User login
› Choose ultrasonography as the initial imaging test for patients with pain in the right upper quadrant. C
› Order computed tomography with contrast of the abdomen and/or pelvis for adults with acute pain of new onset in the right or left lower quadrant, or both. C
› Recommend ultrasound with graded compression as the initial imaging modality for children younger than 14 years who have acute right lower quadrant pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Harry L, age 54, presents with acute onset abdominal pain that began 2 days ago. He reports mild nausea but no vomiting, non-bloody diarrhea, and feeling feverish. The patient denies increased pain with movement.
If Mr. L were your patient, how would you proceed?
Although acute nontraumatic abdominal pain accounts for only about 1.5% of physician office visits, it is the cause of approximately 8% of visits—more than 11 million, a year—to US emergency departments.1,2 In most cases, the location of the pain, coupled with the patient history, physical exam, and clinical judgment, lead to the differential diagnosis and determines what type of imaging, if any, is needed.
Benign self-limiting causes of abdominal pain, such as constipation or gastroenteritis, may not require any imaging. However, if the patient has abdominal pain and fever, is older than age 65, or presents with peritoneal signs and symptoms, imaging will be a crucial diagnostic aid.3,4
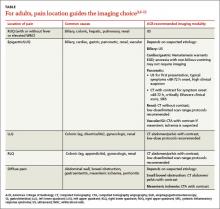
With that in mind, the American College of Radiology (ACR) has developed a 9-point scoring criteria based on both the site and common causes of abdominal pain to determine the best imaging modality to use to rule in—or out—serious disease and conditions for which surgery is required. A rating of 1, 2, or 3 indicates that imaging is usually not appropriate; a rating of 4, 5, or 6 means the imaging test may be appropriate, and a rating of 7, 8, or 9 indicates that the recommended test is usually appropriate. The panel of experts who developed the scores considered the relative radiation level of each imaging modality, as well.5
In the text and TABLE3,6-12 that follow, you’ll find the most likely clinical diagnoses and the optimal tests for abdominal pain, based largely on where it hurts.
CASE 1 › Appendicitis: An 8-year-old girl presented with acute right lower quadrant pain and underwent an ultrasound (left), which showed a dilated ~2 cm (normal <6 mm) non-compressible appendix consistent with acute appendicitis. There was no significant free fluid within the right lower quadrant. Follow-up computed tomography (CT) scan (middle) with IV and oral contrast confirmed the dilated appendix with no evidence of perforation or abscess formation.
CASE 2 › Small bowel obstruction: A 54-year-old man sought care for abdominal pain and distention. A CT with IV and oral contrast (right) revealed multiple, fluid-filled dilated loops of small bowel (arrows) with bowel wall thickening, edema, and inflammatory stranding. The short segment of decreased enhancement (arrowhead) was consistent with bowel ischemia.
Right upper quadrant pain: Beware of acute biliary disease
Abdominal pain of the right upper quadrant (RUQ) is typically related to biliary, colonic, hepatic, or renal causes.12 Because of infection and the potential need for surgical intervention, untreated acute biliary disease can become life-threatening, particularly in the elderly.4
The ACR recommends ultrasound (US) as the initial imaging study for RUQ pain, regardless of whether the patient is febrile or has an elevated white blood cell count or a positive Murphy’s sign (demonstrated at youtube.com/watch?v=9L7N89sOSuc) (score=9). A 2012 meta-analysis found that US has a sensitivity of 81% and specificity of 83% for diagnosing acute cholecystitis.6
Although cholescintigraphy has a higher sensitivity and specificity (96% and 90%, respectively), US remains the initial study of choice because of its availability, study time, and the lack of ionizing radiation. For equivocal findings, computed tomography (CT), magnetic resonance imaging (MRI), and cholescintigraphy have similar levels of evidence.6
Epigastric/left upper quadrant pain: Consider pancreatits
Epigastric and left upper quadrant (LUQ) pain may have a gastric, biliary, pancreatic, vascular, renal, or cardiac etiology.12 The ACR criteria for testing depends on the type of pain suspected.
Pancreatitis. The Revised Atlanta Classification of Acute Pancreatitis requires 2 of the 3 classic criteria for a pancreatitis diagnosis: 1) abdominal pain suggestive of pancreatitis, 2) serum amylase and lipase levels ≥3 times the normal level, and 3) characteristic findings on imaging.13 The ACR recommends US as the initial imaging modality for suspected acute pancreatitis when it is the initial presentation, the patient has typical abdominal pain and increased serum amylase and lipase, and symptom onset was <48 to 72 hours before the patient sought care (score=9).7
For patients who are critically ill, meet the criteria for systemic inflammatory response syndrome (SIRS), have severe clinical scores on either the Acute Physiology and Chronic Health Evaluation (APACHE) II (available at clincalc.com/icumortality/apacheii.aspx) or Bedside Index for Severity in Acute Appendicitis (BISAP; mdcalc.com/bisap-score-for-pancreatitis-mortality/), or who present >48 to 72 hours after onset of symptoms, abdominal CT with contrast is recommended (score=8).
Urolithiasis. Patients with abdominal pain from a presumed renal source should undergo a non-contrast CT of the abdomen and pelvis for initial imaging, according to the ACR (score=8). The sensitivity is 95% to 96% and specificity is 98%.8 To limit radiation exposure, low-dose protocols and limiting scan range are preferred.
