cost and local availability. In this article, we present 3 common outpatient scenarios, and in each case we describe the evidence to support clinical decision-making about imaging.
The American College of Radiology (ACR) Appropriateness Criteria Web site (http://www.acr.org/Quality-Safety/Appropriateness-Criteria) provides radiation exposure information, numerical ratings of imaging studies for individual clinical scenarios, evidence tables, and reference tables for each of its recommendations.1 ACR’s recommendations were developed by expert panels of diagnostic radiologists, interventional radiologists, and radiation oncologists, and designed to help physicians order the most appropriate imaging studies based on patients’ clinical conditions.2 We used these criteria to develop an evaluation strategy for each of our clinical scenarios.
CASE 1 › Carrie D is a 45-year-old woman with a history of migraine without aura generally controlled with Excedrin (acetaminophen, aspirin, and caffeine). She arrives at your office with a 2-day history of severe headache over the top of her head and associated tingling sensation over the left side of her face, but with no vision changes, weakness, or slurred speech. She denies any prior history of numbness or tinging with past headaches. She is a business executive and reports that in the last few weeks, her company has been involved in a high-profile merger. On physical exam, her vital signs are within normal limits. She does not appear acutely ill, but on exam she reports diminished sensation to light touch over the left side of her face, left arm, and left leg compared with the right side.
›› What imaging options might you consider?
A prospective review of physicians in an ambulatory family practice setting found that neurologic imaging was typically ordered for patients with headache who were suspected of having a brain tumor or subarachnoid hemorrhage.3 For our patient, who has a history of migraines without aura and whose current severe headache is accompanied by an abnormal sensation on one side of the face, the following questions are relevant: Is this presentation part of her primary headache syndrome or could there be a different cause? If there is a different cause, is it likely to be detected with brain imaging such as computed tomography (CT) or magnetic resonance imaging (MRI)?
Patients with isolated headache and an absence of neurologic symptoms or abnormalities on neurologic exam are unlikely to have a clinically significant intracranial abnormality.4-10 Imaging of the brain is typically not indicated for these patients.2 However, given that this patient does have a positive focal neurologic finding, a CT or MRI is indicated, as findings are more likely to influence management decisions.
The decision to order CT or MRI should be based on how acutely ill the patient is. CT without contrast is an excellent tool to rule out suspected emergent intracranial abnormalities such as an intracranial hemorrhage, hydrocephalus, or a mass.11 In patients presenting with symptoms suggesting acute illness such as carotid or vertebral artery dissection, the most appropriate test would be CT angiography of the head and neck.2
However, the list of less dire causes of headache is vast. Included in this list would be trauma, other vascular disorders such as arteriovenous malformation or temporal arteritis, infection, abnormal intracranial pressure (mass, pseudotumor cerebri, intracranial hypotension), and disorders of the head/face/spine (eg, temporomandibular joint disorder).12
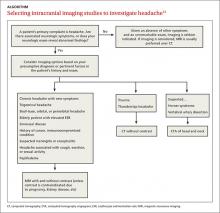
In the non-acute setting where a patient has stable vital signs and is not in acute distress, an MRI with contrast would be the most appropriate test to identify such causes. Avoid contrast only if there is a firm contraindication, such as pregnancy, severely impaired renal function, or known allergy to gadolinium. If history and physical exam findings suggest possible stroke, arrange for MRI and MR angiography with contrast, even if the result of a head CT scan is negative. The ALGORITHM13 offers guidance for choosing imaging studies for headache based on history, physical exam, and laboratory findings.
›› And you order...
…an MRI of the brain with contrast.
Though Ms. D does have a focal neurologic finding in addition to her headache, she does not appear to be acutely ill. Ordering an MRI with contrast is the best first step.
CASE 2 › Anne B is a 72-year-old woman with a history of hypertension, hyperlipidemia, and type 2 diabetes. Her daughter brings her in to see you because she is concerned about Ms. B’s memory. Ms. B’s daughter reports that she has become increasingly forgetful over the past 6 months, often forgetting recent events. At first the forgetfulness was occasional, but now it seems to happen daily and interfere with activities of daily living (ADLs). The week before this visit, Ms. B left a pot heating on the stove because she forgot she had started cooking. She realized what had happened only when her smoke alarm went off. Ms. B’s daughter also thinks her mother may be taking some of her medications incorrectly.
Physical exam and laboratory findings are unremarkable. On the mental status exam, Ms. B has difficulty with registration and recall.
›› What imaging options might you consider?
Ms. B has exhibited progressive memory loss over 6 months and it is now affecting her ADLs. Her symptoms could be secondary to any one of many reversible medical causes, such as adverse medication effects, depression, or vitamin B12 deficiency. If clinical and laboratory evaluations exclude these reversible causes, consider dementia.
