User login
Combined dermatology-rheumatology clinics improve care, spark new research
At the Rheumatic Skin Disease Clinic in Manhasset, N.Y., dermatologist Dr. Amit Garg regularly discusses patient cases and develops care plans alongside rheumatologists after each specialist separately visits the same patient. The dual dermatology-rheumatology clinic has led to countless benefits, including improved quality of care for patients and multi-discipline training for new and veteran physicians, said Dr. Garg, clinic codirector and chair of the dermatology department at North Shore–Long Island Jewish Health System in New York.
Perhaps the greatest advantage of the combined clinic, however, is the research inspiration generated by the collaboration. “Working closely with colleagues in another discipline makes the environment really ripe for new ideas based on observations we may see in the patients we’re treating,” Dr. Garg said in an interview. “It’s amazing how when you’re thinking through a patient’s care together, how quickly you appreciate where the gaps are in our understanding of disease and evaluation and management of disease. From there, you take it to the next step of planning research projects or protocols to essentially fill those gaps in knowledge.”
Dr. Garg’s clinic is one of a growing number at U.S. academic medical centers that combine dermatologic and rheumatologic care for the management of psoriatic arthritis (PsA) and other interrelated skin and musculoskeletal diseases. Clinic operations vary from virtual consults, to simultaneous assessments, to sequential patient visits, but all focus on collaborative care and disease management. The institutions using such models recently united to form the Psoriasis and Psoriatic Arthritis Clinics Multicenter Advancement Network, a national organization that develops research initiatives and assists other centers in creating similar programs. At least 10 institutions are now participating in the network, including NYU Langone Medical Center, New York; Harvard University’s Brigham and Women’s Hospital, Boston; and the National Psoriasis Foundation, Portland, Ore.
Combining dermatology and rheumatology care through a dual clinic follows an ongoing trend by academic medical centers to integrate specialties that treat overlapping conditions, said Dr. Alexis R. Ogdie-Beatty, a rheumatologist at the University of Pennsylvania Health System in Philadelphia and director of the Penn Psoriatic Arthritis Program.
“It was kind of a natural thing for rheumatic disease because our diseases are multisystem in nature in most cases,” Dr. Ogdie-Beatty said in an interview. “I think the increasing knowledge of the need for communication [between specialists] drove this.”
Dr. Ogdie-Beatty leads a virtual rheumatology-dermatology clinic at the University of Pennsylvania where she meets weekly with two dermatologists to discuss research studies, shared patients, and case management. The physicians primarily see patients separately, but occasionally will visit patients at the same time, she said. In addition, dermatologists on the team immediately contact Dr. Ogdie-Beatty if they are seeing a patient who might benefit from an assessment by the rheumatologist and vice versa, she said.
“One of our favorite parts is learning from each other,” Dr. Ogdie-Beatty said in an interview. “I’ve learned a lot about skin disease and psoriasis, and they’ve learned about inflammatory arthritis and management. The ultimate impact for the patient is to have more well rounded care so that both the skin disease and the arthritis are being taken care of in a comprehensive way.”
Dermatology and rheumatology medical students and residents exposed to such clinics have the unique opportunity to learn about disease overlap and strengthen their understanding of the other’s specialty, added Dr. Joseph F. Merola, codirector of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston. Dr. Merola’s center also has created a fellowship program in which either a dermatologist or rheumatologist can spend 1 year training at the clinic.
Research opportunities abound at the combined clinics, physicians said. At the Center for Skin and Related Musculoskeletal Diseases for example, physicians have developed new outcome metrics for measuring psoriasis and screening for PsA, Dr. Merola said. Physicians also commonly refer clinic patients for clinical trials, he said.
“It’s a great place for patients who have been through many other therapies,” said Dr. Merola, who practices dermatology and rheumatology. “If they are at the end of the line, we have a number of clinical trials that we can offer them. Because it tends to be a referral center, these are patients who have more complex disease, so being able to offer them clinical trials and multiple opinions has been really key.”
Dr. Ogdie-Beatty’s clinic is participating in a variety of research studies, including an analysis of vascular inflammation in psoriasis patients. The study is examining markers of early joint inflammation among psoriasis patients who don’t have symptoms of joint pain. Another initiative focuses on how to implement psoriasis and PsA disease activity measures into the medical record, Dr. Ogdie-Beatty said.
At a combined dermatology-rheumatology clinic within the University Health Network, Toronto, doctors are studying the incidence of arthritis and comorbidities in patients with psoriasis, said Dr. Vinod Chandran, a rheumatologist at the University of Toronto. Another ongoing study focuses on identifying risk factors for PsA in patients with psoriasis. The Toronto clinic is participating in the studies as part of the International Psoriasis and Arthritis Research Team.
“There are a number of research opportunities in the combined clinic since a detailed clinical evaluation is extremely important in biomarker and translational studies,” said Dr. Chandran, who codirects the psoriatic arthritis program at the Centre for Prognosis Studies in the Rheumatic Diseases, Toronto. “The clinic also provides an opportunity to participate in phase II and III clinical trials.”
Managing the combined derm-rheum clinics does come with challenges, doctors said. The obstacles are primarily logistical, and include identifying the space, time, and scheduling for the clinic, Dr. Garg said. Other challenges revolve around reimbursement, such as figuring out the best payment structure and ensuring that insurers will cover the simultaneous care, Dr. Merola said. Generally, it also takes longer to see the patient, and physicians may not be able to see as many patients together per day as they could alone, he added. However, physicians stress that the benefits of the combined clinics far outweigh the negatives.
“We’ve always felt the value has been there because we feel the patients really appreciate the service,” he said. “And we think the quality of care around what we do is better.”
On Twitter@legal_med
At the Rheumatic Skin Disease Clinic in Manhasset, N.Y., dermatologist Dr. Amit Garg regularly discusses patient cases and develops care plans alongside rheumatologists after each specialist separately visits the same patient. The dual dermatology-rheumatology clinic has led to countless benefits, including improved quality of care for patients and multi-discipline training for new and veteran physicians, said Dr. Garg, clinic codirector and chair of the dermatology department at North Shore–Long Island Jewish Health System in New York.
Perhaps the greatest advantage of the combined clinic, however, is the research inspiration generated by the collaboration. “Working closely with colleagues in another discipline makes the environment really ripe for new ideas based on observations we may see in the patients we’re treating,” Dr. Garg said in an interview. “It’s amazing how when you’re thinking through a patient’s care together, how quickly you appreciate where the gaps are in our understanding of disease and evaluation and management of disease. From there, you take it to the next step of planning research projects or protocols to essentially fill those gaps in knowledge.”
Dr. Garg’s clinic is one of a growing number at U.S. academic medical centers that combine dermatologic and rheumatologic care for the management of psoriatic arthritis (PsA) and other interrelated skin and musculoskeletal diseases. Clinic operations vary from virtual consults, to simultaneous assessments, to sequential patient visits, but all focus on collaborative care and disease management. The institutions using such models recently united to form the Psoriasis and Psoriatic Arthritis Clinics Multicenter Advancement Network, a national organization that develops research initiatives and assists other centers in creating similar programs. At least 10 institutions are now participating in the network, including NYU Langone Medical Center, New York; Harvard University’s Brigham and Women’s Hospital, Boston; and the National Psoriasis Foundation, Portland, Ore.
Combining dermatology and rheumatology care through a dual clinic follows an ongoing trend by academic medical centers to integrate specialties that treat overlapping conditions, said Dr. Alexis R. Ogdie-Beatty, a rheumatologist at the University of Pennsylvania Health System in Philadelphia and director of the Penn Psoriatic Arthritis Program.
“It was kind of a natural thing for rheumatic disease because our diseases are multisystem in nature in most cases,” Dr. Ogdie-Beatty said in an interview. “I think the increasing knowledge of the need for communication [between specialists] drove this.”
Dr. Ogdie-Beatty leads a virtual rheumatology-dermatology clinic at the University of Pennsylvania where she meets weekly with two dermatologists to discuss research studies, shared patients, and case management. The physicians primarily see patients separately, but occasionally will visit patients at the same time, she said. In addition, dermatologists on the team immediately contact Dr. Ogdie-Beatty if they are seeing a patient who might benefit from an assessment by the rheumatologist and vice versa, she said.
“One of our favorite parts is learning from each other,” Dr. Ogdie-Beatty said in an interview. “I’ve learned a lot about skin disease and psoriasis, and they’ve learned about inflammatory arthritis and management. The ultimate impact for the patient is to have more well rounded care so that both the skin disease and the arthritis are being taken care of in a comprehensive way.”
Dermatology and rheumatology medical students and residents exposed to such clinics have the unique opportunity to learn about disease overlap and strengthen their understanding of the other’s specialty, added Dr. Joseph F. Merola, codirector of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston. Dr. Merola’s center also has created a fellowship program in which either a dermatologist or rheumatologist can spend 1 year training at the clinic.
Research opportunities abound at the combined clinics, physicians said. At the Center for Skin and Related Musculoskeletal Diseases for example, physicians have developed new outcome metrics for measuring psoriasis and screening for PsA, Dr. Merola said. Physicians also commonly refer clinic patients for clinical trials, he said.
“It’s a great place for patients who have been through many other therapies,” said Dr. Merola, who practices dermatology and rheumatology. “If they are at the end of the line, we have a number of clinical trials that we can offer them. Because it tends to be a referral center, these are patients who have more complex disease, so being able to offer them clinical trials and multiple opinions has been really key.”
Dr. Ogdie-Beatty’s clinic is participating in a variety of research studies, including an analysis of vascular inflammation in psoriasis patients. The study is examining markers of early joint inflammation among psoriasis patients who don’t have symptoms of joint pain. Another initiative focuses on how to implement psoriasis and PsA disease activity measures into the medical record, Dr. Ogdie-Beatty said.
At a combined dermatology-rheumatology clinic within the University Health Network, Toronto, doctors are studying the incidence of arthritis and comorbidities in patients with psoriasis, said Dr. Vinod Chandran, a rheumatologist at the University of Toronto. Another ongoing study focuses on identifying risk factors for PsA in patients with psoriasis. The Toronto clinic is participating in the studies as part of the International Psoriasis and Arthritis Research Team.
“There are a number of research opportunities in the combined clinic since a detailed clinical evaluation is extremely important in biomarker and translational studies,” said Dr. Chandran, who codirects the psoriatic arthritis program at the Centre for Prognosis Studies in the Rheumatic Diseases, Toronto. “The clinic also provides an opportunity to participate in phase II and III clinical trials.”
Managing the combined derm-rheum clinics does come with challenges, doctors said. The obstacles are primarily logistical, and include identifying the space, time, and scheduling for the clinic, Dr. Garg said. Other challenges revolve around reimbursement, such as figuring out the best payment structure and ensuring that insurers will cover the simultaneous care, Dr. Merola said. Generally, it also takes longer to see the patient, and physicians may not be able to see as many patients together per day as they could alone, he added. However, physicians stress that the benefits of the combined clinics far outweigh the negatives.
“We’ve always felt the value has been there because we feel the patients really appreciate the service,” he said. “And we think the quality of care around what we do is better.”
On Twitter@legal_med
At the Rheumatic Skin Disease Clinic in Manhasset, N.Y., dermatologist Dr. Amit Garg regularly discusses patient cases and develops care plans alongside rheumatologists after each specialist separately visits the same patient. The dual dermatology-rheumatology clinic has led to countless benefits, including improved quality of care for patients and multi-discipline training for new and veteran physicians, said Dr. Garg, clinic codirector and chair of the dermatology department at North Shore–Long Island Jewish Health System in New York.
Perhaps the greatest advantage of the combined clinic, however, is the research inspiration generated by the collaboration. “Working closely with colleagues in another discipline makes the environment really ripe for new ideas based on observations we may see in the patients we’re treating,” Dr. Garg said in an interview. “It’s amazing how when you’re thinking through a patient’s care together, how quickly you appreciate where the gaps are in our understanding of disease and evaluation and management of disease. From there, you take it to the next step of planning research projects or protocols to essentially fill those gaps in knowledge.”
Dr. Garg’s clinic is one of a growing number at U.S. academic medical centers that combine dermatologic and rheumatologic care for the management of psoriatic arthritis (PsA) and other interrelated skin and musculoskeletal diseases. Clinic operations vary from virtual consults, to simultaneous assessments, to sequential patient visits, but all focus on collaborative care and disease management. The institutions using such models recently united to form the Psoriasis and Psoriatic Arthritis Clinics Multicenter Advancement Network, a national organization that develops research initiatives and assists other centers in creating similar programs. At least 10 institutions are now participating in the network, including NYU Langone Medical Center, New York; Harvard University’s Brigham and Women’s Hospital, Boston; and the National Psoriasis Foundation, Portland, Ore.
Combining dermatology and rheumatology care through a dual clinic follows an ongoing trend by academic medical centers to integrate specialties that treat overlapping conditions, said Dr. Alexis R. Ogdie-Beatty, a rheumatologist at the University of Pennsylvania Health System in Philadelphia and director of the Penn Psoriatic Arthritis Program.
“It was kind of a natural thing for rheumatic disease because our diseases are multisystem in nature in most cases,” Dr. Ogdie-Beatty said in an interview. “I think the increasing knowledge of the need for communication [between specialists] drove this.”
Dr. Ogdie-Beatty leads a virtual rheumatology-dermatology clinic at the University of Pennsylvania where she meets weekly with two dermatologists to discuss research studies, shared patients, and case management. The physicians primarily see patients separately, but occasionally will visit patients at the same time, she said. In addition, dermatologists on the team immediately contact Dr. Ogdie-Beatty if they are seeing a patient who might benefit from an assessment by the rheumatologist and vice versa, she said.
“One of our favorite parts is learning from each other,” Dr. Ogdie-Beatty said in an interview. “I’ve learned a lot about skin disease and psoriasis, and they’ve learned about inflammatory arthritis and management. The ultimate impact for the patient is to have more well rounded care so that both the skin disease and the arthritis are being taken care of in a comprehensive way.”
Dermatology and rheumatology medical students and residents exposed to such clinics have the unique opportunity to learn about disease overlap and strengthen their understanding of the other’s specialty, added Dr. Joseph F. Merola, codirector of the Center for Skin and Related Musculoskeletal Diseases, a combined clinic at Brigham and Women’s Hospital in Boston. Dr. Merola’s center also has created a fellowship program in which either a dermatologist or rheumatologist can spend 1 year training at the clinic.
Research opportunities abound at the combined clinics, physicians said. At the Center for Skin and Related Musculoskeletal Diseases for example, physicians have developed new outcome metrics for measuring psoriasis and screening for PsA, Dr. Merola said. Physicians also commonly refer clinic patients for clinical trials, he said.
