User login
Too much to disagree on to let politics enter an office visit
“I can’t believe you’re drinking that.”
The young woman across the desk from me seemed perplexed, and I didn’t know why.
I’m one of those people who always has something to drink in front of me while working. A bottle of Costco green tea, Diet Coke, coffee. I also have a SodaStream gadget at my office, and that bottle is what I had on my desk at the moment.
I naively said “Why? I doubt it’s any worse for me than any other soda.”
That sure set her off, and I got a lecture about SodaStream being an Israeli company and her opinions on the Middle East, Israel, Palestine, etc. I listened politely for a moment, then redirected her back to the reason for her visit.
Not being someone who follows the news in detail, I‘d been unaware there was any controversy behind the soda bottle on my desk that morning. To me, it was just my choice of beverage.
The trouble here is that it’s possible to politicize pretty much anything in a divided world. I try to stay, for better or worse, ignorant of such things. My soft drink choice reflects nothing more than what I felt like drinking when I went back to my office’s tiny break room between appointments.
If you dig far enough into any company’s – or person’s – background, you’ll find something you disagree with. Just like any drug I prescribe will have side effects.
It’s for this reason that I keep politics out of my office. Patients, such as this lady, may express theirs, but I’ll never express mine. Too many in this world see each other in an “us vs. them” frame, quick to declare someone with different views as the enemy, rather than another decent person with an honest difference of opinion.
And it’s irrelevant to what I’m trying to achieve at my office anyway – caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I can’t believe you’re drinking that.”
The young woman across the desk from me seemed perplexed, and I didn’t know why.
I’m one of those people who always has something to drink in front of me while working. A bottle of Costco green tea, Diet Coke, coffee. I also have a SodaStream gadget at my office, and that bottle is what I had on my desk at the moment.
I naively said “Why? I doubt it’s any worse for me than any other soda.”
That sure set her off, and I got a lecture about SodaStream being an Israeli company and her opinions on the Middle East, Israel, Palestine, etc. I listened politely for a moment, then redirected her back to the reason for her visit.
Not being someone who follows the news in detail, I‘d been unaware there was any controversy behind the soda bottle on my desk that morning. To me, it was just my choice of beverage.
The trouble here is that it’s possible to politicize pretty much anything in a divided world. I try to stay, for better or worse, ignorant of such things. My soft drink choice reflects nothing more than what I felt like drinking when I went back to my office’s tiny break room between appointments.
If you dig far enough into any company’s – or person’s – background, you’ll find something you disagree with. Just like any drug I prescribe will have side effects.
It’s for this reason that I keep politics out of my office. Patients, such as this lady, may express theirs, but I’ll never express mine. Too many in this world see each other in an “us vs. them” frame, quick to declare someone with different views as the enemy, rather than another decent person with an honest difference of opinion.
And it’s irrelevant to what I’m trying to achieve at my office anyway – caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I can’t believe you’re drinking that.”
The young woman across the desk from me seemed perplexed, and I didn’t know why.
I’m one of those people who always has something to drink in front of me while working. A bottle of Costco green tea, Diet Coke, coffee. I also have a SodaStream gadget at my office, and that bottle is what I had on my desk at the moment.
I naively said “Why? I doubt it’s any worse for me than any other soda.”
That sure set her off, and I got a lecture about SodaStream being an Israeli company and her opinions on the Middle East, Israel, Palestine, etc. I listened politely for a moment, then redirected her back to the reason for her visit.
Not being someone who follows the news in detail, I‘d been unaware there was any controversy behind the soda bottle on my desk that morning. To me, it was just my choice of beverage.
The trouble here is that it’s possible to politicize pretty much anything in a divided world. I try to stay, for better or worse, ignorant of such things. My soft drink choice reflects nothing more than what I felt like drinking when I went back to my office’s tiny break room between appointments.
If you dig far enough into any company’s – or person’s – background, you’ll find something you disagree with. Just like any drug I prescribe will have side effects.
It’s for this reason that I keep politics out of my office. Patients, such as this lady, may express theirs, but I’ll never express mine. Too many in this world see each other in an “us vs. them” frame, quick to declare someone with different views as the enemy, rather than another decent person with an honest difference of opinion.
And it’s irrelevant to what I’m trying to achieve at my office anyway – caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The fragile gray mass between your ears
He’s almost 10 years younger than me.
He’d been in the hospital for 3 weeks. The ICU room had been decorated, as many families do, with pictures of his life. His wedding. His kids. He and his wife dressed as Darth Vader and Princess Leia for a Halloween party. A few religious items.
He was off sedation. EEG didn’t show any seizures. Head CT just showed the extensive damage from his head injury. The neurosurgeons can evacuate clots and decrease intracranial pressure, but they can’t repair brain tissue.
His wife was long past the point of shock when I met with her. After 3 weeks, she understood what the new normal was and how the lives of both herself and their kids would never be the same. She held his hand at the bedside as we talked, asked me a few pointed questions, and then thanked me for coming in to see him.
For me, it was just another day on call. I walked back to the nurses station, got some coffee from the galley, and sat down to dictate a note. There are always other patients to see on the coverage list.
But it still reminds you.
The brain doesn’t weigh much, just 2-3 pounds; it’s about the size of your fists put together.
But it’s everything that we are, both as individuals and as a species. All that humanity has achieved, good and bad, came from the brain.
The rest of him was in good shape. A healthy guy in his 40s. Probably in better condition than me. But with his brain irreparably damaged, none of that meant anything.
Even after almost 20 years of doing this work, this sort of thing still reminds me how lucky I, and most of us, are – and to be grateful for what I have.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
He’s almost 10 years younger than me.
He’d been in the hospital for 3 weeks. The ICU room had been decorated, as many families do, with pictures of his life. His wedding. His kids. He and his wife dressed as Darth Vader and Princess Leia for a Halloween party. A few religious items.
He was off sedation. EEG didn’t show any seizures. Head CT just showed the extensive damage from his head injury. The neurosurgeons can evacuate clots and decrease intracranial pressure, but they can’t repair brain tissue.
