User login
Senate bill aims to expand Medicare telehealth
A bipartisan bill aims to expand Medicare coverage of telehealth services and remote patient monitoring.
The Creating Opportunities Now for Necessary and Effective Care Technologies (CONNECT) for Health Act (S.2484), introduced Feb. 3, would increase remote patient monitoring (RPM) for certain patients with chronic conditions and bolster telehealth usage in rural and community health clinics, according to backers of the bill. The legislation would also make telehealth and RPM benefits available in the Medicare Advantage program and establish a program to help physicians meet value-based care goals under the Medicare Access and CHIP Reauthorization Act (MACRA).
“Greater use of technology to connect patients and doctors will benefit both with better outcomes, as well as more timely and efficient use of resources,” cosponsor Sen. Ben Cardin (D-Md.) said in a statement. “We have the technology today to promote the delivery of high-quality care in an efficient and cost-effective way around the country. I’m proud to work with my colleagues on this strong bipartisan effort to expand telehealth and remote patient monitoring services.”
The bill seeks to undo current Medicare restrictions on how and where telehealth services can be used. Medicare patients currently are eligible for telehealth services only if they present from a rural health professional shortage area (HPSA) outside of a metropolitan statistical area (MSA) or in a rural census tract. The Centers for Medicare & Medicaid Services also limits reimbursable telehealth codes and restricts telehealth usage to Medicare-defined physicians.
If enacted, the legislation would allow telehealth and RPM to be used by qualifying participants in alternative payment models without such restrictions. The bill would also enable telehealth to be practiced at originated sites such as telestroke evaluation and management sites, Native American health service facilities, and dialysis facilities for home dialysis patients.
A 2015 analysis of the bill’s primary provisions by Avalere Health found the new policies would save the federal government $1.8 billion over a period of 10 years.
The legislation is supported by medical associations including the American Medical Association, the American Academy of Neurology, the American Osteopathic Association, and the American Heart Association.
“The AMA is pleased to support legislation that would accelerate the adoption of health care delivery models that promote coordinated and patient-centered care,” said AMA President Steven J. Stack said in a statement. “This bill would ensure that patients and their physicians are able to use new technologies that remove barriers to timely quality care. Importantly, the bill would maintain high standards whether a patient is seeing a physician in an office or via telemedicine.”
Jonathan Linkous, CEO of the American Telemedicine Association, called the legislation a necessary move to increase quality health care options and availability and expand telemedicine in Medicare.
“We are proud to support legislation that promotes health care delivery models in the interest of both the patient and the physician,” Mr. Linkous said in a statement. “Telehealth services widen the pool of health care options while enabling physicians to treat even more patients. This bill would bring us a step closer to the best health care quality and outcomes.”
The bill has been referred to the Senate Finance Committee and had five cosponsors at press time. No companion bill has been introduced in the House.
On Twitter @legal_med
A bipartisan bill aims to expand Medicare coverage of telehealth services and remote patient monitoring.
The Creating Opportunities Now for Necessary and Effective Care Technologies (CONNECT) for Health Act (S.2484), introduced Feb. 3, would increase remote patient monitoring (RPM) for certain patients with chronic conditions and bolster telehealth usage in rural and community health clinics, according to backers of the bill. The legislation would also make telehealth and RPM benefits available in the Medicare Advantage program and establish a program to help physicians meet value-based care goals under the Medicare Access and CHIP Reauthorization Act (MACRA).
“Greater use of technology to connect patients and doctors will benefit both with better outcomes, as well as more timely and efficient use of resources,” cosponsor Sen. Ben Cardin (D-Md.) said in a statement. “We have the technology today to promote the delivery of high-quality care in an efficient and cost-effective way around the country. I’m proud to work with my colleagues on this strong bipartisan effort to expand telehealth and remote patient monitoring services.”
The bill seeks to undo current Medicare restrictions on how and where telehealth services can be used. Medicare patients currently are eligible for telehealth services only if they present from a rural health professional shortage area (HPSA) outside of a metropolitan statistical area (MSA) or in a rural census tract. The Centers for Medicare & Medicaid Services also limits reimbursable telehealth codes and restricts telehealth usage to Medicare-defined physicians.
If enacted, the legislation would allow telehealth and RPM to be used by qualifying participants in alternative payment models without such restrictions. The bill would also enable telehealth to be practiced at originated sites such as telestroke evaluation and management sites, Native American health service facilities, and dialysis facilities for home dialysis patients.
A 2015 analysis of the bill’s primary provisions by Avalere Health found the new policies would save the federal government $1.8 billion over a period of 10 years.
The legislation is supported by medical associations including the American Medical Association, the American Academy of Neurology, the American Osteopathic Association, and the American Heart Association.
“The AMA is pleased to support legislation that would accelerate the adoption of health care delivery models that promote coordinated and patient-centered care,” said AMA President Steven J. Stack said in a statement. “This bill would ensure that patients and their physicians are able to use new technologies that remove barriers to timely quality care. Importantly, the bill would maintain high standards whether a patient is seeing a physician in an office or via telemedicine.”
Jonathan Linkous, CEO of the American Telemedicine Association, called the legislation a necessary move to increase quality health care options and availability and expand telemedicine in Medicare.
“We are proud to support legislation that promotes health care delivery models in the interest of both the patient and the physician,” Mr. Linkous said in a statement. “Telehealth services widen the pool of health care options while enabling physicians to treat even more patients. This bill would bring us a step closer to the best health care quality and outcomes.”
The bill has been referred to the Senate Finance Committee and had five cosponsors at press time. No companion bill has been introduced in the House.
On Twitter @legal_med
A bipartisan bill aims to expand Medicare coverage of telehealth services and remote patient monitoring.
The Creating Opportunities Now for Necessary and Effective Care Technologies (CONNECT) for Health Act (S.2484), introduced Feb. 3, would increase remote patient monitoring (RPM) for certain patients with chronic conditions and bolster telehealth usage in rural and community health clinics, according to backers of the bill. The legislation would also make telehealth and RPM benefits available in the Medicare Advantage program and establish a program to help physicians meet value-based care goals under the Medicare Access and CHIP Reauthorization Act (MACRA).
“Greater use of technology to connect patients and doctors will benefit both with better outcomes, as well as more timely and efficient use of resources,” cosponsor Sen. Ben Cardin (D-Md.) said in a statement. “We have the technology today to promote the delivery of high-quality care in an efficient and cost-effective way around the country. I’m proud to work with my colleagues on this strong bipartisan effort to expand telehealth and remote patient monitoring services.”
The bill seeks to undo current Medicare restrictions on how and where telehealth services can be used. Medicare patients currently are eligible for telehealth services only if they present from a rural health professional shortage area (HPSA) outside of a metropolitan statistical area (MSA) or in a rural census tract. The Centers for Medicare & Medicaid Services also limits reimbursable telehealth codes and restricts telehealth usage to Medicare-defined physicians.
If enacted, the legislation would allow telehealth and RPM to be used by qualifying participants in alternative payment models without such restrictions. The bill would also enable telehealth to be practiced at originated sites such as telestroke evaluation and management sites, Native American health service facilities, and dialysis facilities for home dialysis patients.
A 2015 analysis of the bill’s primary provisions by Avalere Health found the new policies would save the federal government $1.8 billion over a period of 10 years.
The legislation is supported by medical associations including the American Medical Association, the American Academy of Neurology, the American Osteopathic Association, and the American Heart Association.
“The AMA is pleased to support legislation that would accelerate the adoption of health care delivery models that promote coordinated and patient-centered care,” said AMA President Steven J. Stack said in a statement. “This bill would ensure that patients and their physicians are able to use new technologies that remove barriers to timely quality care. Importantly, the bill would maintain high standards whether a patient is seeing a physician in an office or via telemedicine.”
Jonathan Linkous, CEO of the American Telemedicine Association, called the legislation a necessary move to increase quality health care options and availability and expand telemedicine in Medicare.
“We are proud to support legislation that promotes health care delivery models in the interest of both the patient and the physician,” Mr. Linkous said in a statement. “Telehealth services widen the pool of health care options while enabling physicians to treat even more patients. This bill would bring us a step closer to the best health care quality and outcomes.”
The bill has been referred to the Senate Finance Committee and had five cosponsors at press time. No companion bill has been introduced in the House.
On Twitter @legal_med
More ob.gyns. find their niche as subspecialists
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
After 12 years as a private practice ob.gyn., Dr. Brigid McCue was beginning to feel overwhelmed. She loved her work, but keeping up with the kaleidoscope of care components and ever-changing clinical developments was daunting.
“I felt like it was hard to stay really good at all the different aspects of care,” Dr. McCue said. “I was doing fine with obstetrics, and I felt like I was managing my office well, but it’s hard to stay on top of the latest developments, especially in surgical areas. The other thing that was really hard to keep up with was the business aspect of medicine and running a private practice.”
So when an opportunity presented itself, Dr. McCue leaped at the chance to narrow her expertise to obstetrical hospital medicine. She helped establish the ob.gyn. hospitalist program at Beth Israel Deaconess Hospital-Plymouth in Massachusetts, and now serves as chief of ob.gyn. and midwifery for the hospital.