“It’s a great place for patients who have been through many other therapies,” said Dr. Merola, who practices dermatology and rheumatology. “If they are at the end of the line, we have a number of clinical trials that we can offer them. Because it tends to be a referral center, these are patients who have more complex disease, so being able to offer them clinical trials and multiple opinions has been really key.”
Dr. Ogdie-Beatty’s clinic is participating in a variety of research studies, including an analysis of vascular inflammation in psoriasis patients. The study is examining markers of early joint inflammation among psoriasis patients who don’t have symptoms of joint pain. Another initiative focuses on how to implement psoriasis and PsA disease activity measures into the medical record, Dr. Ogdie-Beatty said.
At a combined dermatology-rheumatology clinic within the University Health Network, Toronto, doctors are studying the incidence of arthritis and comorbidities in patients with psoriasis, said Dr. Vinod Chandran, a rheumatologist at the University of Toronto. Another ongoing study focuses on identifying risk factors for PsA in patients with psoriasis. The Toronto clinic is participating in the studies as part of the International Psoriasis and Arthritis Research Team.
“There are a number of research opportunities in the combined clinic since a detailed clinical evaluation is extremely important in biomarker and translational studies,” said Dr. Chandran, who codirects the psoriatic arthritis program at the Centre for Prognosis Studies in the Rheumatic Diseases, Toronto. “The clinic also provides an opportunity to participate in phase II and III clinical trials.”
Managing the combined derm-rheum clinics does come with challenges, doctors said. The obstacles are primarily logistical, and include identifying the space, time, and scheduling for the clinic, Dr. Garg said. Other challenges revolve around reimbursement, such as figuring out the best payment structure and ensuring that insurers will cover the simultaneous care, Dr. Merola said. Generally, it also takes longer to see the patient, and physicians may not be able to see as many patients together per day as they could alone, he added. However, physicians stress that the benefits of the combined clinics far outweigh the negatives.
“We’ve always felt the value has been there because we feel the patients really appreciate the service,” he said. “And we think the quality of care around what we do is better.”
On Twitter@legal_med
Half of uninsured patients are eligible for Medicaid or ACA coverage
Nearly half of nonelderly uninsured patients are eligible for Medicaid or subsidized coverage through the Affordable Care Act (ACA) marketplace, according to a study released Oct. 13 by the Kaiser Family Foundation.
More than a quarter of uninsured patients at the start of 2015 were adults eligible for Medicaid or children eligible for Medicaid or the Children’s Health Insurance Program. One in five of the nonelderly uninsured population were eligible for premium tax credits to purchase coverage through the ACA marketplace.
For the study, Kaiser researchers analyzed data from the 2015 Current Population Survey Annual Social and Economic Supplement, which provides socioeconomic and demographic information for the United States population and specific subpopulations. Of 32 million uninsured patients at the start of 2015, 16 million (49%) were eligible for state or federal government assistance through Medicaid or the ACA. One in ten (3.1 million) fell into the coverage gap because of their state’s decision not to expand Medicaid, according to the study. About 15% of the uninsured (4.9 million) patients were undocumented immigrants ineligible for ACA coverage under federal law. The remainder of the uninsured were not eligible for assistance under the ACA because they have access to employer coverage or have incomes too high to qualify for Medicaid or marketplace subsidies.
The rate of uninsured patients eligible for either ACA-based coverage or Medicaid varied widely across states. In Nebraska and Texas, 35% of nonelderly uninsured patients were eligible for coverage, while in West Virginia, 75% of uninsured patients were eligible for coverage under Medicaid or the ACA. Five states account for 40% of the uninsured population that could receive Medicaid or subsidized private coverage under the ACA, including California (2 million), Texas (1.5 million), Florida (1 million), New York (865,000), and Pennsylvania (656,000).
The authors concluded that there are still significant opportunities for the government to increase the number of insured patients under the ACA by reaching these eligible patients before the 2016 open enrollment period begins on Nov. 1. However, the authors note that, in many cases, the uninsured will remain uninsured because they are either undocumented or live in states that have not expanded Medicaid.
On Twitter @legal_med
Nearly half of nonelderly uninsured patients are eligible for Medicaid or subsidized coverage through the Affordable Care Act (ACA) marketplace, according to a study released Oct. 13 by the Kaiser Family Foundation.
More than a quarter of uninsured patients at the start of 2015 were adults eligible for Medicaid or children eligible for Medicaid or the Children’s Health Insurance Program. One in five of the nonelderly uninsured population were eligible for premium tax credits to purchase coverage through the ACA marketplace.
For the study, Kaiser researchers analyzed data from the 2015 Current Population Survey Annual Social and Economic Supplement, which provides socioeconomic and demographic information for the United States population and specific subpopulations. Of 32 million uninsured patients at the start of 2015, 16 million (49%) were eligible for state or federal government assistance through Medicaid or the ACA. One in ten (3.1 million) fell into the coverage gap because of their state’s decision not to expand Medicaid, according to the study. About 15% of the uninsured (4.9 million) patients were undocumented immigrants ineligible for ACA coverage under federal law. The remainder of the uninsured were not eligible for assistance under the ACA because they have access to employer coverage or have incomes too high to qualify for Medicaid or marketplace subsidies.
The rate of uninsured patients eligible for either ACA-based coverage or Medicaid varied widely across states. In Nebraska and Texas, 35% of nonelderly uninsured patients were eligible for coverage, while in West Virginia, 75% of uninsured patients were eligible for coverage under Medicaid or the ACA. Five states account for 40% of the uninsured population that could receive Medicaid or subsidized private coverage under the ACA, including California (2 million), Texas (1.5 million), Florida (1 million), New York (865,000), and Pennsylvania (656,000).
The authors concluded that there are still significant opportunities for the government to increase the number of insured patients under the ACA by reaching these eligible patients before the 2016 open enrollment period begins on Nov. 1. However, the authors note that, in many cases, the uninsured will remain uninsured because they are either undocumented or live in states that have not expanded Medicaid.
On Twitter @legal_med
Nearly half of nonelderly uninsured patients are eligible for Medicaid or subsidized coverage through the Affordable Care Act (ACA) marketplace, according to a study released Oct. 13 by the Kaiser Family Foundation.
More than a quarter of uninsured patients at the start of 2015 were adults eligible for Medicaid or children eligible for Medicaid or the Children’s Health Insurance Program. One in five of the nonelderly uninsured population were eligible for premium tax credits to purchase coverage through the ACA marketplace.
For the study, Kaiser researchers analyzed data from the 2015 Current Population Survey Annual Social and Economic Supplement, which provides socioeconomic and demographic information for the United States population and specific subpopulations. Of 32 million uninsured patients at the start of 2015, 16 million (49%) were eligible for state or federal government assistance through Medicaid or the ACA. One in ten (3.1 million) fell into the coverage gap because of their state’s decision not to expand Medicaid, according to the study. About 15% of the uninsured (4.9 million) patients were undocumented immigrants ineligible for ACA coverage under federal law. The remainder of the uninsured were not eligible for assistance under the ACA because they have access to employer coverage or have incomes too high to qualify for Medicaid or marketplace subsidies.
The rate of uninsured patients eligible for either ACA-based coverage or Medicaid varied widely across states. In Nebraska and Texas, 35% of nonelderly uninsured patients were eligible for coverage, while in West Virginia, 75% of uninsured patients were eligible for coverage under Medicaid or the ACA. Five states account for 40% of the uninsured population that could receive Medicaid or subsidized private coverage under the ACA, including California (2 million), Texas (1.5 million), Florida (1 million), New York (865,000), and Pennsylvania (656,000).
The authors concluded that there are still significant opportunities for the government to increase the number of insured patients under the ACA by reaching these eligible patients before the 2016 open enrollment period begins on Nov. 1. However, the authors note that, in many cases, the uninsured will remain uninsured because they are either undocumented or live in states that have not expanded Medicaid.
On Twitter @legal_med
Small study: Physicians sued for failing to supervise soft-tissue filler procedures
In medical malpractice claims involving soft-tissue fillers, dermatologists and other doctors were frequently named as defendants for allegedly failing to supervise nonphysicians who did the procedures, in a study published in the October issue of the Journal of the American Academy of Dermatology.
In a study of 24 legal and administrative actions, physicians were sued in 13 of the cases, although physician extenders injected the fillers in half of those actions. The results were reported in a research letter (J Am Acad Dermatol. 2015 Oct;73[4]:702-4).
Dr. Navid Ezra, a private practice dermatologist and former resident at Indiana University, Indianapolis, and colleagues analyzed public legal documents from 1995 to 2013 using the national legal research service WestlawNext. They searched three database categories: cases, trial court orders, and administrative guidance and decisions. The categories included opinions by state and federal trial, appellate, and supreme courts, as well as regulatory agencies such as medical boards. A total of 24 legal documents involving soft-tissue fillers were identified – 19 legal cases and 5 disciplinary actions.
Dermatologists and plastic surgeons were sued most often, each accounting for 17% of cases respectively, according to the study. Family practice physicians were named as defendants in 8% of cases. Radiologists, pediatricians, internists, oculoplastic surgeons, and physical medicine/rehabilitation doctors were each named as defendants in 4% of the cases, respectively. Nonphysicians were sued in 25% of cases. Many of the lawsuits named multiple defendants.
The most common injury that resulted in litigation was granuloma formation or other autoimmune reaction. Zyderm was the soft-tissue filler most commonly associated with litigation. However, the authors noted that Zyderm was the first soft-tissue filler approved and temporal bias likely explains the higher number of associated cases.
Of the five disciplinary actions, the majority of doctors were reprimanded for not being present while a nonphysician employee injected patients with soft-tissue fillers. In three of the five reprimands, physicians were functioning as medical directors of medical spas.
The authors concluded that the medico-legal culture is such that physicians are responsible for actions by their physician extenders. They called for further research to evaluate whether the presence of a physician during soft-tissue filler procedures affects the rate of developing complications. They noted that the study’s total number of cases and disciplinary actions underreports the true incidence of legal events related to soft-tissue fillers. The sample size did not include settlements or cases that did not involve an appeal.
On Twitter @legal_med
In medical malpractice claims involving soft-tissue fillers, dermatologists and other doctors were frequently named as defendants for allegedly failing to supervise nonphysicians who did the procedures, in a study published in the October issue of the Journal of the American Academy of Dermatology.
In a study of 24 legal and administrative actions, physicians were sued in 13 of the cases, although physician extenders injected the fillers in half of those actions. The results were reported in a research letter (J Am Acad Dermatol. 2015 Oct;73[4]:702-4).
Dr. Navid Ezra, a private practice dermatologist and former resident at Indiana University, Indianapolis, and colleagues analyzed public legal documents from 1995 to 2013 using the national legal research service WestlawNext. They searched three database categories: cases, trial court orders, and administrative guidance and decisions. The categories included opinions by state and federal trial, appellate, and supreme courts, as well as regulatory agencies such as medical boards. A total of 24 legal documents involving soft-tissue fillers were identified – 19 legal cases and 5 disciplinary actions.
Dermatologists and plastic surgeons were sued most often, each accounting for 17% of cases respectively, according to the study. Family practice physicians were named as defendants in 8% of cases. Radiologists, pediatricians, internists, oculoplastic surgeons, and physical medicine/rehabilitation doctors were each named as defendants in 4% of the cases, respectively. Nonphysicians were sued in 25% of cases. Many of the lawsuits named multiple defendants.
The most common injury that resulted in litigation was granuloma formation or other autoimmune reaction. Zyderm was the soft-tissue filler most commonly associated with litigation. However, the authors noted that Zyderm was the first soft-tissue filler approved and temporal bias likely explains the higher number of associated cases.
Of the five disciplinary actions, the majority of doctors were reprimanded for not being present while a nonphysician employee injected patients with soft-tissue fillers. In three of the five reprimands, physicians were functioning as medical directors of medical spas.
The authors concluded that the medico-legal culture is such that physicians are responsible for actions by their physician extenders. They called for further research to evaluate whether the presence of a physician during soft-tissue filler procedures affects the rate of developing complications. They noted that the study’s total number of cases and disciplinary actions underreports the true incidence of legal events related to soft-tissue fillers. The sample size did not include settlements or cases that did not involve an appeal.
On Twitter @legal_med
In medical malpractice claims involving soft-tissue fillers, dermatologists and other doctors were frequently named as defendants for allegedly failing to supervise nonphysicians who did the procedures, in a study published in the October issue of the Journal of the American Academy of Dermatology.
In a study of 24 legal and administrative actions, physicians were sued in 13 of the cases, although physician extenders injected the fillers in half of those actions. The results were reported in a research letter (J Am Acad Dermatol. 2015 Oct;73[4]:702-4).
Dr. Navid Ezra, a private practice dermatologist and former resident at Indiana University, Indianapolis, and colleagues analyzed public legal documents from 1995 to 2013 using the national legal research service WestlawNext. They searched three database categories: cases, trial court orders, and administrative guidance and decisions. The categories included opinions by state and federal trial, appellate, and supreme courts, as well as regulatory agencies such as medical boards. A total of 24 legal documents involving soft-tissue fillers were identified – 19 legal cases and 5 disciplinary actions.
Dermatologists and plastic surgeons were sued most often, each accounting for 17% of cases respectively, according to the study. Family practice physicians were named as defendants in 8% of cases. Radiologists, pediatricians, internists, oculoplastic surgeons, and physical medicine/rehabilitation doctors were each named as defendants in 4% of the cases, respectively. Nonphysicians were sued in 25% of cases. Many of the lawsuits named multiple defendants.
The most common injury that resulted in litigation was granuloma formation or other autoimmune reaction. Zyderm was the soft-tissue filler most commonly associated with litigation. However, the authors noted that Zyderm was the first soft-tissue filler approved and temporal bias likely explains the higher number of associated cases.
Of the five disciplinary actions, the majority of doctors were reprimanded for not being present while a nonphysician employee injected patients with soft-tissue fillers. In three of the five reprimands, physicians were functioning as medical directors of medical spas.
The authors concluded that the medico-legal culture is such that physicians are responsible for actions by their physician extenders. They called for further research to evaluate whether the presence of a physician during soft-tissue filler procedures affects the rate of developing complications. They noted that the study’s total number of cases and disciplinary actions underreports the true incidence of legal events related to soft-tissue fillers. The sample size did not include settlements or cases that did not involve an appeal.