His wife was long past the point of shock when I met with her. After 3 weeks, she understood what the new normal was and how the lives of both herself and their kids would never be the same. She held his hand at the bedside as we talked, asked me a few pointed questions, and then thanked me for coming in to see him.
For me, it was just another day on call. I walked back to the nurses station, got some coffee from the galley, and sat down to dictate a note. There are always other patients to see on the coverage list.
But it still reminds you.
The brain doesn’t weigh much, just 2-3 pounds; it’s about the size of your fists put together.
But it’s everything that we are, both as individuals and as a species. All that humanity has achieved, good and bad, came from the brain.
The rest of him was in good shape. A healthy guy in his 40s. Probably in better condition than me. But with his brain irreparably damaged, none of that meant anything.
Even after almost 20 years of doing this work, this sort of thing still reminds me how lucky I, and most of us, are – and to be grateful for what I have.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
He’s almost 10 years younger than me.
He’d been in the hospital for 3 weeks. The ICU room had been decorated, as many families do, with pictures of his life. His wedding. His kids. He and his wife dressed as Darth Vader and Princess Leia for a Halloween party. A few religious items.
He was off sedation. EEG didn’t show any seizures. Head CT just showed the extensive damage from his head injury. The neurosurgeons can evacuate clots and decrease intracranial pressure, but they can’t repair brain tissue.
His wife was long past the point of shock when I met with her. After 3 weeks, she understood what the new normal was and how the lives of both herself and their kids would never be the same. She held his hand at the bedside as we talked, asked me a few pointed questions, and then thanked me for coming in to see him.
For me, it was just another day on call. I walked back to the nurses station, got some coffee from the galley, and sat down to dictate a note. There are always other patients to see on the coverage list.
But it still reminds you.
The brain doesn’t weigh much, just 2-3 pounds; it’s about the size of your fists put together.
But it’s everything that we are, both as individuals and as a species. All that humanity has achieved, good and bad, came from the brain.
The rest of him was in good shape. A healthy guy in his 40s. Probably in better condition than me. But with his brain irreparably damaged, none of that meant anything.
Even after almost 20 years of doing this work, this sort of thing still reminds me how lucky I, and most of us, are – and to be grateful for what I have.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Caring for the offensive patient
“I only see Jewish doctors.”
The middle-aged lady across my desk repeated that several times during her visit, apparently hoping to get some response from me. I just ignored it each time.
Imagine if she’d said, “I only see white doctors,” or “I only see black doctors.” To say you came to a doctor solely because of his or her ethnicity is, to me, ignorant at best and blatant discrimination at worst.
Of course, I continued the appointment. While I found her comment offensive, I’m a doctor. Unlike a restaurant owner, I can’t refuse to serve someone because of their personal beliefs, no matter how much I disagree. I took an oath to provide equal care to all, regardless of personal differences. I try hard to measure up to that.
We live in a world that seems to be increasingly divided along tribal lines. Us against them. Me against you. Everyone for themselves.
I’m not going to play that game. For better or worse, I’ll take the high road and continue treating all people as equal. If you want to believe that religion, or color, or any other difference makes someone a better or worse physician (or person, for that matter), you’re entitled to your opinion.
I may not be able to change your mind, but that’s not going to stop me from trying to be the best doctor I can to everyone who comes to me, regardless of who they are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I only see Jewish doctors.”
The middle-aged lady across my desk repeated that several times during her visit, apparently hoping to get some response from me. I just ignored it each time.
Imagine if she’d said, “I only see white doctors,” or “I only see black doctors.” To say you came to a doctor solely because of his or her ethnicity is, to me, ignorant at best and blatant discrimination at worst.
Of course, I continued the appointment. While I found her comment offensive, I’m a doctor. Unlike a restaurant owner, I can’t refuse to serve someone because of their personal beliefs, no matter how much I disagree. I took an oath to provide equal care to all, regardless of personal differences. I try hard to measure up to that.
We live in a world that seems to be increasingly divided along tribal lines. Us against them. Me against you. Everyone for themselves.
I’m not going to play that game. For better or worse, I’ll take the high road and continue treating all people as equal. If you want to believe that religion, or color, or any other difference makes someone a better or worse physician (or person, for that matter), you’re entitled to your opinion.
I may not be able to change your mind, but that’s not going to stop me from trying to be the best doctor I can to everyone who comes to me, regardless of who they are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I only see Jewish doctors.”
The middle-aged lady across my desk repeated that several times during her visit, apparently hoping to get some response from me. I just ignored it each time.
Imagine if she’d said, “I only see white doctors,” or “I only see black doctors.” To say you came to a doctor solely because of his or her ethnicity is, to me, ignorant at best and blatant discrimination at worst.
Of course, I continued the appointment. While I found her comment offensive, I’m a doctor. Unlike a restaurant owner, I can’t refuse to serve someone because of their personal beliefs, no matter how much I disagree. I took an oath to provide equal care to all, regardless of personal differences. I try hard to measure up to that.
We live in a world that seems to be increasingly divided along tribal lines. Us against them. Me against you. Everyone for themselves.
I’m not going to play that game. For better or worse, I’ll take the high road and continue treating all people as equal. If you want to believe that religion, or color, or any other difference makes someone a better or worse physician (or person, for that matter), you’re entitled to your opinion.
I may not be able to change your mind, but that’s not going to stop me from trying to be the best doctor I can to everyone who comes to me, regardless of who they are.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Doctors’ pay involves a lot of unseen work
“Doctors make a lot of money.” We hear that a lot, always from people who aren’t part of the profession.
Last month, I had to do my tax forms. Not my annual forms, but the quarterly withholding ones for the IRS, and for the state, along with the Arizona Department of Economic Security forms.
The whole thing takes me about 2 hours every 3 months. I suppose I could hire an accountant or office manager to deal with that stuff, but in solo practice, you do everything you can to keep the overhead low. So I do it myself.
Eight hours a year doesn’t sound too bad, but it got me thinking about all the other ways that work creeps into my home time.