“I love the fact that I now have the time to get really good at [what] I really like, [such as] labor and delivery,” said Dr. McCue, who is president of the Society of OB/GYN Hospitalists. “Since I made this change, I feel like I’m so much more on top of things. I do simulations here on my unit over things like shoulder dystocia. When I was in private practice, I would go to one meeting a year and pray that I never had a shoulder dystocia [case]. Now I really understand the whole process and I take the time to run through that with my midwives and my other nurses and doctors.”
Dr. McCue is one of a growing number of ob.gyns. who have chosen to target their expertise to a single subspecialty or concentrated practice area. Data show subspecialization is on the rise in ob.gyn.
From 1985 to 2015, certificates issued by the American Board of Obstetrics and Gynecology (ABOG) for gynecologic oncology nearly tripled, and certificates issued for reproductive endocrinology and infertility more than doubled, according to data provided by the American Board of Medical Specialties (ABMS). Certificates issued for maternal-fetal medicine rose from 35 in 1985 to 100 in 2015.

Opportunities for ob.gyns. to subspecialize have steadily increased over the last 50 years. The subspecialties of maternal-fetal medicine, gynecologic oncology, and reproductive endocrinology and infertility were first approved for certification by ABOG in 1973. In 1983, ABMS approved a certificate of “added qualification” for ob.gyns. who complete fellowships in critical care. In 1995, ABOG and the American Board of Urology started the subspecialty of female pelvic medicine and reconstructive surgery, which was approved for certification by ABMS in 2011.
ABMS also approved a certificate of “added qualification” for ob.gyns. who complete a fellowship in hospice and palliative medicine in 2008. And fellowships now exist for minimally invasive gynecologic surgery and ob.gyn. hospital medicine.
The reasons that ob.gyns. choose to subspecialize are multifold, said Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill., and one of the medical editors of the Ob.Gyn. News column, Master Class.
“Physicians subspecialize so that they can provide more medical and surgical expertise for a given population,” he said. “Secondly, physicians may be driven to subspecialize for lifestyle reasons. Generalists refer to subspecialists when technical expertise is desired to help with a clinical situation and potentially reduce medical legal risk.”
Ultimately, it’s patients who benefit from the increased care provided by subspecialists, noted Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology, and women’s health at Rutgers, the State University of New Jersey, Newark. Generalist ob.gyns. are tremendously knowledgeable and experienced, he said, but there’s no way for them to know every area, he said. It’s the difference between someone who might be doing a complicated surgery one or twice a year versus someone who is doing that surgery once or twice a week, he added.
“That is ultimately helpful for patients,” Dr. Einstein said. “It’s really about outcomes. This is all better for the patient. That’s the most important thing.”
Not every consequence of subspecialization is positive, however.
“As with everything, subspecialization has both positive and negative effects,” said Dr. Sandra Ann Carson, vice president for education at the American College of Obstetricians and Gynecologists. “The more time one has to focus on a small area, the better that area becomes. However, if all you have is a hammer, everything looks like a nail. The larger population may not need the care that someone with a rare disease may need.”
Dr. Miller refers to this challenge as “losing the forest.” He explains that subspecialists sometimes become so focused on their area of expertise, that they may overlook suitable treatment plans with which they are unfamiliar. An infertility specialist, for example, who neglects to consider a minimally invasive surgical procedure that could allow a patient to become pregnant naturally and instead recommends in vitro fertilization treatment.
“The infertility specialist does not have that particular skill and therefore directs that patient to IVF,” Dr. Miller said. “In the process of subspecializing, we have a tendency to lose the forest and look only at the trees.”
Finding a job is another challenge for the growing number of subspecialists. In many cases, fellowship-trained minimally invasive gynecologic surgeons may have to go back to practicing general gynecology because of a lack of positions, Dr. Miller said.
“We have to be careful that we do not “oversubspecialize” so that we are oversaturating the field,” he said.
In the future, the number of ob.gyn subspecialists will likely continue to grow and become more refined, said Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center in Phoenix.
“I think subspecialists will continue to become more and more developed,” Dr. Chase said. “Perhaps, some areas like family planning or minimally invasive surgery may grow further and become board certified.”
Dr. Carson foresees subspecialization becoming more focused on centralized teaching hospitals, with patients who need special care being sent to these hubs.
“Telemedicine and long-distance communication with a local obstetrician-gynecologist managing the whole patient will allow the best of both worlds,” she said.
Regardless of how subspecialist growth evolves, general ob.gyns. and other primary care physicians will always be needed, said Dr. Mary E. Norton, a maternal-fetal medicine specialist and clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“With increasing complexity, experts are needed to interpret advances,” Dr. Norton said. “However, patients also need a ‘medical home’ and primary provider who sees the big picture, and provides ongoing care beyond a single pregnancy or pregnancy complication.”
Why I chose to subspecialize
“I went to medical school with a particular interest in obstetrics. Once there, I was exposed to pediatrics and to high-risk OB, which I found to be fascinating. I particularly enjoyed my exposure to genetics during my pediatrics rotation and cared for a few children with genetic diseases that had a big impact and made a substantial impression on me. I ultimately decided to pursue an ob.gyn. residency and loved the OB part, particularly the prenatal genetics and high-risk OB. I found the balance of maternal and fetal medicine to be an exciting opportunity to care for two patients. I did an elective in prenatal diagnosis during my third year, including a bit of research, and was hooked.”
Dr. Mary E. Norton, a maternal-fetal medicine specialist and a clinical geneticist at the Fetal Treatment Center at the University of California, San Francisco.
“In my second year of residency, I became really interested in [gynecology-oncology] because I was fascinated by the surgery and interested in the chemotherapy practice, which is interesting because there’s always new research and new agents and interesting changes in how you treat the various cancers. It’s a very comprehensive, research-based field and that was fascinating to me. It’s a very busy subspecialty with very complex cases on multiple levels. You do these radical surgeries but then you have to be really involved in the choice for which chemotherapy agent to use, what type of radiation to give, and you also get really involved with the families ... Every case is so different and you treat women who are 16 years old, but you also treat women who are 96 years old. You see women from all walks of life with all sorts of different issues. The ability to really get involved with cancer research is a great part of the field.”
Dr. Dana M. Chase, a gynecologic oncologist at the University of Arizona Cancer Center, Phoenix.
“I took the opportunity to come to a new program where they were looking for an ob.gyn. hospitalist. That was exciting for me because I got to help establish the program... I feel like we’re a better department because I’m here monitoring labor, but I’m also writing protocols and making sure everyone is up to date. And I still get to do what I love the most, which is birth and babies.”
Dr. Brigid McCue, an ob.gyn. hospitalist and chief of ob.gyn. and midwifery, Beth Israel Deaconess Hospital-Plymouth, Massachusetts.
“I never considered delivering babies for the rest of my life. I was always focused on treating infertile couples. I completed my fellowship in reproductive endocrinology-infertility at the University of Pennsylvania, Philadelphia, at a time when in vitro fertilization was in its infancy and the laparoscope and hysteroscope were virtually diagnostic tools ... As IVF became more successful, I felt it was essential to add this expertise to my armamentarium ... It is truly gratifying to be part of a subspecialty that has advanced so far that the majority of our patients are able to achieve pregnancy via IVF.”
Dr. Charles E. Miller, a reproductive endocrinologist and minimally invasive gynecologic surgeon in Naperville and Schaumburg, Ill.
“During medical school, I was very interested in the surgical aspects of patient care. When I rotated in gyn-oncology – now knowing that I rotated with some of the best gyn-oncologists who ever practiced – I found myself drawn to the complexity of surgery, acuity of the patients, and the close relationships gyn-oncologists have with their patients. It hit me like a brick that this was the specialty for me. During my residency and fellowship, I was particularly drawn to the multiple modalities we use to treat cancers. I relished the idea that through clinical trials, gyn-oncologists keep pushing the bar to solve the cancer problem. What we do now is different than what we did 5 years ago. It keeps us professionally challenged all the time.”
Dr. Mark H. Einstein, a gynecologic oncologist and chair of obstetrics, gynecology and women’s health at Rutgers, the State University of New Jersey, Newark.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
On Twitter @legal_med
Data, new partnerships key to prepping for value-based care
AUSTIN, TEX. – Gathering data, seeking new partnerships, and showing leadership are the key ways to prepare for value-based medical practice, according to Houston-based health law attorney Ellie Bane.
“We are entering a whole new world in health care reimbursement,” Ms. Bane said at a conference held by the American Health Lawyers Association. “Physicians who think ahead will be well suited to succeed.”
If you don’t have practice data, start collecting the information today, she advised. Data – such as how long it takes for patients to book appointments, primary reasons for patient visits, and trends on care management – can set doctors apart and create leverage when it comes to new networks.
“You want to have reliable data so that when you go to partner with a health system or a health plan, you can show them what you can offer,” Ms. Bane said in an interview.