On Twitter @legal_med
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point: A study shows that some medical malpractice claims involving soft-tissue fillers result from procedures performed by nonphysicians, but dermatologists and plastic surgeons are frequently named as defendants for allegedly failing to supervise.
Major finding: In a study of 24 legal and administrative actions, physicians were sued in 13 of the cases, although physician extenders injected the fillers in half of those actions.
Data source: The cases were identified in a search for relevant public legal documents in a national legal database from 1995 to 2013.
Disclosures: The authors had no relevant disclosures; and there was no funding source.
CDC: Hospital support of breastfeeding grows, but improvements needed
Hospital support for breastfeeding mothers has nearly doubled nationwide through a global initiative, but more work is needed to increase the number of baby-friendly hospitals, according to an Oct. 6 Vital Signs report released by the Centers for Disease Control and Prevention.
The report found the rate of U.S. hospitals using the World Health Organization’s Ten Steps to Successful Breastfeeding rose from 29% in 2007 to 54% in 2013.
“What happens in the hospital can determine whether a mom starts and continues to breastfeed, and we know that many moms – 60% – stop breastfeeding earlier than they’d like,” said CDC epidemiologist Cria Perrine, PhD, in a statement. “These improvements in hospital support for breastfeeding are promising, but we also want to see more hospitals fully supporting mothers who want to breastfeed. The Ten Steps help ensure that mothers get the best start with breastfeeding.”
Of the nearly 4 million babies born each year in the United States, 14% are born in “baby-friendly” hospitals, a number that has almost tripled in recent years, but remains low, according to the CDC. The Baby-Friendly Hospital Initiative was established by the World Health Organization and UNICEF and is endorsed by the American Academy of Pediatrics. The core of the initiative is the Ten Steps to Successful Breastfeeding, which measures a hospital’s breastfeeding support before, during, and after a mother’s hospital stay.
The report, “Vital Signs: Improvements in Maternity Care Policies and Practices That Support Breastfeeding — United States, 2007–2013,” examined data from CDC’s national survey, Maternity Practices in Infant Nutrition and Care, which measures the percentage of U.S. hospitals with practices that are consistent with the Ten Steps to Successful Breastfeeding. Findings showed that in 2013, 93% of hospitals provided high levels of: prenatal breastfeeding education, up from 91% in 2007. A majority of hospitals also taught mothers breastfeeding techniques – 92% in 2013 compared with 88% in 2007. Sixty-five percent of hospitals promoted early initiation of breastfeeding for mothers, up from 44% in 2007.
However, CDC leaders note that other findings demonstrate the need for improvement. For example, just over a quarter of hospitals surveyed had a model breastfeeding policy, commonly the foundation for many of the steps. Additionally, just 26% of hospitals ensured that only breast milk was given to healthy, breastfeeding infants who did not need infant formula for a medical reason in 2013. Only 45% of hospitals in 2013 kept mothers and babies together through their entire hospital stay, a practice which provides opportunities to breastfeed and helps mothers learn feeding cues, the report found. Just 32% of hospitals provided enough support for breastfeeding mothers when they left the hospital, including follow-up visits, phone calls, and referrals for additional support. These percentages were only slight increases from 2007, said CDC Director Dr. Tom Frieden during an Oct. 6 press conference.
“Every 1 of the 10 steps is important to use in the hospital to give babies the best start [and] to help mothers start and continue to breastfeed as recommended,” Dr. Frieden said. “I’d like to ask hospitals to keep making progress. Make a plan for what you can do right now that’s in line with the 10 steps, and phase that in over time. Ideally, we’d like every birth hospital in this country to adopt all of the 10 steps and become baby-friendly.”
Dr. Perrine acknowledged that hospitals are not without challenges in implementing the Ten Steps. Primary obstacles could be convincing hospital leadership to focus on the initiative, training staff, and confronting push-back from senior labor and delivery employees, Dr. Perrine said.
The CDC calls for more hospitals to implement the Ten Steps to Successful Breastfeeding and to work toward achieving baby-friendly status. Hospitals can also participate in CDC’s Maternity Practices in Infant Nutrition and Care survey and get an individualized report that shows how they compare with other hospitals. Additionally, hospitals should work with physicians, nurses, lactation care providers, and other organizations to develop networks that can provide clinic-based, at-home, or community breastfeeding support.
“Doctors can make a really big difference in encouraging and supporting women who choose to breastfeed,” Dr. Frieden said during the press conference. “And hospitals can play a critical role in those first few days of life which really do form the basis of the pattern of breastfeeding.”
On Twitter @legal_med
Hospital support for breastfeeding mothers has nearly doubled nationwide through a global initiative, but more work is needed to increase the number of baby-friendly hospitals, according to an Oct. 6 Vital Signs report released by the Centers for Disease Control and Prevention.
The report found the rate of U.S. hospitals using the World Health Organization’s Ten Steps to Successful Breastfeeding rose from 29% in 2007 to 54% in 2013.
“What happens in the hospital can determine whether a mom starts and continues to breastfeed, and we know that many moms – 60% – stop breastfeeding earlier than they’d like,” said CDC epidemiologist Cria Perrine, PhD, in a statement. “These improvements in hospital support for breastfeeding are promising, but we also want to see more hospitals fully supporting mothers who want to breastfeed. The Ten Steps help ensure that mothers get the best start with breastfeeding.”
Of the nearly 4 million babies born each year in the United States, 14% are born in “baby-friendly” hospitals, a number that has almost tripled in recent years, but remains low, according to the CDC. The Baby-Friendly Hospital Initiative was established by the World Health Organization and UNICEF and is endorsed by the American Academy of Pediatrics. The core of the initiative is the Ten Steps to Successful Breastfeeding, which measures a hospital’s breastfeeding support before, during, and after a mother’s hospital stay.
The report, “Vital Signs: Improvements in Maternity Care Policies and Practices That Support Breastfeeding — United States, 2007–2013,” examined data from CDC’s national survey, Maternity Practices in Infant Nutrition and Care, which measures the percentage of U.S. hospitals with practices that are consistent with the Ten Steps to Successful Breastfeeding. Findings showed that in 2013, 93% of hospitals provided high levels of: prenatal breastfeeding education, up from 91% in 2007. A majority of hospitals also taught mothers breastfeeding techniques – 92% in 2013 compared with 88% in 2007. Sixty-five percent of hospitals promoted early initiation of breastfeeding for mothers, up from 44% in 2007.
However, CDC leaders note that other findings demonstrate the need for improvement. For example, just over a quarter of hospitals surveyed had a model breastfeeding policy, commonly the foundation for many of the steps. Additionally, just 26% of hospitals ensured that only breast milk was given to healthy, breastfeeding infants who did not need infant formula for a medical reason in 2013. Only 45% of hospitals in 2013 kept mothers and babies together through their entire hospital stay, a practice which provides opportunities to breastfeed and helps mothers learn feeding cues, the report found. Just 32% of hospitals provided enough support for breastfeeding mothers when they left the hospital, including follow-up visits, phone calls, and referrals for additional support. These percentages were only slight increases from 2007, said CDC Director Dr. Tom Frieden during an Oct. 6 press conference.
“Every 1 of the 10 steps is important to use in the hospital to give babies the best start [and] to help mothers start and continue to breastfeed as recommended,” Dr. Frieden said. “I’d like to ask hospitals to keep making progress. Make a plan for what you can do right now that’s in line with the 10 steps, and phase that in over time. Ideally, we’d like every birth hospital in this country to adopt all of the 10 steps and become baby-friendly.”
Dr. Perrine acknowledged that hospitals are not without challenges in implementing the Ten Steps. Primary obstacles could be convincing hospital leadership to focus on the initiative, training staff, and confronting push-back from senior labor and delivery employees, Dr. Perrine said.
The CDC calls for more hospitals to implement the Ten Steps to Successful Breastfeeding and to work toward achieving baby-friendly status. Hospitals can also participate in CDC’s Maternity Practices in Infant Nutrition and Care survey and get an individualized report that shows how they compare with other hospitals. Additionally, hospitals should work with physicians, nurses, lactation care providers, and other organizations to develop networks that can provide clinic-based, at-home, or community breastfeeding support.
“Doctors can make a really big difference in encouraging and supporting women who choose to breastfeed,” Dr. Frieden said during the press conference. “And hospitals can play a critical role in those first few days of life which really do form the basis of the pattern of breastfeeding.”
On Twitter @legal_med
Hospital support for breastfeeding mothers has nearly doubled nationwide through a global initiative, but more work is needed to increase the number of baby-friendly hospitals, according to an Oct. 6 Vital Signs report released by the Centers for Disease Control and Prevention.
The report found the rate of U.S. hospitals using the World Health Organization’s Ten Steps to Successful Breastfeeding rose from 29% in 2007 to 54% in 2013.
“What happens in the hospital can determine whether a mom starts and continues to breastfeed, and we know that many moms – 60% – stop breastfeeding earlier than they’d like,” said CDC epidemiologist Cria Perrine, PhD, in a statement. “These improvements in hospital support for breastfeeding are promising, but we also want to see more hospitals fully supporting mothers who want to breastfeed. The Ten Steps help ensure that mothers get the best start with breastfeeding.”
Of the nearly 4 million babies born each year in the United States, 14% are born in “baby-friendly” hospitals, a number that has almost tripled in recent years, but remains low, according to the CDC. The Baby-Friendly Hospital Initiative was established by the World Health Organization and UNICEF and is endorsed by the American Academy of Pediatrics. The core of the initiative is the Ten Steps to Successful Breastfeeding, which measures a hospital’s breastfeeding support before, during, and after a mother’s hospital stay.
The report, “Vital Signs: Improvements in Maternity Care Policies and Practices That Support Breastfeeding — United States, 2007–2013,” examined data from CDC’s national survey, Maternity Practices in Infant Nutrition and Care, which measures the percentage of U.S. hospitals with practices that are consistent with the Ten Steps to Successful Breastfeeding. Findings showed that in 2013, 93% of hospitals provided high levels of: prenatal breastfeeding education, up from 91% in 2007. A majority of hospitals also taught mothers breastfeeding techniques – 92% in 2013 compared with 88% in 2007. Sixty-five percent of hospitals promoted early initiation of breastfeeding for mothers, up from 44% in 2007.
However, CDC leaders note that other findings demonstrate the need for improvement. For example, just over a quarter of hospitals surveyed had a model breastfeeding policy, commonly the foundation for many of the steps. Additionally, just 26% of hospitals ensured that only breast milk was given to healthy, breastfeeding infants who did not need infant formula for a medical reason in 2013. Only 45% of hospitals in 2013 kept mothers and babies together through their entire hospital stay, a practice which provides opportunities to breastfeed and helps mothers learn feeding cues, the report found. Just 32% of hospitals provided enough support for breastfeeding mothers when they left the hospital, including follow-up visits, phone calls, and referrals for additional support. These percentages were only slight increases from 2007, said CDC Director Dr. Tom Frieden during an Oct. 6 press conference.
“Every 1 of the 10 steps is important to use in the hospital to give babies the best start [and] to help mothers start and continue to breastfeed as recommended,” Dr. Frieden said. “I’d like to ask hospitals to keep making progress. Make a plan for what you can do right now that’s in line with the 10 steps, and phase that in over time. Ideally, we’d like every birth hospital in this country to adopt all of the 10 steps and become baby-friendly.”
Dr. Perrine acknowledged that hospitals are not without challenges in implementing the Ten Steps. Primary obstacles could be convincing hospital leadership to focus on the initiative, training staff, and confronting push-back from senior labor and delivery employees, Dr. Perrine said.
The CDC calls for more hospitals to implement the Ten Steps to Successful Breastfeeding and to work toward achieving baby-friendly status. Hospitals can also participate in CDC’s Maternity Practices in Infant Nutrition and Care survey and get an individualized report that shows how they compare with other hospitals. Additionally, hospitals should work with physicians, nurses, lactation care providers, and other organizations to develop networks that can provide clinic-based, at-home, or community breastfeeding support.
“Doctors can make a really big difference in encouraging and supporting women who choose to breastfeed,” Dr. Frieden said during the press conference. “And hospitals can play a critical role in those first few days of life which really do form the basis of the pattern of breastfeeding.”
On Twitter @legal_med
Multistate compact could ease telemedicine licensing woes
As telemedicine hospitalists, one of the biggest challenges for Dr. Dana Giarrizzi and her staff is learning and staying updated on the many different state licensing rules.
Renewal time and dates vary, along with state requirements to become licensed and remain current, said Dr. Giarrizzi, national medical director for telehospitalist services at Eagle Hospital Physicians, based in Atlanta.
“One state renews on your birthday,” she said. Another “renews when you first activated your license. This one is every 2 years. This one requires CME. It’s hard to keep up with all the rules, and it’s costly.”
Dr. Giarrizzi believes a federal licensure process would be ideal, but she is also hopeful about state legislation in the form of the Interstate Medical Licensure Compact. The model legislation was developed by the Federation of State Medical Boards (FSMB) and aims to make it easier for telemedicine physicians to gain licenses in multiple states.
Under the legislation, physicians designate a member state as the state of principal licensure and select the other states they wish to gain licenses within. The state of principal licensure then verifies the physician’s eligibility and provides credential information to the interstate commission, which collects applicable fees and transmits the doctor’s information to the other states. Upon receipt in the additional states, the physician would be granted a license.
As of early October 2015, 11 states had enacted the compact legislation, and at least 19 states had introduced the legislation. In July, the Health Resources and Services Administration awarded the FSMB a grant to support establishment of the commission and aid with the compact’s infrastructure.
Broad support by medical associations, patients, and state leaders have quickly propelled the compact forward, said Lisa Robin, FSMB chief advocacy officer.
“I think the boards recognize the potential for telemedicine and what that can bring as far as access to health care,” Ms. Robin said. “As technologies are here – and it’s changing every day – this is a mechanism that will allow for much more efficiency and less administrative burden on the process for licensure for physicians who want to practice in multiple states.”
There have been several misconceptions tied to the compact law, Ms. Robin noted.
The compact does not change a state’s medical practice act, she stressed, nor does it create a national licensure system. In addition, the legislation does not require a physician to participate in maintenance of certification at any stage. Under the compact, approved physicians would be under the jurisdiction of the state medical board in which the patient is located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight.
The compact hopefully will reduce physicians’ frustrations and lessen administrative hassles for doctors who wish to use telehealth technologies to bring their expertise to patients across multiple states, said Dr. Reed V. Tuckson, president of the American Telemedicine Association.
“There have been several models proposed to address both of these objectives, and it appears that the Federation of State Medical Boards’ licensure model compact has emerged as the most practical and implementable of the various approaches,” Dr. Tuckson explained. “We do hope that this compact model can function efficiently and cost effectively, so that physicians are not overburdened as well-meaning organizations attempt to ensure that the public’s interests are safeguarded.”
