User login
USPSTF annual report highlights gaps in women’s health research
Research must be increased and improved in five key areas of women’s health before any kind of recommendations for screening can be made, according to the U.S. Preventive Service Task Force’s annual report to Congress.
Specifically, more data is needed before recommendations can be made on:
• Screening for intimate partner violence, illicit drug use, and mental health conditions.
• Screening for thyroid dysfunction.
• Screening for vitamin D deficiency, vitamin D and calcium supplementation to prevent fractures, and screening for osteoporosis.
• Screening for cancer.
• Implementing clinical preventive services.
Regarding mental health conditions, USPSTF identified research gaps in the optimal timing for mental health screening in pregnant women, the effectiveness of treatment in pregnant and postpartum women, the development of risk-assessment tools to identify patients at risk for suicide, the effectiveness of tailored therapies in at-risk patients, and linkages between clinical and community resources to help patients at risk for suicide.
Pertaining to breast cancer, the task force found research voids in the effects of new technology (3-D mammography) on improving long-term health outcomes in breast cancer patients, and evidence gaps in the long-term health outcomes in women with dense breasts who receive screening beyond mammography. The task force also identified research deficiencies in the effectiveness of new screening methods and treatment strategies for ovarian cancer. Finally, the task force identified research gaps in the optimal approach to cervical cancer screening using new technologies, in the harms of different screening and treatment options, and in the effect of human papillomavirus vaccination on cervical cancer screening.
Regarding thyroid dysfunction, the task force found a lack of evidence that would help in understanding the natural history of untreated, asymptomatic thyroid dysfunction; a void in the effectiveness and harms of treating thyroid dysfunction in adults without symptoms; and research gaps in the treatment trials of watchful waiting using health outcomes, such as cardiovascular-related morbidity and mortality.
The task force also identified evidence gaps in the benefits of vitamin D and calcium supplements in reducing the risk of fractures in postmenopausal women, the effectiveness of different preparations of vitamin D or different calcium formulations, and the effectiveness of vitamin D supplementation in diverse populations.
Identifying the evidence gaps and prioritizing the areas for research will hopefully move public and private researchers to collaborate and target their efforts to address the lack of research, according to the report.
The Affordable Care Act charged the task force with sending an annual report to Congress that identifies gaps in evidence and recommends priority areas that deserve further examination; this year’s report focused on women’s health. The ACA also requires that preventive care services and screenings given an A- or B-level recommendation by the task force be covered at no cost to the patient.
On Twitter @legal_med
Research must be increased and improved in five key areas of women’s health before any kind of recommendations for screening can be made, according to the U.S. Preventive Service Task Force’s annual report to Congress.
Specifically, more data is needed before recommendations can be made on:
• Screening for intimate partner violence, illicit drug use, and mental health conditions.
• Screening for thyroid dysfunction.
• Screening for vitamin D deficiency, vitamin D and calcium supplementation to prevent fractures, and screening for osteoporosis.
• Screening for cancer.
• Implementing clinical preventive services.
Regarding mental health conditions, USPSTF identified research gaps in the optimal timing for mental health screening in pregnant women, the effectiveness of treatment in pregnant and postpartum women, the development of risk-assessment tools to identify patients at risk for suicide, the effectiveness of tailored therapies in at-risk patients, and linkages between clinical and community resources to help patients at risk for suicide.
Pertaining to breast cancer, the task force found research voids in the effects of new technology (3-D mammography) on improving long-term health outcomes in breast cancer patients, and evidence gaps in the long-term health outcomes in women with dense breasts who receive screening beyond mammography. The task force also identified research deficiencies in the effectiveness of new screening methods and treatment strategies for ovarian cancer. Finally, the task force identified research gaps in the optimal approach to cervical cancer screening using new technologies, in the harms of different screening and treatment options, and in the effect of human papillomavirus vaccination on cervical cancer screening.
Regarding thyroid dysfunction, the task force found a lack of evidence that would help in understanding the natural history of untreated, asymptomatic thyroid dysfunction; a void in the effectiveness and harms of treating thyroid dysfunction in adults without symptoms; and research gaps in the treatment trials of watchful waiting using health outcomes, such as cardiovascular-related morbidity and mortality.
The task force also identified evidence gaps in the benefits of vitamin D and calcium supplements in reducing the risk of fractures in postmenopausal women, the effectiveness of different preparations of vitamin D or different calcium formulations, and the effectiveness of vitamin D supplementation in diverse populations.
Identifying the evidence gaps and prioritizing the areas for research will hopefully move public and private researchers to collaborate and target their efforts to address the lack of research, according to the report.
The Affordable Care Act charged the task force with sending an annual report to Congress that identifies gaps in evidence and recommends priority areas that deserve further examination; this year’s report focused on women’s health. The ACA also requires that preventive care services and screenings given an A- or B-level recommendation by the task force be covered at no cost to the patient.
On Twitter @legal_med
Research must be increased and improved in five key areas of women’s health before any kind of recommendations for screening can be made, according to the U.S. Preventive Service Task Force’s annual report to Congress.
Specifically, more data is needed before recommendations can be made on:
• Screening for intimate partner violence, illicit drug use, and mental health conditions.
• Screening for thyroid dysfunction.
• Screening for vitamin D deficiency, vitamin D and calcium supplementation to prevent fractures, and screening for osteoporosis.
• Screening for cancer.
• Implementing clinical preventive services.
Regarding mental health conditions, USPSTF identified research gaps in the optimal timing for mental health screening in pregnant women, the effectiveness of treatment in pregnant and postpartum women, the development of risk-assessment tools to identify patients at risk for suicide, the effectiveness of tailored therapies in at-risk patients, and linkages between clinical and community resources to help patients at risk for suicide.
Pertaining to breast cancer, the task force found research voids in the effects of new technology (3-D mammography) on improving long-term health outcomes in breast cancer patients, and evidence gaps in the long-term health outcomes in women with dense breasts who receive screening beyond mammography. The task force also identified research deficiencies in the effectiveness of new screening methods and treatment strategies for ovarian cancer. Finally, the task force identified research gaps in the optimal approach to cervical cancer screening using new technologies, in the harms of different screening and treatment options, and in the effect of human papillomavirus vaccination on cervical cancer screening.
Regarding thyroid dysfunction, the task force found a lack of evidence that would help in understanding the natural history of untreated, asymptomatic thyroid dysfunction; a void in the effectiveness and harms of treating thyroid dysfunction in adults without symptoms; and research gaps in the treatment trials of watchful waiting using health outcomes, such as cardiovascular-related morbidity and mortality.
The task force also identified evidence gaps in the benefits of vitamin D and calcium supplements in reducing the risk of fractures in postmenopausal women, the effectiveness of different preparations of vitamin D or different calcium formulations, and the effectiveness of vitamin D supplementation in diverse populations.
Identifying the evidence gaps and prioritizing the areas for research will hopefully move public and private researchers to collaborate and target their efforts to address the lack of research, according to the report.
The Affordable Care Act charged the task force with sending an annual report to Congress that identifies gaps in evidence and recommends priority areas that deserve further examination; this year’s report focused on women’s health. The ACA also requires that preventive care services and screenings given an A- or B-level recommendation by the task force be covered at no cost to the patient.
On Twitter @legal_med
Medical malpractice landscape improving for ob.gyns.
Dr. Marcus E. Tower remembers a time when it was nearly impossible for ob.gyns. to secure and retain medical malpractice insurance in his home state of Ohio.
Skyrocketing lawsuits had forced most physicians to shutter their practices, while insurers were dropping ob.gyns. from coverage and doctors were looking to escape the litigious state. Today, the legal landscape is vastly different, said Dr. Tower, director of ob.gyn. at Hillcrest Hospital, a Cleveland Clinic hospital in Mayfield Heights, Ohio. Malpractice reforms have helped stabilize the environment, he said, reducing frivolous lawsuits and making insurance more affordable.
Dr. Tower now pays $32,000 a year in malpractice premiums, the same rate he paid 30 years ago as a new physician.
“It’s improved quite dramatically,” Dr. Tower said. “Fifteen years ago, we were seeing a physician exodus from the state. Why would someone who just started a career in medicine want to practice in a state where you have to worry constantly about being sued? Now things have improved where you can take care of the patients as opposed to worrying about what you’re going to be facing in the courtroom.”
Dr. Tower’s experience is becoming more common across the country, legal experts say. Although historically obstetrics and gynecology had one of the most challenging legal landscapes, data show that more ob.gyns. are getting some relief. The number of lawsuits against ob.gyns. is on the decline nationwide, and the majority of malpractice premiums are decreasing or holding steady.
“On the whole, obstetricians have benefited from the overall improvement in the medical malpractice climate in the United States, particularly in the last 10 years,” said Paul A. Greve Jr., executive vice president and senior consultant for the Willis Health Care Practice, a global risk management consultant firm. “The number of suits being filed are at an all-time low.”
National medical liability insurer the Doctors Co. reports that ob.gyn. claim frequency has dropped by 50% from 2005 to 2014, according to its claims database.
As for malpractice premiums across specialties, after significant hikes in the early 2000s, rates started to fall across the board in 2006 and 2007. In 2008, 43% of premiums decreased for internists, general surgeons, and ob.gyns. And another 50% of rates did not change, according to 2008 data from the Medical Liability Monitor (MLM), which surveys rates from major liability insurers for internists, general surgeons, and ob.gyns. Steady premiums have continued for the past several years, with 71% of rates remaining unchanged in 2015, according to the latest MLM survey.
Litigation hotbeds
But not all ob.gyns. can attest to these improvements, said Dr. Thad L. Anderson, an ob.gyn. in private practice in Dubuque, Iowa, and chair of the American College of Obstetricians and Gynecologists’ Committee on Professional Liability.
Results from the 2015 American Congress of Obstetricians and Gynecologists’ Survey on Professional Liability show that about 40% of ob.gyns. made changes to their practice as a result of affordability and/or availability of liability insurance from 2012 to 2014. But that’s down from the 2012 survey, when 51% of ob.gyns. reported making changes based on insurance affordability and availability. The latest ACOG survey also found that nearly half of ob.gyns. made changes to their practice as a result of fear of litigation, a decrease from the 58% who responded similarly in the 2012 survey.
“Things may be stable, but if you go state by state, it’s very dependent on the litigation environment in that state,” Dr. Anderson said. “There are always hotbed states of litigation.”
Dr. Karen Harris, a gynecologist in Gainesville, Fla., has practiced in one of these hotbeds for the last 26 years.
In 2015, ob.gyns. in the Sunshine State paid between $80,000 and $190,000 in insurance premiums, according to the 2015 MLM survey, among the highest rates in the country. The excessive costs have forced Dr. Harris and her colleagues in a 10-physician practice to forgo insurance coverage. Instead, they have a prepaid malpractice defense policy with a law firm. The practice pays a monthly charge, and the firm defends them against all claims.
Dr. Harris said she’s paid less in settling claims than she would have paid in insurance premiums. She noted that the decision to skip coverage was driven by a 2005 case in which the settlement exceeded the practice’s insurance coverage.