If the data do not exist, reach out to payers to see if they can help gather it, Ms. Bane suggested. Some health plans will assign a physician assistant or nurse practitioner to follow up with patients and help collect trend data. Other plans provide nurses or case managers to doctors who participate in certain initiatives such as quality, disease management, or performance improvement programs.
Demonstrating leadership also is key. Be vocal to hospitals and health plans about your interest in alternative payment systems and your desire to lead the transition, she advised. Be proactive by researching clinically-integrated networks, for example, and determining which network may work best for your practice.
“You want to become that value-based champion so that others will want to contract with your group,” she added.
When choosing a health system to partner with, assess whether the system is adequately responsive, can pull data in a timely manner, and can shift as measures change.
“Can your practice do the same thing?” Ms. Bane said. “If quality metrics change, are you able to change your systems to respond?”
Be creative and stay ahead of the curve by searching for novel ways to coordinate services and enlisting guidance, she said.
“A joint venture or Physician-Hospital Organization might have worked 5 years ago, but, it may not be the best model today,” she said. “This is where effective counsel is so helpful. A good health law attorney will be able to think of creative alignment strategies that will benefit the providers, health plans, systems, and – most importantly – patients.”
On Twitter @legal_med
AUSTIN, TEX. – Gathering data, seeking new partnerships, and showing leadership are the key ways to prepare for value-based medical practice, according to Houston-based health law attorney Ellie Bane.
“We are entering a whole new world in health care reimbursement,” Ms. Bane said at a conference held by the American Health Lawyers Association. “Physicians who think ahead will be well suited to succeed.”
If you don’t have practice data, start collecting the information today, she advised. Data – such as how long it takes for patients to book appointments, primary reasons for patient visits, and trends on care management – can set doctors apart and create leverage when it comes to new networks.
“You want to have reliable data so that when you go to partner with a health system or a health plan, you can show them what you can offer,” Ms. Bane said in an interview.
If the data do not exist, reach out to payers to see if they can help gather it, Ms. Bane suggested. Some health plans will assign a physician assistant or nurse practitioner to follow up with patients and help collect trend data. Other plans provide nurses or case managers to doctors who participate in certain initiatives such as quality, disease management, or performance improvement programs.
Demonstrating leadership also is key. Be vocal to hospitals and health plans about your interest in alternative payment systems and your desire to lead the transition, she advised. Be proactive by researching clinically-integrated networks, for example, and determining which network may work best for your practice.
“You want to become that value-based champion so that others will want to contract with your group,” she added.
When choosing a health system to partner with, assess whether the system is adequately responsive, can pull data in a timely manner, and can shift as measures change.
“Can your practice do the same thing?” Ms. Bane said. “If quality metrics change, are you able to change your systems to respond?”
Be creative and stay ahead of the curve by searching for novel ways to coordinate services and enlisting guidance, she said.
“A joint venture or Physician-Hospital Organization might have worked 5 years ago, but, it may not be the best model today,” she said. “This is where effective counsel is so helpful. A good health law attorney will be able to think of creative alignment strategies that will benefit the providers, health plans, systems, and – most importantly – patients.”
On Twitter @legal_med
AUSTIN, TEX. – Gathering data, seeking new partnerships, and showing leadership are the key ways to prepare for value-based medical practice, according to Houston-based health law attorney Ellie Bane.
“We are entering a whole new world in health care reimbursement,” Ms. Bane said at a conference held by the American Health Lawyers Association. “Physicians who think ahead will be well suited to succeed.”
If you don’t have practice data, start collecting the information today, she advised. Data – such as how long it takes for patients to book appointments, primary reasons for patient visits, and trends on care management – can set doctors apart and create leverage when it comes to new networks.
“You want to have reliable data so that when you go to partner with a health system or a health plan, you can show them what you can offer,” Ms. Bane said in an interview.
If the data do not exist, reach out to payers to see if they can help gather it, Ms. Bane suggested. Some health plans will assign a physician assistant or nurse practitioner to follow up with patients and help collect trend data. Other plans provide nurses or case managers to doctors who participate in certain initiatives such as quality, disease management, or performance improvement programs.
Demonstrating leadership also is key. Be vocal to hospitals and health plans about your interest in alternative payment systems and your desire to lead the transition, she advised. Be proactive by researching clinically-integrated networks, for example, and determining which network may work best for your practice.
“You want to become that value-based champion so that others will want to contract with your group,” she added.
When choosing a health system to partner with, assess whether the system is adequately responsive, can pull data in a timely manner, and can shift as measures change.
“Can your practice do the same thing?” Ms. Bane said. “If quality metrics change, are you able to change your systems to respond?”
Be creative and stay ahead of the curve by searching for novel ways to coordinate services and enlisting guidance, she said.
“A joint venture or Physician-Hospital Organization might have worked 5 years ago, but, it may not be the best model today,” she said. “This is where effective counsel is so helpful. A good health law attorney will be able to think of creative alignment strategies that will benefit the providers, health plans, systems, and – most importantly – patients.”
On Twitter @legal_med
EXPERT ANALYSIS FROM THE PHYSICIANS & HOSPITALS LAW INSTITUTE
FDA announces new plan to combat opioid abuse
Food and Drug Administration officials are calling for a sweeping overhaul of the agency’s approach to opioid medications, including renewed efforts to improve how opioids are approved, labeled, and prescribed.
The initiative focuses on new policies to help reverse the opioid abuse epidemic, while still providing patients in pain with access to effective relief, Dr. Robert M. Califf, FDA deputy commissioner for medical products and tobacco, said in a Feb. 4 announcement.
“Things are getting worse, not better, with the epidemic of opioid misuse, abuse and dependence,” said Dr. Califf, who has been nominated but not confirmed as FDA commissioner. “It’s time we all took a step back to look at what is working and what we need to change to impact this crisis.”
Under the new plan, the FDA will convene an advisory committee before approving new drug applications for opioids that do not have abuse-deterrent properties and develop changes to immediate-release opioid labeling. The agency also plans to expand access to abuse-deterrent formulations of opioid products and improve the availability of naloxone and medication-assisted treatment options for patients with opioid use disorders.
In a Feb. 4 editorial published in the New England Journal of Medicine, Dr. Califf noted that the number of annual deaths from opioid overdoses now exceeds the number of annual deaths from motor vehicle accidents (doi:10.1056/NEJMsr1601307).
“Regardless of whether we view these issues from the perspective of patients, physicians, or regulators, the status quo is clearly not acceptable,” Dr. Califf wrote in the editorial. “As the public health agency responsible for oversight of pharmaceutical safety and effectiveness, we recognize that this crisis demands solutions. We are committed to action, and we urge others to join us.”
Read the full announcement here.
On Twitter @legal_med
Food and Drug Administration officials are calling for a sweeping overhaul of the agency’s approach to opioid medications, including renewed efforts to improve how opioids are approved, labeled, and prescribed.
The initiative focuses on new policies to help reverse the opioid abuse epidemic, while still providing patients in pain with access to effective relief, Dr. Robert M. Califf, FDA deputy commissioner for medical products and tobacco, said in a Feb. 4 announcement.
“Things are getting worse, not better, with the epidemic of opioid misuse, abuse and dependence,” said Dr. Califf, who has been nominated but not confirmed as FDA commissioner. “It’s time we all took a step back to look at what is working and what we need to change to impact this crisis.”
Under the new plan, the FDA will convene an advisory committee before approving new drug applications for opioids that do not have abuse-deterrent properties and develop changes to immediate-release opioid labeling. The agency also plans to expand access to abuse-deterrent formulations of opioid products and improve the availability of naloxone and medication-assisted treatment options for patients with opioid use disorders.
In a Feb. 4 editorial published in the New England Journal of Medicine, Dr. Califf noted that the number of annual deaths from opioid overdoses now exceeds the number of annual deaths from motor vehicle accidents (doi:10.1056/NEJMsr1601307).
“Regardless of whether we view these issues from the perspective of patients, physicians, or regulators, the status quo is clearly not acceptable,” Dr. Califf wrote in the editorial. “As the public health agency responsible for oversight of pharmaceutical safety and effectiveness, we recognize that this crisis demands solutions. We are committed to action, and we urge others to join us.”
Read the full announcement here.
On Twitter @legal_med
Food and Drug Administration officials are calling for a sweeping overhaul of the agency’s approach to opioid medications, including renewed efforts to improve how opioids are approved, labeled, and prescribed.
The initiative focuses on new policies to help reverse the opioid abuse epidemic, while still providing patients in pain with access to effective relief, Dr. Robert M. Califf, FDA deputy commissioner for medical products and tobacco, said in a Feb. 4 announcement.
“Things are getting worse, not better, with the epidemic of opioid misuse, abuse and dependence,” said Dr. Califf, who has been nominated but not confirmed as FDA commissioner. “It’s time we all took a step back to look at what is working and what we need to change to impact this crisis.”
Under the new plan, the FDA will convene an advisory committee before approving new drug applications for opioids that do not have abuse-deterrent properties and develop changes to immediate-release opioid labeling. The agency also plans to expand access to abuse-deterrent formulations of opioid products and improve the availability of naloxone and medication-assisted treatment options for patients with opioid use disorders.