Dr. Giarrizzi of Eagle Hospital Physicians is also optimistic about the compact.
“I am hoping this helps streamline the information,” she said. “I know it will still take time, because it is not taking away the need to go through the process, but seems more like it is just sharing the information. It will make it easier for us to cross state lines if the states we want to work in agree with this process and participate.”
On Twitter @legal_med
As telemedicine hospitalists, one of the biggest challenges for Dr. Dana Giarrizzi and her staff is learning and staying updated on the many different state licensing rules.
Renewal time and dates vary, along with state requirements to become licensed and remain current, said Dr. Giarrizzi, national medical director for telehospitalist services at Eagle Hospital Physicians, based in Atlanta.
“One state renews on your birthday,” she said. Another “renews when you first activated your license. This one is every 2 years. This one requires CME. It’s hard to keep up with all the rules, and it’s costly.”
Dr. Giarrizzi believes a federal licensure process would be ideal, but she is also hopeful about state legislation in the form of the Interstate Medical Licensure Compact. The model legislation was developed by the Federation of State Medical Boards (FSMB) and aims to make it easier for telemedicine physicians to gain licenses in multiple states.
Under the legislation, physicians designate a member state as the state of principal licensure and select the other states they wish to gain licenses within. The state of principal licensure then verifies the physician’s eligibility and provides credential information to the interstate commission, which collects applicable fees and transmits the doctor’s information to the other states. Upon receipt in the additional states, the physician would be granted a license.
As of early October 2015, 11 states had enacted the compact legislation, and at least 19 states had introduced the legislation. In July, the Health Resources and Services Administration awarded the FSMB a grant to support establishment of the commission and aid with the compact’s infrastructure.
Broad support by medical associations, patients, and state leaders have quickly propelled the compact forward, said Lisa Robin, FSMB chief advocacy officer.
“I think the boards recognize the potential for telemedicine and what that can bring as far as access to health care,” Ms. Robin said. “As technologies are here – and it’s changing every day – this is a mechanism that will allow for much more efficiency and less administrative burden on the process for licensure for physicians who want to practice in multiple states.”
There have been several misconceptions tied to the compact law, Ms. Robin noted.
The compact does not change a state’s medical practice act, she stressed, nor does it create a national licensure system. In addition, the legislation does not require a physician to participate in maintenance of certification at any stage. Under the compact, approved physicians would be under the jurisdiction of the state medical board in which the patient is located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight.
The compact hopefully will reduce physicians’ frustrations and lessen administrative hassles for doctors who wish to use telehealth technologies to bring their expertise to patients across multiple states, said Dr. Reed V. Tuckson, president of the American Telemedicine Association.
“There have been several models proposed to address both of these objectives, and it appears that the Federation of State Medical Boards’ licensure model compact has emerged as the most practical and implementable of the various approaches,” Dr. Tuckson explained. “We do hope that this compact model can function efficiently and cost effectively, so that physicians are not overburdened as well-meaning organizations attempt to ensure that the public’s interests are safeguarded.”
Dr. Giarrizzi of Eagle Hospital Physicians is also optimistic about the compact.
“I am hoping this helps streamline the information,” she said. “I know it will still take time, because it is not taking away the need to go through the process, but seems more like it is just sharing the information. It will make it easier for us to cross state lines if the states we want to work in agree with this process and participate.”
On Twitter @legal_med
As telemedicine hospitalists, one of the biggest challenges for Dr. Dana Giarrizzi and her staff is learning and staying updated on the many different state licensing rules.
Renewal time and dates vary, along with state requirements to become licensed and remain current, said Dr. Giarrizzi, national medical director for telehospitalist services at Eagle Hospital Physicians, based in Atlanta.
“One state renews on your birthday,” she said. Another “renews when you first activated your license. This one is every 2 years. This one requires CME. It’s hard to keep up with all the rules, and it’s costly.”
Dr. Giarrizzi believes a federal licensure process would be ideal, but she is also hopeful about state legislation in the form of the Interstate Medical Licensure Compact. The model legislation was developed by the Federation of State Medical Boards (FSMB) and aims to make it easier for telemedicine physicians to gain licenses in multiple states.
Under the legislation, physicians designate a member state as the state of principal licensure and select the other states they wish to gain licenses within. The state of principal licensure then verifies the physician’s eligibility and provides credential information to the interstate commission, which collects applicable fees and transmits the doctor’s information to the other states. Upon receipt in the additional states, the physician would be granted a license.
As of early October 2015, 11 states had enacted the compact legislation, and at least 19 states had introduced the legislation. In July, the Health Resources and Services Administration awarded the FSMB a grant to support establishment of the commission and aid with the compact’s infrastructure.
Broad support by medical associations, patients, and state leaders have quickly propelled the compact forward, said Lisa Robin, FSMB chief advocacy officer.
“I think the boards recognize the potential for telemedicine and what that can bring as far as access to health care,” Ms. Robin said. “As technologies are here – and it’s changing every day – this is a mechanism that will allow for much more efficiency and less administrative burden on the process for licensure for physicians who want to practice in multiple states.”
There have been several misconceptions tied to the compact law, Ms. Robin noted.
The compact does not change a state’s medical practice act, she stressed, nor does it create a national licensure system. In addition, the legislation does not require a physician to participate in maintenance of certification at any stage. Under the compact, approved physicians would be under the jurisdiction of the state medical board in which the patient is located at the time of the medical interaction. State boards of medicine would retain their individual authority for discipline and oversight.
The compact hopefully will reduce physicians’ frustrations and lessen administrative hassles for doctors who wish to use telehealth technologies to bring their expertise to patients across multiple states, said Dr. Reed V. Tuckson, president of the American Telemedicine Association.
“There have been several models proposed to address both of these objectives, and it appears that the Federation of State Medical Boards’ licensure model compact has emerged as the most practical and implementable of the various approaches,” Dr. Tuckson explained. “We do hope that this compact model can function efficiently and cost effectively, so that physicians are not overburdened as well-meaning organizations attempt to ensure that the public’s interests are safeguarded.”
Dr. Giarrizzi of Eagle Hospital Physicians is also optimistic about the compact.
“I am hoping this helps streamline the information,” she said. “I know it will still take time, because it is not taking away the need to go through the process, but seems more like it is just sharing the information. It will make it easier for us to cross state lines if the states we want to work in agree with this process and participate.”
On Twitter @legal_med
Telemedicine poses novel legal risks for doctors
Physicians who practice telemedicine have a lot to consider, including state laws, payment issues, and licensing regulations. But one overlooked area may pose the greatest risk of all: medical liability.
As the practice of telemedicine continues to grow, so do the legal risks associated with virtual care, said Dr. Joseph P. McMenamin, an emergency physician and health law defense attorney based in Richmond, Va.
“With good reason, there is a concern that as this form of care expands, claims against physicians will increase,” Dr. McMenamin said. “That’s almost inevitable, given how our society looks at litigation and how willing we are to sue our doctors. If you’re a plaintiffs’ attorney, you might be attracted to cases of this kind – partly because jurors may fear the unknown, and they may view [telemedicine] with some concern and suspicion.”
Telemedicine can fuel a wide spectrum of legal dangers, including malpractice, product liability claims, data exposure, and credentialing risks. Making matters more complicated: No uniform standard of care exists for telemedicine when it comes to medical malpractice, said René Y. Quashie, a Washington health law attorney who specializes in telemedicine and e-health practices.
“There are a lot of unanswered questions, including the prevailing standard of care,” Mr. Quashie explained. “Can we use the standard of care that we use for services provided in person for telehealth consults? Informed consent – does that process need to change? There are a lot of unanswered issues, which can only be resolved after a number of cases” are decided in the courts.
Physicians who practice telemedicine should consider legal risks associated with patient and staff privacy, inaccuracies in self-reporting, and symptoms that are more accurately diagnosed in person, said Richard F. Cahill, vice president and associate general counsel for the Doctors Company, a national medical liability insurer.
During 2007-2014, the Doctors Company had 11 claims that closed related to telemedicine, according to data provided by Mr. Cahill.
The majority of claims resulted from the remote reading of x-rays and other films by health providers, usually from home, and the remote reading of fetal monitor strips by physicians when outside of the hospital. Two of the cases were associated with attempts to diagnose a patient via telemedicine. Of the claims, six were diagnosis related, two alleged delay in treatment, two were related to improper performance of treatment, and one was associated with failure to order medication.
“The challenges of remote communications made it difficult to formulate the correct diagnosis due to limitations of radiology resolution, delayed readings of radiographs, or limits on fetal monitor strips,” said Darrell Ranum, vice president of patient safety and risk management for the Doctors Company. “Delays in treatment were closely related to delayed diagnosis. Radiologists did not receive a request for an interpretation, or they did not know that it was an emergency, so they did not provide a rapid turnaround report.”
While telemedicine claims have been low so far, a rise in the number of patient contacts, regardless of modality, may increase the risk of adverse consequences, Mr. Cahill cautioned.
“Because telemedicine is relatively new, and it takes 3-4 years for a claim to work its way through the system, we may see more cases in the future in which telemedicine is a factor,” he predicted.
Other lawsuits could arise from claims that physicians had access to telemedicine but failed to use the technology to properly treat a patient, Mr. Quashie said. Product liability claims also pose a threat, added Dr. McMenamin, who is part of the Legal Resource Team at the Robert J. Waters Center for Telehealth & e-Health Law (CTeL). Such accusations stem from equipment that malfunctioned or failed to work as indicated.
Varying credentialing rules also can trip up doctors who work virtually. Physicians at a large academic medical center, for example, could face trouble if they aren’t credentialed at the small rural hospital where a patient is located, Dr. McMenamin said. He noted that Medicare modified its telemedicine encounter rules several years ago, making it possible for rural hospitals to accept the credentialing process of the health center where the specialist is located. However, other criteria must be met for the telehealth encounter to occur.
Differing credentialing processes are challenging for doctors who practice telehealth, agreed telemedicine hospitalist Dr. Dana Giarrizzi of Eagle Hospital Physicians in Atlanta, which provides hospitalist services to hospitals and health systems nationwide via telehealth.
“The credentialing is certainly difficult at times,” Dr. Giarrizzi said. “It is a long process and sometimes requires fingerprints, taking exams, and other involved steps. It is very time consuming, and each state and certainly [each] facility can have different criteria, which makes it hard to know.”
To ensure its doctors are meeting the requirements of each facility, Eagle Hospital Physicians has its own credentialing department that works with hospitals to learn their processes and verify its physicians adhere to the rules, Dr. Giarrizzi said.
Preventing telemedicine lawsuits
To mitigate potential risks of telemedicine, doctors should clearly define protocols for use of webcams and Web-based portals and ensure such systems are secure, Mr. Cahill said. Take time to learn what constitutes the practice of medicine in each state in which doctors are delivering care, and carefully adhere to those rules, he added. Physicians also should have mechanisms in place to protect the privacy of individuals who do not want to be seen on camera, such as staff or family members.
It’s also critical to confer with malpractice insurance providers to confirm that telehealth services are covered, said Mr. Quashie, a member of the Legal Resource Team at CTeL. If telemedicine is not covered, physicians may want to buy a separate policy from another company that covers telehealth.
If physicians opt to work for a larger telemedicine company, they should check what controls the company has in place to protect them from lawsuits.
For example, national telemedicine company Teladoc has numerous safeguards in place to promote quality care and protect its doctors from claims, said Dr. Henry DePhillips, Teladoc’s chief medical officer. The company has National Committee for Quality Assurance certification, along with proprietary, evidence-based clinical practice guidelines for its physicians, a peer-review quality assurance committee, and regular data and medical reviews, Dr. DePhillips said. Teladoc is close to surpassing its 1-millionth consult and has not had a single claim filed in its history, he added.
Dr. DePhillips stressed that telemedicine is not a separate practice of medicine, and that best practices should remain the same, no matter the location.
“The bottom line is the standard of care for the diagnosis and treatment of these medical problems is the standard of care regardless whether you’re seeing the person in person, in an urgent care center, or through a secure video,” Dr. DePhillips said. “The doctor has to be able to comply with the standard of care and make a decision [about] whether that setting and that equipment at his or her disposal are adequate to make an accurate diagnosis and a medically appropriate treatment plan.”
On Twitter @legal_med
Physicians who practice telemedicine have a lot to consider, including state laws, payment issues, and licensing regulations. But one overlooked area may pose the greatest risk of all: medical liability.
As the practice of telemedicine continues to grow, so do the legal risks associated with virtual care, said Dr. Joseph P. McMenamin, an emergency physician and health law defense attorney based in Richmond, Va.
“With good reason, there is a concern that as this form of care expands, claims against physicians will increase,” Dr. McMenamin said. “That’s almost inevitable, given how our society looks at litigation and how willing we are to sue our doctors. If you’re a plaintiffs’ attorney, you might be attracted to cases of this kind – partly because jurors may fear the unknown, and they may view [telemedicine] with some concern and suspicion.”
Telemedicine can fuel a wide spectrum of legal dangers, including malpractice, product liability claims, data exposure, and credentialing risks. Making matters more complicated: No uniform standard of care exists for telemedicine when it comes to medical malpractice, said René Y. Quashie, a Washington health law attorney who specializes in telemedicine and e-health practices.
“There are a lot of unanswered questions, including the prevailing standard of care,” Mr. Quashie explained. “Can we use the standard of care that we use for services provided in person for telehealth consults? Informed consent – does that process need to change? There are a lot of unanswered issues, which can only be resolved after a number of cases” are decided in the courts.
Physicians who practice telemedicine should consider legal risks associated with patient and staff privacy, inaccuracies in self-reporting, and symptoms that are more accurately diagnosed in person, said Richard F. Cahill, vice president and associate general counsel for the Doctors Company, a national medical liability insurer.
During 2007-2014, the Doctors Company had 11 claims that closed related to telemedicine, according to data provided by Mr. Cahill.
The majority of claims resulted from the remote reading of x-rays and other films by health providers, usually from home, and the remote reading of fetal monitor strips by physicians when outside of the hospital. Two of the cases were associated with attempts to diagnose a patient via telemedicine. Of the claims, six were diagnosis related, two alleged delay in treatment, two were related to improper performance of treatment, and one was associated with failure to order medication.