Radiography can be useful in patients with known kidney stone disease and previous films; however, the sensitivity in other patients is poor (58%-62%).8 Because pelviectasis and ureterectasis can take hours to develop, US will miss more than 30% of acute obstructions in patients who are not fully hydrated and is therefore not recommended as a first-line imaging modality.8 The sensitivity of US increases to 71% when it is combined with kidney, ureter, and bladder radiography, but is still lower than that of CT or IV urography.8
Left lower quadrant pain: Suspect sigmoid diverticulitis
The differential for left lower quadrant (LLQ) pain includes colonic, gynecologic, and renal etiologies.12 The most common cause in adults is acute sigmoid diverticulitis. Patients often present with the clinical triad of fever, LLQ pain, and leukocytosis.14 A decision to obtain imaging should be based on both the clinical presentation and examination. It may not be required for patients who have mild symptoms or have had previous episodes of diverticulitis.
Clinical scoring systems have been studied for LLQ pain. However, none has been validated in all settings and therefore no such system is routinely used.15 CT of the abdomen and pelvis with contrast media is the ACR’s recommendation for the initial imaging study (score=9). CT has a reported overall accuracy of 99%.9
CT can also assess the severity of disease and help determine medical vs surgical treatment.14 US using graded compression has a sensitivity of 77% to 98% and a specificity of 80% to 99%, but is limited by body habitus, technical expertise, and patient comfort. Therefore, US has not gained widespread use (score=4) for patients with LLQ pain.9,14 MRI is emerging as a potential option; however, longer scan times, cost, and availability continue to limit its use.14
Right lower quadrant pain: Is it appendicitis?
The differential for right lower quadrant (RLQ) pain, like that of LLQ pain, includes colonic, gynecologic, and renal etiologies.12 The most common cause of acute RLQ pain requiring surgery is appendicitis. History and physical exam achieve a diagnostic accuracy of 80%.16
If the diagnosis is clear, no imaging is warranted. In patients with equivocal clinical presentations, however, imaging is cost-effective and may reduce the rate of perforation, morbidity, mortality, and postoperative hospital stays.16 In addition, the accuracy of clinical diagnosis for elderly patients and women of childbearing age with RLQ pain tends to be lower than that of adult men. Therefore, some experts call for a lower imaging threshold for these populations.
CT of the abdomen and pelvis with contrast is the recommended initial imaging study in nonpregnant adults (score=8). CT has a sensitivity and specificity of 91% and 90%, respectively.10
CT without contrast is indicated for patients with RLQ pain who have a contraindication to contrast media, although the relative radiation level remains the same.
If limiting radiation exposure is especially important, consider US, followed by CT with contrast if US is inconclusive.10
Low-dose CT has been investigated as an alternative, but is not routinely used. A limited abdominal CT scan from the bottom of the body of the T10 vertebra to the top of the symphysis pubis allows for adequate evaluation and alternate diagnoses of concern when compared with full CT scans of the abdomen and pelvis.17 This limited CT scan has been found to result in a total body effective radiation dose reduction of 23% and, in women, a breast equivalent dose reduction of 85%, without missing a single case of acute appendicitis or pertinent alternative diagnoses.17
Diffuse abdominal pain: Suspect a blockage
Finally, some patients may present with diffuse or non-localizable pain with fever. The etiologies that often present with diffuse or nonspecific pain include small bowel obstruction and mesenteric ischemia.
Small bowel obstruction. When small bowel obstruction is suspected, CT of the abdomen and pelvis with contrast (score=9) is recommended. Oral contrast is not indicated if you suspect a high-grade obstruction, but may add functional information when only a partial or low-grade obstruction is suspected. The relative radiation level remains the same for both.11 For patients with pain and fever, postoperative or not, CT of the abdomen and pelvis with contrast is recommended (score=8).3
Mesenteric ischemia is associated with high morbidity and mortality rates (30%-90%).18,19 Acute mesenteric ischemia is most commonly secondary to embolism, followed by arterial thrombosis, non-occlusive ischemia, and less commonly, venous thrombosis.18 The typical presentation is pain out of proportion to the physical exam.19
Differentiating mesenteric ischemia from other causes of acute abdominal pain can be difficult. Patients with chronic mesenteric ischemia present with postprandial abdominal pain, weight loss, and food avoidance. Although radiography is often the initial test ordered, a negative test does not rule out mesenteric ischemia. Therefore, the ACR recommends CT angiography (CTA) of the abdomen with contrast for the evaluation of both acute and chronic mesenteric ischemia (score=9). US can be useful for excluding other causes of abdominal pain, as well as ischemia related to venous occlusion, but it has a low sensitivity (70%-89%)18 overall and therefore is not recommended as the initial test for acute or chronic mesenteric ischemia.
Magnetic resonance angiography (MRA) has a high sensitivity and specificity for severe stenosis or origin occlusions of the superior mesenteric artery and celiac axis; however, its ability to determine distal embolism and non-occlusive ischemia, and the length and availability of this test limit its usefulness.18
When the patient is a child
Imaging for bilious vomiting in infants up to 3 months varies based on age. In the first week of life, radiography of the abdomen is the ACR’s recommended first-line test (score=9).20 An upper GI series or contrast enema are also options, but less preferred due to their increased radiation exposure.20
For infants between one week and 3 months of age, an upper GI series is the study of choice (score=9) and radiography of the abdomen is second line (score=5). An upper GI series is recommended to evaluate non-bilious, intermittent non-projectile vomiting in those from birth to 3 months.20 Projectile non-bilious vomiting should be evaluated with US of the abdomen.20
In children with RLQ pain suggestive of acute appendicitis, US is the first line imaging method due to its relatively high sensitivity and specificity and lack of ionizing radiation (score=9).10 If US is inconclusive, then CT of the abdomen and pelvis with IV contrast, but not oral or rectal contrast, is recommended (score=7). Although MRI is a non-radiating modality, it should be reserved for use only in specialized pediatric facilities due to lack of experience, increased cost, and the usual need for sedation.10
CASE › Mr. L’s vital signs demonstrated mild tachycardia and his body temperature was 100.5° F. His physical exam revealed significant tenderness to palpation in the LL Q, but no rebound or guarding. A CT scan with contrast of the abdomen revealed diverticulitis without abscess or perforation. The patient was managed with a clear liquid diet and told to return to the clinic 2 days later.