In a Feb. 4 editorial published in the New England Journal of Medicine, Dr. Califf noted that the number of annual deaths from opioid overdoses now exceeds the number of annual deaths from motor vehicle accidents (doi:10.1056/NEJMsr1601307).
“Regardless of whether we view these issues from the perspective of patients, physicians, or regulators, the status quo is clearly not acceptable,” Dr. Califf wrote in the editorial. “As the public health agency responsible for oversight of pharmaceutical safety and effectiveness, we recognize that this crisis demands solutions. We are committed to action, and we urge others to join us.”
Read the full announcement here.
On Twitter @legal_med
Doctors to APM committee: Remember specialists
Physicians are calling on a new federal advisory committee to be sure to include specialists in the coming value-based alternative payment models.
Created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the Physician-Focused Payment Model Technical Advisory Committee (PTAC) is charged with providing comments and recommendations on physician payment models to the Health & Human Services department. At the committee’s first meeting on Feb. 1, members heard from a number of physician associations that expressed disappointment about the role of specialists in current value-based payment models and requested more attention as new models move forward.
“We believe [the Centers for Medicare & Medicaid Services] needs to allow for the widest range of innovative ideas to ensure the greatest number of physicians are not only able to participate, but succeed in future payment models,” said Jenna Kappel, health policy director for the American Academy of Otolaryngology–Head and Neck Surgery. “We are hopeful there will be opportunities for specialists to participate and thrive in [alternative payment models] in the future. However, the current CMS definition of an alternative payment entity provides very limited opportunities for models that include the participation of specialists.”
The American College of Emergency Physicians concurred.
“There have been a significant number of [Center for Medicare & Medicaid Innovation] grants and state Medicaid proposals that include an emergency department [ED] visit as a failure metric,” said Barbara Tomar, federal affairs director for ACEP. “We understand that to a certain point ... but there are always going to be a proportion of patients [who] have serious diseases or conditions that will have exacerbations, and they’re going to land in the ED. This really should be acknowledged in a lot of the alternative payment models.”
Committee members acknowledged concerns about APMs and outlined goals for developing an effective proposal review process.
“We need to involve everybody in developing innovative payment models that do away with all frustration that physicians are currently experiencing and get to better results and higher value,” said committee member Robert A. Berenson, an internist and former vice chair of the Medicare Payment Advisory Commission. “At the same time, these payment models not only have to be elegant in their conception, but they have to be operationally and administratively feasible. ... They need to be such that most payers can adopt them, not simply CMS or Medicare or a state Medicaid agency,” Dr. Berenson said.
Transparency, inclusion, and education are primary aims of the committee, said committee member Dr. Kavita Patel, an internist and senior fellow at the Brookings Institution, Washington.
“Part of my responsibility, having looked at other payment models as well as the trials and tribulations of not just the practicing clinician, but the practicing team is [considering] how the team is going to adapt and learn and strive in this environment,” Dr. Patel said. “So much of what we try to do is think about the financial incentives. We also need to think about what are we asking clinicians to measure? What are we asking patients and families to report on and how do we have the two align?”
Officials at the CMS Innovation Center have said that proposed APMs will be submitted first to PTAC for recommendations and then will go to HHS. The Secretary will make comments about the proposals on the CMS website, followed by testing consideration. Potential evaluation factors include the strength of the evidence base, the potential for cost savings, the probability of model success, feasibility, scalability, and demographic, clinical, and geographic diversity.
“Obviously, we’re not looking for slam dunk data that say it always will be effective because if it were, we wouldn’t need to do the test, but we need some evidence that this is potentially a worthwhile investment,” said Dr. Hoangmai H. Pham, director of accountable care programs at the CMS Innovation Center.
CMS officials stressed that models should be designed as broadly as possible. A proposal can include multiple interventions, but should include a similar theme, procedure, or condition to address.
“It gives us the opportunity to find efficiencies,” Dr. Pham said. “It’s much easier to have one model with multiple tracks that you can ask one application contractor to handle as opposed to six. Much easier to ask for all the payment shared system changes in 1 change request rather than 32. That’s another reason we would urge you to favor comprehensive models.”
CMS officials plan to issue a proposed rule on APMs in April and a final rule Nov. 1.
On Twitter @legal_med
Physicians are calling on a new federal advisory committee to be sure to include specialists in the coming value-based alternative payment models.
Created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the Physician-Focused Payment Model Technical Advisory Committee (PTAC) is charged with providing comments and recommendations on physician payment models to the Health & Human Services department. At the committee’s first meeting on Feb. 1, members heard from a number of physician associations that expressed disappointment about the role of specialists in current value-based payment models and requested more attention as new models move forward.
“We believe [the Centers for Medicare & Medicaid Services] needs to allow for the widest range of innovative ideas to ensure the greatest number of physicians are not only able to participate, but succeed in future payment models,” said Jenna Kappel, health policy director for the American Academy of Otolaryngology–Head and Neck Surgery. “We are hopeful there will be opportunities for specialists to participate and thrive in [alternative payment models] in the future. However, the current CMS definition of an alternative payment entity provides very limited opportunities for models that include the participation of specialists.”
The American College of Emergency Physicians concurred.
“There have been a significant number of [Center for Medicare & Medicaid Innovation] grants and state Medicaid proposals that include an emergency department [ED] visit as a failure metric,” said Barbara Tomar, federal affairs director for ACEP. “We understand that to a certain point ... but there are always going to be a proportion of patients [who] have serious diseases or conditions that will have exacerbations, and they’re going to land in the ED. This really should be acknowledged in a lot of the alternative payment models.”
Committee members acknowledged concerns about APMs and outlined goals for developing an effective proposal review process.
“We need to involve everybody in developing innovative payment models that do away with all frustration that physicians are currently experiencing and get to better results and higher value,” said committee member Robert A. Berenson, an internist and former vice chair of the Medicare Payment Advisory Commission. “At the same time, these payment models not only have to be elegant in their conception, but they have to be operationally and administratively feasible. ... They need to be such that most payers can adopt them, not simply CMS or Medicare or a state Medicaid agency,” Dr. Berenson said.
Transparency, inclusion, and education are primary aims of the committee, said committee member Dr. Kavita Patel, an internist and senior fellow at the Brookings Institution, Washington.
“Part of my responsibility, having looked at other payment models as well as the trials and tribulations of not just the practicing clinician, but the practicing team is [considering] how the team is going to adapt and learn and strive in this environment,” Dr. Patel said. “So much of what we try to do is think about the financial incentives. We also need to think about what are we asking clinicians to measure? What are we asking patients and families to report on and how do we have the two align?”
Officials at the CMS Innovation Center have said that proposed APMs will be submitted first to PTAC for recommendations and then will go to HHS. The Secretary will make comments about the proposals on the CMS website, followed by testing consideration. Potential evaluation factors include the strength of the evidence base, the potential for cost savings, the probability of model success, feasibility, scalability, and demographic, clinical, and geographic diversity.
“Obviously, we’re not looking for slam dunk data that say it always will be effective because if it were, we wouldn’t need to do the test, but we need some evidence that this is potentially a worthwhile investment,” said Dr. Hoangmai H. Pham, director of accountable care programs at the CMS Innovation Center.
CMS officials stressed that models should be designed as broadly as possible. A proposal can include multiple interventions, but should include a similar theme, procedure, or condition to address.
“It gives us the opportunity to find efficiencies,” Dr. Pham said. “It’s much easier to have one model with multiple tracks that you can ask one application contractor to handle as opposed to six. Much easier to ask for all the payment shared system changes in 1 change request rather than 32. That’s another reason we would urge you to favor comprehensive models.”
CMS officials plan to issue a proposed rule on APMs in April and a final rule Nov. 1.
On Twitter @legal_med
Physicians are calling on a new federal advisory committee to be sure to include specialists in the coming value-based alternative payment models.
Created by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the Physician-Focused Payment Model Technical Advisory Committee (PTAC) is charged with providing comments and recommendations on physician payment models to the Health & Human Services department. At the committee’s first meeting on Feb. 1, members heard from a number of physician associations that expressed disappointment about the role of specialists in current value-based payment models and requested more attention as new models move forward.
“We believe [the Centers for Medicare & Medicaid Services] needs to allow for the widest range of innovative ideas to ensure the greatest number of physicians are not only able to participate, but succeed in future payment models,” said Jenna Kappel, health policy director for the American Academy of Otolaryngology–Head and Neck Surgery. “We are hopeful there will be opportunities for specialists to participate and thrive in [alternative payment models] in the future. However, the current CMS definition of an alternative payment entity provides very limited opportunities for models that include the participation of specialists.”
The American College of Emergency Physicians concurred.
“There have been a significant number of [Center for Medicare & Medicaid Innovation] grants and state Medicaid proposals that include an emergency department [ED] visit as a failure metric,” said Barbara Tomar, federal affairs director for ACEP. “We understand that to a certain point ... but there are always going to be a proportion of patients [who] have serious diseases or conditions that will have exacerbations, and they’re going to land in the ED. This really should be acknowledged in a lot of the alternative payment models.”
Committee members acknowledged concerns about APMs and outlined goals for developing an effective proposal review process.