I’m usually at the office around 5:00 a.m., when I start with reviewing charts, doing paperwork, and catching up on dictations until patients start at 8:00 a.m. From then on, they’re a steady stream until 4:00 p.m., when we close up and head home.
I get home and then have 1-2 hours of time paying bills, sorting mail, and catching up on phone calls and other unresolved issues.
On weekends, there’s always other stuff. Payroll for the coming weeks, office bills, and credit card statements I didn’t get to during the week, CME, forms, licensing paperwork, etc.
I’d guess about 15 hours/week goes into nonpatient-related stuff. Each year that’s more than 700 hours (or a little over a month) of extra time. Tack that on to the roughly 60 hours that I spend seeing patients between the office and hospital.
People say we make “a lot” (whatever that is), but they don’t see everything behind it. The 7-12 years of post-college training. The student loans of $200,000 and dating back to when I was 26 years old. The rising costs of overhead and dropping rates of reimbursement. The denied payments in disputes over claims. And, as mentioned above, the huge amount of time this job takes for stuff beyond just seeing patients.
We don’t get paid by the hour, but if we did, the rate would probably be a lot lower than what most would expect.
I suppose I could become employed, and let someone else worry about those things. But the financial impact doesn’t go away. Someone else still has to be doing those things, and since doctors are the ones who generate income in the majority of medical practices, the salaries for everyone else come out of ours. Plus, as I’ve previously written about, I’ve been employed before and got sick of the meetings and memos about cost-sharing, productivity numbers, and dollars earned per square foot.
But whenever I hear the refrain about our field being overpaid, I think about the actual hours the public doesn’t see (or care about). This isn’t a job for slackers, and
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“Doctors make a lot of money.” We hear that a lot, always from people who aren’t part of the profession.
Last month, I had to do my tax forms. Not my annual forms, but the quarterly withholding ones for the IRS, and for the state, along with the Arizona Department of Economic Security forms.
The whole thing takes me about 2 hours every 3 months. I suppose I could hire an accountant or office manager to deal with that stuff, but in solo practice, you do everything you can to keep the overhead low. So I do it myself.
Eight hours a year doesn’t sound too bad, but it got me thinking about all the other ways that work creeps into my home time.
I’m usually at the office around 5:00 a.m., when I start with reviewing charts, doing paperwork, and catching up on dictations until patients start at 8:00 a.m. From then on, they’re a steady stream until 4:00 p.m., when we close up and head home.
I get home and then have 1-2 hours of time paying bills, sorting mail, and catching up on phone calls and other unresolved issues.
On weekends, there’s always other stuff. Payroll for the coming weeks, office bills, and credit card statements I didn’t get to during the week, CME, forms, licensing paperwork, etc.
I’d guess about 15 hours/week goes into nonpatient-related stuff. Each year that’s more than 700 hours (or a little over a month) of extra time. Tack that on to the roughly 60 hours that I spend seeing patients between the office and hospital.
People say we make “a lot” (whatever that is), but they don’t see everything behind it. The 7-12 years of post-college training. The student loans of $200,000 and dating back to when I was 26 years old. The rising costs of overhead and dropping rates of reimbursement. The denied payments in disputes over claims. And, as mentioned above, the huge amount of time this job takes for stuff beyond just seeing patients.
We don’t get paid by the hour, but if we did, the rate would probably be a lot lower than what most would expect.
I suppose I could become employed, and let someone else worry about those things. But the financial impact doesn’t go away. Someone else still has to be doing those things, and since doctors are the ones who generate income in the majority of medical practices, the salaries for everyone else come out of ours. Plus, as I’ve previously written about, I’ve been employed before and got sick of the meetings and memos about cost-sharing, productivity numbers, and dollars earned per square foot.
But whenever I hear the refrain about our field being overpaid, I think about the actual hours the public doesn’t see (or care about). This isn’t a job for slackers, and
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“Doctors make a lot of money.” We hear that a lot, always from people who aren’t part of the profession.
Last month, I had to do my tax forms. Not my annual forms, but the quarterly withholding ones for the IRS, and for the state, along with the Arizona Department of Economic Security forms.
The whole thing takes me about 2 hours every 3 months. I suppose I could hire an accountant or office manager to deal with that stuff, but in solo practice, you do everything you can to keep the overhead low. So I do it myself.
Eight hours a year doesn’t sound too bad, but it got me thinking about all the other ways that work creeps into my home time.
I’m usually at the office around 5:00 a.m., when I start with reviewing charts, doing paperwork, and catching up on dictations until patients start at 8:00 a.m. From then on, they’re a steady stream until 4:00 p.m., when we close up and head home.
I get home and then have 1-2 hours of time paying bills, sorting mail, and catching up on phone calls and other unresolved issues.
On weekends, there’s always other stuff. Payroll for the coming weeks, office bills, and credit card statements I didn’t get to during the week, CME, forms, licensing paperwork, etc.
I’d guess about 15 hours/week goes into nonpatient-related stuff. Each year that’s more than 700 hours (or a little over a month) of extra time. Tack that on to the roughly 60 hours that I spend seeing patients between the office and hospital.
People say we make “a lot” (whatever that is), but they don’t see everything behind it. The 7-12 years of post-college training. The student loans of $200,000 and dating back to when I was 26 years old. The rising costs of overhead and dropping rates of reimbursement. The denied payments in disputes over claims. And, as mentioned above, the huge amount of time this job takes for stuff beyond just seeing patients.
We don’t get paid by the hour, but if we did, the rate would probably be a lot lower than what most would expect.
I suppose I could become employed, and let someone else worry about those things. But the financial impact doesn’t go away. Someone else still has to be doing those things, and since doctors are the ones who generate income in the majority of medical practices, the salaries for everyone else come out of ours. Plus, as I’ve previously written about, I’ve been employed before and got sick of the meetings and memos about cost-sharing, productivity numbers, and dollars earned per square foot.