CORRESPONDENCE
Heidi L. Gaddey, MD, Family Medicine Residency Program, University of Nebraska Medical Center and the 55th Medical Group, 2501 Capehart Road, Offutt Air Force Base, NE 68113; [email protected]
1. Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey: 2010 Summary Tables. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed April 8, 2015.
2. Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf. Accessed February 2, 2015.
3. American College of Radiology. ACR Appropriateness Criteria: Acute (Nonlocalized) abdominal pain and fever or suspected abdominal abscess. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69467/Narrative. Accessed December 15, 2014.
4. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74:1537-1544.
5. Crownover BK, Bepko JL. Appropriate and safe use of diagnostic imaging. Am Fam Physician. 2013;87:494-501.
6. American College of Radiology. ACR Appropriateness Criteria: right upper quadrant pain. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69474/Narrative/. Accessed December 15, 2014.
7. American College of Radiology. ACR Appropriateness Criteria: acute pancreatitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69468/Narrative. Accessed April 8, 2015.
8. American College of Radiology. ACR Appropriateness Criteria: acute onset flank pain—suspicion of stone disease. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69362/Narrative/. Accessed December 1, 2014.
9. American College of Radiology. ACR Appropriateness Criteria: left lower quadrant pain—suspected diverticulitis. American College of Radiology Web site. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/LeftLowerQuadrantPainSuspectedDiverticulitis.pdf. Accessed December 1, 2014.
10. American College of Radiology. ACR Appropriateness Criteria: right lower quadrant pain—suspected appendicitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69357/Narrative/. Accessed December 15, 2014.
11. American College of Radiology. ACR Appropriateness Criteria: suspected small-bowel obstruction. American College of Radiology Web site. Available at: http://www.acr.org/~/media/832F100277004BC69A8C818C7C9BFF33.pdf. Accessed December 10, 2014.
12. Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77:971-978.
13. Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012;262:751-764.
14. American College of Radiology. ACR Appropriateness Criteria: left lower quadrant pain—suspected diverticulitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69356/Narrative/. Accessed December 1, 2014.
15. Andeweg CS, Knobben L, Hendriks JC, et al. How to diagnose acute left-sided colonic diverticulitis: proposal for a clinical scoring system. Ann Surg. 2011;253:940-946.
16. Old JL, Dusing RW, Yap W, et al. Imaging for suspected appendicitis. Am Fam Physician. 2005;71:71-78.
17. Corwin MT, Chang M, Fananapazir G, et al. Accuracy and radiation dose reduction of a limited abdominopelvic CT in the diagnosis of acute appendicitis. Abdom Imaging. 2014; October 21 [Epub ahead of print].
18. American College of Radiology. ACR Appropriateness Criteria: imaging of mesenteric ischemia. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/70909/Narrative/. Accessed December 4, 2014.
19. Herbert GS, Steele SR. Acute and chronic mesenteric ischemia. Surg Clin North Am. 2007;87:1115-1134.
20. American College of Radiology. ACR Appropriateness Criteria: vomiting in infants up to 3 months of age. American College of Radiology Web site. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/VomitingInInfantsUpTo3MonthsOfAge.pdf. Accessed January 5, 2015.
› Choose ultrasonography as the initial imaging test for patients with pain in the right upper quadrant. C
› Order computed tomography with contrast of the abdomen and/or pelvis for adults with acute pain of new onset in the right or left lower quadrant, or both. C
› Recommend ultrasound with graded compression as the initial imaging modality for children younger than 14 years who have acute right lower quadrant pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Harry L, age 54, presents with acute onset abdominal pain that began 2 days ago. He reports mild nausea but no vomiting, non-bloody diarrhea, and feeling feverish. The patient denies increased pain with movement.
If Mr. L were your patient, how would you proceed?
Although acute nontraumatic abdominal pain accounts for only about 1.5% of physician office visits, it is the cause of approximately 8% of visits—more than 11 million, a year—to US emergency departments.1,2 In most cases, the location of the pain, coupled with the patient history, physical exam, and clinical judgment, lead to the differential diagnosis and determines what type of imaging, if any, is needed.
Benign self-limiting causes of abdominal pain, such as constipation or gastroenteritis, may not require any imaging. However, if the patient has abdominal pain and fever, is older than age 65, or presents with peritoneal signs and symptoms, imaging will be a crucial diagnostic aid.3,4
With that in mind, the American College of Radiology (ACR) has developed a 9-point scoring criteria based on both the site and common causes of abdominal pain to determine the best imaging modality to use to rule in—or out—serious disease and conditions for which surgery is required. A rating of 1, 2, or 3 indicates that imaging is usually not appropriate; a rating of 4, 5, or 6 means the imaging test may be appropriate, and a rating of 7, 8, or 9 indicates that the recommended test is usually appropriate. The panel of experts who developed the scores considered the relative radiation level of each imaging modality, as well.5
In the text and TABLE3,6-12 that follow, you’ll find the most likely clinical diagnoses and the optimal tests for abdominal pain, based largely on where it hurts.