“We need to involve everybody in developing innovative payment models that do away with all frustration that physicians are currently experiencing and get to better results and higher value,” said committee member Robert A. Berenson, an internist and former vice chair of the Medicare Payment Advisory Commission. “At the same time, these payment models not only have to be elegant in their conception, but they have to be operationally and administratively feasible. ... They need to be such that most payers can adopt them, not simply CMS or Medicare or a state Medicaid agency,” Dr. Berenson said.
Transparency, inclusion, and education are primary aims of the committee, said committee member Dr. Kavita Patel, an internist and senior fellow at the Brookings Institution, Washington.
“Part of my responsibility, having looked at other payment models as well as the trials and tribulations of not just the practicing clinician, but the practicing team is [considering] how the team is going to adapt and learn and strive in this environment,” Dr. Patel said. “So much of what we try to do is think about the financial incentives. We also need to think about what are we asking clinicians to measure? What are we asking patients and families to report on and how do we have the two align?”
Officials at the CMS Innovation Center have said that proposed APMs will be submitted first to PTAC for recommendations and then will go to HHS. The Secretary will make comments about the proposals on the CMS website, followed by testing consideration. Potential evaluation factors include the strength of the evidence base, the potential for cost savings, the probability of model success, feasibility, scalability, and demographic, clinical, and geographic diversity.
“Obviously, we’re not looking for slam dunk data that say it always will be effective because if it were, we wouldn’t need to do the test, but we need some evidence that this is potentially a worthwhile investment,” said Dr. Hoangmai H. Pham, director of accountable care programs at the CMS Innovation Center.
CMS officials stressed that models should be designed as broadly as possible. A proposal can include multiple interventions, but should include a similar theme, procedure, or condition to address.
“It gives us the opportunity to find efficiencies,” Dr. Pham said. “It’s much easier to have one model with multiple tracks that you can ask one application contractor to handle as opposed to six. Much easier to ask for all the payment shared system changes in 1 change request rather than 32. That’s another reason we would urge you to favor comprehensive models.”
CMS officials plan to issue a proposed rule on APMs in April and a final rule Nov. 1.
On Twitter @legal_med
CMS proposal would allow sharing, selling of claims data
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
The American Gastroenterological Association (AGA) provided this statement on the proposal: "The AGA believes that gastroenterologists in all practice settings and geographic areas should have the opportunity to choose from among the payment models available, based on what best accommodates their practice and the needs of their patients. We encourage CMS to be as broad as possible in defining an alternative payment model (APM). This would allow more physicians to participate in models that may be more applicable to their specialty and patient population. A physician-focused payment model (PFPM) should be defined as a payment model outlined and defined by expert physicians which allows physician practices to migrate to fee for value while improving clinical outcomes, care coordination, and patient experience. We also recommend allowing for variance in meeting the threshold of an APM and a recognition of the inherent inaccuracy of revenue aggregation."
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
The American Gastroenterological Association (AGA) provided this statement on the proposal: "The AGA believes that gastroenterologists in all practice settings and geographic areas should have the opportunity to choose from among the payment models available, based on what best accommodates their practice and the needs of their patients. We encourage CMS to be as broad as possible in defining an alternative payment model (APM). This would allow more physicians to participate in models that may be more applicable to their specialty and patient population. A physician-focused payment model (PFPM) should be defined as a payment model outlined and defined by expert physicians which allows physician practices to migrate to fee for value while improving clinical outcomes, care coordination, and patient experience. We also recommend allowing for variance in meeting the threshold of an APM and a recognition of the inherent inaccuracy of revenue aggregation."
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
The American Gastroenterological Association (AGA) provided this statement on the proposal: "The AGA believes that gastroenterologists in all practice settings and geographic areas should have the opportunity to choose from among the payment models available, based on what best accommodates their practice and the needs of their patients. We encourage CMS to be as broad as possible in defining an alternative payment model (APM). This would allow more physicians to participate in models that may be more applicable to their specialty and patient population. A physician-focused payment model (PFPM) should be defined as a payment model outlined and defined by expert physicians which allows physician practices to migrate to fee for value while improving clinical outcomes, care coordination, and patient experience. We also recommend allowing for variance in meeting the threshold of an APM and a recognition of the inherent inaccuracy of revenue aggregation."
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
CMS proposal would allow sharing, selling of claims data
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Physicians may soon be able to purchase reports that combine their Medicare and private payer claims data, according to the details of a new government proposal.
The proposed rule, released on Jan. 29, would enable entities approved by the government to share or sell Medicare and private claims information to health providers, suppliers, hospital associations, and medical societies. The new rule, as required by the Medicare Access and CHIP Reauthorization Act (MACRA), seeks to increase transparency about provider performance and generate data uses that improve care delivery, according to a statement from the Centers for Medicare & Medicaid Services.
“Increasing access to analyses and data that include Medicare data will make it easier for stakeholders throughout the healthcare system to make smarter and more informed healthcare decisions,” CMS Acting Administrator Andy Slavitt said in a statement.
Under the rule, qualified entities may provide or sell data or analyses of the data to providers and suppliers. CMS encourages the sharing of data analytics that would assist in quality and patient care improvement activities, including the development of new models of care.
Disclosure or use of data for marketing purposes would be barred.
The rule includes strict privacy and security requirements for all entities receiving Medicare analyses or data.
If finalized, the rule could help practices in their efforts to provide value-based care and perform population management, said Dr. Yul D. Ejnes, chair-emeritus of the American College of Physicians Board of Regents and an internist in private practice in Cranston, R.I.
“A barrier, especially for small groups, is access to all-payer data, since what is available now is often partitioned by payer and not easy to compile into practice-wide data covering all patients,” he said in an interview. “Clearly, there is also a need for analysis of the data that is beyond the reach of most practices and is best done by third parties with the resources and expertise, so making the CMS data available facilitates that.”
However, Dr. Ejnes questioned how much these analyses will cost practices, especially smaller practices.
“Another related issue, beyond CMS’ purview, is how affordable this type of data analysis would be for the small practice that might benefit the most from it, since larger organizations have resources that may make much of this available to its physicians at little or no cost,” he said.
Entities supplying the information to providers must be accepted into the qualified entity program. The program, authorized under the Affordable Care Act, allows organizations that meet certain criteria to access patient-protected Medicare data to produce public reports. Qualified entities must combine the Medicare data with other claims data to produce reports that are “representative of how providers and suppliers are performing across multiple payers.”
Thus far, 13 organizations have been accepted into the program. Of these organizations, 2 have completed public reporting, while the other 11 are preparing for public reporting, according to CMS.
Comments on the new rule are due by March 29.
On Twitter @legal_med
Reaction: Poor methodology mars malpractice study
Physicians and insurers are taking exception to a medical malpractice study published Jan. 28 in the New England Journal of Medicine.
“Once again a study of medical liability claims has based unreliable conclusions on information obtained from the inherently flawed National Practitioner Data Bank,” Dr. Steven J. Stack, president of the American Medical Association, said in an interview.
David M. Studdert, Sc.D., of Stanford (Calif.) University, lead author of the study, said that he stands behind the findings, saying that the methodology used was strong and any significant limitations were noted.
“The data bank is the most authoritative repository of information that we have on medical malpractice claims nationwide,” Dr. Studdert said in an interview. “We don’t have an ability to look across the country at what’s happening with medical malpractice claims in any more comprehensive way than the [data bank]. Is it a perfect source of data? No. It has some limitations.”
The National Practitioner Data Bank (NPDB) is a congressionally mandated repository of medical malpractice payments and certain adverse actions related to health care providers, entities, and suppliers. Dr. Studdert and his colleagues calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians, finding, on summation, that if physicians had one claim paid against them, they were more likely to have a subsequent claim paid against them as well (N Engl J Med. 2016; 374:354-62).
The credibility of the data bank has long been in question. An investigation published by the Government Accountability Office (GAO) in 2000 found that reports collected by the data bank were often untimely, inaccurate, or duplicated, which made it appear that “twice the number of disciplinary actions against a practitioner had been taken.”
In addition, most reports in the NPDB are based on legal settlements that were never adjudicated by a court, proven to involve negligence, or settled with a physician’s consent, according to Dr. Stack of the AMA. “Settlement information offers an incomplete and often misleading indicator of physician quality and competence. The nation’s best physicians who practice cutting-edge medicine and take on the riskiest cases are involved in settlements, yet the [NPDB] information does not acknowledge their high-level of competence.”
The study acknowledged that only 3% of the lawsuits studied were paid through trial verdicts, and that the remaining claims were paid by out-of-court settlements. Dr. Studdert and his colleagues also pointed out that payments do not necessarily indicate that a claim has merit, but that paid claims are “much more likely than unpaid claims to involve substandard care.”
Another study limitation was the unknown extent of underreporting to the NPDB, Dr. Studdert said.
As for the GAO report, the findings analyzed disciplinary actions, while the current study evaluated medical malpractice claims, Dr. Studdert said. Investigators tested for duplicate records during the course of their study and did not find repeated cases.