“We had to pay personally out of pocket to settle the case, so I was paying my premium plus I had to pay out of pocket,” she said. “It was really awful. Then you realize, ‘Wow, I can’t buy effective coverage. I can’t afford it. Why should I have any coverage?’ ”
Similar legal woes are felt by many East Coast physicians, including Dr. Henry M. Lerner, a Newton, Mass., ob.gyn. At least one doctor in his eight-physician practice is sued annually, and the group’s premiums regularly increase, he said. Ob.gyns. in the state paid between $95,000 and $110,000 in malpractice insurance premiums in 2015, according to MLM data.
“Of the eight in my group, I don’t know of any that have not been sued,” Dr. Lerner said. “They live in fear of the suits, especially my younger partners. I’ve had a couple just about quit after they’ve been sued. They don’t always do what they would want to do clinically because they think it would increase their liability exposure.”
Claims target deeper pockets
While state malpractice reform laws have contributed to better legal environments in some states, doctors and legal experts say legislation is far from the only reason for relaxed litigation climates. The high cost of preparing a medical malpractice case – $100,000 on average – has also influenced claims, said Mr. Greve, who coauthored the 2015 MLM survey.
“That has caused a lot of plaintiffs’ [attorneys] to be very careful in screening the type of cases they are willing to take to litigation,” he said.
Better technology and stronger clinical training are also potential factors for the improved legal landscape. Plaintiffs are also more apt to go after hospitals and health systems, rather than physicians, said Dr. John Thorp Jr. of the University of North Carolina at Chapel Hill.
“The biggest shift that I have seen is that ob.gyns. have lowered coverage limits coincidentally with the rise in demand to care for neuroinjured babies,” Dr. Thorp said. “This has shifted the focus of litigation from the ob.gyn. to the health system, which has more resources.”
Despite the more stable legal climate, when ob.gyns. do get sued, the financial impact is greater than that for other specialties – a pattern that has not changed. The average court award in an ob.gyn. case is higher than that of all specialties combined, according to the Doctors Co.
“We are not in crisis like we have been in the past, but there’s always the potential for one bad outcome – in the form of a multimillion [dollar] judgment – to clean individuals out of business,” said ACOG’s Dr. Anderson. “Some may choose to retire earlier wbecause of the stress and concern.”
On Twitter @legal_med
Dr. Marcus E. Tower remembers a time when it was nearly impossible for ob.gyns. to secure and retain medical malpractice insurance in his home state of Ohio.
Skyrocketing lawsuits had forced most physicians to shutter their practices, while insurers were dropping ob.gyns. from coverage and doctors were looking to escape the litigious state. Today, the legal landscape is vastly different, said Dr. Tower, director of ob.gyn. at Hillcrest Hospital, a Cleveland Clinic hospital in Mayfield Heights, Ohio. Malpractice reforms have helped stabilize the environment, he said, reducing frivolous lawsuits and making insurance more affordable.
Dr. Tower now pays $32,000 a year in malpractice premiums, the same rate he paid 30 years ago as a new physician.
“It’s improved quite dramatically,” Dr. Tower said. “Fifteen years ago, we were seeing a physician exodus from the state. Why would someone who just started a career in medicine want to practice in a state where you have to worry constantly about being sued? Now things have improved where you can take care of the patients as opposed to worrying about what you’re going to be facing in the courtroom.”
Dr. Tower’s experience is becoming more common across the country, legal experts say. Although historically obstetrics and gynecology had one of the most challenging legal landscapes, data show that more ob.gyns. are getting some relief. The number of lawsuits against ob.gyns. is on the decline nationwide, and the majority of malpractice premiums are decreasing or holding steady.
“On the whole, obstetricians have benefited from the overall improvement in the medical malpractice climate in the United States, particularly in the last 10 years,” said Paul A. Greve Jr., executive vice president and senior consultant for the Willis Health Care Practice, a global risk management consultant firm. “The number of suits being filed are at an all-time low.”
National medical liability insurer the Doctors Co. reports that ob.gyn. claim frequency has dropped by 50% from 2005 to 2014, according to its claims database.
As for malpractice premiums across specialties, after significant hikes in the early 2000s, rates started to fall across the board in 2006 and 2007. In 2008, 43% of premiums decreased for internists, general surgeons, and ob.gyns. And another 50% of rates did not change, according to 2008 data from the Medical Liability Monitor (MLM), which surveys rates from major liability insurers for internists, general surgeons, and ob.gyns. Steady premiums have continued for the past several years, with 71% of rates remaining unchanged in 2015, according to the latest MLM survey.
Litigation hotbeds
But not all ob.gyns. can attest to these improvements, said Dr. Thad L. Anderson, an ob.gyn. in private practice in Dubuque, Iowa, and chair of the American College of Obstetricians and Gynecologists’ Committee on Professional Liability.
Results from the 2015 American Congress of Obstetricians and Gynecologists’ Survey on Professional Liability show that about 40% of ob.gyns. made changes to their practice as a result of affordability and/or availability of liability insurance from 2012 to 2014. But that’s down from the 2012 survey, when 51% of ob.gyns. reported making changes based on insurance affordability and availability. The latest ACOG survey also found that nearly half of ob.gyns. made changes to their practice as a result of fear of litigation, a decrease from the 58% who responded similarly in the 2012 survey.
“Things may be stable, but if you go state by state, it’s very dependent on the litigation environment in that state,” Dr. Anderson said. “There are always hotbed states of litigation.”
Dr. Karen Harris, a gynecologist in Gainesville, Fla., has practiced in one of these hotbeds for the last 26 years.
In 2015, ob.gyns. in the Sunshine State paid between $80,000 and $190,000 in insurance premiums, according to the 2015 MLM survey, among the highest rates in the country. The excessive costs have forced Dr. Harris and her colleagues in a 10-physician practice to forgo insurance coverage. Instead, they have a prepaid malpractice defense policy with a law firm. The practice pays a monthly charge, and the firm defends them against all claims.
Dr. Harris said she’s paid less in settling claims than she would have paid in insurance premiums. She noted that the decision to skip coverage was driven by a 2005 case in which the settlement exceeded the practice’s insurance coverage.
“We had to pay personally out of pocket to settle the case, so I was paying my premium plus I had to pay out of pocket,” she said. “It was really awful. Then you realize, ‘Wow, I can’t buy effective coverage. I can’t afford it. Why should I have any coverage?’ ”
Similar legal woes are felt by many East Coast physicians, including Dr. Henry M. Lerner, a Newton, Mass., ob.gyn. At least one doctor in his eight-physician practice is sued annually, and the group’s premiums regularly increase, he said. Ob.gyns. in the state paid between $95,000 and $110,000 in malpractice insurance premiums in 2015, according to MLM data.
“Of the eight in my group, I don’t know of any that have not been sued,” Dr. Lerner said. “They live in fear of the suits, especially my younger partners. I’ve had a couple just about quit after they’ve been sued. They don’t always do what they would want to do clinically because they think it would increase their liability exposure.”
Claims target deeper pockets
While state malpractice reform laws have contributed to better legal environments in some states, doctors and legal experts say legislation is far from the only reason for relaxed litigation climates. The high cost of preparing a medical malpractice case – $100,000 on average – has also influenced claims, said Mr. Greve, who coauthored the 2015 MLM survey.
“That has caused a lot of plaintiffs’ [attorneys] to be very careful in screening the type of cases they are willing to take to litigation,” he said.
Better technology and stronger clinical training are also potential factors for the improved legal landscape. Plaintiffs are also more apt to go after hospitals and health systems, rather than physicians, said Dr. John Thorp Jr. of the University of North Carolina at Chapel Hill.
“The biggest shift that I have seen is that ob.gyns. have lowered coverage limits coincidentally with the rise in demand to care for neuroinjured babies,” Dr. Thorp said. “This has shifted the focus of litigation from the ob.gyn. to the health system, which has more resources.”
Despite the more stable legal climate, when ob.gyns. do get sued, the financial impact is greater than that for other specialties – a pattern that has not changed. The average court award in an ob.gyn. case is higher than that of all specialties combined, according to the Doctors Co.
“We are not in crisis like we have been in the past, but there’s always the potential for one bad outcome – in the form of a multimillion [dollar] judgment – to clean individuals out of business,” said ACOG’s Dr. Anderson. “Some may choose to retire earlier wbecause of the stress and concern.”
On Twitter @legal_med
Dr. Marcus E. Tower remembers a time when it was nearly impossible for ob.gyns. to secure and retain medical malpractice insurance in his home state of Ohio.
Skyrocketing lawsuits had forced most physicians to shutter their practices, while insurers were dropping ob.gyns. from coverage and doctors were looking to escape the litigious state. Today, the legal landscape is vastly different, said Dr. Tower, director of ob.gyn. at Hillcrest Hospital, a Cleveland Clinic hospital in Mayfield Heights, Ohio. Malpractice reforms have helped stabilize the environment, he said, reducing frivolous lawsuits and making insurance more affordable.
Dr. Tower now pays $32,000 a year in malpractice premiums, the same rate he paid 30 years ago as a new physician.
“It’s improved quite dramatically,” Dr. Tower said. “Fifteen years ago, we were seeing a physician exodus from the state. Why would someone who just started a career in medicine want to practice in a state where you have to worry constantly about being sued? Now things have improved where you can take care of the patients as opposed to worrying about what you’re going to be facing in the courtroom.”
Dr. Tower’s experience is becoming more common across the country, legal experts say. Although historically obstetrics and gynecology had one of the most challenging legal landscapes, data show that more ob.gyns. are getting some relief. The number of lawsuits against ob.gyns. is on the decline nationwide, and the majority of malpractice premiums are decreasing or holding steady.
“On the whole, obstetricians have benefited from the overall improvement in the medical malpractice climate in the United States, particularly in the last 10 years,” said Paul A. Greve Jr., executive vice president and senior consultant for the Willis Health Care Practice, a global risk management consultant firm. “The number of suits being filed are at an all-time low.”
National medical liability insurer the Doctors Co. reports that ob.gyn. claim frequency has dropped by 50% from 2005 to 2014, according to its claims database.
As for malpractice premiums across specialties, after significant hikes in the early 2000s, rates started to fall across the board in 2006 and 2007. In 2008, 43% of premiums decreased for internists, general surgeons, and ob.gyns. And another 50% of rates did not change, according to 2008 data from the Medical Liability Monitor (MLM), which surveys rates from major liability insurers for internists, general surgeons, and ob.gyns. Steady premiums have continued for the past several years, with 71% of rates remaining unchanged in 2015, according to the latest MLM survey.
Litigation hotbeds
But not all ob.gyns. can attest to these improvements, said Dr. Thad L. Anderson, an ob.gyn. in private practice in Dubuque, Iowa, and chair of the American College of Obstetricians and Gynecologists’ Committee on Professional Liability.