With numerous disorders having overlapping symptoms, the diagnosis of degenerative central nervous system (CNS) disease can be extremely tricky. Complicating the issue is the fact that a single patient can have 2 or more concurrent neurodegenerative diseases. Clinical testing is essential in the diagnosis and management of degenerative CNS diseases, but testing sensitivity and specificity are highly variable depending upon the disease.14
Neuroimaging is an important supplement to clinical testing in excluding intracranial abnormalities. There are significant negative consequences of missing reversible causes of memory problems and incorrectly assigning a clinical diagnosis of dementia. Neuroimaging can be subdivided into structural and functional imaging, and structural imaging is the first step in evaluation.15
The American Academy of Neurology recommends the use of structural neuroimaging with CT or MRI in the initial evaluation of patients with dementia to detect such treatable problems as a subdural hematoma, frontal lobe mass, or hydrocephalus.12 Structural imaging may also identify anatomic changes characteristic of degenerative CNS diseases such as Alzheimer’s disease, dementia with Lewy bodies, frontotemporal dementia, vascular dementia, Creutzfeldt-Jakob disease, and Huntington’s disease; however, sensitivities and specificities of testing are low.14
›› And you order...
…an MRI of the brain without contrast.
In Ms. B’s case, structural neuroimaging is indicated as part of the initial work-up of supposed dementia. An MRI without contrast is recommended over CT because it is more sensitive in detecting white matter changes in vascular dementia.16 In cases where an MRI >is unavailable or contraindicated (eg, a patient with a pacemaker), a CT is a reasonable alternative.
CASE 3 › Bob C is a 78-year-old man with a history of chronic obstructive pulmonary disease and hypertension who arrives at your walk-in clinic accompanied by his home health aide a few hours after having tripped and fallen over a rug at home. At baseline, Mr. C is ambulatory and independent in ADLs.
He takes all of his medications, including a daily baby aspirin (81 mg). Mr. C says he did not lose consciousness at the time of the fall and insists he feels fine, but you notice a bruise developing over his right temporal skull.
›› What imaging options might you consider?
With acute head trauma deemed severe enough clinically to warrant imaging, non-contrast CT is the most appropriate initial test to identify possible intracranial hemorrhage.11 The Glasgow Coma Scale (GCS) is the tool most widely used for clinical evaluation17 (TABLE 118). The score is based on an assessment of 3 features: eye response, speech, and movement. Head injury is classified as mild (13-15), moderate (9-12), or severe (≤8). It is universally agreed that patients with moderate or severe head injury should be further evaluated with a head CT.
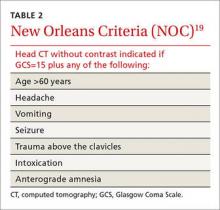
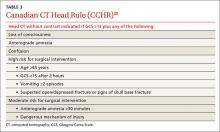
With mild head injury, recommendations for follow-up are less straightforward. The New Orleans Criteria (NOC) and Canadian CT Head Rule (CCHR) are commonly used in triaging patients with minor head trauma in a cost effective way11 (TABLES 219 and 320). The cost-effectiveness of these assessment tools is still questionable, but both have very high sensitivity for identifying patients who will require neurosurgery intervention.21,22 Although the NOC is slightly more sensitive at identifying patients with nonsurgical clinically significant abnormalities, it has a greatly reduced specificity compared with the CCHR.23-25
›› And you order...
…a non-contrast head CT.
Mr. C presents with a GCS of 15, indicating mild head trauma. However, in elderly patients, especially ones taking anticoagulation medication, even mild trauma can result in clinically significant abnormalities such as a subdural hematoma.1 Although Mr. C’s physical and neurologic exams are not worrisome, both the NOC and CCHR recommend further evaluation with a non-contrast head CT based on his age.
CORRESPONDENCE
Urmi A. Desai, MD, MS, Columbia University Medical Center, 610 West 158th Street, New York, NY 10032; [email protected].
1. American College of Radiology. Appropriateness criteria. American College of Radiology Web site. Available at: https://acsearch.acr.org/list. Accessed January 4, 2015.
2. American College of Radiology. About the ACR appropriateness criteria. American College of Radiology Web site. Available at: http://www.acr.org/Quality-Safety/Appropriateness-Criteria/About-AC. Accessed July 20, 2015.
3. Becker LA, Green LA, Beaufait D, et al. Use of CT scans for the investigation of headache: a report from ASPN, Part 1. J Fam Pract. 1993;37:129-134.