CASE 1 › Appendicitis: An 8-year-old girl presented with acute right lower quadrant pain and underwent an ultrasound (left), which showed a dilated ~2 cm (normal <6 mm) non-compressible appendix consistent with acute appendicitis. There was no significant free fluid within the right lower quadrant. Follow-up computed tomography (CT) scan (middle) with IV and oral contrast confirmed the dilated appendix with no evidence of perforation or abscess formation.
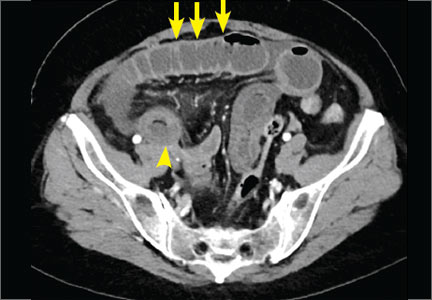
CASE 2 › Small bowel obstruction: A 54-year-old man sought care for abdominal pain and distention. A CT with IV and oral contrast (right) revealed multiple, fluid-filled dilated loops of small bowel (arrows) with bowel wall thickening, edema, and inflammatory stranding. The short segment of decreased enhancement (arrowhead) was consistent with bowel ischemia.
Right upper quadrant pain: Beware of acute biliary disease
Abdominal pain of the right upper quadrant (RUQ) is typically related to biliary, colonic, hepatic, or renal causes.12 Because of infection and the potential need for surgical intervention, untreated acute biliary disease can become life-threatening, particularly in the elderly.4
The ACR recommends ultrasound (US) as the initial imaging study for RUQ pain, regardless of whether the patient is febrile or has an elevated white blood cell count or a positive Murphy’s sign (demonstrated at youtube.com/watch?v=9L7N89sOSuc) (score=9). A 2012 meta-analysis found that US has a sensitivity of 81% and specificity of 83% for diagnosing acute cholecystitis.6
Although cholescintigraphy has a higher sensitivity and specificity (96% and 90%, respectively), US remains the initial study of choice because of its availability, study time, and the lack of ionizing radiation. For equivocal findings, computed tomography (CT), magnetic resonance imaging (MRI), and cholescintigraphy have similar levels of evidence.6
Epigastric/left upper quadrant pain: Consider pancreatits
Epigastric and left upper quadrant (LUQ) pain may have a gastric, biliary, pancreatic, vascular, renal, or cardiac etiology.12 The ACR criteria for testing depends on the type of pain suspected.
Pancreatitis. The Revised Atlanta Classification of Acute Pancreatitis requires 2 of the 3 classic criteria for a pancreatitis diagnosis: 1) abdominal pain suggestive of pancreatitis, 2) serum amylase and lipase levels ≥3 times the normal level, and 3) characteristic findings on imaging.13 The ACR recommends US as the initial imaging modality for suspected acute pancreatitis when it is the initial presentation, the patient has typical abdominal pain and increased serum amylase and lipase, and symptom onset was <48 to 72 hours before the patient sought care (score=9).7
For patients who are critically ill, meet the criteria for systemic inflammatory response syndrome (SIRS), have severe clinical scores on either the Acute Physiology and Chronic Health Evaluation (APACHE) II (available at clincalc.com/icumortality/apacheii.aspx) or Bedside Index for Severity in Acute Appendicitis (BISAP; mdcalc.com/bisap-score-for-pancreatitis-mortality/), or who present >48 to 72 hours after onset of symptoms, abdominal CT with contrast is recommended (score=8).
Urolithiasis. Patients with abdominal pain from a presumed renal source should undergo a non-contrast CT of the abdomen and pelvis for initial imaging, according to the ACR (score=8). The sensitivity is 95% to 96% and specificity is 98%.8 To limit radiation exposure, low-dose protocols and limiting scan range are preferred.
Radiography can be useful in patients with known kidney stone disease and previous films; however, the sensitivity in other patients is poor (58%-62%).8 Because pelviectasis and ureterectasis can take hours to develop, US will miss more than 30% of acute obstructions in patients who are not fully hydrated and is therefore not recommended as a first-line imaging modality.8 The sensitivity of US increases to 71% when it is combined with kidney, ureter, and bladder radiography, but is still lower than that of CT or IV urography.8
Left lower quadrant pain: Suspect sigmoid diverticulitis
The differential for left lower quadrant (LLQ) pain includes colonic, gynecologic, and renal etiologies.12 The most common cause in adults is acute sigmoid diverticulitis. Patients often present with the clinical triad of fever, LLQ pain, and leukocytosis.14 A decision to obtain imaging should be based on both the clinical presentation and examination. It may not be required for patients who have mild symptoms or have had previous episodes of diverticulitis.
Clinical scoring systems have been studied for LLQ pain. However, none has been validated in all settings and therefore no such system is routinely used.15 CT of the abdomen and pelvis with contrast media is the ACR’s recommendation for the initial imaging study (score=9). CT has a reported overall accuracy of 99%.9
CT can also assess the severity of disease and help determine medical vs surgical treatment.14 US using graded compression has a sensitivity of 77% to 98% and a specificity of 80% to 99%, but is limited by body habitus, technical expertise, and patient comfort. Therefore, US has not gained widespread use (score=4) for patients with LLQ pain.9,14 MRI is emerging as a potential option; however, longer scan times, cost, and availability continue to limit its use.14
Right lower quadrant pain: Is it appendicitis?