Results from the 2015 American Congress of Obstetricians and Gynecologists’ Survey on Professional Liability show that about 40% of ob.gyns. made changes to their practice as a result of affordability and/or availability of liability insurance from 2012 to 2014. But that’s down from the 2012 survey, when 51% of ob.gyns. reported making changes based on insurance affordability and availability. The latest ACOG survey also found that nearly half of ob.gyns. made changes to their practice as a result of fear of litigation, a decrease from the 58% who responded similarly in the 2012 survey.
“Things may be stable, but if you go state by state, it’s very dependent on the litigation environment in that state,” Dr. Anderson said. “There are always hotbed states of litigation.”
Dr. Karen Harris, a gynecologist in Gainesville, Fla., has practiced in one of these hotbeds for the last 26 years.
In 2015, ob.gyns. in the Sunshine State paid between $80,000 and $190,000 in insurance premiums, according to the 2015 MLM survey, among the highest rates in the country. The excessive costs have forced Dr. Harris and her colleagues in a 10-physician practice to forgo insurance coverage. Instead, they have a prepaid malpractice defense policy with a law firm. The practice pays a monthly charge, and the firm defends them against all claims.
Dr. Harris said she’s paid less in settling claims than she would have paid in insurance premiums. She noted that the decision to skip coverage was driven by a 2005 case in which the settlement exceeded the practice’s insurance coverage.
“We had to pay personally out of pocket to settle the case, so I was paying my premium plus I had to pay out of pocket,” she said. “It was really awful. Then you realize, ‘Wow, I can’t buy effective coverage. I can’t afford it. Why should I have any coverage?’ ”
Similar legal woes are felt by many East Coast physicians, including Dr. Henry M. Lerner, a Newton, Mass., ob.gyn. At least one doctor in his eight-physician practice is sued annually, and the group’s premiums regularly increase, he said. Ob.gyns. in the state paid between $95,000 and $110,000 in malpractice insurance premiums in 2015, according to MLM data.
“Of the eight in my group, I don’t know of any that have not been sued,” Dr. Lerner said. “They live in fear of the suits, especially my younger partners. I’ve had a couple just about quit after they’ve been sued. They don’t always do what they would want to do clinically because they think it would increase their liability exposure.”
Claims target deeper pockets
While state malpractice reform laws have contributed to better legal environments in some states, doctors and legal experts say legislation is far from the only reason for relaxed litigation climates. The high cost of preparing a medical malpractice case – $100,000 on average – has also influenced claims, said Mr. Greve, who coauthored the 2015 MLM survey.
“That has caused a lot of plaintiffs’ [attorneys] to be very careful in screening the type of cases they are willing to take to litigation,” he said.
Better technology and stronger clinical training are also potential factors for the improved legal landscape. Plaintiffs are also more apt to go after hospitals and health systems, rather than physicians, said Dr. John Thorp Jr. of the University of North Carolina at Chapel Hill.
“The biggest shift that I have seen is that ob.gyns. have lowered coverage limits coincidentally with the rise in demand to care for neuroinjured babies,” Dr. Thorp said. “This has shifted the focus of litigation from the ob.gyn. to the health system, which has more resources.”
Despite the more stable legal climate, when ob.gyns. do get sued, the financial impact is greater than that for other specialties – a pattern that has not changed. The average court award in an ob.gyn. case is higher than that of all specialties combined, according to the Doctors Co.
“We are not in crisis like we have been in the past, but there’s always the potential for one bad outcome – in the form of a multimillion [dollar] judgment – to clean individuals out of business,” said ACOG’s Dr. Anderson. “Some may choose to retire earlier wbecause of the stress and concern.”
On Twitter @legal_med
Supreme Court agrees to hear ACA contraceptive mandate opt-out challenge
The U.S. Supreme Court is once again taking up a challenge to the Affordable Care Act – this time to determine whether a controversial exception under the law’s contraceptive mandate violates religious freedoms. The Nov. 6 decision to hear the debate comes just a year after justices ruled in Burwell v. Hobby Lobby Stores, in which the high court ruled that for-profit firms owned by religiously devout owners could not be forced to provide birth control coverage to their employees under the ACA.
This time, plaintiffs in seven cases argue that the birth control mandate’s accommodation process imposes substantial burdens on the exercise of religion in violation of the Religious Freedom Restoration Act. The accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities such as churches.
To get out of the ACA requirement to cover contraception as a preventive care service, companies must send their written objections to the federal government. Insurers and the government will then provide employees with coverage for birth control without the employer’s assistance.
The plaintiffs, including several religious groups and nonprofits, counter that the process serves as a “trigger” that enables contraceptive use and makes the groups complicit. The government argues the exception does impose a burden on the groups and that courts should not disregard the interest of employees who may not share employers’ religious beliefs.
The Supreme Court’s review will settle a split among circuit courts over the issue. The 8th U.S. Circuit Court of Appeals in September became the first circuit court to rule that the government’s religious freedom accommodation is not enough and that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The court issued two decisions on Sept. 17 striking down the contraception mandate’s exception. The 8th Circuit decisions are at odds with rulings by the 2nd and 5th Circuits. Other judges have ruled that the accommodation relieves, rather than burdens, plaintiffs’ religious rights.
The high court has consolidated the seven cases for its evaluation. A hearing on the challenges is expected by late March.
On Twitter @legal_med
The U.S. Supreme Court is once again taking up a challenge to the Affordable Care Act – this time to determine whether a controversial exception under the law’s contraceptive mandate violates religious freedoms. The Nov. 6 decision to hear the debate comes just a year after justices ruled in Burwell v. Hobby Lobby Stores, in which the high court ruled that for-profit firms owned by religiously devout owners could not be forced to provide birth control coverage to their employees under the ACA.
This time, plaintiffs in seven cases argue that the birth control mandate’s accommodation process imposes substantial burdens on the exercise of religion in violation of the Religious Freedom Restoration Act. The accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities such as churches.
To get out of the ACA requirement to cover contraception as a preventive care service, companies must send their written objections to the federal government. Insurers and the government will then provide employees with coverage for birth control without the employer’s assistance.
The plaintiffs, including several religious groups and nonprofits, counter that the process serves as a “trigger” that enables contraceptive use and makes the groups complicit. The government argues the exception does impose a burden on the groups and that courts should not disregard the interest of employees who may not share employers’ religious beliefs.
The Supreme Court’s review will settle a split among circuit courts over the issue. The 8th U.S. Circuit Court of Appeals in September became the first circuit court to rule that the government’s religious freedom accommodation is not enough and that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The court issued two decisions on Sept. 17 striking down the contraception mandate’s exception. The 8th Circuit decisions are at odds with rulings by the 2nd and 5th Circuits. Other judges have ruled that the accommodation relieves, rather than burdens, plaintiffs’ religious rights.
The high court has consolidated the seven cases for its evaluation. A hearing on the challenges is expected by late March.
On Twitter @legal_med
The U.S. Supreme Court is once again taking up a challenge to the Affordable Care Act – this time to determine whether a controversial exception under the law’s contraceptive mandate violates religious freedoms. The Nov. 6 decision to hear the debate comes just a year after justices ruled in Burwell v. Hobby Lobby Stores, in which the high court ruled that for-profit firms owned by religiously devout owners could not be forced to provide birth control coverage to their employees under the ACA.
This time, plaintiffs in seven cases argue that the birth control mandate’s accommodation process imposes substantial burdens on the exercise of religion in violation of the Religious Freedom Restoration Act. The accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities such as churches.
To get out of the ACA requirement to cover contraception as a preventive care service, companies must send their written objections to the federal government. Insurers and the government will then provide employees with coverage for birth control without the employer’s assistance.
The plaintiffs, including several religious groups and nonprofits, counter that the process serves as a “trigger” that enables contraceptive use and makes the groups complicit. The government argues the exception does impose a burden on the groups and that courts should not disregard the interest of employees who may not share employers’ religious beliefs.
The Supreme Court’s review will settle a split among circuit courts over the issue. The 8th U.S. Circuit Court of Appeals in September became the first circuit court to rule that the government’s religious freedom accommodation is not enough and that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The court issued two decisions on Sept. 17 striking down the contraception mandate’s exception. The 8th Circuit decisions are at odds with rulings by the 2nd and 5th Circuits. Other judges have ruled that the accommodation relieves, rather than burdens, plaintiffs’ religious rights.
The high court has consolidated the seven cases for its evaluation. A hearing on the challenges is expected by late March.
On Twitter @legal_med
Higher medical spending led to fewer malpractice claims
Greater than average spending was associated with reduced risk of incurring a malpractice claim across all physician specialties in a study of almost 25,000 doctors published Nov. 4 in the BMJ. The finding is consistent with widespread beliefs that higher resource use – sometimes defined as defensive medicine – limits the risk of litigation.
Dr. Anupam B. Jena of Harvard Medical School, Boston, and colleagues compared data from the Florida Agency for Health Care Administration on all acute care hospital discharges from 2000 to 2009 with data from the Florida Office of Insurance Regulation on all closed malpractice claims against Florida physicians during the same period. The data included 24,637 physicians (pediatricians, family physicians, general surgeons, obstetrician-gynecologists, and some subspecialists), more than 18 million hospital admissions, and 4,342 malpractice claims (BMJ 2015;351:h5516. doi: 10.1136/bmj.h5516). They looked at total hospital charges associated with patients treated by a given physician in a given year, averaged across all patients treated by that physician in that year, and adjusted for patient personal and clinical characteristics.
Across all specialties, higher average spending per year was associated with a lower probability of an alleged malpractice incident in the subsequent year. For internists, mean risk-adjusted spending per physician ranged from $19,725 for each hospital admission in the bottom fifth of physician years to $39,379 in the top fifth. The probability for an alleged malpractice claim ranged from 1.5% in the bottom spending fifth to 0.3% in the top spending fifth. Similarly, for ob.gyns., the probability of experiencing an alleged malpractice incident ranged from 1.9% in the bottom fifth of spending to 0.4% in the top fifth. Ob.gyns. on the low end of resource utilization spent a risk-adjusted mean of $8,653, while ob.gyns. on the high end spent $18,162.
Dr. Jena and colleagues also studied more than 1.5 million deliveries performed by 1,625 obstetricians; 15% were cesarean deliveries. In total, 496 malpractice claims were filed against these obstetricians. Ob.gyns. with higher cesarean rates per year were less likely to face a malpractice claim. The probability of being sued ranged from 5.7% in the bottom fifth of cesarean delivery rates to 2.7% in the top fifth.
Authors note that if higher spending is motivated by concerns about malpractice, then the spending would be considered “defensively motivated. However, that spending may not be wasteful if it is associated with fewer errors and therefore lower malpractice claims. More study is needed to compare the costs of additional resource use and the value of reduced errors to learn whether such defensively motivated care is socially wasteful or reflects socially beneficial deterrence.”
The study was supported by the National Institutes of Health.
On Twitter @legal_med
It may be tempting for doctors to view the results of the study by Dr. Jena and colleagues as a means to justify additional tests and procedures to mitigate the risk of a malpractice claim. We would suggest that they should view the study results as a contribution to our understanding of the risk of such claims. We need to better understand defensive medicine, how to define it, how to measure it, and how its practice impacts patients and doctors.