“The challenges of remote communications made it difficult to formulate the correct diagnosis due to limitations of radiology resolution, delayed readings of radiographs, or limits on fetal monitor strips,” said Darrell Ranum, vice president of patient safety and risk management for the Doctors Company. “Delays in treatment were closely related to delayed diagnosis. Radiologists did not receive a request for an interpretation, or they did not know that it was an emergency, so they did not provide a rapid turnaround report.”
While telemedicine claims have been low so far, a rise in the number of patient contacts, regardless of modality, may increase the risk of adverse consequences, Mr. Cahill cautioned.
“Because telemedicine is relatively new, and it takes 3-4 years for a claim to work its way through the system, we may see more cases in the future in which telemedicine is a factor,” he predicted.
Other lawsuits could arise from claims that physicians had access to telemedicine but failed to use the technology to properly treat a patient, Mr. Quashie said. Product liability claims also pose a threat, added Dr. McMenamin, who is part of the Legal Resource Team at the Robert J. Waters Center for Telehealth & e-Health Law (CTeL). Such accusations stem from equipment that malfunctioned or failed to work as indicated.
Varying credentialing rules also can trip up doctors who work virtually. Physicians at a large academic medical center, for example, could face trouble if they aren’t credentialed at the small rural hospital where a patient is located, Dr. McMenamin said. He noted that Medicare modified its telemedicine encounter rules several years ago, making it possible for rural hospitals to accept the credentialing process of the health center where the specialist is located. However, other criteria must be met for the telehealth encounter to occur.
Differing credentialing processes are challenging for doctors who practice telehealth, agreed telemedicine hospitalist Dr. Dana Giarrizzi of Eagle Hospital Physicians in Atlanta, which provides hospitalist services to hospitals and health systems nationwide via telehealth.
“The credentialing is certainly difficult at times,” Dr. Giarrizzi said. “It is a long process and sometimes requires fingerprints, taking exams, and other involved steps. It is very time consuming, and each state and certainly [each] facility can have different criteria, which makes it hard to know.”
To ensure its doctors are meeting the requirements of each facility, Eagle Hospital Physicians has its own credentialing department that works with hospitals to learn their processes and verify its physicians adhere to the rules, Dr. Giarrizzi said.
Preventing telemedicine lawsuits
To mitigate potential risks of telemedicine, doctors should clearly define protocols for use of webcams and Web-based portals and ensure such systems are secure, Mr. Cahill said. Take time to learn what constitutes the practice of medicine in each state in which doctors are delivering care, and carefully adhere to those rules, he added. Physicians also should have mechanisms in place to protect the privacy of individuals who do not want to be seen on camera, such as staff or family members.
It’s also critical to confer with malpractice insurance providers to confirm that telehealth services are covered, said Mr. Quashie, a member of the Legal Resource Team at CTeL. If telemedicine is not covered, physicians may want to buy a separate policy from another company that covers telehealth.
If physicians opt to work for a larger telemedicine company, they should check what controls the company has in place to protect them from lawsuits.
For example, national telemedicine company Teladoc has numerous safeguards in place to promote quality care and protect its doctors from claims, said Dr. Henry DePhillips, Teladoc’s chief medical officer. The company has National Committee for Quality Assurance certification, along with proprietary, evidence-based clinical practice guidelines for its physicians, a peer-review quality assurance committee, and regular data and medical reviews, Dr. DePhillips said. Teladoc is close to surpassing its 1-millionth consult and has not had a single claim filed in its history, he added.
Dr. DePhillips stressed that telemedicine is not a separate practice of medicine, and that best practices should remain the same, no matter the location.
“The bottom line is the standard of care for the diagnosis and treatment of these medical problems is the standard of care regardless whether you’re seeing the person in person, in an urgent care center, or through a secure video,” Dr. DePhillips said. “The doctor has to be able to comply with the standard of care and make a decision [about] whether that setting and that equipment at his or her disposal are adequate to make an accurate diagnosis and a medically appropriate treatment plan.”
On Twitter @legal_med
Physicians who practice telemedicine have a lot to consider, including state laws, payment issues, and licensing regulations. But one overlooked area may pose the greatest risk of all: medical liability.
As the practice of telemedicine continues to grow, so do the legal risks associated with virtual care, said Dr. Joseph P. McMenamin, an emergency physician and health law defense attorney based in Richmond, Va.
“With good reason, there is a concern that as this form of care expands, claims against physicians will increase,” Dr. McMenamin said. “That’s almost inevitable, given how our society looks at litigation and how willing we are to sue our doctors. If you’re a plaintiffs’ attorney, you might be attracted to cases of this kind – partly because jurors may fear the unknown, and they may view [telemedicine] with some concern and suspicion.”
Telemedicine can fuel a wide spectrum of legal dangers, including malpractice, product liability claims, data exposure, and credentialing risks. Making matters more complicated: No uniform standard of care exists for telemedicine when it comes to medical malpractice, said René Y. Quashie, a Washington health law attorney who specializes in telemedicine and e-health practices.
“There are a lot of unanswered questions, including the prevailing standard of care,” Mr. Quashie explained. “Can we use the standard of care that we use for services provided in person for telehealth consults? Informed consent – does that process need to change? There are a lot of unanswered issues, which can only be resolved after a number of cases” are decided in the courts.
Physicians who practice telemedicine should consider legal risks associated with patient and staff privacy, inaccuracies in self-reporting, and symptoms that are more accurately diagnosed in person, said Richard F. Cahill, vice president and associate general counsel for the Doctors Company, a national medical liability insurer.
During 2007-2014, the Doctors Company had 11 claims that closed related to telemedicine, according to data provided by Mr. Cahill.
The majority of claims resulted from the remote reading of x-rays and other films by health providers, usually from home, and the remote reading of fetal monitor strips by physicians when outside of the hospital. Two of the cases were associated with attempts to diagnose a patient via telemedicine. Of the claims, six were diagnosis related, two alleged delay in treatment, two were related to improper performance of treatment, and one was associated with failure to order medication.
“The challenges of remote communications made it difficult to formulate the correct diagnosis due to limitations of radiology resolution, delayed readings of radiographs, or limits on fetal monitor strips,” said Darrell Ranum, vice president of patient safety and risk management for the Doctors Company. “Delays in treatment were closely related to delayed diagnosis. Radiologists did not receive a request for an interpretation, or they did not know that it was an emergency, so they did not provide a rapid turnaround report.”
While telemedicine claims have been low so far, a rise in the number of patient contacts, regardless of modality, may increase the risk of adverse consequences, Mr. Cahill cautioned.
“Because telemedicine is relatively new, and it takes 3-4 years for a claim to work its way through the system, we may see more cases in the future in which telemedicine is a factor,” he predicted.
Other lawsuits could arise from claims that physicians had access to telemedicine but failed to use the technology to properly treat a patient, Mr. Quashie said. Product liability claims also pose a threat, added Dr. McMenamin, who is part of the Legal Resource Team at the Robert J. Waters Center for Telehealth & e-Health Law (CTeL). Such accusations stem from equipment that malfunctioned or failed to work as indicated.
Varying credentialing rules also can trip up doctors who work virtually. Physicians at a large academic medical center, for example, could face trouble if they aren’t credentialed at the small rural hospital where a patient is located, Dr. McMenamin said. He noted that Medicare modified its telemedicine encounter rules several years ago, making it possible for rural hospitals to accept the credentialing process of the health center where the specialist is located. However, other criteria must be met for the telehealth encounter to occur.
Differing credentialing processes are challenging for doctors who practice telehealth, agreed telemedicine hospitalist Dr. Dana Giarrizzi of Eagle Hospital Physicians in Atlanta, which provides hospitalist services to hospitals and health systems nationwide via telehealth.
“The credentialing is certainly difficult at times,” Dr. Giarrizzi said. “It is a long process and sometimes requires fingerprints, taking exams, and other involved steps. It is very time consuming, and each state and certainly [each] facility can have different criteria, which makes it hard to know.”
To ensure its doctors are meeting the requirements of each facility, Eagle Hospital Physicians has its own credentialing department that works with hospitals to learn their processes and verify its physicians adhere to the rules, Dr. Giarrizzi said.
Preventing telemedicine lawsuits
To mitigate potential risks of telemedicine, doctors should clearly define protocols for use of webcams and Web-based portals and ensure such systems are secure, Mr. Cahill said. Take time to learn what constitutes the practice of medicine in each state in which doctors are delivering care, and carefully adhere to those rules, he added. Physicians also should have mechanisms in place to protect the privacy of individuals who do not want to be seen on camera, such as staff or family members.
It’s also critical to confer with malpractice insurance providers to confirm that telehealth services are covered, said Mr. Quashie, a member of the Legal Resource Team at CTeL. If telemedicine is not covered, physicians may want to buy a separate policy from another company that covers telehealth.
If physicians opt to work for a larger telemedicine company, they should check what controls the company has in place to protect them from lawsuits.
For example, national telemedicine company Teladoc has numerous safeguards in place to promote quality care and protect its doctors from claims, said Dr. Henry DePhillips, Teladoc’s chief medical officer. The company has National Committee for Quality Assurance certification, along with proprietary, evidence-based clinical practice guidelines for its physicians, a peer-review quality assurance committee, and regular data and medical reviews, Dr. DePhillips said. Teladoc is close to surpassing its 1-millionth consult and has not had a single claim filed in its history, he added.
Dr. DePhillips stressed that telemedicine is not a separate practice of medicine, and that best practices should remain the same, no matter the location.
“The bottom line is the standard of care for the diagnosis and treatment of these medical problems is the standard of care regardless whether you’re seeing the person in person, in an urgent care center, or through a secure video,” Dr. DePhillips said. “The doctor has to be able to comply with the standard of care and make a decision [about] whether that setting and that equipment at his or her disposal are adequate to make an accurate diagnosis and a medically appropriate treatment plan.”
On Twitter @legal_med
California governor signs physician-assisted suicide bill into law
California Gov. Jerry Brown (D) has signed into law a controversial measure that allows physicians to help terminally ill patients legally end their lives, making California the fourth state to permit doctor-assisted suicide through its legislature.
Gov. Brown, a former seminary student, approved the End of Life Option Act Oct. 5, after state lawmakers passed the bill Sept. 11.
In a signing message, Gov. Brown said that he had considered all sides of the issue and carefully weighed religious and theological perspectives that shortening a patient’s life is sinful.
“In the end, I was left to reflect on what I would want in the face of my own death,” Gov. Brown said in the message. “I do not know what I would do if I were dying in prolonged and excruciating pain. I am certain, however, that it would be a comfort to be able to consider the options afforded by this bill. And I wouldn’t deny that right to others.”
Modeled after Oregon’s statute, California’s law requires two doctors to determine that a patient has 6 months or less to live before doctors could prescribe life-ending medication. Patients must have the mental capacity to make medical decisions and would physically have to be able to swallow the drugs.
In addition, patients seeking physician aid in dying must submit two oral requests, a minimum of 15 days apart, and a written request to their physician. The attending physician must receive all three requests directly from the patient and not through a designee. Before prescribing end-of-life drugs, the attending physician must refer the patient to a consulting physician for confirmation of the diagnosis and prognosis and of the patient’s capacity to make the decision.
Oregon, Vermont, and Washington each have laws permitting physician-assisted death. Court rulings in New Mexico and Montana have allowed for the practice, but litigation in those states is ongoing and the decisions have yet to be enforced.
The signing ends nearly a year of passionate debate in California that divided physicians, religious groups, lawmakers, and community members. In May, the California Medical Association (CMA) became the first state medical society to change its stance against physician-assisted suicide to that of being neutral.
“The decision to participate in the End of Life Option Act is a very personal one between a doctor and their patient, which is why CMA has removed policy that outright objects to physicians aiding terminally ill patients in end of life options,” Dr. Luther F. Cobb, CMA president, said in a statement. “We believe it is up to the individual physician and their patient to decide voluntarily whether the End of Life Option Act is something in which they want to engage. Protecting that physician-patient relationship is essential.”
The California law will take effect 90 days after the state legislature adjourns its special session on health care, which may not be until early next year. The earliest likely enactment would be spring 2016.
On Twitter @legal_med
California Gov. Jerry Brown (D) has signed into law a controversial measure that allows physicians to help terminally ill patients legally end their lives, making California the fourth state to permit doctor-assisted suicide through its legislature.
Gov. Brown, a former seminary student, approved the End of Life Option Act Oct. 5, after state lawmakers passed the bill Sept. 11.
In a signing message, Gov. Brown said that he had considered all sides of the issue and carefully weighed religious and theological perspectives that shortening a patient’s life is sinful.
“In the end, I was left to reflect on what I would want in the face of my own death,” Gov. Brown said in the message. “I do not know what I would do if I were dying in prolonged and excruciating pain. I am certain, however, that it would be a comfort to be able to consider the options afforded by this bill. And I wouldn’t deny that right to others.”
Modeled after Oregon’s statute, California’s law requires two doctors to determine that a patient has 6 months or less to live before doctors could prescribe life-ending medication. Patients must have the mental capacity to make medical decisions and would physically have to be able to swallow the drugs.
In addition, patients seeking physician aid in dying must submit two oral requests, a minimum of 15 days apart, and a written request to their physician. The attending physician must receive all three requests directly from the patient and not through a designee. Before prescribing end-of-life drugs, the attending physician must refer the patient to a consulting physician for confirmation of the diagnosis and prognosis and of the patient’s capacity to make the decision.
Oregon, Vermont, and Washington each have laws permitting physician-assisted death. Court rulings in New Mexico and Montana have allowed for the practice, but litigation in those states is ongoing and the decisions have yet to be enforced.
The signing ends nearly a year of passionate debate in California that divided physicians, religious groups, lawmakers, and community members. In May, the California Medical Association (CMA) became the first state medical society to change its stance against physician-assisted suicide to that of being neutral.
“The decision to participate in the End of Life Option Act is a very personal one between a doctor and their patient, which is why CMA has removed policy that outright objects to physicians aiding terminally ill patients in end of life options,” Dr. Luther F. Cobb, CMA president, said in a statement. “We believe it is up to the individual physician and their patient to decide voluntarily whether the End of Life Option Act is something in which they want to engage. Protecting that physician-patient relationship is essential.”
The California law will take effect 90 days after the state legislature adjourns its special session on health care, which may not be until early next year. The earliest likely enactment would be spring 2016.
On Twitter @legal_med
California Gov. Jerry Brown (D) has signed into law a controversial measure that allows physicians to help terminally ill patients legally end their lives, making California the fourth state to permit doctor-assisted suicide through its legislature.
Gov. Brown, a former seminary student, approved the End of Life Option Act Oct. 5, after state lawmakers passed the bill Sept. 11.