4. Sandrini G, Friberg L, Jänig W, et al. Neurophysiological tests and neuroimaging procedures in non-acute headache: guidelines and recommendations. Eur J Neurol. 2004;11:217-224.
5. Sempere AP, Porta-Etessam J, Medrano V, et al. Neuroimaging in the evaluation of patients with non-acute headache. Cephalalgia. 2005;25:30-35.
6. Gilbert JW, Johnson KM, Larkin GL, et al. Atraumatic headache in US emergency departments: recent trends in CT/MRI utilisation and factors associated with severe intracranial pathology. Emerg Med J. 2012;29:576-581.
7. Tsushima Y, Endo K. MR imaging in the evaluation of chronic or recurrent headache. Radiology. 2005;235:575-579.
8. Jordan JE, Ramirez GF, Bradley WG, et al. Economic and outcomes assessment of magnetic resonance imaging in the evaluation of headache. J Natl Med Assoc. 2000;92:573-578.
9. Mitchell CS, Osborn RE, Grosskreutz SR. Computed tomography in the headache patient: is routine evaluation really necessary? Headache. 1993;33:82-86.
10. Frishberg BM. The utility of neuroimaging in the evaluation of headache in patients with normal neurologic examinations. Neurology. 1994;44:1191-1197.
11. Osborn AG. Osborn’s Brain: Imaging, Pathology, and Anatomy. Salt Lake City, Utah: Amirsys Publishing; 2013.
12. Silberstein SD. Chronic daily headache. J Am Osteopath Assoc. 2005;105:23S-29S.
13. Douglas AC, Wippold FJ 2nd, Broderick DF, et al. ACR Appropriateness Criteria Headache. J Am Coll Radiol. 2014;11:657-667.
14. Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1143-1153.
15. Wippold FJ 2nd, Brown DC, Broderick DF, et al. ACR Appropriateness Criteria Dementia and Movement Disorders. J Am Coll Radiol. 2015;12:19-28.
16. Kantarci K, Jack CR Jr. Neuroimaging in Alzheimer disease: an evidence-based review. Neuroimaging Clin N Am. 2003;13:197-209.
17. Teasdale G, Maas A, Lecky F, et al. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol. 2014;13:844-854.
18. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-84.
19. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343:100-105.
20. Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391-1396.
21. Davis PC, Drayer BP, Anderson RE, et al. Head trauma. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215 Suppl:507-524.
22. Stiell IG, Clement CM, Grimshaw JM, et al. A prospective clusterrandomized trial to implement the Canadian CT Head Rule in emergency departments. CMAJ. 2010;182:1527-1532.
23. Smits M, Dippel DW, Nederkoorn PJ, et al. Minor head injury: CT-based strategies for management—a cost-effectiveness analysis. Radiology. 2010;254:532-540.
24. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294:1511-1518.
25. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA. 2005;294:1519-1525.
› Use clinical decision tools and American College of Radiology Appropriateness Criteria to determine levels of evidence for ordering specific imaging studies. A
› Consider ordering an imaging study when headache is accompanied by a new neurologic symptom. Computed tomography (CT) without contrast is best for patients who are acutely ill. In the non-emergent setting, magnetic resonance imaging (MRI) with contrast is the optimal study. A
› Order structural neuroimaging as part of the initial work-up of suspected dementia. MRI is the test of choice. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When patients present with neurologic complaints in outpatient primary care practice, 2 key questions often arise: Should brain imaging be ordered, and if so, which study? Careful history-taking and physical exam findings can suggest differential diagnoses and help determine whether imaging studies could identify potential underlying causes. Further considerations in making a decision are the type of information each modality offers, the possible need for contrast media, benefits vs radiation exposure risks, potential contraindications, and cost and local availability. In this article, we present 3 common outpatient scenarios, and in each case we describe the evidence to support clinical decision-making about imaging.
The American College of Radiology (ACR) Appropriateness Criteria Web site (http://www.acr.org/Quality-Safety/Appropriateness-Criteria) provides radiation exposure information, numerical ratings of imaging studies for individual clinical scenarios, evidence tables, and reference tables for each of its recommendations.1 ACR’s recommendations were developed by expert panels of diagnostic radiologists, interventional radiologists, and radiation oncologists, and designed to help physicians order the most appropriate imaging studies based on patients’ clinical conditions.2 We used these criteria to develop an evaluation strategy for each of our clinical scenarios.