Dr. Tara F. Bishop and Dr. Michael Pesko are with the Department of Health Care Policy and Research at Weill Cornell Medical College in New York. Their comments were taken from an editorial accompanying Dr. Jena’s study (BMJ 2015;351:h5786. doi: 10.1136/bmj.h5786).
It may be tempting for doctors to view the results of the study by Dr. Jena and colleagues as a means to justify additional tests and procedures to mitigate the risk of a malpractice claim. We would suggest that they should view the study results as a contribution to our understanding of the risk of such claims. We need to better understand defensive medicine, how to define it, how to measure it, and how its practice impacts patients and doctors.
Dr. Tara F. Bishop and Dr. Michael Pesko are with the Department of Health Care Policy and Research at Weill Cornell Medical College in New York. Their comments were taken from an editorial accompanying Dr. Jena’s study (BMJ 2015;351:h5786. doi: 10.1136/bmj.h5786).
It may be tempting for doctors to view the results of the study by Dr. Jena and colleagues as a means to justify additional tests and procedures to mitigate the risk of a malpractice claim. We would suggest that they should view the study results as a contribution to our understanding of the risk of such claims. We need to better understand defensive medicine, how to define it, how to measure it, and how its practice impacts patients and doctors.
Dr. Tara F. Bishop and Dr. Michael Pesko are with the Department of Health Care Policy and Research at Weill Cornell Medical College in New York. Their comments were taken from an editorial accompanying Dr. Jena’s study (BMJ 2015;351:h5786. doi: 10.1136/bmj.h5786).
Greater than average spending was associated with reduced risk of incurring a malpractice claim across all physician specialties in a study of almost 25,000 doctors published Nov. 4 in the BMJ. The finding is consistent with widespread beliefs that higher resource use – sometimes defined as defensive medicine – limits the risk of litigation.
Dr. Anupam B. Jena of Harvard Medical School, Boston, and colleagues compared data from the Florida Agency for Health Care Administration on all acute care hospital discharges from 2000 to 2009 with data from the Florida Office of Insurance Regulation on all closed malpractice claims against Florida physicians during the same period. The data included 24,637 physicians (pediatricians, family physicians, general surgeons, obstetrician-gynecologists, and some subspecialists), more than 18 million hospital admissions, and 4,342 malpractice claims (BMJ 2015;351:h5516. doi: 10.1136/bmj.h5516). They looked at total hospital charges associated with patients treated by a given physician in a given year, averaged across all patients treated by that physician in that year, and adjusted for patient personal and clinical characteristics.
Across all specialties, higher average spending per year was associated with a lower probability of an alleged malpractice incident in the subsequent year. For internists, mean risk-adjusted spending per physician ranged from $19,725 for each hospital admission in the bottom fifth of physician years to $39,379 in the top fifth. The probability for an alleged malpractice claim ranged from 1.5% in the bottom spending fifth to 0.3% in the top spending fifth. Similarly, for ob.gyns., the probability of experiencing an alleged malpractice incident ranged from 1.9% in the bottom fifth of spending to 0.4% in the top fifth. Ob.gyns. on the low end of resource utilization spent a risk-adjusted mean of $8,653, while ob.gyns. on the high end spent $18,162.
Dr. Jena and colleagues also studied more than 1.5 million deliveries performed by 1,625 obstetricians; 15% were cesarean deliveries. In total, 496 malpractice claims were filed against these obstetricians. Ob.gyns. with higher cesarean rates per year were less likely to face a malpractice claim. The probability of being sued ranged from 5.7% in the bottom fifth of cesarean delivery rates to 2.7% in the top fifth.
Authors note that if higher spending is motivated by concerns about malpractice, then the spending would be considered “defensively motivated. However, that spending may not be wasteful if it is associated with fewer errors and therefore lower malpractice claims. More study is needed to compare the costs of additional resource use and the value of reduced errors to learn whether such defensively motivated care is socially wasteful or reflects socially beneficial deterrence.”
The study was supported by the National Institutes of Health.
On Twitter @legal_med
Greater than average spending was associated with reduced risk of incurring a malpractice claim across all physician specialties in a study of almost 25,000 doctors published Nov. 4 in the BMJ. The finding is consistent with widespread beliefs that higher resource use – sometimes defined as defensive medicine – limits the risk of litigation.
Dr. Anupam B. Jena of Harvard Medical School, Boston, and colleagues compared data from the Florida Agency for Health Care Administration on all acute care hospital discharges from 2000 to 2009 with data from the Florida Office of Insurance Regulation on all closed malpractice claims against Florida physicians during the same period. The data included 24,637 physicians (pediatricians, family physicians, general surgeons, obstetrician-gynecologists, and some subspecialists), more than 18 million hospital admissions, and 4,342 malpractice claims (BMJ 2015;351:h5516. doi: 10.1136/bmj.h5516). They looked at total hospital charges associated with patients treated by a given physician in a given year, averaged across all patients treated by that physician in that year, and adjusted for patient personal and clinical characteristics.
Across all specialties, higher average spending per year was associated with a lower probability of an alleged malpractice incident in the subsequent year. For internists, mean risk-adjusted spending per physician ranged from $19,725 for each hospital admission in the bottom fifth of physician years to $39,379 in the top fifth. The probability for an alleged malpractice claim ranged from 1.5% in the bottom spending fifth to 0.3% in the top spending fifth. Similarly, for ob.gyns., the probability of experiencing an alleged malpractice incident ranged from 1.9% in the bottom fifth of spending to 0.4% in the top fifth. Ob.gyns. on the low end of resource utilization spent a risk-adjusted mean of $8,653, while ob.gyns. on the high end spent $18,162.
Dr. Jena and colleagues also studied more than 1.5 million deliveries performed by 1,625 obstetricians; 15% were cesarean deliveries. In total, 496 malpractice claims were filed against these obstetricians. Ob.gyns. with higher cesarean rates per year were less likely to face a malpractice claim. The probability of being sued ranged from 5.7% in the bottom fifth of cesarean delivery rates to 2.7% in the top fifth.
Authors note that if higher spending is motivated by concerns about malpractice, then the spending would be considered “defensively motivated. However, that spending may not be wasteful if it is associated with fewer errors and therefore lower malpractice claims. More study is needed to compare the costs of additional resource use and the value of reduced errors to learn whether such defensively motivated care is socially wasteful or reflects socially beneficial deterrence.”
The study was supported by the National Institutes of Health.
On Twitter @legal_med
CMS finalizes 2016 fee schedule with payment for advance care planning
Officials at the Centers for Medicare & Medicaid Services have issued the final 2016 fee schedule for physicians, making modifications to the Physician Quality Reporting System (PQRS) and loosening requirements for its controversial two-midnight rule.
The fee schedule – the first since repeal of the Sustainable Growth Rate (SGR) formula and enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – includes changes to payment policies, modifications to misvalued codes, and updates to quality performance metrics under the PQRS, the Medicare Shared Savings Program, and Physician Compare, among others.
As part of the final fee schedule rule, released Oct. 30, CMS is relaxing its two-midnight rule to allow doctors greater flexibility when determining whether hospital stays are subject to the regulation.
For hospital stays for which physicians expect the patient will need less than two midnights of hospital care, an inpatient admission may still be payable under Medicare Part A on a case-by-case basis based on the admitting physician’s judgment, according to the final rule. Additionally, the agency does not plan to send recovery auditors after doctors suspected of violating the two-midnight rule. Instead, CMS plans to use Beneficiary and Family Centered Care Quality Improvement Organizations to conduct initial medical reviews of claims for short-stay inpatient admissions. The claim reviews will focus on educating physicians and hospitals about the policy for inpatient admissions.
Only physicians with questionable practice patterns, such as high rates of claims denial after medical review, will be referred to auditors, according to CMS.
“These changes continue CMS’ long-standing emphasis on the importance of a physician’s medical judgment in meeting the needs of Medicare beneficiaries,” CMS officials stated in a fact sheet.
CMS also finalized two new advance care planning codes that will pay physicians for time spent discussing patient options for advance directives. The first code will cover an initial 30 minutes of the physicians’ time, and the second code will cover additional 30-minute blocks as necessary.
The AMA Current Procedural Terminology (CPT) Editorial Panel and the AMA Relative Value Update Committee (RUC) created the new CPT codes and recommended the associated payments for calendar year 2015, but CMS delayed the codes’ enactment until collecting public comment.
Modifications to quality programs include a new reporting option under the PQRS that will allow group practices to report quality measure data using a Qualified Clinical Data Registry. In 2016, there will be 281 measures in the PQRS measure set and 18 measures in the Group Practice Reporting Option (GPRO) Web Interface, according to the final rule.
The 2018 payment adjustment will be the last adjustment under the PQRS. Starting in 2019, adjustments to payment for quality reporting and other factors will be made under the Merit-Based Incentive Payment System (MIPS), as required by MACRA.
Changes to the Value-Based Payment Modifier program are also coming in 2016:
• CMS will apply the quality-tiering methodology to all groups and solo practitioners that meet the criteria to avoid the downward adjustment under the PQRS. Groups and solo practitioners would be subject to upward, neutral, or downward adjustments derived under the quality-tiering methodology.
• CMS will continue to set the maximum upward adjustment under the quality-tiering methodology for the CY 2018 value modifier at four times an adjustment factor for groups of physicians with 10 or more eligible professionals, and two times an adjustment factor for groups of physicians with between two and nine eligible professionals and physician solo practitioners.
• CMS will use calendar year 2016 as the performance period for the calendar 2018 value modifier and continue to apply the 2018 value modifier based on participation in the PQRS by groups and solo practitioners.
The fee schedule also includes modifications to the Medicare Shared Savings Program including a new measure on statin therapy for the prevention and treatment of cardiovascular disease in the “preventive health domain” of the Shared Savings Program quality measure set. The final rule also clarifies how PQRS-eligible professionals participating within an Accountable Care Organization can meet reporting requirements.
On Twitter @legal_med
Officials at the Centers for Medicare & Medicaid Services have issued the final 2016 fee schedule for physicians, making modifications to the Physician Quality Reporting System (PQRS) and loosening requirements for its controversial two-midnight rule.
The fee schedule – the first since repeal of the Sustainable Growth Rate (SGR) formula and enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – includes changes to payment policies, modifications to misvalued codes, and updates to quality performance metrics under the PQRS, the Medicare Shared Savings Program, and Physician Compare, among others.
As part of the final fee schedule rule, released Oct. 30, CMS is relaxing its two-midnight rule to allow doctors greater flexibility when determining whether hospital stays are subject to the regulation.
For hospital stays for which physicians expect the patient will need less than two midnights of hospital care, an inpatient admission may still be payable under Medicare Part A on a case-by-case basis based on the admitting physician’s judgment, according to the final rule. Additionally, the agency does not plan to send recovery auditors after doctors suspected of violating the two-midnight rule. Instead, CMS plans to use Beneficiary and Family Centered Care Quality Improvement Organizations to conduct initial medical reviews of claims for short-stay inpatient admissions. The claim reviews will focus on educating physicians and hospitals about the policy for inpatient admissions.