But whenever I hear the refrain about our field being overpaid, I think about the actual hours the public doesn’t see (or care about). This isn’t a job for slackers, and
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Forgoing EMR templates for artisanal notes
I’m a medical note artisan.
Does that term sound overused these days? Well, I’ll stand by it. I handcraft medical notes from nouns, adjectives, verbs, habitual phrases, and other constructs of language.
In an era of mass-produced generic EMR notes, often indistinguishable between doctors, or even specialties, I scorn templates and type mine (or dictate them) fresh for each patient.
Perhaps I’m just old style, though it can’t be from my age. One area neurologist who’s older than I am has encouraged me to switch to using templates. He emphasizes how much time it saves. I don’t bother telling him that his physical exams never change, even though the patient clearly has.
Another, also older than I, has gone even further. Rather than taking his own history he just cuts and pastes it from the admitting internist’s note. I’m sure that saves a lot of time, too, although it will probably come back to bite him if the records ever come up in a legal case.
Notes today are all sizzle and no steak. Templates feed in test results, allergies, medication lists, etc. It’s not that these thing aren’t important, but they overshadow the note’s purpose of stating what’s going on with the patient and what you’re trying to do about it.
Does it take me more time to do this? Probably, but on the flip side it saves me time later when looking to see if an exam has changed or trying to remember what my plan was.
And, like any artisan would say, I’ll take quality over quantity any time.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m a medical note artisan.
Does that term sound overused these days? Well, I’ll stand by it. I handcraft medical notes from nouns, adjectives, verbs, habitual phrases, and other constructs of language.
In an era of mass-produced generic EMR notes, often indistinguishable between doctors, or even specialties, I scorn templates and type mine (or dictate them) fresh for each patient.
Perhaps I’m just old style, though it can’t be from my age. One area neurologist who’s older than I am has encouraged me to switch to using templates. He emphasizes how much time it saves. I don’t bother telling him that his physical exams never change, even though the patient clearly has.
Another, also older than I, has gone even further. Rather than taking his own history he just cuts and pastes it from the admitting internist’s note. I’m sure that saves a lot of time, too, although it will probably come back to bite him if the records ever come up in a legal case.
Notes today are all sizzle and no steak. Templates feed in test results, allergies, medication lists, etc. It’s not that these thing aren’t important, but they overshadow the note’s purpose of stating what’s going on with the patient and what you’re trying to do about it.
Does it take me more time to do this? Probably, but on the flip side it saves me time later when looking to see if an exam has changed or trying to remember what my plan was.
And, like any artisan would say, I’ll take quality over quantity any time.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m a medical note artisan.
Does that term sound overused these days? Well, I’ll stand by it. I handcraft medical notes from nouns, adjectives, verbs, habitual phrases, and other constructs of language.
In an era of mass-produced generic EMR notes, often indistinguishable between doctors, or even specialties, I scorn templates and type mine (or dictate them) fresh for each patient.
Perhaps I’m just old style, though it can’t be from my age. One area neurologist who’s older than I am has encouraged me to switch to using templates. He emphasizes how much time it saves. I don’t bother telling him that his physical exams never change, even though the patient clearly has.
Another, also older than I, has gone even further. Rather than taking his own history he just cuts and pastes it from the admitting internist’s note. I’m sure that saves a lot of time, too, although it will probably come back to bite him if the records ever come up in a legal case.
Notes today are all sizzle and no steak. Templates feed in test results, allergies, medication lists, etc. It’s not that these thing aren’t important, but they overshadow the note’s purpose of stating what’s going on with the patient and what you’re trying to do about it.
Does it take me more time to do this? Probably, but on the flip side it saves me time later when looking to see if an exam has changed or trying to remember what my plan was.
And, like any artisan would say, I’ll take quality over quantity any time.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The retirement horizon creeps up
My lease is up later this year, after 5 1/2 years. It doesn’t seem that long. Some days it feels like I just moved in.
As a result, I had an email exchange recently with the building’s manager and we hashed out an agreement on a new 10-year contract. In the process, I realized that sort of time frame might (and, again, I say might) take me into retirement.
And now I’m starting to think about retiring and the career endgame.
Granted, it’s still 10 years away, and knowing me I’ll probably want to work another 5 years or so beyond that if I can. I like what I do and would probably go stir crazy without this job. Besides, given the current anti-doctor financial climate, I may not be able to retire in 10 years, even if I want to.
But still, it’s an odd realization to think that, after all those applications, and classes, and tests, and rotations, and all the other things you went through ... that your career is closer to wrapping up than it is to the beginning.
How did that happen?
And I’ll continue to try. Even after the halfway point I still get up each morning wanting to help people. The same sentiments I expressed in a personal statement so long ago are still there, and hopefully always will be. When they’re gone, it’s time to leave. Hopefully, they’ll be with me until I’m ready to sign off.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My lease is up later this year, after 5 1/2 years. It doesn’t seem that long. Some days it feels like I just moved in.
As a result, I had an email exchange recently with the building’s manager and we hashed out an agreement on a new 10-year contract. In the process, I realized that sort of time frame might (and, again, I say might) take me into retirement.
And now I’m starting to think about retiring and the career endgame.
Granted, it’s still 10 years away, and knowing me I’ll probably want to work another 5 years or so beyond that if I can. I like what I do and would probably go stir crazy without this job. Besides, given the current anti-doctor financial climate, I may not be able to retire in 10 years, even if I want to.
But still, it’s an odd realization to think that, after all those applications, and classes, and tests, and rotations, and all the other things you went through ... that your career is closer to wrapping up than it is to the beginning.
How did that happen?
And I’ll continue to try. Even after the halfway point I still get up each morning wanting to help people. The same sentiments I expressed in a personal statement so long ago are still there, and hopefully always will be. When they’re gone, it’s time to leave. Hopefully, they’ll be with me until I’m ready to sign off.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My lease is up later this year, after 5 1/2 years. It doesn’t seem that long. Some days it feels like I just moved in.
As a result, I had an email exchange recently with the building’s manager and we hashed out an agreement on a new 10-year contract. In the process, I realized that sort of time frame might (and, again, I say might) take me into retirement.