CASE 1 › Carrie D is a 45-year-old woman with a history of migraine without aura generally controlled with Excedrin (acetaminophen, aspirin, and caffeine). She arrives at your office with a 2-day history of severe headache over the top of her head and associated tingling sensation over the left side of her face, but with no vision changes, weakness, or slurred speech. She denies any prior history of numbness or tinging with past headaches. She is a business executive and reports that in the last few weeks, her company has been involved in a high-profile merger. On physical exam, her vital signs are within normal limits. She does not appear acutely ill, but on exam she reports diminished sensation to light touch over the left side of her face, left arm, and left leg compared with the right side.
›› What imaging options might you consider?
A prospective review of physicians in an ambulatory family practice setting found that neurologic imaging was typically ordered for patients with headache who were suspected of having a brain tumor or subarachnoid hemorrhage.3 For our patient, who has a history of migraines without aura and whose current severe headache is accompanied by an abnormal sensation on one side of the face, the following questions are relevant: Is this presentation part of her primary headache syndrome or could there be a different cause? If there is a different cause, is it likely to be detected with brain imaging such as computed tomography (CT) or magnetic resonance imaging (MRI)?
Patients with isolated headache and an absence of neurologic symptoms or abnormalities on neurologic exam are unlikely to have a clinically significant intracranial abnormality.4-10 Imaging of the brain is typically not indicated for these patients.2 However, given that this patient does have a positive focal neurologic finding, a CT or MRI is indicated, as findings are more likely to influence management decisions.
The decision to order CT or MRI should be based on how acutely ill the patient is. CT without contrast is an excellent tool to rule out suspected emergent intracranial abnormalities such as an intracranial hemorrhage, hydrocephalus, or a mass.11 In patients presenting with symptoms suggesting acute illness such as carotid or vertebral artery dissection, the most appropriate test would be CT angiography of the head and neck.2
However, the list of less dire causes of headache is vast. Included in this list would be trauma, other vascular disorders such as arteriovenous malformation or temporal arteritis, infection, abnormal intracranial pressure (mass, pseudotumor cerebri, intracranial hypotension), and disorders of the head/face/spine (eg, temporomandibular joint disorder).12
In the non-acute setting where a patient has stable vital signs and is not in acute distress, an MRI with contrast would be the most appropriate test to identify such causes. Avoid contrast only if there is a firm contraindication, such as pregnancy, severely impaired renal function, or known allergy to gadolinium. If history and physical exam findings suggest possible stroke, arrange for MRI and MR angiography with contrast, even if the result of a head CT scan is negative. The ALGORITHM13 offers guidance for choosing imaging studies for headache based on history, physical exam, and laboratory findings.
›› And you order...
…an MRI of the brain with contrast.
Though Ms. D does have a focal neurologic finding in addition to her headache, she does not appear to be acutely ill. Ordering an MRI with contrast is the best first step.
CASE 2 › Anne B is a 72-year-old woman with a history of hypertension, hyperlipidemia, and type 2 diabetes. Her daughter brings her in to see you because she is concerned about Ms. B’s memory. Ms. B’s daughter reports that she has become increasingly forgetful over the past 6 months, often forgetting recent events. At first the forgetfulness was occasional, but now it seems to happen daily and interfere with activities of daily living (ADLs). The week before this visit, Ms. B left a pot heating on the stove because she forgot she had started cooking. She realized what had happened only when her smoke alarm went off. Ms. B’s daughter also thinks her mother may be taking some of her medications incorrectly.
Physical exam and laboratory findings are unremarkable. On the mental status exam, Ms. B has difficulty with registration and recall.
›› What imaging options might you consider?
Ms. B has exhibited progressive memory loss over 6 months and it is now affecting her ADLs. Her symptoms could be secondary to any one of many reversible medical causes, such as adverse medication effects, depression, or vitamin B12 deficiency. If clinical and laboratory evaluations exclude these reversible causes, consider dementia.
With numerous disorders having overlapping symptoms, the diagnosis of degenerative central nervous system (CNS) disease can be extremely tricky. Complicating the issue is the fact that a single patient can have 2 or more concurrent neurodegenerative diseases. Clinical testing is essential in the diagnosis and management of degenerative CNS diseases, but testing sensitivity and specificity are highly variable depending upon the disease.14
Neuroimaging is an important supplement to clinical testing in excluding intracranial abnormalities. There are significant negative consequences of missing reversible causes of memory problems and incorrectly assigning a clinical diagnosis of dementia. Neuroimaging can be subdivided into structural and functional imaging, and structural imaging is the first step in evaluation.15
The American Academy of Neurology recommends the use of structural neuroimaging with CT or MRI in the initial evaluation of patients with dementia to detect such treatable problems as a subdural hematoma, frontal lobe mass, or hydrocephalus.12 Structural imaging may also identify anatomic changes characteristic of degenerative CNS diseases such as Alzheimer’s disease, dementia with Lewy bodies, frontotemporal dementia, vascular dementia, Creutzfeldt-Jakob disease, and Huntington’s disease; however, sensitivities and specificities of testing are low.14
›› And you order...