Only physicians with questionable practice patterns, such as high rates of claims denial after medical review, will be referred to auditors, according to CMS.
“These changes continue CMS’ long-standing emphasis on the importance of a physician’s medical judgment in meeting the needs of Medicare beneficiaries,” CMS officials stated in a fact sheet.
CMS also finalized two new advance care planning codes that will pay physicians for time spent discussing patient options for advance directives. The first code will cover an initial 30 minutes of the physicians’ time, and the second code will cover additional 30-minute blocks as necessary.
The AMA Current Procedural Terminology (CPT) Editorial Panel and the AMA Relative Value Update Committee (RUC) created the new CPT codes and recommended the associated payments for calendar year 2015, but CMS delayed the codes’ enactment until collecting public comment.
Modifications to quality programs include a new reporting option under the PQRS that will allow group practices to report quality measure data using a Qualified Clinical Data Registry. In 2016, there will be 281 measures in the PQRS measure set and 18 measures in the Group Practice Reporting Option (GPRO) Web Interface, according to the final rule.
The 2018 payment adjustment will be the last adjustment under the PQRS. Starting in 2019, adjustments to payment for quality reporting and other factors will be made under the Merit-Based Incentive Payment System (MIPS), as required by MACRA.
Changes to the Value-Based Payment Modifier program are also coming in 2016:
• CMS will apply the quality-tiering methodology to all groups and solo practitioners that meet the criteria to avoid the downward adjustment under the PQRS. Groups and solo practitioners would be subject to upward, neutral, or downward adjustments derived under the quality-tiering methodology.
• CMS will continue to set the maximum upward adjustment under the quality-tiering methodology for the CY 2018 value modifier at four times an adjustment factor for groups of physicians with 10 or more eligible professionals, and two times an adjustment factor for groups of physicians with between two and nine eligible professionals and physician solo practitioners.
• CMS will use calendar year 2016 as the performance period for the calendar 2018 value modifier and continue to apply the 2018 value modifier based on participation in the PQRS by groups and solo practitioners.
The fee schedule also includes modifications to the Medicare Shared Savings Program including a new measure on statin therapy for the prevention and treatment of cardiovascular disease in the “preventive health domain” of the Shared Savings Program quality measure set. The final rule also clarifies how PQRS-eligible professionals participating within an Accountable Care Organization can meet reporting requirements.
On Twitter @legal_med
Officials at the Centers for Medicare & Medicaid Services have issued the final 2016 fee schedule for physicians, making modifications to the Physician Quality Reporting System (PQRS) and loosening requirements for its controversial two-midnight rule.
The fee schedule – the first since repeal of the Sustainable Growth Rate (SGR) formula and enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) – includes changes to payment policies, modifications to misvalued codes, and updates to quality performance metrics under the PQRS, the Medicare Shared Savings Program, and Physician Compare, among others.
As part of the final fee schedule rule, released Oct. 30, CMS is relaxing its two-midnight rule to allow doctors greater flexibility when determining whether hospital stays are subject to the regulation.
For hospital stays for which physicians expect the patient will need less than two midnights of hospital care, an inpatient admission may still be payable under Medicare Part A on a case-by-case basis based on the admitting physician’s judgment, according to the final rule. Additionally, the agency does not plan to send recovery auditors after doctors suspected of violating the two-midnight rule. Instead, CMS plans to use Beneficiary and Family Centered Care Quality Improvement Organizations to conduct initial medical reviews of claims for short-stay inpatient admissions. The claim reviews will focus on educating physicians and hospitals about the policy for inpatient admissions.
Only physicians with questionable practice patterns, such as high rates of claims denial after medical review, will be referred to auditors, according to CMS.
“These changes continue CMS’ long-standing emphasis on the importance of a physician’s medical judgment in meeting the needs of Medicare beneficiaries,” CMS officials stated in a fact sheet.
CMS also finalized two new advance care planning codes that will pay physicians for time spent discussing patient options for advance directives. The first code will cover an initial 30 minutes of the physicians’ time, and the second code will cover additional 30-minute blocks as necessary.
The AMA Current Procedural Terminology (CPT) Editorial Panel and the AMA Relative Value Update Committee (RUC) created the new CPT codes and recommended the associated payments for calendar year 2015, but CMS delayed the codes’ enactment until collecting public comment.
Modifications to quality programs include a new reporting option under the PQRS that will allow group practices to report quality measure data using a Qualified Clinical Data Registry. In 2016, there will be 281 measures in the PQRS measure set and 18 measures in the Group Practice Reporting Option (GPRO) Web Interface, according to the final rule.
The 2018 payment adjustment will be the last adjustment under the PQRS. Starting in 2019, adjustments to payment for quality reporting and other factors will be made under the Merit-Based Incentive Payment System (MIPS), as required by MACRA.
Changes to the Value-Based Payment Modifier program are also coming in 2016:
• CMS will apply the quality-tiering methodology to all groups and solo practitioners that meet the criteria to avoid the downward adjustment under the PQRS. Groups and solo practitioners would be subject to upward, neutral, or downward adjustments derived under the quality-tiering methodology.
• CMS will continue to set the maximum upward adjustment under the quality-tiering methodology for the CY 2018 value modifier at four times an adjustment factor for groups of physicians with 10 or more eligible professionals, and two times an adjustment factor for groups of physicians with between two and nine eligible professionals and physician solo practitioners.
• CMS will use calendar year 2016 as the performance period for the calendar 2018 value modifier and continue to apply the 2018 value modifier based on participation in the PQRS by groups and solo practitioners.
The fee schedule also includes modifications to the Medicare Shared Savings Program including a new measure on statin therapy for the prevention and treatment of cardiovascular disease in the “preventive health domain” of the Shared Savings Program quality measure set. The final rule also clarifies how PQRS-eligible professionals participating within an Accountable Care Organization can meet reporting requirements.
On Twitter @legal_med
Medicare auditors collected $2.4 billion in FY2014 overpayments
Recovery audit contractors working on behalf of the Centers for Medicare & Medicaid Services recovered $2.4 billion in overpayments to providers in 2014 and refunded $173 million in underpayments.
The total $2.6 billion in improper payments was 32% below program corrections in fiscal 2013, according to the CMS’ annual audit report to Congress published in October. Auditors in 2013 identified and corrected $3.8 billion in improper payments, including $3.7 billion in overpayments and $102 million in underpayments, according to the CMS’ 2013 report.
Nearly 50% of payment corrections in 2014 resulted from Region C, which covers southern states and some southwestern states, including Texas, Louisiana, Florida, Colorado, and New Mexico. Western states, (Region D) including California, Nevada, and Arizona, had the second highest payment corrections at 21%, followed by eastern states (16%) and Midwestern states (15%). The majority of improper payments resulted from Medicare Part A claims (96%), with 2% stemming from Medicare Part B claims and another 2% resulting from durable medical equipment claims.
Health care providers appealed 799,141 claims identified by the auditors in 2014, down from 836,849 appealed claims in 2013. Of the total claims appealed in 2014, 23% were overturned with decisions in the provider’s favor, an increase from 18% of provider-favorable decisions in 2013.
After the audit program’s administrative costs, underpayments paid to providers, and appeal reversals, the Medicare Recovery Audit Program returned approximately $1.6 billion to the Medicare Trust Funds in 2014. The CMS spent $461 million to operate the Recovery Audit Program, of which $275 million were contingency fees paid to Recovery Auditors. Administrative costs, such as processing appeals at the first two levels, adjusting claims, support contractors, and oversight of the program, accounted for $186 million.
CMS officials attribute the decrease in payment corrections in 2014 to limited reviews that took place during the close-out process of existing recovery auditor contracts. As the CMS completed its procurement process for the next round of recovery auditor contracts, the agency focused its resources on completing open reviews and prohibited the initiation of new complex reviews after February 2014, according to its annual report.
On Twitter @legal_med
Recovery audit contractors working on behalf of the Centers for Medicare & Medicaid Services recovered $2.4 billion in overpayments to providers in 2014 and refunded $173 million in underpayments.
The total $2.6 billion in improper payments was 32% below program corrections in fiscal 2013, according to the CMS’ annual audit report to Congress published in October. Auditors in 2013 identified and corrected $3.8 billion in improper payments, including $3.7 billion in overpayments and $102 million in underpayments, according to the CMS’ 2013 report.
Nearly 50% of payment corrections in 2014 resulted from Region C, which covers southern states and some southwestern states, including Texas, Louisiana, Florida, Colorado, and New Mexico. Western states, (Region D) including California, Nevada, and Arizona, had the second highest payment corrections at 21%, followed by eastern states (16%) and Midwestern states (15%). The majority of improper payments resulted from Medicare Part A claims (96%), with 2% stemming from Medicare Part B claims and another 2% resulting from durable medical equipment claims.
Health care providers appealed 799,141 claims identified by the auditors in 2014, down from 836,849 appealed claims in 2013. Of the total claims appealed in 2014, 23% were overturned with decisions in the provider’s favor, an increase from 18% of provider-favorable decisions in 2013.
After the audit program’s administrative costs, underpayments paid to providers, and appeal reversals, the Medicare Recovery Audit Program returned approximately $1.6 billion to the Medicare Trust Funds in 2014. The CMS spent $461 million to operate the Recovery Audit Program, of which $275 million were contingency fees paid to Recovery Auditors. Administrative costs, such as processing appeals at the first two levels, adjusting claims, support contractors, and oversight of the program, accounted for $186 million.
CMS officials attribute the decrease in payment corrections in 2014 to limited reviews that took place during the close-out process of existing recovery auditor contracts. As the CMS completed its procurement process for the next round of recovery auditor contracts, the agency focused its resources on completing open reviews and prohibited the initiation of new complex reviews after February 2014, according to its annual report.
On Twitter @legal_med
Recovery audit contractors working on behalf of the Centers for Medicare & Medicaid Services recovered $2.4 billion in overpayments to providers in 2014 and refunded $173 million in underpayments.
The total $2.6 billion in improper payments was 32% below program corrections in fiscal 2013, according to the CMS’ annual audit report to Congress published in October. Auditors in 2013 identified and corrected $3.8 billion in improper payments, including $3.7 billion in overpayments and $102 million in underpayments, according to the CMS’ 2013 report.
Nearly 50% of payment corrections in 2014 resulted from Region C, which covers southern states and some southwestern states, including Texas, Louisiana, Florida, Colorado, and New Mexico. Western states, (Region D) including California, Nevada, and Arizona, had the second highest payment corrections at 21%, followed by eastern states (16%) and Midwestern states (15%). The majority of improper payments resulted from Medicare Part A claims (96%), with 2% stemming from Medicare Part B claims and another 2% resulting from durable medical equipment claims.
Health care providers appealed 799,141 claims identified by the auditors in 2014, down from 836,849 appealed claims in 2013. Of the total claims appealed in 2014, 23% were overturned with decisions in the provider’s favor, an increase from 18% of provider-favorable decisions in 2013.