“That wasn’t an issue with the data we examined,” he said. “The information was very complete. I don’t doubt that the GAO report was correct, but it looks like over the last 15 years there must have been some improvements to the quality of the data bank.”
PIAA, a national trade association that represents medical liability insurers, expressed concern over findings that certain specialists face more claims than others.
“We know that certain specialties, such a neurosurgery, obstetrics and gynecology, and others, have been linked with a higher frequency of claims,” PIAA President and CEO Brian K. Atchinson said in a statement. “These doctors experience more claims because of the risk associated with their particular specialty, and not because they are inherently prone to making mistakes more often than their colleagues.”
“Studies have shown that all physicians are likely to be named in at least one medical liability claim during the course of their career with some subject to more based on their specialty,” P. Divya Parikh, PIAA vice president of research, said in a statement. “Thus, this study hasn’t really revealed anything we didn’t already know.”
Dr. Studdert said that he disagrees. “That’s really not an accurate analysis of what our analysis does. Our analysis controls for specialty and then looks at other risk factors for recurrent claims. It’s a regression model.”
On Twitter@legal_med
Physicians and insurers are taking exception to a medical malpractice study published Jan. 28 in the New England Journal of Medicine.
“Once again a study of medical liability claims has based unreliable conclusions on information obtained from the inherently flawed National Practitioner Data Bank,” Dr. Steven J. Stack, president of the American Medical Association, said in an interview.
David M. Studdert, Sc.D., of Stanford (Calif.) University, lead author of the study, said that he stands behind the findings, saying that the methodology used was strong and any significant limitations were noted.
“The data bank is the most authoritative repository of information that we have on medical malpractice claims nationwide,” Dr. Studdert said in an interview. “We don’t have an ability to look across the country at what’s happening with medical malpractice claims in any more comprehensive way than the [data bank]. Is it a perfect source of data? No. It has some limitations.”
The National Practitioner Data Bank (NPDB) is a congressionally mandated repository of medical malpractice payments and certain adverse actions related to health care providers, entities, and suppliers. Dr. Studdert and his colleagues calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians, finding, on summation, that if physicians had one claim paid against them, they were more likely to have a subsequent claim paid against them as well (N Engl J Med. 2016; 374:354-62).
The credibility of the data bank has long been in question. An investigation published by the Government Accountability Office (GAO) in 2000 found that reports collected by the data bank were often untimely, inaccurate, or duplicated, which made it appear that “twice the number of disciplinary actions against a practitioner had been taken.”
In addition, most reports in the NPDB are based on legal settlements that were never adjudicated by a court, proven to involve negligence, or settled with a physician’s consent, according to Dr. Stack of the AMA. “Settlement information offers an incomplete and often misleading indicator of physician quality and competence. The nation’s best physicians who practice cutting-edge medicine and take on the riskiest cases are involved in settlements, yet the [NPDB] information does not acknowledge their high-level of competence.”
The study acknowledged that only 3% of the lawsuits studied were paid through trial verdicts, and that the remaining claims were paid by out-of-court settlements. Dr. Studdert and his colleagues also pointed out that payments do not necessarily indicate that a claim has merit, but that paid claims are “much more likely than unpaid claims to involve substandard care.”
Another study limitation was the unknown extent of underreporting to the NPDB, Dr. Studdert said.
As for the GAO report, the findings analyzed disciplinary actions, while the current study evaluated medical malpractice claims, Dr. Studdert said. Investigators tested for duplicate records during the course of their study and did not find repeated cases.
“That wasn’t an issue with the data we examined,” he said. “The information was very complete. I don’t doubt that the GAO report was correct, but it looks like over the last 15 years there must have been some improvements to the quality of the data bank.”
PIAA, a national trade association that represents medical liability insurers, expressed concern over findings that certain specialists face more claims than others.
“We know that certain specialties, such a neurosurgery, obstetrics and gynecology, and others, have been linked with a higher frequency of claims,” PIAA President and CEO Brian K. Atchinson said in a statement. “These doctors experience more claims because of the risk associated with their particular specialty, and not because they are inherently prone to making mistakes more often than their colleagues.”
“Studies have shown that all physicians are likely to be named in at least one medical liability claim during the course of their career with some subject to more based on their specialty,” P. Divya Parikh, PIAA vice president of research, said in a statement. “Thus, this study hasn’t really revealed anything we didn’t already know.”
Dr. Studdert said that he disagrees. “That’s really not an accurate analysis of what our analysis does. Our analysis controls for specialty and then looks at other risk factors for recurrent claims. It’s a regression model.”
On Twitter@legal_med
Physicians and insurers are taking exception to a medical malpractice study published Jan. 28 in the New England Journal of Medicine.
“Once again a study of medical liability claims has based unreliable conclusions on information obtained from the inherently flawed National Practitioner Data Bank,” Dr. Steven J. Stack, president of the American Medical Association, said in an interview.
David M. Studdert, Sc.D., of Stanford (Calif.) University, lead author of the study, said that he stands behind the findings, saying that the methodology used was strong and any significant limitations were noted.
“The data bank is the most authoritative repository of information that we have on medical malpractice claims nationwide,” Dr. Studdert said in an interview. “We don’t have an ability to look across the country at what’s happening with medical malpractice claims in any more comprehensive way than the [data bank]. Is it a perfect source of data? No. It has some limitations.”
The National Practitioner Data Bank (NPDB) is a congressionally mandated repository of medical malpractice payments and certain adverse actions related to health care providers, entities, and suppliers. Dr. Studdert and his colleagues calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians, finding, on summation, that if physicians had one claim paid against them, they were more likely to have a subsequent claim paid against them as well (N Engl J Med. 2016; 374:354-62).
The credibility of the data bank has long been in question. An investigation published by the Government Accountability Office (GAO) in 2000 found that reports collected by the data bank were often untimely, inaccurate, or duplicated, which made it appear that “twice the number of disciplinary actions against a practitioner had been taken.”
In addition, most reports in the NPDB are based on legal settlements that were never adjudicated by a court, proven to involve negligence, or settled with a physician’s consent, according to Dr. Stack of the AMA. “Settlement information offers an incomplete and often misleading indicator of physician quality and competence. The nation’s best physicians who practice cutting-edge medicine and take on the riskiest cases are involved in settlements, yet the [NPDB] information does not acknowledge their high-level of competence.”
The study acknowledged that only 3% of the lawsuits studied were paid through trial verdicts, and that the remaining claims were paid by out-of-court settlements. Dr. Studdert and his colleagues also pointed out that payments do not necessarily indicate that a claim has merit, but that paid claims are “much more likely than unpaid claims to involve substandard care.”
Another study limitation was the unknown extent of underreporting to the NPDB, Dr. Studdert said.
As for the GAO report, the findings analyzed disciplinary actions, while the current study evaluated medical malpractice claims, Dr. Studdert said. Investigators tested for duplicate records during the course of their study and did not find repeated cases.
“That wasn’t an issue with the data we examined,” he said. “The information was very complete. I don’t doubt that the GAO report was correct, but it looks like over the last 15 years there must have been some improvements to the quality of the data bank.”
PIAA, a national trade association that represents medical liability insurers, expressed concern over findings that certain specialists face more claims than others.
“We know that certain specialties, such a neurosurgery, obstetrics and gynecology, and others, have been linked with a higher frequency of claims,” PIAA President and CEO Brian K. Atchinson said in a statement. “These doctors experience more claims because of the risk associated with their particular specialty, and not because they are inherently prone to making mistakes more often than their colleagues.”
“Studies have shown that all physicians are likely to be named in at least one medical liability claim during the course of their career with some subject to more based on their specialty,” P. Divya Parikh, PIAA vice president of research, said in a statement. “Thus, this study hasn’t really revealed anything we didn’t already know.”
Dr. Studdert said that he disagrees. “That’s really not an accurate analysis of what our analysis does. Our analysis controls for specialty and then looks at other risk factors for recurrent claims. It’s a regression model.”
On Twitter@legal_med
Telemental health reaches underserved children, builds partnerships
The patient, a 10-year-old girl, was exhibiting defiant and angry behavior at home. Her pediatrician in rural Vermont was not able to support the family optimally, so he referred her to Dr. David C. Rettew.
Dr. Rettew soon learned that the girl blamed herself for her father’s absence, and she interpreted efforts by her mother to set limits as evidence that her mom didn’t love her.
“During the course of the interview, it became clear that the girl had some specific thoughts that were likely fueling her anger,” said Dr. Rettew, director of the Pediatric Psychiatry Clinic at the University of Vermont, Burlington. “She also met criteria clearly for ADHD, which had never been diagnosed. The consultation recommendations not only included some possible medications to try, but also some specific areas that could be addressed for psychotherapy that could really help the relationship between this child and her mother.”
The successful intervention took place via a secure, two-way videoconference. It is one example of how physicians at the University of Vermont are using telemental health to treat children in underserved areas. As part of a state-funded training program, child psychiatry fellows at the university consult with primary care doctors at federally qualified health centers across the state. The primary care physicians discuss patient cases with fellows via phone or email and can refer patients for in-person or telemental health assessments.