…an MRI of the brain without contrast.
In Ms. B’s case, structural neuroimaging is indicated as part of the initial work-up of supposed dementia. An MRI without contrast is recommended over CT because it is more sensitive in detecting white matter changes in vascular dementia.16 In cases where an MRI >is unavailable or contraindicated (eg, a patient with a pacemaker), a CT is a reasonable alternative.
CASE 3 › Bob C is a 78-year-old man with a history of chronic obstructive pulmonary disease and hypertension who arrives at your walk-in clinic accompanied by his home health aide a few hours after having tripped and fallen over a rug at home. At baseline, Mr. C is ambulatory and independent in ADLs.
He takes all of his medications, including a daily baby aspirin (81 mg). Mr. C says he did not lose consciousness at the time of the fall and insists he feels fine, but you notice a bruise developing over his right temporal skull.
›› What imaging options might you consider?
With acute head trauma deemed severe enough clinically to warrant imaging, non-contrast CT is the most appropriate initial test to identify possible intracranial hemorrhage.11 The Glasgow Coma Scale (GCS) is the tool most widely used for clinical evaluation17 (TABLE 118). The score is based on an assessment of 3 features: eye response, speech, and movement. Head injury is classified as mild (13-15), moderate (9-12), or severe (≤8). It is universally agreed that patients with moderate or severe head injury should be further evaluated with a head CT.
With mild head injury, recommendations for follow-up are less straightforward. The New Orleans Criteria (NOC) and Canadian CT Head Rule (CCHR) are commonly used in triaging patients with minor head trauma in a cost effective way11 (TABLES 219 and 320). The cost-effectiveness of these assessment tools is still questionable, but both have very high sensitivity for identifying patients who will require neurosurgery intervention.21,22 Although the NOC is slightly more sensitive at identifying patients with nonsurgical clinically significant abnormalities, it has a greatly reduced specificity compared with the CCHR.23-25
›› And you order...
…a non-contrast head CT.
Mr. C presents with a GCS of 15, indicating mild head trauma. However, in elderly patients, especially ones taking anticoagulation medication, even mild trauma can result in clinically significant abnormalities such as a subdural hematoma.1 Although Mr. C’s physical and neurologic exams are not worrisome, both the NOC and CCHR recommend further evaluation with a non-contrast head CT based on his age.
CORRESPONDENCE
Urmi A. Desai, MD, MS, Columbia University Medical Center, 610 West 158th Street, New York, NY 10032; [email protected].
› Use clinical decision tools and American College of Radiology Appropriateness Criteria to determine levels of evidence for ordering specific imaging studies. A
› Consider ordering an imaging study when headache is accompanied by a new neurologic symptom. Computed tomography (CT) without contrast is best for patients who are acutely ill. In the non-emergent setting, magnetic resonance imaging (MRI) with contrast is the optimal study. A
› Order structural neuroimaging as part of the initial work-up of suspected dementia. MRI is the test of choice. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When patients present with neurologic complaints in outpatient primary care practice, 2 key questions often arise: Should brain imaging be ordered, and if so, which study? Careful history-taking and physical exam findings can suggest differential diagnoses and help determine whether imaging studies could identify potential underlying causes. Further considerations in making a decision are the type of information each modality offers, the possible need for contrast media, benefits vs radiation exposure risks, potential contraindications, and cost and local availability. In this article, we present 3 common outpatient scenarios, and in each case we describe the evidence to support clinical decision-making about imaging.
The American College of Radiology (ACR) Appropriateness Criteria Web site (http://www.acr.org/Quality-Safety/Appropriateness-Criteria) provides radiation exposure information, numerical ratings of imaging studies for individual clinical scenarios, evidence tables, and reference tables for each of its recommendations.1 ACR’s recommendations were developed by expert panels of diagnostic radiologists, interventional radiologists, and radiation oncologists, and designed to help physicians order the most appropriate imaging studies based on patients’ clinical conditions.2 We used these criteria to develop an evaluation strategy for each of our clinical scenarios.
CASE 1 › Carrie D is a 45-year-old woman with a history of migraine without aura generally controlled with Excedrin (acetaminophen, aspirin, and caffeine). She arrives at your office with a 2-day history of severe headache over the top of her head and associated tingling sensation over the left side of her face, but with no vision changes, weakness, or slurred speech. She denies any prior history of numbness or tinging with past headaches. She is a business executive and reports that in the last few weeks, her company has been involved in a high-profile merger. On physical exam, her vital signs are within normal limits. She does not appear acutely ill, but on exam she reports diminished sensation to light touch over the left side of her face, left arm, and left leg compared with the right side.