After the audit program’s administrative costs, underpayments paid to providers, and appeal reversals, the Medicare Recovery Audit Program returned approximately $1.6 billion to the Medicare Trust Funds in 2014. The CMS spent $461 million to operate the Recovery Audit Program, of which $275 million were contingency fees paid to Recovery Auditors. Administrative costs, such as processing appeals at the first two levels, adjusting claims, support contractors, and oversight of the program, accounted for $186 million.
CMS officials attribute the decrease in payment corrections in 2014 to limited reviews that took place during the close-out process of existing recovery auditor contracts. As the CMS completed its procurement process for the next round of recovery auditor contracts, the agency focused its resources on completing open reviews and prohibited the initiation of new complex reviews after February 2014, according to its annual report.
On Twitter @legal_med
ACA insurance networks lack specialist coverage
Nearly 15% of insurance plans for sale via healthcare.gov lack in-network physicians for at least one specialty, according to an analysis published Oct. 27 in JAMA. Endocrinologists, rheumatologists, and psychiatrists were most commonly excluded.
Stephen C. Dorner of Harvard T. H. Chan School of Public Health, Boston, and his colleagues examined physician networks in 34 states offering plans through the federal marketplace (healthcare.gov) during 2015 open enrollment. They searched plans’ online directories for in-network specialists in obstetrics/gynecology, dermatology, cardiology, psychiatry, oncology, neurology, endocrinology, rheumatology, and pulmonology. Searches were done for specialists within both 50 and 100 miles.
Of the 135 plans, 18 (13%) were specialist deficient in the 100-mile search, while 19 (14%) of plans lacked in-network specialists in the 50-mile search (JAMA. 2015;16:1749-50. doi. 101001/jama.2015.9375).
Patients in specialist-deficient plans had high out-of-network costs, Mr. Dorner and colleagues found. Of the 19 specialist-deficient plans, 5 did not cover out-of-network services, whereas 11 of the remaining 14 plans required cost-sharing of 50% or more. Nine of the 19 inadequate plans did not cover medications prescribed by out-of-network physicians.
The findings raise concerns about patient access to specialty care and suggest that a number of plans are violating network adequacy requirements, Mr. Dorner said, adding that such inadequate plans precipitate high out-of-pocket costs and may lead to adverse plan selection.
On Twitter @legal_med
Nearly 15% of insurance plans for sale via healthcare.gov lack in-network physicians for at least one specialty, according to an analysis published Oct. 27 in JAMA. Endocrinologists, rheumatologists, and psychiatrists were most commonly excluded.
Stephen C. Dorner of Harvard T. H. Chan School of Public Health, Boston, and his colleagues examined physician networks in 34 states offering plans through the federal marketplace (healthcare.gov) during 2015 open enrollment. They searched plans’ online directories for in-network specialists in obstetrics/gynecology, dermatology, cardiology, psychiatry, oncology, neurology, endocrinology, rheumatology, and pulmonology. Searches were done for specialists within both 50 and 100 miles.
Of the 135 plans, 18 (13%) were specialist deficient in the 100-mile search, while 19 (14%) of plans lacked in-network specialists in the 50-mile search (JAMA. 2015;16:1749-50. doi. 101001/jama.2015.9375).
Patients in specialist-deficient plans had high out-of-network costs, Mr. Dorner and colleagues found. Of the 19 specialist-deficient plans, 5 did not cover out-of-network services, whereas 11 of the remaining 14 plans required cost-sharing of 50% or more. Nine of the 19 inadequate plans did not cover medications prescribed by out-of-network physicians.
The findings raise concerns about patient access to specialty care and suggest that a number of plans are violating network adequacy requirements, Mr. Dorner said, adding that such inadequate plans precipitate high out-of-pocket costs and may lead to adverse plan selection.
On Twitter @legal_med
Nearly 15% of insurance plans for sale via healthcare.gov lack in-network physicians for at least one specialty, according to an analysis published Oct. 27 in JAMA. Endocrinologists, rheumatologists, and psychiatrists were most commonly excluded.
Stephen C. Dorner of Harvard T. H. Chan School of Public Health, Boston, and his colleagues examined physician networks in 34 states offering plans through the federal marketplace (healthcare.gov) during 2015 open enrollment. They searched plans’ online directories for in-network specialists in obstetrics/gynecology, dermatology, cardiology, psychiatry, oncology, neurology, endocrinology, rheumatology, and pulmonology. Searches were done for specialists within both 50 and 100 miles.
Of the 135 plans, 18 (13%) were specialist deficient in the 100-mile search, while 19 (14%) of plans lacked in-network specialists in the 50-mile search (JAMA. 2015;16:1749-50. doi. 101001/jama.2015.9375).
Patients in specialist-deficient plans had high out-of-network costs, Mr. Dorner and colleagues found. Of the 19 specialist-deficient plans, 5 did not cover out-of-network services, whereas 11 of the remaining 14 plans required cost-sharing of 50% or more. Nine of the 19 inadequate plans did not cover medications prescribed by out-of-network physicians.
The findings raise concerns about patient access to specialty care and suggest that a number of plans are violating network adequacy requirements, Mr. Dorner said, adding that such inadequate plans precipitate high out-of-pocket costs and may lead to adverse plan selection.
On Twitter @legal_med
FROM JAMA
Key clinical point: Many patients who buy insurance via healthcare.gov are not getting access to specialists’ care.
Major finding: In a study of 135 federal marketplace insurance plans, nearly 15% lacked in-network physicians for at least one specialty. Of 34 states, 9 had at least one specialist-deficient plan.
Data source: Review of physician networks listed on insurance plans for sale via healthcare.gov in April 2015.
Disclosures: No relevant financial disclosures were reported.
Malpractice Premiums Flat in 2015, but Changes Could Be Ahead
Physicians paid about the same in liability insurance premiums in 2015 as in 2014, and analysts don’t see costs changing anytime soon. A nationwide survey of insurers by the Medical Liability Monitor shows that 71% of insurance premiums did not change this year, while 17% of rates rose and 12% fell.
Internists experienced an average premium increase of 0.6% in 2015, while general surgeons saw a 0.2% average rate decrease, and ob.gyns experienced an average 0.5% rate increase.
The static premium market is being largely driven by the low number of lawsuits filed by patients and family members in recent years, said survey coauthor Paul Greve Jr., executive vice president/senior consultant for the Willis Health Care Practice, a global risk management consultant firm.
“It’s amazing to see the continuing stability in claim frequency,” Mr. Greve said in an interview. “The claims counts are just not rising. Its great for the industry, and it’s great for physicians, but it is puzzling because you wonder what has caused what amounts to a sea change in the attitudes of the general public toward malpractice litigation such that the claim counts were drop off.”
Premiums continue to vary geographically. Southern Florida internists for example, will pay $47,707 for malpractice insurance this year, while their counterparts in Minnesota will pay $3,375. For ob.gyns., premiums range from $214,999 in southern New York to $16,240 in central California. General surgeons in Southern Florida will pay $190,829 this year, while Wisconsin surgeons will pay $10,868.
Various factors influence premium amounts, including the overall legal climate and the rate of insurer competition in each state, said Susan J. Forray, principal and consulting actuary with the Milwaukee office of Milliman, a global provider of actuarial services.
“The dollar amounts themselves are a function of the litigation environment [and] the cost level of medicine or living within the state,” Ms. Forray said in an interview. “In terms of rate changes, we are seeing certain environments where there is more competition. Obviously, those more competitive markets are more likely to have rate decreases or perhaps, stable rates, where perhaps markets with less competition are more likely to see increased rates.”
On a regional basis, Southern physicians experienced the largest rate increases, while doctors in the Northeast, West, and Midwest continued to see decreases. The Midwest’s 0.8% rate decrease was the largest decline, while Western states experienced a 0.2% average rate decrease. On average, the South showed a rate increase of 0.9% and the Northeast experienced a 0.1% average decrease. Doctors in Georgia, North Carolina, and Texas saw rate increases in excess of 5%, while Iowa physicians experienced an 11% rate decrease. Only three western states experienced rate increases: New Mexico at 2.5%, Oregon at 2%, and Idaho at 1%. Premium changes for Northeastern doctors fluctuated from Rhode Island’s 7% increase to Pennsylvania’s 8% decrease. Additionally, for the first time in 8 years, the premium market experienced an average overall increase of 0.3% in 2015, compared with an average overall decrease of 1.5% last year.
The jury is still out on how the Affordable Care Act and other health reforms will impact the malpractice premium market, according to Mr. Greve. He said that he believes the majority of upcoming health reforms will improve patient safety, thus reducing liability for doctors. However, as more physicians become part of larger networks to deliver new models of care, their contractual liability spreads, he said. However, as value-based care becomes the law of the land, new claims could arise.
“We’re just beginning to see the tip of the iceberg here,” Mr. Greve said. “In the past, it was overutilization, [the claim] that you did something in order to put money in your pocket. With putting providers at financial risk with capitated or bundled payments or global payments, then the argument is going to be, ‘You didn’t deliver enough care,’ or ‘You [used that device] because it was less expensive.’ ”
The MLM survey, published yearly in October, gathered July 1 premium data from the major malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
Physicians paid about the same in liability insurance premiums in 2015 as in 2014, and analysts don’t see costs changing anytime soon. A nationwide survey of insurers by the Medical Liability Monitor shows that 71% of insurance premiums did not change this year, while 17% of rates rose and 12% fell.
Internists experienced an average premium increase of 0.6% in 2015, while general surgeons saw a 0.2% average rate decrease, and ob.gyns experienced an average 0.5% rate increase.
The static premium market is being largely driven by the low number of lawsuits filed by patients and family members in recent years, said survey coauthor Paul Greve Jr., executive vice president/senior consultant for the Willis Health Care Practice, a global risk management consultant firm.
“It’s amazing to see the continuing stability in claim frequency,” Mr. Greve said in an interview. “The claims counts are just not rising. Its great for the industry, and it’s great for physicians, but it is puzzling because you wonder what has caused what amounts to a sea change in the attitudes of the general public toward malpractice litigation such that the claim counts were drop off.”
Premiums continue to vary geographically. Southern Florida internists for example, will pay $47,707 for malpractice insurance this year, while their counterparts in Minnesota will pay $3,375. For ob.gyns., premiums range from $214,999 in southern New York to $16,240 in central California. General surgeons in Southern Florida will pay $190,829 this year, while Wisconsin surgeons will pay $10,868.
Various factors influence premium amounts, including the overall legal climate and the rate of insurer competition in each state, said Susan J. Forray, principal and consulting actuary with the Milwaukee office of Milliman, a global provider of actuarial services.
“The dollar amounts themselves are a function of the litigation environment [and] the cost level of medicine or living within the state,” Ms. Forray said in an interview. “In terms of rate changes, we are seeing certain environments where there is more competition. Obviously, those more competitive markets are more likely to have rate decreases or perhaps, stable rates, where perhaps markets with less competition are more likely to see increased rates.”