The program has been running for about 5 years and so far has yielded countless benefits, said Dr. Rettew, who directs the university’s Child and Adolescent Psychiatry Fellowship Program. “It helps keep the care housed and centered within the primary care home. That can help coordination of services so that care isn’t fragmented around multiple centers. It also allows evaluations to happen that wouldn’t happen otherwise because it’s too much of a hardship for families to travel long distances and come for regular follow-up appointments.”
University of Vermont physicians also use telemedicine to consult with other mental health clinicians across the state. Child psychiatrist Allison Y. Hall provides in-person training to clinicians and then counsels and supervises their efforts through a telemedicine unit.
“For this purpose, it’s great,” said Dr. Hall, who practices at the Vermont Center for Children, Youth, and Families, which is housed within the university’s psychiatry department. “There’s more confidentiality than Skype, for instance. It’s wonderful to be able to reach clinicians at a great distance.”
On a broader scale, telemental health is a promising tool to address the shortage of mental health providers in the United States, said Dr. Robert C. Gunther, a pediatrician at the University of Virginia Health System in Fishersville. Recent research found that one in three children receiving outpatient care for mental health conditions saw only their primary care doctor for care (Pediatrics. 2015 Nov;136;e1178-85).
“There is a tremendous need for pediatric mental health care,” Dr. Gunther said in an interview. “There is a great shortage of child psychiatrists and other child mental health specialists. Telemental health can help in areas where geography or financial barriers exist to accessing care.”
Data from the Children’s ADHD Telemental Health Treatment Study (CATTS) illustrates the impact that telemental health can have on children facing such barriers to care. Researchers randomized 223 children referred by 88 primary care providers in seven underserved communities into two study groups. Children in the first group were seen by child psychiatrists via videoconference six times over 22 weeks; treatment included pharmacotherapy. Their caregivers received behavior training provided in person by community therapists who were supervised remotely. Children in the second group were treated by their primary care physicians and received one telepsychiatry consult.
Children in both groups improved; however, those randomized to the telemental health model improved “significantly more than patients in the augmented primary care arm” (J Am Acad Child Adolesc Psychiatry. 2015 Apr;54[4]:263-74).
“The CATTS trial demonstrated the effectiveness of a telehealth service model to treat ADHD in communities with limited access to specialty mental health services,” investigators concluded.
But Dr. Joshua J. Alexander, chair of the American Academy of Pediatrics Section on Telehealth Care, notes that some mental health conditions fit more smoothly within the telemental health model than others. ADHD is the most common condition treated by telemental health, he said. The model also has shown success in the treatment of childhood adjustment disorders, anxiety, oppositional defiant disorder, mood disorders, anxiety, and depression.
“I think you have to be careful in determining where telemental health would be beneficial to use and in which cases it might not be an appropriate method to deliver care,” Dr. Alexander said in an interview.
Developing trust and rapport with patients through videoconferencing also can be a challenge, added Dr. Alexander, who is director of the TelAbility telehealth program at the University of North Carolina at Chapel Hill. He recommends that specialists use the technology to continue an existing doctor-patient relationship or to provide care in a consultative model in which the child’s primary care doctor is present along with the patient and patient’s family.
The AAP advocates for the use of telemedicine so long as it is conducted within the context of the medical home. Fragmented telemedicine services that could disrupt continuity of care should be avoided, according to a 2015 AAP policy statement (Pediatrics. 2015 Jun. doi: 10.1542/peds.2015-1253). The academy also calls for the expansion of pediatric telemedicine to increase access to care for underserved communities and improve quality of care for children.
More partnerships between mental health specialists and primary care providers are a key step in delivering high quality pediatric telemental care, Dr. Alexander said.
“Some larger pediatric practices already do this by hiring and colocating individuals at their practice site, but other, smaller practices might not have the room, finances, sufficient patient population, or enough local providers to make this happen,” he said. “A telemedicine program, located within the practice, could enable this specialized service to be provided in a convenient, coordinated setting.”
On Twitter @legal_med
The patient, a 10-year-old girl, was exhibiting defiant and angry behavior at home. Her pediatrician in rural Vermont was not able to support the family optimally, so he referred her to Dr. David C. Rettew.
Dr. Rettew soon learned that the girl blamed herself for her father’s absence, and she interpreted efforts by her mother to set limits as evidence that her mom didn’t love her.
“During the course of the interview, it became clear that the girl had some specific thoughts that were likely fueling her anger,” said Dr. Rettew, director of the Pediatric Psychiatry Clinic at the University of Vermont, Burlington. “She also met criteria clearly for ADHD, which had never been diagnosed. The consultation recommendations not only included some possible medications to try, but also some specific areas that could be addressed for psychotherapy that could really help the relationship between this child and her mother.”
The successful intervention took place via a secure, two-way videoconference. It is one example of how physicians at the University of Vermont are using telemental health to treat children in underserved areas. As part of a state-funded training program, child psychiatry fellows at the university consult with primary care doctors at federally qualified health centers across the state. The primary care physicians discuss patient cases with fellows via phone or email and can refer patients for in-person or telemental health assessments.
The program has been running for about 5 years and so far has yielded countless benefits, said Dr. Rettew, who directs the university’s Child and Adolescent Psychiatry Fellowship Program. “It helps keep the care housed and centered within the primary care home. That can help coordination of services so that care isn’t fragmented around multiple centers. It also allows evaluations to happen that wouldn’t happen otherwise because it’s too much of a hardship for families to travel long distances and come for regular follow-up appointments.”
University of Vermont physicians also use telemedicine to consult with other mental health clinicians across the state. Child psychiatrist Allison Y. Hall provides in-person training to clinicians and then counsels and supervises their efforts through a telemedicine unit.
“For this purpose, it’s great,” said Dr. Hall, who practices at the Vermont Center for Children, Youth, and Families, which is housed within the university’s psychiatry department. “There’s more confidentiality than Skype, for instance. It’s wonderful to be able to reach clinicians at a great distance.”
On a broader scale, telemental health is a promising tool to address the shortage of mental health providers in the United States, said Dr. Robert C. Gunther, a pediatrician at the University of Virginia Health System in Fishersville. Recent research found that one in three children receiving outpatient care for mental health conditions saw only their primary care doctor for care (Pediatrics. 2015 Nov;136;e1178-85).
“There is a tremendous need for pediatric mental health care,” Dr. Gunther said in an interview. “There is a great shortage of child psychiatrists and other child mental health specialists. Telemental health can help in areas where geography or financial barriers exist to accessing care.”
Data from the Children’s ADHD Telemental Health Treatment Study (CATTS) illustrates the impact that telemental health can have on children facing such barriers to care. Researchers randomized 223 children referred by 88 primary care providers in seven underserved communities into two study groups. Children in the first group were seen by child psychiatrists via videoconference six times over 22 weeks; treatment included pharmacotherapy. Their caregivers received behavior training provided in person by community therapists who were supervised remotely. Children in the second group were treated by their primary care physicians and received one telepsychiatry consult.
Children in both groups improved; however, those randomized to the telemental health model improved “significantly more than patients in the augmented primary care arm” (J Am Acad Child Adolesc Psychiatry. 2015 Apr;54[4]:263-74).
“The CATTS trial demonstrated the effectiveness of a telehealth service model to treat ADHD in communities with limited access to specialty mental health services,” investigators concluded.
But Dr. Joshua J. Alexander, chair of the American Academy of Pediatrics Section on Telehealth Care, notes that some mental health conditions fit more smoothly within the telemental health model than others. ADHD is the most common condition treated by telemental health, he said. The model also has shown success in the treatment of childhood adjustment disorders, anxiety, oppositional defiant disorder, mood disorders, anxiety, and depression.
“I think you have to be careful in determining where telemental health would be beneficial to use and in which cases it might not be an appropriate method to deliver care,” Dr. Alexander said in an interview.
Developing trust and rapport with patients through videoconferencing also can be a challenge, added Dr. Alexander, who is director of the TelAbility telehealth program at the University of North Carolina at Chapel Hill. He recommends that specialists use the technology to continue an existing doctor-patient relationship or to provide care in a consultative model in which the child’s primary care doctor is present along with the patient and patient’s family.
The AAP advocates for the use of telemedicine so long as it is conducted within the context of the medical home. Fragmented telemedicine services that could disrupt continuity of care should be avoided, according to a 2015 AAP policy statement (Pediatrics. 2015 Jun. doi: 10.1542/peds.2015-1253). The academy also calls for the expansion of pediatric telemedicine to increase access to care for underserved communities and improve quality of care for children.
More partnerships between mental health specialists and primary care providers are a key step in delivering high quality pediatric telemental care, Dr. Alexander said.
“Some larger pediatric practices already do this by hiring and colocating individuals at their practice site, but other, smaller practices might not have the room, finances, sufficient patient population, or enough local providers to make this happen,” he said. “A telemedicine program, located within the practice, could enable this specialized service to be provided in a convenient, coordinated setting.”
On Twitter @legal_med
The patient, a 10-year-old girl, was exhibiting defiant and angry behavior at home. Her pediatrician in rural Vermont was not able to support the family optimally, so he referred her to Dr. David C. Rettew.