›› What imaging options might you consider?
A prospective review of physicians in an ambulatory family practice setting found that neurologic imaging was typically ordered for patients with headache who were suspected of having a brain tumor or subarachnoid hemorrhage.3 For our patient, who has a history of migraines without aura and whose current severe headache is accompanied by an abnormal sensation on one side of the face, the following questions are relevant: Is this presentation part of her primary headache syndrome or could there be a different cause? If there is a different cause, is it likely to be detected with brain imaging such as computed tomography (CT) or magnetic resonance imaging (MRI)?
Patients with isolated headache and an absence of neurologic symptoms or abnormalities on neurologic exam are unlikely to have a clinically significant intracranial abnormality.4-10 Imaging of the brain is typically not indicated for these patients.2 However, given that this patient does have a positive focal neurologic finding, a CT or MRI is indicated, as findings are more likely to influence management decisions.
The decision to order CT or MRI should be based on how acutely ill the patient is. CT without contrast is an excellent tool to rule out suspected emergent intracranial abnormalities such as an intracranial hemorrhage, hydrocephalus, or a mass.11 In patients presenting with symptoms suggesting acute illness such as carotid or vertebral artery dissection, the most appropriate test would be CT angiography of the head and neck.2
However, the list of less dire causes of headache is vast. Included in this list would be trauma, other vascular disorders such as arteriovenous malformation or temporal arteritis, infection, abnormal intracranial pressure (mass, pseudotumor cerebri, intracranial hypotension), and disorders of the head/face/spine (eg, temporomandibular joint disorder).12
In the non-acute setting where a patient has stable vital signs and is not in acute distress, an MRI with contrast would be the most appropriate test to identify such causes. Avoid contrast only if there is a firm contraindication, such as pregnancy, severely impaired renal function, or known allergy to gadolinium. If history and physical exam findings suggest possible stroke, arrange for MRI and MR angiography with contrast, even if the result of a head CT scan is negative. The ALGORITHM13 offers guidance for choosing imaging studies for headache based on history, physical exam, and laboratory findings.
›› And you order...
…an MRI of the brain with contrast.
Though Ms. D does have a focal neurologic finding in addition to her headache, she does not appear to be acutely ill. Ordering an MRI with contrast is the best first step.
CASE 2 › Anne B is a 72-year-old woman with a history of hypertension, hyperlipidemia, and type 2 diabetes. Her daughter brings her in to see you because she is concerned about Ms. B’s memory. Ms. B’s daughter reports that she has become increasingly forgetful over the past 6 months, often forgetting recent events. At first the forgetfulness was occasional, but now it seems to happen daily and interfere with activities of daily living (ADLs). The week before this visit, Ms. B left a pot heating on the stove because she forgot she had started cooking. She realized what had happened only when her smoke alarm went off. Ms. B’s daughter also thinks her mother may be taking some of her medications incorrectly.
Physical exam and laboratory findings are unremarkable. On the mental status exam, Ms. B has difficulty with registration and recall.
›› What imaging options might you consider?
Ms. B has exhibited progressive memory loss over 6 months and it is now affecting her ADLs. Her symptoms could be secondary to any one of many reversible medical causes, such as adverse medication effects, depression, or vitamin B12 deficiency. If clinical and laboratory evaluations exclude these reversible causes, consider dementia.
With numerous disorders having overlapping symptoms, the diagnosis of degenerative central nervous system (CNS) disease can be extremely tricky. Complicating the issue is the fact that a single patient can have 2 or more concurrent neurodegenerative diseases. Clinical testing is essential in the diagnosis and management of degenerative CNS diseases, but testing sensitivity and specificity are highly variable depending upon the disease.14
Neuroimaging is an important supplement to clinical testing in excluding intracranial abnormalities. There are significant negative consequences of missing reversible causes of memory problems and incorrectly assigning a clinical diagnosis of dementia. Neuroimaging can be subdivided into structural and functional imaging, and structural imaging is the first step in evaluation.15
The American Academy of Neurology recommends the use of structural neuroimaging with CT or MRI in the initial evaluation of patients with dementia to detect such treatable problems as a subdural hematoma, frontal lobe mass, or hydrocephalus.12 Structural imaging may also identify anatomic changes characteristic of degenerative CNS diseases such as Alzheimer’s disease, dementia with Lewy bodies, frontotemporal dementia, vascular dementia, Creutzfeldt-Jakob disease, and Huntington’s disease; however, sensitivities and specificities of testing are low.14
›› And you order...
…an MRI of the brain without contrast.