The differential for right lower quadrant (RLQ) pain, like that of LLQ pain, includes colonic, gynecologic, and renal etiologies.12 The most common cause of acute RLQ pain requiring surgery is appendicitis. History and physical exam achieve a diagnostic accuracy of 80%.16
If the diagnosis is clear, no imaging is warranted. In patients with equivocal clinical presentations, however, imaging is cost-effective and may reduce the rate of perforation, morbidity, mortality, and postoperative hospital stays.16 In addition, the accuracy of clinical diagnosis for elderly patients and women of childbearing age with RLQ pain tends to be lower than that of adult men. Therefore, some experts call for a lower imaging threshold for these populations.
CT of the abdomen and pelvis with contrast is the recommended initial imaging study in nonpregnant adults (score=8). CT has a sensitivity and specificity of 91% and 90%, respectively.10
CT without contrast is indicated for patients with RLQ pain who have a contraindication to contrast media, although the relative radiation level remains the same.
If limiting radiation exposure is especially important, consider US, followed by CT with contrast if US is inconclusive.10
Low-dose CT has been investigated as an alternative, but is not routinely used. A limited abdominal CT scan from the bottom of the body of the T10 vertebra to the top of the symphysis pubis allows for adequate evaluation and alternate diagnoses of concern when compared with full CT scans of the abdomen and pelvis.17 This limited CT scan has been found to result in a total body effective radiation dose reduction of 23% and, in women, a breast equivalent dose reduction of 85%, without missing a single case of acute appendicitis or pertinent alternative diagnoses.17
Diffuse abdominal pain: Suspect a blockage
Finally, some patients may present with diffuse or non-localizable pain with fever. The etiologies that often present with diffuse or nonspecific pain include small bowel obstruction and mesenteric ischemia.
Small bowel obstruction. When small bowel obstruction is suspected, CT of the abdomen and pelvis with contrast (score=9) is recommended. Oral contrast is not indicated if you suspect a high-grade obstruction, but may add functional information when only a partial or low-grade obstruction is suspected. The relative radiation level remains the same for both.11 For patients with pain and fever, postoperative or not, CT of the abdomen and pelvis with contrast is recommended (score=8).3
Mesenteric ischemia is associated with high morbidity and mortality rates (30%-90%).18,19 Acute mesenteric ischemia is most commonly secondary to embolism, followed by arterial thrombosis, non-occlusive ischemia, and less commonly, venous thrombosis.18 The typical presentation is pain out of proportion to the physical exam.19
Differentiating mesenteric ischemia from other causes of acute abdominal pain can be difficult. Patients with chronic mesenteric ischemia present with postprandial abdominal pain, weight loss, and food avoidance. Although radiography is often the initial test ordered, a negative test does not rule out mesenteric ischemia. Therefore, the ACR recommends CT angiography (CTA) of the abdomen with contrast for the evaluation of both acute and chronic mesenteric ischemia (score=9). US can be useful for excluding other causes of abdominal pain, as well as ischemia related to venous occlusion, but it has a low sensitivity (70%-89%)18 overall and therefore is not recommended as the initial test for acute or chronic mesenteric ischemia.
Magnetic resonance angiography (MRA) has a high sensitivity and specificity for severe stenosis or origin occlusions of the superior mesenteric artery and celiac axis; however, its ability to determine distal embolism and non-occlusive ischemia, and the length and availability of this test limit its usefulness.18
When the patient is a child
Imaging for bilious vomiting in infants up to 3 months varies based on age. In the first week of life, radiography of the abdomen is the ACR’s recommended first-line test (score=9).20 An upper GI series or contrast enema are also options, but less preferred due to their increased radiation exposure.20
For infants between one week and 3 months of age, an upper GI series is the study of choice (score=9) and radiography of the abdomen is second line (score=5). An upper GI series is recommended to evaluate non-bilious, intermittent non-projectile vomiting in those from birth to 3 months.20 Projectile non-bilious vomiting should be evaluated with US of the abdomen.20
In children with RLQ pain suggestive of acute appendicitis, US is the first line imaging method due to its relatively high sensitivity and specificity and lack of ionizing radiation (score=9).10 If US is inconclusive, then CT of the abdomen and pelvis with IV contrast, but not oral or rectal contrast, is recommended (score=7). Although MRI is a non-radiating modality, it should be reserved for use only in specialized pediatric facilities due to lack of experience, increased cost, and the usual need for sedation.10
CASE › Mr. L’s vital signs demonstrated mild tachycardia and his body temperature was 100.5° F. His physical exam revealed significant tenderness to palpation in the LL Q, but no rebound or guarding. A CT scan with contrast of the abdomen revealed diverticulitis without abscess or perforation. The patient was managed with a clear liquid diet and told to return to the clinic 2 days later.
CORRESPONDENCE
Heidi L. Gaddey, MD, Family Medicine Residency Program, University of Nebraska Medical Center and the 55th Medical Group, 2501 Capehart Road, Offutt Air Force Base, NE 68113; [email protected]
› Choose ultrasonography as the initial imaging test for patients with pain in the right upper quadrant. C
› Order computed tomography with contrast of the abdomen and/or pelvis for adults with acute pain of new onset in the right or left lower quadrant, or both. C
› Recommend ultrasound with graded compression as the initial imaging modality for children younger than 14 years who have acute right lower quadrant pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE › Harry L, age 54, presents with acute onset abdominal pain that began 2 days ago. He reports mild nausea but no vomiting, non-bloody diarrhea, and feeling feverish. The patient denies increased pain with movement.
If Mr. L were your patient, how would you proceed?
Although acute nontraumatic abdominal pain accounts for only about 1.5% of physician office visits, it is the cause of approximately 8% of visits—more than 11 million, a year—to US emergency departments.1,2 In most cases, the location of the pain, coupled with the patient history, physical exam, and clinical judgment, lead to the differential diagnosis and determines what type of imaging, if any, is needed.