And now I’m starting to think about retiring and the career endgame.
Granted, it’s still 10 years away, and knowing me I’ll probably want to work another 5 years or so beyond that if I can. I like what I do and would probably go stir crazy without this job. Besides, given the current anti-doctor financial climate, I may not be able to retire in 10 years, even if I want to.
But still, it’s an odd realization to think that, after all those applications, and classes, and tests, and rotations, and all the other things you went through ... that your career is closer to wrapping up than it is to the beginning.
How did that happen?
And I’ll continue to try. Even after the halfway point I still get up each morning wanting to help people. The same sentiments I expressed in a personal statement so long ago are still there, and hopefully always will be. When they’re gone, it’s time to leave. Hopefully, they’ll be with me until I’m ready to sign off.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Office staff cohesiveness remains important
Recently, a lawyer and I were on the phone about a case, and he mentioned how lucky he was to have had the same staff over the course of a 25-year career, and he was afraid they’d retire before he did.
I feel the same way. My medical assistant has been with me since day one 18 years ago, my secretary since 2004. I hope they keep putting up with me until I hang up my reflex hammer.
It’s impossible to put a great team together just by talent alone. The chemistry and ability to work together are as critical as talent, if not more so, and are far more intangible and unpredictable.
I’ve been lucky that way. The three of us are cohesive. We try to keep some degree of fun in our work routine as each day goes on. My secretary’s 2-year-old daughter, who comes with her every day, adds to the family atmosphere that many patients notice. It’s not uncommon to be asked if the group of us are related. (We’re not.)
Back when I started out, it was with a large group that saw its people as replaceable, and treated them as such. As a result there was a high turnover rate of medical assistants and front office and clerical staff. This led to problems with work-flow and patient care, as there was always someone new being trained.
I can’t imagine having a better team than I have now, and will share this advice with anyone starting a practice: When you get the right people, count yourself lucky and do what you have to do to keep them. They’re worth it.
It’s a lot nicer to work with friends than strangers. It makes the drudgery of the job more interesting, the low points better, and the highs fun.
I wouldn’t have it any other way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, a lawyer and I were on the phone about a case, and he mentioned how lucky he was to have had the same staff over the course of a 25-year career, and he was afraid they’d retire before he did.
I feel the same way. My medical assistant has been with me since day one 18 years ago, my secretary since 2004. I hope they keep putting up with me until I hang up my reflex hammer.
It’s impossible to put a great team together just by talent alone. The chemistry and ability to work together are as critical as talent, if not more so, and are far more intangible and unpredictable.
I’ve been lucky that way. The three of us are cohesive. We try to keep some degree of fun in our work routine as each day goes on. My secretary’s 2-year-old daughter, who comes with her every day, adds to the family atmosphere that many patients notice. It’s not uncommon to be asked if the group of us are related. (We’re not.)
Back when I started out, it was with a large group that saw its people as replaceable, and treated them as such. As a result there was a high turnover rate of medical assistants and front office and clerical staff. This led to problems with work-flow and patient care, as there was always someone new being trained.
I can’t imagine having a better team than I have now, and will share this advice with anyone starting a practice: When you get the right people, count yourself lucky and do what you have to do to keep them. They’re worth it.
It’s a lot nicer to work with friends than strangers. It makes the drudgery of the job more interesting, the low points better, and the highs fun.
I wouldn’t have it any other way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently, a lawyer and I were on the phone about a case, and he mentioned how lucky he was to have had the same staff over the course of a 25-year career, and he was afraid they’d retire before he did.
I feel the same way. My medical assistant has been with me since day one 18 years ago, my secretary since 2004. I hope they keep putting up with me until I hang up my reflex hammer.
It’s impossible to put a great team together just by talent alone. The chemistry and ability to work together are as critical as talent, if not more so, and are far more intangible and unpredictable.
I’ve been lucky that way. The three of us are cohesive. We try to keep some degree of fun in our work routine as each day goes on. My secretary’s 2-year-old daughter, who comes with her every day, adds to the family atmosphere that many patients notice. It’s not uncommon to be asked if the group of us are related. (We’re not.)
Back when I started out, it was with a large group that saw its people as replaceable, and treated them as such. As a result there was a high turnover rate of medical assistants and front office and clerical staff. This led to problems with work-flow and patient care, as there was always someone new being trained.
I can’t imagine having a better team than I have now, and will share this advice with anyone starting a practice: When you get the right people, count yourself lucky and do what you have to do to keep them. They’re worth it.
It’s a lot nicer to work with friends than strangers. It makes the drudgery of the job more interesting, the low points better, and the highs fun.
I wouldn’t have it any other way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Serotonin syndrome warnings magnify its rare probability
Serotonin syndrome.
What do those words make you think of? A rare neurological condition? The differential diagnosis you got at 2:00 a.m. from an overly enthusiastic resident? Or a fax from a pharmacy that you get a few times a week?
I’ll say the last.
Triptans are not as common, but are still out there in large numbers. To date, they’re the most effective migraine treatment we have.
Inevitably, these roads will cross, especially because SNRIs, and their older cousins the tricylic antidepressants, are commonly used for migraine prevention. And that’s where the fun begins. There’s a suspected incidence of serotonin syndrome when the two are combined, which became widespread knowledge following a 2006 Food and Drug Administration alert. This is a fact drilled into us by multiple call-backs and faxes from pharmacies, terrified patients who use Google, and electronic prescribing systems that flag our attempts to combine them to make sure we know THIS IS DANGEROUS!
But a study published Feb. 26 in JAMA Neurology found that it’s rarer than anyone suspected (JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144). Breaking down 14 years’ worth of patient data with more than 19,000 patients on both triptans and serotonergic drugs, there were only two cases (0.01%) that clearly met criteria for serotonin syndrome.
I also understand where the warnings come from. When things go bad, medicine becomes a blame game as each side points at another. The pharmacy wants to say they warned us. The e-prescribing system company wants to say they warned us. The patients want to know why no one warned them when a Google search makes it sound common. And the malpractice lawyers want to blame everyone.