In Ms. B’s case, structural neuroimaging is indicated as part of the initial work-up of supposed dementia. An MRI without contrast is recommended over CT because it is more sensitive in detecting white matter changes in vascular dementia.16 In cases where an MRI >is unavailable or contraindicated (eg, a patient with a pacemaker), a CT is a reasonable alternative.
CASE 3 › Bob C is a 78-year-old man with a history of chronic obstructive pulmonary disease and hypertension who arrives at your walk-in clinic accompanied by his home health aide a few hours after having tripped and fallen over a rug at home. At baseline, Mr. C is ambulatory and independent in ADLs.
He takes all of his medications, including a daily baby aspirin (81 mg). Mr. C says he did not lose consciousness at the time of the fall and insists he feels fine, but you notice a bruise developing over his right temporal skull.
›› What imaging options might you consider?
With acute head trauma deemed severe enough clinically to warrant imaging, non-contrast CT is the most appropriate initial test to identify possible intracranial hemorrhage.11 The Glasgow Coma Scale (GCS) is the tool most widely used for clinical evaluation17 (TABLE 118). The score is based on an assessment of 3 features: eye response, speech, and movement. Head injury is classified as mild (13-15), moderate (9-12), or severe (≤8). It is universally agreed that patients with moderate or severe head injury should be further evaluated with a head CT.
With mild head injury, recommendations for follow-up are less straightforward. The New Orleans Criteria (NOC) and Canadian CT Head Rule (CCHR) are commonly used in triaging patients with minor head trauma in a cost effective way11 (TABLES 219 and 320). The cost-effectiveness of these assessment tools is still questionable, but both have very high sensitivity for identifying patients who will require neurosurgery intervention.21,22 Although the NOC is slightly more sensitive at identifying patients with nonsurgical clinically significant abnormalities, it has a greatly reduced specificity compared with the CCHR.23-25
›› And you order...
…a non-contrast head CT.
Mr. C presents with a GCS of 15, indicating mild head trauma. However, in elderly patients, especially ones taking anticoagulation medication, even mild trauma can result in clinically significant abnormalities such as a subdural hematoma.1 Although Mr. C’s physical and neurologic exams are not worrisome, both the NOC and CCHR recommend further evaluation with a non-contrast head CT based on his age.
CORRESPONDENCE
Urmi A. Desai, MD, MS, Columbia University Medical Center, 610 West 158th Street, New York, NY 10032; [email protected].
1. American College of Radiology. Appropriateness criteria. American College of Radiology Web site. Available at: https://acsearch.acr.org/list. Accessed January 4, 2015.
2. American College of Radiology. About the ACR appropriateness criteria. American College of Radiology Web site. Available at: http://www.acr.org/Quality-Safety/Appropriateness-Criteria/About-AC. Accessed July 20, 2015.
3. Becker LA, Green LA, Beaufait D, et al. Use of CT scans for the investigation of headache: a report from ASPN, Part 1. J Fam Pract. 1993;37:129-134.
4. Sandrini G, Friberg L, Jänig W, et al. Neurophysiological tests and neuroimaging procedures in non-acute headache: guidelines and recommendations. Eur J Neurol. 2004;11:217-224.
5. Sempere AP, Porta-Etessam J, Medrano V, et al. Neuroimaging in the evaluation of patients with non-acute headache. Cephalalgia. 2005;25:30-35.
6. Gilbert JW, Johnson KM, Larkin GL, et al. Atraumatic headache in US emergency departments: recent trends in CT/MRI utilisation and factors associated with severe intracranial pathology. Emerg Med J. 2012;29:576-581.
7. Tsushima Y, Endo K. MR imaging in the evaluation of chronic or recurrent headache. Radiology. 2005;235:575-579.
8. Jordan JE, Ramirez GF, Bradley WG, et al. Economic and outcomes assessment of magnetic resonance imaging in the evaluation of headache. J Natl Med Assoc. 2000;92:573-578.
9. Mitchell CS, Osborn RE, Grosskreutz SR. Computed tomography in the headache patient: is routine evaluation really necessary? Headache. 1993;33:82-86.
10. Frishberg BM. The utility of neuroimaging in the evaluation of headache in patients with normal neurologic examinations. Neurology. 1994;44:1191-1197.
11. Osborn AG. Osborn’s Brain: Imaging, Pathology, and Anatomy. Salt Lake City, Utah: Amirsys Publishing; 2013.
12. Silberstein SD. Chronic daily headache. J Am Osteopath Assoc. 2005;105:23S-29S.
13. Douglas AC, Wippold FJ 2nd, Broderick DF, et al. ACR Appropriateness Criteria Headache. J Am Coll Radiol. 2014;11:657-667.
14. Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1143-1153.
15. Wippold FJ 2nd, Brown DC, Broderick DF, et al. ACR Appropriateness Criteria Dementia and Movement Disorders. J Am Coll Radiol. 2015;12:19-28.
16. Kantarci K, Jack CR Jr. Neuroimaging in Alzheimer disease: an evidence-based review. Neuroimaging Clin N Am. 2003;13:197-209.
17. Teasdale G, Maas A, Lecky F, et al. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol. 2014;13:844-854.
18. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-84.
19. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343:100-105.
20. Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391-1396.
21. Davis PC, Drayer BP, Anderson RE, et al. Head trauma. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215 Suppl:507-524.
22. Stiell IG, Clement CM, Grimshaw JM, et al. A prospective clusterrandomized trial to implement the Canadian CT Head Rule in emergency departments. CMAJ. 2010;182:1527-1532.
23. Smits M, Dippel DW, Nederkoorn PJ, et al. Minor head injury: CT-based strategies for management—a cost-effectiveness analysis. Radiology. 2010;254:532-540.
24. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294:1511-1518.
25. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA. 2005;294:1519-1525.
1. American College of Radiology. Appropriateness criteria. American College of Radiology Web site. Available at: https://acsearch.acr.org/list. Accessed January 4, 2015.
2. American College of Radiology. About the ACR appropriateness criteria. American College of Radiology Web site. Available at: http://www.acr.org/Quality-Safety/Appropriateness-Criteria/About-AC. Accessed July 20, 2015.
3. Becker LA, Green LA, Beaufait D, et al. Use of CT scans for the investigation of headache: a report from ASPN, Part 1. J Fam Pract. 1993;37:129-134.
4. Sandrini G, Friberg L, Jänig W, et al. Neurophysiological tests and neuroimaging procedures in non-acute headache: guidelines and recommendations. Eur J Neurol. 2004;11:217-224.
5. Sempere AP, Porta-Etessam J, Medrano V, et al. Neuroimaging in the evaluation of patients with non-acute headache. Cephalalgia. 2005;25:30-35.
6. Gilbert JW, Johnson KM, Larkin GL, et al. Atraumatic headache in US emergency departments: recent trends in CT/MRI utilisation and factors associated with severe intracranial pathology. Emerg Med J. 2012;29:576-581.
7. Tsushima Y, Endo K. MR imaging in the evaluation of chronic or recurrent headache. Radiology. 2005;235:575-579.
8. Jordan JE, Ramirez GF, Bradley WG, et al. Economic and outcomes assessment of magnetic resonance imaging in the evaluation of headache. J Natl Med Assoc. 2000;92:573-578.
9. Mitchell CS, Osborn RE, Grosskreutz SR. Computed tomography in the headache patient: is routine evaluation really necessary? Headache. 1993;33:82-86.
10. Frishberg BM. The utility of neuroimaging in the evaluation of headache in patients with normal neurologic examinations. Neurology. 1994;44:1191-1197.
11. Osborn AG. Osborn’s Brain: Imaging, Pathology, and Anatomy. Salt Lake City, Utah: Amirsys Publishing; 2013.
12. Silberstein SD. Chronic daily headache. J Am Osteopath Assoc. 2005;105:23S-29S.
13. Douglas AC, Wippold FJ 2nd, Broderick DF, et al. ACR Appropriateness Criteria Headache. J Am Coll Radiol. 2014;11:657-667.
14. Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1143-1153.
15. Wippold FJ 2nd, Brown DC, Broderick DF, et al. ACR Appropriateness Criteria Dementia and Movement Disorders. J Am Coll Radiol. 2015;12:19-28.
16. Kantarci K, Jack CR Jr. Neuroimaging in Alzheimer disease: an evidence-based review. Neuroimaging Clin N Am. 2003;13:197-209.
17. Teasdale G, Maas A, Lecky F, et al. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol. 2014;13:844-854.
18. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-84.
19. Haydel MJ, Preston CA, Mills TJ, et al. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343:100-105.
20. Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357:1391-1396.
21. Davis PC, Drayer BP, Anderson RE, et al. Head trauma. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215 Suppl:507-524.
22. Stiell IG, Clement CM, Grimshaw JM, et al. A prospective clusterrandomized trial to implement the Canadian CT Head Rule in emergency departments. CMAJ. 2010;182:1527-1532.
23. Smits M, Dippel DW, Nederkoorn PJ, et al. Minor head injury: CT-based strategies for management—a cost-effectiveness analysis. Radiology. 2010;254:532-540.
24. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294:1511-1518.
25. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA. 2005;294:1519-1525.