In a signing message, Gov. Brown said that he had considered all sides of the issue and carefully weighed religious and theological perspectives that shortening a patient’s life is sinful.
“In the end, I was left to reflect on what I would want in the face of my own death,” Gov. Brown said in the message. “I do not know what I would do if I were dying in prolonged and excruciating pain. I am certain, however, that it would be a comfort to be able to consider the options afforded by this bill. And I wouldn’t deny that right to others.”
Modeled after Oregon’s statute, California’s law requires two doctors to determine that a patient has 6 months or less to live before doctors could prescribe life-ending medication. Patients must have the mental capacity to make medical decisions and would physically have to be able to swallow the drugs.
In addition, patients seeking physician aid in dying must submit two oral requests, a minimum of 15 days apart, and a written request to their physician. The attending physician must receive all three requests directly from the patient and not through a designee. Before prescribing end-of-life drugs, the attending physician must refer the patient to a consulting physician for confirmation of the diagnosis and prognosis and of the patient’s capacity to make the decision.
Oregon, Vermont, and Washington each have laws permitting physician-assisted death. Court rulings in New Mexico and Montana have allowed for the practice, but litigation in those states is ongoing and the decisions have yet to be enforced.
The signing ends nearly a year of passionate debate in California that divided physicians, religious groups, lawmakers, and community members. In May, the California Medical Association (CMA) became the first state medical society to change its stance against physician-assisted suicide to that of being neutral.
“The decision to participate in the End of Life Option Act is a very personal one between a doctor and their patient, which is why CMA has removed policy that outright objects to physicians aiding terminally ill patients in end of life options,” Dr. Luther F. Cobb, CMA president, said in a statement. “We believe it is up to the individual physician and their patient to decide voluntarily whether the End of Life Option Act is something in which they want to engage. Protecting that physician-patient relationship is essential.”
The California law will take effect 90 days after the state legislature adjourns its special session on health care, which may not be until early next year. The earliest likely enactment would be spring 2016.
On Twitter @legal_med
Charging patients for electronic health records: advice for providers
There’s little question that patients should have access to their electronic health records, but what should health care providers charge for copies of the electronic documents? A draft of proposals by the Office of the National Coordinator (ONC) for Health Information Technology aims to help providers determine how to calculate these costs.
Electronic file size was a top issue addressed by the ONC at two recent privacy and security workgroup meetings. The group recommended that electronic file size not be used as a proxy for “pages” in setting patient fees for electronic access. Labor, media, and search and retrieval efforts are more appropriate considerations when calculating costs, said Stanley W. Crosley, chair for ONC’s privacy and security workgroup and a Washington data privacy and health information attorney.
“The answers were pretty clear across the board that it really wasn’t a very good proxy,” Mr. Crosley said during a Sept. 28 workgroup meeting. “Really it’s more about labor charge and media charge.”
ONC’s privacy and security workgroup discussed cost considerations for electronic protected health information (PHI) during a Sept. 21 meeting and proposed suggested guidance to the Office for Civil Rights (OCR) at a follow-up meeting on Sept. 28. The workgroup’s recommendations stem from a request by the Obama administration that the U.S. Department of Health & Human Services and ONC collaborate to address barriers that prevent patients from accessing PHI. The president’s Precision Medicine Initiative calls for the OCR to develop additional guidance for health care providers and the public about accessing electronic health information under HIPAA.
Few states have addressed how physicians and other health providers should charge for EHR requests, and requirements differ widely in states that do regulate the activity, Mr. Crosley said during the meeting. Illinois, for example, allows doctors and hospitals to charge 50% of the paper-based per-page fee for electronic records retrieved from scanning, digital imaging, electronic information, or another digital format. Ohio does not distinguish between paper and electronic records and allows providers to charge the same per-page fee for both. Most states base fees for paper records on pages, with some states setting limits on maximum copying costs.
Developing cost guidelines around electronic PHI is more complex than meets the eye, ONC members noted at the Sept. 28 meeting. Questions include how producible format should affect fees, whether the cost of electronic data should be comparable to paper copies, and to what extent labor should be factored into cost. Making matters more complicated are recent federal regulations under the Health Information Technology for Economic and Clinical Health (HITECH) Act that mandate what costs can and cannot not include. The 2013 Omnibus Rule, which made amendments to HIPAA as required by the HITECH Act, gives patients the right to obtain health information copies in the form and format they wish, as long as that form is “readily producible” by the covered entity. Fees cannot include costs associated with searching for or retrieving the requested information, but may include labor charges such as time spent to create and copy the electronic file or the compiling, extracting, scanning, and burning health information to media.
“The interaction of these two points creates some issues for covered entities as well as for the charges being offered,” Mr. Crosley said.
As part of its recommendations, ONC suggests that OCR define search and retrieval and distinguish between search and retrieval costs versus copying and duplication costs. In future guidance, OCR should also provide more precision around calculation of labor, media, and search and retrieval costs as well as provide examples of hypothetical scenarios for clarity, the workgroup proposes. In addition, ONC would like OCR to clarify how to handle more restrictive privacy state laws if patients want a doctor to send a record to a third party. As part of the 2013 Omnibus rule, patients can direct a covered entity to transmit a record directly to an individual’s designee or third party.
The ONC workgroup based its recommendations on a survey of questions provided to a group of health providers, EHR vendors, and patients about cost for electronic PHI. The Sept. 28 suggestions are not formal recommendations, but will be used by ONC as a basis to develop final consideration points for the OCR.
On Twitter@legal_med
There’s little question that patients should have access to their electronic health records, but what should health care providers charge for copies of the electronic documents? A draft of proposals by the Office of the National Coordinator (ONC) for Health Information Technology aims to help providers determine how to calculate these costs.
Electronic file size was a top issue addressed by the ONC at two recent privacy and security workgroup meetings. The group recommended that electronic file size not be used as a proxy for “pages” in setting patient fees for electronic access. Labor, media, and search and retrieval efforts are more appropriate considerations when calculating costs, said Stanley W. Crosley, chair for ONC’s privacy and security workgroup and a Washington data privacy and health information attorney.
“The answers were pretty clear across the board that it really wasn’t a very good proxy,” Mr. Crosley said during a Sept. 28 workgroup meeting. “Really it’s more about labor charge and media charge.”
ONC’s privacy and security workgroup discussed cost considerations for electronic protected health information (PHI) during a Sept. 21 meeting and proposed suggested guidance to the Office for Civil Rights (OCR) at a follow-up meeting on Sept. 28. The workgroup’s recommendations stem from a request by the Obama administration that the U.S. Department of Health & Human Services and ONC collaborate to address barriers that prevent patients from accessing PHI. The president’s Precision Medicine Initiative calls for the OCR to develop additional guidance for health care providers and the public about accessing electronic health information under HIPAA.
Few states have addressed how physicians and other health providers should charge for EHR requests, and requirements differ widely in states that do regulate the activity, Mr. Crosley said during the meeting. Illinois, for example, allows doctors and hospitals to charge 50% of the paper-based per-page fee for electronic records retrieved from scanning, digital imaging, electronic information, or another digital format. Ohio does not distinguish between paper and electronic records and allows providers to charge the same per-page fee for both. Most states base fees for paper records on pages, with some states setting limits on maximum copying costs.
Developing cost guidelines around electronic PHI is more complex than meets the eye, ONC members noted at the Sept. 28 meeting. Questions include how producible format should affect fees, whether the cost of electronic data should be comparable to paper copies, and to what extent labor should be factored into cost. Making matters more complicated are recent federal regulations under the Health Information Technology for Economic and Clinical Health (HITECH) Act that mandate what costs can and cannot not include. The 2013 Omnibus Rule, which made amendments to HIPAA as required by the HITECH Act, gives patients the right to obtain health information copies in the form and format they wish, as long as that form is “readily producible” by the covered entity. Fees cannot include costs associated with searching for or retrieving the requested information, but may include labor charges such as time spent to create and copy the electronic file or the compiling, extracting, scanning, and burning health information to media.
“The interaction of these two points creates some issues for covered entities as well as for the charges being offered,” Mr. Crosley said.
As part of its recommendations, ONC suggests that OCR define search and retrieval and distinguish between search and retrieval costs versus copying and duplication costs. In future guidance, OCR should also provide more precision around calculation of labor, media, and search and retrieval costs as well as provide examples of hypothetical scenarios for clarity, the workgroup proposes. In addition, ONC would like OCR to clarify how to handle more restrictive privacy state laws if patients want a doctor to send a record to a third party. As part of the 2013 Omnibus rule, patients can direct a covered entity to transmit a record directly to an individual’s designee or third party.
The ONC workgroup based its recommendations on a survey of questions provided to a group of health providers, EHR vendors, and patients about cost for electronic PHI. The Sept. 28 suggestions are not formal recommendations, but will be used by ONC as a basis to develop final consideration points for the OCR.
On Twitter@legal_med
There’s little question that patients should have access to their electronic health records, but what should health care providers charge for copies of the electronic documents? A draft of proposals by the Office of the National Coordinator (ONC) for Health Information Technology aims to help providers determine how to calculate these costs.
Electronic file size was a top issue addressed by the ONC at two recent privacy and security workgroup meetings. The group recommended that electronic file size not be used as a proxy for “pages” in setting patient fees for electronic access. Labor, media, and search and retrieval efforts are more appropriate considerations when calculating costs, said Stanley W. Crosley, chair for ONC’s privacy and security workgroup and a Washington data privacy and health information attorney.
“The answers were pretty clear across the board that it really wasn’t a very good proxy,” Mr. Crosley said during a Sept. 28 workgroup meeting. “Really it’s more about labor charge and media charge.”
ONC’s privacy and security workgroup discussed cost considerations for electronic protected health information (PHI) during a Sept. 21 meeting and proposed suggested guidance to the Office for Civil Rights (OCR) at a follow-up meeting on Sept. 28. The workgroup’s recommendations stem from a request by the Obama administration that the U.S. Department of Health & Human Services and ONC collaborate to address barriers that prevent patients from accessing PHI. The president’s Precision Medicine Initiative calls for the OCR to develop additional guidance for health care providers and the public about accessing electronic health information under HIPAA.
Few states have addressed how physicians and other health providers should charge for EHR requests, and requirements differ widely in states that do regulate the activity, Mr. Crosley said during the meeting. Illinois, for example, allows doctors and hospitals to charge 50% of the paper-based per-page fee for electronic records retrieved from scanning, digital imaging, electronic information, or another digital format. Ohio does not distinguish between paper and electronic records and allows providers to charge the same per-page fee for both. Most states base fees for paper records on pages, with some states setting limits on maximum copying costs.
Developing cost guidelines around electronic PHI is more complex than meets the eye, ONC members noted at the Sept. 28 meeting. Questions include how producible format should affect fees, whether the cost of electronic data should be comparable to paper copies, and to what extent labor should be factored into cost. Making matters more complicated are recent federal regulations under the Health Information Technology for Economic and Clinical Health (HITECH) Act that mandate what costs can and cannot not include. The 2013 Omnibus Rule, which made amendments to HIPAA as required by the HITECH Act, gives patients the right to obtain health information copies in the form and format they wish, as long as that form is “readily producible” by the covered entity. Fees cannot include costs associated with searching for or retrieving the requested information, but may include labor charges such as time spent to create and copy the electronic file or the compiling, extracting, scanning, and burning health information to media.
“The interaction of these two points creates some issues for covered entities as well as for the charges being offered,” Mr. Crosley said.
As part of its recommendations, ONC suggests that OCR define search and retrieval and distinguish between search and retrieval costs versus copying and duplication costs. In future guidance, OCR should also provide more precision around calculation of labor, media, and search and retrieval costs as well as provide examples of hypothetical scenarios for clarity, the workgroup proposes. In addition, ONC would like OCR to clarify how to handle more restrictive privacy state laws if patients want a doctor to send a record to a third party. As part of the 2013 Omnibus rule, patients can direct a covered entity to transmit a record directly to an individual’s designee or third party.
The ONC workgroup based its recommendations on a survey of questions provided to a group of health providers, EHR vendors, and patients about cost for electronic PHI. The Sept. 28 suggestions are not formal recommendations, but will be used by ONC as a basis to develop final consideration points for the OCR.
On Twitter@legal_med
Physicians face telemedicine payment challenges
Emergency department personnel at a remote hospital called Dr. James P. Marcin regarding a baby who was just admitted with an upper respiratory infection. Because the patient had cyanotic congenital heart disease, the team was concerned she was too medically complex for their facility, and they were preparing to helicopter her to the pediatric intensive care unit at the University of California, Davis, Children’s Hospital in Sacramento.
But when Dr. Marcin examined the baby via a two-way video, he remembered the child from a previous visit. Although her oxygen levels were low, Dr. Marcin knew they were normal for her condition. Dr. Marcin spoke with the patient’s parents and after learning more about the patient’s symptoms, he was confident the child could remain at the small hospital. She was treated for the upper respiratory infection and later sent home where she improved, said Dr. Marcin, who leads the Pediatric Telemedicine Program at UC Davis.
Despite the positive outcome, Dr. Marcin’s claim was denied by the insurance company, he said.
“Had I not used telemedicine, that child would have been put in a helicopter, flown to our ICU, [and likely incurred] some $20,000 bill,” Dr. Marcin said in an interview. “I saved the insurance company $20,000, and then they ended up denying my 2 hours of critical care time. It’s discouraging.”
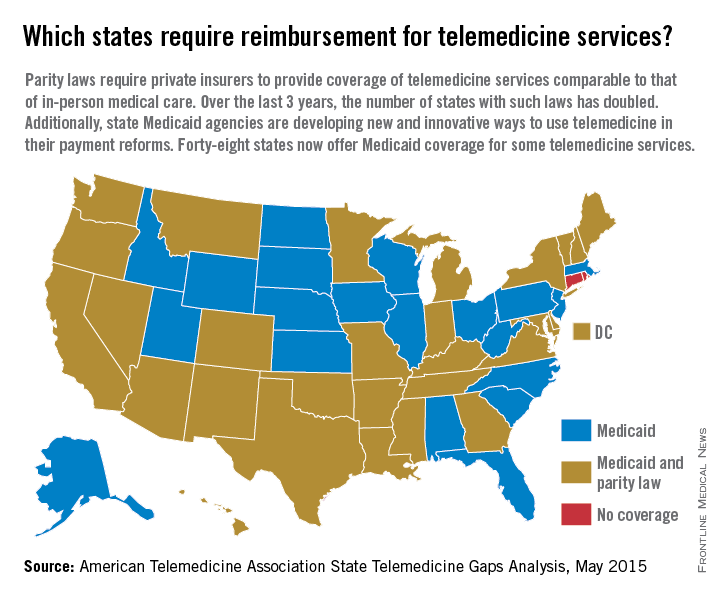
Reimbursement struggles are playing out in medical practices and hospitals across the country. While insurance coverage for telemedicine is growing, experts say payment remains one of the most pressing challenges. So far, 29 states and the District of Columbia have laws that require full parity of coverage and reimbursement for telemedicine services comparable to that of in-person services, according to the American Telemedicine Association (ATA). Medicaid programs in almost all (48) states require some form of compensation for telemedicine, according to a 2015 ATA report.