But there are more serious side effects out there. Dilantin has been linked to lymphoma. Sinemet (possibly) to melanoma. But do you remember the last time you had to click or sign off on a pharmacy warning for those? Me neither.
Using any drug is a balance of risks and benefits. We make our judgments, discuss concerns with the patients, and roll the dice every day. Side effects aren’t uncommon. Most serious side effects are rare. But warnings that magnify issues with a rare probability don’t help the situation and can keep patients from receiving the help they need.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Serotonin syndrome.
What do those words make you think of? A rare neurological condition? The differential diagnosis you got at 2:00 a.m. from an overly enthusiastic resident? Or a fax from a pharmacy that you get a few times a week?
I’ll say the last.
Triptans are not as common, but are still out there in large numbers. To date, they’re the most effective migraine treatment we have.
Inevitably, these roads will cross, especially because SNRIs, and their older cousins the tricylic antidepressants, are commonly used for migraine prevention. And that’s where the fun begins. There’s a suspected incidence of serotonin syndrome when the two are combined, which became widespread knowledge following a 2006 Food and Drug Administration alert. This is a fact drilled into us by multiple call-backs and faxes from pharmacies, terrified patients who use Google, and electronic prescribing systems that flag our attempts to combine them to make sure we know THIS IS DANGEROUS!
But a study published Feb. 26 in JAMA Neurology found that it’s rarer than anyone suspected (JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144). Breaking down 14 years’ worth of patient data with more than 19,000 patients on both triptans and serotonergic drugs, there were only two cases (0.01%) that clearly met criteria for serotonin syndrome.
I also understand where the warnings come from. When things go bad, medicine becomes a blame game as each side points at another. The pharmacy wants to say they warned us. The e-prescribing system company wants to say they warned us. The patients want to know why no one warned them when a Google search makes it sound common. And the malpractice lawyers want to blame everyone.
But there are more serious side effects out there. Dilantin has been linked to lymphoma. Sinemet (possibly) to melanoma. But do you remember the last time you had to click or sign off on a pharmacy warning for those? Me neither.
Using any drug is a balance of risks and benefits. We make our judgments, discuss concerns with the patients, and roll the dice every day. Side effects aren’t uncommon. Most serious side effects are rare. But warnings that magnify issues with a rare probability don’t help the situation and can keep patients from receiving the help they need.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Serotonin syndrome.
What do those words make you think of? A rare neurological condition? The differential diagnosis you got at 2:00 a.m. from an overly enthusiastic resident? Or a fax from a pharmacy that you get a few times a week?
I’ll say the last.
Triptans are not as common, but are still out there in large numbers. To date, they’re the most effective migraine treatment we have.
Inevitably, these roads will cross, especially because SNRIs, and their older cousins the tricylic antidepressants, are commonly used for migraine prevention. And that’s where the fun begins. There’s a suspected incidence of serotonin syndrome when the two are combined, which became widespread knowledge following a 2006 Food and Drug Administration alert. This is a fact drilled into us by multiple call-backs and faxes from pharmacies, terrified patients who use Google, and electronic prescribing systems that flag our attempts to combine them to make sure we know THIS IS DANGEROUS!
But a study published Feb. 26 in JAMA Neurology found that it’s rarer than anyone suspected (JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144). Breaking down 14 years’ worth of patient data with more than 19,000 patients on both triptans and serotonergic drugs, there were only two cases (0.01%) that clearly met criteria for serotonin syndrome.
I also understand where the warnings come from. When things go bad, medicine becomes a blame game as each side points at another. The pharmacy wants to say they warned us. The e-prescribing system company wants to say they warned us. The patients want to know why no one warned them when a Google search makes it sound common. And the malpractice lawyers want to blame everyone.
But there are more serious side effects out there. Dilantin has been linked to lymphoma. Sinemet (possibly) to melanoma. But do you remember the last time you had to click or sign off on a pharmacy warning for those? Me neither.
Using any drug is a balance of risks and benefits. We make our judgments, discuss concerns with the patients, and roll the dice every day. Side effects aren’t uncommon. Most serious side effects are rare. But warnings that magnify issues with a rare probability don’t help the situation and can keep patients from receiving the help they need.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
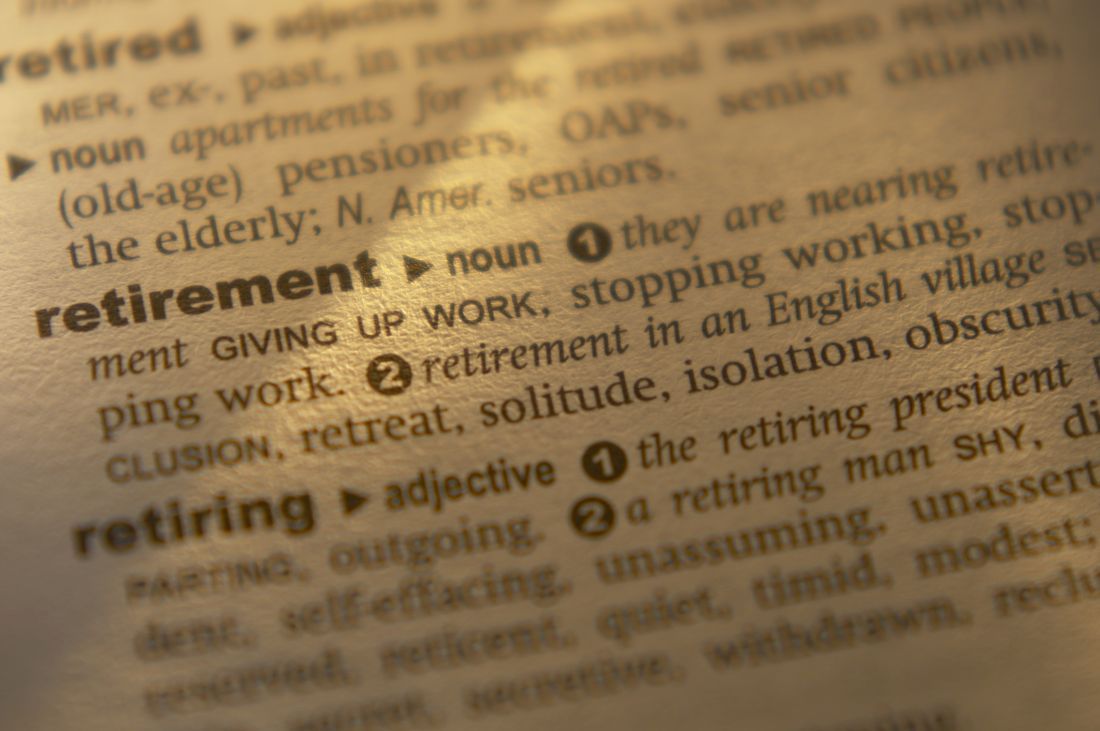
Allscripts’ charges for sending, refilling prescriptions
How much is $9 worth? Not much. Probably less than most people spend on coffee in a given week.