Benign self-limiting causes of abdominal pain, such as constipation or gastroenteritis, may not require any imaging. However, if the patient has abdominal pain and fever, is older than age 65, or presents with peritoneal signs and symptoms, imaging will be a crucial diagnostic aid.3,4
With that in mind, the American College of Radiology (ACR) has developed a 9-point scoring criteria based on both the site and common causes of abdominal pain to determine the best imaging modality to use to rule in—or out—serious disease and conditions for which surgery is required. A rating of 1, 2, or 3 indicates that imaging is usually not appropriate; a rating of 4, 5, or 6 means the imaging test may be appropriate, and a rating of 7, 8, or 9 indicates that the recommended test is usually appropriate. The panel of experts who developed the scores considered the relative radiation level of each imaging modality, as well.5
In the text and TABLE3,6-12 that follow, you’ll find the most likely clinical diagnoses and the optimal tests for abdominal pain, based largely on where it hurts.
CASE 1 › Appendicitis: An 8-year-old girl presented with acute right lower quadrant pain and underwent an ultrasound (left), which showed a dilated ~2 cm (normal <6 mm) non-compressible appendix consistent with acute appendicitis. There was no significant free fluid within the right lower quadrant. Follow-up computed tomography (CT) scan (middle) with IV and oral contrast confirmed the dilated appendix with no evidence of perforation or abscess formation.
CASE 2 › Small bowel obstruction: A 54-year-old man sought care for abdominal pain and distention. A CT with IV and oral contrast (right) revealed multiple, fluid-filled dilated loops of small bowel (arrows) with bowel wall thickening, edema, and inflammatory stranding. The short segment of decreased enhancement (arrowhead) was consistent with bowel ischemia.
Right upper quadrant pain: Beware of acute biliary disease
Abdominal pain of the right upper quadrant (RUQ) is typically related to biliary, colonic, hepatic, or renal causes.12 Because of infection and the potential need for surgical intervention, untreated acute biliary disease can become life-threatening, particularly in the elderly.4
The ACR recommends ultrasound (US) as the initial imaging study for RUQ pain, regardless of whether the patient is febrile or has an elevated white blood cell count or a positive Murphy’s sign (demonstrated at youtube.com/watch?v=9L7N89sOSuc) (score=9). A 2012 meta-analysis found that US has a sensitivity of 81% and specificity of 83% for diagnosing acute cholecystitis.6
Although cholescintigraphy has a higher sensitivity and specificity (96% and 90%, respectively), US remains the initial study of choice because of its availability, study time, and the lack of ionizing radiation. For equivocal findings, computed tomography (CT), magnetic resonance imaging (MRI), and cholescintigraphy have similar levels of evidence.6
Epigastric/left upper quadrant pain: Consider pancreatits
Epigastric and left upper quadrant (LUQ) pain may have a gastric, biliary, pancreatic, vascular, renal, or cardiac etiology.12 The ACR criteria for testing depends on the type of pain suspected.
Pancreatitis. The Revised Atlanta Classification of Acute Pancreatitis requires 2 of the 3 classic criteria for a pancreatitis diagnosis: 1) abdominal pain suggestive of pancreatitis, 2) serum amylase and lipase levels ≥3 times the normal level, and 3) characteristic findings on imaging.13 The ACR recommends US as the initial imaging modality for suspected acute pancreatitis when it is the initial presentation, the patient has typical abdominal pain and increased serum amylase and lipase, and symptom onset was <48 to 72 hours before the patient sought care (score=9).7
For patients who are critically ill, meet the criteria for systemic inflammatory response syndrome (SIRS), have severe clinical scores on either the Acute Physiology and Chronic Health Evaluation (APACHE) II (available at clincalc.com/icumortality/apacheii.aspx) or Bedside Index for Severity in Acute Appendicitis (BISAP; mdcalc.com/bisap-score-for-pancreatitis-mortality/), or who present >48 to 72 hours after onset of symptoms, abdominal CT with contrast is recommended (score=8).
Urolithiasis. Patients with abdominal pain from a presumed renal source should undergo a non-contrast CT of the abdomen and pelvis for initial imaging, according to the ACR (score=8). The sensitivity is 95% to 96% and specificity is 98%.8 To limit radiation exposure, low-dose protocols and limiting scan range are preferred.
Radiography can be useful in patients with known kidney stone disease and previous films; however, the sensitivity in other patients is poor (58%-62%).8 Because pelviectasis and ureterectasis can take hours to develop, US will miss more than 30% of acute obstructions in patients who are not fully hydrated and is therefore not recommended as a first-line imaging modality.8 The sensitivity of US increases to 71% when it is combined with kidney, ureter, and bladder radiography, but is still lower than that of CT or IV urography.8
Left lower quadrant pain: Suspect sigmoid diverticulitis
The differential for left lower quadrant (LLQ) pain includes colonic, gynecologic, and renal etiologies.12 The most common cause in adults is acute sigmoid diverticulitis. Patients often present with the clinical triad of fever, LLQ pain, and leukocytosis.14 A decision to obtain imaging should be based on both the clinical presentation and examination. It may not be required for patients who have mild symptoms or have had previous episodes of diverticulitis.
Clinical scoring systems have been studied for LLQ pain. However, none has been validated in all settings and therefore no such system is routinely used.15 CT of the abdomen and pelvis with contrast media is the ACR’s recommendation for the initial imaging study (score=9). CT has a reported overall accuracy of 99%.9
CT can also assess the severity of disease and help determine medical vs surgical treatment.14 US using graded compression has a sensitivity of 77% to 98% and a specificity of 80% to 99%, but is limited by body habitus, technical expertise, and patient comfort. Therefore, US has not gained widespread use (score=4) for patients with LLQ pain.9,14 MRI is emerging as a potential option; however, longer scan times, cost, and availability continue to limit its use.14
Right lower quadrant pain: Is it appendicitis?