Payment parity for telemedicine has doubled in the last 2 years, noted Dr. Reed V. Tuckson, ATA president.
“We are seeing, on the side of the private insurance world, really exciting acceptance of telehealth services,” Dr. Tuckson said in an interview. There has been “really great movement forward.”
Enforcement of those parity laws can be spotty, said René Y. Quashie, a Washington health law attorney.
“It’s a mixed bag,” Mr. Quashie said in an interview. “In some states, enforcement is lax so you still have a lot of providers submitting claims that are not being paid or not being paid timely.”
State support equals payment success
In rural Wrightsville, Ga., Dr. Jean R. Sumner regularly gets paid to provide telemedicine. Georgia enacted its parity law in 2006 and has greatly embraced telemedicine capabilities, particularly for its rural populations, said Dr. Sumner, associate dean for rural health at Mercer University in Macon. Part of the success is because of the Georgia Partnership for TeleHealth, a statewide network that focuses on increasing access to care through telemedicine. Its hallmark is the state’s open access network, a web of access points based on existing telemedicine programs that enables secure health information exchange. The goal of the program is for all rural Georgians to access specialty care within 30 miles of their homes.
The state’s strong support of telemedicine contributes to payers taking the modality seriously and doctors getting paid for telemedicine care, Dr. Sumner said in an interview.
“Most insurers pay as long as the visit is equal or superior to an exam done in person,” she said. “It has to be quality care.”
Dr. Sumner also can bill a site fee when telemedicine technology is used at her practice, she said. If a patient visits her practice for a psychiatric consultation while Dr. Sumner is busy, for example, a nurse can connect the patient to a psychiatrist through the office’s telemedicine unit. The site fee is minimal, but it helps cover costs, she said.
In states that do not have parity laws, some larger health plans, such as Anthem and UnitedHealthcare, have proactively covered telemedicine services, said Dr. Peter Antall, president and medical director of American Well’s Online Care Group, a national telehealth service. Smaller health plans on the other hand, are sometimes willing to negotiate with providers and consider adding telemedicine services to a fee schedule, Dr. Antall said in an interview.
“I think we’re moving into a phase where reimbursement is normal or expected in telehealth,” he said. “We’re not quite there yet because there are so many health plans and, within the health plans, there are so many different products and subgroups. It’s still a process that needs to evolve.”
Government payers lag behind
Medicaid policies also vary from state by state. Some state programs cover telemedicine services similar to that of in-person treatment. Others limit coverage by technology or geographic area.
Medicare, by far, ranks the worst in paying physicians for telemedicine, experts said. Of $597 billion in total Medicare payments in 2014, 0.0023% was spent on telemedicine, according to data provided to the Robert J. Waters Center for Telehealth & e-Health Law.
“Unless you’re a patient that presents in a rural community, the Medicare telehealth benefit is not available,” said Mr. Quashie, who is part of the CTeL’s legal resource team. “Medicare is almost a no-go under fee-for-service for telehealth.”
CMS reimburses physicians for telemedicine only when the originating site is in a Health Professional Shortage Area or within a county outside a Metropolitan Statistical Area. The originating site must be a medical facility and not the patient’s home. CMS covers care only on an approved list of medical services.
In its 2016 proposed fee schedule, CMS recommended adding two new codes to its accepted telemedicine services, including codes for prolonged service inpatient care and end-stage renal disease–related services. However, the agency denied a handful of other services requested by the ATA and again, refused to end its patient site limitations.
“We are very concerned about Medicare’s decisions in terms of its ability and willingness to reimburse” telehealth services,” Dr. Tuckson said. “Physicians who are trying to care for our nation’s seniors – so many of whom are presenting real challenges in manging their care in an optimal way – those physicians and patients deserve the opportunity to use [telehealth] tools, and physicians deserve to be reimbursed for the appropriate use of those tools.”
Federal legislation to expand Medicare coverage for telehealth has previously failed. Most recently, Rep. Mike Thompson (D-Calif.) proposed H.R. 2948, the Medicare Telehealth Parity Act of 2015, a bill that would broaden Medicare telemedicine coverage to urban areas and cover more services. The bill has been referred to the House Ways and Means Committee’s Subcommittee on Health.
Coverage of telemedicine by all payers is especially necessary as the health care system shifts to a more value-based care structure, Dr. Marcin said. Telemedicine presents great opportunities for preventing illnesses, keeping patients out of the hospital, and lowering health costs, he said. However, financial incentives to utilize telemedicine in these ways is lacking.
“Even though these technologies have been proven to reduce overall health care costs, they result in lower payments to doctors and hospitals,” Dr. Marcin said. “There’s a malalignment with payments to both hospitals and doctors and what should be the goals of health care, which is to keep patients healthy.”
Coming Tuesday, Oct. 6: Can telemedicine expose you to legal risk?
On Twitter @legal_med
Emergency department personnel at a remote hospital called Dr. James P. Marcin regarding a baby who was just admitted with an upper respiratory infection. Because the patient had cyanotic congenital heart disease, the team was concerned she was too medically complex for their facility, and they were preparing to helicopter her to the pediatric intensive care unit at the University of California, Davis, Children’s Hospital in Sacramento.
But when Dr. Marcin examined the baby via a two-way video, he remembered the child from a previous visit. Although her oxygen levels were low, Dr. Marcin knew they were normal for her condition. Dr. Marcin spoke with the patient’s parents and after learning more about the patient’s symptoms, he was confident the child could remain at the small hospital. She was treated for the upper respiratory infection and later sent home where she improved, said Dr. Marcin, who leads the Pediatric Telemedicine Program at UC Davis.
Despite the positive outcome, Dr. Marcin’s claim was denied by the insurance company, he said.
“Had I not used telemedicine, that child would have been put in a helicopter, flown to our ICU, [and likely incurred] some $20,000 bill,” Dr. Marcin said in an interview. “I saved the insurance company $20,000, and then they ended up denying my 2 hours of critical care time. It’s discouraging.”
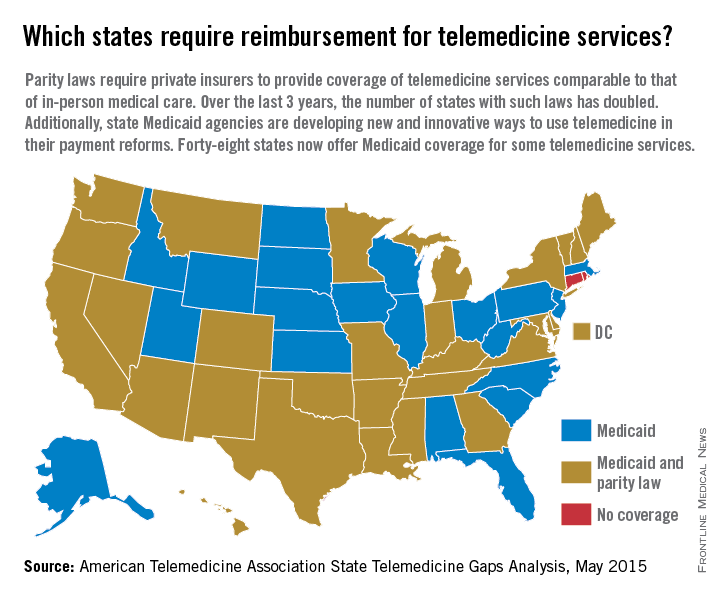
Reimbursement struggles are playing out in medical practices and hospitals across the country. While insurance coverage for telemedicine is growing, experts say payment remains one of the most pressing challenges. So far, 29 states and the District of Columbia have laws that require full parity of coverage and reimbursement for telemedicine services comparable to that of in-person services, according to the American Telemedicine Association (ATA). Medicaid programs in almost all (48) states require some form of compensation for telemedicine, according to a 2015 ATA report.
Payment parity for telemedicine has doubled in the last 2 years, noted Dr. Reed V. Tuckson, ATA president.
“We are seeing, on the side of the private insurance world, really exciting acceptance of telehealth services,” Dr. Tuckson said in an interview. There has been “really great movement forward.”
Enforcement of those parity laws can be spotty, said René Y. Quashie, a Washington health law attorney.
“It’s a mixed bag,” Mr. Quashie said in an interview. “In some states, enforcement is lax so you still have a lot of providers submitting claims that are not being paid or not being paid timely.”
State support equals payment success
In rural Wrightsville, Ga., Dr. Jean R. Sumner regularly gets paid to provide telemedicine. Georgia enacted its parity law in 2006 and has greatly embraced telemedicine capabilities, particularly for its rural populations, said Dr. Sumner, associate dean for rural health at Mercer University in Macon. Part of the success is because of the Georgia Partnership for TeleHealth, a statewide network that focuses on increasing access to care through telemedicine. Its hallmark is the state’s open access network, a web of access points based on existing telemedicine programs that enables secure health information exchange. The goal of the program is for all rural Georgians to access specialty care within 30 miles of their homes.
The state’s strong support of telemedicine contributes to payers taking the modality seriously and doctors getting paid for telemedicine care, Dr. Sumner said in an interview.
“Most insurers pay as long as the visit is equal or superior to an exam done in person,” she said. “It has to be quality care.”
Dr. Sumner also can bill a site fee when telemedicine technology is used at her practice, she said. If a patient visits her practice for a psychiatric consultation while Dr. Sumner is busy, for example, a nurse can connect the patient to a psychiatrist through the office’s telemedicine unit. The site fee is minimal, but it helps cover costs, she said.
In states that do not have parity laws, some larger health plans, such as Anthem and UnitedHealthcare, have proactively covered telemedicine services, said Dr. Peter Antall, president and medical director of American Well’s Online Care Group, a national telehealth service. Smaller health plans on the other hand, are sometimes willing to negotiate with providers and consider adding telemedicine services to a fee schedule, Dr. Antall said in an interview.
“I think we’re moving into a phase where reimbursement is normal or expected in telehealth,” he said. “We’re not quite there yet because there are so many health plans and, within the health plans, there are so many different products and subgroups. It’s still a process that needs to evolve.”
Government payers lag behind
Medicaid policies also vary from state by state. Some state programs cover telemedicine services similar to that of in-person treatment. Others limit coverage by technology or geographic area.
Medicare, by far, ranks the worst in paying physicians for telemedicine, experts said. Of $597 billion in total Medicare payments in 2014, 0.0023% was spent on telemedicine, according to data provided to the Robert J. Waters Center for Telehealth & e-Health Law.
“Unless you’re a patient that presents in a rural community, the Medicare telehealth benefit is not available,” said Mr. Quashie, who is part of the CTeL’s legal resource team. “Medicare is almost a no-go under fee-for-service for telehealth.”
CMS reimburses physicians for telemedicine only when the originating site is in a Health Professional Shortage Area or within a county outside a Metropolitan Statistical Area. The originating site must be a medical facility and not the patient’s home. CMS covers care only on an approved list of medical services.
In its 2016 proposed fee schedule, CMS recommended adding two new codes to its accepted telemedicine services, including codes for prolonged service inpatient care and end-stage renal disease–related services. However, the agency denied a handful of other services requested by the ATA and again, refused to end its patient site limitations.
“We are very concerned about Medicare’s decisions in terms of its ability and willingness to reimburse” telehealth services,” Dr. Tuckson said. “Physicians who are trying to care for our nation’s seniors – so many of whom are presenting real challenges in manging their care in an optimal way – those physicians and patients deserve the opportunity to use [telehealth] tools, and physicians deserve to be reimbursed for the appropriate use of those tools.”
Federal legislation to expand Medicare coverage for telehealth has previously failed. Most recently, Rep. Mike Thompson (D-Calif.) proposed H.R. 2948, the Medicare Telehealth Parity Act of 2015, a bill that would broaden Medicare telemedicine coverage to urban areas and cover more services. The bill has been referred to the House Ways and Means Committee’s Subcommittee on Health.
Coverage of telemedicine by all payers is especially necessary as the health care system shifts to a more value-based care structure, Dr. Marcin said. Telemedicine presents great opportunities for preventing illnesses, keeping patients out of the hospital, and lowering health costs, he said. However, financial incentives to utilize telemedicine in these ways is lacking.
“Even though these technologies have been proven to reduce overall health care costs, they result in lower payments to doctors and hospitals,” Dr. Marcin said. “There’s a malalignment with payments to both hospitals and doctors and what should be the goals of health care, which is to keep patients healthy.”
Coming Tuesday, Oct. 6: Can telemedicine expose you to legal risk?
On Twitter @legal_med
Emergency department personnel at a remote hospital called Dr. James P. Marcin regarding a baby who was just admitted with an upper respiratory infection. Because the patient had cyanotic congenital heart disease, the team was concerned she was too medically complex for their facility, and they were preparing to helicopter her to the pediatric intensive care unit at the University of California, Davis, Children’s Hospital in Sacramento.
But when Dr. Marcin examined the baby via a two-way video, he remembered the child from a previous visit. Although her oxygen levels were low, Dr. Marcin knew they were normal for her condition. Dr. Marcin spoke with the patient’s parents and after learning more about the patient’s symptoms, he was confident the child could remain at the small hospital. She was treated for the upper respiratory infection and later sent home where she improved, said Dr. Marcin, who leads the Pediatric Telemedicine Program at UC Davis.
Despite the positive outcome, Dr. Marcin’s claim was denied by the insurance company, he said.
“Had I not used telemedicine, that child would have been put in a helicopter, flown to our ICU, [and likely incurred] some $20,000 bill,” Dr. Marcin said in an interview. “I saved the insurance company $20,000, and then they ended up denying my 2 hours of critical care time. It’s discouraging.”