On a regional basis, Southern physicians experienced the largest rate increases, while doctors in the Northeast, West, and Midwest continued to see decreases. The Midwest’s 0.8% rate decrease was the largest decline, while Western states experienced a 0.2% average rate decrease. On average, the South showed a rate increase of 0.9% and the Northeast experienced a 0.1% average decrease. Doctors in Georgia, North Carolina, and Texas saw rate increases in excess of 5%, while Iowa physicians experienced an 11% rate decrease. Only three western states experienced rate increases: New Mexico at 2.5%, Oregon at 2%, and Idaho at 1%. Premium changes for Northeastern doctors fluctuated from Rhode Island’s 7% increase to Pennsylvania’s 8% decrease. Additionally, for the first time in 8 years, the premium market experienced an average overall increase of 0.3% in 2015, compared with an average overall decrease of 1.5% last year.
The jury is still out on how the Affordable Care Act and other health reforms will impact the malpractice premium market, according to Mr. Greve. He said that he believes the majority of upcoming health reforms will improve patient safety, thus reducing liability for doctors. However, as more physicians become part of larger networks to deliver new models of care, their contractual liability spreads, he said. However, as value-based care becomes the law of the land, new claims could arise.
“We’re just beginning to see the tip of the iceberg here,” Mr. Greve said. “In the past, it was overutilization, [the claim] that you did something in order to put money in your pocket. With putting providers at financial risk with capitated or bundled payments or global payments, then the argument is going to be, ‘You didn’t deliver enough care,’ or ‘You [used that device] because it was less expensive.’ ”
The MLM survey, published yearly in October, gathered July 1 premium data from the major malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
Physicians paid about the same in liability insurance premiums in 2015 as in 2014, and analysts don’t see costs changing anytime soon. A nationwide survey of insurers by the Medical Liability Monitor shows that 71% of insurance premiums did not change this year, while 17% of rates rose and 12% fell.
Internists experienced an average premium increase of 0.6% in 2015, while general surgeons saw a 0.2% average rate decrease, and ob.gyns experienced an average 0.5% rate increase.
The static premium market is being largely driven by the low number of lawsuits filed by patients and family members in recent years, said survey coauthor Paul Greve Jr., executive vice president/senior consultant for the Willis Health Care Practice, a global risk management consultant firm.
“It’s amazing to see the continuing stability in claim frequency,” Mr. Greve said in an interview. “The claims counts are just not rising. Its great for the industry, and it’s great for physicians, but it is puzzling because you wonder what has caused what amounts to a sea change in the attitudes of the general public toward malpractice litigation such that the claim counts were drop off.”
Premiums continue to vary geographically. Southern Florida internists for example, will pay $47,707 for malpractice insurance this year, while their counterparts in Minnesota will pay $3,375. For ob.gyns., premiums range from $214,999 in southern New York to $16,240 in central California. General surgeons in Southern Florida will pay $190,829 this year, while Wisconsin surgeons will pay $10,868.
Various factors influence premium amounts, including the overall legal climate and the rate of insurer competition in each state, said Susan J. Forray, principal and consulting actuary with the Milwaukee office of Milliman, a global provider of actuarial services.
“The dollar amounts themselves are a function of the litigation environment [and] the cost level of medicine or living within the state,” Ms. Forray said in an interview. “In terms of rate changes, we are seeing certain environments where there is more competition. Obviously, those more competitive markets are more likely to have rate decreases or perhaps, stable rates, where perhaps markets with less competition are more likely to see increased rates.”
On a regional basis, Southern physicians experienced the largest rate increases, while doctors in the Northeast, West, and Midwest continued to see decreases. The Midwest’s 0.8% rate decrease was the largest decline, while Western states experienced a 0.2% average rate decrease. On average, the South showed a rate increase of 0.9% and the Northeast experienced a 0.1% average decrease. Doctors in Georgia, North Carolina, and Texas saw rate increases in excess of 5%, while Iowa physicians experienced an 11% rate decrease. Only three western states experienced rate increases: New Mexico at 2.5%, Oregon at 2%, and Idaho at 1%. Premium changes for Northeastern doctors fluctuated from Rhode Island’s 7% increase to Pennsylvania’s 8% decrease. Additionally, for the first time in 8 years, the premium market experienced an average overall increase of 0.3% in 2015, compared with an average overall decrease of 1.5% last year.
The jury is still out on how the Affordable Care Act and other health reforms will impact the malpractice premium market, according to Mr. Greve. He said that he believes the majority of upcoming health reforms will improve patient safety, thus reducing liability for doctors. However, as more physicians become part of larger networks to deliver new models of care, their contractual liability spreads, he said. However, as value-based care becomes the law of the land, new claims could arise.
“We’re just beginning to see the tip of the iceberg here,” Mr. Greve said. “In the past, it was overutilization, [the claim] that you did something in order to put money in your pocket. With putting providers at financial risk with capitated or bundled payments or global payments, then the argument is going to be, ‘You didn’t deliver enough care,’ or ‘You [used that device] because it was less expensive.’ ”
The MLM survey, published yearly in October, gathered July 1 premium data from the major malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
Malpractice premiums flat in 2015, but changes could be ahead
Physicians paid about the same in liability insurance premiums in 2015 as in 2014, and analysts don’t see costs changing anytime soon. A nationwide survey of insurers by the Medical Liability Monitor shows that 71% of insurance premiums did not change this year, while 17% of rates rose and 12% fell.
Internists experienced an average premium increase of 0.6% in 2015, while general surgeons saw a 0.2% average rate decrease, and ob.gyns experienced an average 0.5% rate increase.
The static premium market is being largely driven by the low number of lawsuits filed by patients and family members in recent years, said survey coauthor Paul Greve Jr., executive vice president/senior consultant for the Willis Health Care Practice, a global risk management consultant firm.
“It’s amazing to see the continuing stability in claim frequency,” Mr. Greve said in an interview. “The claims counts are just not rising. Its great for the industry, and it’s great for physicians, but it is puzzling because you wonder what has caused what amounts to a sea change in the attitudes of the general public toward malpractice litigation such that the claim counts were drop off.”
Premiums continue to vary geographically. Southern Florida internists for example, will pay $47,707 for malpractice insurance this year, while their counterparts in Minnesota will pay $3,375. For ob.gyns., premiums range from $214,999 in southern New York to $16,240 in central California. General surgeons in Southern Florida will pay $190,829 this year, while Wisconsin surgeons will pay $10,868.
Various factors influence premium amounts, including the overall legal climate and the rate of insurer competition in each state, said Susan J. Forray, principal and consulting actuary with the Milwaukee office of Milliman, a global provider of actuarial services.
“The dollar amounts themselves are a function of the litigation environment [and] the cost level of medicine or living within the state,” Ms. Forray said in an interview. “In terms of rate changes, we are seeing certain environments where there is more competition. Obviously, those more competitive markets are more likely to have rate decreases or perhaps, stable rates, where perhaps markets with less competition are more likely to see increased rates.”
On a regional basis, Southern physicians experienced the largest rate increases, while doctors in the Northeast, West, and Midwest continued to see decreases. The Midwest’s 0.8% rate decrease was the largest decline, while Western states experienced a 0.2% average rate decrease. On average, the South showed a rate increase of 0.9% and the Northeast experienced a 0.1% average decrease. Doctors in Georgia, North Carolina, and Texas saw rate increases in excess of 5%, while Iowa physicians experienced an 11% rate decrease. Only three western states experienced rate increases: New Mexico at 2.5%, Oregon at 2%, and Idaho at 1%. Premium changes for Northeastern doctors fluctuated from Rhode Island’s 7% increase to Pennsylvania’s 8% decrease. Additionally, for the first time in 8 years, the premium market experienced an average overall increase of 0.3% in 2015, compared with an average overall decrease of 1.5% last year.
The jury is still out on how the Affordable Care Act and other health reforms will impact the malpractice premium market, according to Mr. Greve. He said that he believes the majority of upcoming health reforms will improve patient safety, thus reducing liability for doctors. However, as more physicians become part of larger networks to deliver new models of care, their contractual liability spreads, he said. However, as value-based care becomes the law of the land, new claims could arise.
“We’re just beginning to see the tip of the iceberg here,” Mr. Greve said. “In the past, it was overutilization, [the claim] that you did something in order to put money in your pocket. With putting providers at financial risk with capitated or bundled payments or global payments, then the argument is going to be, ‘You didn’t deliver enough care,’ or ‘You [used that device] because it was less expensive.’ ”
The MLM survey, published yearly in October, gathered July 1 premium data from the major malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Physicians paid about the same in liability insurance premiums in 2015 as in 2014, and analysts don’t see costs changing anytime soon. A nationwide survey of insurers by the Medical Liability Monitor shows that 71% of insurance premiums did not change this year, while 17% of rates rose and 12% fell.
Internists experienced an average premium increase of 0.6% in 2015, while general surgeons saw a 0.2% average rate decrease, and ob.gyns experienced an average 0.5% rate increase.
The static premium market is being largely driven by the low number of lawsuits filed by patients and family members in recent years, said survey coauthor Paul Greve Jr., executive vice president/senior consultant for the Willis Health Care Practice, a global risk management consultant firm.
“It’s amazing to see the continuing stability in claim frequency,” Mr. Greve said in an interview. “The claims counts are just not rising. Its great for the industry, and it’s great for physicians, but it is puzzling because you wonder what has caused what amounts to a sea change in the attitudes of the general public toward malpractice litigation such that the claim counts were drop off.”
Premiums continue to vary geographically. Southern Florida internists for example, will pay $47,707 for malpractice insurance this year, while their counterparts in Minnesota will pay $3,375. For ob.gyns., premiums range from $214,999 in southern New York to $16,240 in central California. General surgeons in Southern Florida will pay $190,829 this year, while Wisconsin surgeons will pay $10,868.
Various factors influence premium amounts, including the overall legal climate and the rate of insurer competition in each state, said Susan J. Forray, principal and consulting actuary with the Milwaukee office of Milliman, a global provider of actuarial services.
“The dollar amounts themselves are a function of the litigation environment [and] the cost level of medicine or living within the state,” Ms. Forray said in an interview. “In terms of rate changes, we are seeing certain environments where there is more competition. Obviously, those more competitive markets are more likely to have rate decreases or perhaps, stable rates, where perhaps markets with less competition are more likely to see increased rates.”
On a regional basis, Southern physicians experienced the largest rate increases, while doctors in the Northeast, West, and Midwest continued to see decreases. The Midwest’s 0.8% rate decrease was the largest decline, while Western states experienced a 0.2% average rate decrease. On average, the South showed a rate increase of 0.9% and the Northeast experienced a 0.1% average decrease. Doctors in Georgia, North Carolina, and Texas saw rate increases in excess of 5%, while Iowa physicians experienced an 11% rate decrease. Only three western states experienced rate increases: New Mexico at 2.5%, Oregon at 2%, and Idaho at 1%. Premium changes for Northeastern doctors fluctuated from Rhode Island’s 7% increase to Pennsylvania’s 8% decrease. Additionally, for the first time in 8 years, the premium market experienced an average overall increase of 0.3% in 2015, compared with an average overall decrease of 1.5% last year.