Dr. Rettew soon learned that the girl blamed herself for her father’s absence, and she interpreted efforts by her mother to set limits as evidence that her mom didn’t love her.
“During the course of the interview, it became clear that the girl had some specific thoughts that were likely fueling her anger,” said Dr. Rettew, director of the Pediatric Psychiatry Clinic at the University of Vermont, Burlington. “She also met criteria clearly for ADHD, which had never been diagnosed. The consultation recommendations not only included some possible medications to try, but also some specific areas that could be addressed for psychotherapy that could really help the relationship between this child and her mother.”
The successful intervention took place via a secure, two-way videoconference. It is one example of how physicians at the University of Vermont are using telemental health to treat children in underserved areas. As part of a state-funded training program, child psychiatry fellows at the university consult with primary care doctors at federally qualified health centers across the state. The primary care physicians discuss patient cases with fellows via phone or email and can refer patients for in-person or telemental health assessments.
The program has been running for about 5 years and so far has yielded countless benefits, said Dr. Rettew, who directs the university’s Child and Adolescent Psychiatry Fellowship Program. “It helps keep the care housed and centered within the primary care home. That can help coordination of services so that care isn’t fragmented around multiple centers. It also allows evaluations to happen that wouldn’t happen otherwise because it’s too much of a hardship for families to travel long distances and come for regular follow-up appointments.”
University of Vermont physicians also use telemedicine to consult with other mental health clinicians across the state. Child psychiatrist Allison Y. Hall provides in-person training to clinicians and then counsels and supervises their efforts through a telemedicine unit.
“For this purpose, it’s great,” said Dr. Hall, who practices at the Vermont Center for Children, Youth, and Families, which is housed within the university’s psychiatry department. “There’s more confidentiality than Skype, for instance. It’s wonderful to be able to reach clinicians at a great distance.”
On a broader scale, telemental health is a promising tool to address the shortage of mental health providers in the United States, said Dr. Robert C. Gunther, a pediatrician at the University of Virginia Health System in Fishersville. Recent research found that one in three children receiving outpatient care for mental health conditions saw only their primary care doctor for care (Pediatrics. 2015 Nov;136;e1178-85).
“There is a tremendous need for pediatric mental health care,” Dr. Gunther said in an interview. “There is a great shortage of child psychiatrists and other child mental health specialists. Telemental health can help in areas where geography or financial barriers exist to accessing care.”
Data from the Children’s ADHD Telemental Health Treatment Study (CATTS) illustrates the impact that telemental health can have on children facing such barriers to care. Researchers randomized 223 children referred by 88 primary care providers in seven underserved communities into two study groups. Children in the first group were seen by child psychiatrists via videoconference six times over 22 weeks; treatment included pharmacotherapy. Their caregivers received behavior training provided in person by community therapists who were supervised remotely. Children in the second group were treated by their primary care physicians and received one telepsychiatry consult.
Children in both groups improved; however, those randomized to the telemental health model improved “significantly more than patients in the augmented primary care arm” (J Am Acad Child Adolesc Psychiatry. 2015 Apr;54[4]:263-74).
“The CATTS trial demonstrated the effectiveness of a telehealth service model to treat ADHD in communities with limited access to specialty mental health services,” investigators concluded.
But Dr. Joshua J. Alexander, chair of the American Academy of Pediatrics Section on Telehealth Care, notes that some mental health conditions fit more smoothly within the telemental health model than others. ADHD is the most common condition treated by telemental health, he said. The model also has shown success in the treatment of childhood adjustment disorders, anxiety, oppositional defiant disorder, mood disorders, anxiety, and depression.
“I think you have to be careful in determining where telemental health would be beneficial to use and in which cases it might not be an appropriate method to deliver care,” Dr. Alexander said in an interview.
Developing trust and rapport with patients through videoconferencing also can be a challenge, added Dr. Alexander, who is director of the TelAbility telehealth program at the University of North Carolina at Chapel Hill. He recommends that specialists use the technology to continue an existing doctor-patient relationship or to provide care in a consultative model in which the child’s primary care doctor is present along with the patient and patient’s family.
The AAP advocates for the use of telemedicine so long as it is conducted within the context of the medical home. Fragmented telemedicine services that could disrupt continuity of care should be avoided, according to a 2015 AAP policy statement (Pediatrics. 2015 Jun. doi: 10.1542/peds.2015-1253). The academy also calls for the expansion of pediatric telemedicine to increase access to care for underserved communities and improve quality of care for children.
More partnerships between mental health specialists and primary care providers are a key step in delivering high quality pediatric telemental care, Dr. Alexander said.
“Some larger pediatric practices already do this by hiring and colocating individuals at their practice site, but other, smaller practices might not have the room, finances, sufficient patient population, or enough local providers to make this happen,” he said. “A telemedicine program, located within the practice, could enable this specialized service to be provided in a convenient, coordinated setting.”
On Twitter @legal_med
Study: Pay One Malpractice Claim, Expect Second
If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
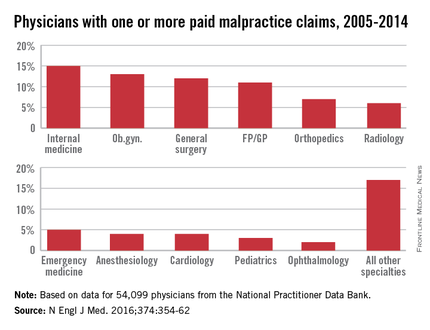
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”
If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
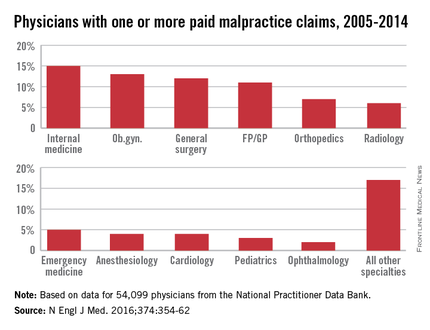
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”
If you pay a medical malpractice claim once, chances are you’ll pay a second claim in the future, according to a study published Jan. 28 in the New England Journal of Medicine (doi: 10.1056/NEJMsa1506137).
David M. Studdert Sc.D., of Stanford (Calif.) University and his colleagues analyzed 66,426 malpractice claims from the National Practitioner Data Bank that were paid against 54,099 physicians between 2005 through 2014. Investigators calculated the cumulative distribution of paid claims in two physician populations: U.S. doctors with one or more paid claims and all active U.S. physicians.
Of all paid claims, 82% involved male physicians. The specialists with the most paid claims were internists (15%), ob.gyns. (13%), general surgeons (12%), and family physicians (11%). Only 3% of the lawsuits were paid through trial verdicts. The remaining claims were paid by out-of-court settlements. The mean payment amount for claims was $371,054, while the median was $204,750.
When using all 915,564 active U.S. physicians as a denominator, only 6% of physicians had a paid claim against them and about 1% had at least two paid claims against them. When looking at physicians with at least one paid claim, 84% had only one paid claim over the study period, accounting for 68% of all paid claims. However, 16% (8,846 physicians) had at least two paid claims, accounting for 32% of all claims. A total of 4% of doctors (2,160 physicians) had at least three paid claims and accounted for 12% of all claims, and 1% (722 physicians) had at least four paid claims and accounted for 5% of all claims.
Specialties had a marked impact on the risk of future paid claims. Compared with internists, the risk of recurrence was double among neurosurgeons, orthopedic surgeons, general surgeons, plastic surgeons, and ob.gyns. Psychiatrists and pediatricians had the lowest risks of recurrence.
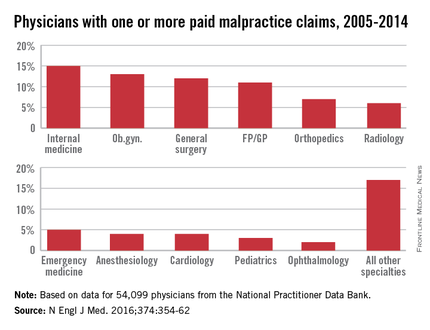
Mr. Studdert said that the investigators were surprised to learn the degree to which past paid claims predicted future claims.
“I think if you ask most people who work in the liability insurance industry, they would tell you that’s probably true,” he said in an interview. “But I don’ t think we’ve seen – at least not on this scale – research finding just how sharply claim risk rises with malpractice history. It does suggest for those multiclaim physicians, that there is something going on that is predisposing them to be the subject of malpractice litigation.”
He noted the analysis suggests that it is feasible to predict which physicians are at higher risk for future claims. The information could then be used to develop interventions to address malpractice claims.
“These multiclaim physicians do appear to have some distinctive characteristics, and that gives us some optimism that it might be possible to predict who is going to [become] a multiclaim physician,” Mr. Studdert said. “More work is needed to make sure that’s technically feasible, but if it is, that opens up a lot of possibilities for liability insurers, hospitals ,medical boards, and other regulators to use this information proactively rather than just reacting to events after they happen.”