The differential for right lower quadrant (RLQ) pain, like that of LLQ pain, includes colonic, gynecologic, and renal etiologies.12 The most common cause of acute RLQ pain requiring surgery is appendicitis. History and physical exam achieve a diagnostic accuracy of 80%.16
If the diagnosis is clear, no imaging is warranted. In patients with equivocal clinical presentations, however, imaging is cost-effective and may reduce the rate of perforation, morbidity, mortality, and postoperative hospital stays.16 In addition, the accuracy of clinical diagnosis for elderly patients and women of childbearing age with RLQ pain tends to be lower than that of adult men. Therefore, some experts call for a lower imaging threshold for these populations.
CT of the abdomen and pelvis with contrast is the recommended initial imaging study in nonpregnant adults (score=8). CT has a sensitivity and specificity of 91% and 90%, respectively.10
CT without contrast is indicated for patients with RLQ pain who have a contraindication to contrast media, although the relative radiation level remains the same.
If limiting radiation exposure is especially important, consider US, followed by CT with contrast if US is inconclusive.10
Low-dose CT has been investigated as an alternative, but is not routinely used. A limited abdominal CT scan from the bottom of the body of the T10 vertebra to the top of the symphysis pubis allows for adequate evaluation and alternate diagnoses of concern when compared with full CT scans of the abdomen and pelvis.17 This limited CT scan has been found to result in a total body effective radiation dose reduction of 23% and, in women, a breast equivalent dose reduction of 85%, without missing a single case of acute appendicitis or pertinent alternative diagnoses.17
Diffuse abdominal pain: Suspect a blockage
Finally, some patients may present with diffuse or non-localizable pain with fever. The etiologies that often present with diffuse or nonspecific pain include small bowel obstruction and mesenteric ischemia.
Small bowel obstruction. When small bowel obstruction is suspected, CT of the abdomen and pelvis with contrast (score=9) is recommended. Oral contrast is not indicated if you suspect a high-grade obstruction, but may add functional information when only a partial or low-grade obstruction is suspected. The relative radiation level remains the same for both.11 For patients with pain and fever, postoperative or not, CT of the abdomen and pelvis with contrast is recommended (score=8).3
Mesenteric ischemia is associated with high morbidity and mortality rates (30%-90%).18,19 Acute mesenteric ischemia is most commonly secondary to embolism, followed by arterial thrombosis, non-occlusive ischemia, and less commonly, venous thrombosis.18 The typical presentation is pain out of proportion to the physical exam.19
Differentiating mesenteric ischemia from other causes of acute abdominal pain can be difficult. Patients with chronic mesenteric ischemia present with postprandial abdominal pain, weight loss, and food avoidance. Although radiography is often the initial test ordered, a negative test does not rule out mesenteric ischemia. Therefore, the ACR recommends CT angiography (CTA) of the abdomen with contrast for the evaluation of both acute and chronic mesenteric ischemia (score=9). US can be useful for excluding other causes of abdominal pain, as well as ischemia related to venous occlusion, but it has a low sensitivity (70%-89%)18 overall and therefore is not recommended as the initial test for acute or chronic mesenteric ischemia.
Magnetic resonance angiography (MRA) has a high sensitivity and specificity for severe stenosis or origin occlusions of the superior mesenteric artery and celiac axis; however, its ability to determine distal embolism and non-occlusive ischemia, and the length and availability of this test limit its usefulness.18
When the patient is a child
Imaging for bilious vomiting in infants up to 3 months varies based on age. In the first week of life, radiography of the abdomen is the ACR’s recommended first-line test (score=9).20 An upper GI series or contrast enema are also options, but less preferred due to their increased radiation exposure.20
For infants between one week and 3 months of age, an upper GI series is the study of choice (score=9) and radiography of the abdomen is second line (score=5). An upper GI series is recommended to evaluate non-bilious, intermittent non-projectile vomiting in those from birth to 3 months.20 Projectile non-bilious vomiting should be evaluated with US of the abdomen.20
In children with RLQ pain suggestive of acute appendicitis, US is the first line imaging method due to its relatively high sensitivity and specificity and lack of ionizing radiation (score=9).10 If US is inconclusive, then CT of the abdomen and pelvis with IV contrast, but not oral or rectal contrast, is recommended (score=7). Although MRI is a non-radiating modality, it should be reserved for use only in specialized pediatric facilities due to lack of experience, increased cost, and the usual need for sedation.10
CASE › Mr. L’s vital signs demonstrated mild tachycardia and his body temperature was 100.5° F. His physical exam revealed significant tenderness to palpation in the LL Q, but no rebound or guarding. A CT scan with contrast of the abdomen revealed diverticulitis without abscess or perforation. The patient was managed with a clear liquid diet and told to return to the clinic 2 days later.
CORRESPONDENCE
Heidi L. Gaddey, MD, Family Medicine Residency Program, University of Nebraska Medical Center and the 55th Medical Group, 2501 Capehart Road, Offutt Air Force Base, NE 68113; [email protected]
1. Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey: 2010 Summary Tables. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed April 8, 2015.
2. Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf. Accessed February 2, 2015.
3. American College of Radiology. ACR Appropriateness Criteria: Acute (Nonlocalized) abdominal pain and fever or suspected abdominal abscess. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69467/Narrative. Accessed December 15, 2014.
4. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74:1537-1544.