The jury is still out on how the Affordable Care Act and other health reforms will impact the malpractice premium market, according to Mr. Greve. He said that he believes the majority of upcoming health reforms will improve patient safety, thus reducing liability for doctors. However, as more physicians become part of larger networks to deliver new models of care, their contractual liability spreads, he said. However, as value-based care becomes the law of the land, new claims could arise.
“We’re just beginning to see the tip of the iceberg here,” Mr. Greve said. “In the past, it was overutilization, [the claim] that you did something in order to put money in your pocket. With putting providers at financial risk with capitated or bundled payments or global payments, then the argument is going to be, ‘You didn’t deliver enough care,’ or ‘You [used that device] because it was less expensive.’ ”
The MLM survey, published yearly in October, gathered July 1 premium data from the major malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Physicians paid about the same in liability insurance premiums in 2015 as in 2014, and analysts don’t see costs changing anytime soon. A nationwide survey of insurers by the Medical Liability Monitor shows that 71% of insurance premiums did not change this year, while 17% of rates rose and 12% fell.
Internists experienced an average premium increase of 0.6% in 2015, while general surgeons saw a 0.2% average rate decrease, and ob.gyns experienced an average 0.5% rate increase.
The static premium market is being largely driven by the low number of lawsuits filed by patients and family members in recent years, said survey coauthor Paul Greve Jr., executive vice president/senior consultant for the Willis Health Care Practice, a global risk management consultant firm.
“It’s amazing to see the continuing stability in claim frequency,” Mr. Greve said in an interview. “The claims counts are just not rising. Its great for the industry, and it’s great for physicians, but it is puzzling because you wonder what has caused what amounts to a sea change in the attitudes of the general public toward malpractice litigation such that the claim counts were drop off.”
Premiums continue to vary geographically. Southern Florida internists for example, will pay $47,707 for malpractice insurance this year, while their counterparts in Minnesota will pay $3,375. For ob.gyns., premiums range from $214,999 in southern New York to $16,240 in central California. General surgeons in Southern Florida will pay $190,829 this year, while Wisconsin surgeons will pay $10,868.
Various factors influence premium amounts, including the overall legal climate and the rate of insurer competition in each state, said Susan J. Forray, principal and consulting actuary with the Milwaukee office of Milliman, a global provider of actuarial services.
“The dollar amounts themselves are a function of the litigation environment [and] the cost level of medicine or living within the state,” Ms. Forray said in an interview. “In terms of rate changes, we are seeing certain environments where there is more competition. Obviously, those more competitive markets are more likely to have rate decreases or perhaps, stable rates, where perhaps markets with less competition are more likely to see increased rates.”
On a regional basis, Southern physicians experienced the largest rate increases, while doctors in the Northeast, West, and Midwest continued to see decreases. The Midwest’s 0.8% rate decrease was the largest decline, while Western states experienced a 0.2% average rate decrease. On average, the South showed a rate increase of 0.9% and the Northeast experienced a 0.1% average decrease. Doctors in Georgia, North Carolina, and Texas saw rate increases in excess of 5%, while Iowa physicians experienced an 11% rate decrease. Only three western states experienced rate increases: New Mexico at 2.5%, Oregon at 2%, and Idaho at 1%. Premium changes for Northeastern doctors fluctuated from Rhode Island’s 7% increase to Pennsylvania’s 8% decrease. Additionally, for the first time in 8 years, the premium market experienced an average overall increase of 0.3% in 2015, compared with an average overall decrease of 1.5% last year.
The jury is still out on how the Affordable Care Act and other health reforms will impact the malpractice premium market, according to Mr. Greve. He said that he believes the majority of upcoming health reforms will improve patient safety, thus reducing liability for doctors. However, as more physicians become part of larger networks to deliver new models of care, their contractual liability spreads, he said. However, as value-based care becomes the law of the land, new claims could arise.
“We’re just beginning to see the tip of the iceberg here,” Mr. Greve said. “In the past, it was overutilization, [the claim] that you did something in order to put money in your pocket. With putting providers at financial risk with capitated or bundled payments or global payments, then the argument is going to be, ‘You didn’t deliver enough care,’ or ‘You [used that device] because it was less expensive.’ ”
The MLM survey, published yearly in October, gathered July 1 premium data from the major malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
On Twitter @legal_med
Delayed diagnosis tops breast cancer malpractice claims
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
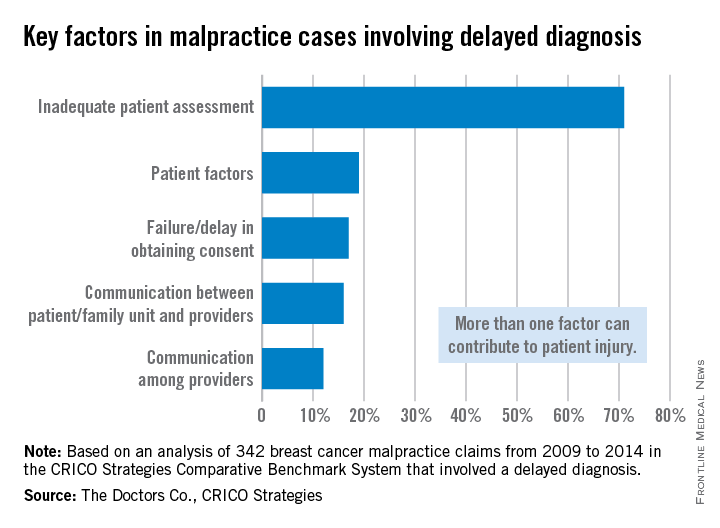
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
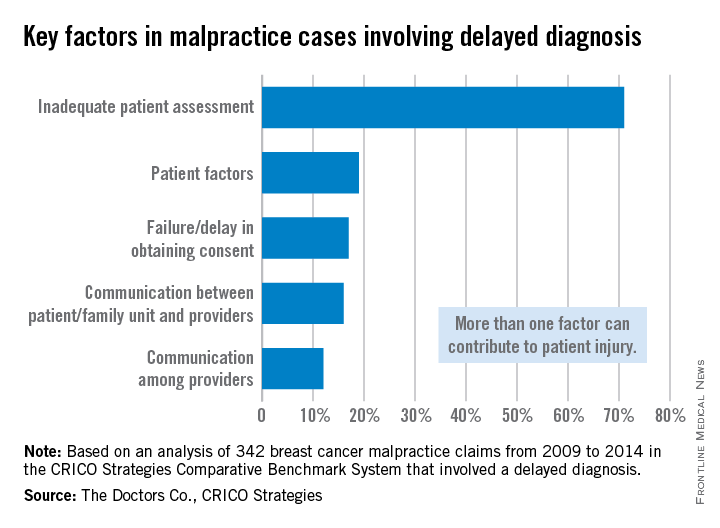
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med
The majority of medical malpractice lawsuits involving breast cancer result from delayed-diagnosis allegations, but a significant portion also stem from alleged poor management of breast cancer patients, a study showed.
In a review of 562 breast cancer malpractice claims from 2009 to 2014, 61% related to alleged delays in diagnosing breast cancer, and 39% stemmed from purported negligent treatment of patients, according to a joint analysis by medical liability insurers the Doctors Co. and CRICO.
“It was a big surprise to us to see that almost 40% of our cases involved patients who had already been diagnosed and were already receiving treatment,” said study coauthor Darrell Ranum, vice president of patient safety and risk management for the Doctors Co. “Breast cancer has been studied primarily from the angle of the diagnosis issues. We looked at our data, and we discovered there [was] really another very sizable bucket of claims involving breast cancer cases that involved treatment and management of breast cancer.”
The Doctors Co. and CRICO Strategies, a division of CRICO, pooled their databases of claims to conduct the study. Of the 562 breast cancer cases identified, 342 related to alleged delays in diagnosis, and 220 involved the management of breast cancer patients.
Nearly half of the delayed-diagnosis cases involved radiology (48%). But cases involving radiology did not necessarily result from a radiologist’s negligence. In some cases, primary care physicians or other clinicians may have misread or misinterpreted a radiologist’s report, Mr. Ranum said.
Physician offices/clinical care settings accounted for 39% of the delayed-diagnosis cases with family medicine and gynecology being the most common office settings in which cases originated. Common contributing factors to delayed-diagnosis lawsuits were inadequate patient assessment, such as misinterpretation of diagnostic studies. Delay in ordering diagnostic tests or failure to order them also topped contributing factors.
The vast majority of patients who had a delayed diagnosis of breast cancer were seriously harmed, with 70% of cases resulting in very severe outcomes, including 43 patient deaths, according to the report.
Of the 220 breast cancer management claims, 42% were surgery-related allegations. Patients often claimed poor performance of the initial surgery to remove a malignancy, or negligent performance of subsequent surgeries to reconstruct the breast, the study found.
Additional surgical allegations related to patient dissatisfaction with preoperative or postoperative management. The remaining nonsurgical cases related to medication management and minor procedures during the treatment course. The outcome of breast cancer claims involving surgical treatment were primarily of medium severity, with outcomes such as postoperative hematomas, injury to adjacent organs, and postoperative infections.
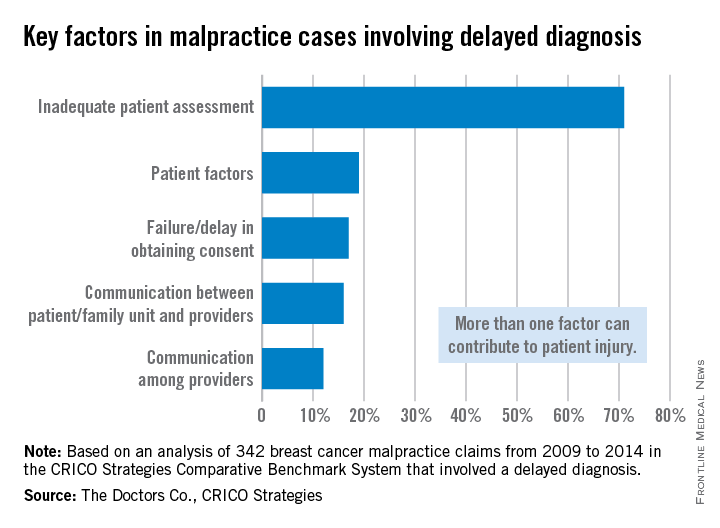
The analysis highlights opportunities for physicians to improve their care of breast cancer patients, both in the timely diagnosis of the disease and the ongoing management of care, Mr. Ranum said. He stressed that obtaining a timely and accurate diagnosis, including a complete history and interpretation of diagnostic studies, is critical. Equally important is the ongoing management of patients once an accurate diagnosis is made. Physicians should also implement processes, including documentation forms, that support and assist clinicians in providing a comprehensive informed consent process and better alignment of patients’ expectations.
“Systems need to be in place and systems need to be tested to make sure they don’t fail so that the information gets to where it needs to go,” Mr. Ranum said. “Our hope is that physicians will take a look at their own internal processes and track a patient from the time the physician says, ‘We need for you to have a mammogram,’ all the way through every step in that process.”
On Twitter @legal_med