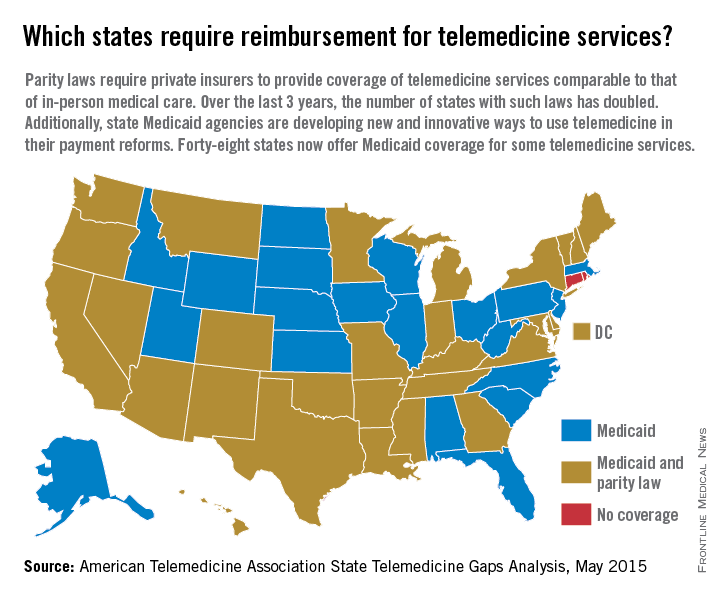
Reimbursement struggles are playing out in medical practices and hospitals across the country. While insurance coverage for telemedicine is growing, experts say payment remains one of the most pressing challenges. So far, 29 states and the District of Columbia have laws that require full parity of coverage and reimbursement for telemedicine services comparable to that of in-person services, according to the American Telemedicine Association (ATA). Medicaid programs in almost all (48) states require some form of compensation for telemedicine, according to a 2015 ATA report.
Payment parity for telemedicine has doubled in the last 2 years, noted Dr. Reed V. Tuckson, ATA president.
“We are seeing, on the side of the private insurance world, really exciting acceptance of telehealth services,” Dr. Tuckson said in an interview. There has been “really great movement forward.”
Enforcement of those parity laws can be spotty, said René Y. Quashie, a Washington health law attorney.
“It’s a mixed bag,” Mr. Quashie said in an interview. “In some states, enforcement is lax so you still have a lot of providers submitting claims that are not being paid or not being paid timely.”
State support equals payment success
In rural Wrightsville, Ga., Dr. Jean R. Sumner regularly gets paid to provide telemedicine. Georgia enacted its parity law in 2006 and has greatly embraced telemedicine capabilities, particularly for its rural populations, said Dr. Sumner, associate dean for rural health at Mercer University in Macon. Part of the success is because of the Georgia Partnership for TeleHealth, a statewide network that focuses on increasing access to care through telemedicine. Its hallmark is the state’s open access network, a web of access points based on existing telemedicine programs that enables secure health information exchange. The goal of the program is for all rural Georgians to access specialty care within 30 miles of their homes.
The state’s strong support of telemedicine contributes to payers taking the modality seriously and doctors getting paid for telemedicine care, Dr. Sumner said in an interview.
“Most insurers pay as long as the visit is equal or superior to an exam done in person,” she said. “It has to be quality care.”
Dr. Sumner also can bill a site fee when telemedicine technology is used at her practice, she said. If a patient visits her practice for a psychiatric consultation while Dr. Sumner is busy, for example, a nurse can connect the patient to a psychiatrist through the office’s telemedicine unit. The site fee is minimal, but it helps cover costs, she said.
In states that do not have parity laws, some larger health plans, such as Anthem and UnitedHealthcare, have proactively covered telemedicine services, said Dr. Peter Antall, president and medical director of American Well’s Online Care Group, a national telehealth service. Smaller health plans on the other hand, are sometimes willing to negotiate with providers and consider adding telemedicine services to a fee schedule, Dr. Antall said in an interview.
“I think we’re moving into a phase where reimbursement is normal or expected in telehealth,” he said. “We’re not quite there yet because there are so many health plans and, within the health plans, there are so many different products and subgroups. It’s still a process that needs to evolve.”
Government payers lag behind
Medicaid policies also vary from state by state. Some state programs cover telemedicine services similar to that of in-person treatment. Others limit coverage by technology or geographic area.
Medicare, by far, ranks the worst in paying physicians for telemedicine, experts said. Of $597 billion in total Medicare payments in 2014, 0.0023% was spent on telemedicine, according to data provided to the Robert J. Waters Center for Telehealth & e-Health Law.
“Unless you’re a patient that presents in a rural community, the Medicare telehealth benefit is not available,” said Mr. Quashie, who is part of the CTeL’s legal resource team. “Medicare is almost a no-go under fee-for-service for telehealth.”
CMS reimburses physicians for telemedicine only when the originating site is in a Health Professional Shortage Area or within a county outside a Metropolitan Statistical Area. The originating site must be a medical facility and not the patient’s home. CMS covers care only on an approved list of medical services.
In its 2016 proposed fee schedule, CMS recommended adding two new codes to its accepted telemedicine services, including codes for prolonged service inpatient care and end-stage renal disease–related services. However, the agency denied a handful of other services requested by the ATA and again, refused to end its patient site limitations.
“We are very concerned about Medicare’s decisions in terms of its ability and willingness to reimburse” telehealth services,” Dr. Tuckson said. “Physicians who are trying to care for our nation’s seniors – so many of whom are presenting real challenges in manging their care in an optimal way – those physicians and patients deserve the opportunity to use [telehealth] tools, and physicians deserve to be reimbursed for the appropriate use of those tools.”
Federal legislation to expand Medicare coverage for telehealth has previously failed. Most recently, Rep. Mike Thompson (D-Calif.) proposed H.R. 2948, the Medicare Telehealth Parity Act of 2015, a bill that would broaden Medicare telemedicine coverage to urban areas and cover more services. The bill has been referred to the House Ways and Means Committee’s Subcommittee on Health.
Coverage of telemedicine by all payers is especially necessary as the health care system shifts to a more value-based care structure, Dr. Marcin said. Telemedicine presents great opportunities for preventing illnesses, keeping patients out of the hospital, and lowering health costs, he said. However, financial incentives to utilize telemedicine in these ways is lacking.
“Even though these technologies have been proven to reduce overall health care costs, they result in lower payments to doctors and hospitals,” Dr. Marcin said. “There’s a malalignment with payments to both hospitals and doctors and what should be the goals of health care, which is to keep patients healthy.”
Coming Tuesday, Oct. 6: Can telemedicine expose you to legal risk?
On Twitter @legal_med
Pioneer ACOs cut out low-value care
In its first year, the Medicare Pioneer accountable care organization (ACO) program resulted in modest reductions in low-value medical services that provide minimal clinical benefit to patients, according to a study published Sept. 21 in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.4525).
The Pioneer ACO model was associated with a differential reduction of 0.8 in low-value services per 100 beneficiaries or a 1.9% decrease in service quantity, and a 4.5% reduction in spending on low-value services.
Lead author Aaron L. Schwartz, Ph.D., of Harvard Medical School, Boston, and his colleagues compared the use of low-value services by Medicare fee-for-service patients whose providers were in the Pioneer ACO program with use of low-value services by beneficiaries of other health care providers. They examined services from 2009 to 2012 using Medicare claims for a random 20% sample of patients. Comparisons were adjusted for sociodemographic and clinical characteristics and for geography. Low-value services were defined as care providing minimal or no average clinical benefit in specific clinical scenarios.
The greatest reductions in service occurred for the most frequent services, including cancer screening and imaging. Cardiovascular testing and procedures underwent the greatest differential reduction – a 6.3% decrease in low-value services for the Pioneer ACO group. ACOs that were providing more low-value care on average experienced greater reductions.
The study findings are consistent with other conclusions that Pioneer ACO models improve the overall value of health care provided, Dr. Schwartz noted. The findings also demonstrate that patient care preferences may not be major obstacles to reducing low-value service use.
The Medicare Pioneer ACO program aims to improve value and lower cost through incentives and penalties. Participating organizations receive a bonus or a penalty if overall spending for patients is based on meeting a financial benchmark. Performance on 33 quality measures determines the proportion of savings or losses shared by the ACO. In 2012, 32 health care provider organizations volunteered to participate in the Pioneer ACO program. In 2015, there were 19 participating organizations, according to CMS data.
On Twitter @legal_med
The study suggests that some ACOs are capable of slowing health care spending growth without jeopardizing the quality of care.
Participants in the first year of the Medicare Pioneer ACO program precisely targeted reduction of low-value services. All doctors increasingly will be called on to apply similar precision in lowering the cost of delivering valuable services without impairing the quality of care. Individually targeted Medicare payment incentives to improve value will begin for physicians in 2019 via a merit-based incentive payment system. One basis for determining individual physician merit will be prudent use of health care resources.
Although adjusting practice to lower costs is a long stretch from physicians’ traditional role, the well-being of their patients and their communities now depend on it.
Dr. Arnold Milstein of the Standford (Calif.) Clinical Excellence Research Center made these comments in an accompanying editorial (doi:10.1001/jamainternmed.2015.5322). He reported no disclosures.
The study suggests that some ACOs are capable of slowing health care spending growth without jeopardizing the quality of care.
Participants in the first year of the Medicare Pioneer ACO program precisely targeted reduction of low-value services. All doctors increasingly will be called on to apply similar precision in lowering the cost of delivering valuable services without impairing the quality of care. Individually targeted Medicare payment incentives to improve value will begin for physicians in 2019 via a merit-based incentive payment system. One basis for determining individual physician merit will be prudent use of health care resources.
Although adjusting practice to lower costs is a long stretch from physicians’ traditional role, the well-being of their patients and their communities now depend on it.
Dr. Arnold Milstein of the Standford (Calif.) Clinical Excellence Research Center made these comments in an accompanying editorial (doi:10.1001/jamainternmed.2015.5322). He reported no disclosures.
The study suggests that some ACOs are capable of slowing health care spending growth without jeopardizing the quality of care.
Participants in the first year of the Medicare Pioneer ACO program precisely targeted reduction of low-value services. All doctors increasingly will be called on to apply similar precision in lowering the cost of delivering valuable services without impairing the quality of care. Individually targeted Medicare payment incentives to improve value will begin for physicians in 2019 via a merit-based incentive payment system. One basis for determining individual physician merit will be prudent use of health care resources.
Although adjusting practice to lower costs is a long stretch from physicians’ traditional role, the well-being of their patients and their communities now depend on it.
Dr. Arnold Milstein of the Standford (Calif.) Clinical Excellence Research Center made these comments in an accompanying editorial (doi:10.1001/jamainternmed.2015.5322). He reported no disclosures.
In its first year, the Medicare Pioneer accountable care organization (ACO) program resulted in modest reductions in low-value medical services that provide minimal clinical benefit to patients, according to a study published Sept. 21 in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.4525).
The Pioneer ACO model was associated with a differential reduction of 0.8 in low-value services per 100 beneficiaries or a 1.9% decrease in service quantity, and a 4.5% reduction in spending on low-value services.
Lead author Aaron L. Schwartz, Ph.D., of Harvard Medical School, Boston, and his colleagues compared the use of low-value services by Medicare fee-for-service patients whose providers were in the Pioneer ACO program with use of low-value services by beneficiaries of other health care providers. They examined services from 2009 to 2012 using Medicare claims for a random 20% sample of patients. Comparisons were adjusted for sociodemographic and clinical characteristics and for geography. Low-value services were defined as care providing minimal or no average clinical benefit in specific clinical scenarios.
The greatest reductions in service occurred for the most frequent services, including cancer screening and imaging. Cardiovascular testing and procedures underwent the greatest differential reduction – a 6.3% decrease in low-value services for the Pioneer ACO group. ACOs that were providing more low-value care on average experienced greater reductions.
The study findings are consistent with other conclusions that Pioneer ACO models improve the overall value of health care provided, Dr. Schwartz noted. The findings also demonstrate that patient care preferences may not be major obstacles to reducing low-value service use.
The Medicare Pioneer ACO program aims to improve value and lower cost through incentives and penalties. Participating organizations receive a bonus or a penalty if overall spending for patients is based on meeting a financial benchmark. Performance on 33 quality measures determines the proportion of savings or losses shared by the ACO. In 2012, 32 health care provider organizations volunteered to participate in the Pioneer ACO program. In 2015, there were 19 participating organizations, according to CMS data.
On Twitter @legal_med
In its first year, the Medicare Pioneer accountable care organization (ACO) program resulted in modest reductions in low-value medical services that provide minimal clinical benefit to patients, according to a study published Sept. 21 in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.4525).
The Pioneer ACO model was associated with a differential reduction of 0.8 in low-value services per 100 beneficiaries or a 1.9% decrease in service quantity, and a 4.5% reduction in spending on low-value services.
Lead author Aaron L. Schwartz, Ph.D., of Harvard Medical School, Boston, and his colleagues compared the use of low-value services by Medicare fee-for-service patients whose providers were in the Pioneer ACO program with use of low-value services by beneficiaries of other health care providers. They examined services from 2009 to 2012 using Medicare claims for a random 20% sample of patients. Comparisons were adjusted for sociodemographic and clinical characteristics and for geography. Low-value services were defined as care providing minimal or no average clinical benefit in specific clinical scenarios.
The greatest reductions in service occurred for the most frequent services, including cancer screening and imaging. Cardiovascular testing and procedures underwent the greatest differential reduction – a 6.3% decrease in low-value services for the Pioneer ACO group. ACOs that were providing more low-value care on average experienced greater reductions.
The study findings are consistent with other conclusions that Pioneer ACO models improve the overall value of health care provided, Dr. Schwartz noted. The findings also demonstrate that patient care preferences may not be major obstacles to reducing low-value service use.
The Medicare Pioneer ACO program aims to improve value and lower cost through incentives and penalties. Participating organizations receive a bonus or a penalty if overall spending for patients is based on meeting a financial benchmark. Performance on 33 quality measures determines the proportion of savings or losses shared by the ACO. In 2012, 32 health care provider organizations volunteered to participate in the Pioneer ACO program. In 2015, there were 19 participating organizations, according to CMS data.
On Twitter @legal_med
FROM JAMA INTERNAL MEDICINE
Key clinical point: The Medicare Pioneer ACO program was associated with modest reductions in low-value services that provide minimal clinical benefit to patients.
Major finding: In its first year, the Medicare Pioneer ACO program was associated with a 0.8 reduction in low-value services per 100 beneficiaries, which was a 1.9% reduction in service quantity and a 4.5% reduction in spending on low-value services.
Data source: Random sample of Medicare claims from the period of 2009-2012.
Disclosures: Dr. Aaron L. Schwartz and Dr. J. Michael McWilliams consult for the Medicare Payment Advisory Commission. Dr. Michael E. Chernew is a partner at VBID Health LLC, which has a contract to develop and market a tool to help insurers and employers quantify spending on low-value services.



