And yet, that $9 is really irritating to me.
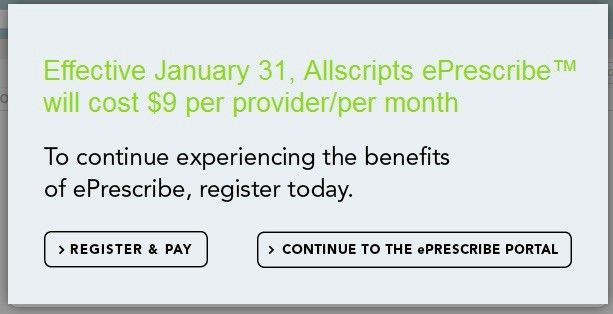
For the last few weeks, when signing into Allscripts to send and refill prescriptions, I’ve encountered this:
I know that $9 a month doesn’t seem like much: It’s $108 a year. But still, it’s irritating.
I understand Allscripts, and every other health care company, is here to make a living. Heck, so am I. Software development isn’t cheap. Neither are the servers hosting it or the security software needed, or the buildings to house them, and a million other things. I get that. None of these things are free.
But, at the same time, it’s part of a general trend of modern health care. Our landlords and vendors can arbitrarily raise prices to keep up with their costs, but we can’t do the same to keep up with ours.
The majority of doctors aren’t in a position to raise our prices to account for these things. We’re stuck with insurance companies and government agencies that tell us to accept a given amount or eat rocks.
There are, of course, concierge practices that can raise their prices, but they’re mostly boutique-level general care with wealthy patients who can afford them. Most small specialists aren’t in that position. We can’t afford to put Keurigs in the lobby.
The few revenue streams most of us have for which we can increase prices, such as legal work and cash patients, are typically not enough of the practice where it would make a difference to overcome it. In fact, the lien company I see patients for recently told me they were lowering their reimbursements to me to compensate for their own higher expenses.
Some people may see the $9 a month as a minor issue and move on. But to a small practice, it’s now another $108 in revenue that I have to bring in each year to cover. And, in a field in which, unlike every other product or service people pay for, I’m not allowed to control my own prices to make up for it.
That doesn’t seem fair, does it?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much is $9 worth? Not much. Probably less than most people spend on coffee in a given week.
And yet, that $9 is really irritating to me.
For the last few weeks, when signing into Allscripts to send and refill prescriptions, I’ve encountered this:
I know that $9 a month doesn’t seem like much: It’s $108 a year. But still, it’s irritating.
I understand Allscripts, and every other health care company, is here to make a living. Heck, so am I. Software development isn’t cheap. Neither are the servers hosting it or the security software needed, or the buildings to house them, and a million other things. I get that. None of these things are free.
But, at the same time, it’s part of a general trend of modern health care. Our landlords and vendors can arbitrarily raise prices to keep up with their costs, but we can’t do the same to keep up with ours.
The majority of doctors aren’t in a position to raise our prices to account for these things. We’re stuck with insurance companies and government agencies that tell us to accept a given amount or eat rocks.
There are, of course, concierge practices that can raise their prices, but they’re mostly boutique-level general care with wealthy patients who can afford them. Most small specialists aren’t in that position. We can’t afford to put Keurigs in the lobby.
The few revenue streams most of us have for which we can increase prices, such as legal work and cash patients, are typically not enough of the practice where it would make a difference to overcome it. In fact, the lien company I see patients for recently told me they were lowering their reimbursements to me to compensate for their own higher expenses.
Some people may see the $9 a month as a minor issue and move on. But to a small practice, it’s now another $108 in revenue that I have to bring in each year to cover. And, in a field in which, unlike every other product or service people pay for, I’m not allowed to control my own prices to make up for it.
That doesn’t seem fair, does it?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much is $9 worth? Not much. Probably less than most people spend on coffee in a given week.
And yet, that $9 is really irritating to me.
For the last few weeks, when signing into Allscripts to send and refill prescriptions, I’ve encountered this:
I know that $9 a month doesn’t seem like much: It’s $108 a year. But still, it’s irritating.
I understand Allscripts, and every other health care company, is here to make a living. Heck, so am I. Software development isn’t cheap. Neither are the servers hosting it or the security software needed, or the buildings to house them, and a million other things. I get that. None of these things are free.
But, at the same time, it’s part of a general trend of modern health care. Our landlords and vendors can arbitrarily raise prices to keep up with their costs, but we can’t do the same to keep up with ours.
The majority of doctors aren’t in a position to raise our prices to account for these things. We’re stuck with insurance companies and government agencies that tell us to accept a given amount or eat rocks.
There are, of course, concierge practices that can raise their prices, but they’re mostly boutique-level general care with wealthy patients who can afford them. Most small specialists aren’t in that position. We can’t afford to put Keurigs in the lobby.
The few revenue streams most of us have for which we can increase prices, such as legal work and cash patients, are typically not enough of the practice where it would make a difference to overcome it. In fact, the lien company I see patients for recently told me they were lowering their reimbursements to me to compensate for their own higher expenses.