5. Crownover BK, Bepko JL. Appropriate and safe use of diagnostic imaging. Am Fam Physician. 2013;87:494-501.
6. American College of Radiology. ACR Appropriateness Criteria: right upper quadrant pain. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69474/Narrative/. Accessed December 15, 2014.
7. American College of Radiology. ACR Appropriateness Criteria: acute pancreatitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69468/Narrative. Accessed April 8, 2015.
8. American College of Radiology. ACR Appropriateness Criteria: acute onset flank pain—suspicion of stone disease. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69362/Narrative/. Accessed December 1, 2014.
9. American College of Radiology. ACR Appropriateness Criteria: left lower quadrant pain—suspected diverticulitis. American College of Radiology Web site. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/LeftLowerQuadrantPainSuspectedDiverticulitis.pdf. Accessed December 1, 2014.
10. American College of Radiology. ACR Appropriateness Criteria: right lower quadrant pain—suspected appendicitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69357/Narrative/. Accessed December 15, 2014.
11. American College of Radiology. ACR Appropriateness Criteria: suspected small-bowel obstruction. American College of Radiology Web site. Available at: http://www.acr.org/~/media/832F100277004BC69A8C818C7C9BFF33.pdf. Accessed December 10, 2014.
12. Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77:971-978.
13. Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012;262:751-764.
14. American College of Radiology. ACR Appropriateness Criteria: left lower quadrant pain—suspected diverticulitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69356/Narrative/. Accessed December 1, 2014.
15. Andeweg CS, Knobben L, Hendriks JC, et al. How to diagnose acute left-sided colonic diverticulitis: proposal for a clinical scoring system. Ann Surg. 2011;253:940-946.
16. Old JL, Dusing RW, Yap W, et al. Imaging for suspected appendicitis. Am Fam Physician. 2005;71:71-78.
17. Corwin MT, Chang M, Fananapazir G, et al. Accuracy and radiation dose reduction of a limited abdominopelvic CT in the diagnosis of acute appendicitis. Abdom Imaging. 2014; October 21 [Epub ahead of print].
18. American College of Radiology. ACR Appropriateness Criteria: imaging of mesenteric ischemia. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/70909/Narrative/. Accessed December 4, 2014.
19. Herbert GS, Steele SR. Acute and chronic mesenteric ischemia. Surg Clin North Am. 2007;87:1115-1134.
20. American College of Radiology. ACR Appropriateness Criteria: vomiting in infants up to 3 months of age. American College of Radiology Web site. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/VomitingInInfantsUpTo3MonthsOfAge.pdf. Accessed January 5, 2015.
1. Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey: 2010 Summary Tables. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed April 8, 2015.
2. Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf. Accessed February 2, 2015.
3. American College of Radiology. ACR Appropriateness Criteria: Acute (Nonlocalized) abdominal pain and fever or suspected abdominal abscess. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69467/Narrative. Accessed December 15, 2014.
4. Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician. 2006;74:1537-1544.
5. Crownover BK, Bepko JL. Appropriate and safe use of diagnostic imaging. Am Fam Physician. 2013;87:494-501.
6. American College of Radiology. ACR Appropriateness Criteria: right upper quadrant pain. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69474/Narrative/. Accessed December 15, 2014.
7. American College of Radiology. ACR Appropriateness Criteria: acute pancreatitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69468/Narrative. Accessed April 8, 2015.
8. American College of Radiology. ACR Appropriateness Criteria: acute onset flank pain—suspicion of stone disease. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69362/Narrative/. Accessed December 1, 2014.
9. American College of Radiology. ACR Appropriateness Criteria: left lower quadrant pain—suspected diverticulitis. American College of Radiology Web site. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/LeftLowerQuadrantPainSuspectedDiverticulitis.pdf. Accessed December 1, 2014.
10. American College of Radiology. ACR Appropriateness Criteria: right lower quadrant pain—suspected appendicitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69357/Narrative/. Accessed December 15, 2014.
11. American College of Radiology. ACR Appropriateness Criteria: suspected small-bowel obstruction. American College of Radiology Web site. Available at: http://www.acr.org/~/media/832F100277004BC69A8C818C7C9BFF33.pdf. Accessed December 10, 2014.
12. Cartwright SL, Knudson MP. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77:971-978.
13. Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012;262:751-764.
14. American College of Radiology. ACR Appropriateness Criteria: left lower quadrant pain—suspected diverticulitis. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/69356/Narrative/. Accessed December 1, 2014.
15. Andeweg CS, Knobben L, Hendriks JC, et al. How to diagnose acute left-sided colonic diverticulitis: proposal for a clinical scoring system. Ann Surg. 2011;253:940-946.
16. Old JL, Dusing RW, Yap W, et al. Imaging for suspected appendicitis. Am Fam Physician. 2005;71:71-78.
17. Corwin MT, Chang M, Fananapazir G, et al. Accuracy and radiation dose reduction of a limited abdominopelvic CT in the diagnosis of acute appendicitis. Abdom Imaging. 2014; October 21 [Epub ahead of print].
18. American College of Radiology. ACR Appropriateness Criteria: imaging of mesenteric ischemia. American College of Radiology Web site. Available at: https://acsearch.acr.org/docs/70909/Narrative/. Accessed December 4, 2014.
19. Herbert GS, Steele SR. Acute and chronic mesenteric ischemia. Surg Clin North Am. 2007;87:1115-1134.
20. American College of Radiology. ACR Appropriateness Criteria: vomiting in infants up to 3 months of age. American College of Radiology Web site. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/VomitingInInfantsUpTo3MonthsOfAge.pdf. Accessed January 5, 2015.