Some people may see the $9 a month as a minor issue and move on. But to a small practice, it’s now another $108 in revenue that I have to bring in each year to cover. And, in a field in which, unlike every other product or service people pay for, I’m not allowed to control my own prices to make up for it.
That doesn’t seem fair, does it?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
No improvement in sight for Alzheimer’s drug development
Another one bites the dust.
Yet another investigational agent joins intepirdine, verubecestat, solanezumab, bapineuzumab, latrepirdine, and many others on the scrap pile of research: The complete release of trial data on idalopirdine found the drug wasn’t of clinically significant benefit in Alzheimer’s disease (JAMA. 2018;319[2]:130-42).
The numbers are bad enough that a handful of companies, including the giant Pfizer, have decided to leave Alzheimer’s drug development entirely to focus on more promising fields. And I get that. All of us – on any exhausting, fruitless, task – will reach the point where it’s time to cut our losses and move on. I don’t blame these companies for mostly leaving the field. (Pfizer is planning to form a neuroscience venture fund to support further research.)
Optimists will argue that you still learn things from a negative trial, which is true, but nothing to date is on the immediate horizon to help. The five agents we’ve had available for the past 15-20 years are all old enough to have lost their patents, and their benefits are modest, at best.
And all this going on as the overall human population, including myself, gradually ages and dementia becomes a medical-cost time bomb on the horizon. This isn’t an American problem. Every country in the world is facing it.
Politicians love to promise hope for these things: creating fast-track programs to get drugs to market faster, finding ways to bring down costs so more people can afford them, and improving methods to treat those in need. But none of those things matter if the medications don’t work.
Many of these trials test similar molecules because the evidence to date suggests they’re targeting the cause of Alzheimer’s. But so far they aren’t working. What if, as the Firesign Theatre and others have said, everything you know is wrong?
Perhaps our greatest quality as a species is resilience. We go on because we have to. The planet keeps moving around the sun as it has for almost 5 billion years, and we face tomorrow. Caregivers wake up for another day of doing their best for a faltering parent. I wake up for another day of doing my best to help them. And the researchers go back for another day hoping to find the real answer and treatment. Without trying, no treatment for anything will ever be found. We owe our patients, and ourselves, a better future than that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Another one bites the dust.
Yet another investigational agent joins intepirdine, verubecestat, solanezumab, bapineuzumab, latrepirdine, and many others on the scrap pile of research: The complete release of trial data on idalopirdine found the drug wasn’t of clinically significant benefit in Alzheimer’s disease (JAMA. 2018;319[2]:130-42).
The numbers are bad enough that a handful of companies, including the giant Pfizer, have decided to leave Alzheimer’s drug development entirely to focus on more promising fields. And I get that. All of us – on any exhausting, fruitless, task – will reach the point where it’s time to cut our losses and move on. I don’t blame these companies for mostly leaving the field. (Pfizer is planning to form a neuroscience venture fund to support further research.)
Optimists will argue that you still learn things from a negative trial, which is true, but nothing to date is on the immediate horizon to help. The five agents we’ve had available for the past 15-20 years are all old enough to have lost their patents, and their benefits are modest, at best.
And all this going on as the overall human population, including myself, gradually ages and dementia becomes a medical-cost time bomb on the horizon. This isn’t an American problem. Every country in the world is facing it.
Politicians love to promise hope for these things: creating fast-track programs to get drugs to market faster, finding ways to bring down costs so more people can afford them, and improving methods to treat those in need. But none of those things matter if the medications don’t work.
Many of these trials test similar molecules because the evidence to date suggests they’re targeting the cause of Alzheimer’s. But so far they aren’t working. What if, as the Firesign Theatre and others have said, everything you know is wrong?
Perhaps our greatest quality as a species is resilience. We go on because we have to. The planet keeps moving around the sun as it has for almost 5 billion years, and we face tomorrow. Caregivers wake up for another day of doing their best for a faltering parent. I wake up for another day of doing my best to help them. And the researchers go back for another day hoping to find the real answer and treatment. Without trying, no treatment for anything will ever be found. We owe our patients, and ourselves, a better future than that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Another one bites the dust.
Yet another investigational agent joins intepirdine, verubecestat, solanezumab, bapineuzumab, latrepirdine, and many others on the scrap pile of research: The complete release of trial data on idalopirdine found the drug wasn’t of clinically significant benefit in Alzheimer’s disease (JAMA. 2018;319[2]:130-42).
The numbers are bad enough that a handful of companies, including the giant Pfizer, have decided to leave Alzheimer’s drug development entirely to focus on more promising fields. And I get that. All of us – on any exhausting, fruitless, task – will reach the point where it’s time to cut our losses and move on. I don’t blame these companies for mostly leaving the field. (Pfizer is planning to form a neuroscience venture fund to support further research.)
Optimists will argue that you still learn things from a negative trial, which is true, but nothing to date is on the immediate horizon to help. The five agents we’ve had available for the past 15-20 years are all old enough to have lost their patents, and their benefits are modest, at best.
And all this going on as the overall human population, including myself, gradually ages and dementia becomes a medical-cost time bomb on the horizon. This isn’t an American problem. Every country in the world is facing it.
Politicians love to promise hope for these things: creating fast-track programs to get drugs to market faster, finding ways to bring down costs so more people can afford them, and improving methods to treat those in need. But none of those things matter if the medications don’t work.
Many of these trials test similar molecules because the evidence to date suggests they’re targeting the cause of Alzheimer’s. But so far they aren’t working. What if, as the Firesign Theatre and others have said, everything you know is wrong?
Perhaps our greatest quality as a species is resilience. We go on because we have to. The planet keeps moving around the sun as it has for almost 5 billion years, and we face tomorrow. Caregivers wake up for another day of doing their best for a faltering parent. I wake up for another day of doing my best to help them. And the researchers go back for another day hoping to find the real answer and treatment. Without trying, no treatment for anything will ever be found. We owe our patients, and ourselves, a better future than that.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.